

Winter Preparedness
Featuring a Report on Supporting the NHS
“Cold weather can worsen inflammatory skin conditions such as eczema, psoriasis and acne.”
Dr Tina Tian, Consultant Dermatologist & British Skin Foundation spokesperson Page 02

“ARI hubs help the NHS to cope with seasonal surges in respiratory illnesses
Rory Deighton, Acute and Community Care Director, NHS Confederation Page 12


Transforming respiratory care for patients, moving beyond symptom control to disease modification, remission and, one day, cure.


WRITTEN BY
Dr Tina Tian Consultant Dermatologist & British Skin
Top winter skin tips from a dermatologist
Winter can strip skin of moisture fast and worsen skin conditions. Discover a dermatologist’s tips for smooth, healthy and hydrated skin throughout the season.

Cold, wind and central heating dry skin fast — here are simple expert tips to keep it comfortable, hydrated and healthy all winter.
Keep showers short and warm
Avoid long, hot baths and showers — they strip away natural oils and worsen dryness. Keep water lukewarm and bathing to under 10 minutes. Apply cream straight after washing while skin is still damp to lock in moisture.
Switch to richer moisturisers
Winter calls for creams or ointments that lock in water more effectively than lotions. Look for barriersupporting ingredients such as ceramides and humectants like glycerine. Niacinamide can help calm irritation and strengthen the skin barrier.
Gentle cleansing for face and body
Choose a fragrance-free, moisturising cleanser for the face. For the body, use any moisturiser containing emulsifiers such as cetyl or stearyl alcohol as a gentle wash for very dry skin. If skin feels tight after cleansing, your water is too hot or the cleanser is too harsh.
Don’t overheat indoors
Central heating lowers indoor humidity and accelerates water loss
from skin. Keep room temperatures comfortable and avoid sitting close to radiators or open fires. Consider using a humidifier in bedrooms overnight. If you have rosacea, temperature changes between indoors and outdoors can aggravate flushing — another reason to keep indoors cooler.
Daily SPF still matters
Even in winter, UVA can damage collagen and speed up photoaging, or skin damage caused by sunlight. Use SPF 30+ with minimum 4-star UVA protection on exposed areas, especially if you spend time outdoors.
When conditions flare
Cold weather can worsen inflammatory skin conditions such as eczema, psoriasis and acne. You may need to increase moisturisation and non-irritating treatments like topical steroids, while reducing irritating actives such as retinoids.
Skiing or mountain trips
UV increases by 10–12% per 1,000 metres of altitude, and snow reflects up to 80% of rays. At 1800m, UV doubles. Apply two layers of SPF 50+ first thing, reapply frequently and don’t forget sunscreen lip balm. Winter skin needs extra care. Short warm washes, richer moisturisers and daily SPF deliver healthy skin all season.
Project Manager: Yasmin Meads yasmin.meads@mediaplanet.com
Manager: Isobel Devine isobel.devine@mediaplanet.com
Rachelle Ong | Paid Media Strategist: Jonni Asfaha | All images supplied by Getty Images, unless
Winter is the season to restore and futureproof your skin
Cold weather, wind and indoor heating can leave skin feeling dry, tight and more reactive. Yet, winter also provides one of the most effective opportunities to strengthen and restore it.
With less ultraviolet exposure, this season allows for treatments that not only improve how skin looks, but also how it functions and ages over time.
Dermatology technology and resurfacing lasers
Modern dermatology increasingly views laser technology as part of long-term skin wellness rather than simple aesthetic correction. When used appropriately, lasers can even out tone, fade sun spots and smooth fine lines while stimulating the deeper layers of the skin to produce fresh collagen and elastin. Over time, this supports the barrier, improves texture and helps slow visible ageing, making it one of the most versatile tools in preventive dermatology.
Resurfacing lasers, in particular, offer wider health benefits. Research shows they can clear areas of sun damage, known as actinic keratoses, which are precancerous changes linked to cumulative ultraviolet exposure. By removing these early lesions, resurfacing may reduce the likelihood of them developing into common forms of skin cancer.
This dual action makes laser

treatments uniquely valuable, combining medical prevention with rejuvenation and contributing to both skin health and confidence.
Holistic skincare and foundations for lasting radiance
Professional treatments achieve the best results when supported by consistent daily care. Hydrating creams containing ceramides, glycerin and fatty acids help restore the skin barrier, while daily sunscreen use remains essential even in winter months. A balanced diet rich in antioxidants, adequate sleep and effective stress management all contribute to repair and resilience. These habits provide the foundation that allows professional treatments to deliver long-lasting results. Winter is an opportunity to reset. It allows time to address existing concerns, repair damage and strengthen the skin ahead of sunnier months. By using this season to restore, protect and invest in skin health, it becomes possible to maintain strength and radiance throughout the year and to view skincare as part of a broader approach to wellbeing, longevity and preventive medicine.

WRITTEN BY Dr Anjali Mahto Consultant Dermatologist and Founder, Self Londony

Why caring for your scalp matters as the winter months approach
Consultant dermatologist explains the importance of incorporating scalp care into your daily skin routine, highlighting a tried-and-tested product range designed to protect the scalp throughout the winter season and beyond.

Dandruff is a topic people may be hesitant to discuss. Yet, half of us will experience it at some point in our lives. Despite affecting around 50% of the global population, the condition still carries an unnecessary stigma. Dr Sharon Wong, consultant dermatologist of over 15 years, has seen an increase in dandruff cases in her clinic over the years.
Scalp care is the new skincare “The scalp is an important extension of the skin, and yet scalp care is regularly forgotten,” explains Dr Wong. “Where skincare is often seen as an essential daily routine, very few people think of scalp care in the same way.” With winter just around the corner, it’s time to start paying attention to proactive scalp management.
Preparing the scalp for winter
Colder temperatures, central heating and a reduction in sunlight can all disrupt the scalp’s natural balance, resulting in dryness, itching and flare-ups of dandruff. “Many people come into the clinic during winter, with it being one of the scalp’s toughest seasons,” explains Dr Wong. “Less sunlight in winter can reduce vitamin D levels, which can exacerbate scalp conditions.”
Vichy has been pioneering skin and scalp health for many years, and its Dercos anti-dandruff shampoo is widely recommended in the UK. Bridging the gap between dermatological science and everyday scalp care, Dercos was formulated to help eliminate up to 100% of visible flakes1 from the first wash and provide up to six weeks2 of anti-dandruff relapse
Paid for by Vichy Dercos
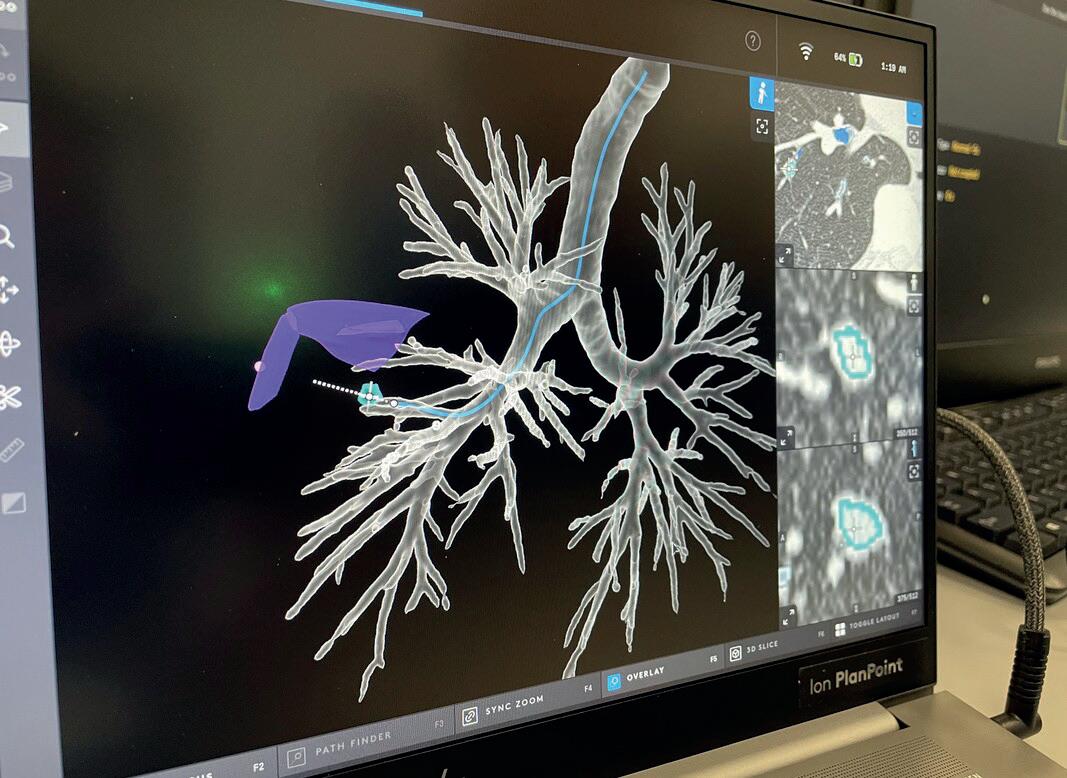
Why new robot technology is a huge advance
for early lung cancer detection

protection. “These are products I have used for years in clinical practice. I’ve seen, firsthand, the benefits for so many people,” explains Dr Wong. “Selenium disulphide, salicylic acid and ceramides are key ingredients that strengthen the scalp barrier and reduce flaking.”
More than just a one-stop solution, Dr Wong encourages a long-term approach to scalp health, supporting both recovery and prevention. “Even when your scalp looks clear, maintenance care once a week helps rebalance the microbiome and prevent relapse,” she advises.
Democratising scalp health
Vichy’s mission is to leverage cosmetic dermatology to deliver effective solutions, empowering everyone to optimise their scalp’s wellbeing throughout every stage of life. “Our goal is to democratise scalp health and make dermatologist-led solutions accessible to everyone,” adds Dr Wong.
Beyond innovation, Vichy is dedicated to upskilling healthcare professionals on the latest research in scalp health, supporting the effective management of conditions like dandruff and seborrheic dermatitis and improving self-misdiagnosis of scalp conditions.
References:
1. Findings based on a consumer test on 262 subjects after two weeks of regular use
2. Findings based on a clinical study on 32 subjects after four weeks of use and six weeks of remanence


Worrying about a persistent cough? Early lung cancer detection is vital for better outcomes and diagnostic technology has advanced greatly.
Winter is the season for coughs and colds, the vast majority of which are due to viral infections. However, if a cough persists for more than four weeks, don’t ignore it. See your GP and, ideally, ask for a chest X-ray, says Professor Pallav Shah, consultant physician in respiratory medicine at Royal Brompton Hospital, part of Guy’s and St Thomas’ NHS Foundation Trust.
Targeted screening for those at increased risk
Professor Shah stresses that, if tumours are discovered in the lungs, the earlier treatment starts, the more successful the outcome is likely to be.
“Thankfully, the UK has one of the best lung cancer screening programmes in the world,” comments Professor Shah. “It’s picking up people who are at increased risk of the disease before symptoms appear. And it’s making a real difference because the reality is, early lung cancer doesn’t present with any signs or symptoms. By the time red flag symptoms do present — including a cough, phlegm, coughing up blood, pain and difficulty swallowing — tumours will be much bigger and have had the potential to spread.” Known as a targeted lung health check, the programme is available on the NHS to current and former smokers, aged 55-74.
Breakthrough diagnostic technology for lung cancer
The UK is also home to some of the best diagnostic innovations worldwide. Since 2023, Royal Brompton Hospital has been trialling new robotic technology, the Ion Endoluminal System, an innovative robotic device from technology company Intuitive, which enters the airways orally and can find and sample lung nodules that are hard to reach and as small as four millimetres.
This isn’t possible with a traditional bronchoscopy, says Professor Shah, who calls the pioneering tech a breakthrough for patient outcomes because it can detect early-stage cancer precisely. Furthermore, where suspicious nodules are found, they can be ablated during the same procedure using a new microwave catheter technology — a type of ablation tool called the MicroBlate Flex, from UK company Creo.
Oncology is an area that’s constantly innovating. “At Royal Brompton, we’ve developed around five technologies which have gone from conception and trials through to global standards,” says Professor Shah. “For example, 20 years ago, we introduced endobronchial ultrasound (EBUS) to sample glands in the lungs, now used globally as the standard of care for diagnosing lymph node abnormalities and the staging of lung cancer. We tend to see important innovation leaps every five to 10 years. Another advantage of this latest diagnostic robotic technology is, it will facilitate other innovations to benefit patients in the years ahead.”
INTERVIEW WITH Dr Sharon Wong Consultant Dermatologist, Hair & Scalp Expert
WRITTEN BY Bethany Cooper
To discover more about their Anti-Dandruff range, scan the QR Code
Image provided by Vichy Dercos
INTERVIEW WITH Professor Pallav Shah Consultant Physician in Respiratory Medicine, Royal Brompton Hospital
WRITTEN BY Tony Greenway
Find out more at gstspecialistcare. co.uk. Paid for by Royal Brompton
Image provided by Royal Brompton
Winter-ready NHS: transforming respiratory care
Respiratory health is a significant driver of NHS admissions. Dr George Godfrey shares strategies to help reduce exacerbations, improve patient quality of life and relieve the burden on the NHS this winter.


Dr George Godfrey, Head of Medical for Respiratory and Immunology at AstraZeneca UK, talks about how their NHS partnerships help to identify and better manage people with respiratory conditions, relieving pressures on healthcare systems and supporting NHS winter resilience.
Burden of asthma and COPD on patients and the NHS
With winter just around the corner, the NHS is bracing again for a seasonal surge in respiratory illness. Asthma + Lung UK reports that breathing issues are the leading cause of emergency hospital admissions, accounting for a staggering 1.7 million admissions last year 1 and that people with Chronic Obstructive Pulmonary Disease (COPD) who are living in severe material deprivation have a higher number of exacerbations, or situations when symptoms suddenly worsen.2 During the colder months of December, January and February, hospital admissions rise significantly, as conditions such as COPD and asthma are exacerbated by cold weather, viral infections and other seasonal triggers.
“Respiratory disease is a major driver of winter pressures,” explains Dr Godfrey. “Every winter we hear the same stories — ambulances queuing up outside hospitals, elective procedures postponed and wards stretched to capacity — and yet respiratory health still isn’t being prioritised as strongly as it should be.”
Despite decades of innovation, the UK continues to face some of the poorest respiratory outcomes in Western Europe.
Asthma and COPD place an enormous strain on both patients and the NHS. Care is often reactive – focused on crises – rather than proactive and preventative, meaning people living with these conditions are not receiving the care they need to stay well.
These conditions also have broader impacts on the workforce and the economy. People with asthma and COPD may need to take time off work due to respiratory illness and may be receiving benefits to support living costs due to the impact these conditions can have on daily living. For the NHS, this means reduced workforce capacity, particularly during high-demand periods. Improving respiratory care could therefore generate farreaching benefits, helping to keep people well and in work and strengthening NHS resilience.
Systemic barriers holding back respiratory care
Despite decades of innovation, the UK continues to face some of the poorest respiratory outcomes in Western Europe.3 Barriers such as poor access to diagnosis and care, variation in access to treatment, and slow implementation of new clinical guidelines mean a proportion of people are missing out on the treatment they need to control their disease and live
well.
Take COPD, for example. Since 2024, the level of basic COPD care in the UK has decreased, from 9.4% in 2024 to 8.8% this year.4
Peter, 74, has received these basics of care, and has been able to remain as active, independent and healthy as possible since being diagnosed with COPD in his 40s. His story, detailed in the Speak Up for COPD coalition’s report5, highlights the importance of proactive patient management. Expanding access to diagnostics, conducting annual inhaler reviews and assessing risk of both lung and heart events are just a few simple measures that can be used to improve care for people with COPD.
When it comes to asthma, an overreliance on the use of short-acting beta-agonists (SABA), more commonly known as the ‘blue inhaler’, remains a persistent challenge. SABA-only relievers may be effective at relieving symptoms, but don’t address underlying inflammation that underpins asthma, with over-reliance on their use linked to poor asthma control and an increased risk of mortality in some cases.6 While these risks have already been outlined in a safety warning by the Medicines and Healthcare Regulatory Agency (MHRA) published in April, shifting attitudes and behaviours is challenging.6 “Changing entrenched behaviours is hard, and it takes coordinated education and support to shift practice,” says Dr Godfrey.
AstraZeneca, a leading global pharmaceutical company, is working alongside the NHS to ensure that the need to act now to improve lung health is seen as urgent and that focus is placed on national and local changes to improve care and access to treatment. Looking at the Government’s 10-Year Health Plan, the need to transform asthma care is acknowledged, but as Dr Godfrey notes, “For conditions with such a significant burden on people, the NHS, the planet and the economy, we now need to turbocharge efforts to deliver on this ambition. Everything the Government can do to improve respiratory care and outcomes will make a real difference.”
Accelerating guideline-directed medical therapy
A winter-ready NHS means delivering the right care at the right time: proactive review for people living with asthma and COPD, especially after a recent emergency or hospital admission, ensuring people with these conditions are on the right treatment, in line with national and local guidelines
“The recently updated BTS/NICE/SIGN asthma guideline sees a major shift from prescribing SABA-only inhalers to combination inhalers as standard, which both relieve symptoms and prevent underlying inflammation,” explains Dr Godfrey.
“There are also a number of biologics available for people with severe asthma, however, access remains uneven due to variations in local service provision.”
Through ongoing partnership with the NHS,
INTERVIEW WITH Dr George Godfrey Head of Medical Respiratory & Immunology, AstraZeneca UK
WRITTEN BY Bethany Cooper
Article created and funded by AstraZeneca
Chronic Respiratory Conditions in the UK

AstraZeneca is supporting the adoption of these guidelines to transform asthma care. This includes scaling a quality improvement programme in asthma7,8, which addresses overreliance on SABAonly inhalers, and the roll-out of a tool which helps primary care teams identify people with severe asthma who need specialist review and could be eligible for biologic treatment. An evaluation of the programme showed that, use of this tool combined with other operational changes, revealed positive results, showing a significant reduction in both asthma-related exacerbations and hospital admissions.9 These initiatives are generating evidence on the impact for patients, the NHS and the planet. With the Government and NHS seeking to deliver new models of care and improve access to innovative medicines, national guidelines in place and the tools available to improve care, respiratory can be the national examplar for 10-Year Health Plan implementation. Dr Godfrey notes, “We’re incredibly motivated to support the NHS to drive this change, but for these improvements to be sustainable, the NHS and local systems need to own these changes and embed them at scale.”
Winter resilience and beyond: better control, fewer admissions
Ahead of this year’s winter surge, the NHS has been asked to identify patients at high risk of admission and to put in place plans to support their urgent care needs at home or in the community, whenever possible.
A joint working project between AstraZeneca and Hartlepool called LOGIC, which was nominated for a Nursing Times Award, demonstrates the importance of this approach. Of the 252 COPD patients

reviewed over the project duration, there was a 60% improvement in the number of people with a COPD care plan, and 71% of people reviewed saw an improvement in their quality of life and symptoms.10
A proactive, risk-based approach to reviews, medicine optimisation and discharge planning enables early intervention and a shift from reactive care to prevention, improving outcomes and reducing hospital admissions. “We have the evidence, tools and treatments to change clinical practice”, says Dr Godfrey.
Winter resilience starts with respiratory care: identify risk, optimise treatment and cut avoidable admissions so people with asthma and COPD can breathe better and pressure on the NHS is eased.
References:
1. Asthma + Lung UK (2024). Breathing issues are the leading cause of all emergency admissions.
2. Asthma + Lung UK (2022). Delayed diagnosis and unequal care.
3. Asthma + Lung UK (2022). Lung conditions kill more people in the UK than anywhere in Western Europe.
4. Asthma + Lung UK (2025). Life with a lung condition 2025.
5. Speak Up for COPD (2024). The state of COPD in the UK.
6. MHRA (2025). Patients with asthma reminded of the increased risk of severe asthma attacks from overusing blue inhalers.
7. AstraZeneca (2023). Executive summary of The SENTINEL Project.
8. AstraZeneca (2025). Executive summary outputs of SENTINEL Plus SABA reduction project.
9. Damery, S et al. (2024). Mixed-methods evaluation of an enhanced asthma biologics clinical pathway in the West Midlands UK. Npj Primary Care Respiratory Medicine.
10. AstraZeneca UK (2024). Breathing New Life.
11. NHS England. Respiratory disease.
12. Nuffield Trust (2024). NHS hospital care: who is waiting and what are they waiting for?
13. The King’s Fund (2023). How does the NHS compare to the health care systems of other countries?
14. Asthma + Lung UK (2024). ‘Asthma care is in crisis’ – charity sounds the siren as asthma death toll rises.
15. NHS England. Delivering high quality, low carbon respiratory care.
Purpose-led Partnerships: Transforming healthcare and advancing practice change
GB-72324
DOP: 15th of December

Protect Your Lungs This Winter
If you have a lung condition, like asthma, chronic obstructive pulmonary disease (COPD) or bronchiectasis, your risk of ending up in A&E doubles during winter 1
Cold weather and viruses can make symptoms such as breathlessness, wheezing and coughing worse by causing irritation and the airways to narrow, and can increase mucus production. However, there are measures to protect yourself, says Dr Andrew Whittamore, Clinical Lead at Asthma + Lung UK.
Protect your lungs this winter
To help protect your lungs in cold weather, try breathing in through your nose when outside to warm up the air or wearing a mask or loosely wrapping a scarf around your nose and mouth if it’s comfortable. Wearing thermal underwear or layers of thinner clothing instead of one thick layer can keep you warmer too.
The best way to boost virus protection is to have your winter vaccines if you’re eligible.
Indoors, heat your home to at least 18 degrees, use blankets and hot water bottles to stay warm, close bedroom windows at night and use draft excluders or blockers to try and reduce the amount of cold air. It’s also a good idea to have regular
hot drinks and stay inside if it’s too cold or windy.
To protect against viruses like colds, flu, pneumonia and Covid, avoid being around people you know are unwell. Stay away from crowded indoor places and wash your hands regularly. If you do get sick, keep an eye on your symptoms, and if they get worse, make an urgent appointment to see your GP or specialist.
Prevention can boost virus protection
The best way to boost virus protection is to have your winter vaccines if you’re eligible, which include flu and pneumonia vaccines. Flu can be a serious illness, especially if you’re living with a lung condition, and the vaccine reduces your risk of hospital admission.
The pneumonia vaccine protects against serious pneumococcal infections and is recommended if you have certain lung conditions. You should also be offered one if you’re over 65.
However, most importantly, whatever your winter triggers may be, use your preventer inhaler as prescribed and carry your reliever inhaler wherever you go, and make an urgent appointment to see your GP, specialist or asthma nurse if your symptoms are getting worse.
References: 1. In 2022/23, there were 332,396 emergency respiratory admissions in winter (December-March) which was 2.1x of the 156,106 emergency respiratory admissions in summer (June-August) in England (NHS England monthly hospital admissions request).
Winter is coming: how to protect against respiratory illnesses this season

Winter can be a magical time. But for many, it’s a time of worry, especially about their respiratory health.
More than one in five people in the UK will need treatment for asthma, chronic obstructive pulmonary disease (COPD) and pneumonia in their lifetime.1 During the winter months, hospital admissions for respiratory infections double, and we’re all at risk. Respiratory illness is distressing for patients and their families and puts immense pressure on the NHS.
Ways to prevent respiratory diseases
The British Thoracic Society (BTS) is committed to supporting respiratory healthcare professionals to care for people with lung disease and preventing as much ill health as possible.
1. Tobacco dependency support
Stopping smoking can improve someone’s health, no matter how long they’ve smoked. Healthcare professionals should offer support to all patients who smoke, and tobacco dependency services should be freely available.
2. Small steps to prevent illness
Individuals with respiratory diseases should practice good hand hygiene, wear a mask in crowded areas and stay warm on colder days. Keeping up to date with flu and COVID-19 vaccinations is essential and effective.
3. Access to early diagnosis and treatment
An early diagnosis helps to receive the correct treatment, reducing the risk of disease progression and the impact of winter. If respiratory specialists can access the right tests to diagnose and treat people with a lung condition, then patients will experience fewer symptoms and are less likely to need hospital admission.
4. Regular reviews of treatment plans
People with chronic respiratory disease should have yearly reviews to ensure they are receiving the right treatment, are taking medicines and inhalers correctly and know what to do if they become unwell.
5. Support for patients to leave the hospital as soon as they are able Supported care at home, delivered by Hospital at Home teams and via Virtual Wards, can help people avoid extended hospital stays. They provide care at home at a time of vulnerability and worry.
With proper diagnostics, good planning and preventive measures, the burden of respiratory infections and NHS winter pressures can be eased and avoided. BTS will continue to work with NHS leaders to support clinicians and patients over the winter period.
Reference:
1. NHS England. Respiratory Disease. Retrieved from: https://www.england.nhs.uk/ourwork/ clinical-policy/respiratory-disease/


WRITTEN BY Dr Andrew Whittamore
Clinical Lead, Asthma + Lung UK
WRITTEN BY Professor Richard Russell Chair of the Board of Trustees, British Thoracic Society
Tips for dry skin and psoriasis flare-up prevention in winter
For many people living with psoriasis, the colder air and lack of sunlight during wintertime can result in a change in symptoms, such as drier skin and irritation.
No one should feel like they must struggle through the winter months. There are ways to help manage your psoriasis.
Lock in winter hydration
Staying hydrated is key; drinking plenty of water is just as important in the winter as it is in the summer. Switching your everyday lotion to a thicker emollient or ointment can help to lock in that moisture in the skin for longer. Avoid using scented products that may irritate the skin.
In addition to changing your lotion, it may be helpful to replace your shower gel or soap with an emollient wash, as these are typically more moisturising and fragrance-free. It also helps to shower in warm, rather than hot, water to help prevent excessive dryness.
Wear the right clothes and pyjamas for winter Try to opt for soft materials such as cotton or silk. If you would like to wear a jumper, consider wearing a layer underneath to protect your skin from irritation.
The drying effects of central heating can be unpleasant for psoriasis, so it may help to have a humidifier while you sleep to add moisture back into the air. Placing a bowl of water near radiators can help with this, too.
Finding treatment, triggers and protection
If you are struggling with your psoriasis during winter, speak to your GP or dermatologist about changing your treatment plan to help manage your psoriasis. This could include changing the dose of your medication or moving you on to a stronger treatment for a while.
The festive period can be a busy time that disrupts your usual routine, which may lead to a flare-up. To help, consider setting an alarm as a reminder to apply or take your treatment, and stay mindful of potential triggers such as alcohol or certain foods.
Finally, we urge anyone who is on immunosuppressant medication for their psoriasis to have their flu jab and Covid-19 vaccination to protect against any other illnesses over the winter months.

How a quick ‘early warning’ test could help prevent asthma flare-ups this winter
A quick breath test, which checks for inflammation in the airways, is a positive step for asthma diagnosis — while also preventing flare-ups for those already on medication.
Winter can be a difficult season for asthma sufferers, with triggers of flare-ups including cold, dry air, plus cold and flu viruses. Typical symptoms include breathlessness, coughing, wheezing and chest tightness.
Difficult nature of asthma diagnosis
Traditionally, asthma diagnosis has been made on symptoms and lung function tests. However, accessibility to these test centres can be really reduced, so patients may face delays in getting treatment. Additionally, symptoms alone can make asthma difficult to diagnose and treat, as they can vary over time and in intensity.1
Meanwhile, people who already have asthma might feel fine and believe they’re managing it, whether they’re taking their regular medication or not. They might not realise that inflammation is building in their airways, which can make asthma symptoms worse over time.2
Checking for inflammation in asthma
However, a quick and simple breath test called a FeNO test is available at GP practices and clinics across the country and has been called a “game-changer” for asthma care.3 It can help to manage asthma better, lower the risk of asthma attacks or hospital visits, and improve quality of life.1,4
FeNO testing measures inflammation in the airways, helping doctors diagnose asthma and get patients onto the right treatment sooner.1 For patients with asthma, it can offer reassurance that treatment is working, reinforce taking medication, or show if a different management approach is needed.1 It’s simple — a gentle 10-second breath is all that’s required, so it’s suitable for children and results are immediate.1
“If you suspect you have asthma — or even have asthma — then talk to your doctor about FeNO testing,” says Dr Sermed Mezher, GP and Online Educator. “It might help in the management of your asthma, or potentially in figuring out what the likelihood is that (asthma is) the explanation for your symptoms.”
References:
1. Loewenthal L et al. Semin Respir Crit Care Med. 2022;43:635-645 2. Meulmeester F et al. The Lancet Respiratory Medicine. 2025; 13(6):505-516. 3. Bonini M et al. Multidisciplinary Respiratory Medicine. 2025;20(2025):1-8.
4. NHS England. Fractional Exhaled Nitric Oxide (FeNO). NHS.UK.

WRITTEN BY Tony

Weathering the cold while managing chronic
pain
Cold weather and seasonal infections can create trouble for people living with chronic pain. Explore evidence-based tips and lifestyle strategies to help minimise pain this season.
Studies show that drops in temperature and changing barometric pressure are associated with increased pain, stiffness and activity limitations in conditions like osteoarthritis, fibromyalgia and other chronic musculoskeletal syndromes,1 all linked to chronic pain.
Winter also brings higher risks of respiratory and systemic infections (influenza, RSV, SARSCoV-2), which can trigger inflammation, pain flares or prolonged musculoskeletal symptoms — case series document post-infectious arthralgia and inflammatory arthritis after viral infections, including COVID-19. Therefore, minimising exposure helps reduce pain exacerbations2.
Evidence-based winter preparedness tips
Evidence-based winter preparedness includes vaccination (influenza, pneumococcus, seasonal boosters). Older adults may benefit from enhanced formulations. Vaccination lowers infection risk and downstream pain flares. Medication continuity is essential: keep analgesics and disease-modifying treatments updated. Also, confirm your treatment plans with clinicians before winter. Infectioncontrol measures — hand hygiene, avoiding crowded, poorly ventilated spaces during peaks3 — remain simple but effective. Immunocompromised adults may be affected harder by influenza4 and consequently be exposed to more pain flares.
Practical steps to minimise pain
Lifestyle strategies also matter. Layer clothing, use local heat (warm baths, packs) to ease stiffness and maintain gentle activity to preserve mobility. Prioritise sleep and hydration. Avoid excessive alcohol, which creates a false sense of warmth, lowers core temperature and raises hypothermia risk5. Choose warm non-alcoholic drinks and stay active to generate internal heat. Plan for assistance with errands during severe weather to avoid falls or overexertion. Check batteries and the condition of assistive devices before winter1
If a person living with chronic pain notices unusual worsening of pain after an infection, new joint swelling or prolonged symptoms, they should contact their healthcare provider. Early assessment can distinguish a transient flare from an inflammatory process that needs treatment. Being proactive about vaccination, infection avoidance, medication continuity and sensible winter self-care reduces risk and helps people with chronic pain stay safer and more comfortable through the season. In this way, weathering the cold becomes easier, with pain kept at low and manageable levels.
References:
1. Jevotovsky, D.S. et al. Weathering the Pain: Ambient Temperature’s Role in Chronic Pain Syndromes. Curr Pain Headache Rep 29, 31 (2025). https://doi.org/10.1007/ s11916-025-01361-8
2. Yadav S, et al. Inflammatory Arthritis After COVID-19: A Case Series. Am J Case Rep. 2023 Jun 27;24:e939870. DOI: 10.12659/AJCR.939870
3. Grohskopf LA, et al. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2025–26 Influenza Season. MMWR Morb Mortal Wkly Rep 2025;74:500–507. DOI: http://dx.doi.org/10.15585/mmwr.mm7432a2
4. Collins JP, et al. Outcomes of Immunocompromised Adults Hospitalized With Laboratory-confirmed Influenza in the United States, 2011-2015. Clin Infect Dis. 2020 May 6;70(10):2121-2130. doi: 10.1093/cid/ciz638
5. Health Service Executive. HSE. (2025). Keeping warm in winter. Available at: https:// www2.hse.ie/living-well/winter/keeping-warm-in-winter/

INTERVIEW WITH Dr Sermed Mezher GP and Online Educator
Greenway
WRITTEN BY Nadia Malliou President, Pain Alliance Europe
WRITTEN BY Georgia Sewell Digital Communications Officer, Psoriasis Association
Weather forecast can predict daily pain levels for millions

Science now proves a popular folklore correct – winter weather can make our joints feel more painful, according to Arthritis UK, which is sharing advice on how to manage symptoms
The link between weather and joint pain has long been passed down through the generations.1
Research from the University of Manchester, funded by Arthritis UK, has validated these early suspicions. Its study, ‘Cloudy with a Chance of Pain’,2 recruited more than 13,000 people across the UK to track their symptoms daily in an app linked to local weather conditions. It found that higher humidity, lower pressure and stronger winds — in that order — were significantly associated with increased pain.
Cold weather can make outdoor activities more challenging.
This means typical British winter days that are damp and windy can take a real toll on the 10 million3 of us living with a form of arthritis in the UK.
The report’s authors advised using the weather forecast to help plan activities to take greater control of your life. Here are some other top tips from Arthritis UK to consider this winter.
Take vitamin D
Vitamin D helps maintain bone health and also has antiinflammatory properties. With fewer sunlight hours in the winter months,
we absorb less vitamin D through our skin. To make up for this imbalance, consider taking a daily supplement of 10 micrograms.
Keep your home warm
The NHS advises keeping your home at 18 degrees or above. With the costof-living crisis, this can be a struggle to maintain, but the Government offers subsidised help through Cold Weather Payments, Warm Home Discount and Winter Fuel Payments. Eligibility for these schemes can be assessed on their website.
Stay active
Staying active is important yearround as physical exercise eases pain and increases joint strength and flexibility. Cold weather can make outdoor activities more challenging, so consider low-impact indoor activities such as swimming, yoga and Tai Chi, which are widely recommended for people with arthritis by healthcare professionals.
Warm clothing
Keeping your body warm can ease stiffness in joints. Remember, lots of loose layers of clothing work better at trapping the heat than thicker clothes. If your hands feel chilly, try hand warmers or heated gloves. Wearing a hat will reduce the amount of heat you lose through your head and wearing thicker or two pairs of socks will help keep your feet warm. Some people find products such as compression wear, microwavable slippers or beanbags helpful. References:
et al. (2019). How the weather affects the pain of citizen scientists using a smartphone app. npj Digital Medicine.
3. Arthritis UK. (2025). The State of Musculoskeletal Health 2025.

TikTok to Tai Chi - ways to keep connected
Living with a chronic health condition like arthritis can be challenging any time of the year, but winter can make this especially hard.
British weather is proven to exacerbate symptoms, and we naturally spend more time indoors, which can add to a sense of isolation.
It’s so important not to feel alone
Arthritis UK is a community of people who understand the fluctuating symptoms, fatigue and pain that can come with arthritis.
Long legacy of providing support to people living with arthritis
If you haven’t come across us before, I’d encourage you to take a look. We have a legacy stretching back almost 90 years and are behind some of the greatest advances in arthritis treatment, including anti-TNF medications. We’re now the largest dedicated funder of arthritis research.
But we’re also support groups, a helpline to offer advice and an understanding ear and campaigners working to get the recognition arthritis deserves in health policies across all four nations.
We’re also trying to get the nation talking about arthritis to break the stigma. Last month, we published a report Left Waiting, Left Behind, which included the findings of a survey of almost 8,000 people living with arthritis. It showed we have a long way to go to help people with arthritis live the lives they choose. This was particularly apparent in responses from younger people. Seven in ten (71%) younger adults felt other people didn’t understand the impact arthritis has on their lives.
To this end, we recently joined forces with TikTok to create a new dance challenge, The Arthur Tut, which combines physio moves in a fun way to manage pain as more people move online for health advice. We hope it will begin to tackle the stigma young people face by changing the way people see arthritis — it’s a disease that can affect anyone at any time of life, and not an inevitable part of ageing.

Paid for by Arthritis UK
WRITTEN BY Deborah Alsina MBE Chief Executive, Arthritis UK
How osteoarthritis affects daily life — and ways to manage its effects
Pain management for osteoarthritis — a progressive joint condition — isn’t enough. What’s also needed is a treatment that targets its underlying causes.

Biresh Roy, CEO at AH Consumer Healthcare, which markets FlexiSEQ, outlines the symptoms of osteoarthritis — and how patients can find both pain relief and improved joint mobility.
What is osteoarthritis?
Osteoarthritis is a condition that causes a person’s joints to become inflamed, painful and stiff, and its effects can be exacerbated by cold weather. It can affect any joint, but commonly is found in the knees, hips, shoulders and small joints in the hands. It’s mainly associated with ageing — typical onset is around the age of 55 onwards — but it can affect younger people regularly taking joint impact exercise like running. It’s also linked to obesity and joint trauma.
What’s the impact on the patient and those around them?
It can be extremely debilitating, reducing mobility, affecting a person’s independence and impacting quality of life. If someone can’t go out and stays at home thinking about their pain, particularly in the darker evenings, it can induce a degree of depression. Constant pain can also affect sleep, which causes irritability and begins to impact the people around them.
How common is it?

According to Arthritis UK, there are more than 10 million people in the UK living with arthritis. An estimated nine million of those have osteoarthritis.

What causes it?
With osteoarthritis, the cartilage in the joint — which stops two bone surfaces from rubbing together — begins to wear thin or is worn away completely. Meanwhile, lubricating molecules in the synovial fluid — which bathes the cartilage to make movement even smoother — become depleted. The resulting friction from joint movement can cause pain, even when resting.
What’s the treatment for it?
Unfortunately, there’s no cure because joint deterioration, by its nature, is progressive. Anti-inflammatories and opioids are used to manage pain but only provide temporary relief. What’s needed is a treatment that targets the underlying causes as well as symptoms. The FlexiSEQ range comprises two drug-free gels designed to do just that. Because of their formulations, they’re able to lubricate the joint so that it moves more freely, causing less friction and less pain. We recommend these be used as part of an overall therapy together with lifestyle changes.
What lifestyle changes can help?
Regular non-high impact exercise, such as cycling, walking and swimming and even gardening, can help burn calories and strengthen the muscles around the affected joint. Make sure your diet is rich in omega-3 fatty acids, like salmon. Take ginger and turmeric, which have naturally anti-inflammatory properties. And eat superfoods such as broccoli, which contain calcium, vitamins C and K, and sulforaphane — which can slow down joint deterioration.






INTERVIEW WITH Biresh Roy CEO, AH Consumer
WRITTEN BY Tony Greenway

WRITTEN BY
Dr Jonathan Anderson Executive Director, Medical Affairs, CSL Seqirus
Protecting family during the winter holidays
Seasonal flu costs the UK £644 million annually, but ensuring we reach the most vulnerable with the recommended vaccines could make all the difference.1
In the UK, flu places a significant strain on people and health services every winter.2 As Christmas approaches and the weather cools, indoor gatherings raise the risk of infection.3 While COVID raised awareness of the risks of respiratory illnesses and the ways it transmits among people, many still underestimate the impact of flu.
Keeping healthy this Christmas
As the flu virus is constantly changing, it presents a unique challenge for prevention, requiring continuous global monitoring and annual vaccine strain updates to match circulating influenza strains.4 Every year, the World Health Organization (WHO) meets to recommend which influenza strains should be included in seasonal flu vaccines based on the latest surveillance data.5 For many people, flu can be short-lived, but for those who are at increased risk, such as the elderly, those with chronic health conditions or with weakened immune systems, it can sometimes be severe, leading to complications, hospitalisation or even death.6
It’s important for vulnerable groups to get vaccinated and to adopt behaviours to help stop the spread of germs. Children are notorious super-spreaders, likely to catch and spread flu. Meanwhile, older adults (65 years and older) who are especially vulnerable to the impact of flu have immune systems less capable of staging a strong defence.7

‘Protecting those most at risk of influenza and reducing pressure on the NHS at a busy time of year starts with protecting ourselves and those we care for through vaccination,’ said Jacqueline Walker, Operational Director for Covid-19 and Influenza Vaccination Programmes, NHS England, London.

The colder months bring rising respiratory illness, surges in A&E attendances and greater pressures on beds, staff and services. This year, we’ve prepared more robustly to protect the NHS and keep patients safe — including stress testing months in advance and a huge drive on vaccinations.
We face not just a harder, longer winter, but the dangerous impact of the BMA’s decision to have resident doctors strike over one of the hardest weeks of the year.
Investing in and supporting NHS staff
We’re backing the NHS with real investment and practical support to help cope with increased demand. Take vaccination — one of the most effective tools to prevent avoidable
Healthy habits to prevent the spread of flu
Every eligible person vaccinated against the flu can help slow the spread of the virus and lessen the impact for when families come together for Christmas.8,9 Handwashing, staying home when unwell, avoiding close contact with people who are sick and ventilating indoor gatherings add extra layers of protection, but vaccination remains the most effective measure to prevent severe disease and maintain public health through winter.4
Vaccines matter
The UK has a robust vaccination programme and strong uptake, but continuing momentum matters as Christmas approaches. Getting vaccinated at a local pharmacy or GP typically takes only a short time and is free for many eligible groups, including people aged 65 and over, those with certain long-term conditions and those who are pregnant.
Acting now may lower the chance of cancelling travel, missing work or school plays or postponing Christmas gatherings. Ask your GP or pharmacist for further information.
References:
1. Romanelli, Robert J, et al. 2023. The Societal and Indirect Economic Burden of Seasonal Influenza in the United Kingdom. Rand Health Quarterly.
2. UKHSA. 2025. Influenza in the UK, annual epidemiological report: winter 2024 to 2025, Figure
28. GOV.UK.
3. UKHSA. 2025. Christmas saw anticipated rise in flu, latest UKHSA data shows. GOV.UK.
4. WHO. Global Influenza Programme, Vaccines. WHO.INT.
5. WHO. Global Influenza Programme, Recommendations for influenza vaccine composition. WHO.INT.
6. CDC. 2024. Influenza: People at Increased Risk for Flu Complications. CDC.GOV.
7. National Institute of Health. Influenza in Children. Cold Spring Harbor Laboratory Press.
8. CDC. 2024. Flu and People 65 Years and Older. CDC.GOV.
9. NHS Inform. Flu vaccine.
How strategic investment, support and preparation can help the NHS through winter pressures
By preparing early, increasing capacity, improving patient flow and offering more ways to get the right care at the right time, we’re building a winter-ready NHS.
illness and keep people out of hospital. This autumn, the NHS delivered 16.2 million flu vaccines, 300,000 more than the same time last year. Vaccination reduces the risk of serious illness and frees up capacity across hospitals. It’s a real way to play your part to protect yourself, your loved ones and the NHS.
But vaccination alone isn’t enough, so we’re investing £450 million into urgent and emergency care. This means up to 500 new ambulances by March 2026, the expansion of urgent treatment centres and tougher performance standards that drive improvement and accountability.
We’re also boosting GP access to keep people well and out of hospital. Through advertising campaigns,
new online access routes and more GP practices open for longer hours over the Christmas period, we’re making sure more people can be seen closer to home. When people get early GP help, they’re less likely to end up in A&E.
Despite the BMA deliberately choosing the worst time of year to put more unreasonable strain on the NHS and their colleagues, our priority remains clear: safeguarding patient care and supporting staff on the front line.
With the right investment, preparation and the dedication of NHS staff, people can get the care they need this winter — and lay the foundations for the long-term modernisation it needs.

WRITTEN BY Karin Smyth Minister of State for Health

Discover how hand hygiene initiatives could help save the NHS millions of litres of water every year
Advanced formulae, more scientific evidence and greater accessibility have enabled alcohol-based hand rubs to become a popular choice for both staff and patients – unlocking new opportunities to help the NHS achieve its net zero ambitions.
Supporting sustainable initiatives
Alcohol-based hand rubs are a quick and effective way to maintain good hand hygiene and ensure compliance with hygiene standards across the NHS, from waiting rooms right into the heart of operating theatres. When used correctly, they provide a safe, waterless solution to remove germs.
Reducing water use is important in spaces like operating theatres, where it’s estimated that a traditional surgical hand scrub can use between 18 and 21 litres of water per person.1,2 Conservative estimates suggest the NHS delivers five million surgical procedures a year. If every surgical team were made up of just four people (and it’s often more), that’s 360 million litres of water every year!
As a global leader in water, hygiene and infection prevention solutions, Ecolab sets ambitious Positive Impact goals3, aiming to help its customers save 1.1 trillion litres of water globally each year by 2030.
Traditional surgical hand scrub can use between 18 and 21 litres of water per person.
At a local level, we work with teams across the NHS to provide evidence-based training, educational tools and best-in-class products to support national initiatives like the Intercollegiate Green Theatre Checklist.4 This checklist combines evidence, guidelines and policies to help surgical teams introduce sustainable changes within their own departments. As recommended in the checklist, surgical teams can use alcohol-based hand rubs to help reduce water and energy consumption in their theatres.4
The importance of compliance
Products used within healthcare are highly regulated and rigorously tested to ensure compliance with technical specifications under a system called European Standards. These standards provide manufacturers with specific codes, which demonstrate that a product has passed testing and can claim certain characteristics.
The latest European Standard, EN 17430, assesses the effectiveness of alcohol-based hand rubs on viruses in a practical test using real volunteers. In healthcare settings, where viruses can spread quickly, this new standard helps to ensure that the most effective products are used. Next time you use a hand sanitiser, look for the EN codes! They will be your guarantee of effectiveness and protection.
Engaging staff with sustainable change
Engaging the NHS with sustainable change involves a multidisciplinary approach. Ecolab works with clinicians, procurement, patient groups and facilities to find practical solutions. We provide a total solution for skin and hand hygiene within the operating theatre and beyond, supporting NHS teams to embed compliance, efficacy and sustainability into their education, training and practice.
References:
1. S. F. J. E. Gasson S, “Sustainable Hand Surgery: Incorporating Water Efficiency Into Clinical Practice,” Cureus, vol. 15, no. 4, 2023.
2. A. V. C. S. e. a. Wormer BA, “The green operating room: simple changes to reduce cost and our carbon footprint.,” The American Journal of Surgery, vol. 79, no. 7, pp. 666-71, 2013.
3. Ecolab, “2030 Positive Impact,” 2024. [Online]. Available: https://www.ecolab. com/corporate-responsibility/2030-positive-impact.
4. Intercollegiate Royal Colleges, “Intercollegiate Green Theatre Checklist v2.0,” November 2024. [Online]. Available: https://www.rcsed.ac.uk/policy-guidelines/ sustainability/environmental-sustainability-and-surgery/intercollegiate-greentheatre-checklist.

WRITTEN BY
Clinical Insight
I’ve been a nurse for more than 35 years and I have seen the significant impact climate change has on population health. In my own NHS trusts, I’ve supported the move to reusable surgical gowns, lower carbon inhalers and plastic-free patient wipes. Implementing green projects like the Intercollegiate Green Theatre Checklist can help us to save energy and water, ultimately reducing the carbon impact of care. By working together with our patients, staff and suppliers, we can deliver a more sustainable NHS that will still be here to care for generations to come.

AI won’t make the NHS more efficient unless it learns to listen to every voice
One AI speech technology provider is building engines that capture every voice, highlighting the advantage of diversity in forcing us to build better systems.
Speechmatics’ Senior Director, Paolina White, discusses the importance of ensuring voice AI is designed to handle a wide range of speakers, accents and environments.
What’s possible when voice AI works well, and what’s needed to make it happen?
When voice AI is designed to recognise and accurately capture a wide range of speakers, accents and environments, admin time can be reduced by almost 2-3 hours daily, and patients receive more sympathetic consultations, but solutions must be built to perform under pressure. Models may perform well in controlled labs, but in real conditions, they must contend with noise, accents, interruptions and overlapping conversations between doctors and patients.
Can voice be seen as a “stress test” for NHS AI readiness, and what issues could AI encounter in practice?
Absolutely. When the NHS paused unsafe transcription deployments this year, it highlighted how complex the challenge is. If the speech engine being used to handle AI note-taking or dictation is unable to handle background noise, distinguish near-field from far-field speech or manage fast-switching speakers, the workflow can collapse, leading to frustration and manual intervention. For this reason, we actively engage with leading AI scribe companies to evaluate and refine performance in real-world environments.
Do accents, dialects and multilingual conversations affect performance, and why should AI be able to distinguish multiple voices?
It’s widely recognised that accents and dialects can trip up speech engines, leading to mistranscription of medical terminology, and exposing poor technological foundations. At Speechmatics, we train voice AI on diverse datasets, ensuring the software can accurately separate and tag every voice in the room. Diarisation errors can misattribute statements, and in healthcare, even a single symptom or misattributed allergy can create real clinical risk.
What should NHS trusts consider prior to deployment? NHS trusts must ask for proof of live deployment in real NHS conditions, in noisy wards, with diverse accents and multiple speakers, because compliance accreditation isn’t always reflective of real-world use. Diversity pushes industry to build more inclusive, globally relevant systems. Getting voice technology right means building AI that works for everyone, not creating new layers of inequality.

From emergency care to community care: rethinking winter care pathways
Winter presents a challenge within the NHS urgent and emergency care (UEC) sector. December often marks a greater surge in A&E pressure – largely due to seasonal illnesses.
Reducing pressures across urgent and emergency care pathways is key to bringing down delays in patient care and the harm they cause. With respiratory illness a major driver of A&E attendance and hospital admission, the NHS is continuing to innovate and using acute respiratory infection (ARI) hubs to try to ease these pressures.
A key tool to improve respiratory care
These hubs offer same-day assessment and treatment for flu, Covid-19 and RSV — keeping patients out of overcrowded emergency departments. Their potential is significant: last winter saw flu consume 315,000 bed-days across England’s hospitals.1 Each case that could be managed in the community can add additional pressure to an already strained emergency care system. Moreover, much of this demand doesn’t require hospital attendance or admission. For example, the number of A&E visits for children aged 2–10 since the pandemic is significantly higher, but has not led to a similar need for admissions.2 ARI hubs may help manage this increased demand outside of hospitals.
Gloucestershire and Greater Manchester lead the way
These hubs are helping to revolutionise UEC pathways in different parts of the country. Gloucestershire, for example, cut A&E attendances by 7% between 2022 and 2023 thanks to ARI hubs. That allowed nearly all patients using the hubs to then receive follow-up treatment from their GP, with three-quarters receiving a prescription.3 Similarly, Greater Manchester’s 19 ARI hubs provide over 50,000 appointments in winter, treating thousands of patients who would likely have gone to A&E instead. Again, the vast majority of patients using the hubs were kept out of hospital and treated within primary care settings.
Faster treatment closer to home
ARI hubs help the NHS to cope with seasonal surges in respiratory illnesses by providing faster treatment closer to home and easing A&E demand. As another challenging winter approaches, the NHS should build on the hubs’ success to embed lessons and drive lasting change.
References:
1.
2. Harker, R. et. al. 2025. NHS key statistics: England. The Commons Library.
Driving NHS sustainability through early diagnosis
From earlier diagnosis to more targeted treatment, innovation in diagnostics is reshaping the NHS’s capacity to deliver preventative, sustainable healthcare.
Harnessing technology for earlier detection
Early and accurate diagnosis remains one of the most effective ways to improve patient outcomes and reduce long-term costs for the NHS. HealthTech innovations, from AI-enabled imaging and molecular diagnostics to rapid point-of-care testing, are helping clinicians detect disease earlier and guide treatment more effectively. These advances are not only improving clinical precision but also allowing patients to begin therapy sooner, avoid complications and, in many cases, remain in the community rather than in hospital care.
Building a culture of prevention
The NHS Long Term Plan and the Government’s Life Sciences Vision both highlight prevention as a national priority. Diagnostic technologies play a central role in this transformation. By enabling populationlevel screening, supporting remote monitoring and personalising care pathways, the sector is helping to move healthcare from reactive treatment towards prevention and early intervention.
This shift can also be an important step in reducing health inequalities and supporting more consistent standards of care across the UK. It also helps relieve pressure on NHS services by reducing demand for emergency and inpatient care.
Collaborating to accelerate progress
To unlock the full potential of diagnostic innovation, collaboration between the NHS, academia and industry is crucial, particularly when it comes to implementation. Evidence-based evaluation, shared learning and coordinated procurement processes help ensure that promising technologies are adopted at scale and embedded effectively within clinical pathways. The HealthTech industry continues to work closely with system partners to improve access, build workforce confidence and demonstrate measurable improvements in outcomes and efficiency.
Driving a sustainable future
Paolina White Senior Director, Speechmatics
WRITTEN BY Bethany Cooper
3. One Gloucestershire Improvement Community. Acute Respiratory Infection (ARI) Hubs – a PCN-led model.

WRITTEN BY Rory Deighton Acute and Community Care Director, NHS Confederation
Preventative diagnostics deliver long-term value for patients, the NHS and the wider economy. By embracing technologies that enable earlier detection and proactive care, we can support a more resilient, efficient and sustainable health service. Through continued partnership and investment, the UK can remain at the forefront of global innovation, helping the NHS meet the challenges of today while preparing for those of tomorrow.

WRITTEN BY Ravi Chana Executive Director, Diagnostics, ABHI
Alarilla, A. et. al. 2025. Did the NHS experience record pressures this winter? The Health Foundation.
INTERVIEW WITH
