Cardiovascular Health
Q3 2023 | A promotional supplement distributed on behalf of Mediaplanet, which takes sole responsibility for its content


“The voice of those living with heart disease in Ireland has largely remained disconnected and unorganised.”
David Kelly,
Chair, Heart and Stroke Voice Ireland (HSVI) Page 02
In this 21st century, why do we allow 19 million people worldwide to die prematurely from CVD every year?
Neil Johnson CEO, Croí the West of Ireland Cardiac & Stroke Foundation

Read more on page 9
www.healthnews.ie
“Around 80% of premature heart disease and stroke is preventable through healthy lifestyles.”
Janis Morrissey, Director of Health, Promotion, Irish Heart Foundation Page 05
 © Emilija Jefremova
Trudie Lobban MBE FRCP Founder STARS (Syncope Trust And Refl ex anoxic Seizures), Arrhythmia Alliance
© Emilija Jefremova
Trudie Lobban MBE FRCP Founder STARS (Syncope Trust And Refl ex anoxic Seizures), Arrhythmia Alliance

Take fainting to heart — there is no such thing as a simple faint
Fainting (syncope) affects one in two people at least once during their lifetime. This unexplained loss of consciousness is a common yet overlooked symptom of an underlying, potentially fatal, heart rhythm disorder.
Why the changing role of the patient can improve cardiovascular healthcare
Many people may faint due to low blood pressure, dehydration or heat-related syncope. However, for others, something more serious can be causing the sudden loss of consciousness.
Fainting can be a sign of underlying heart condition
Any unexplained loss of consciousness or fainting should be investigated, and an electrocardiogram (ECG) should be undertaken and analysed by a heart rhythm specialist (electrophysiologist). Fainting should never be ignored as it can be a sign of an underlying, potentially fatal, heart rhythm condition. If you experience syncope that occurs without warning or is preceded by a racing heart rate, consult your GP urgently.
There is no such thing as a simple faint Fainting is sometimes the only symptom before sudden cardiac death. While many arrhythmias (heart rhythm disorders) are nothing to worry about (after all, we all experience palpitations sometimes), others can prove fatal. Long QT and Brugada are arrhythmia syndromes that can present as ‘simple faints’ leading to sudden death.
Sadly, cases could have been easily identified and prevented with a simple ECG and treatment. Both conditions are genetic, so close family members should also be investigated for a history of fainting. Not everyone with Long QT or Brugada experiences fainting episodes — some have no symptoms and die suddenly.
Support for syncope
STARS (Syncope Trust And Reflex anoxic Seizures) is the only organisation providing information and support to people affected by unexplained loss of consciousness. They have a checklist you can download and share with your GP. During initial assessment, your GP will take a history of your condition and conduct a physical examination, including a blood pressure reading and standard ECG. The Blackouts Checklist, developed under the guidance of STARS’ expert Medical Advisory Committee, will help you prepare for your appointments and equip you with the right questions.
Taking charge of your diagnosis
Unexplained loss of consciousness is traumatic; however, there are ways to manage your condition. Consult your doctor for self-care measures to help manage vasovagal syncope and postural tachycardia syndrome (PoTS), such as isometric counterpressure exercises, compression garments and trigger avoidance.
Additionally, you can join patient-to-patient support groups to learn more about your condition and meet other affected individuals. Get the knowledge to support you throughout your care pathway. If you experience ‘simple faints,’ don’t delay — get checked straight away.
David Kelly Chair, Heart and Stroke Voice Ireland (HSVI)

When it comes to healthcare, the patient should be the central focus of attention. However, in reality, that is not always the case.
Multiple factors contribute to the lack of patient centricity. Among them is the role attributed to the patient in the healthcare ecosystem. Broadly speaking, the healthcare ecosystem is comprised of the key stakeholders, including the policy and decision-makers, payors, system managers and administrators, healthcare professionals — and the patient. Ironically, the weakest link in this lineup is the patient. Every other stakeholder is there by choice, but the patient assumes their role by default when they become ill.
Traditional approach to patient care
Historically, the interaction between key stakeholders and the patient, especially when it came to the actual delivery of care, has been largely autocratic. Notwithstanding individuals who fail to take any responsibility for their own healthcare (for a variety of reasons), typically, patients have been passive recipients of care. They accede to the superior knowledge of the doctor and just accept what they have been told or what has been prescribed.
Evolving patient demands and knowledge
This is changing, however, and there is a new dynamic emerging. Patients and their carers have ever-increased access to information. The rapid advancement of digital technologies is transforming the way patients interact — and will interact — with their healthcare providers. Increased
awareness of rights, stronger expression of preferences and greater demands for choice are fuelling something of a consumer approach to healthcare, which will continue to change the role of the patient.
Increasing patient engagement and support
Exemplars of the more informed and activated patient are seen in the rare disease or cancer communities, for example. Through their networked patient communities, the voice of the patient is being heard on matters ranging from equity of access to highlighting unmet patient needs.
Concepts like ‘patient-centred care’ and ‘patient centricity’ are increasingly called out in health strategies and policies. Despite scepticism in the patient community that this is merely ‘tick boxing,’ there is evidence that ‘patient engagement’ across many areas of healthcare is an emerging reality.
In sharp contrast to most other disease areas, despite the scale and burden of cardiovascular disease, the voice of those living with heart disease in Ireland has largely remained disconnected and unorganised. However, to reverse this, the recent launch of Heart and Stroke Voice Ireland (HSVI) aims to create change in cardiovascular disease patients.
To learn more, visit heartandstrokevoice.ie
02 READ MORE AT HEALTHNEWS.IE AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS CONTENT MEDIAPLANET
michelle.clayton@mediaplanet.com Business Development Manager: Samantha Taylor Managing Director: Alex Williams Country Manager IE: Ross Bannatyne | Head of Print & Design: Thomas Kent Designer: Aimee Rayment Content Editor: Angelica Hackett O’Toole | Head of Digital Operations: Harvey O’Donnell Paid Media Manager: Jonni Asfaha Social & Web Editor: Henry Phillips Digital Assistant: Carolina Galbraith Duarte All images supplied by Gettyimages, unless otherwise specified @HealthnewsIE Contact information: uk.info@mediaplanet.com or +44 (0) 203 642 0737 @MediaplanetUK Please recycle
Project Manager: Michelle Clayton
If you experience ‘simple faints,’ don’t delay — get checked straight away.
the Blackout
on
to
your
for
an unexplained loss of
to receive the correct diagnosis and appropriate
The rapid advancement of digital technologies is transforming the way patients interact — and will interact — with their healthcare providers.
Download
Checklist
stars.org.uk
share with
GP
initial assessment. For 30 years, STARS has supported patients affected by
consciousness
treatment.
Finding treatment that improves quality of life for AF patients
Professor Jonathan Lyne Electrophysiologist, Beacon Hospital


Some people may not know they have atrial fibrillation (AF), but others experience fatigue, lack of energy, breathlessness and palpitations. Consultant cardiologist and electrophysiologist Professor Jonathan Lyne explains that, for patients without symptoms, the condition can be picked up by changes on their wearable devices, such as smartwatches, or in routine medical examinations and preoperative screening.
Who can experience atrial fibrillation?
As a consultant in Beacon Hospital and Blackrock Health in Ireland, Lyne specialises in heart rhythm disorders, diagnosis, treatment and management — including procedures such as catheter ablation and device insertion (pacemakers and defibrillators). He says AF is a common condition in around 10% of people over 80 and 5% over 70 in Ireland. However, AF can also affect younger people.
Drug therapies and ablation treatment
Once diagnosed, treatment options range from drug therapies to ablation. In ablation, a thin wire is passed via a catheter through the blood vessels to the heart. The area of heart muscle identified as causing the issue is then destroyed — using either heat (radiofrequency ablation) or freezing (cryoablation) to create scar tissue, which does not conduct electricity.
Side effects of drug therapies
People with AF have an increased risk of stroke and are assessed for blood thinners or anti-coagulation drugs. Medication can also be used to slow a patient’s heart rate or rhythm, particularly if they have intermittent (paroxysmal) AF. However, Lyne warns: “Rhythm control drugs do not alter progression of disease; some have side effects and require monitoring.
“Ablation restores and maintains sinus rhythm, reduces symptoms and significantly improves quality of life for patients.” Patients generally access treatment via referral from cardiologists; GPs who refer directly to an arrhythmia specialist; or self-referral because of increasing awareness or concern.
Valuable resource for arrhythmia and AF


Lyne points to the getsmartaboutafib.ie website as a valuable resource for patients, with tools and information about the condition. It looks at what arrhythmia and AF are, offers information on ablation and recovery and features disease management tools. There is also a section for healthcare professionals.
“It increases awareness and highlights the importance of diagnosis and referral to appropriate specialists and institutions,” says Lyne. “That increased awareness through getsmartaboutafib.ie is important in reducing long-term morbidity and mortality of AF. Managing the condition and getting earlier treatment, such as with ablation, helps avoid complications from AF,” he adds.

Why people shouldn’t be afraid to seek treatment for atrial fibrillation
Hockey veteran Ed Cherry warns people to seek early diagnosis and treatment for any heart problems after he experienced an episode during a match while on tour in Spain.
It was during a veterans’ hockey tour in Spain, that Ed Cherry first realised he had an issue with his heart. Nearing his 50th birthday, he was fit and active but — while running around in 35-degree heat after what he describes as ‘a good night out the previous evening’ — his heart rate took off. “I felt dizzy,” he recalls. “But within minutes, these symptoms went away; but I got a fright.”
Recurring heart symptoms
Having returned home from Barcelona to Ireland, the sensation of increased heart rate symptoms started happening more frequently; often while watching TV after an evening meal with a glass of wine, he says. Even then, it took months for him to seek medical help, and only after his wife insisted.
Having cut back on his alcohol intake, he visited his GP who referred him to a specialist. “If I ever needed a wake-up call, that was it. From there, I was referred to an electrical heart specialist,” says Cherry, now 53. “Given the delay in my seeking help, I went straight to the interventional treatment.”
Diagnosis and treatment

Via a wearable device, it was identified that he had both atrial fibrillation and an atrial flutter. “This is important information for the consultant to improve the treatment efficacy. If only one problem is identified initially but you have both, then you will need to go back for another procedure.”
Cherry underwent catheter ablation under a general anaesthetic. Although he recalls waking up in the intensive care unit, he was back at work with his healthcare company in a matter of days. “Since the treatment, I have regained my life; I am now symptom-free. Consequently, I have improved my level of exercise and reduced weight.”
Find support for your heart
Having joined Croí, a patient advocacy group for people in Ireland with cardiovascular disease and stroke, he stresses the importance of raising awareness and prompt diagnosis and treatment of heart conditions. Addressing symptomatic people sitting at home who are hesitant to seek treatment, he underlines the importance of early referral for diagnosis and treatment at a specialist centre of excellence — even if it means travelling to receive the right care.
MEDIAPLANET READ MORE AT HEALTHNEWS.IE 03 AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS CONTENT
Early diagnosis and treatment of the heart rhythm disorder atrial fibrillation is key to avoiding more serious cardiac complications as a result of the condition.
Scan the QR code to find out more Page paid for by
Johnson and Johnson
Edward Cherry Patient, who has undergone ablation procedure to treat AF
The minutes matter: how to identify and help someone experiencing a stroke
Stroke is Ireland’s third biggest cause of death and the biggest cause of acquired disability. One in six people here will have a stroke at some time in their life, so it’s useful to know what F.A.S.T. stands for.
They’re the four little letters that could save your life after a stroke — but only 1 in 10 people in Ireland know what F.A.S.T. stands for. Consequently, last year, around 2,500 stroke sufferers failed to get to hospital in time to receive treatment, which can be the difference between walking out of hospital after a few days or never being able to walk or talk again.
Chris Macey Director of Advocacy and Patient Support, Irish Heart Foundation

Be aware of the stroke signs
To tackle this deadly awareness deficit, the Irish Heart Foundation launched its ‘Act F.A.S.T. — Minutes Matter’ campaign fronted by actress Pauline McLynn, iconic for her role as tea-obsessed housekeeper Mrs Doyle in Father Ted.
F.A.S.T. stands for:
F – Facial weakness: Has the person’s face fallen on one side? Can they smile?

A – Arms: Can they keep both arms raised?
S – Speech: Is their speech slurred?
T – Time: It’s time to call an ambulance.
Why people need to act fast
The average stroke destroys 2 million brain cells every minute. So, the faster you get to hospital after a stroke, literally more of your brain can be saved. The ‘T’ is the crucial letter. There’s no point knowing the warning signs unless you ring an ambulance without delay if you see any single one of them.
Treatment possibility for stroke
There have been huge improvements in acute stroke treatment and care in the last decade, cutting the death rate by over 30%, in addition to major reductions in permanent severe disability.

These include the clot-busting treatment thrombolysis and thrombectomy, which involves a tube being fed through the groin to the brain using specialist equipment to retrieve the clot blocking the blood supply to the brain. However, these high-tech treatments and the huge expertise of the doctors who deliver them are worth nothing unless patients get to hospital in time to benefit.
The time window to administer thrombolysis is generally four-and-a-half hours, but only 60% of stroke sufferers are getting to hospital within this time compared to 73% eight years ago. Even if you don’t have a stroke yourself, somebody you love may. Knowing these four little letters — F.A.S.T. — could make all the difference.
04 READ MORE AT HEALTHNEWS.IE AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS
MEDIAPLANET
CONTENT
The average stroke destroys 2 million brain cells every minute.
Heart health for women: how to reduce disease risk and love your heart
Women can reduce their risk of heart disease with lifestyle interventions, including self-care, reducing stress and engaging
One in four women die from heart disease and stroke each year — the same as men. There are female-specific factors that affect a woman’s risk, including menopause. However, the good news is that around 80% of premature heart disease and stroke is preventable through healthy lifestyles.
Empowering women with a healthy heart
Most women already know what makes a healthy lifestyle, but the many demands of modern life can get in the way. The Irish Heart Foundation has developed the ‘Her Heart Matters’ campaign to help women look after their hearts and advocate for themselves.
This September, the Irish Heart Foundation is calling on women to put themselves first and make their heart health a priority. It’s not just up to women themselves, so we are also calling on the public to talk, share and empower women to look after their heart health.
Translating mindset into change

Getting into the right frame of mind is essential for change. You need to feel ready and have clear, powerful reasons for making a change. As part of the Her Heart Matters campaign, the Irish Heart Foundation has created a free Self-Care and Wellbeing Journal to encourage women to reflect on their lifestyle habits and prepare for meaningful change.
Taking steps to manage stress
While stress is a normal part of life, it can be negative when it starts to impact day-to-day tasks. Many women are juggling multiple demands, and this can be particularly challenging during menopause. Try to keep a regular sleep routine, be physically active and stay connected to friends and family. If you are struggling, contact your GP.
Physical activity and nutrition
Regular physical activity and a Mediterranean-style diet are two of the greatest tools for preventing heart disease and stroke as well as helping to reduce some menopause symptoms. Getting at least 150 minutes a week of moderate-intensity activity is recommended for good health.

The Mediterranean-style diet is based around fruit and vegetables, whole grains, beans and other pulses, nuts and seeds. It includes some olive oil, fish, seafood and poultry and is low in sugar, salt, processed foods and red meat.
Start the conversation
Be part of the movement with people who want to see change and protect all women from one of Ireland’s biggest killers. Spread the word with your sisters, mothers, daughters and friends.
AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS CONTENT
in physical activity.
Janis Morrissey Director of Health
Promotion, Irish Heart Foundation
Regular physical activity and a Mediterraneanstyle diet are two of the greatest tools for preventing heart disease and stroke.
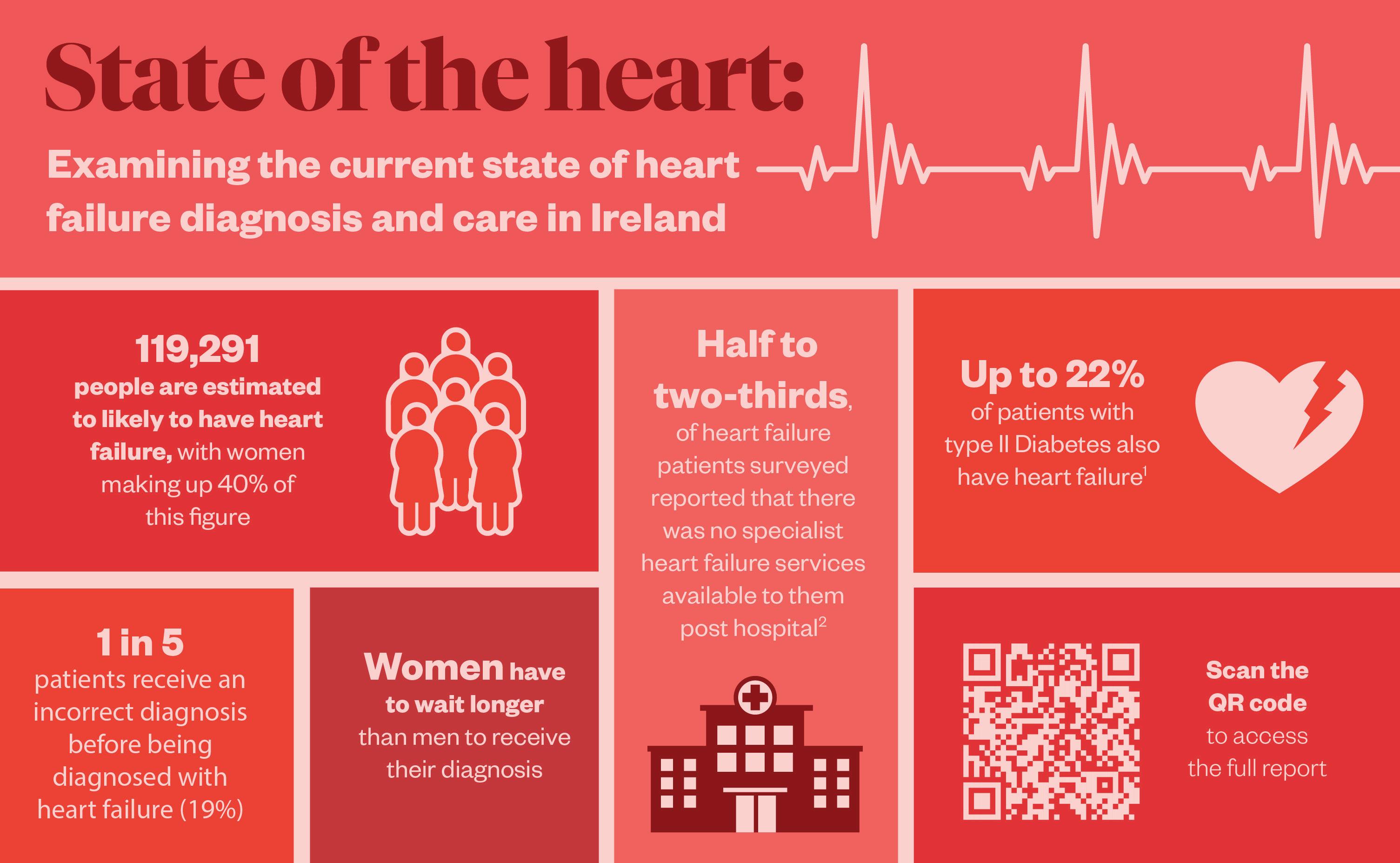
Why more Irish patients need to get teste d and treated for heart failure
An estimated 2% of Ireland has heart failure, but with timely diagnosis and early optimised treatment, living with this condition can be much improved.
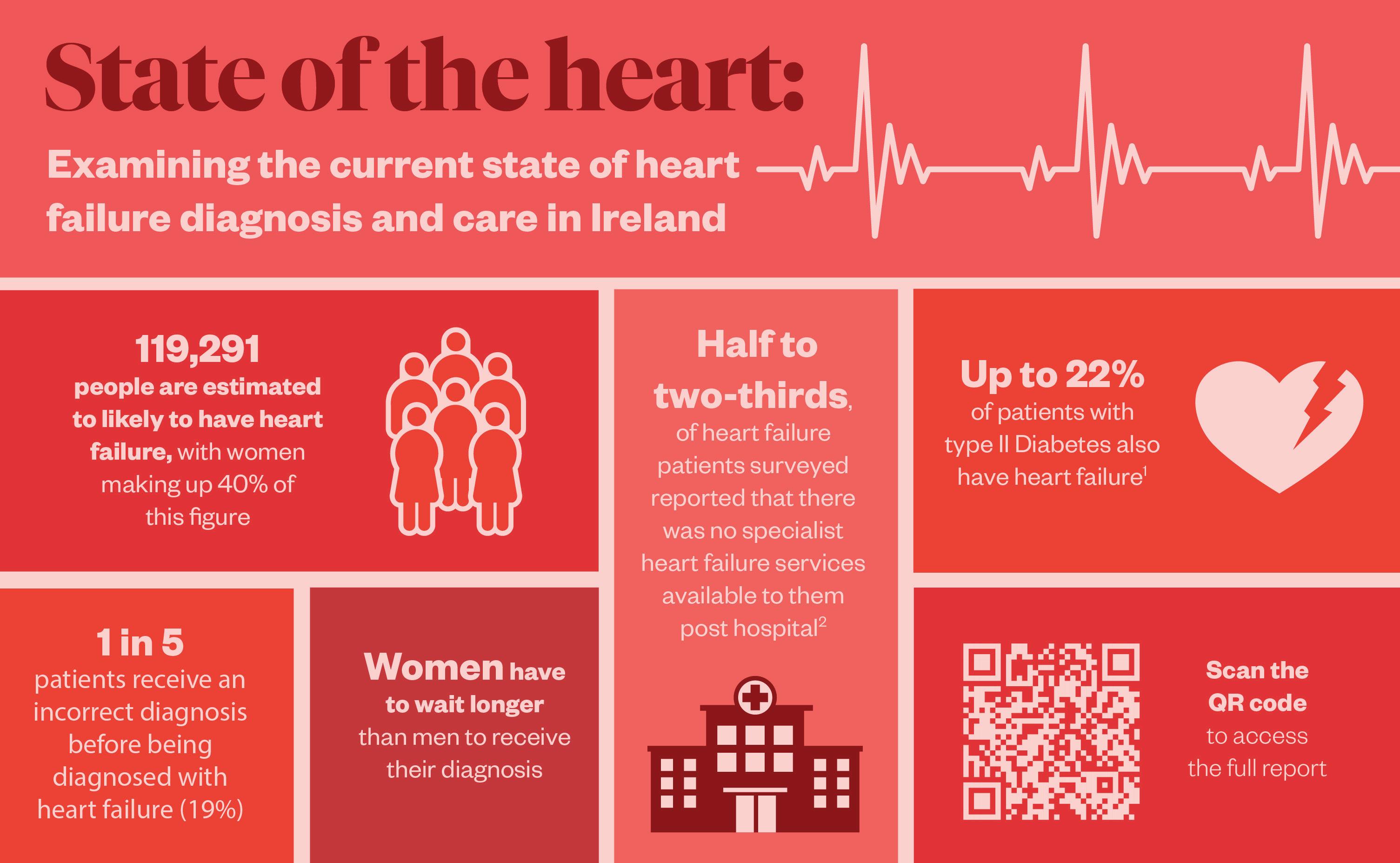
The National Framework for the Integrated Prevention and Management of Chronic Disease has received significant funding over the past two years, contributing to improvement in the Irish healthcare system. Part of the Framework are chronic disease hubs, which are resourced with consultants, advanced nurse practitioners (ANPs), allied health professionals and nurses.
Heart failure treatment with end-to-end care
The Framework demonstrates how ‘end-toend care’ can be provided within the Irish health services. Emer Burke, an ANP based in Galway, says: “There’s never been a better time to be treated for heart failure. The problem is there is still hesitation from some people to acknowledge they have symptoms and go to their GP for a blood test.”

Burke has cared for patients from diagnostics to treatment management through to post-hospitalisation and palliative care. She, therefore, knows that earlier presentations yield a much longer life expectancy. Yet, the five-year mortality rate for patients with heart failure is a staggering 50%. “Patients with fatigue, swelling limbs or breathlessness should promptly speak to their GPs. They will be given a blood test, and that is critical as it means they can be referred to specialists for further investigations.”
Approach to testing and treatment
Treatment options will be decided after an ultrasound of the heart, which assesses how well the heart is squeezing (ejection fraction). If it is less than 40% of blood capacity per heartbeat, then patients will be offered treatment. The overall health of the heart and co-morbidities like diabetes or obesity will also be assessed.
Effective treatments include beta blockers, receptor inhibitors and receptor blockers. The rapid introduction of these therapies to achieve the maximum tolerated dose per patient can optimise treatment. This can improve patients’ quality of life and reduce hospitalisations.

Bumping
up diagnosis and treatment
Aware of the stigma around heart failure, Burke insists: “It’s a frightening term because people think it means their heart has failed, but patients can live well with heart failure if treated early — it might be the heart pump doesn’t relax or pump well enough to circulate blood.”
Her message is to ‘bump up the pump’ and increase awareness that, by acting on signs and symptoms with early diagnosis, patients can access treatment earlier and bump up survival rates.
06 READ MORE AT HEALTHNEWS.IE AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS CONTENT MEDIAPLANET
References: 1. Rodica Pop-Busui, James L. Januzzi, Dennis Bruemmer, Sonia Butalia, Jennifer B. Green, William B. Horton, Colette Knight, Moshe Levi, Neda Rasouli, Caroline R. Richardson; Heart Failure: An Underappreciated Complication of Diabetes. A Consensus Report of the American Diabetes Association. Diabetes Care 7 July 2022; 45 (7): 1670–1690. 2. Irish Heart foundation (June 2023) – The Needs of heart failure patients in Ireland. https://irishheart.ie/wp-content/uploads/2023/06/IrishHeart-Foundation-The-Needs-of-Heart-Failure-Patients-in-Ireland-survey.pdf
Spread paid for by Roche Diagnostics Scan the QR code to find out more
Emer
Galway
Hospitals & Galway Integrated Heart Failure Service PRO of the Irish Association of Heart Failure Nurses
WRITTEN BY James Martin
Burke Advanced Nurse Practitioner,
University
The five-year mortality rate for patients with heart failure is a staggering 50%.
Proactive healthcare via GP to enable early HF detection and virtual referrals
Special blood tests taken in GP surgeries are highlighting heart failure (HF) sooner while virtual consultations between GPs and cardiac specialists are enabling better management of patients closer to home.
Sláintecare reducing hospitalisations
This initiative has been running in the Dun Laoghaire and Bray Integrated Care Hub area for four years and has already led to a reduced burden on emergency and outpatient departments, according to consultant cardiologist Dr Matthew Barrett.


He says that the initiative, which is part of the Sláintecare transformation of healthcare in Ireland, is seeing primary and community health services delivered through new models of care. “One part of that is prevention,” he adds. “In Dun Laoghaire, we are trying to identify patients at risk of developing heart failure.”
Routine NTproBNP blood test to detect heart failure
Earlier identification of HF allows quicker treatment and may avoid deterioration of the condition. Patients at increased risk may be treated with medication while an NTproBNP blood test can efficiently identify potential cardiac problems, including HF. It is offered to patients with diabetes or high blood pressure during routine check-ups. “We hope to identify these patients early and get them treated early so that they will avoid more severe HF,” says Barrett.
Virtual platform for specialist input
An important element is a virtual platform for GPs to discuss their patients with cardiac specialists to decide if they need further investigation, medication or access to clinical HF services. “It is a rapid pathway for GPs to identify problem patients and get a specialist opinion,” he adds. “Sláintecare mandates novel methods of facilitating specialist opinion and review — that is where our virtual model of care comes in.”
GPs are increasingly using the service instead of having to refer patients to the emergency department or outpatient clinics — with longer waiting times. “We have found a 90% drop in referrals to the ED or outpatient clinic, as a direct result,” reveals Barrett.
Benefits and challenges
Patients are getting prompter care with no travel. Hospitals benefit from reduced costs and pressure burden. Against a backdrop of rising HF, Barrett is involved with the PASSION-HF study, which is exploring ways to digitally automate routine engagement with HF patients. However, while the NTproBNP test and virtual platform are identifying potential HF patients, they must now navigate sufficient access to imaging, such as echocardiograms, to confirm the condition.
Digital healthcare programme helps HCPs support heart failure patients remotely
Patients with heart failure in Ireland are being monitored remotely by healthcare specialists in their own homes to deliver a more cost-effective and reassuring level of care.
phone or video call consultation. Early engagement allows HCPs to act promptly on symptom changes to prevent the condition from deteriorating, often with tweaks to medication. Dr Bailey explains: “The crux of the process is making sure that when people start to feel unwell, we intervene as soon as possible and determine what to do next.”
Giving HF patients reassurance
Dr Bailey says patients feel reassured and less anxious and, over time, gain the confidence to self-manage and “take more power back over their condition.” He insists: “That is one of the big successes of this model of care.”
Adigital healthcare programme has been implemented in Ireland to better manage patients with serious heart conditions in their homes and help reduce hospital admissions. It uses smart technology to remotely monitor patients with heart failure (HF) and can alert healthcare professionals (HCPs).
Monitoring patients with heart failure
Remote care for HF patients is being offered through Care-Connect, a partnership between primary care services provider Centric Health and private health insurer Irish Life Health. To better support patients with complex chronic diseases, the digital-first option was favoured over
a physical centre for people with HF. Care-Connect CEO, Dr Donal Bailey, says: “It’s about staying digitally connected to patients — wherever they are — to collect information, so we can see who is doing well and not so well as early and equitably as possible.”
Smart technology for prompt intervention
Following discussions with healthcare giant Roche, HF patients were given smartphones, smart blood pressure monitors and weighing scales, aiming to keep the programme simple and not to ‘hospitalise the home.’
Patients transmit weight, heart rate and blood pressure data. If it shows concerning changes, a GP nurse makes contact for a more detailed
With HF, there are ‘critical windows’ where the condition can get worse and result in hospital admission. “With our model, we are reducing admissions because we are intervening earlier,” he adds. “If we keep patients out of hospital, those beds are available for someone else. We are also reducing the workload on cardiologists, meaning they can spend time with the most complex patients.”
Economically beneficial model
The model, launched this year following a research phase, is constantly evaluated by Care-Connect via the team’s health economist and liaison with Roche.
“Aside from patient benefits and capacity creation, evidence suggests there is an overall health economic benefit,” concludes Dr Bailey.
MEDIAPLANET READ MORE AT HEALTHNEWS.IE 07 AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS CONTENT
Specialist blood tests taken in community healthcare settings are helping identify patients at risk of developing heart failure at the earliest opportunity.
Scan the QR code to find out more Scan the QR code to find out more
WRITTEN BY Mark Nicholls
Dr Matthew Barrett Consultant Cardiologist, St Vincent’s and St Michael’s Hospitals in Dun Laoghaire and The Bray Integrated Care Hub
WRITTEN BY Mark Nicholls
Dr Donal Bailey CEO, Care-Connect
Helping to care for the cardiovascular health of each person in Ireland
As cardiovascular disease remains a major cause of morbidity and mortality, we must work to enhance cardiovascular health on the island of Ireland.
The Irish Cardiac Society was established in 1949 as the professional society for clinicians in Ireland whose primary interest is in cardiovascular medicine and surgery.
Strategy promoting cardiovascular health
World Heart Federation. This facilitates our members to keep abreast of developments on the global stage.
Relevant and recent research
Professor Pascal McKeown President, Irish Cardiac Society

Over the past seven decades, we, at the Society, have grown and embraced the advancements that have taken place. This has led to an expansion in services, including subspecialisation, with a focus on prevention, diagnostics and treatments for established cardiac diseases.
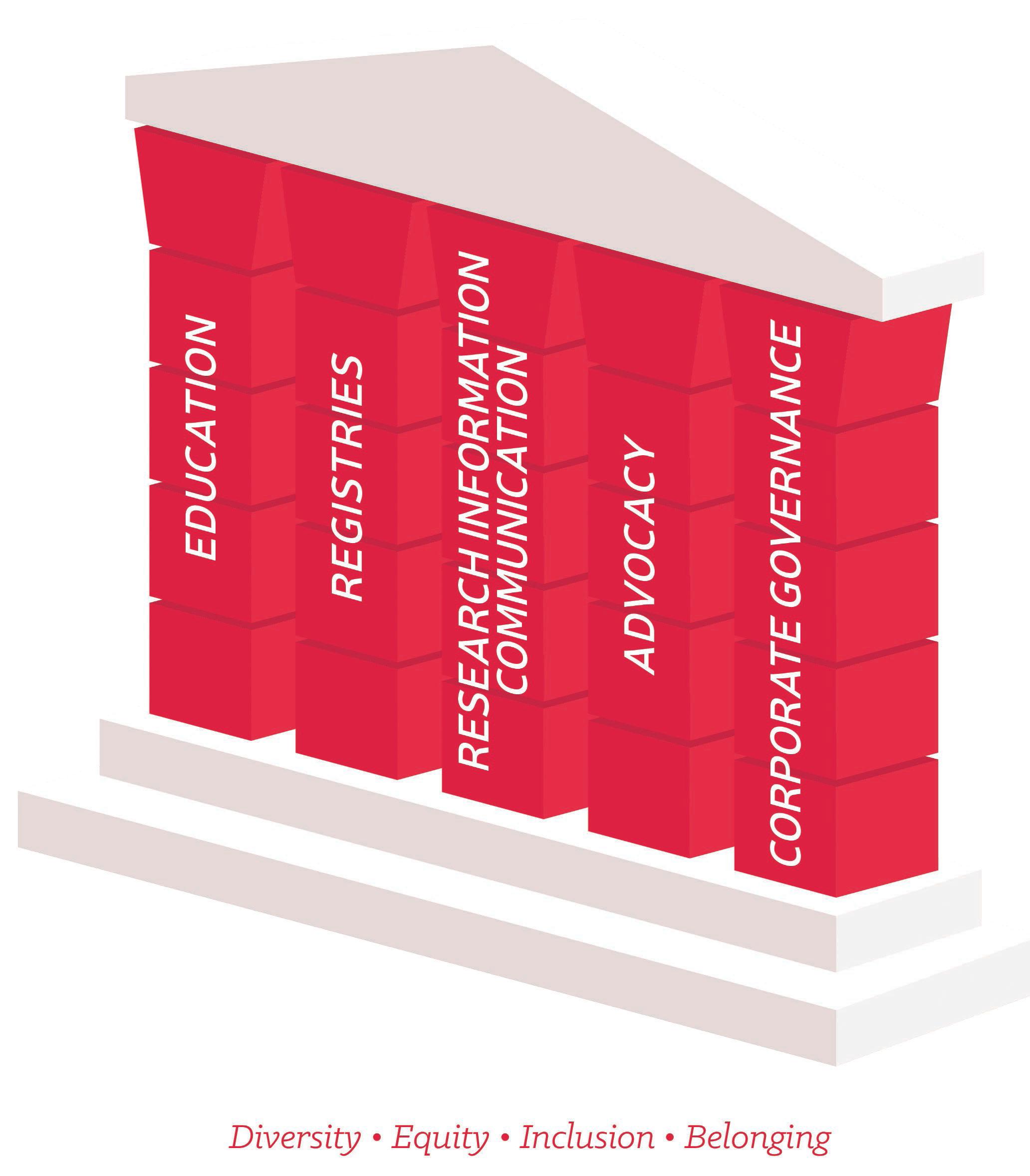
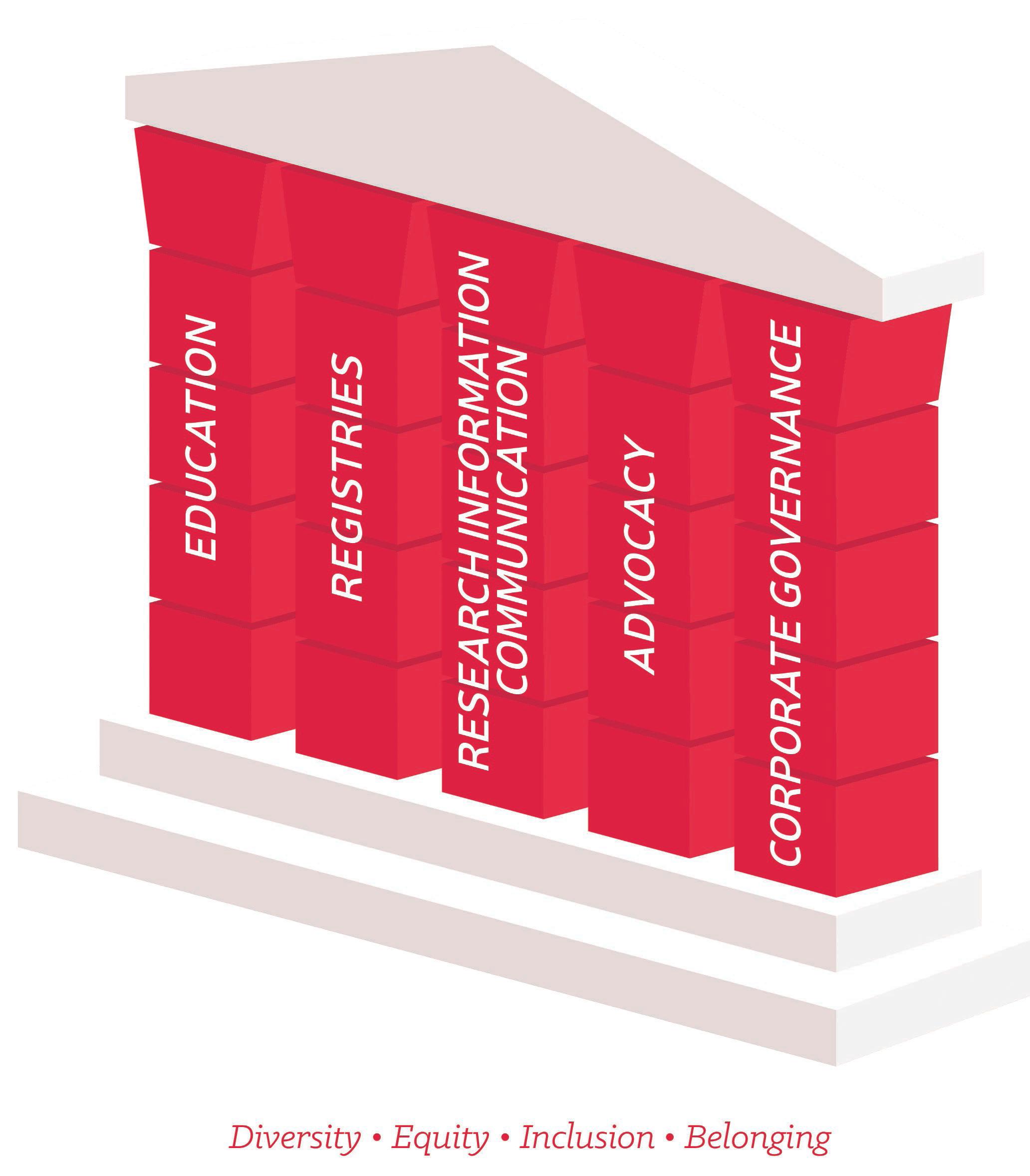
In 2022, we developed a new strategy, which will set a roadmap for the coming years. There are five main pillars: education; registries; research; advocacy; corporate governance. Education is a core activity, where we offer access to resources, training support and a range of educational events.
Connected to cardiology globally
We encourage our trainees to undertake Fellowships outside of Ireland and bring back their enhanced knowledge and skills for the benefit of our population. We also focus on maintaining strong partnerships with many international organisations, including the British Cardiovascular Society, the European Society of Cardiology, the American College of Cardiology and the
There is increasing evidence that patients managed in research-active centres have better outcomes, so we aim to ensure that our patients have access to relevant and innovative research studies. The need to have up-todate information on disease prevalence, risk factors, treatments, outcomes and quality of care necessitates the development of registries. This information will allow us to benchmark how Ireland compares to other countries.
Patient-centric and inclusive support
We recognise the importance of advocacy for our patients and members to ensure optimal cardiovascular health and wellbeing. Our core values are underpinned by diversity, equity, inclusivity and belonging and we have a very active ‘Women in Cardiology’ group. We also support the work of our wider cardiology multidisciplinary team members. As we strive for excellence in our activities, we can improve cardiovascular health for our population.
08 READ MORE AT HEALTHNEWS.IE AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS CONTENT MEDIAPLANET
The Irish Cardiac Society 74th Annual Scientific Meeting will take place in Killashee House Hotel, Kildare from October 12th–14th 2023. For more information: irishcardiac society.ie
We aim to ensure that our patients have access to relevant and innovative research studies.
Graphic provdided Irish Cardiac Society
In 2022, we developed a new strategy, which will set a roadmap for the coming years.
What makes ASCVD an ‘invisible killer’ and how to prevent it
Cardiovascular disease (CVD) is the world’s biggest killer. This is a statement of shame when you consider that as many as 80% of these premature cardiovascular deaths could be prevented.
In this 21st century, why do we allow 19 million people worldwide to die prematurely from CVD every year?
Danger of atherosclerotic cardiovascular disease
Atherosclerotic cardiovascular disease (ASCVD) is the underlying cause of 85% of heart attack and strokerelated deaths and affects more than 500 million people worldwide, according to Invisible Nation. ASCVD is an umbrella term used to describe different diseases caused primarily by the build-up of fatty deposits, called plaques, in the arteries.
What’s especially worrying about ASCVD is its invisible nature. The plaques subtly build up over time, with many people not experiencing any symptoms until a plaque ruptures. When this happens, it can cause devastating consequences, such as a heart attack or stroke.
Causes of ASCVD and risk factors
A key cause of ASCVD is high levels of cholesterol in the body. While cholesterol is essential to the normal functioning of our bodies, too much of the ‘bad’ type (called LDL-C) contributes to the build-up of plaques in our arteries. High cholesterol levels often go unnoticed because there are no symptoms until a sudden heart attack or stroke occurs. Several research studies show
that large numbers of Irish adults are living with levels of ‘bad’ cholesterol, which significantly increases their risk.
United in ASCVD prevention
The invisible nature of ASCVD and high cholesterol are perhaps two reasons why CVD deaths are so high. However, high cholesterol is easily identifiable through a simple blood test, and levels can be managed through lifestyle changes (such as exercise and diet) and medication.
Despite the scale of the problem, many countries, including Ireland, do not have a national cardiovascular health strategy. As a society, we are just not taking this burden seriously. We need to reframe the discussion about cardiovascular disease, take a fresh look at it and wake up to the reality of just how significant a burden this disease has on individuals and populations.

On World Heart Day, I urge you to join the fight against complacency around the dangers of ASCVD. Support The Global Cholesterol Action Plan as it aims to reduce the impact of unhealthy cholesterol levels as recommended by the World Heart Federation. At Croí, we are at the forefront of the fight against heart disease and stroke in Ireland.

MEDIAPLANET READ MORE AT HEALTHNEWS.IE 09 AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS CONTENT
Neil Johnson
Learn more about ASCVD: croi.ie/ascvd Add your name to the pledge to show your support of the Global Heart Hub’s Global Cholesterol Action Plan on invisible nation.com
CEO, Croí the West of Ireland Cardiac & Stroke Foundation
Paid for by Novartis
We track our patients’ results with great clarity so we can identify opportunities to improve care quickly and efficiently
There is increasing evidence that patients managed in research-active centres have better outcomes.
~Prof Pascal McKeown President, Irish Cardiac Society
Within our grasp: better heart health for all
The global death toll of cardiovascular disease (CVD) in 2021 exceeded 20 million, nearly doubling in 30 years. Often premature and preventable, awareness and access to care involves us all.
On World Heart Day, 29 September, we urge everyone to join the movement to make access to cardiovascular care everyone’s right. It must be a priority in policy and investment. When we know more about our hearts, we can make careful choices.
Prevalence of cardiovascular conditions
Four in five CVD deaths occur in low and middle-income countries (LMICs). Learning about our cardiovascular health for ourselves and those around us — and encouraging others to do the same — will increase awareness and promote the human connection that contributes to heart health.
Cardiovascular conditions can be caused by lifestyle or a genetic predisposition. In addition, neglected CVDs such as rheumatic heart disease and Chagas disease occur in some of the most vulnerable communities, affecting nearly 50 million people combined.

Improving knowledge, investment, equity

With in-depth analysis of CVD risk and mortality data worldwide and trends across gender and regions, the World Heart Report offers insight into approaches and policies to reverse the trend. One priority is Universal Health Coverage for interventions to prevent, manage and treat cardiovascular conditions and reduce the suffering they cause.
Healthcare investment as a percentage of gross domestic product (GDP) and lower death rates are correlated. CVD death rates are higher in countries where people pay more out-of-pocket for healthcare. Countries must invest at least 5% of GDP in cardiovascular health — a practice currently seen in 97% of high-income countries.
Building on breakthroughs
The signs are encouraging. Today, 91% of countries have policies or programmes targeting tobacco’s harmful impacts while 86% have established guidelines for managing CVD. The digital health landscape is another potential gateway to access by all.
The WHO Essential Medicines List now includes polypills that combine medicinal agents. Polypills offer hope for strengthening access and affordability of care and enhancing patients’ adherence to taking their medication. Breakthroughs and positive developments often result from pooling resources and committing to change. Together, we can confront cardiovascular disease and give every person and all societies the best chance to flourish.
#UseHeart #KnowHeart
10 READ MORE AT HEALTHNEWS.IE AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS CONTENT MEDIAPLANET
Daniel José Piñeiro President of the World Heart Federation and Professor of Medicine, The University of Buenos Aires, Argentina
How remote clinical management can improve patient care

Remote monitoring and virtual nurse support can help patients with heart failure (HF) or chronic obstructive pulmonary disease (COPD) improve their daily lives and, critically, avoid preventable visits to the hospital.
Today, at least 90,000 people in Ireland live with HF and 380,000 live with COPD, according to The Cost of Heart Failure in Ireland report and COPD Support Ireland. With constant remote monitoring, supported by technology and managed by a team of nurses, patients with cardiac and respiratory conditions can live with more support and swift access to care.
Convenient, remote patient health monitoring

For years, clinical guidelines have recommended regular monitoring of certain signs (e.g. blood pressure, heart rate and body weight), as they are invaluable for managing heart failure. By giving patients the tools to measure these signs at home, they can send valuable information to a clinical team that can monitor and assist in managing their condition more effectively. At Care-Connect, that allows us to see trends and indicators of deterioration in the patient’s condition earlier — often before symptoms start. This model of care helps people stay well at home and can reduce visits to the emergency department or lengthy hospital admissions.
Evidence-based care approaches
We aim to provide the best evidence-based care possible. For years, we have been investigating how remote care can impact patient outcomes by reviewing international
best practices and conducting detailed research. We team up with GPs and hospital specialists to best support people with HF and COPD. We aim to implement guideline-directed standards of care as efficiently as possible. With technology, we can track our results with clarity, so we can identify opportunities to improve care quickly and efficiently. This can increase the potential for an individual’s chronic condition to be clinically managed early.
Toward better health outcomes for patients

Many patients with HF or COPD can achieve improved outcomes and symptom control by following a structured team approach to their medication and treatment plan. Specifically, for patients with HF, optimising their medications promptly after diagnosis lowers their risk of subsequent hospital admission. However, researchers have reported that it is challenging to achieve this for patients with long-term conditions, partly because there are so many interactions to navigate — each carrying a risk of slight delay.
A large part of Care-Connect’s role is to work with our patients and their doctors to coordinate everyone’s treatment plan to be as efficient as possible. We can then collaboratively reduce the risk of avoidable complications while providing a supported and positive experience to our patients.
MEDIAPLANET READ MORE AT HEALTHNEWS.IE 11 AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS CONTENT
Dr Donal Bailey CEO, Care-Connect
a new
Paid for by Care-Connect
Dr Fiona Kiernan Chief Economist, Care-Connect Care-Connect
is
healthcare provider established in partnership between Irish Life Health and Centric Health. To find out more, visit Care-Connect.ie
We track our patients’ results with great clarity so we can identify opportunities to improve care quickly and efficiently.
We recognise the importance of advocacy for our patients and members to ensure optimal cardiovascular health and wellbeing.
~Prof. Pascal McKeown President, Irish Cardiac Society
Four
~Daniel José Piñeiro, President, World Heart Federation
STEMI intervention: how to deal with severe ischaemic heart disease
According to the Central Statistics Office 2022, 9,652 people died from cardiovascular disease in Ireland. Of these, 43% died from ischaemic heart disease — the most serious type is STEMI.
Ischaemic heart disease means that the heart is not getting enough blood and oxygen, usually caused by a narrowing of the coronary arteries. This narrowing can be caused by a blood clot or by a build-up of plaque (atherosclerosis).
steps to improve long-term outcomes after STEMI.
Reducing risk of developing ischaemic heart disease
Some risk factors can’t be changed, such as age, gender and family history.
Tom Kiernan Consultant Interventional Cardiologist


The most serious is an ST-elevation myocardial infarction (STEMI). A STEMI occurs when one of the coronary arteries becomes completely blocked. This is a life-threatening condition and requires immediate emergency treatment.
Treatment services for STEMI
The current gold standard of treatment for STEMI is primary percutaneous coronary intervention (PPCI). This emergency procedure opens up the coronary artery and restores blood flow to the heart muscle. In January 2013, UL Hospitals Group (ULHG) was chosen as one of five 24/7 PPCI centres to provide this service.
Spearheaded by Professor Tom Kiernan, we, at ULHG began accepting patients diagnosed with STEMI directly from our paramedic colleagues. We cover the geographical region of Limerick, Clare, Tipperary and North Kerry. We are the youngest of the five PPCI centres but our research has shown that we have decreased mortality from STEMI, improved outcomes for patients and decreased length of hospital stay.

Patients at ULHG have timely access to many nurse specialists, such as in cardiac rehabilitation and heart failure, who see patients in outpatient clinics and take

However, the following risk factors can be managed to reduce the risk of developing coronary artery disease: stopping smoking; regular blood pressure checks; normal cholesterol; healthy diet; regular moderate-intensity physical exercise; maintaining a healthy weight; and managing stress.

Common signs and symptoms of a heart attack
• Chest pain: sensation of pressure, tightness or squeezing in the centre of your chest; it can sometimes travel to the arms, jaw, neck or back
• Feeling lightheaded or dizzy
• Sweating
• Shortness of breath
• Feeling sick or vomiting
Although the chest pain is often severe, some people may only experience mild pain. In some cases, there may be no pain at all.
If you suspect you may be having a heart attack
Immediately dial 999/112 and ask for an ambulance. A heart attack is a medical emergency.
12 READ MORE AT HEALTHNEWS.IE AN INDEPENDENT SUPPLEMENT FROM MEDIAPLANET WHO TAKE SOLE RESPONSIBILITY FOR ITS CONTENT MEDIAPLANET
Prof
ULHG Scan the QR code to find out more Paid for by Munster Heart Foundation
Dr Samer Arnous Consultant Interventional Cardiologist and Cardiology Clinical
Lead
in five CVD deaths occur in low and middle-income countries.



 © Emilija Jefremova
Trudie Lobban MBE FRCP Founder STARS (Syncope Trust And Refl ex anoxic Seizures), Arrhythmia Alliance
© Emilija Jefremova
Trudie Lobban MBE FRCP Founder STARS (Syncope Trust And Refl ex anoxic Seizures), Arrhythmia Alliance