Empowering Older Americans

A Shot at Prevention: Closing the Immunization Gap in Older Adults
Perhaps one of the greatest public health achievements over the past century has been the dramatic extension of human life expectancy, from an average of 32 years in 1900 to 78 years today. This increase is not by accident; rather, it is the result of systematic public health campaigns that have improved the length and quality of life in the United States.
A cornerstone of these efforts has been developing and delivering safe, scientifically backed vaccines, which have helped contain outbreaks and even resulted in disease eradication. Although the thought of immunizations may lend itself to images of crying babies receiving their childhood shots, they are essential for protecting health at every stage of life. For example, childhood
vaccinations protect against immediate illness and help prevent serious health complications later in life by building long-term immunity, preventing complications from illnesses, and reducing the risk of disease resurgence.
The importance of vaccines at every age
One unfortunate misconception is that immunizations are only necessary early in life. In reality, vaccinations remain essential in older adulthood and are critical to our public health system. As we age, our bodies become more vulnerable to infection, highlighting the importance of ensuring regular immunization. The National Institutes of Health and the Centers for Disease Control and Prevention (CDC) recommend a series of vaccinations
based on age. The annual COVID-19 and flu vaccines are recommended for most age groups; the pneumococcal vaccine and shingles vaccine for those aged 50 and above; the RSV vaccine for those aged 75 and older; and vaccinations against tetanus, diphtheria, and pertussis every 10 years.
Staying current on recommended vaccinations helps older adults maintain their health, independence, and quality of life. This is especially important for those with chronic conditions or weakened immune systems, as immunizations offer critical protection against preventable illnesses and help support better long-term health outcomes. Yet, according to the CDC, only 26% of those age 65 and over are current on all recommended vaccinations.
Battling misconceptions
We cannot let unfounded vaccine skepticism undo over a century of progress.
Vaccines are one of the safest, most effective tools to protect the public’s health, and that protection doesn’t stop at childhood. Decades of rigorous scientific research and real-world outcomes have shown that vaccines save lives, prevent suffering, and reduce healthcare costs across all age groups. The American Public Health Association’s website has helpful resources on vaccines.
For older adults, staying up to date on immunizations is not just a personal health decision; it’s a powerful act of prevention that safeguards communities and supports aging with dignity and vitality. It can provide you with more time with those you love.
As we continue to face evolving health challenges, older adults must speak with their healthcare providers, trust the evidence, and take advantage of the vaccinations recommended for their age. The path to longer, healthier lives improves when we stay protected.

Sponsored by GSK
Finding the Fairway: How Competitive Golf Has Enhanced One
With older age, many adults find themselves on the metaphorical sidelines of life — watching others enjoy the activities they once loved.
Michael is a patient advocate and survivor of respiratory syncytial virus (RSV). This is his experience; others’ experiences with RSV may be different. Michael is not a healthcare provider. He was compensated by GSK to share his story.
That’s not the case for 60-yearold Michael, a father of five daughters and 11 grandchildren, who lives in a city about 50 miles east of Tampa, Florida. In addition to spending time outdoors with his wife, Deborah, playing with his grandkids, and working in administration at a private school, Michael plays competitive golf as a National Senior Games athlete.
“It’s addicting,” said Michael, who began competing in college after an injury led him to transition from baseball to golf. “It’s my therapy now because when you just go out and hit balls and you’re by yourself, nobody’s bothering you. And it’s great to just have a little escape,” he added, explaining that he also enjoys playing golf with Deborah, whom he met at a golf course.
Prioritizing his health
Golf also keeps Michael’s body moving — and that structured exercise is just one of many habits he’s developed to stay in tip-top shape as he’s aged.
“I have a great relationship with my doctor,” he said. “And I’ve completely changed my diet … [I] come home and eat the fish, eat the vegetables, and do the things that you’re supposed to do to just help maintain your health.”
Another thing he prioritizes is his respiratory health. Michael lives with asthma, which, paired with his age, leaves him at an increased risk for
Man’s Well-Being

severe respiratory syncytial virus (RSV).
For adults 60 and older, including those with certain health conditions like chronic heart or lung disease, severe RSV infections can develop into pneumonia and may lead to hospitalization or even death.
Each year in the US, approximately 177,000 adults 65 and older are hospitalized due to RSV, and an estimated 14,000 of those cases result in death.
Finding his drive
Michael noted that he once developed RSV, which led to two ER visits.
“When I had RSV, it was horrible,” said Michael, noting the infection forced him to take three weeks off work. “RSV just flat knocked me out.”
The illness led to “violent” coughing, he said. When Michael’s doctor told him that he could catch RSV again, he took action. “After I recovered, I decided to have a discussion with my doctor and he recommended I get vaccinated against RSV. So, I did, and I’m still going to take other measures to help protect myself in the future … because I want to do what I can to help prevent myself from going
through that again.”
Since his bout with RSV, Michael has become an avid hand-washer, especially after shaking hands or giving high-fives to students. When his grandchildren are sick, he also tries to keep his distance, opting for a wave instead of a hug during greetings.
Golfing has helped motivate Michael to stay committed to his well-being.
“[Golf has] really made an impact on my life health-wise, because now I’m really focused on what I eat, what I do, what my regimen is,” said Michael, who is further motivated by his faith and the example he wishes to set for his students, children, and grandchildren.
“I don’t get as many days to practice as I did when I was in my 20s, because of grandkids and life. And so, your priority shifts, but you still enjoy the competitiveness of it. … It’s a lot more fun now than it was in my 20s.”
Written by Melinda Carter
Trademarks are owned by or licensed to the GSK group of companies.
©2025 GSK or licensor.
NPUS-RVUADVR250001 July 2025 Produced in USA.

Know your risks to help Sideline RSV. Talk to your doctor or pharmacist about vaccination and visit SidelineRSV.com for more information.

INTERVIEW WITH Michael Athlete, National Senior Games
National Senior Games athlete Michael hitting balls on the driving range | Photo courtesy of GSK
Nursing Education Plays a Vital Role in Meeting the Dynamic Needs of America’s Elderly
Public health policy and healthcare delivery resources hold the keys to senior adults’ well-being. How do nurses — considered the nation’s most trusted frontline caregivers — respond to the difficult realities of the job?
Today’s nurses have the advantage of high-level, evidence-based academic and clinical instruction, developed through rigorous investigations of live classroom, bedside, and, increasingly, remote teaching and innovative learning strategies.
For nurse educators to bring their A-game, they may access the host of resources readily available, many online and free of charge. Historically, there has also been scholarship assistance for continuing nursing education authorized under Title VII and Title VIII of the Public Health Service Act. Nursing workforce development scholarships and grants have also been awarded to applicants of diverse ethnic and racial backgrounds across higher education who commit to teaching and practicing in underserved, economically disadvantaged, or remote, rural communities that lack easy access to healthcare services; provide mental healthcare for at-risk youth; and, notably, deliver primary and specialized geriatric nursing care. With budgets for nurse recruitment and retention potentially threatened by funding cuts, it is important for nurses and nurse educators to make their voices heard at the national and state levels by reaching out to lawmakers to preserve and increase spending on these vital initiatives. Our seniors deserve no less.

America’s Unseen Workforce: The New Reality of Family Caregiving
The more than 63 million family caregivers will continue to soar in number as adults aged 65 and older increase from 58 million to over 78 million by 2035.
The U.S. life expectancy has increased by more than 10 years in the last seven decades. However, there is a 12.4-year gap between lifespan and healthspan — the years lived in good health. This means many Americans spend over a dozen years in poor health, requiring care. Consequently, 41% of family caregivers now provide care to an older adult.
A sudden phone call about a fall, stroke, or cancer diagnosis — or the increasing recognition of Mom’s repetitive questions and personality changes that lead to a diagnosis of dementia — is life-altering. Family members step in to provide care that can be episodic or become so intense that holding a fulltime paid job becomes untenable.
America’s family caregiving landscape has often been measured by the “caregiver support ratio,” or the number of potential caregivers (ages 45–64) available for every person age 80 or older. This ratio was 7:1 in 2010 but is projected to fall to 4:1 by 2030 and to 3:1 by 2050. Since this measure first emerged in the 1990s, the projections have shaped policy discussions and fueled concerns about our aging society’s future.
As striking as these figures are, the narrow age band of 45 to 64 and sole focus on care recipients aged 80 and over don’t fully capture the extent and complexity of today’s caregiving experience. Not only does the caregiver support ratio ignore millions of younger and older caregivers alike, but it also doesn’t account for the 1.9 million Americans ages 65 to 74 who are living with Alzheimer’s dementia — a condition that puts enormous demands on families.
Supporting our caregivers
Fundamental societal shifts have reshaped family caregiving. Men represent nearly 40% of caregivers, though they are both less visible and are less likely to seek support. Blended families, chosen families, and community networks outside of biological relationships are providing care.
Older adults themselves actively care for partners and siblings. Nearly 1 in 4 Millennials are caregivers, many assisting an older adult. A growing group of Gen Z caregivers, about 3 million, also provides care for an older adult while balancing educational and career pursuits.
Caregiving extends beyond physical support to include financial tasks like paying bills, navigating insurance, preparing taxes, managing appointments, and assisting with technology for remote monitoring and telehealth.
We have an expanding caregiver population and must be thoughtful about what is needed to support the spectrum of the experience. Today’s family caregivers need financial support, inclusive policies like paid leave and tax credits, and open dialogue with employers. They need access to community resources, such as respite care, and technology that supplements human presence. Measurement metrics must be updated to match the day-today realities of caring for our loved ones.
Above all, it is time for caregivers across all generations to be recognized and valued in new and meaningful ways by employers, policymakers, and society.

WRITTEN BY Beverly Malone, Ph.D., RN, FAAN, President and CEO, National League for Nursing
WRITTEN BY Diane Ty
Managing Director, Future of Aging, The Milken Institute
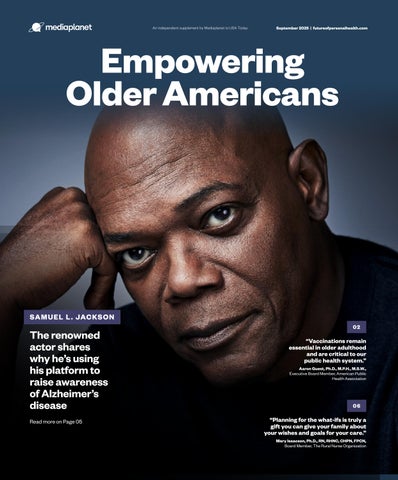
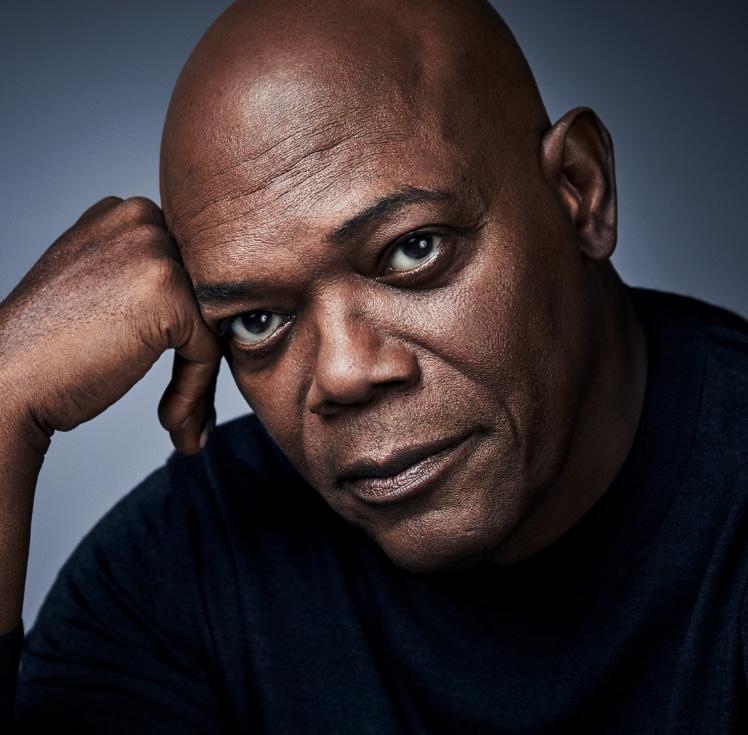
Samuel L. Jackson Raises New Awareness for Alzheimer’s
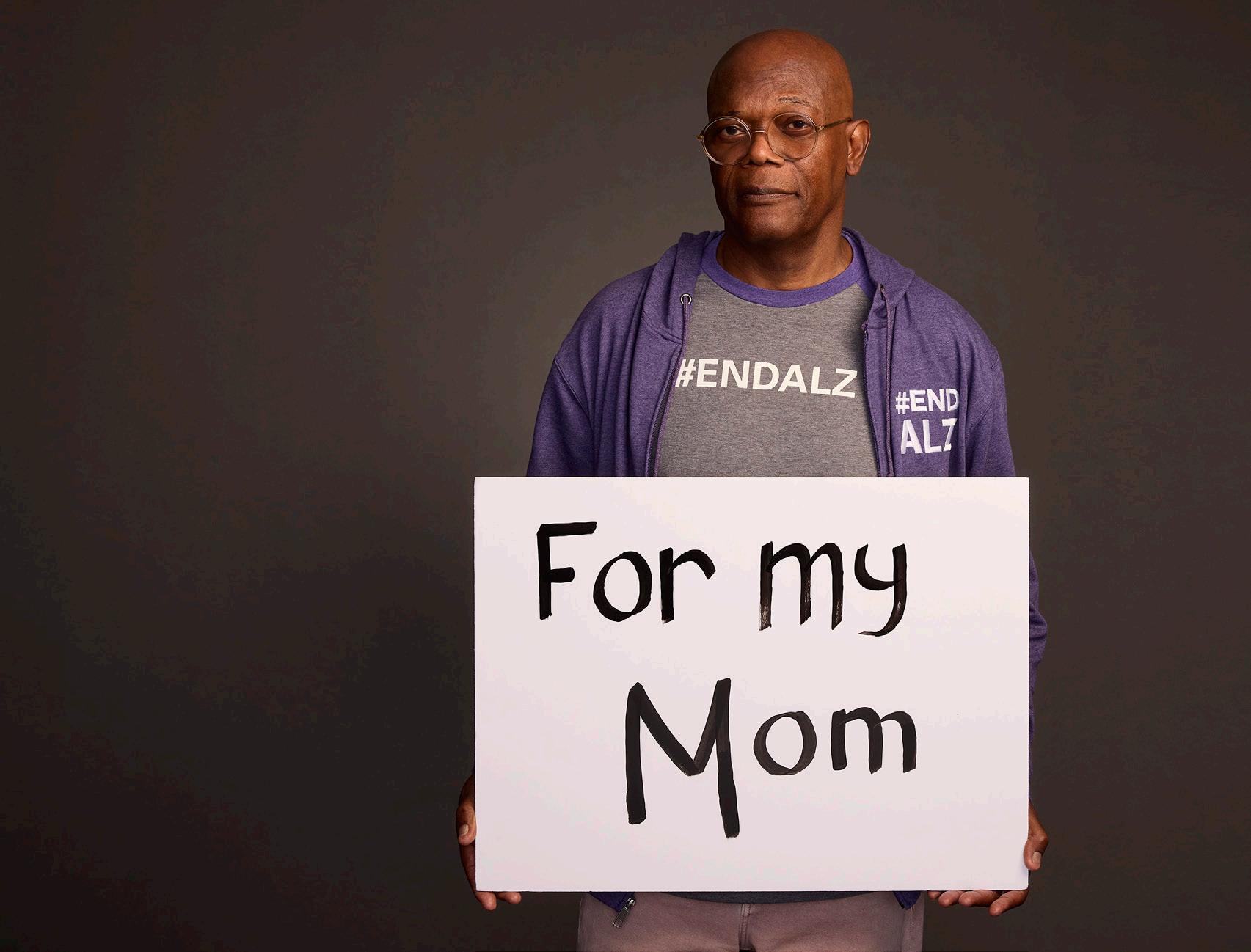
Samuel L. Jackson has spent decades in the spotlight portraying iconic characters in blockbusters like “Star Wars” and the Marvel Cinematic Universe.
Now, the actor is using his platform to bring attention to a disease that has greatly impacted his family and millions of others: Alzheimer’s.
Jackson has a personal connection to the progressive brain disorder. His mother, grandfather, aunts, and uncles have all been diagnosed with Alzheimer’s.
“I have been surrounded by the disease for a very long time,” he said.
He has since partnered with the Alzheimer’s Association to raise awareness about the disease. The actor is now speaking out about the importance of caregiving and early screening.
Caregiving is difficult but necessary
When a loved one is diagnosed with Alzheimer’s, they usually need a caregiver, which is not an easy job. According to an Alzheimer’s Association survey from 2023, 70% of caregivers said coordinating care for people with dementia is stressful.
Between costs, finding the right medical help, and doctor’s visits, caregiving can be difficult, especially for people who already have jobs.
However, Jackson says it’s still important to care for your loved ones with compassion.
“Be patient and empathetic with your loved one, and show them as much love and comfort as you can,” Jackson said. “Be sure not to treat them any differently than you normally do because of the disease.”
He went on to say that he sees caregiving as an opportunity to
nurture his loved ones the same way they nurtured him when he was young.
of the people with the disease have never been diagnosed and don’t even know they have it.
However, Jackson says he has hope for the future of because of the many advancements being made in early detection of the condition.
Be sure not to treat them any differently than you normally do because of the disease.
Earlier screening is key
Early detection of Alzheimer’s allows people to more easily organize a healthcare team and plan. And studies show that an early diagnosis can lower healthcare costs over time.
But according to research from the Alzheimer’s Association, half
“They can diagnose Alzheimer’s much earlier and more accurately than ever before,” Jackson said. “There are also new medicines available that can significantly slow Alzheimer’s progression if treatment begins early enough.”
With more research, the hope is that the disease can be stopped.
“That’s why I have partnered with the Alzheimer’s Association for the last several years to raise public awareness and to support their mission of ending Alzheimer’s for good,” Jackson said.
Written by Frank James
The actor partnered with the Alzheimer’s Association after facing the disease in his own family.
Samuel L. Jackson | Photo by Robert Trachtenberg, courtesy of Alzheimer’s Association
Aging in Place: Elevating Healthy, Independent Aging
“Aging in place” is more than a housing option; it is a fundamental expression of dignity, autonomy, and connection. For many older adults, it simply means the ability to live in the environment of their choice, surrounded by people they trust and love.
While often associated with remaining in one’s long-time family home, aging in place encompasses a broader range of living arrangements, from urban apartments and retirement communities to shared homes with family or friends. The key is choice. That choice reflects, for many, a deep desire for continuity, community, and control in later life.
As a gerontological specialist nurse practitioner, I’ve seen firsthand how aging in place — when safe and thoughtfully supported — can lead to better health outcomes, greater life satisfaction, and prolonged independence. However, it requires a proactive, interdisciplinary approach integrating clinical, social, technological, and environmental strategies.
Home
At the core of aging in place is ensuring a safe, accessible living environment. Whether an older person lives in a suburban house or a downtown condo, the space must be adapted to meet changing physical and cognitive needs. Simple modifications — such as grab bars, no-step entries, adequate lighting, and leverstyle doorknobs — can prevent falls and make daily tasks easier. Smart home technologies, such as motion sensors or voice-activated systems, offer additional support, especially for those managing chronic conditions or mild cognitive impairment.
However, safety is only one component. The emotional value of “home” also matters. A familiar neighborhood, access to cherished routines, and connection to

neighbors can be as essential to well-being as any structural feature. Aging in place must also protect these less visible but equally powerful elements of an older adult’s sense of home.
Healthcare
For aging in place to succeed, healthcare must meet older adults where they are. This means more than occasional office or home health visits. It involves an integrated model of care and longitudinal relationships with healthcare providers, especially those trained in gerontology.
Community
Isolation is one of the greatest threats to successful aging in place. Studies consistently link social isolation and loneliness to depression, cognitive decline, and increased mortality. Therefore, empowering older adults to
remain socially connected is as critical as ensuring physical safety. Community programs, adult day services, volunteer opportunities, and intergenerational activities all play vital roles.
As our population continues aging, we must shift our systems to support where and how people want to live.
Nutrition & mobility
Nutrition and mobility are foundational to living well at
home. Malnutrition, whether due to limited income, poor appetite, or difficulty preparing meals, can derail an older person’s health. Community meals, home-delivered food programs, and nutrition education help address these risks.
As our population continues aging, we must shift our systems to support where and how people want to live. By investing in the infrastructure, healthcare models, and social systems that allow individuals to thrive at home, we honor their preferences and the full spectrum of what it means to age well, with dignity, safety, and choice.

The Power of Community: Supporting Healthy Aging in Rural America
Alan Morgan, chief executive officer of the National Rural Health Association (NRHA), discusses how a sense of community and proactive care can help older adults in rural areas live longer, healthier lives.

How do social connections and community engagement affect the health and longevity of older adults?
INTERVIEW WITH
Alan Morgan, M.P.A. Chief Executive Officer, National Rural Health Association (NRHA)
We often talk about the challenges of aging in rural areas, but we don’t always highlight the inherent strengths. In rural areas, you often have multiple generations living in the same town, which creates built-in family networks that serve as social safety nets. There’s also a strong presence of faith communities and local organizations that provide regular opportunities for engagement, whether it’s adult learning classes or social gatherings. Those interactions aren’t just nice to have; they’re central to successful aging. That’s something rural communities often get right.
How can caregivers and family members better support the physical and mental well-being of aging loved ones?
Communication is absolutely key, especially for family members supporting aging loved ones. In rural areas, we also have to factor in transportation. Helping coordinate or provide transportation can make a huge difference, especially when it comes to accessing healthcare or simply attending community events. Two of the biggest issues are a lack of transportation and limited access to healthcare providers. Family members who can help address those barriers are playing a crucial role in their loved ones’ overall well-being.
What are some signs that an older adult might need more support at home, and how can families approach those conversations with care and respect?
This is a very important question that applies broadly, rural or urban. At NRHA, we’re working with organizations like the John A. Hartford Foundation to train community health workers to serve as bridges between families and healthcare providers. These professionals are often uniquely positioned to recognize early signs that someone may need additional support and can help families navigate those conversations. Sometimes it’s easier to have that input come from a trained, neutral person rather than a family member.
What misconceptions do people often have about aging?
One major misconception is that older adults in rural areas are forgotten or left behind. The truth is, many are choosing to age in place in the communities where they feel most connected and supported. We’ve found that the sense of belonging — being close to family, rooted in community, and maintaining autonomy — contributes significantly to positive aging experiences. Reframing aging as a chapter filled with purpose, connection, and continued growth helps shift the narrative away from loss and decline. When people understand that rural living can actually support aging well, it changes the way we think about what older Americans need and deserve.
Why Advance Care Planning Is the Greatest Gift to Family
The National Institute on Aging suggests that individuals who document and discuss their wishes with their family are more likely to receive the care they desire.
Documenting your wishes and goals of care can be done through a living will and/or a durable power of attorney for healthcare. Both are legal documents and provide guidance to the healthcare team about your care choices and who you have designated to make those decisions on your behalf.
A living will (also called an advance directive) provides written documentation for your healthcare team about medical care you would and would not want, should you be unable to state your wishes. A living will is not a will, which is a legal directive about your personal estate; the living will is specific to your health and medical decisions.
The durable power of attorney is a document where you identify the person who will make decisions about your medical care when you are unable to participate in your care decisions. We often think that we should select our spouse or eldest child. However, it is important to ask yourself, “Even if they know my wishes, will they be comfortable making them?” Once they are identified, talk to them to ensure they will be able to honor your wishes.
Planning for the what-ifs as we age is a way of expressing our love to our family. Now is the time to begin.

WRITTEN BY Mary Isaacson, Ph.D., RN, RHNC, CHPN, FPCN Associate Professor, University of Nebraska; Board Member, The Rural Nurse Organization (RNO)