The Michael G. DeGroote Institute for Pain Research & Care



To further the understanding of the origins and management of chronic pain by bringing together behavioural, clinical and basic scientists to explore underlying mechanisms and therapeutic paradigms.
About Michael G. DeGroote & His Gift
page 4 A Message from the Scientific Director
page 6 Year at a Glance
Education and Outreach
Trainee Network
Opioid Series
page 7
page 8
page 10
page 11
page 12 eChronic Pain Recommendation Map
page 13 Pain Symposium
page 14 Annual Research Day ... page 15
Canadian Pain Care Forum
Centre for Medicinal Cannabis Research
Chronic Pain Centre of Excellence
page 16
page 17
page 18 for Canadian Veterans
Chronic Pain Network
page 19 At McMaster and Around the World
page 20 A Brief History
Research Graduate Studentships
page 23
page 29
page 31 Seed Grants
Grant
page 33
page 42
page 45
In 2003, businessman Michael G. DeGroote made history when he made the largest single donation ever to a Canadian university or institution. His donation of $105 million has had a wide impact on health sciences research, education and care, and accelerated the pace of discovery at McMaster.
“Mr. DeGroote’s gift has been pivotal to advancing pain research in Canada. Not only did it enable the creation of the Institute for Pain Research and Care, but it also paved the way for both the Chronic Pain Network and the Chronic Pain Centre of Excellence for Canadian Veterans.”
- Dr. Norm Buckley, Scientific Director of the Michael G. DeGroote Institute for Pain Research and Care
McMaster’s Faculty of Health Sciences followed a “people first” strategy in allocating the $105 million gift from Mr. DeGroote. Emphasis was placed on hiring international caliber experts in health education, research and care, particularly in the areas of pain, infectious diseases, stroke prevention and cancer. One of the key initiatives was the Michael G. DeGroote Institute for Pain Research & Care, which received a $15 million endowment. “With this gift,” Mr. DeGroote said, “I know McMaster will be able to make new breakthroughs and make a real difference in more people’s lives.”
Michael G. DeGroote died in September 2022, at the age of 89. Though he is no longer with us, his generosity and philanthropic efforts ensure his legacy will live on and enable innovation in research for years to come.

“Though more than 20% of Canadians will experience chronic pain within their lifetime, it still remains an underfunded area of researchaccounting for less than 1% of research funding provided by the Canadian Institutes of Health Research.
”
- Dr. Norm Buckley Scientific Director, Institute for Pain Research and Care

Singers and songwriters have long explored the depths of human suffering in their music, drawing attention to the ways in which emotional pain can overshadow daily life. Joni Mitchell’s lyrics in her song “Man from Mars” reflect this intimately, as she sings, “Since I lost you, I can’t get through the day without at least one big boo-hoo. The pain won’t go away. What am I to do?” These words capture the raw experience of grief, a profound emotional pain that lingers and transforms, sometimes even presenting with physical manifestations. Music frequently gives voice to this connection between emotional and physical pain - something that science is only starting to scratch the surface of.
Studies have shown that individuals experiencing significant emotional pain, such as depression, anxiety, or grief, report higher levels of physical pain and have a greater risk of acute pain developing into chronic.
Norm Buckley, BA (Psych), MD, FRCPC Scientific Director
Michael G. DeGroote Institute for Pain Research and Care McMaster University
For many Canadians, the experience of chronic pain is compounded by long wait times to see pain specialists and limited access to interdisciplinary pain clinics, particularly in rural areas. Most pain clinics are concentrated in urban centers, creating barriers for those in need of comprehensive care. This lack of access can contribute to the persistence of both physical and emotional pain, leaving many patients feeling frustrated and unsupported.
Emerging technologies, such as virtual care platforms, are beginning to bridge the gap for rural patients, providing them with access to mental health professionals, pain specialists, and selfmanagement tools. Meanwhile, initiatives like the development of the e-Chronic Pain Recommendation Map (RecMap) are working to consolidate the best available evidence to guide healthcare providers and patients in making informed decisions about pain management.
59
10 $738 7
Research awards and projects funded every year.
thousand
Spent on research awards and projects
Multidisciplinary research team members from 10 health disciplines.
Publications on the topic of pain by our members last year.
Full-time and 11 part-time Institute staff members overseeing all operations and activities.
20
Years advancing the understanding and treatment of pain through research and innovation.
Sixty-two percent of our annual budget was spent directly on research awards (grad studentships and postdoctoral fellowships) and research projects (seed grants, IPRC/MIRA catalyst grant, and other funded research projects). Annual administrative cost was 29% of the total budget, while the operating cost (including community engagement throughout IPRC Symposium, Canadian Pain Care Forum meetings, National Faculty meetings) made up of 9% of the annual expenses.
Additional to the research and operational activities within the Institute, our IPRC research and operational team administers 30 current projects funded in the last seven years by various sponsors:
Amount Awarded to Research by Year
$4,000,000
$3,500,000
$3,000,000
$2,500,000
$2,000,000
The current balance available amounts to $4M for research projects to complete by 2030.
Over the past several years, the Institute for Pain Research & Care has seen significant growth across both digital and traditional media. Our efforts on X (formerly Twitter), LinkedIn, Instagram and Threads have led to steady increases in followers and engagement, while our web pages continue to serve as key means of disseminating research findings.
On X, our audience has grown by nearly 10% over the last year, with top-performing tweets taking place during the Canadian Pain Society’s Annual Scientific Meeting generating 1,145 impressions. Our strategy includes leveraging more videos and infographics to enhance engagement.
The IPRC grew to 1,350 followers and tweets received more than 36,000 impressions and 1,763 engagements.
LinkedIn remains an area of growth for the IPRC Business2Business communication. Strong engagement with posts has been a highlight, with an engagement rate of 7.1%, and we are looking into boosting posts to expand our reach. Posts received nearly 4,000 impressions and 281 engagements.
This year, the Instagram and Threads accounts were launched. The coming year will be spent looking to increase
audiences on both platforms.
The Institute was one of 444 unique participants to take part in the 2024 National Pain Awareness Week social media campaign. The aim of the campaign was to create dialogue and draw attention to chronic pain.
Led by Pain Canada, the overarching campaign saw a reach of 2.2 million, with 7.6 million impressions.
Both the IPRC website and the National Pain Centre (NPC) website continue to serve as our key means of disseminating information. Over the reporting period, traffic to the IPRC website saw more than 15,000 page views, with significant contributions from organic searches. The NPC website saw more than 22,000 page views, with most traffic directed to the page hosting NPC-produced guidelines.
Looking ahead, the IPRC aims to enhance its social media presence by increasing cross-platform collaboration and maintaining its current level of engagement. The IPRC will also investigate expanding paid advertising campaigns and will explore partnerships to expand our reach to our target audiences more effectively.
40,412 Impressions
2,044 Engagements
5.1% Engagement Rate (per impression across platforms)
307 Post Link Clicks
In addition to its ongoing funding of studentships and fellowships, the Institute for Pain Research & Care (IPRC) has spent the last year focusing on expanding its trainee network and offering more opportunities for mentorship and collaboration. July 2024 marked the
including information on funding opportunities, networking events, and guidance for writing research proposals. As it develops, the hub will become a comprehensive platform for trainees to grow their expertise and connections within the pain research community.
communicate their work effectively to broader audiences. With ongoing support and a commitment to mentorship, the IPRC is dedicated to shaping the next generation of pain researchers.
The
IPRC is not only educating the next generation of healthcare professionals, but also fostering a community of learners who are committed to advancing evidence-based medicine. I'm particularly drawn to its focus on building leaders in this field and the way it brings together students from a variety of healthcare disciplines.
- Dr. Nora Bakaa 2021 Graduate Studentship Recipient
first of our lunch and learn sessions, with special guest Filipe Reis from the Federal Rural University of Amazonia discussing the role of artificial intelligence in pain research. These sessions are designed to provide trainees with opportunities to share their research, gain feedback, and improve their presentation skills, particularly for explaining complex topics to those outside their immediate field.
The IPRC also launched a new Trainee Hub on its website. Still in its early days, the hub aims to provide trainees with valuable resources,
In addition to expanding the Trainee Hub and hosting lunch and learn sessions, the IPRC has set specific goals to grow its trainee network further. Increasing membership and fostering a more robust network of early-career researchers will create more opportunities for collaboration and learning.
The ultimate goal is to offer an environment where trainees can not only learn from established experts but also gain the skills necessary to

With addiction-related issues and overdose deaths increasing, it is imperative for healthcare providers, policymakers and the public to better understand the role of opioids and grasp the nuances of opioid therapy. With so much at stake, and so much misinformation readily available, Drs Jason Busse and Norm Buckley worked with Open Access Governmentan open access digital publication based in the UK - to create a series of informative articles addressing some of the most prominent issues surrounding opioids.
The series, which began with five articles - the first of which was published in April 2023, represents a new route to Knowledge Translation for the Institute for Pain Research and Care (IPRC). The series focuses on understanding the complexities of opioid use, pain management, and the implications for public health policy. Articles cover topics such as the role of opioids in treating chronic pain, challenges with prescribing guidelines and current prescribing practices, the impact of the opioid crisis in Canada and government response and strategies.
Open Access Government plays a crucial role in this partnership by
providing a platform to disseminate research findings and insights from IPRC experts to a broader audience. This series serves as a succinct resource for stakeholders, including healthcare professionals, policymakers, and the general public, facilitating informed discussions and promoting evidence-based decision-making.
The opioid crisis has been an issue in Canada for nearly 25 years. Tragically, even though prescribing has declined since 2010, the number of deaths associated with opioids has soared. Most deaths are now associated with highly potent synthetic opioids acquired through illicit markets and often mixed with other drugs or sold as other drugs without user awareness of their high potency.
Following the success of the first series
Institute for Pain Research and Care (IPRC) decided to expand its efforts by producing even more insightful content. The most recent article reports on the Canadian Pain Care Forum and the
Canadian Pain Task Force, highlighting the pressing need for enhanced collaboration among pain experts. It is only through fostering these connections that we will continue to improve pain management practices and find a more cohesive approach to addressing the challenges faced by individuals living with pain in Canada.
Articles can be accessed by visiting: openaccessgovernment.org/stakeholder/ michael-g-degroote-institute-for-painresearch-and-care/147553/

Chronic pain is a condition that affects one in five Canadians, but despite its prevalence, many people receive suboptimal care due in part to the inconsistent quality of guidelines and varying recommendations. In response to this issue, the Canadian Institute of Health Research has backed the creation of the e-Chronic Pain
researchers, clinical experts, policy makers, and individuals with lived experience, including those from equity-deserving groups. This structure will include an equity committee and an advisory board composed of both national and international advisors, with a steering committee overseeing the entire process from development to mobilization.
summaries, decision aids for patientphysician discussions, identifying trustworthy recommendations and guidance on contextualizing them.
Ultimately, the e-Chronic Pain RecMap is expected to promote shared decision-making and support evidence-based management for individuals living with chronic pain.
"The pursuit of evidence-based care for people living with chronic pain is complicated due to the presence of hundreds of guidelines of variable quality often
providing inconsistent recommendations.
My
hope is that the development and dissemination of this RecMap, will help users identify trustworthy recommendations to better align clinical care with current best evidence.”
- Dr. Andrea Darzi
Recommendation map (e-Chronic Pain RecMap). Led by Dr. Andrea Darzi, this project will create a freely accessible digital tool to consolidate and present preappraised recommendations in key areas, including opioid use, cannabis for medical purposes, and interventional procedures for chronic pain. To achieve this, several methods will be employed. First, we will collaborate with national and international
Relevant guidelines are being systematically gathered by employing manual searches of specific websites and conducting a thorough search of electronic databases. Existing infrastructure is being utilized to extract key information, including data aligned with the PROGRESS PLUS framework. Knowledge mobilization activities are being developed with stakeholders, including resources such as plain language

The Pain Symposium, hosted annually by the Michael G. DeGroote Institute for Pain Research & Care (IPRC) at McMaster University, has been pivotal in advancing chronic pain research. The event draws clinicians, researchers, and trainees to explore persistent post-surgical pain as a model for understanding chronic pain. At the 2019 symposium, 11 speakers shared cutting-edge insights. Keynote speaker Dr. Karen Davis from the University of Toronto discussed the use of functional MRI to predict chronic pain relief after treatment. Dr. Jennifer Rabbitts from the University of Washington focused on pediatric post-surgical pain and the transition from acute to chronic pain. Dr. Manon Choinière from the University of Montreal emphasized the need for clinical research beyond randomized controlled trials to improve pain management, while Dr. Mark Lema from the University of Buffalo provided an engaging talk on new developments in chronic pain pathophysiology.
After a two-year hiatus due to the COVID-19 pandemic, the symposium returned as a hybrid event - allowing participants to join both in person
and remotely. The event featured a keynote by Dr. Brice Gaudilliere from Stanford University, who discussed biomarker analysis to predict recovery and post-surgical pain. Other presentations explored risk assessments for surgery, enhanced recovery programs, and pre-surgical rehabilitation. McMaster’s Dr. Gurmit Singh presented compelling research on chronic pain as an autoimmune disease, showing how immune modulation differs between men and women, with testosterone dampening the immune response in males and a stronger immune system impacting pain perception in females.
The 2023 symposium saw Dr. Jason Busse furthering the discussion around opioid use in chronic pain, highlighting the rising number of opioid-related deaths in Canada, as well as identifying risk factors for fatal and non-fatal overdoses after opioid prescriptions. Dr. Kristin Schreiber from Harvard Medical School introduced patient phenotyping and the biopsychosocial model as tools for predicting chronic post-surgical pain. Other notable speakers included Dr. Shirin Modarresi, who focused on managing knee osteoarthritis
through informed movement, and Dr. Peter Emary, who discussed the role of chiropractic care in reducing opioid use for non-cancer spinal pain.
The symposium continues to be a vital platform for collaboration and innovation, pushing the boundaries of chronic pain research and management.
Keynote Speakers over the years include:
• Dr. Manon Choinière
University of Montreal
• Dr. Mike Salter
University of Toronto
• Dr. Matthew Chan
Chinese University of Hong Kong
• Dr. Martin Angst
Stanford University
• Dr. Jane Quinlan
University of Oxford
• Dr. Karen Davis
University of Toronto
• Dr. Brice Gaudilliere
Stanford University
• Dr. Kristin Schreiber
Harvard University


The inaugural Michael G. DeGroote Institute for Pain Research & Care (IPRC) Research Day took place in 2019, bringing together researchers, clinicians, and trainees to discuss pain research advancements and foster collaboration across disciplines. Held on February 14, 2019, at McMaster University, the event showcased a wide range of studies, including NMDA antagonists, cannabidiol for postsurgical pain, and the role of T cells in chronic pain and sex differences. Notable presenters included Dr. Harsha Shanthanna and Dr. Jason Busse, who examined the effects of cannabis legalization and persistent post-surgical pain.
Since then, Research Day has expanded to include contributions from the Department of Pathology, School of Rehabilitation Science, and others. Topics have ranged from post-surgical pain to pain management for veterans and using proteomics and deep learning to predict susceptibility to Complex Regional Pain Syndrome.
After a brief hiatus, the 2022 Research Day returned in a hybrid format at the Royal Botanical Gardens, with Dr. Tara Packham presenting on
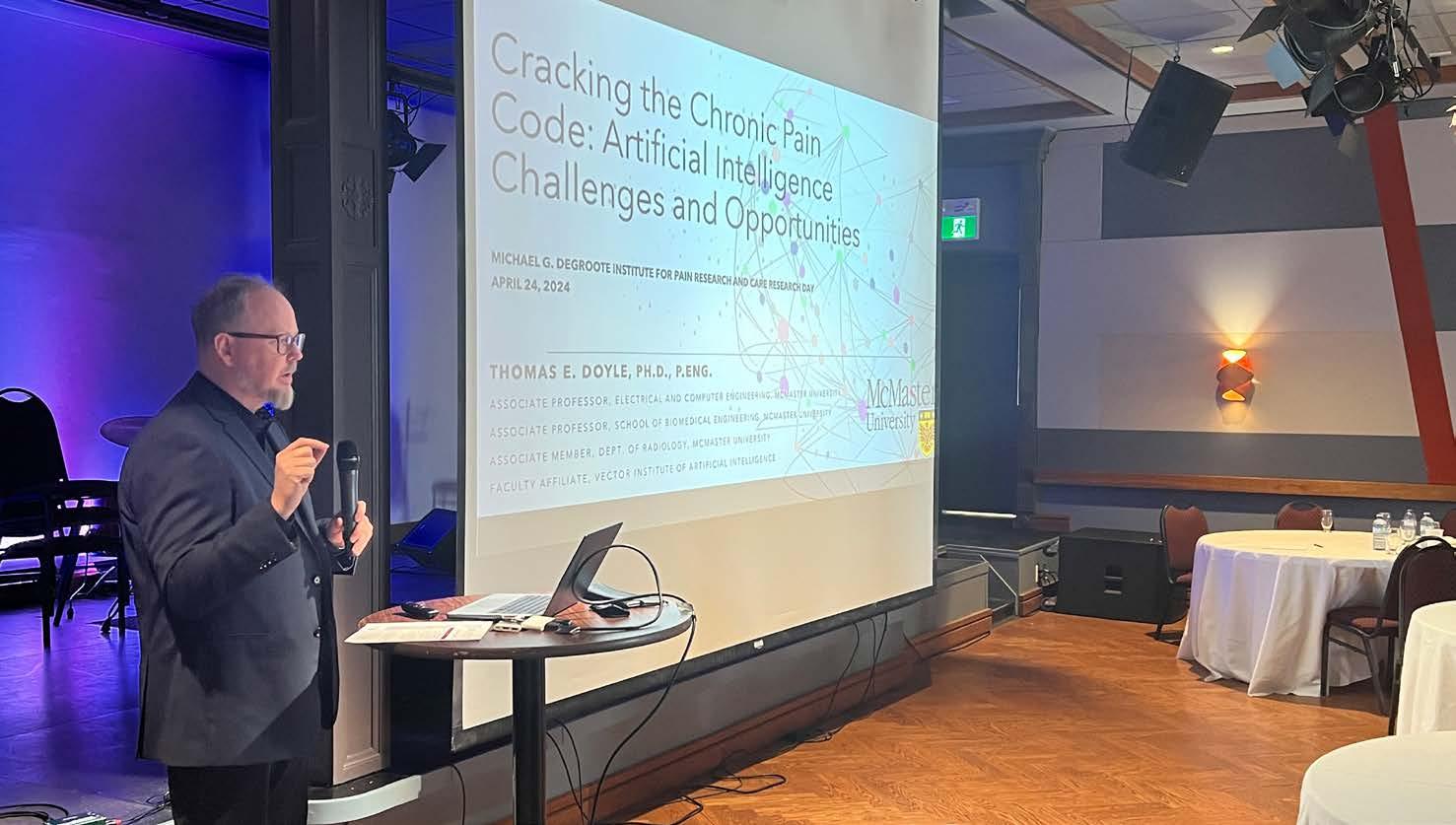
Dr. Thomas E. Doyle, of McMaster’s Department of Computer and Electrical Engineering, discusses the role of artificial intelligence in medicine, health research and chronic pain at the MGD 2024 Annual Research Day.
allodynia and Dr. Parminder Raina highlighting opportunities for pain research in aging populations.
In 2023, Research Day moved to the Rock Garden Bistro, featuring discussions on statin-induced muscular pain, corticomuscular coherence brain-computer interfaces, opioid reduction in surgeries, and the cognitive effects of postoperative pain.
The most recent Research Day was held at The Gas Works in Hamilton.
Dr. Eleni Hapidou opened with a presentation on chronic pain among veteran women, revealing
higher rates than in both civilian women and veteran men. Other topics included childhood anxiety in medical contexts, skeletal muscle damage in Type 1 Diabetes patients, and AI’s role in pain research. The event continued to demonstrate how pain research is evolving across disciplines, with presentations on pain mechanisms in knee osteoarthritis and biomarkers for aging-related chronic pain processes.
Established in 2016, the Canadian Pain Care Forum (CPCF) is a collaborative initiative focused on advancing pain care and education across Canada. It brings together healthcare professionals, researchers, and individuals with lived experiences of chronic pain to promote knowledge exchange, research collaboration and policy advocacy.
Speakers have included a wide range of people. Katie Gasparelli, (Six Nations Health Services) discussed McMaster University’s Pain Program, focusing on Indigenous experiences with chronic pain. Dr. Fiona Campbell (University of Toronto) and Maria Hudspith (PainBC) , co-chairs of the Canadian Pain Task Force, provided an overview of the work that group. The Task Force developed a comprehensive national pain strategy, emphasizing interdisciplinary care that includes the voices of people living with pain.
During the COVID-19 pandemic, CPCF meetings transitioned from a hybrid format to online, with a heightened focus on improving pain education for healthcare professionals. Early 2021 discussions included Dr. Lisa Graves and Fran Kirby, addressing the opioid crisis and a new curriculum
for better physician training. Other speakers have highlighted the gaps in pain education for nurses and psychologists.
The forum presented on the importance of interdisciplinary pain care. Presentations included Dr. Hillel Finestone’s nurse-led pain management program and discussions on equity in care led by Dr. Jennifer Nash and Dr. Fiona Webster. These discussions examined the challenges marginalized populations face in accessing adequate pain care.
In 2023, initiatives like the Power Over Pain Portal and the Circa Pain Project were highlighted, exploring individual pain experiences and non-pharmacological approaches to pain management.
Most recently, presenters have included Julie Masse and Dr. Joanne Higgins, discussing the role of occupational therapy in chronic pain management; Dr. David Flusk, highlighting interdisciplinary approaches in the Atlantic Mentorship Network; Virginia McIntyre, of the People in Pain Network, sharing her story as a chronic pain patient; Veteran and advocate Tom Hoppe, addressing the unique challenges faced by
Veterans in managing pain; Ontario Provincial Police Detective Constable Chris Auger, providing an overview of prescription drug diversion in Canada and Susan Tupper, of Saskatchewan Health Authority, looking at graphic storytelling to challenge stigma with chronic pain and substance use.
Over the years, a reoccurring theme has been the need for increased funding for pain research, as, historically, less than 1% of the Canadian Institutes of Health Research’s budget has been allocated to this area. With more than 130 members representing 80 organizations, the CPCF continues to push for improved pain care through collaboration, advocacy and education across Canada.
In the coming year, the Canadian Pain Care Forum aims to strengthen its engagement with policymakers, advocating for the implementation of the Canadian Pain Task Force’s findings into actionable policy. Our goal is to ensure these recommendations translate into meaningful changes that improve pain care across the country.
A collaboration between McMaster University and St. Joseph’s Healthcare Hamilton, the Michael G. DeGroote Centre for Medicinal Cannabis Research (CMCR) leverages world-class scientists and acclaimed expertise in health research and evidence-based medicine to advance the science of medical cannabis, assessing its potential benefits and risks. Since 2017, it has united nearly 50 McMaster faculty and initiated 26 research projects.
The Centre’s vision is to establish a research-based understanding of medical cannabis, encompassing its therapeutic effects and potential risks. Its mission revolves around three key strategies:
1. Curating existing literature to determine the state of evidence.
2. Conducting cutting-edge research for generating new evidence.
3. Establishing a network of cannabis researchers to support its vision.
The Centre’s commitment to advancing medical cannabis knowledge is reflected in its funded external grants totaling $7.54 million, supporting topics like cannabis and psychosis, metabolism, pain management, anxiety, and more. Recently, the CMCR

is also leading the Canadian Medical Cannabis Clinical Trials Network, which seeks to meaningfully connect cannabis researchers and experts across the country.
Communications, Events and Continued Education
The Centre continues to prioritize outreach via its communication channels, enhancing knowledge sharing on medicinal cannabis through revamped social media and newsletters.
This past year saw the launch of the CMCR launch its new knowledge translation initiative known as “Bud
Talks.” A character named Bud presents scientific evidence to a mainstream audience in an approachable, engaging way. Medical cannabis patients are currently receiving information from a variety of sources who may not have received specialized training on cannabis. “Bud Talks” combines the expertise of researchers, clinicians, learning design specialists and a team of talented animators to breakdown the latest cannabis research in a way that is accessible to everyone.
To learn more about Bud Talks, visit: budtalks.ca
The Chronic Pain Centre of Excellence for Canadian Veterans (CPCoE) is honoured to have a collaborative relationship with the Michael G. DeGroote Institute for Pain Research and Care (IPRC). The IPRC was integral to the creation of the CPCoE and embedded our organization with a focus on the importance of working with people with lived experience. The CPCoE continues to uphold this principle of engagement and have recently adopted a new priority setting process. Using a process based on the work of the James Lind Alliance, the CPCoE solicited issues of importance from the Veteran, clinician and policymakers’ stakeholders. The research team then explored these issues with the assistance of their Advisory Council for Veterans (ACV) and then prioritized the areas to be explored through research. Through this challenging but rewarding process, the ACV identified top research priorities for the CPCoE that will help set the scientific direction for their research over the next few years. In fiscal year 2023-2024, the CPCoE funded 10 new research projects bringing the total number of active research projects focused on chronic pain in Veterans to 34.

To date, the CPCoE has partnered with a total of 29 different research institutions across Canada as well as in the United States and Australia. To accelerate the knowledge mobilization of research findings, the CPCoE actively collaborates with funded researchers to support the development and dissemination of knowledge mobilization resources. Knowledge mobilization projects can include anything from lay summaries of projects and presenting at conferences to more interactive ones, such as courses for journalism students and interactive videos.
The IPRC looks forward to working with the CPCoE to reach new milestones in the goal of keeping hope alive through Veteran-first chronic pain research.
To learn more about the CPCoE visit: http://veteranschronicpain.ca
This past year marked a significant period of growth and achievement for the Chronic Pain Network (CPN), as we successfully completed the second year of our Knowledge Mobilization Implementation Science focused grant. A key highlight was the addition of Rachel Roy, our new Knowledge Broker based at McMaster University. Rachel’s immediate contributions were evident with the launch of our In Motion series, which distills the research outcomes of CPN-funded projects into accessible, publicfriendly formats.
CPN hosted a high-profile breakfast panel at the inaugural Canadian Pain Society/Health Canada National Congress on Pain in Ottawa. This event provided a crucial platform to showcase CPN’s work to federal policymakers, including the Hon. Ya’ara Saks, Minister of Mental Health and Addictions. The panel featured insightful contributions and discussion from Drs. Rachael Bosma, Norm Buckley, and Nader Ghasemlou, along with Jennifer Daly-Cyr, a person with lived experience and co-chair of the CPN Executive committee, further underscoring the importance and impact of our initiatives.

Left to Right: Dr. John Pereira (President of the Canadian Pain Society), The Honourable Ya’ara Saks, Dr. Norm Buckley, Tania Di Renna (Medical Director of the Toronto Academic Pain Medicine Institute (TAPMI)), Kate Nicholson (Executive Director of the United States National Pain Advocacy Centre), Dr. Hance Clarke (President Elect of the Canadian Pain Society), Maria Hudspith (Director of PainBC), Virginia McIntyre (President of the People in Pain Network) and Jennifer Daly Cyr (patient partner with the Chronic Pain Network) at a meeting held in Ottawa following the National Congress on Pain.
Looking ahead, CPN anticipates several accomplishments in the coming year. Our annual meeting in October will debut our firstever hackathon for trainees, where teams will tackle challenges outlined in the Action Plan for Pain in Canada, with a strong emphasis on knowledge mobilization. Another milestone will be the official launch of Pain Connect during National Pain Awareness Week (NPAW) in November, a dynamic new hub designed to link researchers with individuals living with pain. Additionally, during NPAW, we will co-host a virtual panel event on chronic pain with Research Canada and the Parliamentary Health Research Caucus.
Stay connected and informed by visiting our newly updated website: https://cpn-rdc.ca/
Collaboration is an essential dimension of research. It brings together diverse expertise and perspectives from different cultural and clinical contexts. It allows for the sharing of ideas, data, best practices, research methodologies and even solutions, accelerating discoveries and ensuring projects are relevant to broader audiences - across disciplines, across conditions and across countries.
The Institute for Pain Research and Care continues to strive towards creating meaningful opportunities to
collaborate at the institutional level within McMaster; at the national level, engaging with researchers across the country; and at the international level, forming relationships with health researchers abroad to include more diverse populations, addressing widespread issues and incorporating new best practices and approaches.
This year, saw the Institute form partnerships across Canada, at postsecondary institutions like Western University, the University of Toronto,
Queen’s University, the University of Montreal, the University of Alberta and the University of British Columbia; as well as around the world, in countries like the United States, Australia, the United Kingdom, Iran, Switzerland, China, Denmark, Netherlands, Norway, Brazil, Ireland, India, Spain, Greece, Poland, Germany, Finland, Italy and Sweden. Institute research and collaborations have produced more than 340 publications since 2018, resulting in more than 5,000 citations.
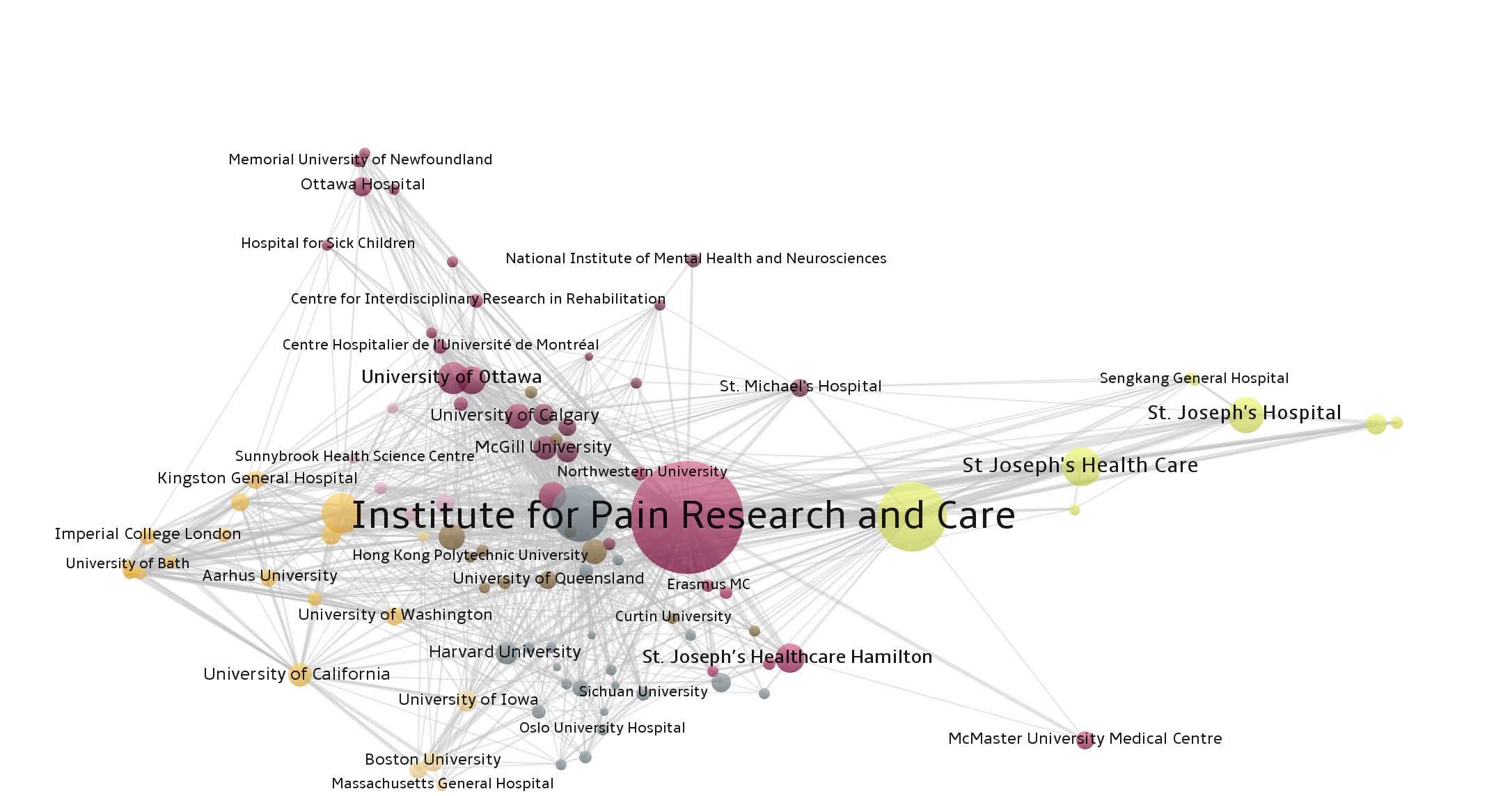
The Institute for Pain Research and Care has produced more than 300 publications since 2018, with more than 1,800 co-authorships and representing collaborations with more than 50 organizations and institutions.

“The IPRC serves as an interdisciplinary incubator for trainees. Reflecting the diversity of our members, students from different programs and professional backgrounds are engaged and mentored in our work. They gain valuable experience in conducting research built on innovation, robust methods, patient engagement and multidisciplinary collaborations across the Faculty of Health Sciences and beyond.”
- Dr. Tara Packham
Assistant Professor, School of Rehabilitation Science and 2017 Pain Fellowship Recipient
Over the last 20 years, the Institute for Pain Research and Care (IPRC) has been instrumental in laying the groundwork for several key initiatives that have advanced pain research in Canada. A prime example of this is the Canadian Pain Task Force (CPTF), which arose out of a deliberative dialogue, held in conjunction with the McMaster Health Forum and the IPRC’s Canadian Pain Care Forum (CPCF). Attendees, which included people with lived experience, identified key steps needed to begin the process of creating a national pain strategy. Insights gained during the discussion inspired Health Canada to form the CPTF, an important body responsible for providing recommendations on pain care policies across the country. The IPRC’s Scientific Director, Norm Buckley, served as a member of the external advisory panel for the Task Force, helping to shape its direction and impact. Beyond its work on national pain policy, the IPRC hosts and was a key part of establishing the Chronic Pain Network (CPN), one of five research networks funded through the Strategy for Patient Oriented Research, which engages people with lived experience actively as partners throughout the research process to ensure Network-funded research is relevant to the needs of patients and that outcomes are directly applicable to improving patient care, access to treatment and health outcomes. Acting as the host institution, the IPRC provided logistical support—such as staffing and office space—and strategic guidance to ensure the Network’s success. Further expanding its influence, the IPRC helped support the development of the Chronic Pain Centre of Excellence for Canadian Veterans (CPCoE). This Centre focuses on the unique pain management needs of veterans, blending research, clinical care and educational initiatives to improve outcomes for those who have dedicated their lives serving our country.
Twenty twenty-four marks 20 years since the founding of the Institute for Pain Research and Care, and 10 years since the Institute launched its fellowships, studentships and seed grant awards. Since 2014, the IPRC has provided more than $870,000 in funding to 11 pain fellows, who represent seven different disciplines and have authored more than 462 publications. It has provided more than $260,000 in funding through 13 graduate studentships. And it has provided 29 research projects with more than $865,000 in funding. One of the key initiatives aimed at promoting groundbreaking research is the Catalyst Grant, introduced in 2019. This joint effort with McMaster’s Institute for Research on Aging (MIRA) supports interdisciplinary studies exploring novel pain treatment methods. IPRC awards have funded projects that span a wide range of approaches to pain management. For instance, the Topicals for Osteoarthritis
Pain In Knee Surgery (TOPIKS) trial is examining the use of topical treatments postknee surgery. Other studies, such as Opioid Reduction in Orthopedic Surgery (OREOS), explore strategies to minimize opioid use in following surgery, critical to addressing the ongoing opioid crisis. The IPRC is also leading research on cannabinoids and their potential in pain management. One such project investigates the Analgesic Effects of Cannabinoids in an Animal Model of Post-Surgical Chronic Pain, particularly examining sex differences in response to treatment. This exploration into sex-based differences extends to other studies, including one on the Neuroprotective Mechanisms of Progesterone and Pregabalin for treating chronic neuropathic pain. With its commitment to advancing the understanding of pain, the IPRC has also embraced cutting-edge technologies. Projects like the use of Artificial Intelligence to Understand the Biological Mechanisms of Chronic Neuropathic Pain and the development of a Corticomuscular Coherence Brain-Computer Interface for treating chronic neck pain highlight the Institute’s drive to innovate. Through its research initiatives, the IPRC seeks to improve pain management for those living with chronic pain and guide future researchers in developing evidence-based treatments.
McMaster University receives an unprecedented donation of $105 million from Michael G. DeGroote. The Institute for Pain Research and Care is founded.
The Institute for Pain Research and Care establishes Pain Postdoctoral Fellowships, Graduate Studentships and Seed Project Awards.
The Institute for Pain Research and Care becomes the host institution and home of the coordinating centre for the Chronic Pain Network - one of five national networks addressing chronic disease, funded through the Strategy for Patient Oriented Research.


McMaster University and St. Joseph’s Healthcare Hamilton launch the Michael DeGroote Centre for Medicinal Cannabis Research, which becomes partner to the Institute in funding medicinal cannabis research for a total million. The National Pain Centre releases the Opioid Guideline for Chronic Non-Cancer Pain.. partner to the Institute in funding the Medicinal Cannabis Research for a total
In April, the Honorable Ginette Petitpas-Taylor announces the Canadian Pain Task Force and its External Advisory Panel, which includes Dr. Norm Buckley. In July 2019, the Honorable Lawrence MacAulay visits McMaster to announce the Chronic Pain Centre of Excellence for Canadian Veterans, seeking to develop therapies for health professionals nationwide.
The National Pain Centre receives funding from Canadian Institutes of Health Research (CIHR) to develop a guideline for medical cannabis use to treat chronic pain. the Medicinal partner to the Institute in funding medicinal cannabis research for a total million. The National Pain Centre releases the Opioid Guideline for Chronic Non-Cancer Pain.
The Chronic Pain Network receives additional funding to support Knowledge Translation efforts. The National Pain Centre receives funding from Substance Use and Addiction Program to update the Opioid Guideline for Non-Cancer Chronic Pain.

eChronic Pain Recommendation Map receives $750,000 in funding from CIHR. National Pain Centre finalizes revisions to the Opioid Guideline for Non-Cancer Chronic Pain.

“In the next 10 years, I would like to see the IPRC and NPC achieve groundbreaking advancements in pain research and management. Establishing conditions that leverage AI and novel technologies will position them as flagship institutions in pain research and evidence synthesis. This strategy will drive innovative, evidence-based treatment protocols, foster international collaborations, and support interdisciplinary research initiatives.”
- Dr. Malahat Khalili 2022 Pain Fellowship Recipient
“The IPRC Graduate Studentship has provided me direct financial support to pursue research training and project work focused on guideline development pertaining to pain research. It has also connected me to a broader network of talented trainees, clinicians, and researchers.”
- Arnav Agarwal

Arnav Agarwal, BSc Masters Student
Project Titles: The development of trustworthy guidance addressing whether spinal fusion surgery, when added to spinal decompression, improves patient-important outcomes among individuals with low back pain related to lumbar spinal stenosis and spondylolisthesis
Supervisor: Dr. Jason Busse
The proposed work was a trustworthy practice guideline regarding spinal decompression with or without fusion surgery for adults with low back pain related to lumbar spinal stenosis and spondylolisthesis. Landmark longitudinal five-year data from a multi-centre, non-inferiority randomized trial has been published in recent months, officially triggering initiation of the Rapid Recommendation process. A multi-disciplinary, unconflicted guideline panel has been identified and invited to participate. Linked systematic reviews and meta-analyses have been initiated to inform the guideline, one including randomized trials evaluating benefits and harms of spinal decompression with versus without fusion surgery; and another of observational studies regarding infrequent and serious harms. The guideline panel will be convened shortly, initially to define the definitive clinical question, any subgroups of interest and values and preferences of average patients that will underly recommendations; and subsequently to review summaries of available evidence and to move from evidence to recommendations. We anticipate completion of this work by early spring 2025. Evidence summaries and associated practice guidance will be made available via MAGICapp, and recommendations will be cross-published in The BMJ with an international readership, accompanied by interactive visual infographics and decision aids for shared decision-making.
Stevie Foglia, BSc
PhD Candidate
Project Title: Understanding the mechanisms that underpin the development of chronic post-surgical pain; predicting risk using neurophysiology and predictive modeling
Supervisor: Dr. Harsha Shanthanna
Brief Overview and Progress to Date
Chronic post-surgical pain (CPSP) following thoracic surgery has been shown to be one of the most prevalent with an incidence of 30-50% following both thoracotomy and thoracoscopy procedures. CPSP is a debilitating condition associated with depression, anxiety, and decreased quality of life. Despite this, challenges remain in identifying accurate preoperative risk factors that may predict the development of CPSP following thoracic surgery. Transcranial magnetic stimulation (TMS) and electroencephalography (EEG) offers an opportunity to investigate neurological biomarkers that may contribute to the development of CPSP. The goal of this project is to identify pre-operative risk factors that may make some more likely to develop CPSP. The goal of this project is also to investigate cortical changes associated with the genesis of CPSP. This project has been submitted to the Hamilton Integrated Research Ethics Board and study recruitment is planned to commence in August 2024.
“The IPRC funding has been integral in supporting my PhD and allowing me to conduct my research in chronic post surgical pain. The support has allowed me to gain the skills and knowledge necessary to conduct the research.”
-

“Our IPRC funding is instrumental in helping us to establish feasibility of a definitive trial, which if successful will be critical to supporting a grant for a definitive cluster RCT.”
- Peter Emary

Peter Emary, DC
Postdoctoral Fellow
Project Title: Impact of Chiropractic Care on Opioid Use for Non-Cancer Spinal Pain: A Systematic Review and Pilot Cluster Randomized Controlled Trial
Supervisor: Dr. Jason Busse
Brief Overview and Progress to Date
This past year, I was awarded funding in excess of $200,000 from the CIHR, the Michael G. DeGroote IPRC, and the Canadian Chiropractic Research Foundation to support our pilot cluster RCT on the impact of chiropractic care on opioid use among adults with chronic non-cancer spinal pain. This trial has been registered on ClinicalTrials.gov (ID: NCT06160947), and we are currently working with Dr. Sheila Sprague, PhD and her team at the Surgical Methods Centre at McMaster University to finalize our study protocol and data collection forms. We are also preparing a submission for ethics approval. We have successfully engaged four Ontario Community Health Centres (CHCs) in Cambridge, Kitchener-Waterloo, Guelph, and Cornwall to participate in our pilot trial. Our next step is to train physicians at each CHC on trial-related activities and Good Clinical Practice guidelines. Our aim is to conduct onsite initiation visits and enroll our first trial participants in December, 2024.
Malahat Khalili, MSc, PhD Postdoctoral Fellow
Project Title: Comparative effectiveness of pharmacological prophylaxis for chronic migraine: a systematic review and network meta-analysis of randomized controlled trials Supervisor: Dr. Behnam Sadeghirad Brief Overview and Progress to Date
We have conducted a network meta-analysis (NMA) on pharmacological prophylaxis for migraine management. The research includes 185 RCTs with 41,642 participants, aiming to provide insights into the most effective and tolerable interventions for preventing migraines. Key findings indicate that calcium channel blockers, CGRP antagonists, and beta-blockers are among the most effective treatments for reducing monthly migraine days The results highlight the importance of these pharmacological treatments in managing chronic migraines and provide a hierarchy of their effectiveness based on high to moderate certainty evidence. Clinicians can use our findings to prescribe and decide the best treatment for patients based on their profiles. The primary draft of the manuscript is ready.
I am also working on another NMA focused on pharmacological prophylaxis for patients with a history of preventive treatment failure; findings would be interesting for clinicians in this topic.
“The IPRC award has allowed me to concentrate fully on my research, providing a valuable opportunity to collaborate with experts and significantly advance my NMA project on migraine management.”
- Dr. Malahat Khalili

“This study will facilitate the development of a robust prognostic model to guide clinical decisions or enrolment in interventional studies, with the ultimate goal of identifying pathways for effective prevention and management of chronic pain after knee replacement surgery.”
- Dr. Behnam Sadeghirad

A systematic review and individual patient data (IPD) meta-analysis of perioperative prognostic factors associated with chronic pain after total knee arthroplasty and development of a risk prediction model
Primary Investigator: Behnam Sadeghirad, Pharm.D., M.P.H., Ph.D.
Co-Investigator: Jason Busse, DC, PhD
Start Date: 2023
Mac-PROSPER project aims to perform a systematic review of prospective randomized and nonrandomized studies to identify eligible data, design and develop an international repository of individual patient data for perioperative prognostic factors of chronic post-surgical pain after TKA, and develop and validate a prediction model for the development of chronic pain after knee replacement surgery. We have recruited an international group of researchers willing to collaborate on this project and have acquired commitments from investigators to provide access to their ongoing or completed study data which exceeds 22,000 patients. We have developed a website (https://mac-prosper.ca) for the project that provides details of our plans, collaborators, data sharing requirements, and resources available for knowledge users, and current and future collaborators.
Primary Investigator: Jason Busse, DC, PhD
Start Date: 2020
An influential survey of 5,130 patients attending 10 outpatient chronic pain clinics found that 23% attributed their complaints to a surgical procedure. According to Google Scholar, this survey has been cited over 350 times; however, there are limitations with this report. The sample was restricted to patients in North Britain, there are no details reported regarding the response rate, and the data was acquired between 1989 and 1992. These issues suggest that generalizability to the current Canadian context is uncertain. We surveyed 756 Canadian adults living with chronic pain to establish to what cause they attributed the development of their pain, and what interventions they have pursued and perceived effectiveness.
Due to the complexity of collected data on chronic pain, there were some inconsistencies on initial data analyses. As such, we have reviewed the validity of multiple variables and other strategies with investigators and researchers to ensure accurate regression analysis and other statistical analyses. We are now creating and organizing data into tables and figures, in order to finalize the manuscript for publication.
“Surgery is a controlled injury and allows an opportunity to understand the genesis of chronic pain. Our survey will help inform this issue, and identify which interventions have been associated with improvement.”
- Dr. Jason Busse

“Cannabis products are increasingly used to manage pain, but often with little empirical evidence. Our pilot trial will provide critical information about the feasibility of a definitive trial to explore the effectiveness of cannabidiol for reducing persistent pain after total knee replacement.”
- Dr. Jason Busse
Feasibility of a Definitive Trial to Evaluate the Effect of Cannabinoid Oil, Versus Placebo, on Chronic Pain Post-Surgical Pain and Functional Outcomes in Patients Undergoing TKA
Primary Investigator: Jason Busse, DC, PhD Start Date: 2017
Brief Overview and Progress to Date
We were funded to launch a pilot randomized controlled trial of cannabidiol (CBD; a non-psychotropic cannabinoid) vs. placebo for patients undergoing total knee replacement. Demonstration of feasibility would support a definitive trial to explore the effectiveness for reducing persistent post-operative pain. A complication that we estimate affects 1 in 4 patients.
Our efforts were complicated as Health Canada only requires that cannabis producers adhere to Good Production Practices (GPP) in order to sell to consumers, but require products that are compliant with Good Medical Practices (GMP) for use in a clinical trial. The latter is a much higher bar, and after meeting with close to 200 producers we were unable to find any that had developed a GMP product. We were not alone, and other groups attempting randomized trials of cannabis products had been similarly affected.
In response, we arranged for an open letter signed by 200 scientists across Canada to Heath Canada alerting them to this problem.
In response, Health Canada changed their regulations to permit use of GPP cannabis products in pilot trials. We have now completed enrollment of 40 patients undergoing total knee replacement, randomized to CBD or placebo, and are completing follow-up. We anticipate completion of our trial in 2025.
Advanced controlled transcranial magnetic stimulation to modulate neural plasticity and alleviate pain in diabetic neuropathy’ and uses a new TMS technology that aims to reduce pain symptoms in diabetic neuropathy
Primary Investigator: Aimee Nelson, PhD
Start Date: 2023
Brief Overview and Progress to Date
The goal of the research is to improve symptoms of pain in individuals living with painful diabetic neuropathy. In a double-blinded cross-over design, individuals will receive two weeks of real or sham non-invasive brain stimulation, followed by a washout period, followed by the opposite brain stimulation (real or sham). Measures of pain intensity, and neurophysiological measures are performed before and after each arm of the intervention. To date, we have acquired data from ~6 participants.
“Funding from IPRC has allowed this pilot study to occur - these funds have been used to pay transportation costs to and from McMaster and provide study honorariums. The funds have also been used to purchase a biothesiometer for an objective assessment of vibrotactile perception.”
- Dr. Aimee Nelson

“Using AI one can predict the electrophysiological patterns of neuropathic pain.”
- Dr. Gurmit Singh

Artificial Intelligence to Improve Understanding of the Biological Mechanism(s) of Chronic Neuropathic Pain
Primary Investigator: Gurmit Singh, PhD
Start Date: 2022
Brief Overview and Progress to Date
The project was based on computer modelling using experimental data from electrophysiological studies in an animal model of neuropathic pain. We used the Huxley model to fit data to the sodium channel Nav1.8. This was the first study to accurately predict the functionality of sodium channel using experimental data.
Publications: https://doi.org/10.3389/fncom.2024.1327986
A Pilot Study of Association of BIOmarkers and Neuropathic Pain with Intercostobrachial Nerves
Sparing in breast surgery to improve Persistent post-surgical pain-an International RandomizEd controlled trial (BIO-INSPIRE)
Primary Investigator: Harsha Shanthanna, MD, PhD, FRCPC
Start Date: 2021
Brief Overview and Progress to Date
BIO-INSPIRE is a feasibility study that evaluated cytokine levels of IL-1β, IL-6, and TNFα and neuropathic pain in patients participating in the INSPIRE study (a multicentre pilot study of 50 patients to establish the effect of intercostobrachial nerve preservation on persistent post-surgical pain following breast cancer surgery) and underwent axillary lymph node dissection during breast cancer surgery. The INSPIRE study recruited participants from two hospitals in Canada and two hospitals in India and 46 of the 50 patients were included in the BIOINSPIRE study. Study samples of BIOINSPIRE were analyzed at Hamilton (Canada) and Bangalore (India) separately. We plan to publish the study results in the next few months.
for Pain Relief After Caesarean Section
Primary Investigator: Harsha Shanthanna, MD, PhD, FRCPC
Start Date: 2023
Brief Overview and Progress to Date
In this RCT, 180 pregnant women planned for elective CS will be randomized to receive either active or inactive
PBMT. Pain outcomes along with wound healing, post natal depression and chronic post surgical pain will be collected.
So far, we have randomized 85 of 100 patients recruited (50% of the target). The study has been going well. We plan to complete the study in the next 6-12 months.
“The funding from IPRC has been an important source of support and encouragement.”
- Dr. Harsha Shanthanna

for Osteoarthritis Pain in Knee Surgery (TOPIKS): A Pilot Randomized Controlled Trial
Primary Investigator: Harsha Shanthanna, MD, PhD, FRCPC
Start Date: 2019
Brief Overview and Progress to Date
Topicals for Osteoarthritis Pain In Knee Surgery (TOPIKS) is a proposed pilot trial evaluating the effect of topical cannabis (CBD) with or without non-steroidal anti-inflammatory drugs (NSAIDS) as against placebo. The trial has not yet been started because of the regulatory (Health Canada) requirements necessary for a Cannabis based trial. We also had challenges in obtaining the product from a suitable manufacturer. Presently, we are working with Dr. Joseph Gabriele of Delivra and we are testing the CBD patches for safety. This is a crucial step in obtaining Health Canada approval for the study. We are hopeful that we will be ready to apply for regulatory approval and start the study in the next 12-18 months.
Primary Investigator: Harsha Shanthanna, MD, PhD, FRCPC
Start Date: 2022
Brief Overview and Progress to Date
The main objective of this pilot trial is to assess the feasibility of a multicomponent pathway on patients having elective total knee arthroplasty, while the clinical objectives are to determine the effects of the pathway on opioid-free pain control, persisting pain and opioid use, functional knee outcomes, quality of life, and return to function. Patients in the intervention group will undergo a multicomponent intervention pathway that will be facilitated by an intervention coordinator linking each patient and their surgical/ perioperative team.
Full recruitment and follow up has been completed. 100 patients were recruited from 3 centres, with 56% of them being women. Nearly one third patients reported increased pain after knee arthroplasty with 17% qualifying as CPSP. We demonstrated that a largescale trial comparing our intervention pathway is feasible. We will be applying for the main study grants.
An Investigation into the Effectiveness of a New Transitional Pain Service (TPS) on Opioid Cessation After Broad Range of Surgeries Done at Hamilton Health Sciences (HHS) and its Affiliated Hospitals
Primary Investigator: James Paul, MD, MSc, FRCPC
Start Date: 2019
Brief Overview and Progress to Date
Hamilton Health Sciences (HHS) affiliated hospitals use the Transitional Pain Service (TPS) model. Collecting data from the Acute Pain Service (APS), TPS and chronic pain clinic, our retrospective study seeks to elucidate risk factors associated with the development of chronic post-surgical pain (CPSP) and long-term opioid use and evaluate the efficacy of TPS in reducing opioid use in the Hamilton-Niagara Region.
Very few studies have taken a comprehensive largescale approach in assessing whether a TPS is more effective at getting patients off opioid analgesia (in comparison to patients in a control group with usual pain care), instead choosing to examine the incidence of and risk factors for developing CPSP. Results from our study will provide additional evidence for TPS as a standard of care for managing CPSP, decreasing opioid use and giving insight into the role of the pain clinician’s increasing role in the opioid crisis.
“The IPRC funding has enabled us to develop the tools necessary to evaluate our newly established Transitional Pain Service to see if it’s achieving its objective of providing high quality analgesia to our complex pain patients and assisting them in transitioning off opioid analgesia after surgery.”
- Dr. James Paul

“The IPRC-MIRA funding has allowed to start my program on the relationship between pain and cognition in older people, in the perioperative setting.”
- Dr. Maura Marcucci

Who is Susceptible to Developing CPSP? A HighThroughput Clinical Proteomics-Based Approach for the Prediction of Susceptibility
Primary Investigator: Maura Marcucci, MD, MSc Start Date: 2021
Brief Overview and Progress to
The ArthroCaP project is a mixed methods study exploring the association between chronic postsurgical pain and cognitive decline in ≥50 years old patients who are undergoing total arthroplasty. The quantitative part is a cohort study of patients who are longitudinally followed after surgery and assessed remotely upon their pain and cognitive function; it includes also the evaluation of biomarkers associated with pain and cognitive dysfunction. We just closed the study with the completion of the 1-year follow-up for the last participant. We recruited 93 participants, of whom, 67 completed the 1-year visit. 30 participants consented to the biomarkers evaluation. We obtained extension of the project timeline (at the same funding). We are currently cleaning the database for analyses for the first publication. Given the disruption due to the pandemics we decided to put the qualitative component of the study (which would explore expectations and lived experience with surgery) on hold.
Primary Investigator: Matiar Howlader, B.Eng, PhD
Start Date: 2023
Aging and chronic diseases are closely intertwined. As we grow older, our bodies experience significant cellular and molecular damage. Conditions such as diabetes, cancer, Post-Traumatic Stress Disorder (PTSD), and depression often accompany chronic pain, making diagnosis and management challenging due to the pain’s invisible nature and the variability in patientreported scales. To address these challenges, this project aims to develop electrochemical sensors for biomarker detection, revolutionizing the diagnosis of chronic pain and aging-related health issues. We are working on creating and validating electrochemical technology for the quantitative monitoring of biomarkers, with the goal of correlating this data with pain treatment efficacy for personalized pain management. However, the start of the project was delayed due to difficulties in finding a suitable postdoctoral fellow to carry out the research. The project officially began on December 18, 2023.
“These biosensors will enable personalized medicine, monitor pain medication effects, and offer an affordable device for home and clinical use, tracking pain and alternative therapies like yoga and mindfulness.”
- Dr. Matiar Howlader

“IPRC has been instrumental in allowing for this important work to occur by providing funds to accommodate the participants costs associated with travel to and from McMaster and parking expenses.”
- Dr. Aimee Nelson

Corticomuscular Coherence Brain-Computer Interface to Treat Chronic Neck Pain
Primary Investigator: Aimee Nelson, PhD
Start Date: 2022
Brief Overview and Progress to Date
This project aims to reduce pain in individuals living with chronic neck pain. Using a combination of augmented reality sensorimotor training targeting the muscles of the neck and head movement, combined with non-invasive brain stimulation, the goal is to increase the range of motion of head movements and reduce the perception of pain. This work involves participants allocated to receive either real or placebo brain stimulation immediately prior to augmented reality sensorimotor training of the neck. It is anticipated that the real brain stimulation group will experience greater benefits than those experienced by the placebo brain stimulation group.
A Feasibility Study to Assess the Added Value of Integrated Musculoskeletal BioFeedback Device (IMBED) Combined with Neuromuscular Exercise and Education (GLA-Dtm) to Decrease Chronic Pain in Older Adults with Osteoarthritis
Primary Investigator: Pasqualina Santaguida, PhD, PT, Stuart Phillips, PhD, MSc, BSc and Qiyin Fang, BSc, MSc, PhD, LEL
Start Year: 2020
Brief Overview and Progress to Date
The goal of our research project was to use technology to improve training in a group exercise format and evaluate the impact on patient outcomes. We developed a system to capture muscle activity and motion (IMBED) but found it did not work well in a group exercise format setting. We have switched technologies and are now adapting an artificial intelligence (AI) based technology in the osteoarthritis exercise group training. Early results of our user testing of patients and clinicians find the MOTRACK acceptable. We are preparing for the commencement of a pilot feasibility trial to evaluate the impact on patient outcomes and clinician acceptability with the MOTRACK.
“The funding has allowed us to develop and explore two types of technology to monitor movement while performing a standardized group exercise program. We will shortly start the pilot trial to evaluate effects on patient training outcomes and acceptability to patients and clinicians for the use of MOTRACK.”
- Dr. Pasqualina Santaguida

Norm Buckley
Scientific Director, Michael G. DeGroote Institute for Pain Research and Care; Professor Emeritus, Department of Anesthesia, McMaster University
Eugene Maida
Medical Director, Michael G. DeGroote Pain Clinic; Assistant Clinical Professor, Division of Physical Medicine & Rehabilitation, Department of Medicine; Assistant Clinical Professor (Adjunct), Department of Anesthesia, McMaster University
Manon Choinière
Professor, Centre de recherche du Centre hospitalier de l’Université de Montréal
Mark Lema
Professor and Chair, Department of Anesthesiology, Jacobs School of Medicine & Biomedical Sciences State University of New York, Buffalo
Jason Busse
Professor, Department of Anesthesia; Director, Michael G. DeGroote National Pain Centre; Joint Member, Department of Health Research Methods, Evidence and Impact (HE&I), McMaster University; Canada Research Chair in Prevention & Management of Chronic Pain
Luciana Macedo
Assistant Professor, School of Rehabilitation Sciences, Institute for Applied Health Sciences, McMaster University
Ian Rodger
Professor Emeritus, Department of Medicine, McMaster University
Ian Gilron
Director of Clinical Pain Research, Professor of Anesthesiology and Biomedical Sciences, Faculty in the Centre for Neuroscience Studies at Queen’s University
Mike Salter
Professor, Departments of Physiology and Institute for Medical Sciences and Faculty of Dentistry, University of Toronto
Joel Katz
Distinguished Research Professor of Psychology, Canada Research Chair in Health Psychology York University
Lisa Carlesso
Associate Professor, School of Rehabilitation Sciences, McMaster University
Michael McGillion
Associate Professor and Assistant Dean Research, School of Nursing, Heart and Stroke Foundation/Michael G. DeGroote Endowed Chair of Cardiovascular Nursing Research, McMaster University
Gurmit Singh
Professor, Department of Pathology and Molecular Medicine, McMaster University
Eleni Hapidou
Associate Clinical Professor (PT), Department of Psychiatry and Behavioural Neurosciences; Psychologist, Michael G. DeGroote Pain Clinic, McMaster University Medical Centre, Hamilton Health Sciences
James Paul
Professor & Chair of Anesthesia, Research Chair & Director, Acute Pain Services, Department of Anesthesia, McMaster University
Florentina Miftodi
Manager, Finance and Administration
Michael G. DeGroote Institute for Pain Research and Care; Michael G. DeGroote National Pain Centre, McMaster University
James Bain
Professor, Department of Surgery; Head, Division of Plastic Surgery, McMaster University
Laura Katz
Assistant Clinical Professor (PT), Department of Psychiatry and Behavioural Neurosciences, McMaster University; Psychologist, Community Practice
Aimee Nelson
Professor, Department of Kinesiology, Associate Professor, Department of Biomedical Engineering, McMaster University
Behnam Sadeghirad
Assistant Professor, Department of Anesthesia; Biostatistician, Michael G. DeGroote National Pain Centre, McMaster University
Harsha Shanthanna
Associate Professor, Department of Anesthesia, McMaster University
Brandon Van Dam
Managing Director, Chronic Pain Network, McMaster University
Jessica Bottomley
Administrative Assistant, Chronic Pain Network, McMaster University (Maternity Leave)
Mohit Bhandari
Professor and Chair, Department of Surgery; Associate Faculty, Department of Health Research Methods, Evidence and Impact, McMaster University
Joy MacDermid
Professor (PT), School of Rehabilitation Sciences, Institute for Applied Health Sciences, McMaster University; Professor, School of Physical Therapy, Western University
Tara Packham
Assistant Professor, School of Rehabilitation Sciences, McMaster University
Louis Schmidt
Professor, Department of Psychology, Neuroscience & Behaviour, McMaster University
Li Wang
Assistant Professor, Department of Anesthesia; Michael G. DeGroote National Pain Centre, McMaster University
Philip J. Devereaux
Director, Division of Perioperative Care, Department of Health Research Methods, Evidence and Impact; Professor, Department of Medicine, McMaster University
Randi McCabe
Professor, Department of Psychiatry and Behavioural Sciences, McMaster University
Irena A Rebalka
Assistant Professor, Pathology and Molecular Medicine, McMaster University
Holger Shünemann
Professor, Department of Health Research Methods, Evidence and Impact, Director, Michael G. DeGroote Cochrane Canada Centre; McMaster University
Kim Madden
Research Director, St. Josheph’s Healthcare, Hamilton
Rachel Couban
Librarian, Michael G. DeGroote National Pain Centre, McMaster University
Rachel Roy
Knowledge Broker, Chronic Pain Network, McMaster University
Megan Groves
Communications Coordinator, Michael G. DeGroote Institute for Pain Research and Care, McMaster University
Sandra Rodwell
Administrative Assistant, Chronic Pain Network, McMaster University
The mission of the Michael G. DeGroote Institute for Pain Research and Care is to become a cutting-edge institute in the field of chronic pain and to establish a network of researchers and trainees in the field.