THE MAGAZINE OF THE UNIVERSITY OF MARYLAND SCHOOL OF NURSING SPRING 2024
A Workforce to Be Reckoned With UMSON Counters the Nationwide Nursing Shortage with Transformative Solutions

GLOBAL TO LOCAL
In the fall, the University of Maryland, Baltimore convened the Global Learning for Health Equity Network, developed through nearly $2 million of funding from the Robert Wood Johnson Foundation. Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN, the Bill and Joanne Conway Dean, serves as the grant’s principal investigator. During the two-day event, participants from across the United States joined a bus tour narrated by Lori A. Edwards, DrPH, BSN ’80, RN, CNS-PCH, BC, FAAN,

(pictured, left) assistant professor and associate dean for the Master of Science in Nursing program. The tour, themed “The Real B’More Story: Strong and Engaged Communities, District Neighborhoods, Hidden Gems, and Centuries of Resilience,” aimed to show Baltimore’s strengths through the voices of community-engaged leaders, contextualize the city’s history, and illuminate cultural treasures.
B. Elias Snyder, PhD, FNP-C, ACHPN, assistant professor, (pictured, center) joined the tour.


Caring for Our Community
We get the question all the time: What are you doing to combat the current nursing workforce shortage? UMSON continues to create innovative solutions to develop nurses prepared to adapt to the changing demands of the profession –and to keep them there.
Take a look at UMSON’s community/ public health nursing impact through a variety of partnerships and initiatives that place our faculty and students where they can do the most good in our communities.
UMSON’s Equity, Diversity, and Inclusion Efforts Supporting NCLEX Success A Peek at UMSON’s Renovated Building at USG The Research Roster
Upholding CHOICEs in Maternity Care Hospital to Hospice Transitions Cultural Exchange to Compassionate Care
Class Notes
Alumni Profiles: Unleashing Inclusivity in Health Care The First of Her Kind Events
Donor Profile: Champions for Challenging the Status Quo Legacy Society Charitable IRA Rollovers
FEATURES
16 The
In Touch Advance 22 A Workforce to Be Reckoned With 3 12 26 38
DEPARTMENTS
Pulse Impact
cover illustration: Anthony Zinonos
THE
SPRING 2024 END-OF-LIFE CARE, PAGE 14
photo at left: Rachel Sale
MAGAZINE
OF THE
UNIVERSITY OF MARYLAND SCHOOL OF NURSING
From the Dean

This May, nearly 480 students graduated from the School of Nursing, walking across the stage at the Hippodrome Theatre in Baltimore. This included new entry-into-practice nurses and nurses advancing their careers through RN-to-Bachelor of Science, master’s, Doctor of Nursing Practice, and PhD degrees. They represent our ongoing commitment to ensuring that Maryland and the nation have the nurses needed – now and in the future.
With each new graduate, we are, in the words of our mission statement, “shaping the profession of nursing and the health care environment by developing leaders in education, research, and practice.” In “A Workforce to Be Reckoned With” (Page 16), you’ll learn about how we are addressing multiple challenges of the future. To respond to the nursing shortage, we are increasing enrollments at the entry level. To respond to the shortage of nurse faculty, a key barrier to expanding the nursing workforce, we have launched an innovative residency program to support nurses new to teaching and have expanded scholarship support for our Teaching in Nursing and the Health Professions Certificate. We are addressing the need for improved access to primary care through our advanced practice nursing specialties, covering the lifespan from neonatal to pediatrics, family practice, and geriatrics.
A critical component of helping our students complete their degrees is the scholarship support derived from funds donated over many years by countless alumni, faculty, and friends of the School of Nursing. Now generating close to $1 million a year in income, our 160 endowed scholarships provide significant financial assistance. In conjunction with additional funds raised on an annual basis, these scholarships provide access to a nursing education, meet our students’ financial needs, and keep their education on track.
One of our premier, and often game-changing, scholarship initiatives is the Conway Scholars program. Launched in 2015, through the generous and visionary philanthropy of Bill and Joanne Conway and their Bedford Falls Foundation, the program is providing more than 1,100 scholarships, including those that supported the 375 Conway Scholars who have graduated to date. Very sadly, Joanne Conway passed away unexpectedly in January. Although she preferred to remain out of the spotlight, it was Mrs. Conway’s experience listening to a restaurant waitress describe her struggle to afford a nursing degree that informed the Conways’ philanthropic vision, shaping it into the Conway Scholars program and other significant initiatives to support nursing education.
As we celebrate the graduation season, we are grateful for the vision of the Conways, we salute the enduring legacies of our past donors, and we give thanks to those who have followed. We are also indebted to all those who contribute in their own unique ways. Without this ongoing generosity across time and into the present, it could have been an empty stage in May.
 Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN
Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN
The
Bill and Joanne Conway Dean
SPRING 2024
NURSING FOR/UM is published by the University of Maryland School of Nursing.
EDITOR-IN-CHIEF
Giordana Segneri
ASSOCIATE EDITORS
Jillian Dreicer
Erin Merino
Mary Therese Phelan
EDITORIAL BOARD
Stacey Conrad
Yvette Conyers
Amy Daniels
Elizabeth Galik
Jana Goodwin
Veronica Gutchell
Yolanda Ogbolu
Deborah Prout
Cynthia Renn
Barbara Resnick
Jennifer Schum
Cynthia Sikorski
Susan Wozenski
CONTRIBUTORS
Stacey Conrad
Monica Maggiano
Nicole Nash
Deborah Prout
Cynthia Sikorski
Lorrie Voytek
DESIGN
Skelton Sprouls
We welcome comments, suggestions, and story ideas from alumni, partners, and friends.
Send correspondence to Giordana Segneri, Editor-in-Chief, at nrscommunications@umaryland.edu or 410-706-4115.
© University of Maryland School of Nursing, 2024
2 • NURSING FOR/UM • SPRING 2024
The Pulse
‘This Is Our Work’ UMSON’s
Efforts in Equity, Diversity, and Inclusion Focus on Buy-In
BY EMILY BLEIWEIS
Over the past decade, UMSON has made significant progress toward its diversity goals, especially when it comes to increasing the percentage of students, faculty, and staff who identify as racially and ethnically diverse. The number of historically underrepresented faculty, for example, has more than doubled since 2014, said Yvette Conyers, DNP, RN, FNP-C, CTN-B, CFCN, CFCS, CNE, assistant professor and associate dean for equity, diversity, and inclusion (EDI).
This progress is important – but far from complete, Conyers points out, especially as it relates to the School’s male and Latino populations, both among students and employees – because representation in health care is critical. It can impact things like understanding discharge instructions and medication adherence.
Nurses hear from their patients that they are looking for caregivers who share their culture and experiences, Conyers said. And statistically, she added, data shows that there are better health outcomes when there is racial and ethnic concordance – when a patient is cared for by someone who looks like them.
“If we know that someone’s going to be able to understand what we’re saying to them better and be able to adhere to the plan of care, that cuts down on the chance of them coming back to the hospital for something they didn’t understand or because we didn’t really understand why they didn’t want to take their medications,” she said. “Having that cultural piece of it is so important.”
For Conyers, who stepped into her role last June, making sure there is adequate representation among
“This work really is based on inclusivity, collaboration, and creating an environment where folks feel like they can thrive, where they are welcome, where they are supported.”
YVETTE CONYERS

faculty, staff, and students is just the start. She is only the second person to serve in the associate dean for EDI role after UMSON became the first school on the University of Maryland, Baltimore campus to establish the leadership position in 2016. In her role, Conyers serves as the primary advisor to UMSON’s dean, senior academic leadership team, senior administrative team, and Equity, Diversity, and Inclusion Council on operational and strategic goals related to EDI.
Conyers’ focus so far has been on building a team, consisting of herself, a manager, and a coordinator, plus a faculty member who also serves as the director of restorative justice, which blends a proactive, relationship-focused methodology with restorative tools designed to strengthen community bonds and address instances of harm and conflict. They are also working on creating a new mission and vision to guide their efforts.
The vision is being developed in collaboration with the School’s EDI Council, formed in 2021, that acts as an advisory board to Conyers’ office. It is chaired by members of the faculty and staff and supports the EDI office with strategic planning and professional development, Conyers said.
“This work really is based on inclusivity, collaboration, and creating an environment where folks feel like they can thrive, where they are welcome, where they are supported,” Conyers said. “It’s also about providing tools for people to be able to continue the work that has been done.” The team has been working to identify specific goals and how to measure progress.
NURSING FOR/UM • SPRING 2024 • 3
MATTHEW D’AGOSTINO/UMB
The School of Nursing joined many other University of Maryland, Baltimore entities to host a Native American Heritage Month celebration in November. The Baltimore American Indian Center showcased a traditional dance performance and served a cultural meal.
They have put significant effort toward increasing professional development opportunities for faculty and staff and creating paths for faculty, alumni, and other professional nurses to earn continuing education credits through EDI programming. Conyers’ team has also been working to ensure different populations of the UMSON community – from students at UMSON’s location at the Universities at Shady Grove in Rockville, Maryland, to alumni near and far – feel embraced and integrated and have access to the resources and support they need.
Essential Experiential Education: A Passport to Practice
Percentage of historically underrepresented students at UMSON
UMSON’s mapping tools have been downloaded more than 15,000 times from AACN’s website since December.
In 2021, the American Association of Colleges of Nursing (AACN) introduced a new version of The Essentials: Core Competencies for Professional Nursing Education, dubbed simply The Essentials, delineating the essential knowledge and skills for students in Commission on Collegiate Nursing Education–accredited programs along with a call for a shift to competency-based education (CBE) principles in nursing education. UMSON has embraced this initiative, leading nationwide efforts to integrate CBE into our curricula.
UMSON was among the first nursing schools in the country to launch a revised Bachelor of Science in Nursing (BSN) curriculum in fall 2022. The School initiated the CBE process by mapping 150 current courses to Essentials competencies, identifying program gaps and
This is part of the work involved in a three-year Josiah Macy Jr. Foundation grant, “Eliminating Structural Racism in Nursing Academia: A Systems Change Approach to Anti-Racist Nursing Education,” that UMSON is one of only 12 nursing schools nationwide to receive. The dozen schools will form a learning collaborative to develop projects to address structural racism and promote anti-racist nursing educational environments at their respective institutions.
For Conyers, EDI work can only
overlaps. Our mapping tools, now widely used nationwide, are available on AACN’s website.
Subsequently, faculty began revising courses to ensure student and program outcomes aligned with The Essentials. As more national guidance on CBE and assessment has emerged since UMSON’s BSN launch, the program will undergo higher-level revisions. The MSN and DNP program curricula are also being revised and are scheduled to launch in upcoming semesters. Students will have more learnerfocused experiences, including coaching from faculty, increased experiential activities, and frequent assessments, enhancing their success and workforce readiness.
UMSON’s Essential Experiential Education: A Passport to Practice (E3 to P2) curricular revision taskforce facilitates a collaborative approach to this work, with monthly meetings featuring discussions about best practices, faculty development, and subgroup reports. We emphasize providing students with multiple opportunities to demonstrate
be successful when there’s buy-in and when people feel empowered. And none of that happens without relationships built on trust. To find success, Conyers said, she knows EDI must be a holistic part of the School’s fabric and can’t be used solely as a reactionary method to a problem or conflict.
“I may be leading these efforts, my team may be leading these efforts, but this is our work,” she said, referring to the entire UMSON community.

what they can do with what they know, aligning learner outcomes with assessments, and enhancing teaching strategies, all with a focus on equity, diversity, and inclusion. The integration of Essentials and CBE principles is ongoing, guided by emerging national CBE standards, and we continue to engage with practice partners to produce practiceready graduates.
— Dawn Mueller-Burke, PhD ’07, MS ’98, CRNP, NNP-BC, Assistant Professor; Chair, UMSON’s E3 to P2 Taskforce; and AACN Essentials Champion; and Susan L. Bindon, DNP ’11, MS ’96, RN, NPD-BC, CNE, FAAN, Associate Professor; and Co-Chair, E3 to P2 Taskforce
4 • NURSING FOR/UM • SPRING 2024
THE PULSE
2018 2023 47% 60%
Leadership Updates
UMSON is pleased to announce that three faculty members have been named to leadership roles, lending their significant expertise to enhance teaching and learning, research and scholarship, and the student experience as the School strives to develop leaders in nursing education, research, and practice.



Veronica Gutchell, DNP ’13, RN, CNS, CRNP Assistant Professor; Chair, Department of Partnerships, Professional Education, and Practice
Kathleen “Katie” McElroy, PhD ’16, MS ’10, BSN ’98, RN Associate Professor; Associate Dean for the Baccalaureate Program
Nicole E. Smith, PhD, MS ’14, RN, CNE, CHSE, CNE-cl Assistant Professor; Co-Director, Bachelor of Science in Nursing Program

UMSON Day at Lexington Market
UMSON faculty, staff, and students were invited to gather with their colleagues and classmates for the University of Maryland, Baltimore’s (UMB) first school-specific day at Lexington Market in Baltimore in October. The event was part of UMB’s EMBRACE Initiative, an effort to increase the vibrancy of the greater UMB campus and boost the University’s community impact in West Baltimore. UMSON second-semester Bachelor of Science in Nursing students in a community/ public health rotation provided market patrons with information about chronic obstructive pulmonary disease, cardiovascular disease and stroke, and diabetes. Faculty, staff, and other students joined EMBRACE Initiative representatives and members of the PEACE Team, a community-based violence prevention program, for lunch purchased from market vendors.
A Piece of the Pi
News from Sigma’s Pi at-Large Chapter at
I am delighted to share updates and important information on Sigma Pi at-Large Chapter’s latest happenings.
The spring induction ceremony, held April 9, was a momentous occasion during which we inducted more than 150 new members committed to nursing excellence and celebrated the achievements of our continuing members. Looking ahead, Pi at-Large Chapter is preparing for elections to shape the leadership team for the 2024 - 26 term. This is a critical opportunity for members to contribute to our governance. Nominations are open for key positions, including president-elect, treasurer, and
chairs of the leadership succession, governance, Key Award, program planning, and continuing education committees. If you are interested in a leadership role or know a deserving candidate, please reach out to me at pthurman@umaryland.edu. This is your chance to make a lasting impact on our chapter’s direction and contribute to the advancement of nursing knowledge. Your dedication is key to the vibrancy of our community.
Together, we can foster a community of excellence and make a positive impact on the field of nursing.
— Paul A. Thurman, PhD ’18, MSN ’07, RN, ACNPC, CCNS, CCRN Pi at-Large Chapter President
NURSING FOR/UM • SPRING 2024 • 5
UMSON MATTHEW D’AGOSTINO/UMB
“We provide personalized coaching sessions to assist students at all stages of their academic journey.”
DENIECE BENNETT

At the Ready
Supporting Students’ NCLEX Success
BY MARY THERESE PHELAN
About a year ago, a new version of the National Council Licensure Examination (NCLEX-RN) was launched, dubbed the “NextGeneration (or NextGen) NCLEX,” that is designed to assess clinical judgment in nursing candidates. It includes new item types that measure whether future nurses can think critically about how to care for patients. UMSON is strengthening entry-into-nursing graduate readiness for the new licensure exam by enhancing academic rigor, creating a robust prep program, and ultimately continuing to improve first-time pass rates. Supporting students this way not only improves NCLEX-RN success, but it better prepares UMSON graduates for safe and effective practice.

DeNiece Bennett, DNP, RN, assistant professor, joined UMSON two years ago as the director of the NCLEX Success Program. Bennett works with entry-into-nursing program faculty to ensure that content, teaching strategies, learning activities, student support services, and assessment align with the National Council of State Boards of Nursing’s (NCSBN) clinical judgment model.
We recently chatted with Bennett to learn about the progress being made in NCLEX readiness.
Q: What are the changes that were made to the NCLEX and why?
A: About 10 years ago, the NCSBN decided that the NCLEX-RN needed a more suitable approach to assessing and evaluating the graduate nurse. After extensive research, it identified the appropriate measure to gauge the test-takers’ responses, translating to safe practices. The test plan pivoted to questions that underscore the clinical judgment measurement model, in which test-takers encounter three case studies that center on recognizing, analyzing, hypothesizing/prioritizing, generating solutions, taking action, and evaluating.
Q: How did UMSON respond to the NCLEX changes?
A: UMSON took measures to prepare students and faculty for the NextGen NCLEX. We organized faculty-centered workshops to enhance their skills in creating NextGen NCLEX case studies and in writing sample questions; integrated more intuitive resources in courses, such as video case studies for better understanding of concepts; and hired additional NCLEX-RN support faculty and staff to strengthen the NCLEX Success Program.
Q: What does UMSON’s NCLEX Success Program offer?
A: The program comprises two nurse faculty members, each of whom teaches half-time and focuses half-time on faculty development and students’ success on the NCLEX exam, and an NCLEX program coordinator. Together, they work to develop engaging activities that help students bridge the gap between curricular competencies and the NextGen NCLEX exam. We provide personalized coaching sessions to assist students at all stages of their academic journey, and we collaborate with faculty to facilitate a seamless integration of NCLEX preparation tools into their course content, creating an intentional and effective learning experience with the test prep for students.
UMSON’s Strategies for NextGen NCLEX Success
Some initiatives that have led to continued improvements in the first-time pass rate for entry-into-nursing students include:
• a standardized NCLEX Learning Plan across the curriculum, which accounts for 10% of the grade in selected courses, and customized plans in response to students’ performance on practice assessments
• student-centered workshops on NextGen NCLEX-type questions, case studies, and best practices for remediation
• a faculty NCLEX task force that has designed professional development sessions focused on practice readiness, realigning learning modules to include NCLEX practice in direct response to students’ assessments, and adjusting course exam questions to emulate those in the NCLEX
• a mandatory NCLEX study hall for students who earn less than 65% on their predictor assessment
• maintaining contact with entry-intonursing graduates through check-ins after five and eight weeks, offering one-on-one coaching sessions.
6 • NURSING FOR/UM • SPRING 2024 THE PULSE
DAVID PLUNKERT
“Being able to do this simulation made me feel like this school is really preparing and helping us to be great and competent nurses.”
STUDENT QUOTE FROM A POST-SIMULATION SURVEY
Renewed Realism
UMSON’s Renovated Building at USG Enhances Outcomes
BY GIORDANA SEGNERI
Students collaborate on reviewing patient records in the new Hospital Simulation Suite (below, top) while others find quiet study and social space in a new lounge on the third floor (below, bottom) Realistic acute-care spaces, technology, and mannikins provide opportunities for practice in the Hospital Simulation Suite (right)
After UMSON put the finishing touches on a substantial renovation of Building I at the Universities at Shady Grove (USG), making it a space dedicated entirely to the School of Nursing at the Rockville, Maryland location, the building returned to 100% occupancy last fall. Now, 447 students between the entry Bachelor of Science in Nursing program and the Doctor of Nursing Practice Family Nurse Practitioner specialty and 36 employees add to the building’s bustle.
The $8.2 million renovation, funded in part by the University System of Maryland, UMSON, USG, Bill


and Joanne Conway’s Bedford Falls Foundation, and a Health Resources and Services Administration grant through U.S. Sen. Chris Van Hollen’s office, expanded space in the building by approximately 12,000 square feet, for a total of 27,000.
This has made room for increased spaces for studying and gathering; expansion of the Office of Academic and Career Success suite; a large, multipurpose simulation room; and space that allows the clinical simulation team to be housed together, increasing efficiency, collaboration, and a sense of community. But perhaps the crown jewel is the Hospital Simulation Suite, a five-room, ultra-realistic space that features high-fidelity mannikins and a control room. The renovation increased the number of USG’s simulation labs from eight to 13.
“The realism of the new hospital suite makes an impression on anyone who enters,” said Patricia “Pat”
Schaefer, DNP, RN, CNE-cl, CHSE, CNE, assistant professor and director of the clinical simulation labs at USG.
“A student can answer a patient call light from the nurses’ station, pull medication from a hospital-grade medication dispenser, and manage multiple patients in multiple rooms. Immersive realism is a game-changer for students. We now can provide realistic transitions of care, as students can admit and discharge patients from our hospital and then make a home visit in our simulated apartment.”
Jana Goodwin, PhD, RN, CNE, assistant professor and department chair of UMSON at USG, said she loves seeing how energized students are when they exit the hospital suite after a simulation. “I have noticed an increase in the number of students honoring the simulation contract of suspending disbelief,” she added. “This allows them to focus on the objectives of simulation, and that makes a difference in their learning.”

NURSING FOR/UM • SPRING 2024 • 7
IMAGES AT LEFT: CHRIS HARTLOVE; IMAGE AT RIGHT: KATE WICHLINSKI
Learn more about the fascinating work of our nurse researchers at nursing.umaryland.edu/ nurseresearchers.
The Research Roster
As usual, our researchers have been quite busy, addressing issues ranging from improving communication within families of children with serious pediatric illness to determining better ways to assist dementia patients living in nursing homes. Here’s a snapshot of what some of our researchers have been up to:
RESEARCH FOCUS RESEARCHER FUNDING AMOUNT OBJECTIVE
CANCER CARE Ian Kleckner, PhD, MPH
SERIOUS PEDIATRIC ILLNESS
Kim Mooney-Doyle, PhD, RN, CPNP-AC
CHRONIC PAIN Cynthia L. Renn, PhD, MS ’97, RN, FAAN
DEMENTIA AND LONG-TERM CARE
—M.T.P.
Kirschling Named Dean Emerita

$400,000, National Cancer Institute
$460,000, National Institute of Nursing Research
testing the preliminary efficacy of exercise vs. nutrition education on cancer patients with chemotherapy-induced peripheral neuropathy
understanding how family communication during serious pediatric illness provides opportunities to prevent longterm distress
$3 million, National Institute of Nursing Research
Barbara Resnick, PhD ’96, RN, CRNP, FAAN, FAANP
$2.13 million, National Institute on Aging
identifying genetic markers that will predict who will transition from acute to chronic pain in trauma patients with a lower extremity fracture
addressing the treatment of pain in nursing home residents with dementia
U.S. News Rankings Continue to Recognize UMSON’s Excellence
• Master of Science in Nursing Health Services Leadership and Management specialty: Ranked No. 3 in the nation (No. 1 among public schools of nursing) in the Nursing Administration/ Leadership category of U.S. News & World Report’s 2024 “Best Online Programs”
• Bachelor of Science in Nursing program: Ranked No. 10 (tied) in the nation (No. 3, tied, among public schools of nursing) in U.S. News & World Report’s 2024 “Best Colleges”
—M.T.P.
Jane Kirschling, PhD, RN, FAAN, the former Bill and Joanne Conway Dean of the University of Maryland School of Nursing, has been named dean emerita by University of Maryland, Baltimore (UMB) President Bruce E. Jarrell, MD, FACS, in recognition of her “decade of service, dedication, and extraordinary contributions to the University.”
The University president may confer the dean emeritus title upon a retiree who demonstrated exceptional service as a UMB dean for a minimum of 10 years. Kirschling retired after the 2022 - 23 academic year.
Upon arriving at UMSON in January 2013, when she was appointed dean and director of the UMB Center for Interprofessional Education, Kirschling exemplified leadership, vision, and an unwavering commitment to academic excellence, Jarrell wrote in a letter to Kirschling about awarding her the dean emerita title.
Kirschling’s formal portrait, shown above, was hung in the School’s auditorium in Baltimore in July, joining portraits of other former deans. True to Kirschling’s spirit, a small image of her beloved rescue dog, Frankie, is included.
—M.T.P.
8 • NURSING FOR/UM • SPRING 2024 THE PULSE
MATTHEW D’AGOSTINO/UMB
Graduation
DECEMBER 2023
“Regardless
of the source of inspiration, what unites us today is the shared commitment to service and the understanding that our impact extends far beyond the boundaries of immediate gratification.”
KIARA GABRIELLE STEVENS, BSN ’23 STUDENT SPEAKER





UMSON celebrated an extraordinary group of health care professionals on Dec. 21 at a ceremony honoring 278 summer and fall 2023 graduates from its locations in Baltimore and at the Universities at Shady Grove in Rockville, Maryland.
Held at the Hippodrome Theatre in Baltimore, it was the first graduation ceremony led by Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN, the Bill and Joanne Conway Dean, who began her tenure in July.
“This is always an exciting time for us, as educators, when we celebrate the milestones reached by our students and revel in their success, because their success is our success as well,” Ogbolu said. “It is a time for us to reflect on our essential

purpose – to foster the development of human potential that lies within each of us, to enrich our lives and enable us to contribute to improving the lives of others – in particular, through our nursing careers.”
The event’s keynote speaker, Katie Boston-Leary, PhD, MBA, MHA, RN, NEA-BC, director of nursing programs at the American Nurses Association, acknowledged the challenges that exist in nursing but also implored graduates to recognize their strengths and their power to bring change.
“You have light and darkness, two opposing forces that play off of each other. And they also depend on each other to function. It is also a choice of who we choose to be every day. Darkness cannot drive out darkness. Only light can do that,” she said. “Hope and despair, another set of opposing concepts. It is easy to feel despair at the state of the world that we live in today. Almost everything is being upended, and there’s so much unrest. We need hope.”
— E.B.
NURSING FOR/UM • SPRING 2024 • 9
1. Ogbolu leads her first graduation ceremony as dean
2. Keynote speaker Boston-Leary
3. BSN graduates show off their colorful stoles
4. Master’s graduates are all smiles
5. Student speaker Stevens
THE PULSE
6. Prepping for the processional
PHOTOGRAPHY: MATTHEW D’AGOSTINO/UMB See more photos from the ceremony at nursing. umaryland.edu/graduation Click on “Photo, Video, and Program Archive.” 5 6 1 2 3 4
Face to Face with Dean Ogbolu
BY BRUCE E. JARRELL, MD, FACS PRESIDENT, UNIVERSITY OF MARYLAND, BALTIMORE
Dean Ogbolu wants every student at UMSON to be successful, and that includes thinking broadly about what they might need. Watch a recording of this Virtual Face to Face at umaryland.edu/ face-to-face.
What does it mean to shape the next generation of nurses? In December, I had the privilege to chat with Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN, the Bill and Joanne Conway Dean of the University of Maryland School of Nursing, during a session of the University of Maryland, Baltimore’s virtual program Face to Face, during which I interview various subject matter experts. We talked about how UMSON is educating future nurses who provide culturally competent care and reflect the rich diversity of our country — nurses who will help fight the current shortage in the profession.
A recent study by the National Council of State Boards of Nursing reports that an estimated 100,000 registered nurses have left the workforce over the past two years because of burnout, stress, and retirement, and another 610,388 reported an intent to leave by 2027. According to the Bureau of Labor
Statistics, the United States will need to fill 190,000 nursing positions in each of the next 10 years to keep up the country’s health care needs. Graduates from UMSON stand ready to fill those positions.
Despite widespread reports of low enrollment in nursing schools across the United States and problems recruiting students, UMSON stands out as an exception. Dean Ogbolu, who began her role last July, stated that the School is experiencing growth and increased diversity in its student body. Over 50% of students in Baltimore and over 80% at the Universities at Shady Grove are underrepresented minorities. She also highlighted an encouraging increase in male enrollment, with 11% of students now being men, a notable improvement from when she began working at UMSON in 2010.
Dean Ogbolu wants every student at UMSON to be successful, and that includes thinking broadly about what they might need. She shared that when thinking about the diverse student body, UMSON considers race and ethnicity, but also caregiver status, military status, and many other characteristics of the future nursing workforce. In discussing faculty and
school administration preparing to engage students effectively, she highlighted the impact of social determinants of health on students and the importance of understanding and addressing these factors, such as hunger and housing insecurity. UMSON has implemented a Student Emergency Fund to support students facing challenges outside the classroom.
The next generations of nurses will leave UMSON with education and preparation that align with the evolving needs of the health care industry. By integrating the latest advancements in health care and technology into the curriculum, UMSON is equipping nursing students with the skills and knowledge necessary to excel in addressing health care challenges and an understanding of culturally competent care.
I enjoyed my conversation with Dean Ogbolu, and it was wonderful to hear about UMSON’s successful strategies in addressing nursing education, staffing shortages, and promoting diversity and inclusion within the nursing profession. It’s inspiring to watch how UMSON continues to shape the nursing workforce of the future.

10 • NURSING FOR/UM • SPRING 2024 GUEST AUTHOR
Ogbolu (left) and Jarrell (right) during their virtual conversation
Vitals
“ Virtual reality can be therapeutic. By ourselves, we can’t detach from the pain and anxiety we are experiencing. Through virtual reality, however, you can turn someone’s attention away from the symptoms they are experiencing with strong visual stimulation and three-dimensional sounds. This multisensory stimulation helps modulate the brain’s perception of pain and other symptoms.”
Luana Colloca, MD, PhD, MS, professor; director of the Placebo Beyond Opinions Center; and MPower Professor New Scientist, February 2024
The Maryland Nurses Association 120th Convention last October in Ocean City featured presentations by 13 faculty members
Eight faculty members have been named Maryland state New Nurse Faculty Fellows, receiving the maximum award amount of $50,000. These awards are part of the Nurse Support Program II, a statewide initiative funded by the Health Services Cost Review Commission and administered by the Maryland Higher Education Commission.
For the sixth year in a row, UMSON has earned the Health Professions Higher Education Excellence in Diversity Award from INSIGHT Into Diversity magazine, which recognizes colleges and universities that demonstrate an outstanding commitment to diversity and inclusion.

Bridgitte Gourley, DNP ’08, FNP-BC, assistant professor and director of the Doctor of Nursing Practice Family Nurse Practitioner specialty, has been named one of three co-directors of the University of Maryland, Baltimore Center for Interprofessional Education.
Among public schools of nursing nationwide, UMSON ranked 21st in research funding received from the National Institutes of Health.
Charlotte Nwogwugwu, DrPH, BSN, RN, HIV PCP, CPH-BC, assistant professor and interim director of the Office of Global Health, launched an initiative that aims to integrate mental health services into HIV care in Nigeria, impacting an estimated 2,000 patients annually.
Three faculty researchers received prestigious R-level grants totaling $3.65 million from the National Institutes of Health during the last award cycle to develop, support, and expand upon healthrelated research projects.
NURSING FOR/UM • SPRING 2024 • 11
— Compiled by Erin Merino
Impact Upholding CHOICEs in Maternity Care
BY MARY THERESE PHELAN
Global warming. Gun violence. COVID-19 economic recovery. Substance use.
“The value of having a measure of shared decision-making for maternity care is that we need to have a way to include the pregnant and birthing person’s voice in their care.”
RACHEL
BLANKSTEIN BREMAN
OUR RESEARCHER
Rachel Blankstein
Breman, PhD ’18, MPH, RN
These are the issues that fill the news, important topics deserving of our attention, of course. But Rachel Blankstein Breman, PhD ’18, MPH, RN, assistant professor, asks that you please not overlook the United States’ maternal health crisis, which she says could be improved with better communication between providers and patients.
According to the Centers for Disease Control and Prevention (CDC), in 2021, the most recent year for which data is available, 1,205 women died of maternal causes in the United States, compared to 861 in 2020 and 754 in 2019. The maternal mortality rate for 2021 was 32.9 deaths per 100,000 live births, compared with a rate of 23.8 in 2020 and 20.1 in 2019, according to the CDC. The U.S. Government Accountability Office also reports the COVID19 pandemic exacerbated maternal health outcomes and highlighted racial disparities.
INSIDE THE RESEARCH
Breman also received a one-year, $60,000 grant from the Maryland Department of Public Health in collaboration with the Maryland Patient Safety Center and Your Birth Partners, a nonprofit organization. This grant will fund interactive webinars on how to implement trauma-informed care for all birth workers in Maryland. Through these webinars, the sponsoring partners will explore what additional information and resources are needed or are available, such as training, hospital policy updates, and increased support within hospitals to address implementation of traumainformed care.
“There is a maternal health crisis in this country, and part of the problem has to do with health care systems and providers not offering person-centered care and listening to pregnant people,” says Breman, whose research focuses on maternal health, intrapartum care, shared decision-making (SDM), implementation and dissemination research, and outcomes research. SDM ensures the care preferences and personal values of the patient are directly integrated into the clinical decision-making process with the health care team.
To support her research on how effective communication impacts birth outcomes,
Breman has received an R01 research grant of $1.06 million from the Department of Health and Human Services’ Agency for Healthcare and Research Quality. The R01 grant designation is used for mature research projects that are hypothesis driven with strong preliminary data. Breman’s project, titled “A Measure for Shared Decision Making in Maternity Care through Communicating CHOICEs: CHildbirth Options, Information, and Person-Centered Explanation,” will be funded over three years.
U.S. professional perinatal care organizations recommend SDM in maternity care to provide person-centered, highquality care to pregnant and birthing people during their perinatal care. But there is no valid and reliable measure of SDM so that the pregnant person’s experience with SDM during their pregnancy and birthing care can be determined.
The main objective of the project is to provide a metric for measuring SDM from the pregnant person’s perspective during their prenatal and intrapartum hospital care; this will be achieved by testing the validity and reliability of a revised version of the CHOICEs measure, which Breman previously developed.
“The value of having a measure of shared decisionmaking for maternity care is that we need to have a way to include the pregnant and birthing person’s voice in their care,” Breman says.
The revised CHOICEs SDM will be translated culturally and linguistically into Spanish. Breman and her research team plan to recruit 505 people who have given birth within the previous six months through the smartphone apps What to Expect, the Baby Center, and What to Expect Español. To reach populations that do not traditionally participate in research, they will use social networking recruitment through Mary’s Center, which serves more than 65,000 people of all ages, incomes, and backgrounds in the Washington, D.C., metro area. The researchers expect to determine whether the SDM items perform equally across different clinical situations and demographic groups.
12 • NURSING FOR/UM • SPRING 2024

NURSING FOR/UM • SPRING 2024 • 13 MICHELLE MILDENBERG LARA
“We have to offer a personcentered approach focused on individual needs.”
JOAN CARPENTER
Smooth Transitions in End-of-Life Care
BY ERIN MERINO
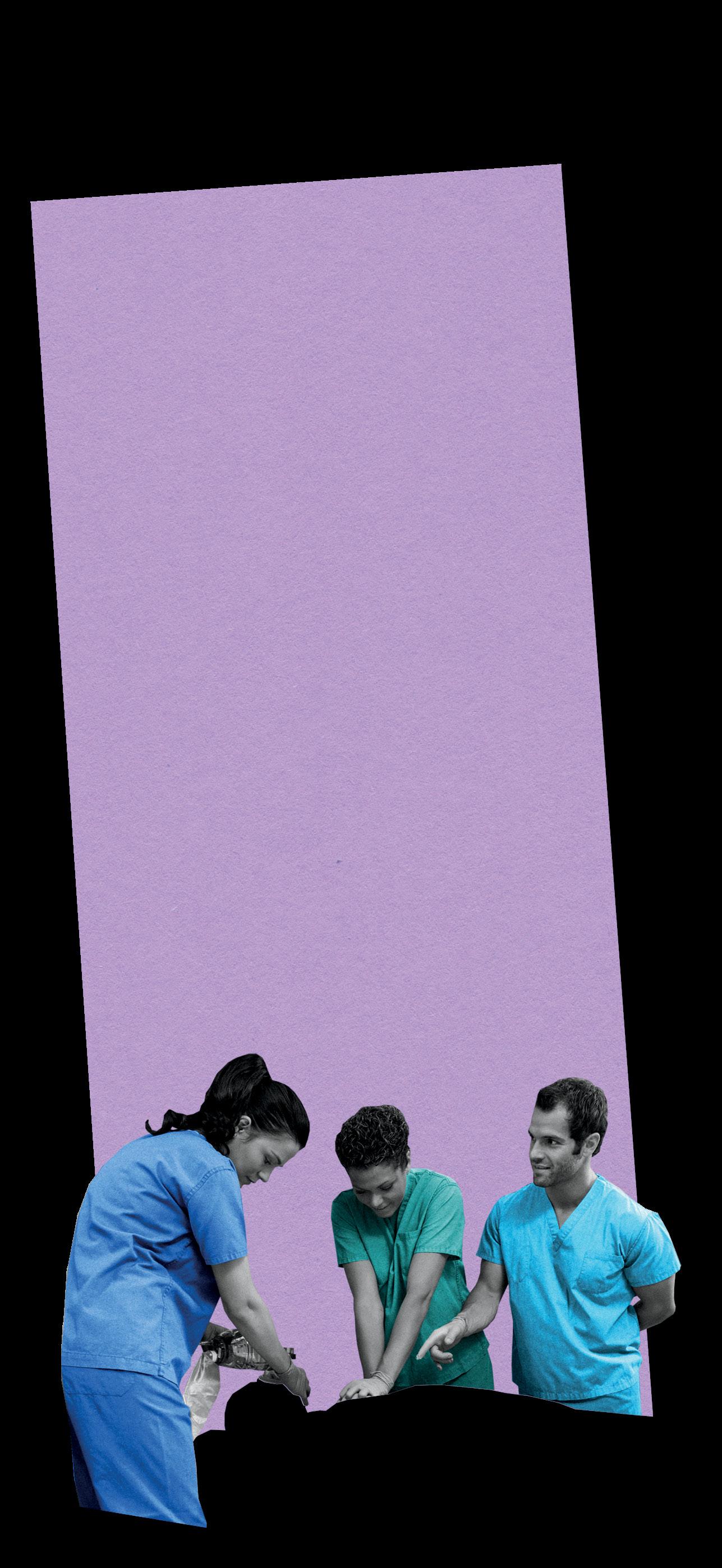
Transitioning to hospice care is one of the most vulnerable and delicate phases in a terminally ill patient’s life, and the goal is to prioritize comfort by reducing pain and suffering. It must be done with care to ensure “that patient and caregiver stress and fear are reduced,” explains Joan Carpenter, PhD, CRNP, ACHPN, FPCN, assistant professor.
Timing is crucial to facilitate a smooth transition. “When a person with limited life expectancy is no longer seeking curative or lifeprolonging treatments, the goal of care is to maintain the best quality of life, and the primary focus is

symptom management,” Carpenter explains. Some indicators that it is time for end-of-life care are recurrent hospitalizations and emergency department visits, a decline in health and in the ability to complete daily activities, loss of appetite, unintended weight loss, recurrent infections, and uncontrolled pain.
Carpenter, who has been working in hospice and palliative care for almost two decades, says, “A coordinated plan will reduce uncertainty for both patients and their caregivers alike.” Her experience includes working in nursing homes, inpatient hospitals, and private residences, which has allowed her to witness the challenges from different perspectives. She offers recommendations for ways to facilitate a smooth transition and guide patients to a peaceful journey:
1
Provide an Efficient Discharge Plan
An efficient discharge plan from the hospital to home should “support the caregiver with the necessary information, medical equipment, medications, and treatments to maintain optimal symptom management for the hospice patient,” Carpenter suggests. This sets the caregiver up for success on continuing care at home.
2 Don’t Overload the Patient or Caregiver
“Recognize that people can usually only handle small amounts of information during times of stress,” Carpenter says. It’s important to ask people to repeat
what you tell them and make sure directions are provided in a format that the patient and caregiver can understand and reference.
3 Ensure Expectations Are Clear
“The hospice care model is focused on managing care at home and shifting care away from acute care,” Carpenter explains. Be sure that it’s understood that routine care will be managed at home by a caregiver with support from hospice staff. Carpenter continues, “Intense 24-hour care is only the case for short-term general inpatient care when a patient needs intense symptom management or when a caregiver needs respite care.”
4 Involve Hospice Staff
Hospital staff should collaborate with hospice staff to ensure a smooth discharge to home. “The hospice agency can and should be called for patient and caregiver concerns and can be reached 24 hours a day,” Carpenter says. This allows the patient and caregiver to feel supported while they manage care.
5 Customize the Care
“One size does not fit all, and we have to offer a person-centered approach focused on individual needs,” Carpenter says. Attend to what is most important to a patient and their family. This may include emotional, spiritual, or educational support and resources.
14 • NURSING FOR/UM • SPRING 2024
IMPACT
OUR EXPERT
MICHELLE MILDENBERG LARA
Joan Carpenter, PhD, CRNP, ACHPN, FPCN
Cultural Exchange to Compassionate Care
Diego Macedo
BY ERIN MERINO
Diego Macedo, MSN, BS, a student in the Doctor of Nursing Practice (DNP) Psychiatric Mental Health Nurse Practitioner specialty, arrived in the United States at 17 from Brazil, embarking on a new chapter that ignited his interest in behavioral health and nursing.
Macedo’s journey began when he joined Rotary International, an organization dedicated to global volunteer service. Through Rotary’s exchange student program, Macedo completed his senior year of high school in upstate New York. The experience opened his eyes to opportunities in the United States, prompting him to return for college.
“Nurses are there in very vulnerable times for people, and to be there present without judgment, you really have to just care for humanity. It’s a beautiful profession.”
DIEGO MACEDO
After graduating with a double major in biology and linguistics, Macedo joined the U.S. Army through the Military Accessions Vital to National Interest (MAVNI) program, which recruited non-citizens with certain language skills or those who were health care professionals. After serving for four years, he was granted U.S. citizenship. During his time in the MAVNI program, he opted to specialize in behavioral health, drawing inspiration from his mother, a psychologist. “I remember reading some of her books for fun, and I liked them,” Macedo explains. He worked

under the supervision of health care professionals to conduct evaluations and follow-up appointments. “I worked with numerous soldiers dealing with mental health issues,” Macedo says.
Upon completion of his contract with the Army, Macedo wanted to deepen his knowledge of mental health, so he considered programs in psychology, medicine, and nursing. He ultimately decided nursing was the best fit. “Nursing is a profession where you can really connect with people,” he says. “Nurses are there in very vulnerable times for people, and to be there present without judgment, you really have to just care for humanity. It’s a beautiful profession.”
Fluent in Portuguese, Spanish, and English, Macedo’s language skills facilitate his ability to connect with diverse individuals.
Macedo’s desire to contribute to mental health led him to pursue a Master of Science in Nursing degree and to set his sights on UMSON for his doctoral degree. “At the time that I was applying to nursing schools, I already dreamed about the DNP
program at UMSON,” Macedo says, adding that he was impressed by the robust curriculum of the Psychiatric Mental Health Nurse Practitioner specialty. “I am so grateful for the stellar faculty, the small cohort, being able to have in-person classes, and I appreciate the School’s commitment to identifying clinical practicum sites for students.”
Last fall, Macedo participated in an internship at the American Association of Colleges of Nursing (AACN), assisting with two AACN competency-based education workshops that were held at UMSON as well as the organization’s Academic Nursing Leadership Conference. He is on track to graduate this semester, and after earning his DNP, he hopes to work with military populations again and to become a faculty member. “Each chapter of my life, from being an exchange student to being a soldier, was marked by encounters with mentors who nurtured my growth and pushed me to excel,” he says. “These relationships were pivotal, inspiring the confidence to tackle the next challenge.”
NURSING FOR/UM • SPRING 2024 • 15
STUDENT SPOTLIGHT
MATTHEW D’AGOSTINO/UMB

A Workforce to Be Reckoned
16 • NURSING FOR/UM • SPRING 2024
BY MEREDITH LIDARD KLEEMAN

UMSON Counters the Nationwide Nursing Shortage with Transformative Solutions
Reckoned With
Nursing has long been plagued by the specter of a workforce shortage. “I’ve been a nurse for 40 years – it seems like there’s always been a nursing shortage,” says Susan Bindon, DNP ’11, MS ’96, RN, NPD-BC, CNE, FAAN, associate professor and associate dean for faculty development.
ILLUSTRATION BY ANTHONY ZINONOS COVER STORY
NURSING FOR/UM • SPRING 2024 • 17
The last significant warning bells went off in the late aughts, as the United States was grappling with the financial crisis and ensuing Great Recession. At that time, population growth, and the approaching retirement of baby boomers who made up a significant portion of the nursing workforce, fueled the crisis.
This time around, the shortage is being driven by the exodus of workers burned out by the COVID-19 pandemic and by older, more experienced nurses leaving the profession. The Maryland Hospital Association 2022 Health Care Workforce Report notes that one in every four hospital nursing positions is vacant due to high staff turnover, shifting care delivery models, and an insufficient talent pipeline.
Throughout it all, UMSON’s mission to prepare exceptional new nurses has remained consistent, and it continuously seeks innovative solutions to develop nurses prepared to adapt to the changing demands of the profession.
MORE STUDENTS REQUIRE NEW OPPORTUNITIES
UMSON’s class numbers for entry students continue to grow year over year. Last fall’s entry Bachelor of Science in Nursing (BSN) class was the largest in UMSON’s history, at nearly 215 students. The School’s current challenges revolve around adequate classroom space, recruiting enough qualified faculty, and ensuring requisite clinical education opportunities. To accommodate the increase in the number of students enrolled, the School has had to be creative to overcome these barriers, says Katie McElroy, PhD ’16, MS ’10, BSN ’97, RN, CNE, associate professor and associate dean for the baccalaureate program. “We’re so fortunate to be in this region that has a number of outstanding, high-quality facilities that partner with us to educate our students,” McElroy says.
The School has partnered with the University of Maryland Medical System (UMMS) to establish a Practicum to Practice Program (P3), which creates a path for BSN students to move seamlessly from their senior practicum experience to a registered nurse position at an UMMS hospital. P3 participants complete their senior practicum on a specific unit, serving as a nurse graduate following graduation. Once the graduate successfully completes
“We’re debunking the idea that there are natural teachers or born teachers. It’s really a skillset like any other that one needs to practice and learn.”
SUSAN BINDON

18 • NURSING FOR/UM • SPRING 2024
A WORKFORCE TO BE RECKONED WITH
exam and licensure requirements, they transition to a Clinical Nurse I position. More than 200 UMSON students have gone through the P3 program since its introduction in spring 2022, and UMMS hospitals have retained over 70% of the graduates.
This opportunity merges a hiring strategy with a high-quality and personalized practicum experience. It incentivizes graduating students to consider employment at an UMMS hospital, and it gives them the autonomy to select their practicum placement while also relieving the stress of job searching.
Hospitals win by getting commitments from students early, and onboarding times for these new hires decrease. “When the student graduates and becomes a staff nurse, that orientation time can be shortened,” McElroy says. “They’ve already been on that unit for months, so they’re familiar with a lot of the policies and the physical layout and the location of things. Those logistics that can take a while to learn have hopefully already been learned.”
The clinical education experience is essential to preparing new nurses for practice. The hours spent in clinical rotations allow students to integrate their theoretical knowledge with hands-on experiences that enhance critical-thinking, decision-making, and problemsolving abilities.
Lisa Rowen, DNSc, MS ’86, RN, CENP, BCC, FAONL, FAAN, chief nurse executive of UMMS who created the P3 concept, developed another model that modernizes the traditional clinical education model and aligns with the American Association of Colleges of Nursing (AACN) Essentials, an updated framework for nursing education using a competency-based approach. UMMS and UMSON partnered again on the pilot for the Academy of Clinical Essentials (ACE), which matches up to four entry students with an UMMS-funded clinical instructor for a full shift.
“We’re really focused on the experience of the students,” McElroy says. “The students are immersed in that unit, they’re working with a nurse who’s intimately familiar with that setting and who’s functioning as a staff nurse, picking up an extra shift on that particular day.”
ACE elevates nursing education by providing students with an authentic inpatient nursing experience but also addresses staffing issues and the faculty shortages plaguing schools of nursing. “An ACE cohort will create
better staffing ratios on units where there may be some nurse vacancies,” Rowen said in a 2022 article. “It also provides experienced UMMS nurses an opportunity to diversify their role by being a clinical instructor for future nurses.” Another perk for instructors is removing the requirement to grade assignments and supervise students during simulation labs. A clinical liaison takes over those duties.
RECRUITING AND PREPARING MORE FACULTY
In addition to the clinical nurse shortage plaguing hospitals across the country, nursing schools are struggling with a talent pipeline for faculty positions. According to a 2022 AACN report, a survey of 909 nursing schools identified a national nurse faculty vacancy rate of about 9%. Most of the vacancies (85%) were faculty positions requiring or preferring a doctoral degree. The impending increase in faculty retirements will likely create “a significant ‘brain drain’ that will exacerbate the current faculty shortage,” states a 2021 report from the National Advisory Council on Nurse Education and Practice.
UMSON had the foresight to address faculty preparation two decades ago, when it launched the Institute for Educators in 2004, the first of its kind in the country. The institute has two primary initiatives: prepare nurses for teaching roles in Maryland’s academic and practice settings and provide ongoing professional development for faculty and educators in clinical settings. Since the institute’s inception, nearly 800 graduate and postgraduate students have taken academic courses in the institute’s Teaching in Nursing and Health Professions Certificate. This 12-credit, graduate certificate prepares nurses and other health professionals for teaching roles.
Increasing the number of prepared nurse educators is critical to expanding the nursing workforce. “So many faculty have great expertise in their clinical specialty but are not prepared as teachers,” says Bindon, who also serves as director of the institute and of the teaching certificate. “Just having a doctorate or master’s degree in nursing doesn’t guarantee teaching skills. That was a really important gap to address.”
Bindon is passionate about preparing educators who can attract great students to become nurses that make
NURSING FOR/UM • SPRING 2024 • 19
a positive impact on health care. She recently created a pilot program funded by a $145,000 Innovation Challenge grant from the Bedford Falls Foundation Charitable Trust, a donor-advised fund established by philanthropists Bill and Joanne Conway. The UMSON Nursing Professional Residency for Outstanding Faculty (N-PROF) is a yearlong program aimed at facilitating nurses who are transitioning from careers in practice to careers as nurse faculty. The program, scheduled to launch this year, is modeled after the nurse residency programs (NRPs) that have become a gold standard for new graduates in acute-care settings (more on that in “Residencies to Retain Nurses,” Page 21). NRPs help attract and retain new nurses as they transition from being students to working in a professional setting. The N-PROF program offers a similar model to new educators as they transition into teaching roles, providing structure and support to meet the needs of new faculty through a cohort model as they learn about effective ways to develop curriculum, deliver content, advise and grade students, collaborate on grants and projects, and more.
“Sometimes that first year can be very bumpy for faculty because of the expectations of the faculty role, especially in a school as large and complex as ours,” Bindon says.
This pilot program continues the work of the institute to advance the art and science of nursing education. “Students learn that there are learning theories – there’s science around teaching and learning,” Bindon says. “We’re debunking the idea that there are natural teachers or born teachers. It’s really a skillset like any other that one needs to practice and learn.”
NPS IN DEMAND
Nurse practitioner (NP) is tied with wind turbine services technician for the fastest growing occupation in America, according to the U.S. Bureau of Labor Statistics, which predicts a 45% surge in the number of NPs needed by 2032, equating to nearly 124,000 new NP positions.
UMSON is a leader in preparing advanced practice nurses to meet the growing need for health care in the region and beyond. In response to a 2004 position statement from AACN, the School transitioned its NP

“We want to increase the longevity and the quality of their careers, so when they do go out into the workforce, they’re going to stay at that first job longer. And stay in the nursing profession longer.”
KATIE MCELROY
20 • NURSING FOR/UM • SPRING 2024 A WORKFORCE TO BE RECKONED WITH
program from a Master of Science degree to the Doctor of Nursing Practice (DNP) degree. Since that change took place in 2006, the school has graduated nearly 1,000 doctorally prepared nurses.
UMSON has increased the number of available primary care providers, in particular, by expanding the School’s DNP Family Nurse Practitioner (FNP) specialty to its Universities at Shady Grove (USG) location in Rockville, Maryland, in 2017, enhancing the output of FNPs who can make a substantial contribution to the well-being of Maryland’s communities and, in particular, better meet the needs of underserved areas in the western and southern areas of the state.
CARING FOR NEW NURSES
It has come increasingly to the forefront of public consciousness that the professionals caring for patients also need to be cared for. Health care organizations are recognizing that a commitment to nurse well-being is essential to employee retention. The AACN Essentials call for nursing schools to prepare students with specific competencies related to developing wellness and resilience for themselves and others.
The School’s new BSN curriculum introduces these competencies in a first-semester course that addresses how to manage stress and counter burnout as a student and future nurse by practicing evidence-based skills to promote resilience. The course utilizes resources from R3: The Renewal, Resilience, and Retention of Maryland Nurses Initiative, a state Nurse Support Program II-funded project that aims to address root causes of burnout and disengagement to improve well-being, strengthen the bridge from education to practice, and increase retention.
RESIDENCIES TO RETAIN NURSES
Supporting new nurses through their first year of clinical practice is essential to retention.
“When students graduate, they pass the National Council Licensure Exam, but they don’t just hit the ground running – there are gaps,” says Jennifer Zipp, DNP ’18, MS ’12, BSN ’00, RN, executive director of the Maryland Organization of Nurse Leaders/Maryland Nurse Residency Collaborative (MNRC).
“New graduates need training and support.”
Kelsey Bradford, MD, MPH, assistant professor, was appointed as the school health officer at the beginning of the COVID-19 pandemic, and her role has expanded to include a focus on student wellness.
In 2022, Bradford surveyed students about their feelings regarding the School’s commitment to their wellness. The results revealed that students believe UMSON cares about student wellness, but students don’t have the time or available resources to prioritize their personal well-being. Bradford is working with the
The MNRC supports Maryland hospitals in offering the 12-month Vizient/AACN Nurse Residency Program™ model, which features a series of synchronous, asynchronous, or simulation experiences that support new nurses as they transition from students to professionals.
“The NRP supports growth in three basic areas that are critical to new nurses: competence, confidence, and professional identity,” Zipp says. After completing the NRP, new nurses reflect an increase in those three areas, and hospitals have seen improvements in patient safety and quality of care. The program is a boon for the workforce, too. In 2022, MNRC organizations saw an 89% retention rate of nurses in their first 12 months of hire, compared to a national retention rate of 67%.
School’s student affairs team and her counterpart at USG to create more resources for students. “The hope is to incorporate wellness strategies into the curriculum since our students feel like they don’t have the time outside of class to focus on them,” Bradford says.
The changing demands of the profession are straining nursing schools, faculty, and new graduates, but passionate nursing champions are adapting and innovating. Increasing the number of students, faculty, and educational opportunities is essential, but the right support ensures that “each student is ready to hit the ground running,” McElroy says. “We want to increase the longevity and the quality of their careers, so when they do go out into the workforce, they’re going to stay at that first job longer. And stay in the nursing profession longer because they have those tools and those skills to take care of themselves in this incredibly demanding career.”
NURSING FOR/UM • SPRING 2024 • 21

22 • NURSING FOR/UM • SPRING 2024 ERIK NEILSEN/UMB
Caring for our Community
BY MARY THERESE PHELAN
A woman with a long history of debilitating migraines was so happy with the care she received from William Mangana, DNP ’20, CRNP, FNP-C, assistant professor, she regretted not being able to name her grandson after him.
“She told me that if her grandson didn’t already have a name, she would have told her daughter to name him after me. I still laugh and smile about that one,” says Mangana, who had prescribed a new medication for her, ending years of suffering.
Mangana serves as clinical faculty in the Doctor of Nursing Practice (DNP) program and as a primary care provider for patients at the University of Maryland Medical Center Midtown Campus through the West Baltimore RICH Collaborative, an UMSON-led partnership of community- and faith-based organizations, academia, and hospitals and hospital-related entities in Baltimore seeking to address racial disparities by focusing on hypertension and social isolation.
“UMSON produces culturally competent, tech-savvy, empathetic providers who are well versed in evidence-based treatment and protocols,” Mangana says. “We are vital to health care in this community simply because we care and strive to make a difference each and every day without bias and indifference.”
“We
are vital to health care in this community simply because we care and strive to make a difference each and every day without bias and indifference.”
WILLIAM MANGANA
A Closer Look At UMSON’s Community/Public Health Nursing Impact:
Interdisciplinary Clinic with Enterprise Properties
After Barbara Resnick, PhD ’96, RN, CRNP, FAAN, FAANP, professor, Sonya Ziporkin Gershowitz Chair in Gerontology, and associate dean for research, spent several years providing health education at senior apartment complexes owned by Enterprise Properties, the Baltimore-based property management company asked Resnick and her fellow interprofessional providers to set up clinics at four low-income senior housing sites in and around the city.
With the help of several other University of Maryland, Baltimore (UMB) faculty, Resnick initiated the clinics in 2023. Several DNP students, a PhD student, and University of Maryland School of Pharmacy students also contribute to the clinic work.
Resnick and her team keep busy during weekly visits to the sites, educating seniors on proper medication management, providing blood pressure checks, administering immunizations and vaccinations, removing ear wax, and providing skin and nail care, among other clinical interventions. They also conduct Medicare annual wellness visits during residents’ birthday months, complete with a small birthday gift from the care team.
“The response has been wonderful,” Resnick says. “In the first year, we were able to reach and provide care for 61% of all residents living in these communities, which is pretty amazing. We can’t fix most of the social determinants of health. But we can provide care, right here, right now.”
THE CLINIC, COMPUTED
In the first year: nearly 230 residents seen, on average 3 or 4 times 131 immunizations
576 blood pressure checks
92 footcare assessments 69 hearing evaluations 119 wellness visits 13 assessments for acute medical issues
opposite page: Tech. Sgt. Irene Mortera, BA, ADN, RN, an RN-to-BSN student and a member of the U.S. Air Force, provides a health assessment to a community member in the UMB Community Engagement Center’s Health Suite.
NURSING FOR/UM • SPRING 2024 • 23
FEATURE
“Students will often say that it was an eye-opening experience, that it changed the way that they think about health care and the way that they think about their own practice.”
MEGAN DOEDE
The Governor’s Wellmobile Program
Operated by UMSON, the Governor’s Wellmobile program delivers primary and preventive health care to underserved patients in Maryland. Staffed by nurse practitioners and a Spanish-speaking outreach worker, the Wellmobile program serves areas in Prince George’s County. Without visits from the Wellmobile team, many of the patients would have limited or no access to health care.
“We want to bring really strong nursing care right to the community,” says Veronica Gutchell, DNP ’13, RN, CNS, CRNP, assistant professor; chair of the Department of Partnerships, Professional Education, and Practice; and director of the Wellmobile Program. “We have quite a lot of knowledge about delivering primary care. I think the School of Nursing is perfectly poised to have a nursemanaged clinic out there that helps the underserved stay healthy and well.”
In fiscal year 2023, the Wellmobile program conducted 723 primary care telehealth visits, all in Prince George’s County, primarily serving immigrants from El Salvador and Guatamela.
The Wellmobile also provides important interprofessional learning opportunities as a clinical site for nursing, pharmacy, and social work students, who gain skills in assessment, diagnosis, and management of common chronic diseases and uncomplicated acute illnesses.
Health Care in the Library
Last spring, UMSON placed Bachelor of Science in Nursing (BSN) students in multiple branches of the Enoch Pratt Free Library throughout Baltimore in a partnership that was the first of its kind in Maryland. Through the community/public health clinical experience, students offered blood pressure checks, health screenings, and more to library patrons.
The following semester, the program expanded to Prince George’s County Memorial Library System, placing entry BSN students from UMSON’s location at the Universities at Shady Grove in the Greenbelt Branch Library, where they provided health screenings, light physical activity programs, and educational presentations. Thanks to a new grant from the U.S. Health Resources and Services Administration and the Baltimore City

Health Department, the Enoch Pratt Free Library is again partnering with UMSON for a program in which nursing students assist older city residents to access patient portals.
“Every time you go to the doctor these days, they want you to use a patient portal, and a lot of our older community members don’t know how to do that,” says Michelle R. Spencer, DNP ’19, MS ’06, BSN ’84, RN, assistant professor and director of the Master of Science in Nursing Community/Public Health Nursing specialty. BSN students rotate among the Central and Pennsylvania Avenue library branches and the health department’s Harford and Oliver senior centers.
Paul’s Place
One of UMSON’s longest-standing community partnerships is with Paul’s Place, a nonprofit human services outreach center that aims to improve quality of life in Southwest Baltimore. For nearly 40 years, the School has provided nursing services there. Megan Doede, PhD ’19, MS ’13, RN, assistant professor, serves as the center’s community health nurse.
During the academic year, UMSON students provide basic health and wellness services and nursing case management at Paul’s Place and participate in an interprofessional street outreach program to neighbors experiencing unsheltered homelessness; students regularly deliver essential supplies, refer neighbors to community resources, and follow up with neighbors’ progress. Paul’s Place gives nursing students opportunities to learn community-based care, an essential skill for building a well-rounded and informed nursing workforce.
“It’s certainly the most rewarding type of nursing that
24 • NURSING FOR/UM • SPRING 2024 CARING FOR COMMUNITY
above: Folahanmi Suberu (center), a Bachelor of Science in Nursing student, provides health information to a patron at the Prince George’s County Memorial Library System Greenbelt Branch Library.
MATTHEW D’AGOSTINO/UMB
right: A student checks the blood pressure of a neighbor at Paul’s Place human services outreach center in Southwest Baltimore.
I’ve ever done,” says Doede, who used to work as an emergency nurse. “And students will often say that it was an eye-opening experience, that it changed the way that they think about health care and the way that they think about their own practice.”
University of Maryland, Baltimore Community Engagement Center
The UMB Community Engagement Center (CEC) in the Poppleton neighborhood of West Baltimore provides a variety of programs that leverage University resources to meet community-identified needs such as exercise, food, and after-school and educational programming.
It also offers a free public health nurse program through its Health Suite that serves anyone in Baltimore city but focuses on residents in West Baltimore. Health Suite visits include interventions such as

“We’re trying to bring the best of UMB into the community.”
KELLY DORAN
health assessments, screenings, linkage to care, care coordination, clinical case management, and more. Reinforcing the partnership aspect of the CEC, the suite doubles as a weekly interprofessional clinical site for UMSON and other UMB students, which Kelly Doran, PhD ’11, MS ’08, RN, FAAN, associate professor, leads. This semester, four RN-to-BSN students and two University of Maryland School of Medicine students are gaining clinical experience there.
“We’re trying to bring the best of UMB into the community and to help use that expertise to increase residents’ quality of life,” Doran says. “You know it’s working when a neighbor sends somebody in, and we say, ‘How did you hear about us?’ and they say, ‘My neighbor came here, and you helped her.’”
Christopher Place Employment Academy
Second-semester BSN students are placed at Christopher Place, a residential employment program in Baltimore that provides education, training, and recovery support to formerly homeless men, for their community/ public health nursing clinical. There, they conduct needs assessments, blood pressure screenings, and care navigation activities and connect residents to primary and specialty care, health and social resources, and health
“The gentlemen of Christopher Place learn from the students, but I believe the students learn even more from them.”
RACHAEL HOLTON PARRAN
management programs. Students also provide weekly health education presentations on a variety of topics.
“We have a responsibility to our neighbors to work to improve health outcomes and not simply rely on community members as patients or learning opportunities,” says Rachael Holton Parran, MS ’14, BSN ’03, RN, clinical instructor. “With so much of health care happening outside of the acute care setting, there is no better way than to work within the community to change health care outcomes, and the learning that takes place is bidirectional. The gentlemen of Christopher Place learn from the students, but I believe the students learn even more from them.”
NURSING FOR/UM • SPRING 2024 • 25
MATTHEW D’AGOSTINO/UMB


SPONSOR A WHITE SCRUB JACKET
We invite you to sponsor a white scrub jacket for our incoming entry students for the fall 2024 semester. A sponsorship of $50 provides a student with a white scrub jacket. Donors can write notes of encouragement to the students at the time of donation. These donations and notes show how much we support and welcome these future Maryland Nurses into our family! Donations can be made at www.nursing.umaryland.edu/ give/whitecoat.
26 • NURSING FOR/UM • SPRING 2024

The Welcome Ceremony
Ten years have passed since the inception at UMSON of the White Coat Ceremony, in 2014. Incoming entry-into-nursing students in the Bachelor of Science in Nursing (BSN) and Master of Science in Nursing (MSN) programs have been cloaked in white coats each semester, marking the first time the students are donning the professional uniform of a nurse. Held in Baltimore and at the Universities at Shady Grove, the ceremony also includes the recitation of an oath, an address by a distinguished alumnus, and a reception. The students receive “Keeping Healthcare Human” pins from the Arnold P. Gold Foundation. In 2014, UMSON was one of 100 nursing schools to receive funding support through a collaborative effort between the foundation and the American Association of Colleges of Nursing to pilot the ceremony.
In 2023, the ceremony was renamed the Welcome Ceremony and made the culminating event of orientation. Students now receive white scrub jackets provided through donations from alumni and friends, along with notecards featuring encouraging messages from the donors.
After a decade of this welcoming tradition, our most recent entering class reflects a marked increase in diversity among students. The percentage of students identifying as members of historically underrepresented populations has increased from 36% in fall 2014 to 60% in spring 2024. The main photo is from spring 2023, while the inset image shows the incoming class celebrated during the inaugural White Coat Ceremony in 2014.
— Jillian Dreicer
NURSING FOR/UM • SPRING 2024 • 27
2014 PHOTO: FROM THE UMSON ARCHIVES; 2023 PHOTO: AL GENERAL
Class Notes
Let your fellow alumni know what’s happening in your professional life. Submitting an update to Class Notes is easy; just visit nursing.umaryland.edu/ classnotes or contact us at alumni.nursing@umaryland.edu or 410-706-7640. You can also send us mail courtesy of the University of Maryland School of Nursing Office of Development and Alumni Relations, 655 W. Lombard St., Baltimore, MD 21201.
As we are unable to confirm all alumni credentials, only UMSON degrees and graduation years are included.
1960s
Marilyn Laken, BSN ’64, published the book I’ve Never Been Old Before: A Practical Guide to Aging and is the host of a podcast, Never Been Old B4.
1970s
J Taylor Harden, MS ’77, BSN ’72, received the Doris Schwartz Gerontological Nursing Research Award from the Gerontological Society of America at its 2023 Annual Scientific Meeting, held in Tampa, Florida, in November.
Robin Quivers, BSN ’74, who has been Howard Stern’s co-host on his radio show, The Howard Stern Show, for decades, was featured in a July article in The (Waynesville, North Carolina) Mountaineer and in a September article in the Longview (Texas) News-Journal about celebrities who have served in the military. Quivers joined the U.S. Air Force in 1975, when she was commissioned as a second lieutenant.
Patricia C. McMullen, MS ’81, BSN ’75, was a recipient of the Arnold P. Gold Foundation and American Association of Colleges of Nursing’s (AACN) inaugural AACNGold Interprofessional Humanism in Healthcare Award for supporting comprehensive women’s health care and disseminating best practices on women’s health to clinicians across a wide range of disciplines.
Deborah L. Kennedy, MS ’84, BSN ’79, was inducted into the Circle of Excellence by The Daily Record after having been named by the publication as one of Maryland’s Top 100 Women for the third time.
1980s
Eileen Vorbach Collins, BSN ’81, published a collection of essays, Love in the Archives, A Patchwork of True Stories About Suicide Loss, in November. Her writing has received the Diana Woods Memorial Award for Creative Nonfiction, The Gabriele Rico Challenge Award, and a Gold Royal Palm Award. Her work has been nominated twice for a Pushcart Prize.
Patricia (Bielski) Patterson, BSN ’82, has served as a state chapter officer of the American Nephrology Nursing Association (ANNA) in Maryland and Colorado. She published three articles in the Nephrology Nursing Journal and was a co-author for the Peritoneal Dialysis chapter of the Contemporary Nephrology Nursing Textbook, 4th edition. Patterson served as the keynote speaker for the 2023 national ANNA fall conference, presenting “Overcoming Obstacles to Home Hemodialysis.”
Laura J. Wood, MS ’83, was appointed president of the American Nurses Credentialing Center in August.
LOVE FINDS ITS WAY AT UMSON


Monika Bauman, MS ’10, BSN ’90, director of patient care services, women and children’s health, at the University of Maryland Medical Center (UMMC), and Mark Bauman, BSN ’89, senior clinical nurse II at UMMC, met in 1987 when they were students in the Anne Arundel (Maryland) Community College pre-nursing program.
When Mark enrolled at UMSON, he fell out of contact with Monika, his former lab partner. In 1990, Mark started working at UMMC and one day grabbed lunch at the University of Maryland, Baltimore’s former student union cafe, where he recognized Monika taking a break from classes at UMSON. After reconnecting, they married the following year and started a family. This year marks 30 years of working at UMMC together. The key to their success: Keep work at work.
Did you meet your spouse or partner at UMSON? We’d love to hear your story! Email us at nrsalumni@umaryland.edu to let us know.
28 • NURSING FOR/UM • SPRING 2024
IN TOUCH
1990 2024
Visit nursing.umaryland.edu/classnotes to update your email address and we’ll send you our monthly events and quarterly updates newsletters.
Karen Doyle, DNP ’20, MS ’91, BSN ’85, senior vice president of patient care services and chief nursing officer at the University of Maryland Medical Center (UMMC), was a guest on “The Resilient Nurse,” a Johns Hopkins School of Nursing podcast series, in October, during which she discussed confronting workplace violence and nurturing resilience among nurses.
Renee Franquiz, DNP ’16, MS ’90, BSN ’85, UMSON assistant professor and director of the Doctor of Nursing Practice (DNP) Post-Master’s option, participated in the University of Maryland, Baltimore’s Costa Rica Faculty Development Institute in December.
Lisa Rowen, MS ’86, UMSON Visionary Pioneer and chief nurse executive for the University of Maryland Medical System (UMMS), was quoted in a Baltimore Sun article about UMMS’ Academy of Clinical Essentials (ACE), an education model aimed at addressing the nursing workforce shortage. Rowen, along with Elizabeth Cushing, BSN ’14, a trauma nurse at UMMC, also participated in an episode of WYPR “On the Record,” discussing the impact of ACE on staffing at UMMS hospitals. WYPR is Baltimore’s National Public Radio affiliate.
Sandra Griffin, MS ’01, BSN ’87, was appointed to the board of directors for Providence of Maryland, a nonprofit organization serving adults with intellectual and developmental disabilities, in December.
1990s
Marjorie Simpson, PhD ’10, MS ’01, BSN ’90, received the Advanced Practice Provider of the Year Award at Carroll Hospital in Westminster, Maryland.
Ann Warner, MS ’92, was named dean of the McNeese State University College of Nursing and Health Professions in Louisiana in July.
Elizabeth Elliott, MS ’02, BSN ’95, nurse administrator for the Montgomery County Department of Health and Human Services and president of the Maryland Association of School Health Nurses, authored a commentary on the Maryland Matters news site in January, supporting the Maryland Kids Code, a bill designed to provide online guardrails and address the teen health crisis exacerbated by social media.
Barbara Moore, MS ’95, pediatric nurse practitioner and clinical director of the Lead Poisoning Program at Mt. Washington Pediatric Hospital in Baltimore, was quoted in a November Washington Post story about lead poisoning caused by tainted foil-lined fruit puree pouches.
Marla De Jong, MS ’96, UMSON Visionary Pioneer and dean of the University of Utah School of Nursing, was featured in September in a segment on WKSL News, Salt Lake City’s NBC affiliate, about the school’s 75th anniversary celebration.
Sarah Arnett, MS ’13, BSN ’97, was appointed president of Your Doc’s In, a provider of urgent and immediate care on Maryland’s Eastern Shore, in June.
Sylvia Trent-Adams, MS ’99, UMSON Visionary Pioneer, shared her vision as president of The University of North Texas Health Science Center at Fort Worth in a “Spotlight On” article by Capital Analytics Associates in November.
2000s
Joyce McMahon, BSN ’00, staff nurse at the UMMC Midtown Campus Center for Addiction Medicine, was quoted in a story on NurseJournal in September about caring for substance use patients.
Brittany Altermatt, MS ’05, joined the medical oncology team in September as an adult nurse practitioner at the May Cancer Center at the University of Texas Health San Antonio.
BACK TO THEIR ALMA MATER
The following alumni have returned to UMSON in faculty or staff positions, shaping the next generation of nurses.
Lindsay Ward, MS ’14, BSN ’09 clinical instructor
Jessica Page Sullivan, MS ’14 clinical instructor
Nyree Williams, DNP ’21, MS ’16 assistant professor
Ozioma Erondu, DNP ’20 assistant professor
Taylor Melton, DNP ’21 assistant professor
Lillian Abraham, MSN ’22 nursing development and education specialist
GREATNESS IN MARYLAND
During the Maryland Nurses Association (MNA) 120th Annual Convention in October in Ocean City, Maryland, two UMSON alumnae received awards.
Barbara Biedrzycki, MS ’96
MNA Board of Directors Distinctive Service Award
Christie Simon-Waterman, DNP ’16 Outstanding Leadership Award and Linda Stierle Exemplary Service Award
NURSING FOR/UM • SPRING 2024 • 29
Want the scoop from UMSON?

Lt. Col. Tekia Jones, BSN ’07, a Phase 2 clinical site director and assistant professor at the Uniformed Services University of Health Sciences in Maryland, was recently promoted to lieutenant colonel.
Hershaw Davis Jr., BSN ’09, UMSON assistant professor, completed a dual DNP/Master of Business Administration degree at Wilmington University in Delaware last fall.
2010s
Michelle D’Alessandro, DNP ’10, was named the chief nursing officer at University of Maryland Upper Chesapeake Health.
Tonii Gedin, DNP ’14, MS ’11, was appointed the Anne Arundel County (Maryland) Health Officer.
Oluwatosin Olateju, MS ’15, BSN ’11, was appointed co-chair of the new Maryland Commission on Public Health by Gov. Wes Moore.
Maj. Regine Faucher, BSN ’12, earned a DNP degree from Uniformed Services University of Health Sciences in Maryland in May 2023. She serves in the U.S. Army Nurse Corps.
PURSUING EXCELLENCE IN PUBLIC HEALTH
Rear Adm. Jennifer Moon, DNP ’20, was appointed chief nurse officer of the U.S. Public Health Service (USPHS) Commissioned Corps. In this role, Moon advises the Office of the Surgeon General and the U.S. Department of Health and Human Services on the recruitment, assignment, deployment, retention, and career development of nurse professionals. Moon’s vision for the USPHS Commissioned Corps is the pursuit of excellence; she has said she believes that nurses are the heart and the hope of the USPHS Commissioned
Deirdre Smith, MS ’15, BSN ’12, a vascular surgery nurse practitioner at University of Maryland Baltimore Washington Medical Center, talked about the prevalence and warning signs of vascular disease on a Maryland Public Television “Your Health” segment in September 2022.
Nicole E. Smith, MS ’14, UMSON assistant professor, was selected to participate in the 2023 National League for Nursing LEAD program.
Diane Constantine, MS ’16, director of clinical informatics for UMMS, was accepted into Healthcare Leadership Academy’s class of 2025 Technology Fellowship Program.
Samantha Hoffman, DNP ’23, MS ’16, UMSON assistant professor, joined the Choptank Community Health System’s Denton (Maryland) Health Center as a pediatric nurse practitioner in August. She also serves as the secretary and continuing education chair of the Chesapeake Chapter of the National Association of Pediatric Nurse Practitioners.
Corps as well as the health of the nation. Previously, Moon served as the deputy assistant director for health care compliance and chief compliance officer at the Immigration and Customs Enforcement Health Service Corps. Moon is a board-certified family nurse practitioner and earned her DNP at UMSON with a concentration on health care management and evidence-based practice. She was commissioned as a lieutenant at the Centers for Medicare and Medicaid Services headquarters in Baltimore in 2005.
2020s
Richard P. Conley Jr., DNP ’20, UMSON assistant professor and assistant director of the DNP Nurse Anesthesia specialty, is serving a second term as chair of the American Association of Nurse Anesthesiology Continuing Education Committee.
Melissa Hibdon, BSN ’20, was appointed vice president, stem cell transplant and cellular therapy for Community Health Network in Indianapolis.
Ameera Chakravarthy, PhD ’22, UMSON assistant professor and director of the DNP Adult-Gerontology Acute Care Nurse Practitioner/AdultGerontology Clinical Nurse Specialist specialty, was appointed as a member of the Maryland Board of Nursing by Gov. Wes Moore in December. Last summer, she attended the Boy Scouts of America Baltimore Area Council Piedmont Adventure Day Camp to teach scouts and youth leaders first aid and wound treament.
30 • NURSING FOR/UM • SPRING 2024 IN TOUCH
In Memoriam
Yvonne J. Narad, DIN ’45
Rebecca Lilliard Umstead, DIN ’45
Ethel “Rusty” G. Brandon, DIN ’47
Nolly S. Chess, DIN ’48
Betty Jane Byers Cooper, MS ’61, DIN ’48
Florence Wolfel, DIN ’50
Carolyn Myers Baer, BSN ’53
Delores Tucker Bouzoukis, DIN ’53
Fae L. Renniger Reber, DIN ’53
Joan R. Baugher, BSN ’56
Patricia D. Curtis Brooks, BSN ’56
Nancy J. Coram, BSN ’56
Roberta Settle Barlow, BSN ’57
Joyce F. Kaetzel, BSN ’58
Shirley L. Hale, BSN ’60
Jane Morris Penny, BSN ’63
Joan F. Glick Leinweber, BSN ’67
Constance J. Meyd Johnson, MS ’72, BSN ’68
Rosemary Weber Sheehan, BSN ’68
Melanie Kambic, MS ’69
Sr. Beatrice Kellet, MS ’69
Mary E. Hogan, BSN ’70
Phyllis Koenig Marion, BSN ’70
Linda S. Ziegler Dubansky, BSN ’71
Dolores P. Niedzwiecki, MS ’71
Eva L. Rauseo, MS ’72
Barbara E. Hitchcock Scott, BSN ’73
Mary Jean Shekiro Kotch, BSN ’74
Diane C. Bartoo, BSN ’75
Jeanne Picariello Murphy, BSN ’75
Faye Ann Poff Niner, BSN ’75
Gwendolyn M. Bradford Kurtz, MS ’76
Mary D. Sattazahn, MS ’85, BSN ’76
Janice E. Richardson, BSN ’79
Sharon Peoples Ramsay, BSN ’80
Deborah J. Repkorwich, BSN ’80
Sarah K. Polk, MS ’82
Gail Burdsall Cowan, MS ’85
Mary J. Cooper, MS ’89
Sybil Greenhut, MS ’90
Brenda J. Roup, PhD ’95
Allyson Kellner Villamater, MS ’98
Jane J. Solberg, BSN ’13
This list includes notices the School of Nursing received from June 23, 2023 - March 27, 2024.
Remembering
Marisa L. Wilson
1957 - 2024

Marisa L. Wilson, DNSc, MHSc, RN-BC, CPHIMS, FAMIA, FIAHSI, FAAN, a former UMSON associate professor, died Jan. 5 from cholangiocarcinoma. Wilson joined the UMSON faculty in 2004 and served as the director of master’s programs from 2011 until she retired in 2013. She was a longtime member of UMSON’s Summer Institute in Nursing Informatics (SINI) planning committee and helped establish the conference’s SINI U track, which focuses on teaching informatics.
In addition to her role at UMSON, she had faculty and administrative appointments at the University of Alabama at Birmingham and the Johns Hopkins University School of Nursing. She also worked at Johns Hopkins Bayview Medical Center, the Maryland Department of Health, and the Governor’s Office for Children.
Wilson was a board-certified informatician with an interest in health information technology (IT) policy, implementation, and positive patient outcomes and clinical efficiency supported by technology. She spent more than 15 years as a nurse clinician working in acute physical rehabilitation, medical-surgical, and telemetry units. In addition, she spent more than 25 years as an analyst, project leader, and manager implementing information systems in public health and acute care settings.
Her research interests were varied and centered on health IT, clinical informatics, organizational leadership and change, evidence-based practice, public policy, patient engagement, clinical decision support, and more.
CALLING ALL ALUMNI
Contribute Your
Stories to UMSON’s Oral History Project
In recognition of UMSON’s 135th anniversary this year, we have partnered with Publishing Concepts Inc. (PCI) for a comprehensive Oral History Project that will gather stories from alumni about your experiences at UMSON. These stories will be compiled in a commemorative print and digital book that celebrates the impact UMSON has had on your lives and on who you are today.
You should have received a postcard and/ or email asking you to call PCI to update your information. Once you contact them, a team member will ask you questions about your contact information and your UMSON stories and memories. There is no obligation to purchase the book for your stories to be included.
If you have any questions, please contact us at nrsalumni@umaryland.edu or 410-706-7640.
NURSING FOR/UM • SPRING 2024 • 31
VOLUNTEERS MAKE A DIFFERENCE! YOU WE NEED YOU
SHARE YOUR TIME AND TALENT HOW AND WHEN YOU CHOOSE
SPOTLIGHT ON
THE ALUMNI COUNCIL
Get involved at a leadership level! Nominate yourself or a fellow alum for an Alumni Council position.
The UMSON Alumni Council is the Alumni Association’s advisory group that meets twice a year to discuss alumni-related matters, including event planning, alumni outreach, student/alumni relations, and raising funds for the School.
Any UMSON alum can recommend candidates to the Nominating Committee for consideration. For nominations to be considered for the 2025 slate, please submit the nomination form at nursing.umaryland.edu/ alumniassociation by July 1.
For more information, contact the Office of Development and Alumni Relations at nrsalumni@umaryland.edu or 410-706-7640.

For more than four decades, the University of Maryland School of Nursing’s PhD program has prepared scholars and researchers to tackle the greatest challenges facing health care. Join Dean Yolanda Ogbolu, a 2011 graduate of UMSON’s PhD program, at this 45th anniversary celebration of excellence.
Friday, Sept. 20, 4 - 7 p.m., and Saturday, Sept. 21, 9 a.m. - 4 p.m.
UMSON, Baltimore
Contribute to our PhD Profiles in Excellence: We’re creating a digital collage to highlight the accomplishments of our PhD alumni. If you would like to be included, scan the QR code at right and complete the questionnaire on the website by July 1, 2024. Learn more and register at nursing.umaryland.edu/phd45.
32 • NURSING FOR/UM • SPRING 2024 IN TOUCH
Unleashing Inclusivity in Health Care
Asha Storm, PhD ’23
BY JILLIAN DREICER
Asha Storm, PhD ’23, began their career in the animal behavior field, interning as a zookeeper at the San Antonio Zoo and later caring for the welfare of primates at the National Institutes of Health (NIH) and training them to give blood voluntarily to find a cure for HIV.
Storm’s interests began to shift to human behavior and trauma research as they witnessed how their friends, who worked in hospitals, suffered from secondary traumatic stress in their health care professional roles. When a therapy dog visited Walter Reed National Military Medical Center, Storm saw how the animal’s presence had a positive effect on patients’ and providers’ mental health.
“My research area of interest became how to help the helpers.”
ASHA STORM
Storm chose to attend UMSON’s PhD program as a non-nurse, initially interested in the humananimal interaction research in which their advisor, Erika Friedmann, PhD, faculty emerita, was involved. At the time, Friedmann was researching how canine interaction affects stress levels in military veterans with post-traumatic stress disorder.
However, a few years into the program, Storm’s focus again shifted to traumatic stress in nurses due to the COVID-19 pandemic. “My research area of interest became how to help the helpers,” Storm explains.
“I was interested in determining where points of intervention might be located in the case of another major medical disaster, so that nurses and other emergency frontline personnel could receive support before, during, and after the disaster to have better mental health outcomes.”

As an LGBTQIA+ person with chronic pain and invisible disabilities, Storm has experienced firsthand how health care does not always work for historically marginalized individuals. In addition to their role as a program analyst/health specialist for the NIH National Institutes of Biomedical Imaging and Bioengineering (NIBIB), Storm serves on multiple diversity, equity, inclusion, and accessibility (DEIA) groups. These initiatives include NIH’s UNITE Committee, focused on addressing structural racism at NIH and among the greater scientific community; the Sexual and Gender Minority Research Coordinating Committee; and NIBIB’s internal DEIA group. During their time at UMSON, Storm served as a student representative on the School’s DEI committee.
Storm was awarded the 2023 NIBIB DEIA Director’s Award for their
work advancing DEIA, both at NIBIB and throughout NIH, and they have been honored with several additional NIH awards for their work across the agency, including the NIH UNITE initiative.
“My hope is to help be part of the movement to recognize that DEIA is important in health care research and that diverse perspectives improve science and health care,” Storm says. “DEIA in health care research improves the design and conduct of research, ensuring that studies are culturally aware and reflect the diversity of patients in this country, as well as improving workplace culture and idea generation.”
NURSING FOR/UM • SPRING 2024 • 33
ALUMNI PROFILE
COURTESY OF ASHA STORM
The First of Her Kind
Janice “Jan” Wilson, DNP ’09, MS ’94, BSN ’74
BY MARY THERESE PHELAN
Like many twins, Janice Wilson and her sister, Janet – they both go by “Jan” – share a strong connection. As young girls, they shared toys, clothes, and a career goal: to become a nurse.
“We both knew as early as we can remember that we wanted to be nurses, we both wanted to make a difference,” says Janice Wilson, DNP ’09, MS ’94, BSN ’74, CRNP, NNP-BC, FAANP.
With that goal in mind, the sisters enrolled at UMSON, each earning a Bachelor of Science in Nursing degree in 1974.
Having developed an interest in pediatrics during her senior practicum course, Janice Wilson spent a month in the NICU at the
“The biggest reward I have ever gotten and continue to get is from the students. I would miss the interaction with the students if I didn’t teach. It feeds your soul.”
JANICE WILSON
University of Maryland Medical Center (UMMC), where she met the neonatologist Ronald Gutberlet, MD, who became her mentor.
“That’s how I got interested in neonatal nursing. There weren’t too many, if any, neonatal nurse practitioner programs that were close by, so it took me another few years to get that education,” says Wilson, who enrolled in the first cohort of Georgetown University’s continuing education neonatal nurse practitioner program in 1990. When she finished, Gutberlet offered her a full-time job as a neonatal nurse practitioner (NNP) at UMMC – officially making Wilson the first NNP in the state of Maryland.
“Most people didn’t know what the role was,” Wilson says. “It was a time when nurse practitioners were coming onto the scene and more visible, but neonatal nurse practitioners were not necessarily well understood or well accepted.”
Wilson returned to UMSON to earn her master’s degree in 1994 and then, pursuing another passion of hers, taught as a guest lecturer at the School in the Master of Science NNP program, eventually joining the faculty and becoming the program’s clinical coordinator.
“I almost became a grade school teacher,” Wilson says. “I think learning is exciting and sharing that with students is priceless.”
Beginning in 2015, when the School launched its Doctor of Nursing Practice (DNP) NNP specialty, Wilson served as its director. She worked to grow the program, eventually graduating 28 NNPs over the course of her career. The NNP specialty continues to boast a 100% certification pass rate nearly every year.
Wilson left UMSON in December but continues to teach DNP project courses.
As a tribute to her dedicated service and devotion to UMSON, Wilson was selected to serve as the mace carrier at the school’s most recent December Graduation ceremony, leading the procession of faculty and graduates.
“The biggest reward I have ever gotten and continue to get is from the students,” Wilson says. “I would miss the interaction with the students if I didn’t teach. It feeds your soul.”
Now, Wilson is looking forward to gardening. Incidentally, her younger sister, Jane, also became a nurse and is now retired.
Bill and Joanne Conway Dean, during the December 2023 Graduation ceremony
“It’s funny, nobody else in the family was a nurse, but that’s what we all chose to do,” Wilson says.
34 • NURSING FOR/UM • SPRING 2024
ALUMNI PROFILE
above: Wilson seeing a young pediatric patient, 2016; right: Who’s who? Janice Wilson (right) and her twin sister, Janet Wilson, during their junior year at UMSON, 1973; far right: Wilson (left) as mace carrier with Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN, the



NURSING FOR/UM • SPRING 2024 • 35 IMAGE AT LEFT: COURTESY OF JANICE WILSON; IMAGE AT RIGHT: MATTHEW D’AGOSTINO/UMB
DAVIS
JOHN
Alumni Event Bluestone Restaurant, Oct. 26, 2023


p Black Student Nurse Association ConnectFest USG, Nov. 16, 2023
Conway Scholars Luncheon UMB, Nov. 6, 2023




Welcome Ceremonies UMSON Baltimore, Jan. 17, 2024
BSN and MSN Clinical Nurse Leader Poster Day UMSON Baltimore, Dec. 4, 2023 u USG, Jan. 18, 2024
36 • NURSING FOR/UM • SPRING 2024
IN TOUCH
Events
p
MATTHEW D’AGOSTINO/UMB; OTHERS SUBMITTED AS COURTESY
PHOTOGRAPHY:
Sweet Start to the Semester UMSON Baltimore, Jan. 23, 2024


p Living History Museum
Docent Appreciation Tour University of Maryland School of Dentistry Museum, Jan. 24, 2024
Alumni Event
Jimmy’s Famous Seafood, Feb. 27, 2024
National Black Nurses Association Day on Capitol Hill Washington, D.C., Feb. 1, 2024


Save the Dates
Maryland Nursing Workforce Center: The State of the Maryland Nursing Workforce Symposium Thursday, June 6
Clinical Faculty Workshop Networking Event Wednesday, June 12
Monthly Research Seminar: Exemption and Risk Determination in Human Research Using Devices Thursday, June 20
33rd Summer Institute in Nursing Informatics (SINI) Thursday, July 18 - Friday, July 19
PhD Program 45th Anniversary Friday, Sept. 20 - Saturday, Sept. 21
Learn more about these events and others at nursing.umaryland.edu/events
Considering an advanced nursing degree? Learn more about our continuously nationally top-ranked Master of Science in Nursing, Doctor of Nursing Practice, and Doctor of Philosophy programs through online chats and information sessions offered regularly. See the schedule at nursing.umaryland.edu/visit


Pie Your Professor UMSON Baltimore, March 14, 2024
Orioles Spring Training Sarasota, Florida, March 16, 2024
NURSING FOR/UM • SPRING 2024 • 37
In December, UMSON graduated nearly 300 students, including 195 new nurses.
Advance

Often, spring awakens thoughts about new beginnings, but this issue of Nursing For/um has led me in a different direction. Beginnings are exciting, sometimes scary, and can be the start of something great. But continuing and persevering in the journey are just as important as that very first step.
The nation is facing a nursing shortage – a crisis that’s now reported on almost as regularly as the weather. The thought of fewer nurses – our health care heroes and educators of the next generation – when we’re facing a growing patient population is, of course, alarming.
UMSON was addressing the nursing shortage long before it became a headline. We graduate significant numbers of highly educated, competent, and compassionate new nurses. Our master’s and doctoral graduates are on the front lines of health care and teach those new to the profession in the classroom and in clinical environments.
UMSON has been at the forefront of innovative ways to address the national nursing shortage (see “A Workforce to Be Reckoned With,” Page 16). But did you know that our alumni and donors are an integral part of the process? They share their ideas, experiences, and resources to ensure that UMSON continues to lead the charge.
We invite each of you to be a part of this journey. Whether it’s reconnecting at an alumni event, mentoring a new student or recent graduate, or making a gift to educate students and develop new faculty, your support truly makes a difference. If you’d like to be more involved in these important moments of nursing and health care history, please connect with us. We are better together.
The Louisa Parsons Legacy Society

The School of Nursing’s Legacy Society is named in honor of pioneering nurse and philanthropist Louisa Parsons, the University of Maryland School of Nursing’s first superintendent; she made the first planned gift to the School in 1916. The Louisa Parsons Legacy Society comprises people who, like Parsons, are committed to supporting future generations of students and nurses by providing funding for scholarships, research, faculty positions, and other critical needs. Joining the Louisa Parsons Legacy Society allows you to make a significant difference to future nursing students without impacting your current lifestyle.
To learn more about making a planned gift, contact Stacey Conrad, associate dean for development and alumni relations, at sconrad@umaryland.edu or 410-706-7640.
Estate of Myrtle Ageton, DIN ’44, and Robert Ageton
Janet D. Allan
Stacey M. Conrad, MBA
Associate Dean for Development and Alumni Relations sconrad@umaryland.edu 410-706-7640
Anonymous
Floraine B. Applefeld
Estate of Carolyn V. Arnold
Jeanne Ascosi, BSN ’74
Estate of Zabelle S. Howard Beard
Deborah S. Beatty, MS ’96
Abbe R. Bendell, BSN ’74
Estate of Ann F. Bennett, MS ’69
Marjorie Stamler Bergemann
Estate of Jean L. Bloom, DIN ’46
Estate of Margaret Brandt, DIN ’50
Estate of Mary J. Brewer
Estate of E.L. Bunderman, DIN ’31, and Clarence Q. Bunderman
38 • NURSING FOR/UM • SPRING 2024
Estate of Ann Ottney Cain
Estate of Dorothy C. Calafiore, BSN ’51
Estate of Shirley E. Callahan, BSN ’52
Sharon A. Childs, MS ’91
Estate of Avon B. Chisholm
Marlene H. Cianci, MS ’66, BSN ’65
Estate of Gladys B. Clagett and Lansdale G. Clagett
Estate of Bonnie L. Closson, BSN ’61
Jon B. Closson
Claudette C. Clunan, BSN ’72
Steven S. Cohen
Regina M. Cusson, MS ’79
Estate of Mary Jane Custer
Jill A. DeCesare, BSN ’69
Carol Distasio, MS ’73, BSN ’71
Nancy Donovan, BSN ’76
Susan G. Dorsey, PhD ’01, MS ’98
Carol Drake, BSN ’68*, and Francis D. Drake
Celeste A. Dye, BSN ’66
Kay F. Edwards, PhD ’81, BSN ’67
Estate of Barbara Elgin, BSN ’54, and Lee Elgin
Estate of Lura Jane Emery, MS ’79
Julie C. Fortier, MS ’68
Judith A. Freitag, BSN ’77
Beth Ann Gan, BSN ’77
Estate of Mary H. Gilley, DIN ’44
Debbie Gilbert Glassman, MS ’79, BSN ’75
Estate of Judah Gudelsky
Carolyn Cook Handa, BSN ’63*
Laurette L. Hankins
Sharon Hanopole, BSN ’66
Phyllis B. Heffron, BSN ’74
Barbara R. Heller
Estate of K. Cornelia Hesselbach
Estate of Marie L. Hesselbach
Estate of Kjerstine K. Hoffman, DIN ’47
Carol A. Huebner, PhD ’90
Margaret H. Iles, DIN ’53
Catherine Ingle, BSN ’61
Estate of Mary McCotter Jackson
Jeanette Jones, MS ’70*
Estate of Jean W. Keenan, DIN ’48
Jane M. Kirschling and Robert Flick*
Anita M. Langford, MS ’79, BSN ’77
Cynthia P. Lewis, BSN ’58, and Jack C. Lewis
Estate of Phyllis R. Luckenbaugh, MS ’79, BSN ’72, and Paul Luckenbaugh
Estate of Ann Madison, BSN ’62
Estate of Mildred Madsen, BSN ’73
Estate of Rita Malek, DIN ’49
Myrna Mamaril, MS ’93
Estate of Demetria Manandic, BSN ’54
Estate of Lois Marriott
Joan Nicholason Martellotto, BSN ’66
Margaret A. McEntee, MS ’73
Estate of Wealtha McGurn
Beverly J. Meadows, PhD ’06, MS ’84, BSN ’69
Norma J. Melcolm, MS ’69
Estate of Joan L. Meredith, BSN ’62
Sharon L. Michael, BSN ’71
Nancy J. Miller, BSN ’73
Patricia Gonce Morton, PhD ’89, MS ’79
Sondra M. Mroz, BSN ’66
Elizabeth A. Ness, MS ’93
Evelyn Norwitz
Elizabeth O’Connell, MS ’74, BSN ’73
Daniel J. O’Neal III, BSN ’66
Harriet Palmer-Willis, MS ’70, BSN ’68
Barbara J. Parker, PhD ’86, MS ’76
Charlene M. Passmore, BSN ’77
Thomas S. Paullin
Margot A. Regen, MS ’79
Ann E. Roberts, BSN ’93
Estate of Margaret Robinson
Linda E. Rose, PhD ’92, and William G. Smillie
Estate of Amelia Carol Sanders, DIN ’53
Patricia A. Saunders, BSN ’68
Estate of William Donald Schaefer
Estate of Phyllis J. Scharp, BSN ’50
Sandra Schoenfisch, MS ’76
Eleanor B. Schron, PhD ’08, MS ’79, and Spencer R. Schron
Estate of Alta Fay Schuster, BSN ‘54
Estate of Beverly Seeley
Christine K. Shippen, MS ’98, BSN ’73
Martha J. Shively, BSN ’72
Deborah K. Shpritz, MS ’82, BSN ’78, and Louis Shpritz
Estate of Betty Lou Shubkagel, BSN ’54
Estate of Anna Mae Slacum
Estate of Connie Slewitzke, BSN ’71
Rebecca S. Stanevich, BSN ’73
Barbara A. Stepura, MS ’85
Estate of Marie V. Stimpson, MS ’89, BSN ’84
Jacquelyn M. Jones Stone, MS ’71
Estate of Sandra Sundeen, MS ’68
Estate of Ginger V. Swisher, DIN ’49
Susan L. Tancredi, MS ’79, BSN ’69, and Peter Tancredi
Courtney Ann Kehoe Thomas, BSN ’66
Diane L. Thompkins, MS ‘84
Virginia D. Thorson, BSN ’55
Estate of Norma C. Tinker, BSN ’48
Estate of Martha C. Trate, BSN ’48
Marion Burns Tuck, MS ’80
Robin Varker, BSN ’75
Elena V. Virts, PhD ’15, BSN ’00
Joella D. Warner, MS ’70, BSN ’64
Estate of Helen Parker Wear
Doris Baumgardner Webb, BSN ’59, and John H. Webb*
Margaret C. Wilmoth, MS ’79, BSN ’75
Susan Dorsey Wilson, BSN ’66
Estate of Patricia Yow
As we are unable to confirm all alumni credentials, only UMSON degrees and graduation years are included.
Champions for Challenging the Status Quo

Steve Cohen, MS, says his connection to nursing “goes back quite a bit.” He earned his bachelor’s degree from the University of Maryland School of Pharmacy at the University of Maryland, Baltimore and started working at what is now MedStar Good Samaritan Hospital in Baltimore in the late 1960s, when it first opened. “It’s a rare opportunity to start in a brand-new hospital,” he says. “Literally, one day we had one patient, one day we had two patients, etcetera. That afforded me a lot of extra time to get into the clinical areas and get to know what the nurses do, what their challenges are. And over the years, I used to tell people I was a nurse-trained pharmacist.”
Cohen went on to become a hospital executive, serving as executive vice president and chief operating officer at what was then Howard County General Hospital in the early 1990s and then returning to MedStar as senior vice president, integrated operations until he retired in 2010. In the late 1990s, he also served as commissioner for the Maryland Health Resources Planning Commission. But he has always given nurses the credit they’re due. “I learned that the care that patients were afforded in the hospital had so much to do with the quality and nature of the nursing staff,” he says. “I developed a very significant appreciation for the burdens they carry and how committed they are. In fact, you can pretty much judge a hospital based on its nursing staff.”
Which is why, in 2009, during the five years he served as chair of UMSON’s Board of Visitors, he and his wife, Sandy, a former nurse herself, made their first $50,000 bequest to UMSON. “We have to focus on growing the nursing workforce, and that means going to where the nurses are — at the school,” Steve Cohen says. “We need bedside nurses.”
Last fall, the Cohens made another $2 million bequest to the Alex Harrison Memorial Scholarship Endowment in addition to a $150,000 gift to the same fund, named after the Cohens’ son who “died very early in his adult life but lived long enough to share our affection of nursing,” Steve Cohen says. The scholarship specifically supports entry-intonursing students with a preference to those employed by a Baltimore MedStar hospital prior to graduation, and for its part, UMSON agrees to provide scholarship recipients with clinical rotation opportunities at MedStar hospitals.
“I’ve always believed from direct observation that nurses who are trained at a site tend to stay there because they know the people, they know the system,” Steve Cohen explains. “And like most such things, if there isn’t an active champion to make sure it’s working, it probably won’t work.” The Cohens, he says, are ready to serve as those champions.
— G.S.
*deceased NURSING FOR/UM • SPRING 2024 • 39
Sandy and Steve Cohen
Minimum distribution. Maximum impact. Support UMSON and save on taxes with a charitable IRA rollover.

If you are age 70 1/2 or older, you have a unique giving opportunity to support UMSON.
A qualified charitable distribution (QCD), also called a charitable IRA rollover, allows you to make a tax-free transfer of up to $100,000 a year from an individual retirement account.
A QCD gift will benefit you by:
• reducing your taxable income
• counting toward your required minimum distribution
• providing a tax-efficient way to make a difference at UMSON!
PLEASE NOTE: All gifts to UMSON should be made payable to the University of Maryland Baltimore Foundation, Inc. for the benefit of the School of Nursing.
IRA QUALIFIED CHARITABLE DISTRIBUTION
For more information about QCDs, bequests, gifts that pay income for life, and other strategic ways to support the School of Nursing, please visit umaryland.edu/planned-giving.
If you have any questions about giving to UMSON, please contact Stacey Conrad, associate dean for development and alumni relations, at sconrad@umaryland.edu or 410-706-7640.
“Several years ago, I began rolling over part of the annual required minimum distribution (RMD) from my deferred retirement account to my endowed scholarship at the School of Nursing. The process has been incredibly easy! The RMD dollars are tax exempt, and the donations have kept my taxable income in a comfortable bracket. I would encourage others to consider this same strategy; it’s a win-win in many ways!”
COURTNEY
THOMAS, BSN ’66

40 • NURSING FOR/UM • SPRING 2024
TOP: AL GENERAL; RIGHT: COURTESY OF BRIGITTE BARD BACK COVER: MATTHEW D’AGOSTINO/UMB
Donor Your Gift IRA Request a qualified charitable distribution Charitable distribution
70 1/2 or older IRA Custodian Your QCD will have an immediate impact on our mission.
Age
Close-Up
DOGGONE IT!
Warrior Canine Connection’s (WCC) Heath, a yellow Labrador, was named after a World War II sailor, U.S. Navy Chief Petty Officer Charles Thomas Heath. The dog bounded into Brigitte Bard’s life when he was 9 weeks old; she had volunteered to serve as a Puppy Parent, raising and training Heath for an eventual life

Read more of Heath’s story and see more puppy pictures by scanning the QR code.

with a veteran. WCC is a nonprofit organization that trains service dogs for wounded veterans. Bard, BA, (seated at right) assistant director of student services, made bringing Heath to UMSON’s building at the Universities at Shady Grove (USG) part of his training, so he could be socialized through interactions with students and employees.
“Raising and training Heath has been the most rewarding volunteer work I have ever done,” Bard says. “It changed my life.” Heath, however, was deemed not to have the specific characteristics necessary to serve a vet, and WCC determined he would be a better fit for an active military family. Enter Jen Dalton, PhD, RN, CNE, CHSE, (seated at
left) assistant professor at USG, whose husband is in the U.S. Navy, making them eligible to adopt him. And they did, officially, on Dec. 8.
“Heath keeps us on our toes and really adds laughter and snuggles to our daily routine,” Dalton says.
“I’m forever grateful to Brigitte for bringing him into our lives at USG.”
— G.S.
“�The financial help you have provided is not for me alone, but also for all the lives that I will impact as a nurse and the contributions I will make to the nursing profession.”
Abena Donkor, Bachelor of Science in Nursing Student

Abena received the David Vlahov Endowed Scholarship to support undergraduate students, created by David Vlahov, MS ’80, BSN ’77, a member of UMSON’s Board of Visitors and one of our 25 inaugural Visionary Pioneers. MAKE YOUR GIFT TODAY at nursing.umaryland.edu/give
Nonprofit Org U.S. Postage PAID Baltimore, MD Permit #7012
655 W. Lombard St. Baltimore,
Office of Communications
MD 21201 nursing.umaryland.edu






 Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN
Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN