Driving Impact For Maryland Hospitals
“AS CHALLENGES IN HEALTH CARE CONTINUE TO EVOLVE, SO TOO MUST OUR STRATEGIES AND OUR SUPPORT.”
- Melony G. Griffith
“AS CHALLENGES IN HEALTH CARE CONTINUE TO EVOLVE, SO TOO MUST OUR STRATEGIES AND OUR SUPPORT.”
- Melony G. Griffith

“This year, our shared work has taken on new urgency.”
Maryland hospitals and health systems are more than places of healing—they are pillars of strength, economic engines, and the heart of our communities. At the Maryland Hospital Association, we are proud to stand with you—our members—as champions, collaborators, and trusted advocates for your organizations and our shared mission to support the health of every Marylander.
This year, our shared work has taken on new urgency. As challenges in health care continue to evolve, so too must our strategies and our support.
Since joining MHA as President & CEO, I’ve traveled across our state to visit hospitals and hear directly from the people who make healing possible. From the emergency department to the boardroom, I’ve seen the dedication, innovation, and resilience that define our field. These visits reaffirm what we all know to be true: Healthy hospitals are essential to healthy and thriving communities.
In this 2025 Annual Report, you’ll find a clear story: MHA delivers.
We listened to you, and we acted. On your behalf, we:
• Advanced priority legislation to reduce regulatory burden and expand access to care
• Secured significant funding to strengthen hospital finances and support workforce needs
• Elevated solutions to shape the future of Maryland’s Model
• Promoted the power and potential of Maryland hospitals through statewide and national advocacy
Guided by our new strategic plan, we focused on what matters most: advancing sound policies, strengthening financial sustainability, amplifying your voice, and building an Association that is prepared to respond to your immediate and future needs.
In this 2025 Annual Report, we detail how MHA elevated data-informed solutions on behalf of the field. We grew our partnerships and strengthened relationships to build champions across the state. And we worked to ensure every hospital has the tools and resources to thrive.
We accomplished all of this together—because your engagement and leadership drive our success.
I look forward to continuing this work with each of you.
Melony G. Griffith President & CEO Maryland Hospital Association
This year, MHA’s Board of Trustees adopted a new strategic plan to guide the Association’s work on behalf of our members. This plan isn’t just a vision—it’s a commitment to our members that we will remain focused, agile, and mission-driven.
The multi-year plan is built around three core strategic priorities—each designed to strengthen hospitals, empower caregivers, and advance health care in Maryland. These priorities will serve as the bedrock of our work—laying the foundation for deeper impact, stronger support, and healthier communities across our state.
1
Proactive Advocacy on Member Issues
Actively address and advocate for solutions to member-identified issues, enhancing policy impact and member support.
2
Broadening MHA Relationships
Strengthen and expand collaborations with key stakeholders to amplify MHA’s influence in health care advocacy.
“It’s a commitment to our members that we will remain focused, agile, and mission-driven. “
- Melony G. Griffith
3
Advocacy for Financially Supportive Fiscal Policies
Champion fiscal policies that bolster the financial health of hospitals, helping ensure sustainability and improved healthcare delivery.

MHA’s advocacy is grounded in listening to our members and turning those insights into action. Every policy position we take, every partnership we build, and every message we deliver is shaped by your needs, your challenges, and your goals.
This year, we fought for and secured meaningful gains that strengthened Maryland hospitals and protected the patients and communities they serve.
In Annapolis, MHA worked alongside hospital leaders to advance a forward-looking policy agenda. Our government affairs and policy team advocated for legislation that supports hospital operations, strengthens access to care, and invests in our hospitals. We also took a strong stand against bills that would have constrained hospital operations or imposed unfunded mandates.

IMPROVED PEDIATRIC CARE COORDINATION
Passed legislation to reduce pediatric overstays
Secured $3M to expand treatment options and placement support
HELD PAYERS ACCOUNTABLE
Created a state work group on adverse decisions
Strengthened reporting and oversight of payer denials and AI use
Defeated hospital staffing committee mandate
Blocked unworkable reimbursement requirements
PROTECTED OPERATIONS & SAFETY
Secured exemption from security guard licensing regulations
Preserved hospitals’ use of critical energy infrastructure by exempting facilities from Building Energy Performance Standards
EXPANDED ACCESS THROUGH TELEHEALTH
Made audio-only telehealth permanent with payment parity
PRESERVED MEDICAL LIABILITY PROTECTIONS
Defeated attempts to raise caps on noneconomic damages

STRENGTHENED THE HEALTH CARE WORKFORCE
Protected hospital input on midwife scope of practice
Delayed CNA/GNA consolidation for better hospital readiness
Removed duplicative English proficiency barriers for licensed professionals
Improved emergency transfer protocols with midwives
Shifted proposed cybersecurity mandates into a collaborative work group
Expanded access to forensic telehealth using state grant funds
Maryland hospitals secured $20 million in funding through the state budget
MHA’s capital bond program included $22.6 million for 22 hospital projects
In the past several years, your hospitals have been under incredible financial strain at a time when you are returning record savings to Medicare through the Total Cost of Care Model. In response, MHA helped the Health Services Cost Review Commission (HSCRC), state and federal lawmakers, and others to understand hospital sustainability is the foundation of access and innovation.
This year, MHA continued to support Maryland’s path forward by advocating for critical adjustments to the hospital payment system and successfully pushed for increased resources to help hospitals weather volatility in inflation and workforce shortages.
As Maryland prepares for a new chapter in its unique hospital payment system, MHA ensured the voices of hospitals were heard at every step.
For fiscal year 2025, MHA secured a historic 4.53% per capita annual update to hospital global budgets—one of the most significant increases in recent history.
Our advocacy also ensured that Maryland hospitals were not the sole funding source for new population health and Medicaid initiatives, and we continued to urge HSCRC to account for inflation, labor pressures, and deferred capital needs.
· Secured $25 million in transition funding
· Secured $50 million in permanent rate support for workforce and inflation
· Secured $150 million in rate support for underfunded respiratory-related volumes and RSV immunizations
· Postponed and improved HSCRC’s hospital financial condition analysis to reflect today’s fiscal realities
MHA ensured the voices of hospitals were heard at every step.
MHA fought for—and secured—funding increases and reforms to ensure hospitals can continue to invest in safe, high-quality care while navigating economic headwinds:

Capital Funding Policy Improvements: MHA supported HSCRC policy changes to ensure inflation and project-specific factors are considered in capital funding reviews, helping hospitals invest in critical infrastructure

CDS-A Drug Funding Policy: We successfully advocated for revisions to the CDS-A drug funding methodology to better reflect real-world acquisition costs for high-cost drugs

Specialty Hospital Payment Updates: MHA secured a 4.24% payment update for psychiatric hospitals and Mt. Washington Pediatric Hospital, recognizing their unique cost structures and financial needs

$51 million in additional relief funding was obtained to address specific cost pressures experienced by hospital members
As commercial payer denials surged, MHA spotlighted their impact on patient care and hospital operations. We:
· Championed the passage of SB 776/HB 995 to launch a work group on adverse decisions
· Supported the legislative request to MIA to establish a standing advisory commission on insurance transparency and oversight
· Fought to ensure premium increases aligned with hospital rate updates

Quality-Based Reimbursement (QBR): We successfully pushed HSCRC to lower the rate year 2025 reward threshold from 41% to 32%, reducing hospital penalties and returning $42 million to the field.

Electronic Clinical Quality Measures (eCQM): In response to MHA’s concerns, HSCRC aligned its requirements with federal timelines and created a $150,000 rate incentive for hospitals meeting the expedited state submission schedule—while avoiding penalties for those that comply with the national CMS timeline.

Emergency Department (ED) Best Practices: MHA secured timeline flexibility for implementing new ED quality requirements and successfully advocated for a phased approach that acknowledges workforce challenges and external capacity constraints.
HSCRC committed to working with the ED Wait Time Reduction Commission to address systemic throughput barriers.


MHA pushed for refinements to the Medicare Performance Adjustment (MPA) and Care Transformation Initiative (CTI) scoring methodologies to reduce unfair penalties and account for non-claims-based payments—ensuring hospitals aren’t penalized for delivering care in innovative, value-based ways.
MHA extended its reach by building bridges with state agencies, lawmakers, federal officials, community organizations, and national hospital groups. These partnerships helped drive solutions for everything from maternal health to behavioral health to long-term payment reform.
MHA strengthened engagement with HSCRC, the Maryland Department of Health, legislative leaders, and the federal delegation to drive solutions, including:
· Briefing the entire Maryland Congressional delegation
· Partnering with Howard County on a successful discharge hospitality suite pilot
· Collaborating with hospital government affairs teams on stakeholder visits and legislation


We met with nearly every hospital leader this year through MHA Board and G8 meetings, member retreats, and targeted roundtables. We also:
· Hosted exclusive member briefings with Attorney General Anthony Brown, Comptroller Brooke Lierman, and Jon Kromm, chair of the Health Services Cost Review Commission
· Brought together all hospital and health system Presidents and CEOs to provide updates and receive feedback
In November 2024, MHA was pleased to host our first open house at our Elkridge office. The event brought together more than 100 members who networked, learned about MHA’s work, and engaged with special guests, including eight legislators from districts statewide.

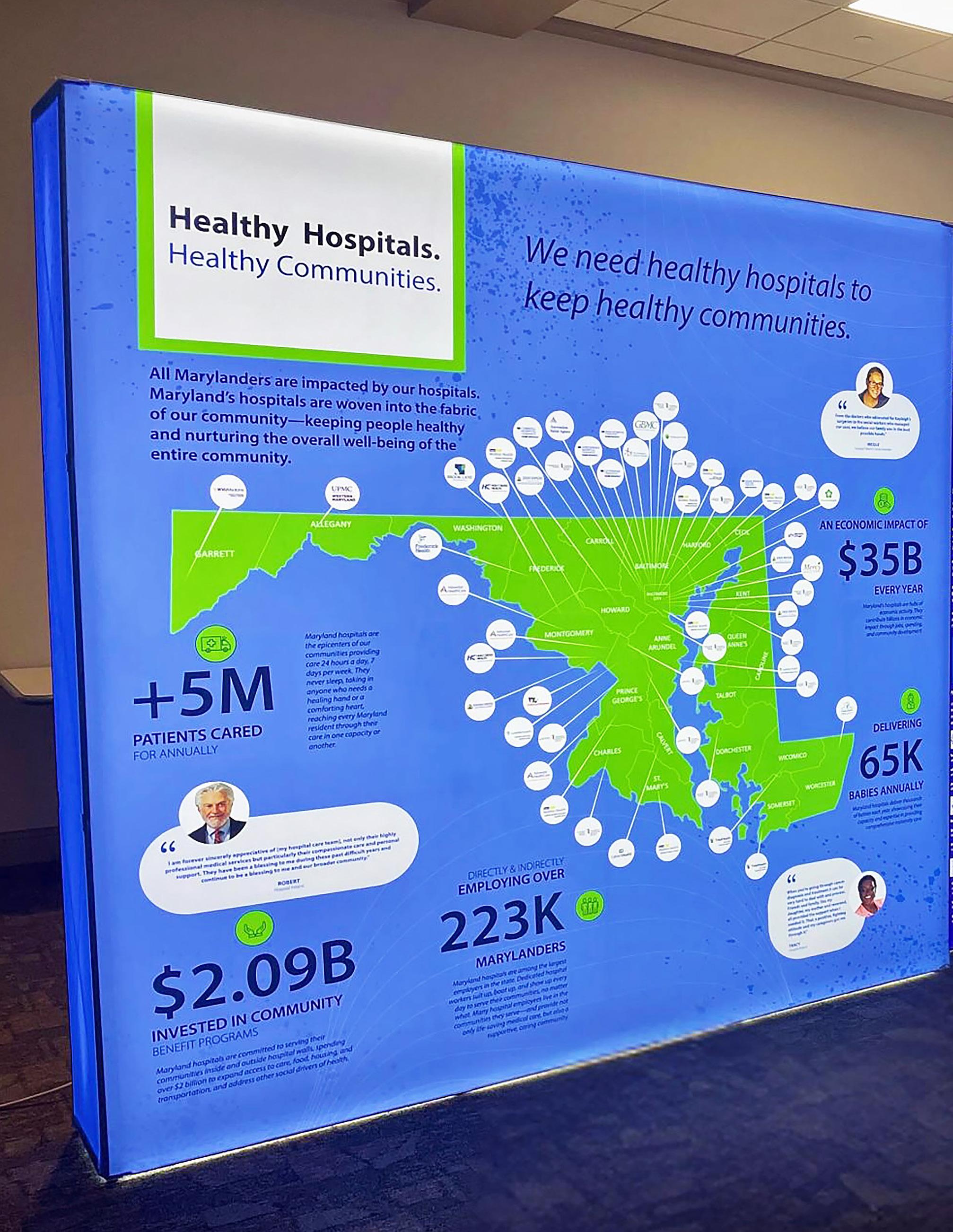
MHA’s Healthy Hospitals. Healthy Communities. campaign showcases the vital role hospitals play in our communities. Through videos, events, and stories from across the state, the campaign highlights that strong hospitals are essential to strong communities.
· 20-foot, by 10-foot campaign display
· 10 stops across the state
· 57 campaign videos
MHA also used its social media platforms to showcase Maryland hospitals and their incredible employees, resulting in:
· 14,000 YouTube views
· 9,900 post impressions on LinkedIn and 3,000 user impressions on Instagram
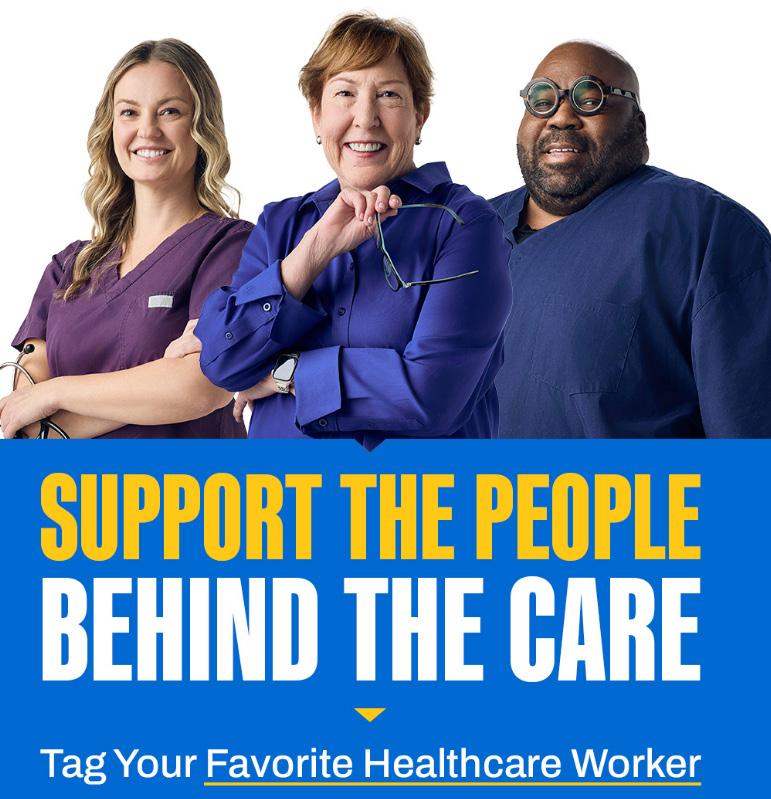
Health care is only as strong as its people. As workforce challenges persist across the country, MHA has worked aggressively to bolster recruitment, support retention, and elevate the voices of frontline caregivers.
Our online job board connects talented professionals to opportunities at Maryland hospitals. This year, it drew thousands of job seekers and helped hospitals find the right candidates faster.
This statewide campaign reminded Marylanders—and their elected leaders—that caregivers need care, too. Through stories, testimonials, ads on TV, bus, and billboards in Maryland, and social media, we reinforced the value of the health workforce and advocated for policies that support them.
Maryland’s
Workforce challenges remain one of the most pressing issues facing Maryland hospitals. MHA tackled these challenges headon—driving meaningful policy change and building long-term solutions. These achievements reflect key goals outlined in MHA’s 2022 State of Maryland’s Health Care Workforce Report—goals we committed to and successfully advanced through focused advocacy, collaboration, and innovation.
· Expand Maryland’s Workforce Pipeline
· Retain the Health Care Workforce
· Remove Barriers to Health Care Education
· Leverage Talent with New Care Models
Your support for the MHA Political Action Committee fuels our efforts to educate lawmakers, elevate hospital priorities, and elect health care champions.
Individual Contributors representing Organizations
Totaling in 2024 The year ahead offers critical opportunities— and we are ready. 206 41 $91,427.59





As we look ahead to fiscal year 2026, we remain committed to our mission and inspired by what’s possible. The year ahead offers critical opportunities—and we are ready.
MHA is focused on advancing policies that support hospitals’ financial sustainability, reducing administrative burden, ensuring strong payment updates, and supporting the workforce. Our strategic priorities and your continued partnership will ensure Maryland’s hospitals remain strong, resilient, and ready to lead.
MHA’s strategic analytics team ensures our advocacy is backed by data that resonates. From workforce trends to cost-of-care savings, we help turn complex data into actionable insight.
Monitored workforce data covering 80,000+ FTEs
Notable reductions in both vacancy (13.8% à 9.7%) and turnover (31.8% à 21.5%)
Achieved $509 million in Medicare savings in 2023
Projected to exceed $600 million in savings in 2024

Workplace Violence Survey
Captured 1,800+ incident-level reports from hospitals
Revealed over 1,200 lost workdays due to violent incidents
Maternal Morbidity Analysis
Analyzed over 360,000 birthing records to identify patterns and disparities in outcomes
Your Association is only as strong as the members who lead, advise, and participate in our work. Across more than a dozen councils, task forces, and advisory groups, MHA members dedicated their time, insights, and voices to shape the field’s advocacy and policy priorities.
Thank you to members who served on the following member-led groups during fiscal year 2025.
Thomas Kleinhanzl, Chair
President & CEO
Frederick Health
Victoria Bayless, Vice Chair
Chief Executive Officer
Luminis Health
Savas Karas, Treasurer/Secretary
Board Member, MedStar Harbor Hospital; Chief Technology Officer/Chief Transformation Officer
CAPREIT, Inc.
Bradley Chambers, Chair, Governance Committee
Senior Vice President & COO
Baltimore Region MedStar Health
David Maine, M.D., Chair, Council on Clinical & Quality Issues
President & CEO
Mercy Medical Center
Kevin Sowers, Chair, Council on Legislative & Regulatory Policy
President
Johns Hopkins Health System
Mohan Suntha, M.D., Chair, Council on Financial Policy
President & CEO
University of Maryland Medical System
Harsh Trivedi, M.D., Chair, Compensation Committee
President & CEO
Sheppard Pratt
Alexander Austin
Chief Executive Officer
Prince George’s Chamber of Commerce
Jeremy Bradford
President & CEO
CalvertHealth System, Inc.
Diana Léon Brown
Chief of Staff, Government & External Affairs
Maryland Aviation Administration
Christina Fitts
Board Member, GBMC HealthCare; CEO, AJ Fitts Unlimited, LLC
Steven Leonard, Ph.D. President & CEO
TidalHealth
Michele Martz
President UPMC Western Maryland
Neil Meltzer
President & CEO LifeBridge Health
Donald Owrey
President & CEO
Atlantic General Hospital
Elizabeth Wise
President & CEO
University of Maryland Upper Chesapeake Health System
COUNCIL ON CLINICAL & QUALITY ISSUES
David Maine, M.D., Chair
President & Chief Executive Officer
Mercy Medical System
Mohammed Shafeeq Ahmed, M.D. President
Johns Hopkins Howard County Medical Center
Laural Brinkley Chief Nursing Officer CalvertHealth Medical Center
John Chessare, M.D.
President & Chief Executive Officer
GBMC HealthCare
Bonita Conner
Director, Quality and Infection Prevention
Atlantic General Hospital
Kathryn Fiddler, DNP
Vice President, Population Health
TidalHealth
Angela Green
Vice President, Safety and Quality
Johns Hopkins Health System
Janis Green, MD
Interim Chief Clinical Officer
Holy Cross Health
Maryland Region of Trinity Health
Heather Kirby
Vice President, Integrated Care Delivery, and Chief Population Health Officer Frederick Health
David Lang, M.D.
Chief, Office of Patient Safety & Clinical Quality
NIH Clinical Center
Ralph Lebron, M.D.
Medical Director, Quality & Patient Safety
Mercy Medical Center
Stuart Levine, M.D.
President, MedStar Franklin Square Medical Center, and Senior Vice President, MedStar Health
Michele Martz
President UPMC Western Maryland
Patsy McNeil, MD
Executive Vice President & System Chief Medical Officer Adventist HealthCare
Stephen Michaels, M.D.
President, MedStar Southern Maryland Hospital Center, and Senior Vice President, MedStar Health
Jonathan Patrick, M.D.
Senior Director, Hospital Quality Performance Co-Chair, MedStar Health
Matthew Poffenroth, M.D.
Senior Vice President & Chief Physician Executive LifeBridge Health
Michael Anne Preas
Vice President, Quality Management University of Maryland Medical Center
Nitza Santiago
Assistant Vice President, Quality & Patient Safety Sinai Hospital of Baltimore
Mitchell Schwartz, M.D.
Chief Physician Executive, Luminis Health, and President, Luminis Health Clinical Enterprise
Rahul Shah, M.D.
Senior Vice President, Hospital-Based Specialties Children’s National Health System
Neel Vibhakar, M.D.
Senior Vice President & Chief Medical Officer University of Maryland Baltimore Washington Medical Center
Julie Vitko
Senior Director, Quality & Patient Safety UPMC Western Maryland
Mohan Suntha, M.D., Chair
President & Chief Executive Officer University of Maryland Medical System
Ed Beranek
Vice President, Revenue Management and Reimbursement
The Johns Hopkins Hospital & Health System
Amy Boothe
Vice President, Finance and Operations Garrett Regional Medical Center
Joshua A. Campbell, MBA, FHFMA
Vice President, Finance & Reimbursement GBMC HealthCare
Alicia Cunningham
Senior Vice President, Corporate Finance and Revenue Advisory Services University of Maryland Medical System
Justin C. Deibel
Executive Vice President & Chief Financial Officer Mercy Medical Center
Katie Eckert, CPA
Senior Vice President, Strategic Operations Adventist HealthCare
Stephanie Gary
Vice President, Finance and Chief Financial Officer TidalHealth
Carolyn Heithaus
Vice President, Finance & Chief Financial Officer
CalvertHealth
Hannah Jacobs
Senior Vice President & Chief Financial Officer
Frederick Health
David Krajewski
Executive Vice President & Chief Financial Officer
LifeBridge Health
Mitch Lomax
Chief Financial Officer
Ascension Saint Agnes
Susan K. Nelson
Executive Vice President and Chief Financial Officer MedStar Health
Cheryl Nottingham
Vice President, Finance
Atlantic General Hospital
Amber Ruble
Chief Financial Officer
UPMC Western Maryland
Kelly Savoca
Vice President and Chief Financial Officer
Sheppard Pratt
Thomas J. Senker
President, MedStar Good Samaritan Hospital & MedStar Union Memorial Hospital
Mario Voli
Vice President, Finance
ChristianaCare, Union Hospital
COUNCIL ON LEGISLATIVE & REGULATORY POLICY
Kevin Sowers, Chair
President
Johns Hopkins Health System
Elizabeth Wise
President & CEO
University of Maryland Upper Chesapeake Health System
Timothy Adelman
General Counsel & Chief Legal Officer
Luminis Health
Craig Carmichael
President & Chief Operating Officer, Northwest Hospital;
Senior Vice President, LifeBridge Health
Cheryl Cioffi
Senior Vice President & Chief Operating Officer
Frederick Health
Daniel Cochran
President
Adventist HealthCare Shady Grove Medical Center
Jill Donaldson
President, MedStar Harbor Hospital
Senior Vice President, MedStar Health
Marjorie Fridkin, M.D.
Chief Medical Officer & Vice President of Medical Affairs
Garrett Regional Medical Center
Jeffrey Grossi
Chief of Government Relations
Sheppard Pratt
Christopher Hall
Vice President Strategy/Chief Business Officer TidalHealth
Beau Higginbotham
President & CEO
Ascension Saint Agnes
Kasia Sweeney
Vice President of Strategy & Business Development
CalvertHealth
Kristin Jones Bryce
Senior Vice President & Chief External Affairs Officer
University of Maryland Medical System
Kathleen McCollum
President & CEO
UM Baltimore Washington Medical Center
Mimi Novello, M.D.
President & Chief Medical Officer
MedStar St. Mary’s Hospital
Ryan O’Doherty
Senior Vice President, External Affairs
Mercy Medical Center
Bradley Schlaggar, M.D., Ph.D.
President & CEO
Kennedy Krieger Institute
Maria Harris Tildon
Vice President, State & Local Affairs
The Johns Hopkins University & Medicine
Meredith Tweedie
Vice President, Government Affairs & Policy, and Senior Counsel
ChristianaCare, Union Hospital
Jason Weiner
Senior Vice President, General Counsel
LifeBridge Health
Bradley Chambers, Chair
Senior Vice President & Chief Operating Officer
MedStar Health
Jeremy Bradford President & CEO
CalvertHealth
Kristy Daphnis
Chief Operating Officer
Maryland Hospital Association
Christina Fitts
Board Member
GBMC HealthCare
Jessica Melton
Vice President, Strategic Initiatives Suburban Hospital
Elizabeth Wise
President & CEO
University of Maryland Upper Chesapeake Health System
MHA
Savas Karas
Board Member, MedStar Harbor Hospital Chief Technology Officer/Chief Transformation Officer CAPREIT, Inc.
Alexander Austin
Chief Executive Officer
Prince George’s Chamber of Commerce
Steven Leonard, Ph.D.
President & CEO
TidalHealth
Michele Martz
President & CEO
UPMC Western Maryland
Don Owrey
President & CEO
Atlantic General Hospital
MHA POLITICAL ACTION COMMITTEE
Victoria Bayless, Chair CEO
Luminis Health
John Chessare, M.D.
President & CEO
GBMC HealthCare
Garrett Hoover
President & COO
Carroll Hospital
Stuart Levine
President
MedStar Franklin Square Medical Center
MHA COMPENSATION COMMITTEE
Harsh Trivedi, M.D., Chair
President & CEO
Sheppard Pratt
Thomas Kleinhanzl
President & CEO
Frederick Health
Neil Meltzer
President & CEO
LifeBridge Health
Eunmee Shim
President
Adventist HealthCare Fort Washington Medical Center
We also thank the many members who serve on our work groups, task forces, and other groups:
Birth Outcomes Accountability Work Group
Health Equity Advisory Committee
Health Care Payment Work Group
Hospital Quality Operations Work Group
Labor & Employment Work Group
Legislative Strategy Group
Medicare Performance Adjustment (MPA) Work Group
Task Force on Maryland’s Future Health Workforce
Technical Work Group
Adventist HealthCare
Adventist HealthCare Fort Washington Medical Center
Adventist HealthCare Rehabilitation
Adventist HealthCare Shady Grove Medical Center
Adventist HealthCare White Oak Medical Center
Ascension Saint Agnes
Atlantic General Hospital
Brook Lane
CalvertHealth
Carroll Hospital
Children’s National Hospital
ChristianaCare, Union Hospital
Encompass Health Rehabilitation Hospital of Bowie
Encompass Health Rehabilitation Hospital of Salisbury
Frederick Health
Garrett Regional Medical Center
GBMC HealthCare
Grace Medical Center
Holy Cross Germantown Hospital
Holy Cross Health, A member of Trinity Health
Holy Cross Hospital
Johns Hopkins Bayview Medical Center
Johns Hopkins Health System
Johns Hopkins Howard County Medical Center
Kennedy Krieger Institute
Levindale Hospital
LifeBridge Health
Luminis Health
Luminis Health Anne Arundel Medical Center
Luminis Health Doctors Community Medical Center
MedStar Franklin Square Medical Center
MedStar Health
MedStar Good Samaritan Hospital
MedStar Harbor Hospital
MedStar Montgomery Medical Center
MedStar Southern Maryland Medical Center
MedStar St. Mary’s Hospital
MedStar Union Memorial Hospital
Mercy Medical Center
Mt. Washington Pediatric Hospital
NIH Clinical Center
Northwest Hospital
Sheppard Pratt
Sinai Hospital of Baltimore
Suburban Hospital
The Johns Hopkins Hospital
TidalHealth McCready Pavilion
TidalHealth Peninsula Regional
University of Maryland Baltimore Washington Medical Center
University of Maryland Bowie Health Center
University of Maryland Capital Region Medical Center
University of Maryland Charles Regional Medical Center
University of Maryland Laurel Medical Center
University of Maryland Maryland Capital Region Health
University of Maryland Medical Center
University of Maryland Medical Center Midtown Campus
University of Maryland Medical System
University of Maryland Rehabilitation & Orthopaedic Institute
University of Maryland Shore Medical Center at Cambridge
University of Maryland Shore Medical Center at Chestertown
University of Maryland Shore Medical Center at Easton
University of Maryland St. Joseph Medical Center
University of Maryland Upper Chesapeake Health
UPMC Western Maryland