

football medicine & performance
In this issue
From Medial Hamstring Rupture to Return in Sub 50 days; Is Surgical Repair a Waste of Time?
Adam Paxton
‘Setting the Benchmark’ Part 5: The Contextual and Tactical Factors that Influenced the Physical Match Demands at the FIFA Men’s & Women’s World Cups
Dr Paul S. Bradley
Prescribing Trends & Practices in Professional Football
Dr Richard Porter, Dr Rishi Dhand, Dr Adam Drummond
Hamstring Injuries: What Role does the Lumbar Spine & Pelvis Play? Part 2
Nick Metcalfe
Local Cryotherapy in Elite Football: The Cold-Hearted Truth
Dr Olivia Greenhalgh
A Return to Performance Pathway – from the Onset of Injury Back to Performance Andrew Mitchell, Mark Palmer, Mo Gimpel
Exertional Heat Illness: Should this be a Hot Topic in Football Medicine?
Dr Dan Fitzpatrick
Performance, Injury Reduction & Avoiding Pushing Youth Athletes too far via Pre-season Adolescent Screening
Craig Hagan
Sacroiliitis: Finding a Pathway for a Rare Inflammatory Back Condition - A Comparative Case-study Analysis
Liam Donovan
Enigma Legal provides legal services and advice to managers, coaches and professionals working within the sports industry, its unique structure utilising a panel of expert barristers all with extensive experience of the sports industry, most notably their work with the League Managers Association.
Enigma Legal lawyers are tried and trusted to work in a flexible, agile and responsive way, demonstrating their understanding of the unique demands of the sports industry. A creative and pragmatic approach will ensure that Enigma Legal offers real value to the FMPA Membership.

www.enigmalegal.com
admin@fmpa.co.uk

CEO MESSAGE
Finding quotes that celebrate the power of education is a breeze, while discovering ones that criticise it seems nigh on impossible. Education truly shines as a wholly positive force for all.
Consider this statement:
“Continuous learning is the minimum requirement for success in any field.”
In today’s fast-paced world, this is even more important, especially with online learning and internet-based programs becoming the go-to for Continuing Professional Development (CPD).
At the FMPA, we know how crucial CPD is for our members, and we’re delighted to offer a wide array of support, including:
• Our flagship publication, showcasing high quality articles that resonate with members, whether they’re interested in academic studies or hands-on practical tips.
• A monthly podcast that’s gaining traction, covering a diversity of topics in our sector, and engaging 3000 interactions each month.
• Complimentary access for members to the British Journal of Sports Medicine.
• A monthly CPD overview that builds a portfolio of evidence for our members—perfect for those who need to demonstrate CPD to their professional bodies or employers.
• The FMPA Diploma: ‘Preparation for Working in Professional Football’—an essential credential for new graduates and junior staff.
• Excitingly, we are looking to introduce a series of Regional Network Events in 2025 which will feature a high quality line-up of speakers and host breakout sessions for medicine and performance practitioners alongside our traditional trade exhibitors.
Moreover, we’re thrilled to announce our partnerships with esteemed organizations like the Society of Sports Therapists (SST), British Association of Sports and Exercise Science (BASES), British Association of Sports Rehabilitators and Therapists (BASRaT), and the International Universities Strength and Conditioning Association (IUSCA), with other discussions currently underway. Through these partnerships, we will prioritise sharing information about educational opportunities, CPD, courses, conferences, workshops, and events, all designed to enhance the offerings of each organization and promote collaboration for the benefit of all professionals involved.
Education is important for all, and continued learning should be the backbone of any practitioners pathway to a healthy and fruitful career. FMPA Members already possess a significant advantage!
Chief Executive Officer
Football Medicine & Performance Association
ONLINE COURSE MPA DIPLOMA
PREPARATION FOR WORK IN PROFESSIONAL FOOTBALL
✓ Health and safety
✓ Safeguarding
✓ Equality/Diversity
✓ Mental Health/wellbeing
✓ Confidentiality
✓ Record keeping
✓ Media TV
✓ Social Media
✓ Expectations of behaviour/general professionalism
✓ Integration within the MDT environment
✓ Insight into the working week
✓ Awareness of un-clinical skills
✓ From `Theory to Practice’
✓ How the science sits in the working environment
✓ What an employer is looking for – Employability, CPD, Reflective Practice, CV
✓ Portfolio design
Includes FREE FMPA membership access for 6 months:
• FMPA resources
• FMPA publication
• Free access to BJSM
• FMPA podcasts
• FMPA education
• Latest Jobs

• Sports Scientists
• Physiotherapists
• Doctors
• Analysts
• Sports Therapists
• S & C Coaches
• Fitness Coaches
• Soft Tissue Therapists
• Sports Rehabilitators
• Sports Psychologists
• Nutritionists
• Podiatrists
Contact us at:
admin@fmpa.co.uk 0333 4567897 www.fmpa.co.uk/courses/mpa-diploma

FROM THE EDITORS
The first edition of 2025 brings together world class professionals working in elite football. As we are halfway through the 2024/2025 season various challenges are imposed on the medical and performance staff.
Andrew Mitchell from RB Leipzig and colleagues, Mark Palmer and Mo Gimpel discuss the Return to Play pathway as well as recommendations for the multidisciplinary team on how to recondition an injured footballer back to performance. On the other hand, Adam Paxton, Head of Medical at West Ham United Football Club discusses semimembranosus rupture return to play.
Craig Hagan, Newcastle Jets A-League Sports Trainer touches upon the need for early athlete screening and the impact it has on performance, development and how it can be a gateway to developing elite habits. First team physiotherapist at Cardiff City FC, Liam Donovan explores the route for two separate incidences of sacroiliitis in professional footballers at the same club.
As the physical demands are increasing in the beautiful game, Paul Bradley explores the contextual and tactical factors that influenced the physical match demands at the FIFA Men’s and Women’s World Cups. The rise in demands poses a greater emphasis on medical departments to deal with an increased workload related to injuries. For this reason, Richard Porter, Adam Drummond and Rishi Dhand discuss prescribing trends and practices in professional football.
Dan Fitzpatrick, an academy doctor at West Ham United and Member of the UK Heat Illness Advisory Group provides an overview on exertional heat illness and its impact on Football Medicine. This follows on from recent work in the prehospital care space.
Recovery modalities are a consistent hot topic in performance medicine. Olivia Greenhalgh explores the role of cryotherapy in elite football.
Nick Metcalfe continues from his article in the previous edition on hamstring injuries by discussing the importance of Gluteus maximus strength and activation.
We hope you find this edition useful and applicable to your everyday practice. We would also like to take this opportunity to wish you all the best for the new year.



Dr. Fadi Hassan Editor, FMP Magazine
Dr. Andrew Shafik Editor, FMP Magazine
Dr. Daniela Mifsud Editor, FMP Magazine
ASSOCIATE EDITORS

Ian Horsley Lead Physiotherapist

Dr. Jon Power Director of Sport & Exercise Medicine
REVIEWERS

Matthew Brown Academy Sports Scientist

Lisa Edwards Sports Therapist

Dr. Danyaal Khan Academy Doctor

Mike Brown Head of Physical Performance

Jake Heath Elite Sports Specialist Podiatrist

Dr. Dáire Rooney Doctor

Dr. Manroy Sahni Medical Doctor

Dr. Andrew Butterworth Senior Lecturer

Frankie Hunter Lead Sports Scientist

Dr. Jose Padilla MD Sports Medicine Specialist

Dr. Eleanor Trezise Doctor

Dr. Avinash Chandran Director

Callum Innes Medical Doctor

Kevin Paxton Strength & Conditioning Coach
Medicine And Performance Association t/a Football Medicine & Performance Association Office 5, Bank House, King St, Clitheroe, Lancs, BB7 2EL T: 0333 4567 897 E: info@fmpa.co.uk W: www.fmpa.co.uk
FMPA_Official Officialfmpa fmpa_official LinkedIn: Football Medicine & Performance Association
FMPA_Register FMPARegister fmpa_register
Chief Executive Officer Eamonn Salmon eamonn.salmon@fmpa.co.uk
Commercial Manager Angela Walton angela.walton@fmpa.co.uk
Design Oporto Sports www.oportosports.com
Photography Alamy, FMPA, Unsplash
Cover Image
Manchester United’s Harry Maguire is helped from the field after suffering an injury during the Premier League match at Villa Park, Birmingham, Sunday October 6, 2024
Photo: Alamy
© Football Medicine & Performance Association. All rights reserved.
The views and opinions of contributors expressed in Football Medicine & Performance are their own and not necessarily of the FMPA Members, FMPA employees or of the association. No part of this publication may be reproduced or transmitted in any form or by any means, or stored in a retrieval system without prior permission except as permitted under the Copyright Designs Patents Act 1988. Application for permission for use of copyright material shall be made to FMPA. For permissions contact admin@fmpa.co.uk






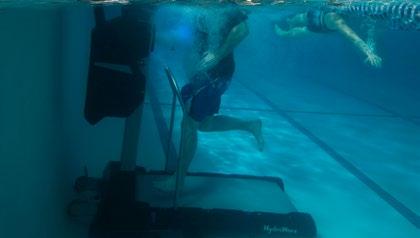


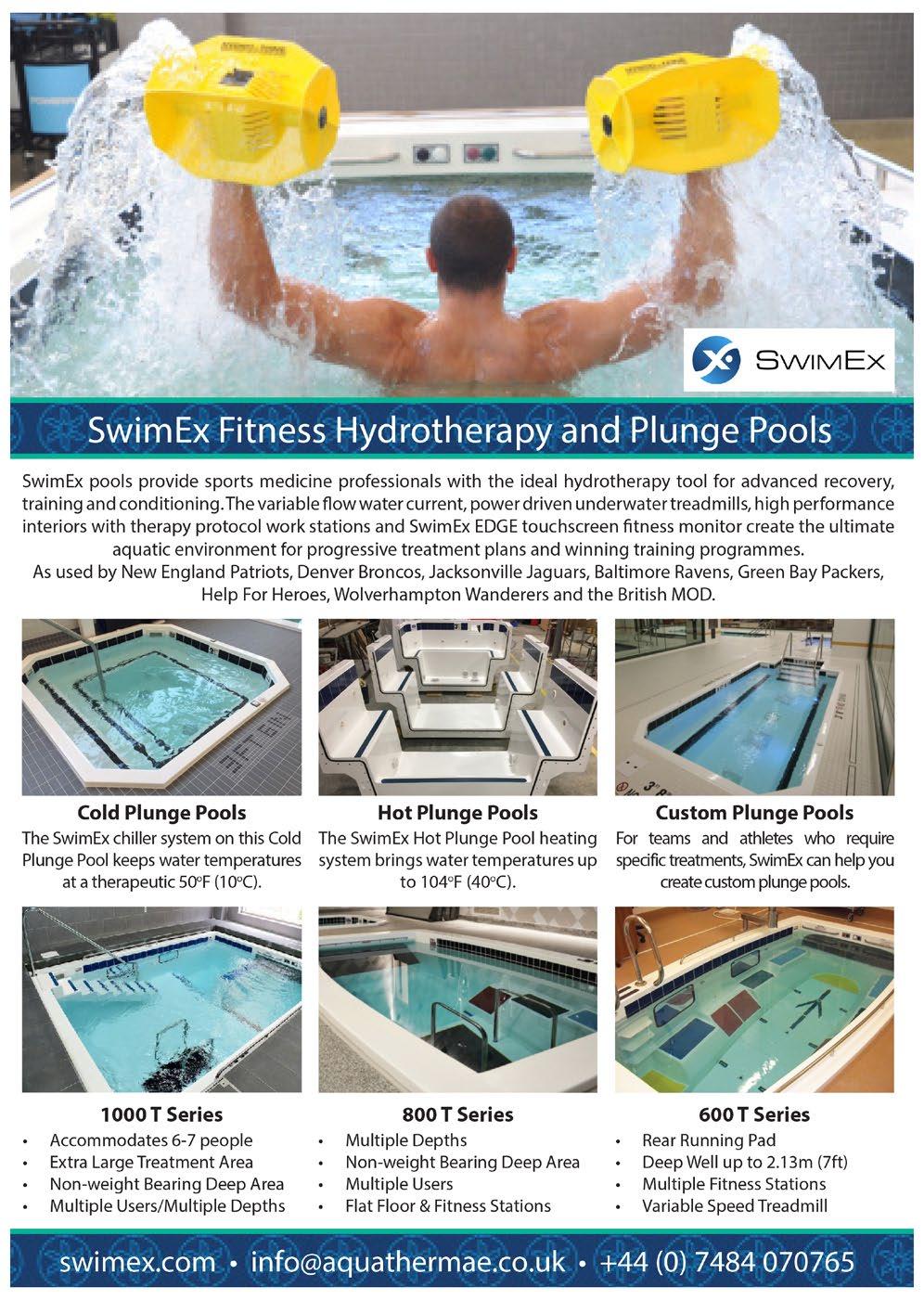
SWIMEX POOLS AT NZCIS
In 2021, the brand-new facilities at the New Zealand Community and Innovation of Sport were installed to support multidisciplinary athletes across all sports and all levels in New Zealand.
SwimEx were proud to be invited to design and supply the hydrotherapy performance and recovery pools for this prestigious project - the head office in USA, SwimEx technical insight design, and supplier connections from Richard Bishop who oversees SwimEx in the UK and Europe.
Larger team squads can bath simultaneously in the SwimEx 1000T with a motorised underwater treadmill, SwimEx 800T and two custom-built deep water plunge pools. The cold ice bath plunge pool aids relief of D.O.M.S.
Since opening in 2022, the facilities have hosted several world class teams and become the Official Training Base of New Zealand Rugby All Blacks, Black Ferns, Hurricanes, Wellington Rugby, IRANZ - International Rugby Academy of New Zealand and Wellington Phoenix FC. Also, more recently, the Sweden women’s football side during the 2023 World
Cup and the England Roses women’s rugby team visited.
In addition to delivering world class facilities, a defining core aim was to embrace and provide an authentic Māori culture.
Jamie Tout (JT) Director of the Performance Institute at the New Zealand Campus of Innovation and Sport (NZCIS) endorses the SwimEx facilities for resilience and optimal fitness: “At NZCIS, recovery is a fundamental pillar in ensuring our athletes maintain peak performance while reducing the risk of injuries. The state-of-the-art SwimEx pools at NZCIS have been integral in providing the ideal environment for optimal recovery.”
“SwimEx’s innovative water-based therapy and resistance systems create a low-impact yet highly effective environment for highperformance athletes. These pools allow for intense recovery exercises that reduce strain on the body, improving circulation and accelerating healing from injury. Whether it’s for posttraining recovery or rehabilitating from an injury, the controlled environment that SwimEx provides ensures that athletes can continue to


push their limits in training, knowing that they have the tools they need to recover and reduce the risk of injury.”
“At NZCIS, we rely on these facilities to deliver consistent, efficient recovery outcomes that support our athletes in training with intensity, avoiding setbacks, and ultimately enhancing their performance on the field. SwimEx pools are a game-changer in recovery, playing a vital role in elevating high-performance outcomes for our athletes.”
Aqua Thermae contacts:
Phone: 07484 070765
Email: info@aquathermae.co.uk
Website: www.aquathermae.co.uk www.SwimEx.com
NZCIS website: www.nzcis.co.nz





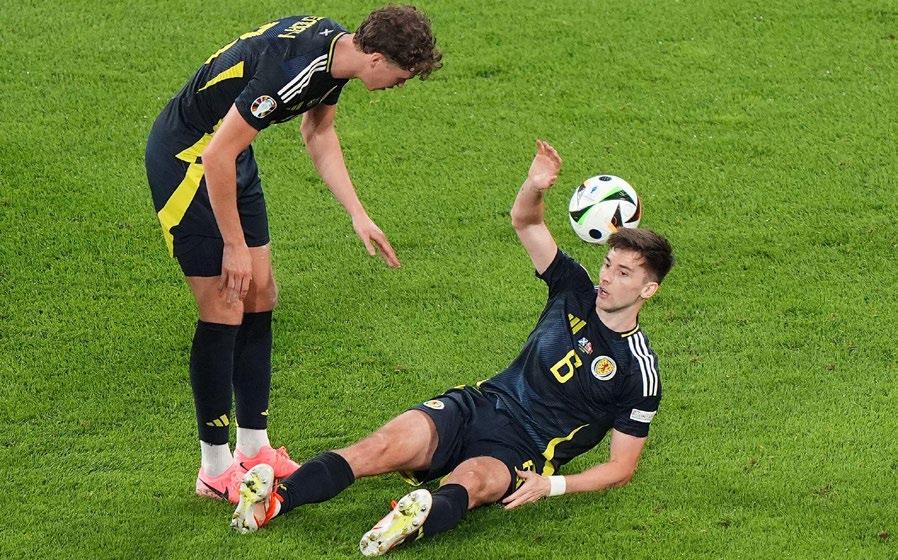
FROM MEDIAL HAMSTRING RUPTURE TO RETURN IN SUB 50 DAYS; IS SURGICAL REPAIR A WASTE OF TIME?
Introduction
Hamstring injuries (HSI) are the most significant cause of time loss in professional football and their prevalence have significantly increased in training and matches over the last decade (Ekstrand et al 2023). The English Premier League (EPL) financial burden and team success estimates based on individual club injury rates were reported in 2016-17 by Eliakim et al (2020). It was estimated that the average overall cost per club was £45 million. Considering the estimated prevalence of hamstring time loss over a ten-year period in the elite football leagues was 19%, this is a huge cost for hamstring injuries alone.
Injuries to the medial hamstrings (semimembranosus (SMB) and semitendinosus (STD)) are reported to be less common (20%) than injuries to Biceps Femoris (BF) (Ekstrand et al 2023). Injuries to the medial hamstrings also
equate to lower overall time loss than those to BF in football. Most hamstring injuries are successfully managed conservatively. Different opinions and management strategies have been discussed for partial or indeed complete ruptures of distal medial hamstring tears. Schilders et al (2005) suggested that surgical tenotomy and resection of chronic STD injuries can provide a swift resolution to ongoing pain and return to full function. The timeframes of full return to performance (RTP) were not disclosed.
Recommended RTP timeframes for a distal medial hamstring rupture have not been widely documented in elite professional football, however it has been suggested that a 3.2-month RTP for distal tendon surgical cases is normal (Plastow et al 2023). Surgeons and Sports Medicine clinicians are still debating the best management for these injuries with the former swaying towards surgical
intervention having a better outcome than conservative.
This article illustrates two successful examples of conservative rehabilitation in professional footballers in the EPL. Both returned to play within 50 days without recurrence over at least a six-month period. These examples aim to provide a rehabilitation framework for this type of injury and raise further discussion on the rehabilitation alone versus surgical or interventional (e.g. platelet rich plasma) treatment options. Written consent was gained from both players to share their rehabilitation journeys anonymously.
Patient cases
Player One (P1)
P1 sustained an acute left medial hamstring injury during the second half of an EPL fixture when accelerating to cut
FEATURE / ADAM PAXTON BSC (HONS), MSC, MCSP
Head of Medical West Ham United Football Club
out an opposition pass. P1 is a professional footballer who has no previous history of hamstring injuries. He has made over 200 EPL appearances and is a full international. The injury was sustained in the month of December during a normal premier league season.
Subjectively the player reported a sharp pain during sprinting, however, was unsure during which part of the running phase. On clinical assessment a clear significant injury was present in the medial distal hamstring tendon region. An MRI confirmed these findings the following day showing ‘complete disruption of a tendinopathic semitendinosus with retraction to the posteromedial joint line’.
Pain reduced and function improved very quickly in this case. The player had no abnormal sensations in their hamstring complex three days post injury. Range on ALSR returned and surpassed (possibly to altered or reduced tension in the hamstring structures) at three days post injury as well. Debates internally started to arise around how quickly this player could be pushed as function had returned so swiftly. It was also theorised that considering this was a complete rupture any ‘healing’ timeframes of the injured tendon could be ignored. This player has a notoriously high pain threshold and had accelerated a few different injuries previously. Considering pain free function had returned so quickly it seemed
Hamstring time loss over a ten-year period in the elite football leagues was 19%
paramount that early hamstring specific loading ensued aiming for the healthy tissues to surpass previous expectations to make up for the now free semitendinosus tendon and consequent muscular tissues. In previous hamstring tendon rehabs an escalating loading programme was utilised to minimise risk of re-injury. In this case, ‘high risk’ exercises such as heavy eccentrics and plyometric were used early considering there was no risk of further tear to the tendon.
In summary, P1 returned to jogging on tarmac at day seven whilst working with a personal therapist in his home country at their request. On return to England and due to Covid-19 restrictions was unable to return to the training ground and subsequently returned to the care of club medical staff on day 16. This day was the first formal pitch

session at the club and marked the start of his progressive return to play. In total the player participated in 24 pitch and 17 lower body sessions before returning to play in the English Premier League (EPL) at day 49. P1 returned to modified team training (RTT) at day 41 however this was planned for day 32 had the player not tested positive for Covid-19 on this day. He then was required to isolate at home for nine days until returning a negative test which delayed his return. He was however set treadmill and pitch sessions at home under club staff guidance. Specialist gym equipment was delivered to his house to ensure rehabilitation could continue progressing whilst isolating. His hamstring scores improved on return from isolation which was testament to the player’s application and professionalism throughout this period. P1 started and played 90 minutes of an EPL game on day 49, however as explained earlier his return was delayed by Covid-19 restrictions. An earlier return date on day 43 was originally planned.
P1 went on to start all remaining games he was available for (16 EPL, six Europa League and two FA Cup) missing one through personal reasons and three due to a contact ankle injury. He did not sustain an injury to either hamstring for the entirety of the following two seasons.
Player Two (P2)
P2 sustained an acute left hamstring injury in the first half of a domestic cup game whilst accelerating to retrieve the ball. P2 is a professional footballer with no previous history of hamstring injuries. He has made over 140 appearances in Europe’s top five leagues and is a full international. An MRI performed the next day revealed a ‘partial tear of approximately 50% crosssectional area of the distal semitendinosus tendon at the supra-genicular region’. P2 had a specialist consultation via Zoom and surgical options were discussed. The player declined the suggestion of resection surgery.
At the request of P2, he travelled to Madrid to seek treatment with a personal therapist and remained there until day 19. A repeat MRI was planned for day 20 which showed that the partial tear had progressed to a full thickness rupture and the free tendon had retracted 5cm. On questioning the player recalled an innocuous incident at day 13 which may have caused the additional trauma to the tendon. The player sought a surgical opinion at this stage and was discussed at the club. Due to the extended nature of a surgical rehabilitation for this injury and P2 discussing the conservative option with P1 it was decided to progress conservatively. P2 also disclosed that he had additional motivations to be available for his national team selection during the next international break which was during week 11 post injury. Timeframes were planned from the initial incident rather than the subsequent mechanism in Madrid as like P1 we weren’t adhering to healing timeframes of the tendon anymore, rather conditioning the healthy tissue to compensate. An accelerated protocol was therefore planned to achieve the player’s goals.
During P2’s time in Madrid it was recommended that he started hamstring isometrics on day seven and did a total of 12 movement and hamstring specific gym sessions over an 18-day period. P2 commenced rehabilitation at the club on day 22 and first session on pitch at day 23. Prior to modified RTT at day 38, P2 completed seven formalised lower body gym sessions and 11 pitch sessions. In comparison to P1, P2 did have twinges of discomfort throughout the rehab which were short-lived in duration and did not limit him in any actions.
P2 trained fully with the team on seven occasions to include one in house game of 65 minutes and one lower body sessions prior to RTP at day 50 in an EPL fixture. Post injury P2 started every club game for the remainder of the season totalling 13 EPL, three Europa league, and two international fixtures. He did not sustain a further injury to his hamstring or any other area for the remainder of the season. The player continued a pretraining activation programme specific to his needs and intermittent loaded hamstring specific gym sessions amongst fixtures.
Objectivity
Amongst other tests the chosen markers that had the most specificity for these players were an eccentric Nordic hamstring curl and a four-point kneeling
isometric knee flexion in 10 and 90 degrees of knee flexion. As shown in the graphs below both players were considerably under their premorbid or indeed contralateral hamstring before returning to training and games. Both players did not achieve results within 10% of premorbid levels until weeks post returning to performance.
P1 showed a steady increase in isometric hamstring curls in both 0 and 90 degrees however their scores regressed at times of pitch load progressions such as return to training or increased match exposure. His eccentric Nordic scores on the injured limb peaked at 4.03N/kg with a premorbid personal best of 5.8N/kg on the ipsilateral side and 7.2N/kg on the contralateral. The length of time between tests four and six of the eccentric Nordic was 69 days.
P2 saw a steady increase in all three tests, however experienced dips in both isometric strength tests as the pitch loads increased closer to returning to training. Both isometric at ten degrees and eccentric Nordic surpassed pre-morbid scores on the injured side, however not until after returning to full match play. For player two the length of time between tests three and five on their eccentric Nordic was 13 days and between tests five and seven on the 90 degree hamstring iso curl was 14 days.
Summary
Coincidentally (or possibly not) we were able to rehab two very similar injuries over a three-season period with radically different anatomy/physiology/ biomechanical variances. P1 was extremely focused on returning as quickly as possible conservatively and would not consider the surgical option. Due to a successful and swift return to play this gave a tangible example for P2 to follow. Both returned in much shorter time frames than suggested for tendon surgeries (Plastow et al. 2023) without recurrence and full return to performance. Chang et al. (2020) infer that high grade hamstring injuries tend to have poor outcomes and high recurrence rates.
Very little research has been published regarding return to play for distal hamstring tendon injuries however, much more literature exists for proximal (Rudisill et al. 2021). Surgical timeframes mentioned by Rudisill et al. (2021) for proximal medial hamstring ruptures suggest a mean RTP of 83.3 days. This is markedly longer than the sub fifty-day rehabs presented in this article. The question must be asked whether the surgical option should ever be chosen over conservative in these types of injuries.
Early objective hip profile strength scores showed good ability of both players to
generate force throughout the range proximally. Hip hinge and hip thrust movements under high tensile load were integrated into their gym programmes early, which may well have had a positive outcome in return to play timeframes and subsequently their availability for the remainder of the season.
Conversely how important are isolated objective measures? What is clearly shown is that both players were significantly below premorbid isometric and eccentric strength scores on returning to training and indeed returning to play. This decision was not taken lightly amongst the medical department and involved a full multidisciplinary debate and agreements discussed with the players acknowledging knowns and unknowns. Ultimately both players were surpassing pitch/GPS premorbid markers and subjectively moving and performing well in training. This joint decision making and philosophy was validated by van der Horst et al (2017). Both players were not medicated throughout, and no injection therapies used. The decisions were then made not to hold the players back based on gym-based markers and instead respect what the players are showing us they can do. Of note, both players were tested intermittently post returning to play and both took at least two months to be within ten percent of their premorbid scores. Returning to baseline objective markers has previously been suggested as the aim for return to play for hamstring injuries (Dunlop et al 2019), however in this example the players had played multiple games and match play minutes before they were in ‘acceptable’ ranges. Dunlop et al. (2019) have suggested that clinicians are debating which testing is the most accurate for RTP and avoiding recurrences when considering hamstring injury rehabilitation.
Both players adhered to bespoke gym maintenance programmes in addition to their on-pitch demands of matches and training. This compliance was key to maintaining their availability especially under such strenuous match schedules.
Conclusion
• A rupture of a medial hamstring tendon can potentially be expedited due to rapid return of baseline clinical markers and reduction in pain.
• Objective measures are important in context; however, sport specific function and performance markers should be utilised in return to play decisions.

• If the surgical option is considered, resection of the tendon stump may be preferable rather than repair to speed up return to play with potentially similar outcomes.
• Ongoing gym loading of the hamstring post return to play is vital to achieve premorbid markers and ultimately avoid subsequent injuries.
Acknowledgments
West Ham United: Josh Ewens – Head of Sports Science and Innovation
Richard Collinge -Performance Director
Richard Weiler – Sports Physician Lead Luke Ford-Thomson – Sports Science and Nutrition Intern
References
1. Ekstrand, J. et al. (2022) ‘Hamstring injury rates have increased during recent seasons and now constitute 24% of all injuries in men’s professional football: The UEFA Elite Club Injury Study from 2001/02 to 2021/22’, British Journal of Sports Medicine, 57(5), pp. 292–298. doi:10.1136/bjsports-2021-105407.
2. Eliakim, E. et al. (2020) ‘Estimation of injury costs: Financial damage of English Premier League teams’ underachievement due to injuries’, BMJ Open Sport& Exercise Medicine, 6(1). doi:10.1136/bmjsem-2019-000675.
3. Schilders, E. et al. (2006) ‘Partial rupture of the distal semitendinosus tendon treated by tenotomy—a previously undescribed entity’, The Knee, 13(1), pp. 45-47.doi:10.1016/j. knee.2005.05.004.
4. Plastow, R. et al. (2023) ‘London International Consensus and Delphi Study on Hamstring Injuries Part 2: Operative Management’, British Journal of Sports Medicine, 57(5), pp. 266–277..
5. Rudisill, S.S. et al. (2021). Evidence-Based Management and Factors Associated With Return to Play After Acute Hamstring Injury in Athletes: A Systematic Review. Orthopaedic Journal of Sports Medicine, 9(11).
6. Van Der Horst, N. et al. (2017b) ‘Return to play after hamstring injuries in football (soccer): a worldwide Delphi procedure regarding definition, medical criteria and decisionmaking,’ British Journal of Sports Medicine, 51(22), pp. 1583–1591.
7. Dunlop, G. et al. (2019). Return-to-Play Practices Following Hamstring Injury: A Worldwide Survey of 131 Premier League Football Teams. Sports Medicine, (50).


‘SETTING THE BENCHMARK’ PART 5: THE CONTEXTUAL AND TACTICAL FACTORS THAT INFLUENCED THE PHYSICAL MATCH DEMANDS AT THE FIFA MEN’S & WOMEN’S WORLD CUPS
FEATURE / DR PAUL S. BRADLEY
Introduction
It is exceedingly challenging to pinpoint the exact moment scientists first investigated the match demands of football 1. Arguably, Tom Reilly and Vaughan Thomas were the first to examine the demands of football in the mid 1970’s 2. Since then, an expansive body of work on this subject has revolutionised our understanding of the game through insights that optimise training preparation. Despite encouraging progress in this area over time, a deeper knowledge of how various contextual and tactical factors impact match demands is still at an embryonic stage 3. A myriad of factors
can up or downregulate the match physical demands experienced by elite players. Indeed, given the multifaceted nature of the game, technical, tactical, social and psychological elements amalgamate during a match 4. Although these factors are countless, some of the most influential aspects include the competition stage, game state, style of play and the standard of both teams involved in a match 5,6. Information on such factors may be valuable to practitioners and enable them to fully grasp the sheer complexity surrounding these contextual and tactical variables. To assist our understanding of this area, FIFA have
recently devised their own Enhanced Football Intelligence metrics to provide much-needed context as to how teams physically exerted themselves during official FIFA tournament matches 7 Consequently, this piece delves into how physical match demands vary according to shifting contexts and tactics during the FIFA Men’s World Cup Qatar 2022 and the Women’s World Cup Australia and New Zealand 2023. This piece of work complements previous ‘Setting the Benchmark’ papers 8-11, so readers are advised to examine Parts one to four (free online resources) to gain a more holistic understanding of team and positional demands.
FIFA, Zürich, Switzerland
Contextual Influences
Team Match Demands Across Tournament Stages
When teams progress from the group stage to the knockout rounds of a major tournament, more significance is naturally placed on winning. Previous research has found that this added incentive to win in the knockout stage increases the intensity of match play. For instance, at the FIFA Women’s World Cup Canada in 2015 and France in 2019, the distance covered sprinting increased by 8-12% in the knockout rounds compared to the group stage12
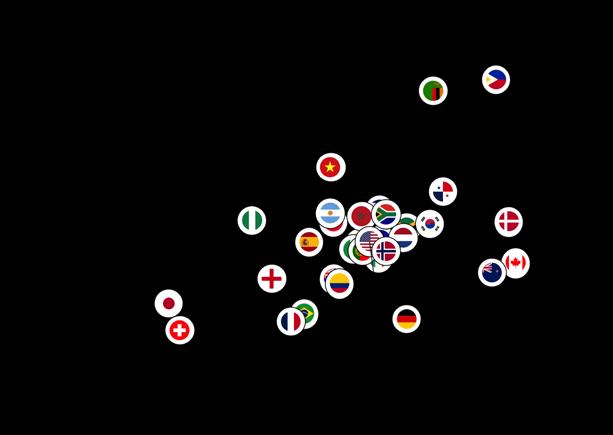
This trend continued at the FIFA Women’s World Cup 2023, particularly in the semifinals and final, where the distances covered sprinting were greater than in the group stage and the earlier knockout rounds. Both England and Spain recorded their highest sprinting outputs of the whole tournament in the final (Figure 1A). Interestingly, the two finalists at the FIFA World Cup Qatar 2022, Argentina and France, also produced their greatest sprint distances in the competition’s most important game (Figure 1B). This suggests that the intensity of match play could be at its greatest at the business end of a tournament.
Relationships Between Match Demands and Average Points Per Game
The previous section highlighted that teams physically prime themselves for the latter stages of a tournament. However, do teams that have a higher physical output also obtain more points per game? To gauge this, results in all games at the FIFA Men’s and Women’s World Cups were assigned a points value: three points for a win, one point for a draw and zero points for a loss. Relatively weak non-significant correlations were found for both the FIFA Men’s and Women’s World Cups between the average points per game and overall
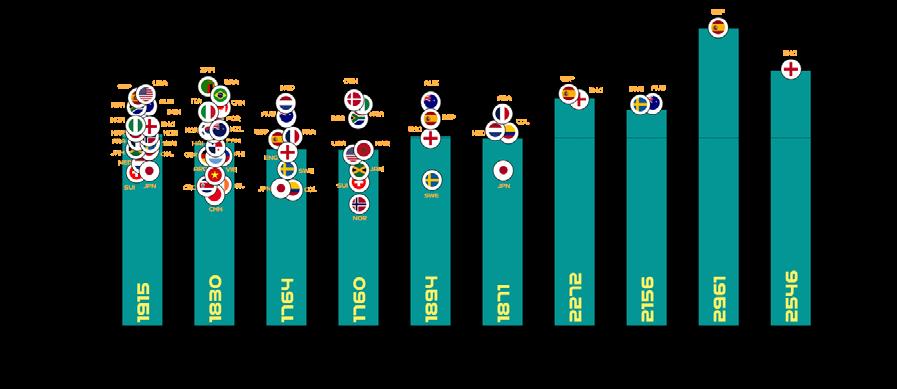
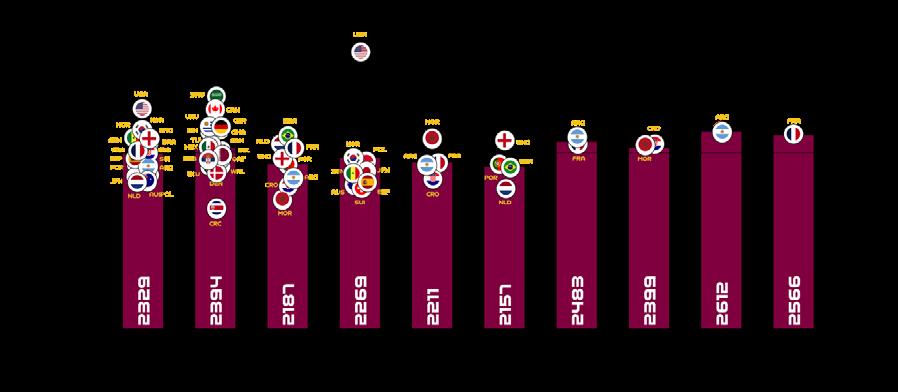
Figure 1: Team Sprint Distance Across Tournament Stages at: (A) the FIFA Women’s World Cup Australia and New Zealand 2023 (≥23.0 km·h-1), in addition to: (B) the FIFA Men’s World Cup Qatar 2022 (≥25.0 km·h-1). Data redrawn from Bradley9, 11
(A) FWWC 2023
(B)
FWC 2022
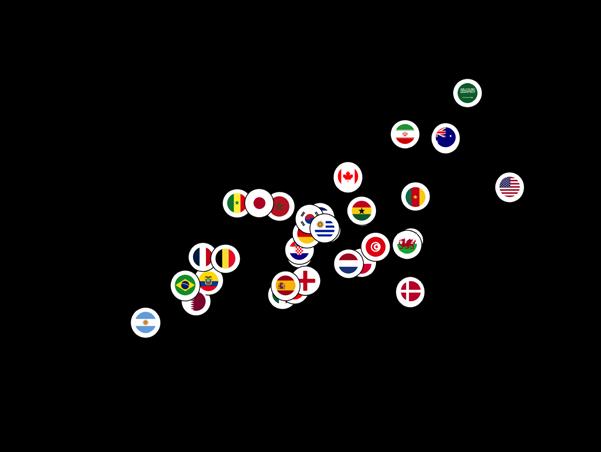
distance covered (r=-0.27 and 0.24; P>0.05), high-intensity running (r=-0.17 and 0.25; P>0.05) and sprint distance (r=-0.12 and 0.31; P>0.05). On the other hand, Figure 2A revealed a moderate association was identified between sprint distance covered by a team in-possession of the ball and average points per game for the FIFA Women’s World Cup (r=0.49; P<0.01), but not in the FIFA Men’s World Cup (r=0.10; P>0.05) in Figure 2B.
To help identify trends, crosshairs based on the tournament averages were drawn to create quadrant plots (e.g., upper-right, upper-left, lower-right and lower-left). At the FIFA Women’s World Cup 2023, 10 out of the 16 teams that reached the knockout stage were found in the upper-right quadrant, featuring the teams that sprinted the most in-possession and also picked up the most points per game (Figure 2A). This trend was less pronounced at the FIFA Men’s World Cup 2022, as only 5 out of the 8 teams that reached the quarter finals were found in the upperright quadrant (Figure 2B). Interestingly, the FIFA World Cup winners at both tournaments are both highly ranked in the upper-right quadrant. Although it is tempting to attribute this finding heavily to physical characteristics, the reader should be cognisant of the complexities surrounding game outcomes. For instance, some games were won during penalty shoot-outs, which obviously required no sprinting in-possession of the ball. This section also used a crude method of allocating points, with three points being assigned for a win despite knockout games being part of an elimination process and therefore their importance not being comparable to that of group games. Moreover, any inferences from these types of correlations must be treated with caution as it indicates that numerous unexplained factors could be impacting the relationships evaluated.
(A)
FWWC 2023
(B) FWC 2022
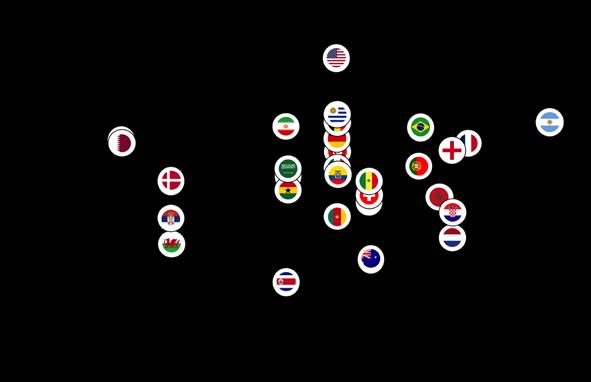
Figure 2: Relationship Between Team Sprint Performance and the Average Points Per Game at the: (A) FIFA Women’s World Cup Australia and New Zealand 2023 (≥23.0 km·h-1), in addition to the: (B) FIFA Men’s World Cup Qatar 2022 (≥25.0 km·h-1). Data redrawn from Bradley9, 11

Links Between Match Demands and Phases of Play
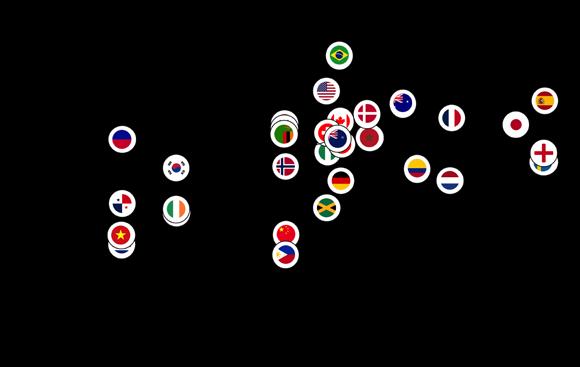
There was an expectation that utilising FIFA’s Enhanced Football Intelligence metrics would shed some light on the tactical factors that up or downregulated the teams’ physical exertions during FIFA Women’s and Men’s World Cup games. Thus, to further contextualise the trends from both tournaments, physical and tactical metrics were correlated against each other to determine any noteworthy associations. Specifically, this was carried out using the phase-of-play metrics that captured the tactical approach of teams during games. Interestingly, strong associations between the number of high-intensity runs that a team completed and the various phases of play occurred for game situations that had a real sense of urgency attached to their outcome (e.g., a risk of conceding/chance of scoring).
Figures 3A and 3B reveal that the number of high-intensity efforts outof-possession were correlated with the number of defensive transition/ recoveries a team performed at both the FIFA Women’s and Men’s World Cups, (r=0.48-0.63; P<0.01). Due to the potential consequences of not tracking back, it is not surprising that teams work intensely out-of-possession during defensive recoveries and/or transitions 9, 11. At the FIFA Women’s World Cup, debutantes the Philippines, Zambia and Panama clearly resided within the upper-right quadrant, performing a plentiful number of each type of action. This could suggest that some of the least experienced teams (e.g., less experience at FIFA World Cup events) found it difficult to cope tactically against more seasoned opponents and thus had to recover intensely more often. This trend could also be applied to nations with less experience at the FIFA Men’s World Cup such as Saudi Arabia, Iran, Canada and Cameron that also resided in the upper-right quadrant.
(B) FWC 2022
Figure 3: Relationship Between the Number of Team High-Intensity Runs and the Number of Recovery/Defensive Transition Phases Per Game at: (A) the FIFA Women’s World Cup Australia and New Zealand 2023 (≥19.0 km·h-1), in addition to: (B) the FIFA Men’s World Cup Qatar 2022 (≥20.0 km·h-1). Data redrawn from Bradley9, 11
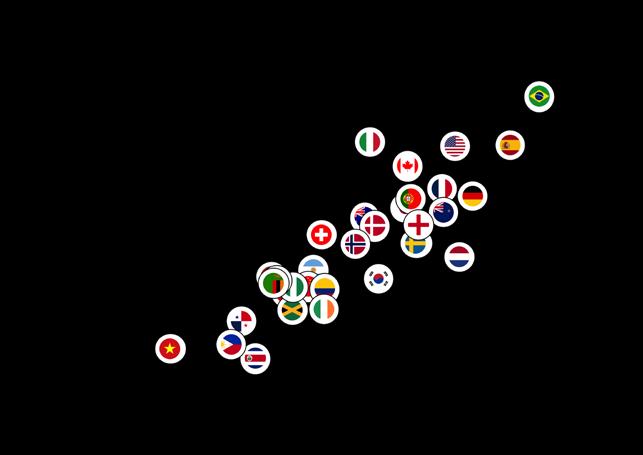
Similarly, Figures 4A and 4B indicate that the number of high-intensity efforts in-possession were associated with movements to progress quickly up the pitch and carry an attacking threat into the final third (r=0.75-0.86; P<0.01). These associations could suggest that teams up their intensity once they progress the ball forward, including into the final third, via vertical passes or dribbles in an attempt to pose an attacking threat. In both tournaments more attacking teams in the upper-right quadrant such as Brazil, Spain and the USA, progressed up the pitch and into the final third quicker and more frequently than deeper, more defensive teams in the lower-left quadrant. Research has revealed that the greatest proportion of a team’s high-intensity actions occur during fast transition-based activities3, 13. Thus, the correlations above could indicate that players produce intense running either to recover defensively into a better position or to get forward as part of an attack. However, the reader should view these associations with some caution as numerous factors impact these types of relationships.
The Opposition’s Impact on Match Demands
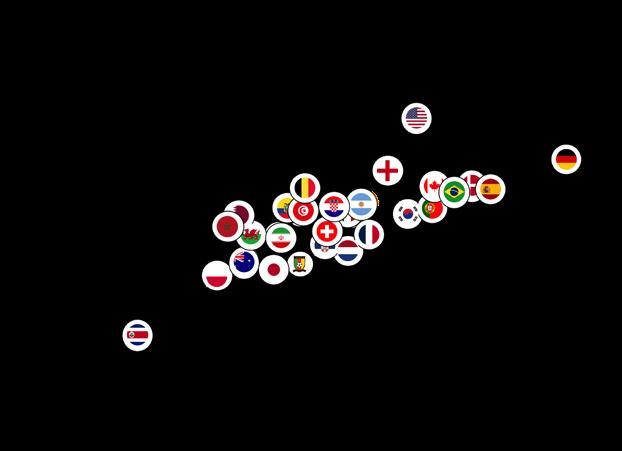
A powerful factor modulating a team’s physical outputs is the opposition that they face. This is especially evident when the opposition perform at an extremely high or low intensity. This, among many other factors, may require a team to up or downregulate their exertions accordingly5,6. Figures 5A and 5B illustrate teams at both the FIFA Women’s and Men’s tournaments with high or low physicality and the impact that this may have had on the work rates of their opposition. Teams at the extremes of the high-intensity continuum at the FIFA Women’s (Spain and Zambia) and Men’s competitions (USA and Canada) at the high end alongside those at the low end (FWWC 2023: Costa Rica and Jamaica; FWC 2022: Costa Rica and Ecuador). When teams played against Zambia and Spain in the FIFA Women’s World Cup or USA and Canada in the Men’s competition, they covered more highintensity running distance compared to the average of their other games. By contrast, when playing against Costa Rica or Jamaica in the FIFA Women’s World Cup or Costa Rica and Ecuador in the Men’s tournament, teams covered less high-intensity running distance than in their other games.
(B) FWC 2022
Figure 4: Relationship Between the Number of Team High-Intensity Runs and the Number of Final Third Phases Per Game at: (A) the FIFA Women’s World Cup Australia and New Zealand 2023 (≥19.0 km·h-1), in addition to: (B) the FIFA Men’s World Cup Qatar 2022 (≥20.0 km·h-1).
Data redrawn from Bradley9, 11
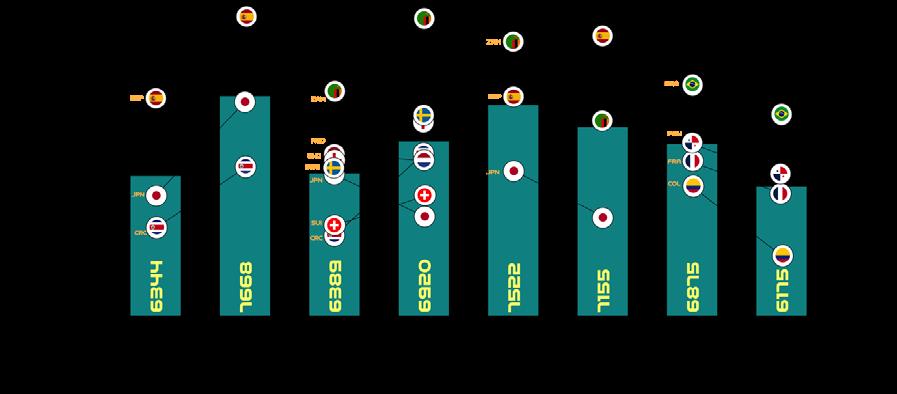
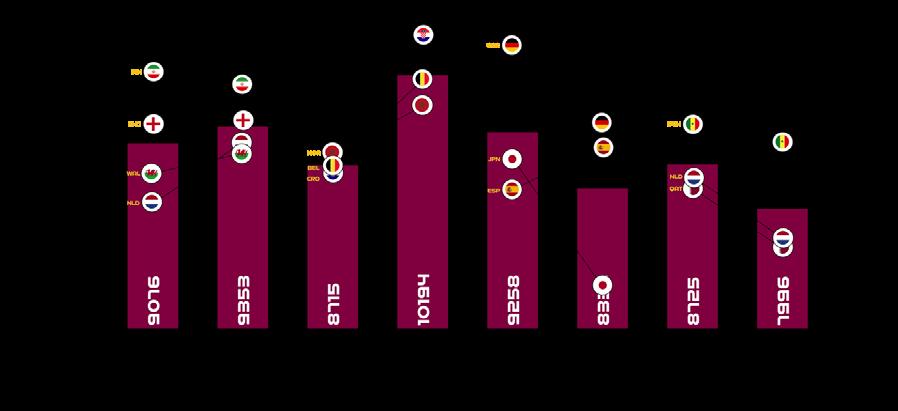
Figure 5: The Influence of Teams High or Low Physicality on the High-Intensity Performance of Their Opposition at: (A) the FIFA Women’s World Cup Australia and New Zealand 2023 (≥19.0 km·h -1), in addition to: (B) the FIFA Men’s World Cup Qatar 2022 (≥20.0 km·h -1). Data redrawn from Bradley 9, 11
Data obtained from FIFA’s Enhanced Football Intelligence metrics provides valuable context regarding the reason(s) why certain teams impacted their opposition’s physicality. For instance, the high-intensity nature of Champions Spain at the FIFA Women’s World Cup could be linked to their dominance on the ball. Spain recorded the highest number of movements to receive and the secondgreatest number of progression and final-third phase of play events at the tournament. When Spain advanced, they
regularly utilised the wide areas to cross or sought to penetrate through runs in behind the opposition’s defensive line, ranking first at the tournament for both. Although Spain averaged the highest ball possession at the tournament, they still occasionally lost the ball and would intensely press, defensively transition and/or recover when required. Similarly, the USA’s intensity at the FIFA Men’s World Cup could be associated with their frequent transitions to recover defensively and to progress offensively, which may
require players to produce long linear highintensity runs. Logically, these activities may not only be physically taxing for Spain’s and the USA’s players but seem to have influenced the work rate of their opponents, who have to react to their high-intensity activity.
By contrast, Costa Rica in both the FIFA Women’s and Men’s tournaments were a nation that downregulated the highintensity work rates of their opponents. Costa Rica produced some of the lowest
(B) FWC 2022
in-possession distances at high-intensity at each tournament. They frequently sat compactly in a defensive low- or mid-block for extended periods. This reduced their own opportunities to move into space and more importantly limited the scope for the opposition to perform high-intensity movements – especially in behind. Hence, why playing against them may reduce their oppositions intensity.
Conclusions
This piece peels away the complex layers associated with the contextual and tactical factors that influence the demands placed on women’s and men’s international teams. It provides some basic evidence to suggest that the match demands are altered based the competition stage, game state, style of play and the standard of both teams involved in a match. The reader should be cognisant that the trends presented are complex and dynamic with a multitude of interacting factors occurring simultaneously.
Sources Reproduced and Funding
The present piece includes content already within the public domain (e.g., FIFA Training Centre and Biology of Sport). The author would also like to thank the FIFA High Performance Division for supporting and funding this important research.
Contact: paulbradley94@yahoo.co.uk

References
1. Bradley PS. The Premier League Way: Contextualising the Demands of the World’s Most Intense League. 2022; Amazon, UK.
2. Thomas V, Reilly T. Application of motion analysis to assess performance in competitive football. Ergonomics. 1976;19(4):530
3. Ju W, Hawkins R, Doran D, Gómez-Díaz A, Martín-García A, Evans M, Laws A, Bradley P. Tier-specific contextualised high-intensity running profiles in the English Premier League: more on-ball movement at the top. Biol Sport. 2023; 40:561–573.
4. Bradley PS, Ade JD. Are Current Physical Match Performance Metrics in Elite Soccer Fit for Purpose or Is the Adoption of an Integrated Approach Needed? Int J Sports Physiol Perform. 2018; 13:656–664.
5. Bradley PS, Noakes TD. Match running performance fluctuations in elite soccer: indicative of fatigue, pacing or situational influences? J Sports Sci. 2013; 31(15):1627–1638.
6. Paul DJ, Bradley PS, Nassis GP. Factors affecting match running performance of elite soccer players: shedding some light on the complexity. Int J Sports Physiol Perform. 2015; 10:516–519.
7. FIFA. EFI Explanation Documents. FIFA. 2022. Available from: https://www.fifatrainingcentre.com/en/fwc2022/efi-metrics/efimetrics-pdfs.php.Accessed March 2023.
8. Bradley PS. ‘Setting the Benchmark’ Part 1: The Contextualised Physical Demands of Positional Roles in the FIFA World Cup Qatar 2022. Biol Sport. 2024; 41(1):261–270.
9. Bradley PS. ‘Setting the Benchmark’ Part 2: Contextualising the Physical Demands of Teams in the FIFA World Cup Qatar 2022. Biol Sport. 2024;41(1):271–278.
10. Bradley PS. ‘Setting the Benchmark’ Part 3: Contextualising the Match Demands of Specialised Positions at the FIFA Women’s World Cup Australia and New Zealand 2023. Biol Sport. 2025;42(1):99–111.
11. Bradley PS. ‘Setting the Benchmark’ Part 4: Contextualising the Match Demands of Teams at the FIFA Women’s World Cup Australia and New Zealand 2023 Biol Sport. 2025;42(2):3–15.
12. Bradley PS, Scott D. Physical Analysis of the FIFA Women’s World Cup France 2019™. Zurich: FIFA. 2020; Available from: https://img. fifa.com/image/upload/zijqly4oednqa5gffgaz.pdf. Accessed February 2024.
13. Bortnik L, Burger J, Rhodes D. The mean and peak physical demands during transitional play and high-pressure activities in elite football. Biol Sport. 2022; 39:1055–1064.
PRESCRIBING TRENDS & PRACTICES IN PROFESSIONAL FOOTBALL
FEATURE / DR RICHARD PORTER1,2, DR ADAM DRUMMOND3, DR RISHI DHAND4
The physical demands of elite football are increasing, with players consistently covering greater distances at higher speeds. Therefore, there is an increasing need for athlete robustness to prevent injury and illness, placing a greater emphasis on medical departments to optimise all aspects of health and wellbeing. This can be difficult, given the limited evidence base for many treatment options within musculoskeletal medicine and the restricted opportunities to develop high quality studies within elite sport.
Pain is the most common symptom of musculoskeletal injury and multiple studies have demonstrated high levels of non-steroidal anti-inflammatory (NSAID) use in players. In recent years, the use of medication within the international setting has been monitored by FIFA. A large review involving German athletes highlighted the concerning use of analgesia amongst players, with prevalence of use as high as 54.2%.1 This is comparatively much higher than a non-elite population, which is particularly concerning given the potential deleterious effects of these medications in sport.2
Paracetamol is a widely used analgesic with a favourable safety profile. However, its efficacy is relatively low for acute pain and is no different to placebo in chronic musculoskeletal pain.3,4 NSAIDs are effective analgesics and can improve symptoms associated with injury related inflammation, but can have negative effects on muscle, bone and tendon healing.5,6
Opiate based analgesics have their own risks, such as addiction, GI disturbance and coordination impairments, leading to the recent WADA ban on tramadol. Parenteral analgesia, such as local anaesthetic injections, are also commonly requested. However, these have their own risks that have been discussed extensively, alongside the potential ethical implications associated with their use.7 In addition, the long-term safety profile of local anaesthetic injection to allow participation in the short term is unclear. 22% of players felt local anaesthetic delayed recovery from their primary injury.8
Principles of good prescribing practice remain constant regardless of setting;
suitable knowledge of patient, condition and medicine alongside shared decision making and consent.9 In elite sport, there can be an emphasis on management strategies which prioritise sporting aims and outcomes in the short-term, which could be dubbed ‘prescribing pressure’.
This article reviews recent survey data from prescribers in elite football. It includes responses from 126 practitioners, 79.4% of whom were based in the UK. 78.6% work in teams at international, Premiership or Championship equivalent level and 15.1% practice in Women’s football.
Throughout the survey cohort, high levels of analgesic prescribing were found, both in training and match settings (figure 1).
Paracetamol was by far the most prevalent drug prescribed, with 52% of practitioners prescribing this regularly in matches, 57% regularly in training and 96% in utilising at some point. This is to be expected, given its overall safety profile and familiarity among clinicians. Additionally, it is commonly used in minor illness.

1. Department of Rheumatology, Manchester Foundation Trust
Football Association, St George’s Park
Burnley FC 4. Leeds United FC
Interestingly, there were significant correlations in prescribing habits. For example, those who prescribe paracetamol for training were more likely to prescribe all NSAIDs and opiates (R slope range 0.284-0.689, p≤0.002 for all) in both training and matches. Whilst viewed as potentially harmless, paracetamol prescribing could be seen as a gateway to use of multiple different agents, some which practitioners should be wary of in terms of self-audit.
Clinicians in the UK were more likely to use both paracetamol and opiates than other international practitioners (p=0.011 and p<0.001 respectively). No significant differences were seen with other analgesics and opiate prescribing did not correlate to perceived prescribing pressure. The recent WADA ban on tramadol could conceivably have shifted some prescribing load towards a preference of codeine. Although codeine
has a slightly lower association with addiction compared to tramadol, it may still modulate training and performance.10 This data raises the question as to whether specific audit of its usage in sport is warranted. Codeine also carries an anticholinergic burden, and cumulative dosing of medications in this category can be associated with cognitive impairment which is also important for prescribers to be aware of.
Prescribing of all types of analgesia was more prevalent in senior squads compared to academies. This could be due to the perceived “higher-stake environment” associated with senior football, and a greater pressure to get key players onto the pitch. However, there was a nonsignificant trend towards higher perceived ‘prescribing pressure’ in lower tiers of competition (R=0.190, p=0.060). Another explanation could be that academy doctors are responsible for a wider age
variation, including multiple paediatric cohorts where conservative approaches are understandably more common due to limited drug options and variable dosing. In addition, a longitudinal focus on player development may lend itself more strongly to conservative or lowerrisk management strategies. Academy doctors are also more likely to be based at their club part-time and have multiple squads Therefore, the amount of contact time and opportunity to prescribe may be lower when compared to senior teams. In addition, academy teams may train less than full-time due to educational constraints and longitudinal care is more likely to be governed by a General Practitioner external to the club.
On average, clinicians felt 26% (range 0-96%) of prescribing decisions were made due to a ‘pressure to prescribe’, but this did not correlate to increased prescribing of any given medication
Figure 1: Bar chart demonstrating the percentage of clinicians who prescribe various types of analgesia regularly, defined as >50%
Prescribing rates in the management of acute muscle strain
Figure 2: Bar chart demonstrating the percentage of clinicians using various forms of prescribable medication following acute muscle injury according to frequency of use
compared to others. Whilst this number may be lower than some expect, the degree of variation could be seen as cause for concern. Prescribing pressure is known to affect prescribing decisions and errors in hospital medicine. 11,12
Whereas hospital medicine pressures may arise when dealing with acutely unwell patients or high workload, prescribing pressures in elite sport may arise proportionally more from the patients themselves and third parties (other medical staff, management staff, other squad members, supporters). Dealing with emergency scenarios and triaging tasks during busy periods are core aspects of learning to work effectively as a clinician, but we are rarely trained to the same degree in managing external pressure and weaving this into a risk:benefit decision on treatment. As clinicians, it is important that we can reflect on this and feel empowered to trust our own training and experience, but also be able to communicate this in response to requests. Not doing so may remove an opportunity to manage a situation in a more holistic manner and subsequently result in overprescribing. The core of GMC prescribing guidance states “you must be satisfied that the drugs serve your patient’s need”.
Differences in prescribing rates for nonselective NSAIDs and selective COX-2 inhibitors likely reflect the duration of use in sporting settings, the population being treated and the cost, with COX-2
You must be satisfied that the drugs serve your patient’s need
inhibitors between five and fifteen times more expensive. Non-selective NSAIDs (ibuprofen, naproxen and diclofenac) inhibit COX-1 and COX-2 pathways. COX-1 is responsible for gastric mucosal protection and platelet aggregation (via thromboxane-A2 production) whereas COX-2 is more specifically involved in generation of pain, inflammation and fever. COX-1 inhibiting drugs are more associated with adverse gastro-intestinal issues and bleeding whereas COX-2 inhibitors have a proportionally increased risk of cardiovascular complications which may be due to a compensatory increased COX-1 activity.
Prescription of COX-2 selective NSAIDs occurred at significantly higher rates in higher competition tiers (p<0.001). Clinicians working with Premier League and Championship equivalent teams are also
more likely to be responsible for long-term injuries, with fewer outsourced to relevant specialists. This may account for increased COX-2 inhibitor prescribing given their favourable gastrointestinal safety profile for longer-term use.
There is also wide variation in prescribing trends following acute muscle injury as displayed in figure 2. Regarding NSAIDs, both immediate use within 48 hours and delayed prescription (initiation >48hr post-injury) were common, with a slight preponderance towards delayed use. UK-based clinicians used <48-hour NSAID significantly less than others (p=0.047). Clinical rationale for early NSAID could be reduction in myositis ossificans in the context of significant contusion. However, this may also reduce early inflammation cascade and reduce healing capacity, as well as bleeding risk in the case of non-selective

NSAID13 although the evidence base in this regard is limited to gastrointestinal14 and solid organ trauma.15
Tranexamic acid (TXA) was used by a total of 21% of respondents in the setting of acute muscle injury, most likely for bleeding prevention following contusion. There were no differences in use across competition tier, gender or player status. TXA works by competitive inhibition of the lysine receptor on plasminogen, preventing plasmin binding to a clot which helps its stabilisation. Use of TXA in hospital settings changed significantly after the HALT trial showed no benefit for upper
References
gastrointestinal bleeds and significantly higher rates of venous thromboembolism associated with its use.16 However, TXA may still have use within the setting of polytrauma.17 This may prompt a rethink on the justification of prescribing in an elite football setting. Serial ultrasound examination could be a useful modality during the first few hours after injury.
Conclusion
As expected, there is a wide variation in the prescribing habits of those working in elite football. This could be reflective of multiple factors, such as the variation in training and experience of doctors working
in elite football, in addition to medical team budgets. The survey data does not have the ability to quantify the volume of prescribing, which is an important consideration when interpreting the results. Nevertheless, several important practices have been raised. As clinicians, we should be able to justify our prescribing based on medical and ethical principles. Consideration of the short and long-term goals of our athletes, which can conflict one another, should form the basis of this. Reflective practice and audit is critical for individual practitioners and clubs when building a robust framework to deliver high-standards of medical care for our athletes.
1. Leyk D, Rüther T, Hartmann N, Vits E, Staudt M, Hoffmann MA. Analgesic Use in Sports: Results of a Systematic Literature Review. Dtsch Arztebl Int [Internet]. 2023 Mar 10 [cited 2024 Sep 26];120(10):155. Available from: /pmc/articles/PMC10201949/
2. Alaranta A, Alaranta H, Helenius I. Use of Prescription Drugs in Athletes. Sport Med 2008 386 [Internet]. 2012 Oct 7 [cited 2024 Sep 26];38(6):449–63. Available from: https://link.springer.com/article/10.2165/00007256-200838060-00002
3. Moore. What’s the point of paracetamol? | University of Oxford [Internet]. 2022 [cited 2024 Sep 26]. Available from: https://www. ox.ac.uk/research/what’s-point-paracetamol
4. Saragiotto BT, Machado GC, Ferreira ML, Pinheiro MB, Abdel Shaheed C, Maher CG. Paracetamol for low back pain. Cochrane database Syst Rev. 2016;(6):CD012230.
5. Chan K-M, Fu S-C. Anti-inflammatory management for tendon injuries - friends or foes? Sport Med Arthrosc Rehabil Ther Technol SMARTT [Internet]. 2009 Dec [cited 2024 Sep 26];1(1):23. Available from: /pmc/articles/PMC2770552/
6. Ghosh N, Kolade OO, Shontz E, Rosenthal Y, Zuckerman JD, Bosco JA, et al. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) and Their Effect on Musculoskeletal Soft-Tissue Healing: A Scoping Review. JBJS Rev [Internet]. 2019 [cited 2024 Sep 26];7(12). Available from: https://pubmed.ncbi.nlm.nih.gov/31851037/
7. Orchard JW. Is it safe to use local anaesthetic painkilling injections in professional football? Sports Med [Internet]. 2004 [cited 2024 Sep 26];34(4):209–19. Available from: https://pubmed.ncbi.nlm.nih.gov/15049713/
8. Orchard JW, Steet E, Massey A, Dan S, Gardiner B, Ibrahim A. Long-term safety of using local anesthetic injections in professional rugby league. Am J Sports Med [Internet]. 2010 Nov [cited 2024 Sep 26];38(11):2259–66. Available from: https://pubmed.ncbi.nlm.nih. gov/20595546/
9. Council GM. Good practice in prescribing and managing medicines and devices - professional standards - GMC [Internet]. 2021 [cited 2024 Sep 26]. Available from: https://www.gmc-uk.org/professional-standards/professional-standards-for-doctors/good-practice-inprescribing-and-managing-medicines-and-devices
10. Holgado D, Hopker J, Sanabria D, Zabala M. Analgesics and Sport Performance: Beyond the Pain-Modulating Effects. PM&R [Internet]. 2018 Jan 1 [cited 2024 Sep 26];10(1):72–82. Available from: https://onlinelibrary.wiley.com/doi/full/10.1016/j.pmrj.2017.07.068
11. Dornan T, Ashcroft D, Heathfield H, Lewis P, Miles J, Taylor D, et al. FINAL report An in depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education. EQUIP study.
12. Green W, Waseem Shahzad M, Wood S, Martinez Martinez M, Baines A, Navid A, et al. Improving junior doctor medicine prescribing and patient safety: An intervention using personalised, structured, video-enhanced feedback and deliberate practice. 2020; 13. Trojian TH. Muscle Contusion (Thigh). Clin Sports Med. 2013 Apr 1;32(2):317–24.
14. Rahme E, Nedjar H. Risks and benefits of COX-2 inhibitors vs non-selective NSAIDs: does their cardiovascular risk exceed their gastrointestinal benefit? A retrospective cohort study.
15. Hill JH, Kuhlman J, Lariccia A, Ngo A, Hyland SJ, Spalding MC. Nonsteroidal Anti-inflammatory Drugs Are Not Associated With Increased Bleeding in Blunt Solid Organ Injury. J Trauma Nurs. 2022 Sep 1;29(5):235–9.
16. Roberts I, Shakur-Still H, Afolabi A, Akere A, Arribas M, Brenner A, et al. Effects of a high-dose 24-h infusion of tranexamic acid on death and thromboembolic events in patients with acute gastrointestinal bleeding (HALT-IT): an international randomised, double-blind, placebo-controlled trial. Lancet [Internet]. 2020 Jun 20 [cited 2024 Sep 26];395(10241):1927–36. Available from: http://www.thelancet. com/article/S0140673620308485/fulltext
17. Nutbeam T, Roberts I, Weekes L, Shakur-Still H, Brenner A, Ageron FX. Use of tranexamic acid in major trauma: a sex-disaggregated analysis of the Clinical Randomisation of an Antifibrinolytic in Significant Haemorrhage (CRASH-2 and CRASH-3) trials and UK trauma registry (Trauma and Audit Research Network) data. Br J Anaesth [Internet]. 2022 Aug 1 [cited 2024 Oct 1];129(2):191–9. Available from: http://www.bjanaesthesia.org/article/S0007091222001842/fulltext


HAMSTRING INJURIES: WHAT ROLE DOES THE LUMBAR SPINE & PELVIS PLAY?
PART 2: GLUTEUS MAXIMUS STRENGTH & ACTIVATION
Introduction
At last year’s London International Consensus and Delphi Study on hamstring injuries (Paton et al., 2023) which involved over 112 physicians, physiotherapists, surgeons, scientists, researchers and trainers, a level of agreement was reached on various aspects of managing hamstring injuries. As part of their study 91% of the experts agreed it was “important to assess, treat and prescribe exercises addressing the whole kinetic chain”. The authors go further and discuss a number of lumbopelvic considerations in hamstring injuries.
In issue 47 of Football Medicine and Performance, we covered how sacroiliac joint mobility, force closure and anterior pelvic tilt might relate to hamstring injuries. In this edition we will discuss the
importance of gluteus maximus (GMax) strength and activation and attempt to distill the current research into a handful of simple clinical take-homes for our athletes.
Gluteus maximus strength in relation to hamstring injuries
1. GMax contributes to force closure: The GMax overlies the SIJ, it connects to the sacrotuberous ligament and contributes to the posterior oblique sling (see pictures below) all mechanisms which contribute to force closure and pelvic stability. In the previous FMPA article we discussed in detail how increasing force closure of the pelvis may reduce hamstring injury risk.
2. Synergistic dominance: The GMax and hamstring muscles work together as synergists for hip extension. When the GMax is weak, the hamstrings may
compensate by becoming the primary hip extensor, a phenomenon known as “synergistic dominance” (Page et al., 2010; Sahrmann, 2013). If we ask the hamstrings to overwork there may be a greater risk of fatigue and subsequent injury (Ekstrand et al., 2023).
3. Reciprocal inhibition: Restricted hip flexor muscle length is theorised to decrease neural drive to the GMax, termed “reciprocal inhibition”. Footballers with hip flexor tightness on the modified Thomas test exhibited less GMax strength (Mills et al., 2015). This pattern has been implicated in lower extremity injury (Opar et al., 2012; Liebenson, 2006) and has also been linked to an anterior pelvic tilt. We covered anterior pelvic tilt in relation to hamstring injuries in the previous article.
Consultant Chiropractor in professional football
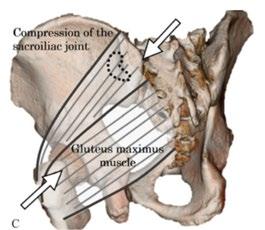
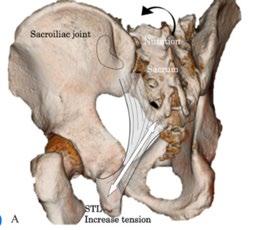
The GMax overlies the SIJ, contributing to force closure and pelvic stability. It also has direct connections into the sacrotuberous ligament, an additional way in which it contributes to force closure of the pelvis. This would be particularly important in the swing phase of running when GMax contraction is at its peak and the sacrotuberous ligament is under most tension (Lenhart et al., 2014; Novachek,1998, Soames et al., 1995; Vleeming et al., 2012). Picture taken from Sasaki et al., 2021.

Traditionally, GMax strength testing would look like the picture on the left (taken from Chandaran et al., 2023). However, in relation to hamstring injuries, GMax strength in the swingphase position appears more relevant (Schuermans et al., 2017) so the test on the right mimics this functional position more closely by having the involved hip in more flexion. Hand-held dynamometry testing in this position showed good-high intrasession reliability when using a three-trial average (Keep et al., 2016).


The GMax has connections to the thoracolumbar fascia and the opposite latissimus dorsi, forming the posterior oblique sling and helping to create pelvic stability (Vleeming et al., 2007). Picture taken from Santana et al. (2015).
The modified Thomas test: Assessing for hip flexor tightness might be one way of indirectly assessing for glute max activation. There is high intraand inter-rater reliability for this test if lumbopelvic movement is controlled (Cady et al., 2022).
Gluteus maximus activation timing in relation to hamstring injuries
Some authors have found there to be altered biceps femoris to GMax ratios in athletes with previously injured hamstrings (Daly et al., 2016), yet others have found no changes (Bourne et al., 2021; Higahihara et al., 2019). The evidence is conflicting.
In a clinical setting, the prone hip extension
test might be a way of monitoring GMax activation timing. However, research regarding this is also conflicting. It was originally thought that in healthy subjects the hamstrings should fire first, then glutes, then lumbar erectors, then thoracic erectors (Janda, 1991) but subsequent studies have found more variety in activation patterns. What’s more, only 57% of the hamstring injury experts agree that the prone hip
extension test is useful, saying it is “not performed upright, and does not approach the speed or amount of hamstring strain in sprinting…”. Should we throw the test out?
One suggestion is to use the prone hip extension test but instead of assessing for GMax activation timing we use it to assess for other hamstring injury risk factors as shown below.

be eight times more

from the
and instead assess the
is good inter-rater agreement for this test (Bruno et al., 2014).
in
Does the lumbar
Prone hip extension test, variation 1: Ignore the glutes altogether. One study showed that if the lumbar erectors fire before the hamstrings the athlete might
likely to go on to sustain a hamstring injury (Schuermans et al., 2017).
Prone hip extension test, variation 2: Ignore activation sequencing
GMax’s role
lumbo-pelvic stability.
spine deviate
midline? There
Optimising gluteus maximus strength adaptations
Footballers who did not develop a hamstring injury had an increased GMax activity in the swing phase on maximal sprinting acceleration (Schuermans et al., 2017). A systematic review found that the ‘step-up’ elicited the highest level of GMax activation when comparing different exercises (Neto et al., 2020). This exercise mimics this important swing phase position. Other exercises that elicited very high levels of GMax activation included hip thrusts, squats, deadlifts, and lunges. It might also be worth considering exercises which combine the GMax and the opposite latissimus dorsi, thus involving the entire posterior oblique sling and improving force closure.
As a chiropractor in a MDT, I may use manual therapy before a physio-led or S&C-led strength session. Here the attempt is to improve the mechanics of the area so that the athlete’s body can then better “accept” the subsequent training stimulus. One example might be in addressing any limited posterior innominate rotation before exercises like the step up or lunge. Posterior innominate rotation (and relative sacral nutation) tensions the sacrotuberous ligament and contributes to force closure, thus allowing the GMax to
contribute less to pelvic stability and more to hip extension strength (Jae Hong et al., 2019; Lee et al., 2013).
Another example might be with reciprocal inhibition; we saw earlier how increasing the length or reducing the tone of antagonists like the iliopsoas, TFL or rectus femoris may influence the neural drive to the GMax. Arthrogenic inhibition might be a consideration here too (Freeman et al., 2013); Does optimising the function of the underlying hip joint or sacroiliac joint with manual therapy have a beneficial effect on the overlying GMax?
Lastly, addressing any pelvic asymmetry might be a consideration. It starts with a skilled assessment and clinical reasoning. We will cover this topic in a future article in how it directly relates to hamstrings.
Summary
• Experts appear in agreement that the kinetic chain, lumbopelvic area and GMax strength is a consideration in hamstring injuries.
• A strong GMax avoids synergistic dominance of the hamstrings, preventing fatigue and injury. It also aids force closure of the pelvis and may allow the biceps femoris to contribute more to knee flexion and hip extension.
• Mimicking a swing phase position when testing or strengthening the GMax appears appropriate. Manual therapy before a strength session might be one tactic to help optimise GMax strength adaptations.
• There is mixed evidence for a “correct” timing or sequence of GMax activation. Testing for this in a clinical setting also has questionable validity. However, the prone hip extension test might be helpful when looking for other patterns associated with hamstring strain.
Nick is a chiropractor with 16 years’ experience working with a range of athletes and seven years’ experience consulting in professional football (Fulham FC and Brentford FC). In a multidisciplinary medical team he will assess spine, pelvis and hip function and co-manage both fit and injured athletes alongside the other therapists. He owns two multidisciplinary clinics in south-west London. He has a special interest in lumbopelvic function and its influence on lower limb injuries and provides CPD sessions to medical teams on this topic. Contact@nickjmetcalfe.com

References
Paton BM, Read P, van Dyk N, Wilson MG, Pollock N, Court N, Giakoumis M, Head P, Kayani B, Kelly S, Kerkhoffs GMMJ, Moore J, Moriarty P, Murphy S, Plastow R, Stirling B, Tulloch L, Wood D, Haddad F. London International Consensus and Delphi study on hamstring injuries part 3: rehabilitation, running and return to sport. Br J Sports Med. 2023 Mar;57(5):278-291.
Ekstrand J, Ueblacker P, Van Zoest W, et alRisk factors for hamstring muscle injury in male elite football: medical expert experience and conclusions from 15 European Champions League clubs BMJ Open Sport & Exercise Medicine 2023;9:e001461.
Sasaki, Takeshi & Kurosawa, Daisuke & Murakami, Eiichi & Watanabe, Takashi. (2021). Physical therapeutic options for residual sacrotuberous ligament pain after treatment of sacroiliac joint dysfunction. Journal of Physical Therapy Science. 33. 646-652. 10.1589/jpts.33.646.
Lenhart R, Thelen D, Heiderscheit B. Hip muscle loads during running at various step rates. J Orthop Sports Phys Ther. 2014 Oct;44(10):766-74, A1-4. Vleeming A ,Mooney V . Movement, Stability & Lumbopelvic Pain 2nd Edition . Philadelphia.Churchill Livingstone .1st March 2007
Choi Jae-hong, Oh Jae-seop, Kim Moon-hwan. The Effect of Pelvic Compression Belt on the Strength of Hip Muscle and EMG Activity in Individuals with Sacroiliac Joint Pain during Prone Hip Extension. J Musculoskelet Sci Technol 2019;3(1):14-21.
Kang Sung Lee, Eunhye Ko, Chae Gil Lim, Effect of Pelvic Belt on Gluteal Muscles Activity during Therapeutic Exercise, Journal of Physical Therapy Science, 2013, Volume 25, Issue 3, Pages 337-340, Released on J-STAGE May 10, 2013, Online ISSN 2187-5626, Print ISSN 0915-5287
Arumugam A, Milosavljevic S, Woodley S, Sole G. Effects of external pelvic compression on form closure, force closure, and neuromotor control of the lumbopelvic spine--a systematic review. Man Ther. 2012 Aug;17(4):275-84.
Arumugam A, Milosavljevic S, Woodley S, Sole G. THE EFFECT OF A PELVIC COMPRESSION BELT ON FUNCTIONAL HAMSTRING MUSCLE ACTIVITY IN SPORTSMEN WITH AND WITHOUT PREVIOUS HAMSTRING INJURY. Int J Sports Phys Ther. 2015 Jun;10(3):291-302.
Keep, H., Luu, L., Berson, A., & Garland, S.J. (2016). Validity of the Handheld Dynamometer Compared with an Isokinetic Dynamometer in Measuring Peak Hip Extension Strength. Physiotherapy Canada, 68, 15 - 22.
Page P, Frank C, Lardner R: Assessment and treatment of muscle Imbalance: the Janda Approach. Chicago: Human Kinetics, 2010.
Daly C, Persson UM, Twycross-Lewis R, Woledge RC, Morrissey D. The biomechanics of running in athletes with previous hamstring injury: A casecontrol study. Scand J Med Sci Sports. 2016 Apr;26(4):413-20.
Higashihara A, Ono T, Tokutake G, Kuramochi R, Kunita Y, Nagano Y, Hirose N. Hamstring muscles’ function deficit during overground sprinting in track and field athletes with a history of strain injury. J Sports Sci. 2019 Dec;37(23):2744-2750.
Bourne MN, Pollard C, Messer D, Timmins RG, Opar DA, Williams MD, Shield AJ. Hamstring and gluteal activation during high-speed overground running: Impact of prior strain injury. J Sports Sci. 2021 Sep;39(18):2073-2079.
Janda V. Muscle spasm – a proposed procedure for differential diagnosis. Journal of Manual Medicine. 1991;6:136–139
Murphy DR, Byfield D, McCarthy P, Humphreys K, Gregory AA, Rochon R. Interexaminer reliability of the hip extension test for suspected impaired motor control of the lumbar spine. J Manipulative Physiol Ther. 2006 Jun;29(5):374-7.
Mills M, Frank B, Goto S, Blackburn T, Cates S, Clark M, Aguilar A, Fava N, Padua D. EFFECT OF RESTRICTED HIP FLEXOR MUSCLE LENGTH ON HIP EXTENSOR MUSCLE ACTIVITY AND LOWER EXTREMITY BIOMECHANICS IN COLLEGE-AGED FEMALE SOCCER PLAYERS. Int J Sports Phys Ther. 2015 Dec;10(7):946-54. PMID: 26673683; PMCID: PMC4675195.
Opar DA Williams MD Shield AJ. Hamstring strain injuries: factors that lead to injury and re‐injury. Sports Med. 2012;3:209‐226
Liebenson C. Rehabilitation of the Spine: a Practitioner’s Manual. 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2006 Sahrmann S. Diagnosis and Treatment of Movement Impairment Syndromes. Oxford, UK: Elsevier Health Sciences; 2013.
Schuermans J, Danneels L, Van Tiggelen D, Palmans T, Witvrouw E. Proximal Neuromuscular Control Protects Against Hamstring Injuries in Male Soccer Players: A Prospective Study With Electromyography Time-Series Analysis During Maximal Sprinting. Am J Sports Med. 2017 May;45(6):13151325. doi: 10.1177/0363546516687750. Epub 2017 Mar 1. PMID: 28263670.
Soames, R. (1995) Skeletal system. In: Williams, P.L., Bannister, L.H., Berry, M.M., et al., Eds., Gray’s Anat- omy, 38th Edition, Churchill Livingstone, New York, 425-736.
Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012 Dec;221(6):537-67. doi: 10.1111/j.1469-7580.2012.01564.x. Epub 2012 Sep 19. PMID: 22994881; PMCID: PMC3512279.
Sasaki, Takeshi & Kurosawa, Daisuke & Murakami, Eiichi & Watanabe, Takashi. (2021). Physical therapeutic options for residual sacrotuberous ligament pain after treatment of sacroiliac joint dysfunction. Journal of Physical Therapy Science. 33. 646-652. 10.1589/jpts.33.646.
Chandran, Aiswarya & P., Madhuripu & Mariarathinam, Premkumar & Menezes, Carolin. (2023). Association between genu recurvatum and gluteus maximus muscle strength in college students - Case control study. Journal of Orthopaedic Reports. 3. 100229. 10.1016/j.jorep.2023.100229.
Bruno PA, Millar DP, Goertzen DA. Inter-rater agreement, sensitivity, and specificity of the prone hip extension test and active straight leg raise test. Chiropr Man Therap. 2014 Jun 16;22:23. doi: 10.1186/2045-709X-22-23. PMID: 24982755; PMCID: PMC4075776.
Cady K, Powis M, Hopgood K. Intrarater and interrater reliability of the modified Thomas Test. J Bodyw Mov Ther. 2022 Jan;29:86-91. doi: 10.1016/j. jbmt.2021.09.014. Epub 2021 Oct 12. PMID: 35248293.
Neto WK, Soares EG, Vieira TL, Aguiar R, Chola TA, Sampaio VL, Gama EF. Gluteus Maximus Activation during Common Strength and Hypertrophy Exercises: A Systematic Review. J Sports Sci Med. 2020 Feb 24;19(1):195-203. PMID: 32132843; PMCID: PMC7039033.
Santana, Juan & Mcgill, Stuart & Brown, Lee. (2015). Anterior and Posterior Serape. Strength and Conditioning Journal. 37. 8-13. 10.1519/ SSC.0000000000000162.
Freeman S, Mascia A, McGill S. Arthrogenic neuromusculature inhibition: a foundational investigation of existence in the hip joint. Clinical Biomechanics. February 2013:28(2):171–177.


LOCAL CRYOTHERAPY IN ELITE FOOTBALL: THE COLD-HEARTED TRUTH
FEATURE / DR OLIVIA GREENHALGH, PHD
Introduction
Cryotherapy is an umbrella term which refers to any treatment that involves cooling the body or specific tissues to promote recovery and manage injury. The primary mechanism of cryotherapy is based on removing heat energy from the body to reduce tissue temperature. Reducing tissue temperature leads to physiological changes that can aid in reducing pain, managing inflammation, and accelerating recovery (Michlovitz, 1990; Nadler, Weingand, & Kruse, 2004).
From whole-body cryotherapy (WBC) to localised cold treatments, elite football clubs are increasingly incorporating cryotherapy into their recovery and injury management protocols. This article focuses on the use of local cryotherapy for injury management purposes, and the existing knowledge gaps in applying local cryotherapy effectively.
Clinical Guidelines
The Association of Chartered Physiotherapists in Sports and Exercise Medicine (ACPSM) introduced the ‘PRICE’ (Protection, Rest, Ice, Compression, Elevation) guidelines for acute soft tissue injury management in 2011 (Bleakley et al., 2011), later updated to ‘POLICE’ (Protection, Optimal Loading, Ice, Compression, Elevation) (Bleakley, Glasgow, and MacAuley, 2012). Cryotherapy is recommended within these guidelines, yet optimal protocols for temperature and dosage remain unclear (Selfe et al., 2020). Several factors related to the best methods for applying cryotherapy still need further investigation (see Figure 1).
Optimal level of simultaneous compression
Optimal
Defining ‘optimal’ local cryotherapy protocols
Frequency of treatments
Dosage (duration)
Figure
Interestingly, Dubois and Esculier (2019) introduced the acronym ‘PEACE & LOVE’ (Protection, Elevation, Avoid Anti-Inflammatories, Compression, Education & Load, Optimism, Vascularisation, Exercise) to address the sub-acute and chronic phases of tissue healing, unlike the earlier acronyms (PRICE and POLICE), which focused primarily on acute injuries. The authors noted that cryotherapy was excluded from this new framework due to insufficient high-quality evidence supporting its effectiveness for treating soft tissue injuries. While they acknowledged the analgesic benefits of cryotherapy, they also raised concerns about its potential to disrupt tissue repair and collagen synthesis. This has sparked discussions among clinicians about the possible negative effects of cryotherapy in sports healthcare (Long and Jutte, 2020). However, as the editorial by Dubois and Esculier (2019) lacks empirical data and support, further research is needed to confirm or challenge this proposed change in guidelines. More recently, a review by Racinais et al. (2024) critiques the common use of cryotherapy in sports medicine, noting limited evidence from human studies supporting benefits for tissue healing beyond pain relief. Pending further human research, the authors suggest that cryotherapy may be recommended within the first 6 hours post-injury to reduce pain and possibly haematoma, but it should be applied cautiously beyond 12 hours due to the lack of evidence and potential affects to tissue healing. It is clear that more human studies are needed to validate the physiological changes observed in previous animal studies.
Considering the variability of injuries, researchers have noted that a universal or ‘one size fits all’ cooling and compression protocol is unlikely to be effective for managing soft tissue injuries across the entire spectrum (Bleakley et al., 2011; Bleakley, Glasgow, and MacAuley, 2012). Furthermore, an individual’s response to thermal stress can vary based on several physiological factors (Figure 2). Fu et al. (2016) identified characteristics such as gender, skin type, and body fat percentage as influential in thermal responses to environmental conditions. As a result, there is an increasing recognition that a ‘personalised’ approach to intervention may yield better outcomes (Bleakley et al., 2011; Alexander et al., 2020; Selfe et al., 2020).
Factors affecting an individual’s response to thermal stress
Figure 2: Physiological factors affecting thermal response (Fu et al., 2016)
Breaking down the Protocols
i) Temperature
Skin temperature is often the main measure discussed when analysing the effectiveness of cryotherapy as the thermal receptors in the skin are the first site to respond to an external stimulus and can also help to monitor an adverse effect (such as skin burns).
The therapeutic objective of local cryotherapy is to reduce tissue temperature to a level that triggers beneficial physiological responses such as vasoconstriction, reduced nerve conduction, and decreased cellular metabolism. Achieving these responses hinges on precise temperature control, duration, and application technique. Research shows that cooling to a skin temperature (T sk) between 10-15°C optimally triggers these responses, with significant analgesic effects occurring below 13°C and a 50% reduction in cellular metabolism achieved at around 10-11°C (Bugai, 1975; Rivenburgh, 1992; Jutte et al., 2001).
However, the ideal therapeutic range was first proposed in 1992 and remains under review. While we know that cooling below 13°C provides effective pain relief, temperatures between 10-13°C may offer enhanced benefits. Current guidelines recommend not lowering T sk below 5°C to avoid ice burns, yet new devices with precision cooling capabilities could warrant studies exploring whether a tighter 6-10°C range could yield even better outcomes for injury management. Understanding the physiological changes at various temperatures can enable healthcare professionals to harness the full therapeutic potential of cryotherapy, while safely guarding against adverse effects like ice burns or nerve damage.
Advances in technology now allow for more precise control of skin temperature in cryotherapy, potentially unlocking enhanced therapeutic benefits. By enabling precise temperature management, these advancements may help clinicians optimise physiological responses, which are critical for effective
injury management. Enhanced precision also minimises the risk of adverse effects, allowing for safer, more efficient treatment that can be customised to each player’s specific needs. This capability could lead to a more refined and personalised applications of cryotherapy, aligning treatment variables with the type and severity of injury to maximise clinical outcomes. New advancement in technology devices offer the opportunity to control temperature and duration parameters. Thus, more research is required to define specific cryotherapy protocols for different injuries and individual characteristics, to enable a more personalised approach to optimise cryotherapy use in the future.
ii) Dosage
Cryotherapy cools deeper tissues through unidirectional heat transfer from the skin to the cold modality (Kennet et al., 2007). When applied, heat moves from warmer superficial tissues to the cold surface, causing deeper tissues to cool as they lose heat to the alreadycooled skin layer (Merrick et al., 2003). Even after removing the cold source, cooling continues as deeper tissues transfer heat to rewarm the skin (Zemke et al., 1998; Jutte et al., 2001). This extended cooling effect highlights the
importance of treatment duration and modality selection in injury management. Rewarming curves of T sk are usually an important indicator of the lasting effects of the treatment. An immediate return of T sk to baseline would suggest a superficial treatment.
The ideal treatment length is still debated due to variables such as injury type, individual response, and device specifications. Typically, in elite football, local cryotherapy sessions of 10 to 20 minutes are used, with approximately an hour between treatments to allow for rewarming. Longer durations are generally avoided to reduce the risk of adverse effects, time limitations and water/ice-based applications often struggle to maintain temperatures within the ideal therapeutic range for over 20 minutes. However, more consistent cooling is now possible through advanced cryotherapy devices, exploring tailored durations for specific injuries could enhance protocols in the future.
iii) Surface Area
The rate of heat transfer via conduction is affected by surface area, thermal conductivity, temperature of the surfaces and tissue thickness (Michlovitz, 1990). It
is common that once a player is injured, practitioners will cool the entire limb or a large proportion of the affected limb. Contemporary research has shown that cooling a smaller surface area, through a targeted cooling approach, may have therapeutic benefits as it can minimise adverse effects to muscle strength and proprioception, whilst achieving the desired effects for cooling in the specific area (Alexander et al., 2021b). However, the targeted approach is only possible once you are aware of the injury details and exact location so has practical limitations immediately post injury. Further research is needed to determine optimal surface areas to cool for different injury types, locations and individual characteristics.
iv) Modality
Football clubs invest heavily in technologies that promise to enhance performance, and cryotherapy is no exception. The allure of faster recovery, reduced injury lay off times, and improved player readiness is a powerful motivator.
For one, achieving and maintaining T sk within the ideal therapeutic temperature range is the main goal to induce the physiological changes desired.

Interestingly, the effectiveness of cryotherapy depends not only on how cold the treatment is but also on the duration and type of cooling used. Thermoelectric devices that can precisely regulate temperature and duration of the cold application, could allow for greater control in the physiological responses achieved compared to water/ice-based modalities. This allows clubs to tailor the cryotherapy treatment to an individual player’s needs, making recovery more efficient and effective.
Conclusion
• Local cryotherapy is crucial for managing football injuries, but optimal parameters like temperature, duration, and
References
modality need further refinement as requirements for different injuries and individuals may vary.
• Advanced devices enable personalised treatment, allowing clinicians to tailor cooling to specific injuries and individuals.
• A targeted cryotherapy approach shows promise in enhancing therapeutic effects and reducing risks, though more research is needed to define best practices.
• As football clubs invest in cryotherapy technology, refined protocols could better support injury recovery and players’ return to play.
Affiliations:
• Senior Research Associate at Lancaster University, Lancaster Medical School.
• Visiting Researcher at Manchester Metropolitan University (MMU).
• Previously at Swellaway Ltd, where I worked collaboratively with MMU on my PhD and KTP around the development of clinical interventions for knee injury management using ProMOTION EV1. Currently still provide adhoc support to Swellaway as a scientific advisor.
1. Alexander, J., Greenhalgh, O., Selfe, J. and Rhodes, D. (2021a) ‘Cryotherapy and Compression in Sports Injury Management: A Scoping Review’, International Journal of Therapy and Rehabilitation.
2. Alexander, J., Selfe, J., Greenhalgh, O. and Rhodes, D. (2021b) ‘Exploratory evaluation of muscle strength and skin surface temperature responses to contemporary cryotherapy modalities in sport’, Isokinetics and Exercise Science, pp. 1-9.
3. Bleakley, C. M., Glasgow, P., & MacAuley, D. (2012). Evidence-based ice treatment for acute soft tissue injury: the POLICE guidelines. British Journal of Sports Medicine, 46(3), 220-223.
4. Bleakley, C. M., McDonough, S. M., & McAuley, D. (2011). The use of ice in the management of acute soft tissue injury: a sys tematic review. British Journal of Sports Medicine, 45(4), 275-283.
5. Bugai, A. V. (1975). Temperature dynamics in cryotherapy: A study of the analgesic effects. Physical Therapy, 55(5), 25-31.
6. Dubois, J. & Esculier, J. F. (2019). The PEACE & LOVE framework: A new approach to managing soft tissue injuries. British Jo urnal of Sports Medicine, 53(21), 1347-1353.
7. Fu, F. H., Wong, E. K., & Wong, Y. (2016). Physiological factors influencing the thermal response to cold exposure. Clinical Rehabilitation, 30(7), 653-660.
8. Jutte, L. S., Bodo, T., & Choi, J. (2001). Understanding skin temperature response to cold applications: implications for in jury management. Journal of Athletic Training, 36(3), 291-296.
9. Kennet, J., Sullivan, J. P., & McMillan, C. (2007). The mechanism of heat transfer in cryotherapy applications: A review of current research. Journal of Sports Sciences, 25(3), 301-310.
10. Long, A. S., & Jutte, L. S. (2020). The potential negative impact of cryotherapy on tissue repair: A critical review. Sport s Medicine, 50(7), 1259-1272.
11. Michlovitz, S. L. (1990). Cryotherapy: The effectiveness of cold in the treatment of soft tissue injuries. Physical Therapy , 70(10), 740-748.
12. Merrick, M. A., & O’Connor, J. (2003). The effectiveness of cryotherapy in treating acute musculoskeletal injuries: A revie w. Athletic Training, 38(3), 231-236.
13. Nadler, S. F., Weingand, K., & Kruse, R. J. (2004). The physiologic effects of cryotherapy: A review of the literature. Arc hives of Physical Medicine and Rehabilitation, 85(1), 114-122.
14. Racinais, S., Dablainville, V., Rousse, Y., Ihsan, M., Grant, M.E., Schobersberger, W., Budgett, R. and Engebretsen, L., 20 24. Cryotherapy for treating soft tissue injuries in sport medicine: a critical review. British Journal of Sports Medicine, 58(20), pp.12151223. Available at: https://bjsm.bmj.com/content/58/20/1215
15. Rivenburgh, D. W. (1992). The impact of temperature on the healing process in cryotherapy. Journal of Rehabilitation Resear ch and Development, 29(2), 1-7.
16. Selfe, J., Thorpe, C., May, K. and Alexander, J. (2020) ‘Cryotherapy: physiology and new approaches (in: A Comprehensive Gu ide to Sports Physiology and Injury Management)’, pp. 79-96
17. Zemke, J. E., Tyndall, J. E., & Miller, J. L. (1998). Effects of body fat on the response of deeper tissues to cryotherapy. Journal of Orthopaedic & Sports Physical Therapy, 28(2), 128-134.

A
RETURN TO PERFORMANCE PATHWAY – FROM THE ONSET OF INJURY BACK TO PERFORMANCE
FEATURE / ANDREW MITCHELL, MSC, MSC, BSC (HONS),
MARK PALMER, BHSC (HONS), MO GIMPEL, BSC (HONS), HCPC
Introduction
How to return to performance (RTP erf) after injury is unclear. 9 A lack of consensus on valid objective criteria, and inconsistency in thresholds to achieve prior to return to play (RTP lay) can lead to inadequate rehabilitation, premature RTP lay and reinjury. 20,37 This RTP erf pathway offers a framework and recommendations for a multidisciplinary team (MDT) on how
to recondition an injured player from the onset of injury, back to performance (Figure 1). The pathway design is timeindependent and provides clear phases with exit criteria for mild, moderate or severe injuries to facilitate informed decisions. Each phase is named to provide a common language to improve day-to-day communication between practitioners, players and coaches. 2
`From the Onset of Injury Back to Performance´
Diagnosis and Planning Phase
Once injured, players can experience extreme and sometimes life-changing physical and emotional distress. Physical treatment and psychological support are vital while an accurate diagnosis is made, with the medical team also taking
RETURN TO PERFORMANCE PATHWAY



into account factors such as the player’s age, severity of injury, underlying medical history and psychosocial situation. Centring the plan around the player by providing full transparency about the pathway and phases they will go through will increase their trust in the process.18 Trust can also be fostered by informing and involving the player’s support team (family, friends, peers and any external practitioners they may use)
5-10m Passing / In-place Headers Introduction to COD, ACCs & DECs (1m, 2m, 4m Drills)

about management options. Once the RTPerf plan has been agreed, specific roles and responsibilities can be organised so positive relationships between the player and members of the MDT are initiated from the outset.31 As news about injured professional players often becomes public, the precision of the vocabulary used at this phase also helps to set expectations and manage media pressure on the player (Figure 1). MAXIMUM SPEED & POSITIONAL DRILLS

Intensive / Extensive… <85% Max Speed
<40m Passing, 5-10m Headers,Contact Intro
COD, ACCs & DECs <18m Drills<85%Max
Aerobic / Anaerobic Conditioning
<85% Volume (m) of Total Match Distance
REACTIVE STRENGTH PROFILING
Positional…
>85% Max Speed
Shooting / Clearing / Positional Headers / Contact Drills
COD, ACCs & DECs
Positional >85%Max
Positional Conditioning
>85% Volume (m) of Total Match Distance
Graded Exposure… Warm-ups / Passing Drills /Phases of Play Neutral Player / Partial to Full Contact SSG / MSG / LSG
Physical & Technical ‘Top ups’
Achieve Normal Weekly Loads
RESUME TEAM GYM SESSIONS & MONITOR INJURY SPECIFIC CRITERIA AS REQUIRED
Acute Phase - Acute Management and Modified Conditioning
Initially, it is necessary to protect all injured sites or surgically repaired structures to enable the formation of scars and healing to occur.14 Cryotherapy can reduce pain and swelling which through neuromuscular inhibition causes muscle atrophy and reduced proprioception. Exercise aims to restore range of motion, minimise atrophy and regain neuromuscular control. Increased
Graded Exposure…
Progressive Increase of Match Minutes <30mins <60mins 60-90mins
Practice Games
Development Squad Games First Team Games
CONTINUE TEAM GYM SESSIONS & MONITOR INJURY SPECIFIC CRITERIA AS REQUIRED
RETURN TO PERFORMANCE THE PLAYER IS PERFORMING AT THEIR PREINJURY LEVEL (OR HIGHER)
MONITOR PLAYER IN ALIGNMENT WITH CLUB PHILOSOPHY
`Consider Previous Injury History´
Figure 1: The return-to-performance pathway - `from the onset of injury back to performance.´
Abbreviations: ACCs, accelerations; CMJ, countermovement jump; COD, change of direction; DECs, decelerations; Hams, hamstrings; LSG, large-sided games; M, metres; Max, maximum; MSG, medium-sided games; Mins, minutes; Ms, milliseconds; NWB, non-weight bearing; Quads, Quadriceps; RFD, rate of force development; SL, single leg; SSG, small-sided games.
pain (>2-4/10 on a visual analogue scale, where 0 = no pain, 10 = worst pain imaginable) or swelling levels (using a stroke test for the knee or limb girth measurements [CMS] for other injuries) suggests the stress on the injury is not well tolerated and excessive.15 Excessive loading can lead to poorly healed structures that pose clinical problems such as pain, instability, and weakness later in the pathway. Also in this phase when it is safe, contralateral limb strength and plyometric training should be encouraged as this reduces detraining and has cross education effect that enhances recovery of the injured limb.24 Off-feet conditioning that off-loads the injured tissue (e.g. seated battle ropes, boxing, upper body circuits, core and arm bike) helps to maintain player fitness, motivation and reduce the feeling of isolation.25
Gym Phase 1 – Early Loading and Normal Movement
This phase aims to start early loading and restore normal movement patterns. Proficiency in fundamental weightbearing exercises (e.g. squats, lunge patterns, heel raises, single leg [SL] balance exercises) and a pain-free gait pattern are the primary goals.4 Mild injuries can start immediately in the gym, but for moderate to severe injuries the
Supplementary Exit Criteria to Support Each Phase of the Return-to-Performance Pathway
Must not experience an increase in injury specific pain (>2-4/10 on a visual analogue scale)
Must not experience an exacerbation of swelling levels suggesting excessive loading
Must demonstrate movement proficiency
Assessed visually to ascertain there is no loss of balance, contralateral hip drop, ipsilateral knee valgus, or any excessive trunk movement
Must not experience fear
Must not experience anxiety
Utilising of the global rating scale from 0 to 100% on a daily and sessional basis
A score of 0% being the feeling of an inability to start the next progression and 100% being complete confidence to start the next progression
Experience suggests the premature exit of a phase leads to recurrent episodes of swelling, increases in pain, and compensatory movement strategies reducing players’ well-being and overall confidence.
*During the return-to-performance pathway the specific phase criteria need to be achieved along with the supplementary criteria described here.
Table 1: The supplementary clinical, physical, and psychological criteria used to safely progress through the phases of the return-to-performance pathway - `from the onset of injury back to performance.´

process may begin in the pool to restore neuromuscular control and coordination. Mastery of bilateral body weight (BW) exercises maintains the ground reaction force (GRF) at <1 × BW through each limb before progressing these to split squats, lunge patterns (forward and backward), and SL exercises. Finally, step-ups and SL squats progressively increase the GRF through the working limb to <1.2 x BW.6 This systematic progression of exercises ensures the player can absorb and produce force in the aforementioned exercises in preparation for the gait cycle. To support these criteria in this and all subsequent phases, the additional physical, clinical and psychological criteria listed in Table 1 are used.26
Gym Phase 2 – Reconditioning Pathways
Gym Phase 2 is an opportunity to develop qualities such as strength, capacity, injury-specific qualities, and a theme of movement retraining (plyometric, running preparation, and indoor ball skills pathways).26 Each of the reconditioning pathways is progressed in a systematic way. For example, the capacity reconditioning pathway increases the repetitions and sets, whereas the strength reconditioning pathway creates
progressions by reducing repetitions and increasing weight accordingly. For the running preparation pathway, the number of single-foot ground contacts or the percentage of BW prescribed on the antigravity treadmill can be easily graded and progressed. Similarly, the techniques are advanced in a step-by-step fashion for the plyometric and indoor ball skills pathways as the complexity of the movements is progressed.29 Mild injuries (4-7 days), can complete these progressions in minutes or one solitary session as opposed to moderate (8-28 days) and severe injuries (>28 days),11 where progressions may require multiple sessions to achieve competency.
Gym Phase 3 – Return to Running
Once injured, a classic question players ask is “when I can start running on the grass?” Gym Phase 3 objectively profiles a player to determine their readiness to return to running (RTRunning). Table 2 demonstrates exercise examples from the RTRunning criteria checklist and outlines how the reconditioning pathways of Gym Phase 2 are objectively profiled in Gym Phase 3.26
At this point, the Performance Symmetry Index (PSI) is used to help interpret the player’s data (Box 1).26 For mild injuries, pathways can be prioritised and only the relevant criteria need to be profiled. For moderate and severe injuries, however, it is recommended all pathways are profiled. In reality, the RTRunning criteria checklist needs to be flexible and reasoned, as low-grade muscle injuries should progress to running earlier than high-grade injuries. However, consideration of pathways and potential deficits should not be overlooked.
Grass Phase 1 – Reloading and Technical Reintroduction
Grass Phase 1 has two clear objectives. Firstly, every player, regardless of position, needs a period of technical re-introduction and reloading to increase their confidence and aerobic fitness levels on the grass. Secondly, to restore the necessary power criteria (Table 3) to start the high-speed running (HSR) and agility drills in Grass Phase 2. On the grass, players begin linear running or low-intensity dribbling circuits (e.g. Hoff circuits) with a high degree of control, as these are performed at running speeds ≤65% of their maximal speed.36 By limiting the distances (≤4m) of sportspecific skills, any exposure to HSR or high-intensity accelerations (ACCs) and decelerations (DECs) is limited.13 Passing (0-10m), ball manipulation and in-place heading drills are introduced, which is a natural progression from the exercises completed during the indoor ball skills pathway.29
Gym Phase 3 - Return to Running `Criteria Checklist’
CRITERIA
CAPACITY
STRENGTH
Maximum Strength
STRENGTH
Isokinetic Dynamometry
MOVEMENT RETRAINING
Plyometric
a) Hop Battery
b) Forceplate Jumps
MOVEMENT RETRAINING
Running Preparation
a) 1000 Single Foot Ground Contacts
b) Antigravity Treadmill Running
MOVEMENT RETRAINING
Indoor Ball Skills
Completion of 2 sets to fatigue (Single Leg)
1) SL Squat
2) SL Hamstring Bridge in 90°
3) SL Hamstring Bridge in 30°
4) SL Heel Raise (Straight Leg - Gastrocnemius
Bias)
5) SL Heel Raise (Knee Flexed - Soleus Bias)
3-4 sets x 3-5 repititions. Exercise examples from;
Anterior Chain - Leg press, RFESS, Knee extenstion
Posterior Chain - Nordics, SL RDL, SL Hams bridge Calf Complex - Gasctrocnemius / Soleus heel raises
3 Speed Profiling - Quads/Hams;Con:Con
1 x 5 repetitions at 60°/s each limb
1 x 10 repetitions at 180°/s each limb
1 x 15 repetitions at 300°/s each limb
a) Hop Battery 1 x 3;
1) SL Horizontal, Medial, Lateral Hop
2) SL Triple Hop
b) Forceplate Jumps 1 x 3;
1) DL CMJ and Drop Jumps
2) SL CMJ and Drop Jumps
a) 1000 Single Foot Ground contacts in a variety of exercises to replicate running mechanics. Exercise examples from; A Skips, B Skips, Butt Kicks, High Knees, Lateral Shuffles, Ankle Jumps, In/out Heel Taps,
b) 95% BW / 1-2mins / 4-6 repetitions / 8-12km/h
Player completes a game of teqball (head tennis across a table tennis table)
Injury dependent. Example exercises;
*SL Isometric profiling of hamstrings (Supine in 90° or 30° knee flexion)
*SL Isometric profiling of Soleus (Seated knee in 90° flexion pushing against fixed bar)
INJURY SPECIFICS
≈100% of Performance Symmetry
Index
1) 25 repetitions
2) 30 repetitions
3) 30 repetitions
4) 35 repetitions
5) 35 repetitions
>90% Performance Symmetry Index
Anterior chain SL leg leg press - 1.5 x BW
Posterior chain nordic - 425 Newtons Calf complex - SL heel raise 80% BW
>90% Performance Symmetry Index
1) PT of Quadriceps at 60°/s (3 x BW)
2) PT of Hamstrings at 60°/s (1.8 x BW)
3) Total Work of Quadriceps at 300°/s
4) Total Work of Hamstrings at 300°/s
>80% Performance Symmetry Index
a) Session completion
b) Session completion
Session completion
Case by case basis
Individualised metrics to achieve
*SL Isometric profiling of Gastrocnemius (Stood in rack, pushing against fixed bar)
*Time to stabilisation hops
*Outlier type exercises (Curtsy squat for knee LCL or ankle syndesmosis) ´
*Exercises with a rotational bias
Table 2: Demonstrates exercise examples from the return to running criteria checklist (Gym Phase 3). Abbreviations: BW, body weight; CMJ, countermovement jump; DL, double leg; LCL, lateral collateral ligament; ms; metres per second; PT, peak torque; RDL, roman deadlift; RFESS, rear foot elevated split squat; RM, repetition maximum; SL, single leg.
The Performance Symmetry Index defined.
I. Restore pre-injury, pre-season, or ideally, previous metrics from longitudinal limb monitoring.
II. In the absence of these data, aim to recover normative data from a comparative cohort.
III. In the absence of these data, a limb symmetry index may be used, but with caution due to deconditioning of the contralateral limb or positive adaptation of the contralateral limb during the rehabilitation process.
IV. In all cases, an individualized and contextual interpretation of the metrics must be considered from a clinical and performance perspective.
Power Profiling (>250ms)
In the gym, appropriate exercises (examples in Table 3) are introduced before and / or after grass sessions to enhance power development. These expose the player to the slow stretch shortening cycle (SSC), with the triple hop being the most explosive with (ground contact times) GCTs of around >300 milliseconds. 21 Reducing repetitions and sets encourages explosive movements with maximal intent, which can be further enhanced by appropriate coaching. Regular (weekly or fortnightly at most) profiling of PSI in the vertical (SL countermovement jump), 27,28 horizontal (SL horizontal hop, SL triple hop, and SL crossover hop), and frontal planes (medial and lateral hops) 10 is encouraged, as these power criteria act as injury and performance prerequisites for Grass Phase 2.
Grass Phase 2 – High-Speed Running and Agility Drills
Grass Phase 2 has two distinct aims. Firstly, players are required to run at high speeds and complete intensive agility drills. Secondly, restoration of the necessary reactive strength qualities (Table 3) in order to begin the maximum speed and positional drills in Grass Phase 3. On the grass, due to the increased physical demands, players complete extensive (plus volume-based drills) and intensive sessions on separate days. For intensive sessions, it has been shown that progressively increasing the drill distance from 4m to 18m increases the intensity of these types of ACC and DEC actions. 13 Passing distances (10 to 20 to 30 to 40m) and heading distances (0-5 to 5-10m) are increased to replicate more sport-specific actions. 3 During extensive sessions, the first part of the session focuses on HSR as speed (≤85% maximum speed) and volume (% of total match HSR/ Sprint metres) gradually increase. Later in the same session, the player accumulates further volume (total metres) as total session distances are increased (≤85% total match distance). 26
PEAK SPEED (km/h)
HSR METRES (>19,8 km/h)
SPRINT METRES (>25,2 km/h)
ACCs (+m/s-2) and
volume (metres) in sessions from 3 to 4 to 5 to 6km as
to Box runs, 100m pitch runs, 500m runs, 1km runs and / or dribble circuits (prescribed running intensities from aerobic Þtness testing)
Player limited to jogging style in all running exercises
No of Medium (2-3m/s-2)
(-m/s-2) Total Volume Introduction to ACCs and DECs patterns in a 1 x 1m, 2 x 2m and a 4m x 4m square
No of High (3-4m/s-2)
No of Very High (>4m/s-2)
PEAK Intensity
GYM BASED
HOP BATTERY
FORCEPLATE JUMPS / ISOMETRICS
ISOKINETIC DYNAMOMETRY
Limit the ACCs and DECs drill distances to 4m will limit the peak intensities to <65%
Practice all hop battery variations plus, Hurdle Hops - Horizontal, Medial and Lateral Broad Jumps - DL and SL
Practice all forceplate jump variations plusto enhance both the hop battery and forceplate jumps further power based jumps are encouraged, e.g, squat jumps, lunge jumps, rear foot elevated jump positions and also split stance jumps etc.
Practice of the IKD at test speeds (180°/s ± 30°/s) Plus - practice of power exercises listed above
Reactive Strength Profiling (<250ms)
Restoration of appropriate reactive strength criteria (examples in Table 3) is targeted by the practitioner before and or after grass sessions during this phase. The player must demonstrate the fast SSC as the GCTs for these exercises are approximately <0.25 milliseconds.12 Progressions can be enhanced by adding height, distance and movement variability while continuing to reduce GCTs. Profiling the PSI in the vertical (SL drop jump and 10/5 jumps),34 and horizontal (6m timed hop) planes remain the priority. In addition, the isometric rate of force development of the quadriceps, (using the isokinetic dynamometer),7 hamstrings,35 and calf complex (using the force plates)5,32 can be profiled in players (Table 3). As
Grass Phase 3 involves intensities ≥85%, an exponential load is placed on the tissues,16 and in the authors’ experience, an injured player must have met the Grass Phase 2 metrics and the gym-based reactive strength metrics listed in Table 3 in order to be able to safely perform maximum speed and positional drills.
Grass Phase 3 – Maximum Speed and Positional Drills
During this phase players must complete maximum speed and positional drills prior to resuming team training in Grass Phase 4. At the same time, players continue to address any individualised physical ‘outliers’ that are yet to be achieved (examples in Table 3). In
volume Increase volume (metres) in sessions from 6 to 7 to 8km as tolerated
Box to Box runs, 100m pitch runs, 500m runs, 1km runs and / or dribble circuits (prescribed running intensities from aerobic Þtness testing)
Step by step increase in running speeds to <85% of peak speed
Prescribed distances to achieve desired HSR metres, e.g, a pitch width run (68m) in 13s provides 20m (approx) of high speed running with a peak speed of 21km/h
Prescribed distances to achieve an introduction into sprint metres, e.g, a box to box run (72m) in 11s provides 20m (approx) of sprint metres with a peak speed of 26km/ h
Introduction to ACCs and DECs patterns progressing through 8m, to 12m to 18m distances
ACCs ACCs and DECs patterns in a 4 x 4m square
ACCs and DECs patterns progressing from 8m, to 12m to 18m distances
- -
Player encouraged to achieve high ACCs and DECs <85% of peak intensity
Introduction to exercises against a tackle bag / gym ball
Run and heading techniques in 5-10m distances
and Progress variety of kicking actions as able from 10-20-30-40m
Hop21
Practice all plyometric variations with an emphasis on reduced GCTs.
Hurdle Bounds - Horizontal, Medial and Lateral
Practice all drop jump forceplate variations plus - to enhance both the hop battery and forceplate jumps with a reactive strength emphasis are encouraged as previously stated
***To enhance isometrics ‘fast and hard’ 1s contraction times are used
Practice of the IKD at test speeds (180°/s ± 30°/s)
Plus - practice of reactive strength exercises listed above
<85% of individualised match volume
<85% of individualised peak speed
<66% of total match volume
<33% of total match volume (as long as 85% of peak speed is not exceeded)
<66% of total match volume
<66% of total match volume
Safe completion of medium intensity ACCs and DECs
<66% of total match volume
Safe completion of medium intensity ACCs and DECs
<85% of individualised peak speed
Controlled
<66% of total match volume
Safe completion of all kicking actions <40m
1. SL 6m Timed Hop
2. SL Drop Jump
3. SL 10/5 Jumps (pogos)
Isometrics RFD at 100ms
4a. Hamstrings (Supine lying hip/. knee at 90°)
4b. Soleus (Seated knee at 90°) 4c. Gastrocnemius (Stood ankle at plantargrade)
5a. PT Quadriceps at 0.18ms 5b. PT Hamstrings at 0.18ms
Increase volume (metres) in sessions from 8 to 9 to 10km as tolerated All variations of runs previously mentioned
Player encouraged to run at maximum speeds >85% of peak speed
Prescribed distances and times to achieve required HSR metres, e.g, box to box runs or more positional based runs.
Prescribed distances and times to achieve required sprint metres, e.g, a runway (50m) in <8s provides 35m (approx) of sprint metres.
Completion of all ACCs and DECs volumes through positional drills in unlimited drill distances
ACCs and DECs patterns in a 4 x 4m square
ACCs and DECs patterns progressing through 8m, to 12m to 18m distances33
Positional drills to achieve very high ACC and DEC intensities
Player encouraged to achieve maximum ACCs and DECs >85% of peak intensity
Progression of positional blocking, tackling, colliding against colleagues
Defensive headers or attacking headers depending on positional requirements
Positional requirements, e.g. Shooting / clearing drills / long passing drills
>85% of individualised match volume
>85% of individualised peak speed
>85% of individualised match volume e.g. such as centre forwards running into the penalty area to score goals or defenders running back into the penalty area to defend crosses
>85% of individualised match volume
>85% of individualised match volume
>85% of total match volume
Safe completion of medium intensity ACCs and DECs
>85% of total match volume
Safe completion of high intensity ACCs and DECs
>85% of total match volume
Safe completion of very high intensity ACCs and DECs
>85% of individualised peak speed
Safe completion of contact drills
Safe completion of required positional heading exercises
Safe completion of required positional ball exercises
‘Outliers’
CLINICAL EXAMPLES
- ACLR (Hamstring Graft) - ACHILLES TENDON RUPTURE
Despite restoring through range hamstring strength, inner range (80-100° of knee ßexion) strength in the prone position can still be deÞcit
Exercises - Isolated inner range (80-100° of knee ßexion) hamstring isometrics to increase tendon stiffness and strength in this position
1. IKD inner range hamstring proÞling with short 1-2s and longer 3-5s durations
Despite seemingly restoring plantarßexion strength and plantar ßexion capacity, players can still lack heel raise excursion height
Exercises - isometrics focusing on this Þnal part of the heel excursion to increase tendon stiffness and strength
2.Forceplate end of range plantarßexion proÞling with short 1-2s and longer 3-5s durations
Table 3: Highlights the minimum criteria required to exit Grass Phases 1-3 prior to starting Grass Phase 4 (Return to Training).
Abbreviations: ACCs, accelerations; ACLR, anterior cruciate ligament reconstruction; CMJ, countermovement jump; DECs, decelerations; DL, double leg; GCTs, ground contact times; IKD, isokinetic dynamometry; PT, peak torque; RDL, roman deadlift; RFESS, rear foot elevated split squat; SL, single leg.
Grass Phase 3, the drills are match related (chaotic and highly variable) and can be enhanced with the support of a technical coach or two or three additional players.36 Positional heading and controlled collision drills with the physiotherapist and peers are implemented to build confidence in preparation for the next phase. The addition of uncontrolled external stimuli is a critical factor in skill development and cognitive overload. Peak speed (>95% of maximum speed) and volume of speed (>85% of
total match HSR/sprint metres) must be reproduced, ensuring the player is ready and prepared for the demands of team training.23 Equally, the peak intensity (>95% of maximum) and volume (>85% of total match) of ACCs and DECs must be safely achieved before exiting this phase.
Injury Specific Gym Criteria still to be Achieved - `Outliers´
Although key physical qualities such as strength, power and reactive strength
have been restored, it is not uncommon for a player to still have injury-related criteria to achieve or previous medical deficits (e.g. footballer’s ankle, femoralacetabular impingement or pre-injury deficits) that were initially highlighted in the initial diagnosis and planning phase. For instance, after anterior cruciate ligament (ACL) reconstruction (hamstring graft), inner range hamstring isometric strength (80-100° knee flexion) can often still be reduced. 19 By contrast, ankle
excursion height can be reduced after an Achilles tendon rupture even if all other performance metrics are met. 33 These could go unnoticed and special attention must be paid to their recovery to help the player achieve a true RTP erf
Grass Phase 4 – Return to Training
Players are reintroduced to team warmups, passing drills and phases of play. Often, players start as neutral players (free from contact with opponents) and progress from partial to full contact (Figure 1).30 The cumulative load achieved during the first three grass phases, balanced with the expected training load in Grass Phase 4, reduces excessive overload that can predispose the player to further injury.23 However, the competitive environment, training with peers, and input from the coaches are psychologically very different from the first three grass phases and undoubtedly leads to cognitive overload. This causes an increased sympathetic drive and subsequent increase in heart rate. Sessional monitoring of heart rates, GPS and perceived rates of exertion need to be monitored carefully,17 as the physical training load may need to be plateaued initially to compensate for this overload and increased risk of injury.
At this point, it is vital `expectation setting´ has been shared and communicated between all key stakeholders, notably the
References
players, coaches, and members of the MDT.8 Expectations maybe different, so it is crucial they are aligned. In Grass Phase 4, the medical input is less as the player has met the criteria listed in Table 2. The performance team (football coaches, physical trainers) now judge the physical capabilities and the player must also voice their level of confidence and readiness to transition to play using the global assessment scale (Grass Phase 5).22 From experience, if there is a malalignment here and Grass Phase 4 is prematurely exited, the player will enter match play with a 50% greater chance of reinjury in their first match back.1
Grass Phase 5 - Return to Playing
In Grass Phase 5, players are reintroduced to competitive match play and continue to be monitored against gym-based criteria (Tables 2 and 3). Players failing to fulfil the criteria inevitably lack confidence in their injury and also their ability to perform at the highest level, in contrast to players who have restored their physical criteria and psychological confidence. Mild injuries may play 90 minutes in their first game back (Figure 2), whereas for severe injuries, all criteria should be met, and a stepwise increase in match minutes is recommended.2
Strategically using development squad matches restores match minutes and
confidence, as RTPlay is the greatest psychological challenge in the RTPerf pathway. Injury risk is higher in the first game (47 per 1000 hours) than in match play in general (25 per 1000 hours) compared to training incidence (4.1 per 1000 hours);1,11 so this balance requires careful attention on a case-by-case basis.
Grass Phase 6 – Return to Performance
To achieve a true RTPerf the player is now performing at their previous injury level (or higher), with unrestricted availability. This is supported by the superior gymbased and match outputs which further supports this observation. Conversely, longitudinal observation may suggest severely injured players may occasionally experience reduced match availability and technical performance due to their injury.26
Summary
This RTPerf pathway offers objective criteria and thresholds to be achieved from the onset of injury back to performance. The clarity of the terminology surrounding the phases helps to improve communication between key stakeholders throughout the injury process. The RTPerf pathway can be implemented for mild, moderate, or severe injuries, with evidence-based criteria for each phase to help inform decisions and progress.
1. Bengtsson H, Ekstrand J, Waldén M, Hägglund M. Few training sessions between return to play and first match appearance are associated with an increased propensity for injury: a prospective cohort study of male professional football players during 16 consecutive seasons. Br J Sports Med. 2020;54(7):427-432. doi:10.1136/bjsports-2019-100655
2. Buchheit M, King R, Stokes A, Lemaire B, Grainger A, Brennan D. Return to play following injuries in pro football: insights into the real-life practices of 85 elite practitioners around diagnostics, progression strategies and reintegration processes. Sports Performance & Science Reports. 2023;(Jan):v1. doi:https://sportperfsci.com/wp-content/up- loads/2023/01/SPSR180_Buchheit.pdf
3. Buckthorpe M, Della Villa F, Della Villa S, Roi GS. On-field Rehabilitation Part 2: A 5-Stage Program for the Soccer Player Focused on Linear Movements, Multidirectional Movements, Soccer-Specific Skills, Soccer-Specific Movements, and Modified Practice. J Orthop Sports Phys Ther. 2019;49(8):570-575. doi:10.2519/jospt.2019.8952
4. Buckthorpe M, Tamisari A, Villa FD. A ten task-based progression in rehabilitation after ACL reconstruction: from post-surgery to return to play –a clinical commentary. Intl J Sports Phys Ther. 2020;15(4):611-623. doi:10.26603/ijspt20200611
5. Burgess KE, Connick MJ, Graham-Smith P, Pearson SJ. Plyometric vs. isometric training influences on tendon properties and muscle output. J Strength Cond Res. 21(3):986-989.
6. Comfort P, Jones PA, Smith LC, Herrington L. Joint Kinetics and Kinematics During Common Lower Limb Rehabilitation Exercises. Journal of Athletic Training. 2015;50(10):1011-1018. doi:10.4085/1062-6050-50.9.05
7. Davies GJ, Riemann B, Ellenbecker T. Role of Isokinetic Testing and Training After ACL Injury and Reconstruction. In: Noyes FR, Barber-Westin S, eds. ACL Injuries in the Female Athlete. Springer Berlin Heidelberg; 2018:567-588. doi:10.1007/978-3-662-56558-2_24
8. Dijkstra HP, Pollock N, Chakraverty R, Ardern CL. Return to play in elite sport: a shared decision-making process. Br J Sports Med. 2017;51(5):419420. doi:10.1136/bjsports-2016-096209
9. Draovitch P, Patel S, Marrone W, et al. The Return-to-Sport Clearance Continuum Is a Novel Approach Toward Return to Sport and Performance for the Professional Athlete. Arthroscopy, Sports Medicine, and Rehabilitation. 2022;4(1):e93-e101. doi:10.1016/j.asmr.2021.10.026
10. Ebert JR, Du Preez L, Furzer B, Edwards P, Joss B. Which Hop Tests Can Best Identify Functional Limb Asymmetry in Patients 9-12 Months After Anterior Cruciate Ligament Reconstruction Employing a Hamstrings Tendon Autograft? International Journal of Sports Physical Therapy. 2021;16(2):393-403. doi:10.26603/001c.21140
Figure 2: The application of the return-to-performance pathway - `from the onset of injury back to performance´ illustrated by two case study examples. Abbreviations: ACL, anterior cruciate ligament; LCL, lateral collateral Ligament; Regen, regeneration; Wks, weeks.
11. Ekstrand J, Hagglund M, Walden M. Injury incidence and injury patterns in professional football: the UEFA injury study. British Journal of Sports Medicine. 2011;45(7):553-558. doi:10.1136/bjsm.2009.060582
12. Flanagan EP, Comyns TM. The Use of Contact Time and the Reactive Strength Index to Optimize Fast Stretch-Shortening Cycle Training. Strength & Conditioning Journal. 2008;30(5):32-38. doi:10.1519/SSC.0b013e318187e25b
13. Harper DJ, McBurnie AJ, Santos TD, et al. Biomechanical and Neuromuscular Performance Requirements of Horizontal Deceleration: A Review with Implications for Random Intermittent Multi-Directional Sports. Sports Med. 2022;52(10):2321-2354. doi:10.1007/s40279-022-01693-0
14. Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring Strain Injuries: Recommendations for Diagnosis, Rehabilitation, and Injury Prevention. J Orthop Sports Phys Ther. 2010;40(2):67-81. doi:10.2519/jospt.2010.3047
15. Herrington L, Myer G, Horsley I. Task based rehabilitation protocol for elite athletes following Anterior Cruciate ligament reconstruction: a clinical commentary. Physical Therapy in Sport. 2013;14(4):188-198. doi:10.1016/j.ptsp.2013.08.001
16. Higashihara A, Ono T, Kubota J, Okuwaki T, Fukubayashi T. Functional differences in the activity of the hamstring muscles with increasing running speed. Journal of Sports Sciences. 2010;28(10):1085-1092. doi:10.1080/02640414.2010.494308
17. Kelly DavidM, Strudwick AnthonyJ, Atkinson G, Drust B, Gregson W. The within-participant correlation between perception of effort and heart ratebased estimations of training load in elite soccer players. Journal of Sports Sciences. 2016;34(14):1328-1332. doi:10.1080/02640414.2016.1142669
18. King J, Roberts C, Hard S, Ardern CL. Want to improve return to sport outcomes following injury? Empower, engage, provide feedback and be transparent: 4 habits! Br J Sports Med. 2019;53(9):526-527. doi:10.1136/bjsports-2018-099109
19. Konrath JM, Vertullo CJ, Kennedy BA, Bush HS, Barrett RS, Lloyd DG. Morphologic Characteristics and Strength of the Hamstring Muscles Remain Altered at 2 Years After Use of a Hamstring Tendon Graft in Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44(10):2589-2598. doi:10.1177/0363546516651441
20. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946-951. doi:10.1136/bjsports-2015-095908
21. Lloyd RS, Oliver JL, Kember LS, Myer GD, Read PJ. Individual hop analysis and reactive strength ratios provide better discrimination of ACL reconstructed limb deficits than triple hop for distance scores in athletes returning to sport. The Knee. 2020;27(5):1357-1364. doi:10.1016/j. knee.2020.07.003
22. Logerstedt D, Di Stasi S, Grindem H, et al. Self-Reported Knee Function Can Identify Athletes Who Fail Return-to-Activity Criteria up to 1 Year After Anterior Cruciate Ligament Reconstruction: A Delaware-Oslo ACL Cohort Study. J Orthop Sports Phys Ther. 2014;44(12):914-923. doi:10.2519/ jospt.2014.4852
23. Malone S, Owen A, Mendes B, Hughes B, Collins K, Gabbett TJ. High-speed running and sprinting as an injury risk factor in soccer: Can welldeveloped physical qualities reduce the risk? Journal of Science and Medicine in Sport. 2018;21(3):257-262. doi:10.1016/j.jsams.2017.05.016
24. Manca A, Dragone D, Dvir Z, Deriu F. Cross-education of muscular strength following unilateral resistance training: a meta-analysis. Eur J Appl Physiol. 2017;117(11):2335-2354. doi:10.1007/s00421-017-3720-z
25. Mitchell A. The psychology of the athlete – the physiotherapist’s perspective. In: Psychologically Informed Physiotherapy: Embedding Psychosocial Perspectives within Clinical Management. 1st ed. Elsevier Saunders; 2017:162-187.
26. Mitchell A, Gimpel M. A Return to Performance Pathway for Professional Soccer: A Criteria-based Approach to Return Injured Professional Players Back to Performance. JOPST-Open. 2024;May:166-178. doi:doi.org/10.2519/josptopen.2024.1240
27. Mitchell A, Holding C, Greig M. Factors influencing optimum countermovement jump performance and movement strategy in Championship professional football players: implications for player profiling. Research in Sports Medicine. 2022;30(1):30-40. doi:10.1080/15438627.2020.1860049
28. Mitchell A, Holding C, Greig M. The Influence of Injury History on Countermovement Jump Performance and Movement Strategy in Professional Soccer Players: Implications for Profiling and Rehabilitation Foci. Journal of Sport Rehabilitation. 2021;30(5):768-773. doi:10.1123/jsr.2020-0243
29. Mitchell A, Waite O, Holding C, Greig M. The Development of a Return to Performance Pathway Involving A Professional Soccer Player Returning From A Multi-Structural Knee Injury: A Case Report. International Journal of Sports Physical Therapy. 2023;18(2). doi:10.26603/001c.73317
30. Owen A, Wong D, Paul D, Dellal A. Physical and Technical Comparisons between Various-Sided Games within Professional Soccer. Int J Sports Med. 2013;35(04):286-292. doi:10.1055/s-0033-1351333
31. Podlog L, Dimmock J, Miller J. A review of return to sport concerns following injury rehabilitation: Practitioner strategies for enhancing recovery outcomes. Physical Therapy in Sport. 2011;12(1):36-42. doi:10.1016/j.ptsp.2010.07.005
32. Rhodes D, Jeffery J, Brook-Sutton D, Alexander J. Test-Retest Reliability of the Isometric Soleus Strength Test in Elite Male Academy Footballers. International Journal of Sports Physical Therapy. 2022;17(2). doi:10.26603/001c.31047
33. Silbernagel KG, Nilsson-Helander K, Thomeé R, Eriksson BI, Karlsson J. A new measurement of heel-rise endurance with the ability to detect functional deficits in patients with Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):258-264. doi:10.1007/s00167-0090889-7
34. Stratford C, Dos’Santos T, McMahon JJ. Comparing drop jumps with 10/5 repeated jumps to measure reactive strength index. Professional Strength & Conditioning. 2020;Summer(57):23-28.
35. Taberner M, Cohen DD. Physical preparation of the football player with an intramuscular hamstring tendon tear: clinical perspective with video demonstrations. Br J Sports Med. 2018;52(19):1275-1278. doi:10.1136/bjsports-2017-098817
36. Taberner M, Van Dyk N, Allen T, et al. Physical preparation and return to performance of an elite female football player following ACL reconstruction: a journey to the FIFA Women’s World Cup. BMJ Open Sport Exerc Med. 2020;6(1):e000843. doi:10.1136/bmjsem-2020-000843
37. Thomeé R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1798-1805. doi:10.1007/s00167-011-1669-8



EXERTIONAL HEAT ILLNESS: SHOULD THIS BE A HOT TOPIC IN FOOTBALL MEDICINE?
Exertional Heat Illness (EHI) has been a common issue facing medical teams working in endurance sport for many years. However as global temperatures rising and football teams are spending more time playing and training in warmer condition putting footballers at increasing risk of EHI. This article aims to provide an overview of EHI including risk factors, clinical presentation, treatment and preventative measures.
Global change in climate and football
Over the past 50 years, global temperatures have increased by around 0.2˚C per decade with this rate increasing since 1990. However, 2023 was the
warmest year on record globally.1 Modelling suggests this change will continue and as an example, it is predicted that by 2050 the climate in London will feel similar to current conditions in Barcelona.2 As well as increases in average temperature, we are also expected to see more frequent periods of extreme high temperatures in the UK with longer and hotter summers.3
The football landscape is also changing; clubs are frequently travelling to hot or tropical climates during pre-season to aid commercial success. The 2022 FIFA World Cup was hosted in Qatar requiring a change in scheduling and stadium air conditioning to allow it to take place.
It is therefore clear to see that a hotter planet will be increasingly important for football teams playing in the UK and around the world.
The risk of EHI in football is not well known. One review article found a risk of 0.07 per 1000 athlete exposures, which is low compared to marathon running at 30 per 1000 athlete exposures.4 This means, however, that the risk is around 20 times higher than cardiac arrest in sport, and given EHI can also result in death, medical teams should understand and prepare for it.
Heat and performance
Although this article will focus on heat illness, it will briefly touch on heat and
FEATURE / DR DAN FITZPATRICK
Member of UK Heat Illness Advisory Group, Rotational Academy Doctor, West Ham United Lead Men’s Academy Doctor, Harlequins Rugby Club, Sport and Exercise Medicine Registrar, London Deanery
Individual
Previous episode of EHI
Recent upper respiratory or gastrointestinal infection
Low grade systemic inflammation can predispose to impaired intrinsic cooling
Body surface area (BSA) and muscle mass Larger muscle mass produces more heat and lower BSA impairs heat loss
Aerobic fitness
Medication use
Degree of acclimatisation
Cooling requires increased perfusion of skin. This requires increased cardiac output compared to cooler conditions.
Certain medications such as psychiatric medications affecting serotonin can increase risk
Full acclimatisation results in increased plasma volume, increased sweat rate and other adaptations that improve an individual’s cooling ability
Dehydration Reduced plasma volume to cool
Sleep deprivation Mechanism unknown
performance. Heat has varying effects on performance depending on the discipline. Sprint performance may improve in hotter conditions due to increased muscle contractility5 but there are well known detrimental effects on endurance athletes.6 In footballers, heat has been shown to impair both physical and cognitive performance7 and has been shown to alter on field behaviours in response to heat.8 Some of these changes may be mitigated by a period of heat acclimatisation, details of which are outside the scope of this article but should be considered.
Exertional Heat Illness
EHI refers to a spectrum of conditions whereby the core temperature (Tc) increases with varying degrees of body system dysfunction. Mild EHI is often referred to as “Heat Exhaustion” and severe EHI as “Heat Stroke”. Interestingly, there is evidence that an elevated Tc is normal when exercising,9 even in cool conditions, and so the diagnosis should not be made on Tc alone.
In Mild EHI, Tc will be raised above 38.5˚C and the individuals may feel weak and unable to continue. Importantly, they will not be confused, will have a normal level
Ambient temperature
Wind speed
Relative Humidity
Length of heat exposure
Increased temperature increases risk
Increased wind enhances cooling
Higher humidity reduced efficacy of cooling by sweating
Longer durations of exercise infer increased risk
of consciousness and be haemodynamically stable. Individuals with Severe EHI will likely have a higher Tc of 40.0˚C or higher and will have evidence of central nervous system dysfunction. This dysfunction may range from mild confusion to coma or seizure. They may also have signs of haemodynamic instability such as hypotension or persistent tachycardia, though this is not required to make a diagnosis of severe EHI. Ultimately severe EHI can result in death if untreated.
Why does it happen? How do we normally cool?
The human body has several ways of cooling including radiation to the environment, evaporation through sweat and conduction through the air and contact with other objects.
In health, our body will increase blood flow to the peripheries and sweat more to enhance the effects of these cooling mechanisms. This is controlled by the hypothalamus which senses temperature from peripheral thermoreceptors.10
In EHI, there is impairment in cooling efficiency. This may be because of environmental factors such as high In EHI, there is impairment in cooling efficiency. This may be because of environmental
factors such as high ambient temperature and humidity-meaning sweat cannot evaporate as quickly or a failure of our inbuilt mechanisms. Individuals with infection may have low-level systemic inflammation that affects their small blood vessels responsible for cooling. These people may then not be able to perfuse these tissues properly and therefore not lose heat from the periphery as they are meant to. As Tc increases, there is hypothalamic dysfunction which can result in paradoxical shivering and other effects that increases Tc further rather than lowering it. This is why individuals with severe EHI cannot be cooled by passive means and need more aggressive treatment as detailed below.
Risks
There are several known risk factors for EHI which are summarised in Table 1. Importantly, some of the individual risk factors such as recent infection, aerobic fitness and degree of heat acclimatisation will change over time, so any risk assessment should take place specific to the individual and circumstances.
Presentation and assessment of EHI
Players with EHI may present with collapse. It is important to consider other significant
Table 1: Known risk factors for EHI
causes of this such as cardiac arrest, hypoglycaemia and hyponatraemia along with assessment for EHI. This can be done alongside assessment for EHI if it is suspected but practitioners should always confirm the presence of a pulse before continuing any assessment. As per general principles of assessing an acutely unwell or injured player, an A-E approach should be used. However, if there is a high suspicion of EHI, it would be advisable to consider checking temperature earlier in the process, once signs of life are stablished, as treating the elevated temperature is likely to improve circulatory and neurological impairments.
An important part of assessment for EHI is the measurement of temperature. Whilst normal practice may be to use oral, tympanic or axillary temperatures, this is not sufficient in EHI and a rectal temperature should be performed. This is because at higher temperatures, other methods have been shown to underestimate Tc by as much as 2˚C with increasing error as Tc increases.11 A normal tympanic temperature may therefore be falsely reassuring for EHI. Clearly, it is important to maintain the dignity of any individual and so this should be performed in a private, medical environment. A chaperone should also be present routinely. However, it should be performed, especially in an individual
who may have signs of severe EHI as it will inform treatment.
In mild EHI the player may be:
• Conscious
• Exhausted, unable to continue
• Sweating excessively, likely hot to touch
• Nauseous
• Complaining of a headache
• Tc between 38.5˚ and 40.0˚C
An individual with severe EHI will be more unwell. They may be:
• Confused, agitated or reduced consciousness
• Vomiting
• Incontinent
• Shocked with hypotension
• Hot and sweaty or feel cold and be shivering
• Tc above 40.0˚C
Treatment
EHI is very treatable if recognised early and treated aggressively. It is strongly suspected that the longer someone remains hot, the greater the risk of damage to the brain, liver, kidneys and muscles.
It is not necessary to transfer a patient to a hospital to treat them for EHI as transporting risks a prolonged period with elevated Tc. The mantra “cool first, transport second” should be used; this has been done successfully at recent Olympic Games and in military settings.12,13
In mild EHI ‘passive cooling’ methods can be used. One method is “Shade, Strip, Fan and Spray”. The individual should be removed from play and placed in a cool environment. They should have clothing removed whilst maintaining dignity. Cold water should be sprayed over them whilst air is fanned using either an electric fan or a large towel or sheet. This is effective because their own cooling mechanisms will still be working and by stopping exercise, they should stop producing heat. Cool drinks and ice packs in the axilla, groin, wrists and ankles can be used but will not be as effective as the method detailed above.
This should be performed before transport and is done by placing the individual into something with ice cold water covering as much as their torso as possible. There are various ways to do this, including using paddling pools, but a new device called I-CWIK may be a good solution for use in football (Fig1). It is a waterproof bag that the individual can be placed in along with 80-100l of water and 20kg of ice. This has been successfully used on military exercises and so could be used in a training ground or stadium.
Individuals undergoing CWI should have continuous measure of Tc throughout as there is as risk of over-cooling. This can be performed with a rectal temperature probe that connects to a monitor. This is likely to

Figure 1: I-CWIK. Photo: Ross Hemingway
be beyond the scope of the normal team medical staff and so consider discussing with the emergency care provider if there is a risk of EHI and prepare appropriately.
Paracetamol, ibuprofen and other antipyrectics should not be used as their mechanism of action is different to the cause of EHI and they may increase the risk of liver or renal damage respectively.
There is a risk of renal and liver injury or rhabdomyolysis following severe EHI. Therefore, individuals who sustain severe EHI should be transferred to hospital for blood tests to assess for this.
Aftercare
Serial blood tests should be performed as advised by medical staff until normalised. In football, a decision around return to play is important but there is a risk of recurrence if the player returns too soon. It is recommended that the underlying reason for severe EHI is found and understood. This may be a concurrent
References
infection but there are other, rarer, muscle and brain disorders that could predispose to EHI. Individuals may need referral for assessment of these factors before returning to play. Members of the general population are advised to rest for up to six weeks following EHI and then gradually return to activity. In a supervised environment, it may be safe to start earlier but specialist advice should be taken on this.
Prevention
There are steps that medical staff, clubs and tournament organisers can take to reduce the impact of heat on performance and health. FIFA details these in their Emergency Care Manual.14,15 . They focus on prevention and include reference to Wet Bulb Globe Thermometer (WBGT) measurements. WGBT is a device that measures ambient temperature, humidity, wind speed and sunlight to provide a measure of solar stress. There are cutoffs for mandatory water breaks and recommendations to consider rescheduling
football to evenings or early mornings. These should also be applied for training given similar risks.
Other measures include heat acclimatisation, effective prehydration of players and precooling with devices like ice vests or ice slurry drinks to lower Tc prior to competition. There is little evidence precooling can reduce the risk of EHI, but it may mitigate performance impairment in the heat.
Conclusion
The football world is getting hotter and the risk of EHI is increasing. Football medical teams should understand how to assess and recognise EHI and have plans in place for its treatment. This may involve expanding existing emergency action plans and increasing preparation. Further research is needed to fully understand the risk specific to football. For more information or advice consider contacting the UK Heat Illness Advisory Group (www.hiag.org.uk)
1. Samset BH, Lund MT, Fuglestvedt JS, Wilcox LJ. 2023 temperatures reflect steady global warming and internal sea surface temperature variability. Communications Earth & Environment 2024 5:1 2024; 5: 1–8.
2. Bastin JF, Clark E, Elliott T, et al. Understanding climate change from a global analysis of city analogues. PLoS One 2019; 14: e0217592.
3. Hanlon HM, Bernie D, Carigi G, Lowe JA. Future changes to high impact weather in the UK. Clim Change 2021; 166. DOI:10.1007/S10584021-03100-5.
4. Gamage PJ, Fortington L V., Finch CF. Epidemiology of exertional heat illnesses in organised sports: A systematic review. J Sci Med Sport 2020; 23: 701–9.
5. Girard O, Brocherie F, Bishop DJ. Sprint performance under heat stress: A review. Scand J Med Sci Sports 2015; 25 Suppl 1: 79–89.
6. Racinais S, Alonso JM, Coutts AJ, et al. Consensus recommendations on training and competing in the heat. Br J Sports Med 2015; 49: 1164–73.
7. Pompeo A, Afonso J, Cirillo ELR, et al. Impact of temperature on physical and cognitive performance in elite female football players during intermittent exercise. Scand J Med Sci Sports 2024; 34. DOI:10.1111/SMS.14646.
8. Nassis GP, Brito J, Dvorak J, Chalabi H, Racinais S. The association of environmental heat stress with performance: Analysis of the 2014 FIFA World Cup Brazil. Br J Sports Med 2015; 49: 609–13.
9. Stacey MJ, Leckie T, Fitzpatrick D, et al. Neurobiomarker and body temperature responses to recreational marathon running. J Sci Med Sport 2023; 26: 566–73.
10. Osilla E V., Marsidi JL, Shumway KR, Sharma S. Physiology, Temperature Regulation. StatPearls 2023; published online July 30. https:// www.ncbi.nlm.nih.gov/books/NBK507838/ (accessed Oct 11, 2024).
11. Ganio MS, Brown CM, Casa DJ, et al. Validity and reliability of devices that assess body temperature during indoor exercise in the heat. J Athl Train 2009; 44: 124–35.
12. Wood F, Roiz-De-Sa D, Pynn H, Smith JE, Bishop J, Hemingway R. Outcomes of UK military personnel treated with ice cold water immersion for exertional heat stroke. BMJ Mil Health 2024; 170: 216–22.
13. Hosokawa Y, Racinais S, Akama T, et al. Prehospital management of exertional heat stroke at sports competitions: International Olympic Committee Adverse Weather Impact Expert Working Group for the Olympic Games Tokyo 2020. Br J Sports Med 2021; 55: 1405–10.
14. FIFA. FIFA Emergency Care Manual. 2022.
15. Gouttebarge V, Duffield R, Den Hollander S, Maughan R. Protective guidelines and mitigation strategies for hot conditions in professional football: starting 11 Hot Tips for consideration. BMJ Open Sport Exerc Med 2023; 9: e001608.
Hemingway R, Stourton F, Leckie T, Fitzpatrick D, Jones G, Wood F, Boalch A, McNulty Ackroyd J, Thurgood A, Boulter M, Hartle A, Walter E, Pynn H, Kipps C, Stacey M. Consensus Statement on the Pre-Hospital Management of Exertional Heat Illness, November 2024, https://fphc.rcsed.ac.uk/media/3665/fphc-exertional-heat-illness-consensus-statement-2024-v14-_final.pdf


PERFORMANCE, INJURY REDUCTION & AVOIDING PUSHING
YOUTH ATHLETES
TOO FAR VIA PRE-SEASON ADOLESCENT SCREENING
FEATURE / CRAIG HAGAN
This article will touch on the need for early athlete injury screening, why this is necessary for performance, development, how it can be a gateway to developing elite habits such as educating and systemising and lastly where it fits into the current system of academies and clubs.
What is athlete injury screening? Athlete injury screening can be conducted using various systems or methods all following some common themes: A battery of Joint and muscle ROM and strength testing- standardised performance tests aimed at each energy system and performance markers specific to the sporting demands. In the case of football you have Sprinting, endurance over distances/ time, COD ie agility, Vertical and horizontal leap etc.
Pre-season screening can be used to and not limited to benefitting:
• Optimise physical preparation
• Identify injury risk in those at higher risk
• Improve movement efficiency
• Used as a baseline to further develop individualised programs
• Prevent overuse injuries which are most common in the growing athlete
• Baseline for psychological readiness
• Help with team bonding
Think of this as an adolescent medical test where its not about passing or failing but rather extrapolating data that can help the athlete perform better and have a better handle on their training load or from a coaching perspective gaining an insight into positional athletic abilities and/ or requirements.
When can screening be useful for safety and performance?
Screening in particular is a great way to extrapolate multiple data sets and pieces of information that can then be recycled for rehabilitation, performance and to also
highlight any outliers for better or for worse. For the purpose of this article, I will touch on the latter. As we know, players are at a higher risk of injury during their Peak Height Velocity- as this is the period when their bodies and growing and adapting at their fastest, thus requiring greater recovery demands than those during normal or steady growth phase. Screening can also be used as a tool to measure strength and mobility that can be compared from Left to Right, in the case of muscles used as a ratio. An example of this in the hip may be Left to right hip adduction or hip ADDuction to ABDuction ratio.
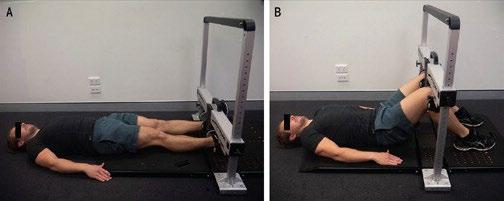
As a result of varying growth person to person, in elite pools of players it is possible to “Bioband” players with the assistance of the data collected. This is where players are matched to play against others of the same or similar biological development. This can avoid early developers from playing against late maturing athletes in an environment where skill and other factors aren’t at play. From a safety perspective this is an easy decision however from a tactical and overall player development perspective this allows the athletes to be suitably challenged, and thus develop to the best of their ability.
Additionally having such a system is a great opportunity to develop and understand load management for players, parents, coaches and others involved in the process.
Where it fits in
Currently in the Premier League academies Growth and maturation screening are performed as a standardised, national benchmark fitness testing for u12 and u13 levels which is independently verified for each player and club.
This fitness data is entered into the PMA (Performance Management Application) to allow the Premier League to benchmark the athletic development of all academy players. This allows comparison to benchmark the physical profile of each player against Biological (bio-banded), chronological and positional standards across the whole academy system. This system has been running since 2012 and is the biggest data collection of physicality that has ever been conducted.
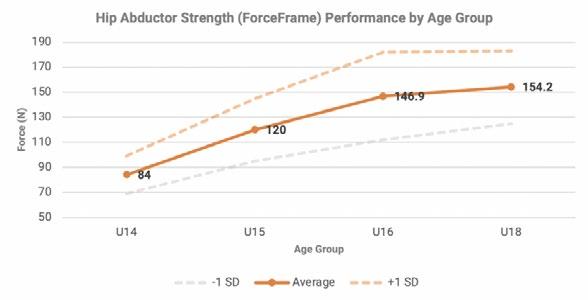
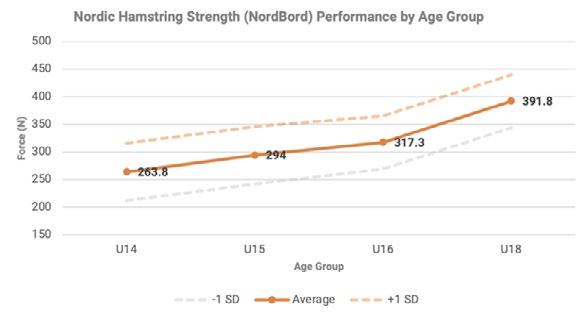

PMA Ranking of Academy Systems
Category 1-4
Criteria


Above is a ranking system the Premier League has put in place based on how well such implementations are made. In an ideal world it is easy to recommend such system to every and all levels of competition however I would make some practical recommendations when finances, player numbers, resources and standard are an issue:
- Club based pre-season screening done in collaboration by Sports Scientists, S&C, Physios or Doctor, ideally any professional who is confident in running through the testing. Likely a multidisciplinary approach is better.
- Use this information to be banded into a document for the club to use or refer back to using any database of preference
Additionally, with limited resources it is often easier to outsource this testing and focusing more on reading the data to understand what needs to be done
Author Affiliations: West Tigers NRL Physiotherapy Intern, Newcastle
Jets A-League Sports Trainer, Ex Barca

Academy Australia Head Trainer, NPL2
Southern District Raiders Sports Trainer, Ex National level Dragon Boater for Australia (Multiple world medals).
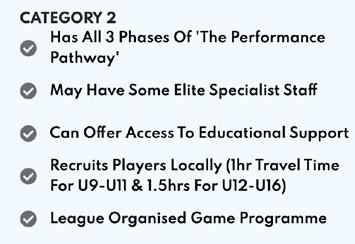
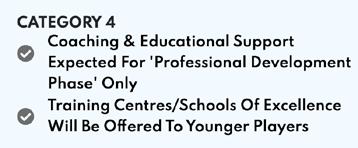
with it. For example, a preseason could see a club partnering with their local High-Performance gym, Physio clinic etc. From there the testing can be conducted and the data is secured. It would then me the club’s responsibility to use the professionals they have at hand ie S&C, Sports science etc to communicate with the experienced tester to provide practical solutions for their pre-season, in season training blocks.
Takeaway message
Overall, pre-season screening provides valuable and crucial feedback that can be held onto and used as a means for:
• Improving performance
• Reducing injury risk
• Providing feedback from previous sessions
• It can be a useful gateway to educate and mould good habits that overall can increase athletes’ performance

References
1. Moreno-Pérez, V., Travassos, B.F., Calado, A., Gonzalo-Skok, O., Del Coso, J., & MéndezVillanueva, A. (2019). Adductor squeeze test and groin injuries in elite football players: A prospective study. Physical therapy in sport : official journal of the Association of Chartered Physiotherapists in Sports Medicine, 37, 54-59 .
2. Normative data in youth academy football: Impacts on hip and groin injuries. (no date) Technology for human performance. Available at: https://valdperformance.com/news/ youth-academy-football-impacts-on-hip-and-groin-injuries-12440 (Accessed: 12 October 2024).
FMPA MEMBERSHIP
Expert legal support and representation across employment medico legal and regulatory law
All the benefits of Union membership through the FMPA
Priority member only access to job listings and email alerts 24/7 support from the FMPA and much more…
“I believe FMPA membership is now essential and should be a pre-requisite for any member of staff within our sector.”
Head of Sport Science & Medicine, Premier League

SACROILIITIS: FINDING A PATHWAY FOR A RARE INFLAMMATORY BACK CONDITION
A COMPARATIVE CASE-STUDY ANALYSIS
FEATURE / LIAM DONOVAN
Introduction
Sacroiliitis is the term used to describe the painful inflammation of the sacroiliac joint. Sacroiliitis may occur secondary to mechanical stress of the SI joint, trauma, infective causes, autoimmunity or because of an unknown reason (Baronio et al, 2020). This can make the diagnosis of sacroiliitis, and its management, a diagnostic challenge (Slobodin et al, 2018). Sacroiliitis has also been highlighted as the first manifestation of more complex spondyloarthropathies such as ankylosing spondylitis, inflammatory bowel disease and rheumatic disease (Baronio et al 2020). It’s rarity in professional sport has meant there is no definitive RTP pathway or evidence-based approach to managing this pathology.
The purpose of this article is to discuss and explain the route for two separate incidences sacroiliitis in professional footballers at the same club. We highlight
the challenges in diagnosis and predicting Return to Play (RTP) timeframes whilst discussing ongoing management during a competitive football schedule. We also provide a pathway to follow should you come across or suspect this in an athlete under your care.
Player 1 – 18 years old academy player – gradual onset of left sided SIJ related symptoms over the course of 2/52.
Player 2 – 22 year old first team playerReturning from a high grade hamstring tear – at very end of rehab whilst in team training began complaining of SIJ pain that was debilitating to the point of dropping out of training.
Diagnosis
Player 1 - was originally treated as a general lower back tightness with referral into his glute – an MRI was conducted after 2/52 of limited improvement where we queried a pars interarticularis fracture
– due to his age, activity and frequency of these injuries in young athletes. On bed based assessment presented with glute pain without mechanism or incident, gradual onset with a vague history, player was observed being unable to accept force through hopping/decelerating – the MRI confirmed diagnosis of left sided sacroiliitis.
Bloods completed - CRP 1mg/L. HLA B27 +ive. All other bloods normal.
Player 2 – 22 year old first team player. Originally presented as SIJ dysfunction as was RTP from a long term hamstring injury – player had hit all markers on his RTP and was 6/52 post injury when player sneezed in a twisted position and felt had a twinge in his thoracic spine. Over the course of 2/52 gradually noticed L SIJ discomfort through training. On assessment such was the severity of symptoms even lying on his back was in 6-7/10 pain but was eager to return
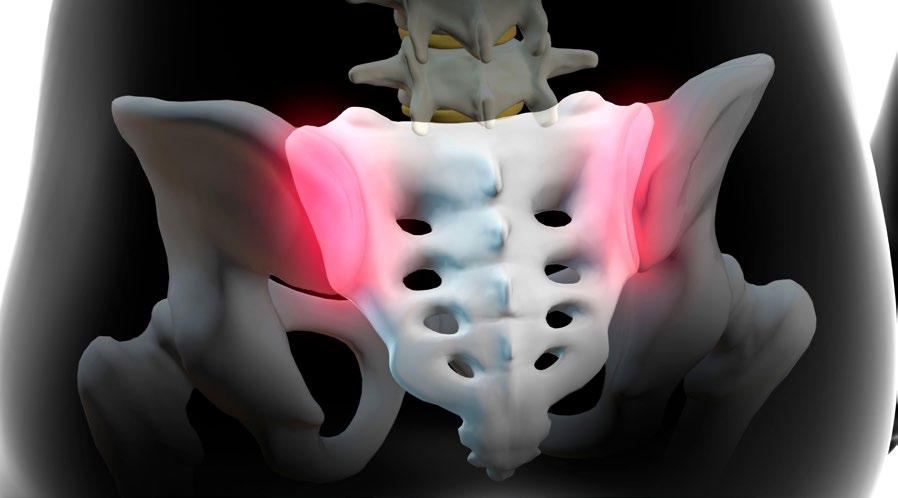
to training after a long injury lay off. Symptoms in the morning became more pronounced and the player described not being able to sleep and turning over in bed as the most debilitating of tasks. Player also had an MRI which confirmed the diagnosis of:
“unilateral right sided sacroiliitis with subchondral oedema and early subchondral erosion. No inflammatory change in left sacroiliac joint”
The decision was made to image higher up the spine as had thoracic symptoms prior to his sacroiliac symptoms. This showed:
“There is inflammatory changes at the first chondrosternal junction on the left side. He has inflammatory change in the right T6, T7 and T8 costoverterbral and costotransverse joints ... No other positive findings in the thoracic / cervical spine... Findings are those of a seronegative spondyloarthropathy”
Bloods completed - CRP 11mg/L, ESR 10, HLAB27 –ive. All other bloods normal.
As a medical team we sought the valued opinion of Dr Jon Houghton of the well
renowned Fortius Clinic to help guide us with a treatment plan.
Treatment
Both players were immediately removed from all football related activity whilst we waited for the return of the blood test results. However, both were started on eterocoxib (a selective Cox-2 inhibitor) –to help manage the symptoms and help reduce the inflammation of the SIJ.
Player 1 saw a remarkable improvement when beginning the medication – within 72 hours symptoms had improved significantly and was able to begin some light gym based loading. We were advised to let the symptoms dictate the RTP but with the player having missed a significant amount of football and with us having no experience of managing a condition like this we decided on a full 6/52 return to manage his loadings as closely as possible.
Player 2 did not respond so quickly to the eterocoxib and it took significantly longer for the medication to have an effect, even after taking the eterocoxib his presentation and clinical markers were unchanged. Due to the severity of the symptoms this prompted the introduction
of prednisolone which required a Therapeutic Use Exemption (TUE). A TUE allows athletes to use prohibited substance or method for legitimate medical reasons without facing sanction (WADA, 2024). On assessment after the course of prednisolone had begun – player settled to a 1/10 on the thigh thrust and was happy to begin loading.
Ongoing management
Flare ups
Player 1 had 2 separate incidences of the pain returning in the first year post diagnosis. The first came when reporting back for pre-season – gradual onset as the training load had increased and subsequently missed 9 days – we temporarily increased his etorocoxib to 90mg OD for a 3 month period, while we continued to work on areas surrounding the SIJ. The second incidence came when the player was being utilised by both first team and 21’s team, this is commonplace for a young professional and led to a sporadic training load.
Screening/Profiling
Physical screening/profiling is now a common occurrence in professional football, it allows the performance team to identify if a player is physically unable
1: Breakdown of profiling data Player 1 – significant discrepancy in ISO Prone/Nordic/Adduction score coincided with symptoms.
ISO PRONE
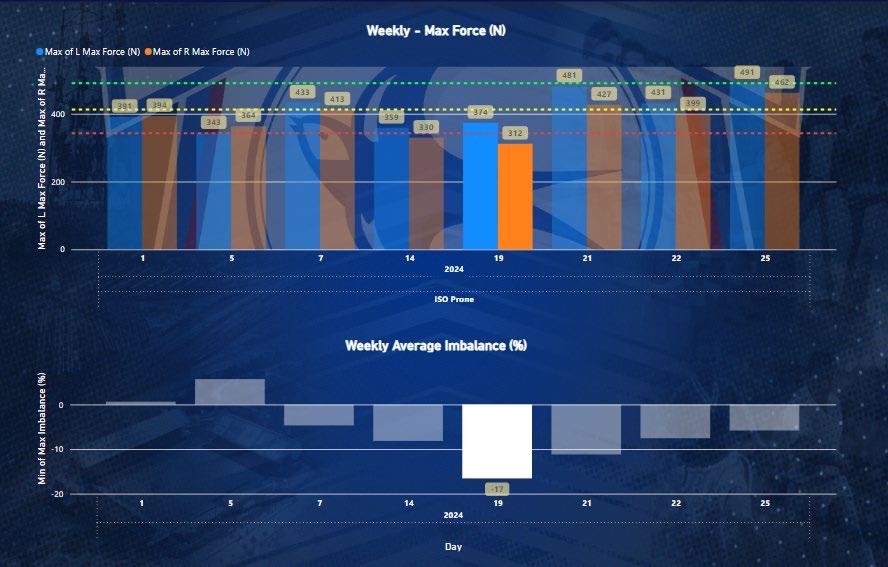
Figure
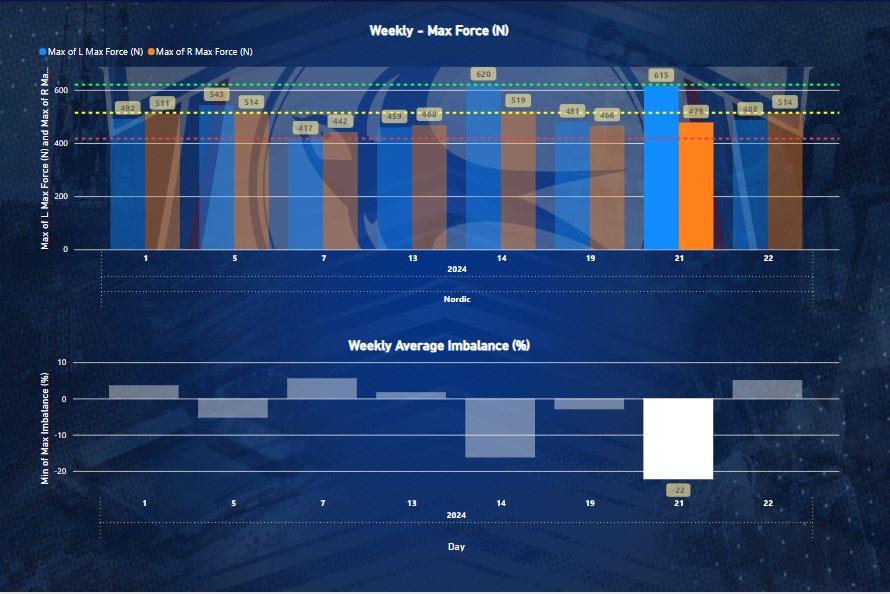
ADDUCTION

Non-specific LBP
Rule out red flags
Assess response to NSAIDs
Blood testing inc. CRP, ESR, HLA B27
Imaging: MRI
Referral to rheumatologist
Figure 2: Referral pathway for someone suspected to have sacroiliitis.
to perform to their usual athletic capabilities thus highlighting a potential increased injury risk (Carling et al, 2018).
We developed a continuous screening process on a MD+2 that allowed us to monitor and modify gym/training load based from a set of criteria we believe relate to the function of the SIJ and the players symptoms.
Single leg hip extension test on the force decks, ISO prone and Nordic testing on the nordbord allowed us to monitor the isometric capabilities of the posterior chain. This would highlight whether the player was comfortable/confident or able to achieve baseline figures of force production through the posterior chain – a drop in their baseline score or rolling average would indicate either a lack of recovery or the need for a more in-depth assessment.
Glute add/abduction gave us information around the force production capabilities of the adductor and abductor muscle groups. Adduction was identified as the most sensitive to change in Player 1, in addition to this over the course of 2/52 his ISO prone/Nordic scores also showed significant inter limb discrepancy – this coincided with him developing symptoms and meant he missed 1/52 of training until we were able to increase his medication dose and calm down his symptoms with some manual therapy
techniques alongside activating the structures supporting the SIJ. See Figure 1 for a breakdown of Player 1’s profiling.
We also used the forcedecks to complete countermovement jump testing (CMJ) – this allowed us to review the eccentric rate of force development (RFD) and landing asymmetries to see how the SIJ reacted on maximal weightbearing through a ballistic activity. If symptoms or discomfort were present we expected this to be reflected in the jump data e.g. a potential discrepancy in eccentric RFD, or a discrepancy in weight distribution on double leg tasks. We would use this data to identify whether the players were offloading the reactive SIJ subconsciously which would give us further indication on whether the player was managing their load or whether they needed further assessment or intervention.
Although all data was not used to make decisions in isolation, it contributed to a multifaceted approach on player management and availability.
Early interventions may include:
• More specific prehab around the posterior chain
• More time being assessed/treated on the bed before/after training
• A change in gym approach to offload/ activate the posterior chain
• Further scrutiny of change in training data.
In addition, as symptoms can be insidious in onset, adding objective data to the subjectivity of pain or discomfort can allow the medical department to be more proactive in its management. This can also add some reasoning as to why the player may be feeling the way they do, which can help with the players understanding of their condition.
Conclusions/Reflections
Reflecting on both cases our biggest learning point was the need to have a clear pathway for these injuries (See Figure 2). Hopefully this article has shed some light on the challenges that we faced as an MDT with both of these cases reacting differently at different times highlighting the important of flexibility with the treatment approach.
Diagnosing the injury early is key, involving a doctor early if any red flags are present, getting in touch with the right consultant to manage the blood tests/medication will help to manage the symptoms. Having a clear monitoring system in place is also

References
key to player availability and being able to intervene as soon as possible.
Comparing RTP dates between both players diagnosis in Figure 3 it is clear that having this process in place this has significantly sped up the RTP process. Regular gym screening and monitoring has helped us identify when Player 1 could potentially develop issues – having a support team to help with this and being able to educate the coaches around modifications or explanations for unavailability encouraged the player to be honest with symptom reporting. We feel when reflecting on the RTP process in the 2nd and 3rd incidence in Player 1 we can see time loss has significantly decreased (Figure 3). Finally, having a clear process to decrease RTP time and maximise player availability is key to player trust and honesty in reporting symptoms.
(Diagnosis)
(17 days to consultant
Acknowledgements
I would like to thank Matt Giles and Arron Garrett for their extensive contributions to this article and their excellent support with the ongoing management of both players.
Chung, H.Y.; Machado, P.; van der Heijde, D.; D’Agostino, M.-A.; Dougados, M. HLA-B27 positive patients differ from HLA-B27 negative patients in clinical presentation and imaging: Results from the DESIR cohort of patients with recent onset axial spondyloarthritis. Ann. Rheum. Dis. 2011, 70, 1930–1936
Baronio M, Sadia H, Paolacci S, Prestamburgo D, Miotti D, Guardamagna VA, Natalini G, Bertelli M. Etiopathogenesis of sacroiliitis: implications for assessment and management. Korean J Pain. 2020 Oct 1;33(4):294-304. doi: 10.3344/kjp.2020.33.4.294. PMID: 32989194; PMCID: PMC7532300.
Slobodin, G., Hussein, H., Rosner, I., & Eshed, I. (2018). Sacroiliitis – early diagnosis is key. Journal of Inflammation Research, 11, 339–344. https://doi.org/10.2147/JIR.S149494
Carling C, Lacome M, McCall A, Dupont G, Le Gall F, Simpson B, Buchheit M. Monitoring of Post-match Fatigue in Professional Soccer: Welcome to the Real World. Sports Med. 2018 Dec;48(12):2695-2702. doi: 10.1007/s40279-018-0935-z. PMID: 29740792; PMCID: PMC6244616

