98
2. THYROID GLAND Table 2.10 Causes of hyperthyroidism More common causes Graves-Basedow disease Toxic adenoma Multinodular toxic goiter De Quervain thyroiditis Painless thyroiditis Iatrogenic causes, medication (e.g. amiodarone) thyrotoxicosis Less common causes Initial phases of Hashimoto’s thyroiditis Postpartum thyroiditis Hyperemesis gravidarum Struma ovarii, trophoblastic tumors TSH secreting pituitary adenoma Metastatic thyroid cancer
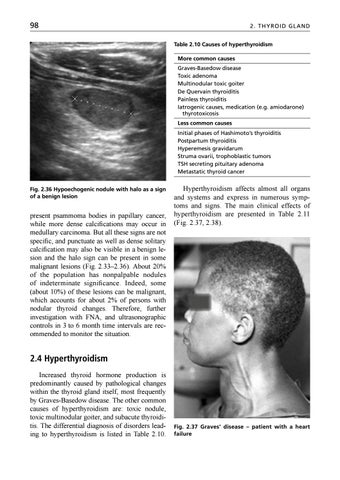
Fig. 2.36 Hypoechogenic nodule with halo as a sign of a benign lesion
present psammoma bodies in papillary cancer, while more dense calcifications may occur in medullary carcinoma. But all these signs are not specific, and punctuate as well as dense solitary calcification may also be visible in a benign lesion and the halo sign can be present in some malignant lesions (Fig. 2.33–2.36). About 20% of the population has nonpalpable nodules of indeterminate significance. Indeed, some (about 10%) of these lesions can be malignant, which accounts for about 2% of persons with nodular thyroid changes. Therefore, further investigation with FNA, and ultrasonographic controls in 3 to 6 month time intervals are recommended to monitor the situation.
Hyperthyroidism affects almost all organs and systems and express in numerous symptoms and signs. The main clinical effects of hyperthyroidism are presented in Table 2.11 (Fig. 2.37, 2.38).
2.4 Hyperthyroidism Increased thyroid hormone production is predominantly caused by pathological changes within the thyroid gland itself, most frequently by Graves-Basedow disease. The other common causes of hyperthyroidism are: toxic nodule, toxic multinodular goiter, and subacute thyroiditis. The differential diagnosis of disorders leading to hyperthyroidism is listed in Table 2.10.
Fig. 2.37 Graves’ disease – patient with a heart failure
Ukázka elektronické knihy, UID: KOS196184