http://www.inosr.net/inosr-experimental-sciences/
Kyakimwa
INOSRExperimentalSciences11(1):34-66,2023.
©INOSRPUBLICATIONS
InternationalNetworkOrganizationforScientificResearch
ISSN:2705-1692
Surgical Site Infection prevention among Nursing Staff at Kampala InternationalUniversityTeachingHospitalBushenyi,Uganda
KyakimwaNaume
SchoolofNursingScienceKampalaInternationalUniversity-WesternCampus,Uganda.
ABSTRACT
Surgicalsiteinfections(SSIs)areinfectionsrelatedtoanoperativeprocedurethatoccursat or near the surgical incision within 30 days after the surgery. The incidence of SSI Varies from hospital to hospital in different countries with developed countries having lower incidences ranging from 2% to 6.4%, and developing countries with higher incidence ranging from 5.5% to 25%. The aim of this study was to assess knowledge and practices regarding surgical site infection prevention among Nursing Staff at Kampala International UniversityTeachingHospitalBushenyi,Uganda.Thiswasacrosssectionaldescriptivestudy and quantitative in nature. The main objective of this study was to examine the level of knowledge and practices regarding surgical site infection prevention among nursing staff atKampalainternationaluniversityteachinghospital. Itinvolved 33respondents who were convenientlyselectedtoparticipateinthesturdy. Resultsfromthisstudyindicatedthatan average of 16(48.5%) respondents had adequate knowledge on SSI infection prevention while an average of 17(51.5%) respondents had inadequate knowledge on SSI prevention. Thestudyrevealedthattherewasnopositiverelationshipbetweenknowledgeandpractice regarding surgical site infection prevention since respondents were found to have slightly higher knowledge but with less practice of the recommended precautions about surgical site infection prevention. In conclusion, basing on the findings of this sturdy, nurses have low level of knowledge about prevention of infection of surgical sites. The areas that registered extremely poor knowledge were areas of wound assessment, pre-operative showering, timing and importance of preoperative prophylactic antibiotics and correct diagnosis of surgical site infection. This study also concludes that the level of practices of the recommended precautions as far as prevention of infection of surgical sites was low amongnursingstaffatKIU-TH. Theareasthatregisteredextremelypoorpracticeincluded use of masks during wound care procedures, nutritional assessment (BMI) for surgical patients,andadministrationofpreoperativeprophylacticantibiotics,pre-operativeshaving anduseofseparatesterilepressingpackforeverypatientduringwoundcare.
Keywords: Surgical site infections, developing countries, surgical incision, prophylactic antibiotics.
INTRODUCTION
Surgical site infections (SSIs) are infections related to an operative procedure that occurs at or near the surgical incision within 30 days after the surgery,[1].
Humaun et al [2] defined SSIs as infections that occur after the operation within 30 days if no implants or within one year if there is an implant. SSIs are one of the nosocomial in which an infection occurs after an invasive procedure. The incidence of SSI Varies
from hospital to hospital in different countries with developed countries having lower incidences ranging from 2% to 6.4%, [1] anddeveloping countries with higher incidence ranging from 5.5% to 25%[3]
There are patient related (intrinsic) factors including; age extremities, poor nutritional status, metabolic diseases, smoking, obesity, hypoxia, immune suppression and length of pre-operative stay that increase the risk of developing
34
http://www.inosr.net/inosr-experimental-sciences/
SSI. The extrinsic factors that influence the risk of SSI include, application of skin antiseptics, preoperative shaving, antibiotic prophylaxis, preoperative skin pre-operative skin preparation, inadequate sterilization of instruments, surgical drains, surgical hand scrub and dressingtechniques,[4,5,6,7,8,9]
SSIs contribute substantially to surgical morbidity and mortality, leading to increased duration of postoperative hospital stay, higher rates of hospital readmission, impaired health outcomes and increased costs. In 2009, in the USA, it was estimated that a SSI extended the length of hospital stay by 9·7 days on average[6,10,11,12,13,14,15]
Sepsis is a common diagnosis, a frequent cause of hospitalization, and a leading cause of death in the United States [8]. Becoming familiar with sepsis is essential fornursesinallsettings[16,17,18,19].
Approximately 24% of patients who develop severe sepsis or septic shock will do so on a medical-surgical unit [8] Sepsis was the principal reason for hospitalization in 836,000 hospital stays and the secondary diagnosis in an additional 829,500 hospital stays in 2009 [9]. Levit, et al; [10] tracked sepsis data from1997to2006,notingthatsepsisasa principal diagnosis increased 48%. The rate of hospitalization for sepsis as a primary or secondary diagnosis rose to70% from 2000 to 2008 [11]. Between 1997 and 2008, hospital stays for septicemia increased by 91% (Healthcare CostandUtilizationProject[HCUP],2010).
It is estimated that 1.4 million people worldwide are suffering from HAI. Approximately 2 million patients develop HAI and nearly 90,000 of these patients areestimatedtodieannually,whichranks HAI as the fifth leading cause of death in the United States of America (USA) [12,20,21,22,23,24].
Accordingly, among the HCWs, nurses have a critical role to play in prevention efforts and they are an important population to study their level of knowledge, and practices regarding SSIs prevention. However, up to date these issues have received only limited attention and obtaining information may
be useful for developing programs to increasecompliance,[13,25,26,27].
Problem statement
It is estimated that SSI develop in 2% to 5% of the more than 30 million patients who undergo surgical procedures representing 14% to 16% of all HAIs annually in US. These infections account 3% of all surgical mortality and lead to increased re admission, increased length of hospital stays and higher medical costs,[14,28,29,30,31,32,33].
In the past 20 years, the overall incidence ofHCAIshasincreasedby36percent.The substantial human suffering and financial burden of the infections is staggering.510 percent of patients acquire one or more infections and 15-40% of patients are affected by Hospital acquired infections(HAI)[15,28,29,30,31,32,33].
WHO [16] estimated the burden of SSI in developing world where sub-Saharan Africa falls at 29%, Europe at 17%and USA at 20% of all patients undergoing surgical procedures. In East Africa, Tanzania leads the region with the burden of SSI estimated to be at 26% of all patients undergoingsurgicalprocedures
In Uganda Literature about SSI is still scarceandthetrueincidenceandcostper patient is unknown. However, research done at Mbarara regional referral hospital in south western Uganda to determine the incidence of SSIs on surgical wards in 2016, put post-operative incidence densityat16.4%[17].
At Kampala international university teaching hospital, unpublished hospital recordsindicatethat,forevery10patients undergoing surgical procedures, 5 suffer post-operative SSI and the situation is worse with patients undergoing orthopedicsurgeries whereabout8outof 10 suffer SSI leading to long duration of hospital stay and the very increased medicalcosts.
Nurses are directly involved in the assessment of patients at risk for developing SSI and in the treatment of patients with it and can, therefore, affect outcomes for critically ill patients [18]. It is from this back ground that the researcher derives the interest to carry out this study about knowledge and
35
http://www.inosr.net/inosr-experimental-sciences/
practice among nursing staffs regarding SSIprevention.
Aim of the study
The purpose of this study was to examine the level of knowledge and practices regarding surgical site infection prevention among nursing staff at Kampala international university teaching hospital
Specific objectives
1. Assessment of the level of nurses’ knowledge on surgical site infectionprevention
2. Examine the practices of nurses regardingSSIprevention Research questions
1. What is the level of nurses’ knowledgeonSSIprevention?
2. Whatarethepracticesofnurseson SSIinfectionprevention?
Study design and rationale
Justification of the study
Despite being largely preventable, SSI continues to represent about fifth of all healthcareassociatedinfections[19]. Despite many advances in infection control practices, including improved operating room ventilation, sterilization methods,barriers,surgicaltechnique,and antimicrobial prophylaxis, SSIs still cause a substantial amount of morbidity and mortalityamonghospitalizedpatients. The increase of transmissible infections, not only in health care institutions but also in the home, is an issue of great societal concern, [20] The findings of the study will therefore help in policy formulation at ministry level and implementation in hospitals as well as for referencepurposesbyfutureresearchers.
METHODOLOGY
The study was a descriptive crosssectional of quantitative in nature. This design was used because; it is cheap in terms of resources like time and money sincedatacollectedonce.
Study setting and rationale
The study was conducted at Kampala international university teaching hospital (KIU-TH), found in ishaka municipality, Bushenyi districtKIU-THisprivatenotfor profit institution which was founded in 2004 and it serves as a teaching hospital for KIU medical school. It’s located approximately 395 km North West of Kampala capital, 45 km north of Mbarara along the Mbarara Fort portal high way. The hospital has a capacity of about 300 bedsandservesalsoas areferral hospital for the entire greater Bushenyi region. The researcher intends to carry out this because of its convenience in terms of accessibility but also the observation made by the researcher about the burden of the problem necessitated that the studybecarriedoutatthissite Study population
The sturdy involved nursing staff of all cadresatKIU-TH
Sample size determination
The sample size will be determined using [21]
n=z2pq/r2
Where: nisthesamplesizedesired Z is the degree of accuracy, 95% which is 1.96
P is Proportion of KIU staffs that are nurses working in surgical units ie 50(0.05)
Q=1-p
By substitution in the above formula=33. Therefore, the study used a sample size of33nursesworkinginsurgicalunits Sampling procedure (methods)
The research respondents were selected using convenient method of sampling since the entire can nursing staff not be ondutyatsametime
Inclusion criteria
The nursing staffs that were on duty and voluntarilyconsentedtoparticipateinthe studyatthetimeofdatacollection
Exclusion criteria
The staff who were not nursing professionals
Nursing staff that did not consent to participate in the sturdy on voluntary basis
Independent variable
Knowledge of nurses about SSIs prevention
36
http://www.inosr.net/inosr-experimental-sciences/
Dependent variable
Practices of nurses regarding SSIs prevention
Research instruments
Data was collected using an approved structured questionnaire which consisted of both open and close ended questions. The questionnaire was divided into 3 parts ie the demographic characteristics, knowledge of nurses about surgical site infection prevention and practices of nurses on surgical site infection prevention.
Data collection procedures
Afterthesamplingprocess,theresearcher distributed the questionnaires to the consented respondents who were requiredtofillthem.
Data management
Data collected was edited before leaving the area, to ensure completeness and if any blank spaces found, they we refilled thereandthen.
Data processing and analysis
Data entry, coding, and analysis were performed using SPSS version 20software package. To explain the study population in relation to relevant variables, frequencies, percentages, and summary
Social
statistics were used. Association between dependent and independent variables wereassessedandpresentedusingtables, graphs,andpiecharts.
Ethical considerations
The researcher sought approval of the proposal from the supervisor before handing it in to the school of nursing research coordinator for further scrutiny and approval. Thereafter, the proposal was submitted to Kampala international university research and ethics committee for review, approval, and granting permission to proceed with data collection. The researcher also requested for letters of introduction to hospital administration in order to be allowed collect data from hospital nursing staff andthiswasgranted.
Confidentiality was maintained to the best of the researcher’s ability and no name was required on the questionnaires and the information generated was only usedforacademicpurposes.
Participant autonomy was respected by giving them full information and allowing them to freely decide whether to participateornot.
RESULTS
Table
years of age while only 4 (12.1%) were of age41andabove.
37
demographic characteristics
Age range of respondents Frequency(n) Percentage (%) 18-30 16 48.5 31-40 13 39.4 41andabove 4 12.1 Total 33 100
Table 1: shows the age distribution among respondents (n=33)
1 shows that majority of the respondents16 (48.5%) fell in the age range 18-30 years, 13 (39.4%) were 31-40
http://www.inosr.net/inosr-experimental-sciences/
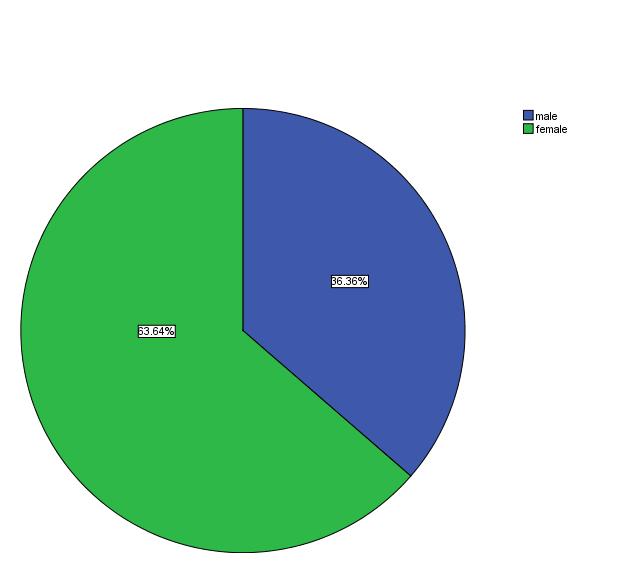
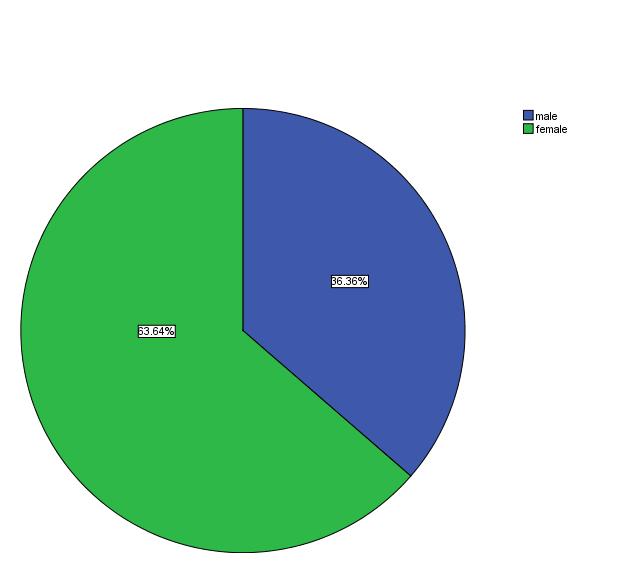
Majorityoftherespondents21(63.6)werefemalesand12(36.4%)weremale
38
Figure 1: sex of respondents
http://www.inosr.net/inosr-experimental-sciences/
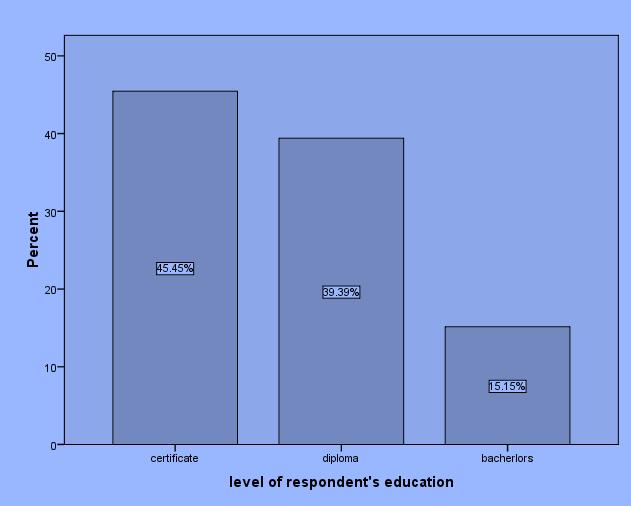
From figure2 above, the majority of the respondents 15 (45.5) are certificate holders, followed by diploma, 13 (39.4%)
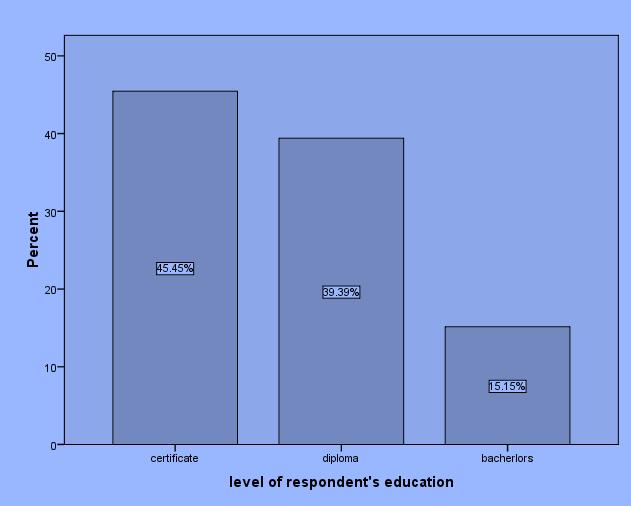
and the smallest proportion of respondents 5 (15.2%) are graduates of nursing.
n=33
From table 2 above the majority of respondents16 (48.5) had worked for 1-5 years, followed by those who had served 6-10 years, 7(21.2) while less than 1 year
and 11 years and above had the least number of respondents, 5(15.2%) respectively.
39
Figure 2: Distribution of the respondent’s level of education
Table 2: shows distribution of respondents according to years spent in service (experience)
of years respondents
Frequency(n) Percentage (%) Lessthan1year 5 15.2 1-5years 16 48.5 6-10years 7 21.2 11years 5 15.2 Total 33 100
Number
have spent in service
http://www.inosr.net/inosr-experimental-sciences/
Figure3: Shows the distribution of respondents according to religion (n=33)

From figure 3 above, it is evident that most of the respondents 17 (51.5%) were Anglicans by faith followed by Roman
Catholics 8 (24.2%) with the least being seventhdayAdventists3(9.1)
40
http://www.inosr.net/inosr-experimental-sciences/
KNOWLEDGE ON PREVENTION OF SURGICAL SITE INFECTION
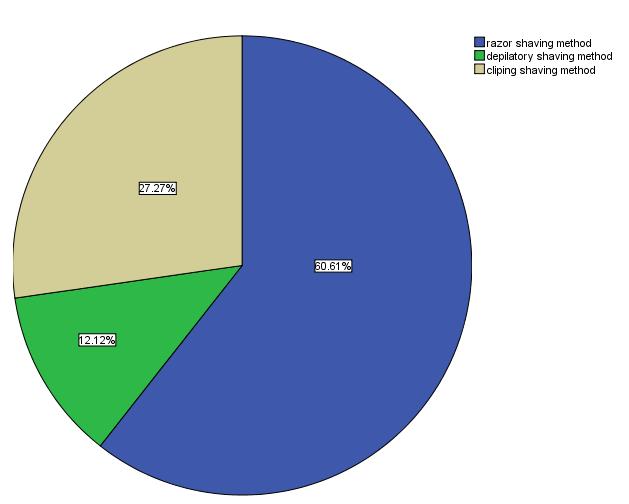
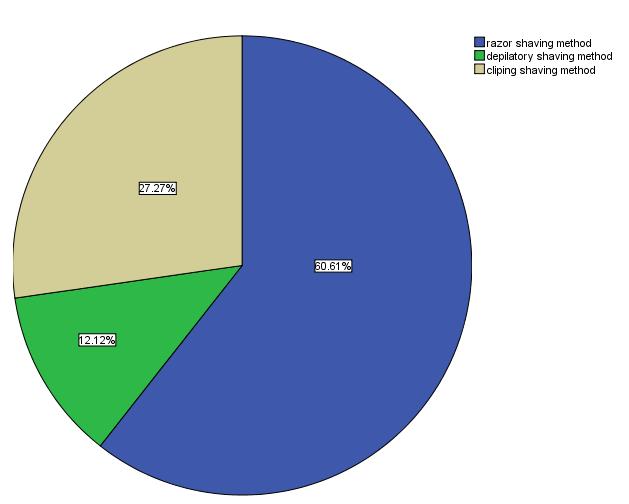
Respondents were given alternatives to choose which one is the best method of preoperative shaving. From figure 4 above, most of the respondents 20(60.6%)
thought shaving with a razor blade is the best followed by clipping shaving 9 (27.3%) and the least 4(12.1) chose depilatoryshaving.
41
FIGURE 4: Respondents’ responses regarding the best preoperative shaving method (n=33)
http://www.inosr.net/inosr-experimental-sciences/
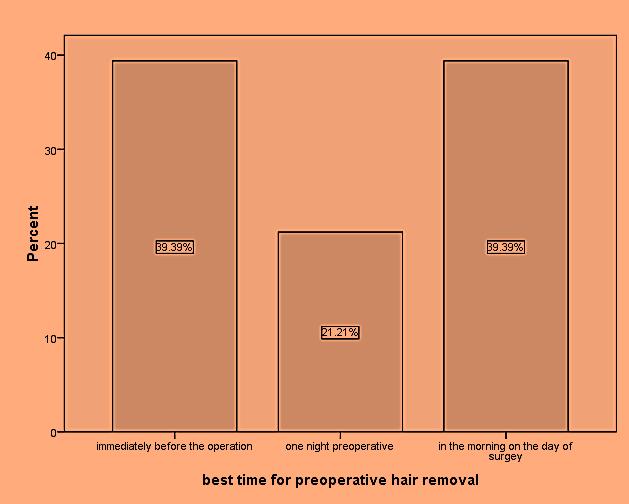
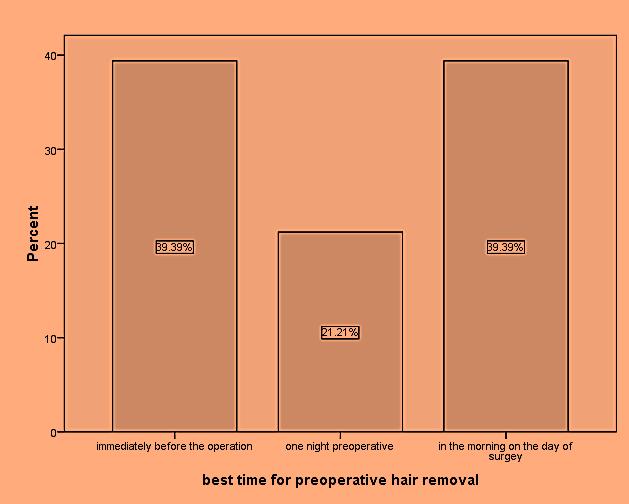
Respondents were asked to choose from the alternatives which one was the best time for preoperative hair removal. An equal proportion 13(39.4%) selected shaving immediately before surgery and
another 13(39.4%) chose shaving in the morning on the day of surgery, with least number respondents 7(21.2%) choosing shavingonenightpre-operative.
42
Figure5: respondent’s responses regarding best time for pre-operative hair removal (n=33)
http://www.inosr.net/inosr-experimental-sciences/
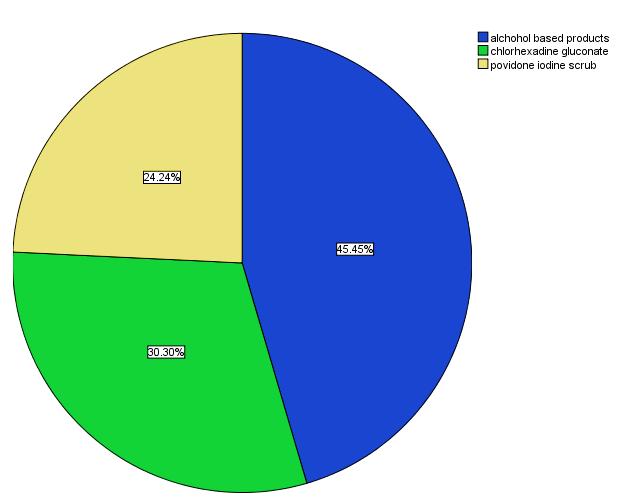
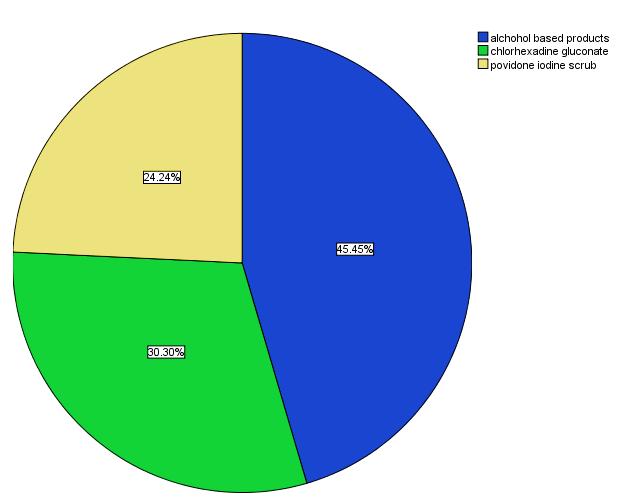
From figure 6 above, most 15(45.5%) of the respondents thought that alcohol based solutions are the best for preoperative skin preparation, followed by
10(30.3%)whothoughtthatchlorhexidine is the best and finally 8(24.2%) of the respondentsthoughtthatpovidoneiodine isthebest
43 n=45
Figure 6: Participant’s responses regarding the best agent for preoperative skin preparation
http://www.inosr.net/inosr-experimental-sciences/
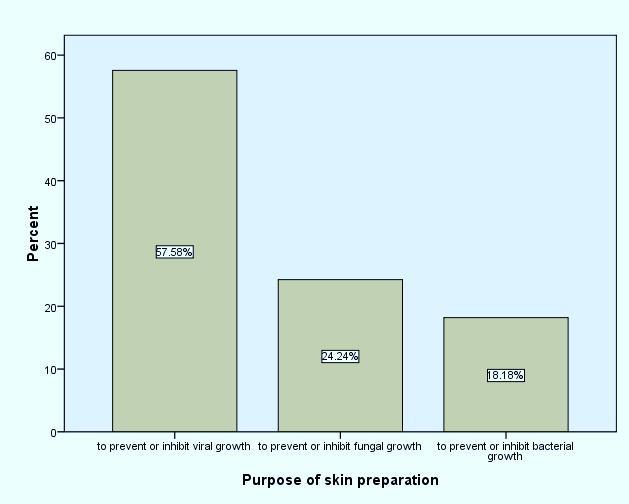
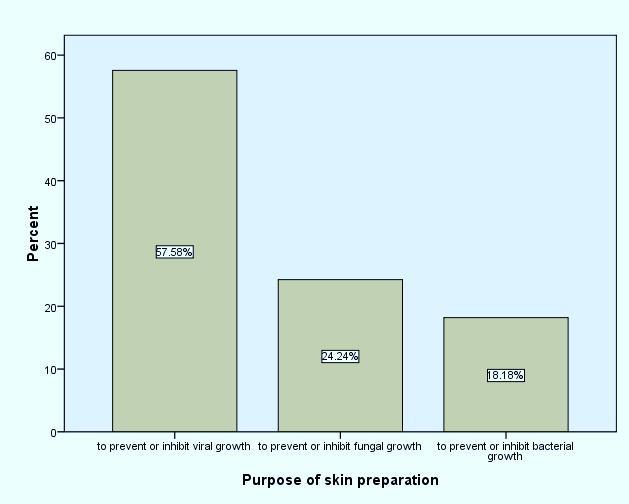
From figure 7 above most 19 (57.6%) of the respondents thought that preoperative skin preparation helps inhibit viral growth, 8(24.2%) thought it
helps prevent to inhibit fungi growth while 6(18.2%) correctly thought it inhibitsorpreventsbacterialgrowth.
44
Figure 7: Participants responses regarding the purpose of pre-operative skin preparation (N=45).
http://www.inosr.net/inosr-experimental-sciences/
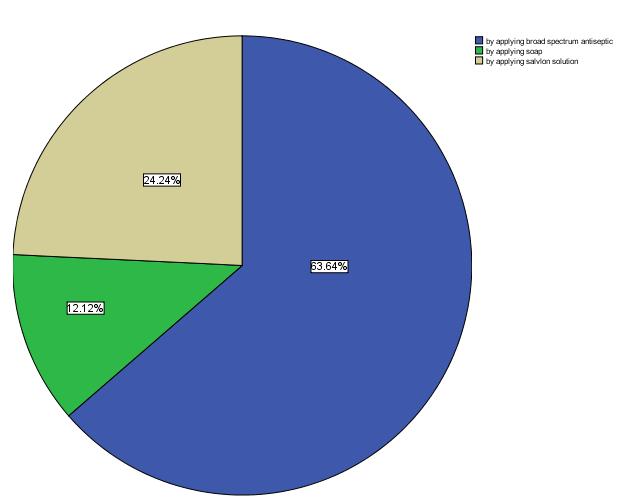
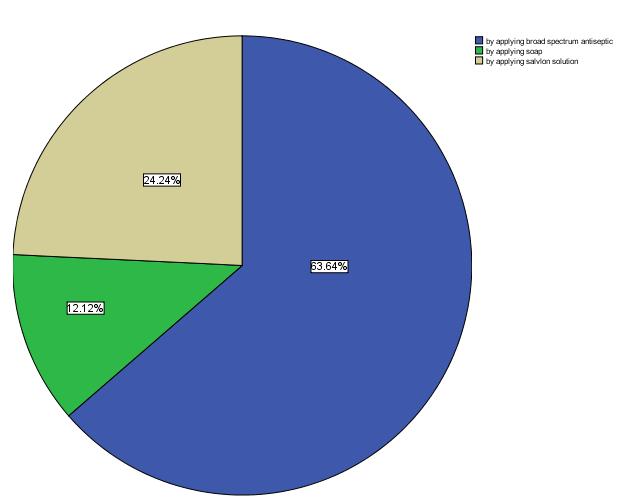
Participants were asked how they would disinfect a surgical site before the operation. From the figure above,
majority 21(63.2%) of respondents would use broad spectrum antiseptics, 8(24.2%) wouldusesavlonsolutionand4(24.2%).
45
Figure 8: Participants responses regarding surgical site disinfection before the operation(n=33)
http://www.inosr.net/inosr-experimental-sciences/
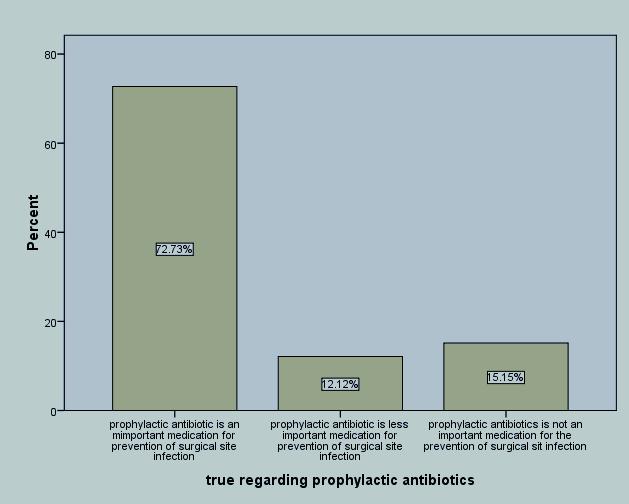
Figure 9: Participants’ choices regarding what is true about prophylactic antibiotics
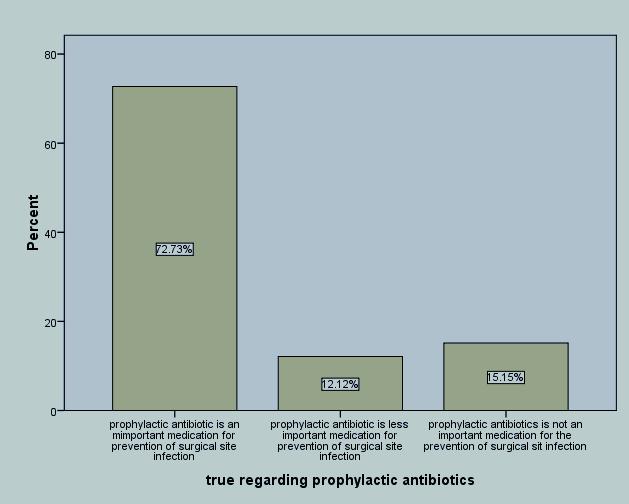
Respondents were asked to choose from the alternatives what is true regarding prophylactic antibiotics and from the figure above, overwhelming majority24 (72.7%) of the respondent indicated that
prophylactic antibiotics are important in prevention surgical site infection while 5(15.2%)oftherespondentsindicatedthat prophylactic antibiotics are not important inpreventionofsurgicalsiteinfection.
46
http://www.inosr.net/inosr-experimental-sciences/
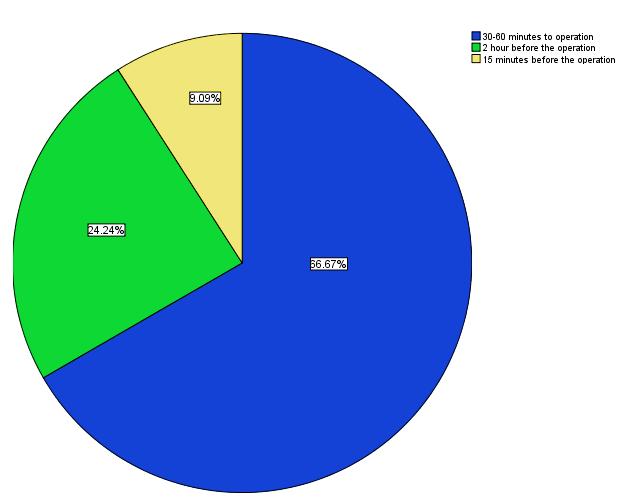
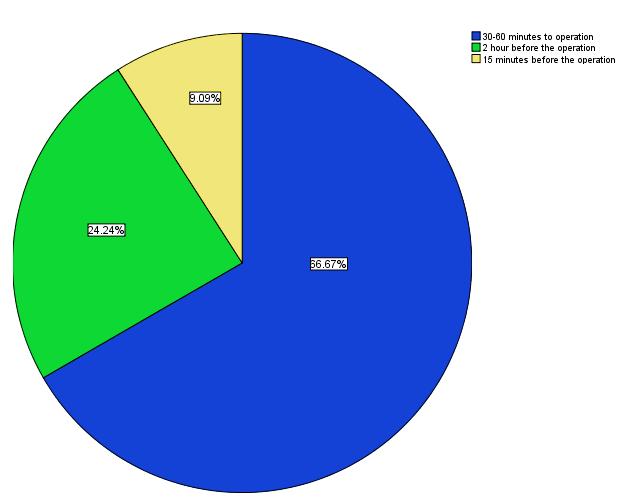
From the figure above, most 22(66.7) of the respondents would consider giving a prophylactic antibiotic 30-60 minutes
before surgery while only 8(24.2%) would give the prophylactic antibiotic 2 hours beforesurgery.
47
Figure 10: Participants responses regarding the appropriate time to administer prophylactic antibiotic before surgery
http://www.inosr.net/inosr-experimental-sciences/
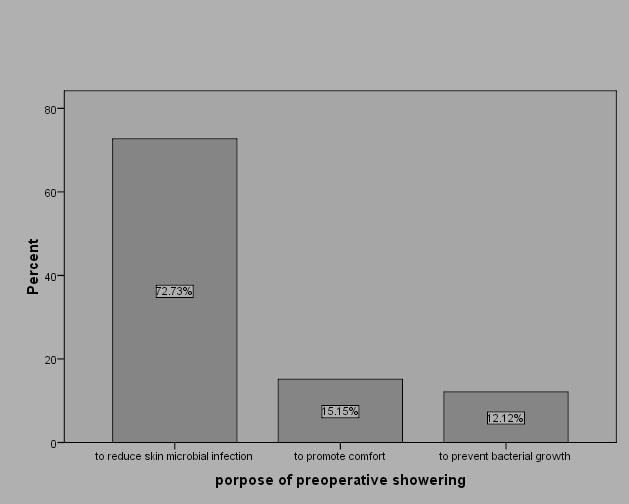
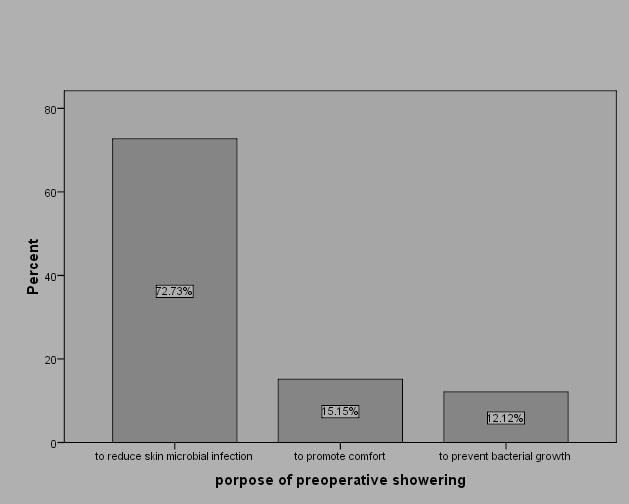
Participants were asked about the importance of preoperative showering. Most 24(72.7%) said it reduces skin microbial infection 5(15.2%) said it
promotes comfort of the patient while 4(12.2%) said it prevents bacterial growth ontheskin.
48
Figure 11: Participants responses about the importance of preoperative showering
http://www.inosr.net/inosr-experimental-sciences/
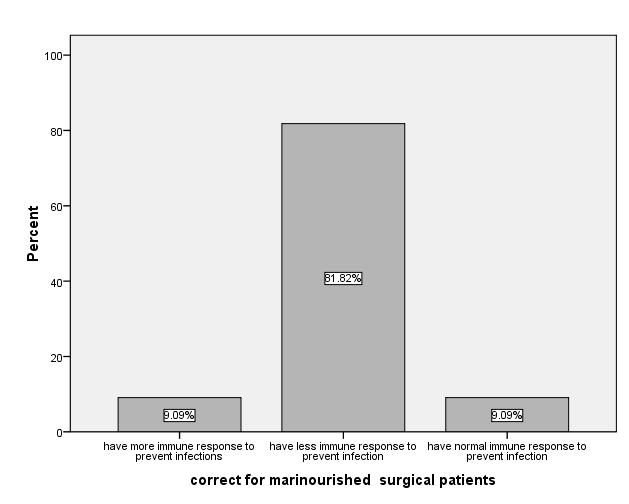
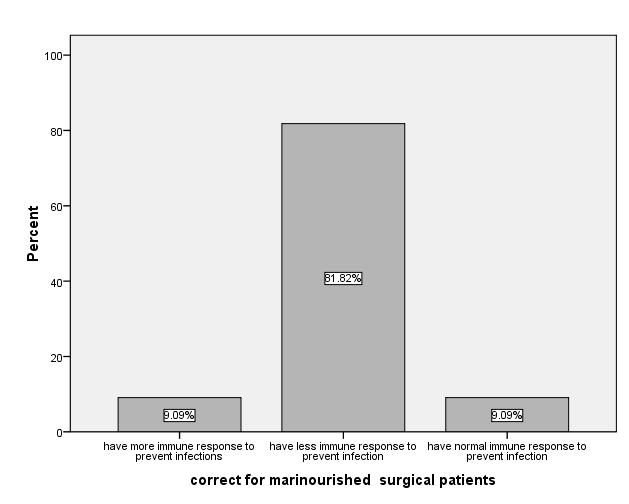
Participants were asked to choose from alternative what is correct regarding malnutritionAmongsurgicalpatients,and majority 27 (81.8%) correctly said that these patients have compromised
immunity to prevent infection while 3(9.1%) saidthatthe patients have normal immune response to prevent the infections.
49
Figure 12: Participant responses on malnutrition affect the immunity of a patient undergoing surgery
http://www.inosr.net/inosr-experimental-sciences/
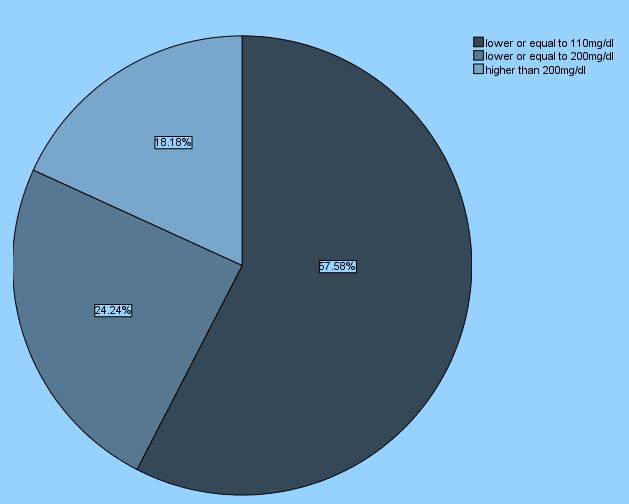
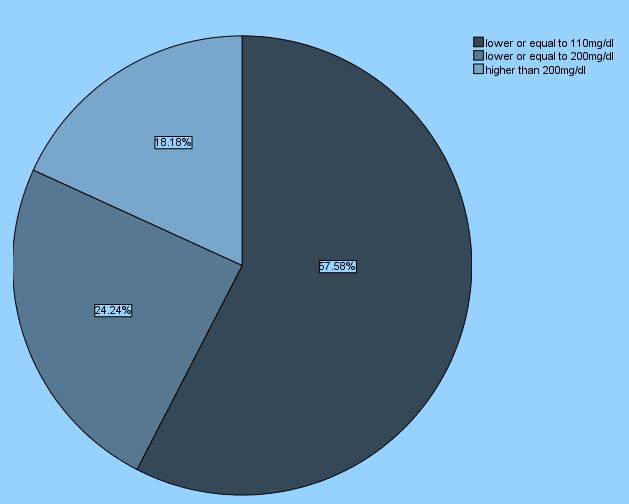
Majority19(57.58%) of the respondents thought blood sugar less or equal to 110mg/dl is appropriate while 6(18.2)
thought blood sugar level should be higher than 200mgdl to enhance white bloodcellfunctioning.
50
Figure13: Participant responses about what level of blood sugar that is appropriate for normal white blood cell function.
http://www.inosr.net/inosr-experimental-sciences/
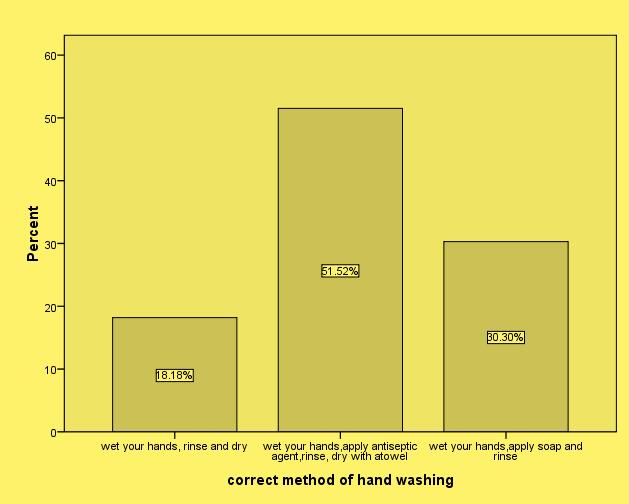
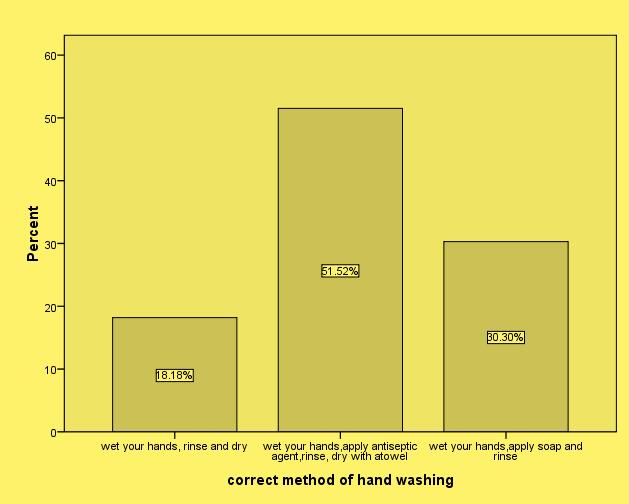
From the figure above, most 17(51.5%) of the respondents would wet their hands, apply antiseptic agent, rinse and dry with
a towel, 10 (30.3%) would wet hands, apply soap and rinse and 6 (18.2) would wethands,rinseanddry.
51
Figure 14: Participants responses regarding the correct method of hand washing.
http://www.inosr.net/inosr-experimental-sciences/
Participants responses regarding the benefits of wound dressing
Most 20(60.6%) of the respondents that wound dressing absorbs exudates, 7(21.2%) said wound dressing doesn’t
absorb exudates while 6(18.2%) said wounddressingreducespain.

52
Figure15:
http://www.inosr.net/inosr-experimental-sciences/
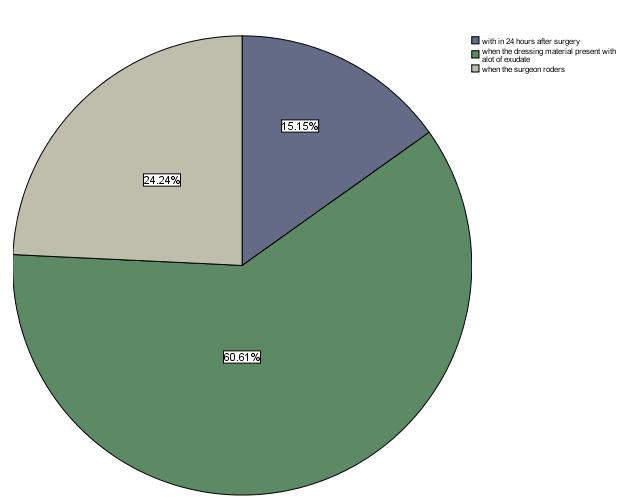
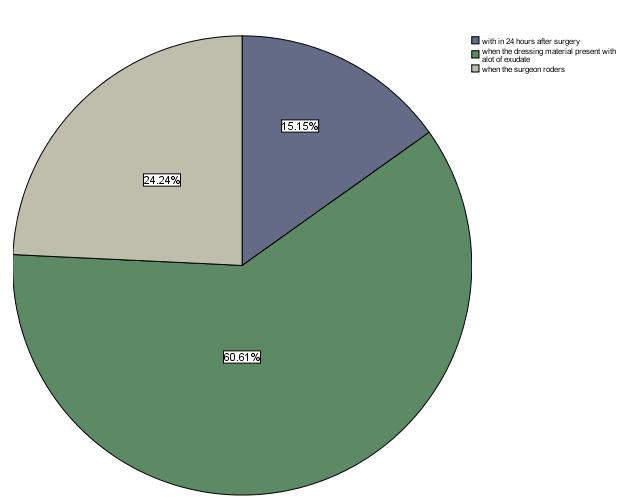
Figure 16: Respondents responses about when they would change a wound dressing
From figure 15 above, most 20(60.6%) of the respondents would only change the wound dressings whenever they are performing wound dressing procedures
while 8(24.2%) would only change the dressings whenever the surgeons order themtodoso.
53
http://www.inosr.net/inosr-experimental-sciences/
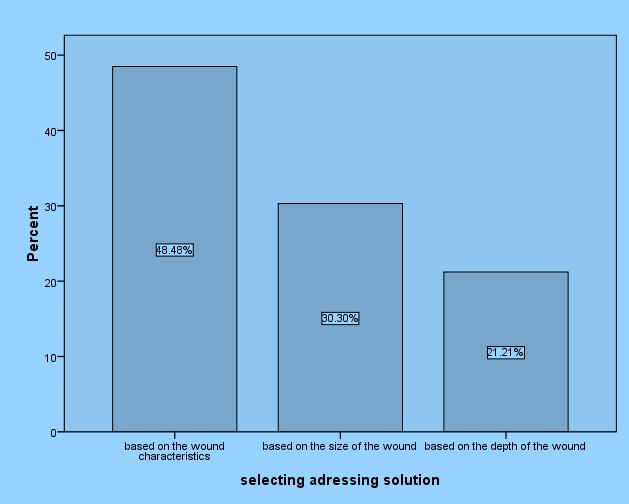
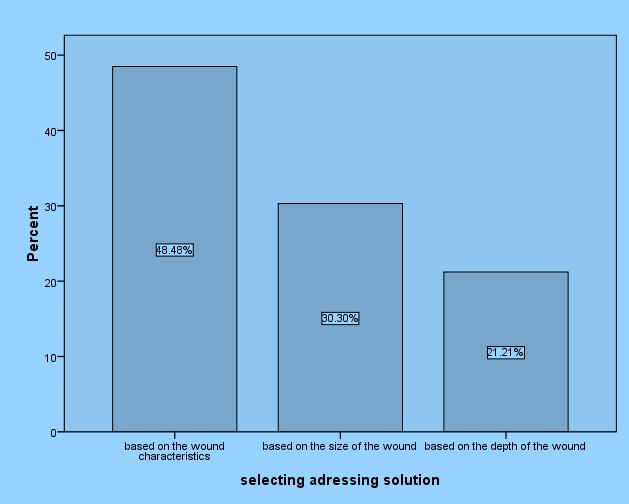
Most 16 (48.5%) of the respondents would chooses a dressing solution basing on the wound characteristics while 10(30.3%) would choose the dressing solution
depending on the wound size, and 10(21.2) would base on the depth of the wound.
54
Figure 17: Participants responses regarding how they would choose addressing solution
http://www.inosr.net/inosr-experimental-sciences/
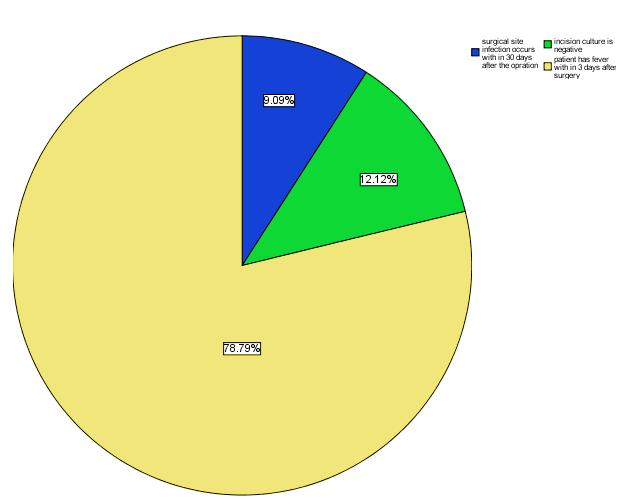
Participant were also giving alternative statements and were require to choose one that was correct regarding the diagnosis of surgical site infection. From figure 17 above, majority 26 (78.8%) of the respondents, would diagnose SSI
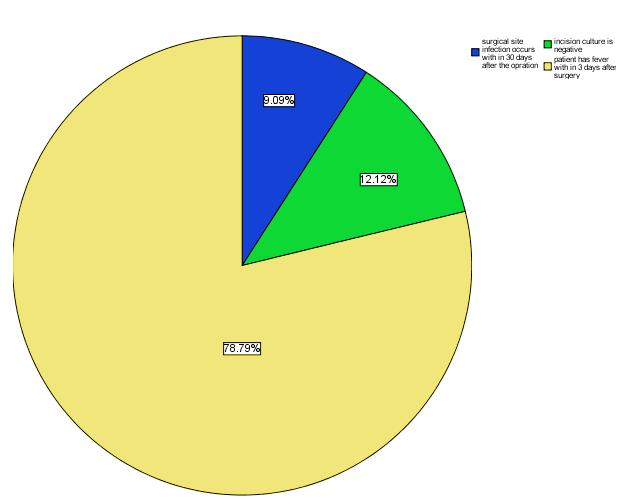
when the patient has fever with 3 day after surgery, 4(12%) would only diagnose SSI when the in cisional culture is negative and 3(9.1%), know that it occurs with30daysaftersurgery.
PRACTICES OF NURSES REGARDING SURGICAL SITE INFECTION PREVENTION
Table3: Participant’s responses about use of alcohol and chlorhexidine gluconate for preoperative skin preparation. N=33
55
Figure 18: participant responses regarding the correct diagnosis of surgical site infection
Participants response Frequency(n) Percentage (%) Never practice 0 0 Seldompractice 3 9.1% Sometimespractice 6 18.2 Alwayspractice 24 72.7% Total 33 100
http://www.inosr.net/inosr-experimental-sciences/
Table 4: Participants responses regarding the practice of hand washing during wound care procedures
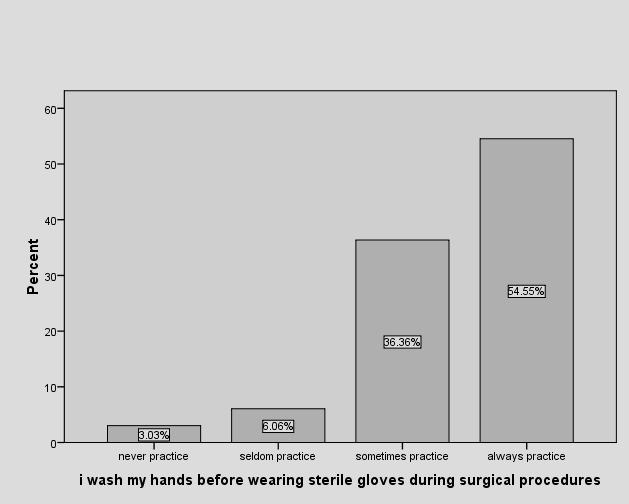
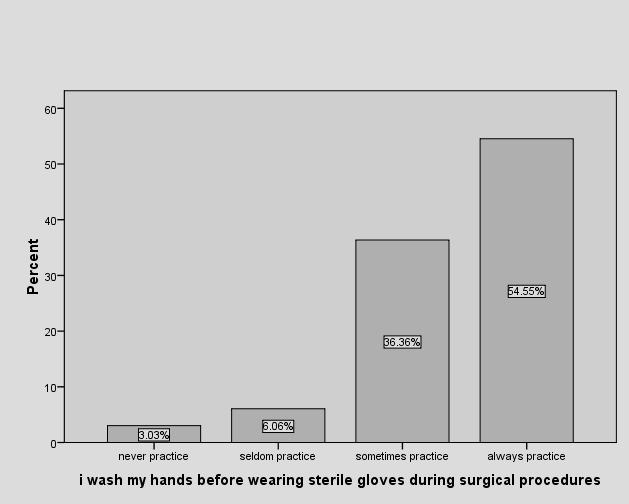
Participants were asked about their practice regarding use of surgical gloves and hand washing; from figure 18 above, majority18 (54.5&) always wash hands
before wearing sterile gloves,12 (36.4%) sometimes wash hands before putting on sterile gloves,2(6.1%) seldom practice and1(3%)neverpracticeso.
56
N=33 Participants response Frequency(n) Percentage (%) Never practice 0 o Seldompractice 2 6.1 Sometimespractice 10 30.3 Alwayspractice 21 63.6 Total 33 100
Figure19: Participants responses about practice of washing hands before wearing sterile gloves during wound dressing.
http://www.inosr.net/inosr-experimental-sciences/
TABLE 5: Participants responses regarding performance of pre-operative shaving right before surgery.
Majority 18(54.2%) of the respondents sometimes perform pre-operative shaving right beforesurgery.
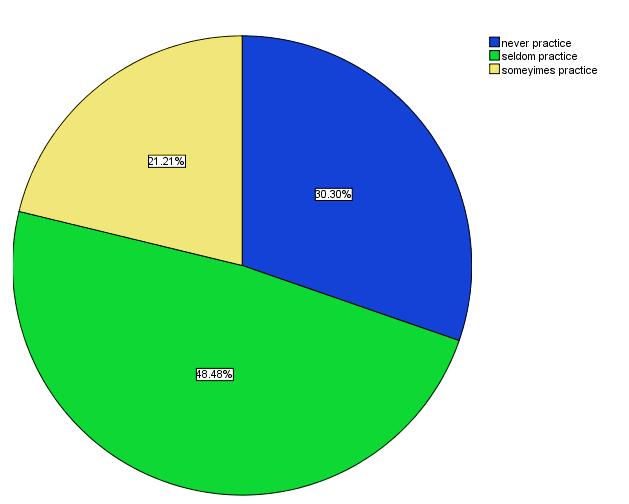
Table 6: Participant’s responses about administration of prophylactic antibiotics one hour before surgery
From table 7 above, most 24(72.7%) only administer prophylactic antibiotic one hour before surgery on some occasions,
3(9.1%) seldom practice, 2(6.1%) never practiceandonly4(12.1)alwayspractice.
57
Participants response Frequency(n) Percentage (%) Never practice 5 15.2 Seldompractice 8 24.5 Sometimespractice 18 54.5 Alwayspractice 2 6.1 Total 33 100
Participants response Frequency(n) Percentage (%) Never practice 2 6.1% Seldompractice 3 9.1% Sometimespractice 24 72.7 Alwayspractice 4 12.1 Total 33 100
Figure 20: Participants responses on whether they advise the patients to take a shower 6-12 hours before surgery (N=33).
http://www.inosr.net/inosr-experimental-sciences/
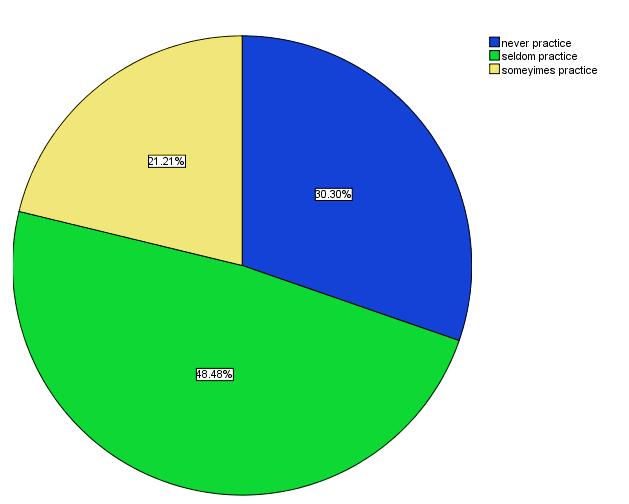
Almost half,16(48.5%) of the respondents advises patients to take shower 6-12 hours before surgery on rare occasions,10(30.3%) never do so, while
therewasnoparticipant0(0%) whoalways advises patients to take a shower 6-12 hoursbeforesurgery.
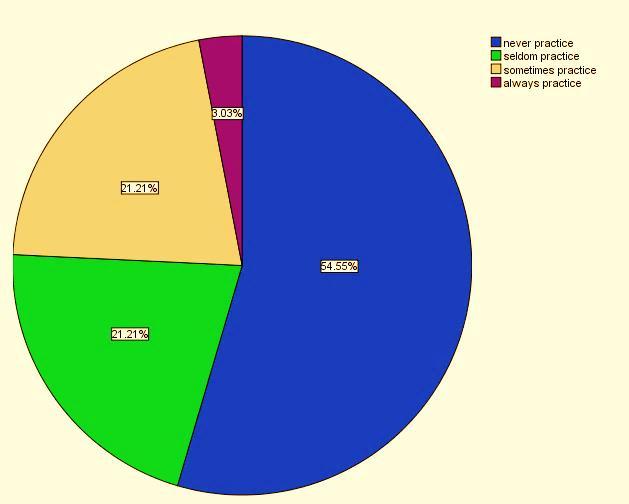
Figure 21: Participants responses on BMI assessment before and after surgery
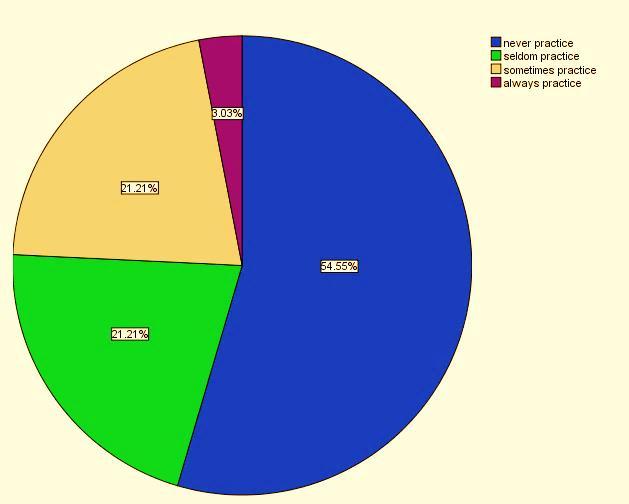
From figure 20 above more than half 18 (54.5%) of the respondents never assess their patients BMI before and after
surgery while only 1(3.0%) of the respondents always assess the patients BMIbeforeandaftersurgery.
Table 7: Participant’s responses regarding to whether they always use sterile materials for wound dressing
From table 7 above, it is evident that majority15 (45.5%) sometimes uses sterile materials in wound care, followed by
14(42.4%) who always use sterile materialsinwounddressing.
58
Participants response Frequency(n) Percentage (%) Never practice 2 6.1 Seldompractice 2 6.1 Sometimespractice 15 45.5 Alwayspractice 14 42.4 Total 33 100
http://www.inosr.net/inosr-experimental-sciences/
Table
From table9 above, only 5(15.2%) of the participants always use aseptic technique during wound dressing while majority
26(78.8%) use aseptic technique some times.
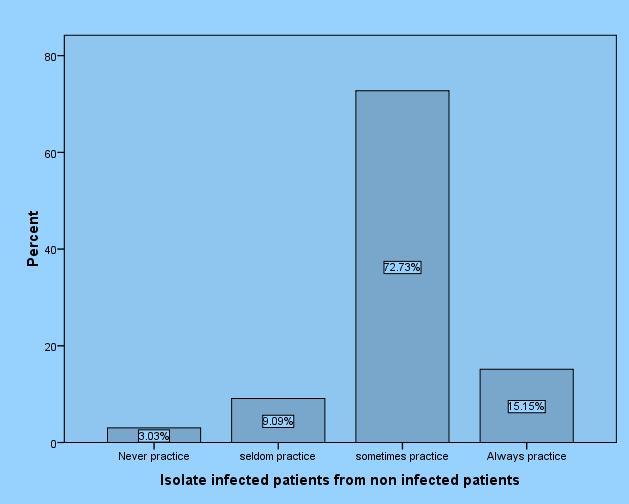
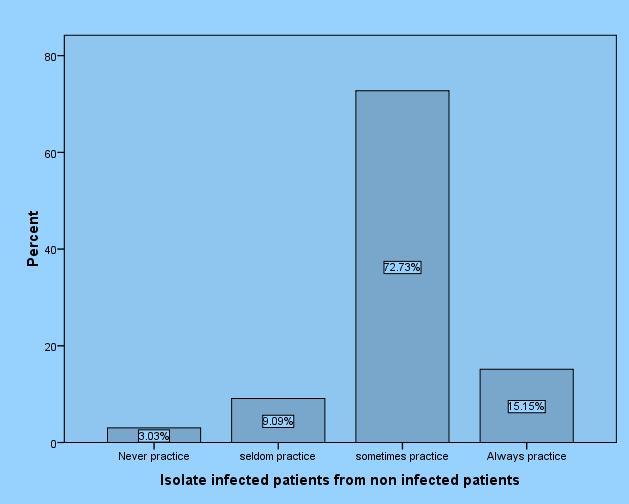
Respondents were asked whether they have a practice of isolating surgical infected patients from non-infected ones; from the figure above it is evident that
majority24(72.7%)do sosometimes while only5(15.2%) always separate infected patientsfromnon-infected.
59
Participants response Frequency(n) Percentage (%) Never practice 1 3 Seldompractice 1 3 Sometimespractice 26 78.8 Alwayspractice 5 15.2 Total 33 100
8: Participants responses on use aseptic technique (nontouch method) during wound dressing
Figure 22: Participants responses on isolation of surgical infected patients from noninfected ones
http://www.inosr.net/inosr-experimental-sciences/
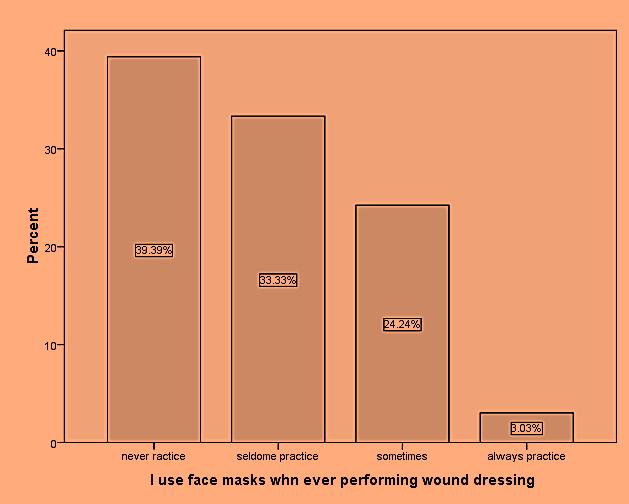
Figure 23: Participants responses on use of face masks during wound dressing
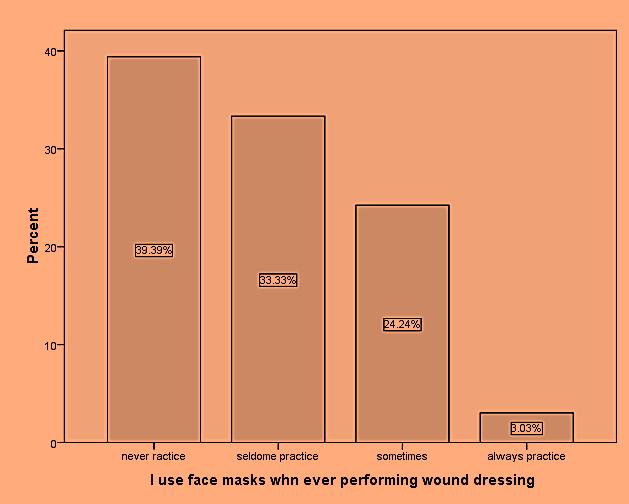
From the figure 22 above, majority 13(39.4%) said the never use masks during wound dressing, 11(33.3%) use
masks on rare occasions and only 1(3.0%) always use masks during wounddressing.
60
http://www.inosr.net/inosr-experimental-sciences/
Most 16(48.5%) of the respondents disinfect dressing trolley before wound dressing sometimes while 11(33.3%) always disinfect dressing trolley before
wound dressing,2 (6.1%) admit to have never disinfected dressing trolley before wounddressing.

61
Figure 24: Participants responses on disinfection of dressing trolley before wound dressing
Response Frequency(n) Percentage Neverpracticed 0 0 Seldompractice 0 0 Sometimespractice 05 15.2 Alwayspractice 28 84.8 Total 33 100
Table 9: Participants responses on appropriate waste disposal after wound dressing
http://www.inosr.net/inosr-experimental-sciences/
From table 10above, it is well shown that an overwhelming majority 28 (84.8%) of
the respondents always appropriately disposewastesafterwounddressing.
8(24.2%) of the respondents have never used separate dressing packs for each patient while performing wound dressing, 14 (42.4%) do so some times while only
Demographic characteristics
4(12.1%) always use separate sterile dressing packs for each patient during wounddressing.
DISCUSSION
Majority of the respondents16 (48.5%) fell in the age range 18-30 years, 13 (39.4%) were 31-40 years of age while only 4 (12.1%) were of age 41 and above. This is perhaps because Uganda has one of the youngest populations in the world and the even in the work force, it is expected that most of the workers are younger and this is also shown with the above finding where only 4(12.1%) of the respondents were above 41 years of age. The researcher was unable to find literature that classifies Ugandan work force in this casenursesbyage.
In this study majority of the respondents 21 (63.6) were females and 12 (36.4%) were male. This is because, traditionally, nursing id regarded as profession of females and so most of the time females are readily available to take up nursing jobs compared to their male counter parts. The researcher was unable to access records from the Uganda Nurses and Midwives council for comparison purposes to see which gender dominates theNursingprofession.
On the level of qualification, most of the respondents were 15(45.5%) were certificate holders, followed by diploma 13(39.4%), 5(15.2%) and none of the respondents had a master’s degree. This
could be due to the fact that there many trainings institution awarding certificates than diploma and bachelors, entry requirements for certificates are low and so the numbers are more. But also, it is important to note at this point that in Ugandasalaryisdeterminedbyoneslevel of education and so this implies that certificateholdersoffercheaplabourthan diploma and bachelor holders hence organization hire more of them in order to maximize profits and this probably explains why they dominated in this study. There is no literature available for comparisonwiththisfinding
In this study most 16(48.5%) of the respondents had an experience in service of1-5years,7(21.2%)hadworkedfor6-10 years and 5(15.2%) had worked for over 11years. If wearetogobythenumberof years spent in service to translate into experience in service delivery, then this study reveals that most of the respondentswerelessexperienced. Most 17(51.5%) of the respondents in this study were Anglican by faith, followed by Roman Catholics 8(24.2%), and 3(9.1%) were seventh Adventists. This also portrays the national picture because the majorreligionsinUgandaarecatholicand Anglican. There is no data showing
62
Response Frequency(n) Percentage (%) Neverpracticed 8 24.2 Seldompractice 7 21.2 Sometimespractice 14 42.4 Alwayspractice 4 12.1 Total 33 100
Table 10: participant’s responses on use of separate sterile dressing packs for each patient during wound dressing
http://www.inosr.net/inosr-experimental-sciences/
categorization of nurses according to theirreligions.
Knowledge of nurses on prevention of surgical site infection
Results from this study indicated that 9(27.3%) knew the recommended method of shaving while 24(72.7%) did not know therecommendedmethodofhairremoval before surgery;13 (39.39%) correctly on the best time pre-operative shaving(immediately before surgery) while 20(60.61%) did not know the recommended time for pre-operative hair removal;15(45.5%) of the respondents said alcohol based solutions are the best for pre-operative skin preparation while18(54.5%) did not know;6(18.1%) of the respondents knew the importance of pre-operative skin preparation while 27(81.82%) did not know;24(72.3%) said thatpreoperative prophylacticantibiotics are important in prevention of SSI. These agree with [22] “40 % to 60% of the SSI would be preventable with properly administered prophylactic pre-operative antibiotics; while 9(27.27%) thought preoperative antibiotics are not important in preventionofSSI;22(66.7%)Knewwhento give prophylactic pre-operative antibiotics, “timing of the antibiotic is considered critical for effective antibiotic prophylaxisis” [23] while 11(33.3%) did not know; 27(81.8%) knew the importance of pre-operative showering while 6(18.2%) did not know; 17(51.5%) knew the correct procedure of hand washing while 16(48.5%) did not know the correct procedure of hand washing; 20(60.6%) knew the importance of wound dressing while 13(39.4%) did not know the importance of wound dressing;20(60.6%) would correctly judge when to change the wound dressings while 13(39.4%)would not;16(48.5%) of the respondents would objectively based on the wound characteristics choose addressing solution while17(51.5%) would not; which agrees with [22] who stated “appropriate dressing materials should be selected according to the wound characteristics” only 3(9.09%) would correctly diagnose SSI while 30(90.9%) would not correctly diagnose SSI. From the above results, an
average of 16(48.5%) respondents had adequate knowledge on SSI infection prevention while an average of 17(51.5%) respondents had inadequate knowledge on SSI prevention. The above findings are similarto findings of [24] whose studyon knowledge and practices of nurses on SSI prevention in Bangladesh revealed low level of knowledge. Humaun, [24] in his sturdy also asserted that for effective prevention of surgical site infection, nurses should have sufficient knowledge and skills on pre-operative, intra operative and post-operative care of surgical patients for better outcome of the care. However, se this is direct oppositeofthefindingsofthissturdy Practices
of nurses regarding surgical site infection prevention
Approximately 25% infections could be prevented by nursing personnel by following proper precautions during nursing care to surgical patients [25] the findings from this study revealed differentlevelsofpracticesaboutsomeof the precautions taken during wound care procedures.
On use alcohol-based solution for preoperative skin care, majority 24(72.7%) always use and also there was high performance of hand washing before and after procedures at 21(63.6%) of the respondents.
There was low practice when it came to pre-operativeshavingrightbeforesurgery withan over whelming majority18 (54.5%) doing so only some times, and only2 (6.1%)alwaysperforming
On administration of pre-operative prophylactic antibiotics, only 4(12.1%) always do and majority24 (72.7%) only do sosometimes.
When it came to BMI assessment in surgical patients, level of performance was extremely poor standing at 1(3.03%) of the respondents and 18(54.5%) saying theyhaveneverpracticedthat.
On use of sterile materials during wound dressing, 14(42.4%) always do and 2(6.1%) said they have never; 5(15.2%) dress wounds using non touch technique and only 5(15.2%) always separate infected surgicalpatientsfromnon-infected
63
http://www.inosr.net/inosr-experimental-sciences/
Whenitcametouseofmasks,the levelof performance was so miserable, 13(39.4%) of respondents never using masks during wound dressing and only 1(3.03%) always usingmasks.
16(48.5%) of the respondents disinfect trolleys some times while only11 (33.3%) alwaysdisinfectthedressingtrolleys. This study also found out that there was no positive relationship between knowledge and practices which contradicts the findings of [27] whose study in India revealed appositive relationship between the two. This study alsorevealsslightlyhigherknowledgebut lowlevels of practices regarding infection
prevention. This contradicts the findings of [28] whose study on the same topic revealed low level of knowledge but higher level of practice regarding surgical siteinfection.
Williamson et al; [27] in their study found out that nurses who received higher level of education had higher levels of knowledge and practices on surgical site infection prevention. This was not the case for this study because there was no significant correlation between level of education of respondents and the level of knowledge and practices regarding surgicalsiteinfectionprevention
CONCLUSION
In conclusion, basing on the findings of this sturdy, nurses have low level of knowledge about prevention of infection of surgical sites. The areas thatregistered extremely poor knowledge were areas of wound assessment, pre-operative showering, timing and importance of preoperative prophylactic antibiotics and correct diagnosis of surgical site infection.
This sturdy also concludes that the level of practices of the recommended precautions as far as prevention of infection of surgical sites was low among nursing staff at KIU-TH. The areas that registered extremely poor practice included use of masks during wound care procedures, nutritional assessment (BMI) for surgical patients, and administration of preoperative prophylactic antibiotics, pre-operative shaving and use of separate sterile pressing pack for every patient duringwoundcare.
There was no positive relationship between knowledge and practices. The Nurse who knew the recommended precautions regarding surgical site infection prevention, did not necessarily practicethem
Recommendations
The Uganda nurses and midwives examination board that mandated under
Ministry of Education and sports to monitor the implementation of nursing curriculum should ensure that areas concerning infection prevention are sufficiently catered for in the curriculum as well as coverage during training of nursesandmidwives
For nurses that are already in service, arrangements should be put in place to take them through refresher courses in infection prevention with emphasis on surgicalsiteinfectionprevention. The hospital management should step up supervision of staff nurses on ward to ensure that the right things are being done and also avail the necessary items forinfection prevention if these problems aretobereduced.
Implications to nursing practice. Nurses are with patients all the time and soplayagreatroleinthehealingprocess. However with inadequate knowledge and skillsinsurgicalsiteinfectionprevention, they are handicapped and cannot be able to practice evidence based nursing care. Therefore, the stake holders at all levels should ensure that a nurse is empowered all round in order to perform their duties confidently and also improve patient outcomes regarding this area of surgical siteinfectionprevention
REFERENCES
64
1. Anderson, D. J. and Sexton, D. J. (2008). Epidemiology and pathogenesis of and risk factors for surgicalsiteinfection.
2. Danielson, L. R., Righter, K. and Humayun, M. (2009). Trace element chemistry of Cumulus Ridge 04071 pallasite with implications for main
http://www.inosr.net/inosr-experimental-sciences/
group pallasites. Meteoritics & PlanetaryScience,44(7),1019-1032.
3. Desa, A., Kadir, N. and Yusooff, F. (2012). Environmental Awareness and Education: A Key Approach to Solid Waste Management (SWM) – A Case Study of a University in Malaysia. 10.5772/48169.
4. Seltzer, A., Ng, J., Aeschbach, W., Kipfer, R., Kulongoski, J. T., Severinghaus, J. P., Stute, M., Wieser, M., Deshpande, R. D., Van Khoi, L., Schlosser, P., Love, A., Herczeg, A., Clark, J F. and Simpson, J (2021) Paleotemperature Records of the Last Glacial Maximum from Noble Gases in Groundwater. PANGAEA, https://doi.org/10.1594/PANGAEA.92
9176
5. Kiernan, M. (2012). Reducing the risk of surgical site infection. ÂNursing Times;108:27,12-14.
6. Macfie, J. (2013). The future of surgical training.British journal of hospital medicine (London, England: 2005),74(5),282–284.
7. Kochanek, K. D., Xu, J. Q. and Murphy, S.L. (2011) Deaths: Preliminary data for 2009. http://www.cdc.gov/nchs/data/nvsr/n vsr59/nvsr59_04.pdf
8. Sebat, F, Johnson, D, Musthafa, A A, Watnik, M., Moore, S., Henry, K. and Saari, M. (2005). A multidisciplinary community hospital program for early and rapid resuscitation of shock in nontrauma patients. Chest, 127:17291743.
9. Elixhauser, A, Steiner, C. and Harris, D R (1998). Comorbidity measures for use with administrative data.Med Care;36:8–27.
10.Levitt, H., Motulsky, S., Wertz, F., Morrow, S. and Ponterotto, J. (2017). Recommendations for Designing and Reviewing Qualitative Research in Psychology: Promoting Methodological Integrity.QualitativePsychology.4.
11.Nelson, S. and Patrica, W. (2011). Patient safety climate: variation in perceptions by infection prevention andqualitydirectors.volume2011
12.Chan, M F, Ho, A. and Day, M C (2008) Investigating the knowledge,
attitudes and practice patterns of operatingroomstafftowardsstandard and transmission-based precautions: results of a cluster analysis. J Clin Nurs,17:1051-1062.
13.Meeks, D W, Lally, K P and Carrick, M M (2011). Compliance with guidelines to prevent surgical site infections: as simple as 1-2-3? Am J Surg,201(1):76-83.
14.World Health Organization (2007). Collaborating center for patient safety solution,volume1(9).
15.World Health Organization.(2011) World health statistics 2011.World Health Organization.https://apps.who.int/iri s/handle/10665/44552
16.Abu, B. M. A., Reeve, N., Conkey, A. A. T., Macdonald, D. W. and Yamaguchi, N. (2017). Hedgehogs on the move: Testing the effects of land use change on home range size and movement patterns of free-ranging Ethiopian hedgehogs.PLoSONE12(7):e0180826. https://doi.org/10.1371/journal.pone. 0180826
17.Kilpatrick, K. (2013). Understanding acute care nurse practitioner communication and decision-making in healthcare teams.Journal of ClinicalNursing,22(1-2),168-179.
18.Kiernan, M (2012) Reducing the risk of surgical site infection. ÂNursing Times;108:27,12-14.
19.Oden, J. T. and Demkowicz, L. F.(2010). Applied Functional Analysis, SecondEdition.CRCPress.
20.Fisher, R A. (1935). The logic of inductive inference (with discussion).Journal of Royal StatisticalSociety,98:39–82.
21.Mangram, A., Horan, T., Pearson, M., Silver, L. and Jarvis, W. (1999). Guidelines for prevention of surgical site infection. Infection Control and Hospital Epidemiology, 20(4), 247 –278.
22.Lohsiriwat, V., Prapasrivorakul, S. and Lohsiriwat, D. (2009). Perforated Peptic Ulcer: Clinical Presentation, Surgical Outcomes, and the Accuracy of the Boey Scoring System in Predicting Postoperative Morbidity
65
http://www.inosr.net/inosr-experimental-sciences/
and Mortality.World J Surg33, 80–85. https://doi.org/10.1007/s00268-0089796-1
23.Goldberg, K. and Humayun, M. (2010). The Applicability of the Chemical Index of Alteration as a Paleoclimatic Indicator: An Example from the Permian of the Parana Basin, Brazil. Palaeogeography, Palaeoclimatology, Palaeoecology, 293, 175-183. http://dx.doi.org/10.1016/j.palaeo.20 10.05.015
24.Parvez,S,Malik,K A,AhKang,S.and Kim, H Y (2006) Probiotics and their fermented food products are beneficial for health. J Appl Microbiol 100:1171–1185
25.Williamson, D., Lynch-Wood, G. and Ramsay, J. (2006). Drivers of Environmental Behaviour in Manufacturing SMEs and the Implications for CSR. Journal of Business Ethics. 67. 317-330. 10.1007/s10551-006-9187-1.
26.Najeeb. N. and Taneepanichsakul. S. (2008). Knowledge, attitudes and practices of standard and transmission-based precautions of Drs and Nurses in tertiary and secondary health care setting of Maldives, JournalofResearch,45-48.
27.B Petrus, E Nzabandora, E Agwu (2022). Evaluation of the bacterial agents associated with PID among women of reproductive age at Kampala International University Teaching Hospital. IDOSR Journal of Biochemistry, Biotechnology and Allied Fields 7(1),64-74
28.N Gloria, AO Yamile, E Agwu (2022).Prevalence patterns of bacterial urinary tract infections among febrile children under-five years of age at Kampala International University Teaching Hospital. IDOSR Journal of Biology, Chemistry and Pharmacy 7 (1),41-55
29.B Petrus, E Nzabandora, E Agwu (2022).Factors associated with Pelvic Inflammatory Disease among Women
Attending the Gynecology Clinic at Kampala International University Teaching Hospital, Uganda. IDOSR Journal of Biochemistry, Biotechnology and Allied Fields 7(1),48-63
30.B Petrus, N Emmanuel, A Ezera (2022).Prevalence of Pelvic Inflammatory Disease among Women
Attending the Gynecology Clinic at Kampala International University Teaching Hospital, Uganda. IDOSR Journal Of Science And Technology 8 (1),38-46.
31.B Petrus, N Emmanuel, A Ezera. Bacteriology of Pelvic Inflammatory Disease among Women Attending the Gynecology Clinic at Kampala International University Teaching Hospital, Uganda. IDOSR Journal Of Experimental Sciences 8(1),1-14.
32.B Petrus, N Emmanuel, A Ezera (2022). Factors Associated With Pelvic Inflammatory Disease among Women Attending the Gynecology Clinic at Kampala International University Teaching Hospital, Uganda. IDOSR Journal of Science and Technology 8 (1),1-14.
33.AK Lauben, SA Wan, H Lule (2022).The perioperative factors following open inguinal hernia repair with MROP mesh versus Desarda technique at Kampala International University Teaching hospital IDOSR Journal of Experimental Sciences 8(1),15-30
66