http://www.inosr.net/inosr experimental sciences/ Banga etal
INOSRExperimentalSciences9(1):10 20,2022.
©INOSRPUBLICATIONS
InternationalNetworkOrganizationforScientificResearch ISSN:2705 1692 Evaluation of the proportion of in hospital mortality among children under five years of age admitted with Severe Acute Malnutrition (SAM) in the nutritional unit of Jinja Regional Referral Hospital Uganda.
Desire Ngudjolo Banga, Melvis Baren and Namale Vivian SsonkoDepartmentofMedicine,PaediatricsandChildHealthofKampalaInternationalUniversity Uganda
ABSTRACT
Mortality among children with severe acute malnutrition remains an immense health concern in the hospitals in Africa, but its attributes are not fully known various hospital settings. This study evaluated the proportion of in hospital mortality among children under five years of age admitted with Severe Acute Malnutrition (SAM) in the nutritional unit of Jinja Regional Referral Hospital Uganda. The proportion of mortality and the Comorbidities and associated with in hospital mortality among children under five years of age admitted with severe acute malnutrition at Jinja Regional Referral Hospital was evaluated. This was a hospital based analytical descriptive prospective cohort study conducted at in the nutritional unit of Jinja Regional Referral Hospital.This study was performedfromJuly to October 2019 with children under five years of age admitted withsevere acute malnutrition andtheircaregivers fromand their caregivers. A total of 338 children and their caretakers who met the criteria were consecutively enrolled into the study. Children were followed until discharge from the nutritional unit or until death. Data collected from questionnaires, WHO chart and culture media were entered into Microsoft Excel version 10 and imported into Stata 12 for data analysis.Allindependentvariables with p values ≤0.05 were entered into a multivariate model for comorbidities independently. Of the 338 children under 5 years of age enrolled, 49(14.5%) died. Although the majority children were diagnosed with dehydration, 128(37.9%) and pneumonia, 127(37.6%) and malaria, 87(25.7%).Anemia (aRR=2.9, 95%CI: 1.23 6.62, p=0.01), bacteremia (aRR=10.0, 95%CI: 3.62 29.01, p=0.01), HIV (aRR=4.8, 95%CI: 1.42 16.30, p<0.01), TB (aRR=4.3, 95%CI: 1.28 14.49, p <0.02) and shock (aRR=60.9, 95%CI: 9.05 410.28, p <0.01) were the Comorbidities significantly associated with a likelihood of mortality. This study has shown that there was a relatively high in hospital mortality of 14.5% among children under 5 years of age admitted with Severe Acute Malnutrition, with an increased risk among males, thoseadmittedforless than72hoursandpresentinganemia,bacteremia,HIV,TBandshock. Keywords: In hospital,mortality,childrenandSevereAcuteMalnutrition(SAM).
INTRODUCTION
Globally, approximately 52 million (8%) of children under the age of five years in 2011 were wasted and more than 70% were from Sub Saharan Africa and Asia [1]. Globally, severe acute malnutrition accounts for about 35 per cent of deaths among children below five years, stunting, severe wasting and intra uterine growth retardation are the major contributors to child mortality, accounting for about 2 million deaths annually [2]. SAM is the majorcause of morbidity for all age groups accounting for 11 per cent of the disease burden globally [3]. A study on mortality andmorbidityin under five years withSAM in Zambia showed a mortality of 46%, with children with marasmus having lowest survival. HIV infected children were 80% more likely to die compared to uninfected
children while diarrhea and pneumonia were the most common comorbidities [4]. Since the study was a retrospective quantitative review of hospital based records, the sample collected could have had some of the records missing or with incomplete information. There is also a possibility that some registers and files could have been missing from the ward, which could have led to missing data for most of the variables. The current study was a prospective cohort study, the likelihood of missing records was minimized since the study participants were followed up from the first day of admission.
In a four year retrospective study on children with severe acute malnutrition in Ethiopia, it was found that among the
principal causes of death in young children, 60.7% of deaths from diarrhea, 52.3% from pneumonia, 44.8% from measles and 57.3% from malaria were attributable to malnutrition [5] Also, a study in Kenya found a proportion of 15.8%, 19.5% and 15.6 respectively, in children 1 59 months, 1 5 months and 6 59 months, among children hospitalized with SAM in clinical information network hospitals [6] Another study by [7] in Sudan showed a mortality rate of 9.3% among children with SAM [7]. The trends of mortality due to SAM vary irregularly across the different countries, which could have been due to the difference in the quality of medical interventions employed and the expertise of the health professionals involved in care of the children withSAM.Another possible reason for the variation in the trend of mortality could be due to the different study settings.
A prospective study from Uganda showed a proportion of 9.8% among children with severe acute malnutrition during in patient therapeutic care [8] Another study on treatment outcome among children with severe acute malnutrition in Lacor hospital in Northern Uganda revealed a proportion of 11.9%; hypothermia and HIV were the factors strongly associated with mortality, and infections were major contributors to mortality[9].This underscorestheneedfor improved prevention and management of these infections among children with severe malnutrition. Both the two studies
Study design
were carried out in central and northern regions, respectively, where the proportion of mortality was found to be high. Since our current study was done in Jinja Regional Referral hospital, it provided information about the proportion of death under five due to SAM in the eastern region of Uganda. The study design used was similar to the one that was used by [8] at Mulago except that her study was nested in a randomized controlled trial, investigating the effect of probiotics on diarrhea among children admitted with SAM. Also, their study did not capture the history of vomiting and immunization status of the child which were captured by this current study.
Aim of the Study
The aim of this study was to evaluate the proportion of in hospital mortality among children under five years of age admitted with Severe Acute Malnutrition (SAM) in the nutritional unit of Jinja Regional Referral HospitalUganda.
Specific objective
1. To determine the proportion of in hospital mortality among children under five years of age admitted with SAM in the nutritional unit of JinjaRegionalReferralHospital.1.4
Research questions
1. Whatis theproportion ofin hospital among children under five years of age admitted with SAM in the nutritional unit of Jinja Regional ReferralHospital?
METHODOLOGY
This was an analytical descriptive prospective cohort study to determine the proportion of mortality, demographic, biological and associated with mortality among children below 5 years admitted with severe acute malnutrition in the nutritional unit of Jinja Regional Referral Hospital.
Study site
The study was conducted at Jinja RRH. Jinja RRH is located in South eastern Uganda, approximately 87 kilometers East of Kampala, the capital of Uganda. The coordinates of Jinja hospital are; 00 25 52 N, 33 12 18E (Latitude; 0.4310; Longitude 33.2050). Jinja district sits along the northern shores of Lake Victoria, near the sourceof theWhite Nile andhasanaverage elevation of 1,204 meters above sea level. It is bordered by Kamuli district to the north, Luuka district to the east, Buvuma district to the south, and Buikwe district to thenorth west.Itisadesignatedinternship hospital where medical graduate internship
centre and has several consultant staff and specialists in medical and surgical disciplines. Jinja RRH, also provides comprehensive HIV/AIDS services. It is also a KIU Satellite Teaching Hospital aimed at training undergraduates and postgraduate students including postgraduate in Pediatrics. The nutritional unit is in pediatric ward,around 1km from the main hospital, it has 32 beds and 3 trained nurses assigned for the ward. Patients are categorized into moderate acute malnutrition, severe acute malnutrition, and edematous and non edematous malnutrition withaminimumof 60admissionspermonth.
Study population
The study included all children under five years of age admitted with SAM in the nutritional unit of Jinja Regional Referral Hospital and their caregivers. According to the 2014 census data, Jinja RRH serves a population of 471,242 in Jinja district,and the hospital also serves Bugiri, Kamuli, Iganga, Mayuge, Namutumba, Kaliro,
Buyende, Luuka, Namiyongo and Jinja district.
Selection criteria
Inclusion criteria
All children under five years of age admitted with severe acute malnutrition in the nutritional unit of Jinja Regional Referral Hospital and their caregivers who consentedwereincludedinthisstudy.
Exclusion criteria
Those who were referred for further management were excluded from this study. Also, children with pre existing congenital malformations, and cerebral palsywereexcludedfromthisstudy.
Sample size estimation
Sample size calculation was done using a formula for estimating a population proportion(DanielWW,1999).
n = Zα/2 2 *p*(1 p) / MOE2 , And
Zα/2 is the critical value of the Normal distribution at α/2 (e.g. for a confidence level of 95%, α is 0.05 and the critical value is1.96), MOE is the margin of error, estimated at 0.05
P is the estimated proportion of children with SAM that died in hospital= 0.33 based onastudy donein Kenyathatreported33% (TalbertAlisonetal.,2012)
n= 1.962 x 0.33 (1 0.33) /0.052 = 339.7 = 340 children with Severe Acute Malnutrition.
Estimating the sample size for the socio demographic, biological and economic factors associated with mortality among children under five years of age with severe acute malnutrition in the nutritional unitcare.
Using the modified Daniel’s formula n = Zα/2 2 *1 /R*P (1 P)/ d2 Where n=desiredsamplesize
Z= value corresponding to 95% confidence interval=1.96
R= Odds ratio for the SAM mortality according to the socio demographic factors associated with mortality in children under five years of age with SAM that died in hospital based on a study done in Uganda (Mulago) that reported an OR=1 in females (Bachouetal,2006)
P= proportion of mortality among females under five years admitted with SAM based ontheabovestudywas 0.25. d=degree of error to be accepted which is 5%.
n= 1.962 *1 /1*0.25 (1 0.25)/ 0.052 =147 children under five years of age admitted withSAM.
Estimating the sample size for the co morbidities associated with mortality of children under five years of age admitted withSAMinthenutritionalunitcare.
Using the same modified Daniel’s formula n = Zα/2 2 *1 /R*P (1 P)/ d2 Where: n=desiredsamplesize Z= value corresponding to 95% confidence interval=1.96
R= Odds ratio for children with SAM mortality according to the associated co morbidities based on a study done in Mulago that reported an OR=3.62 of children with HIV that died of SAM (Nabukeeraetal.,2018).
P= proportion of mortality among HIV patients with SAM in the nutritional unit basedontheabovestudywas0.34. d= degree of error to be accepted which is 5% n = 1.962 *1 /3.62*0.34 (1 0.34)/ 0.052 = 95 children under five years of age admitted withSAM.
The overall sample size is 340 children underfiveyearsofage admitted withSAM.
Sampling technique
All children under five years of age admitted with SAM in the nutritional unit of Jinja Regional Referral hospital, who met our inclusion criteria were consecutively enrolled into the study until when the requiredsamplesizehasbeenattained.
Data collection tools
The following tools will be used to collect data: questionnaires, tape measure, thermometer, pediatric size stethoscope, stadiometer, infantometer, WHO chart, vacutainers, gloves, and syringes, culture medium.
Study procedures
Screening for eligibility
Screening and inclusion were performed upon admission of the child in the paediatric ward as long as they met inclusion criteria. The principal investigator explained the purpose and the process of the study to the patient and/or guardian and a written consent was obtained.
Demographic information and biological information
Information regarding the place of residence, sex, age and date of birth and relationship of the child with the caretaker were collected by the principal investigator
using the data collection tool. Complaints of diarrhea, vomiting, loss of appetite, fever, cough and others were also recorded in the data collection tool as well as the child’s immunization history, nutrition history, HIV status, occupation of the caretaker. All information obtained was entered in the data collection tool. The emergency cases were managed first; information fromthemwascollectedlater.
Clinical examination
Children underwent general examination with special emphasis on temperature, presence of visible wasting, presence of edema, dehydration, eye signs of vitamin A deficiency and pallor, respiratory distress, tachypnea, some dehydration was distinguished from septic shock according to the WHO protocol. Systemic examination was done with special emphasis on the respiratory, cardiovascular system where pulse rate, capillary refill time, temperature gradient in the limbs were assessed and the central nervous system where the level of consciousness was noted. Pulse rate and oxygen saturation were taken using a pulse oximeter. Findings on clinical exam were entered in the data collection tool by the principal investigator; they helped to diagnose some comorbidities. All the patients were followed up from admission to the discharge with the clinical care pathway form(AppendixV).
Sample collection and laboratory procedures
Blood sample was collected during insertion of IV cannula for measurement of full bloodcount,blood glucose,bloodslide for malaria and HIV test and culture. Prior to drawing of blood, the area will be swabbed with cotton dipped in ethyl alcohol 70% and iodine to prevent contamination. Three to four milliliters of blood were drawn for blood culture, determination of blood glucose, full blood count, HIV test and blood slide for malaria and serum electrolytes. The blood sample for culture was taken and analyzed using Automated Blood Culture System (BACTEC) in the main hospital laboratory of JRRH. These laboratory investigations were done on admission except serum electrolytes that was done during transition phase. For the HIV test, pre and post test counseling were done. A first Determine® HIV rapid test was performed and confirmed with a 2nd rapid test StatPak®. In case of discordance, a Unigold® test will be done.
Children under 18 months with positive rapid tests will be referred for DNA PCR testintheHIVclinicin theJinjaRRH.Blood samples will be taken off only once at admission.
Full blood count was analyzed using Sysmex® Automated Hematology Analyser at Jinja RRH. Blood glucose was measured using Freestyle optium glucometer by the principal investigator at admission. Thick blood smears for malaria parasites was done using Field stains A&B and examined by a Laboratory technician using the microscope in the pediatric ward laboratory. Early morning gastric aspirate was collected in a sterile for gene expert at admission. The sample was taken to the pediatric ward laboratory of JRRH for analysisatadmission.
Patient management
Children with severe acute malnutrition were treated according to updated WHO guidelines. Prescription of treatments for the participants was done by doctors and clinical officers who were availed with guidelines on treating children with SAM. The role of the principal investigator was limited on recommendations. All children were routinely treated with IV Ampicillin and IV Gentamycin that was modified according to the blood culture and sensitivity results. They were also routinely started on a feeding program with F75 formula feeds. Caretakers took the responsibility for the feeding of the children under the supervision of the hospital Nutritionist. Children with diarrhea were routinely given Zinc tablets in addition to the routine deworming tablet that was given to all the enrolled patients. Those with some dehydration were given ReSoMal solution while those with septic shock were given IV half strength Darrow’s and 5% Dextrose solution. All patients were followed up from admission to the dischargeaccordingtotheWHO protocol
Data management
Hard copy questionnaires were kept in lockable safes. Data was checked manually by the principle investigator to verify the completeness of information. Where missing information was found, the principle investigator cross checked to find out whether the information was indeed missing from the field. The data was entered and cleaned using EPI info version 7 and was exported to STATA 12.0 for further analysis. The data was kept in a password protected computer to avoid
unauthorized persons from accessing it. The data was made accessible to authorized persons like the biostatistician, research supervisors, hospital administrators and any other authorized person. Descriptive statistics like frequencies, percentages and means was calculated.
Data analysis
Characteristics of study participants: Socio demographic were summarized descriptively as frequencies, percentages (categoricalvariables).
In hospital mortality was analyzed as frequency and percentage and presented in apiechart.
Ethical considerations
Forthestudytobeethical,thefollowing wasconsidered.
Institutional consent
Approval was sought from the Research and Ethics Committee of Kampala International University and also by the hospital administration of Jinja RRH where theresearchwascarriedout.
Privacy and confidentiality
Allquestionnairesdidnothaveprovisions for participant’s names, and participants willbeinterviewedseparatelyfromother
clientstomaintainprivacyand confidentiality.
Informed consent
Written consent was obtained from the parents or caretakers of the participants. Forparentorcaretaker who does not know how to read and write, the consent form was translated in local language (Lusoga) and we identified a witness who had to explain the consent form to him/her after which the parent/caretaker gave consent using his/her thumbprint. Mothers who were emancipated minors gave their consent after being clearly informed about the risks and benefits of the study by the principal investigator. Pre and post test counselling for HIV were performed separately by the Research nurse. Written consent for HIV testing was obtained on a specific form. The refusal of HIV test by the parent/caretaker did not stop the participant from getting care. Informed consent was sought from the attendant of the participants after clearly explaining the purpose of the study. Participation was voluntary and parents or guardians were free to refuse to participate or withdraw from the study without any penalties.
PRESENTATIONANDINTERPRETATIONOFTHERESULTS
Study profile of study participants
Overall, 340 participants under 5 years of age with severe acute malnutrition were consecutively enrolled in the study in the nutritional unit of Jinja Regional Referral Hospital after an informed consent of their caregivers from July to September 2019. Of the 340 participants, 2 participants were excluded from the study because of refusal
to consent. A total of 338 participants were followedupfromadmissiontodischarge A total of 49 participants died and 289 participantssurvived.
340 Participants under 5 years of age admitted with Severe Acute Malnutrition
2 Participants were excluded as caregivers did not consent.
338 participants under five years enrolled in the study.
49 died 289 recovered.
Figure 1: Study profile of study participants


Socio-demographic characteristics of children under five years of age admitted with SAM in the nutritional unit of Jinja Regional Referral Hospital
Table 1 shows that of the 338 children under five years of age studied, majority were males,208(61.5%) aged 13 24 months with a mean age of 18.months (SD = 10.7). Most of children had complete
immunization status, 177 (52.4%) presented with fever 229(67.8%) and cough 204(60.4%). Most of the children had completed immunization, 177(52.4 %). Majority of the children were not exclusively breastfed up to 6 months, 229 (67.7%). Almost all the children had a hospital stay/duration of admission of at least72hours.
Table 1: Socio demographic and biological characteristics children under five years of age admitted with SAM in the nutritional unit of Jinja Regional Referral Hospital (n = 338) Variable n(%) Sex Males 208(61.5) Females 130(38.5) Age in months ≤12 107(31.66) 13 24 179(52.96) >24 52(15.38)
Immunisation Status Complete 177(52.4) Incomplete 154(45.6) No 7(2.1)
Duration of admission <24hours 5(1.5) 24 48hours 12(3.6) >48hours 321(95.0)
Exclusive breast feeding up to 6 months Yes 109(32.3) No 229(67.7)
Socio demographic characteristics of the caretakers of children under five years of age admitted with SAM in the nutritional unit of Jinja Regional Referral Hospital
Table 2 shows that of the 338 caregivers, the majority were mothers, 237(70.1%) and
were from rural settings, 274(81.1).Mostof caregivers were aged 20 29 years, 165(48.8%). Most of the caregivers had attained primary education, 188(55.6%) and were engaged in business, 205(60.7%)
although they earned less than 100,000 Ugx,259(76.6%).
Table 2: Socio demographic characteristicsof the caretakersofchildrenunder five yearsofage admittedwith SAMin thenutritional unitofJinjaRegionalReferral Hospital(n=338)
Variable n(%)
Relationship with child
Mother 237(70.1) Father 28(8.3) Grandparent 55(16.3) Others 16(5.3)
Age in years
<20years 25(7.4) 20 29years 165(48.8) 30 49years 121(35.8) 50+years 27(8.0)
Residence
Urban 64(18.9) Rural 274(81.1)
Highest education level
Noformal 79(23.4) Primary 188(55.6) Secondary 69(20.4) Tertiary 02(0.59)
Occupation
Peasant 56(16.6) Business 205(60.7) Civilservant 71(21.0) Other 6(1.78)
Average monthly income of caregiver (Ugx)
<100,000Ushs 259(76.6) 100,000 500,000Ushs 72(21.3) >500,000Ushs 7(2.1)
Comorbidities among children under 5 years admitted with SAM in the nutritional unit of JRRH Figure 2 shows that of the 338 children under 5 years of age admitted with SAM,
the majority were diagnosed with dehydration, 128(37.9%) and pneumonia, 127(37.6%)andmalaria,87(25.7%).
120
100
80
60
40
140 Frequency (%)
20
128(37.9) 127(37.6)
87(25.7) 73(21.6) 61(18.5) 23(6.8) 20(5.9) 17(5.0) 14(4.1) 12(3.6) 6(1.8) 3(0.9) 0
Figure2: Comorbidities among children under 5 years admitted with SAM in the nutritional unit of JRRH
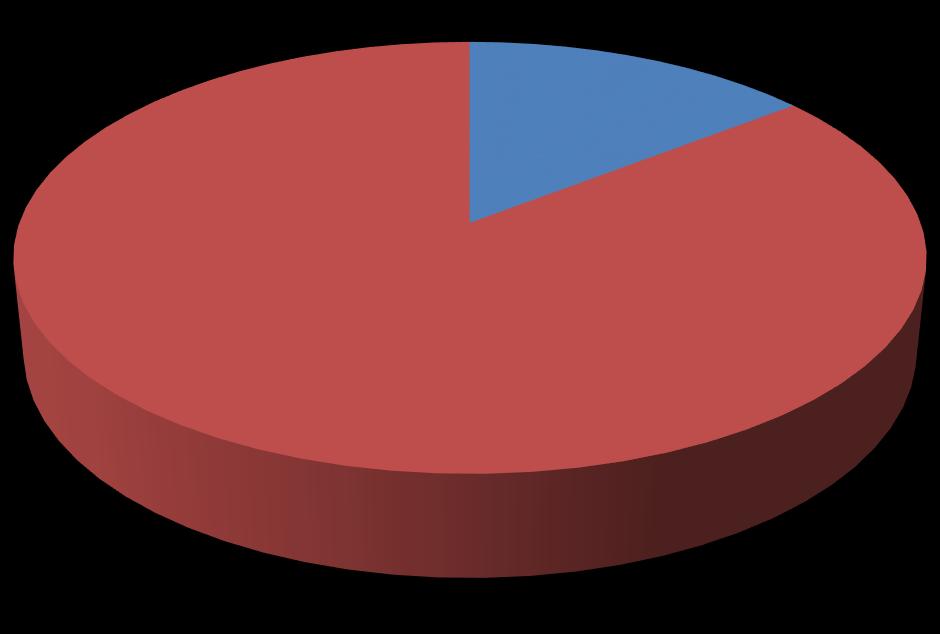
Proportion of mortality among children under 5 years admitted with SAM in the nutritional unit of JRRH Figure 3 shows that of the 338 children under five years of age admitted with SAM
in the nutritional unit of Jinja Regional Referral Hospital, a total of 49 children died,givinganoverallmortalityof145%.
Figure 3: Mortality of children admitted with SAM at Jinja Regional Referral Hospital
DISCUSSION
The first objective of the study was to determine the proportion of children under 5 years admitted with severe acute malnutrition who died in the nutritional of Jinja Regional Referral Hospital. The proportion of mortality in our study population was 14.5 %( 39/338). This mortality of 14.5 % is above the acceptable rates according to the WHO. With strict adherence to international recommended treatment guidelines, the case fatality for severe malnutrition ought to be less than 5%. In African hospitals, fatality rates of 20% are common and are often attributed to poor training and faulty case management [10]. The mortality of 14.5% found in this study is however low compared to the global perspective whereby severe acute malnutrition accounts for about 35 per cent of deaths among children under five years [2]. The difference in the mortality was attributed to the difference in the study populations in that the study population of the present study was small and taken from only one regional referral hospital but world health organization comes up with proportion after considering mortality of children with severe acute malnutrition from various parts of the world. Another reason for the lower mortality rate among children under 5 years with severe acute acute malnutrition could possibly be due to the appropriate in hospital interventions employed by the health workers who handle children under 5 with severe acute malnutrition at Jinja Regional Referral Hospital. The mortality of 14.5% is also lower that the mortality of 46% found in study on mortality and morbidity in under five years with SAM in Zambia [4]. The discrepancyin the studyresults couldhave risen due to the differnce in the study designs employed in the two studies since the previous study was a retrospective quantitative review of hospital based records whereas the present study is a cohort study. With the previous study utilizing only hospital records, there is a possibility of over exaggeration of mortality rate due to inaccuaracy during the entry of information in the hospital database. Another reason for the high mortality rate among children under 5 years with severe acute malnutrition in the previous study could be because the previous study was a five year
retrospective study whereas the present study took a period of only 3 months. Also the previous study was done in a univerity teaching hospital whereas the current study was conducted in a regional referral hospital. The high mortality rate in the previous study may be attributed to insufficient staff training and poor compliance with the recommended protocol, resulting in faulty case management. The study findings on mortality of children under 5 years of age admitted with SAM in the nutritional unit of Jinja Regional Referral is almost similar to the findings of a study done in Kenya which found a proportion of 15.6% [6]. The similarity of the study findings in the two studies can possibly be explained by the geographical areas where the two studies were conducted in that both studies were conducted in East Africa. Another reason for the similarity in the proportion of mortality found in the previous study and the present study could be because both studies were done among hospitalized children.The proportion of children admited with severe acute malnutrition in the study site of the present study was higher compared to the proportion of 9.3% found in a study done from Sudan [7] Looking at the discrepancy in the findings of the previous study and the present study, it could have come about due to the difference in the quality of medical interventions employed and the expertise of the health professionals involved in care of the children with SAM. Another possible reason for the difference in mortality rates could be due to the different study settings.
Furthermore, the mortality observed in the present study is higher compared to the mortality observed in a prospective study fromUganda which showeda proportion of 9.8% among children with severe acute malnutrition during in patient therapeutic care [8]. Much as the previous study and the present study were both conducted in Ugandainadditiontobothstudies utilizing similar study designs, the difference in the mortality rated between the two studies could have resulted from that fact that the previous study was nestedin a randomized controlled trial, investigating the effect of probiotics on diarrhea among children admittedwithSAM.The findingofstudyon treatment outcome among children with
severe acute malnutrition in Lacor hospital in Northern Uganda which showed a mortality of 11.9% is lower when compared to the 14.50% found in the present study [9]. Both studies were conducted in Uganda much as the previous study was conducted in Northern Uganda whereas the current study was conducted in Eastern Uganda; this could the reason behind the difference in the mortality rates among under 5 with severe acute malnutrition in the 2 studies. Another possible reason for the difference in the study findings could be due to the
variation inthestudydesignsevidencedby the cohortstudydesign usedin the present study and the retrospective study design used in the previous study. It was expected that adherence to these steps by health care providers would reduce mortality to less than 10% [11]. However, adherence to the treatment guidelines is a challenge and mortality of 10 40% among SAM hospitalized children have been reported in studies from sub Saharan Africa, though these often represent single hospital settings[12].
CONCLUSION
The proportion of death among children under 5 years admitted in the nutritional
unit of Jinja Regional Referral Hospital was 14.5%andhigherthanthenationalaverage.
REFERENCES
1. Legason, I.D., & Dricile, R. (2018). Prevalence of acute malnutrition among children ages 6 59 months: Results from a baseline nutrition surveyinNorth WesternUganda.
2. World Health Organization. (2016). Consolidated Guidelines on The Use Of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations For A Public Health Approach. World Health Organization, 20 Avenue Appia, 1211Geneva27,Switzerland
3. Cantero , L. (2014). Integrated Nutrition Survey Of 6 To 59 Month Children Rathedaung Township Rakhine State , Republic Of The Union Of Myanmar December 2014.Unicef, 4(2)45 56.
4. Munthali, T., Jacobs, C., Sitali, L., Dambe, R., & Michelo, C. (2015). Mortality and morbidity patterns in under five children with severe acute malnutrition (SAM) in Zambia: a five year retrospective review of hospital based records (2009 2013). ArchivesofPublicHealth, 73(1),23.
5. Yohannes, T., Laelago, T., Ayele, M. &Tamrat, T. (2017). Mortality and morbidity trends and predictors of mortalityinunder fivechildren with severe acute malnutrition in Hadiya zone, South Ethiopia: a four year retrospective review of hospital based records (2012 2015). BMC Nutrition, 3(1),18.
6. Gachau, S., Irimu, G., Ayieko, P., Akech, S., Agweyu, A., & English, M. (2018). Prevalence, outcome and quality of care among children hospitalized with severe acute malnutrition in Kenyan hospitals: A
multi site observational study. PloS one, 13(5),e0197607.
7. Kanan,S.O.H.,&Swar,M.O.(2016). Original Article Prevalence and outcome of severe malnutrition in children less than ive year old in Omdurman Paediatric Hospital , Sudan. Sudanese Journal of Paediatrics,16(1),23 30.
8. Nabukeera Barungi, N., Grenov, B., Lanyero, B., Namusoke, H., Mupere, E., Christensen, V. B., & Friis, H. (2018). Predictors of mortality among hospitalized children with severe acute malnutrition: a prospective study from Uganda. PediatricResearch, 84,92 98.
9. Nyeko, R., Calbi, V., Ssegujja, B. O & Ayot, G. F. (2016). Treatment outcome among children under five years hospitalized with severe acute malnutrition in St. Mary’s hospital Lacor, Northern Uganda. BMC Nutrition, 2(1),19.
10.Maitland, K., Berkley, J.A., Shebbe, M., Peshu, N., English, M. and Newton, C.R. (2006) Children with severe malnutrition: Can those at highest risk of death be identified with the WHO protocol. PLOS Medicine,3,e500.
11.World Health Organization. (2013). Pocket book of hospital care for children: guidelines for the management of common childhood illnesses.WorldHealthOrganization
12.TickellKD,DennoDM (2016). Inpatient management of children with severe acute malnutrition: a review of WHO guidelines.2016 Sep 1;94(9):642 51
13.Yves Tibamwenda Bafwa, Dafiewhare Onokiojare Ephraim, Charles Lagoro Abonga and Sebatta Elias (2022).Factors AssociatedwithElectrocardiographic Abnormalities among Heart Failure Patients at Kampala International University Teaching Hospital, Ishaka, Uganda. IAA Journal of BiologicalSciences9(1):166 175.
14.Yves Tibamwenda Bafwa, Dafiewhare Onokiojare Ephraim,
Charles Lagoro Abonga and Sebatta Elias (2022). Electrocardiographic Pattern among Heart Failure Patients at Kampala International University Teaching Hospital, Ishaka, Uganda. IAA Journal of Biological Sciences 9(1):159 1652022.
