THRU COLLEAGUES, CAREERS, CRAFT, CALLING, AND COMMUNITY







VOLUNTEERISM Summer 2023
Bringing CNS Members Together to Make Children’s Lives Better
CONNECTING
CHILD NEUROLOGY SOCIETY



































































































52nd ANNUAL MEETING


October 4-7, 2023 • Vancouver, BC











Don’t miss out on the CNS Annual Meeting!



It is the perfect opportunity to network, learn about cutting-edge research, and stay up-to-date with clinical practices in the field. Attend scientific sessions and workshops to deepen your knowledge and exchange ideas with experts and colleagues.


2023 CNS Annual Meeting
2023
CONNECTING WITH...
CNS Connections is the official news magazine of the Child Neurology Society. The title references the passionate professional interest members share in neural connections and their commitment to connecting to and staying connected with the peers, colleagues, mentors, mentees – and, above all else, friends – in the field with whom they share a career, craft, calling, and community.
Child Neurology Society
1000 West Cty Rd. E, Suite 290 St. Paul, MN 55126
Tel: 651/486-9447
Fax: 651/486-9436
nationaloffice@childneurologysociety.org www.childneurologysociety.org
EDITOR
Daniel Bonthius, MD, PhD
MANAGING EDITOR
Monique Terrell
DESIGN & LAYOUT
Kimberlea Weeks | CEVA Design
Published 3 times yearly
©2023 Child Neurology Society

COLLEAGUES
Letter
the Executive Director
Year of Achievements and the
of Volunteerism
Letter
the Editor
Tribute to Dr. William Bell
Research Focus
Marriage of Hematology and Neurology: Studying Sickle Cell Disease in the Pediatric Brain
The CNS Scientific Program and Planning Committee
Letter from the Co-Chairs 14 CNS Board of Director Candidates Active Members: Vote via your email link through August 30. CAREERS 54 Personnel Directory CRAFT 22 Synapses Is AIDP triggered by an antecedent infection? 24 Synapses Genetic Mutations can Mimic Hypoxic-ischemic Encephalopathy in Newborns 26 Synapses Fetal Exposure to Anticonvulsants and Later Risk of Psychiatric Disease CALLING 28 2023 Award Recipients
to this year’s award recipients. COMMUNITY 48 Child Neurology Foundation
Letter from CNF President 50 CNF Grants and Scholarships Congratulations to Our Recipients
4
from
A
Power
6
from
A
8
A
10
A
Congratulations
A
CONTENTS MAGAZINE
Child Neurology Society | Summer 2023 3
A Year of Achievements and the Power of Volunteerism
I hope this letter finds you all in good health and high spirits. As I reflect upon the past year, I am humbled and honored to express my heartfelt gratitude for your incredible support, dedication, and unwavering commitment to our organization. The value you bring through your volunteerism has been the cornerstone of our collective success.
It has been a momentous and transformative journey for me personally as well, as I complete my first year as Executive Director/CEO. From the beginning, this community has welcomed me with warmth and kindness, and I am truly grateful for that. Your trust and confidence in my leadership have driven our accomplishments over the past year. Volunteerism lies at the heart of our organization’s ethos, and I am continually inspired by the dedication you demonstrate day in and day out. Your selfless contributions of time, expertise, and passion have helped us advance our initiatives and make a meaningful impact on the lives of those we serve. Your unwavering commitment is a testament to your incredible value to our organization, and I want to express my sincerest appreciation for your involvement.
In my tenure as Executive Director/ CEO, we have achieved significant milestones that have laid the foundation for a stronger and more cohesive organization. One of our primary objectives was to create a more open and

transparent process for joining our CNS Committees, and I am thrilled to share that we have accomplished that goal. This approach ensures that every member has an equal opportunity to contribute their talents and ideas, fostering an inclusive environment for all.

I am delighted to share that our membership remains robust, with over 2,000 active and junior members and encouraging participation of over 300 medical students. We’re supported by 200 volunteers across 15 committees and 25 member-led special interest groups.
Together with our Bylaws and Membership committees, we’ve modernized our bylaws to enhance member engagement and governance. The updates make us more efficient, transparent, and adaptable to our members’ needs. You’ll have the opportunity to vote on these changes in September.
We recognized the need to fortify our internal capabilities to support our members better and further our mission. We took strategic steps to add critical staff and expertise to our team, which has significantly enhanced our ability to address challenges and deliver greater value to you.
Another significant accomplishment has been the launch of our employee handbook. This comprehensive guide ensures clarity and consistency in our practices, fosters a positive and harmonious work environment, and

COLLEAGUES
CNS EXECUTIVE DIRECTOR/CEO
4 Child Neurology Society | Summer 2023
Monique Terrell
empowers our team to deliver excellence in all aspects of our work.

As we celebrate these achievements, we eagerly anticipate the upcoming 52nd CNS Annual Meeting, which promises to be a grand occasion for networking, knowledge sharing, and collective growth. I am excited about this year’s annual meeting held October 4-7 in Vancouver, BC. The stunning locale will undoubtedly serve as an inspirational backdrop to further strengthen the bonds within our community and chart a course for a brighter future.

None of these accomplishments would have been possible without your steadfast support and the collective effort of our remarkable team. With great pride and enthusiasm, I look forward to the next phase of our journey together as we continue to build on our successes and overcome new challenges with the unwavering spirit that defines our organization.
In closing, I extend my heartfelt thanks to CNS President Bruce Cohen, President-Elect Peter Kang, SecretaryTreasurer Lori Jordan, and the full board for driving the positive changes we have achieved thus far. Together, we shall embrace the opportunities that lie ahead and profoundly impact the lives of those we touch.
With utmost gratitude and warmest regards. •
Let your voice be heard!
Ballots for the CNS Board of Directors and the CNS/PECN merger are in your e-mail box now.

Child Neurology Society | Summer 2023 5
30
Vote by
Bringing CNS Members Together to Make Children’s Lives Better
Daniel J. Bonthius, MD, PhD Medical Director, Pediatric Neurology Levine Children’s Hospital

Goodbye to a Brilliant Physician, Scholar, and Mentor A Tribute
 BY DANIEL J. BONTHIUS, MD, PHD, CNS CONNECTIONS EDITOR
BY DANIEL J. BONTHIUS, MD, PHD, CNS CONNECTIONS EDITOR
Astronomers teach us that, when a star implodes in the heavens, the night sky becomes measurably darker. This same principle applies on earth, in the affairs of humans. When a dazzling intellect is lost, the rest of us are left groping in the dark. Such is the case following the death of Dr. William Bell. Bill Bell was a giant beacon in the field of child neurology. His death on June 28, 2023, at the age of 93 years, leaves a dark void, not only for child neurologists, but for the whole world.
Dr. William (“Bill”) Bell was a superb physician, skilled administrator, and erudite scholar. But mostly, he was a consummate thinker and teacher. Twentysix years ago, I was officially the last of his many trainees in child neurology, and I had a chance to witness, firsthand, the actions that made him legendary.
Bill was born in Fairmont, West Virginia in 1929. He attended the University of West Virginia as an undergraduate and received his MD degree from the Medical College of Virginia in 1955. Bill was Phi
Beta Kappa at WVU, so he clearly excelled as a student. But I wonder what it was like to be a teacher of someone like Bill Bell. Did his instructors recognize what an unusual and brilliant mind their student had? It would be fascinating to know.
Following medical school, Dr. Bell completed an internship and residency in neurology at the University of Iowa. He then served for three years as a captain in US Airforce, where he was stationed in Japan and was the only Airforce neurologist in the Pacific. Following his stint in the military, he returned to the University of Iowa, where he received one year of training in pediatrics and joined the faculty as the sole pediatric neurologist. It’s astounding to think that this individual, who had very little official training in pediatrics and none from an actual child neurologist, would become one of the most authoritative figures in child neurology that the world has known. He achieved this by way of his voracious appetite for knowledge, capacity to learn
COLLEAGUES
CNS CONNECTIOINS EDITOR
6 Child Neurology Society | Summer 2023
Dr. William Bell, 19292023, was one of the eight founding members of the Child Neurology Society and recipient of the 1996 Hower Award.
from patients and colleagues, and uniquely capable mind.
Dr. Bell contributed mightily to the field of child neurology. He authored two highly lauded textbooks, including Neurologic Infections in Children, and Increased Intracranial Pressure in Children Both were the authoritative texts of their time, and, outside of the new information that has been discovered since their publication, one would be hard-pressed to find better sources today.
Dr. Bell was a towering figure in the “institutions” of child neurology. He was one of the eight founding members of the Child Neurology Society. He served as an oral examiner and Director of the American Board of Psychiatry and Neurology and was elected President of the board in 1992. He contributed to several committees within the Accreditation Council for Graduate Medical Education (ACGME) and served as Chair of the Review Committee for Neurology, as well as a member of the Appeals Committee for Child Neurology Training Programs. He authored numerous articles in the fields of pediatrics and neurology and was a member of the Editorial Board for the Annals of Neurology and Pediatric Neurology.
All of these achievements reflect his success and skill as a physician and leader. But none of these feats capture the real reason why people were so fascinated and inspired by Dr. Bell. People were drawn to him because of his mind. He was, simply, the smartest
person that anyone had ever met. He absorbed information instantly and voluminously and never forgot it. He was, literally, a walking encyclopedia. With a voracious appetite for knowledge, he read widely and deeply, and he could converse with awareness and humor about any subject. This was especially true regarding the subject of medicine. He could tell you, off the top of his head, why a child did or did not likely have Rubenstein-Taybi syndrome, or how a newborn with isovaleric acidemia differs from one with glutaric aciduria.
He seemed to have a specialist’s grasp of knowledge for virtually every branch of medicine - not just pediatrics and neurology. At the University of Iowa Hospital, when physicians in any department were confronted with a diagnostic dilemma and had run out of ideas, they would get a “Bill Bell Consult.” As a fledgling resident who accompanied him to some of these consults, I saw him accurately diagnose schistosomiasis in an adult gynecology patient and Budd Chiari syndrome in a jaundiced man.
When I was a medical student at the University of Iowa, I was told that there was this legendary guy on the pediatrics faculty, named Dr. Bell, who had a photographic memory and could quote to you the content, article title, journal, and year of publication of almost any subject in pediatrics or neurology in which you might be interested. I greeted this rumor with skepticism that bordered on disbelief. Several years later, I was tasked with writing a review article on
Sydenham’s Chorea. I asked Dr. Bell for advice, and he promptly provided, from memory, a list of three articles with their content, article title, journal, and year of publication. Everything was correct. A skeptic I was no more.
While his knowledge of medicine was seemingly endless, he had wideranging interests outside of medicine. He was an avid book collector and reader. He enjoyed travel, good food, and wine, and he was a skilled amateur photographer. He loved the outdoors, especially Nantucket Island, which he visited with his wife, Dr. Gail McGuinness, annually for over 40 years. He could converse about anything and always did so with respect and humor.
Because of his mastery of medicine and ability to teach it, he received numerous important honors and awards. One was the Ernest Theilan Faculty Award at the University of Iowa for excellence in clinical care and teaching. At the University of Iowa, there is an endowed chair in his name, the William E. Bell and Gail A. McGuinness Chair in Neurodevelopment. And, of course, he received the 1996 Hower Award from the Child Neurology Society for outstanding teaching, scholarship, and contributions to the Child Neurology Society.
Dr. Bell was a truly unique individual, and it was an experience just to know him. The field of child neurology is lucky and enriched by the fact that he landed among us. Although we have lost the light of his brilliant mind, he inspired all who met him to illuminate their own paths forward. •
Child Neurology Society | Summer 2023 7
Daniel J. Bonthius, MD, PhD Medical Director, Pediatric Neurology

 Children’s Hospital
Children’s Hospital
Research Focus
A Marriage of Hematology and Neurology: Studying Sickle Cell Disease in the Pediatric Brain






 BY DANIEL J. BONTHIUS, MD, PHD, CNS CONNECTIONS EDITOR
BY DANIEL J. BONTHIUS, MD, PHD, CNS CONNECTIONS EDITOR
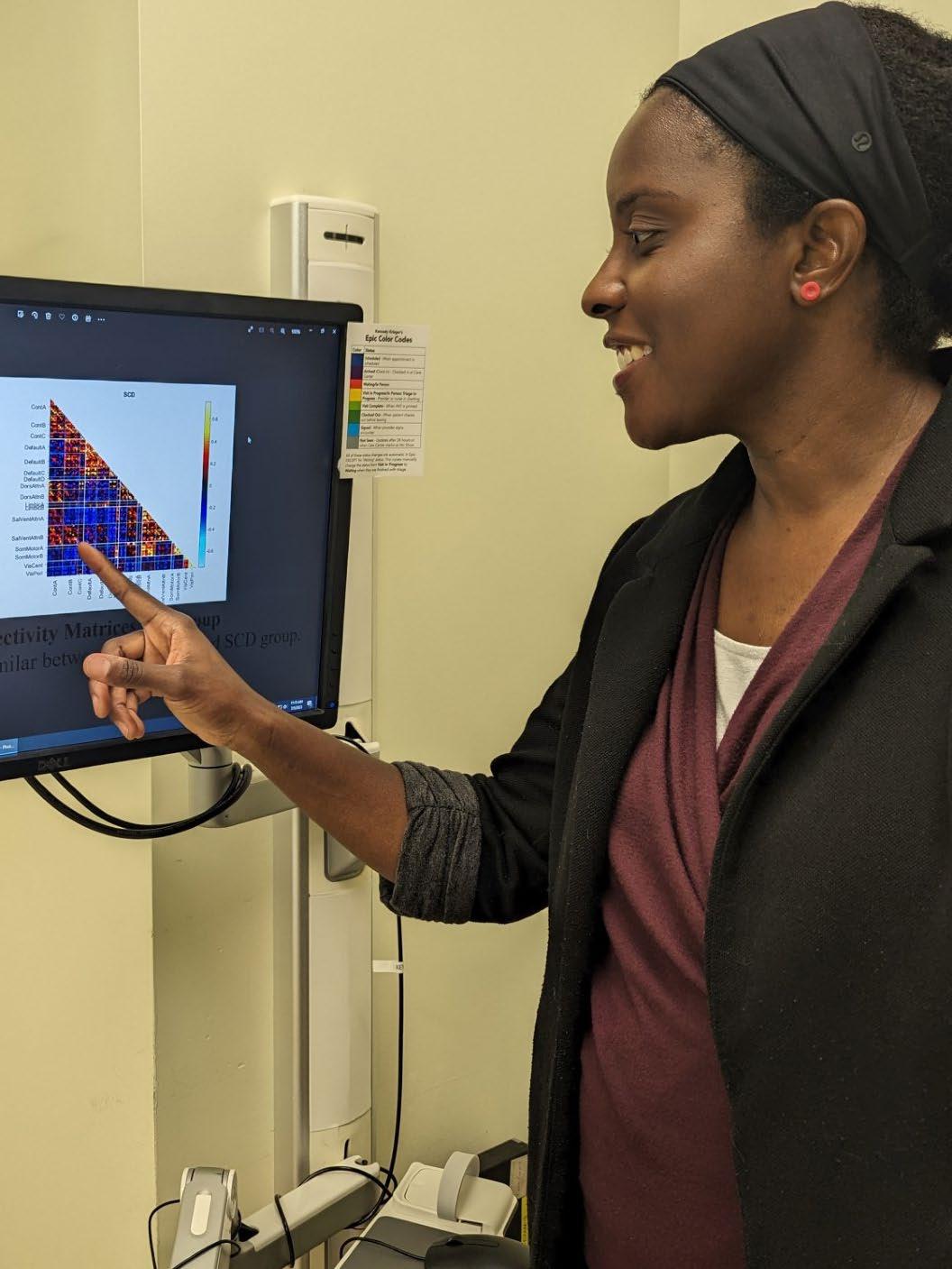
As we all learned in medical school, sickle cell disease is an inherited hemoglobinopathy, caused by a single base pair mutation in the beta-globin gene. Although sickle cell disease was one of the first genetic diseases discovered, research into its clinical manifestations has lagged behind many other more recently discovered disorders. As a result, the neurological and developmental consequences of sickle cell disease and the optimal ways of preventing and treating them remain largely unknown. Dr. Eboni Lance (Figure 1) aims to fill that void.
Dr. Lance is a physician at Kennedy Krieger Institute and an Associate Professor at Johns Hopkins University School of Medicine. She first became interested
in sickle cell disease as a medical student when she evaluated a home sleep study monitoring device as part of a summer research project. While fascinated by the field of hematology, she was especially captivated by her experience in neurology, and she struggled to decide which field to enter. Her problem was solved by wise mentors who guided her to the realization that she could pursue both fields by specializing in the neurology of sickle cell disease.
As a fellow in neurodevelopmental disorders (NDD), she founded the Kennedy Krieger Institute Sickle Cell Disease Neurodevelopmental Clinic, a multidisciplinary clinic that has grown to prominence and she continues to lead.
COLLEAGUES
CNS CONNECTIOINS EDITOR
Levine
Link to CNS Research Focus Library 8 Child Neurology Society | Summer 2023
Figure 1. Dr. Eboni Lance explains her research findings regarding neurodevelopmental disabilities in children with sickle cell disease.
In this clinic, she has observed the many ways in which sickle cell disease adversely impacts the neurodevelopment of children. These effects include not only stroke – a well known complication of sickle cell disease – but also silent cerebral infarction and a host of neurodevelopmental deficits, including ADHD, cognitive impairment, language disorders, and executive function impairment.
Dr. Lance encountered many patients with neurodevelopmental disorders and sickle cell disease during her NDD fellowship period. However, she discovered that there was a gap in knowledge regarding the mechanisms underlying these disorders as well as diagnosis and treatment. She decided that, if she wanted to provide optimal clinical care for these patients, she would have to conduct research herself. Therefore, she enrolled in a Clinical Investigation graduate program and received her PhD four years later.
Armed with a passion to understand the neurology of sickle cell disease and the skills to conduct research, Dr. Lance launched a clinical research program, The Sickle Cell Disease and Neurodevelopment Clinic and Research Center. She leverages a variety of techniques and collaborators to study multiple facets of sickle cell neurology, including its molecular underpinnings, physiology, neuroimaging, and behavioral manifestations.
Dr. Lance has studied the co-occurrence rates and clinical phenotypes of various neurodevelopmental disorders in pediatric sickle cell disease (figure 2). She found that 24% of children with sickle cell disease have neurodevelopmental disorders. Further, even when patients with stroke are excluded, the rate is still high at 19%. Dr. Lance found that silent cerebral infarctions underlie the deficits in some of these cases, but that no evidence of stroke can be found in others. This suggests that sickle cell disease disrupts brain activity in ways other than stroke. Indeed, her physiologic studies have revealed evidence for alterations in cerebral blood flow, oxygen extraction fraction, and cerebral metabolic rate of oxygen.
Dr. Lance’s molecular studies have shown that patients with sickle cell disease have elevated circulating levels of certain brain-derived proteins, including brainderived neurotrophic factor (BDNF) and neurogranin. Elevated plasma levels of these proteins likely represent biochemical evidence of neurological injury.
The over-riding goal of Dr. Lance’s research is to improve neurodevelopmental outcomes in children with sickle cell disease. The undaunted way in which she addresses complex research issues makes it highly likely that she will accomplish this ambitious goal. •
Figure 2. Bar
showing the co-occurrence of specific neurodevelopmental disorders in four pediatric populations: pediatric patients with sickle cell disease, the general US pediatric population, Black children in the general US population, and Hispanic children in the general US population. Different neurodevelopmental disorders occur at markedly different rates in all four populations, including those with sickle cell disease. (Lance EI, et al. J Dev Behav Pediatr 42:463471, 2021)

Child Neurology Society | Summer 2023 9
graph
SCIENTIFIC SELECTION & PROGRAM PLANNING CO-CHAIR
Yasmin Khakoo, MD, FAAN, FAAP


CHILD NEUROLOGY SOCIETY 2023
52nd Annual Meeting
The CNS Scientific Program and Planning Committee
 BY YASMIN KHAKOO, MD, FAAN, FAAP
BY YASMIN KHAKOO, MD, FAAN, FAAP
SCIENTIFIC SELECTION & PROGRAM PLANNING CO-CHAIR
It’s hard to believe the 52nd CNS Annual Meeting, in Vancouver, BC, Canada, is 2 months away. Thanks to Monique Terrell, the new CNS Executive Director and CEO and the CNS team, we are on track to learn, teach and play! Bhooma Aravamuthan and I, in our second term as co-chairs of the CNS Scientific Program and Planning Committee, began working with our 31 member committee from October 2022 onward to choose programming to appeal to a broad audience of scientists, clinicians, and practitioners, at all career stages. To all who completed the post-meeting survey, we listened to you and focused on Sleep, Headache and Metabolic conditions. Like last year, we favored submissions which included diverse co-authors, consistent with the CNS Leadership, Diversity, Equity and Inclusion (LDEI) mission; provided feedback to the primary authors of each proposal; and encouraged those whose submissions were not accepted, to resubmit for next year. We received 50 proposals and accepted 22: 4 symposia and 9 seminars onsite, with 9 webinars to be scheduled in 2023-24.
In addition to an “energizing” Presidential Symposium: Mitochondrial Disease: 10 Years of Advances & Progress, highlights include: the Year in Review
Symposium which will provide 10-12 min synopses of the 11 most important recent breakthroughs in Child Neurology; Sexual and Gender Minority Healthcare in Child Neurology; and Biomarkers and Surrogate Markers in Neurodevelopmental Disorders. Junior member programming will begin on Wednesday, with Lobby Talks sprinkled throughout the week.
We received 347 abstracts and selected 21 for platform presentations, and 294 traditional for traditional poster presentation. Twelve best-in-show abstracts will be featured in 2 guided poster sessions. Late-Breaking abstract submission closed on July 30, 2023, so stay tuned for additional groundbreaking research presentations. Awards will be presented to 4 trainees and 2 postgraduates for outstanding abstracts. We appreciate the enthusiasm and creativity of the CNS members who submitted their ideas and look forward to meeting in-person in Vancouver. Special shout-out to Sue Hussman, Katelyn Geiger, Julianne Bruce, and William Stanton for supporting us. In October, I conclude my 11-year term on this committee, the last 3 as co-Chair. I look forward to passing the torch to the new leadership and being a spectator at the 53rd CNSAM in San Diego in November 11-14, 2024. •
COLLEAGUES 10 Child Neurology Society | Summer 2023
Bhooma Aravamuthan, MD, DPhil










 Sonika Agarwal
Shawn Aylward
Clarimar Borrero-Mejias
J. Nicholas Brenton
Audrey Christine Brumback
Meeryo Christa Choe
Bruce H. Cohen
Louis Dang
Jay Desai
Matt Elrick
Timothy Robin Gershon
Sonika Agarwal
Shawn Aylward
Clarimar Borrero-Mejias
J. Nicholas Brenton
Audrey Christine Brumback
Meeryo Christa Choe
Bruce H. Cohen
Louis Dang
Jay Desai
Matt Elrick
Timothy Robin Gershon
Child Neurology Society | Summer 2023 11
Grace Gombolay











 Wilfreda Lindsey
Ariel Lyons-Warren
Kiran Prasad Maski
Melanie McNally
Xilma Ortiz-Gonzalez
Scott Otallah
Temitayo Oyefunmike Oyegbile Chidi
Rachit Patil
E. Steve Roach
Jonathan Douglas Santoro
Renee A Shellhaas
Wilfreda Lindsey
Ariel Lyons-Warren
Kiran Prasad Maski
Melanie McNally
Xilma Ortiz-Gonzalez
Scott Otallah
Temitayo Oyefunmike Oyegbile Chidi
Rachit Patil
E. Steve Roach
Jonathan Douglas Santoro
Renee A Shellhaas
12 Child Neurology Society | Summer 2023
Jennifer Vermilion
CHILD NEUROLOGY SOCIETY


52nd ANNUAL MEETING
October 4-7, 2023 • Vancouver, BC
Don’t miss out on the CNS Annual Meeting!

It is the perfect opportunity to network, learn about cutting-edge research, and stay up-to-date with clinical practices in the field. Attend scientific sessions and workshops to deepen your knowledge and exchange ideas with experts and colleagues.

 Amy Robichaux Viehoever
Amy Robichaux Viehoever
Child Neurology Society | Summer 2023 13
JoJo Yang
2023
CNS Board of Director Candidates
The CNS Nominating Committee is pleased to present the following slate of candidates for consideration by Active Members of the Child Neurology Society eligible to vote to elect two Councilors to serve two-year terms on the CNS Board of Directors. Your vote is crucial, so mark your calendars for the 30-day voting period starting from August 1 to 30, 2023. Let your voice shape the future of our organization.
COUNCILOR FOR THE MIDWEST: Soe Mar, MD
Dr. Mar Is a professor of Neurology and Pediatrics at Washington University in St. Louis. Prior to coming to Washington University for a faculty position in 2005, Dr. Mar had extensive international experience training in pediatrics in her home country of Myanmar, and subsequently admitted to the British Royal College of Physicians and Surgeons. She continued her training at Queen’s Medical Center in Nottingham University followed by Diana Princess of Wales Children’s Hospital in the UK. She then traveled to the United States in the year 2000 for her pediatric neurology residency where she trained under the mentorship of Dr. Isabel Rapin at Albert Einstein College of Medicine in the Bronx. Joining Washington University in St Louis in 2005, she became a full Professor in 2018, then associate pediatric neurology residency program director from 2010 to 2013 and program director of child neurology residency at Washington University since 2013. Dr. Mar has been responsible for the training of over 50 child neurology residents as well as 100s of medical students since she joined Washington University. In the process, she has become extremely involved nationally and internationally in collaborations with other pediatric neurologists in research, program administration and mentorship.
Always active in the Child Neurology Society, Dr. Mar has been a member since 2005 and joined the Professors of Child Neurology in 2011. She has
been on the Child Neurology Society Finance Committee since 2018, served as a Director at Large for Professors and Educators of Child Neurology (PECN) from 2020 to 2022. Dr. Mar is now current president of PECN and serving in this role since October 2022. She works in close collaboration with the board of directors of PECN, CNS, ACGME and ABPN, providing input and monitoring the changing landscape of child neurology education and training nationwide.
Dr. Mar maintains an active neuroimmunology clinical practice at Children’s Hospital in St. Louis, at the same time devoting much time to clinical training and the research program at Washington University that includes specific expertise in demyelinating diseases of childhood. She was a recent chair and a current executive and steering committee member of the US Network of Pediatric MS Centers (NPMSC), where she continues to oversee multiple research projects, writing grants, reviews concept proposals, prioritizing manuscript writing projects and mentoring junior faculty with interest in pediatric MS and demyelination diseases across the country. She has led international collaborations with researchers from the US and Europe to study encephalitis and HIV on pediatric patients in Myanmar. Dr. Mar is the medical director and a board member of a Missouri nonprofit charity, the Myanmar Children and Family Medical Foundation, which supports several HIV orphanages, a

COLLEAGUES
14 Child Neurology Society | Summer 2023
Soe Mar, MD
large school and distributes emergency medical and nutritional supplies to internally displaced families. Her work with the foundation also includes a long history of nurturing the development of a pediatric neurology program at the largest Children’s Hospital in Myanmar. Several residents in her program at Wash U have joined her in Myanmar, assisting with bedside clinical instruction of the Myanmar hospital staff. She has volunteered in Haiti and Guatemala as well and believes in the importance of nurturing the intellectual curiosity and involvement of her trainees in her research and educational activities in underserved areas of the world.
Dr. Mar’s long experience in diverse medical, educational and scientific environments and her demonstrated collaborative leadership roles are certain to be an asset to the community of child neurology through her participation on the board of directors of CNS.
What are the most challenging issues facing child neurologists today, and how would the CNS, under your leadership, help its members meet those challenges?
In my years with CNS, I always remember with pleasure, getting know the junior members, supporting and mentoring them as to how to navigate and advance their career in the field of child neurology. On a day to day basis, I have many opportunities to collaborate one to one, or in small groups with colleagues; to teach, participate in research and protect the clinical discipline of child neurology; But, aside from vigorously and conscientiously treating my patients, to achieve the best outcome possible, I am most satisfied when I am in a leadership role that can amplify my impact across the field. For example, In my leadership positions with PECN I have been honored to have a respected nationwide platform to participate in
and lead the process of imagining, determining and implementing the best ways to train future child neurologists, in a changing landscape. My participation and leadership roles with US Network of Pediatric MS Centers has been invaluable, providing me with opportunities for mentorship and facilitating and participating in multicenter clinical research projects. But, again, the best part has been the opportunity form close professional relationships and personal friendships with child neurology colleagues throughout nationwide networks of education and research, and learning from previous generations of child neurologists.
My vision for CNS is to grow the child neurology community nationally and internationally so we can better take care of children with neurological disorders. I hope to see CNS as the major authoritative body for the development of more efficient and appropriate methods for the training child neurologists and funding of the educational programs of our future child neurologists. In addition, I would like to see CNS taking a leadership role recommendation of good practices for child neurologists in the country.
I would also like see CNS provide research and educational opportunities for students, residents and junior faculty in collaboration with AAN and AAP; and to expand advocacy for health care and research funding for children with neurological disorders at the national level.
What are the most challenging issues facing child neurologists today, and how would the CNS, under your leadership, help its members meet those challenges?
There are multiple challenges that child neurologists face today, but the most pressing one is a shortage of child neurologists nationally and
globally. We need to produce more excellent child neurologists and also help training pediatricians to become comfortable with managing common neurological problems such as seizures and headaches.
To this end, under my leadership, I would like CNS to become involved with the curriculum of medical schools, recommending that child neurology rotations become part of general pediatrics or general neurology rotations so that all students are exposed to child neurology. In addition, we should explore the possibility of making child neurology training more attractive to potential trainees by reforming the training curriculum to be shorter, more focused, rigorous and condensed training than the current curriculum, trainees will have more opportunities to do other important things in their lives such as pursuing more fellowships, earning decent incomes sooner as attending physicians to pay off those medical school loans, or starting or growing family.
Under my leadership, I would encourage CNS to become more involved in AAP to have more child neurology exposure for pediatric residents. Pediatricians should be trained to become comfortable with evaluating headaches, treating migraines, and treating febrile seizures and ‘easy to treat’ epilepsy. It is our responsibility to expose pediatric residents to common neurological problems and teach them how to manage. Presently many child neurology practices are crowded with patients who could be equally well served by their pediatricians, with a little training. That would help with work force shortages in child neurology and the inconvenience for many patients and their families resulting from the current waiting list for general child neurology. •
Child Neurology Society | Summer 2023 15
COUNCILOR FOR THE MIDWEST: Anup D. Patel, MD

Dr. Patel is board certified in neurology with special qualifications in child neurology. In addition, he is board certified in epilepsy and clinical neurophysiology. He is the President for the Child Neurology Foundation Board of Directors and will complete his term in October 2023. He is the Chair of the Pediatric Epilepsy Research Consortium (PERC) until December 2023. He is the Vice-Chair of the Quality Committee for the American Academy of Neurology. He serves as a member of the Child Neurology Society Finance Committee. Previously, he served as a member on the Child Neurology Society Electronic Communications Committee. He is a part of the Child Neurology Society Quality Special Interest Group. He is a medical director of quality in the Center for Clinical Excellence at Nationwide Children’s Hospital. He is a Professor in Clinical Pediatrics and Neurology at the Ohio State University College of Medicine. He has interests in child neurology, pediatric epilepsy, and quality improvement.
What have been your most important or rewarding experiences in your years with CNS or with other professional organizations, and how have these experiences shaped your vision of the direction the CNS might take under your leadership?
I have had several meaningful experiences with the Child Neurology Society (CNS). I remember the first meeting I attended in Ottawa and the awe of all the great science and clinical experience that was being shared. I remember meeting people and starting to foster connections and friendships that remain today. The Child Neurology Society (CNS) was and remains my first professional home. I was fortunate to
serve as a member on the Electronics Communications Committee. Here is where I learned how the structure of CNS worked and how a professional organization runs. Shortly afterward, I was selected as the CNS representative for the American Academy of Neurology (AAN) Quality Safety Subcommittee. It was an amazing opportunity to represent CNS in this capacity. My role grew and soon I became the Vice-Chair of this subcommittee and then Vice-Chair of the AAN Quality Committee. I led the creation of the first quality measure set in Child Neurology, a collaboration between AAN and CNS. This experience taught me the importance of relationships between professional organizations. As a pediatric epileptologist, I felt it was also important to advocate and represent the needs of children with epilepsy and their families. Therefore, I became involved with the American Epilepsy Society (AES) on the Practice Management Committee becoming Chair until 2022.
Soon, my term as the President of the Child Neurology Foundation (CNF) Board of Directors will end, which has been a huge honor. I have worked closely with CNS and other important professional organizations. During the COVID-19 Pandemic, many organizations that help people with epilepsy and their families came together to ensure coordinated efforts occurred to effectively help all. Having previously established relationships with other organizations helped me represent the needs of the CNF and CNS communities. The CNF offers so many caregiver and patient resources and reaches many children with neurological illness. Through alignment and coordinated efforts with CNS, we are improving the lives of patients, families, and child neurology providers.
16 Child Neurology Society | Summer 2023
Anup D. Patel, MD
We have made significant progress together. Representing the needs of the child neurology community which includes child neurology providers is important.
Through my previous work, I worked to help child neurologists deliver effective and high-quality care in an efficient manner. Through CNF and CNS led efforts, we are developing clinical informatic and other tools to make implementation of quality measures and guidelines easier.
Getting to learn about CNS in these past years and being a presenter for the Presidential Symposium has given me the passion to contribute more to CNS. Sharing our work and those of others was the highlight of my academic career. Therefore, it would be an honor to serve as the councilor of the Midwest. I feel that having these strong relationships with many of the organizations that interface with CNS will help me in this role and help make CNS even stronger for years to come. These leadership experiences have helped me create a vision of collaboration, growth, and success for CNS.
What are the most challenging issues facing child neurologists today, and how would the CNS, under your leadership, help its members meet those challenges?
Our field is ever changing, creating challenges moving forward. The demands on child neurologists grows each year while compensation for services we provide decreases. The need for support and connections to ensure efficiency of clinical care delivery and the growth of our field is essential.
Understanding how different groups operate and function will assist me if I were to be elected.
We need to continue to increase the number of child neurologists. CNS can greatly assist in cultivating awareness and interest in child neurology. Recently, the jointly administered CNS/ CNF Swaiman scholarship program for medical students was expanded through a generous gift which will assist in bringing more students to our great field. Specifically, we have an opportunity to reach states with medical schools where few child neurology providers are available in the given state. Focusing on expanding our workforce with child neurologists from diverse backgrounds will strengthen our field. Work has started in this area with partnerships with CNF and I would like to continue to this work.
Advancements in our field have expanded tremendously within areas of lifesaving treatments, diagnostics, thus creating a need for child neurologists to stay informed due to this great expansion of knowledge. CNS is perfectly poised to ensure we deliver the information through the annual meeting, workshops, webinars, and other novel educational delivery mechanisms. Through my previous leadership, I have experience and have participated in creating such educational opportunities.
Access and affordability of treatments is an important challenge for our patients and their families. CNS can assist our members in understanding methods to help get treatments to the right children. In addition, CNS can partner with other organizations to advocate for the needs of children with
neurological illnesses. Ensuring that the treatments are available to all is vital to decrease any potential disparities in care.
CNS has made strides to ensure our organization grows in conjunction with our diverse community. Ensuring inclusion and equity principles are the key to our future. These principles should continue to expand in how we grow and cultivate the membership and the leadership of CNS. I have learned through experiences in CNS and other organizations how important a focus on diversity, inclusion, and equity (DEI) is to the health of an organization. By ensuring leadership positions are represented properly will allow all voices of CNS to be heard. In addition, a diverse, inclusive, and equitable organization allows us to best assist all children with neurological illness and their families.
In summary, our field faces challenges in our future. I am confident with the right leadership at CNS that we can overcome any challenges and be successful for years in providing the best for the child neurology community. I would be honored to serve as the councilor of the Midwest to assist in our mission. •
Child Neurology Society | Summer 2023 17
COUNCILOR FOR THE EAST: Andrea Gropman, MD

Originally from Boston, I moved to the DMV after medical school to complete my training in pediatrics, neurology, and genetics, successfully lost my Boston accent, serve as Division Chief of Neurodevelopmental Disabilities and Neurogenetics at the Children’s National Hospital (past 10 years). I am Principal investigator of the Urea Cycle Disorders Consortium and serve as interim director of Genomics and Personalized medicine at the Children’s National Research Innovation Campus.
I obtained my medical degree at the University of Massachusetts Chan Medical School. I got hooked on child neurology after my mentor (Paul Marshall) sent me to work with Paul Rosman at NEMC. I then completed pediatrics at Johns Hopkins (Frank Oski), followed by child neurology at Children’s National (Roger Packer) and genetics training at NIH (Bill Gahl). During my fellowship at Children’s, I developed the first neurogenetics clinic when the most sophisticated test we had was karyotype!
After 11 years of training post medical school including clinical fellowships and a Howard Hughes Research fellowship, I was finally ready to become faculty! I joined Georgetown in 2000 Children’s National Hospital and the George Washington University School of Medicine in 2003. In 2013 I was promoted to professor with tenure.
I have had the privilege of committee work and leadership in national organizations. I served on the RRC for genetics as the inaugural trainee and remain active in the NIH genetics training program as well as the North American Metabolic Academy. I participated as an examiner for the ABPN oral boards and serve on several ABPN item writing committees. I serve an associate editor for Journal of Child Neurology, previously on the editorial board of Pediatric Neurology, and section editor for Swaiman’s Pediatric Neurology, and editor in chief for Mitochondrial Medicine. I have served on NIH grants review committees. I am deputy clinical director of the Mito EpiGen research collaborative and Director of the Clinical Translational Core of the Intellectual Disabilities and Developmental Disabilities Research Center at CNH. I served as the chair of the steering committee of the Rare Disease Clinical Research Network (RDCRN) that brings together more than 20 rare disease consortia.
In the CNS I served on the scientific selection committee, the legislative affairs committee, CNS foundation, and currently the awards committee, and of the neurogenetics SIG which has grown from an original audience of three, to 100s. I am cochair of the NG special interest group and vice chair of the Neurogenetics SIG for the AAN.
I maintain an active funded research portfolio while also serving as mentor for students, trainees, and faculty at all levels. My research interest focuses on understanding neurological injury in inborn errors of metabolism using multimodal neuroimaging and cell markers to better characterize and understand the underpinnings of neurological injury, their impact on complex cognitive functions and establishing neuromonitoring protocols that can be implemented universally in clinical settings. Always looking for new challenges outside my comfort zone, I tried my hand at screen writing after attending a “screen writing for physicians” course.
What have been your most important or rewarding experiences in your years with CNS or with other professional organizations, and how have these experiences shaped your vision of the direction the CNS might take under your leadership?
My most important and rewarding experiences during my 23+ years in the CNS have been engaging with colleagues, researchers, and experts in the field, fostering collaborations, and building a network of professionals working towards a common goal through my work on committees and participation in posters and presentations. These interactions can provide valuable insights, exchange of ideas, and opportunities for collective growth and guide how the field will advance.
More recently I have found reward in mentoring younger professionals, students, and newcomers to the field. Supporting the growth and development of individuals by sharing expertise and experiences can be highly rewarding and contribute to the overall success of the future of the CNS. My work in advocacy and outreach through the CNS and other endeavors such as working with the NUCDF, UMDF and PRISMS has taught me the importance of CNS and its impact on society
18 Child Neurology Society | Summer 2023
Andrea Gropman, MD
through public outreach, policy advocacy, and engagement with stakeholders. Working towards creating awareness and influencing decision-makers can shape the direction and priorities of the organization and attract trainees to our profession. How we train the future generation is important and I am working with colleagues to understand what tools the future workforce will need and how to address that during training.
These experiences can shape the future vision of CNS by emphasizing key areas such as collaboration, knowledge sharing, mentorship, and advocacy.
Under my leadership I would work with the CNS to foster interdisciplinary collaborations, encourage open-access research and data sharing, facilitate mentorship programs at all levels, and actively engage in public discourse to promote the understanding and relevance of child neurology and neuroscience in society, while fostering inclusivity and diversity, promoting ethical practices in research, embracing emerging technologies and methodologies, and addressing critical challenges in the field such as access, work force shortages, training the next generation of child neurologists and transition to adulthood.
Ultimately, I would strive to advance the field of neuroscience, promote its societal impact, and ensure the CNS remains at the forefront of scientific discovery and innovation. To do so, we need to continue to attract and recruit students and researchers to our field. It is important to plant the seed early in medical school.
Since neurologic disorders in children can have a significant psychosocial impact on both the affected child and their family, I would work with the CNS foundation and patient advocacy to address the emotional and behavioral issues, developmental delays, cognitive impairments, and the burden of ongoing care that can affect the mental well-being and quality of life for the child and their caregivers. Addressing these psychosocial aspects is an essential part of comprehensive child neurology care. Addressing these challenges requires ongoing research, collaboration, and the
development of specialized resources and support systems for children with neurologic disorders. By advancing our understanding, improving access to care, and promoting multidisciplinary collaboration, we can enhance the outcomes and quality of life for children with neurologic conditions.
What are the most challenging issues facing child neurologists today, and how would the CNS, under your leadership, help its members meet those challenges?
Child neurology faces several challenges including workforce shortage, patient access, increased patient complexity and need for multidisciplinary care models, prior authorizations for genetics testing and expensive medications, and transition to adult neurology clinics, especially for those with Autism or IDD.
Child neurology is at an exciting crossroads and we as the leading organization for child neurologists, should decide how to define and prepare ourselves and future generations for these advances which may provide creative solutions for our stated challenges.
Pediatric neurology services may be concentrated in major medical centers creating challenges for children and families who live in remote or underserved regions. The pandemic opened our eyes to opportunities for the integration of digital health technologies, remote monitoring, and telemedicine platforms as ways to decrease the burden of research, but more importantly, to deliver equitable care and enhance access to care, especially for patients in remote areasOur role in telehealth is an ongoing discussion
Child neurology often requires a multidisciplinary approach, and the future may see increased collaboration among healthcare providers, including neurologists, geneticists, developmental pediatricians, psychologists, and therapists. Collaborative care models can lead to more holistic and comprehensive management of neurological conditions, addressing the medical, developmental, and psychosocial needs of children and their families. Health care as it is, does not have these models
built into capitated care. Many pediatric neurologic disorders are chronic or lifelong conditions that require long-term management. Ensuring consistent access to care, monitoring disease progression, and addressing evolving needs as children grow and develop and require transition to adult services pose ongoing challenges
As our understanding of genetics and molecular mechanisms improves, child neurology is likely to benefit from more precise and personalized approaches to diagnosis and treatment. In order to have precision medicine, precision diagnosis is essential. Child neurologist must be comfortable ordering and interpreting genetic testing results and work closely with genetic counselors and geneticists. Child neurologists should be at the table in this arena to advocate for involvement of our specialty in decisions around precision medicine and engage with stakeholders on all fronts.
Neuroimaging techniques continue to evolve, providing greater insights into the structure and function of the developing brain, which may help in earlier diagnoses, treatment monitoring, and predicting longterm outcomes and may need to be part of clinical care.
New treatment modalities and interventions are emerging in child neurology. This includes the development of novel pharmacological agents, gene therapies, DNA and RNA based therapies, etc. These innovations hold the potential to improve outcomes and quality of life for children with neurological disorders. Child neurologists need training and comfort with these new drugs that may not just include oral agents and IVs, but complex delivery into the brain.
With the increasing availability big datasets and electronic health records, this presents an opportunity for child neurologists to collaborate on research, data sharing, and use this technology for the development of evidence-based guidelines. This collective effort may promote development of standardized practices, clinical decisionmaking support and accelerate scientific innovation and discoveries. •
Child Neurology Society | Summer 2023 19
COUNCILOR FOR THE EAST: Yasmin Khokoo, MD, FAAN, FAAP
I am honored to be considered for the Child Neurology Society Councilor for the East position for 2023-2025. While some of my colleagues are winding down their careers, I am just hitting my stride. I am the child of 2 immigrant physicians who worked in underserved NYC hospitals, and modeled a culture of service to others, which I have strived to emulate. I am a boardcertified pediatrician, child neurologist and neuro-oncologist at Memorial Sloan Kettering Cancer Center (MSKCC) and Professor of Clinical Pediatrics at Weill Cornell Medical College (WCMC). I care for children and young adults with primary brain tumors and have focused my career on onco-neurology: the diagnosis, treatment, and prevention of neurologic complications in patients receiving cancer treatment. While I have been recognized for clinical excellence annually since 2013 by Castle Connolly, I am more honored to be seen as a trusted resource for medical colleagues and others. I have been recognized as an educator and received the 2021 WCMC Pediatric Neurology Faculty Teaching Award from the neurology residents. I have developed leadership expertise in faculty development, especially for women and underrepresented physicians, APPs and trainees. I have gained national recognition as a leader within the: 1) Child Neurology Society [Co-chair of the Scientific Selection and Program Planning Committee {SSPPC} from 2020-2024]; 2) American Academy of Neurology [one of 12 recipients of the Women Leading in Neurology fellowship in 2019; inducted as a fellow of the AAN in 2021; and the AAN Topic Chair for Child Neurology abstract selection 2020-present];

3) United Council on Neurologic
Subspecialties as a neuro-oncology examination question writer [2019-2023] and as one of 2 CNS representatives on the certification council [2019-present]. In 2022, I became Editor-in-Chief of Pediatric Neurology and continue to increase diversity of board members, authors, reviewers, readers, and article subjects. I recently learned that I am the recipient of the 2023 CNS Arnold P. Gold Humanism in Medicine Award. I ma truly humbled by this honor
I have been heavily involved in clinical research projects in neuro-oncology and opened my first IRB protocol in 2020: a registry for patients with large congenital melanocytic nevi and/or neurocutaneous melanocytosis to identify risk factors for developing CNS melanoma [https:// classic.clinicaltrials.gov/ct2/show/ NCT04548817]. I am the MSKCC PI of the Boston Children’s Hospital led PediatricOnset Opsoclonus Myoclonus Ataxia Syndrome (POOMAS) program.
My most rewarding experiences within the CNS are many, from my first platform presentation as a resident in 1993, symposia in 2017 & 2021, and more recently, working to help CNS become more inclusive, not only of gender, race, and ethnicity, but also rank, institution and career type. As co-Chair of the SSPPC, I worked with the team to increase transparency of the proposal and abstract process: we give points for diversity and provide feedback to proposal submitters both successful and unsuccessful. Many child neurologists have participated in the AAN leadership programs and as Councilor I will encourage formation of similar mentoring networks within CNS. The recently created Junior member programming is essential for succession planning, and thankfully applicants to
20 Child Neurology Society | Summer 2023
Yasmin Khokoo, MD, FAAN, FAAP
child neurology residency programs are at an all-time high.

Challenges facing child neurologists include transition of care, advocacy (for patients and medical staff), and training. As Councilor I will build and maintain CNS connections with other organizations including the AAN, American Epilepsy Society, and the American Academy of Pediatrics to harmonize transition of care models. Our most active CNS members have developed webinars and workshops and I will support Special Interest Group development for this topic. The Child Neurology Foundation is already leading in this space and I will work with the other board members to help maintain this connection.
I will advocate for recruitment and retention of our workforce, prioritizing our mental and physical health to ensure outstanding medical care for our patients and their caregivers. To promote generational harmony, I will develop workshops/webinars on team building and professional development. In 2021 I gave a CNS symposium talk on the impact of caregiving on medical education to encourage trainees and junior faculty to open lines of communication around starting a family and caring for elders. Division chiefs in attendance received tools on supporting faculty and trainees and the session was well received. Other advocacy issues include gun control, preservation of reproductive health rights and LGBTQI+/ gender issues for patients and medical teams. The CNS Annual Meeting 2023 includes a symposium on sexual and gender minority healthcare in child neurology. Training is another challenge
we all face in medicine. I will continue to encourage us to reach out to students as young as school age to pursue careers in child neurology. We need to make medical education more accessible to all, especially underrepresented minorities by increasing loan forgiveness programs and continue to tailor Child Neurology training based upon the trainees’ goals. Physician scientists and general child neurologists have different needs during training. We must encourage research focused trainees to apply to the Child Neurologist Career Development Program-K12 so that we better understand the neurobiology of disease and develop even more new therapies for our most vulnerable patients. The Professors and Educators of Child Neurology is one CNS program working to maintain high quality training. I will encourage the use of technology in curriculum development. It’s an exciting time to be a Child Neurologist and I hope you will consider me for the job of Councilor for the East. •
Child Neurology Society | Summer 2023 21
Daniel J. Bonthius, MD, PhD Medical Director, Pediatric Neurology Levine Children’s Hospital

Child Neurology Synapses

Is AIDP triggered by an antecedent infection?
“Impact of infections on the incidence of acute inflammatory demyelinating polyneuropathy in children”. Gilber H, et al. Annals of the Child Neurology Society 2023; 1(2): 129-136.
What the researchers did:
Acute inflammatory demyelinating polyneuropathy (AIDP), the predominant form of Guillain-Barre syndrome, is commonly encountered by child neurologists. Traditional teaching states that the pathogenesis of AIDP is driven by an antecedent infection that triggers an immune response against crossreactive epitopes on peripheral nerves.
The strongest evidence that a preceding infection can underlie AIDP lies with Campylobacter jejuni. However, only a small portion of AIDP cases are preceded by C. jejuni infections, and the majority
of AIDP are presumably due to different community acquired infections. Evidence that an antecedent community acquired infection plays a role in AIDP is weak, especially in children. Interestingly, the recent COVID-19 pandemic and society’s response to it, created a unique opportunity to examine this issue. In particular, the preventive measures enacted to slow the spread of SARSCOV-2 (the virus that causes COVID-19) simultaneously decreased virtually all community acquired infections. A group of American researchers utilized this “natural experiment.” They reasoned that, if antecedent community acquired infections play a vital role in the pathogenesis of AIDP in children, then the dramatic reduction in the rate of these infections should be paralleled by a similar reduction in the rate of AIDP.
CRAFT
CNS CONNECTIOINS EDITOR
22 Child Neurology Society | Fall 2022
What the researchers found:
The researchers conducted a cross sectional study, utilizing data from the Pediatric Health Information System, a large database providing information regarding diagnoses, demographics, and treatments from 47 United States tertiary children’s hospitals. They compared rates of community-acquired infections (respiratory, gastrointestinal, and COVID19) with rates of AIDP during a time period before the pandemic (January 2017 – February 2020) and during the pandemic (March 2020 – February 2021). The researchers found that, during the pre-COVID-19 period, the incidence of AIDP was not associated with the incidence of respiratory infections, influenza, gastrointestinal infections, or C. jejuni. Furthermore, during the pandemic, the incidence of COVID-19 was not associated with the incidence of AIDP. Most importantly, while there were substantial reductions in the frequencies of respiratory, gastrointestinal, and influenza infection admissions during the pandemic, there was no corresponding substantial reduction in admissions for AIDP.






Admissions for AIDP were only modestly reduced during the pandemic and were in-line with the reductions observed in virtually all diagnoses during that period. Thus, rates of AIDP persisted during the pandemic, despite dramatic reductions in infection-related encounters – a result not expected if antecedent infections trigger the pathology of AIDP.
What the research means:
One weakness of this study is the fact that the period of time during which the usual community-acquired infections were low actually coincided with a pandemic, a time when infection with SARS-CoV-2 was high. Thus, the reduction in AIDP stemming from the decrease in community acquired infections may have been counteracted by an increase in AIDP from COVID-19 or the immunizations designed to prevent it. The authors offer arguments discounting the role of COVID19, but I found them less than convincing. Nevertheless, the results of this study are highly interesting and suggest that AIDP in children is not triggered by an antecedent community-acquired infection. This begs the question: Then what is the trigger for AIDP? The answer is among the great unknowns. The authors offer several possibilities: uncommon infections, high lag time between infection and AIDP onset, and infections not impacted by social distancing. The evidence for any of these is meager. Thus, the triggering factor for the most common acquired neuropathy in childhood remains a mystery. •


Child Neurology Society | Summer 2023 23
Link to CNS Synapses Library
Daniel J. Bonthius, MD, PhD Medical Director, Pediatric Neurology Levine Children’s Hospital

Child Neurology Synapses
Genetic Mutations can Mimic Hypoxic-ischemic Encephalopathy in Newborns
“Identifying genetic susceptibility in neonates with hypoxic-ischemic encephalopathy: A retrospective case series.” Woodward KE, et al. Journal of Child Neurology 2023; 38: 16-24.

What the researchers did: Neonatal hypoxic-ischemic encephalopathy (HIE) is a major cause of neurologic injury and death in newborns. This encephalopathy, which is due to perinatal asphyxia, can be treated with therapeutic hypothermia to mitigate its associated brain injury and improve its outcome, if the diagnosis is made promptly. However, some neonates present with a clinical picture of HIE but lack risk factors for perinatal asphyxia. For example, not uncommonly, babies are born encephalopathic, sometimes
even with MRI scans suggestive of HIE, following labor and delivery that seemed uncomplicated and without any sentinel event. In some of these cases, alternative diagnoses are found, including inborn errors of metabolism, infections, vascular lesions, and congenital malformations. However, in other cases, no alternative explanation is readily noted, and these babies are often diagnosed with HIE and treated with hypothermia, despite weakness in supportive evidence. For some of these babies, the cause may be genetic. In this study, a group of Canadian researchers hypothesized that some of these patients have mutations in susceptibility genes, particularly in genes that mediate energy metabolism pathways, thus increasing their risk of cerebral energy failure during labor and delivery.
CRAFT
CNS CONNECTIOINS EDITOR
24 Child Neurology Society | Fall 2022
What the researchers found:
The researchers conducted a retrospective case series in which they reviewed all neonates diagnosed with HIE over a five-year period at several neonatal ICUs in Calgary, Alberta, Canada (n=210). Of these patients, they identified 28 who had undergone genetic testing, including microarray, whole exome sequencing, or a gene panel because of clinical suspicion that perinatal hypoxia was not the full explanation for their condition. The researchers found that ten of the 28 patients had genetic mutations that explained or contributed to their encephalopathy. Most of these genes encode proteins involved in ion channels or cellular metabolism. Of these ten patients with genetic defects, five had refractory seizures, and seven had MRI findings consistent with severe hypoxic-ischemic encephalopathy. Based on the genetic results, the choice of anticonvulsant was changed for two patients (both with channelopathies, prompting a switch to oxcarbazepine) with subsequent substantial improvement in seizure control. All of these patients with genetic defects who were followed had global developmental delay, and most had epilepsy, again mimicking the outcome of HIE.








What the research means:
As is probably true of all diseases, HIE can be impacted by a patient’s genes. A patient’s genetic background can make his or her acute disease and longterm outcome from HIE either better than expected or worse than expected, based on the risk factors alone. When genetic mutations are discovered that underlie or contribute to a newborn’s encephalopathy, specific measures can sometimes be taken, such as choice of anticonvulsant or exposure to or avoidance of therapeutic hypothermia, that can substantially impact the patient’s outcome. Thus, for newborns with encephalopathy who lack significant risk factors, especially those whose histories do not include a clear sentinel event, alternative diagnoses should be strongly considered, and genetic testing should ensue. •
Child Neurology Society | Summer 2023 25
Link to CNS Synapses Library
Daniel J. Bonthius, MD, PhD Medical Director, Pediatric Neurology Levine Children’s Hospital

Child Neurology Synapses
Fetal Exposure to Anticonvulsants and Later Risk of Psychiatric Disease
“Prenatal exposure to antiseizure medication and incidence of childhoodand adolescence-onset psychiatric disorders.” Drier JW et al. JAMA Neurology 2023; 80:568-577.

What the researchers did:
As many as 2% of all children born in Western countries are prenatally exposed to anti-seizure medications (ASM). These fetal exposures occur not only because of maternal epilepsy, but also for other indications, including maternal migraine, mood disorders, and neuropathic pain. Antiseizure medications bind to and interact with neuronal receptors. Indeed, this interaction with neurons is the very essence of their action and usefulness for epilepsy and other neurologic disorders. However, since they are interacting with the maternal
nervous system, then they are certainly interacting with the fetal nervous system as well, and this interaction may cause harm. Indeed, there is already strong evidence that valproate during pregnancy can cause neural tube defects and other congenital anomalies, along with an increased risk of attention deficit hyperactivity disorder (ADHD), autism spectrum disorder, and impaired cognition in the offspring. However, information regarding other anti-seizure medications during pregnancy and their link to psychiatric disorders in childhood is limited. To address this deficit, an international group of researchers from the Nordic countries of Europe systematically examined the association between prenatal exposure to common anti-seizure medications and psychiatric disorders of childhood and adolescence.
CRAFT
CNS CONNECTIOINS EDITOR
26 Child Neurology Society | Fall 2022
What the researchers found:
The researchers performed a prospective, population-based study of children born in Denmark, Finland, Iceland, Norway, and Sweden. They defined a child as “prenatally exposed” if the mother took an anti-seizure medication throughout gestation. They followed the children from birth up to 22 years and calculated incidence rates of psychiatric diseases, which they broke down into early-onset disorders (intellectual disability, developmental disorders, ADHD, autism, and attachment disorder) and late-onset disorders (anxiety, mood, substance abuse, schizophrenia). The investigative group was children of mothers with epilepsy who were treated with medications, while the reference group was children of mothers with epilepsy who were unexposed. The researchers identified more than 38,000 children of mothers with epilepsy, of whom more than 16,000 were prenatally exposed to anti-seizure medications. Prenatal exposure to valproate monotherapy led to 1.80-fold significantly increased risk of one of the combined psychiatric disorders. Monotherapy with none of the other anti-seizure medications led to an increased risk of the combined psychiatric disorders. However, polytherapy, with or without valproate, led to an increased risk of a psychiatric disorder. The children prenatally exposed to valproate had an increased risk specifically of the early-onset disorders (intellectual disability, autism, ADHD, and attachment disorder), and not of the late-onset disorders (anxiety, mood, schizophrenia, and substance use). Lamotrigine, oxcarbazepine, and carbamazepine had no increased risk of
any psychiatric disorder in the offspring. Analyses of levetiracetam and topiramate were limited by low numbers, but prenatal levetiracetam exposure was associated with increased rates of anxiety and ADHD, while topiramate exposure appeared to increase the risk of ADHD, intellectual disability, and autism.








What the research means:
As child neurologists, we all see children whose mothers have epilepsy and were treated with antiseizure medications during pregnancy. In addition, many of us prescribe anticonvulsants to girls or young women of child-bearing age. This research can strongly guide the information and advice that we give our patients and their families. Valproate is clearly a dangerous medication during pregnancy and should only be used with necessity and warnings. This research also supports ongoing concerns about the use of topiramate by pregnant women and raises similar issues regarding levetiracetam. On the other hand, this research provides reassuring evidence that oxcarbazepine, carbamazepine, and lamotrigine during pregnancy are not associated with behavioral or developmental disorders in the offspring. One other note to be made regarding this research is the illustrative power of the collaboration that it required. Data for this study was gathered from five Nordic countries, each of which was probably too small to yield a data set with adequate power. By combining the data from five countries, the researchers were able to construct a powerful data set that yielded valuable insights. •
Child Neurology Society | Summer 2023 27
Link to CNS Synapses Library
2023 Arnold P. Gold Foundation Humanism in Medicine Award
 Yasmin Khakoo, MD, FAAN, FAAP
BY ALISON CHRISTY, MD, PHD
Yasmin Khakoo, MD, FAAN, FAAP
BY ALISON CHRISTY, MD, PHD
As a pediatric neuro-oncologist, a physician-scientist, a devoted mentor, and Editor-in-Chief of Pediatric Neurology, Dr. Khakoo exemplifies extraordinary humanism through her caring and thoughtful communication with patients and colleagues; her devotion to patient advocacy; and her work with medical education and support of women and underrepresented minorities in medicine.
Born in the Bronx, to Hamida Khakoo, MD and Yusuf Khakoo, MD, two immigrant physicians from India and Africa, Dr. Khakoo initially wanted to be a third grade teacher. At Barnard College, a women’s liberal arts college, she won the Best Freshman in Chemistry Award and subsequently decided to study medicine to become a pediatrician. She graduated from Barnard in 1986 and attended Columbia University College of Physicians and Surgeons for Medical School. Though she fondly remembers working with Doug Nordli, MD during “Introduction to the Patient,” and shadowing Arnold Gold. MD, once or twice, she was terrified of neuro-anatomy. Even when working with Columbia adult neurology stars Carolyn Britton, MD and John Brust, MD, she never envisioned a career in neurology.

Dr. Khakoo then went to the University of California, San Francisco (UCSF) for pediatric residency, where she was required to do a month of Child Neurology in her second year. Working with Tom Koch, MD, FAAP, she realized that a career in child neurology would check two important boxes: working with children and solving medical mysteries. While working at the Veteran Affairs Medical Center in San Francisco in 1993, she learned about paraneoplastic syndromes in lung cancer patients. Several months later, she saw a child with neuroblastoma-
associated opsoclonus myoclonus ataxia syndrome (NB-OMAS). With pediatric oncologist Katherine Matthay, MD, she drafted a proposal to study the serum of children with NB-OMAS and faxed this proposal to adult neuro-oncologists Josep Dalmau, MD, PhD, and Jerome Posner, MD, at Memorial Sloan Kettering Cancer Center (MSKCC). This project led to 3 publications, and her final resident presentation at UCSF: “Dancing eyes dancing feet: all ‘Hu’ ever wanted to know.”
During her 6 years at UCSF, Dr. Khakoo received 2 pediatric resident teaching awards. Donna Ferriero, MD, MS (who would later become president of the Child Neurology Society), encouraged her to study neuro-oncology. By then Dr. Khakoo had met and married another New Yorker, physician scientist Robert P. Fisher, MD, PhD. They left the Bay Area to return to the Big Apple, she as an adult neuro-oncology fellow and he as faculty at MSKCC. Other mentors at UCSF included former CNS President Bruce Berg, MD and Bill Weiss, MD, PhD. Dr. Khakoo stayed on at MSKCC, becoming full professor of clinical pediatrics at Weill Cornell Medical College (WCMC) in 2020. In addition to Drs. Dalmau and Posner, her mentors at MSKCC included Myrna Rosendfeld, MD, PhD, Lisa and DeAngelis, MD.
Dr. Khakoo started the MSKCC Pediatric Neuro-oncology (PNONC) Fellowship in 2005, training both oncologists and neurologists. One of her favorite events at CNS annual meetings is the Neuro-oncology Special Interest Group, where she reunites with former fellows, now leaders in neuro-oncology. Dr. Khakoo started and leads the Child Neurology MSKKids WCMC Joint Pediatric OncoNeurology Program and helped
28 Child Neurology Society | Summer 2023
CHILD NEUROLOGY SOCIETY 52nd ANNUAL MEETING October 4-7, 2023 • Vancouver, BC 2023
Yasmin Khokoo, MD, FAAN, FAAP
CALLING
develop the Leukodystrophy Transplant and Gene Therapy program across both campuses. She has always advocated for her patients at MSKCC where she works with pediatric and young adult children with CNS tumors and onconeurologic complications of other pediatric cancers. She is an international expert in neurocutaneous melanocytosis and continues her work in NB-OMAS.
Her significant scientific work allowed her to provide the very best care for her patients. Because the diseases she works with are rare, she created a national registry for patients with neurocutaneous melanocytosis; was a founding member of the Collaborative Ependymoma Research Network; and is part of the MSK team awarded membership in the Pediatric Brain Tumor Consortium, a national cooperative group dedicated to bringing new therapeutic agents into the pediatric arena.
Dr. Khakoo – in her eleventh postgraduate year when she became an attending – is an eternal student. In an ongoing pursuit of development, she participated in the Association of American Medical Colleges Leadership Development Programs. In 2019 the American Academy of Neurology selected Dr. Khakoo for the Women Leading in Neurology Program, which catapulted her into many leadership roles, including Vice Chair of the AAN Advancing Women in Academics Working Group alongside Chair Kathleen Shannon, MD, and former CNS President Ann Tilton, MD FAAN (202023), and joining the AAN Academic Hub Working Group. In 2020, she was named the Child Neurology Society Scientific Selection and Program
committee co-chair alongside Carl Stafstrom, MD, PhD, and from 20212023 was chair with Dr. Bhooma Aravamuthan, MD, DPhil. Due to their efforts, the CNS abstract/proposal review process now provides feedback to authors and gives credit for diversity, including gender, rank, institution and race.
At MSKCC she served on the Women’s Task Force and on ABLE (Abolishing Barriers and Limitations for Everyone), a committee to aid employees with health challenges and disabilities. She has been an active participant in the WCMC Pediatric Diversity Coalition since 2020, providing outreach to NYC public schools in underserved areas and encouraging trainees to apply for Pediatric Fellowships at WCMC. She is enthusiastic about medical education, and won the Pediatric Neurology Teaching Award at Weill Cornell Medical College in 2021. Dr. Khakoo seeks out opportunities to mentor others, and her list of formal mentees includes high school students, undergraduates, medical students, residents, fellows and faculty. She also mentors physician assistant students at WCMC and advanced practice providers in pediatrics at MSKCC. She is an active participant in the MSK Summer Medical Student Pipeline Program, a program that works to increase representation of underrepresented minorities in cancer care and research. She is thoroughly involved with her mentees and is an active sponsor for positions and awards. The summer medical students participate in clinics and clinical research but also join her at national advocacy conferences to meet patients with the
diseases they study. This extra step is emblematic of how Dr. Khakoo makes women and underrepresented minorities feel included – like we belong – in medicine. She offers “mentorship for life” and encourages her mentees to keep in touch.
As editor-in-chief of Pediatric Neurology since 2022, she is poised to change the future of our field. Her goals are to bring pediatric neurology into the digital age; diversify the board of the journal and the manuscript reviewers; engage trainees and junior faculty in the world of editing and publishing; and align child neurology with pediatric scientist development pathways. She was mentored in this role by former editor and current editorin-chief of Annals of Child Neurology, Steve Roach, MD. She has already used her position to advocate for vulnerable populations, discuss controversial topics, and promote and support those underrepresented in healthcare.
Dr. Khakoo lives in New York with her husband, physician-scientist Robert Fisher, MD, PhD and two children: Alex, a black belt in karate and martial arts instructor, and Aliya, a rising sophomore in college. Her daughter won a 2020 award from the New York Times for a high school essay about circadian rhythms and received one of four American Academy of Neurology Student Research Awards, presented to her as the Bhuwan Garg High School Neuroscience Award at the CNS annual meeting in 2022. Dr. Khakoo is also mom to Benny, the family pup. In her free time she enjoys learning languages, teaching cooking, reading, rooting for the Yankees and traveling. •
Child Neurology Society | Summer 2023 29
2023 Roger & Mary Brumback Lifetime Achievement Award
Radha Giridharan, MD
 BY HARVEY BENNETT, MD; YASMIN KHAKOO, MD, FAAN, FAAP; RAJESHWARI MAHALINGAM, MD; AND SAKKUBAI NAIDU, MD
BY HARVEY BENNETT, MD; YASMIN KHAKOO, MD, FAAN, FAAP; RAJESHWARI MAHALINGAM, MD; AND SAKKUBAI NAIDU, MD

Throughout her illustrious career, Radha Giridharan, MD (“Dr. Giri”) has combined clinical expertise, excellence in teaching and a humanistic approach to the care of patients. Her clinical skills were honed by two excellent neurologists, Drs. Joseph Marcus and Mahendra Somasundaram. In addition, Radha was mentored by some of the giants of pediatric and adult neurology – among them are Drs. Arthur Rose, Joseph H. French, Henryk and Krystina Wisiniewski, and Joan and Roger Cracco. Dr. Giri is a superb clinician –from her ability to connect with pediatric patients of all ages, to the methodical way in which she examines children, to the thought process behind localization, differential diagnosis and workup.
After fellowship, Radha joined the faculty at SUNY Downstate and has cared for the children of Brooklyn, a population who has often felt the negative impacts of healthcare disparities. In 2010, she helped found the non-profit organization, The Brooklyn Children’s Society of SUNY Downstate which supports supplemental health care programs for underprivileged children in the borough of Brooklyn.
The impact she has had in the field of Pediatric Neurology is far-reaching and extends beyond the individual patients she has taken care of directly. Her influence is felt in the medical students and pediatrics residents she inspired to pursue Child Neurology as a specialty through the many pediatric neurologists that she has mentored and trained throughout her career who are taking care of children across the country.
Radha has mentored more than 40 fellows over her career. Some of the more prominent Downstate and Brooklyn Hospital alumni that were her fellows include Dr. Andrew Mower at Nemours Children’s Health in Philadelphia, Dr. Kapil Arya at Children’s Hospital of Arkansas in Little Rock, Dr. Christian Ionita at Yale School of Medicine in New Haven, Dr. Namrata Shah at Le Bonheur Children’s Hospital in Memphis, Dr. Charuta Joshi at UT Southwestern, Dr. Priyamvada Tatachar at Ann and Robert H. Lurie Children’s Hospital of Chicago and Dr. Sagarika Nallu at USF in Tampa.
Radha is known to be unflappable and a great sport. She is a beloved and admired figure at the annual Child Neurology Society (CNS) meetings. Over the last forty years, since her first meeting in Hanover, New Hampshire in 1979 as a fellow in pediatric neurology at SUNY Downstate, she has been a regular attendee. Radha has also developed a niche in mentoring young Pediatric Neurologists of Indian Descent (PNID or APNI). She relays that at a CNS meeting in the mid 80’s she and Dr. Saku Naidu looked around and saw just two other pediatric neurologists of Indian descent. They decided to have a luncheon and so was launched the annual PNID dinner that has taken place now for so many years. It generally takes place on a Wednesday or Thursday night at a local Indian restaurant in the host city. There are over 130 names on Radha’s invite list and many honorary APNI attend as well. Roger Larson attended, and President emeritus
30 Child Neurology Society | Summer 2023
Radha Giridharan, MD
CHILD NEUROLOGY SOCIETY 52nd ANNUAL MEETING October 4-7, 2023 • Vancouver, BC 2023 CALLING
Phillip Pearl has promised to attend an upcoming dinner. It appears that PNID (APNI) have become a substantial percentage of our Society. She participated in a terrific CNS webinar for AAPI month in June 2022 and was interviewed by previous CNS executive director Roger Larson in 2021.
Radha’s concern for humanity goes beyond clinical medicine. Since 1985 she has been leader and active member of Heart and Hand for the Handicapped (HHH), an organization that supports programs for handicapped children in India and the U.S. ensuring that their medical and social needs are being met through funding programs for children with developmental disabilities and autism as well as polio vaccination programs, eyesight restoring surgeries to name a few.
This giant of Pediatric Neurology comes from humble beginnings. She was born in South India to a nurturing mother and a father who was in the military. Due to his career, the family had to move frequently. Radha relayed that her father decided that she would be a physician and so it was. She attended Sri Venkateswara Medical College. Admiration for her excellence in clinical skills and teaching began early. She was a brilliant medical student who was awarded a ‘Gold Medal’ for Best out Going Medical Student in India with Honors in Physiology, Forensic medicine, Gynecology & Surgery. In the United
States she was also appreciated as an outstanding attending in the Deportment of Pediatrics at Brooklyn Jewish hospital (1982), Brookdale Hospital, Brooklyn, N.Y (1987, 1990), Attending of the year Brooklyn Hospital NY (1996) and Maimonides Hospital (2000). She was given a Certificate of Appreciation for “Outstanding service and dedication at SUNY Downstate University in Kings County Hospital (2007). At a national level, she was recognized with the “Teacher Recognition Award “ from the America Academy of Neurology and A.B. Baker section on Neurologic Education – AAN Annual Meeting, April 2009.
In 1972 she was married to Dr. Swaminathan (Giri) Giridharan. Giri had been accepted to a residency in Internal Medicine in Brooklyn, NY, and when their daughter was 6 months old, the young family moved across the oceans and began their sojourn in the United States.
Radha and Giri have two children, Varsha and Sivaswami (Siv). Varsha followed in her parents’ medical footsteps and is a Family Physician. She and her husband, Karthik, live in Chicago where they are raising their 2 sons. Siv is a Solution Manager at AIM Specialty Health and also lives in Chicago with his wife, Cecilia, and their 2 young children. Giri continues to practice Internal Medicine and Endocrinology in Brooklyn as he has done for the last 40+ years.
Radha also has many hobbies. Among them, reading and travel are her favorites. Places she has visited include China, Hong Kong, Singapore, Dubai, Egypt, Israel, Tanzania, and many European countries. She frequently visited her mother in India. Radha and Giri also have traveled to see the Olympics (Lake Placid, Los Angeles, and Atlanta) and several international tennis tournaments (US Open and Wimbledon).
Radha’s love affair with the borough of Brooklyn, its children, Downstate Medical Center, and the field of Child Neurology, never stops even in semiretirement. Her keen mind and big heart continue to push forward. We are proud to have her as a friend, colleague, and mentor. She is a credit to the field of Pediatric Neurology, to the Society, and to the world at large. •
Child Neurology Society | Summer 2023 31
2023 Roger & Mary Brumback Lifetime Achievement Award
Robert Greenwood, MD
BY O’NEILL D’CRUZ, MD, MBA, FAAN
Two score and ten years ago, a young Chief Military Pediatrician at Walter Reed Army Medical Center completed military service, received an Army Commendation medal for setting up a child developmental evaluation clinic, and returned to Washington University, St Louis, MO. He resumed Child Neurology training under the guidance of Dr Phillip Dodge, a compassionate clinician and mentor who became his model. The young resident also joined the Child Neurology Society, which today recognizes and celebrates fifty years of contributions by Dr Robert (Bob) Greenwood for his service to society and humanity with the Brumback Lifetime Achievement Award. Anyone who knows Bob will readily acknowledge that he’s had the time of his life adding life to the years of those around him!
Bob fondly recalls growing up in Texas in a family that installed in him a keen work ethic, a sense of community and kinship with children and families of various ethnic and socio-economic backgrounds, and an attitude of gratitude when sharing one’s gifts and talents “to cure rarely, to relieve suffering often, to comfort always” (Osler’s aphorism for healers). These values have shaped and guided Bob in all his professional endeavors over the years.
When Bob joined Thomas Farmer, a founder-parent figure in Child Neurology, at the faculty at University of North Carolina-Chapel Hill (UNC) in 1977, he set upon a career path that combined lifelong learning, leading and lighting the path for later generations of child neurologists.

In each of these fields of endeavor, he walked and talked with others, and rarely, if ever, talked about his achievements and accolades. Thus, one has to listen in at UNC Child Neurology picnics and reunions to learn what Bob meant to trainees, as they recall the impact he had on shaping their career path.
It is said that the best way to learn is to teach – Bob’s passion for lifelong learning is evident in his commitment to teaching at all levels. His teaching activities span across high-school level, pre-med, medical students and residents in the US and visiting international graduate students. In addition to serving as medical school faculty since joining UNC, Bob served on the faculty of UNC’s Neurodevelopmental Disorders Research Center and the Carolina Institute for Developmental Disabilities for close to two decades. As a member, and later Chair, of ACGME’s Neurology Resident Review Committee(RRC), Bob was instrumental in gaining ACGME approval for training programs in Neurodevelopmental Disabilites, Vascular Neurology and Pain Management. He also partnered with neurosurgery and neuroradiology RRCs to allow neurologists to train in Interventional Neuroradiology. Bob received UNC’s Neurology Faculty Teaching Award and NIH’s Teacher Investigator Award and National Research Service Award in recognition of his commitment to both teaching and research at local and national levels. Bob is highly sought after both in the US and overseas to teach, help set up curricula and training programs in Child
32 Child Neurology Society | Summer 2023
Robert Greenwood, MD
CHILD NEUROLOGY SOCIETY 52nd ANNUAL MEETING October 4-7, 2023 • Vancouver, BC 2023 CALLING
Neurology. Most recently, he was Chairman and invited speaker at the Annual Conference of the Neurology Department at Mansoura University in Egypt.
Bob’s earlier research focused on pathologic plasticity in epilepsy (longterm changes in neuroendocrine function following recurrent seizures, use of mRNA to modify epileptogenesis) and his more recent work on neurofibromatosis (morphological changes in white and gray matter in type 1, MR spectroscopic changes in type 1 and 2). His research in neurofibromatosis was supported by NIH grants for the study of cognition and behavior in children with NF1. Over a period of fourteen years, Bob served as a reviewer of Congressionally Directed Medical Research Programs (CDMRP) in the Department of Defense Neurofibromatosis Research program, and chaired both the Neurofibromatosis and Tuberous Sclerosis Research Program committees. He also served as reviewer for CDMRP’s clinical trial awards in Fragile X and Angelman Syndromes, and as a member of Citizen’s United for Research in Epilepsy (CURE) scientific review board.
Bob is a level 5 leader – one who combines extreme personal humility and intense professional will – in clinical settings. He is on the lists of America’s Top Pediatricians, Top Neurologists and Best Doctors in America since the 1990s. He is unhesitant and unassuming in what
he does so well – find ways to help associates and colleagues grow and thrive by providing opportunities, resources and mentoring at all phases of their careers. He always took his full share of on-call duty and outreach clinics. His regular clinics were consistently oversold, and with good reason – he combines extensive clinical acumen with a passion for patient care and a wonderful personal touch that makes him extremely popular, even (and especially) when he is working on “Greenwood Time!”
The people of North Carolina have benefited tremendously through Bob’s lifelong service. He received the Volunteer of the Year service awards from NC Epilepsy Association and Kiffin Penry Quality of Life from the Epilepsy Foundation of North Carolina for his contributions to the care of children with epilepsy. He served in various leadership roles, including Chair of the Professional Advisory Board and Board of Directors of North Carolina Epilepsy Association, and Vice-President of North Carolina Neurological Society. He facilitated statewide access to child neurology services through outreach clinics in underserved areas, serving on Governor’s Health forums and BCBS Neurology Advisory panels. Summer camps for children with epilepsy resemble family gatherings for Bob’s patients and their families!
Bob has long been active in various professional roles at a national level –examiner in Neurology for ABPN,
serving on CNS’ Legislative, Phillip Dodge Young Investigator Award, and Nomination committees; serving on the Executive Committee of AAN’s Child Neurology Section; and is a longstanding member of numerous national and international professional societies, including Professors of Child Neurology.
On a personal note, in 1991 Bob recruited me – the first person of color and international medical graduate in the Child Neurology division at UNC. His influence and example were so inspiring that it was the first and last job until my retirement from academia! After all, how often does one meet a division chief who shares one’s hobbies and is also a colleague, friend, mentor and tennis partner?
Finally, Bob is a model par excellence for child neurologists at all stages of their careers. He leads by example and serves with head, hands, heels (Go Heels!) and most of all, heart. Therein lies Bob’s secret worth emulating – it is the same one that was shared with the Little Prince: What is essential is invisible to the eye; it is only with the heart that one can see clearly! •
Child Neurology Society | Summer 2023 33
2023 Roger & Mary Brumback Lifetime Achievement Award
James Riviello, MD
BY HOWARD GOODKIN, MD, PHD
Dr. James “Jim” Riviello was born in Philadelphia and grew up in the Philadelphia suburb of Cherry Hill, N.J. His father was a general medical practitioner and his mother an office manager. During high school, he was interested in politics and history and briefly considered law as a career until he spent a week shadowing in a law practice.
Jim entered Tufts University in 1970 thinking he might be a classical historian, an area of study that his father did not view as very practical. Jim graduated from Tufts in 1974 with a double major in the classics and biology and remained at Tufts for medical school. During medical school, he quickly fell in love with Pediatrics. Then, at the start of his Pediatrics internship at St. Christopher’s Hospital for Children (SCHC), he fell in love with his co-intern and lockermate Susan B. Torrey, MD, whom he later married.
As a medical student and pediatrics resident, he worked with Dr. Angelo DiGeorge (of DiGeorge syndrome) and strongly considered pediatric endocrinology as a subspecialty. Unfortunately, when he asked Dr. DiGeorge about doing a fellowship, Dr. DiGeorge had just given away the last fellowship slot for the following year and didn’t have a position available. Inspired by his time working with the neurologist Warren D. Grover in the ICU, Jim decided to pursue a child neurology fellowship at SCHC with Dr. Grover. Notably, Dr. DiGeorge called him later to say that one of the endocrinology fellows was dropping out and he now had a position he’d like to offer Dr. Riviello. Not one to back out of a promise, Jim declined. The rest is history!
Jim’s very first weekend of child neurology training in 1980 provided him with a crash course in neurocritical care as he cared for 3 near-drowning patients and 2 patients with Reye Syndrome. During his

training, Jim credits Lawrence Brown as a standout teacher of child neurology who, along with Catherine Foley, introduced Jim to and refined his skills in EEG. After completing his child neurology fellowship, Jim expanded on his building interest in neurocritical care by doing a year of anesthesiology at Temple University.
After a brief stint on faculty at the A.I. duPont Institute in Wilmington, he was recruited back to SCHC by Dr. Grover in 1985. Together, they developed a fiveyear plan for Dr. Riviello to become a neurocritical care specialist while helping with the epilepsy service. Many of his early papers from SCHC were on status epilepticus or neurocritical care topics. He recalls caring for patients with maplesyrup-urine disease with Dr. DiGeorge and co-authoring his favorite paper with Dr. DiGeorge and Dr. Foley (Riviello et al. “Cerebral edema causing death in children with maple-syrup-urine disease”. Journal of Pediatrics 1991).

In 1990, he left SCHC and moved to Maine Medical Center where he joined the Maine Neurology group. Jim served as the epilepsy specialist for the practice and teamed with Walter Allan and Steven Rioux to create a pediatric intensive care service, which he directed. After a year, his wife Susan (a pediatric emergency medicine specialist) was recruited to Boston Children’s Hospital (BCH) by Gary Fleisher to develop their satellite program in Framingham. Dr. Joseph Volpe created a position in the Epilepsy Program for Jim with the goal of expanding the ICU EEG monitoring.
At BCH, Jim had the privilege of working with many excellent pediatric epileptologists including Gregory Holmes, Mohamad Mikati, Frank Duffy, and Sandy Helmers as well as excellent EEG technicians like Lewis Kull and Faye McNall. While in Boston, he
34 Child Neurology Society | Summer 2023
James Riviello, MD
CHILD NEUROLOGY SOCIETY 52nd ANNUAL MEETING October 4-7, 2023 • Vancouver, BC 2023 CALLING
developed expertise in epilepsy surgery and international recognition for the treatment of epileptic encephalopathies (specifically Landau-Kleffner Syndrome and ESES). In addition to his pediatric epilepsy role, he also directed the BCH inpatient neurology service for which he developed a comprehensive teaching curriculum and quickly become a soughtafter mentor and teacher of many of today’s leading pediatric epileptologists including Elizabeth Thiele, Ignacio Valencia, Howard Goodkin, Cigdem Akman, Elizabeth Donner, Rana Said, Ann Poduri, Cecil Hahn, Alex Rotenberg, Tristan Sands, and many others. In 1996, Dr. Riviello along with Adre du Plessis, Michael Rivkin, Daivd Urion, and Basil Darras created the Neurocritical Care Service, the first dedicated pediatric neurocritical care service in the US. He worked full-time on the Neurocritical Care Service, furthering his interests in status epilepticus, refractory status epilepticus, continuous EEG monitoring, and Neurocritical Care, while also remaining active on the Epilepsy/EMU service.
Dr. Riviello left BCH in 2007 for Texas Children’s Hospital (TCH)/Baylor University. He spent time in New York City at NYU (2011-2013) and Columbia (2013-2017) before returning to TCH. During this period of his career, he worked alongside many leaders of pediatric neurology and epilepsy including Gary Clarke, Dan Curry, Orrin Devinsky, and Howard Weiner. He is especially proud of his work at TCH with Drs. Weiner and Curry, with whom he pioneered the field of minimally invasive pediatric neurosurgery, starting with laser ablation and neuromodulation.
At TCH, Dr. Riviello has served as the Director of Epilepsy and Clinical Neurophysiology, the Chief of
Neurophysiology, and developed a Neurocritical Care program. Since his arrival at TCH, he has been part of tremendous growth of the faculty and facilities. The TCH Neurocritical Care and Epilepsy Programs now include 20 faculty members, an 11-bed Pediatric Neurointensive Care Unit with hard-wired continuous EEG machines, a dedicated EMU within the Neurointensive Care Unit, a neurocritical care fellowship, and (soon) a Neonatal Neurology Service.
Included in Dr. Riviello’s research portfolio are several projects on FIRES, including the use of anakinra, biomarkers, and a Delphi analysis. He is now a Board member for the NORSE institute and was a founding member of the Pediatric Status Epilepticus Research Group (pSERG) along with Tobias Loddenkemper, Tracy Glauser, Kevin Chapman, William Gaillard, and Howard Goodkin. The pSERG collaboration has now produced about 15 papers. His other favorite paper is the one he wrote along with Mustafa Sahin (while he was a his child neurology resident) on “Outcome of severe refractory status epilepticus in children” (Epilepsia 2001). He and Mustafa wrote three papers together on refractory status epilepticus.
Dr. Riviello is a beloved educator and has been recognized with teaching awards at Boston Children’s in 1995 and 2007, the teaching award for the entire Department of Neurology at Columbia in 2015, and the Neurology Teaching Award at Texas Children’s Hospital/Baylor College of Medicine in 2018. He has been inspired by his TCH Neurocritical care colleagues including Jenny Erklauer, Yi-Chen Lai, and Sarah Risen. Several of the Child Neurology residents on the TCH Neurocritical care service created a T-Shirt with Jim’s likeness on it, wearing
sunglasses, with the initials W.W.R.D., meaning, “What would Riviello do?”
Dr. Riviello is proud to be the descendant of two other lifetime achievement award winners, Dr. Grover, awarded in 2011 (for whom Jim wrote the biography), and Dr. Grover’s mentor at CHOP, Dr. Charles Kennedy, in 2007. He is also proud to have worked closely with Dr. Lombroso at BCH, another lifetime achievement awardee.
Dr. Riviello believes that this Mary and Roger Brumback Lifetime Achievement Award also belongs to the many residents and fellows he has been fortunate to work with and receive stimulation from (“some of the best people ever!”), the great colleagues he has learned so much from, and the patients and their families. He is humbled that many of his trainees who have gone on to be world leaders in their specialties still look up to him and consider him a mentor. He is grateful for what they generously continue to teach him.
Finally, Dr. Riviello is so proud of his family. His wife, Susan B. Torrey, MD, a Pediatric Emergency Medicine and Global Health specialist, was the founding director of the Emergency Medicine Global Health program at TCH, and more recently the Division Director of Pediatric Emergency Medicine at NYU from 2011 to 2017. His sister has a PhD in nursing and has been the director of nursing programs and nurse practitioner PhD programs. His son, Peter, is a neuroradiologist at NYU, and his daughter, Elizabeth, works in the interface between the users and IT at WGBH in Boston. He is particularly grateful to his wife for so graciously supporting his academic career over their many years together. •
Child Neurology Society | Summer 2023 35
2023 CNS-PECN Training Director Award

Rana Said, MD
BY DALLAS ARMSTRONG, MD
Dr. Rana Said has built one of the largest child neurology residency programs in the country, established herself as a highly sought-after speaker covering topics ranging from refractory status epilepticus to the use of cannabidiol for epilepsy, built a ketogenic diet program, won teaching award after teaching award, and ushered six new subspecialty fellowship programs through their first years. That alone would be enough to rest assured that all her long hours have left their mark on scores of physicians and hundreds of young patients, but Dr. Said is more than an expert clinician and astute researcher. She is a wholehearted leader, a champion of the entire person behind the residency application paperwork, a caring beacon to guide families through the hardest decisions of their lives with grace and candor. This signature aspect of her practice means that for generations, her gifts will live on in the researchers she mentors, the physicians she trains, and the patients who journey toward living a life unencumbered by their epilepsy.

It is only fitting that Dr. Rana Said entered the world with her twin, internist Dr. Nuha Said – bringing another along with her on the next big adventure from her very first breath. Dr. Said’s parents, Drs. Riyad and Salwa Said emphasized careful study and thoughtful curiosity in their children, and fanned the flame of each child’s uniqueness. Early on, Dr. Said was a nurturing force on her younger brothers, Dr. Fuad Said, now an adult nephrologist like his father before him, and Dr. Maher Said, Associate Professor of Economics at Stern Business School at NYU. The foursome grew up first in Chicago and later in Amman, Jordan, watching both their parents balance studious attention to their field with loving cultivation of their children’s gifts.
When time came to begin postsecondary education, Dr. Said and her sister traveled together to the University of Jordan School of Medicine, then crossed an ocean to study together in Boston, where Dr. Said trained at Tufts University’s Floating Hospital for Children in both Pediatrics and Child Neurology. Dr. Said is a consummate pediatrician: officially, as she continues to sit for pediatric boards at each renewal, and pragmatically, as she diligently listens to breath and heart sounds in even the busiest of visits. During appointments full of complex epilepsy management decisions, she never neglects to address practical mental health boosting choices a teen can make. While studying adult neurology at Tufts, she inadvertently attracted attention from co-residents as she laid a hand on the forearm of an elderly patient alone in a hospital room, or crouched to eye level to speak softly to patients with a loving lilt in her voice. You could take the pediatrician out of the children’s hospital, so the joke went, but Rana would still be Rana.
The time at Tufts was full of highlights: exposure to a breadth of clinician perspectives, notably Dr. Paul Rosman whose warmth toward patients and trainees alike as well as the exhaustive differential diagnosis lists made his teaching particularly significant, the realization that despite her fascination with all aspects of child neurology, she was drawn to the intrigue of EEG interpretation. Most memorable of all was the double wedding Dr. Said planned with her sister, ensuring that limited resident vacations wouldn’t keep them from standing beside one another on their wedding day.
Epilepsy fellowship began at Boston Children’s Hospital under the tutelage of Dr. Blaise Bourgeois, amongst so many other influential voices. The volume of EEGs alone was a selling point, given that the
36 Child Neurology Society | Summer 2023
Rana Said, MD
CHILD NEUROLOGY SOCIETY 52nd ANNUAL MEETING October 4-7, 2023 • Vancouver, BC 2023 CALLING
old neurology adage that one “learns neurology one stroke at a time” has a clear corollary in neurophysiology. It was in the fellow’s chair that those early questions began regarding best practice in status epilepticus, a series of questions that shaped her career as an expert in new-onset status epilepticus (NORSE) and the related entity febrile infectionrelated epilepsy syndrome (FIRES). Her second year at Boston Children’s Hospital was a treasured opportunity to conduct research and an important seed was planted that has grown into the current Angelman Syndrome clinic she now leads.
As a freshly-minted assistant professor, Dr. Said came to Dallas, Texas in 2004 with two young children and her husband Dr. Gaith Semrin, a pediatric gastroenterologist. She walked into a child neurology training program that was struggling. On probation from the ACGME, the program only intermittently filled its single position prior to her arrival. Her first act as Program Director was to approach the program as she did her patient’s medical work-up: with clear eyes, laser focus, inexhaustible energy, and her characteristic vision. Dr. Said transformed the program, innovating with each passing year, even growing from one resident per class to the current complement of five trainees each year. Residents were learning and working on a busy service but — for the first time — had an advocate focused on preventing burnout, long before it was widely talked about. She also worked to support the development and growth of the Neurodevelopmental Disabilities residency during that time. In recognition of her impact, she was recently the inaugural awardee of
the Excellence in Graduate Medical Education Award by UT Southwestern GME. As a testament to her contributions, she received no less than 16 nominations for this award.
Dr. Said’s leadership during the COVID-19 pandemic was truly inspiring. She changed the inpatient processes to incorporate in-person and virtual rounding and was instrumental in the process to pivot to telehealth clinics, all while personally covering for colleagues, without hesitation, when they were quarantined or had risk factors too high for in-person work. The latter is a particular and long-standing interest of Dr. Said’s, giving rise to her current position as Chair of the Resident Wellness and Wellbeing Committee. Even as the department grew and service commitments were less frequent, she made sure to spend significant time on general neurology service with residents, in addition to the busy epilepsy service weeks she spent with fellows, always arriving with characteristic enthusiasm, ready to teach and eyes bright as she showed a medical student the power of a careful neurologic examination.
During her years as program director, she led numerous culture-shaping initiatives such as the Dr. Iannaccone Pediatric Research Days, which has grown over the past three years to a two-day event that showcases neurology residents, fellows, post-doctoral research fellows and medical students and a nationally invited keynote speaker. In the short span of the last four years, she has been essential to the creation of several fellowships and has directly mentored new fellowship directors in Pediatric Headache Medicine, Pediatric Epilepsy, Pediatric Clinical Neurophysiology, Fetal and Neonatal
Neurology, Pediatric Vascular Medicine, and most recently, Pediatric Movement Disorders fellowship. She developed and implemented the institutional clinical protocol for the management of status epilepticus and sits on the American Epilepsy Society’s NORSE/ FIRES Consensus Treatment Guidelines committee. Even in the case of resident research days or a fairly standard response to status epilepticus, Dr. Said takes something already excellent and makes it better — every time.
Even wearing her many hats, the one call Dr. Said never lets go to voicemail is the one from her sons. Her two sons are now men, Omar a sophomore at the University of Colorado Boulder and Saeed a recent graduate of the same alma mater now working in the consulting industry. Just as her own mother’s trailblazing path to becoming a pediatric specialist in allergy and immunology inspired Rana to look for the intersection of her own talents and the needs in her community, so Dr. Said has paved the way for her own children to follow in the same legacy of service.
On any given Tuesday, Rana can be found either in clinic, in the lecture hall, or on the wards, often teaching, always making a difference in big ways and small. Since 2009 Dr. Said has served dutifully as the Medical Director for the Epilepsy Foundation of Texas’s Kamp Kaleidoscope, a camp for teenagers with epilepsy, where she earned the moniker “Razzle Dazzle.” In so many ways, and certainly as a program director, dazzle she has indeed. •
Child Neurology Society | Summer 2023 37
2023 Martha Bridge Denckla Award
William Davis “Bill” Gaillard, MD
BY PHILLIP L. PEARL, MD
William Davis “Bill” Gaillard, MD is well known for his innumerable contributions to the pediatric neurology and epilepsy communities. He is a preeminent leader in the clinical investigation of language plasticity during development and in the epilepsy population, as well other populations of neurodevelopmental disabilities including autism and pediatric stroke.
Dr. Gaillard graduated from Yale College Magna Cum Laude with a degree in History. He continued at Yale University for medical school. There, he won awards for History of Science and Medicine for his work on The Great Plague at Athens as well as for his medical thesis studying single-cell neurophysiology in Aplysia californica. He spent two years as a Pediatrics resident at the Children’s Hospital of Pittsburgh and completed Pediatric Neurology fellowship at Johns Hopkins. After Pediatric Neurology training, he pursued a fellowship at the Clinical Epilepsy Branch at NINDS in epilepsy, clinical neurophysiology, and neuroimaging, under the mentorship of Drs. William H. Theodore, and Susumu Sato, among others. There, in collaboration with Dr. Lucie HertzPannier and others, he conducted the first functional (fMRI) studies of cognitive and language development in children (e.g., Gaillard et al, Functional anatomy of cognitive development: fMRI of verbal fluency in children and adults, Neurology 2000).
He was quickly recruited to the faculty at George Washington University and Children’s National Medical Center in 1993. Because of his experiences at Johns Hopkins and NINDS, he developed a longstanding interest in brain development, epilepsy, and the effects of pathologic processes, especially epilepsy, on the developing brain. Much of his work, using various neuroimaging tools and detailed neurocognitive assessments, performed in collaboration with superb neuroimagers and neuropsychologists, has centered on

the impact of epilepsy on brain structure, function, and connectivity with an emphasis on cognitive systems, especially language as well as in other developmental disorders and stroke. His initial publications were focused on the use of PET for localization of epileptic foci in an era when FDG PET was just emerging as an important evaluative tool for epilepsy surgery candidacy (Theodore, Gaillard, et al, PET Measurement of CBF and Temporal Lobectomy, Ann Neurol 1994; Gaillard et al, FDG-PET and Volumetric MRI in the Evaluation of Patients with Partial Epilepsy, Neurology 1995; Gaillard et al, Interictal Metabolism and Blood Flow are Uncoupled in Temporal Lobe Cortex of Patients with Complex Partial Epilepsy, Neurology 1995; among others).
Over the next decade, his work segued into a progression of innovative and subsequently landmark studies on the use of functional MRI to map language in children (following work using O-15 Water PET in adults). Exemplars include: Gaillard et al, Language dominance in partial epilepsy patients identified with an fMRI reading task, Neurology 2002; Gaillard et al: Atypical language in lesional and nonlesional complex partial epilepsy, Neurology 2007; Berl et al (Gaillard – senior author): Characterization of atypical language activation patterns in focal epilepsy, Ann Neurol 2014; Berl et al (Gaillard – senior author): Vulnerability of the ventral language network in children with focal epilepsy. Brain 2014 Croft et al (Gaillard – senior author). These represent an elegant series of papers demonstrating reorganization of cortical language representation in children with epilepsy, including elucidation that early seizure onset and atypical handedness are determinants of language reorganization, and differences in activation between dorsal and ventral language networks.
He has published over 260 original articles and over 75 chapters and reviews. Further examples of the breath of his scholarship

38 Child Neurology Society | Summer 2023
William Davis “Bill” Gaillard, MD
CHILD NEUROLOGY SOCIETY 52nd ANNUAL MEETING October 4-7, 2023 • Vancouver, BC 2023 CALLING
include his senior authorship on multiple publications including: identification of region-specific developmental trajectories in activation of the language network (Human Brain Map, 2012); fMRI pattern separation of language networks in pediatric epilepsy (Human Brain Map, 2012); sub-patterns of language re-organization in pediatric localization related epilepsy (Human Brain Map, 2011); functional connectivity of the inferior frontal cortex in children with autism spectrum disorder (Cereb Cortex, 2009); limitations in language plasticity of language re-organization after locationrelated epilepsy (Brain, 2009; and the use of fMRI to identify regional specializations of neural network in reading for young children (Neurology, 2003).
Extension of this work has also led to seminal findings in typical and atypical language development, from the demonstration of brain hyperconnectivity in autism (Supekar et al: Brain hyperconnectivity in children with autism and its links to social deficits, Cell Rep 2013) to the development of language lateralization with age (Olulade et al: The neural basis of language development: Changes in lateralization over age, Proc Natl Acad Sci 2020). This 2020 paper makes the seminal observation of right hemisphere homolog activation in young children, ages 4 through 6 years, with an age-related decrease in language activation only in the right hemisphere homolog of Broca’s area. This has major implications for early right hemisphere language activation as a developmental mechanism for recovery following early left hemispheric injury.
Dr. Gaillard has pioneered this work at the Children’s National Hospital in Washington D.C., where he has been on staff since 1993. He is presently both Chief of the Division Neurology and the Division of Epilepsy and Neurophysiology
at Children’s National. In addition to leading these two large divisions, he is also co-Director of the DC Intellectual Developmental Disability Research Center (IDDRC) which has been continuously funded since 2001 and is funded through 2025. Dr. Gaillard has been Associate Director of the IDDRC since 2011. He has also served as Director of its neuroimaging core.
For his work to unlock the mysteries of brain development, brain connectivity, and the impact of epilepsy on language development he has received multiple peerreviewed grants. Dr. Gaillard has received many honors for his clinical research, and he has been visiting professor at leading institutions across the world including Harvard, Hospital for Sick Children (Toronto), University College of London, Johns Hopkins, Washington University (St. Louis), and Cleveland Clinic. He has served on multiple national committees, has been a member of the Research Committee of the Child Neurology Society, is a member of the Steering Committee of the Child Neurology Career Development Program (since 2016), and has recently completed his term as President of the American Epilepsy Society (AES) after serving as first Vice-President and second Vice-President, and Treasurer. He is also a member of the International League Against Epilepsy (ILAE) North America Epilepsy commission and has served as chair of the ILAE Diagnostic Commission and chair of the Pediatric Epilepsy Task Force.
Over the last 25+ years, Bill has mentored legions of child neurologists, psychologists, and neuropsychologists, many of whom are pursuing independent academic careers in child neurology and behavioral/cognitive sciences. His postdoctoral students have performed research on functional language network in
children with epilepsy (Drs. Madison Berl, and Leigh Septa, among others). His child neurology fellow trainees have continued their research into childhood developmental disabilities at leading institutions, including NIH (Drs. Marjory Garvey and Maria Acosta) and Children’s Hospital of Philadelphia (Dr. Adeline Vanderver), as well as becoming independent clinical / translational research investigators at Children’s National (Drs. Madison Berl, Andrea Gropman, Leigh Sepeta, John Schreiber, among others).
Sporting his trademark bowties, Bill has a signature sense of humor that delights and disarms any situation. He is well known for the salutation “Good Morning” any time of day, evening, or night, with the disclaimer that it’s morning in… (name an esoteric place in the other hemisphere). His trademark laugh is immediately recognizable to members of the CNS and AES communities. His wife, Adelaide “Sherri” Robb, M.D., is an accomplished Child and Adolescent Psychiatrist, and Chief of Psychiatry and Behavioral Health at Children’s National. Their son, Jonathan, is a pediatric neurology resident at the University of Michigan who will then enter an epilepsy fellowship, and their daughter, Schuyler, is 4th year medical student at Georgetown University School of Medicine.
In summary, the emphasis of Dr. Gaillard’s investigative focus during his outstanding career in child neurology has been the discovery of altered cortical language representation in early onset epilepsy, with applications to autism and other neurodevelopmental disorders as well as to the ontogeny of language development in the human brain. It is for this remarkable body of work that he is being awarded the Martha Bridge Denckla Award. •
Child Neurology Society | Summer 2023 39
2023 Philip R. Dodge Young Investigator Award
Siddharth (“Sid”) Srivastava, MD
BY ANNAPURNA PODURI, MD, MPH
Dr. Siddharth (“Sid”) Srivastava is the recipient 2023 Philip R. Dodge Young Investigator Award. This award recognizes his service, innovation, generosity, and impact on the field of child neurology, specifically in the areas of neurogenetics and cerebral palsy (CP).

Sid was born in Delhi, India, and moved to the US as a toddler. His father’s academic teaching career took their family to Raleigh, NC, then to New Paltz, NY, and finally to Baton Rouge, LA, where Sid grew up from age 6 until college. Sid obtained his B.A. in Biochemistry from Columbia University. He went on to medical school at the Johns Hopkins School of Medicine, where he received his M.D. as well as the award for excellence in medical student research. Sid deepened his keen interest in neurogenetic disorders and completed his residency in Pediatrics at Johns Hopkins and Child Neurology and Neurodevelopmental Disabilities (NDD) at the Kennedy Krieger Institute. This was just the beginning of what has blossomed into a career focused on neurogenetics that blends patient care with patient-oriented research.
Early research and clinical impact on genetic neurodevelopmental disorders

Sid’s research during NDD training focused on delineating the clinical spectrum and natural history of several neurodevelopmental disorders. His early work is exemplified by his 2014 article on clinical whole exome sequencing for childhood neurological disorders, which was selected as one of the best advances in the field of neurogenetics by Neurology Today. Sid’s robust foundation of clinical training and astute observations led him to delineate the phenotypes of many important neurogenetic syndromes (e.g., BRAT1, HIVEP2, PTEN, SHANK3), creating a path toward future clinical trials with well-
defined genetic conditions and well-defined outcome measures. In the rare disease space, Sid’s reports, for example, his paper with Dr. Sakkubai Naidu and team on the gene BRAT1 (Srivastava et al., Am J Med Genet, 2016), provide such an invaluable resource to those of us seeing patients with these rare conditions. Following his pediatrics and NDD training, Sid pursued a neurogenetics fellowship at Boston Children’s Hospital, supported through an NIH T32 grant.
During his neurogenetics fellowship, in addition to research, Sid immersed himself in various neurogenetics clinics and saw patients with tuberous sclerosis complex, brain malformations, genetic epilepsies, and unknown but suspected genetic disorders. He was noted to demonstrate clinical excellence, compassion, and collegiality in our multidisciplinary clinics. He also brought his neurodevelopmental training to our patients – what a gift it was to have Sid as part of any clinic, as he provided real-time neurodevelopmental evaluation and offered advice to parents of children with often newly diagnosed neurogenetic syndromes.
Sid’s research in neurogenetics impacts both precision diagnosis and precision treatment. In 2018, Sid contributed to a consensus development conference in Boston focused on the molecular diagnostic yield of exome sequencing for NDDs. He was the first author of the resulting manuscript, “Meta-analysis and multidisciplinary consensus statement: exome sequencing is a first-tier clinical diagnostic test for individuals with neurodevelopmental disorders,” which was published in Genetics in Medicine. The recommendations of this report have been echoed by the evidence-based clinical guideline of the American College of Medical Genetics and Genomics (ACMG)
40 Child Neurology Society | Summer 2023
Siddharth Srivastava, MD
CHILD NEUROLOGY SOCIETY 52nd ANNUAL MEETING October 4-7, 2023 • Vancouver, BC 2023 CALLING
in 2021. He has also been working closely with several patient advocacy groups such as PMS Foundation, PTEN Research, iDefine, and his work was crucially instrumental in the approval of an ICD-10 code by the CDC for Kleefstra Syndrome, which is going to accelerate research in this ultra-rare disorder. Finally, Sid’s active role in the NIH-supported Developmental Synaptopathies Consortium has led to highly significant results, including the first clinical trial examining the effects of mTOR inhibitors on neurocognition in individuals with PTEN Hamartoma Tumor Syndrome (Srivastava et al., Human Molecular Genetics, 2022) and the “Updated consensus guidelines on the management of Phelan-McDermid syndrome” (Srivastava et al., Human Am J Med Genet A., 2023).
Genetics of CP – changing the landscape of CP and changing clinical practice
Sid’s insightful observations that a great many patients who are labeled as having “CP” may not actually meet strict definitions of CP formed the kernel of his current very active phenotype-genotype project, now supported by a K23 award from the NINDS with institutional support for trio exome sequencing from our Boston Children’s Hospital Rare Disease Cohorts (CRDC) Initiative. Since many patients referred to Sid and his clinical colleagues in our Cerebral Palsy Program have what is classified as ‘atypical CP,’ Sid raised the question about their etiologies and challenged the assumption that is prevalent among many individuals that all CP is acquired.
Sid’s path to uncover the genetics of CP has already started to transform the field of CP, long thought to be exclusively acquired and not genetic. Sid rapidly established an efficient and productive clinical research team, enrolling patients, performing rigorous research-level phenotyping that includes the precise delineation of phenotypic features, and conducting state-of-the-art genomic analyses. The first 50 patients sequenced from his clinic demonstrated a 25% diagnostic yield, with results that
Sid delivered back to the families. This is on par with the diagnostic yield of cohorts with epilepsy, autism spectrum disorder, and intellectual disability and were published with Sid as co-senior author (Chopra, Gable, et al., ACTN, 2021). Sid’s is one of only a few wellphenotyped cohorts of patients with verified CP, and the results have led to clinical impact locally already as well as independent collaborations between Sid and bench scientists at Boston Children’s and other hospitals around the country. Sid’s work brings a critically important level of rigor to push the field of CP genetics forward, and he has engaged actively with others in the field, including his K23 Co-Mentor, Dr. Michael Kruer, and last year’s Dodge Award recipient, Dr. Bhooma Aravamuthan.
Sid’s CP exome sequencing cohort now includes more than 250 individuals. This is an extraordinary number for such a short period of time and a testament to the true integration of his clinical practice with his research. Preliminary analysis has shown a molecular diagnosis in approximately 20% of his cohort, representing a wide spectrum of different biological pathways. He continues to collaborate with internal and outside partners delineating the phenotype of neurodevelopmental disorders including CP. He has most recently delineated a novel human disease gene, SPTSSA, implicated in a phenotype of complex hereditary spastic paraplegia (Srivastava et al., Brain, 2023). He has conducted a meta-analysis highlighting the diagnostic yield of exome sequencing and chromosomal microarray for CP, recently published in JAMA Neurology (Srivastava et al., 2022), demonstrating the generalizability of the research he and others are conducting and serving as the basis for evolving clinical practice guidelines for child neurologists seeing patients with CP.
Academic productivity, impact, and future promise
Over his relatively short career so far, Dr. Srivastava has had stellar productivity. This example is one from among 70 papers related to
neurogenetics (25 of them first-author, including in high-impact journals, such as Annals of Neurology, Brain, and JAMA Neurology). Sid’s publication record is remarkable on its own but even more so given that he started his career with a heavy clinical workload, and with great discipline and maturity, he has found a balance between honoring his commitment to our patients with CP and pursuing his critically important research. In 2014 and 2015, Sid was awarded an Outstanding Junior Member award from the Child Neurology Society. In 2020, Sid was promoted to Assistant Professor in Neurology at Harvard Medical School, a position he currently holds today.
Finally, Sid is incredibly thoughtful, collaborative, and kind. His resilience through the pandemic is exemplified by his impressive willingness to step up and help anyone and by his continued academic productivity. Sid and his wife, also a physician, have three young children. Sid has a genuine passion for working with families of children with developmental disabilities and complex disorders and bestows kindness and devotion to his patients and colleagues the way he does to his own family. He is actively engaged in training residents and students and embraces collaborations with a spirit of inclusiveness. His infectious enthusiasm for patient-oriented research has led to several residents and students seeking him out for mentorship, and Sid has indeed provided both content expertise and academic mentoring to all who come his way. His exceptional level of involvement in such a wide range of clinical, academic, and mentoring activities is a testament to his dedication to bringing science and scholarship to influence practice in the field of child neurology. Sid’s commitment to improve the lives of his patients and patients everywhere with childhood neurodevelopmental disorders is matched by his great potential for continued success, impact, and leadership in the field. •
Child Neurology Society | Summer 2023 41
2023 Bernard Sachs Award
Amy Brooks-Kayal, MD
 BY TALLIE BARAM, MD, PHD; JONATHAN MINK, MD, PHD; AND BRENDA PORTER, MD, PHD
BY TALLIE BARAM, MD, PHD; JONATHAN MINK, MD, PHD; AND BRENDA PORTER, MD, PHD
Dr. Amy Brooks-Kayal is a global leader in epilepsy research, with seminal contributions to our understanding of the cellular and molecular pathways that mediate the development of epilepsy following brain injury, with particular emphasis on GABAergic signaling and its regulation. Dr. Amy Brooks-Kayal embodies the seamless blending of individual research contributions and extraordinary contributions to research via guidance and mentoring of junior individuals as well as via influencing the policy and research directions of whole institutions.
She grew up in Florida and moved to Cornell for undergraduate studies and to enjoy snowy weather. She met her husband, Rana, at Cornell, and they are proud parents of two grown children Anjali and Zach, that keep her flying all over the world for adventures. Balancing work and family has always been a priority. She is a wine collector with a large cellar and a keen interest in keeping the table supplied with a pairing of good food and great wine.
Professionally, Dr. Brooks-Kayal has worked to develop novel therapeutic approaches to the prevention and treatment of both seizures and cognitive co-morbidities associated with epilepsy. She pioneered the development of pediatric rodent epilepsy models. These are now well established, but at the time there was controversy around the mild injury and limited or even absent cell loss that occurs in young animals following an episode of status epilepticus. The widespread acceptance that age dramatically alters epilepsy and epileptogenesis is in large part due to the work of Dr. Brooks-Kayal. The BrooksKayal lab, as well as several other labs,
have demonstrated that immature animals develop epilepsy without cell loss and with minimal to no neuronal sprouting, highlighting the distinct importance of incorporating development into the study of epilepsy. Her lab has been the major proponent of the role of GABA subunit switch in the development of epilepsy and the distinct difference in GABA subunit expression depending on the age of the animal at the time of epileptogenic insult.
Dr Brooks-Kayal has made three seminal discoveries: 1. Changes in GABAergic neurotransmission following epileptogenic brain injuries. Her laboratory first reported changes in GABA receptor subunits occurring within single dentate granule neurons in the hippocampus, specifically a reduction in α1 and increase in a4 subunits that correlated with changes in GABA receptor function including reduced Type I benzodiazepine sensitivity and increased sensitivity to zinc inhibition that would be predicted to reduce the effectiveness of inhibition during times of repetitive stimulation such as occurs at seizure onset. These findings suggest that as occurs during development, the GABAergic system is highly plastic following brain injuries and in chronic epilepsy, and that these changes vary by cell type and subregion of the hippocampus. With respect to scholarly activities, Dr. BrooksKayal has authored a large number of original research articles as well as review papers. She has some of the most cited publications (Hsu et al., PNAS 2003; Raol et al., Ann. Neurol. 2003; Brooks-Kayal et al., Nat. Med. 1998) in the field of GABA receptors and epilepsy. 2. Regulation of GABA receptor expression changes after epileptogenic brain injuries. Her research in this area focused on the

42 Child Neurology Society | Summer 2023
CHILD NEUROLOGY SOCIETY 52nd ANNUAL MEETING October 4-7, 2023 • Vancouver, BC 2023 CALLING
Amy Brooks-Kayal, MD
mechanisms regulating GABA receptor subunit expression and uncovered a role of BDNF in regulating seizureinduced regulation of GABAA receptor α4 and α1 subunits via the JAK/STAT pathway. Furthermore, her lab showed that blockade of this pathway with a JAK/STAT inhibitor could reverse BDNFinduced Gabra1 downregulation in cultured hippocampal neurons and most importantly in the dentate gyrus following pilocarpine- induced SE in rats in vivo. Towards this goal she published a seminal paper in Science Signaling (Lund et al., Sci. Signaling 2008) demonstrating the role of BDNF in regulation of GABAA receptor transcriptional activation via the JAK/ STAT pathway. 3. Development of disease modifying and preventative therapies for epilepsy. Her lab demonstrated that preventing the reduction in GABAA receptor subunit α1 expression after SE via viral-mediated transfer of an a1 subunit transgene in adult rodents reduced subsequent epilepsy development (Raol et al., J. Neurosci. 2006). These studies highlight the importance of a1 subunit downregulation as a critical mechanism contributing to development of acquired epilepsy. Her recent efforts have been focused on molecular dissection of the signaling pathway controlling the α1 subunit so that its expression can be therapeutically targeted. Towards this goal, her lab showed more recently that inhibition of the JAK/STAT pathway was disease modifying in adult rodent models of acquired epilepsy. They have identified a brain permeable STAT3 inhibitor, WP1066, that when administered systemically at the time of SE results in partial and transient inhibition of STAT3 phosphorylation in hippocampus in the rat pilocarpine model. Her discoveries are ripe for translation in human epilepsies.
The contribution of Dr. BrooksKayal to Neuroscience research extends far beyond her own work and is transforming the field in the present-
and the future through her leadership mentoring and scholarly activities:
Dr. Brooks-Kayal is currently Professor and Chair of the Department of Neurology at the University of California Davis. In her prior role as Chief of Pediatric Neurology at the University of Colorado, She established a division that grew to be a top 10 program nationally both in clinical care and research. Over the past 20 years, she has served as a mentor for numerous graduate students, postdoctoral trainees, and junior faculty in Pediatric Neurology and Neuroscience at the University of Pennsylvania, the University of Colorado and now, at Davis. Many have gone on to have successful independent careers in academic research.
The success of research with high relevance to child neurology demands that institutions at national and international levels recognize the vital importance of this research and provide appropriate funding and funding opportunities. Dr. Brooks-Kayal has championed this cause for two decades, with stunning commitment, aplomband effectiveness.
Commencing with her specialty, Epilepsy, Dr. Brooks-Kayal literally transformed the American Epilepsy Society. As Vice-president then President (2012-15), she revamped the management structure, which allowed funneling of millions of dollars to research rather than management companies. She led a 5-year strategic plan which prominently recognizes developmental epilepsies, and increased research funding provided to trainees and junior investigators by ~3 fold.
Dr. Brooks-Kayal, acting as member of the Scientific Advisory Board of Citizens United for Curing Epilepsy (CURE): was instrumental in guiding the research direction of the foundation, resulting in many millions of dollars directed towards earlycareer awards (e.g., ‘taking flight’) for pediatric neuroscience. Dr. BrooksKayal embarked on a major set of
transformative contributions to child neurology-relevant research through her efforts with NIH/NINDS: First, she led two benchmark Conferences (2007 and 2013) where she highlighted the importance of Cognitive and Psychological Co-Morbidities of Epilepsy and the serious gap in the study of these problems. Second, she actively participated in the Program Review Panel of the NINDS Antiepileptic Drug Discovery (ADD) Program, that had traditionally ignored neonatal and childhood seizures and epilepsies. Here two Review Panels (2012 and 2015) resulted in major changes in the direction of the program. Dr. Brooks-Kayal is now continuing her national guidance role as member of the External Advisory Board (20152019) of the NINDS Epilepsy Therapy Screening Program (ETSP). Again, she is providing guidance and oversight of implementation of changes in program direction.
The most powerful way to influence policy and emphasize changes at the national / NIH levels is via service on the individual institutions’ Council. This is a rare honor, and members work with Institute Directors and colleagues to influence research priorities. Dr. BrooksKayal is a rare Child Neurologist on the NINDS Council (2014-18). As such, she has advised NINDS Directors and the Institute on policy and procedures affecting the extramural research programs and provides a second level of review for grant and cooperative agreement applications considered by the Institute for funding.
In summary, Dr Brooks-Kayal is an internationally recognized leader in research with strong relevance to child neurology. She is a passionate and gifted educator and mentor at individual, institutional and national levels. Uniquely, she is also contributing to developmental neuroscience research through her vision of enabling the resources mandatory for this research via leadership at societies, foundationsand the NIH. •
Child Neurology Society | Summer 2023 43
2023 Hower Award
Phillip L. Pearl, MD
BY BRUCE COHEN, MD, FAAN

Born in Baltimore, Phillip Pearl has spent his life, aside from a few years of residency training, on the East Coast of the United States. He received his undergraduate degree from Johns Hopkins and medical degree from University of Maryland, completed child neurology residency at Baylor with Ralph Feigin and Marv Fishman, a former CNS President and Hower awardee, and epilepsy fellowship at Boston Children’s with Greg Holmes. He joined the faculty of Children’s National Medical Center and rose to chief of child neurology and Professor of Neurology, Pediatrics, and Music at George Washington University (GWU). He directed medical student education in neurology at GWU and received the faculty Arnold Gold Humanism Award in 2004 and Distinguished Teacher Award in 2005. He was recruited to Boston Children’s to lead the Epilepsy Division following a national search by a committee of very distinguished faculty at Harvard Medical School. Since arriving in Boston, in addition to serving as Director of the Division of Epilepsy and Clinical Neurophysiology, William Lennox Chair and Professor of Neurology at Harvard Medical School, he initiated and directed the Pediatric Leadership Program at Harvard Medical School and has maintained a faculty appointment at the Berklee College of Music. His contributions to the Child Neurology Society are remarkable, including the Awards Committee (chair 2004-2011), co-chair of the Jack Pellock Course in Pediatric Epilepsy (2016 – present), CNS Councilor for the East (2015-2017), and most notably President-elect and President of the Child Neurology Society (2018 – 2021). As president of the CNS from 2019-2021, he
led us through perhaps the most difficult period in the history of our society. The Lifetime Achievement Award was created during his tenure as Chair of the Awards Committee. Throughout his many years in the CNS, he has expressed his deep sense of humanity through music he has played at innumerable events, most recently as co-organizer of the course, “American Creativity, Ingenuity, and Diversity” that accompanied the virtual 2020 CNS meeting combined with ICNA, representing the diversity of American culture in the arts for our international colleagues.
In addition to his contributions to CNS, he has held multiple national leadership positions, including ACGME Neurology RRC member for six years and principal author of the revised training requirements, and President of the Professors and Educators of Child Neurology (2012-2014). As PECN President, he promoted the endowment for the Philip R. Dodge Young Investigator Award and initiated the Blue Bird Circle Outstanding Training Program Director Award. He served as Section Chief of Child Neurology for the American Academy of Neurology (2017-2019) and was previously a board member of the Child Neurology Foundation. He served on the accreditation board of the UCNS and has served on the editorial boards of Annals of Neurology, Neurology, Epilepsia, Music and Medicine, Future Neurology, and Journal of Child Neurology (the latter as Associate Editor). He is an editor on the recent (sixth) edition of Swaiman’s Pediatric Neurology and currently co-senior editor with Steve Ashwal for the upcoming (seventh) edition of the venerable Swaiman test. During his CNS presidency, he had the unenviable task of renewing the debated contract with

44 Child Neurology Society | Summer 2023
CHILD NEUROLOGY SOCIETY 52nd ANNUAL MEETING October 4-7, 2023 • Vancouver, BC 2023 CALLING
Phillip L. Pearl, MD
the ANA for the Annals of Neurology to serve as the society’s official journal. Phil managed to renew the journal contract and add a new societal journal to the “Annals family,” the Annals of the Child Neurology Society, and serves as Senior Associate Editor under Editor-inChief, Steve Roach.
Phil may be best known for his contributions to the understanding of SSADHD (succinic semialdehyde dehydrogenase deficiency). He writes, “SSADHD was not discovered by me, but it’s fair to say it discovered me!” A metabolic disorder first described by Mike Gibson PhD, Phil recounts the story of his seminal patient, with thanks to a resourceful mother, allowed Drs. Gibson and Pearl to team up circa 2000. With Dr. Gibson’s mouse model and Phil’s growing clinical database, Phil was able to describe the clinical, EEG/epilepsy, sleep, metabolic, and other features of the condition. This grew his interest from one disease into a focus on inherited metabolic epilepsies, that culminated in many presentations and ultimately the book, Inherited Metabolic Epilepsies, considered relatively authoritative in the field, and now in its 2nd edition. His SSADHD database has now more than 100 patients as well as continuous NIH funding for research in this condition since 2004, including his current R01.
As much as the field of child neurology is a focus of Phil’s life, music is part of his DNA as well. For years, members of the CNS, AAN, and AES have listened to Phil entertain, along with his band at the social events during annual meetings. In addition, he has taught numerous courses about humanity and the brain as it
relates to music and musicians. Phil’s music career began with playing the drums at age six, inspired by his father, a professional jazz trumpeter and older brother, a trumpet virtuoso at the time. He was more interested, in his words, in “banging on skins and making noise than making sense out of music”. However, by age eleven, his local music teacher, a friend and colleague of his father, told his parents he “couldn’t teach Phil anything else” and recommended that they enroll him at the Peabody Conservatory of Music in the city. By then he was mastering all the percussion instruments, including xylophone, marimba, and vibraphone, and appearing on television as a musically gifted and talented youth. He ultimately enrolled at Johns Hopkins University, which acquired the Peabody and saved it from bankruptcy, and was in the first class of Hopkins students simultaneously enrolled after passing auditions to the Peabody. Phil ultimately played music professionally starting in high school and throughout college until this came to a grinding halt in medical school. In his words, he “needed more time to study and less late nights playing weddings and clubs.” However, he never gave up music as literally a second career, and has performed in the Longwood Symphony Orchestra, had an adjunct appointment as Professor of Music (as well as Neurology and Pediatrics) when at George Washington University School of Medicine, and is currently a member of the Music and Health Institute at the Berklee College of Music in Boston. His first CD, Live at Jazzmatazz, made its debut at the famous Blues Alley Jazz Club in
Georgetown and its proceeds had supported the care of indigent children in the nation’s capital. Putting bands together for the annual CNS meeting, as well as seminars on neurological problems of the musical masters for CNS and ICNA, has been a particularly wonderful aspect of his career.
These accomplishments could not happen without the wonderful support of his wife, Maria Tartaglia Pearl MD, an alumna of Georgetown Medical School and currently a primary care pediatrician at Boston Children’s Hospital. Phil has five grandchildren from his older two children now in their mid-thirties, Melinda and Adam, who lost their mother at ages 11 and 9 years from breast cancer. He and Maria have two daughters, Suzanne, currently a sophomore at Georgetown University, and Natalie, a high school senior.
These remarkable accomplishments bear witness to Phil’s extraordinary ability to get things done with kindness and humility; he is truly a mensch who promotes and celebrates the successes of all and the achievements of others. Phil is simply outstanding in his approach to leadership, he is a consummate gentleman, educator, scientist, musician, and physician. •
Child Neurology Society | Summer 2023 45
Bernard D’Souza International Fellowship Award



Priyanka Madaan, MD Amrita Institute of Medical Sciences and Research Centre, Faridabad, Haryana

Unveiling the 2024 CNS Award Nominations
Nominate now for the Hower, Bernard Sachs, Brumback Lifetime Achievement, Gold Humanism, and Martha Bridge Denckla Awards.
Submitting nominations is smoother than ever with our user-friendly application.
Let's honor the game-changers together! Make

46 Child Neurology Society | Summer 2023
Prem Chand, MBBS, FCPS Aga Khan University, Karachi, Sindh, Pakistan
CALLING
Nominations
Your
Today!
Shape the future of neuroscience today!
Celebrate brillance in child neurology!
2023 Junior Member Awards



Tauen Chang Outstanding Junior Member Award
Tauen Chang Outstanding Junior Member Post Graduate Award




 Alexandra Santana Almansa, MD Boston Children’s Hospital, Boston, MA
Claudia GambrahLyles, MD Children’s Hospital of Philadelphia, PA
Mary Rolfes, MD University of California, San Francisco, San Francisco, CA
Alexandra Santana Almansa, MD Boston Children’s Hospital, Boston, MA
Claudia GambrahLyles, MD Children’s Hospital of Philadelphia, PA
Mary Rolfes, MD University of California, San Francisco, San Francisco, CA
Child Neurology Society | Summer 2023 47
Alexander Sandweiss MD, PhD Baylor College of Medicine, Texas Children’s Hospital, Houston, TX
M. Richard Koenigsberger Scholarship
Hui Li, MD, PhD Department of Neurology, University of Wisconsin Hospitals and Clinics at Madison, WI
AAP Section on Neurology Trainee Travel Award
Miranda Creasey, MD Virginia Commonwealth University, Richmond, VA
Bhuwan Garg High School Student Neuroscience Prize
Rania Sophia Lateef Charles J. Colgan High School, Manassas, VA
Milena Andzelm, MD, PhD Boston Children’s Hospital, Boston, MA
Jenny Harmon, MD, PhD Atrium Health Wake Forest Baptist Medical Center, Winston-Salem, NC
Child Neurology Foundation

Dear Members of the Child Neurology Society
BY ANUP D. PATEL, PRESIDENT, CHILD NEUROLOGY FOUNDATION








I wanted to take a moment to reach out personally and share some heartfelt updates with my fellow CNS colleagues. Throughout my tenure as President of the Child Neurology Foundation (CNF) Board of Directors, I’ve had the pleasure of connecting with our CNS Board President, Dr. Bruce Cohen, on a weekly basis. Over the course of these conversations, we came to the collective realization that many members of CNS may not be familiar with CNF and how we execute our vision and mission to support everyone in the pediatric neurology community. Therefore, I’d like to share about our impact and work with the hope that it will help you as you navigate your career in the child neurology field.
At CNF, we envision a future where children affected by neurologic disorders are not limited by their condition but empowered to thrive. Our mission is rooted in serving as a collaborative center of education, resources, and support for these children, their families, and the child neurology providers who care for them. Together, we form a network of medical professionals, caregivers, patients, and
advocates, all dedicated to enriching lives and making a positive impact.
Grounded in data, CNF regularly surveys families and medical professionals –receiving feedback from 5,000+ caregivers and 60+ patient advocacy organizations since 2018. Leveraging the knowledge we gain through surveys, focus groups, and collaborations, CNF seeks to identify and address gaps in knowledge across the community. Below are some key program areas, as well as some impact highlights:
Child and Family Support
• Our Neurology Social Services Network (NSSN) connects families to over 21,000 local community services and patient advocacy organizations in the neurology space through direct referrals.
• More than 1,500 families have benefited from direct connection with our Social Worker and Peer Support Specialists.
• Contact CNF’s Executive Director, Amy Brin (abrin@childneurologyfoundation. org) to discuss how your clinical practice can refer to these free, credible services.

COMMUNITY
Anup D. Patel President
48 Child Neurology Society | Summer 2023 Link to CNF Website
Child Neurology Foundation
Education
• CNF has provided education to 2,000+ medical professionals, covering essential topics crucial to the wellbeing of children with neurologic conditions.
• CNF’s comprehensive education brings together patient, family, and medical professional perspectives, empowering them with practical knowledge and tools on difficult topics to help deliver the highest quality of care.
• CNF’s education is offered virtual and in-person, and with CME credit.
Research & Care Advancement
• Through more than $5.7 million in funding, CNF has supported the research of child neurologists, young investigators, and medical students.
I invite you to learn more about the Child Neurology Foundation and the inspiring stories of the children, families, and providers we support by visiting our website at www. childneurologyfoundation.org. There, you’ll find a wealth of educational opportunities and resources for both you

and the children and families you care for, as well as opportunities to get involved and help us support more families and providers.
As I approach the end of my tenure as President of the CNF Board, I’m even more committed to supporting the work of CNF and ensuring we’re able to provide these critical programs to our community in alignment with CNS. I hope you will join me and many of our other colleagues to support the work of the Foundation.
With warm regards and heartfelt appreciation. •
Child Neurology Society | Summer 2023 49
Child Neurology Foundation Grants and Scholarships







2023 Pediatric Epilepsy Research Foundation (PERF) Shields Research Grant
Jordan Garris, MD


The Rector and Visitors of the University of Virginia
Mentors
Alberto J. Espay, MD, MSc, FAAN, FANA; Mark Quigg, MD, MSc, FANA, FAES
Research Title
“Tremor Retrainer Software Application for Treatment of Functional Tremor: Pilot Dose-Finding Study”

Bio
Dr. Jordan Garris is an Assistant Professor of Neurology and Pediatrics at the University of Virginia. She graduated with an MD from the Medical University of South Carolina prior to completing Child Neurology Residency and Pediatric Movement Disorders at Cincinnati Children’s Hospital Medical Center. She has clinical interests in pediatric movement disorders and functional neurologic disorders, with a goal to expand accessible treatment options for patients facing poor access to treatment for functional neurologic disorders.
Research Summary
Dr. Garris’s project, funded by the 2023 PERF Shields Grant, is a pilot dose finding study of a smartphone application for treatment of functional tremor, the
most common functional movement disorder. The intervention is based on the premise of “retraining” the tremor through entrainment, a key diagnostic feature of functional tremor in which a new movement performed by the patient at an externally cued frequency causes the tremor to abate or to adapt this new frequency. The Tremor Retrainer application measures a patient’s baseline tremor frequency and provides a new frequency for the patient to match with voluntary movements while receiving continuous visual feedback from the application. The goal is to re-establish self-agency of voluntary movements in a cost-effective, immediately accessible intervention which can be performed in a patient’s home. This initial pilot study will provide essential data to plan a definitive dose-finding study.
Mentors
Nicholas Abend, MD, MSCE; Hao Huang, PhD; Betsy Ostrander, MD
Research Title
“White matter microstructural abnormalities in neonatal seizures due to hypoxic ischemic encephalopathy”
50 Child Neurology Society | Summer 2023
2023 Pediatric Epilepsy Research Foundation (PERF) Elterman Research Grant
Amanda G. Sandoval Karamian University of Utah
Link to CNF Website
Bio
Amanda G. Sandoval Karamian, MD is an Assistant Professor of Pediatric Neurology and Epilepsy at the University of Utah and Primary Children’s Hospital. Dr. Sandoval Karamian’s undergraduate training was at Yale University; she received her medical degree from the Keck School of Medicine of the University of Southern California, completed her Child Neurology residency at the Lucile Packard Children’s Hospital at Stanford University, and her Pediatric Epilepsy Fellowship at the Children’s Hospital of Philadelphia, with a focus on neonatal epilepsy. She is now a pediatric epileptologist at the University of Utah with a clinical and research focus on neonatal EEG and neonatal seizures. Dr. Sandoval Karamian’s research interests include epilepsy genetics, neonatal EEG, white matter abnormalities in seizures and epilepsy, and neonatal HIE, and she hopes to leverage advanced neuroimaging modalities to identify novel biomarkers for post-neonatal epilepsy and neurodevelopmental outcomes after neonatal seizures.
Research Summary
The brain’s white matter develops through normal activity and learning. Studies of animals and humans with epilepsy indicate that white matter is abnormal, indicating that seizures may impair white matter development. However, this process is incompletely understood. White matter is undergoing its most rapid period of development in the neonatal period. If seizures affect white matter, then the impact on normal development, subsequent cognitive function, and the development of epilepsy could be evident in neonates. Neonates with seizures due to hypoxic ischemic encephalopathy, the most common cause of seizures in newborns, provide a unique opportunity to further explore this connection. This study will
use advanced neuroimaging techniques to study white matter structure in neonates with hypoxic ischemic encephalopathy with and without seizures to determine whether seizures in this population are associated with white matter abnormalities.
2023 Neurodevelopmental Disabilities (NDD) Summer Research Scholarship

Erin Hendry Medical Student at University of Rochester
Mentor
Jennifer Vermillion, MD

Research Title
“Anxiety Phenotype and Functional Impact in Youth with Chronic Tic Disorders”
Career Goals Statement
Understanding the brain’s mechanics has been my interest since I was fifteen. Several of my friends in high school suffered life-altering concussions, and their experiences caused me to become interested in learning more about how the brain heals. I followed this curiosity through undergrad, pursuing research projects examining environmental factors on behavior. After college, during my years as a research assistant at Beth
Israel Deaconess Medical Center, I became well acquainted with the impact neurological diseases have on patients. Many of the patients I worked with had anxiety surrounding their neurologic diagnosis. Through this experience, I became very involved in helping patients understand their condition and what they could expect their future quality of life to be. These interactions have made me passionate about improving our understanding of the intersection of neurological conditions such as Tourette’s Syndrome with psychiatric comorbidities like depression and anxiety. As a medical student at the University of Rochester, I have been able to start investigating the relationship between neurological and psychiatric diseases. I plan on continuing similar research throughout my career. In my future practice, I hope to work on an integrated care team specializing in the treatments for children with rare neurological diseases that enhance and improve the care these patients receive.
Mentor
Zachary Grinspan, MD, MS
Child Neurology Society | Summer 2023 51
2023 Swaiman Medical Student Scholarship
Ashwin Mahesh Medical Student at Weill Cornell School of Medicine
Research Title
“Evidence-based Quality Measures for Genetic Testing in Pediatric Epilepsy”








Career Goals Summary
I am an aspiring neurologist passionate about the intersection between social disparities, data science, and clinical practice. I am eager to learn data-centered approaches to uncovering disparity and to directly fuel interventions to serve patients in need.
In my future career as a neurologist, I am determined to make an impact on systemic inequity through clinical practice, research, community intervention development, and policy advocacy. Prior to medical school, I had the privilege of cofounding and directing the expansion of a free medical clinic network in Charlottesville dedicated to serving patients experiencing homelessness. My experiences in Charlottesville have sparked a determination within me to further investigate ways in which Health System interventions can lead to drastic improvements in social disparities and systemic neglect. This work has further informed my current work building a similar medical clinic network in NYC. In my future as a neurologist, I am eager to continue learning methods to uncover disparity and to partner with our patients to build evidence-based systems of support.
I am drawn to neurology for many reasons. Not only am I fascinated by the brain and our nervous system, but the rapid advances in neurological discovery over the last two decades excites me. Many of these discoveries have led to incredible impacts on patient care and have worked to ameliorate pain that many of our patients face each day. As a future neurologist and scientist, I hope to work alongside my colleagues to contribute to discovery in this amazing field and make a real difference for patients experiencing pain.
I am incredibly thankful to the Child Neurology Foundation for the opportunity to partner this summer, to learn from my mentor Dr. Zachary Grinspan, and to work together towards our common goal of improving outcomes for children with neurological conditions.
2023 Swaiman Medical Student Scholarship
Mentor
Temitayo Oyegbile-Chidi, MD, PhD, FAAN

Career Goals Summary
Tracy has had a longstanding passion for providing care to individuals with disabilities, particularly neurodevelopmental disabilities. This passion was sparked from the time of her youth. She grew up with a little brother with autism, epilepsy, and congenital aural atresia. As a consequence, she has developed an interest in child neurology as a career and is working in my research lab this semester. She has been diligent, hardworking, responsible and has been an absolute pleasure to work with. Her problem-solving skills have been remarkable and her bright and thoughtful personality is shone through when working with study participants.
Before enrolling in medical school, Tracy worked as a psychometrist at the UCLA Child and Adult Neurodevelopmental Clinic and Center for Autism Research and Treatment (CART), where she administered cognitive and diagnostic tests and interviews to provide clinical diagnoses to individuals across the life span with the supervision of Clinical Psychologists. She would help identify behaviors that corresponded with specific diagnoses within the DSM-V. In addition, she phenotyped for over 14 research projects at the CART Center and interviewed over 1000 study participants. Her hard work and intelligence led to her advancement
52 Child Neurology Society | Summer 2023
Tracy de los Santos MD/PhD Student at University of California, Davis School of Medicine
Link to CNF Website
to the most senior psychometrist role where she was responsible for overseeing the training of undergraduate volunteers in addition to her other duties. In this senior role, she supported the training of graduate psychology interns in specialized clinical assessments, including the Autism Diagnostic Observation Schedule-II and Autism Diagnostic Interview-II. She also co-led a study that sought to determine how mobile technology could increase access to resources, particularly among mothers of children with autism who are of Latin American descent. The focus groups that were held confirmed how much these parents rely on their provider for guidance on resources, but also brought up concerns of the scarcity of providers available who are conscious or aware of the basics of working with their family members. These experiences along with working with several behavioral neurologists cemented her desire to pursue medicine, and specifically child neurology.
As a UCD medical student, she revived the UCD Student Interest Group in Neurology and served as the co-president. In this role, she led and hosted sessions on research in Neurology, the path to residency, and case studies. In spite of the COVID-19 related restrictions in the clinic setting, she has been able to shadow several pediatric neurologists at UCDH to gain experience of the scope of pediatric neurology. To learn more about the scope of practice and research, particularly within the realm of public health, she completed a literature review under the guidance of Dr. Choe exploring similarities in executive functioning between children with autism spectrum disorder and posttraumatic brain injury. This experience re-invigorated her interest in advocacy; as she began to advocate for providing executive functioning therapy to pediatric TBI patients with limited access to therapy resources/options.
Mariella Filbin MD, PhD
Career Goals Summary

There is no question that the human brain is the most complex and fascinating organ. I entered medical school with a deep fascination for the brain and learning more about it clinically has only reinforced that interest. Unfortunately, neurological diseases remain as some of the most devastating and complex pathologies that affect adults and children alike. As a future physician, I aspire to have a career in which I can help advance our understanding of neurological diseases and make a significant impact in the lives of my patients. I am particularly interested in the field of pediatric neuro-oncology and hope to be involved in efforts to develop new therapies for children affected by brain tumors. I am immensely grateful to the Child Neurology Foundation and Dr. Phyllis Sher for their generous support of my research in pediatric neurological malignancies. •

Child Neurology Society | Summer 2023 53
2023 Swaiman Medical Student Scholarship
Ernesto Luna Melendez Medical Student at Rush Medical College, Rush University Mentor




CHILD NEUROLOGY SOCIETY 53rd ANNUAL MEETING Nov. 11-14, 2024 • San Diego, CA 2025 CHILD NEUROLOGY SOCIETY 54th ANNUAL MEETING October 8-11, 2025 • Charlotte, NC 2026 CHILD NEUROLOGY SOCIETY 55th ANNUAL MEETING October 14-17, 2026 • Montreal, QC CHILD NEUROLOGY SOCIETY 52nd ANNUAL MEETING October 4-7, 2023 • Vancouver, BC 2023 We look forward to seeing you...
You Calendar for Future Meetings
Mark










































































































 BY DANIEL J. BONTHIUS, MD, PHD, CNS CONNECTIONS EDITOR
BY DANIEL J. BONTHIUS, MD, PHD, CNS CONNECTIONS EDITOR



 BY DANIEL J. BONTHIUS, MD, PHD, CNS CONNECTIONS EDITOR
BY DANIEL J. BONTHIUS, MD, PHD, CNS CONNECTIONS EDITOR
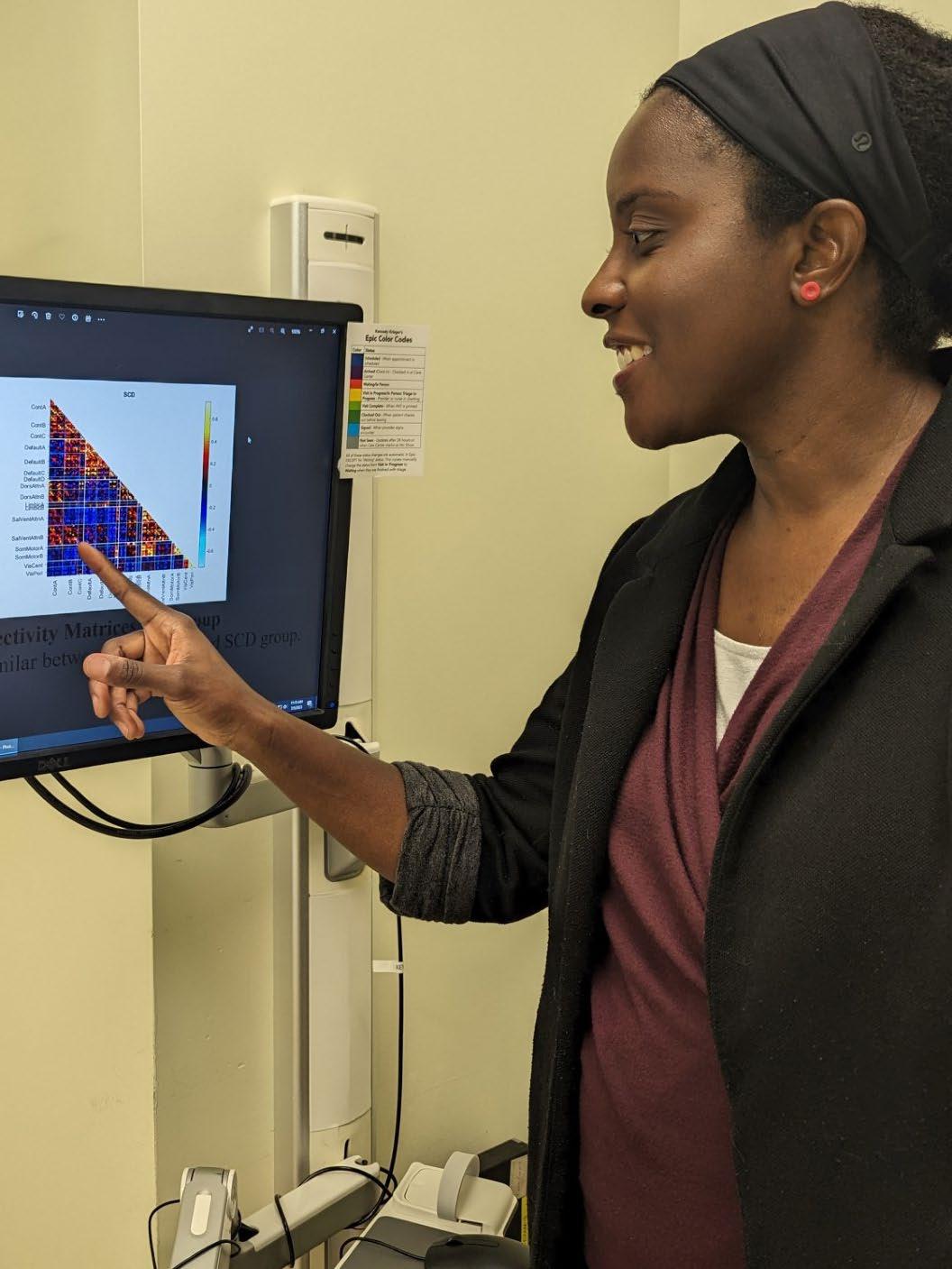



 BY YASMIN KHAKOO, MD, FAAN, FAAP
BY YASMIN KHAKOO, MD, FAAN, FAAP










 Sonika Agarwal
Shawn Aylward
Clarimar Borrero-Mejias
J. Nicholas Brenton
Audrey Christine Brumback
Meeryo Christa Choe
Bruce H. Cohen
Louis Dang
Jay Desai
Matt Elrick
Timothy Robin Gershon
Sonika Agarwal
Shawn Aylward
Clarimar Borrero-Mejias
J. Nicholas Brenton
Audrey Christine Brumback
Meeryo Christa Choe
Bruce H. Cohen
Louis Dang
Jay Desai
Matt Elrick
Timothy Robin Gershon











 Wilfreda Lindsey
Ariel Lyons-Warren
Kiran Prasad Maski
Melanie McNally
Xilma Ortiz-Gonzalez
Scott Otallah
Temitayo Oyefunmike Oyegbile Chidi
Rachit Patil
E. Steve Roach
Jonathan Douglas Santoro
Renee A Shellhaas
Wilfreda Lindsey
Ariel Lyons-Warren
Kiran Prasad Maski
Melanie McNally
Xilma Ortiz-Gonzalez
Scott Otallah
Temitayo Oyefunmike Oyegbile Chidi
Rachit Patil
E. Steve Roach
Jonathan Douglas Santoro
Renee A Shellhaas



 Amy Robichaux Viehoever
Amy Robichaux Viehoever













 Yasmin Khakoo, MD, FAAN, FAAP
BY ALISON CHRISTY, MD, PHD
Yasmin Khakoo, MD, FAAN, FAAP
BY ALISON CHRISTY, MD, PHD
 BY HARVEY BENNETT, MD; YASMIN KHAKOO, MD, FAAN, FAAP; RAJESHWARI MAHALINGAM, MD; AND SAKKUBAI NAIDU, MD
BY HARVEY BENNETT, MD; YASMIN KHAKOO, MD, FAAN, FAAP; RAJESHWARI MAHALINGAM, MD; AND SAKKUBAI NAIDU, MD




 BY TALLIE BARAM, MD, PHD; JONATHAN MINK, MD, PHD; AND BRENDA PORTER, MD, PHD
BY TALLIE BARAM, MD, PHD; JONATHAN MINK, MD, PHD; AND BRENDA PORTER, MD, PHD













 Alexandra Santana Almansa, MD Boston Children’s Hospital, Boston, MA
Claudia GambrahLyles, MD Children’s Hospital of Philadelphia, PA
Mary Rolfes, MD University of California, San Francisco, San Francisco, CA
Alexandra Santana Almansa, MD Boston Children’s Hospital, Boston, MA
Claudia GambrahLyles, MD Children’s Hospital of Philadelphia, PA
Mary Rolfes, MD University of California, San Francisco, San Francisco, CA












