

Medical Assistant Training Manual

Overview
Welcome to River Region Dermatology & Laser. We are honored to have you join our dynamic team.
This manual is meant to serve as a comprehensive guide for medical assistants working at River Region Dermatology and Laser. It covers various aspects of dermatology, including anatomy and physiology, common skin conditions, diagnostic techniques and procedures, treatment options and therapies, medication administration, wound care and management, surgical procedures, skin cancer detection and prevention, office protocols, and communication strategies.
Please be advised that this is just a general outline and may vary depending on the specific needs of our providers, workplace and organization.
Introduction to Dermatology
As a medical assistant at River Region Dermatology & Laser, you will be working closely with Dr. Porcia Love and other healthcare professionals to provide high-quality patient care. In this section, we will introduce you to the basics of dermatology, the role of a dermatology medical assistant, and the importance of proper patient communication and confidentiality. Dermatology is a branch of medicine that deals with the diagnosis, treatment, and prevention of disorders and diseases of the skin, hair, nails, and mucous membranes. Dermatologists are medical doctors who specialize in the diagnosis and treatment of skin-related disorders, including skin cancers, acne, eczema, psoriasis, and other conditions.
The skin is the largest organ in the body and performs several important functions:
1. Barrier function: The skin acts as a barrier against external factors such as bacteria, viruses, and other pathogens.
2. Regulation of body temperature: The skin helps to regulate body temperature by releasing heat through sweating.
3. Waste removal: The skin helps to remove waste products from the body through sweat and excretion.
4. Sensation: The skin contains sensory receptors that allow us to feel sensations such as touch, pressure, pain, and temperature.
The skin is composed of several layers:
1. Epidermis: The outermost layer of the skin that contains melanin-producing cells (melanocytes) responsible for pigmentation.
2. Dermis: The middle layer of the skin that contains blood vessels, nerve endings, and hair follicles.
3. Hypodermis: The innermost layer of the skin that connects to underlying tissues.

Job Function:
Your role as a medical assistant will involve supporting the dermatologist and other healthcare professionals in diagnosing and treating skin-related disorders. Your duties may include:
▪ Preparing patients for exams and procedures
▪ Taking vital signs and recording patient information
▪ Assisting with minor procedures such as biopsies and injections
▪ Preparing medications and treatments for application
▪ Maintaining accurate records and documentation
▪ Providing patient education on skincare and treatments
Effective communication is essential in dermatology as patients often have concerns about their appearance and may be anxious about their condition. As a medical assistant, you will need to:
1. Listen actively: Pay attention to patients' concerns and ask questions to clarify their needs.
2. Communicate clearly: Explain procedures, treatments, and instructions clearly and concisely.
3. Empathize: Show understanding and empathy towards patients' emotions and concerns.
4. Maintain confidentiality: Respect patients' privacy by maintaining confidentiality about their personal information.
Confidentiality is crucial in dermatology as patients may have sensitive information about their personal lives or medical conditions. As a medical assistant, you must:
1. Respect patient privacy: Always keep patient information confidential
2. Maintain accurate records: Ensure that patient records are accurate, complete, and up to date
3. Protect patient information: Follow hospital policies and procedures for handling sensitive information.
Patient Communication and Confidentiality
Effective communication is a critical component of patient care, as it plays a significant role in building trust, ensuring patient satisfaction, and promoting better health outcomes. As a healthcare professional, it is essential to possess effective communication skills to interact with patients, their families, and other healthcare providers. This section will discuss the importance of effective communication techniques, active listening, empathy, confidentiality guidelines, and HIPAA (Health Insurance Portability and Accountability) regulations.
Effective communication involves more than just speaking; it involves understanding the patient's needs, concerns, and emotions. To achieve effective communication, consider the following techniques:
1. Active Listening: Pay attention to the patient's words, tone, and body language. Maintain eye contact, nod to show understanding, and ask clarifying questions to ensure you understand their concerns.
2. Clear and Concise Language: Use simple language to convey information. Avoid using jargon or technical terms that may confuse patients.
3. Empathy: Show understanding and compassion by acknowledging the patient's feelings and emotions.
4. Nonverbal Cues: Use nonverbal cues such as smiling, maintaining eye contact, and open body language to create a welcoming atmosphere.
5. Open-Ended Questions: Ask open-ended questions that encourage patients to share their thoughts and feelings.
Active listening and empathy are essential components of effective communication. By actively listening to patients, you demonstrate that you value their concerns and are committed to understanding their needs. Empathy helps build trust and fosters a positive patient-provider relationship.
▪ Active Listening: Helps patients feel heard and understood, reducing anxiety and increasing satisfaction.
▪ Empathy: Fosters trust and promotes a positive patient-provider relationship.
Maintaining confidentiality is crucial in healthcare settings. Confidentiality refers to the duty to protect sensitive patient information from unauthorized disclosure. The Health Insurance Portability and Accountability Act (HIPAA) regulates the use and disclosure of protected health information (PHI).
HIPAA requires healthcare providers to:
1. Maintain confidentiality: Protect PHI from unauthorized disclosure.
2. Use appropriate safeguards: Implement policies and procedures to ensure confidentiality.
3. Dispose of PHI properly: Securely dispose of PHI when no longer needed.
Handling Sensitive or Difficult Patient Situations:
Dealing with sensitive or difficult patient situations requires skill, empathy, and professionalism. Consider the following strategies:
1. Remain Calm: Stay composed and professional when faced with challenging situations.
2. Listen Actively: Listen attentively to the patient's concerns and feelings.
3. Empathize: Acknowledge the patient's emotions and show understanding.
4. Focus on Solutions: Work with the patient to find solutions or compromises.
5. Seek Support: Don't hesitate to seek support from colleagues or supervisors when needed.
In conclusion, effective communication is a critical component of patient care. By utilizing effective communication techniques, active listening, empathy, confidentiality guidelines, and HIPAA regulations, you can build trust with patients, promote better health outcomes, and maintain a positive reputation as a healthcare professional.
Common Dermatological Conditions and Diseases
It is essential to be familiar with the most common skin conditions and diseases that affect patients. This section will provide an overview of these conditions, their signs and symptoms, and treatment options.
Acne:
Definition: A chronic inflammatory skin condition characterized by comedones (blackheads and whiteheads), papules, pustules, nodules, and cysts.



Signs and Symptoms:
▪ Comedones: blackheads and whiteheads
▪ Papules and pustules: red bumps on the skin
▪ Nodules: larger, painful bumps on the skin
▪ Cysts: deep, painful bumps that can cause scarring
Treatment Options:
▪ Topical retinoids and antibiotics
▪ Oral antibiotics
▪ Hormonal treatments
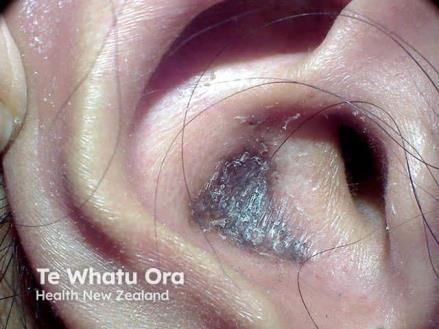
Seborrheic Dermatitis:
Definition: A chronic inflammatory skin condition characterized by flaky, red patches on the scalp, face, and other oily areas.






Signs and Symptoms:
▪ Flaky, red patches on the scalp
▪ Flaking, scaling on the face
▪ Redness and itching in the affected areas
Treatment Options:
▪ Antifungal shampoos
▪ Topical corticosteroids
▪ Ketoconazole cream or shampoo for scalp treatment
Eczema (Atopic Dermatitis):
Definition: A chronic inflammatory skin condition characterized by dry, itchy, and scaly skin.







Signs and Symptoms:
▪ Dry, scaly skin
▪ Redness and itching
▪ Small bumps or blisters on the skin
Treatment Options:
▪ Moisturizers
▪ Topical corticosteroids
▪ Topical immunomodulators
▪ Oral antihistamines
BIOLOGIC THERAPIES
Psoriasis:
Definition: A chronic autoimmune condition characterized by red, scaly patches on the skin.



Signs and Symptoms:
▪ Red, scaly patches on the skin
▪ Silvery scales on the affected areas
▪ Redness and itching
Treatment Options:
▪ Topical corticosteroids
▪ Topical vitamin D analogs
▪ Phototherapy
▪ Oral medications
Vitiligo:
Definition: A chronic autoimmune condition characterized by loss of pigment-producing cells in the skin.








Signs and Symptoms:
▪ White patches on the skin
▪ Loss of pigment in hair, eyes, or mucous membranes
Treatment Options:
▪ Topical corticosteroids
▪ Topical immunomodulators
▪ Phototherapy
Discoid Lupus:
Definition: An autoimmune condition characterized by inflammation of the skin.



Signs and Symptoms:
▪ Red lesions on the face, ears, and scalp
▪ Scars from previous lesions
Treatment Options:
▪ Topical corticosteroids
▪ Oral antimalarials

Telogen Effluvium:
Definition: A condition characterized by excessive hair shedding due to hormonal changes.



Signs and Symptoms:
▪ Excessive hair shedding
▪ Thinning or loss of hair
Treatment Options:
▪ Minoxidil topical solution or foam
▪ Low-level laser therapy
Alopecia:
Definition: A condition characterized by hair loss due to various factors.



Signs and Symptoms:
▪ Hair loss on the scalp or body
Treatment Options:
▪ Minoxidil topical solution or foam
▪ Oral hormonal therapy
▪ Low-level laser therapy
Central Centrifugal Cicatricial Alopecia:
Definition: A condition characterized by hair loss due to inflammation and scarring.


Signs and Symptoms:
▪ Hair loss on the scalp or body
Treatment Options:
▪ Corticosteroid injections or creams
▪ Oral hormone therapy
Skin Cancers:
▪ Melanoma: The most aggressive type of skin cancer.
▪ Basal Cell Carcinoma: The most common type of skin cancer.
▪ Squamous Cell Carcinoma: A type of skin cancer that can be aggressive if left untreated.
▪ Cutaneous T-cell lymphoma: A rare type of lymphoma that affects the skin.



Treatment options for skin cancers include:
1. Excisional surgery to remove the tumor.
2. Mohs surgery to remove the tumor while preserving as much surrounding tissue as possible.
3. Radiation therapy to destroy cancer cells.
4. Chemotherapy to destroy cancer cells.
5. Targeted therapy to target specific genetic mutations in cancer cells.
In conclusion, this section has covered common dermatological conditions and diseases that affect patients. It is essential for those who are working in dermatology to understand these conditions, their signs and symptoms, and treatment options to provide effective care for patients.
Skin Examination Terms and Techniques
A thorough skin examination is a crucial step in diagnosing and managing various skin conditions. Dermatologists use specific techniques and terminology to describe the skin lesions, rashes, and moles they encounter. In this section, we will explore the Fitzgerald Phototype Chart, techniques for inspecting skin lesions, and common findings during a skin check.
The Fitzpatrick skin type (or phototype) depends on the amount of melanin pigment in the skin. This is determined by constitutional color. It is as followed:
1. Type I: Pale white skin
2. Type II: Fair skin, blue eyes
3. Type III: Darker white skin
4. Type IV: Light brown skin
5. Type V: Brown skin
6. Type VI: Dark brown or black skin
Here are some common terms used to describe skin lesions, rashes, moles, and other skin findings:
▪ Macule: A flat lesion that is usually less than 1 cm in diameter.
▪ Papule: A small bump or elevation on the skin.
▪ Plaque: A flat-topped elevation on the skin that is usually greater than 1 cm in diameter.
o Nodule: A solid or cystic lesion that is usually greater than 1 cm in diameter.
o Vesicle: A small blister or fluid-filled sac on the skin.
o Pustule: A small pus-filled blister on the skin.
o Crusting: The formation of a crust or scab over a wound or lesion.
o Scaling: The shedding of dead skin cells or flakes from the surface of the skin.
During a routine skin check, dermatologists often encounter various benign and malignant lesions. Some common findings include:
▪ Lentigines: Small, flat brown spots on the skin caused by sun exposure.




▪ Benign appearing nevi (moles): Small growths on the skin that are typically benign but may require removal due to cosmetic concerns.

▪ Seborrheic keratoses (SK): Benign growths that appear as small, brown, or black spots on the skin.



▪ Actinic keratoses (AK): Precancerous lesions that appear as small, rough patches on sun-exposed areas of the skin.



▪ Angiomas: Benign growths caused by abnormal blood vessel formation.



▪ Cherry angiomas: Small, bright red spots on the skin caused by abnormal blood vessel formation.




Accurate documentation and recording of findings during a skin examination are crucial for several reasons:
1. Tracking changes over time: Documenting findings allows dermatologists to track changes in lesions or rashes over time, which can help diagnose and monitor disease progression.
2. Comparison with previous examinations: Comparing current findings with previous examinations helps dermatologists detect any changes or new developments that may indicate underlying disease.
3. Communication with other healthcare providers: Accurate documentation ensures effective communication with other healthcare providers involved in patient care.
4. Informed decision-making: Documented findings enable dermatologists to make informed decisions about treatment options and patient management.
In conclusion, a thorough understanding of skin examination techniques and terminology is essential for accurate diagnosis and management of various skin conditions. By using the Fitzgerald Skin Type Chart, inspecting lesions and rashes using specific techniques, and documenting findings accurately, dermatologists can provide high-quality patient care.
Biopsy Techniques in Dermatology
A biopsy is a medical procedure in which a small sample of skin tissue is removed and examined to diagnose and manage skin conditions. There are several types of biopsies used in dermatology, including:
1 Punch biopsy: A punch biopsy involves using a specialized tool to remove a cylindrical piece of skin, usually 2-4 mm in diameter, from the affected area. This type of biopsy is often used to diagnose conditions such as melanoma, basal cell carcinoma, and squamous cell carcinoma.
2. Shave biopsy: A shave biopsy involves using a razor-like instrument to remove the top layers of skin, usually 1-2 mm deep. This type of biopsy is often used to diagnose conditions such as acne, psoriasis, and eczema.
3. Excisional biopsy: An excisional biopsy involves removing the entire abnormal growth or lesion, usually under local anesthesia. This type of biopsy is often used to diagnose and treat conditions such as skin cancer.
4. Punch excision: A punch excision is a combination of a punch biopsy and an excisional biopsy. It involves removing a cylindrical piece of skin, usually 6-8mm in diameter, and then removing the entire abnormal growth or lesion.
Indications for Biopsy:
Biopsies may be indicated for a variety of skin conditions, including:
▪ Skin cancer
▪ Suspected skin infections or inflammation
▪ Abnormal moles or growths
▪ Chronic skin conditions such as psoriasis or eczema
▪ Skin lesions that do not respond to treatment
Preparation for Biopsy:
Before undergoing a biopsy, patients should:
▪ Avoid shaving or waxing the area to be biopsied
▪ Inform their doctor if they have any allergies or sensitivities
▪ Stop taking certain medications that may affect bleeding or healing
▪ Arrive at the appointment with a clean and dry area
Post-Biopsy Care:
After a biopsy, patients should:
▪ Keep the biopsy site clean and dry
▪ Avoid soaking the area in water (e.g., bathing, swimming) for 24-48 hours
▪ Apply antibiotic ointment and cover the area with a bandage
▪ Monitor for signs of infection, such as redness, swelling, or increased pain
Complications of Biopsy:
Complications of biopsy are rare but can include:
▪ Bleeding or hematoma
▪ Infection
▪ Scarring or keloid formation
▪ Delayed healing
It's essential to follow post-biopsy instructions carefully to minimize the risk of complications and ensure proper healing
Treatment Options and Medications
Dr. Love uses a variety of treatment options and medications to manage and treat various skin conditions. These can be categorized into three main groups: topical treatments, systemic treatments, and light-based treatments.
Topical Treatments:
Topical treatments are applied directly to the skin and can be used to treat a range of conditions, including:
▪ Creams: Thick, moisturizing creams that can help to hydrate and soothe the skin.
▪ Ointments: Thicker, more emollient products that can help to lock in moisture and protect the skin.
▪ Lotions: Lighter, more watery products that can help to hydrate and soften the skin.
Examples of topical treatments include:
▪ Topical steroids for itching and inflammation
▪ Retinoids for acne and skin texture
▪ Salicylic acid for acne and exfoliation
Systemic Treatments:
Systemic treatments are taken orally or injected into the body and can be used to treat a range of conditions, including:
▪ Oral medications: Pills or capsules that are taken by mouth, such as antihistamines for itching or antibiotics for bacterial infections.
▪ Injectables: Medications that are injected directly into the skin or underlying tissues, such as biologic therapy.
Examples of systemic treatments include:
▪ Isotretinoin for acne
▪ Methotrexate for psoriasis
▪ Corticosteroids for autoimmune disorders
▪ Biologics for psoriasis and other autoimmune conditions
Cryotherapy (Liquid Nitrogen): Cryotherapy involves using liquid nitrogen to freeze and destroy abnormal skin cells. It may require multiple sessions to achieve the desired results. This can be used to treat a range of conditions, including:
▪ Warts
▪ Moles
▪ Skin tags
▪ Cysts
Preventative Skin Care and Education
Preventive skin care is an essential part of maintaining healthy skin and reducing the risk of skin-related problems. As a dermatologist, it is crucial to educate patients on the importance of sun protection, skin cancer prevention strategies, and healthy lifestyle habits.
Importance of Sun Protection:
Sun exposure is a significant risk factor for skin cancer and premature aging. Therefore, it is essential to educate patients on the importance of sun protection. The American Academy of
Dermatology recommends the following sun protection measures:
▪ Use a broad-spectrum sunscreen with an SPF of 30 or higher
▪ Apply sunscreen 15-30 minutes before going outside
▪ Reapply sunscreen every 2 hours or immediately after swimming or sweating
▪ Wear protective clothing, including hats with a 3-inch brim, long-sleeved shirts, and pants
▪ Seek shade, especially during peak sun hours (10am-4pm)
▪ Avoid tanning beds and artificial sources of UV radiation
Skin Cancer Prevention Strategies:
Skin cancer is one of the most common types of cancer, and early detection is crucial for effective treatment. The following skin cancer prevention strategies should be emphasized:
▪ Regular self-examination: Encourage patients to perform regular self-examinations to detect any changes in their skin.
▪ Skin checks: Schedule regular skin checks with a dermatologist to detect any suspicious lesions or moles.
▪ Avoid tanning beds: Tanning beds emit UV radiation, which can increase the risk of skin cancer.
▪ Wear protective clothing: Wear protective clothing, including hats, long-sleeved shirts, and pants, when spending time outdoors.
Healthy Lifestyle Habits:
Healthy lifestyle habits can play a significant role in maintaining healthy skin. The following habits should be encouraged:
▪ Nutrition: A balanced diet rich in fruits, vegetables, and whole grains can help maintain healthy skin.
▪ Hydration: Drink plenty of water to keep the skin hydrated and plump.
▪ Exercise: Regular exercise can improve circulation and overall health.
▪ Stress management: High stress levels can exacerbate skin conditions such as acne and rosacea. Encourage patients to practice stress-reducing techniques such as meditation yoga.
Additional Tips for Patients:
In addition to the above recommendations, provide patients with the following tips:
▪ Be gentle with your skin: Avoid using harsh exfoliants or products that can strip the skin of its natural oils.
▪ Use gentle cleansers: Choose cleansers that are gentle and fragrance-free.
▪ Moisturize regularly: Use a moisturizer that suits your skin type to keep the skin hydrated and supple.
▪ Avoid smoking: Smoking can damage the skin and increase the risk of wrinkles and age spots.
By emphasizing the importance of sun protection, skin cancer prevention strategies, and healthy lifestyle habits, patients can take proactive steps to maintain healthy skin and reduce their risk of skin-related problems.
Administrative Tasks for Medical Assistant
As a medical assistant, administrative tasks are an essential part of your role. This section will cover the importance of managing patient flow, maintaining accurate medical records and charts, and responding to patients via phone and other communication channels.
Managing Patient Flow:
Effective patient flow management is crucial in ensuring that patients receive timely and efficient care. As a medical assistant, you play a critical role in managing patient flow by:
1. Coordinating Patient Flow: Coordinate with healthcare providers and other staff members to ensure that patients are seen in the correct order and that there are no delays or bottlenecks.
2. Maintaining a Smooth Transition: Ensure a smooth transition from one stage of care to another by communicating with patients and healthcare providers.
Maintaining Accurate Medical Records and Charts:
Accurate and complete medical records are essential for providing quality patient care. As a medical assistant, you are responsible for:
1. Maintaining Accurate Patient Information: Ensure that patient information is accurate, up-to-date, and complete.
2. Completing Medical Charts: Complete medical charts in a timely and accurate manner.
3. Updating Medical Records: Update medical records as necessary to reflect changes in patient information or treatment plans.
Responding to Patients via Phone and Other Communication Channels:
Effective communication is critical in providing excellent patient care. As a medical assistant, you should be prepared to respond to patients via phone, email, or other communication channels by:
1. Answering Phone Calls: Answer phone calls promptly and professionally.
2. Returning Phone Calls: Return phone calls in a timely manner to address patient concerns or questions.
3. Communicating with Patients: Communicate with patients clearly and effectively via phone, email, or other communication channels.
Documentation:
If it is not documented, it did not happen
▪ Accurately documenting all patient interactions, including phone calls, visits, and test results
▪ Maintaining a record of all medications administered, including dosages and instructions.
▪ Documenting patient education and instructions provided
▪ Ensuring that all documentation is complete, legible, and up to date
▪ Participating in quality assurance activities to ensure accuracy of documentation
By mastering these administrative tasks, you can provide excellent support to healthcare providers and contribute to the success of your medical practice.
Preparation for Patient’s Encounter
Pre-Care Preparation (Before the Patient Arrives):
1. Review the patient's medical history:
▪ Check the patient's chart to review their medical history, including any previous diagnoses, treatments, and medications.
▪ Document any relevant allergies, sensitivities, or conditions that may impact their care.
2. Prepare the exam room:
▪ Ensure the exam room is clean and organized.
▪ Remove any unnecessary items from the room to create a comfortable and private space for the patient.
▪ Restock supplies
3. Familiarize yourself with the patient's chart:
▪ Review the patient's chart to understand their reason for visit, medications, and any previous treatments or procedures.
▪ Note any relevant test results or lab work that may impact their care.
During Care Preparation (During the Patient Visit):
1. Call the patient to the back by his/her last name.
▪ Verify that you have the correct patient by having them confirm patient identifiers. The full name and date of birth are the most common to ask.
2. Greet the patient and introduce yourself:
▪ Welcome the patient and introduce yourself by name and title (e.g., "Hello, my name is [Your Name], the medical assistant, what brings you in today?”)
▪ Review the patient's medical history and current symptoms:
▪ Take notes on any relevant information that may impact their care.
▪ If the patient is new, find out what brings them in.
▪ If the patient is returning, get the status of their condition, and ensure that they are following prescription and treatment regimens as directed.
▪ Update medications, allergies, surgeries, and pharmacies.
▪ Take pictures of the areas of concern
Post-Care Preparation (After the Patient Visit):
1. Document the visit:
▪ Accurately document all findings, diagnoses, treatment plans, and instructions given to the patient.
▪ Update the patient's chart with any new information or changes to their care plan.
2. Provide instructions and education:
▪ Reiterate instructions on follow-up appointments, medication schedules, and selfcare instructions.
▪ Educate the patient on any new treatments or procedures performed during the visit.
▪ Answer any questions that the patient may have.
3. Clean and disinfect equipment:
▪ Clean and disinfect all equipment used during the visit to maintain infection control protocols.
By following these steps, you can help ensure a smooth and efficient dermatology encounter for both you and your patients!
Addendum
DOCUMENTATION CHECKLIST
Please complete all tasks below for each patient.
Clipboard updated (PMH, Skin disease history, Meds, Allergies, Social history, Family history)
Photo taken
Pharmacy added to chart
Prescriptions added to chart
Provider and active selected
Type of visit selected (New, Consult, Established)
HPI completed (history coherent, overrides selected)
Referring provider included in HPI
Review of systems
Exam completed (always detailed with appearance, etc.)Pdg
Impressions (all have morphology, counseling
Biopsies (morphology, differential diagnosis, site, size of lesion)
Follow up completed
Demographics scanned and attached to chart
BIOPSY
Consent signed
Photo taken of each site and labeled with location
Biopsy tray set up for Provider
Bottles labeled with patient name, date and location
Post biopsy, enclose specimen in bottle before closing the lid
Select size of lesion, morphology, ddx and Vaseline
cc lidocaine
Document how many sutures placed and size of punch
Remove instruments prior to leaving the room
Log path on sheet at Nurse’s Station
EXCISION CHECKLIST
Please complete all tasks below for each patient.
Consent
Vitals
Site
Morphology
Anesthesia (type & cc)
Pre-Op size
Post-Op size
Margins
Procedure (elliptical)
Suture type
Repair type
Destination
Number of deep sutures
o Epidermal sutures (running/interrupted)
o # of deep sutures
Post-care instructions provided to patient
Follow up completed
Demographics scanned and attached to chart
PROCEDURE ROOM CHECKLIST
Cavi Wipes Drysol
Hibiclens
Cotton Tipped Applicators
Hyfrecator Tips (sharp and blunt)
#15 Blades (stainless steel)
2x2 Gauze Lancets
4x4 Gauze
Gloves (Small & Medium)
Blood Pressure Cuff
Sterile Water
Monsel’s solution *check date
Kenalog (10 &40) *check date
Nonsterile Hyfrecator Sheaths
Procedure Packs
Bottom Cabinets Surgifoam
Extra Hibiclens Acetone
Gowns
Sheets
Hydrogen Peroxide
Isopropyl Alcohol
Pillowcase Wound wash
Vest Timer
Specimen Jars Razors
Procedure Packs
Sterile Cotton Tipped Applicators
Sterile 4x4
Sterile 2x2
Penrose Drains
Bandages: spots, ovals, strips (opened and unopened)
Alcohol Pads Telfa (adhesive and Nonadhesive)
Needles:
30G 1in
30G ½ in
31G ½ in
27G 1 ¼ in
20G 1 in
Sterile gloves (6 ½)
#15 blades (carbon steel) Dermablades
NaCl Mirrors
Lidocaine Polysheets
Syringes: 1cc, 3cc, Botox, insulin Culturettes
Prefilled lidocaine syringes Paper Tape 1in & ½ in
Small Surgical Pens Masks
Large Surgical Pens
Vaseline
Mupirocin
Hypafix
EXAM ROOM SUPPLIES
Cavi Wipes Sheets
2x2 Gauze Gowns
4x4 Gauze Pillowcases
Cotton Tipped Applicators Table Paper
Tongue Depressors Mirror
Note Pads (Clear)
Spots, Oval and Strips
Premade Procedure Kits
Specimen Containers
Vaseline Polysheets
Alcohol Pads
Lancets
Skin Markers
Steri Strips (1/2 in and ¼ inch)
Dermablades Benzoin
#15 Blades (Stainless Steel) Non-Stick Telfa
Needles: 20G 1 in
27G 11/4 in
30G 1 in
30G 1 ½ in Adhesive
Prefilled Lidocaine Syringes Masks
Syringes: 1cc, 3cc syringes,
TB/Insulin Syringes
Paper Tape 1 in and ½ in
Punch Box: 2mm, 3mm, 4 mm, 6mm 8mm
Paper Towels- C-Fold
Kenalog 10 & 40 * check dates Sharps Containers
Monsel’s Solution * check dates Tissues
Drysol Solution Paper Towels
Hyfercator Sheaths Lidocaine Vials * check dates
Hyfercator Tips Culturettes Vests
Air Freshener
Copy Paper
OFFICE SUPPLIES
Lysol Wipes
Message Pads
Cups Pens
Dish Soap Plates
File Cabinet
Post It Notes
File Folder Red Trash Bags
Hand Sanitizer Staples
Hand Soap Tape
Highlighters Trash Bags
