Mental Health Matters — Every Single Day
Breaking the Stigma in Ghana
By Mabelle Prior
Journalist and Author
Abstract
Mental health is one of the most neglected areas of healthcare worldwide, particularly in low- and middle-income countries. In Ghana, despite the passage of the Mental Health Act (2012), stigma, underfunding, and a shortage of mental health professionals continue to undermine care. This research-based feature investigates the hidden struggles of individuals living with mental illness in Ghana, highlights systemic challenges, and provides recommendations for change. Drawing on case studies, international comparisons, and authoritative data from the World Health Organization (WHO), Human Rights Watch, and Ghana Health Service, this report emphasizes that mental illness is not a curse but a treatable health condition.
1. Introduction
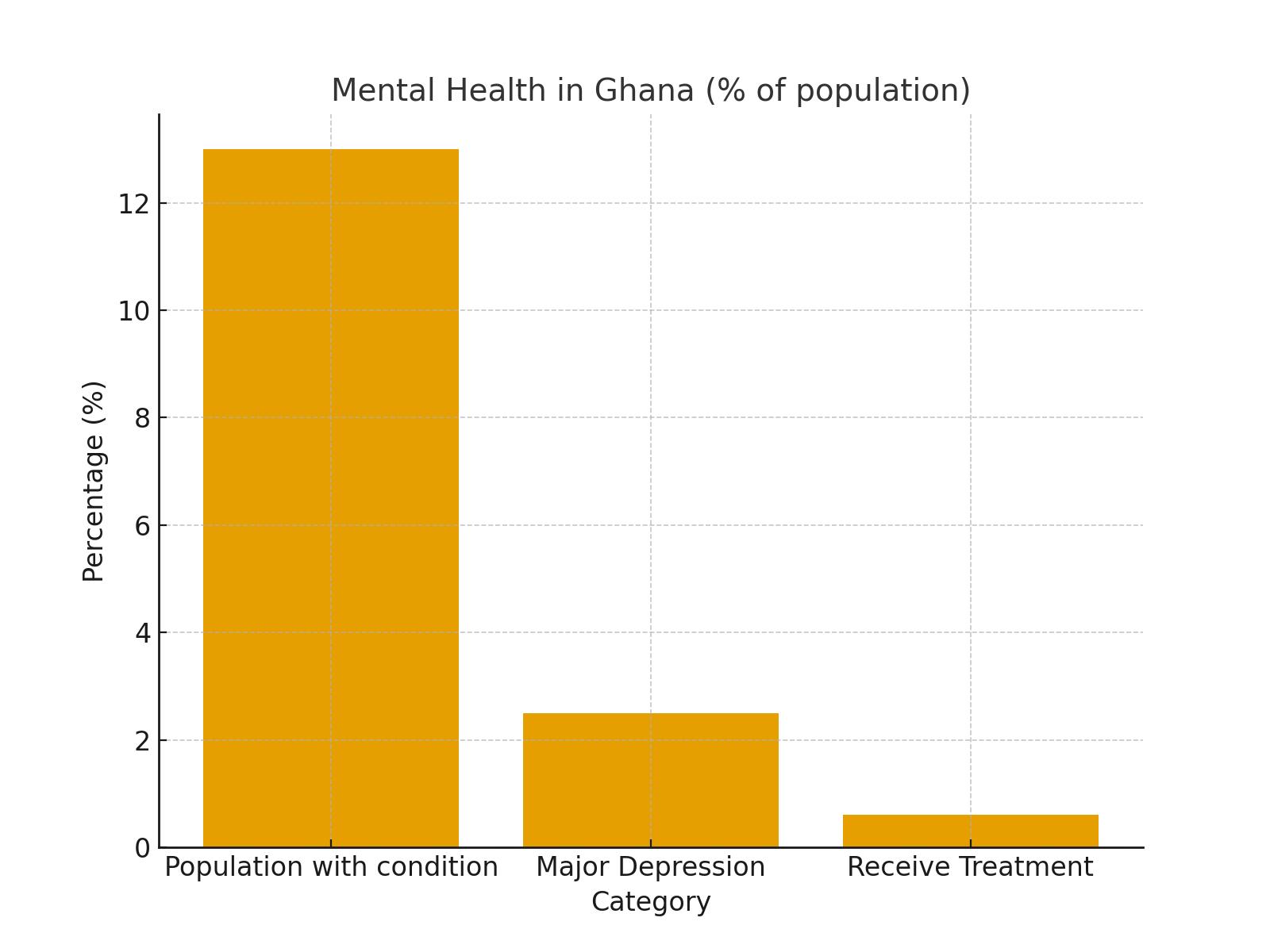
Every day, people across the world endure silent battles with depression, anxiety, bipolar disorder, schizophrenia, and other mental health conditions. These illnesses are medical in nature, but they are often misunderstood, misdiagnosed, or ignored. The consequences of neglect are severe, leading to worsened symptoms, social exclusion, and in extreme cases, loss of life. In Ghana, cultural perceptions surrounding mental health are deeply entrenched. Many people still believe mental illness is caused by spiritual attacks, curses, or witchcraft. Such beliefs not only create fear but also lead to stigma, discrimination, and mistreatment. Instead of seeking medical intervention, many families turn to prayer camps, traditional healers, or confinement, practices which too often result in human rights violations. Globally, mental health is recognized as an urgent health priority. The World Health Organization (WHO) estimates that 1 in 8 people worldwide live with a mental health condition. In Ghana, the prevalence is significant: about 13% of the population experiences some form of mental disorder, with 2.5% suffering major depression. Despite this burden, the country’s support systems remain fragile, underfunded, and overstretched.
2. Literature Review
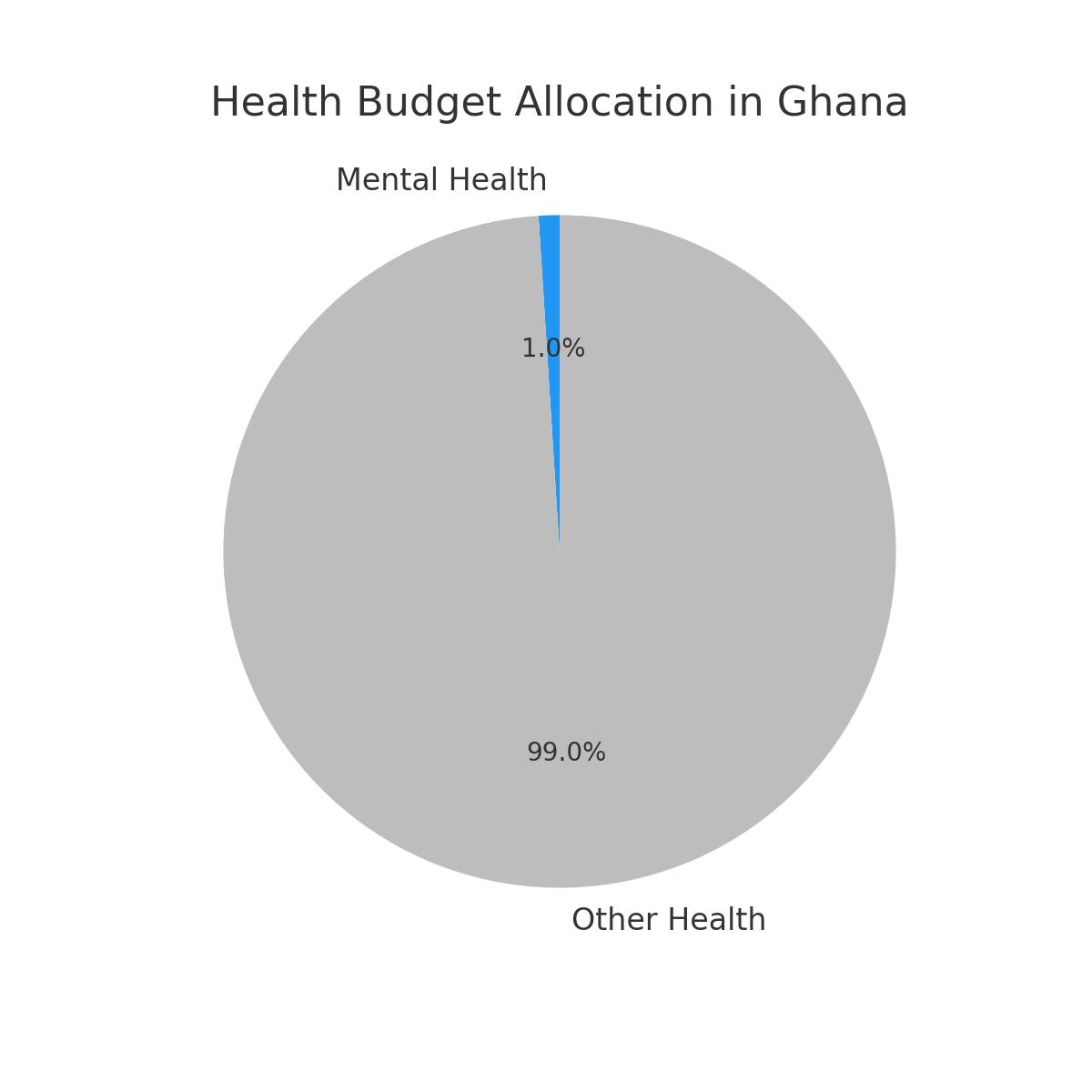
Scholarly studies highlight a critical gap in Ghana’s mental health care. Ofori-Atta et al. (2018) emphasize that despite the Mental Health Act, implementation has been slow due to funding shortages and stigma. Ae-Ngibise et al. (2010) explored cultural beliefs, finding that many Ghanaians attribute mental illness to spiritual causes, leading families to seek help from prayer camps instead of hospitals. The WHO Mental Health Atlas (2020) reveals that Ghana spends less than 1% of its health budget on mental health, far below global recommendations. Human Rights Watch (2019) documented severe abuse, chaining, and forced confinement in prayer camps, despite the existence of legal frameworks forbidding such practices. Globally, countries like South Africa and Kenya have made progress in integrating mental health into primary care systems. These models emphasize community-based services, early intervention, and reducing stigma through education—strategies Ghana could learn from and adapt. However, the gap between policy and practice remains Ghana’s biggest challenge.
3. Case Studies
Case Study 1: Ama — The Silent Battle with Depression
Ama (pseudonym), a 24-year-old university student in Accra, suffered from major depression. For years, her symptoms were dismissed as laziness or spiritual affliction. She explained: 'I kept telling people I couldn’t sleep, I couldn’t focus, I felt hopeless. They told me to pray harder. My parents even took me to a prophet. No one suggested seeing a doctor.' Without intervention, her condition worsened until she attempted self-harm. Only after a crisis did she receive psychiatric care at Korle Bu Teaching Hospital. With therapy and medication, she is gradually recovering.
Case Study 2: Kofi — Chained in a Prayer Camp
Kofi, 32, was diagnosed with schizophrenia. Instead of being referred to a hospital, his family brought him to a prayer camp in the Eastern Region. There, he was chained outdoors, subjected to fasting rituals, and beaten during 'deliverance.' Human Rights Watch (2019) confirms that thousands of people across Ghana endure similar abuses. Chaining, forced isolation, and denial of food remain common practices in unregulated camps, despite the Mental Health Act of 2012 banning them.
Case Study 3: Efua — A Story of Recovery
Efua, a teacher, developed postnatal depression after childbirth. Unlike many, she was referred to Accra Psychiatric Hospital, where she accessed therapy and medication. Within months, she stabilized and returned to teaching. Her case illustrates that with proper treatment, recovery is possible. Efua’s story demonstrates hope—but also highlights the rarity of timely medical intervention in Ghana.
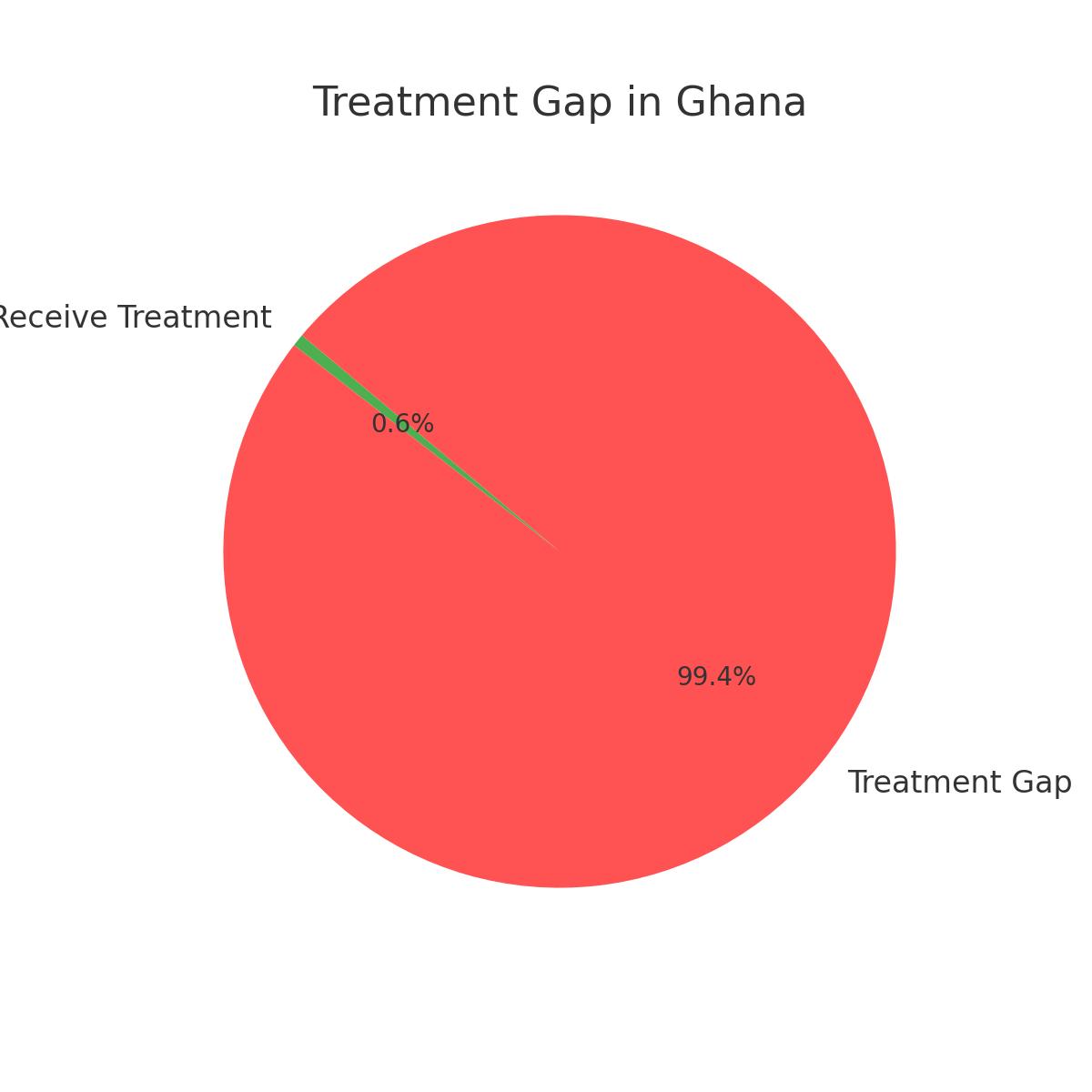
4. Statistical Overview
The data illustrates the scale of Ghana’s mental health burden and the severity of the treatment gap. Prevalence is high, depression is widespread, yet treatment access remains minimal. The following infographics highlight the most pressing statistics.
5. The Mental Health Act (2012): Progress and Limitations
The Act was a historic step, establishing rights and protections for those with mental illness. Its aims included promoting community-based care, regulating faith-based healing centers, and reducing stigma. However, underfunding prevents effective enforcement, rural areas remain underserved, and awareness campaigns are limited.
6. Challenges in Ghana’s Mental Health System
The challenges are multidimensional: stigma rooted in cultural beliefs, only three psychiatric hospitals for the nation, continued human rights abuses, severe workforce shortages, and less than 1% of the health budget allocated to mental health.
7. Voices of Change
Organizations such as BasicNeeds Ghana, MindFreedom Ghana, and WHO initiatives are working to integrate mental health into community care, advocate for rights, and train healthcare workers. Yet without strong government support, scaling remains limited.
8. Recommendations
Recommendations include: increasing funding (at least 5% of the health budget), expanding the workforce of psychiatrists and psychologists, creating community counseling centers, running public education campaigns, enforcing laws on prayer camps, and leveraging telemedicine.
9. Conclusion
Mental health is not a curse—it is a medical condition that requires compassion, care, and treatment. Ghana has made progress through the Mental Health Act, but stigma, underfunding, and abuse persist. Every day is an opportunity to change perceptions, offer help, and support those silently battling storms. Mental health matters—every single day.
10. References
Ae-Ngibise, K. A., et al. (2010). ‘Whether you like it or not people with mental problems are going to go to them’: A qualitative exploration into the widespread use of traditional and faith healers in the provision of mental health care in Ghana. International Review of Psychiatry, 22(6).
Human Rights Watch. (2019). “Like a Death Sentence”: Abuses Against Persons with Mental Disabilities in Ghana.
Ofori-Atta, A., Read, U. M., & Lund, C. (2018). Mental health in Ghana: Progress and challenges. International Journal of Mental Health Systems, 12(1).
World Health Organization. (2020). Mental Health Atlas. Geneva: WHO.
World Health Organization. (2022). Depression and Other Common Mental Disorders: Global Health Estimates.