Skin Reference Book 2025
Written by the Skin Team



Team Leader
Rachel Densing, BSN, RN, CWOCN, RNC-NIC




The Team
P2 Mia Treadwell, BSN, RN, WTA, APONC
PICU Amy Lozano, MSN, RN, WTA
PICU Clare Parilla, BSN, RN, WTA, CCRN
PICU Paige Stoessel, BSN, RN, WTA
PICU Lauren Shavzin, BSN, RN, WTA
P4S Janessa Alcaide, BSN, RN, WTA
PCICU Jenifer Calix Marin, BSN, RN, WTA
PCICU Jamie Alison Sembrano, MSN, CPNPAC/PC, RN, WTA
P5 Kayla Bradshaw, BSN, RN, WTA
NICU Srishti Mehta, BSN, RN, CCRN, WTA
NICU Nicole Syage, BSN, RN, WTA
WOC RN: Wound, Ostomy, Continence RN
• Certified specialty nurse with knowledge and training on wounds, ostomies, and continence care
• Leaders in care, care delivery, and education for patients, families, and frontline staff
WTA: Wound Treatment Associate
• Collaborates with team, bedside RN, and WOC RN to provide routine care for healthy skin
• Assists with identification of patients at risk for pressure injuries and promoting preventative care
• Trained in identifying and addressing factors that contribute to skin breakdown
• Trained in assessing and documenting wound status and healing progress
Active surveillance
A systemic proactive approach to regularly assess patients for the development of pressure injuries, ensuring early detection and timely interventions to prevent potential injury.
• In the PICU and the PCICU, active surveillance is done on a weekly basis by WTA trained nurses
• Throughout Kravis Children’s Hospital, active surveillance is conducted on a monthly basis; findings are reported monthly to Solutions for Patient Safety and quarterly to Press Ganey
Hospital-Acquired (HAPI) and Community-Acquired (CAPI)


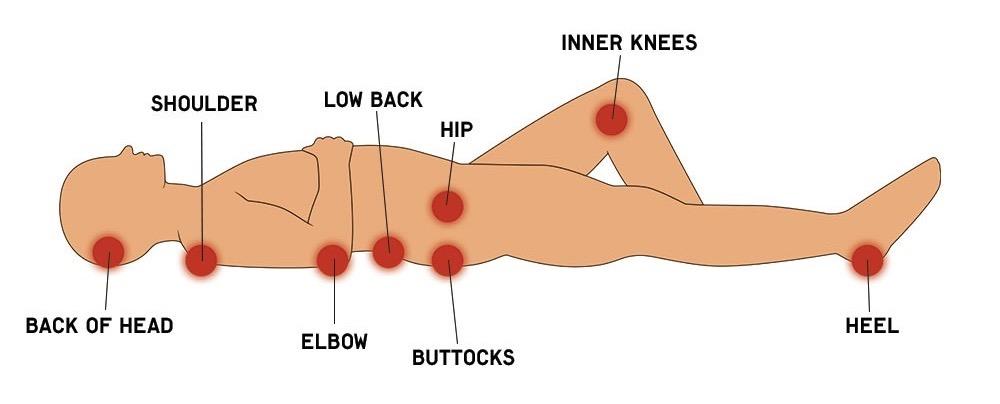
A pressure injury (PI) is defined as localized damage to the skin and soft tissues, usually over a bony prominence and can be related to a medical device. (NPIAP, 2019)
Intense, prolonged pressure, friction, and/or shear are all forces that contribute to patients getting pressure injuries. These injuries can look different in patients of different ages, populations, skin tones, illnesses, and comorbidities. (NPIAP, 2019)
Not all skin breakdown is a pressure injury!
Our patients can also get MARSIs, IAD, MASD, and more. Ask your unit skin champions and/or your WOC RN for clarification.
All RNs have the knowledge to assess and manage wounds, but ALL pressure injuries must be validated and staged by a certified WOC RN!

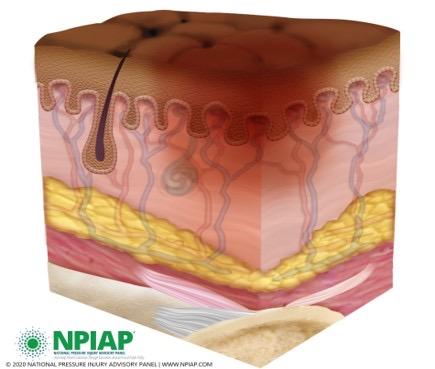
Healthy skin
Light and dark pigmented
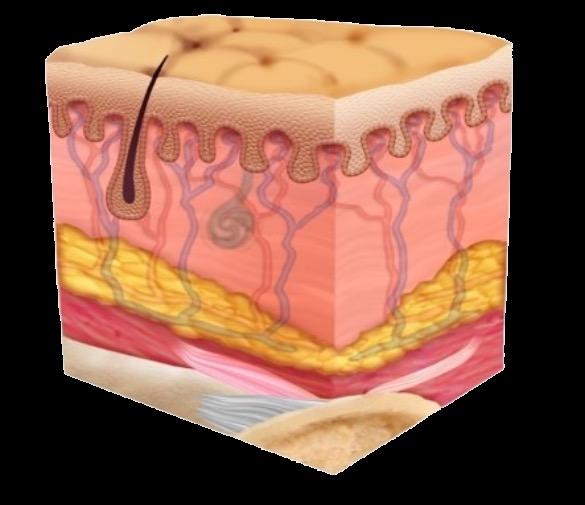


Stage 1 PI: Non-blanchable erythema of intact skin
This can easily be missed in darker skin tones.
Assess for changes in temperature, sensation, and firmness of the area, indicating skin/tissue damage.
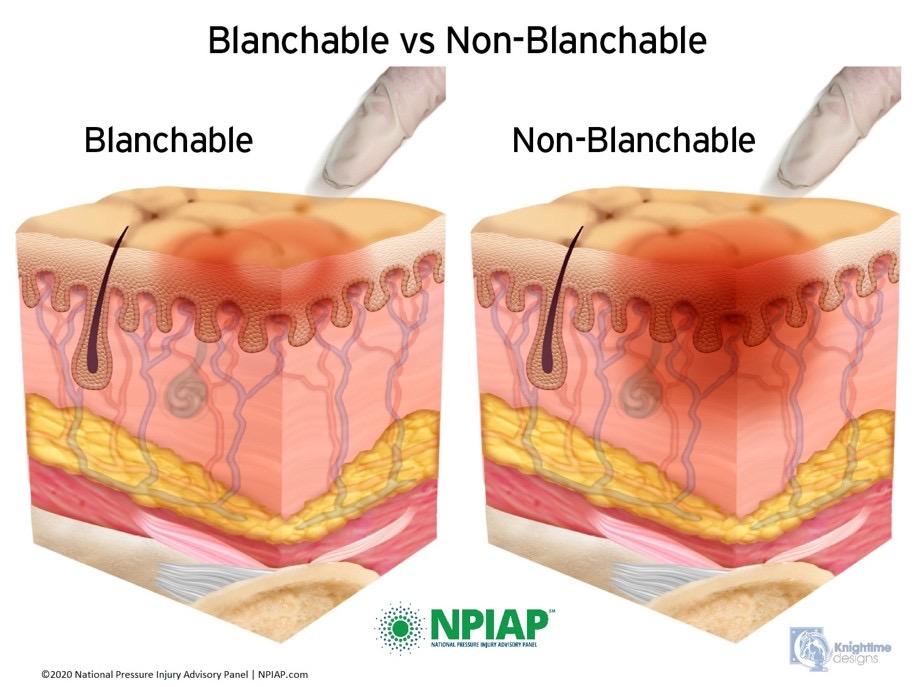
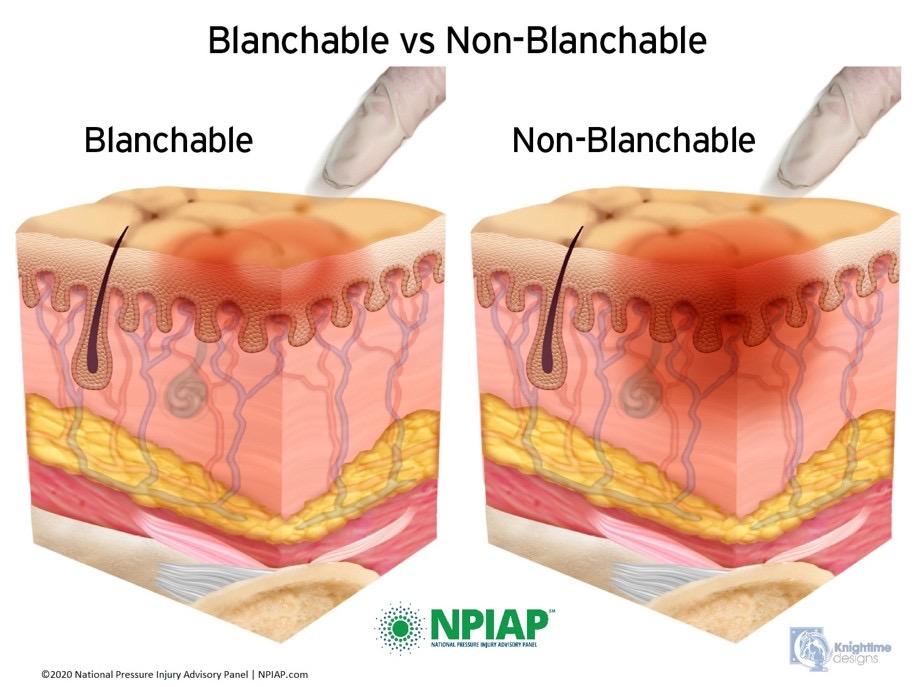
Blanchable Non-Blanchable vs.


Sample Stage 1 images


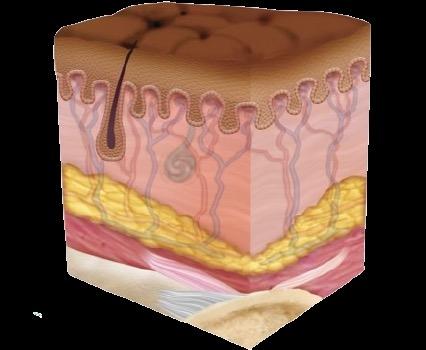
Stage 2 PI:
Partial thickness skin loss with exposed dermis
The wound bed is pink/red and moist; can present as an intact or ruptured blister. Granulation tissue and underlying tissue are not visible and the wound bed itself is viable.




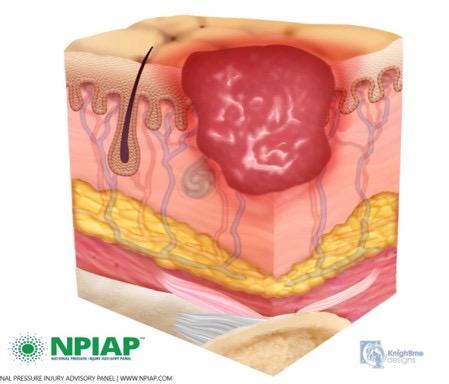
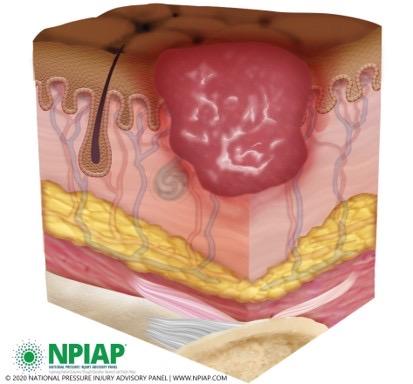
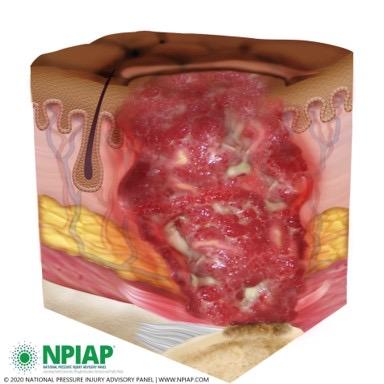
Stage 3 PI: Full thickness skin loss
Adipose tissue and granulation tissue are visible. Slough, eschar, and epibole (rolled wound edges) are typically present. Wound depth varies based on the anatomical location of the wound. Undermining and tunneling may be present.
Notice how, in the darker skin tone, the redness around the wound is less visible.




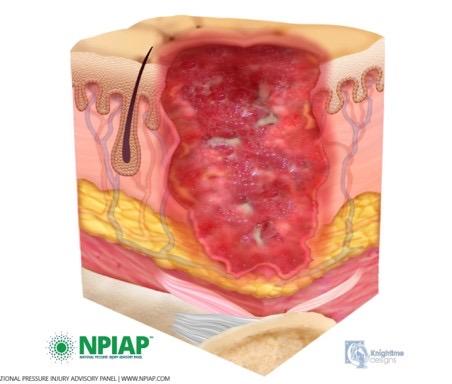
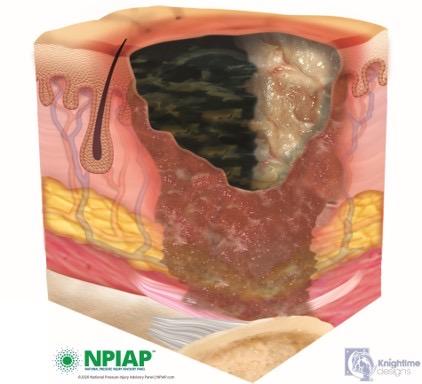
Stage 4 PI: Full thickness skin and tissue loss
Underlying fascia, muscle, tendon, ligament, cartilage, and/or bone can be visible. Like in Stage 3, eschar, slough, epibole, undermining, and tunneling are likely present.

Sample Stage 4 image


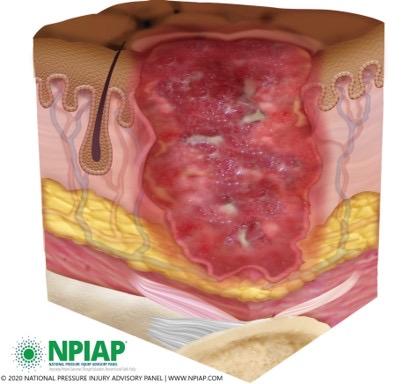
Unstageable:
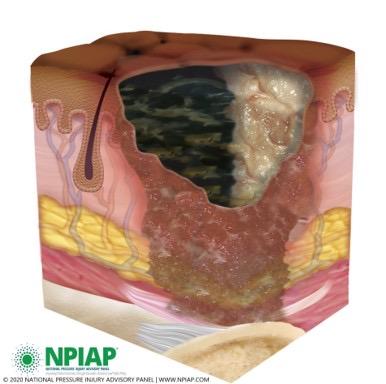
Obscured full thickness skin loss
Eschar and/or slough are covering a part or entire wound bed and staging cannot be confirmed.
If bone, muscle, fascia, tendon, ligament, and/or cartilage are visible, can be considered a Stage 4.




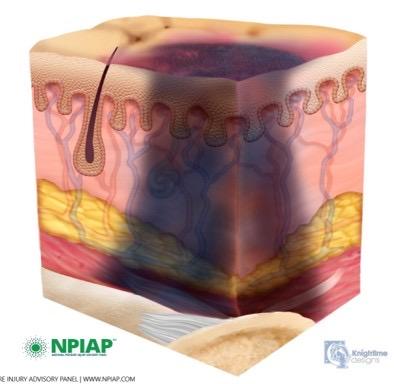
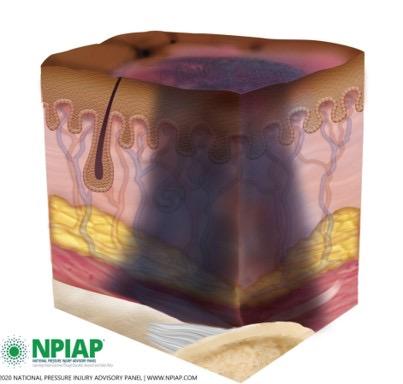
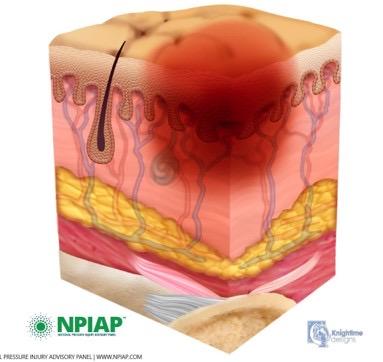
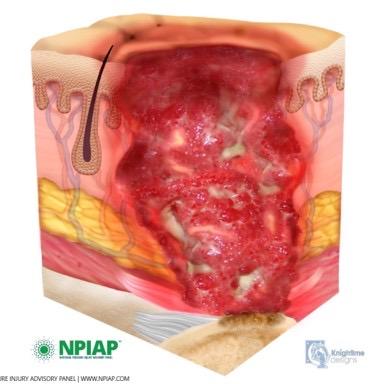
Deep tissue injuries:
Non-blanchable deep red, maroon, or purple discoloration
Intact or non-intact skin that reveals a dark wound bed or blood-filled blister. In these wounds, pain and temperature changes can precede the color changes.





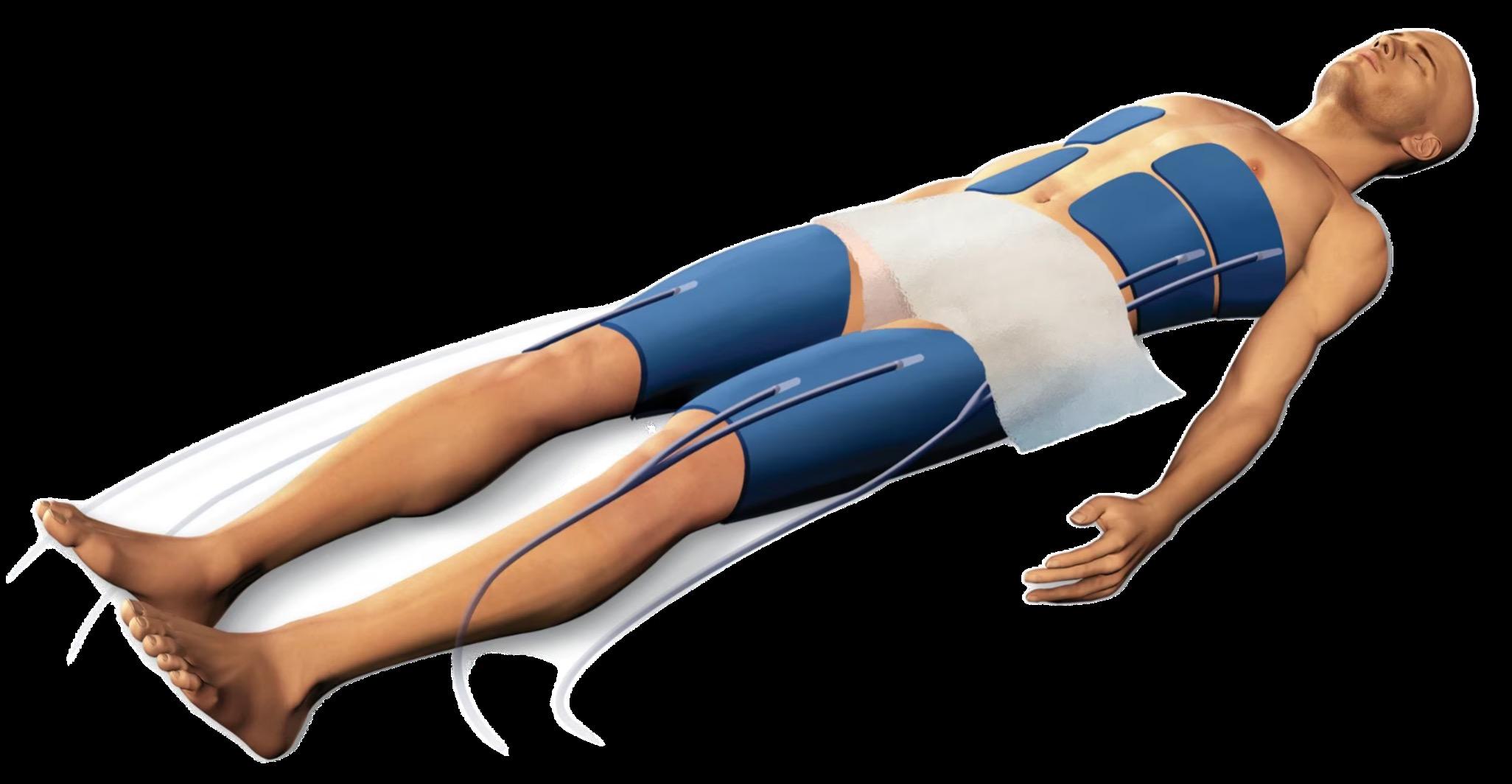
Skin care protocol for patients on ECMO
• Perform head-to-toe skin assessment every shift
• Note any areas of redness from devices
• Ensure patient is on the appropriate bed/surface
‒ Giraffe warmer vs. Crib vs. Progressa
• Rotate devices if able
1. EKG leads q12hr (0800, 2000)
2. Pulse ox q6hr (0800, 1400…)
3. BP cuff q6hr (0800, 1400…)
• CHG bath completed during day shift
• Minimal adhesive use
• Daily linen/draw sheet change (team discretion)
‒ Coordinate for necessary team members to be present (at least RN, RT, perfusionist)!
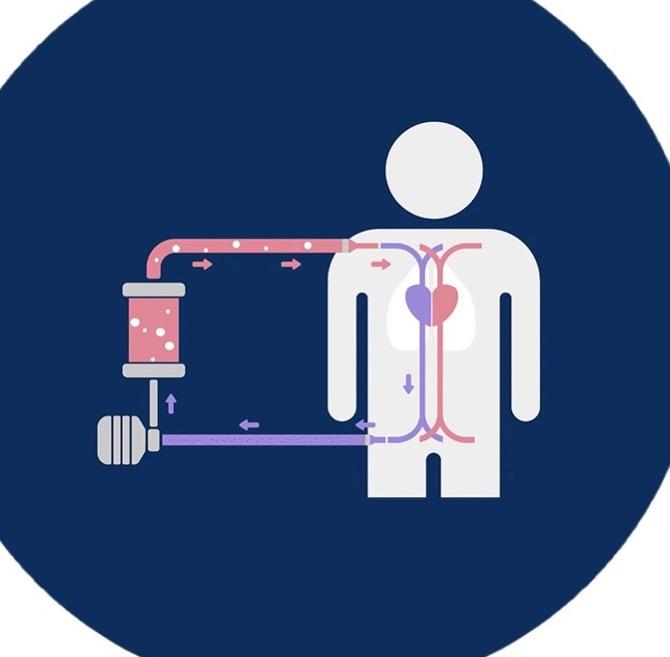

Repositioning
• Dependent on cannulation (if unsafe to reposition/turn patient, obtain a “Do Not Turn” order).
• With help of perfusionist, RT, and RN, micro-turn patient q3hr with MD/APP present.
• If patient is tolerating microturns, position patient from supine to slightly side-lying with help of fluidized positioners (e.g., Z-Flo).
• Always ask for help from multiple team members when turning, lifting, or repositioning.
Skin protection
Apply foam dressings on pressure points:
• Occiput
• Sacrum
• Elbows
• Heels Make sure dressings are clean, dry, and intact; change PRN if soiled.
Utilize fluidized positioners to cushion bony prominences.

Follow manufacturer guidelines for Arctic Sun and Blanketrol cooling systems by avoiding direct contact between the infant/pediatric patient’s skin and cooling pads.
Continuously monitor skin temperature using a temperature probe.
Temperature monitoring can also be done with built-in sensors in foley catheters, endotracheal tubes, or a rectal probe.
• Use a thin barrier, such as a baby blanket, between the skin and cooling device.
• For larger pediatric patients, use a flat sheet as a barrier between the patient and the cooling blanket.

Use hydrogel dressings, e.g., Kerralite, DermaGel (special order from materials management), over bony prominences or other areas of concern to prevent pressure ulcers without compromising temperature management.

Avoid placing fluidized positioners directly on the patient’s skin, as they can conduct heat and hinder the cooling blanket’s function. Instead, place positioners under the cooling blanket, ensuring they do not create divots that disrupt water flow.
Use endotracheal tube (ETT) holders when appropriate:
• ETT sizes 5-10: Use an endotracheal tube holder (Hollister Anchor Fast), which allows for repositioning of the tube at left, center, and right sides of the mouth.
• Reposition the tube site q4hr.
• Inspect the patient’s lips, skin, and oral cavity at least q2hr or more frequently if the patient’s condition dictates. Patients requiring 3M ETT taping:
• When taping/retaping the tube, assess the skin where adhesive is placed.
• Consider alternating sides of securement with every retaping.

Due to the nature of acute care/intensive care units, peripheral access/central access and blood pressure monitoring are needed.
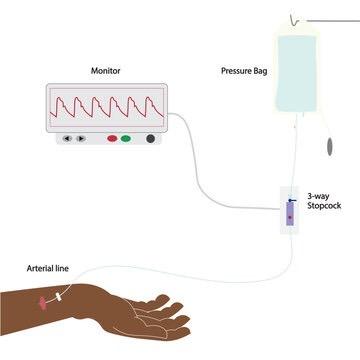
Dressing/redressing
Proper dressing kits should be used and dressing changes should be done as per policy.
• When redressing these sites, assess skin once dressing is taken down
• Note the areas underneath the catheter and suture sites
• Place protective/securement devices provided by dressing kits. These provide padding to prevent formation of medical device-related PIs (MDRPIs)

• Hubguard for peripheral IVs
• Stat locks for PICC lines
Trach dressing
• Clean with normal saline, then dry.
‒ Other wound cleansers such as hydrogen peroxide or hypochlorous acid (e.g., Vashe) must be ordered by a licensed provider.
• Apply a thin foam dressing under trach ties if excess moisture is expected.
• Thin foam dressings are placed around the trach by ENT during trach surgery.
• Maintain foam dressing or split gauze around trach stoma and change every shift.
• Offload ventilator tubing from resting on skin by using supportive equipment or foam dressings.

Tracheostomy tube
Rotation is key!
• EKG: Rotate once a shift or every 12 hours
• BP cuff: Rotate limb twice a shift (when applicable)
• Pulse ox: Rotate twice a shift or every 6 hours
• G-tube: Offload G-tube with thin foam dressing or single layer of split gauze
• Video EEG: Daily skin checks with vEEG tech after the first 48 hours.
‒ Inquire about a scalp rest if patient on vEEG for > 48 hours
‒ Refer to Policy PED-GEN-06 on PolicyTech for “Skin Safety During EEG Procedure”



Definition: Skin loss or irritation related to medical adhesive used during patient care, typically mirrors the pattern of the adhesive.
Common causes: EKG leads, vEEG leads, IV dressings, transparent dressing (e.g., Tegaderm), hydrocolloids (e.g., Duoderm).
• Make sure skin is clean and dry.
• If using skin sealant (e.g., Skin Prep), allow sealant to dry completely before applying adhesive.
• When removing adhesive, hold patient’s skin while slowly pulling adhesive at a low angle, keeping adhesive parallel to patient’s skin. Avoid pulling up at a 90º angle!
• Use adhesive remover.
• Avoid stretching adhesive during application.
• Rotate sites and replace adhesives per manufacturers’ recommendations.
• If blister is present and intact, leave open to air and avoid any trauma to blister.
• Gently clean with normal saline or wound cleanser. Pat dry with gauze.
• Apply clear, porous dressing (e.g., Mepitel One) over skin injury. Change every 7 days or PRN.
• Apply ointment over dressing if ordered.
• If wound has exudate, cover with foam dressing.
• Does not need a skin/wound consult unless not healing after 2 weeks of above treatment.
Definition: Partial thickness wound caused by moisture or friction at the surface of the skin.
Presents as: A linear break in the skin or as tears with partial or total skin loss, with or without a flap.
Prevention:
• Avoid tape if possible in vulnerable populations (e.g., neonates, radiation therapy, cardiac issues, etc.).
• Pad hard surfaces in patient’s room.
• Keep skin supple with emollients.
• Gentle patient handling.
Treatment:
• If no or minimal tissue loss and flap present, clean wound with normal saline flush, roll flap into place, and secure with a non-adherent dressing/wrap.
• Foam/silicone dressings or non-adhesive foam with wrap gauze.


Definition: Skin breakdown resulting from prolonged exposure to moisture.



Type of MASD
Incontinence
Associated
Dermatitis (IAD)/Diaper
Dermatitis
Intertriginous
Dermatitis (ITD)
Description
Superficial skin breakdown of areas exposed to urine and/or stool
Prevention/ Treatment
Toileting program, scheduled checks and diaper changes, use of pH-balanced cleansers, moisturizers, and moisture barrier creams
Skin breakdown due to moisture trapped in skin folds (under breasts, abdominal folds, axillae, groin, buttock folds, between fingers and toes)
Periwound/ Peristomal MASD
Breakdown of surrounding skin of wounds or stomas (e.g., Ostomies, G-tubes, trachs) due to large amount of exudate or stoma output
Routine skin assessment, use of absorptive/wicking products between skin folds (e.g., InterDry Ag), moisture barrier agents, and bed surfaces that support airflow
Keep surrounding skin clean and dry. Use polymer film dressings (e.g., skin sealants like Skin Prep or 3M Cavilon).
Skin assessment
No rash, intact skin

Redness, intact skin
Treatment
Vitamin A&D / Petroleum jelly
EPC

Bleeding diaper rash
How to apply
• A thin layer should be applied to clean, dry skin with every diaper change.

Crusting w/ Triad Cream

• A thick layer should be applied to clean, dry skin.
• Apply a layer like “icing a cake”. Does not need to be completely wiped off with every diaper change.
• Remove the top soiled layer only.
• Make sure the area is as clean and as dry as possible. Lukewarm water in a peri bottle is preferred over blue wipes for cleaning the area.
• Apply a thin dusting of stoma powder over open wounds, spray skin sealant (e.g., Cavilon), repeat 2x if needed, then cover with Triad Cream.
• Reapply with diaper changes as needed.
• If your patient is continent, educate them on the importance of using the bathroom and the risk of skin breakdown when urine/stool sit on the skin.
• Offer going to the bathroom frequently to prevent patients from having accidents.
• If parents are changing diapers, educate them on the importance of applying a barrier ointment/cream to the patient’s skin with every diaper change.
• Offer to help turn or reposition patients with limited mobility every 2 hours.
‒ For involved family present at the bedside, a turning clock in their room can be helpful!
What is crusting?

Crusting is a technique used to create an artificial skin membrane using powder and a skin sealant.
What is Triad cream?
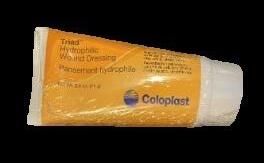
Triad cream is a hydrophilic wound cream that draws moisture away from the skin and into the cream while providing a moist wound healing environment. Can also be used on hard-to-cover wounds.


Definition: Abnormal hair loss; most common cutaneous reaction seen in cancer patients receiving chemotherapy.
Seen as early as 3 days to 3 months after treatment starts.
Though many chemo agents are known to cause some form of hair loss, common drugs used to treat pediatric cancer patients that have the highest rate of hair loss are individual or combination agents like Cyclophosphamide, Cisplatin, Ifosfamide, Carboplatin, and Temozolomide, all noted as alkylating agents.
Hair regrowth usually begins after treatment is complete, however, gently massaging and shampooing the scalp can help optimize blood flow to hair follicles and stimulate hair growth.
Definition: Darkened areas or patches on skin.
• Common cutaneous reaction affecting skin, nails, and mucosa in chemo patients
• Can be seen with: 5-FU (Flourouracil), Vinorelbine, and Daunorubicin
• Treatments with Busulfan and Thiotepa: Skin darkening following diffuse rash
• Discoloration may improve over time, while others may be long lasting
• Avoid overexposure to sunlight
‒ Use of sunscreen may help minimize hyperpigmentation






Toxic Erythema of Chemotherapy (TEC)
• AKA hand-foot syndrome
• Reddened and painful patches on palms, soles, and within skin folds
• Swelling, peeling of outermost layer of skin
• Occurs days to weeks after the start of treatment
• Related Chemo: Antimetabolites (6-MP)
• Treatment: Postponing chemo, dose adjustment, and supportive care (steroid creams)
Xerosis
• Rough, dry skin; scaly, cracked, or bleeding, typically seen on skin over joints
• Can be seen 2-3 months after the start of treatment
• Related chemo: Anti-tumor antibiotics (Bleomycin, Dactinomycin, and Doxorubicin)
• Treatment: Moisturize skin routinely
– Apply recommended lotions or emollients
– Drink plenty of water to keep hydrated
Chemo rash
• Broad term that describes the many types of skin rashes that result from chemotherapy
• Usually presents as groups of small pimples and pus-filled blisters that commonly appear on face, neck, chest, scalp, and back
• Treatments:
– Mild/Moderate: Topical steroid creams with oral antibiotics
– Severe: Oral steroids, adjustment of chemo, antihistamines for itchiness
Mucositis
• Inflammation of the mucosal lining; affects the mouth, pharynx, and GI tract
• Most debilitating side effect of chemotherapy; needs pain management, progressing to painful ulcerations ultimately altering nutrition
• Prevention: Routine oral hygiene, saline rinses, use of soft toothbrushes or toothettes
• Treatment: Emollients/balms for the lips, analgesic oral rinses, cool compress




Neonates have extremely immature and vulnerable skin, putting them at higher risk for skin injuries.
Limited mobility, edema due to prematurity, and decreased adhesion between the layers of the skin make them susceptible to breakdown.
Medically necessary devices, such as respiratory devices, are one of the major causes of breakdown to neonatal skin, accounting for 35-90% of all injuries.
Premie skin is difficult to assess; transparent and gelatinous skin makes superficial, subtle, and early signs of injury challenging to visualize.
Increased inflammation due to prematurity can cause these injuries to lead to permanent scarring, especially in high-risk areas for neonates: around their noses, temples, cheeks, and hands.




Stage 1
Non-blanchable erythema

Stage 2
Intact/ruptured blister
Stage 3
Full thickness skin loss

Stage 4
Full thickness tissue loss
Unstageable
Full thickness skin loss

Deep tissue injury–depth unknown
Epidermal stripping: Skin tear

Epidermal stripping: Skin stripping
Respiratory devices such as ETTs, tracheostomies, and nasal prongs (e.g., Hudson Prongs) are the leading cause of pressure injuries in neonates.
G-tubes and video EEG electrodes also cause pressure injuries due to the neonate’s inability to reposition themselves.
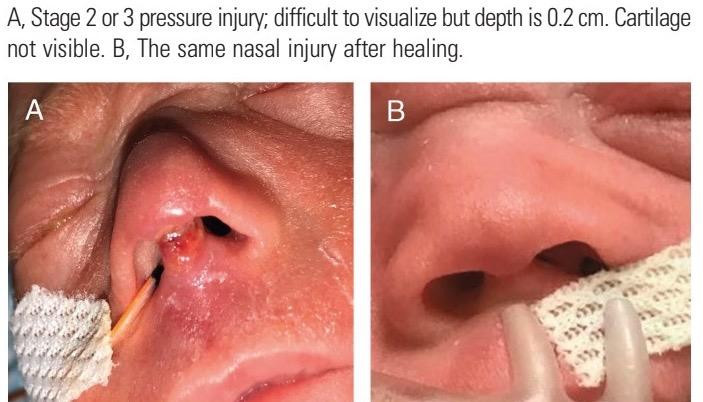
Assessment of small wounds on small surface areas can be difficult.

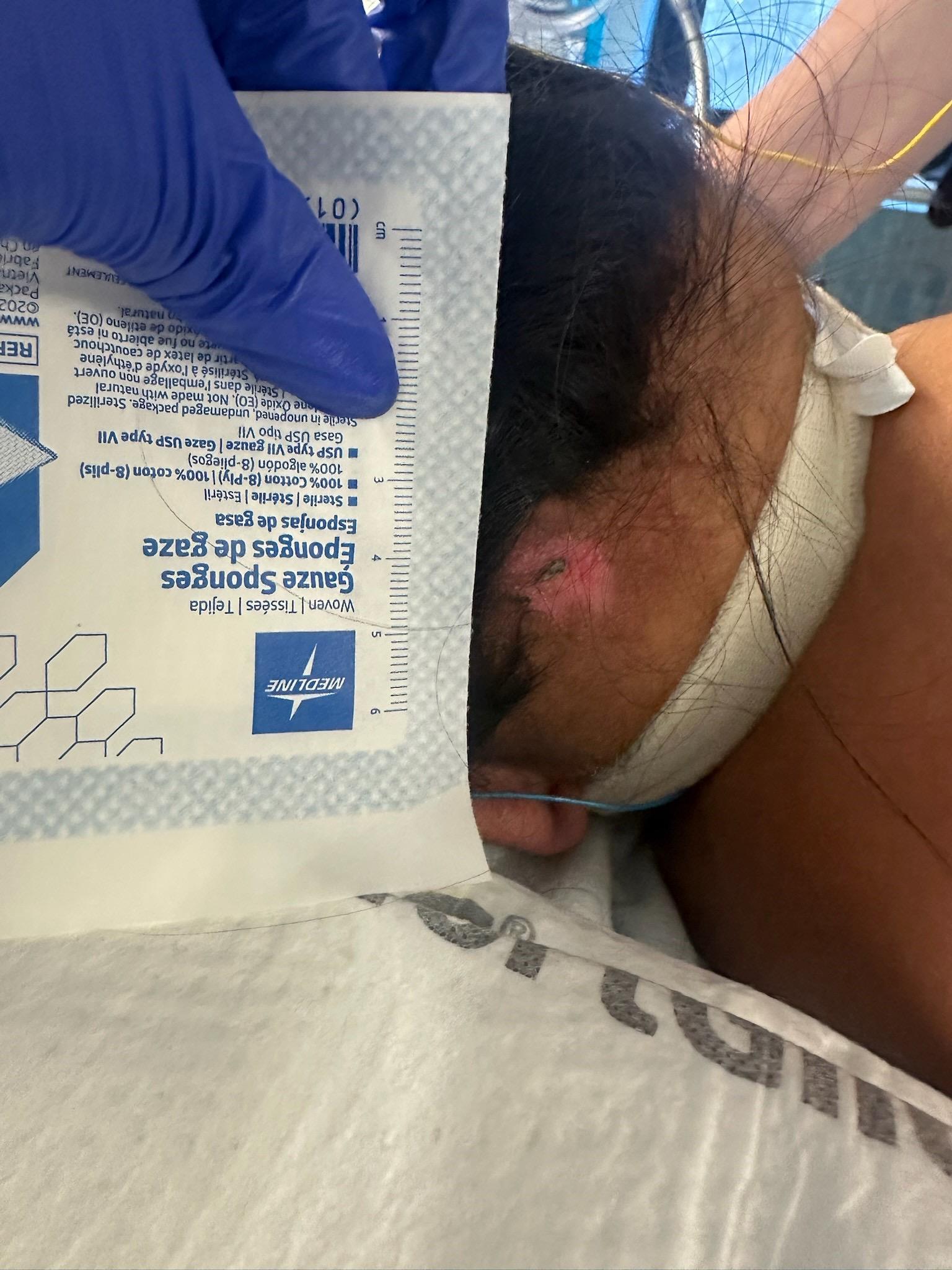
Deep tissue pressure injury from near-infrared spectroscopy probe.
Pressure injury at the Columella caused by bubble continuous positive airway pressure device.
A: Stage 2 or 3 pressure injury; difficult to visualize but depth is 0.2 cm. Cartilage not visible. B: Same nasal injury after healing.
Most pressure injuries in the NICU are related to nasal prongs (e.g., Hudson Prongs).
Prevent injury by:
• Offloading the prongs and tubing set every 3 hours or with cares.
• Removing any moisture from the tubing, prongs, and babies’ faces.
• Using assistive devices such as velcro clips, “arms” for isolettes, or jellies to secure heavy CPAP tubing in place.
• Ensuring the proper size of nasal prongs are used.
Ask your unit
Respiratory Therapist, Skin Champion, or nurse leader for assistance if needed!



• HIGH score = HIGH risk
• Considers medical devices and tissue perfusion/ oxygenation
• Scores ≥13 are considered AT RISK

• HIGH score = LOW risk
• Does NOT include medical devices or tissue perfusion/oxygenation
• Scores ≤16 are considered HIGH RISK
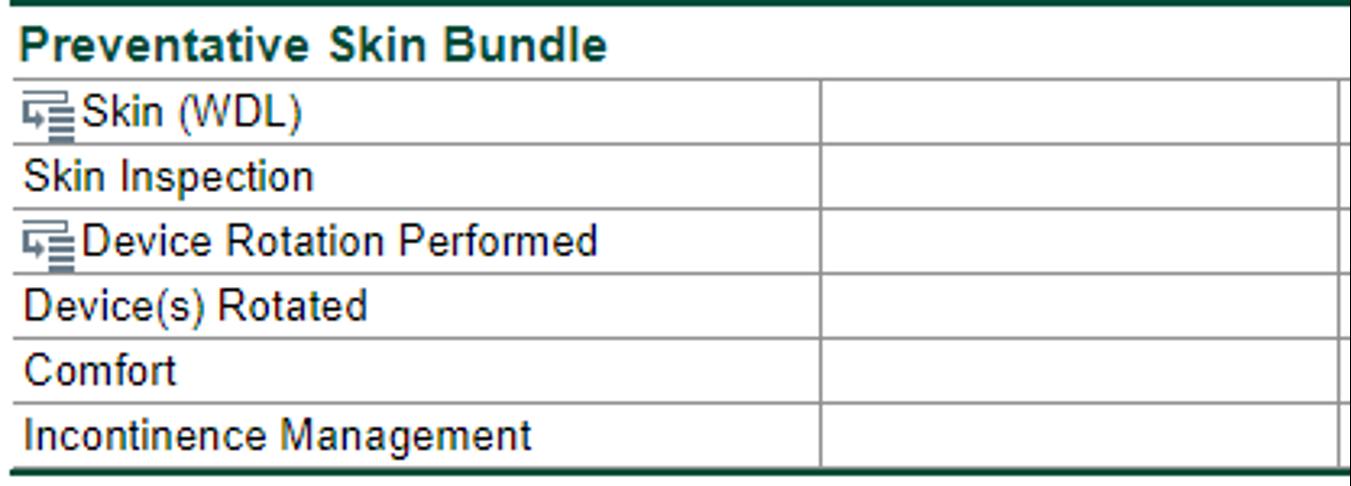
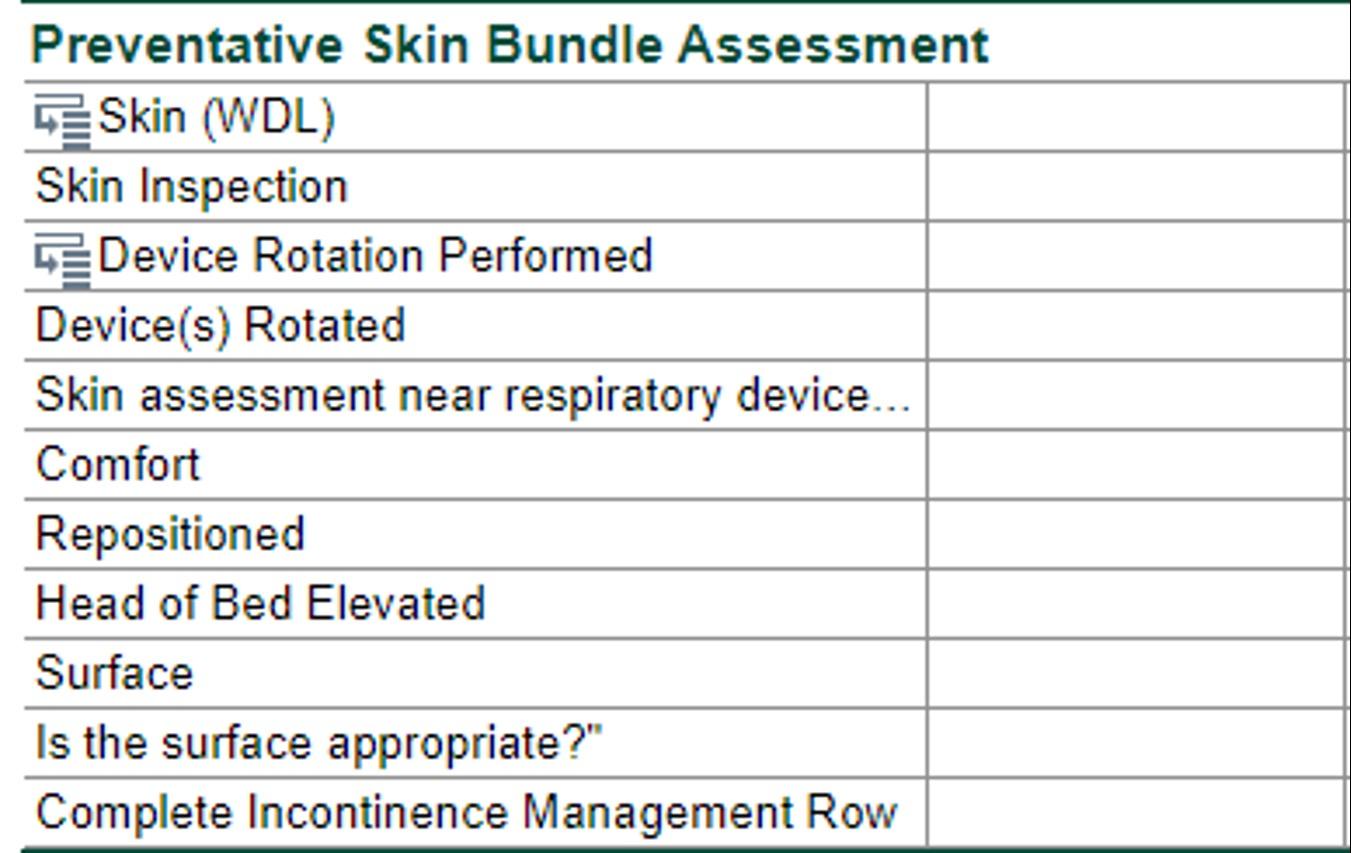
Documentation guidelines
• Skin assessment: Every 12 hours at minimum
‒ Correlates with the “Skin” section from “Head-to-Toe” flowsheet
• Device rotation/protection of skin under devices:
‒ EKG leads: Once a shift
‒ Pulse ox/BP cuff/NIRS: Every 6 hours, at 8 am/pm and 2 am/pm
‒ Respiratory devices: Every 4 hours
• Reposition:
‒ If independent: “Turns self” once a shift
‒ If assist/complete assist needed: Every 2-3 hours
• Head of bed: Once a shift or with changes
• Surface: Once a shift or with changes
• Moisture management:
‒ If continent: Once a shift
‒ If incontinent: Every 3-4 hours or with every diaper change
“NICU
“Pediatric

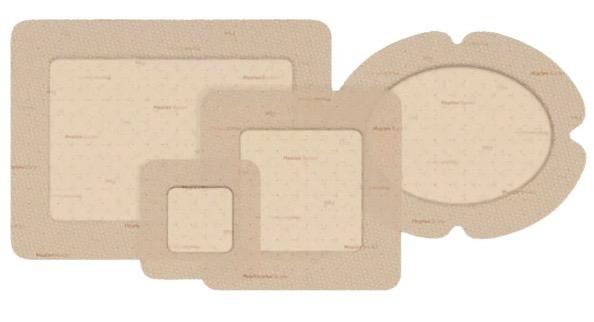
Mepilex is a gentle skin protectant that forms a barrier against external forces, redistributes pressure, and supports healing by absorbing exudate while keeping the wound environment moist.
Mepilex border flex
Purpose: A self-adherent foam dressing designed for wounds with moderate to high exudate, such as pressure ulcers or surgical wounds.
• Key features: Cushioning effect protects against pressure injuries; absorbs moderate to highly exuding wounds
• Ideal uses: Pressure ulcer prevention, especially on high-risk bony areas like the sacrum, heels, shoulder blades, elbows, knees
• Change every 3-5 days or when exudate reaches the borders

Purpose: A thin foam dressing designed for low-exuding wounds or areas requiring light cushioning and protection
Key features: Thin and flexible for hard-to-dress areas
Ideal uses: Superficial wounds with low exudate, such as abrasions or small surgical wounds; skin protection under medical devices like oxygen tubing or tracheostomy flanges
Change every 3-5 days or when clinically indicated (e.g., when saturated or no longer adhering properly)

Purpose: A foam dressing shaped specifically for the heel, used to prevent and treat pressure injuries
Key features: Anatomically shaped for the heel
Ideal uses: Absorbs exudate and redistributes pressure; prevention and management of pressure injuries
Change every 3-7 days or sooner if saturated with exudate

Purpose: A dressing specifically designed for the sacral area to prevent pressure injuries and manage wounds
Key features: Shaped to fit the sacrum, absorbs exudate while redistributing pressure
Ideal uses: Prevention of sacral pressure ulcers; treatment of wounds in the sacral area with moderate to high exudate
Change every 3-7 days or when the dressing is saturated or begins to lift

Purpose: A gentle wound contact layer designed for use on delicate or sensitive skin, ensuring minimal trauma upon removal
Key features: Made from soft silicone, allowing it to be atraumatic upon removal; open mesh design allows exudate to pass through to a secondary absorbent dressing
Ideal uses: Burns, skin grafts, superficial wounds, skin tears; minimizes damage when changing dressings frequently
Change every 7-14 days or as needed when used in combination with a secondary dressing
Purpose: Standard foam dressing used for managing non-infected wounds with moderate exudate and protecting vulnerable skin areas/ A foam dressing containing silver, which provides antimicrobial action to reduce the risk of infection in wounds
Key features: Absorptive foam layer with gentle silicone adhesive that provides a cushioning effect/
Silver component for sustained antimicrobial activity; Foam design to absorb exudate and maintain a moist healing environment
Ideal uses: Infected wounds or wounds at risk of infection; burns, pressure injuries, and surgical wounds with moderate to high exudate
Change every 3-7 days or as needed based on the amount of exudate and clinical signs of infection


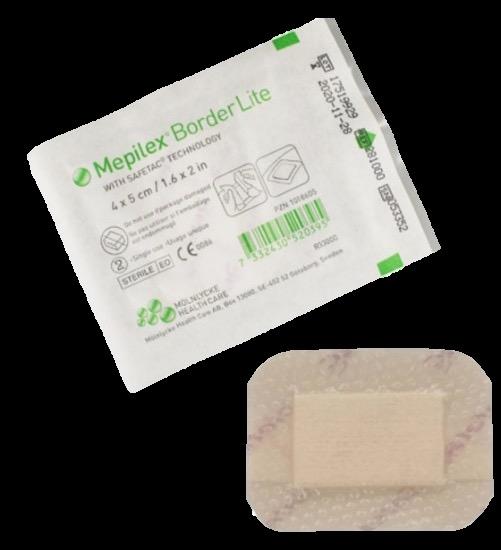
Purpose: A thin, self-adherent foam dressing designed to manage low-exuding wounds and provide protection from friction and shear. It is often used to prevent pressure injuries or as a secondary dressing
Key features: Small and slim profile can be used where flexibility is needed; absorptive foam layer is capable of managing low exudate
Ideal uses: Superficial wounds, minor burns and abrasions, or postoperative sites with minimal exudate; use under medical devices to protect against friction and pressure
Change every 3-7 days or when clinically indicated (e.g., when saturated or no longer adhering properly); up to 7 days for preventative use under medical devices
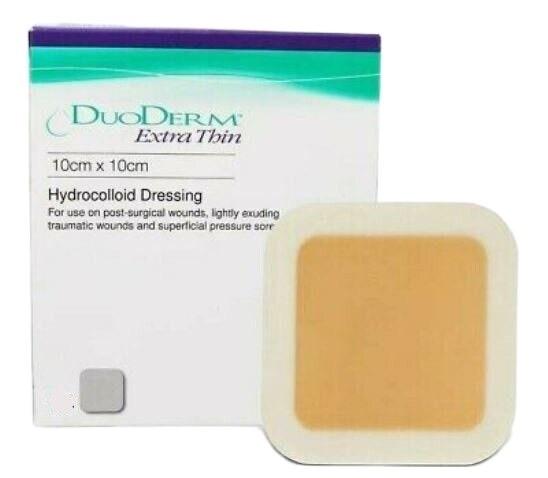
Purpose: A hydrocolloid dressing that is designed to promote healing by providing a moist wound environment that supports autolytic debridement, which accelerates tissue repair and reduces the risk of infection
Key features: Forms a gel-like layer that promotes a moist healing environment; absorbs wound exudate and acts as a protective barrier
Ideal uses: Superficial burns, partial-thickness wounds, postoperative wounds, abrasions and minor cuts, protective barrier
Change every 5-7 days or as needed based on the amount of exudate
Preparation
• Assess patient’s individual risk factors for pressure injury development
• Secure all tubes, drains, and IV lines prior to prone/supine positioning
• Apply Mepilex dressings under devices
• Place EKG leads on back when patient is prone
• Choose best foam dressing size for patient if various sizes are available
Prone and supine pressure injury prevention guide
Mepilex Border Flex
Mepilex BorderLite
Mepilex Border Sacrum
Mepilex Border Heel
Z-Flo Fluidized Positioner
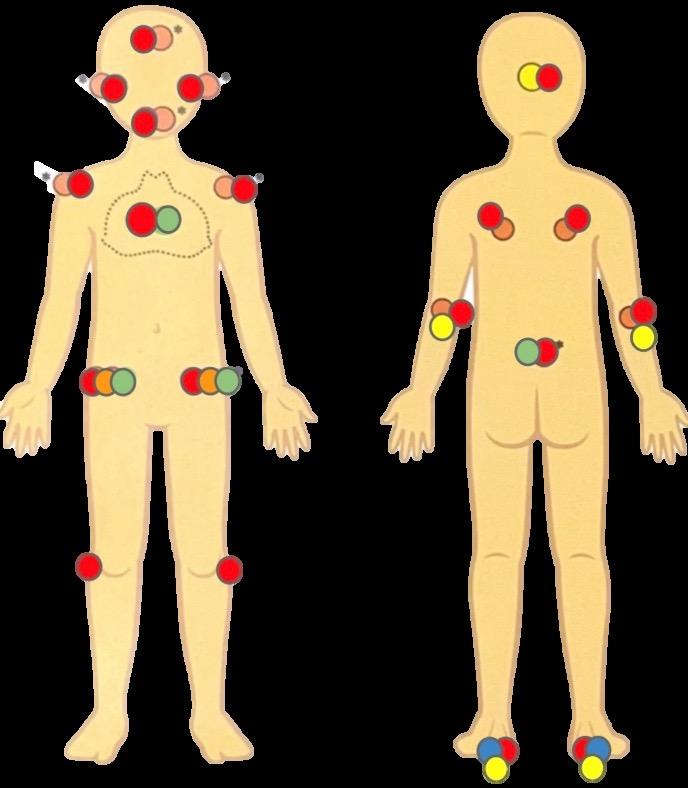
Facility note
Using clinical judgement, please consider the individual patient’s anatomy and surgical position to determine appropriate size and location of preventative dressings.
Foam dressings like Mepilex prevent pressure injuries, protect fragile skin, and reduce the impact of friction and shear for high-risk patients.
• Surgical procedure
• Inability to reposition oneself
• Past history of pressure injuries
• Malnutrition
• Braden QD Score > 13
• Braden Score < 18
• Traction
• Quadriplegia, paraplegia, SCI, spina bifida, or other neurological disorders
• Morbid obesity
• Bony prominences
• Bedrest

Place Mepilex under medical devices that cannot be repositioned every 6-12 hours to minimize device-related skin breakdown and/or absorb minor exudate.
Facility instructions
• Turn patients every two hours.
• Apply Mepilex to bony prominences and under medical devices.
• Apply the date and “P” for prevention or “T” for treatment on dressings.
• Offload the heels with Z-Flo positioner or pillow.
• Keep HOB 30 degrees or less (as allowed).
• Provide prompt incontinence care.
• Use one underpad for incontinent patients.
• Order a specialty bed per protocol.
ECMO cannulas/VAD
Large bore catheters
CVL, PICCs, Broviac
Trach site
Drains/Chest tubes/ Foley
Arterial line
Gastronomy tube
Ram cannula/ Nasal cannula
BiPAP/CPAP
Rectal probe
If patient is ambulatory or able to move self in bed: Document “Turns Self” once a shift.
If the patient is immobile, intubated, sedated, or <1 years old: hours with the help of positioning devices. Document in “IV Flowsheets” under the “Preventative Skin Bundle” section.
For smaller patients, Z-Flos or pillows may be used for repositioning

Utilize slide sheet and positioning wedges for repositioning larger patients


For patients who …
• … are ambulatory and T&P independently (pressure redistribution surface is documented as N/A)
• … are at low risk for pressure injuries
Non-powered air surface
Non-powered air surface = Not a pressure redistribution surface
For patients who …
• … are immobile and unable to T&P independently
• … have pressure injuries/are at risk (can help prevent/treat pressure injuries from Stage 1 to 4, when combined with turning protocols)
Powered air surface (at end of bed)
Functions
Functions

• Move patient to trendelenburg (and reverse) position
• Allows patient to control bed movement (raise HOB, etc.)
• Weigh the patient (max 500 lbs)

• Does everything the BLACK mattress does
• Turn assist: Allows user to turn bed to left and right, in any degree needed
CPR Lever: Flattens and hardens the mattress for CPR (look for the lever below the mattress).
For patients who …
• … are immobile, unable to T&P independently OR
• Have pressure injuries/are at risk OR
• Need chest physiotherapy
Powered air surface
Weight-based pressure redistribution
Functions

• Does everything a BLUE mattress does
• Full chair position available

• Vibration/Percussion function with low, medium, high power + change duration of time (look for lung icon on right-hand menu)
CPR Lever: Flattens and hardens the mattress for CPR look for the lever below the mattress).
For patients who …
• … are immobile, unable to T&P independently
• For burns, flaps, grafts, burns/pressure injuries on TWO turning surfaces/extensive Stage 4 on buttocks/severe contractures
Fluid-like environment
Pressure redistribution surface pushes air through millions of tiny beads, creating a fluid-like environment
For patients who …
• … are unable to T&P independently
• … are up to 500 lbs
Powered air surface (at end of bed)
Functions
Functions

• Does everything a BLUE mattress does
• Allows provider to modify temperature on bed to control skin’s microclimate
• Max weight: 320 lbs

*ENVELLA NOT READILY AVAILABLE: Will need to be requested for rent.
• Does everything a PROGRESSA ICU mattress does
• Able to adjust width size of bed from 40" to 50"
• … are infants and are immobile/unable to T&P
• Must document use of Z-Flo in “Comfort” under “Daily Care and Safety” to count as pressure redistribution surface
• Crib with NO Z-Flo and AT-RISK patient = not an appropriate surface
• Crib with Z-Flo and AT-RISK patient = appropriate surface
Image Functions/What to know

• Acts as pressure redistribution for infants, but babies will still need to be turned
• Not affected by gravity/resistant to flattening/heating
• Can be used for microturns

When do I place a wound care consult?
• Validate a pressure injury (known or unsure)
— this is especially important if the patient came from outside of the hospital or a different unit.
• Need for wound care recommendations
• Chronic wound or poor wound healing
How do I place a wound care consult?
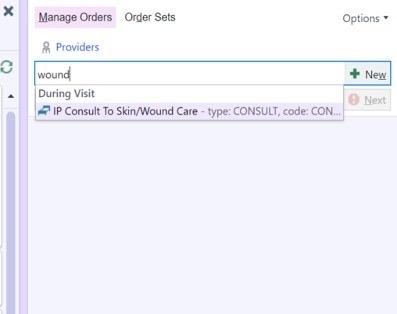
1. Go to your “Orders” tab in Epic. A sidebar should appear allowing you to place and sign orders
2. Type “wound” into the search bar; click on “IP Consult To Skin/Wound Care”
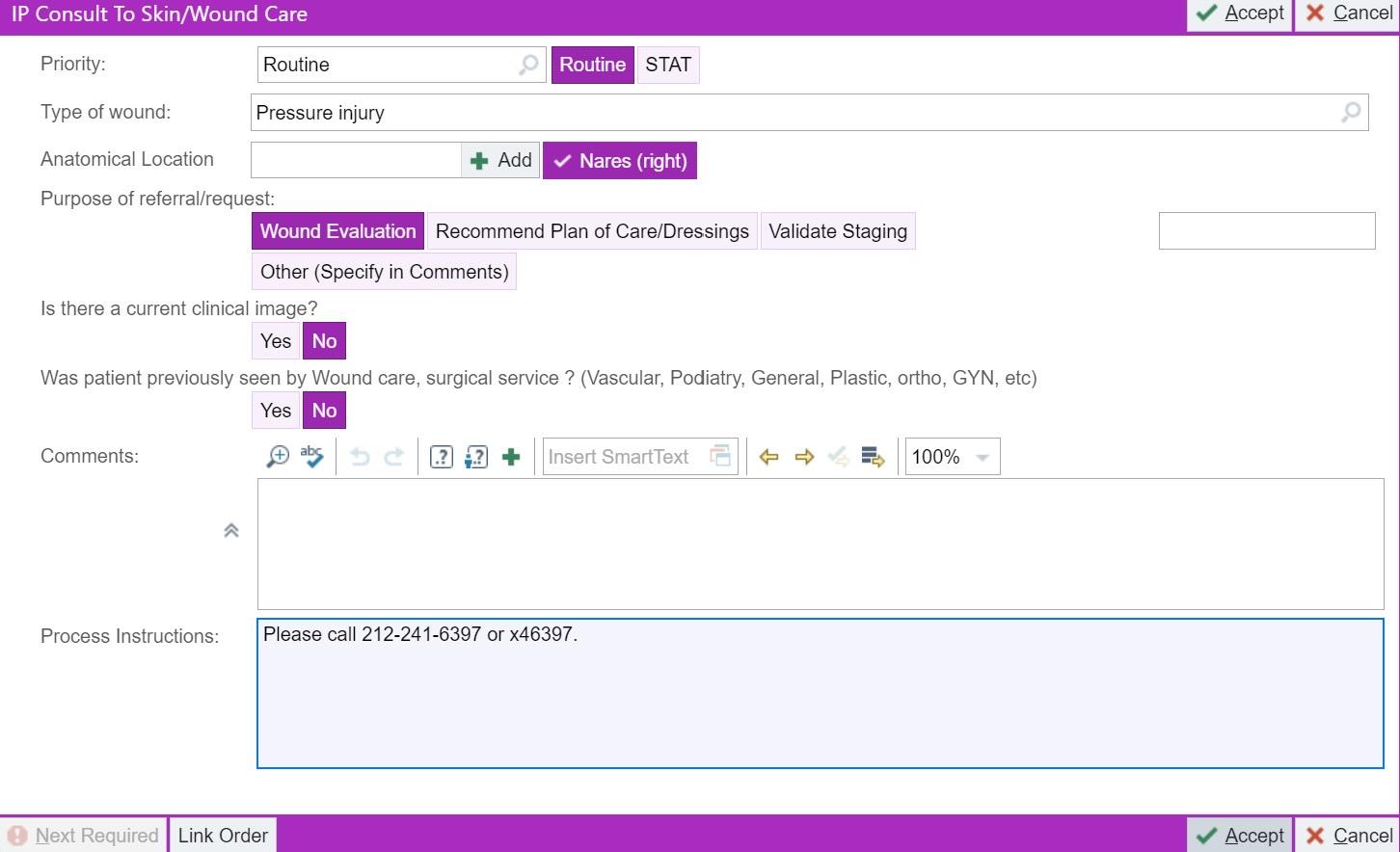
3. A pop-up box will appear. Choose the best option for the following:
a) Type of wound (e.g., pressure injury, skin tear, etc.)
b) Anatomical location (if “Other,” indicate where in “Comments”)
c) Purpose of request
4. Answer remaining questions based on your specific situation.
Optional: Leave a comment if you want to further describe the location/wound.
5. Click “Accept.”
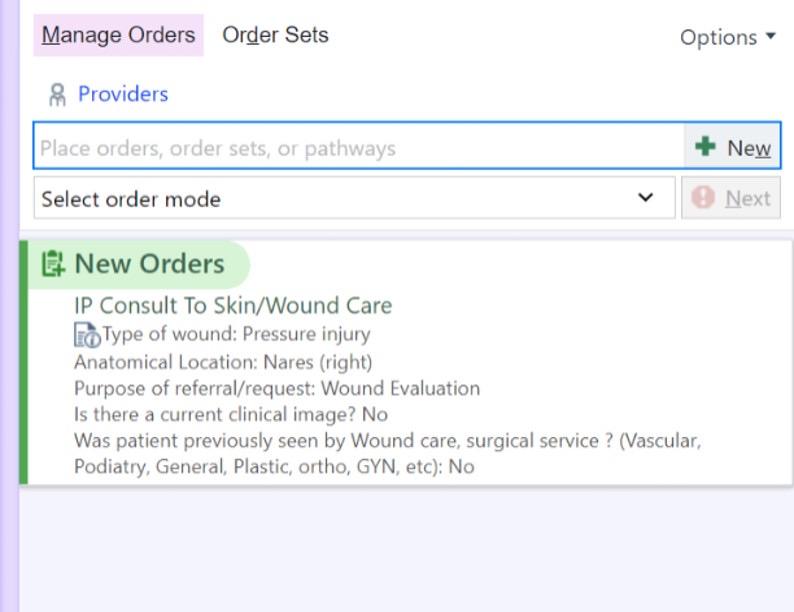

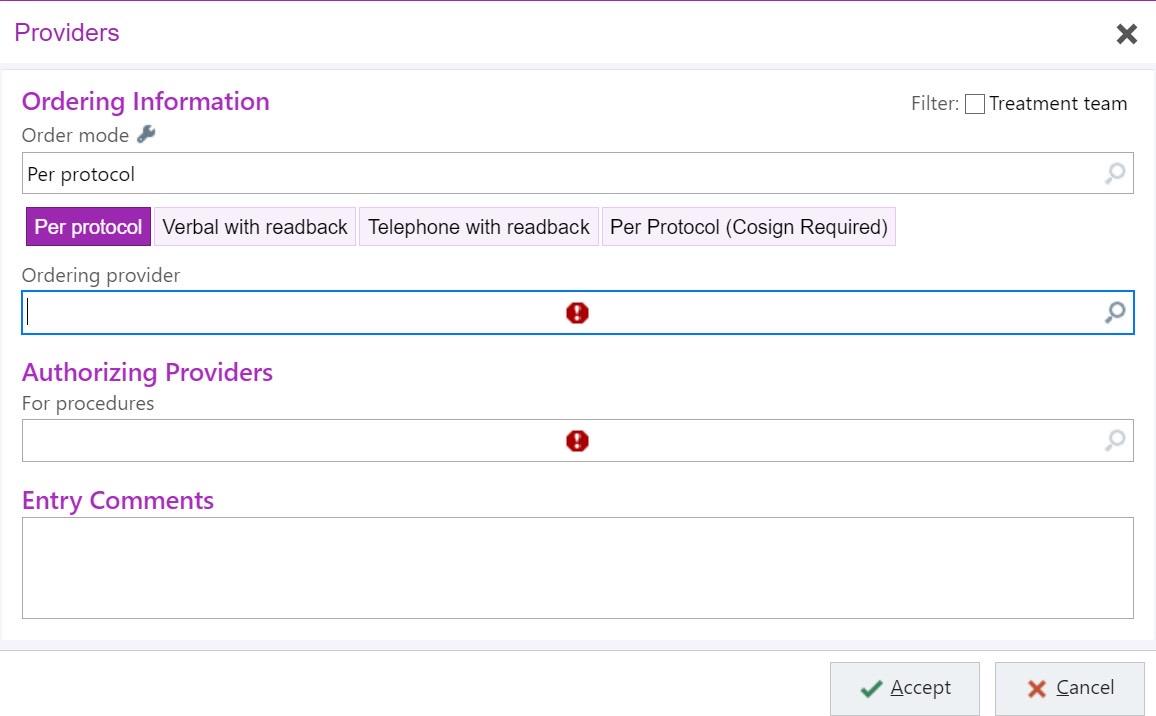
8. Search for your name under “Ordering Provider.” 9. Search for the patient’s current frontline provider under “Authorizing Providers.”
Patient care team identifies pressure injury
Patient care team consults WOCN
Patient care team implements action plan and/or consults additional team (i.e., surgical team)
Consulting WOCN validates HAPI
Any provider can enter a consult, including nursing
Improvement pathway begins
Serious HAPI?
(Stage 3, 4, and unstageable)
Patient care team enters nursing communication order with action plan
WOCN enters validated HAPI into RedCAP NO
YES
WOCN enters validated HAPI into RedCAP
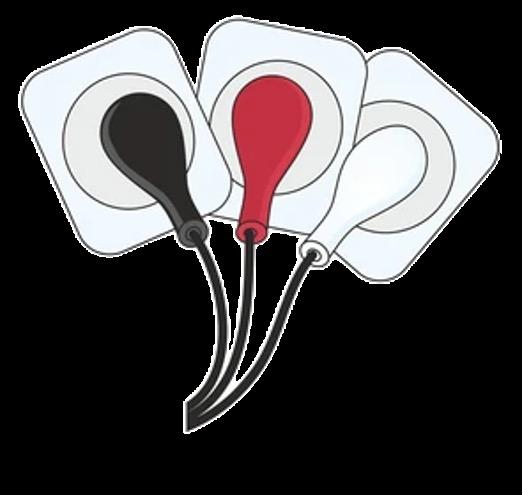
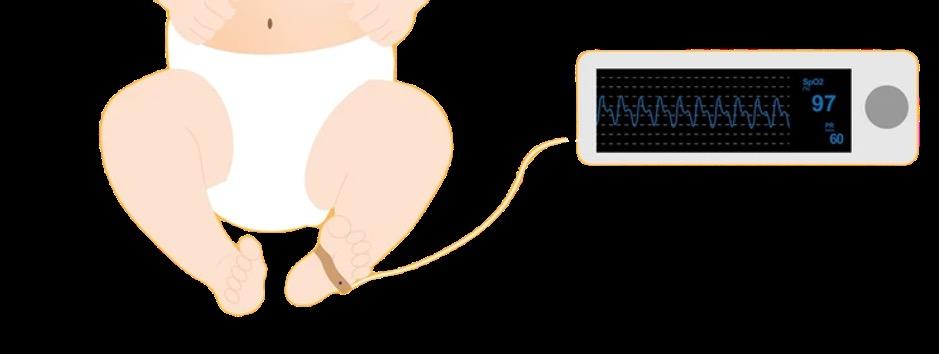
How often do you need to rotate EKG leads and pulse oximeter?
The EKG leads should be changed and rotated at least every 12 hours (every shift). The location of the pulse ox should be rotated every 6 hours; if you’re in the NICU, coordinate with care times (i.e., 8 am, 2 pm, 8 pm, 2 am).
Which wounds can shift RNs place as an LDA?
Any wound or pressure injury can be entered as an LDA in the patient’s EMR by the shift RN.
• MSHS-147: Pressure Injury Prevention in the Pediatric and Neonatal Population
• PED-GEN-06: Skin Safety During EEG Procedure
• PED-38: Tracheostomy Care in the Pediatric Population
• NICU-59: Skin Care
• NICU-11: Bubble CPAP
• NICU-21: Noninvasive Continuous Positive Airway Pressure (CPAP): Care and Maintenance
• NICU-34: Incubator Humidity Settings and Care for the Premature Infant
• MSHS-141: Pressure Injury/Wound Management: Prevention and Treatment for Adults
• MSHS-139: Photographing Wounds and Pressure Injuries
• NU-113: Bed Preparation, Linen, and Supplies
• NU-269: Bed Rental, Specialty
