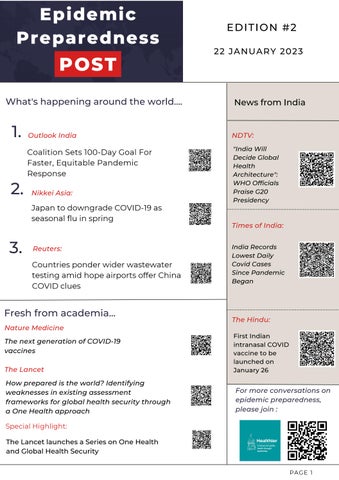
News from India
Outlook India
Coalition Sets 100-Day Goal For Faster, Equitable Pandemic Response
Nikkei Asia:
Japan to downgrade COVID-19 as seasonal flu in spring
Reuters:
Countries ponder wider wastewater testing amid hope airports offer China COVID clues
Fresh from academia...
Nature Medicine
The next generation of COVID-19 vaccines
The Lancet
How prepared is the world? Identifying weaknesses in existing assessment frameworks for global health security through a One Health approach
Special Highlight:
The Lancet launches a Series on One Health and Global Health Security

"India Will Decide Global Health Architecture": WHO Officials Praise G20 Presidency
Times of India:
NDTV: India Records Lowest Daily Covid Cases Since Pandemic Began
The Hindu: For more conversations on epidemic preparedness, please join :
First Indian intranasal COVID vaccine to be launched on January 26

22 JANUARY 2023 EDITION #2 PAGE 1
What's happening around the world....
1. 2. 3.
Articles from the field:
Holistic Service Delivery approach for Epidemic preparedness
Service delivery is one of the health systems blocks and it plays a crucial role in planning epidemic preparedness. COVID-19 has put the entire world in a situation where each country across the globe has to revisit health service delivery to cope with the pandemic. In India following are a few examples of approaches to revising service delivery in face of an epidemic/pandemic
Triage – Facility-based triage was successfully implemented and suspected or positive patients were categorized as mild, medium, and severe care prompting the change in the line of treatment
Geography-based services – In the face of an epidemic, not all services can be delivered at one facility, hence the services were divided based on geography. The district place was designated as a center to handle medium and severe cases.
Special care for COVID-19 positive based service – In one of the districts of India, one 30 bedded facility was designated as a Maternity Care hospital was COVID-19 positive and all the positive pregnant women were transferred to that facility. They were provided food, medicine, and care during the pandemic
Home-based care – Mild cases of advised to remain at home and a self-care kit provided containing medicines and sanitation consumables. These patients were followed up via tele calling to ascertain their health condition.
But in my view, we can add the following services, when we think of service delivery for epidemic preparedness (#100daysforepidemicpreparedness) to make it holistic. It means taking into consideration every available channel of service delivery and reaching out to everyone affected by the new infection (COVID-19).
In addition to the above efforts, can we involve the following service delivery channels
Pet Care – Pets are adorable and our partners in every aspect of life. So, while planning the services for humans, can we plan the same for our beloved pets; cats, dogs, cattle, and birds, (to name a few)? We can plan the vaccination, special clinics, and treatment center for them. It will help us better fight the epidemic/pandemic.
Indigenous knowledge – Indigenous people have good knowledge, in fact, it is the wisdom they are having on protection from diseases. We can include this, whenever the situation demands.
Cross referral between medical streams – In India, there are different branches of medicine practiced to protect the health of people Namely, Ayurveda, Allopathy, Unani, Homeopathy, Sidhha, Yoga, and Sowa Rigpa, each has their merits that can be used to protect and maintain the health of the people of India. It can be achieved through cross-referral between all these branches.
Tukaram Khandade
Epidemic
Post
Preparedness
EDITION #1 15 JANUARY 2023
Written
Dr
by,
Articles from the field:
Chronic Care Service Delivery during pandemics
While dealing with the #pandemic in the past it was experienced that, during the sudden surge of COVID cases, most of the hospitals were converted into COVID hospitals. The specialists were also diverted towards providing immediate care to the COVID patients. In-person appointments were limited to minimize exposure to the patients. These resulted in the disruption of the services to a chronically ill patient, who requires long-term follow-up and management. A survey conducted by WHO in 134 countries found a compromise in services for chronic care in 44% of countries.
Availability and accessibility of services for patients suffering from chronic illnesses become crucial during the pandemic condition Delays in accessing diagnostic and therapeutic services could lead to an increase in mortality and morbidity in this group A few studies have noted a significant increase in cardiovascular events during the pandemic
The patients with the chronic illness could be:
1 Stable, need to visit the facility for consultation and follow-up on periodic basis - those who are stable on therapy and does not require any active intervention or invasive procedure, may need a few laboratory tests –Remote monitoring of such patients is possible
2 Critically ill, needing frequent active interventions such as dialysis, chemotherapy, surgery etc - These patients require to visit the hospital even during the pandemic
A few insights for the ensuring continuity of services for chronic illnesses during the pandemic:
At national level
- Guidance to the states to identify zone/block-wise facilities for the districts/cities to provide services for chronic illnesses This includes facilities providing primary, secondary and tertiary care services
- A section in the Aarogya Setu app can be added to help citizens locate the nearby hospitals where these services are made available The state can furnish this information at regular intervals
At state level
- Guidance note for ensuring the continuity of the services for chronic illnesses such as issuing MMD - MultiMonth Dispensation (MMD) for stable, compliant patients.
- Strengthening and popularizing telemedicine services.
At the city/district level
- Area/zone/block-wise mapping of the hospitals providing the primary, secondary and tertiary care services for chronic illnesses during the pandemic.
- Develop a communication strategy to generate awareness amongst the citizens regarding the availability of the hospitals providing services for chronic illnesses
- Home delivery of the medicines and sample collection services for laboratory testing – To seek support from the volunteers, faith-based and private organizations.
- Use of electronic devices for the remote monitoring of the vitals (in high resource settings)
Written by, Dr Saurabh Parmar
Epidemic Preparedness Post
EDITION #1 15 JANUARY 2023
Articles from the field:
Pandemic Preparedness and Response Strategy
While PPR is frequently used to connote Performance progress reviews in the management world and polypropylene random in civil engineering and construction, in clinical medicine, the most frequent use of the acronym PPR is Patient Progress Record and for Photo paroxysmal Response which is an indicator of epilepsy in Neurology. In veterinary science, PPR means Peste des Petits Ruminants which is a contagious notifiable viral disease as per World Organization for Animal Health (WOAH) and is also known as Sheep & Goat plague. But in the post-COVID (or in-COVID) world, PPR for #publichealthpersonnel like me has a different connotation. The whole world including the recent G-20 partnership meetings are talking about the new PPR which stands for a pandemic prevention, preparedness, and response strategy that aims to detect, prevent, and respond to potential pandemics
The PPR strategy includes several key elements:
1. Surveillance: Conducting surveillance of potential pandemic threats, such as influenza and other emerging infectious diseases, to detect and respond to outbreaks.
2 Laboratory network: Maintaining a network of laboratories around the world that can test for and confirm cases of pandemic-causing pathogens
3 Risk assessment: Conducting risk assessments of potential pandemic threats to identify and prioritize the most significant risks.
4. Preparedness planning: Developing and implementing preparedness plans, including stockpiling medical supplies and training healthcare workers.
5 Response and coordination: Leading the global response to pandemics, coordinating with other organizations, countries, and partners to provide technical assistance and support
6 Communication : Providing accurate and timely information to the public, governments and partners about the outbreak and its management.
Key stakeholders of the PPR strategy include Governments and International organization like World Bank, WHO, WOAH, USAID, CDC and others who are responsible for implementing and coordinating PPR efforts globally and within countries They also play a key role in funding and supporting PPR efforts Other stakeholders include healthcare providers, local health departments as well as private companies and organizations, such as pharmaceutical companies Academic and research institutions and NGOs like Jhpiego who also play a key role in healthcare capacity enhancement and also Media and Civil society organizations that play a crucial role in disseminating accurate and timely information about pandemics to the public act as necessary stakeholders for PPR as well.
Overall, PPR strategy is based on the principles of being proactive, anticipatory, comprehensive, coherent, and inclusive requiring coordination and cooperation from various sectors of the society
Epidemic
Post
Preparedness
Written
Dr Nochiketa Mohanty
by,
EDITION #1 15 JANUARY 2023
Epidemic Preparedness Post
In low- and middle-income countries (LMICs), technology has been crucial in the fight against epidemics. Technology has enabled governments, health organizations, and communities to plan effectively for and respond to epidemics in many areas, from data collection and analysis to communication and logistics.
Mobile technology is a vital technological enabler for preparation against epidemics A large portion of the population does not have access to conventional healthcare facilities in many low- and middleincome countries (LMICs) Even in isolated and underdeveloped places, it may still use mobile phones This has made it possible for mobile health (mHealth) initiatives to be created, which employ text messages, phone calls, and mobile applications to link individuals to health providers, give health information, and track epidemics. For instance, several nations have implemented a text-based surveillance system that employs mobile devices to gather and examine information on infectious illnesses. The technology notifies health professionals of possible epidemics, enabling them to act swiftly and successfully.
It can be tricky to reach isolated and rural locations in many LMICs, making it difficult to deliver healthcare services to these groups This issue has been resolved by telemedicine, which enables medical experts to diagnose and treat patients while consulting with them remotely Once established, these networks can be used successfully during epidemics. For instance, the government of Mexico created a telemedicine platform to offer remote consultations to residents in rural and isolated locations, which aided in efficient triage.
The use of technology like Geographic Information Systems (GIS) mapping is essential for tracking and limiting the spread of diseases. Asia has seen the use of artificial intelligence (AI) to enhance disease surveillance and outbreak response.
Although technology has numerous advantages in preparing for epidemics, some significant challenges and limitations have been identified during the COVID-19 pandemic While architecting tech-enabled systems for epidemic preparedness, we should consider the following challenges and plan for mitigation.
Has technology enabled the preparation for epidemics?
Digital divide
Data Privacy
Data standardization and interoperability
Communication
Sustainability
Infrastructure and regulatory barriers
Srinivas
EDITION #1 15 JANUARY 2023
Challenges: ·
·
·
·
·
·
Written by,
Balusu Articles from the field:
Tech enabled systems in epidemic preparedness
Articles from the field:
Systems Thinking and Epidemic Preparedness
The theory of change is a method for planning and evaluating the intended impact of a program or initiative. It is a logical framework that outlines the causal linkages between an intervention and the desired outcome.
It usually considers following five components in order to create linkages between planned intervention and desired outcome:
Inputs: The raw materials required (e g money, materials, technical expertise, training, relationships and personnel) by your project in order to deliver activities and achieve the outputs and objectives
Activities: The process or actions taken that will transform inputs and resources into the desired outputs.
Outputs: The direct results of the project activities. All outputs are things that can be achieved during the period of the grant and are linked to the objectives and goals
Outcomes: Specific statements of the benefits that a project or intervention is designed to deliver These should support the goal and be measurable, time-bound and project-specific Many projects have more than one objective.
Impact: The long-term, large-scale challenge that your program will contribute to addressing.
The theory of change is a tool for #planning and #decisionmaking, as well as for evaluating the effectiveness of programs and initiatives It helps organisations and programs to clarify their objectives, design effective strategies, and measure progress
But when it comes to #epidemicpreparedness and program development for complex issues such as #epidemics , is theory of change robust enough of a model to be helpful in program design?
I don’t think that we can use a simple tool like theory of change to design programs for epidemic preparedness. In fact, if we take a lens of epidemic preparedness, linear theory of change - which is a linear and cause-and-effect model - may not even be effective in epidemic preparedness because it assumes that the relationships between different factors are straightforward and predictable However, epidemics are complex systems that involve many interacting factors, including the characteristics of the virus, population density, healthcare infrastructure, and human behaviour. Additionally, the spread of an epidemic can be influenced by both intentional and accidental factors, such as the effectiveness of #publichealth measures, population mobility, and the development of new #variants of the #virus. Linear theory of change may not account for the complex interactions between factors and the potential for unexpected outcomes or feedback loops. It also may not be able to anticipate the ripple effects of interventions and policies on different sectors of society, such as #healthcare, #transportation, and the #economy
So if theory of change is not the best possible tool to design programs for epidemic preparedness, what is the alternative?
I believe systems thinking is a probable solution.
Thakkar
Written
Dr Abhishek
Epidemic Preparedness Post
by,
EDITION #1 15 JANUARY 2023
Articles from the field:
Strengthening Primary Care Provider Competence: A Step towards Increasing Resilience for Future Infectious Disease Outbreaks
Provider Competence is one of the critical determinants to improve Primary Care performance Competence is an overarching capability built on specific competencies, which attributes to improvedquality of service. Global Pharmacy Framework defines competency as the knowledge, skills, attitudes, and behaviors individuals develop through education, training, and work experience. Primary Care is the pillar of the health system that meets 80% of health care needs and acts as the link between the communities and the health service delivery system. Performance of Primary Care Providers (PCP) becomes more requisite during Outbreaks to meet the elevated demand for services due to the addition of outbreak led new cases
Evidence from Ebola Outbreak in Western Africa in 2013 reaffirms the importance of Primary Care towards preparing, responding, and recovering from disease outbreaks. Similarly, in India, the resilient primary health care system enabled Kerala to respond quickly to the Nipah Outbreak in 2018-19. In Surveillance, Diagnosis, Treatment, Prevention, and Control, the Primary Care strategies were foundational. In India, Study reports that only 4% of public PCPs and 6% of private PCPs diagnose the common ailments appropriately Regarding treatment, only 21% of public and 27% of private PCPs treat the patients correctly for the common ailments
Learnings from the infectious disease outbreak, Nipah (2018-19) in Kerala suggests enhancing the providers’ awareness about disease case definition, strengthening infection control, standard operating procedures, and incident management protocol could better arm the PCPs to respond the infectious disease outbreak. The study conducted in Bihar reports that the rural PCPs have poor compliance with recommended case management protocol for COVID – 19.
Based on lessons learned from infectious disease outbreaks worldwide, WHO issued interim guidance on the role of Primary Care in the COVID – 19 response It outlined six critical principles for Primary Care: Maintain Essential Health Services, Identify and Manage Potential Cases, Avert the risk of transmission of infection to Contacts and Healthcare Workers, Enhance Surveillance, Risk Communication, Community Engagement, Provision of COVID –19 Vaccination Services.
Maintaining essential health services is one of the utmost priorities during the outbreak. Segregation of the outbreak-related patients and the patients who need essential health services is vital Triaging, therefore, becomes acritical skill for PCPs in such scenarios Interpersonal Communication (IPCs)skills assume importance for effective delivery of these services, including during triaging
Identification of Cases is one of the key strategies under Primary Care response. Contact tracing is an allimportant skill that is required during an infectious disease outbreak. It includes the understanding of both the Case-definition and Case-identification. Case-identification techniques vary in different settings (household and community contacts, closed settings, healthcare settings, public /shared transport, schools, worship places, and private social events) Case identification may be made through direct interviews with patients – either through telephone or at times by reviewing the list of patients hospitalized in the same ward or sharing the same bathroom (continued on page 8)
Epidemic Preparedness Post
EDITION #1 15 JANUARY 2023
Written
Sanjeev Kumar
by,
Articles from the field:
Strengthening Primary Care Provider Competence: A Step towards Increasing Resilience for Future Infectious Disease Outbreaks
In infectious disease outbreak response strategy, preventing transmission of infection to contacts and healthcare workers is one of the critical steps Infection can spread through the direct or indirect spread of droplets Practices such as hand hygiene, respiratory hygiene, masks, social distancing, quarantine of contacts need to be ensured by PCPs to restrict the spread of infection. Under Institutional Quarantine, standard operating procedures (SOPs), including referral SOPs, infection control measures, and use of Personal Protective Equipment, are essential. For laboratory services, competencies on good practices for sample collection and packaging are also vital.
The Primary Care system plays a significant role in active surveillance through community health workers (CHWs) Based on the case definition, CHWs visits house to house to trace the cases Interpersonal Communication and Use of Personal Protective Equipment are the competencies that matter most during this process
Establishing a trust for outbreak intervention measures among the population, building public awareness and knowledge, and increasing public motivation to participate in Outbreak response are the objectives for risk communication during an outbreak. Identification of key messages and strategies to deliver culturally acceptable messages to the citizen are the key competencies.
Vaccine hesitancy is one of the bolsters that affect Vaccine coverage Tailored communications through local health providers are solutions to all forms of hesitancies, i e , Complacency, convenience, and confidence Primary Care providers’ interpersonal communication skills are the key to delivering tailored messages to reduce vaccine hesitancy.
Conclusion: Primary Care system plays a fundamental role in infectious disease outbreak management. Competency is one of the most significant determinants to drive Primary Care Provider performance. More precisely, for infectious disease outbreak response, Primary Care Providers need to have competencies in Triaging, Interpersonal Communication, Contact Tracing, Infection Control Measures including PPEs, Active Surveillance, Risk Communication, and Provisioning Vaccine Services Telemedicine and other digital interventions further enhance the effectiveness and reach of Primary Care services. Such competencies in the Primary Care Providers boost the Primary Care resilience to respond to future infectious disease outbreaks globally.
Read full article on: https://yoursay.plos.org/2021/08/strengthening-primary-care-provider-competence-a-steptowards-increasing-resilience-for-future-infectious-disease-outbreaks/
Epidemic Preparedness Post
Written
Sanjeev Kumar EDITION #1 15 JANUARY 2023
by,
Please post essays/articles on LinkedIn using #100daysforepidemicpreparedness to get highlight in the newsletter For questions, comments or to submit essays: Please email to: athakkar 2409@gmail com