

INSIDE:
Robot-assisted feeding Northwood, a continuing care provider in Atlantic Canada, has worked with partners to bring feeding robots to the table. They’re helping patients without use of their arms or hands.
Page 4
Traverse Exchange Canada Hospitals in Ontario using MEDITECH have been signing on to the Traverse Exchange to connect with other hospitals and nursing homes. We report on experience.
Page 10
Powering cancer imaging
Lawson researchers, in London, Ontario, received a major boost with $7.2 million in funding to fuel new ways of investigating cancer and Alzheimer’s disease. The researchers will work with partners on advanced molecular imaging and theranostics.
Page 13

Canada hosts its first global Connectathon
Toronto became the first Canadian city to hold an international healthcare IT Connectathon, which tests and advances standards for interoperability among health IT systems. Hosted by Infoway, it was attended by digital health leaders and innovators. Pictured above are Souleymane Thiam, session manager at Kereval, and Bo Yang, senior solutions architect at Canada Health Infoway. SEE STORY ON PAGE 6.
Quebec solution helps reduce pressure on EDs
BY NORM TOLLINSKY
uebec’s Ministry of Health and Social Services has found a way to relieve the overcrowding of Emergency Departments (ED) and increase access to primary care. Using Petal Health’s Orchestration Platform, the ministry now has a provincewide, real-time view of primary care appointment availabilities that triage nurses in EDs can fill for non-urgent cases.
By redirecting less urgent patients to other sites, such as nearby walk-in clinics with availability, the EDs are able to focus on more urgent cases.
The ‘magic’ in the Orchestration Platform solution is that it can provide a view of
the available time slots at various clinics, regardless of the scheduling platform used, so that patients can be scheduled for care at another location.
The solution, which went live in 2021, has resulted in 191,000 fewer ED visits and 118,000 more ED visits redirected based on a study by consultants from the Analysis Group that compared ministry data from 2018-2019 with data from 2022-2023.
Using the Orchestration Platform, less urgent ER patients can be redirected to sites with capacity.
The study found that savings attributable to the Orchestration Platform’s improved
access to primary care totalled $73.8 million, said study author and Analysis Group vice-president Marie-Hélène Lafeuille.
Given the full hospital cost of $361 per ED visit and the large number of non-urgent cases that clog EDs – generally estimated to be anywhere between 30 and 50 percent of all visits – the potential savings attributable to the Orchestration Platform are considerable.
“When people aren’t able to find an appointment in primary care, they end up in the ED, so we equipped nurses in triage with access to the system,” said Petal Health CEO Patrice Gilbert. “When someone shows up in the ED and they’re not feeling well but it’s a non-urgent case, the triage nurse will offer
Quebec solution helps reduce pressure on emergency departments
them an available appointment at a nearby clinic or pharmacy.
The Orchestration Platform is connected to the scheduling systems in EMRs at more than 900 clinics across Quebec and results in the redirection of between 700 and 900 patients per day to primary care.
Prior to the introduction of the solution, redirections from hospital EDs were at a very low volume and based on one-off agreements between a particular hospital and a nearby clinic. “To do it at scale, you need access to a tech system with all the data,” said Gilbert.
The availabilities in primary care can be cancelled appointments or unfilled time slots a family doctor reserves for emergencies, so the Orchestration Platform fills holes and optimizes physician schedules.
A physician may reserve time slots between 1 to 3 pm for emergencies, but if it’s 11 a.m. and they’re unfilled, the physician can release them to the platform.
Triage nurses will attempt to book unrostered patients with the same doctor or clinic for repeat visits to ensure continuity
of care but will book with another primary care provider if necessary.
Family doctors are paid more for appointments made through the platform based on an agreement negotiated with the ministry.
“Quebec is the first jurisdiction in Canada to have real-time data on available appointments in primary care provincewide,” said Gilbert. This allows the ministry to see the demand and supply for primary care appointments by municipality or region.
“Last year, minister of Health and Social Services Christian Dubé was in our office and was blown away when we showed him all the data,” said Gilbert.
By clicking on Montreal or Laval, for example, he was able to see the number of patients who couldn’t be redirected because of a shortage of supply. Armed with this information, the ministry knows where to invest in the healthcare system.
“For example, they can provide shortterm incentives to encourage doctors to relocate to regions of insufficient supply,” said Gilbert.
A major cause of ED overcrowding


stems from the shortage of primary care clinicians and the high number of patients without a family doctor or nurse practitioner. In Quebec, two million patients are unattached and largely responsible for the pressure on ED services.
The ministry also has an online Primary Care Access Point service that Quebecers without a family doctor or nurse practitioner can use to find an appointment.
They can either call 811 and speak with an agent to find a resource to help them with their health needs or fill out an online form that uses AI to direct them to a health-
care resource based on their symptoms. For a simple, rash, for example, it may direct them to a pharmacy. If an appointment with a family doctor of nurse practitioner is necessary, the agent will use the Orchestration Platform to find an appointment.
The ministry sent letters to Quebecers registered on the waiting list for family doctors promoting the Primary Care Access Point service, or GAP, an acronym for its name in French – Guichet d’accès à la première ligne.
Another online ministry service called Rendez-vous Santé Québec, helps Quebecers make an appointment with their family doctor. If their doctor is booked up or otherwise unavailable, the system lets them book an appointment with another healthcare professional at their clinic or a healthcare professional practising at another clinic in the patient’s community.
The system is integrated with Petal Health and allows patients to browse the calendar, enter their reason for the consult and select an available date and time. The system directs them to their family doctor’s schedule based on their health insurance card number.
Asked about media reports of Montreal EDs at over 200 per cent capacity in early January this year, Gilbert explained that it’s an anomaly related to the Christmas and New Year’s holidays.
Issue DateFeature ReportFocus Report
April Mobile SolutionsArtificial Intelligence
May EHR / EMR TrendsPrecision Medicine
June/July IT Resource GuidePoint-of-Care Systems
September Community CareStart-ups
October Virtual CarePhysician IT
Nov/Dec AI/AnalyticsCardiology
For advertising or editorial inquiries, contact Jerry Zeidenberg, Publisher, jerryz@canhealth.com
Coming up in 2025 www.canhealth.com

Publisher & Editor
Jerry Zeidenberg jerryz@canhealth.com
Doctors take time off like everyone else and people get sick, he said, so rostered patients can’t get appointments to see their family doctors and triage nurses in EDs can’t redirect non-urgent cases if there are no available time slots in the Orchestration Platform.
The study, which was sponsored and paid for by Petal Health but independently executed by the authors, identified several additional benefits of the solution, said Lafeuille. With less congestion in EDs, patients requiring urgent care experience reduced wait times and there is less risk of infection. Also, with easier access to primary care, patient health concerns can be addressed earlier, resulting in fewer hospitalizations and shorter hospital stays. In the ED itself, less congestion results in improved efficiency and higher levels of staff satisfaction.
For patients and the economy as a whole, there’s an impact on productivity if a patient can see a family doctor or nurse practitioner in a few hours instead of waiting 18 hours in the ED and taking a whole day off work, said Lafeuille.
With the value of the Orchestration Platform confirmed by Lafeuille’s study, Petal Health hopes to bring the solution to the rest of the country and has already had discussions with B.C., New Brunswick, Nova Scotia, Ontario and Alberta.
Contributing Editors
Dianne Craig dcraigcreative@yahoo.ca
Art Director
Walter Caniparoli art@canhealth.com
Dianne Daniel dianne.l.daniel@gmail.com
Address all correspondence to Canadian Healthcare Technology, 1118 Centre Street, Suite 204, Thornhill ON L4J 7R9 Canada. Telephone: (905) 709-2330. Fax: (905) 709-2258. Internet: www.canhealth.com. E-mail: info2@canhealth.com. Canadian Healthcare Technology will publish eight issues in 2025. Feature schedule and advertising kits available upon request. Canadian Healthcare Technology is sent free of charge to physicians and managers in hospitals, clinics and nursing homes. All others: $67.80 per year ($60 + $7.80 HST). Registration number 899059430 RT. ©2025 by Canadian Healthcare Technology. The content of Canadian Healthcare Technology is subject to copyright. Reproduction in whole or in part without prior written permission is strictly prohibited. Send all requests for permission to Jerry Zeidenberg, Publisher. Publications Mail Agreement No. 40018238. Return undeliverable Canadian addresses to Canadian Healthcare Technology, 1118 Centre Street, Suite 204, Thornhill ON L4J 7R9. E-mail: jerryz@canhealth.com. ISSN 1486-7133
Office Manager Neil Zeidenberg neilz@canhealth.com
Dr. Sunny Malhotra Twitter: @drsunnymalhotra
Norm Tollinsky tollinskyn@gmail.com Funded by the Government of Canada
Digital Media Specialist
Rebecca Downer rebecca@canhealth.com
Patrice Gilbert Marie-Hélène Lafeuille
high-osmolar CM (HOCM)...
CM (LOCM)... Omnipaque (Iohexol)


Imaging agents from GE HealthCare The Imaging Company for Imaging Experts
CM (IOCM)Cardiac Safety Patient Comfort Renal Tolerability Visipaque (iodixanol)
GE HealthCare has a distinguished heritage in contrast media development.1,2 We at Pharmaceutical Diagnostics have been supporting healthcare providers for over 150 years. Today, we’re a global leader in diagnostics, with 110M+ doses of our imaging agents produced globally every year.3



Wide product offering with flexible options



Gluten-free, latex-free & Halal certified Used in more than 100 countries

Over 30 years of clinical excellence
References: 1. Widmark JM. Imaging-related medications: a class overview. Proc (Bayl Univ Med Cent). 2007; 20: 408-17; Greco A, McNamara MT, Lanthiez P, Quay SC, Michelozzi G. Gadodiamide injection: nonionic gadolinium chelate for MR imaging of the brain and spine-phase II-III clinical trial. Radiology. 1990; 176: 451-6; GE HealthCare. This is Pharmaceutical Diagnostics. October 2023.
Restoring mealtime independence: Robotic feeders empower people
BY MICHAEL UHLARIK
For persons without the use of their hands and arms or limited motor control, the simple joy of eating requires assistance from others. A delicious plate of food at your table might as well be a mile away if no one is there to manually feed it to you. Lacking agency over something so fundamental has meaningful impact on a person’s dignity and quality of life.
But innovations and advances in technology are helping to restore independence to people in this situation. Northwood, the largest not-for-profit continuing care provider in Atlantic Canada, has been working with partners in academia and the commercial sector to bring feeding robots to the table with a joint innovation program called SMARTech.
The program was built as a multidisciplinary collective of healthcare professionals, researchers, data scientists and the Northwood community to deliver practical solutions for long term care, by linking policy, technology and clinical practices together.
As the senior care partner, Northwood worked directly with Dr. Susan Kirkland, the principal investigator, professor and head of the Department of Community Health and Epidemiology at Dalhousie University. She also leads the SMARTech team. Searching for assistive technology solutions that apply to continuing care, robotic feeders were identified early on as potentially game-changing and were introduced in February 2023.
“The benefit of robotic feeders is, once a caregiver has set up the device for use,

the resident is in control,” said Gail Giffin, occupational therapist at Northwood Care. “They choose the food they want and the speed at which they eat. There is no need to feel rushed so staff can assist someone else.”
For users, this autonomy while eating provides a dramatic improvement in life quality.
The SMARTech program is funded by Age-Well, the Nova Scotia Innovation Fund and Northwood, which has been investigating and implementing innovations in assisted living. The Northwood Innovation team is an in-house laboratory that explores the ways that technology can be adapted for continuing care needs. Last
year it completed a research program that took off the-shelf products and repurposed them to control lights, curtains, and other elements of assisted living facilities.
For Jacklyn, a Northwood resident for eight years, using the robot has made mealtimes altogether more pleasurable. She has enough upper body movement to use her Obi, an American feeder robot, via two control switches under each of her elbows. When Jacklyn shrugs, she can command the Obi to select one of four dishes on her plate, scoop up food and bring it to her mouth.
For persons requiring a different interface, Northwood introduced the fully voice-controlled Neater Eater. For one
Northwood resident, his Bluetooth-enabled robot can pair to any phone or tablet, or accept commands natively using a built-in display.
He now enjoys eating in the privacy of his room while watching documentaries on TV. The feeder robot means that he has the power to eat alone whenever he feels like it.
The robots have multiple cutlery attachments, like spoons, forks and sporks, and can be trained and set up to adjust for different individuals and food types, depending on the model. Plates and bowls can be switched out easily, and both are remarkably portable and easy to clean. The downside is cost, with prices ranging between $8,000 and $12,000 per unit.
For a leading large care organization like Northwood this is a manageable expense, but for individuals living on fixed or limited incomes it can be prohibitive.
“We’ve introduced innovations in longterm care for decades, so we know how steep the adoption curve can be,” said Northwood CEO Charbel Daniel. “We expect that as the rollout of new SMARTech devices continues and more data is captured through increased use, they will not only get more capable but more efficient and less costly.
“There are encouraging signs that artificial intelligence is going to make strong contributions in this field.”
Data-driven insights are also subject of this year’s annual Northwood Research Symposium in June, where the keynote presentation will focus on the role of artificial intelligence in continuing care. “Innovation and research are two of our six strategic pillars,” said Charbel.
SE Health develops programs to transition patients from hospital to home
BY SARAH QUADRI
MARKHAM, ONT. – SE Health, a national, not-for-profit social enterprise, is a leader in the creation and development of Acute Care Transitions Programs. These programs are designed to deliver exceptional care and service to patients and families, ensuring a focus on continuity of care as they move from hospital to home.
SE Health has partnered with hospitals and community organizations on its Acute Care Transitions Programs since 2015. Today, with over 40 programs across Ontario, SE Health continues to build, scale and evolve, shaping the future of care at home.
“This innovative and integrated model is reinventing how we deliver authentic patient and family-centered care and inspiring our commitment to home care modernization,” said Nancy Lefebre, chief operating officer and senior vicepresident at SE Health.
“Through strong partnerships and an interdisciplinary, flexible care model, we facilitate a safe and seamless transition from hospital to home for our patients and their families. We continue to
enhance and expand this approach every day.”
Acute Care Transitions is an up to 16week, integrated bundled care model that provides a direct path home for patients who have completed acute care treatment but require a complex postacute care plan.
The program connects patients with community-based staff, social support services, primary care, and acute care teams to create personalized care plans that support their transition from hospital to home.
The program offers continuous support, a 24/7 helpline for additional patient and family support, a shared care plan, and the integration of cutting-edge technology that enhances care coordination and promotes self-management.
As part of its commitment to modernizing home care, SE Health has evolved many of its Transitions programs to include Remote Patient Monitoring for eligible patients.
“By integrating RPM into our programs, we are improving patient outcomes, enhancing quality of care, and making it easier for patients to manage their health at home,” said Shelby Fisch, vice president, Telehealth, Acute Care
Partnerships and Rehabilitation Strategy at SE Health.
“For example, patients can monitor their blood pressure and respond to health assessments from the comfort of their home, while our teams provide timely support based on real-time data and escalate to the appropriate level of care as necessary.”
To ensure accessibility, SE Health provides data-enabled tablets to patients

who may not have access to technology or the internet. RPM captures patient biometrics, personalized assessments, and standardized data triggers, allowing secure, real-time communication between care teams. This is particularly valuable in community settings, where healthcare providers often work inde-
pendently but need a connected and collaborative care approach.
“SE Health is truly at the forefront as they continue to evolve this model of care,” said Joshua Liu, CEO and cofounder at SeamlessMD. “We partnered with them to co-design patient pathways tailored to their care model, ensuring patient and family needs come first. This is leading-edge innovation in action, and we are proud to collaborate with SE health as they bring these advancements to life.”
Over 80 percent of patients were able to remain at home once discharged from the program. Moreover, over 22,000 hospital/alternate level of care days were saved, and 94 percent of patients were able to work with their care team to adjust their care as needed
“At SE Health, we go beyond delivering care – we create value-based care solutions that benefit hospitals, patients and communities,” said Kim Utley, SE Health’s clinical director, Health Care Solutions. “Our approach evolves with the healthcare system, continuously pivoting to meet new challenges and opportunities.
“We leverage technology, foster strong hospital relationships, and remain deeply committed to community impact and giving back.”
A robotic feeder gives independence at mealtime to a person without use of their arms or hands.

Unlock Data’s Full Potential with Traverse Exchange Canada


Clinicians save time and reduce cognitive load with meaningful data presented in a digestible format.
Healthcare Organizations increase efficiencies by eliminating redundancies and identifying targeted treatments.
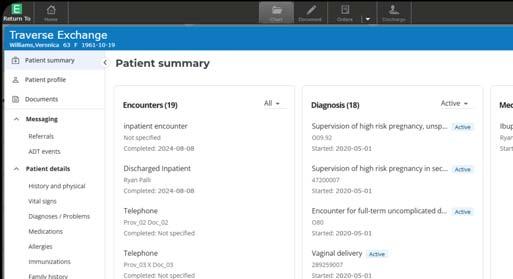

Patients
benefit from more connected, informed care.



Advancing data exchange with Traverse Exchange Canada was just the beginning. In 2025, MEDITECH will further the interoperability network’s impact by delivering a single, high-level view of the data available for a patient across all external data sources within the EHR workflow. This summary transforms fragmented data collected from all participating care networks, provincial assets, and other vendor solutions into meaningful and actionable insights.


International Connectathon aims to improve health IT connectivity
BY JERRY ZEIDENBERG
Writing about Canadian healthcare in the February 7, 2025 edition of the Globe and Mail, columnist Andre Picard states: “Our health information systems are pitiful, marked by a lack of access and interoperability.”
Ouch! To be sure, Canada’s unconnected EMRs and EHRs have driven doctors to exhaustion by forcing them to search for data in countless repositories. They report spending excessive hours looking for computerized information – something that has contributed to physician burnout.
Lately, however, significant advances have been made in connecting various systems so that physicians can quickly find the information they need – including patient histories, test results, allergies and medication records.
On this front, healthcare IT experts gathered in Toronto in February for the annual, international Connectathon – an event that brings teams from around the world to solve the challenge of healthcare IT connectivity. Over 150 interoperability specialists from around the world worked through the week on solving health IT connectivity problems.
The Connectathon – organized by a global body called IHE – has been held annually for 25 years, but this was the first time it was staged in Canada. It’s a sign of the importance Canadians are placing on improving the interoperability of health IT systems.
“We now have an interoperability roadmap – it was announced two years ago by Infoway,” said Attila Farkas, an AI strategy specialist with Canada Health Infoway. He explained that the roadmap shows what’s needed for connectivity but doesn’t mandate participation.
It’s up to the vendors to use standards from the Canadian roadmap, and from international organizations like the IHE. Connectathons and other forums give them the opportunity to pair up and test what they’ve devised.
“We’ve got 26 different vendors represented here on the floor, testing 30 different systems,” said Michael Nussbaum, a wellknown Canadian healthcare IT consultant and a board member of IHE International.
Not only do companies test connectivity solutions at the event, but they’re also vetted by IHE and Infoway representatives to make sure they do indeed function as claimed.
“One of the big things we do is testing,” said Nussbaum. “Interoperability doesn’t mean anything unless you can demonstrate it.”
During the Connectathon, vendors who pass the tests under supervision of IHE monitors are given “seals of approval” for various forms of interoperability. They can then assure their customers that their systems do indeed work as advertised, and that they have earned IHE endorsement.
Participants in the Toronto Connectathon included MEDITECH and Epic, along with software from many other companies that are used by clinicians. Oracle/Cerner, another dominant hospital information system, has regularly participated in previous Connectathons.

And in this age of smart devices, vendors of medical equipment and consumer devices are participating, as well. They want to ensure their gear can integrate with the leading software systems.
A major focus of participants at the Toronto gathering was the International Patient Summary – a synopsis of key patient data, including medications, allergies, problems, immunizations and test results.
The goal is to find a way of extracting this information from various databases that contain it and packaging it in a form that’s easily accessible and transferable.
“People around the world are seeing the importance of the International Patient Summary,” said Nussbaum.
He noted that it was recently used in the annual Hajj, in which 2 million Muslims made the annual pilgrimage to Mecca. These visitors are often elderly, and they’re traveling in the 55-degree heat of Saudi Arabia. When they need medical treatment – such as care for stroke, heart attacks and other emergencies – local hospitals and clinics benefit from access to their histories.
In 2024, a coordinated effort was made to enlist the International Patient Summary, and many of the religious pilgrims participated. Before travelling, they allowed their records to be scanned and represented by a QR code, an innovation that enabled medical authorities in Saudi Arabia to obtain the medical data they needed quickly and easily.
That kind of innovation provides better medical outcomes for patients and makes things easier for medical practitioners. “We’re learning a lot from our international partners,” said Nussbaum. “It’s this kind of innovation that could reduce burnout for physicians in Canada, too.”
For its part, Canada is at work on creating a Canadianized form of the International Patient Summary called the Pan-
ferral and e-consult solutions must break down these walls and talk to each other. It should be noted that other initiatives are occurring across Canada to address the healthcare IT connectivity gap.
Project AMPLIFI, in Ontario, is connecting the IT systems of nursing homes to hospital EHRs, enabling data to be transmitted much more easily when patients are transferred from LTC to hospital and back again.
Funded by the Ontario Ministry of Health, the initiative was launched in a pilot project that connected the PointClickCare system used by St. Joseph’s Villa, a nursing home in Dundas, Ont., with St. Joseph’s Healthcare Hamilton, which uses Epic.
The pilot was so successful that Ontario quickly gave the green light to roll out the solution across the province. Since then, the project has expanded to include many nursing homes using PointClickCare and hospitals running on Epic, Oracle and MEDITECH.
Meanwhile, the major hospital vendors – Epic, Oracle and MEDITECH – have created their own interoperability initiatives in Canada. They’re enabling these formerly disparate systems to communicate with each other.
Canadian Patient Summary (PS-CA), which was tested by health IT vendors at the Toronto gathering.
“Several jurisdictions are already implementing it, and New Brunswick is one of the leaders,” said Farkas. He noted that New Brunswick’s Ministry of Health, in partnership with a Canadian company called VeroSource, have recently created and deployed the PS-CA.
The benefit? It’s portable and patients can carry the code with them as they travel to different care providers within the
European countries are driving many of the advances in interoperability, and North Americans are watching closely.
province. The long-term goal is to enable its use across other provinces and even internationally.
Still, it’s not so easy to create these solutions, as various sessions held during the Connectathon showed. At one of them, a speaker was asked how to be sure the data contained in the IPS is correct and hasn’t been tampered with.
“These are real-world problems,” said Farkas. “You must make sure the solutions are secure and trustworthy. We’re brainstorming to come up with solutions.”
Another major stream of the conference consisted of work on e-referral and econsult systems. Referrals and consultations with specialists are often mired in telephone calls and even fax transmissions. The goal now is to create closed-loop, electronic systems that quickly communicate between GPs and specialists and which also keep patients informed.
A challenge is that doctors in clinics and hospitals use a variety of systems. The e-re-
One of the benefits of the Connectathon is that it’s international, and Canadians can learn from the experiences of countries around the globe. Farkas asserted that European countries are at the leading-edge of the International Patient Summary. “They’re driving much of what’s happening. We’re watching them very closely.”
Representatives of European nations were at the Toronto event, including a speaker from Austria. The next Connectathon, coincidentally, will be held in Vienna.
Blanda Helena de Mello, a representative from Brazil, noted in a presentation that connectivity efforts using the FHIR standard have improved health IT connectivity across the country – especially in the past five years. And while different Brazilian states and municipalities may use differing medical vocabularies, software has been deployed to “translate and understand” so that everyone speaks a common language, she said.
Daniel Doane, a consultant with the Pan American Health Organization, discussed an initiative to create interoperable health IT in countries connected by the highway that runs from Alaska to Argentina. Called the ‘Pan-American Highway for Health’, the project launched last October with 12 countries but hopes to expand to 35.
The idea is to deploy common standards so that health data can be shared more easily. One of its first projects is a Yellow Fever Digital Vaccine Certificate, and the group intends to make forays into cross-border telehealth. “The IPS is important for this,” said Doane.
What’s on the minds of the participants is migrant health, with thousands of people on the move each year throughout the Americas. Doane said PAHO’s efforts will be modeled on the European health experience, as much as possible. Doane quipped that his group has borrowed its theme song from AC/DC’s popular “Highway to Hell” and recast it as the “Highway to Health”.
Robert Hausam, consultant (standing) and Matt Blackmon, a manager at the Sequoia Project, in Toronto.






























Boosting our efforts for a sustainable future
























At Siemens Healthineers, our sustainability strategy is deeply rooted in the needs and priorities of our stakeholders, organized into three core pillars Healthcare Access, Resource Preservation, and Diverse and Engaged Healthineers and supported by two cross-cutting enablers Volunteering and Employee-led Initiatives, and Global and Regional Partnerships. Together, these pillars and enablers leverage our foundation of innovation and robust governance, aligning seamlessly with broader organizational objectives under Strategy 2025.

Healthcare Access
3.3 billion patient touchpoints worldwide by 2030
6 million hours of training provided by 2030

Resource Preservation
90% reduction of Scope 1 and 2 emissions reduction by 2030
28% reduction of Scope 3 emissions reduction by 2030
Scan to learn more or visit: siemens-healthineers. com/en-ca/sustainability



















Diverse and Engaged Healthineers
Named as Best Workplaces in Canada, Best Workplaces with Most Trusted Executive Teams and Best Workplaces for Women by Great Place To Work® in 2024
30% women representation in senior management roles by 2025







Heart failure patient recovers at home thanks to Canadian first at HHS
BY LISE DIEBEL
It felt like an elephant was sitting on my chest.” That’s how Hamilton resident Peg Kelly describes chest pressure she experienced one night in December, during the holidays. Kelly has been living with heart failure (HF) for 10 years and recognized the seriousness of her symptoms.
“I couldn’t breathe when I tried lying down in bed. I was sitting up all night long, trying to breathe better, and I felt dizzy and faint. I knew something was very wrong, because these were the same symptoms I had 10 years ago when my heart problems started,” she said.
Kelly visited the emergency department at Hamilton Health Sciences (HHS) Hamilton General Hospital and was admitted for three days, until she was well enough to return home. While in the hospital, she was invited to take part in a new remote home monitoring program launched by HHS for patients living with HF and chronic obstructive pulmonary disease (COPD).
Symptom monitoring program: Thousands of HHS surgical patients recovering at home from their operations have benefited from remote home monitoring since this form of virtual care was introduced several years ago and expanded during the pandemic.
Recently, HHS launched a remote symptom monitoring program specifically for patients living with HF and COPD. This new program includes nurse practitioners, and is supported by MyChart Care Companion, a feature in Epic, the state-ofthe-art, digital hospital information system launched at HHS in 2022.
Epic is considered among the best hospital information systems in the world and

Iclinical informatics and solutions delivery for Hamilton Health Sciences were instrumental in launching a remote symptom monitoring program for patients discharged from hospital and living with heart failure and chronic obstructive pulmonary disease.
is used internationally by many topranked hospitals. MyChart is Epic’s patient portal that allows patients with a computer, tablet or mobile phone to connect with HHS and access their lab and test results, appointment information, doctors’ consult notes and more.
If this program proves successful, it could be expanded to include patients with other health conditions. The clinical pathways developed through this model could also be shared with other Epic hospitals in Canada resulting in improved patient and health system outcomes.
An area of efficiency could be the elimination of some costs associated with home monitoring equipment while also
streamlining the data collection process.
Developing custom remote monitoring protocols: “MyChart provides integrated clinical pathways for patients with HF and COPD who are discharged from HHS,” said Jennifer Lounsbury, chief nursing information officer for HHS. “This created an opportunity for HHS teams to develop MyChart Care Companion custom remote monitoring protocols and to test drive this approach to care, starting in November 2024, with HF and COPD patient populations.”
Patients are remotely monitored from the comfort of their homes by a team of HHS virtual care nurses and nurse practitioners through a custom program created
by HHS and made possible through the Care Companion platform.
HHS is the first Epic hospital system in Canada to develop a streamlined, remote monitoring system using the integrated Care Companion model. Potential benefits include:
• Improved patient care. For example, patients with HF and COPD rely on their primary care physicians, specialists, home care and other community providers when they return home after being in hospital. Remote symptom monitoring can enhance their care from their home with Care Companion, since with early intervention it’s possible to avoid the worsening of HF and COPD conditions. This can improve patients’ health outcomes, well-being, as well as system outcomes such as reducing emergency department visits and readmissions.
• Health equity and cost savings. By providing patients with hospital-owned kits containing home monitoring equipment, all patients have access to technology and there’s no need to rent this equipment from outside providers.
• A better provider experience for HHS virtual nursing staff and other team members. Since HHS-owned monitoring equipment is integrated with Epic, nurses will not have to manually input data from another source into the Epic system. Integration between home and hospital: Eligible patients with HF and COPD are identified by HHS teams and receive a home monitoring kit consisting of an HHSowned iPad so they can log into MyChart’s health tracking application, said Prathiba Harsha, HHS interim director of clinical informatics and solutions delivery. Kits also include an HHS-owned blood
Interoperability in healthcare: Breaking down silos to improve care
nteroperability in healthcare is essential to delivering high-quality, patient-centered care, especially as healthcare systems become increasingly complex. To explore this critical topic, Stratford Group recently hosted a roundtable discussion with six industry experts:
• Dr. Chandi Chandrasena, chief medical officer at OntarioMD
• Ann Chapman, director of spending and primary care at the Canadian Institute for Health Information (CIHI)
• Rana Chreyh, vice president, and practice leader of digital at Stratford Management Consulting
• Dr. Geetha Mukerji, staff endocrinologist, Department of Medicine, and corporate medical information officer at Women’s College Hospital
• Steve Sagodi, chief technology officer at Mustimuhw Information Solutions (MIS)
• Shafique Shamji, president and chief executive officer of OCINet
Their diverse perspectives provided valuable insights into interoperability’s meaning, its challenges, and the successes that can inform future efforts.
“Interoperability is key to transforming healthcare delivery into a more cohesive, efficient, and innovative system. Breaking down silos and ensuring information flows seamlessly, securely, and efficiently across touch points is the only way we can move toward achieving better outcomes and delivering high quality care in a more personalized and accessible way,” said Dr. Geetha Mukerji.
Defining interoperability: Interoperability bridges gaps between systems, technologies, and platforms, ensuring critical patient information is accessible to the right people at the right time. Whether for a primary care provider, specialist, First Nations Community Health Nurse, or hospital interdisciplinary team, interoperability enables effective communication across settings, empowering clinicians to make informed decisions, ensuring physicians and other clinicians can focus on patient care and not administrative tasks.
By breaking down data silos, interoperability creates a complete picture of a patient’s history, reducing inefficiencies, redundancies, unnecessary tests, and
medication errors, while improving care quality and collaboration.
Interoperability operates at multiple levels, each representing a step forward in the ability to integrate and utilize healthcare data. At a foundational level, it may be as simple as accessing a PDF of a patient’s record from another organization.
Structural interoperability relies on standardized formats like FHIR to align and integrate data across systems effec-
Stratford Group recently hosted a roundtable discussion on interoperability with six industry experts.
tively. The next step, semantic interoperability, will allow us to infer meaning from unstructured or diverse data formats, making it actionable.
“The technology to achieve interoperability already exists. The real barriers aren’t technical; they’re the fragmented systems and other challenges we’ve discussed – it’s now about addressing the
systemic and structural obstacles standing in the way,” said Rana Chreyh.
Empowering patients through interoperability: From a patient perspective, interoperability ensures continuity of care and empowers individuals to take an active role in managing their health. With improved access to personal health information, patients can better understand their treatments and engage in informed discussions with clinicians.
This ability to connect the pieces of a fragmented healthcare system places patients at the centre of their own care, often becoming a “puzzle maker,” tasked with assembling the complete picture of their health. With interoperability, this burden is reduced, as information flows more freely between primary care health professionals, creating a unified view of the patient’s medical history. This not only improves outcomes but also fosters a more person-centered approach to care.
“Interoperability is more than connecting systems – it’s about connecting people to their own health. By giving patients access to their own health data,
Kelly O’Halloran, director of community and population health services; Jennifer Lounsbury, chief nursing information officer; and Prathiba Harsha, interim director of

MEDITECH’s Traverse Exchange connects Ontario hospitals and LTC
BY JERRY ZEIDENBERG
To help break down the silos of patient data and connect clinicians to the information they need, MEDITECH last year launched Traverse Exchange Canada in Ontario. The network now ties together 43 hospitals using MEDITECH, allowing them to more easily transfer data.
via the Oracle eHub. Connections to hospitals running on Epic have now begun.
What’s more, the system is also connected to over 300 long-term care homes using PointClickCare and all 60 Oracle/Cerner EHR customers in Ontario
“We’re committed to reducing the burden on physicians,” said Mike Cordeiro, senior director of interoperability market and product strategy at MEDITECH. “We want to eliminate data fragmentation barriers.”

Cordeiro emphasized that just connecting clinicians to data isn’t always the solution. It must be done in a way that helps their workflow and doesn’t add to their problems.
“You don’t want to simply give them 30 pages of patient data. You want to provide them with answers to their questions,” he noted.
To this end, MEDITECH has been working with its partners in Ontario to deploy the network in an intelligent way. By using the FHIR (Fast Healthcare Interoperability Standard), they’re able to provide more refined searches and exchanges of data for clinicians.
“By using FHIR, the system is much more searchable,” said Cordeiro. Leveraging this FHIR framework, the company is also working with its partners on complementary AI use cases to support advanced search and clinical summarization features.
One of the Ontario hospitals that’s been using Traverse Exchange Canada network is Southlake Health, which serves northern York Region and southern Simcoe County in Ontario.
Sam Fielding, chief information officer, explained that the hospital joined in 2024 as part of Project AMPLIFI, a provincially funded effort designed to promote interoperability in the healthcare sector. He said hospital clinicians have started to use it, and he sees “a massive amount of potential in it.”
Fielding said most of the traffic on the network has been between the hospital and surrounding nursing homes, as they send patients back and forth.
Most of these nursing homes are using the PointClickCare electronic patient record system, and Traverse Exchange enables data to flow directly from PointClickCare into the hospital’s MEDITECH system and vice versa.
“It wouldn’t be possible without Traverse Exchange Canada,” said Fielding. “Traverse Exchange is the critical infrastructure that sits in the middle. It’s the hub of the data exchange.”
He said that most of the data exchange consists of patient summaries – key information about the patient’s medications, allergies, vaccinations, and problem lists. It’s necessary when patients are transferred from long-term care to hospital or hospital to LTC so that clinicians can make accurate diagnoses.
Fielding said more data is now starting to flow between Southlake and other regional hospitals. Southlake, Oak Valley Health, and Stevenson Memorial Hospital (they share a common MEDITECH instance) have also been working with Mackenzie Health to flow critical patient data between MEDITECH and Epic, connecting hospital patient data across York Region and southern Simcoe County.
“We share a lot of patients and there are a lot of transfers,” said Fielding. “The exchange of data in these cases becomes critical.”
He explained that reports can now be sent digitally between the hospitals – a big change from how things worked until recently. “We used to use fax, or we’d sometimes attach a patient chart and send it with the patient.”
CA:FeX: Building the foundation for healthcare interoperability in Canada
BY JORDAN SCHROECKER
The Canadian FHIR Exchange (CA:FeX), developed by Canada Health Infoway, represents a practical approach. It doesn’t claim to solve all of the challenges of interoperability. Instead, it offers a pragmatic way forward – a shared framework that provides a common language for healthcare systems to communicate more effectively.
This isn’t about fixing everything overnight. It’s about making meaningful progress that lasts. Finally.
Why interoperability remains critical: Interoperability isn’t just a technical hurdle – it has real human consequences. Patients may need to waste time and resources redoing tests, explaining the same symptoms to many doctors. They may also be unable to access critical information from their own records.
Doctors are spending precious time searching for test results buried in isolated systems or navigating disjointed systems. Piecemeal solutions often solve one problem but introduce another, perpetuating inefficiency, and wasting hospital and other institutions’ limited time, resources and budget on temporary patches.
Though CA:FeX won’t overcome all obstacles alone, by establishing a common framework it helps ensure that improvements don’t create new barriers.
The goal is a healthcare environment where hospital budgets are maximized for patient benefit, clinicians focus on patient care, and patients focus on getting well, rather than managing digital roadblocks.
Where CA:FeX fits in: CA:FeX departs

from the all-or-nothing approaches we have been pursuing so far. According to Infoway’s 2023 white paper, the Canadian FHIR Exchange Specification (CA:FeX), the framework “reduces the burden of protocols that both vendors and jurisdictions must manage” by offering a predictable, scalable method for health information exchange.
Built on the globally recognized FHIR standard, CA:FeX integrates with both legacy and modern systems.
It doesn’t replace existing tools, or even brand-new tools you want to add. Instead it helps all tools “speak” to each other.
Rather than forcing the adoption of entirely new infrastructures, CA:FeX uses RESTful APIs so organizations can share
modular “resources” – like lab results, prescriptions or patient demographics – incrementally, without overhauling everything at once.
Key features of CA:FeX:
•FHIR profile alignment: Meets or exceeds international standards while respecting uniquely Canadian needs, including jurisdictional autonomy, legislative complexities, privacy and security
•Standardized APIs: Simplifies integration, reducing the need for costly custom interfaces.
•Flexibility for jurisdictions: Supports compliance with diverse legislative and operational requirements.
•Incremental implementation: Enables step-by-step adoption, minimizing disrup-
tion. CA:FeX can provide the foundation that vendors and providers need in order to move towards predictable, repeatable integration patterns that can scale across Canada.
Proving it works: Venuiti’s deployment: CA:FeX’s potential is evident in practice. Consider Venuiti Healthcare’s deployment within a large network serving hundreds of thousands of patients.
Before implementing CA:FeX the network faced common healthcare development challenges, including:
•Complexity: Custom-built interfaces made updates risky.
•Scalability issues: Adding facilities or systems often required costly, time-consuming reconfigurations – sometimes taking weeks or months.
•Data bottlenecks: Fragmented infrastructure slowed patient information flow, forcing IT teams to spend hours troubleshooting.
These problems can be surmounted. By implementing a centralized FHIR server guided by CA:FeX, Venuiti created a standardized, interoperable environment. Data exchange between mobile point-of-care systems and the central EMR improved, errors declined, and expansions became more predictable.
Venuiti’s implementation shows how CA:FeX can serve as a future-focused foundation for any organization seeking to adopt emerging technologies – like AI-driven decision tools – more quickly and at lower cost.
Jordan Schroecker is director of the Venuiti Group of Companies.
Unlocking foundational interoperability in Canada after Bill C-72
BY GURPREET (GP) SINGH
Foundational Interoperability refers to establishing a layer where data is transmitted by one HIT system and received by another. For example, a patient’s hospital records should be accessible to their outpatient practice, and providers should be able to access data from a patient’s wearable device.
Access to this data is crucial for providing comprehensive and timely patient care. Currently, Canada does not have a national network connecting EMR vendors and other clinical data systems across provinces.
This issue was addressed in Bill C-72, the Connected Care for Canadians Act on June 6th, 2024. Parliament recognized the increased mobility of Canadians and healthcare professionals within Canada.
Canada Health Infoway estimates that improved interoperability would save as much as $2.4 billion annually.
Canada’s healthcare system is provincially managed under federal guidelines with significant funding. However, regional service delivery varies, and inconsistent digital health integration creates data exchange gaps.
Challenges such as disparate EHRs, incompatible systems and lack of standardized protocols have led to limited information sharing. A 2020 CIHI report noted progress in some provinces, but highlighted that Canada largely lags in comprehensive, interoperable health information systems.
A significant barrier to healthcare interoperability in Canada is the lack of national standards for health data exchange.
Without proper standardization, healthcare organizations use proprietary solutions that may not be compatible with other systems. This complicates data integration and hinders real-time, accurate decision-making.
Currently, Canada Health Infoway is working through a FHIR implementation guide to define a patient’s profile that EMRs can use for data transfer.
Though standards in the Pan-Canadian Interoperability roadmap are due for finalization in 2027, it will take time for EMRs and other systems to adopt these standards, potentially delaying the implementation of nationwide interoperability.
Potential solutions : There are a few approaches that could be taken to promote nationwide interoperability in several areas:
• HIE (Health Information Exchange):
In this approach, healthcare systems store clinical data in one central location. This makes it easy to access all of a patient’s information from one place. For example, Malaffi, an HIE in the Middle East, uses this method. However, storing large amounts of data for millions of people can be expensive and hard to scale, especially in countries like Canada with a much larger population.

• Network approach without EMPI and RLS: This model uses a network where each healthcare system has a directory of patient data but does not store any demographic details. When a request is made, the system searches for patient data within a specific area (e.g., a 50-mile radius). Carequality in the U.S. uses this method. It doesn’t require long-term storage of patient information, but instead depends on accurate patient matching, with a risk of missing data
outside the search radius.
•Network approach with EMPI and RLS: This approach stores only patient demographics (such as name and address) and uses an EMPI (unique patient identifier) and an RLS (service indicating where a patient’s data is stored). When a request is made, the system locates the patient’s data and sends the request to those locations. CommonWell Health Alliance in the U.S. uses this method. As a result, this approach makes finding patient data easy but requires maintaining the EMPI and RLS systems.
Conclusion: Improving healthcare interoperability in Canada may be challenging but is essential to a high-quality healthcare system that benefits all Canadians. Efficient data exchange will enhance patient care, reduce administrative burdens, and minimize medical errors. All patients will benefit from accurate, timely, and coordinated care.
Gurpreet (GP) Singh, vice president of interoperability solutions at ELLKAY, has over 25 years of experience in healthcare IT. He was instrumental in earning ELLKAY the position of Technical Service Provider for CommonWell Health Alliance and is involved in the Canadian market.
Gurpreet ‘GP’ Singh
INITIO deploys Western Canada’s first GE Omni Legend PET/CT system
VANCOUVER – Initio Medical Group has become the first site in Western Canada to purchase and install the innovative GE HealthCare Omni Legend PET/CT system with cardiac capabilities.
This advanced technology helps to enhance the region’s diagnostic and treatment landscape, particularly in the realm of oncology due to its ability to deliver more than two times the sensitivity of prior GE HealthCare digital scanners, enabling faster total scan times and impressive small lesion detectability.
The addition of the Omni Legend PET/CT will be just the sixth PET/CT scanner in all British Columbia and underscores Initio Medical Group’s commitment to pioneering advancements in nuclear medicine and theranostics.
Nuclear medicine is a specialized field employing small amounts of radioactive materials to diagnose and treat diseases, notably cancer. The technology provides impressive precision in tumor visualization and targeting, essential in the fight against cancer.
Theranostics, an innovative approach combining therapy and diagnostics, is poised to revolutionize personalized cancer care.
This method leverages molecular imaging and targeted treatments to tailor therapy plans to individual patient needs, with the goal of enhancing treatment efficacy while minimizing side effects. Such advancements have the potential to improve the quality of life for patients navigating the daunting cancer landscape.
“As we move forward, it is crucial to re-

member that cancer affects us all,” remarked Mina Bechai, CEO at Initio Medical Group. “By investing in nuclear medicine and theranostics, we invest in brighter futures for countless individuals and families touched by this disease.”
In Canada, access to advanced cancer treatments is limited, with effective therapies often out of reach for many patients who frequently turn to costly alternatives abroad.
Currently, Canada ranks 24th out of 32 OECD countries in the number of PET scanners per capita. Initio Medical Group aims to change this narrative by working
alongside provincial authorities to expand healthcare infrastructure, ensuring cutting-edge diagnostics and treatment options are available to all, regardless of financial situation.
The installation of the Omni Legend PET/CT scanner is a step towards bridging this gap, helping to support the possibility of improved outcomes for cancer patients with access.
“We are proud to see our technology used to improve the experience of clinicians and patients at Initio Medical Group,” said Mike Hamilton, president, GE HealthCare Canada. “With more than
30 years of experience in PET, we remain dedicated to pushing the boundaries of what is possible with molecular imaging, so clinicians have the tools and quantitative data they need to make more confident and accurate diagnoses for their patients in British Columbia.”
Initio Medical Group is at the forefront of advancing cancer care through innovative medical solutions like nuclear medicine and theranostics. Its mission is to bridge gaps in healthcare, working collaboratively with provincial authorities to increase access to life-saving technologies in Canada.
Siemens Healthineers believes in driving sustainable, equitable care
OAKVILLE, ONT. – Siemens Healthineers is committed to more than just advancing medical technology –it is actively working to expand access to healthcare, preserve resources and foster a diverse and engaged workforce. The company’s global sustainability mission is driven by a firm belief in social responsibility and innovation, to reach underserved communities, mitigate environmental impact and create a more inclusive workplace.
“Sustainability is not just a corporate initiative for us – it’s deeply embedded in how we innovate and operate,” said Rene Boyer, senior director, sales and marketing, Diagnostic Imaging, Siemens Healthineers Canada. “Over the past few years, we’ve made remarkable progress in reducing our environmental footprint, optimizing resource efficiency and developing technology that contributes to a more sustainable planet. Our Canadian operations are fully aligned with this vision and we take great pride in implementing tangible measures that make a difference.”
Siemens Healthineers aims to reach 3.3 billion patient touchpoints by 2030 globally, including 1.25 billion in low-
and middle-income countries, using technology and partnerships to close healthcare gaps.
At RSNA 2024, Siemens Healthineers unveiled the expanded MAGNETOM Flow, a highly sustainable MRI platform. The 70 cm bore model features AI-powered image reconstruction, accelerating scans and enhancing quality. DryCool technology cuts helium use from 1,500 to 0.7 litres, reducing costs and conserving resources. Engineered for efficiency, it streamlines workflows and lowers energy consumption.
Additionally, the MAGNETOM Free. platform can now be portably installed in places where MRI was previously not an option. The company’s varied mobile and remote diagnostic solutions, including relocatable MRI solutions like the MAGNETOM Free. platform, bring essential imaging to underserved regions.
“It’s a great way to serve remote populations,” said Boyer. “We’ve been partnering with provinces and healthcare institutions to bring portable MR, CT and mammography to where people live so they don’t have to travel. It’s a new concept, it’s imaging on wheels.”
To further support access to care, the
syngo Virtual Cockpit allows remote experts to assist local technologists in operating imaging systems, ensuring highquality diagnostics in areas with limited healthcare infrastructure.
Boyer noted that the company, together with key stakeholders worldwide, aim to deploy artificial intelligence for remote X-ray scanning. In northern regions where tuberculosis rates are higher, AI adoption could significantly enhance TB diagnosis – an
Siemens Healthineers is working to bring essential imaging, including CT and MRI, to underserved regions.
infectious disease that, despite being preventable and treatable, remains the deadliest globally.
Another key pillar of the company’s sustainability strategy is resource preservation. Siemens Healthineers is committed to reducing healthcare’s 4.4 percent share of global GHG emissions by creating a decarbonized, circular value chain. The company designs upgradable, reusable and recyclable products, with
refurbishment playing a key role. For instance, reusing materials in the MAGNETOM Sola ecosystem cuts 79 percent of material-related emissions.
Efforts extend to energy efficiency, with Siemens Healthineers Canada transitioning its company auto fleet to hybrid with a future goal of becoming fully electric. “We are committed to sustainability at every level,” said Boyer.
On an additional front, Siemens Healthineers fosters a workplace culture that encourages employee engagement and innovation. “Our employees are the driving force behind our success,” said Rene Boyer, “For five consecutive years, Siemens Healthineers Canada has been recognized as a Great Place to Work. This achievement reflects our commitment to fostering an engaging, collaborative and supportive environment where employees can thrive.”
The workforce, including its leadership, are also actively involved in community projects, with employees contributing time to Ronald McDonald House, food banks, Indigenous causes and more. “Our commitment extends beyond the workplace – it’s about strengthening the communities where we live and work,” Boyer emphasized.
The Omni Legend PET/CT scanner delivers more than two times the sensitivity of prior GE systems, enabling faster scans and impressive small lesion detectability.
Groundbreaking Alzheimer’s and cancer studies receive $7.2 million boost
LONDON, ONT. – The quest to advance detection and treatment of Alzheimer’s disease and to personalize cancer care has received a major boost, with $7.2 million in funding to Lawson Research Institute of St. Joseph’s Health Care London for first-of-its kind research.
Lawson scientists will partner with a broad team of researchers at London Health Sciences Centre Research Institute (LHSCRI), McMaster University, University Health Network and BC Cancer on the ground-breaking studies focused on molecular imaging and theranostics as a potential game-changer in detecting and treating neurodegeneration and cancer, particularly prostate, brain and breast cancer.
Principal investigator Ting-Yim Lee, PhD, Lawson’s Director of PET/CT Re-

search, and his team of investigators were awarded $2 million through the Ontario Research Fund – Research Excellence for the study titled Improving Cancer and Alzheimer’s Disease Diagnosis and Treatment Through Cutting-edge Molecular Imaging and Theranostics. Co-principal investigator is radiation oncologist Dr. Glenn Bauman at LHSCRI.
Additional funding from private-sector partners and Lawson, as well as from donors through St. Joseph’s Health Care Foundation, brings the total research investment to $7.2 million.
The research has the potential to offer hope for solutions to some of the most prevalent and pernicious diseases affecting Canadians, Dr. Lee explained.
“Both research projects are the first of their kind in Canada aimed at advancing how we diagnose and treat Alzheimer’s disease and cancer,” he said.
“This collaborative funding initiative will also drive innovation in the exciting field of molecular imaging and theranostics at St. Joseph’s, at the heart of which is St. Joseph’s new, high-sensitivity GE HealthCare Omni Legend 2 PET/CT – the first in Canada.”
The studies encompass the following:
•Alzheimer’s disease: The new PET/CT allows researchers to simultaneously study both blood flow and glucose metabolism in the brain. Both these mechanisms are believed to be contributing factors in the onset of Alzheimer’s.
By measuring both at the same time, the research team hopes to uncover early signs that the brain is in trouble and at risk of plaque deposits and toxic proteins that have been linked to the development of Alzheimer’s.
•Cancer: The cancer study will focus on developing theranostic techniques to achieve personalized dosimetry – a
method used to determine the exact amount of radiation a patient should receive during treatment, based on their individual characteristics. This maximizes effective treatment while minimizing harm to healthy tissues.
Molecular imaging and theranostics is a rapidly emerging field of medicine that combines ultra-precise scans and theranostics (a term that melds the words therapeutics and diagnostics).



Together, they offer a one-two punch by integrating imaging and radiotracers that can identify the location and extent of dis-


eased tissues and selectively destroy the abnormal cells while leaving surrounding healthy cells undamaged.
In collaboration with GE HealthCare, St. Joseph’s is developing Canada’s first GE HealthCare Centre of Excellence in Molecular Imaging and Theranostics.
























Lawson Research Institute’s Ting-Yim Lee, PhD.
Tariff war may harm Canadian exporters, but could spur progress in home market
The Trump administration trade war threatens supply chains and bottom lines.
BY NORM TOLLINSKY
MedTech, the Canadian medical technology association, and its U.S equivalent, AdvaMed, have both taken a stand against the imposition of tariffs on medical technology products as the Trump administration trade war threatens supply chains and bottom lines.
On February 12, MedTech president and CEO Nicole DeKort called on the federal and provincial governments “to ensure that medical devices are excluded from any retaliatory tariffs or sanctions, as the impacts on our healthcare system and patients would be too immense.
“We urge all governments across the country to work with our sector and our healthcare partners to preserve patient care and protect our healthcare systems in Canada by doing whatever we can to keep medical devices out of these potential trade wars,” added DeKort.
And in a February 1 press release, AdvaMed president and CEO Scott Whitaker, said “We shared with the (Trump) administration our concerns about the potential impact of tariffs on the medical technology supply chain that American patients depend on for their care.
“In light of that risk, an exemption was provided for most medical devices during President Trump’s first term with respect to the tariffs on China, and we are advocating for a similar approach this time,” added Whitaker.
According to MedTech, annual exports of Canadian medical technology products to the U.S. are valued at $3.1 billion, while imports from the U.S. are worth $3.4 billion, or 40 percent of total medical technology imports, translating into a trade deficit for Canada.
So far, MedTech has received no “concrete assurances” of an exemption on reciprocal tariffs on US medical goods coming into Canada, “but I think we are being heard,” said Gerry Frenette, MedTech vicepresident for public and member relations.
The sanctions MedTech is concerned about in-
clude threats of banning U.S.-based companies from bidding on procurement opportunities in Canada’s healthcare sector.
“There are situations where there wouldn’t be an alternative product available, so a blanket move to block all U.S.-based medical device companies from providing their products in Canada would be hugely disruptive to the healthcare system,” said Frenette.
MedTech has 120 members, including both Canadian and U.S. based companies doing business in Canada. Supply chain disruptions resulting from Trump’s tariffs and any reciprocal tariffs or sanctions by Canada could affect the availability and price of diagnostic imaging devices, orthopaedic implants, pacemakers, wound care products and thousands of other products used every day to care for Canadian patients.
AdvaMed warns that tariffs on medical technology imports from Canada, Mexico and China would result in higher prices for the U.S. healthcare system


because tariffs are paid by U.S. importers. “Additionally, moving manufacturing from one facility to a different one or new facility requires FDA (Food and Drug Administration) approval, which makes it difficult in the short term to adjust production to the U.S.,” AdvaMed acknowledges.
Trump’s obsession with tariffs is aimed at increasing U.S. manufacturing and reducing or eliminating the U.S. trade deficit, but he’s gambling on the pain of higher prices and rising inflation being offset in the medium to long term by employment gains and increased domestic production.
Frenette is reluctant to predict the impact of a 25
percent tariff on Canadian medical technology companies, explaining: “It would depend on how reliant companies are on U.S. sales. They may be the only provider, so there wouldn’t be an alternative domestic supplier for a U.S. importer, in which case they’d have to absorb the increased cost.”
One company that would be affected by a 25 percent tariff is Toronto-based Medirex Systems Inc., a manufacturer and supplier of hospital wristbands.
Medirex is worried about U.S. tariffs because it recently signed up its first distributor in the U.S. for a wristband product it manufactures domestically, but it’s also concerned about reciprocal tariffs by Canada because it imports products from south of the border.
“During the COVID pandemic, 100 percent of our product came from the U.S. and we realized that made us vulnerable to supply chain disruptions,” said managing director Mark Caskenette.
“For example, the U.S. cancelled hand sanitizer exports to Canada. That’s why Purell hand sanitizer wasn’t available. If you went to a hospital, the Purell dispensers were all empty. That forced the Canadian government to grant licences to distillers to produce hand sanitizer.”
He added, “When we saw this happen, we decided to look at manufacturing wristbands in Canada and doing something unique. We’ve been working on that since COVID and started selling made-in-Canada wristbands domestically within the last year.”
Medirex signed up a distributor in California with hopes to break into the U.S. market.
“They have our samples, and we’re scheduled to go to a show together next month, but I don’t know how our cost structure is going to be affected depending on what happens,” said Caskenette. “We’re also looking at Europe because Canada can’t continue just thinking north-south for trade. We need to start thinking east-west.”
The made-in-Canada product is a direct thermal wristband that uniquely uses a UV coating to minimize exposure for patients and staff to residual chemicals commonly found in thermal paper. The company is also exploring the possibility of manufacturing another type of wristband for laser printers and hopes to have that on the market later this year.
Digital transformation in homecare management
BY AL HAMILTON
Stagnation in approach is no longer an option for care-providing organizations looking to thrive in the dynamic healthcare sector. Patient expectations are rising, and there are significant shifts in their preferred mode of care delivery. For instance, the demand for home-based care is surging and is projected to reach $340.2 billion in the United States by 2027 – we are seeing similar growth in Canada. This growing demand is putting significant pressure on the ability of the healthcare sector
to deliver high-quality services. At the same time, regulatory compliance requirements are also increasing, which organizations must prepare for. How can healthcare organizations efficiently address the dynamic environment with new complexities and heightened expectations?
The answer lies in embracing digital transformation for modern healthcare management. This isn’t just about adopting the latest technology but strategically leveraging healthcare management software to streamline operations, enhance care quality, and ensure long-term sustainability.
In this article, we spotlight how implementing effective healthcare management systems can help you unlock the potential to modernize
Homecare providers can streamline operations and improve delivery using management software.
critical areas such as data management, real-time access to patient information, and comprehensive reporting. Effective software and systems:
• Support efficient data management. Managing patient data effectively is critical for delivering quality, consistent, and compliant care. Disjointed or outdated information often leads to miscommunications, treatment delays or mistakes, and even regulatory non-compliance. When systems are siloed and healthcare setups distributed, ensuring seamless data flow across departments and external partners becomes highly cumbersome. Advanced healthcare management software helps seamlessly consolidate all patient data into a secure, centralized system accessible
Gerry Frenette, MedTech VP Mark Caskenette, Medirex
Canadian healthcare transformation: the power of cloud platform migration
As healthcare organizations continue to grow and innovate, transitioning to cloud-based systems has become a necessity. This transition offers a multitude of benefits. Here are some of the most significant advantages:
Enhanced data accessibility and collaboration: Cloud integration platforms enable seamless access to patient data from anywhere, at any time. This ensures that healthcare providers can collaborate more effectively and make informed decisions based on complete patient histories.
Scalability and flexibility: Cloud-based solutions offer unparalleled scalability, allowing healthcare organizations to adjust their resources dynamically based on demand. This flexibility is essential for managing fluctuating patient loads and seamlessly integrating new technologies.
Cost efficiency: Unlike traditional onpremise systems, cloud migration can significantly reduce IT infrastructure costs.
The pay-as-you-go model means healthcare organizations pay only for the resources they use, saving money and freeing up funds for other priorities.
Improved security and compliance: Leading cloud providers incorporate robust security features, such as encryption, realtime threat detection and multi-factor authentication. These measures safeguard patient data against potential breaches. Additionally, cloud systems simplify compliance with healthcare regulations like PHIPA, ensuring data privacy and integrity.
Innovation and agility: The cloud enables faster deployment of new applications and services, fostering innovation and agility. For example, by implementing AIdriven diagnostic tools, telehealth or virtual care services become faster and more accessible, helping healthcare organizations quickly adapt to evolving industry needs.
Key areas to prioritize for a smooth transition: To ensure patient care remains uninterrupted, healthcare organizations must prioritize the following areas:
•Interoperability: Seamless data exchange across diverse systems is critical. Adhering to healthcare messaging standards such as HL7v2, HL7v3, FHIR, JSON and DICOM is essential for maintaining interoperability, empowering organizations to deliver connected and consistent patient care.
•Data security and privacy: Protecting sensitive patient data should be paramount. Implementing robust security measures and complying with stringent regulations like PHIPA not only safeguards data but also reinforces patient trust in the system.
•System downtime minimization: Transitioning to the cloud requires careful planning to minimize downtime. A wellexecuted strategy ensures critical systems continue operating smoothly, preventing disruptions in patient care.
•Staff training: Shifting to cloud-based systems often requires new workflows and tools. Comprehensive staff training enables healthcare providers to navigate these changes confidently, ensuring a smooth transition.
How Calian supports your cloud integration: Calian’s phased approach to cloud integration ensures healthcare organizations can successfully transition to a cloud platform while minimizing disruptions
and maintaining full compliance. This structured process allows organizations to anticipate challenges, maintain operational excellence and seamlessly adopt innovative solutions.
•Pilot testing with non-critical systems: Before full-scale implementation, Calian
conducts pilot tests with non-critical systems. This controlled environment helps identify and resolve potential issues without impacting patient care.
•Gradual migration of high-priority systems: Calian adopts a phased migration strategy, focusing first on high-priority systems for gradual integration. Breaking the process into manageable stages ensures continuity and minimizes risks.


•Monitoring interoperability performance: Throughout the migration, Calian continuously monitors system performance









When the going gets tough, the tough shouldn’t have to disrupt their workflow to get the information they need.
Introducing the Sync Badge, our next generation hands-free, wearable communication device. With the Sync Badge, care teams can collaborate seamlessly across units and roles. Receive alarms, critical directly.* And see and do the most important

Scan or click to learn more
Quebec steadily expands its use of Hospital at Home to reduce pressure on hospitals
Ontario too has been increasing its treatment and monitoring of home-based patients.
BY DIANNE DANIEL
The notion of ‘going to the hospital’ is evolving to ‘let the medical treatment come to me’ as a growing number of Canadians get used to receiving hospital-level care in the comfort of their own home.
After a slow start compared to countries like Austria, Spain and France, hospital-at-home programs are expanding across this country to ensure continued access to care in the face of staffing and bed shortages, as well as to reduce hospital visits and readmissions.
“We don’t have a healthcare infrastructure that followed the trends of the aging population, but we still have to maintain access and care to that population,” said Erin Cook, director of quality, transformation, evaluation, value, clinical & organizational ethics, and virtual care, at CIUSSS West-Central Montreal, calling the lack of hospital resources an “everywhere problem.”
CIUSSS West-Central Montreal launched its hospital-at-home program – co-created by Cook and CIUSSS West-Central Montreal director of virtual care Dr. Lawrence Rudski – at Quebec’s Jewish General Hospital (JGH) in January 2022.
Following an influx of investment by the Quebec government last year, the program is now live at nine additional sites in the province, with six more expected to ramp up this year.
JGH is supporting the expansion by providing a community of practice framework, outlining details such as the clinical policies and procedures that need to be put in place, how to set up project management, and the types of patient communications that need to happen.
The goal of home hospitalization is to allow people whose clinical condition is considered stable and safe to recover at home, where they receive clinical monitoring, remote health assessment through the use of connected medical devices, follow up of treatments, as well as physical and moral assistance.
to the point that they were at risk of shutting down units and potentially, the whole hospital,” recalled Cook. “They reached out and said, ‘We need help, can you send us nurses?’ We said, ‘We can’t send you nurses, but we can help you with virtual care.’”
The community hospital’s nursing assistants were provided with augmented reality HoloLens smart glasses from Microsoft so they could connect with nurses in the JGH command centre, enabling them to ‘see’ patients and perform assessments from a distance as they coordinated with physicians to ensure orders were carried out and medications were administered.
The same sensors and tablets used in the hospital-at-home program were used to support vital signs monitoring and video communication between care teams.
Over the course of several months, roughly 150 patients were treated in this manner while Hôpital du Suroît simultaneously focused on building and staffing its own virtual care model. Within six months they were live.
“The thing that was extraordinary was that we brought together two completely different establish-
knows what care is available to supplement remote monitoring.
When the onboarding nurse acquires patient consent, it triggers a message to the treating physician. When the physician writes orders, all caregivers are alerted including the pharmacy which goes ahead and fills any prescriptions.
“It’s a sequential handing-off of the ‘rugby ball’ across the entire process,” explained Dr. Rudski, adding that a corporate dashboard in the command centre indicates the trajectory of all patients, showing any time delays or problems.
Another example of an expanding hospital-athome service is Toronto Grace Health Centre’s Remote Care Monitoring (RCM) program, a ‘hub and spoke’ model that coordinates resources between hospitals, community paramedics, primary caregivers and home care agencies, including Ontario Health at Home.
Roughly 20,000 seniors, aged 60 or higher, are now being monitored at home across all regions of Ontario, in addition to smaller patient groups in PEI and B.C. In order to be eligible, people must be identified as either at risk of requiring alternate level of care services during a hospital stay, or at risk of hospitalization or long-term care placement if they are at home.

Involvement in the program is voluntary. Patients are recommended by an attending physician and screened to ensure they meet the criteria for remote monitoring.
They are provided with a smartphone or tablet that contains the necessary apps, plus a SIM card for internet connection, and may also be equipped with a Biobeat sensor for vital signs monitoring. Once at home, they connect to and are closely monitored by virtual care nurses in the JGH command centre.
In addition to supporting the provincial rollout, JGH is also demonstrating a willingness to offer more personalized assistance to Quebec hospitals looking to replicate their virtual care service. Last year, for example, they were approached by Hôpital du Suroît in Salaberry-de-Valleyfield, which was facing a significant labour shortage due to the Quebec government’s recent move to phase out agency nursing in hospitals.
“They were struggling to maintain their resources
ments – a university affiliated hospital with a ton of specialized missions working with a very small community hospital that was struggling just to maintain staffing,” said Cook. “I really think this is a success story of institutions coming together to innovate in times of crisis.”
The command centre model breaks down silos of care, she added, because it facilitates knowledge sharing across departments and teams. Recently, JGH introduced new technology to automate the patient onboarding process for virtual care, giving the command centre a firsthand view of patient status.
Based on clinician feedback, a Microsoft Power App was developed to map the hospital-at-home admission process, which starts with a patient being identified as a candidate.
The home care services available in the patient’s region are automatically displayed so the team
Once admitted to the program by the Toronto Grace intake team, they are provided with a fall pendant offering two-way voice communication and outdoor locating via GPS, and an automated medication dispensing device. Door and motion sensors are also provided for their home, to capture motion and activity in 10-second increments, with the added benefit of being able to identify transfer issues or ‘stuck’ in the bathroom situations, as well as other behavioural and functional changes.
A secure cloud-based Home Health Hub portal is used to collect and report data from remote monitoring devices such as weight scales, oximeters, thermometers and blood pressure cuffs as required. A 24/7 call centre staffed by Toronto Grace responds to all alerts and liaises with other service providers, as required.
Additional services available to RCM clients include a virtual exercise program to strengthen balance and mobility, and a community care program designed to ease the burden of isolation through regular phone or video check-ins handled by trained staff. Through a separate RCM+ program, integrated transitional care is provided to patients identified as ALC or ALC risk, supporting them at home with both remote monitoring and high intensity PSW support for up to 90 days.
The focus now, said Toronto Grace director, integrated transitional care, Danielle Kilby-Lechman, is on building out strong pathways to facilitate client flow using data-driven decision making.
“What we’ve done, is we’ve started as an adjunct to existing hospital-at-home programs, so they can
use our technology and we can monitor the clients 24/7,” said Kilby-Lechman, adding that home care teams can adjust their interventions based on the data supplied by Toronto Grace.
Toronto Grace CEO Jake Tran said the integration piece is the most important aspect of the program when it comes to proactively preventing unnecessary trips to hospital and keeping people safe at home.
A key piece of the RCM program is helping people navigate a complex healthcare system so that they know what services are available and can access the right service at the right time.
“It’s all about using technology that allows us to work with our partners to create integration of care,” said Tran.
Toronto Grace realized early on in its hospital-at-home journey that a cookie cutter approach wouldn’t work. They recognized the importance of standards, but at the same time they knew they had to be mindful of adapting to regional nuances to scale appropriately.
As it expands its holistic program, Toronto Grace is meeting with hospitals, Ontario Health teams and other local care providers to understand their processes. Similarly, they’ve visited their partners in B.C. and PEI to learn how they operate. “We learn their system, look at their needs and align our system with theirs,” said Tran.
Data generated by the RCM program –such as alert data and escalation data – is routinely reported on and patient satisfaction surveys are conducted each month. Kilby-Lechman said feedback is positive, with clients expressing relief that they don’t have to pay, that their family members have peace of mind about their well-being.
“We’ve always tried to customize the program as much as possible and within reason,” she said. “We really adapt to our partners needs and capacities, which I think is important because not every client is the same and not every service provider is the same.”
According to a February 2023 article in the Canadian Medical Association Journal, conventional hospitalization can “inadvertently make older patients sicker as they spend most of their time in bed,” whereas patients receiving hospital-level service at home tend to improve because they keep normal routines.
Dr. Rudski calls it value-based care and said more needs to be done to train physicians to ask what’s best for the patient, what does the patient want?
“Doctors keep being taught about disease processes and how to treat disease,” he said, pointing to distinct benefits that athome patients get such as the ability to stay active which leads to faster recovery.
“They are never taught to ask the patient, ‘What is your goal?’ and their goal is always to get home,” he added.
Both Dr. Rudski and Cook point to a professional education gap that needs to be closed in order to support wider adoption of hospital-at-home programs throughout Canada, including more emphasis on how to read remote patient vital signs, and how to use technology as a complement to in-person care.
They also call for continued integration between traditional lines of hospital and community care as virtual care expands. When JGH initially deployed hospital-at-
home in 2022, for example, Cook said they were challenged to provide their own dedicated team of home care nurses.
She pushed back, citing the need to collaborate with existing agencies and to tap into their knowledge and expertise.
“Anybody who’s going down this transformation towards a hospital-at-home model really has to give thought to not creating another silo in the healthcare system,
but figuring out how this program can be part of the existing clinical entities and missions for the benefit of patients,” she said.
JGH, for example, leveraged its program to support point-of-care testing for influenza A and B, RSV and COVID-19 among the elderly. Seniors were encouraged to phone a dedicated number if they had flu-like symptoms and a home care nurse was sent out to do the testing.
Roughly 160 patients were cared for and only nine ended up in the Emergency department.
While Quebec has made impressive progress in Hospital at Home services, its providers are learning quickly as they go, and ideas about how to deliver care most effectively are evolving. As a result, it is continually refining and developing expertise in this relatively new area.

Patient care with hospital at home programs: a technological perspective
BY KASSAUNDRA MCKNIGHT-YOUNG
In the face of ongoing nursing and clinician challenges, the healthcare industry is exploring innovative solutions to deliver quality care while optimizing resource utilization. One such innovation is the Hospital at Home (HaH) model, which leverages technology to provide hospitallevel care in the comfort of patients’ homes.
This encompasses delivering medical care in a home setting through patient visits, telehealth, remote care coordination and patient monitoring to ensure that recovery is progressing as expected.
Typically, this model involves patients wearing or using devices that track vital signs and other key health indicators. This approach not only helps to alleviate some of the critical resource constraints but, importantly, improves the patient experience, which contributes to patients’ recovery.
In a 2021 study in JAMA, patients with chronic illnesses recovering at home, rather than in a hospital, showed a 26 percent lower risk of long-term care readmission, along with reduced depression and anxiety scores. A different study, by the National Institutes of Health, revealed that delivering care to patients at home can reduce the cost of care by up to 40 percent compared to traditional hospitalization.
The rise of the hospital at home model: At this stage, HaH programs are being offered to patients who need hospitalization but are stable enough to be cared for safely at home.
Examples include primary and secondary care patients, or even tertiary care patients, steadily recovering after a major treatment. This approach reduces the financial burden on healthcare systems and frees up essential hospital beds for more acute cases.
While in certain European countries this approach has been routinely practiced for decades, the HaH trend is rapidly catching up and expanding globally be-

cause of its benefits. This innovative model has been adopted by various countries, each tailoring it to meet their unique healthcare needs and challenges.
A global perspective: In the United States, the HaH model has gained significant traction as healthcare systems strive to reduce costs and enhance patient comfort. Several major health systems have implemented these programs, leveraging technology to monitor patients remotely.
The onset of the COVID-19 pandemic accelerated its adoption, with the Centers for Medicare & Medicaid Services (CMS) offering waivers to broaden its use, highlighting its potential to reshape the healthcare landscape.
Across the Atlantic, the United Kingdom’s National Health Service (NHS) has also experimented with HaH services. These services are particularly useful in alleviating pressure on hospitals during peak seasons, such as winter. By managing
The power of cloud platform migration
to ensure data is seamlessly exchanged between platforms, maintaining the integrity and accessibility of patient information.
•Comprehensive staff training: To ease the transition, Calian provides tailored training programs for healthcare IT teams. This hands-on approach equips teams with the skills to confidently leverage cloud-integrated workflows.
By adopting this phased approach, healthcare organizations can troubleshoot challenges early and refine their interoperability strategies before broader deployment, ensuring operational continuity and quality of care throughout the migration process.
The path forward: Migrating to a cloud integration platform offers numerous benefits for healthcare organizations – from enhanced data accessibility to improved security and cost savings. With Calian’s phased approach, healthcare providers can
navigate this transition seamlessly, ensuring compliance, minimizing disruptions and prioritizing patient care every step of the way.
Take the next step: Ready to take the next step in your interoperability journey? Connect with Calian’s healthcare transformation experts at healthinfo@calian.com for a free
As with other major technological changes, a move to the cloud requires comprehensive staff training.
discovery consultation. Discover how seamless and secure cloud integration migration can be – download our eBook Cloud migration made seamless and secure: a playbook for healthcare integrations.
For more information on our health services and products visit calian.com/health
chronic conditions and post-operative care at home, the NHS aims to reduce bed occupancy and improve patient outcomes.
Meanwhile, in Australia, the concept is well-established under the name Hospital in the Home (HITH). Supported by both public and private healthcare sectors, this model allows patients to receive acute
While hospital at home programs offer benefits, they also produce new challenges in documentation and regulation.
care at home, handling conditions that can be managed outside traditional hospital settings.
In Spain, various regions have embraced programs designed to provide continuity of care for chronic patients and to reduce hospital readmissions. These programs emphasize personalized care, facilitated by home visits and telemedicine, ensuring that patients receive the attention they need without the need for hospital stays.
France offers a similar model known as “hospitalisation à domicile” (HAD), which is widely used for managing chronic diseases, palliative care, and post-surgical recovery. Integrated into the public health system, HAD programs provide comprehensive care at home, showcasing France’s commitment to innovative healthcare solutions.
Canada, too, is exploring the HaH model as a strategy to manage healthcare costs and enhance patient satisfaction. Pilot programs have been initiated in several provinces, focusing on elder care and chronic disease management, as the country seeks to balance quality care with economic efficiency.
Enhancing patient experience - Addressing obstacles with technology: While the HaH model offers numerous benefits, it also presents challenges, particularly in documentation, legal issues, and patient monitoring. However, advancements in healthcare technology are pivotal in overcoming these hurdles.
Experts confirm the importance of
leveraging technological advancements made available in recent years: handheld mobile computers and tablets, such as those provided by Zebra, enable real-time communication and access to Electronic Health Records (EHRs) for both patients and healthcare providers.
These devices facilitate medication administration, telehealth consultations, and remote monitoring, ensuring that patients receive comprehensive care at home. Moreover, the integration of 5G technology addresses connectivity issues, allowing for seamless communication even in areas with limited Wi-Fi access.
Regulatory and reimbursement challenges: Despite technological advancements, regulatory and reimbursement frameworks remain a challenge. While some hospitals in the U.S. and Canada have adopted this model, reimbursement policies have yet to fully align with the intricacies of the approach. Currently, some U.S. healthcare systems continue to classify home-based patients as inpatients to secure necessary reimbursements.
A vision for the future: As healthcare systems strive to do more with less, the HaH model represents a significant shift toward more personalized and efficient care delivery. By leveraging cutting-edge technology, healthcare providers can ensure that patients receive safe, effective, and comfortable care in their own homes.
Technological integration throughout the patient journey – from hospital admission to home recovery – plays a crucial role in supporting this innovative approach to healthcare.
For healthcare IT professionals, the continued development and implementation of technologies like EHR-integrated devices, telehealth platforms, and 5G connectivity are key to overcoming current obstacles and enabling the widespread adoption of HaH programs. As this trend gains momentum, it promises to redefine the landscape of patient care, offering a glimpse into the future of healthcare delivery.
Kassaundra McKnight-Young is Healthcare CNIO Industry Principal, Zebra Technologies.
Interoperability in healthcare:Breaking down silos to improve care
we empower them to actively participate in their care. This is a fundamental shift that delivers immense value to every Canadian,” said Ann Chapman.
Challenges to overcome: Canada faces significant hurdles in achieving healthcare interoperability, including a lack of standardized health data and fragmented digital health systems. Health data remains siloed within EMR systems that were not designed to support modern interoper-
Leaders must work together with robust regulation, legislation and policy to create a framework for interoperability.
ability requirements. As a result, data is often difficult to extract and share. Adding to that is Canada’s decentralized healthcare model, where provinces and territories have developed their own solutions without a coordinated national approach.
While these jurisdiction-specific systems may meet local needs, they lack the compatibility for seamless care across the country, creating barriers for patients who move between regions or require care in multiple locations. Additionally, they force EMR vendors to develop unique interfaces for each province to address the same fundamental needs, adding complexity and inefficiency to the system.
Beyond technical challenges, governance, policy, and resource issues persist. Historically, Canada has operated under a custodial model of data ownership, where data resides with institutions, limiting ac-
Digital transformation
CONTINUED FROM PAGE 14
to authorized personnel in real-time.
This integration enhances efficiency in several aspects, from intake to service delivery management. The result of such centralized electronic health records is reduced manual errors, improved data governance, and increased efficiency –all while maintaining internal and external compliance.
• Unlock real-time mobile access. In fast-paced healthcare environments, timely access to information is vital for effective care-based decision-making. Delays in patient data access, especially in remote and home-based care settings, negatively impact treatment outcomes and staff productivity.
Mobile-enabled healthcare management software empowers care teams to securely access and update patient records from any location. In a hospital, care facility, or home-based care setting, frontline staff can easily access clinical management tools, schedules, and treatment plans in real-time.
This easy accessibility reduces the risk of errors and improves care coordination. Consequently, care decisions are always based on the latest, most accurate information, and care quality and operational efficiency are top-notch.
cess and use. Privacy concerns further complicate efforts to balance security with accessibility.
“Putting data into the right context –identifying the ‘signal’ amidst the ‘noise’ –is one of the greatest challenges to interoperability. Yet, what seems like noise today might become valuable for a future visit, adding complexity to the process. This is where AI could play a pivotal role in sifting through vast amounts of data to extract what’s relevant,” said Shafique Shamji.
Keys to success: Successful interoperability in healthcare requires more than just the ability to exchange information between systems; it demands that the data be meaningful, actionable, and seamlessly integrated into workflows. Bidirectional interoperability is essential, enabling data to flow both ways, from primary care to specialists and back.
Another critical component is managing the sheer volume of data. To avoid information overload, interoperability must promote the exchange of relevant information that enhances care delivery. Additionally, data should be curated for both clinicians and patients in an understandable and empowering way.
“It’s important to recognize the multifactorial nature of interoperability. At the end of the day, it is about patient care and safety. That’s our common goal. If we say the focus is on people/patients, I think everyone can agree to that,” said Dr. Chandi Chandrasena.
Learning from success: The successes we’ve seen so far in interoperability demonstrate that progress is not only possible but scalable. The Sequoia Project in the U.S. has shown how vendors and healthcare organizations can collaborate to
• Streamline appointment scheduling and staff workload management. Efficient appointment scheduling is necessary to ensure patients receive timely care. At the same time, it also helps balance staff workloads effectively to avoid burnout and operational inefficiencies.
On the other hand, poor scheduling often leads to patient dissatisfaction and increased operational costs. According to research from Statista, 46 percent of survey respondents cite access to treatment and/or long waiting times as the biggest problem facing the healthcare system in their country.
Modern healthcare management software solutions simplify this predicament and help expedite appointment scheduling. The software helps to efficiently match patients with the right employees based on skills, availability, and patient needs. The automation also reduces the time required for coordination and enhances the patient experience by ensuring timely appointments.
For leadership, the benefit is twofold: improved staff utilization and a better care experience for patients.
• Simplify financial management. Effective financial management is a cornerstone of long-term success for any healthcare organization. Inefficient financial processes often result in billing errors, delayed payments, and economic instability. Healthcare management software
share a billion records monthly across diverse systems.
This is interoperability at scale, operating with varying technologies and standards. Closer to home, initiatives in Canada have also yielded promising results. Legislation such as the former Bill C72 – The Connected Care for Canadians Act and pan-Canadian initiatives led by CIHI and Canada Health Infoway will define core data and profile specifications, leveraging international standards. OCINet in Ontario collects 1.5 million exams every month and shares over 2.5 million exams across hospitals and clinics every month, seamlessly and in context.
“PrescribeIT has been a major achievement – using the same interface and code base in two provinces without any changes. Being able to turn it on, connect with different pharmacies, and send e-prescriptions seamlessly is, to me, one of the
biggest successes I’ve seen in my career,” said Steve Sagodi.
A call to action: In moving forward with interoperability in healthcare, collaboration across technical, clinical, governmental, and regulatory spheres is essential –strong, accountable leadership must guide these efforts to ensure progress is unified and impactful.
Leadership must work together with robust regulation, legislation, and policy to create the framework for interoperability. Equally important is funding – adequate resources tied to clear, outcome-driven goals will be key to scaling solutions effectively and ensuring they deliver meaningful results.
By adopting the new interoperability data and technical standards developed by CIHI and Infoway that leverages international standards, we can accelerate implementation and achieve a cohesive, interoperable system more efficiently.
Heart failure patient recovers at home
CONTINUED FROM PAGE 8
pressure cuff, a weight scale, a pulse oximeter for measuring blood oxygen levels and pulse, and a thermometer, with results for all the devices automatically entered into the patient’s electronic health record in the Epic system via MyChart.
Kelly O’Halloran, director of community and population health services for HHS, came up with the idea of offering remote home monitoring to HF and COPD patients. She partnered with the informatics team on the development of custom MyChart Care Companion protocols.
provides integrated financial management capabilities to streamline billing, invoicing, accounts receivable/payable, and payroll. Robust tools reduce errors and redundancies by automating routine financial tasks, improving period-end processing and overall cost management. With their support, leadership can access comprehensive reporting to analyze financial performance and make datadriven decisions to maintain financial health and compliance.
• Support comprehensive reporting for better decision-making. In today’s data-
GoldCare’s digital health solutions are built to empower healthcare leaders to modernize workflows.
driven healthcare environment, leadership must make decisions backed by hard facts. Without the support of robust reporting tools, tracking key performance metrics such as patient outcomes, staff efficiency, and compliance can be a struggle and more like shooting arrows in the dark. Healthcare management software provides sophisticated reporting capabilities, turning raw data into instantly actionable insights. The tools enable leaders to monitor care quality, track clinical management metrics, and optimize resource allo-
“I believe patients discharged from hospital can really benefit from remote symptom monitoring overseen by registered nurses and nurse practitioners,” said O’Halloran, who elicited funding support from Ontario Health West/Ontario Health to develop and implement the custom Care Companion protocols.
“We have been fortunate to have the expertise of Dr. Catherine Demers, HHS director of heart function services, Dr. Natya Raghavan, HHS head of the service for respirology, and other clinicians to develop the clinical pathways,” said O’Halloran.
cation. Detailed reports on operational performance also allow the leadership to forecast needs, identify trends, and ensure their organization is prepared to meet internal and external challenges.
Want to transform your healthcare management operations for long-term success?
Maintaining the status quo is no longer an option in an era of rapidly evolving healthcare. By embracing comprehensive healthcare management software, you can move beyond short-term operational fixes to achieve long-term transformation.
The benefits are many, right from improved efficiency to better financial implications – all resulting from state-ofthe-art integrated systems.
GoldCare’s digital health solutions are built to empower healthcare leaders to modernize workflows, improve patient outcomes, and remain compliant with industry regulations. Partner with us to stay agile in response to emerging trends and reap strategic advantages such as easy data-driven decision-making, realtime access to critical information, seamless scheduling, accurate financial management, and much more.
Talk to our experts to find out how we can help you optimize clinical and administrative functions and drive efficiency across the board. Book a GoldCare Demo.
Al Hamilton is the COO of GoldCare.















ONTARIO’S OF THE YEAR


















































































































