

INSIDE:
Group reaches EMRAM 6
A four-hospital partnership in Ontario has hit a significant milestone with the achievement of Stage 6 in the HIMSS EMRAM scale. Now, they’re well on their way to reaching HIMSS EMRAM Stage 7.
Page 4
Using genomics in the EHR Ontario Shores is the first mental health centre in Canada to use pharmacogenomics to routinely prescribe medications to inpatients. It’s facilitated by the use of MEDITECH’s Expanse Genomics solution.
Page 6
Sourcing skilled employees
We interview leaders at two Canadian companies who are hiring certificate-holders from Toronto’s Data Sciences Institute. They are a new source of skilled IT workers. Page 8

Sinai Health tests new robotic surgery application
A team led by Dr. Tim Van Mieghem, maternal fetal medicine specialist at Mount Sinai Hospital, is trialing the state-of-the-art da Vinci Xi robot to perform fetal surgery, aimed at decreasing the adverse effects of spina bifida. This pioneering technology is currently not offered for spina bifida repair in any other clinical setting around the world and could transform the procedure. SEE STORY ON PAGE 15.
OntarioMD highlights the growing use of AI scribes
BY JERRY ZEIDENBERG
MISSISSAUGA, ONT. – Many of the discussions at the annual OntarioMD conference – held in September –focused on AI Scribes for doctors. Seems these newfangled solutions, powered by ChatGPT and other forms of generative AI, actually work! They’re saving doctors who try them hours of administrative toil, as they’ve got the smarts to do a lot on their own.
A new study led by OntarioMD with partners at Women’s College Hospital and the eHealth Centre of Excellence, in Kitchener, Ont., confirmed these benefits. They quickly tested six AI Scribes and then rolled out three of the services to 152 family physicians and nurse practitioners, who worked with them for three months.
“It resulted in a reduction in after-hours documentation time of three hours (per week). That’s an enormous benefit,” commented Dr. Onil Bhattacharyya, director of
the Women’s College Hospital Institute for Health System Solutions and Virtual Care–also known as WHIV.
AI Scribes can listen-in on the encounters between doctors and patients. They automatically write-up draft notes for the encounter, complete with specialized medical terms. Doctors must then review these notes,
The trial showed a reduction of three hours per week of after-hours documentation time.
edit them, and add them to their electronic patient records.
In the three-month test, that process not only saved time, but it also resulted in more complete record-keeping. Dr. Bhattacharyya observed that in his own practice, before deploying an AI scribe, he used to catch up on notes at the end of the day. By 6:45 pm or 7 pm, however, he’d pack it in, so that he
wouldn’t miss seeing his children that night.
“I would plan on finishing the notes later, but what often happened is that months went by without doing this. Now, using an AI Scribe, the notes are complete.”
And by reducing the keystrokes a doctor makes during a patient encounter, AI Scribes are transforming the nature of the meeting– the encounter is more like the days before computers arrived in clinics.
“Doctors are looking at patients again, they’re forming bonds,” said Dr. Bhattacharyya.
Commenting on the time that’s being saved on administrative tasks like recordkeeping, he mentioned that the generative AI systems are restoring work-life balance. “It’s remarkable,” he observed. “Physicians told us they’re volunteering again in their communities. And they’re getting closer to their kids.”
So even though the timesaving is just
Annual OntarioMD conference highlights the growing use of AI scribes
three hours a week, “those are very important hours,” he said.
Highlights from the study include:
•70 percent less time spent on clinical documentation and up to 4 hours a week freed from administrative tasks.
•83 percent of participants said they would use an AI scribe in their practice long term.
•82 percent of participants said they would recommend AI scribes to their colleagues.
•79 percent of participants said they were able to spend more time on patient care.
•76 percent of participants reported a reduction in mental effort during patient consultations.
Part of the evaluation included the use of Robotic Process Automation (RPA), or bots, to automate actions documented by the AI scribe during patient visits, such as sending appointment reminders to patients.
Benefits included faster follow up with patients to book appointments, a more streamlined booking process for patients, and improved continuity of care.
Of course, not everything was resolved in
the three-month study. Many issues remain, such as how much AI scribes are worth, in dollar terms, and whether the Ministry of Health will help doctors pay for them.
Indeed, during a panel discussion on physician usage of AI, Dr. Rosemarie Lall, a family doctor in Scarborough, Ont., noted that she has tried several of the systems and has found them to be incredibly helpful.
“AI scribes are saving my sanity,” she said.
She commented that her AI scribes–she has used several different brands – are quite able to take on many of the administrative tasks she used to do. These tasks were on the verge of overloading her to the extent that she was contemplating leaving the profession, she averred.
But with an AI scribe reducing the paperwork, “I was able to take Christmas off for the first time in many years. My kids were wondering what was going on!”
At the same time, she ventured that AI scribes are another cost for doctors, who are essentially small business operators. She already pays for an EMR, IT support, online booking, faxes, phone lines (her clinic has seven of them), email, security software and more.


“I’m not complaining, but I kinda am,” quipped Dr. Lall. “At some point, we are going to reach the breaking point.”
Another issue, observed Ariane Siegel, OntarioMD’s general counsel and chief privacy officer, is the legal and business challenge of obtaining an AI scribe. “The physician has to enter into a contract, and it can be very complicated,” she said.
While acknowledging the effectiveness of AI scribes, she also cautioned, “We don’t want to send doctors to the negotiating table.”
Dr. Lall concurred. “The contract for one of my AI scribes is 21 pages long. I signed, but I hoped I wasn’t signing away my first-born child.”
Ms. Siegel noted that OntarioMD is working with critical stakeholders, such as the Ministry of Health, Ontario Health and the Ontario Medical Association to consider ways of helping doctors reduce the burden of evaluating AI scribes and their contracts.
Speaking at a different session, Dr. Payal Agarwal, a family doctor and the integrated chief information and innovation officer at Grand River Hospital and St. Mary’s Hospital, in Kitchener, Ont., commented that policy makers are aware of the challenges of deploying AI in physician practices.
“They’ve been involved from the start with the study, and they’re working with the information and feedback,” she said. It’s possible they may come up with solutions to both the challenge of contracting with private-sector companies and the mounting costs of IT solutions for doctors.
What was most valuable about the AI scribe study, however, is that it quickly established the value of the systems for doctors.
And in the process, Dr. Agarwal said, “we developed a template for how to test things quickly.”
Issue DateFeature ReportFocus Report
February Medical ImagingSurgical Technologies
March Hospital at HomeInteroperability
April Mobile SolutionsArtificial Intelligence
May EHR / EMR TrendsPrecision Medicine
June/July IT Resource GuidePoint-of-Care Systems
September Community CareStart-ups
October Virtual CarePhysician IT
For advertising or editorial inquiries, contact Jerry Zeidenberg, Publisher, jerryz@canhealth.com
Coming up in 2025 www.canhealth.com

Address all correspondence to Canadian Healthcare Technology, 1118 Centre Street, Suite 204, Thornhill ON L4J 7R9 Canada. Telephone: (905) 709-2330. Fax: (905) 709-2258. Internet: www.canhealth.com. E-mail: info2@canhealth.com. Canadian Healthcare Technology will publish eight issues in 2024. Feature schedule and advertising kits available upon request. Canadian Healthcare Technology is sent free of charge to physicians and managers in hospitals, clinics and nursing homes. All others: $67.80 per year ($60 + $7.80 HST). Registration number 899059430 RT. ©2024 by Canadian Healthcare Technology. The content of Canadian Healthcare Technology is subject to copyright. Reproduction in whole or in part without prior written permission is strictly prohibited. Send all requests for permission to Jerry Zeidenberg, Publisher. Publications Mail Agreement No. 40018238. Return undeliverable Canadian addresses to Canadian Healthcare Technology, 1118 Centre Street, Suite 204, Thornhill ON L4J 7R9. E-mail: jerryz@canhealth.com. ISSN 1486-7133 CANADA’S MAGAZINE FOR MANAGERS AND USERS OF INFORMATION TECHNOLOGY IN HEALTHCARE Volume 29, Number 8 Nov/Dec 2024
Publisher & Editor
Jerry Zeidenberg jerryz@canhealth.com
Office Manager Neil Zeidenberg neilz@canhealth.com
The partnership between OntarioMD, Women’s College Hospital and the eHealth Centre of Excellence worked extremely well.
There’s now a methodology in place, she said, for testing other AI-driven solutions.
Indeed, she noted that the partners are currently creating a “living laboratory” that will be able to evaluate other systems that could reduce the administrative logjams now facing doctors.
The living laboratory is already at work on e-referrals– it’s applying a similar methodology to assessing solutions that are on the market. “We’re looking at factors like how many clicks are needed, and how much time is needed, versus paper workflows.”
She said the living laboratory will consist of three components: an artificial setting, like a traditional lab that can measure product performance and conduct things such as time/motion studies.
A second part will consist of natural settings, where systems can be tested in “real-world” clinics.
And a final component will assess how systems can be scaled up, so they can be used across the province.
To learn more about AI scribes, visit OntarioMD’s website at https://www.ontariomd.ca/pages/ai-scribe-overview.aspx. To discuss adopting an AI scribe, please contact support@ontariomd.com.
Contributing Editors
Dianne Craig dcraigcreative@yahoo.ca
Dianne Daniel dianne.l.daniel@gmail.com
Dr. Sunny Malhotra Twitter: @drsunnymalhotra
Norm Tollinsky tollinskyn@gmail.com
Art Director
Walter Caniparoli art@canhealth.com
Art Assistant Joanne Jubas joanne@canhealth.com
Dr. Onil Bhattacharyya Dr. Payal Agarwal



Neurofilament Light Chain (NfL) Assay


The first Health Canada licensed NfL blood test
siemens-healthineers.ca/cht-nfl

Now available in Canada
Unlock insights into relapsing multiple sclerosis (MS) with a simple blood test
This groundbreaking blood test provides fast, reproducible, and novel insights into relapsing MS disease activity with just a simple blood draw.
Gain critical early information to effortlessly enhance patient care and disease management.1
Clinical utility †
• The first NfL blood test for the prognostication of MS disease activity.
• A clear clinical cutoff of 12.9 pg/mL.
• Provides confidence in decision making.3,4,5
• Recommended in clinical guidance.
Healthcare impact
Powerful assay advancement
Delivers innovative , reproducible results for improving MS management.3
4. Calabresi
Predicting the risk of disease activity
Approved prognostic risk assessment test setting a new standard, with a clear decision threshold 1
5. Kosa P, et al. Enhancing the clinical value of serum neurofilament light chain measurement. JCI Insight. 20
6. Data

Advancing MS Management



“NfL addresses a major unmet need in management of MS
Making the novel routine
Easily consolidates into your clinical laboratory workflow—available for serum and plasma 1
Hospital partnership reaches milestone with EMRAM 6 certification
In an era where healthcare delivery is increasingly dependent on technology, a recent accomplishment by a four-hospital partnership in Ontario marks a significant milestone in the journey toward better patient care and operational efficiency.
Collingwood General and Marine Hospital (CGMH) in Collingwood, Georgian Bay General Hospital (GBGH) in Midland, Headwaters Health Care Centre (HHCC) in Orangeville and Royal Victoria Regional Health Centre (RVH) in Barrie achieved Stage 6 of the Healthcare Information and Management Systems Society (HIMSS) Electronic Medical Record Adoption Model (EMRAM).
It is an eight-stage (0-7) model that measures the use and utilization of EMR capabilities within hospitals.
HIMSS has reported hospitals that reach Stage 6 have robust capabilities for clinical decision support, a highly secure health information exchange, and a sophisticated level of EMR integration that enables improved safety, quality, and efficiency in healthcare delivery.
These hospitals are also well-positioned to move toward Stage 7, which represents the pinnacle of digital integration and data-driven healthcare.
Attaining HIMSS EMRAM Stage 6 is a

monumental achievement for any hospital – only six other hospitals in Canada have earned it.
What makes this achievement unique is the partnership between the four hospitals and the coordination and dedication it took to make it possible.
In 2021, during the height of the pandemic, the four hospitals implemented MEDITECH Expanse, a shared Health Information System (HIS) designed to enhance patient care, its delivery throughout
the organizations, and to enable improved transitions of care between the hospitals.
Following deployment, the four sites set their sights on a long list of improvements and optimizations in pursuit of HIMSS EMRAM 6, despite the complexity and challenges involved.
“Working as a partnership is not easy,” said Dave Brewin, VP of digital health and regional chief information officer. “Achieving this milestone together required not only a strong digital health partnership,
but also the alignment of clinical practices, showcasing our collective commitment to the patients and families in our region.”
To meet the rigorous standards set by HIMSS, digital health strategies and operational goals had to be aligned and clinical workflows, data entry processes, and decision-making protocols were standardized to ensure consistency and reliability at each of the partner sites.
Just as important as the technical prowess and logistical coordination required was the four partners’ commitment to doing the right thing for the communities they serve.
The pursuit of HIMSS EMRAM Stage 6 certification was not an external mandate or provincial requirement. The four sites voluntarily chose to seek certification to ensure that each person who walks through their doors receives care informed by the best possible use of technology.
The HIMSS EMRAM Stage 6 certification achieved by the four-hospital partnership is a testament to the power of collaboration in digital health. Together, they have successfully implemented advanced EMR systems and are striving to use them to their full potential to enhance clinical care.
As they continue on their digital health journey, these hospitals are setting a standard for others to follow in the pursuit of high-quality, data-driven healthcare.
VHA consolidates and automates many HR functions using Workday
BY NORM TOLLINSKY
Managing an organization with thousands of home healthcare providers (including nurses, personal support workers, and rehabilitation therapists) in today’s environment of staffing shortages and burnout can be more efficient and effective with a human resource management solution that provides leadership teams with an overview of their workforce.
VHA Home HealthCare (VHA), whose workforce of 3,400 provided 3.7 million episodes of care in the Greater Toronto Area, London and Ottawa last year, came to that conclusion after transitioning to a subscription-based Workday human resource management system.
“Prior to acquiring a Workday solution, we used a standalone HRIS and payroll system but had a variety of other HR software applications to support our business,” said Kelley Myers, VHA’s vice-president of HR and organizational development.
“That’s because the HRIS system didn’t have the capacity to deliver everything we needed. That web of separate systems became increasingly complex to manage and overly burdensome, requiring a lot of administration for staff and leaders who had to go to different places for many related functions. One of our key drivers was to acquire a much more sophisticated enterprise-wide system to provide a more seamless experience for our workforce.”
In the context of the health human resource crisis and the recruitment and retention challenges facing healthcare organizations, the decision to acquire a Workday HR management solution was a “major strategic imperative for us,” said Myers.
VHA issued a request for proposals in 2022 and selected the Workday platform and Mercer as our implementation partner. The project kicked-off in the summer of 2023 and went live in just under 12 months with Workday’s core HR and Finance modules, including human capital management, payroll and recruitment.
Phase two of the implementation is currently underway and includes modules for talent, performance management and a learning management system that employees can use to access VHA training.
“We’re really excited about our employees having increased visibility to their own training records and our offerings,” said Myers.
VHA’s IT leadership is also upbeat about Workday. “This move gave us the opportunity to franchise out IT support because Workday doesn’t require a ton of technical expertise to configure,” said Alistair Forsyth, VHA’s vice-president, digital health and chief information officer.
“HR, finance and payroll staff are able to tackle a lot of the maintenance and enhancements themselves, which reduces IT staffing requirements and reduces bottlenecks for the business. Moving from an on-premise system to the cloud also made a huge difference to our security posture.”
By using Workday’s mobile app, employees can access payroll and benefits information, manage time off and more all while working in the community. Workday also streamlines the recruiting and onboarding process, automating processes such as prompting new hires for key information right from the app.
“Delivering positive employee experiences is so important in a high turnover business,” said Myers. “Workday helps us put our best foot forward with these critical HR functions with new recruits and our entire workforce.” Another benefit, she added, is increased visibility for team leaders, allowing them to more eas-
Using Workday’s mobile app, employees can access payroll and benefits information, manage time off, and more.
ily manage turnover, new hires and pending performance reviews.
Having a powerful HR management application like Workday can also positively impact patient care, she said, because “we know that happy employees make for happy clients. Great tools also help improve retention and one of the things we hear most from clients is how much they value consistency in their care providers.”
To stay on top of employee morale, VHA can take advantage of Workday’s surveying capability that queries employees anonymously about how they’re
feeling. This allows management to anticipate staffing issues before they become critical, said Colette Lepine, Workday’s Canadian sales lead for healthcare.
Released in September, Workday Illuminate, the next generation of Workday AI, assists with decision making and streamlines actions. When VHA employees ask a question about their pay or benefits using the AI-powered Workday Assistant, for example, the application automatically brings up the information they’re looking for.
“It can also be used to forecast staffing needs based on historical data, but what’s really cool about it is that it’s embedded across the platform,” said Lepine. “For example, if an employee hasn’t taken advantage of any training in the previous year, it will ask them if they want to have some learning opportunities presented to them.”
Founded in 2005 by Dave Duffield and Aneel Bhusri, Workday has 18,800 employees, 2024 revenues of $7.26 billion and a global clientele. The company’s healthcare human resource management solution serves all parts of the healthcare sector, including acute care, long-term care as well as home care providers.
VHA Home HealthCare, headquartered in Toronto, is a not-for-profit charitable organization and one of the largest providers of publicly funded home care in Ontario. VHA was founded in 1925 and holds exemplary standing with Accreditation Canada and is a leading research organization in home care science.
Dave Brewin, RVH VP, digital health and regional CIO; Maria Ma, team lead, clinical informatics; and Jennifer Bourne, manager, clinical informatics.

Enterprise Imaging Cloud
Ontario Shores integrates genomic data with EHR to personalize doses
BY NORM TOLLINSKY
Ontario Shores Centre for Mental Health Sciences in Whitby, Ontario, is the first mental health organization in Canada to use pharmacogenomics on a routine basis to prescribe anti-psychotic medications to inpatients diagnosed with schizophrenia and schizoaffective disorder.
The milestone, achieved in September, was made possible by Ontario Shores’ acquisition of MEDITECH’s Expanse Genomics solution, which brings discrete genetic data into MEDITECH’s Expanse electronic health record (EHR).
“Anti-psychotic pharmacotherapy is often a trial-and-error process,” said Dr. Phil Klassen, Ontario Shores’ vice-president of medical affairs and research. “While psychiatrists do have some guidance based on research, clinical experience and a patient’s personal and family history, without genetic data, their ability to tailor medication choices to an individual’s unique needs is limited.”
The effectiveness of an antipsychotic drug, and risk of side effects, can be dependent on a patient’s genetic profile and the rate at which they metabolize a drug. Genetic testing provides psychiatrists at Ontario Shores with guidance on prescribing and dosage based on a patient’s genetic makeup and whether they are slow or fast metabolizers.
Without this information, it can take weeks or months to know if a drug or dosage is effective, potentially suggesting that patients are non-responders to a particular drug. During this time patients may be prescribed different drugs and different
doses on a trial-and-error basis. Using pharmacogenomics, psychiatrists are more likely to prescribe the right drug and the right dose the first time.
“This is important because schizophrenia and schizoaffective disorder are responsible for 50 percent of all bed days in mental health,” Dr. Klassen said. “Administering the right drug and the right dose,” he added, “can improve a patient’s experience and potentially shorten their length of stay.”
“To my knowledge, no one in Canada’s mental health field routinely uses pharma-

cogenomics. While tests can be ordered, there is an out-of-pocket cost. Occasionally, a physician might have paid for a genetic test if they were particularly concerned about a patient. This will be the first time all patients with these conditions are offered pharmacogenomic testing.”
Ontario Shores is able to order tests from Dynacare directly from the Expanse Genomics solution.
“It’s important to note that the genetic testing we’re ordering does not diagnose genetically-based illnesses,” said Dr. Klassen. “The genetic testing that we’re doing looks only at the genetic pattern a patient has in relation to metabolizing drugs.”
Reports from genetic testing have traditionally been available as up-to 50-page PDFs, which are difficult to access, said Jennifer Ford, MEDITECH’s manager of clinical strategy and genomics.
MEDITECH, however, brings the discrete genetic data into the EHR so it’s eas-

ily accessible. It also links to clinical practice guidelines from the Clinical Pharmacogenomics Implementation Consortium (CPIC) and the Dutch Pharmacogenomics Working Group through First Databank’s drug database to generate alerts if a physician prescribes a drug or a dose that doesn’t align with the patient’s genetic profile.
“Having discrete data in the EHR is important because you can’t easily update a
PDF with new information about a gene or drug,” Dr. Klassen said. “Plus, you need this data for proper research. Researching from PDFs is tedious; you’d have to hire someone to sift through them manually. With discrete data in an EHR, you can load it and get to work right away.”
While routine genetic testing is currently being performed only for inpatients with schizophrenia and schizoaffective disorder, Dr. Klassen expects to see expansion of testing for patients with other conditions and potentially for ambulatory patients as well.
Next steps for advancing the use of pharmacogenomics will be guided by research made possible through the recent appointment of Dr. Daniel Mueller by Ontario Shores and the University of Toronto as a joint chair in precision medicine.
Expanse Genomics has been in development for almost a decade and has been in use by early adopters in the U.S. for several years, notes Ford. For one of the most promising use cases, oncology, the solution also allows for clinical trials and alternative therapy matching.
“With the specific genetics of a patient’s cancer, their hereditary risk and all of the demographic and other information in the EHR, Expanse Genomics is able to search clinical trial databases and find a match,” Ford said. “And if a new therapy hits the market that might be better for the patient, we can immediately match them to it by having all the information in the EHR.”
Evidence from early adopters indicates significant time savings for clinicians in ordering genetic tests and prepping patients for appointments because all the relevant genetic and demographic information is so easily accessible.
CIRA survey shows cyber attacks have more than doubled in frequency
BY DIANNE CRAIG
Anew cybersecurity survey conducted by the Canadian Internet Registration Authority (CIRA) reveals almost half of respondents (44 percent) experienced attacks in the past year, up from 17 percent in 2021.
CIRA is the non-profit organization which operates the .ca domain, supports internet infrastructure and provides a range of cybersecurity services, such as DNS Firewall, which serves 129,000 healthcare workers.
After polling 500 decision-makers across three categories – private sector, public sector, hospitals and healthcare organizations, and the education sector, CIRA’s key findings highlight the surge in cybersecurity risks and the need for organizations to maintain a strong cybersecurity posture and awareness of current and emerging risks.
Cyber-criminals can quickly gain access to thousands of records through a server, commented Jon Ferguson, CIRA’s vice president, Cybersecurity & DNS. “And ransomware is a top threat,” said Ferguson.
While recovery times [to become oper-
ational] are improving to about two weeks on average, the time to recover some of the lost data can take weeks or months.
According to the survey, 79 percent of respondents pay the ransom – something that encourages future breaches, Ferguson noted. Moreover, insurance costs typically go up, while coverage may come down.
In light of this, “You want to be looking at good cybersecurity posture and digital hygiene,” Ferguson said. Digital hygiene can include password re-sets, and other preventative measures.
Another significant fallout from a ransomware attack is reputational damage. In fact, 28 percent of respondents felt they suffered reputational damage following a cybersecurity incident – a big increase from the 6 percent who cited it in 2018.
Some key findings from 2024 CIRA Cybersecurity Survey respondents:
•98 percent conduct cybersecurity training
•44 percent indicate the organization experienced a cyberattack in the past 12 months
•28 percent report they have been victims of ransomware in the past 12 months – up from 17 percent in 2021
•Of those who experienced ransomware attacks, 73 percent said data was exfiltrated, 79 percent paid ransomware demands (at least $25,000) and 74 percent support legislation that would prohibit paying ransomware demands
•The biggest perceived threats are malicious software, unauthorized access and theft of data
•83 percent have a cybersecurity response plan
79 percent of those who experienced a ransomware attack paid the ransom, which encourages future breaches.
•52 percent say it took less than a week for their IT systems to recover Cybersecurity threats in healthcare settings are increasingly common.
In November, August 2023, the Canadian Medical Association (CMA) journal stated in an article entitled Cyberattacks on Canadian Healthcare Systems that 48 percent of all reported breaches occurred in the health sector.
Asked about this, Ferguson also noted that with more consolidation in healthcare, more health networks are connected, and breaching those networks gives access to more records.
Last year, when five hospitals in southwestern Ontario were breached, 326,000 patients were impacted, recalls Ferguson.
The most common impact of attacks is preventing employees from being able to do their work.
Two in 10 respondents also reported direct financial costs. “But you’re usually not talking about loss of life,” notes Ferguson, indicating that in certain cases, such as some busy healthcare settings, if they are offline for some time and services are delayed, or records are tampered with, there are risks of a more severe impact.
With the introduction of AI in many different businesses and organizations, typically to improve productivity and automate repetitive tasks, there are new cybersecurity challenges.
According to the CIRA survey, among those worried about generative AI threats, AI-powered cyber attacks, privacy breaches, and data poisoning are likely to be of greatest concern.
Dr. Phil Klassen, Ontario Shores
Jennifer Ford, MEDITECH














































UofT’s Data Sciences Institute helps place the data scientists it’s producing
Participants are seeking employment as data and reporting analysts, data coordinators and technicians.
The Data Sciences Institute (DSI) is a tri-campus, multidisciplinary hub for data science at the University of Toronto (datasciences.utoronto.ca). It facilitates research connections, fosters innovation and enhances teaching and learning in data sciences, including emerging data-driven disciplines. The DSI, with the financial support of Upskill Canada, powered by Palette Skills and the Government of Canada, also offers an intensive, 16-week certificate in data science or machine learning software for people with a university or college degree who have three years or more of work experience. They’re learning programming skills in languages such as Python and SQL. The participants are seeking employment in sectors like healthcare as data analysts, reporting analysts, data coordinators and data technicians.
In this article, we interview leaders at two Canadian companies who are hiring certificate-holders from the Data Sciences Institute. They discuss why they’re working with the DSI, and how hiring Data Science Institute participants will benefit their organizations.
Javier Diaz, PhD, is head of data science at Phenomic AI Inc., a rapidly growing start-up biotech company that’s devising solutions for combatting cancer. In particular, it aims to raise the survival rate for patients with the hardest to treat solid tumours. Phenomic AI is doing this by identifying new targets in tumours for drugs. The work involves AI and machine learning. The company recently partnered with global pharmaceutical giant Boehringer Ingelheim in a business deal that’s potentially worth more than $500 million to Phenomic AI, which is based in Toronto and Boston.
Canadian Healthcare Technology: What appealed to you about hiring people who have completed the DSI’s certificate?
Javier: What I like about the Data Sciences Institute is that they don’t only train students in terms of technical aspects like programming and machine learning, but also they look for so-called soft skills, and they try to improve that in the students. I also like that the students have backgrounds in different areas, including healthcare. These are the ones we are interested in, as we’re collecting data about cancer. These persons know about cancer, know the cancer terms that biologists and clinicians use, which is not often trivial. Candidates from other places might have more experience with software engineering or machine learning, but they might not be aware of the terminology that is used by biologists or cancer biologists. So, they had the technical skills and the business knowledge, which was great. It saves a lot of time from our side in terms of onboarding them into the team.
Canadian Healthcare Technology: How many people have you hired from the DSI?
Javier: We have one person working already with us from the Institute and one more starting next week.
Canadian Healthcare Technology: Was the DSI sensitive to your needs? Did they filter the candidates they sent your way?
Javier: Yes, I spoke to them about our needs and then they sent me about four or five resumes of candidates that they thought would be relevant. We put
out a job description that was shared with the students. The candidates they sent me were outstanding in terms of the business knowledge that they are bringing to the team. They know about cancer biology. They even know about the particular type of technology that we’re using, which is called single cell RNA sequencing. So, I think what made their candidates different from others was the biology knowledge that they have. And then they also know how to program, which is great. They really met our needs. They have the two aspects that we were looking for, the technical and the domain knowledge.
Canadian Healthcare Technology: What kind of work will your new hires from the DSI be doing?
Javier: They are going to help us keep up with onboarding new data from public repositories. So, we have a database with about 150 studies collected. We built some computational tools that will help us to streamline things so that we can onboard more data in a faster way. These two new team members will continue on

that, making use of our tools and developing new tools to make this process even faster and more streamlined.
Canadian Healthcare Technology: So, they’re going to continue to develop the database?
Javier: Exactly. They’re going to curate the database –get more data and standardize it. We will identify data that we might be missing for some cancer types and some particular treatments, because we want to keep making our database more inclusive of all cancer types and bigger, and they will help us with that.
Canadian Healthcare Technology: As well as the domain knowledge, do the DSI hires have the technical skills?
Javier: They do know how to program, which is very important. The Data Sciences Institute spend most of the time teaching them how to use Python, and that’s exactly what we need. If you are going to pick only one language, speak Python. Because it’s more standard in the industry, regardless if they stay in the health sciences or they go to banks or finances or other industries. Python is the gold standard in industry.
Sepehr Sisakht is CEO of Shyftbase Inc., a Torontobased company that produces software for supplychain management. The five-year-old company has
grown quickly by applying new technologies like machine learning (ML) and other forms of artificial intelligence to improve product deliveries and returns in a variety of industries. It is targeting healthcare, which Mr. Sisakht sees as needing modernization in the area of supply chain management. At the time of this interview, the company was about to hire a Data Sciences Institute participant.
Canadian Healthcare Technology: Have you hired a DSI participant?
Sepehr: We are interviewing three candidates. There were quite a few who were interested, but we have one position available. We haven’t finalized it yet, but we will decide on the candidate this week. All three are very, very good.
Canadian Healthcare Technology: What appeals to you about the skills of the participants from the DSI?
Sepehr: Well, they are being educated in data science,

but they also have an education in other areas. If you are aspiring to be a really successful data scientist, I think previous experience is very important because you bring all those perspectives and you are able to look at problems from different angles. And with the technical knowledge that they’ve acquired through this program, I think those candidates can definitely excel, compared to a lot of other conventional computer science programs.
Canadian Healthcare Technology: What abilities do you need in a new hire, and do you see these skills in the DSI candidates?
Sepehr: I love to see hints of problem-solving skills and abilities. You want your data scientists to be able to take initiatives and look at problems from different angles. If they’re going to join your team, you want them to add value by looking at the data and being able to solve problems. Technical skills are great, but I think everybody can learn more on the job. On the other hand, not everybody has the drive in them to look at different angles for certain problems. The people from DSI have these problem-solving abilities.
Canadian Healthcare Technology: Do you think it’s productive to hire a person from DSI, who has
Javier Diaz, head of data science at Phenomic AI Inc.
Sepehr Sisakht, CEO of Shyftbase Inc.


Medtronic CarePathIQ


A suite of solutions for intelligent patient pathways



























Dedicated to collaborative partnerships.













































Our customer-centric approach ensures that we are a strategic partner in achieving healthcare excellence together.





































GoAutomate brings AI,financial-sector tech know-how to healthcare
BY JERRY ZEIDENBERG
TORONTO – GoAutomate is developing AI-based solutions that are designed to improve workflow in diagnostic imaging departments, which often get bogged down with faxes and paper-based processes. They’re also slowed down by mistakes in documents that are sent electronically. All of these documents regularly contain missing or incorrect data, and staff must fill in the blanks and fix the incorrect information –a time-consuming and tedious process.
Correcting DI requisitions can lead to delays in getting patients into the imaging suite. “Our goal is to reduce patient booking times from two-to-three weeks to one or two days, improving overall patient care,” said Jag Basrai, chief executive officer of GoAutomate.ai.
He added, “Diagnostic imaging can be a stressful environment. We’re trying to alleviate the stress and make sure everyone is as efficient as possible. We want to take away the more tedious tasks.”
The company is devising an AI solution that can automatically check forms, for example, to ensure that a patient’s Ontario Health number is valid, and fixing it when it’s incorrect. It can also check that the name of the referring physician is right, along with his or her contact details – important data for reporting and follow-ups.
Using AI, the system can refer to other documents to fill in missing information.
“It’s not ChatGPT, as we’re training our own large language models,” asserted GoAutomate’s chief technology officer, Jason Daly. He said that the company is already testing the solution.
The company has been working on projects at several Ontario hospitals, automating different paper-based processes. “Our users are giving us feedback,” said Daly,

helping to improve the product. The deployments allow GoAutomate to use and refine the models in real world scenarios. Moreover, the AI system can even check to see that the requested exam protocol is appropriate for the condition of the patient, something that staff and radiologists often spend time doing.
The referral can then be booked more quickly.
As Basrai noted, “We’re eliminating a lot of the tedious steps, including re-keying information.” He explained that radiologists will still review the referral and chosen protocols. But for them too, the process has been improved.
Instead of requiring writing or keystrokes, GoAutomate’s solution will let them “tick off boxes”, a much faster and easier process.
Once the exam is approved, the system can search and bring up prior exams for

the radiologist. It will automatically contact the patient to remind him or her about the appointment – reducing the number of no-shows. And it will enable the referring physician to log-in to see where the patient is in the diagnostic process.
Daly said that many members of the GoAutomate team – himself included –have backgrounds in the financial industry, where they created bots and other automated solutions to improve workflows.
They’re now bringing these secure technologies to the healthcare sector.
In a separate application, GoAutomate is using AI to blur-out patient names, numbers and other identifiers in diagnostic images when privacy is needed for certain procedures – such as organ transplants.
The company is currently at work outside of Ontario on a large project of this kind. “It’s a new process created by GoAutomate,” said Daly. He said it could be used
in research studies, too, when privacy of the patients must be protected, or anonymity is needed for blind studies.
“We know there’s hundreds of use cases this technology could address,” he added.
Basrai mentioned that patients and their families often contact several hospitals or health organizations to get on the list for a wide range of procedures.
That means clerical staff at these hospitals are essentially receiving the same information, and two or three clerical teams could all be keying in the same data. Instead, AI could determine if an application has already been made, and could duplicate the data at the different institutions, saving staff time and eliminating a tedious chore.
“If a large language model does the work, it frees up people to do other things,” said Basrai.
The company says it could even build ‘bots’ that could search across the entire provincial healthcare system when physicians need access to reports and images. While Ontario has been creating repositories that physicians can enter when looking for patient information, it’s still a time-consuming process to go into various systems.
“Even if they’re quick, it could still take a clinician two minutes to search,” said Basrai. “AI does it in 20 seconds.”
Daly, who spent 20 years in the banking sector developing technological solutions, said the healthcare industry is ripe for this kind of “intelligent automation”. And while bots can quickly obtain the desired data, when AI is added, it takes things to a higher level of usefulness.
“The bots can bring the data in, and the large language models can process it,” said Daly. In this way, an AI-powered system can continue to do more of the tiresome tasks in healthcare, enabling humans to focus on higher value and more meaningful work.
Siemens Healthineers’ MS blood test is Canada’s first to gain licensing
Siemens Healthineers now has a blood test for multiple sclerosis (MS) disease management available for sale in Canada. The company is the first in Canada to receive Health Canada licensing for its Neurofilament Light Chain (NfL) assay for use on the Atellica IM Analyzer, developed in collaboration with Novartis Pharma AG.
The test will be useful alongside other clinical, imaging, and laboratory findings to help predict the risk of MS disease activity in a patient with Relapsing Multiple Sclerosis (RMS). Identifying the risk of MS-related neuronal injury earlier in patients with RMS would support neurologists and other physicians in better managing the disease, and potentially help to prevent relapses and worsening of disease.
MS is an autoimmune, inflammatory, and neurodegenerative disease in which axonal loss is the major cause of irreversible neurological damage leading to disability. Multiple Sclerosis af-
fects nearly 2.8 million people worldwide, although the number is anticipated to be higher as many people remain undiagnosed in underserved and remote communities without access to neurologists or adequate imaging equipment.
“While there is no cure for MS, treatments exist to decrease the frequency of relapses, thought to be associated with nerve cell damage and disease progression. What patients still need is an easily accessible, cost-effective, and accurate blood-based test that would indicate early signs of neuronal injury and disease activity,” said Dr. Dennis Gilbert, head of research, development, and innovation for diagnostics at Siemens Healthineers.
“Neurofilament light chain, or NfL, has emerged as a leading biomarker of nerve cell damage. Having access to a test that measures this protein capable of crossing the blood-brain barrier to support earlier prognostication of disease activity would be a critical scien-
tific advancement for MS patients,” he added.
“NfL is a promising blood biomarker for assessing prognosis in multiple sclerosis, offering a noninvasive and cost-effective tool for monitoring disease activity and relapse risk,” said Catherine Bodroghy, market
NfL is a promising blood biomarker for assessing prognosis in multiple sclerosis, says Catherine Bodroghy.
development manager at Siemens Healthineers, Canada “We are so proud to be able to provide access to this test to patients in Canada.”
The NfL assay from Siemens Healthineers is for in vitro diagnostic use in the quantitative measurement of NfL in both human serum and plasma. The blood test, in conjunction with clinical, imaging, and laboratory findings, is in-
tended to be used as an aid in identifying adult patients between 18-55 years of age with RMS, who are at a higher versus lower risk of MS disease activity, as defined by new or enlarging T2 magnetic resonance imaging lesions, within a two year period.
Blood-based biomarkers such as NfL are expanding our understanding of neurological diseases. They also are expected to rapidly change the practice of neurology. Siemens Healthineers is wellpositioned with the Atellica Solution to support neurological diseases with tests that can be run on widely accessible laboratory platforms, making these types of tests available to more physicians for their patients.
To learn more about the NfL assay, please visit: siemens-healthineers.ca/cht-nfl To talk to someone at Siemens Healthineers about NfL, please contact Catherine Bodroghy, market development manager - assays, Canada: catherine.bodroghy@siemenshealthineers.com
Jag Basrai, CEO of GoAutomate.ai
Jason Daly, chief technology officer, GoAutomate.ai
Digital empathy can be built into screening programs to improve engagement
Adiagnosis of cancer for an adolescent and young adult (AYA) is life changing, no matter the final outcome. While medical treatment and prognosis are disease-dependent, all young people living with cancer face the same developmental challenges as their healthy peers, with the added burden their condition brings.
A holistic approach from supportive care teams, promoting good mental health and wellbeing at the same time as identifying and supporting those at risk, has a substantial impact on both quality of life and outcomes. Until recently, the time and effort of this type of intervention had been prohibitive. It was evident there was a significant gap in care.
Dr. Tyler Ketteryl and the AYA Oncology team at Seattle Children’s hospital are pioneers in the field of enhanced oncology care. They realized that advancements in digital health technology could provide them with new avenues to connect with patients, to effectively triage those that need enhanced services and streamline quality of life intervention.
Tickit Health, based in British Columbia and founded by pediatrician Dr. Sandy Whitehouse over a decade ago, has built digitally empathetic screening and patient engagement tools for historically underserved populations. In Vancouver, the Provincial Health Services Authority, with the Department of Mental Health and Substance Use, engaged Tickit Health to support patients waitlisted for rehab treatment.
Customizable assessments and screeners can serve multiple purposes, from educating patients and their families about treatment protocols to facilitating realtime symptom tracking and providing crucial emotional support. The challenge with many digital tools has been delivery and uptake. For example, overall adoption of portal rates has been reported at 23 percent.
Tickit Health’s focus on digital empathy, grounded in validated emotive design heuristics, has been shown to improve engagement, and encourage participation over other screening platforms.
The AYA Oncology team observed a notable improvement in patient satisfaction and overall well-being following the integration of Check Yourself into their Epic Electronic Health Record (EMR).
In an evaluation study when the platform launched, 83 percent of patients elected to take the screener, and 74 percent felt the feedback information was both relevant and useful to them.
Patient engagement is greatly enhanced when a screener, assessment, or survey is designed with the ability to ask sensitive questions in a gentle manner and offers value back to the participant.
Critical to the success of these digital initiatives is their integration with Seattle Children’s Epic EMR system, ensuring that all patient data is centrally managed and readily accessible to authorized healthcare providers.
The integration streamlined workflow by allowing the patients to complete Check Yourself a few days in advance of their visit, resulting in the data being available during the consultation. Live data gave the
AYA Oncology team anticipatory guidance, making the visits much more effective and efficient.
Logic built into the screener offers relevant information for providers highlighting critical issues while at the same time preparing patients with feedback and resources to
discuss with their provider. The majority of the healthcare team (74 percent) reviewed and utilized the results of the screener directly into the patient visit. Eighty seven percent (87 percent) of providers reported that incorporating the results in the EMR positively impacted care.

Canadian Healthcare Technology magazine
Effective communication is key to providing comprehensive care in pediatric oncology. Tyler Ketteryl and the AYA Oncology team have successfully utilized digital tools to streamline communication among patients, their families, and healthcare providers.
One-stop shopping.
Canadian Healthcare Technology offers the country’s leading healthcare I.T. publications. Are you getting all the news?
Canadian Healthcare Technology breaks the news about important projects, programs and technologies, and provides hospital executives and senior managers with an excellent source of information for improving the delivery of healthcare. It’s sent to over 5,200 readers in print format and to 6,800 opt-in subscribers as a digital edition.

White Papers
eMessenger newsletter

Canadian Healthcare Technology’s e-Messenger contains breaking news about important deals, installations and developments. Four blasts are sent each month, via e-mail, to over 7,000 senior managers and executives in hospitals, clinics and health regions.
Canadian Healthcare Technology’s White Papers are sent out once a month, via e-mail, to over 5,000 senior managers and executives in Canadian hospitals and health regions. The monthly blast contains summaries and links to White Papers issued by various organizations, providing cutting-edge information about topics of interest to healthcare decision-makers.

Roundtable: Driving digital health success, from buy-in to impact
Stratford Group recently hosted a roundtable discussion, bringing together six healthcare experts to explore the most pressing challenges in digital health. The discussion was organized around three key topics: gaining approval and buy-in, effectively measuring benefits, and scaling successful initiatives. As our experts shared their experiences a unifying theme emerged: digital transformation makes a meaningful impact when leaders align people, processes, and technology.
“There’s that phrase, “Change happens at the speed of trust”, and I think at the end of the day, all of this depends on trust. And that comes with thoughtful change management.”
– Viren Naik Medical Council of Canada
Moderated by Shelagh Maloney of Stratford Management Consulting, the roundtable participants provided valuable perspectives about driving digital transformation in complex healthcare environments.
Participants included Susan Anderson, chief information officer and leader of the Health Information Unit for the Department of Health and Government in Nunavut; Rana Chreyh, vice president and practice leader for Digital at Stratford; Simon Hagens, vice president, Performance at Canada Health Infoway; Dr. Sarah Muttitt, chief information officer, Hospital for Sick Children and University Health Network, Toronto; Dr. Viren Naik, CEO, Medical Council of Canada; and Nicole Vandenborre, director of Operations, CAN Health-Atlantic.
Securing approval, buy-in, and implementing successfully: Beginning with a discussion about gaining approval and buy-in for digital health initiatives, it was stressed that these projects often represent large-scale business transformations, not simply IT implementations, and require long-term commitment from across the organization. To secure executive sponsor-

ship, it’s crucial to clearly define the problem and outline specific, measurable objectives. A well-defined goal is essential to rally the organization behind the initiative, help overcome resistance and drive change.
“We’re not implementing technology for technology’s sake. We are solving a big problem for the organization; that’s how it gets behind a technical implementation.”
– Dr. Sarah Muttitt Hospital for Sick Children and University Health Network
Securing buy-in, however, extends beyond executives. Frontline staff must be onboard, as the ones who typically interact with the technology daily. “Co-creating” was mentioned often as a means to encourage buy-in and ensure the technology implementations are addressing the needs of the people they serve – including patients and families.
The goal is not to create a digital strategy, but to build a digitally enabled system that supports the achievement of corporate objectives.
While everyone works toward a go-live date, this date is only the beginning. Continued investment and assessment during subsequent days, months and years are required to ensure the system delivers on its promises. By involving sponsors and users from the outset, setting clear goals, and being adaptive, organizations can effectively implement and scale digital health initiatives. Clarity and collaboration are also key, especially in an already resource-constrained system.
“…with a very thoughtful front-end startup, some significant success can be accrued.”
– Susan Anderson Department of Health and Government, Nunavut
Measuring and communicating benefits: Achieving benefits is dependent on defining the problem and expected outcomes upfront and a benefits model should connect project outputs to measurable results. This creates a roadmap for tracking short-term successes and linking
them to long-term impacts. Efforts to realize and communicate success fall short when goals and benefits are not clear.
“…a project does not lead to benefits. The project delivers an output and it’s only through the correct design that you realize your outcomes.”
– Rana Chreyh Stratford Management Consulting
User involvement impacts benefits realization. By engaging clinicians, administrators, and patients in both design and governance, organizations ensure that technology addresses specific problems. This avoids common pitfalls like technology failing to integrate into daily workflows. Strong leadership is also critical in driving projects to success. Leaders must establish a clear vision, make decisions effectively, and communicate progress and value to all, continually.
Successfully scaling and spreading projects: To move projects beyond pilot mode and achieve widespread adoption, organizations need a strategic approach that aligns objectives and priorities. Securing buy-in is a critical first step, but the process does not stop there. Co-creating solutions with patients, families, and vendors ensures that systems are not only functional but meaningful. As projects scale, ongoing investment in training, optimization, and user proficiency is essential for unlocking the technology’s full potential and delivering lasting value.
“To scale, we need to get to a place where we have ecosystem understanding internally so that we understand where we play externally”.
– Nicole Vandenborre CAN
Health Network
Scaling innovations nationally may introduce technological and cultural complexities. Occasionally circumstances arise where the organization that is responsible to drive the project is not receiving the
Transformative project to enhance shared access to patient records
BY NEIL ZEIDENBERG
Just three years ago, Perth Smiths Falls District Health was still managing its daily workflows in a mostly paper-based environment.
Perth Smiths Falls is a community hospital composed of two sites, both of which are within an hour’s drive of Ottawa, serving approximately 70,000 residents.
In 2022, however, the management team at Perth Smiths Falls embarked on journey to modernize its clinical documentation infrastructure – to ultimately benefit the quality of care given to patients and to improve workflow for staff and clinicians. Instead of going alone, it partnered with five other regional hospital organizations.
Over the last three years of this clinical transformation, Perth Smiths Falls has in-
vested approximately $20 million. For this community hospital, it’s the single largest digital investment it’s ever made. Funding comes directly from the hospital.
“We’re in the final 100-metres of the marathon, training staff and making final preparations,” said Michael Cohen, president and CEO of Perth Smiths Falls District Health. “After two years, it’s full steam ahead.”
The six hospitals – Brockville General Hospital; Kingston Health Sciences Hospital (lead Hub); Lennox and Addington County General Hospital; Perth Smiths Falls District Hospital; Providence Care, and Quinte Health –are deploying the Cerner Millennium platform, a cloud-based solution from Oracle Health that offers effective tools such as evidence-based decision making for clinicians, staff shift planning
and real-time bed management.
With a goal to improve the care they provided to patients every day; the six hospitals agreed to tackle their challenges together and formed a regional health information collaborative called Lumeo. When complete, the project is
Six hospital organizations agreed to tackle their IT challenges together and formed a collaborative called Lumeo.
expected to greatly improve patient care, clinical efficiency and information security.
Lumeo will connect patients with their care teams at the six healthcare organizations, providing secure, shared ac-
cess to complete patient information. That will save clinicians valuable time resulting in better quality patient care.
For the health system, it means realtime electronic records at the point-ofcare, standardized workflows, computerized physician order entry for medications and instructions, and integrated care plans across all partner organizations.
“This is a great regional initiative,” said Tyson Roffey, vice president, Digital Health Solutions at Nova Networks (www.novanetworks.com) – the project lead behind the I.T. transformation at Perth Smiths Falls.
For its part, Nova Networks is providing the go-to-market strategy and helping customers wherever and whenever it’s needed. “We are involved in the implementation of professional and

Read
Canadian Healthcare Technology, published eight times per year, is sent free of charge to managers of hospitals and clinics, and executives in nursing homes and home-care organizations. Qualified subscribers need only periodically renew their subscription information to ensure continued delivery of the magazine. Please take a minute to complete your renewal and make sure Canadian Healthcare Technology keeps coming to you – absolutely free.
ARE TWO WAYS YOU CAN SUBSCRIBE:
COMPLIMENTARY SUBSCRIPTION REQUEST
(PLEASE PRINT)
Your organization’s business or industry?
Hospital
Health region
Long-term care institution
Home care Clinic
Computer or software vendor
Telecommunications vendor
Medical
VAR or systems integrator
Education
Finance/insurance
Consulting/legal
Public relations
Other
If you are employed by a hospital, which of the following categories would best apply to you?
CEO/President/VP/Executive Director
Finance
MIS
Medical Director
Physician
Purchasing
Nursing
Pharmacy
Radiology
Pathology & Laboratory
Human resources
Health records
Public relations
Quality assurance
Other
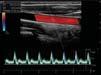
Study finds AI-powered ultrasound at point-of-care shows promise
VANCOUVER – Researchers have confirmed that artificial intelligence (AI) software has the potential to enhance heart failure diagnostics. The study, led by Vancouver Coastal Health Research Institute researcher Dr. Christina Luong, shows that the machine learning tool could be safely used to improve the timeliness of heart failure diagnosis and treatment.
“Wait times for essential echocardiogram diagnostic tests for heart failure presently take up to six months for nonurgent cases, which we would ideally like to see reduced to one month or less,” said Dr. Luong. Since around 2014, her research has focused on the development of machine learning algorithms for imaging diagnostics and research trials that incorporate echocardiography.
At around $200,000 each, cart-based echocardiogram machines found in diagnostic imaging labs use sound waves to capture detailed images of blood flow throughout the heart and its many valves. Echocardiograms are the bread-and-butter of diagnostic tests for heart function, as they provide a big picture view of cardiac structure and function, giving insights into the flow of blood inside the heart and throughout the body’s circulatory system, said Dr. Luong.
Clinicians use these images to diagnose conditions, such as reduced cardiac pumping function and abnormal relaxation that can decrease blood flow and result in conditions such as pulmonary edema: a buildup of fluid in the lungs that can lead to breathing difficulties.
However, the process of analysing images captured by echocardiograms can be

time-consuming and requires expertise and experience to reach an accurate clinical diagnosis.
The machine learning algorithm Dr. Luong and her team developed and used in her recent study, published in Echo Research & Practice, was assessed for its performance identifying the indicators of disease present in point-of-care ultrasound (POCUS) images.
The handheld POCUS devices use sound waves to record video footage of heart function at the bedside on miniature machines, instead of through an appointment with a specialist for an echocardiogram.
The research team wanted to know how well their machine learning algorithm measured left ventricular ejection fraction in images captured by both novice and moderately experienced healthcare workers.
Left ventricular ejection fraction is the amount of blood being pumped by the heart within a given time frame – essential information for assessing heart failure and making treatment recommendations.
The machine learning model was previously trained to identify normal and abnormal left ventricular ejection fraction using 2,920 videos from 2,127 patients. While it sifts through video footage, the AI’s assessments are made by video segments, frame by frame, stated Dr. Luong.
For the study, two nurse practitioners with little to no experience using POCUS and seven physicians with moderate POCUS training performed POCUS scans on 138 adult patient volunteers recruited from a heart failure clinic in Vancouver.
The 1,257 videos of the patient scans were analyzed by the research team’s ma-
chine learning algorithm and an expert echocardiographer.
Dr. Luong and her team found a high degree of correlation – around 80 percent similarity between the AI and expert’s estimation of left ventricular ejection fraction for cardiac POCUS images of heart failure patients. The performance of the model was preserved even when accounting for the scanners with lower levels of POCUS experience.
However, the AI algorithm was less accurate in cases of poor image quality or when a patient had an irregular heartbeat, also called atrial fibrillation, which the research team concluded should be considered in potential clinical applications of this type of machine learning model.
“Instead of an expert echocardiographer needing to stop and assess individual frames of cardiac ultrasound scans, machine learning models integrated into clinical workflows can highlight features in the scans and perform tasks, such as taking measurements for the echocardiographer, saving them countless hours of work,” said Dr. Luong.
Given the high degree of accuracy of the machine learning model tested, she envisions that something similar will be integrated into clinical practice in the near future.
“We are still waiting for larger studies to further validate the use of machine learning in POCUS scans of left ventricular ejection fraction,” said Dr. Luong. “The AI space is evolving quickly, which is why we also anticipate its use in many other facets of heart care, including in the prediction of clinical outcomes based on diagnostics.”
Using AI to help cardiac patients find the best test or treatment
HAMILTON, ONT. – A Hamilton Health Sciences (HHS) study will harness the power of artificial intelligence (AI) to help determine which cardiac patients need an invasive procedure to check for life-threatening artery blockages to the heart, and which patients would benefit from a simpler, non-invasive test using CT scanning.
The two-year randomized control trial, where participants are assigned into the research study group or a control group, was launched in June and will involve up to 150 patients from HHS Hamilton General Hospital (HGH) and Niagara Health’s St. Catharines Hospital site.
“Very few randomized control trials of AI are happening in healthcare, so this is considered a landmark study,” said Dr. J.D. Schwalm, an interventional cardiologist at HGH and director of HHS’ Centre for Evidence-Based Implementation (CEBI), established to advance healthcare through research and education. CEBI partnered with HHS Centre for Data Science and Digital Health (CREATE) for this trial, and research leading up to it.
The trial received funding from
Hamilton Academic Health Sciences Organization and the Population Health Research Institute, a joint institute of HHS and McMaster University.
Based on previous research including a study of patient data going back 12 years, this AI tool is expected to be faster and better at ensuring patients are directed to the best test for their condition. For example, the AI tool will recommend patients for an invasive coronary angiogram if they have a higher chance of blockage in their heart arteries based on their medical information.
The AI tool can also identify patients who likely don’t have a blockage and will recommend them for CT scanning. This tool has the potential to improve patient outcomes, advance health equity and lower the cost of healthcare.
“Ultimately we want to scale this AI tool provincially, if we can prove through this latest study that it delivers what we believe it can,” said Dr. Schwalm, adding that the team is also in the process of validating this model at the provincial level with data from ICES, an independent, non-profit research corporation.
“The province, in its Auditor General report, found that there’s a need
for system-level improvements to ensure patients don’t undergo unnecessary and costly treatments,” said Dr. Ted Scott, HHS vice president of innovation and partnerships. “This new trial, and the work leading up to it, illustrate the power of AI when it is implemented using evidence-based methods to improve patient care and drive system efficiencies.”
An invasive coronary angiogram procedure is considered the gold standard for
The AI tool is expected to be faster and better at ensuring patients are directed to the best test for their condition.
diagnosing coronary artery disease, caused when vessels supplying blood to the heart get narrowed, clogged or completely blocked by plaque. It involves inserting a catheter into the patient’s groin or arm as a route to the heart via the arteries.
Then a special dye is released into the bloodstream for contrast, and an X-ray is taken to show doctors how blood is flowing and identify any blockages which can
be opened with a stent as part of the procedure, or in a separate surgery called coronary artery bypass grafting.
The problem is, all patients suspected of having coronary artery disease are sent for an invasive coronary angiogram, even though many were found to not have any significant blockage, or to have a minor condition that could be treated with medication instead of stenting or bypass surgery. In other words, many patients were undergoing this unnecessary invasive procedure.
There’s also some risk with this procedure, though it’s rare. Provincially, about one in 1,000 patients will have a bad outcome that could include a stroke, heart attack or death. HGH and St Catharines perform over 10,000 of these invasive procedures each year.
A study of Hamilton and Niagara patients found that 44 out of 100 patients who underwent an invasive coronary angiogram could have avoided the procedure, said Dr. Jeremy Petch, who leads the team of digital data and tech experts at CREATE, as the centre’s director. The remainder of patients had an obstruction and needed a stent to open clogged arteries.
VCHRI’s Dr. Christina Luong: Machine learning models can take measurements and save hours of work.
Ontario Fetal Centre’s robotics research paves way for innovation in surgery
BY SONYA FERNANDES
Ateam at the Ontario Fetal Centre, led by Dr. Tim Van Mieghem, is trialing the da Vinci Xi robot to repair spina bifida.
Since its debut at Mount Sinai Hospital, the state-of-the-art da Vinci Xi robot has revolutionized the way surgeries are performed, enabling teams to perform more complex laparoscopic operations on patients with complicated health concerns.
Building on this success, a team led by Dr. Tim Van Mieghem, maternal fetal medicine specialist at Mount Sinai Hospital, is trialing the robot to perform fetal surgery, aimed at decreasing the adverse effects of spina bifida.
Each year in Canada, spina bifida affects approximately 120 to 150 fetuses. Spina bifida is a structural defect of a baby’s central nervous system that appears when the spinal column fails to close in early fetal development, which can lead to varying degrees of disability.
There are currently two methods of repairing spina bifida: open fetal surgery or fetoscopic (keyhole) surgery.
With open fetal surgery, the large incision made in the uterus can carry long term problems, including an increased incidence of preterm birth, and uterine scarring, which necessitates cesarean delivery in subsequent pregnancies.
Although fetoscopic repair is effective in improving patient outcomes, technical challenges have been a driving force for Dr. Van Mieghem and his team at the OFC to explore other interventions.
“Traditional laparoscopic instruments are rigid and cannot easily replicate the delicate movements that you normally can make with your hands,” says Dr. Van Mieghem.
Enter the four-armed wonder, the da Vinci Xi.
This pioneering technology is currently not offered for spina bifida repair in any other clinical setting around the world; the research, which is funded by a grant from the Canada Foundation for Innovation, could transform the way this fetal surgery is performed not only at Mount Sinai Hospital, but globally.
Robots not only enhance surgical precision and control, but also require a smaller incision, which can lead to reduced patient recovery times and decreased pain post-operatively.
The first phase of research involved training on a virtual simulation model to learn the controls of the robot, and to practice surgical techniques, such as suturing.
The second phase involved the development of a model to simulate the procedure. Support was enlisted from a diverse panel of experts, including engineers for mathematical modelling, and an artist from the Ontario College of Art and Design, who designed a silicone uterus and a fetus with spina bifida.
The surgeon operates the robot from a stable and controlled environment, sitting in an ergonomic position inside of the console. The two controllers that steer the robot are linked to instruments which are carefully inserted into the uterus with small ports.
“On the silicone model we are doing the
same hand movements as we would on an actual patient. The wristed instruments on the robot can seamlessly replicate the movement that your hands make, so you have the full dexterity of open surgery combined with the benefits of a keyhole surgery.”
While the robot has not yet been put
into practice in real case scenarios, the success of these early trials sets a promising precedent for future implementation of this groundbreaking innovation to fetal surgery, on Mount Sinai patients; the extensive research has enabled the team to learn the functionality of the da Vinci Xi,
evaluate the most optimal approach to the procedure, and to course correct.
Sonya Fernandes is Marketing & Communications Specialist, Corporate Communications, Women’s & Infants’ Health, at Sinai Health in Toronto.









Healthcare lags other industries in Gen AI, but many use cases beckon
Generative AI could anticipate next steps, book referrals, populate follow-up notes and order tests.
BY ANDREW FRANCES
To the patient’s eye, a family doctor’s job begins and ends in the exam room. Medical professionals know that’s not true. According to the Ontario College of Family Physicians, doctors spend 19 hours a week on administrative tasks –reports, referrals, and more.
A full-day’s slate of patients amounts to five hours of such paperwork, and 94 percent of Ontario family practitioners feel “overwhelmed” by the workload.
“Your family doctor, on average, usually has about 1,200 to 1,800 patients,” said Dr. Chandi Chandrasena, a family doctor and chief medical officer of OntarioMD, a subsidiary of the Ontario Medical Association charged with digital health initiatives in the community.
“When they see you in your office, that’s only a small part of the work that they do. A good bulk of the work is managing the documentation: writing in the notes, the forms, reading and managing the reports that come in their EMR, letters, the messages that patients and requests.”
“Some of this administration work is expected and this is part of caring for our patients, but a large amount is the administrative burden, which is caused by the health system and the way we are expected to operate.”
Generative artificial intelligence (Gen AI) could ease that burden. In fact, medical scribe applications – which transcribe entire patient interactions, generate the corresponding paperwork and integrate with electronic health records – can save physicians up to four hours a week by reducing documentation workload by 71 percent, Dr. Chandrasena said.
Generative AI could anticipate next steps, booking referrals, populate follow-up notes for future visits and order tests, for example.
Still, healthcare, particularly in Canada, is trailing other industries in the uptake of generative AI, ac-
cording to a recent survey by data and AI firm SAS Institute and Coleman Parks.
Even though survey respondents in Canadian healthcare were more likely to consider themselves to have a good understanding of Gen AI (53 percent) than those from Canadian and global general industry respondents (51 percent and 48 percent, respectively), only 20 percent said they use Gen AI daily,
Acquisition issues remain. For example, doctors question who will pay for the AI software and training, and support contract reviews and privacy protection.
compared to 29 percent of respondents from global industry in general.
Artificial intelligence – specifically, the intersection of disciplines including predictive analytics, machine learning, speech and visual recognition, among others – has played a business role for some years now, particularly in financial institutions.
In healthcare, it has been helping predict appointment no-shows and in some radiology departments, it’s assisting with interpretations of images.
But generative or creative AI only made a commercial splash in the late 2022, and it was aimed at consumers, not business. And while it has been writing endless episodes of Seinfeld or producing convincing images of penguins playing bagpipes, it has been largely a solution in search of a business application.
“It took hold of our curiosity and of course, as individuals we’d love to play with it. What’s possible? What’s not?” said Jay Upchurch, SAS executive vicepresident of technology, and chief information officer. “(But) you’ve got to have business strategy that’s being realized by the technical application of generative AI.”
Medical scribe applications, which are numerous, check those boxes. But there are other challenges to Gen AI adoption, especially in a community health setting.
Health system pushes family doctors into other unfamiliar roles: Unlike clinicians in hospitals, family doctors must acquire software and do their own tech support. And they must pay for it out of their own pockets, Dr. Chandrasena noted.
Onboarding, training, rollout, troubleshooting – hospitals have discrete staff to deal with the technology.
“It’s a different resourcing structure in the community. It’s a different support structure in that there really isn’t anything, it’s just us” she said.

The healthcare system pushes family doctors into roles that they’re not trained for, she added. “We are trained as physicians, not administrators or IT or privacy officers, these are unfamiliar roles.
“As physicians, we want to learn about new technology and we want to innovate,” she said. “But what about legal issues, the contracts, the liability, the consent? Who’s responsible if there’s an information breach? We don’t have any protected time to learn about all of this. We’re trained to solve your problems in the medical sense, but we’re not trained to be administrators. We’re not trained to even run a clinic, and we’re certainly not trained to be privacy officers or procurement officers.”
Upchurch cautions against
Strategy and standards are needed for data interoperability
BY GURPREET (GP) SINGH
Interoperability in Canada’s healthcare environment has grown more complex. The challenges include managing data migration and archiving from legacy systems, establishing bi-directional connectivity with internal and external endpoints, and aggregating live data for insights in analytics and population health. The overarching feedback is that at its core, data exchange and actionability are still difficult to achieve. With the right data strategy, however, interoperability can be attained. As part of the data strategy, the goal is to uncover what a robust plan and workflow looks like for a health system or healthcare organization. It’s
important to explore concepts that are required to yield the most comprehensive workflows to achieve true interoperability, enabling better financial viability, patient-centered care, and efficiency across the care continuum.
Data accessibility within an organization: Breaking data strategy into three streams – infrastructure, connectivity, and reporting – we understand that a ripple in one of these areas can lead to downstream interoperability challenges, including outright data blockages. It’s important to understand what an organization has in each of these streams, and what it wishes to achieve. Infrastructure begins with optimized systems that are fueled with quality

data, can communicate electronically to avoid data siloes, and are maintained using industry best-practices. The first step to achieving a comprehensive data strategy starts with enterprise-wide rationalization – a full analysis of applications, usage, costs, and maintenance to understand where the prevailing issues stem from. This includes right-sizing data infrastructure as well as decommissioning and archiving legacy data while maintain-
ing access to important patient data. We know by now that the intelligent use of technology helps not only to reduce costs, but also ensures data quality and data integrity while allowing clinicians to focus ultimately on patient care.
Establishing connectivity internally and externally is essential to providing clinicians and administrators with complete patient records, history, and a way to ease the burdens of moving across care settings. The days of fax, email, phone calls, data siloes, and manual workflows to obtain pertinent clinical data should be behind us. Electronic data exchange between primary care, acute care, laboratories, pharmacies, and
Dr. Chandi Chandrasena
Gurpreet ‘GP’ Singh
CSA Group develops new standard to guide digital transformation
BY KAY PENN
The Canadian healthcare system is at a crossroads, grappling with unprecedented challenges. As it faces a number of factors such as accelerated digitization, labour shortages, and an aging population, the integration of digital health technology offers a promising path forward. Artificial intelligence (AI), virtual care, and big data are becoming integral to patient care, offering solutions that could reshape the future of healthcare.
However, to fully realize the potential of these technologies, a robust framework is essential. This is why CSA Group has developed CSA Z8005, Special requirements for digital infrastructure and digital healthcare technologies in Canadian healthcare facilities, a new standard designed to guide the implementation of digital infrastructure in healthcare facilities across Canada.
Without a standardized approach, healthcare facilities risk falling behind, unable to leverage these innovations to improve patient care and operational efficiency. CSA Z8005 addresses this need by providing guidance on planning and implementing digital infrastructure with a focus on scalability, security, and future-proofing.
The standard emphasizes the importance of developing a digital health vision and strategy that aligns with an organization’s goals and the needs of the community it serves. It’s not just about adopting the latest technology – it’s about integrating these technologies in a way that supports longterm growth and adapts to evolving technologies and healthcare demands.
At the core of CSA Z8005 is a comprehensive framework for digital health infrastructure that includes both strategic and tactical planning. This involves establishing a project development plan, defining work streams, and coordinating various project components. The standard also highlights the need for a governance structure, risk management, and future-looking methodologies to enable infrastructure to adapt to evolving technologies and healthcare demands.
Key to the successful implementation of digital health systems is engaging with interested parties, including clinicians, IT personnel, and patients. This collaborative approach supports digital systems to be not only technically sound but also meet the practical needs of those who will use them daily.
CSA Z8005 places a significant emphasis on the foundational elements of digital infrastructure. It provides detailed guidance on the design, construction, installation, and commissioning of critical components like data centres, telecommunication pathways, and structured cabling. These elements are essential for supporting a range of healthcare systems, from network equipment and wireless networks to nurse call systems.
The standard also advocates for planning that anticipates future growth. As digital health technologies evolve, healthcare facilities need to be equipped to support high bandwidth demands and other technological advancements. By designing structured cabling systems that can accommodate future needs, facilities can avoid costly and disruptive upgrades.
One of the most critical aspects of CSA Z8005 is its focus on integration and interoperability of digital health systems. The standard encourages the use of standardsbased and open solutions rather than proprietary ones so that different systems can communicate effectively and support clinical workflows. This emphasis on interoperability is particularly relevant considering the Connected Care for Canadians Act (Bill C-72), which aims to create a connected care system where health information can be securely accessed and shared between providers. For hospital adminis-
trators and policymakers, CSA Z8005 serves as a tool in driving the digital transformation needed to meet the demands of modern healthcare delivery.
Kay Penn is Director, Health & Safety Standards, CSA Group.
The finance, HR, and supply chain system that adapts to changes in healthcare.
In healthcare today, agility alone isn’t enough. To keep up with whatever comes your way, healthcare organizations need to plan continuously and prepare for all possibilities. Workday allows you to do just that by providing real-time visibility to reduce costs and boost revenues without compromising care.
Workday. For a changing world.™
With Montreal’s Scale AI, hospitals across Canada are testing new AI applications
The focus is on improving productivity and enabling organizations to do more with their existing resources.
BY DIANNE DANIEL
McGill University Health Centre (MUHC) in Montreal identified opportunities to perform hundreds of additional surgeries each year. Toronto’s Princess Margaret Cancer Centre decreased the mortality rate from delayed radiology treatment by up to 13 percent. And the Centre Hospitalier de l’Université de Montréal (CHUM) achieved a 5 percent increase in efficiency in its infusion clinic – amounting to 11 hours of extra treatment capacity per day – by accurately predicting patient treatment times.
How did they do it? By applying artificial intelligence (AI) to find efficiencies and optimize limited resources, the proverbial ‘do more with less’ strategy that Montreal-based innovation hub Scale AI is working to accelerate across Canada’s healthcare sector.
Funded by the federal and Quebec governments, Scale AI is on a mission to build a national AI ecosystem by helping organizations to implement real-world applications.
In October 2023, the hub announced investments of $21 million for nine AI healthcare projects as part of the Pan-Canadian Artificial Intelligence Strategy. The announcement marks the second time Scale AI decided to open a funding call geared specifically to hospitals.
The first took place during the early days of the pandemic and resulted in projects that optimized surgery schedules at MUHC and radiation patient scheduling at Princess Margaret Hospital, and led to the development of an AI-guided tool to maintain safety and quality of cancer treatment at CHUM.
“We hear a lot about how AI can be used for therapeutic applications such as pre-analysis of medical imagery … or genAI apps to facilitate report writing and patient visit summaries,” said Scale AI senior director, Investments, Marc Vaucher. “But there is a third use of AI that we promote a lot at Scale AI, which is to improve productivity, optimizing the operations around the healthcare system and allowing the healthcare system to treat more patients with the same resources.”
“We know we have limited resources (in healthcare),” said Vaucher. “If you allocate staff better, then you avoid overtime hours and reduce turnover, improve quality of life for your staff, and at the end of the day, it’s also improving the quality of care you provide to your patients.”
Global professional services firm Deloitte has partnered on several Scale AI-funded projects in the Canadian healthcare sector, including one that is applying AI to build a physician scheduling model at a large western Canadian health authority and another that is harnessing AI to improve medication adherence at a home and community healthcare provider by segmenting patients into personalized care pathways.
An earlier project, representing a total investment of $6 million with $1.8 million coming from Scale AI, was aimed at helping SE Health, a homecare and community care provider, to better manage its Ontario home care workforce – respon-
Tool for Geographic Optimization, and used by clinical and administrative managers in each region –uses the model to generate recommended team geographical boundaries on a quarterly basis, suggesting where to draw borders in order to minimize the distance travelled by caregivers so they spend more time caring for patients.
From the start, the GO Tool was designed with end-users in mind, said Deloitte Digital Studio partner Arslan Idrees, who focuses on leveraging technology to improve the citizen experience across Canada as the lead for Deloitte’s national life sciences, healthcare and aging well market cluster.
“We wanted non-technical clinical staff to be able to go in and play around, to move the line and see how it changes the whole dynamic,” said Idrees, explaining that the AI model does the heavy lifting in the background to calculate the impact on business metrics.

sible for roughly 120,000 client visits per week – at a macro level.
The nine projects included in the recent round of healthcare-focused funding range from virtual triaging and queue management in busy emergency rooms, to optimizing workflow operations and patient care management, to improving demand forecasting.
Each received a Scale AI investment of $1.5 million and though led by and deployed into specific hospitals, all projects involve a solution provider or system integrator with the goal of making the final deliverables available to any Canadian hospital.
Part of Scale AI’s role is to ensure every funded project sets out a clear change management plan that engages end-users from the beginning. The hub also structures projects in levels so that impacts can be measured at each stage of deployment and challenges can be addressed, with the intent of ensuring implementations are seen through to completion.
The goal was to create an AI-enabled decision support tool capable of better matching staff resources to patient demand while supporting the social enterprise’s over-arching goal of providing continuity of care.
“Everything we do for home care is geography based,” explained SE Health vice-president of Business Transformation, Jennifer Hayward, noting that teams operate from 13 regional service delivery centres. “Our staff are going into people’s homes across the province, so the challenge is trying to figure out what team sizes and regional boundaries are needed to optimize capacity,” she said.
The AI model built by Deloitte’s data sciences team uses postal code data from Canada Post and demographic data aggregated by Manifold Data Mining Inc. to forecast patient demand and the type of caregiver skill required at a regional level.
The decision support tool – referred to as the GO
“They can see the business impact of moving the geographic boundary – including how many patients they can serve – in real-time and then make a decision to go forward with the change or not,” he added.
Before using the GO Tool, workforce planning was a tedious manual ask that wasn’t performed very often and didn’t always provide reliable information. Now teams are better aligned, and managers have a deeper understanding of capacity and the impact that small changes can make.
“In some cases, we were pleasantly surprised that the tool validated that what we were doing was good, now we can just do it quicker,” Hayward said. “In other cases, it was ‘Oh my goodness! I can’t believe I can generate that many extra visits or better utilization just by changing this boundary.’”
Since being deployed, the AI solution has led to an increase in staff utilization, a decrease in travel time, higher patient volumes and increased employee satisfaction, she added.
Idrees said the idea behind the Scale AI innovation model is simple: we need to solve challenges in the Canadian healthcare sector and doing that requires marrying a human-centred design approach with technology to ensure the right problem is being solved in the right way.
An excellent example of that is the Scale AIfunded virtual triaging and queue management project currently under way at Humber River Health in Toronto, supported by Deloitte and the MEDITECH collaborative.
When Humber River Health first launched the project as a way to reduce patient wait times in a busy emergency department, they were focused on using AI to help screen potential patients from home and make a judgment as to whether they should or should not visit emergency.
When Scale AI and partners came on board last fall, the focus shifted. “We asked, ‘What’s the novel problem here?’ And it’s actually not the screening
function but the queuing function,” said Humber River Health CIO Peter Bak. “And that has proven to be really interesting.”
The main challenges in the emergency department are overcrowding and extended wait times due to scarce workforce and limited capacity. The idea is to solve the problem using AI, without adding resources.
The new ED Queue app is designed to provide emergency department patients with a personalized time slot that is updated according to real-time conditions in the ER, historical analysis and other factors, so that they can wait at home as long as possible before arriving at the hospital.
Currently in the pilot stage, ED Queue will be rolled out over the next three months and the project is expected to be completed by March 2025.
As Idrees explained, there are three possible scenarios: a patient is advised to call 911 immediately, get themselves to the emergency department right away, or wait at home until their time slot is available.
“We ask simple questions about how you are feeling and the magic happens at the backend,” said Idrees, stressing the time slot is not an appointment. Rather it’s a moving target that will change as circumstances change, but patients will always be in the know rather than sitting helplessly in a busy waiting room.
The shift in focus has opened up new possibilities for the app, such as partnering with a digital twin of the emergency department to better drive performance. Bak envisions a scenario in which patients are categorized into care pathways. If it’s likely they’re going to require bloodwork or an X-ray, the algorithm can be massaged to take into consideration radiology and lab capacity.
“We can actually start to coordinate the time slot not just based on activity in the emergency department, but on activity in the emergency department and the supporting services that are required,” he said.
Deloitte's and HRH's initial analysis of ED queue demonstrates that patient wait times in the ED could decrease by as much as 78 percent in the Fast-track zone. Possible future enhancements to the algorithm include adding real-time traffic data so that a patient’s estimated drive time can be included, or partnering with ride hailing apps so patients without a vehicle can book a ride from within ED Queue.
To support Scale AI’s goal of developing a Canadian AI ecosystem, the queuing app is designed to be replicable in other hospitals. The front-end user interface is decoupled from the backend so that hospitals can use their existing portals, digital platform or other form of patient engagement.
Right now, the backend data stream is integrated with MEDITECH, but the integration layer is “light touch”, meaning support for other electronic medical record systems can easily be added, said Idrees.
When it comes to implementing cutting-edge AI solutions in healthcare, Idrees believes the lack of a robust AI governance framework remains a critical challenge.
Whereas other sectors focus on outcome when embarking on an innovation project, solving security, privacy, ethical or regulatory challenges as they come along, healthcare entities tend to have those discussions upfront causing long delays.
“In healthcare, the paradigm of innovation is flipped upside down and what happens is you’re asking questions that
should be handled downstream,” said Idrees. “An AI governance framework would allow champions of the idea to make sure concerns are handled at a certain stage and the rigour depends on the stage you’re at.”
A key benefit of the Scale AI approach, said Bak, is that it allows hospitals to come with up ideas, validate them and then rely

on system integrators and partners to help commercialize them.
“We’re very grateful for Scale AI to have funded us. We’ve worked well with Deloitte and we’re very interested in commercialization,” he said. “What we’re hoping is that this is something that does indeed get scaled-out for the benefit of the Canadian health system.”









Family docs create HippoAI to speed up access to clinical data and forms
The Canadian healthcare system is facing a severe crisis with family physicians reporting record high levels of burnout across the country. A growing administrative burden, combined with the need to stay updated with rapidly evolving medical knowledge, has
created a situation where doctors are stretched thin. Among those feeling the strain is Dr. Stacy Nguyen, a family physician practicing in Toronto.
“I know that my medical knowledge, together with my time, allows me to provide the high-quality care my patients deserve,” Dr. Nguyen commented. “But the reality is that staying on top of the latest medical information is becoming increasingly difficult.”
medical reference texts – many of which are hundreds of pages long.
About two-thirds of her patient encounters, she said, generate clinical questions that require her to delve into dense,

AI Scribes: More Time with Patients, Less Time on Paperwork






The challenge of accessing timely and reliable information adds to the growing physician burnout. The burden isn’t limited to medical guidelines alone – doctors must also navigate pharmaceutical information, insurance policies, and billing rules, all while trying to provide comprehensive care to their patients.
In fact, research shows that doctors would need to spend 29 hours reading in a single day just to stay up-to-date with the latest medical publications – a task that is simply impossible.
Recognizing the need for a solution to this problem, Dr. Nguyen, alongside cofounder Dr. Omri Nachmani, developed HippoAI – a new clinical reference tool designed to revolutionize the way clinicians access medical information at the point-of-care.
Their company, Pendium Health, has set out to save physicians time so they can focus on high quality interactions with patients.
At its core, HippoAI harnesses AI-powered algorithms to simplify the process of finding reliable answers to clinical queries.
“We took the hours-long manual search and reading process and reduced it to just a few seconds with HippoAI,” said Dr. Nguyen.
“The tool allows physicians to enter clinical questions in natural language, and using HippoAI’s proprietary medical specific search algorithm, doctors receive a concise, relevant answer sourced from a comprehensive database of trusted Canadian medical resources.”
In addition to Canadian clinical practice guidelines, HippoAI’s database includes general medical references (in partnership with Merck Manuals), Health Canada-approved drug monographs, and provincial drug formularies.
Unlike other popular medical databases, HippoAI allows for contextual, case-based queries, enabling doctors to adapt their searches in real-time.
HippoAI’s initial users have been overwhelmingly positive in their feedback. As Dr. Harpreet Arora of Cambridge, Ont., said, “Great product and idea. I was using ChatGPT Pro to enhance my work but knew that the answers were not always accurate. This product [HippoAI] has been amazing.”
While AI tools have become more accessible in recent years, many physicians have remained skeptical about their use due to concerns about accuracy and reliability. HippoAI addresses these concerns head-on by sourcing its answers only from trusted resources and enhanced by a platform with built-in guardrails to prevent misinformation and hallucinations.
Dr. Gritters, a rural family physician and early user, emphasized how much time the tool saved during his workday: “I no longer have to read through long articles to find the answer I need, it is such a time saver.”
For any clinician interested in signing up for HippoAI, the Pendium Health team offers a free trial of the reference tool as well as free onboarding sessions to get users started.
The HippoAI mobile application will also be available for use in the coming months on the IOS app store.
Medtronic leverages AI and partnerships to solve healthcare’s challenges
As Canada’s healthcare system faces unprecedented strain, Medtronic Canada is building on decades of innovation and harnessing the power of artificial intelligence (AI) to help hospitals transform patient care and improve operational efficiency.
The health system continues to grapple with a host of challenges: A chronic shortage of family doctors and other healthcare professionals is making it harder for millions of Canadians to access timely care. A significant number of seniors are in hospital waiting for a long-term care bed. There are long wait lists for surgeries and other treatments. And emergency departments are packed with patients having difficulty finding the care they need in the community.
At a time when Canadians are living longer with more complex illnesses, these challenges are making it more difficult for patients to access the care they need, when they need it.
Medtronic is working with hospitals, other innovative technology and digital health companies, and partners across the healthcare system to leverage the rapid evolution of AI as part of the cure.
“Bringing novel solutions and services to the table to help hospitals and health organizations overcome challenges is not new to us. For many years, we’ve been
working with hospitals to deliver operational efficiencies, improve capacity and help improve patient access to care,” says Rob Clifton, president, Medtronic Canada. “AI and machine learning are the latest tools we’re using to help our partners solve problems and focus on patient care.”
Medtronic is adding innovative AI technologies to its research and design capabilities to push the boundaries of innovation. Already, AI plays a pivotal role in the company’s robotic-assisted surgery platforms, colonoscopy and endoscopy systems, cardiac monitoring, and insulin pumps technology.
For example, Medtronic recently launched the first computer-aided endoscopy module using AI during colonoscopies to enhance visualization, analyze imagery in real-time to help physicians identify polyps, including those with flat (non-polypoid) morphology.
The system – called GI Genius – relies on a deep-learning algorithm to act as a second set of eyes for physicians.
It scans every visual frame of the procedure in real-time and highlights suspected regions to physicians of the presence of lesions – including small, flat polyps that can easily go undetected by the human eye. Earlier detection, powered by AI, enables hospitals to increase colon cancer prevention.
Medtronic is also leveraging the huge data-crunching power of AI to help hospitals better detect patients who may have cardiac disease. In two pilot projects, Medtronic is working with cardiology

clinics to review and analyze diagnostic images with a custom-written algorithm to identify patients who may have underlying aortic stenosis.
These patients are flagged for further investigation by a cardiologist who can then confirm the finding and determine a course of treatment.
“These pilots are about helping hospi-
tals improve access to care and potentially provide better outcomes for patients,” Clifton explained. “Already, Medtronic’s AI tool is helping hospitals find patients whose disease might otherwise not have been detected as early.”
As it embraces AI to help overcome challenges across the healthcare system, this fall Medtronic is preparing to launch a comprehensive suite of services, called CarePath IQ, which is designed to optimize patient pathways through cuttingedge technologies and expert consulting.
CarePath IQ offers turnkey solutions developed in-house by Medtronic and by a carefully curated list of strategic partners, including specialists in AI, health informatics, remote patient monitoring, and digital platforms for patient engagement and education.
Medtronic’s consulting services in operational excellence will continue to ensure that healthcare organizations are not only efficient but also effective in delivering exceptional patient outcomes.
“We are all in this together and there’s a role for technology to play to address some of these challenges,” added Clifton. “Technology is part of the solution, but it needs to work in partnership with people and processes to deliver the best possible outcomes for patients and our healthcare system.”
Digital Twin technology can transform population health management
BY MICHAEL MILLAR
We hear it often: healthcare doesn’t need more technology. It’s hard to disagree. For many clinicians, the prospect of new technology means more steps added to their workflow, more time staring at screens, and consequently, less time spent interacting with patients.
Nowhere is this truer than in primary care. Family doctors spend in excess of 19 hours per week on administrative tasks, based on a 2023 Ontario College of Family Physicians survey of more than 1,300 family doctors. And nowhere else in our health system are the effects of burnout more consequential.
A staggering 40 percent of family physicians say they are considering retiring in the next five years, according to the 2022-23 OMA member survey. Another recent survey found that twothirds of family physicians plan to change their practice model, reduce their hours or retire in the next five years. At a time when more than 2 million Ontarians are without a family doctor, this is simply not sustainable.
Primary care is the foundation of our health system and underpins recent provincial efforts to better manage population health through initiatives like Ontario Health Teams. However, you can’t manage what you cannot measure, and the nature of modern health data makes measuring difficult, if not impossible.
How can a family doctor reasonably
be expected to enroll their patients in relevant cancer screening programs when the process of finding eligible patients is yet another manual, time-consuming task (on top of all their other, manual time-consuming tasks)?
Effective population health management in primary care requires the ability to handle and analyze vast amounts of patient data, much of which is stored in disparate electronic formats and medical records. This challenge is compounded by the fact that much of the information in EMRs is unstructured free text notes, which makes it hard to analyze and use effectively for larger-scale population health initiatives.
A novel approach in this space is to bridge the gap by creating a digital twin – a virtual representation of an entire patient’s healthcare journey – using data from multiple data sources (e.g., primary care data, hospital information, provincial data repositories). This allows for a more refined, holistic approach to managing population health, focusing on proactive care and early intervention, particularly for at-risk populations.
So, what does this look like in action? One example is to convert free-text fields into a structured, machine-readable format using the International Patient Summary (IPS) standard.
This ensures that the data is interoperable across different platforms and systems. Canada Health Infoway has made great strides in expanding the uptake of this approach through their localization efforts by creating the pan-
Canadian Patient Summary (PS-CA), a key pillar of their pan-Canadian Interoperability Roadmap.
The structured data can then be used for further analysis, driving more precise decision-making in population health management. Importantly, this approach does not disrupt the workflows of primary care providers, as it can be automatically triggered to run in the background without the need for clinician intervention.

Once the data is structured and machine-readable, the next step is to make it useful for clinical purposes. This can be achieved by encoding and normalizing clinical concepts related to a target condition. The process involves mapping clinical data to the Unified Medical Language System (UMLS), a standardized language for medical terminology that includes many of the most commonly used standards (e.g., ICD-10, SNOMED). By doing so, we ensure that all clinical concepts are aligned and consistent, allowing for accurate comparisons and analysis across different EMRs and other health information systems.
The ability to map clinical concepts in this way is crucial for identifying at-risk patient cohorts. With a clear, normalized dataset, a digital twin enables healthcare
providers to identify patients who may be on a suboptimal health trajectory. This early identification is key to proactive care, allowing for timely interventions that can improve outcomes and reduce the strain on healthcare systems.
With clinical concepts encoded and data unified, the next step is all about recreating patient pathways for a given chronic condition. This digital recreation of patient journeys provided invaluable insights into where patients might be falling through the cracks and offers a way to intervene earlier in the care process.
This capability allows for targeted, proactive interventions designed to improve health trajectories before patients reach critical stages of their conditions. For example, the results of a patient’s worrying blood test can automatically be flagged to their family doctor to prompt a check in or enrollment in a conditionspecific support program. Instead of needing to review their entire roster of patients in detail to identify at-risk patients, clinicians can use AI to automatically surface those that are relevant.
The use of digital twin technology offers exciting opportunities for improving the quality of care by enabling proactive, data-driven decision-making. But like all new innovations, its adoption depends on its ability to provide value without increasing the administrative burden of clinicians.
Michael Millar is the CEO and founder of Verto Inc., a Toronto-based digital health organization.
GI Genius acts as a second set of eyes for doctors.
Michael Millar
Why Canada needs to accelerate AI adoption in healthcare diagnostics
BY LOUISE PICHETTE
Imagine finding a strange lesion on your leg. Typically, you’d book time to see your doctor, have some tests done, get a referral to a specialist, and then wait about seven months to secure an appointment. What if there was a better way?
Imagine if you could take a photo of your leg with your phone and send it to a physician. A few minutes later, that photo could be fed into an artificial intelligence (AI) tool that informs your physician of the severity of the lesion, which can then help them make the decision on whether to treat it with a simple topical cream or flag for immediate attention: no bloodwork, no wait times, no stress.
This scenario isn’t that far off from reality. Advances in AI-driven diagnostics are helping doctors make faster, more accurate decisions without requiring patients to undertake invasive procedures, wait for test results or even visit a clinic.
Canada is a powerhouse in AI and many of these smart diagnostic tools are being built here, such as Toronto’s Mimosa Diagnostics, which has developed a mobile health platform that uses near-infrared light and AI to monitor skin injuries.
Linda Lifetech is working on a contactless breast cancer detection tool that could help make more routine screening more accessible. And Retispec is harnessing AI to screen for early biomarkers of Alzheimer’s during routine eye exams.
Tools such as these can help Canada’s overtaxed healthcare system by triaging cases based on the need for care or offloading to other providers like pharmacists, which frees up valuable physician time and provides relevant clinical decision support.
The impact of these solutions could be significant: If AI tools were used at scale in
healthcare, Canada could save as much as $26 billion each year – nearly 10 percent of its yearly spend.
However, while Canada is a leader in AI development, the country lags behind in the adoption of the technology at the organizational level. Report after report underscores the need for Canadian businesses to accelerate their AI adoption strategies if they want to remain competitive on the global stage.
To realize the potential of these gamechanging diagnostic tools, our health-tech entrepreneurs need much more support.
“In Canada, we currently lack sufficient funding programs to support early-stage prototype development and clinical validation,” said Saumik Biswas, CEO and cofounder of Tenomix.
A lack of funding, resources and physician availability is slowing down progress for Biswas’s London, Ont.-based medtech company, which is streamlining colon cancer scanning using AI. Its bench-top device, which radically speeds up the search for cancerous lymph nodes in biopsy samples, is undergoing clinical engagements and usability testing has the potential to reduce wait-times and improve accuracy for colorectal cancer diagnosis.
But there needs to be funding with milestone-based checkpoints that enable innovative medtech companies to engage with hospitals throughout the entire product development lifecycle, Biswas said. “This is especially crucial for startups in the early minimum viable product stages,” he added. “Insights from clinical partners – on the economics of the clinical problem, usability and workflow integration – can save significant time and resources in the long run while ensuring that the solutions being developed address real-world clinical needs.”
That close-knit collaboration between medtech startups and physicians is starting
to take shape in places like the Nova Scotia Health Innovation Hub in Halifax. Its researchers work on more than 1,400 research projects annually with 17,500 participants and collaborate with clinicians and staff to identify solutions and help validate homegrown ideas.

A focus on delivering virtual care across the province has led to a partnership with Virtual Hallway that connects primary care providers with specialists to seek advice on patient care.
Meanwhile, hospitals are embracing AI with some even creating their own in-house AI teams to develop customized tools aimed at improving internal systems and protocols. Unity Health Toronto was the first in Canada to do so and has launched more than 50 AI tools into regular practice across its healthcare network.
Indeed, it’s a start, but AI-focused startups also need access to capital, and we have yet to see investment happening at a scale that could significantly move the needle.
Last June, Canada’s Strategic Innovation Fund committed to spending $10.7
million to help fund research and development work for seven medtech companies, including Mimosa Diagnostics. That funding will help Mimosa continue its commercialization plans, both here and in the U.S., while also working to develop its technology for other health issues its mobile platform can help monitor.
Meanwhile, Tenomix closed a funding round earlier this year that raised $2 million from several investors including the Ontario Centre for Innovation (OCI).
While these are good investments from federal and provincial policy-makers, it’s still a drop in the bucket of what most early-stage medtech startups require to get their novel technologies into hospitals and in front of physicians, especially considering Canada spends about $200 billion in total healthcare spending each year.
The quicker AI is embraced in healthcare, the sooner we can start saving lives, reducing unnecessary strain on our doctors and nurses, and building a system that can work better for everyone. Canada has the talent and the means to lead this AI revolution. Let’s work together and make it happen.
Louise Pichette, senior manager of health sciences at MaRS Discovery District, works with local and international communities to help the most promising Canadian biotech and medtech startups achieve their greatest potential.
Project to enhance shared access to records
managed services, project management, and training of staff. Essentially everything it takes – I.T. wise – to get up and running, and stay on track,” said Roffey.
A unique part of the project includes a
Bayshore’s AI Wellness Notes aims to improve homecare
BY MICHELLE RAMOS
Bayshore HealthCare (Bayshore) is set to transform the homecare experience in Canada with the upcoming launch of its artificial intelligence (AI) Wellness Notes feature on its MyBayshoreCare (MBC) digital platform.
Available on mobile and web browsers, MBC is a secure online hub designed that provides clients and families with everything they need to know about their personal or loved one’s home healthcare.
The AI Wellness Notes feature is designed to support caregivers by automatically refining the language in their notes, making them easier to understand. It will use AI to enhance the grammatical accuracy and clarity of caregivers’ documentation, ensuring high-quality communication throughout the caregiving process.
Dorie Marcellus, a registered practical nurse with Bayshore in Hamilton, Ont., believes the AI Wellness Notes will
significantly enhance the experience for family members.
“The Wellness Notes feature helps families stay included in their loved one’s care when they can’t be around at all times and creates a better relationship with the care team,” she said. “With clearer and more concise updates using AI, families will easily be able to stay informed about their loved one’s health. This will provide them with peace of
AI Wellness Notes is designed to support caregivers by making their notes clearer and easier to understand.
mind and foster better communication.”
This enhancement is essential in healthcare, where accurate communication can greatly affect patient results. In addition to text documentation, caregivers can also take and attach photos of the person in their care, allowing for a richer, more comprehensive record of
the patient’s health status.
Besides improving documentation quality, the AI system provides robust summarization features. It can review wellness data to create detailed health overviews, highlighting key trends and information. This is especially helpful for managing patients with complex conditions where tracking subtle changes over time is essential.
“The upcoming AI Wellness Notes is a significant step forward in our mission to leverage technology for better patient care,” said Dheeraj Paul, chief digital officer, Bayshore. “By improving the accuracy of caregivers’ notes, enabling photo documentation, and providing a more holistic view of patient health, we are empowering our teams to deliver more effective and personalized care.”
One notable aspect of MBC’s AI Wellness Notes is its flexible date range feature, enabling users to create wellness summaries for selected time frames. This will allow caregivers and healthcare professionals to track a patient’s health progress over selected time frames.
patient portal, called HealtheLife, where patients have secure access to their own health record, including a list of medications with instructions, test results, upcoming appointments, physician notes and educational resources. This reduces paper and handwritten notes and gives caregivers a convenient place to review details from patient appointments.
With the integration of technology in their workflows, clinicians can expect an improved patient-caregiver experience thanks to better data, fewer medication errors and less duplication of patient tests. Moreover, the cluster sites will have a closed-loop medication management environment that will reduce errors and potential patient harm, all leading to significant improvements in patient safety and best practices.
“On the cusp of AI, we’ll be using data more effectively along the way of the patient journey,” said Roffey.
After the go-live, Nova Networks intends to assist, ensuring everything is running smoothly, and any problems or scenarios can be resolved efficiently by the current I.T. team. “We’ll require support for numerous months to address post project stabilization,” said Cohen. “We’ll review our needs as they emerge.”
Currently, the care team is in training and feedback has been positive. “The biggest challenge is in people changing how they work, and learning to do it differently,” said Cohen. “We are doing our utmost to ensure that our staff is well supported with the appropriate training, tools and post-live resources to ensure a smooth transition from paper to the digital world.” CONTINUED FROM PAGE 12
Louise Pichette
Driving digital success
benefits of that initiative. This mismatch can lead to initiatives with great value to other parts of the health system not being implemented.
Successful examples, like the rapid adoption of virtual care during the COVID-19 pandemic, demonstrate that with the right infrastructure, clear value proposition, and sufficient investment, scaling can be achieved. However, addressing resistance to change and misaligned incentives is critical to ensuring broad implementation of these innovations. Leveraging key drivers such as a compelling business case, adequate funding, and a supportive regulatory environment can help overcome barriers.
Achieving lasting success requires designing systems for scale from the beginning. Often, systems are implemented without considering how they will connect, which leads to fragmentation and costly integration efforts. A forward-thinking approach and collaboration across all parties and all geographies ensures that digital health innovations can be scaled effectively and sustainably. Roundtable participants have had success with transformative change by aligning objectives, sharing lessons learned, and coordinating efforts.
Overcoming cultural resistance was mentioned throughout the discussion. All agreed that the ingrained mindset of “this is the way we’ve always done it” creates substantial barriers to change.
Healthcare professionals may be hesitant to change their established workflows or don’t have the capacity to learn new methods. Demonstrating tangible, realtime outcomes builds momentum for adoption. For example, when clinicians see
positive results, they are eager to adopt. Shorter evaluation periods and clear, immediate results can significantly reduce reluctance, ensuring that technology is embraced by frontline workers.
In Canada, the fragmented, provincially mandated healthcare system adds complexity to national efforts. While many acknowledge the need for change, entrenched practices and varying priorities and needs can make it difficult to break from outdated systems and approaches.
To address these hurdles, small, strategic shifts rather than sweeping legislative changes may offer the best chance for success. By focusing on collaborative, incremental improvements and encouraging
Healthcare
people to solve problems for themselves and for the broader system, organizations can start to shift cultural norms, share the workload, and avoid duplication.
Easing the entry points for others to participate in these changes – by standardizing specific language in RFPs for healthcare operators, for example – is one way to gradually push the system forward, fostering a culture that embraces innovation while balancing the need for stability and familiarity.
“With these three levers – some rules, some ‘moral suasion’ and some funding, then most things are achievable”. –
Simon Hagens Canada Health Infoway
Final insights: As the discussion concluded, the critical role of strong leadership in driving successful technology implementation was emphasized. In this context, it’s important to note that leadership was defined by mindset, and not by title. While technology serves as a powerful enabler, it is leadership that ensures initiatives are endorsed, scaled, and sustained. Without strong leadership guiding people, culture, and collaboration even the most promising innovations risk stalling. Fostering a culture of continuous learning and innovation will be essential to scaling digital health initiatives and moving beyond the argument “we’ve always done it this way”.
lags in Gen AI, but many use cases beckon
losing sight of the “Gen” in GenAI, especially in healthcare.
“It’s generative. It’s trying to predict next best word (or to be) creative,” he said. “And in a lot of cases, businesses can’t be creative when trying to make business decisions, or healthcare decisions about treatment or drug development or something like that. That’s where other AI techniques come into play, and we need to make sure that we again apply Gen AI in a point-specific way that is effective to the business outcome or need.”
Enter synthetic data: One such application is the development of synthetic data. GenAI can be used to generate masses of data consistent with a smaller volume of actual data collected, providing a bigger dataset for theoretically more accurate analysis. It’s also literally anonymous; it can’t
Uof T helps place the data scientists
completed a short but intensive course in data science, rather than a person who may have done several years in a universitybased computer science program?
Sepehr: In the long term, it’s the personality and the drive that you get from the person, rather than technical skill. It might be counterintuitive to a lot of hiring managers, because there’s a lot of focus on the resumes. But it’s somewhat ridiculous in terms of what is expected of candidates these days. Even when hiring for a junior role, everybody’s expecting five years of experience, which is unrealistic.
We’d rather hire someone who can think outside the box. We like to get a sense of their problem-solving skills. At the end of the day, that gives us a good indication of their skill set. And of course, we also look at their personality and whether they’ll fit in our team or not.
Canadian Healthcare Technology: Do you have confidence in the training DSI participants receive?
Sepehr: For sure, I mean U of T is obviously a very credible university and a credible source of talent. I came in contact with the DSI a while ago and learned about their programs. I myself used to do data science mentorship a few years ago,
and I worked with aspiring data scientists. Once I learned about this program at the University of Toronto, I reached out and had a conversation. I wanted to work with them, as we had available positions. We wanted to part of their program and draw on their people.
Standards needed
CONTINUED FROM PAGE 16
vendors needs to happen more regularly within the Canadian healthcare ecosystem. Transformational connectivity, leveraging tools to meet each endpoints connectivity methodology, protocol, and specification will help healthcare organizations to achieve meaningful data exchange and provide actionable solutions to improving patient care and outcomes. Initiatives within CIHI and Infoway to produce the Canadian Core Data for Interoperability (CACDI) patient summary is an impactful example of what standards-based connectivity can look like at scale. With infrastructure and connectivity in place, reporting for population health, analytics, research, and national registries becomes much more achievable within one repository. The benefits of having normalized, aggregated data
be attributed to individuals that don’t exist. This is a guardrail for healthcare practitioners looking to share data for in-depth analysis of trends and training AI models.
“We’re always worried about privacy and data handling and governance and management of that data. In some cases, creating
AI could be used to convert a medical encounter into discrete data fields, which are then loaded into a central record.
synthetic versions of that will allow us to move a little bit faster,” Upchurch said.
For example, he explains, researchers could model the impact of an event like 2020’s COVID pandemic. The data set might not yet exist. “Then it’s a question of, can I create a version of that data that would emulate things that start to suggest a pandemic? And then, can I model out what that would do to my supply chain and how I could handle that?
It always starts with data: Most conversations related to technology adoption in healthcare begins with the quality of the data, not the predictive or machine learning models, said Dr. Onyi Daniel, board member for the Sinai Health System in Chicago and former vice-president of data and analytics strategy for Highmark
should not be understated – it can change the way healthcare organizations diagnose, treat, practice medicine, and operate. This tenet requires the reliability of data exchange from disparate sources to make meaningful impact.
Utilizing this framework, organizations can work to achieve their individual data strategies. However, without re-
Examples of large-scale interoperability can be found in healthcare projects in the UK and United States.
quirements for standards, and the acceptance and deployment of these standards, Canadian healthcare organizations will continue to face challenges when it comes to system-wide interoperability and data sharing.
Enabling national standards-based data exchange across the care contin-
Health, an American national non-profit healthcare company based in Pittsburgh.
“It really starts upstream at the data collection, the data quality, and the data governance,” she said. [The emergence of generative AI] “has sparked a little bit more of investment and attention to that upstream data quality, data collection, and data governance, ... so that we are including all the populations, specifically the target populations which cross all demographics, groups, etc., in the model building.”
Even with some of the challenges associated with GenAI adoption, Dr. Chandrasena sees an upside to AI in healthcare as well.
“Could AI be used outside of just AI Scribe? Could it populate forms, can it auto-populate requisitions, referrals, different platforms? Could it auto-populate my electronic health record (EMR) using proper terminology and coding?
Dr. Chandrasena said AI scribe is just the beginning, but it can do more.
“We always talk about the incredible need for “one patient, one record,” she said. “So, during these visits with your physicians, your nurse practitioners, your social workers or any health professionals, could AI convert the discussion into discrete data fields that then get exported and put into the “one record” for your patient that travels with them from province to province? I believe so. We’re just not there yet.
uum: Looking to examples of connectivity at any point of care (primary care organizations, acute care settings, laboratories, pharmacies, national registries, etc.), real-time lessons can be learned from national frameworks like the Trust Exchange Framework and Common Agreement (TEFCA), as well as the CommonWell Health Alliance to understand how to implement interoperability at scale across a country of disparate data sources. At ELLKAY, we support the push to a national data exchange standard to encourage continuity across the care setting and improve the clinician and patient experience.
Gurpreet (GP) Singh, vice president of interoperability solutions at ELLKAY, leads the company’s interoperability solutions. He helped earn ELLKAY the position of Technical Service Provider for CommonWell Health Alliance and is involved in interoperability initiatives in the Canadian market.

