




For more information on how philanthropic gifts can help support our research, teaching and patient care missions, contact:
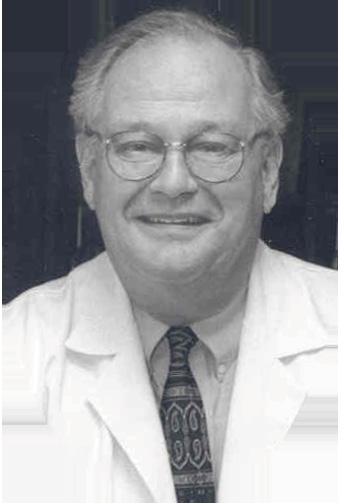
Leonard G. Gomella, MD, FACS
The Bernard W. Godwin Professor of Prostate Cancer Chair, Department of Urology
Senior Director Clinical Affairs, Sidney Kimmel Comprehensive Cancer Center, Thomas Jefferson University
Enterprise VP for Urology, Jefferson Health 1025 Walnut Street, Suite 1100 | Philadelphia, PA 19107 215-955-1702; Leonard.Gomella@jefferson.edu
P. Kenneth Brownstein, MD, FACS
Department of Urology Director of Philanthropy
Harold A. Honickman Physician Director of Jefferson Signature Services
Office of Institutional Advancement
Thomas Jefferson University and Jefferson Health 1101 Market Street, Floor 22 | Philadelphia, PA 19107 215-503-2111; Kenneth.Brownstein@jefferson.edu
Elena Boroski
Director of Development, Office of Institutional Advancement
Thomas Jefferson University and Jefferson Health 1101 Market Street, Floor 22 | Philadelphia, PA 19107 267-225-8380; Elena.Boroski@jefferson.edu
“Jefferson Urology 2024 Year in Review”
Design and Production Editor: Tricia Shea
Editor-in-Chief: Leonard G. Gomella, MD
Associate Editor: Marlene Vallett
Contributors:
Elena Boroski
Sonny Figueroa, MD
Tricia Gomella, MD
Jennifer Hagerty, DO
Kyle Harding
Janice Harper
Lisette Hilton
Alex Kolesnikov
Amy Leader, PhD
Denise Tropea
Photography:
Robert Neroni, Karen Kirchoff, Britney Lillya, Ellen Miller
Additional Department of Urology information can be found at: www.jefferson.edu/university/jmc/ departments/urology
For digital versions of “Jefferson Urology 2024 Year in Review” and other years 2019-2023, search “Jefferson Urology” on the issuu.com website.
Published by the Department of Urology, Sidney Kimmel Medical College, Thomas Jefferson University 1025 Walnut Street, Suite 1100, Philadelphia, PA 19107 215-955-6961 (tel), 215-923-1884 (fax)
Correspondence: Dr. Leonard Gomella, Editor, leonard.gomella@jefferson.edu
Copyright @2025 Thomas Jefferson University. All rights reserved. v2.0
FEATURES
4 Jefferson Urology’s 1st 200 Years
12 History of Pediatric Urology
20 Honickman Center Opens
22 Urology Expands in NJ
23 Lehigh Valley Urology Joins Jefferson Health
TECHNOLOGY UPDATES
26 Urologic Technology 2024
FACULTY PROFILES
30 Patrick Shenot, MD, FACS
31 Deborah Glassman, MD, FACS
32 Masaya Jimbo, MD, PhD
33 Notable and Newsworthy
38 Media and Web Events 2024
40 Staff Spotlights
MEETING ROUNDUP
43 AUA Meeting 2024
44 AUA Reception
45 Mid-Atlantic AUA Annual Meeting
GLOBAL AFFAIRS & INTNERNATIONAL ENGAGEMENT
46 India Connections ICMOE MedOptics
47 Fatuma Doka Uganda Trip
48 International Visiting Trainees
49 Dr. Gomella, Martini Clinic Visit KLE Student Rotations
VISITING PROFESSORS & GUEST LECTURERS
50 DM Davis Visiting Professor 2024
52 Brownstein Lectureship
53 2024 Grand Round Speakers
COMMUNITY OUTREACH & ENGAGEMENT
54 Community-based Prostate Cancer Screening Programs
56 BCAN Walk
RESEARCH UPDATES
57 Clinical Trials Division Philadelphia Prostate Cancer Working Group
58 Biome Project Racial Disparity on Prostate Cancer
60 Alumni News
64 Residents and Fellows 2024-25
68 2024 Graduation and Awards
73 Special 2024 Graduation Celebration
78 Student News
82 Faculty Listing
84 Year in Photos
88 Publications
90 2025 Scheduled Events
91 CSGUS 2025
Dear Friends and Colleagues:
The past year, 2024, was a very important one in Jefferson’s history. We celebrated the 200th anniversary of Thomas Jefferson University. Our new SKMC Dean, Dr. Said Ibrahim, completed his first year on the job and we welcomed Dr. Susan Aldridge as the 7th and first female president of Thomas Jefferson University. This issue of our “2024 Year in Review” presents Jefferson’s first 200 years and the related history of our Department of Urology (page 4). Our University’s bicentennial year officially ended with the closure of the Jefferson Time Capsule. A copy of our 2004 Department of Urology 100-year anniversary publication was selected for inclusion, with the Time Capsule to be opened in 2074, 50 years from now (page 85).

The year was also noteworthy for the designation of the Sidney Kimmel Cancer Center as a Comprehensive Cancer Center, now officially known as the SKCCC, the highest level recognized by the National Cancer Institute (NCI) and one of only 57 in the US. It was a great pleasure for me to see this top designation. I arrived at Jefferson in the late 1980’s as a recruit from the NCI to help our visionary medical school dean, Dr. Joseph Gonnella, establish a true cancer center at Jefferson. Since our first clinical cancer center designation as the SKCC in 1996, I’ve participated in our center’s development over the years. Congratulations to Dr. Andrew Chapman, Director of the SKCCC, and the center’s leadership on this achievement.
Another noteworthy event in 2024 was the opening of the new state-of-the-art Honickman Center on 11th and Chestnut Streets. You can read more about this important new clinical center and Urology’s space on the 11th floor on page 20.
The Department of Urology and our related Enterprise Urology practices continue to expand in Jefferson Health. This includes the growth of our Sidney Kimmel Medical College/Jefferson Urology Physicians (JUP) footprint in South Jersey (page 22), the addition of many new Jefferson system hospitals, now totaling 32, and multiple new affiliated Jefferson Medical Group (JMG) urology practices. Our latest Jefferson Health urology expansion is the 2024 merger with the Lehigh Valley Health Network, and we look forward to our Urology partnership with them (page 23).
Some of our departmental leadership changes in 2024 are noteworthy. Dr. Perry Weiner is now our Clinical Director for Jefferson Urology Practice Operations. Dr. Weiner will manage day-to-day clinical practice operations at all of our 5 sites and work closely with Marlene Vallett, Enterprise Ambulatory Operations Manager along with our physician site directors. With Dr. Weiner’s new role, the leader of the Men’s Health Program will be Dr. Paul Chung working with Associate Directors Drs. Perry Weiner, Irv Hirsch and Masaya Jimbo. Dr. Jimbo is our newest faculty addition. He completed an MD/PhD at Sidney Kimmel Medical College, a residency at the Mayo Clinic, and a Men’s Health Fellowship at the University of Utah. Beyond his Men’s Health training, he brings new expertise in urologic microsurgery to Jefferson Health (page 32).
With 2024 behind us, we look forward to the upcoming year’s activities. We are honored that Dr. Inderbir “Indy” Gill will be our 2025 David M. Davis Visiting Professor. Dr. Gill is Chair of Urology at the University of Southern California in Los Angeles and one of the most internationally recognized practitioners and innovators in the field of robotic surgery. Our Martin Dresner Jefferson Urology Achievement Award will be given to Dr. Frank Keeley, a 1996 residency graduate. Dr. Keeley has been practicing in England since he completed his endourology fellowship in Scotland and has held many important roles in the British Urology system.
The Department of Urology is honored to have been selected to host the October 2025 annual meeting of the Clinical Society of Genitourinary Surgeons (CSGUS). CSGUS members represent an elected group of urology chairs and other leaders, who will spend 3 days learning about our Department, the University and our city’s rich history (page 91).
There is much more to read about inside our “2024 Year in Review.” Other topics include our new Prostate Cancer Focal Therapy Program and other new urologic technologies and changes in our Division of Pediatric Urology. Dr. Sonny Figueroa has transitioned leadership at Nemours Children’s Hospital to Dr. Jennifer Hagerty.
Thank you for your support of our department and for reading our 2024 yearly update. Contact me if you have any questions.
Sincerely,
Leonard G. Gomella, MD, FACS
The Bernard W. Godwin Professor of Prostate Cancer Chairman, Department of Urology Senior Director Clinical Affairs, Sidney Kimmel Comprehensive Cancer Center Enterprise VP for Urology, Jefferson Health Office: (215) 955-6961 leonard.gomella@jefferson.edu

In 1969, Thomas Jefferson University was established that incorporated Jefferson Medical College, the College of Allied Health Sciences, the College of Graduate Studies and the Jefferson Hospital. Philadelphia University was founded in 1884 as the Philadelphia Textile school. In 2017, the merger of the two universities established the “new” Jefferson (Philadelphia University + Thomas Jefferson University).
Thomas Jefferson University was originally founded as Jefferson Medical College in 1824, the 5th medical school in the U.S. Dr. George McClelland petitioned Jefferson College at Canonsburg (now Washington and Jefferson College) to add a medical school to their institution. While technically part of Jefferson College in western Pennsylvania, Jefferson Medical College was to be in Philadelphia under the direction of the medical faculty. By 1838, Jefferson Medical College gained its own charter and was no longer affiliated with Jefferson College. As a proprietary school, the faculty administrated and managed all the finances of the school. This included the sale of “tickets” to attend lectures to support faculty salaries.
When Jefferson Medical College changed from a proprietary private institution to a non-profit status in 1895, the Professors in basic sciences became salaried, and the Professors in clinical branches obtained minimal stipends. (Editor’s Note: In the late 1950’s and through the 1960s the JMC Clinical Chair’s became fully salaried and previous volunteer Chairs were phased out).
An infirmary to treat the poor was established in 1825 with this facility to treat indigent patients under student observation; it was the first instituted by any medical school in the United States. Eventually, all U.S. medical schools adopted Jefferson’s example of combining lectures with practical hands-on patient experience.
Samuel D. Gross, MD, was the fourth Chairman of Jefferson’s Department of Surgery (1856-1882). He was considered the foremost surgeon in Philadelphia, and among the most celebrated U.S. surgeons in the 19th century. While he is best remembered as the surgeon in Thomas Eakin’s 1875 painting, The Gross Clinic, he also authored some of the most widely read medical texts of his time.

Jefferson Medical College Hospital surgical amphitheater known as the “pit” used to demonstrate surgical cases. Dr. Orville Horwitz, first chair of Jefferson’s Department of Genito-Urinary Surgery, is seated along the right wall of the "pit" with clinic staff who are posing in the clinical amphitheater of the 1877 Hospital.
Photo dated 1907. (https://jdc.jefferson.edu/historical_photos/497/)
In the 1800’s, surgeons practiced all types of surgery from abdominal, orthopedic, obstetric and ophthalmic. It should also be recalled that Dr. Gross was also an eminent urologic surgeon. In 1851, he wrote one of the first American urologic texts: Practical Treatise on the Diseases, Injuries, and Malformations of the Urinary Bladder, the Prostate Gland and the Urethra. It contained 925 pages with 184-woodcut images. He made the first attempt in the literature to report the prevalence of bladder stones and calculous disease in the U.S. and other countries. He was well-known for his skill at lateral lithotomy surgery, and it is described in detail in this book. This urologic procedure is immortalized with his iconic lithotomy knife that has been preserved in the Jefferson archives (see this page). A reproduction of The Gross Clinic painting hangs in the SKMC College building on the 2nd floor and can also be seen as the backdrop for our recent 2024 faculty photo (page 82). As an aside, Dr. Gross was Professor of Surgery from 1840 to 1856 at the Louisville Medical Institute, later the University of Louisville. During the first winter in Philadelphia on his return to Jefferson as Chair, on December 24, 1856, Gross was handed a telegram informing him that the University of Louisville had been totally consumed by fire, including all his books. This amounted to a loss of approximately 2,000 volumes of the finest and most extensive collection of books on the Genito-Urinary organs that had ever been collected in the United States.
Some of Dr. Gross’s many contributions to surgery include using stay sutures to prevent wound dehiscence, a special catheter for draining urine when mixed with blood and describing laparotomy to repair rupture of the bladder.
Dr. Samuel D. Gross’ son, Samuel W. Gross, MD, was a Jefferson graduate and a surgeon in the Civil War. Upon returning to Jefferson after the war, he lectured on Urinary diseases, updated his father’s 1851 urology book and wrote a new book, Disorders of the Male Sexual Organs, in 1881.
John Hill Brinton, MD, was the fifth surgery Chair at Jefferson. In 1856, he reported a previously undescribed valve in the right spermatic vein and suggested its relationship to the lesser frequency of varicocele on that side, another early urologic Jefferson contribution. Other Jefferson surgeons who wrote about or practiced urologic surgery toward the end of the nineteenth century included W.W. Keen (1862), J. Ewing Mears (1865) and W. Joseph Hearn (1867). By the late 1890’s, urologic surgery became increasingly recognized as a distinct surgical specialty in Europe and by 1935, the American Board of Urology was formed, identifying urology as an official surgical specialty.
THE DEPARTMENT OF GENITOURINARY DISEASES IS ESTABLISHED
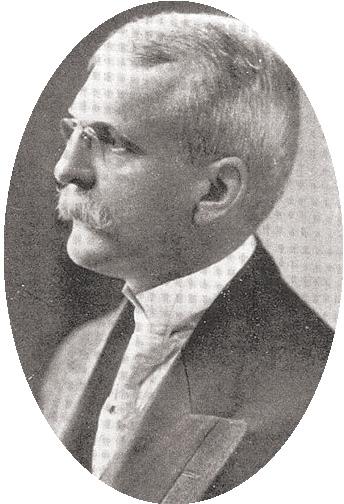
In May 1904, a formal Department of GenitoUrinary Diseases at Jefferson Medical College was established with Orville Horwitz, MD, as the Professor and Chair. Dr. Horwitz equipped Jefferson’s Genito-Urinary department at his own expense. His continued departmental support for equipment and maintenance was not incurred by the hospital but also came from donations of grateful patients. The GenitoUrinary service began with 10 cases and by the end of 1904 became one of the largest departments in the Hospital.
Hiram Rittenhouse Loux, MD, presided as the second Chairman of Genito-Urinary Diseases at Jefferson Medical College from 1912 until 1930. The admiration of the medical students for him was professed by the establishment of the Hiram R. Loux Urological Society, a society of historical interest only.
Thomas Cooke Stellwagen, DMD, MD, succeeded Dr. Loux as the third Chairman of Genito-Urinary surgery and served from 1930 until 1935. Dr. Stellwagen was a member of the Clinical Society of Genito-Urinary Surgeons (CSGUS) as well as the American Association of Genito-Urinary Surgeons (AAGUS). In 1932, Jefferson hosted the CSGUS meeting, and it will be hosted again by Jefferson in 2025.
David Melvin Davis, MD, was the fourth Chairman of the Department from 1935 to 1951. Dr. Davis interned at Baltimore City Hospital and returned to Johns Hopkins as an assistant pathologist. His research endeavors paved the way for his directorship of the Brady Urological Institute. The main research interest of Dr. Davis was in the field of genito-urinary infection including sexually transmitted diseases. Back at the Brady Institute, Dr. Davis completed a urological residency and over a two-year period coauthored with Dr. Hugh H. Young, the acclaimed urological textbook of the time titled, Practice of Urology. He served as Associate Editor of the Journal of Urology at the time of its inception in 1917.
Dr. Davis served as chairman of the Department of Urology at the newly formed Medical School of the University of Rochester. However, his desire to perfect his unending training placed him once again as an associate of Dr. Hugh Young. Dr. David M. Davis was appointed as Chairman in 1935. This was to be the beginning of 16 fruitful and dynamic years for the Urology Department and Residency Program at Jefferson. The Nathan Lewis Hatfield Professorship was originally established in 1944 with the original gift from the estate of Dr. Henry Reed Hatfield (Jefferson/SKMC 1881) in honor of his father. In 1944, Dr. Davis became the first Nathan Lewis Hatfield Professor.
The flank lithotomy knife used by Professor Samuel Gross in the late 1800’s, one of Dr. Gross’s contributions to urologic surgery at that time. (Courtesy of the Marion Siegman Archives collection, Jefferson Scott building).


URINARY
Shortly after Dr. Davis’ appointment at Jefferson, the Department of Genito-Urinary diseases changed its name to the Department of Urology. Under Dr. Davis’ leadership, advanced training in Urology was established when the first urology residency at Jefferson started in 1939. World War II caused a delay in increasing the number of residents, but a second position was created in 1946 and has now grown to three residents per year. In 1948, an arrangement with John H. Gibbon, MD, Professor of Surgery, provided a year training in General Surgery before beginning three years in the Urology Residency.
Dr. Davis greatly improved the standard of care in the Urology Ward and outpatient Curtis Clinic. In addition to more than 130 journal articles, after academic retirement, Dr. Davis wrote a textbook, Mechanisms of Urologic Disease (1953). He designed a cystoscopic-roentgenographic-fluoroscopic table constructed in Philadelphia by the Franklin X-ray Corporation. His interests were in hypospadias, hydronephrosis, and early diagnosis and radical operations for carcinoma of the prostate and the famous “Davis Intubated Ureterotomy.”
He retired at age 65 in 1951 but remained active in practice, research, and authorship of articles for another 17 years until his death in 1968. To honor his memory, the Annual David M. Davis Visiting Professorship in Urology was established in 1981.
Theodore R. Fetter, MD, was the fifth Chair and Nathan Lewis Hatfield Professor from 1951 to 1967. His numerous publications expanded a wide spectrum of urinary topics and were significant literary contributions on genitourinary disease in the classical text, Anspach,
Gynecology. He served as President of the Pennsylvania State Medical Society in 1952 and as President of the Mid Atlantic Section of the American Urological Association.
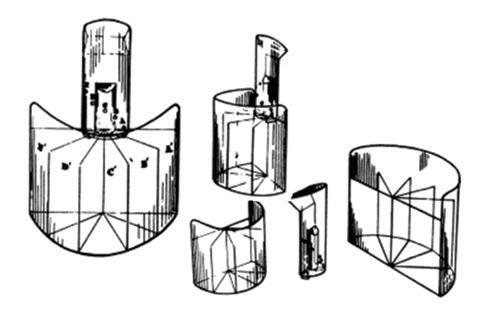
During Dr. Fetter’s chairmanship, modern urology was developing rapidly. Intravenous pyelography, better cystoscopes, resectoscopes with Bovie machines for electric cutting and coagulation, use of antibiotics, and anesthesia with use of intravenous fluids and blood loss replacement were all major advances. The residents and medical students were trained using the latest instrumentation. During this time at Jefferson urologist Dr. Willard Drake was the first to use the word "urodynamics” and he invented and patented the Drake uroflowmeter. An original “Drake Uroflowmeter” can be found in the Museum of Jefferson Urology in Urology’s SKMC College office. (See photos 2, 6, and 7, page 10.)
Paul Zimskind, MD, PhD, succeeded Dr. Fetter as the sixth chairman serving from 1967 to 1976 as the Nathan Lewis Hatfield Professor of Urology and was one of the youngest men to reach the status of Chair at the age of only 36. He completed medical training and urology residency at Jefferson. During his residency, Dr. Zimskind carried out human and animal experiments on the physiology of urethral dynamics for which he earned his PhD. He was heavily involved in the formative years of urodynamics and was a charter member of the Urodynamics Society, now known as SUFU (Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction) and presented at the Inaugural Meeting at the 1969 AUA in San Francisco. The McGuire-Zimskind award is given annually by SUFU to a member who has made significant contributions to the field. Dr. Zimskind engaged his residents as volunteer technicians in executing his research endeavors. He was a member of various prestigious urologic societies and was able to publish 43 scientific papers and give 77 presentations at scientific meetings worldwide, before his sudden death at age 44 of Addison’s
Chairs of the Department of Urology
disease. He is remembered by our biennial Zimskind Lectureship.
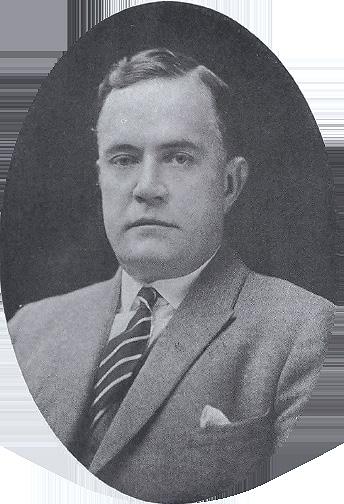
S. Grant Mulholland, MD, was appointed as Nathan Lewis Hatfield Professor and Head of the Department in 1977 and served as the Department’s seventh Chairman for the next 25 years (1977-2002). He followed closely in his father’s footsteps, Dr. Stanford Wallace Mulholland. His father was a prominent Philadelphia urologist who was Professor and Chair of the Department of Urology at the Medical College of Pennsylvania.
At the time of Dr. S. Grant Mulholland’s Chair appointment, the Department was almost completely composed of volunteer faculty (3 urologists), who were talented clinicians with large private practices. The Department, however, needed academic modernization and expanded research. Over his tenure, a large, diversified department offering both primary and tertiary urologic care and a research initiative was established. He orchestrated the merger of several private practices, Drs. Ken Brownstein, Larry Goldstein and Perry Weiner into the academic Department of Urology. At the end of Dr. Mulholland’s tenure as chair, the Department had 77 employees, including 14 attendings, 8 residents (2 years surgery plus 4 years urology), 2 PhDs and several clinical fellows and post-docs. Over 20 fellows were trained in areas including oncology, endourology and neuro-urology. During his tenure as chair, residents had dedicated time as a “Research” resident. Over the ensuing years due to changes in the structure of Urology residencies, the 6-year program was converted into a 5-year training program with the elimination of the full academic research year.
In August, 2002, Leonard G. Gomella, MD, FACS, was appointed the Bernard Godwin Professor of Prostate Cancer and the 8th Chair of the Department. Dr. Gomella, originally from New York, graduated from Queens College, CUNY and completed medical school, general surgery and urology training at the
Jefferson Medical College/Sidney Kimmel Medical College Thomas Jefferson University, 1904-2024



University of Kentucky in Lexington, Kentucky. This was followed by a two-year Urologic Oncology Fellowship with Drs. Marston Linehan and Steven Rosenberg at the National Cancer Institute in Bethesda, Maryland. He has been a faculty member since 1988 and in 1994, the Board of Trustees appointed him the first Bernard W. Godwin Jr. Associate Professor in Prostate Cancer, the first prostate cancer specific chair at any US medical school.
Dr. Gomella was recruited to Jefferson to assist Dean Joseph Gonnella in his mission to establish an NCI designated cancer center. Dr. Gomella has served numerous roles in our Cancer Center journey since our first NCI designation in 1996 including Associate Director, Director of the Jefferson Kimmel Cancer Center Network and now as Senior Director for Clinical Affairs. Other external leadership roles have been as Urology Chair for RTOG (now NRG), President of the Mid Atlantic AUA, and President of the Society of Urology Oncology.
In 1991, working with resident Dr. Jose Moreno
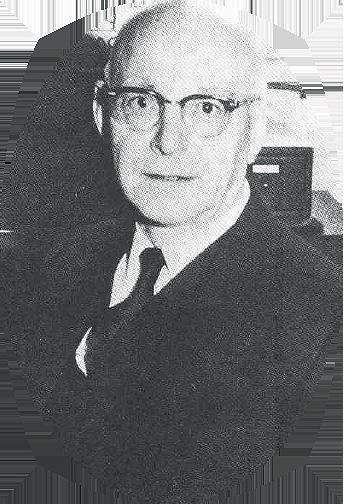
and others, Dr. Gomella’s team was the first to use RT-PCR to detect hematogenous circulating micro metastasis in patients with prostate cancer. This is the first report of a molecular “liquid biopsy” in prostate cancer. Dr. Gomella is involved in both basic science and clinical research in the development of new diagnostic techniques and treatments for urologic cancers through Jefferson’s Sidney Kimmel Comprehensive Cancer Center.
In addition to having given over 500 presentations at local, national and international meetings, he has written over 650 papers, book chapters and monographs in the field of Urology and has served as a member of the Editorial Board of numerous journals in urology and oncology and most prominently, he is Editor in Chief of the Medline referenced “Canadian Journal of Urology”.
Dr. Gomella has authored and edited over two dozen books for medical students, house officers, and practicing physicians. He is the editor of the 5 Minute Urology Consult, with the 4th edition currently in preparation.

Recovering From Prostate Cancer, co-authored by Dr. Gomella, was the first book for the public dedicated to this topic in 1994. In the field of medicine, Dr. Gomella is widely known for Gomella and Haist’s Clinician's Pocket Reference, with the 12th edition published in 2022. The book, popularly known as the Scut Monkey Handbook, is a widely used reference for medical students and other health care providers.
As Jefferson Health Vice President for Urology, Dr. Gomella’s focus as chairman has been to expand urology throughout the enterprise to keep up with the clinical demand for Jefferson University Urology physicians, and academically, to promote educational opportunities and expand basic science and translational research programs.
In 2014, Jefferson Medical College is renamed Sidney Kimmel Medical College after a $110 million gift is made by the Sidney Kimmel Foundation.

Nathan Lewis Hatfield Professors
David M. Davis, MD 1944-1951
Theodore Fetter, MD 1951-1967
Paul Zimskind, PhD, MD 1967-1976
S. Grant Mulholland, MD 1977-2002
Demetrius H. Bagley, MD 2002-2022
Costas D. Lallas, MD 2023-present
Bernard W. Godwin Jr. Professor of Prostate Cancer
Leonard G. Gomella, MD (Associate Professor 1994-2002), Professor 2002-present
Demetrius H. Bagley Jr., MD Professorship
Scott G. Hubosky, MD (Associate Professor 2015), Professor 2021-present
JEFFERSON UROLOGY'S FIRST 200 YEARS REFERENCES
Part III: Clinical Departments and Divisions
Continued --- Chapter 32: Department of Surgery (pages 505-579)" (1989). Thomas Jefferson University - tradition and heritage, edited by Frederick B. Wagner, Jr., MD, 1989. Paper 31. https://jdc.jefferson.edu/wagner2/31
Nicolas R. Varano, MD. (Chapter 47, “Department of Urology,” in Thomas Jefferson University: Tradition and Heritage, Ed.: F.B. Wagner, Jr., Publisher: Lea & Febiger, Philadelphia, 1989).
Julia S. Berkowitz. Adorn the Halls, History of the Art Collection at Thomas Jefferson University. Publisher: Thomas Jefferson University, Philadelphia, PA, 1999
The Urology Residency training program is currently a 5-year program that provides a well-balanced experience in all major disciplines of Urology. Three residents are accepted each year through the AUA Match Program. Upon completion of the program, the individual is equally well prepared to enter private practice, academics or a competitive fellowship training.
Dr. Patrick Shenot (TJUH Residency ’97), Professor of Urology, was appointed the Director of the TJUH Urology Residency Training Program at Jefferson in 2002 by Dr. Gomella. (See page 30 for a faculty profile on Dr. Shenot.) The urology residency combines exposure to a variety of practice settings: academic medical center (Thomas Jefferson University Hospital and Methodist Hospital), the Wilmington Veterans Administration Hospital, and the Nemours Health/Alfred I. duPont Hospital for Children. Surgical exposure to microsurgery is in the outpatient surgery center at Jefferson New Jersey Cherry Hill facility. In addition to a comprehensive conference and grand rounds schedule, the program also incorporates ongoing involvement with scholarly activity, participation in local and national meetings, translational research and clinical trials. Departmental resources include a variety of surgical simulators in the Hamilton Building (laparoscopy, DaVinci Robotic Simulator, TUR and ureteroscopy simulators), all designed to enhance the learning of our house-staff and allow us to provide state-of-theart care for our patients.
The current urology faculty consists of 18 full time academic physicians, several adult urology volunteer faculty and one educationally focused PhD. Our pediatric staff includes five full-time attending physicians who primarily practice at Nemours Children’s Health/A.I. duPont Hospital in Wilmington, Delaware. Additional affiliate faculty work with our residents at the Wilmington VA Medical Center. Our department features nationally
Leonard Gomella, MD, Appointed the Bernard W. Godwin Jr. Professor and Chair

Patrick Shenot, MD, Appointed Residency Program Director
Jefferson Urology Centennial Celebration
Jefferson Museum of Urology Established in honor of Dr. Leonard Frank
and internationally recognized faculty in all major disciplines including endourology, laparoscopy, robotic surgery, urologic oncology, neurourology, female urology, andrology, and pediatric urology. Basic science and translational research efforts are in collaboration with Radiology, Cancer Biology and other basic science departments.
The Department has a 1-year Fellowship in Endourology and Laparoscopy, which is certified by the Endourology Society. The Fellow works with the physicians who specialize in endourology and minimally invasive urologic oncology in the Department of Urology and the Kimmel Cancer Comprehensive Center of Thomas Jefferson University.

A residency program graduation tradition is a photo of all Jefferson residency program alumni to gather for a photo with the David M. Davis Visiting Professor. Here our 2019 DMD Visiting professor Dr. David Penson, Urology Chair at Vanderbilt, is posing with our alumni along with the statue of Dr. Samuel Gross on the Lubert Plaza outside of the Scott Building.
2005 In October, Costas Lallas, MD, performs first robotic procedure at TJUH
Leonard Gomella, MD, President MidAtlantic American Urologic Association 2006 Live Robotic Radical Prostatectomy broadcast on web
2007 Second Edition 5-Minute Urology Consult published
2009
First Department of Urology SKCC Men's Event to Support Prostate Cancer Research
2015 Scott Hubosky, MD, Investiture as Demetrius H. Bagley Jr. Professor of Urology
FIRST REPORT OF RENAL PEDICLE TOURNIQUET applied around renal artery and vein while closing after partial nephrectomy by Dr. T. C. Stellwagen.
CAREFUL STAGING OF BLADDER CANCER BY DEPTH OF INVASION.
Dr. George Strong, Jefferson Urologist coauthored the historic “Jewett-Strong” classification of bladder cancer with Dr. Jewett in 1946.
FEMALE URETHRAS WERE DILATED FOR A VARIETY OF INDICATIONS including bladder emptying, irritable bladder syndrome with or without incontinence, and urethral discomfort investigated and promoted by Dr. T.R. Fetter.
CONTROLLED DECOMPRESSION OF CHRONICALLY DISTENDED BLADDERS by slowly lowering the pressure over intervals up to 24 hrs. was pioneered by Dr. David M. Davis.
THE MODERN UROFLOWMETER WAS INVENTED BY WILLARD M. DRAKE, JR., MD, IN 1946. The original manuscript, entitled "The Uroflowmeter: an aid to the study of the lower urinary tract," appeared in Journal of Urology in 1948. Drake obtained a US patent for the device, entitled "Uroflowmeter" in 1953. Dr. Willard Drake was the first to use the word “urodynamics”.
FIRST REPORT OF ENDOSCOPIC RECANALIZATION OF THE OBLITERATED UPPER URINARY TRACT, by Dr. Bagley (1985).
URETEROSCOPIC FIRSTS by Dr. Demetrius Bagley include: ULTRASONIC LITHOTRIPSY (1983), HOLMIUM LASER LITHOTRIPSY OF UPPER URETERAL CALCULI (1995) AND RENAL CALCULI (1998), AND ENDOLUMINAL ULTRASOUND OF THE URETER (1995).
FIRST REPORT OF ELECTROEJACULATION OF A QUADRIPLEGIC MAN resulting in pregnancy was by Dr. Irvin Hirsch (1990).
FIRST FORMAL UROLOGIC LAPAROSCOPY PROGRAM in Philadelphia in 1991.
FIRST USE OF MOLECULAR METHOD (RT-PCR) TO IDENTIFY CIRCULATING CELLS IN PROSTATE CANCER PATIENTS, 1992 Drs. Moreno, Mulholland and Gomella. Four U.S. Patents were awarded to Jefferson for this discovery, now called “liquid biopsy”.
FIRST BOOK ON PROSTATE CANCER FOR THE PUBLIC TITLED “RECOVERING FROM PROSTATE CANCER”, co-authored by Dr. Leonard Gomella and Philadelphia Inquirer writer John Fried (1993).
Board of Trustees appointed Dr. Leonard Gomella the FIRST BERNARD W. GODWIN ASSOCIATE PROFESSOR OF PROSTATE CANCER, the first prostate cancer specific chair in the U.S. (1994).
2015-18 Leonard Gomella, MD, President Society of Urologic Oncology
2016 Men’s Health Program Established, Perry Weiner, DO, MSC, Founding Director
2017 Edouard Trabulsi, MD, President Mid-Atlantic Section American Urologic Association
Third Edition 5-Minute Urology Consult Published
First Philadelphia International Prostate Cancer Consensus Meetings on Genetic Testing for Prostate Cancer: “The Role of Genetic Testing for Inherited Prostate Cancer Risk”
FIRST FULLY INTEGRATED MULTIDISCIPLINARY GU CANCER CENTER, established at the Kimmel Cancer Center (1996).
FIRST MICROWAVE PROSTATE THERMOTHERAPY UNIT in the Delaware Valley at the Pennsylvania Prostate Center at Jefferson (1997).
FIRST LAPAROSCOPIC RADICAL PROSTATECTOMY IN DELAWARE VALLEY by Drs. McGinnis and Strup (2000).
The first clinical report of using INTRAVESICAL LIVE VIRUSES TO TREAT BLADDER CANCER (2001).
FIRST IMPLANTATION OF A LABORATORY GROWN BLADDER REPLACEMENT in an adult by Dr. Patrick Shenot (2008).
NOVEL TECHNIQUE OF DETECTION OF SHED CANCER CELLS Drs. Gomella and Thakur, Jefferson awarded 10 international patents (2016).
FIRST-EVER CONSENSUS MEETING on the role of genetic testing in prostate Cancer (Dr. Gomella Co-Chair with the Sidney Kimmel Cancer Center) 2017.

Visit History of the Department of Urology at: www.jefferson.edu/ academics/colleges-schoolsinstitutes/skmc/departments/urology/ about/history/centennial
2019 P. Kenneth Brownstein, MD, Investiture as Honickman Director of Signature Services
Second Philadelphia International Prostate Cancer Consensus Meetings on Genetic Testing for Prostate Cancer: “Implementation of Genetic Testing for Inherited Prostate Cancer”
2022 Costas Lallas, MD, President Mid-Atlantic Section American Urologic Association
2023 Costas Lallas, MD, Investiture as Nathan Lewis Hatfield Professor
2024 The launch of Prostate Cancer Focal Therapy Program
Center City Urology offices move to new Honickman Center
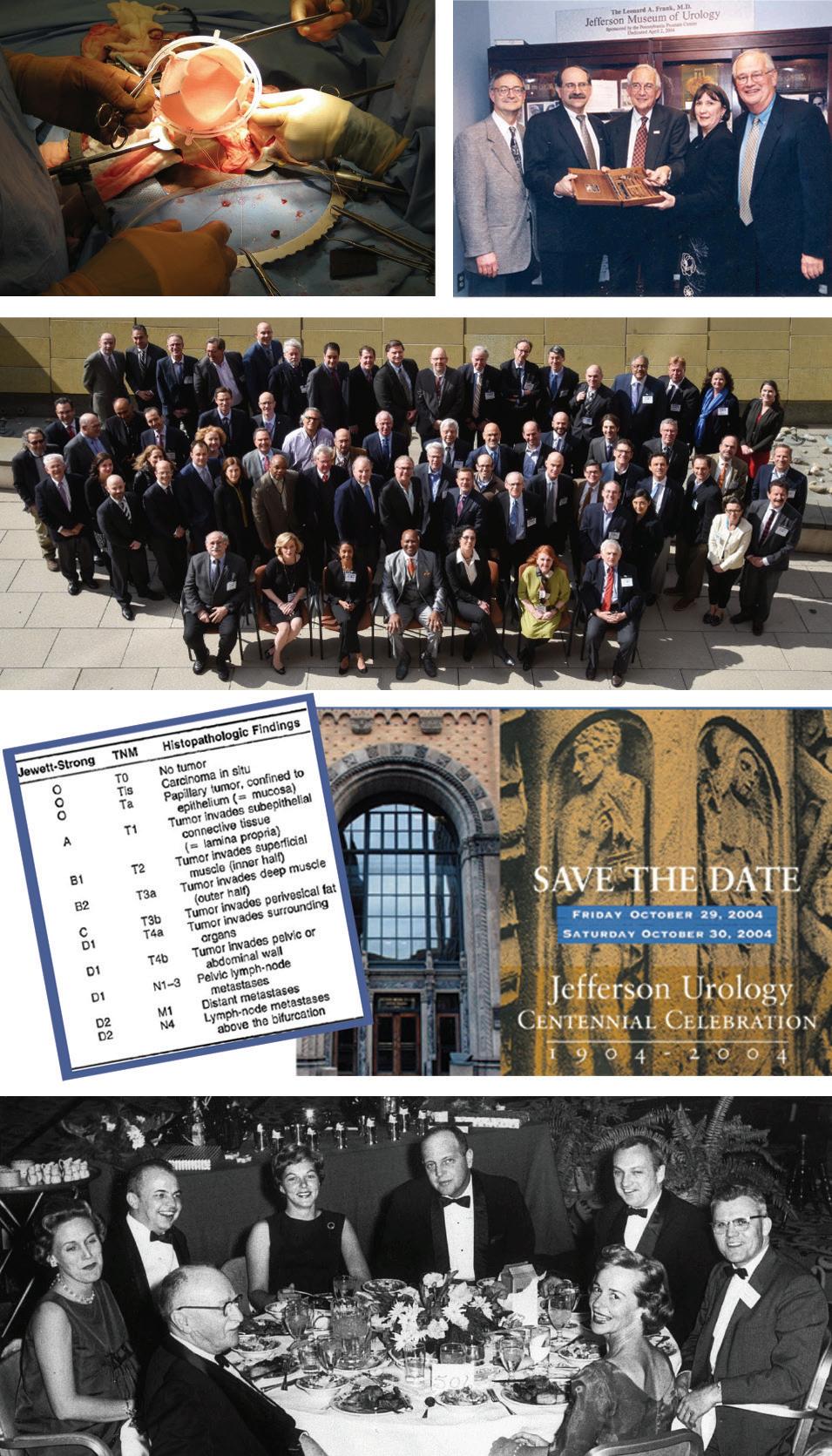
1 Intraoperative photo of first lab grown bladder replacement surgery in an adult performed by Dr. Patrick Shenot 2008. Other centers had previously performed the procedure only in children.
2 Dedication of the Jefferson Museum of Urology, April 2, 2004, in honor of Dr. Leonard A. Frank. Drs. D’Elia, Gomella, Frank, Byrne and Mulholland participating.
3 2017 First Philadelphia International Prostate Cancer Consensus Meetings on Genetic Testing for Prostate Cancer: “The Role of Genetic Testing for Inherited Prostate Cancer Risk.” (Giri VN, et al. J Clin Oncol. 2018 Feb 1;36(4):414-424).
4 The first bladder cancer staging system by Dr. George Strong, Jefferson Urologist, who co-authored the “JewettStrong” classification of bladder cancer with Dr. Jewett in 1946. The table compares the system with the more modern TNM staging. (Jewett HJ, Strong GH. Infiltrating carcinoma of the urinary bladder; diagnosis and clinical evaluation of curability. South Med J. 1946 Mar;39:203-8).
5 Announcement of Department of Urology Centennial Celebration October, 2004.
6 Photograph taken at the 1948 Mid-Atlantic American Urological Association Annual Meeting reception. Dr. Willard Drake, who developed the first uroflowmeter (far left, wearing glasses), and Dr. David M. Davis, urology chair (far right, wearing glasses).
7 Diagram of the uroflowmeter developed at Jefferson by Dr. Willard Drake. The original protype is in the Jefferson Museum of Urology in the SKMC departmental office in the College Building. (Chancellor MB, et al. The invention of the modern uroflowmeter by Willard M. Drake, Jr. at Jefferson Medical College. Urology. 1998 Apr; 51(4):671-4).

8 Our department did a live webcast of a robotic prostatectomy in 2006, one of the earliest real time broadcast robotic prostatectomy procedures in the U.S.
9 On February 7, 2023, Dr. Costas Lallas became the 6th Nathan Lewis Hatfield Professor of Genito-Urinary Surgery. From left to right: Mr. Harry Donahue, Philadelphia radio broadcasting legend and Master of Ceremonies, Dr. Mark Tykocinski, former Dean of Sidney Kimmel Medical College, portrait of Dr. Hatfield, Dr. Lallas with the professorship proclamation and Dr. Leonard Gomella, Chair, Department of Urology.
10 SKCCC GU Multidisciplinary Clinic founding members in 1996 include Dr. Leonard Gomella (4th from right), Dr. Richard Valicenti (3rd from left) and Dr. Adam Dicker (2nd from left). Also seen are Dr. S. Grant Mulholland, the former Jefferson Urology Chair, Dr. Steve Strup, now Chair of Urology at the University of Kentucky and Dr. Mo Ismail Chief of Urology at the Wilmington, VA Medical Center. The program has been in continuous operation since its creation where patients can be seen by multiple specialists in one office visit. Our unique program has now become a standard model at many cancer centers.
11 In 2015, Dr. Scott Hubosky was awarded the first Demetrius H. Bagley Jr, MD Professorship. Shown are Dr. Mark Tykocinski, former SKMC Dean, Dr. Bagley and Dr. Hubosky.
12 The first book for the public on prostate cancer was published in 1993 by Dr. Leonard Gomella and Philadelphia Science writer John Fried. (Harper-Collins Press, New York)
13 The first clinical report of using intravesical live viruses to treat bladder cancer, 2001.
Since the early 1990’s, the duPont Hospital for Children in Wilmington, Delaware, has been an integral part of Jefferson’s Department of Urology residency training. In the fall of 2024, Dr. T. Ernesto “Sonny” Figueroa, turned the leadership of the Division of Pediatric Urology to Dr. Jennifer Hagerty. With that leadership transition, Dr. Figueroa was asked to provide a retrospective on the history of Pediatric Urology at Nemours and the duPont Hospital for Children and their longstanding engagement with Jefferson’s Urology residency program.
This narrative history has been provided by Dr. Figueroa, Professor of Urology and Pediatrics, Sidney Kimmel Medical College Nemours Children's Health, Delaware Valley.
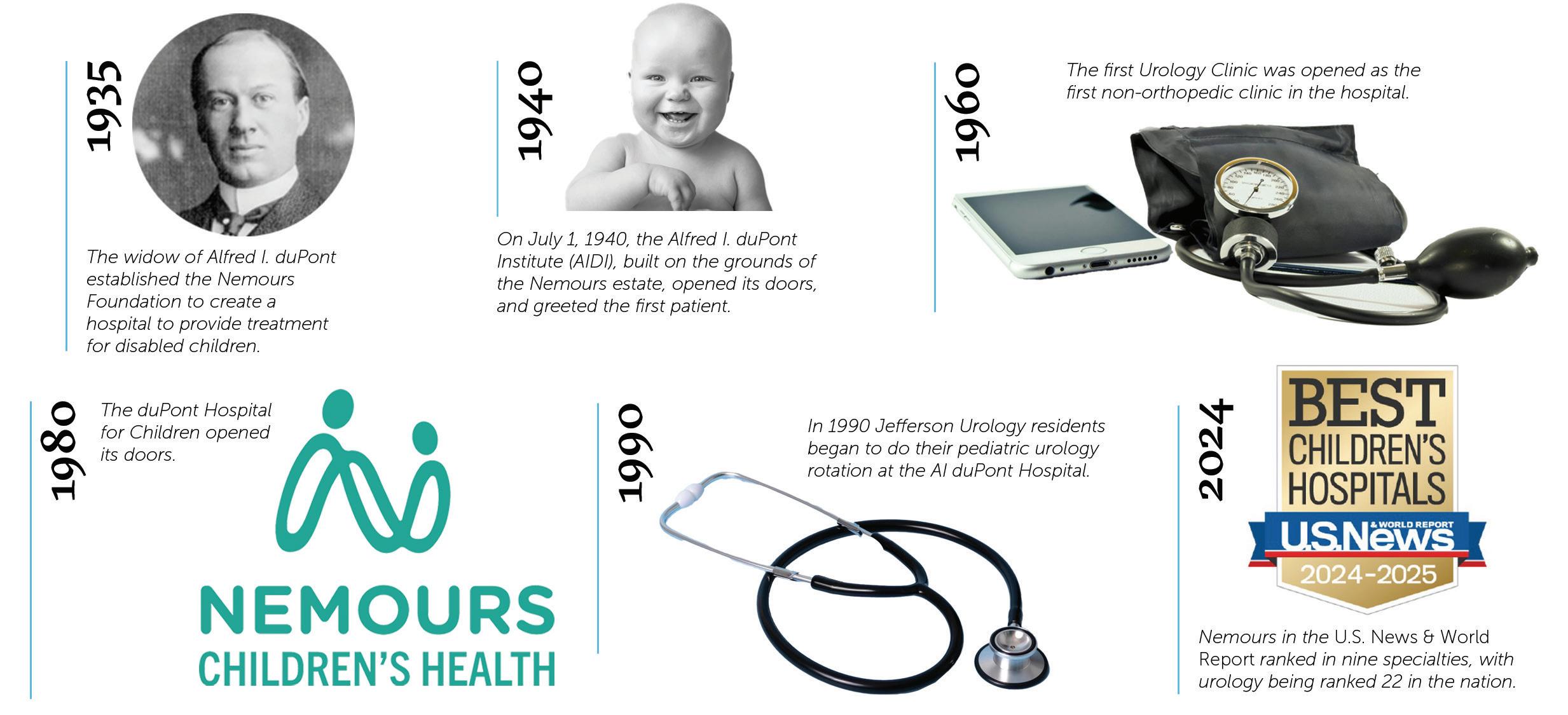
Upon his death in 1935, the widow of Alfred I. duPont, Mrs. Jesse Ball duPont, established the Nemours Foundation, a charitable corporation to realize Mr. duPont’s wishes to create a hospital to provide treatment for disabled children. On July 1, 1940, the Alfred I. duPont Institute (AIDI), built on the grounds of the Nemours estate, opened its doors, and greeted the first patient. The hospital was created with three important goals in mind: 1) to offer excellent patient care, 2) to develop a support structure for research to enhance clinical care, and 3) to promote the education of young physicians, medical students, and nurses to be the next generation of care providers. For the first 20 years, AIDI was an exclusive orthopedic hospital, leading the nation in the management of many pediatric orthopedic conditions, particularly scoliosis. In 1960, the first Urology Clinic was opened as the first non-orthopedic clinic in the hospital. As the diversity of pediatric conditions expanded, the Board of the Nemours Foundation approved the creation of a multidisciplinary hospital which was then named the duPont Hospital for Children. This hospital opened its doors in 1980.
With the expansion of clinical services, and a transition from a primary orthopedic hospital to a multidisciplinary hospital in the mid-80s, a new surgeon-in-chief was recruited to lead the surgical services at the newly named duPont Hospital for Children, or duPont, for short.
Dr. John Noseworthy, a pediatric surgeon who
also had completed a joint general surgery and urology residency at Case Western, became the first surgeon–in-chief in 1986. He was a multitalented surgeon who was as comfortable repairing the imperforate anus as he was doing hypospadias surgery. In 1990, he recruited R. Bruce Filmer, MBBS, as the first Chief of Urology. At the time of his recruitment, Dr. Filmer was Associate Chief and Associate Professor of Pediatric Urology at the Children's Hospital of Michigan working alongside Dr. Alan Perlmutter, a renowned pediatric urologist of the era, who was also the Secretary to the Board of Urology.

Drs. Sonny Figueroa, John Noseworthy, and Bruce Filmer, 1993.

Our 1996 Pediatric Urology Visiting Professor, Dr. David Bloom, from the University of Michigan along with urology resident Dr. Steve Strup, and Jefferson faculty Drs. Grant Mulholland, Bruce Filmer, Lenny Gomella, and Michael Chancellor.
As part of the recruitment of Dr. Filmer, Dr. S. Grant Mullholland, then Chair of the Department of Urology at Jefferson, was integral in securing this recruitment, and restructuring the urology residency by moving the Jefferson residents from Children’s Hospital of Philadelphia (CHOP), where they were doing their pediatric urology rotation, to duPont. The first Jefferson urology resident to rotate at duPont was Dr. Michael Grasso.
As a third year medical student at Tulane University, I met a very determined and energetic Urology Chief Resident, Dr. Raju Thomas, on the wards of Charity Hospital. For the last 4 decades, Raju has remained a mentor and a dear friend. Raju remained at Tulane, and eventually was named Chairman of Urology. After more than 25 years as Chairman, he remains one of the most energetic and inspiring
urologists that I have known. Drs. Gomella and Thomas became close friends since the earliest days of Urologic laparoscopy with each of them participating in numerous hands-on courses as faculty in the early days of this “new” surgical technique.. They have led each of their Departments to extraordinary achievements. In 2008, Dr. Thomas visited Jefferson, giving presentations to the residents and in 2022, Dr. Thomas assumed the role of President of the American Urological Association. This past year several of our Urology residents were mentored by Dr. Thomas at an endourology training program (see page 67).
With the arrival of Dr. Filmer to Wilmington, the seeds for the growth of the Division of Urology through the "Detroit connection" were planted. While in Detroit, Dr. Filmer mentored and trained two pediatric urology
fellows who eventually would relocate to Wilmington to join the Division of Urology. In 1993, Dr. Filmer contacted me, one of his former fellows, to " come and take a look at this hospital". After one visit, I was ready to move. In 2000, we recruited a second former fellow at the Children’s Hospital of Michigan, Dr. Julia Barthold. Julie had been working with the famed Dr. Ricardo Gonzalez in Detroit. In 2002, we were able to also recruit Ricardo, and to establish the pediatric urology fellowship. The four pediatric urologists then working together in Wilmington had spent time at the Children’s Hospital of Michigan.
During my initial interview in 1993, I met a young Mike Erhard, who at the time was a PGY-5 urology resident rotating at duPont. This first meeting was the beginning of a 30year personal and professional relationship
with Mike. After his residency at Jefferson, Mike completed a fellowship in pediatric urology at the combined program of the University of Florida and Nemours in Jacksonville, Florida. Upon completion of his fellowship, Mike stayed at Nemours in Jacksonville, where he steadily rose through the many administrative ranks, from Chief of Urology to Medical Director of the Nemours Clinic, to Physician-in-Chief of the Florida Practices, to Vice President of the Nemours Foundation. Among his innumerable contributions to the Nemours Foundation, he promoted the pediatric practice in Florda to expand in volume and locations; he orchestrated the opening of the Nemours Children’s Hospital in Orlando, and he fostered cross campus collaboration, where urology was always the first division leading this important collaborative effort. All of us at Nemours owe Dr. Erhard tremendous gratitude for his selfless commitment and vision. See his write up in the Alumni News section, page 60.
In 1994, Dr. Filmer recruited me to join AIDI. Although I was very happy in Tampa working at the University of South Florida at the time, the opportunity to work in a dedicated children’s hospital along with many other pediatric specialists, as well as the affiliation with a superb institution and the Department of Urology at Jefferson, were too strong to pass. Upon arriving, I learned that one of the faculty members at Jefferson, Dr. Michael Chancellor, had secured a lab space at duPont. Along with Mike Chancellor, Associate Professor of Urology, and later with David Rivas and Pat Shenot, we started an animal lab at Nemours to study bladder function using a spinal cord injured rat model. Many projects came out of that lab including work supported by the American Foundation for Urological Disease (AFUD) and the Nemours Foundation. Eventually, the growing clinical demands for both adult and pediatric urology pulled each of us away from the lab.
When I joined Nemours, there was no laparoscopic equipment. In 1995, we convinced the Storz corporation to lend us the necessary equipment to perform the first laparoscopic procedure at duPont, a laparoscopic nephrectomy on a pelvic kidney. As we ventured into uncharted waters, we were able to safely complete the case as planned. It is remarkable that 30 years later, robotic assisted laparoscopy has become the way to manage many of the anatomical challenges faced by pediatric urologists. In 1996, we recruited Richard Silver from Hopkins. In 1997, I took over the division, and was named Chief of the Division of Urology, a position I was honored to hold until 2024.
In the early 2000’s, with the strong support and encouragement of the newly named Chair of Urology at Jefferson, Dr. Lenny Gomella,
we started to further expand the Division of Urology at Nemours. In 2000, we recruited Julie Barthold, as the Associate Chief, Professor of Urology, and Director of Urologic research. Julie was a pillar in the expansion of this Division. Her clinical and research efforts were instrumental in the growth of the Division. Julie retired from Nemours in 2018, after completing her term as first female president of the Societies for Pediatric Urology (SPU) and joining the NIH as a NIDDK program director. In 2001, we invited the internationally renowned Dr. Ricardo Gonzalez as the Visiting Professor. Ricardo and Julie had worked together in Detroit. During the social dinner on the day of the conference, after a few glasses of an excellent red wine, we pondered about the possibility of Ricardo joining us. This became a reality in 2002, when Ricardo joined us and transferred his fellowship in pediatric urology from the University of Miami to Nemours. Dr. Gonzalez was named Director of the Pediatric Urology Fellowship and Professor of Urology at Jefferson. The fellowship lasted from 2002 to 2012, and during this decade, we graduated 9 fellows in pediatric urology. Ricardo retired from Nemours in 2010, but he continued to have a prolific career in Germany until his untimely death.
As the Department of Urology continued to grow and add residency positions, we went from one Jefferson urology resident rotating at Nemours, to two. Dr. Paul Noh joined our faculty in 2004, and helped expand the laparoscopic service directed by Dr. Gonzalez. In 2008, Dr. Ahmad Bani Hani was recruited from Riley’s Children’s Hospital in Indiana. He quickly established a remarkably busy clinical practice centered on the neurogenic bladder and spearheaded our program on the management of the adolescent varicocele. Ahmad, Associate Professor of Urology, was the resident program director until his departure from Nemours in 2022, when he was recruited for the position of Chief and Professor of Urology, Texas Children’s Hospital-Austin.
In 2010, we recruited Dr. Jennifer Hagerty from Chicago. Jennifer had left Philadelphia to complete a fellowship at Lurie Children’s Hospital in Chicago, where she remained as faculty upon the completion of her fellowship. While in Chicago, Jennifer helped develop the robotic program. Since her arrival to
FELLOWS WHO COMPLETED THEIR TRAINING AT NEMOURS
Julie Franc Guimond Montreal, Canada, 2004
Lisandro Piaggio Mar de Plata, Argentina, 2005
Amos Neheman Haifa, Israel 2006
Mark Wehry Pensacola, Florida 2007
Rob Chacko Denver, Colorado 2009
Monica Metzdorf Los Angeles, California 2009
Richard Ashley Tucson, Arizona 2010
Ahmad Abed el Noor Aman, Jordan 2011
Omaya Bani Hani Aman, Jordan 2012

Wilmington, Jennifer has transformed the Division and created an extensive and highly complex clinical practice. She developed and has directed two highly successful and sophisticated programs, the Robotic program and the Interstim™ program, the first such program dedicated to children in the Delaware Valley. She is Associate Professor of Urology and Pediatrics at Jefferson. In 2022 she was invited to sit on the Residency Review Committee for Urology, and in 2023 she led Nemours in the USNWR application process, successfully ranking nine specialties, with urology being ranked 22 in the nation.
In 2024, Dr. Hagerty was named the new Chief of the Division of Urology. Dr. Puneeta Ramachandra joined us in 2016, and she serves as the Urology Quality Officer for Nemours. Puneeta had completed her fellowship in San Diego in 2013, and then joined the Valley Children’s Hospital in Madera, California before returning to the Philadelphia area in 2016. She is Assistant Professor of Urology. Dr. Keara De Cotiis, Assistant Professor, joined us in 2020 after completing her fellowship in Toronto. Keara serves as the Urology Resident Program Coordinator and Urology liaison on the fertility preservation program and solid organ transplantation program. Our most recent addition is our old friend and former Jefferson resident, Dr. Pat Casale, Professor of Urology. After completing his fellowship in 2004, Pat joined the faculty at CHOP and created one of the first pediatric robotic programs in the nation. Eventually, he returned to his native New York as Chief of Pediatric Urology at Columbia. More recently, Pat was the director of the pediatric robotic program at Advent Health in Orlando. In 2023 we were able to convince Pat to return to Nemours and Jefferson to complement our robotic and minimally invasive program.
With the addition of Puneeta, Keara and Pat, we have been able to assemble a very cohesive and highly skilled group of pediatric urologists with unique expertise including robotic surgery in the pediatric population.
The initial rotation for the Urology residents at duPont, was a long and
demanding six-month rotation for one single resident. As the program at Jefferson expanded, we were able to add a second, and eventually, a third resident to the pediatric rotation. The rotations were adjusted from 6 months to two 4-month rotations for the residents. The expansion of the program has allowed the residents to experience a more rounded education while at Nemours, including clinic, exposure to urodynamic testing, operating room, robotic experience, and didactic sessions, while admittedly, facing a more tolerable call schedule. Feedback from the residents has been uniformly positive, particularly related to the level of faculty engagement, supervision and exposure to open surgical experience.
In the last 30 years, the following Jefferson residents have pursued careers in pediatric urology: Dr. Michael Erhardt (University of Florida/Nemours), Dr. Pat Casale (Seatle Children’s Hospital), Dr. Eric Nelson (Texas Children’s Hospital) and Dr. Victor Kucherov (Children’s National Hospital). In addition, a rotating resident from the Cooper residency, Dr. Christina Ho (Children’s National Hospital), also became a pediatric urologist. Each contributed immensely to our program in Wilmington, and we are extremely proud of each of them.
While in Detroit, Bruce Filmer was introduced to Alan Perlmutter’s approach to the Pediatric Urology Visiting Professorship, a conference intended to expose the residents to interesting cases and timely presentations, and at the same time, creating a stimulating interaction between the visiting professor and the audience. Once in Wilmington, Bruce hosted Alan Perlmutter as the first visiting professor in Urology at Nemours in 1991. Since then, we have had 39 visiting professors, a long list of the “Who’s Who” in Pediatric Urology, travel to Wilmington to participate in this conference and recently they also participate in a Grand Rounds presentation at Jefferson. As much pressure as the residents have felt about the need to prepare and present the challenging cases to the inquisitive visiting



We have been able to assemble a very cohesive and highly skilled group of pediatric urologists with unique expertise including robotic surgery in the pediatric population.

professors over the last 3 decades, the longterm benefit of this experience for the residents has been immense. In 2022,the conference was renamed the Pediatric Urology Visiting Professor Conference sponsored by the Hohn Family, after their generous donation to the Division of Urology.
In 2021, almost 20 years after their son, Matt, had been a patient in the Urology Clinic at duPont, Bill and Donna Hohn approached Nemours with their desire to create an endowment in honor of the care that Matt received as a young man. In 2024, the endowment was named the “T. Ernesto (Sonny) Figueroa MD Urology Endowed Fund”. This endowment will allow the Division of Urology to greatly expand its academic, research and educational endeavors (see this page).
The Division of Urology at Nemours is poised to continue to achieve great accomplishments under the direction of Dr. Hagerty. We look forward to continuing our close work with the Department of Urology at Jefferson’s Sidney Kimmel Medical College. Dr. Hagerty is a visionary and highly skilled surgical leader, the right person at the right time, to advance the clinical, academic and educational goals of pediatric urology at Nemours and Jefferson.
Dr. Sonny Figueroa is now in this 30th year at Nemours in Delaware, including 27 years as Chief of the Division of Pediatric Urology. While Sonny has passed the leadership to Dr. Jennifer Hagerty, he will continue to care for pediatric urology patients, teach our SKMC students, and train our Jefferson Urology residents for years to come.
In 2024, the Hohn family pediatric urology endowment was renamed the “T. Ernesto (Sonny) Figueroa MD, Urology Endowed Fund” in his honor, acknowledging his long-term service to his patients and his trainees.

Dr. Figueroa with members of the Hohn family, benefactors of the “T. Ernesto (Sonny) Figueroa MD, Urology Endowed Fund,“ at the acknowledgment program. Drs. Kate Deans, Surgeon in Chief (l), and Pete Minneci, Chief of Surgery (r), were also in attendance.
In October, 2024 Peter C. Minneci, MD, MHSc, Chair of Surgery Nemours Children’s Health, Delaware Valley, announced Jennifer Hagerty, DO, as the new Chief of Urology at Nemours Children’s Hospital, Delaware.
Dr. Minneci went on to state that: “Dr. Hagerty is an accomplished academic clinical surgeon and recognized leader in her field. Over the past 14 years, she has made a major impact at Nemours Children’s Health. Her kindness, compassion and dedication, coupled with her expertise in pediatric urology, have helped thousands of children with a wide range of urologic conditions across multiple states.”
Dr. Jennifer Hagerty, New Chief of Pediatric Urology at Nemours with Dr. Sonny Figueroa.
“Nemours Children’s Health has greatly benefited from Dr. Hagerty’s leadership. She serves on several committees with professional organizations and at Nemours Children’s Hospital, Delaware. Notably, she oversees the hospital’s U.S. News & World Report clinical submissions, and I’m grateful to her and her team members who recently helped NCHDE achieve ranking in nine pediatric specialties (including Pediatric Urology), and a position among the top 10 Best Children’s Hospitals in the Mid-Atlantic region.”
She is co-author of more than 30 peer-reviewed articles and many other publications, she has been invited to speak at countless conferences, delivering lectures across the country. She has been named a Top Doctor by Main Line Today and Delaware Today and has earned awards from professional organizations and Nemours in the areas of research, service excellence, literary achievement and innovation.
Certified by the American Osteopathic Board of Surgery, Dr. Hagerty is currently Associate

Congratulations to Dr. Hagerty who was selected as Nemours Children’s Health, Physician of the Year, 2024. (See page 84.)
Professor of Urology and Pediatrics at Sidney Kimmel Medical College at Thomas Jefferson University, where she is involved with the student and urology resident rotations at Nemours. She earned her BS in biology at Ursinus College and her DO at Philadelphia College of Osteopathic Medicine (PCOM). After her residency at Albert Einstein Medical Center and PCOM, she completed a pediatric urology fellowship at Children’s Memorial Hospital/Northwestern University in Chicago. She has served as an attending pediatric urologist at Children’s Memorial Hospital, Lutheran General Hospital Chicago, North Shore University Health System, Jefferson University Health System, Main Line Health System and Christiana Care Health System.
A Montgomery County, Pennsylvania, native and a resident of Chester County, Dr. Hagerty says she knew she wanted to help others since she was a young child and is driven by the opportunity to provide great care and impact the lives of her patients and their families. We are thankful for Dr. Hagerty and all she will contribute at Nemours as we strive to create the healthiest generations of children. Please join me in congratulating her on her important new role!
A part of the announcement, Dr. Minneci also extended a special “thank you” to Dr.“Sonny” Figueroa for his 27 years of leadership of the Division of Urology. “Now in his 30th year at Nemours, he is a highly accomplished urologist and has guided our Urology Division to become a national and international leader in pediatric urologic care. Sonny has been a visionary leader who has raised the bar on the quality of care and compassion in the division, department, and at Nemours as a whole. While stepping down as the Division Chief, we are fortunate that Sonny is going to remain an active member of the division, continuing to see and treat patients throughout the Delaware Valley. Please join me in expressing our thanks to Dr. Figueroa for his leadership.”
The past year, 2024, was an incredibly significant year for the Division of Pediatric Urology, with many milestones achieved. All the members actively participated in clinical, academic, and educational endeavors. Among the most important milestones, in October, after a nation-wide search, Dr. Jennifer Hagerty was named the new Chief of the Division. This is a well-deserved and timely appointment for Dr. Hagerty, who has continued to excel in clinical program development, academic productivity, journal editorial responsibilities, and participation in national committees. Under Dr. Hagerty’s leadership and oversight at Nemours, 9 Divisions, including 4 surgical Divisions, made the U.S. News & World Report ranking list this year, with Urology ranking as number 22 in the nation, an impressive milestone. Dr. Hagerty becomes the third Chief of the Division of Urology, following Sonny Figueroa, who assumed the position in 1997, and the late R. Bruce Filmer, who was named the first Chief in 1990. In October, the Hohn Family established an endowed fund in honor of Dr. Figueroa for his compassionate and unwavering care of their son 20 years ago to support academic and educational endeavors.
In clinical care, two significant milestones were reached in 2024: the 500th robotic case and the 50th Interstim™ case were completed. Both the Robotic program and the Interstim™ program are led by Dr. Hagerty. During this year, the members of the Division participated in many regional and national academic meetings. Dr. Figueroa presented the “Second Annual Doug Canning Memorial Lecture” at JeffersonEinstein in March, Dr. Hagerty participated in a panel at the International Children’s Continence Society/Societies for Pediatric Urology in September on the use of sacral neuromodulation for refractory OAB in pediatrics. During the same meeting, Dr. Ramachandra participated in a presentation of the PKIDS project on the multicenter prospective clinical trial comparing ESWL, PCNL and ureteroscopy for the management of urinary stones in children. Dr. De Cotiis presented at the Mid Atlantic AUA meeting on transitional health concerns in neurogenic bladder. Jackie Nguyen, PA-C, presented a poster on testicular torsion illustrating many of the advances achieved at Nemours in the management of this condition. There was also a noticeable presence of pediatric urological topics presented in the Department of Urology at Jefferson including a debate on ureteral clipping vs heminephrectomy, moderated by Dr. Ramachandra, augmentation enterocystoplasty in pediatric urology, by Dr. Figueroa, and sexual health in spina bifida and urodynamic essentials by Dr. De Cotiis.
Members of the Division of Urology were also recognized for their accomplishments, including Alice Hoffman, APRN, receiving the 2024 APP Leadership Excellence Award, and Jackie Nguyen, PA-C, receiving the APP Rising Star Award. Drs. Figueroa and Hagerty were recognized as “Infinite Advocates.” Nemours Children’s Health created the “Infinite Advocate and Grateful Patient & Family Philanthropy Program” to provide appreciative families a simple way to express thanks for the world-class care their loved ones receive at Nemours Children’s Health. For generations, families have told us that giving back is an integral part of their healing


Dr. Kraft, 2024 Pediatric Urology Visiting Professor from the University of Michigan with the Pediatric Urology faculty. (Also see page 53).
process particularly when they know their contributions will ensure future families will receive our exceptional care. We congratulated Dr. Figueroa on celebrating 30 years at Nemours and his special recognition form the Hohn family (see “In Honor of Dr. Figueroa” on page 17). Lastly, we were honored to host Dr. Kate Kraft, Chief and Professor of Pediatric Urology at the University of Michigan as our 2024 Pediatric Urology Visiting Professor.
We are proud to announce the opening of the futureready, patient-focused Honickman Center. A milestone for Jefferson and healthcare in Philadelphia as a whole, the Honickman Center embodies our vision of a patient experience that is not only technologically advanced, but also deeply compassionate.
The Honickman Center represents a new era for Jefferson’s Department of Urology, combining the expertise of our nationally recognized team with truly state-of-the-art facilities and technologies.
The department’s outpatient headquarters is on Level 11 of the building, where our team provides patients with the full range of outpatient urology services—offering advanced procedures with a focus on minimally invasive techniques and robotic surgery. A key benefit of the Honickman Center is our ability to work in tandem with Jefferson’s major specialty service lines throughout the building, delivering worldclass urology treatment options, enhanced clinical trial capabilities, and unprecedented convenience for our patients.
Urology Programs and Outpatient Services at the Honickman Center
Jefferson’s Department of Urology provides care in the diagnosis and treatment of all urological diseases at the Honickman Center, including (but not limited to):
• Endourology and Kidney Stones
• Genito-Urinary Oncology
• Women’s Pelvic Health
• Robotic Surgery
• Men’s Health
• Reconstructive Urology
Honickman Center 1101 Chestnut Street, Philadelphia, PA 19107


To view giving opportunities on Level 11 of the Honickman Center, please scan the QR code on the left.
For more information about how to support our Urology Department, please contact Elena Boroski at Elena.Boroski@jefferson.edu.
“The opening of the Honickman Center marks an exciting new phase for our department.
This facility brings urology patients and providers together and offers comprehensive care where clinical research, outpatient surgery, laboratory testing, pre-operative testing, medical oncology, and pharmacy services are all provided under one roof. It is a testament to Jefferson's commitment to growth and our position as a leader within the region.
Our department now has a dedicated space in the center where we can continue providing the most advanced clinical, surgical, and research-driven care available.”
Paul H. Chung, MD, FACS Associate Professor Department of Urology
Health Physician Site Director, Honickman Center
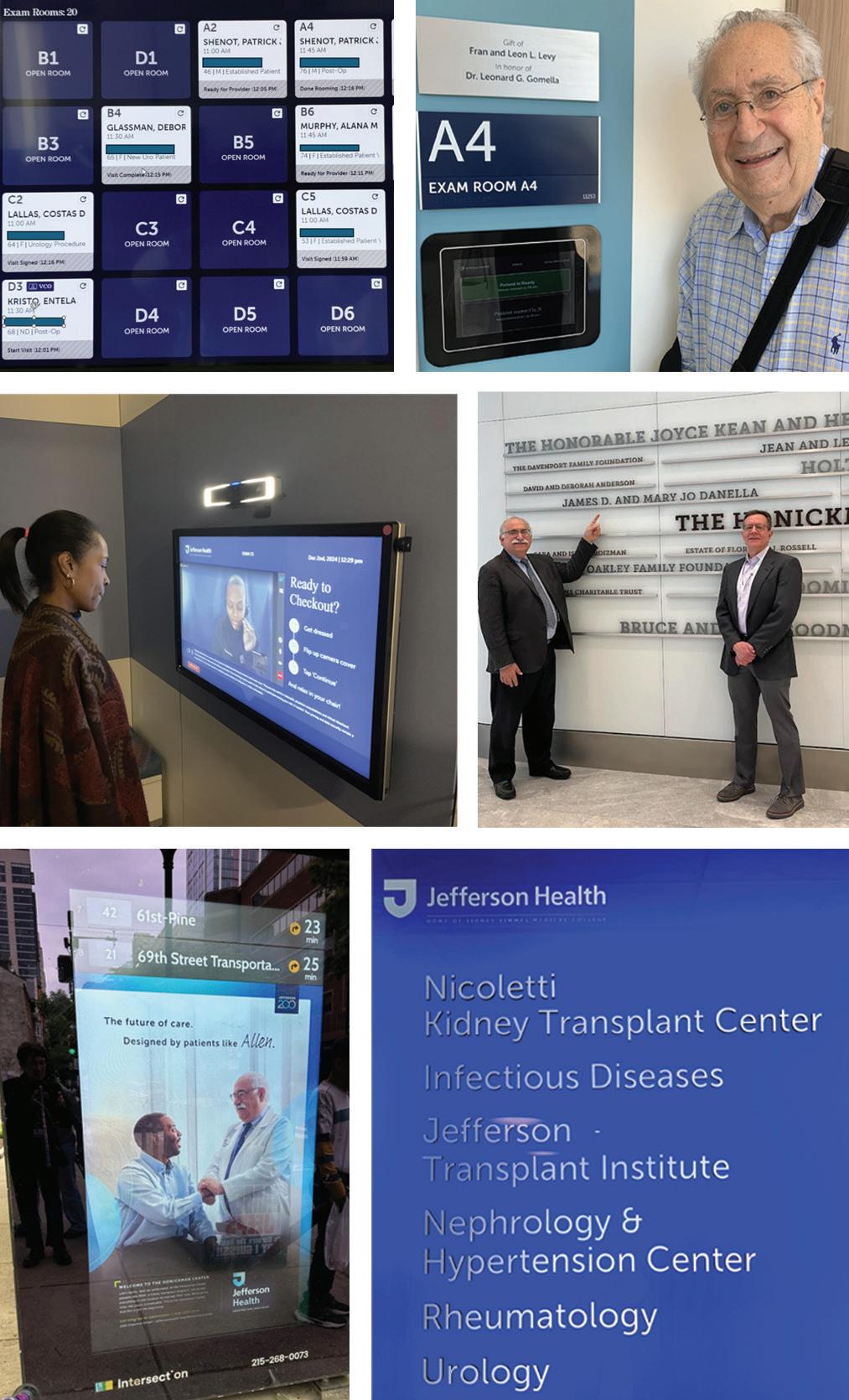
1 A new feature in our Honickman Center office is an exam room tracking system to provide the most efficient rooming for patients.
2 The Department of Urology expresses thanks to donors like Fran and Leon Levy for their generous support of Urology in the new Honickman Center.
3 Another pioneering feature of the Honickman Center is the ability for patients to do efficient in-room self-check-out using a stateof-the-art video system.
4 Drs. Leonard Gomella and Kevin Kelly, Chair of Medical Oncology, acknowledging major Honickman Center donors such as Jim and Mary Jo Danella on the lobby donor wall.
5 Dr. Gomella was honored to be included in the Jefferson Health promotion of the new Honickman Center.
6 On the Honickman Center’s 11th floor, Urology is located next to related clinical practices.
Starting in July 2024, our fellowship-trained Urologic Oncology specialists, Drs. Mihir Shah and Adam Metwalli, partnered with our Jefferson Cherry Hill Hospital Sidney Kimmel Comprehensive Cancer Center colleagues to expand our NCI Comprehensive Cancer Center Care in South Jersey.
A new Jefferson Urology faculty member has joined the South Jersey care team, Dr. Masaya Jimbo. He is a Graduate of Sidney Kimmel Medical College with an additional PhD in Cell Biology. After urology residency at the Mayo Clinic, in Rochester, Minnesota, he completed a fellowship in Men’s Health at the University of Utah. In addition to providing general urology care, most of his practice will focus on Men’s Health. He brings unique expertise to Jefferson Health and our region as an expert in microsurgery treating conditions such as infertility in males and microsurgical vasectomy reversal. Cherry Hill Hospital has installed a new state-of-the-art ORBEYE® surgical microscope to facilitate his work there (see page 26). In addition, he will be collaborating with Reproductive Medicine Associates (RMA) in Marlton.

On September 10, 2024, Jefferson Urology welcomed our first patients at our newest Southern New Jersey practice location in Sewell on Fish Pond Road. It is conveniently located 2.5 miles from the Jefferson Washington Township Hospital. The Fish Pond Road site is a 15,000-squarefoot building shared by Urology, Otolaryngology, General/Vascular/Bariatric Surgery, Rheumatology, Allergy/Immunology, Non-Oncology Infusion, and Gastroenterology.
This $15 million facility is surrounded by a large parking lot and is adjacent to the Jefferson Primary and Specialty Care building. The building is fully staffed with a check-in/check-out team managed by a multi-specialty site manager. LabCorp is also on-site for phlebotomy orders. In addition, there is a lab, medication room, combined break room/conference room, and many shared touchdown spaces for providers and staff. Allocated for Urology are 4 exam rooms and 1 large procedure room.
Dr. Paul Bloch, Assistant Professor of Urology, sees general Urology and Men’s Health patients at Fish Pond. In addition, he performs surgery at Washington Township Hospital, including patients interested in Aquablation™ procedures. Deborah T. Glassman, MD, FACS, Associate Professor of Urology, sees general Urology patients and has dedicated procedure time at the Fish Pond location.
Along with seeing patients at Fish Pond, Dr. Whitney Smith, who is certified in FPMRS (female pelvic medicine and reconstructive surgery), has OR privileges at Washington Township Hospital and the nearby Surgery Center. She serves as Section Chief of Urogynecology for Jefferson, New Jersey, and works closely with other Women’s Health Specialists in Jefferson Health. She serves as Core Faculty Member for the Jefferson New Jersey UROGYN and OBGYN residency program.


To schedule a visit with Jefferson Urology, 354 Hurffville Cross Keys Rd., Building 3, Sewell, NJ, 08080, call 844.542.2273.
Urology staff at Fish Pond include 1 RN, 1 APP, and 1 MA. Urologic procedures, treatments, and studies include: non-video UDS, PTNS, cystoscopy, vasectomy, TRUS, and Botox. In addition to provider visits, Urology offers nurse visits as needed with the RN. Patients, providers, and staff like the office accessibility, convenient location, free parking, and close proximity to the main Jefferson Hospital. See page 86 for our Fish Pond Urology staff members.
According to Owen C. Montgomery, MD, FACOG, Physician Vice President for Jefferson Medical Group East Region, “We are excited to have expanded care options from our Sidney Kimmel Medical College Urology faculty in our Jefferson New Jersey system. In addition to our long-term Jefferson Urology providers in Cherry Hill, the addition of urologic oncology, microsurgical expertise and our new urology access options in Washington Township are welcome additions to Jefferson Health in South Jersey.” And, yes, there really is a fish pond at the location! The site was formerly a farm!

Jefferson and Lehigh Valley Health Network (LVHN) officially merged on August 1, 2024, creating a leading integrated academic healthcare delivery system, alongside a national research university and an expanded not-forprofit health plan. The unified system will increase access to high-quality and affordable care, clinical research, and health plan offerings and address health inequities for urban and rural communities in Eastern Pennsylvania and Southern New Jersey. The combination creates one of the 15 largest nonprofit hospitals in the U.S. with 32 hospitals, more than 700 care sites, and employs more than 65,000 people. This merger includes Jefferson’s 18 hospitals with 15 in Pennsylvania and three in New Jersey and the LVHN with 14 hospitals, all in Pennsylvania. With the merger of Lehigh Valley Health Network and Jefferson, Sidney Kimmel Medical College (SKMC) has initiated key Jefferson faculty appointments so we can begin sending students to LVHN this academic year. Drs. Angelo Baccala and Jatin Gupta are the first LVHN urologists scheduled for these new SKMC faculty appointments.
With this historic system merger, Dr. Angelo Baccala, Chief, Division of Urology, was asked to review Urology care in the LVHN.
OF
The merging of different urology subspecialists in one network allows us to optimally serve patients in the prevention, diagnosis, and treatment of all urologic disorders through collaboration like in the academic setting. By aligning physicians with shared expertise in different disciplines, we can offer patients the best in clinical care, research, treatment, and prevention.
Jefferson Urology looks forward to collaborating with our new urology partners as part of Jefferson Health.
At Lehigh Valley Physician Group (LVPG) Urology, we are dedicated to achieving excellence in patient care, teaching, and research. We treat individual urologic conditions with specialized treatments designed for each condition specifically through our different centers of excellence. We bring academic urology to the community setting. This is one reason why we are so excited to join forces with Jefferson Urology.
Our unique centers of excellence enable us to provide a complete range of urology care including urologic sub-specialties to our community. Our team is a cohesive one, consisting of full-time faculty, advanced practitioners (Physician Assistants and Nurse Practitioners), residents, and medical students. As part of the accepted mission of the Lehigh Valley Network, our physicians are all committed to providing exceptional, personalized patient care and share a passion for better medicine.
The physicians within our practice are grouped based on their expertise in specific disciplines in urological disease care. These groupings form centers of excellence that focus on specific diseases and conditions with clinicians that collaborate which each other to provide collectively developed dynamic solutions for our patients.
LVPG Urology is divided into four clinical subspecialty centers to ensure the most specialized care for our patients: Center for Urologic Oncology and Advanced Robotic Surgery, Center for Endourology and Stone Disease, Center for BPH and Men’s Health, and the Center for GenitoUrinary Reconstruction and Voiding Dysfunction.
Angelo A. Baccala, Jr., MD, MBA, FACS, is Chief, Division of Urology for the LVHN and Deputy Physician-in-Chief Lehigh Valley Institute for Surgical Excellence
is directed by Dr. Jim Johannes who completed his urology training at Jefferson in 2011 (see Alumni Update, page 63). The center is supported by a urologist in Scranton, Dr. Rajbabu Krishnemoorthy. Dr. Kevan Iffrig at our Muhlenberg location joined in 2023. The Center is supported by 2 physician assistants.
We are the center for comprehensive stone care in the Lehigh Valley. Our center emphasizes follow-up care and prevention as much as innovative surgical care. We employ a patient centered approach to our stone patients. To improve timely access, our PAs are often first to meet an acute stone patient, often within 24-48 hours of presentation. We offer the full spectrum of stone care from ESWL, ureteroscopy, and
FOR UROLOGIC ONCOLOGY AND ADVANCED ROBOTIC SURGERY is directed by Dr. Angelo Baccala, Chief of the Urology Division, and Co-directed by Dr. Joseph Feliciano. We are supported by 5 physician assistants.
The Center has one of the region’s most well-trained and largest bodies of collective experience in urologic laparoscopic and robotic surgery. By collaborating with physicians from the area’s only NCI-selected cancer center, we can provide patients with greater access to the latest clinical trials and research-based treatments. Our affiliation with Memorial Sloan Kettering and now

both mini and traditional PCNL. We have been on the forefront of adopting new technology whether it's improved ureteroscopes and higher power laser systems. We medically manage our stone patients aggressively and have an excellent collaboration with our nephrology colleagues utilizing their expertise for our more complex metabolic stone formers.
Our endourology center also is active in research. As a highvolume community hospital, we have participated in clinical trials evaluating new laser systems and devices. Most recently we are one of 7 U.S. sites for the SOUND trial. This is the definitive human trial of a new low-amplitude ultrasound system that allows us to fragment stones in the office setting negating the need for anesthesia.
with our new partners at the Sidney Kimmel Comprehensive Cancer Center and Jefferson Urology further increases access to breakthrough clinical research and increases our ability to provide leadingedge treatment for kidney, prostate, bladder, and testicular cancers. Our experience, coupled with our dedicated research staff, makes us one of the most thorough urologic oncology centers in the region. Our specialized urologists are recognized leaders in minimally invasive approaches for the treatment of urologic malignancies and benign urologic conditions including laparoscopic and robotic approaches for kidney-sparing surgery for kidney cancer, prostatectomies for prostate cancer, and
cystectomies and urinary diversion for bladder cancer. By perfecting minimally invasive surgical procedures, researching new ideas, and providing education, our urologists in the center are committed to providing state-of-the-art patient care for all urologic oncology needs. We have adopted the latest technology in this effort. Currently, we are performing single port surgery for prostate and kidney surgery as well as HIFU (High-Intensity Focused Ultrasound) for prostate cancer.
We are using blue light technology for trans-urethral detection and resection of bladder tumors as well. Our group developed clinical pathways based on AUA guidelines and recommendations for all the cancer disease states we treat. This ensures uniform and best-in-class care for our oncology patients across all our offices.
CENTER FOR RECONSTRUCTIVE UROLOGY AND VOIDING DYSFUNCTION
is composed of two physicians, our center director Dr. Matthew Loecher and Dr. Kaveh Kousari, as well as two physician assistants and several dedicated urodynamic nurses.
We are fortunate to provide the only subspecialized care for urologic reconstruction in the Lehigh Valley for both men and women. We also manage the urodynamic program and offer video urodynamics in the office to provide our complex and transitional patients with complete care of their voiding dysfunction.
We are excited to continue to
modernize the reconstructive options at Lehigh Valley with the introduction of Optilume™ for urethral stricture, Bulkamid™ for female stress incontinence and ProACT™ for male stress urinary incontinence in the last year. We have recently begun our experience with upper urinary tract robotic reconstruction and have performed the first buccal mucosa urethroplasty in the Lehigh Valley. In addition to our newest procedures, we have a large breadth of prosthetic urology and lower urinary tract reconstruction for urethral stricture. We aim to improve our research footprint and are excited to collaborate with our academic partners and provide even better care to our community.

Jefferson Health and Lehigh Valley Network Hospitals
The CENTER FOR MEN’S HEALTH is co-directed by Drs. Clifford Georges, Jatin Gupta, and Kiranpreet Khurana. The center is supported by 2 Urologists in the Poconos, Drs. James Moyer and Michael Eufemio and 1 in Scranton, Dr. Eric Rottenberg. This group has 7 physician assistants as well as a team that consists of expert nurses and medical assistants trained to triage common men’s health concerns and educate patients on therapies such as testosterone injections and intracavernosal penile injections for erectile dysfunction.
We are proud to serve the Lehigh Valley and surrounding areas by providing comprehensive care for various men’s health conditions such

as Benign Prostatic Hypertophy, Male Infertility, Male Contraception, Erectile Dysfunction, Peyronies Disease/ Syndrome, Male Hypogonadism, Ejaculatory Dysfunction, and Chronic Testicular Pain. Not only do we counsel patients on medical therapy options for the above conditions but also perform a wide range of surgical procedures if medical therapy is unsuccessful.
For the treatment of BPH we perform bipolar TURP (transurethral resection of the prostate), REZUM (convective water vapor therapy), Urolift™ (prostatic urethral lift), and Aquablation™. We also are a high-volume center for HOLEP. Having started the program in 2015, we were early adopters in performing

LVHN urologist Dr. Jatin Gupta with urology PA, Jim McGovern
HOLEP in the ambulatory setting. Our HOLEP experience in the community hospital setting has produced numerous presentations at meetings. We are also the first urology practice within the greater Lehigh Valley to offer Aquablation™ and have performed over 215 Aquablation procedures since the inception of the program in July of 2023. We are a key opinion leader site for Aquablation™ and have educated many surgeons across the greater USA on achieving clinical success with the procedure.
In addition to performing routine vasectomies, we also perform male infertility consultations including a comprehensive workup consisting of
semen analysis, specialized blood work, and ultrasound if indicated. We offer cutting edge treatments such as microscopic varicocele surgery and care for men desiring vasectomy reversals.
We are also expertly poised to treat the prevalence of male sexual conditions such as erectile dysfunction and Peyronies disease. Our surgical expertise not only extends to penile prosthesis implantations but also penile plications and graft surgery for refractory Peyronies disease.
Chronic testicular pain is an unfortunate affliction that affects many males but is widely underreported. We are the only urology practice in the Lehigh Valley region to provide a comprehensive testicular pain clinic to medically and surgically manage testicular pain.

COMPREHENSIVE
In partnership with the Sidney Kimmel Comprehensive Cancer Center, the Department of Urology launched the first of its kind program in the Philadelphia region: A Comprehensive Focal Therapy Program for Prostate Cancer. This program is led by Co-Directors Drs. Patrick Gomella and Adam Metwalli, both fellowship trained urologic oncologic surgeons who have experience with focal therapy based on their work at the National Cancer Institute in Bethesda, Maryland.
Localized prostate cancer, the most common non skin cancer affecting men in the United States, has traditionally been treated with whole gland therapies such as radical prostatectomy and external beam radiation therapy. As our knowledge of prostate cancer biology has evolved, for some men, whole gland therapies represent an overtreatment; exposing men to significant quality of life impacts that can be life changing. These side effects involve both urinary and sexual function. Personalized approaches to prostate cancer treatment are important to provide options for patients that balance both cancer control and risks of these side effects. For men with adequate life expectancy, low-risk prostate cancer is managed with active surveillance and highrisk prostate cancer is usually managed with surgery and radiation therapy. For patients with intermediate risk prostate cancer, focal therapy offers a potential alternative with the goal of reducing the risk of permanent urinary and sexual dysfunction. This approach is a natural evolution of prostate cancer treatment with the development of advanced imaging and biopsy techniques that have allowed us to improve the detection of prostate tumors while simultaneously reducing the risk of low-risk cancer diagnosis. Eligibility for a focal

Irreversible Electroporation (IRE) of the prostate is achieved using the proprietary NanoKnife™ system.
Image courtesy AngioDynamics, Latham, NY

The FocalOne™ team following inservice and installation of the unit at TJUH in the summer of 2024.
therapy approach is evaluated with blood work, prostate magnetic resonance imaging, fusion guided biopsy and after a multi-disciplinary evaluation, a personalized treatment plan is developed.
There are numerous focal therapy techniques that have been developed and studied, however, there are only a few currently in widespread usage. These energy sources are designed to deliver a targeted treatment to the prostate tumor, while leaving the rest of the prostate untouched. These techniques are separated into thermal and non-thermal techniques. While many hospitals only have a single modality available, Jefferson’s Department of Urology has three different focal therapy energy sources available to tailor the best approach for each patient’s tumor size and location within the prostate. These include High Intensity Focused Ultrasound (HIFU), Irreversible Electroporation (IRE) and Cryoablation
HIFU is a thermal technique that uses focused ultrasound waves to generate high temperatures in the prostate tissue that leads to targeted coagulative necrosis and cell death. Our platform is the most advanced transrectal HIFU platform available: the robotic Focal One™ system manufactured by EDAP-TMS and the only Focal One™ unit currently available in Philadelphia. Cryoablation, another thermal technique, utilizes argon and helium gas to create ice balls around the probes followed by rapid thawing that lyses cells leading to cell death within the targeted area. Cryoablation has been used extensively in whole gland therapy for post-radiation therapy prostate cancer recurrence and has been adapted for focal therapy treatment of smaller lesions. Cryoablation technology has also been applied to other urologic malignancies such as kidney cancer. IRE is a unique approach that is non-thermal and utilizes high voltage electrical energy, which induces permanent pores in cell membranes leading to death of these cells. In the future, a variety of focal radiation therapy options will be available.
All these current techniques are performed while the patient is asleep under general anesthesia. HIFU treatment is delivered by a trans rectal ultrasound probe and the
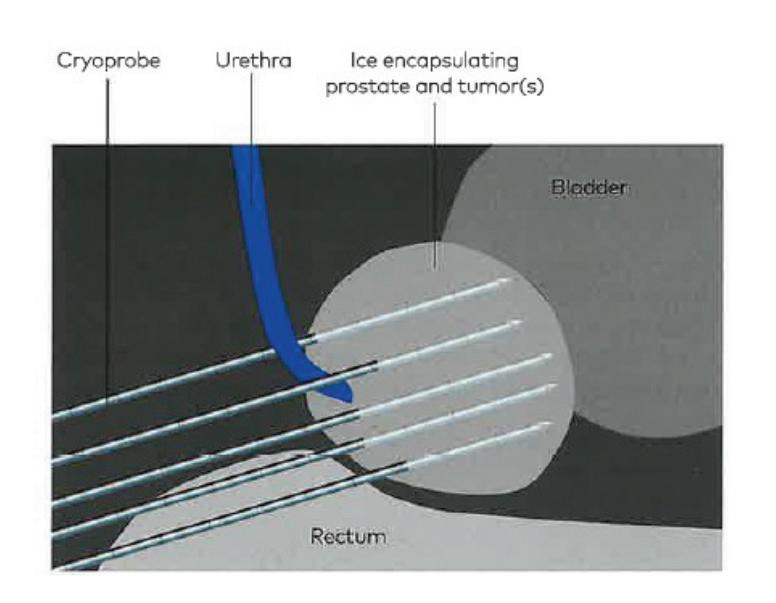
This illustration demonstrates the use of cryoprobes positioned in the prostate. The ice balls will form around the probes and will eventually reach their maximum size, typically at 10 minutes after which the thawing cycle begins. (Image courtesy of Varian Medical Systems, Palo Alto, CA).
cryotherapy and IRE techniques use needles passed into the prostate through the perineal skin. An additional benefit of these treatments is that they are same day outpatient surgeries allowing patients to recover at home after their procedure. A catheter is required in the immediate post-operative recovery period which is removed about 5-7 days after in the clinic. While patients can have short term urinary symptoms such as increased frequency and urgency, these tend to be short lived, in contrast to other urinary symptoms after radical prostatectomy or radiation therapy. As with other prostate cancer treatments, patients are followed closely after focal therapy with routine blood work, prostate imaging and repeat biopsy to ensure treatment success.
According to Dr. Andrew Chapman, Director of the Sidney Kimmel Comprehensive Cancer Center at Jefferson, “There is growing scientific support for prostate cancer focal therapy in the properly selected patient. Many studies are demonstrating similar oncologic outcomes compared to radical prostatectomy or radiation therapy. We are pleased to be able to provide patients with our comprehensive evaluation program at our NCI designated cancer center and offer treatment using different focal therapy techniques where appropriate.”
The Focal Therapy team would also like to acknowledge Alex Khariton, Chief Operating Officer of the SKCCC, Dr. Ed Pribitkin, President, Jefferson Medical Group, and Dr. Baligh Yehia, President of Jefferson Health for their support of this program.
A special hotline has been established for both patients and providers who may be interested in learning more about our Focal Therapy Program, part of our GU Multidisciplinary Clinic in the Sidney Kimmel Comprehensive Cancer Center.

Call 215-50-FOCAL (215-5036225), and a provider will return the call to determine the patient’s initial eligibility for a focal therapy approach.
ORBEYE EXOSCOPE™ BRINGS MICROSURGERY EXPERTISE TO THE DEPARTMENT OF UROLOGY
The Department of Urology is most pleased that Masaya Jimbo, MD, PhD has joined our department (see page 32). During his two years of fellowship, Dr. Jimbo received extensive training in microsurgery - surgeries performed with the assistance of a high-powered operating microscope. Common microsurgical procedures that he performs include vasectomy reversal, varicocelectomy, and microsurgical testicular sperm extraction for infertile men, and spermatic cord denervation for men with primary testicular pain.
Jefferson Health has contracted with Olympus to have the state-of-the-art ORBEYE Exoscope™ for Dr. Jimbo’s use at the Cherry Hill campus. “A traditional operating microscope requires the surgeon and his/her assistant to look through tiny eyepieces,” Dr. Jimbo explains. “Over time, there can be issues for the surgeon such as increased neck strain and risk of injury, especially for longer surgeries like vasectomy reversal. Additionally, if the assistant is not well experienced with using an operating microscope, there can be a challenging learning curve in visualizing structures through the eyepieces and trying to coordinate hand movements. This could lead to longer and less efficient surgery, increased surgeon fatigue, and potentially
Ran increased risk of complications.” Dr. Jimbo goes on to explain the benefits of the ORBEYE as follows: “With this microscope, a small camera is positioned over the patient, and there are no eyepieces to look through. Instead, the surgeon and the assistant wear a specially designed pair of glasses and look at a large 55-inch monitor that provides 3-D images of the operating field in 4K high-definition resolution. This leads to improved ergonomics and reduced surgeon fatigue, easier learning curve for assistants, and ultimately a more efficient and safer surgery for the patients.”
In addition to the ORBEYE Exoscope™ that is now available for more complex cases at our Jefferson Cherry Hill hospital location, some of the less complex microsurgery procedures are also available at the Honickman Surgical Center in Philadelphia.

The ORBEYE Exoscope™ system is available at our Jefferson Cherry Hill Hospital surgical center.
The ORBEYE Exoscope™ microsurgical system provides the surgeon, wearing special glasses, with a 4K 3D image displayed on a large in-room monitor, enhancing the efficiency and accuracy of the procedure being performed. (Image courtesy of Olympus America, Center Valley, PA)


WATER VAPOR THERMOTHERAPY FOR BENIGN PROSTATIC HYPERPLASIA
ezum™ is a minimally invasive treatment for BPH that was FDA approved in 2015. This procedure uses a small volume of steam to ablate prostate tissue and reduce urinary obstruction and improve lower urinary tract symptoms. Rezum was included in the 2018 AUA guidelines and has its own dedicated CPT code. Unlike other BPH surgical treatments, Rezum™ does not lead to permanent retrograde ejaculation in 94% of cases and does not involve permanent indwelling implants within the gland. The short- and medium-term outcomes published in the urologic literature have been very favorable with 5-year outcomes demonstrating an average 10-point reduction in AUA Symptom Score, a nearly 30% reduction in prostate volume and a retreatment rate <5% which is 70% lower than other competing minimally invasive BPH treatments. Operative time for Rezum™ is typically less than half of other surgical interventions. Dr. Adam Metwalli has extensive experience with Rezum™ prior to joining the Jefferson Urology faculty in 2023, and he was instrumental in bringing Rezum™ to Jefferson.
This procedure was introduced to Thomas Jefferson University Hospital in 2024 and was approved for a 10-patient trial by the Value Analysis Committee. This trial was successfully completed in October 2024. Overall, this was a successful trial and now the VAC is evaluating the clinical outcomes and the appropriate reimbursement for this procedure. Full approval of the procedure by the VAC is anticipated, and there is a list of patients awaiting final approval so they can be treated. This is a useful addition to the spectrum of BPH treatments available at Jefferson Health. In addition to the gold standard transurethral resection of the prostate (TURP), variety of other surgical modalities are available at Jefferson Health in Center City based on the size and configuration of the obstructing prostate. Some of these include holmium laser enucleation of the prostate (HoLEP), the diode laser enucleation of the prostate (DiLEP), Urolift™, robotic simple prostatectomy and robotic Aquablation.™

Dr. Paul Bloch with the robotic Aquablation™ unit in Washington Township.
Rezum™ Water Vapor Thermotherapy system to treat benign prostatic hyperplasia.
Courtesy Boston Scientific, Marlborough, MA


IIn a significant advancement in the treatment of erectile dysfunction, in 2024 Boston Scientific released the TENACIO™ pump, the newest update to the AMS 700 implant series. The TENACIO™ pump, with its advanced engineering and new design, offers a more reliable and efficient inflation experience, addressing common issues such as "sticky pump" scenarios where the pump can be difficult to inflate and deflate the penile cylinders. Key features of the
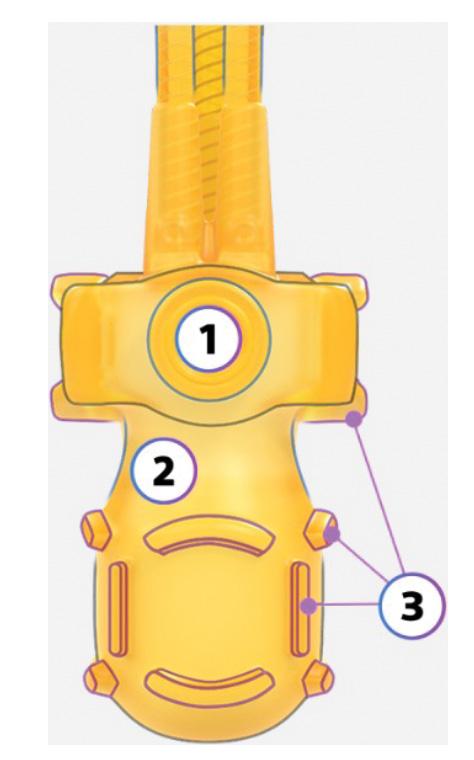
THE TENACIO™ PENILE
PROSTHESIS new pump design aims to impact outcomes and streamline the patient experience. It features a high-profile deflation button to initiate one press automatic deflation an elongated neck to distinguish deflation button from inflation landmarks and prominent pump grips designed to facilitate pump control and ease of use
Image courtesy Boston Scientific, Marlborough, MA
Residents Drs. JY Leong, and Carlos Perez with Dr. Paul Chung (center) after the first AMS 700 TENACIO™ penile implant at Jefferson. Dr. Chung was one of a select group of prosthetic urologists to participate in the early release of the innovative product.
AMS 700™ INFLATABLE PENILE PROSTHESIS with the new TENACIO™ Pump
Image courtesy Boston Scientific, Marlborough, MA
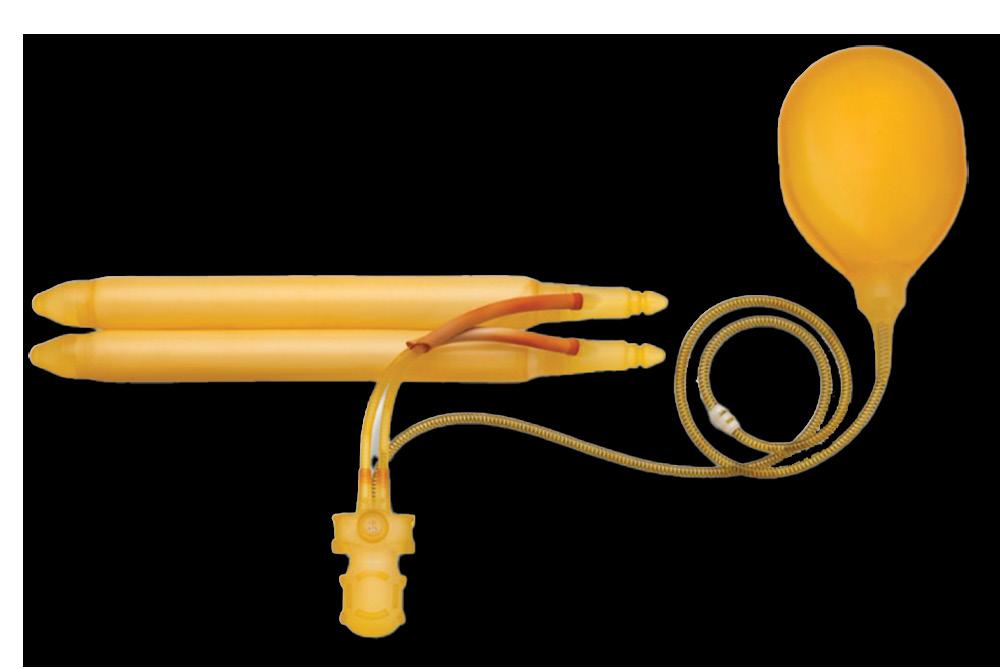
TENACIO™ pump that is implanted in the scrotum, include prominent pump grips for better control and support, channels designed to reduce sticking, and a high-profile deflation button that provides tactile feedback and requires only a one-press release, even when pressed off-axis. These enhancements are designed to streamline the patient experience, providing a more natural and intuitive use of the device.
Dr. Paul H. Chung was selected as one of only a handful of prosthetic urologists across America to participate in the early market release of the product and was the first surgeon in Pennsylvania to utilize the TENACIO™ implant. Additionally, Dr. Chung participates in the IT MATTERS registry (https:// clinicaltrials.gov/) a post-market clinical trial focused on assessing the impact of penile prostheses on the quality of life in men with erectile dysfunction. Dr. Chung continues to grow a high-volume prosthetic practice focusing on both erectile dysfunction and stress urinary incontinence. His research interests also include evaluating advanced ultrasound modalities to diagnosis erectile dysfunction, developing methods to mitigate penile implant infection, and developing novel methods to treat urethral stricture disease.
Enhancements that are designed to streamline the patient experience.
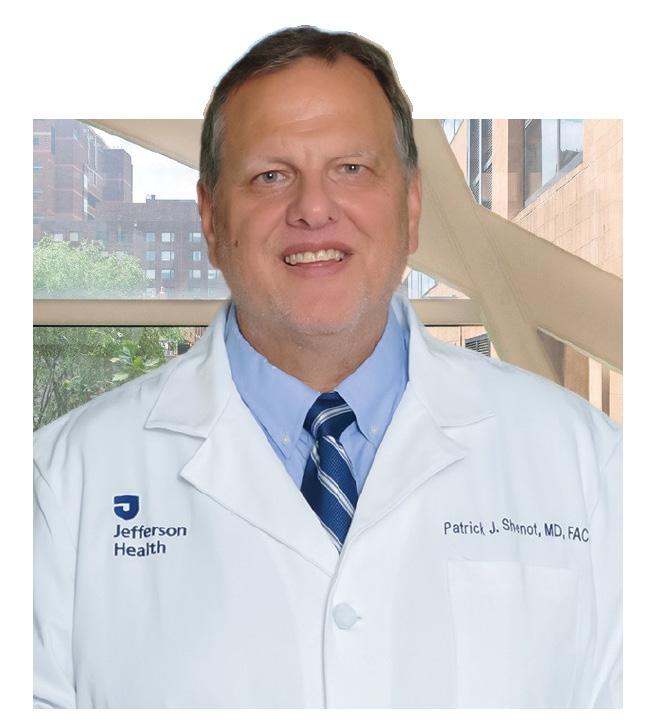
As he completed medical school in the early 1990s, Patrick Shenot, MD, FACS, was determined to pursue his residency at a big-city hospital. But even he was surprised by what he found when he interviewed at Jefferson.
“It was immediately apparent to me that the culture here was completely different than those of other programs,” Dr. Shenot says. “The environment was uniquely collegial, and the level of trust and autonomy offered to residents was impressive.”
Fast forward three decades later, and Dr. Shenot now plays an integral role in furthering the collaborative approach to education at Jefferson. As the Director of the Urology Residency Program for more than 20 years, Dr. Shenot has left an indelible mark on generations of future urologists, shaping both medical education and the specialty.
Dr. Shenot’s love of science is what drew him to medicine. “I decided to become a urologic surgeon because I love working with my hands,” he says. After completing his residencies in General Surgery and Urology, Dr. Shenot became an Instructor of Urology in 1997 while also pursuing a fellowship in neurourology.
A turning point in his career came in 2002, when Leonard G. Gomella, MD, FACS, became Chair of the Department of Urology. Dr. Gomella asked Dr. Shenot to serve as the Program Director for the Urology Residency. It didn’t take long for him to accept.
“At the time, the Accreditation Council for Graduate Medical Education (ACGME) was instituting a measurement-driven approach to residency programs,” Dr. Shenot recalls. “One
of my first priorities was to create objective milestones for our residents so our program could keep pace with the evolving GME landscape.”
Today, Jefferson’s Urology Residency has gone more than 15 years without a citation from ACGME, a recognition of the highquality standards implemented under Dr. Shenot’s leadership. Additionally, the program consistently ranks among the top 20 nationally in annual lists compiled by Doximity and U.S. News & World Report
As a mentor and teacher, Dr. Shenot instills the importance of hard work as a core value that defines successful urologists. “I always tell residents to do their homework so they’re always well prepared whether they’re lecturing, presenting, seeing patients or performing surgery,” he says. His other key learning lesson: don’t take shortcuts.
The most rewarding part of his teaching work, Dr. Shenot says, is watching residents evolve from medical students to competent surgeons. “When a resident calls me five years later and wants to collaborate on a complex case, I’m thoroughly impressed,” he says.
In addition to leading the residency program, Dr. Shenot is an accomplished urologist and researcher. His major clinical interests include neurourology, voiding dysfunction
and urologic care for patients with spinal cord injuries. Last year, in recognition of his contributions to the field, Dr. Shenot was awarded the Sidney Kimmel Medical College Outstanding Clinician Award for Surgery and Surgical Subspecialties.
Additionally, Dr. Shenot has served as a principal investigator in multiple clinical trials, studying ways to ameliorate neurogenic bladder and other urologic conditions in spinal cordinjured patients. “When you look at medical complications, the bladder is responsible for a very high percentage of complications these patients face,” Dr. Shenot says. “These bladder issues also impede these patients’ quality of life.”
Dr. Shenot played a key role in a series of multicenter clinical trials across the U.S. and Continued on next page

As Urology Residency Program Director since 2002, Dr. Shenot takes pride in all our successful residency graduates. Here Dr. Shenot is presenting presenting former resident Kymora Scotland, MD, PhD, her signed graduation gift. In 2023, the American Urological Association announced her as the recipient of the Rising Star in Urology Research Award. Dr. Scotland is an assistant professor in the Department of Urology, Division of Endourology at UCLA in Los Angeles.
One of my first priorities was to create objective milestones for our residents so our program could keep pace with the evolving GME landscape.

Deborah T. Glassman, MD, FACS
interested in urology. The program began eight years ago with two first-year students at our Center City campus. Today, it’s grown to include 15 first-year and second-year students annually across both the Center City and East Falls campuses.
Dr. Patrick Shenot
Europe that led to Food and Drug Administration approval of Botox™ for treatment of neurogenic bladder in spinal cord patients. Currently, he’s conducting a trial examining whether viral vector therapy can create Botox™like compounds within the bladder to potentially reduce the frequency of treatment for these patients. Dr. Shenot has also participated in research studying the potential viability of the autologous neobladder, a tissue-engineered bladder replacement. (See page 10.)
Not surprisingly, Dr. Shenot is an explorer at work and in his personal life. A married father of three, Dr. Shenot is an avid hiker, having visited numerous National Parks with his sons. He also regularly gets his family together for pilgrimages to State College, where they cheer on his alma mater’s nationally ranked football team, the Penn State Nittany Lions.
When he looks to the future, Dr. Shenot wants to ensure his valuable work continues. “About half of my patients have spinal cord injuries,” he says. “When it’s time for me to find a replacement, I want to find someone who will continue to make Jefferson a destination for these patients now and for generations to come.”
Deborah T. Glassman, MD, FACS, is far more than a urologist. She’s also a researcher, an educator, a parent, a yoga teacher and a playwright. While each of these roles may appear distinct, they share a common thread: a commitment to forming deep, human connections.
“Yoga teaches you to be present, good actors are always present, and doctors need to be present with their patients,” Dr. Glassman says. “Our patients are people; they have emotion, feeling and energy. When you’re present with them, you can treat them as a whole person and help them develop a holistic sense of wellbeing.”
Dr. Glassman’s lifelong exploration of both the science and human side of medicine began in the mid-1990s when she chose to study urology. “I was attracted by the breadth of the field and the fact that we care for a wide variety of patients,” she says. “Generally, patients do very well in terms of their outcomes in urologic diseases.”
As an active investigator, Dr. Glassman has advanced the field through research. She was a pioneer in examining the use of telemedicine in urology, publishing multiple journal articles exploring the efficacy of and patient satisfaction with virtual visits prior to telehealth’s widespread adoption during the SARS-CoV-2 pandemic. Additionally, Dr. Glassman has served as the Telehealth Champion in the Department of Urology.
As an educator, Dr. Glassman has spearheaded the growth of the urology component within the Master of Science in Physician Assistant Studies program at Jefferson, which includes one week of didactic teaching to students
“My goal in teaching is to help students combine the science of urology with humanism,” says Dr. Glassman, who earned a SMKC Dean’s Award for Excellence in Education in 2022. “It’s incredibly satisfying to see that ‘a-ha’ moment when my students realize the human sitting across from them is more than a disease process.”
In addition to inspiring the next generation of urologists, Dr. Glassman is also widely respected by her peers. She’s earned a place on Philadelphia Magazine’s Top Doctors list three times, and in 2022, she was chosen as an Exceptional Woman in Medicine award, a recognition of her outstanding accomplishments and dedication to the field of medicine.
Throughout her 22-year career, Dr. Glassman has explored her own personal growth. She started practicing yoga as a medical student and, in 2009, became certified as a yoga teacher, first teaching classes at her synagogue and then creating her own online teaching business – Shabbhakti Yoga – during the pandemic.
“My intention from the start was to bring yoga into the practice of medicine,” Dr. Glassman says. “Yoga gives me a universalistic way of looking at the world, helping me live in my body and not just in my head, and allowing me to understand how one pursuit in life influences the others.”
More recently, Dr. Glassman rekindled her passion for acting, something she had done initially in high school and college. In 2017, she enrolled in online acting classes through HB Studio, a renowned New York City school that trains actors, playwrights and directors. She also participated in The Empathy Project, which today is a series of workshops designed to introduce Jefferson students and health professionals to the theater.
Continued on page 32
Continued from page 31
“Acting reminds me that we are all different beings and have different world views,”
Dr. Glassman says. “It’s taught me how to respect other’s views and not impose my world view on my patients.”
Earlier this year, Dr. Glassman made her debut as a playwright, director and producer. Her production, titled “Vigil,” chronicles the last days in the life of a beloved family matriarch.
“It’s autobiographical in that it explores my family’s experience at my grandmother’s bedside,” Dr. Glassman says.
Presented as a table read at the Philly Fringe Festival in September, ‘Vigil’ was wellreceived. Another table read is likely, following which Dr. Glassman will assess whether the production can move into full staging.
Dr. Glassman acknowledges that juggling medicine, yoga, acting and family (she’s a mother of two children) isn’t always easy. “Balance is fleeting, and there is no magic answer,” she says. “But I believe it’s important to make time for the things you really love and feed your soul, and I have a wonderful, understanding family that encourages me to make time for myself.”

Every one of her unique life experiences, Dr. Glassman says, has helped to make her a better provider. “I’ve learned that humans aren’t neat—they’re messy—and if we try to make them neat, we’re missing out, because we end up treating the disease and not the patient,” she says. “And in urology, we all have to learn to treat the patient, because sometimes we can’t treat the disease.”
Our patients are people;
they have emotion, feeling and energy. When you’re present with them, you can treat them as a whole person and help them develop a holistic sense of well-being.
Now, drawing on her extensive experience and passion for holistic care, Dr. Glassman will take on a new challenge as the “Chief Wellness Officer” for the Department of Urology. In this new role, she will be an active participant in the Jefferson Provider and APC Wellbeing (JPAW) Council. Additionally, Dr. Glassman will participate in training sessions and serve as a well-being expert for departmental, faculty, house staff and APCs in our department. Her contributions will help Jefferson continue to build a holistic environment where both caregivers and patients can thrive.

The Department of Urology is pleased to welcome back to Jefferson Dr. Masaya Jimbo. He is a major addition to our department as well as a key member of Jefferson Men’s Health team.
Dr. Jimbo graduated from Thomas Jefferson University / Sidney Kimmel Medical College in 2017 with dual MD/PhD degrees. He completed his 5-year Urology residency at the Mayo Clinic in Rochester, MN, then completed a 2-year fellowship in Andrology and Men’s Health with a focus in microsurgery at the University of Utah in Salt Lake City, UT. He is joining Sidney Kimmel Medical College as an Assistant Professor in Urology. Dr. Jimbo is a member American Urological Association, the Sexual Medicine Society of North America and the American Society for Reproductive Medicine.
As a Men’s Health provider, Dr. Jimbo’s areas of focus include male sexual health (e.g. erectile dysfunction, Peyronie’s disease, testosterone deficiency/hypogonadism) as well as male infertility. He is available to see general urology and men’s health patients both in Center City at our brand-new Honickman center and at Jefferson New Jersey in Cherry Hill. He brings unique expertise to Jefferson Health and our region as an expert in microsurgery treating conditions such as infertility in males and microsurgical vasectomy reversal. Cherry Hill Hospital has installed a new state of the art ORBEYE® surgical microscope to facilitate his work there (see also page 28). In further support for his expertise in infertility, he will also be collaborating with Reproductive Medicine Associates (RMA). Jefferson Health is proud to partner with as RMA to bring the most advanced reproductive endocrinology and fertility care to the Philadelphia area.
Dr. Jimbo is a strong addition to our Department of Urology Men’s Health team that includes urologists Drs. Paul Chung, Perry Weiner, Irv Hirsch and who also work alongside other providers in our Men’s Health team.
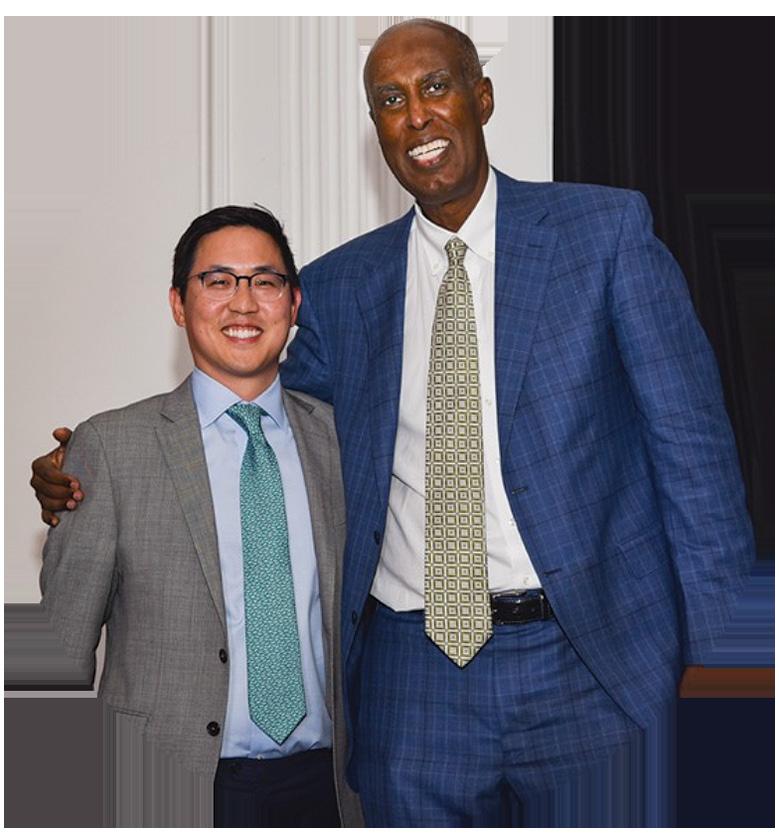
Congratulations to Dr. Paul Chung, Associate Professor of Urology, and Director of Jefferson’s Men’s Health Program, who received an SKMC Deans Award for Excellence in Education at the annual Faculty Awards Dinner. The recognition was presented by Said A. Ibrahim, MD, MPH, MBA, the Anthony F. and Gertrude M. DePalma Dean of Sidney Kimmel Medical College.
In addition, we congratulate Dr. Paul Chung who has become the new Director of Jeffersons Men’s Health Program with Dr. Perry Weiner recognized as the program’s Founding Director. Associate Directors of the Jefferson Men’ Health Program include Drs. Weiner, Hirsch and Jimbo.
Dr. Burnett is shown here with Dr. Alana Murphy, Associate Professor in the Department of Urology, who served as President of the Philadelphia Urology Society in 2024.

Drs. Pat Shenot and Alana Murphy join in celebrating Dr. Smith’s FPMRS certification. Both Dr. Shenot and Murphy are also FPMRS certified.
Assistant Professor of Urology, Dr. Whitney Smith, has obtained her specialty board certification in Female Pelvic Medicine and Reconstructive Surgery (FPMRS). Female Pelvic Medicine and Reconstructive Surgery focuses on the surgical and non-

and pelvic pain. Before joining our Jefferson faculty, Dr. Smith completed a two-year fellowship in FPMRS at Wake Forst University. The American Board of Urology has only three levels of certification for urologists: General Urology, Pediatric Urology and Female Pelvic Medicine and Reconstructive Surgery.
On February 12, 2024, the annual Philadelphia Urology Society “BA Thomas Oration” was delivered by Arthur Louis (Bud) Burnett, II, MD, MBA, FACS. He is the Patrick C. Walsh Distinguished Professor of Urology Professor, in the Department of Urology and the Oncology Center at Johns Hopkins University School of Medicine in Baltimore. The title of his talk was: “Novel Techniques and Technological Innovations to Preserve Erectile Function after Radical Prostatectomy.”

On September 19-20, 2024, Dr. Leonard Gomella served as the Department of Urology Oregon Health Sciences University (OHSU) Department of Urology 2024 Slusher Visiting
Professor in Portland, Oregon. The professorship is named in honor of Mr. Howard Slusher, a well-known professional sports agent and executive leader for Nike based in Beaverton, a
The Department of Urology at Oregon Health Sciences University welcomed Dr. Gomella as their 2024 Slusher Visiting Professor. Shown here are Dr. Chris Amling, Urology Chair, Dr. Michael Conlin, former Jefferson Urology fellow and Dr. John Barry, Chair Emeritus and Past President of the American Urological Association.
suburb of Portland. He was a longtime friend and supporter of Dr. John Barry, Urology Chair Emeritus at the University of Oregon.
Congratulations to Dr. Mihir Shah who achieved his fellowship certification in the American College of Surgeons (FACS) this past year. Dr. Shah is Assistant Professor in the Department of Urology and has recently been appointed Vice Chair for Research.

Dr. Shah also recently participated in the Sidney Kimmel Medical College Jefferson Winter CME symposium in Jackson Hole, Wyoming, where he presented Jefferson’s experience with “Single-Port Robotic Urologic Surgery.”


Drs. Lenny and Tricia Gomella share personalized books with Mr. Bruce Ratner during his Honickman Center presentation.
On June 26, 2024, Mr. Bruce Ratner, author of the new book, Early Detection: Catching Cancer When It’s Curable, visited the Honickman Center for an interactive program focusing on cancer early detection. Mr. Ratner is also a wellknown New York real estate developer. At the event, Dr. Leonard Gomella, Department of Urology Chair, presented Mr. Ratner with a personalized copy of his 1993 book, Recovering from Prostate
Cancer, the first book written specifically for patients on prostate cancer detection and treatment.
The cancer center event was sponsored by Margie and Jeffrey Honickman and Linda E. Johnson and moderated by Keith Leaphart, DO, MBA, Executive Vice President, and Humana Chief Health Equity and Community Impact Officer for Jefferson Health.

On an Alaska Airlines flight to Portland, Oregon on Friday, March 22, 2024, Dr. Glassman responded to a medical emergency for a male passenger who had passed out. A call was made to anyone who was a doctor to assist. Dr. Glassman and two other passengers performed CPR for 45 minutes while the plane was diverted to Billings, Montana.
A letter by another passenger recounting the event and specifically recognizing Dr. Glassman was sent to Dr. Matt Dane Baker, Provost, and Chief Academic Officer, Thomas Jefferson University.
According to Dr. Baker: “I wanted to share this acknowledgment with the Jefferson Community of Dr. Glassman’s heroic efforts in saving this man’s life.”
Dr. Paul H. Chung, Director of Men’s Health and Reconstructive Urology, participated as faculty for the first “Educational Course for Motivated Implanters” sponsored by the Society of Urologic Prosthetic Surgeons (SUPS) on November 1-2, 2024 in Philadelphia. Attendees from across the nation came to improve their skills and knowledge of penile prosthesis surgery. The program included
a half day of didactics and a full day of livestream penile prosthesis surgery at Thomas Jefferson University Hospital and Fox Chase Cancer Center. Topics covered all aspects of penile prosthesis surgery ranging from patient counseling to surgical technique. The SUPS strives to educate and support the highest standards of practice, research, education, and surgical study of anatomy, physiology,
pathology, diagnosis and surgical treatment of male erectile dysfunction, urinary incontinence and other penile disorders. In addition, the Society of Urologic Prosthetic Surgeons provides a forum for the exchange and discussion of new ideas, thoughts and concepts in this field. Dr. Masaya Jimbo, our newest Assistant Professor of Urology, participated in the course.
Urology

CASTLE CONNOLY AND PHILADELPHIA MAGAZINE
JEFFERSON HEALTH
2024 UROLOGY TOP DOCTORS
We are pleased to present our Jefferson Health Urologists who have been recognized in “Top Doctor” listings. The Philadelphia Magazine publishes this list each April based on the Castle Connoly nomination process. However, Castle Connoly now includes their formal “Top Doctors” listing on a rolling basis throughout the year. This list represents both the most recent Philadelphia Magazine and ongoing Castle Connoly updated list as of December 2024.
Jefferson University Physicians
Deborah T. Glassman
Leonard G. Gomella
Patrick T. Gomella
Joseph K. Izes
Costas D. Lallas
Adam Metwalli
Alana M. Murphy (Urogynecology/FPMRS)
Mihir Shah
Patrick J. Shenot
Jefferson Medical Group
Physicians
Philip H. Abbosh
Howard Altman
Lee M. Blatstein
Cadence A. Kim
Marc Lavine
Edouard J. Trabulsi


DR. GOMELLA CONNECTS WITH SKMC GRADUATE AND AUA SECTION PRESIDENT DR. GREG ADEY
During the 2024 New England AUA meeting in Providence, RI, Dr. Gomella presented data on the Society of Urology Oncology Clinical Trials Consortium using Adstiladrin™ (nadofaragene firadenovec). This is the first intravesical gene therapy approved for bladder cancer. Dr. Gomella is shown here with Dr. Greg Adey, JMC/SKMC 2000 graduate, who was New England AUA Section President (see alumni news, page 63). Meeting participants also

included New England Section Past Presidents Dr. Kevin Loughlin, Professor of Surgery, Emeritus at Harvard and Dr. William Bihrle, Associate Professor of Surgery (Urology) at the Geisel School of Medicine at Dartmouth. Of note, Dr. Loughlin serves as Associate Editor on the Canadian Journal of Urology with Dr. Gomella and Dr. Bihrle is a former high school classmate of Dr. Gomella.
Dr. Adam Metwalli, Professor in the Department of Urology, has been appointed the Department of Urology Liaison for the Sidney Kimmel Comprehensive Cancer Center. In this role he will also support the new SKCCC Surgical Oncology program led by Dr. Nader Hannah, Jefferson’s new Enterprise Leader for Surgical Oncology. Dr. Metwalli also serves as Co-Director for our brand-new Prostate Cancer Focal Therapy Program (see page 27). He is also involved GU Multidisciplinary Clinic as well as our Small Renal Mass evaluation program located in Center City.
Before joining the Department of Urology in 2023, Dr. Metwalli was an attending Physician in the Urologic Oncology Branch of the NCI in Bethesda and most recently, he was Division Chief of Urology at Howard University in Washington, DC.

Our SKCCC GU Multidisciplinary Clinic has been in operation since 1997. In September 2024, the weekly GU clinic operations moved to our new location on the 14th floor of the Honickman Center. Our team is a collaboration between Urology, Medical and Radiation Oncology, Radiology, Pathology, and Clinical Trials all orchestrated by our GU MDC Coordinator Crystal Sypherd. Patients with prostate, bladder, and kidney cancer can receive consultation with all specialists in one convenient visit.
In April 2024 Jefferson announced that the Sidney Kimmel Cancer Center (SKCC) earned a National Cancer Institute (NCI) "Comprehensive" Cancer Center designation, the highest recognition awarded by the NCI. This 2024 NCI Comprehensive Cancer Center recognition places SKCC among an elite group of only 57 cancer centers nationwide, providing exceptional and personalized cancer care and superior outcomes, fueled by a robust research program. The SKCC has been recognized for its leadership and resources, in addition to demonstrating an added depth and breadth of basic science, clinical research, and population science.
Jefferson’s cancer center journey began in 1990 when our then medical college Dean, Dr. Joseph Gonnella, brought together renown cancer researcher, Dr. Carlo Croce and philanthropist Sidney Kimmel together to establish the Jefferson Cancer Institute. The Jefferson Cancer Institute allowed us to develop the infrastructure to receive our first NCI designation as a Clinical Cancer Center in 1996. Since that first NCI designation, our center has received multiple NCI Clinical Cancer Center designation

renewals over the years. We are honored to now have the highest designation from the National Cancer Institute. Congratulations to Dr. Andrew Chapman, Director of the SKCCC and all of the cancer center leaders on this achievement.
Along with Drs. Dan Petrylak and Maha Hussein, Dr. Leonard Gomella served as Co-Chair of the 17th Annual New York GU conference in March 2024 held in Manhattan. Dr. Petrylak leads the Genito-Urinary cancers medical oncology team at the Smilow Cancer Hospital at the Yale Cancer Center in New Haven, CT. Dr. Hussein is the Genevieve E. Teuton Professor of Medicine in the Division of Hematology/Oncology at the Feinberg School of Medicine, Northwestern University in Chicago. The 2025 program will be held on March 28 and 29. Visit www.gotoper.com/courses/newyork-gu for information on the updated New York City metro location.






1 MEN’S HEALTH WEBINAR WITH DRS. CHUNG AND WEINER As part of Jefferson Health Wellness Webinar Series, Drs. Paul Chung and Perry Weiner participated in an online program that addressed erectile dysfunction, the impact on men’s health and the variety of treatment options available. Replays for this and many other Jefferson Health Wellness Webinar Series are available on YouTube (www. youtube.com/watch?v=UlaKFC64-lI&list=PLq-eEddi_ wgFckqfGT0aLHtaHtnKlx2I0&index=25).
2 JEFFERSON UROLOGY FEATURED IN WORLD NEWS TONIGHT SPOTS During the ABC World News Tonight program with David Muir, several Jefferson Urology spots were featured throughout 2024. During September, Prostate Cancer Awareness Month, Dr. Mihir Shah, Assistant Professor of Urology, was featured in a public service announcement that discussed PSA based prostate cancer screening. In December 2024, a recurring TV spot recognized the Department of Urology as one of the top programs in the country based on the U.S.News and World Report ranking. (see back cover of this 2024 "Year in Review").

3 FOCAL THERAPY FOR PROSTATE CANCER During Prostate Cancer Awareness Month, “Your Radio Doctor” highlighted Jefferson’s Prostate Cancer Focal Therapy Program (see page 26). Dr. Patrick Gomella, from the Department of Urology at Jefferson University Hospital, discussed focal therapy and the range of treatment options available through the program. He also shared valuable insights on prostate cancer risk factors, screening, and testing.
4 DR. ADAM METWALLI PODCAST WITH DR. BRIAN MCDONOUGH Dr. Adam Metwalli, Professor of Urology, was an invited guest on the Dr. Brian McDonough Show where he discussed the evolving role of focal therapy in the management of prostate cancer. See page 26 of this 2024 Year in Review to learn more about our new Prostate Cancer Focal Therapy Program at Jefferson. This show replay is available as a Spotify Podcast (https://open.spotify.com/ episode/3x9OhPVAWGDOzVR6kIVYfE).

5 DR. WEINER 6 ABC NEWS INTERVIEW ON GLOBAL CANCER
INCREASES Dr. Perry Weiner, Associate Professor of Urology, was interviewed by local affiliate 6 ABC News on August 12 to address a recent global study projecting an increase in cancer diagnosis rates among men in the coming decades. He discussed the study’s findings, the types of cancers most prevalent in men and certain risk factors. Globally, lung cancer is the most common but prostate cancer appears to be the most lethal. The interview also reiterated the importance of preventative screenings and early detection.
6 DR. WHITNEY SMITH INTERVIEWED ON DEFENSE SECRETARY LLOYD AUSTIN'S PROSTATE CANCER Defense Secretary Lloyd Austin's “secret surgery” for prostate cancer gained national headlines in early January, 2024. But behind those headlines there was another story: men who are reluctant to discuss prostate cancer. It's a big issue, especially in the African American community, which is impacted at a higher rate. Dr. Whitney Smith, Assistant Professor in the Department of Urology was interviewed and addressed the prostate cancer challenges in the African American community.


7 PA CANCER ADVOCATES TO GATHER AT CAPITOL TO HONOR GOV. SHAPIRO’S DECLARATION OF SEPTEMBER AS PROSTATE CANCER AWARENESS MONTH, URGE LAWMAKERS TO IMPROVE ACCESS TO EARLY DETECTION The Pennsylvania Prostate Cancer Coalition hosted a press conference on September 18, 2024 to recognize the impact that prostate cancer has had on countless Pennsylvanians’ lives and spotlight where lawmakers can limit the deadly impact.
Governor Josh Shapiro signed a Proclamation designating September as Prostate Cancer Awareness Month in Pennsylvania to highlight the scope of prostate cancer, which is the second most common cancer and second leading cause of cancer death among men in the Commonwealth. The Proclamation also reinforces the power for detection to improve survival rates.
Recognizing the importance of early detection for prostate cancer patients, partners, including the Sidney Kimmel Comprehensive Cancer Center, American Cancer Society Cancer Action Network (ACS CAN), ZERO Prostate Cancer, Force, and the PA Prostate Cancer Coalition are urging lawmakers to prioritize legislation that would address barriers to prostate cancer screening, particularly for high-risk men.
Dr. Patrick Gomella, Assistant Professor of Urology and Surgery in the Department of Urology, represented Jefferson’s Sidney Kimmel Comprehensive Cancer Center at the press conference held at the Pennsylvania State Capitol Building, Harrisburg, PA.
“One of the things that I admire most about Leah McDermott, PA-C, is how she seamlessly blends clinical excellence with genuine human connection,” a coworker recently wrote about Leah, who is a physician assistant in the Department of Urology.
Leah, who has been with the department for three years, said she’s the perfect fit for urology. She loves the variety of patients and urologic subspecialties and procedures.
Under the supervision of Perry R. Weiner, DO, Leah sees about 20 patients a day.
“I see everything. … I see new patients and do a lot of procedures in the office,” Leah said.
She agrees, however, that her connection with patients is above and beyond.
The coworker goes on to write, “Watching Leah walk patients to the door, speaking to them with the warmth of an old friend, and thanking them for entrusting her with their care is truly inspiring.”
Dr. Weiner just rolls his eyes when he gets the weekly Press Ganey update, saying he doesn’t have to read it because its just more wonderful things being said about Leah.
During the next six months of Leah’s life, she had a double mastectomy, chemotherapy and radiation. Her hair fell out. She gained 30 pounds because of medically-induced menopause.
“Having cancer is horrendous,” she said. The experience, however, led to good things, including Leah’s pivoting her career plans into urology, where she thought she could help patients get through the types of treatments she had experienced.
Having cancer was a defining moment, according to Leah.
“There’s ‘before-cancer Leah’ and ‘after-cancer Leah,’” she said.
Today, when she’s not working, Leah puts more time into traveling. She wants to be a mom but can’t right now because of the medicine she takes to keep breast cancer at bay.
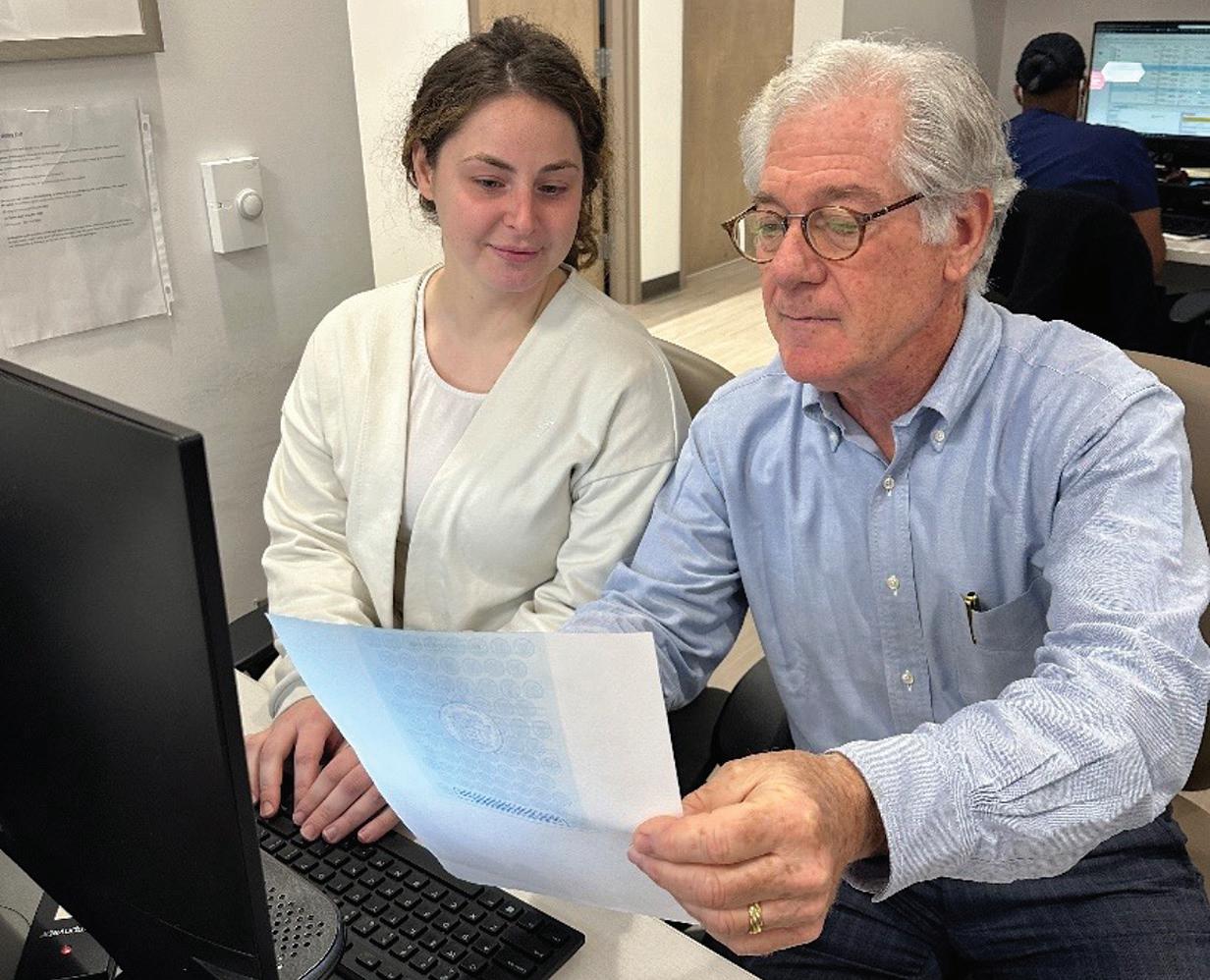
Leah loves the comments—especially those that say she takes time to explain things well.
“Patients are coming in to give a piece of themselves to me. Often it’s like a 65-yearold man coming in to talk about erectile dysfunction, and that’s embarrassing to him. I’m a 28-year-old female, and that really doesn’t mesh in their heads,” Leah said. “So, I often give them a vulnerable piece about myself to allow them to open up to me.”
Leah describes herself as a professional patient and PA.
Before starting with Jefferson, Leah was finishing her PA program with the intention of going into emergency medicine or dermatology. But months before graduating, at age 24, she found out she had breast cancer.
“I never thought that I would be the person to tell people that they had cancer,” Leah said. “The ‘c-word’ makes people’s faces go blank and their minds go numb. I hate telling people they have cancer, but I love being the person to hold their hands through it. It’s very meaningful to me.”
Today, Leah works 60 or 70 sometimes stressful hours a week. But when it comes down to it, she said she got into medicine to help people and that’s exactly what her job at Jefferson allows her to do.
“Every piece in my house has a story behind it. I just got an 18th century French clock from an estate sale that’s just beautiful,” she said.
Leah describes herself as “kind of a nerd,” who does a lot of reading about urology. She watches videos of surgeries before she falls asleep, so she can better talk with patients about operations they may be having.
Oh, and she bakes. Baking is her thing and the Department benefits when she brings in her signature cinnamon rolls (from scratch) and killer apple cider doughnuts.
Leah likes being involved with the expansion of the Department of Urology, including the expanding men’s health program and prostate specific antigen (PSA) efforts to help men get diagnosed in earlier, more treatable stages.
Leah’s dedication to the Department is impressive, the coworker writes.
“She is constantly looking for ways to improve our processes…,” according to the coworker’s letter. “Leadership is often about how you treat those around you, and Leah exemplifies this every day. She treats every member of our team—whether they are fellow providers, medical assistants or front-end staff—with the highest level of respect and kindness.”
Leah’s dedication to the Department is impressive.
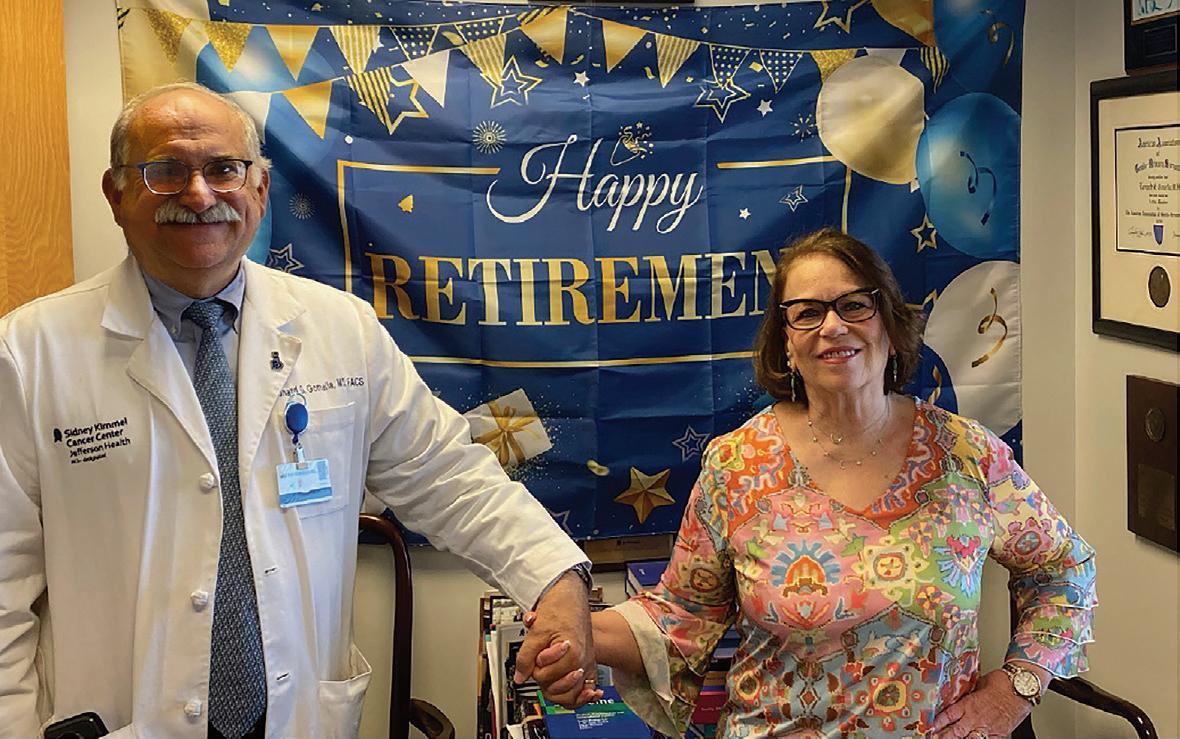
Pictured above: Dr .Gomella congratulates Barbara Devine on her years of service to the Department of Urology.
THINGS WERE DIFFERENT BACK THEN
Barbara, who retired in 2024, was 25 years old in 1983 when she interviewed with the late Dr. Demetrius H. Bagley, Jr. Dr. Bagley had recently joined Jefferson’s Department of Urology and needed a personal secretary.
“Dr. Bagley was very soft spoken and friendly,” Barbara said. “I don’t recall what we talked about, but he said, ‘When can you start?’”
The late Dr. Grant Mulholland was Department Chair at the time. Barbara describes the department in 1983 as small with four urologists and hardly any staff in the college or clinical office. As secretary, Barbara typed Dr. Bagley’s journal manuscripts and book chapters on a typewriter (word processors and computers came later).
Dr. Irvin Hirsch joined the department in 1985 and Dr. Leonard Gomella, who became Department Chair in 2002, joined in 1988. Drs. Patrick Shenot and Scott Hubosky were chief residents when Barbara was early in her career at Jefferson.
For Barbara, a bad turn of events led to a good career move.
In 2019, Barbara was diagnosed with
Life’s milestones happened during the four decades that Barbara Devine worked in the Department of Urology. Barbara got married, gave birth to her daughter, became a grandmother, and survived lymphoma. All the while, the Department of Urology has been like family, she said.
lymphoma and was out of work for a year. Jefferson said she’d have a job when she returned but it wouldn’t be in her previous role as the front desk administrative assistant. She was known for being conscientious, having good organizational skills and keeping calendars up to date.
In 2020, Dr. Gomella asked if Barbara would return to work for him.
“That was lucky for me,” Barbara said.
Barbara said she could have transferred to another department for more money, but her ties and family were in Urology. Dr. Bagley, for example, was at Barbara’s wedding and her daughter’s christening.
At 65, Barbara planned to retire months later than she did because of another unforeseen life happening. While walking, she was hit by a pickup truck and badly injured.
“I had a brain injury, broken ribs, fractured pelvis, lumbar spine pain and that was the middle of March,” she said. “I’m walking now without a cane, but that took a mental and physical toll.”

A Department of Urology gathering in 1984 when Barbara Devine joined the department. In addition to Barbara, Drs. Demetrius Bagley, Frank D’Elia, and several members of the nursing staff including Micki Baltish.
A survivor, Barbara plans to get back on track with the traveling that she and her husband like to do, including plans to go to the Florida Keys. The couple takes daily walks and helps to babysit their granddaughter, who recently started preschool.
As for words of wisdom, Barbara says simply try to be nice to everyone. That includes having good customer service.

Members of the Department of Urology, including Barbara’s husband, Tom, joined in the celebration of Barbara Devine’s retirement from the Department after 40 years of service.
If you ask the Department of Urology’s Practice Manager
Janelle Browning what she does. Her answer is “everything.”
Janelle is responsible for staffing, department orders and laying out the doctors’ templates for scheduling. She responds to emails and calls. And when she needs to “fill in,” she’ll schedule surgeries, do authorizations, scan radiology studies...the list goes on.
Janelle began in the Department 17 years ago with jobs that prepared her for her role today. She started at the front desk, checking patients in and out. Janelle worked her way up the administrative ladder, obtaining authorizations for radiology studies, then working as procedural scheduler.

Janelle said she would position herself for the next role by helping where needed.
“I somehow managed to try to tap into other office areas, to see where I could help,” she said. “At the front desk especially, I would always try to keep up on basic things — the letters, letterhead, supplies, just various things to keep the office going.”
Janelle’s helpful nature resulted in a promotion to office supervisor, soon after being promoted to procedure scheduler. During the pandemic, Janelle was promoted to Practice Manager, a position she has had for about four years.
Janelle said looking at what needs to be done and doing it has been a secret to her success and helped her transition into management.
“I try to think about not only what has to happen that day but what needs to take place thereafter,” she said.
Janelle said doing her job is a joy because she has a genuine love for the department, itself. “I’ve worked with Dr. Gomella for just as long as I’ve been here, so you grow to have a certain respect and dedication for what you do and the people you work with,” she said.
The other thing that drives Janelle to come to work each day is her ability to impact patient
care. “I feel like if there is anything that I or the staff can do to make the patients a little bit better when they walk out, I feel like we’ve done our jobs,” she said.
THERE’S SOMETHING YOU MIGHT NOT KNOW ABOUT JANELLE… Janelle has a strong history in the arts. In fact, the Moore College of Arts and Design had awarded Janelle two scholarships.
While she admits these interests have been on the back burner, Janelle has experience as an actor and singer, and she enjoys writing poetry.
“Music, to me, is therapy,” she said. “Artsyfartsy is really me at heart.”
Welcome Kathleen M. Quinn, RN, BSN to the Department of Urology. Kathleen is our new Ambulatory Nurse Supervisor in our new Honickman Center Office. Kathleen was born and raised in Philadelphia and has been a RN at Jefferson for almost 22 years. For the last 8 yrs she has been the Administrative Charge Nurse for her hospital unit that included Med/Surg/Telemetry. According to Kathleen “I'm a huge Philly sports team and country music fan and love going to games and concerts. I'm a big traveler and I'm pretty much up for going anywhere. Basically, my bags are always packed for my next trip.”
This past year we also welcomed Jordan DeHoratius to the Department of Urology. Jordan is our new Clinical Research Coordinator working closely with Alex Kolesnikov. Jordan completed her undergraduate degree at the University of Pittsburgh, majoring in History and Political Science along and a 2-year Postbaccalaureate Pre-Professional Program at Jefferson. Jordan is very busy also completing her Master’s in Neuroscience at Thomas Jefferson University. Before joining Urology, I worked as a Clinical Research Coordinator for the Department of Oral and Maxillofacial Surgery and Dentistry. According to Jordan: “One of my favorite pastimes is reading, and I will read any genre. Currently, I am in two book clubs, so if you have any book recommendations, let me know! I also love attending Phillies games and trying new restaurants in the city.”
Other new Center City nursing staff include Greta Sopaj, MA and Nicole Konzerowsky, RN, BSN.
You grow to have a certain respect and dedication for what you do and the people you work with.

May 2-May 6
Jefferson’s Department of Urology was well represented at the annual AUA Meeting. Our faculty, residents and students participated in a variety of scientific presentations and educational programs.
L. Gomella: The Evolving Landscape of Advanced Prostate Cancer Treatment: A Guidelines and Case-Based Discussion Presented by the AUA in Partnership with the Society of Urologic Oncology (SUO)
A. Shakir: MP06-11: Patients with hypertrophic scarring disorders are at elevated risk of urethral stricture, bladder neck contracture and urethroplasty failure (Prebay, Z.J.; Wahlstedt, J.; Wahlstedt, E.; Chung, P.H.; Shah, M.S.)
J.Y. Leong: MP10-19: Management of Chronic Pain and Overall Mortality in Metastatic Renal Cell Carcinoma: A Multicenter Investigation from a Large Global Health Research Network (TriNetX) (Im, B.H.; Hochberg, A.; Lallas, C.D.; Shah, M.S.; Gomella, P.T.; Mark, J.R.; Izes, J.K.; Zarrabi, K.; Metwalli, A.R.)
C. Lallas: 011IC – Chemotherapy and Immunotherapy for Urologists and Advanced Practice Providers
A. Gosh: PD24-10: Evaluating Genito-Urinary Syndrome of Menopause Treatment Pathways Utilizing the TriNetX Global Database (D’Amico, M.; Shah, S.; Shah, Y.B.; Murphy, A.M.; Smith, W.; Shah, M.S.; Lallas, C.D.)
Y.B. Shah: PD31-04: Rates of Penile Fracture and Peyronie’s Disease in Patients with Connective Tissue Disorders (Simhal, R.K.; Mandel, A.L.; Sholklapper, T.N.; Wang, K.R.; Sun, K.; Poluch, M.; Chung, P.H.)
C. Lallas: MP39: Education Research II
Y. Shah: MP55-02: Determining Radiologic Response to Neoadjuvant Chemotherapy for Wilms Tumor Prior to Partial Nephrectomy (Mittal, S.; Kakde, S.; Hamdan, D.; Back, S.; Long, C.J.; Kolon, T.F.)
S. Hubosky: 062IC – Maximizing New Technological Advances in Ureteroscopy and Associated Instrumentation
Y. Shah MP70-03: Racial Disparities in the Treatment of Depression in Patients with Prostate Cancer on Androgen Deprivation Therapy (Simhal, R.K.; Mandel, A.L.; Wang, K.R.; Shah, Y.B.; Shah, M.S.)
A. Hochberg: PD58-03: Undercoding of Von Hippel-Lindau in a multicenter, large-scale global health database limits informative investigations: An assessment of the TriNetX database (Ghosh, A.; Im, B.; Shah, S.; Gomella, P.; Shah, M.S.; Mark J.R.; Izes, J.; Metwalli A.R.)
A. Murphy: Complications of Urogynecologic and Reconstructive Pelvic Surgery (Sajadi, K.; Firoozi, F.; Tenggardjaja, C.)
B. Im: MP76-14: Prophylactic Dips and Irrigation Solutions Can Considerably Alter the Antimicrobial Efficacy of Inflatable Penile Prosthesis Hydrophilic Surface Coatings (Shah S.; Simhal, R.K.; Guillame S.; Evans R.; Perez, C.; Hickok, N.J.; Chung, P.H.)


Chief Resident JY Leong, MD, participating in a podium discussion at the AUA 2024 in San Antonio, Tx.

Dr. Leonard Gomella, second from right, was invited faculty for the AUA/SUO educational course at AUA 2024: ”The Evolving Landscape of Advanced Prostate Cancer Treatment: A Guidelines and Case-Based Discussion.“
From left to right:
Dr. Elisabeth Heath, Karmanos Cancer Center, Detroit, Dr. Kelvin Moses, Vanderbilt University, Dr. Joshua Lang, University of Wisconsin, Dr. Kristen Scarpato, Vanderbilt University, Dr. Michael Cookson, University of Oklahoma, Dr. David Jarrad, University of Wisconsin, Dr. Kelly Stratton, University of Oklahoma, Dr. Gomella and Dr. Steve Boorjian, Mayo Clinic, Rochester.
The AUA and Mid-Atlantic AUA are the major meetings that our Department participates in. Throughout the year, there are multiple other specialty meetings that our faculty residents and students contribute to.
Some of these include the Society of Academic Urologists (SAU), American Society of Andrology, Society of Urologic Oncology (SUO), Society for Women in Urology (SWIU), ASCO GU, Sexual Medicine Society of North America (SMSNA), Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction (SUFU), the American College of Surgeons (ACS) and others.


Our Peruvian colleagues, who attended the Annual AUA meeting, joined our Jefferson/Einstein/Canadian Journal of Urology reception. Dr. Fernando Quiroa Vera (left) from Lima, Peru, is a member of the Canadian Journal of Urology International Editorial board.
The Jefferson Urology Alumni /Einstein Urology/Canadian Journal of Urology reception was held on Sunday, May 5th, 2024, in the Marriot Rivercenter. Over 60 faculty, residents, students, alumni and friends attended the reception.


The Mid-Atlantic AUA Section meeting is another important annual meeting for our Department and was held at the Greenbrier in White Sulfur Springs, West Virginia. Over the years, our Department faculty have held important positions in the organization, including many past presidents and numerous board and committee members.
Jefferson Urology had 7 moderated posters that were discussed over the 3 days of the meeting. Drs. Costas Lallas, Paul Chung, Deborah Glassman, and resident Dr. Zachary Prebay all presented their research. Dr. Chung co-moderated the Resident’s Bowl, and Dr. Glassman was a mentor for the Society for Women in Urology (SWIU) forum. Social events included the Young Urologists Bowling event, continuing the theme of the “Resident’s bowl” and the Doomsday bunker party.

The Mid-Atlantic AUA program included social bowling events with Drs. Glassman and Lallas competing for highest score.
Inflatable Penile Prosthesis Hydrophilic Surface Coatings Rebind Antiseptic Solutions Ex Vivo
Paul Chung, MD
Antibiotic-Impregnated Penile Implant Surfaces Are Unaffected by Irrigation with 0.05% CHG and Antibiotic Solutions
Paul Chung, MD
A Contemporary Analysis of Use, Clinical Outcomes, and Costs of Roboticassisted, Laparoscopic, and Open Radical Nephrectomy Using the National Inpatient Sample
Costas Lallas, MD, FACS
The Impact of Telehealth on Treatment Decision-making in Prostate Cancer
Deborah Glassman, MD, FACS
Androgen Deprivation Therapy Does Not Increase Rates for Reintervention, Complication, or Infection in Penile Implant or Artificial Urinary Sphincter Surgery

Zachary Prebay, MD
The Relationship Between Hypertrophic Scarring, Ureteral Strictures, and Upper Tract Reconstruction Failure
Zachary Prebay, MD
A TriNetX Analysis on Testosterone Replacement and the Risk of Fractures in Men with Hypogonadism
Zachary Prebay, MD
The Jefferson India Center is based at the KLE University, Belagavi, India. KLE University, which includes the Jawaharlal Nehru Medical College. KLE has a history of more than 100 years and is ranked among the top of India's universities. Early in 2024, visitors to the Department of Urology met to discuss the successful endourology program held at KLE in Belagavi in 2023 that included Drs. Radhika Ragam and Scott Hubosky. The group also reviewed potential future urology research, teaching and clinical collaborations. In the summer of 2024, Urology hosted two medical students from KLE (see page 49).

The Department of Urology and KLE University meeting participants included: Dr. Mrityunjay C. Metgud, Professor and Unit Chief, Dept of Obstetrics and Gynecology, KLE; Dr. Manjunath Somannavar, Professor, Dept of Biochemistry, KLE; Parth Lalakia, MPH, Jefferson’s Program Director Dr. Avinash Kavi, Associate Professor, Dept of Community Medicine, KLE; Urology Chief Resident Radhika Ragam; Dr. Mat Thakur, Professor of Radiology and Urology; Dr. Richard Derman, Vice Provost for Global Affairs at Thomas Jefferson University; Dr. Shivaprasad Goudar, MD, Director of Research and Professor, KLE University; Dr. Scott Hubosky, Professor of Urology and Dr. Anmol Patted, MBBS, MPH, KLE University Alumni and Post-Doc, Office of Global Affairs, Thomas Jefferson University.


Liberty Hotels Lykia
| Turkey October 8-11, 2024
Dr. Mathew L. Thakur, Professor of Radiology, Radiation Oncology and Urology was an invited speaker at Medical Optics meeting held in Turkey in October, 2024. Dr. Thakur is also Director, Laboratories of Radiopharmaceutical Research, Molecular Imaging and Biofluid Diagnostics at Sidney Kimmel Medical College. Dr. Thakur addressed our joint Department of Urology work with him on shed cell technology based on the VPAC marker expressed on cancer cells. In addition, to our NCI grant to study shed urinary cells in prostate cancer, Jefferson holds a series of international patents on this cancer cell detection technology applicable to a variety of epithelial malignancies.
Fatuma Doka, MSN, CRNP, a nurse practitioner in the Department of Urology, recently returned from a month-long trip to her home country of Uganda, with the nonprofit she started in 2019 Tender Grassroots.
“Doka,” as she’s called by colleagues, started Tender Grassroots in 2019 to provide underserved communities throughout Uganda with resources, knowledge and skills aimed at empowering the people there to end the cycle of poverty.
Tender Grassroots representatives from the U.S. and other countries make annual treks to Uganda to volunteer in local schools, hold a health fair and more. Two physicians and their children, as well as a teacher from the UK and Doka’s daughter, a financial professional, joined her on the journey.
“The kids volunteered at the school, helping to teach the children about computers,” Doka said. “We brought some computers and had some donated to start a computer program at the local school. We also brought books and helped to teach the children how to read and write.”
Doka and her health care colleagues cared for 1,113 patients during the annual Tender Grassroots two-day health fair, which local universities support. They screened patients for nearly everything, and while the team didn’t offer mammograms, they did breast exams. They also did circumcisions in children and adults.
Doka recalls identifying a breast mass in one woman and referring her for further treatment. They cared for another patient who said she was always weak and found she had diabetes and unmanaged high blood pressure. Doka had
checked on the patient after her return to find the treatment they prescribed for the women put her on the road to recovery.
And then there was the story of a gentleman going for his master’s degree, who dropped out of school because he couldn’t see. He thought his life was over, according to Doka.
“An ophthalmologist at the health fair found this gentleman had glaucoma and cataracts, which are treatable. The ophthalmologist started him on eyedrops and is going to follow up,” she said.
Spending a month in Uganda reminded Doka of how easy it is to take things for granted here in the U.S.“I think everyone needs to see what happens in other places. The clinical skills needed there are totally different than here. Here we rely a lot on labs and imaging. There you don’t have those and have to rely on the assessment,” Doka said.
While Department of Urology residents have made sporadic and shorter trips to Uganda, Doka said she is working on a more structured program for the residents to provide care and spend time with mentors in Uganda. “We can learn from them, and they can learn from us,” she said.
In addition to her inpatient work with the Department of Urology at Jefferson, Doka participates actively in our Sidney Kimmel Comprehensive Cancer Center prostate cancer community screening and awareness programs (see page 54).

Doka can be contacted by email: Fatuma.doka@jefferson.edu


A message from Executive Director, Fatuma Doka, NP on behalf of The Tender Grassroots Team
”A Heartfelt Thank You!!
We extend our deepest gratitude to everyone who made this summer's mission possible—from our incredible volunteers to our generous supporters that includes many members of the Jefferson Community. Your commitment to our cause is what drives us forward, and the positive outcomes of this trip are a testament to the power of collective effort. As we reflect on this impactful summer, we look forward to continuing our work and exploring new opportunities to support and uplift the communities we serve. Stay tuned for more updates and ways you can get involved!“




In addition to our international students from KLE in India, who participated in formal rotations (see page 49), the Department of Urology was pleased to interact with several other international trainees over the past year.
Through the Jefferson Consortium for African Partnerships (JCAP), our department had the opportunity to host several Visiting Scholars through the JCAP. Dr. Derrick Shema Graduated from University of Rwanda in 2023 with a Bachelor of Medicine and Surgery and
Through the Jefferson Consortium for African Partnerships (JCAP), our department had the opportunity to host several Visiting Scholars.
is currently an intern in General medicine and surgery at University of Rwanda. Dr. Josiane Izere Graduated from University of Rwanda in 2023 with a Bachelor of Medicine and Surgery and is currently doing her internship in general medicine and surgery. As part of their twomonth observership at Jefferson, they had the opportunity to rotate in Urology.
During their time in our department, they met with our Chair Dr. Leonard Gomella, interacted with our attendings, residents and
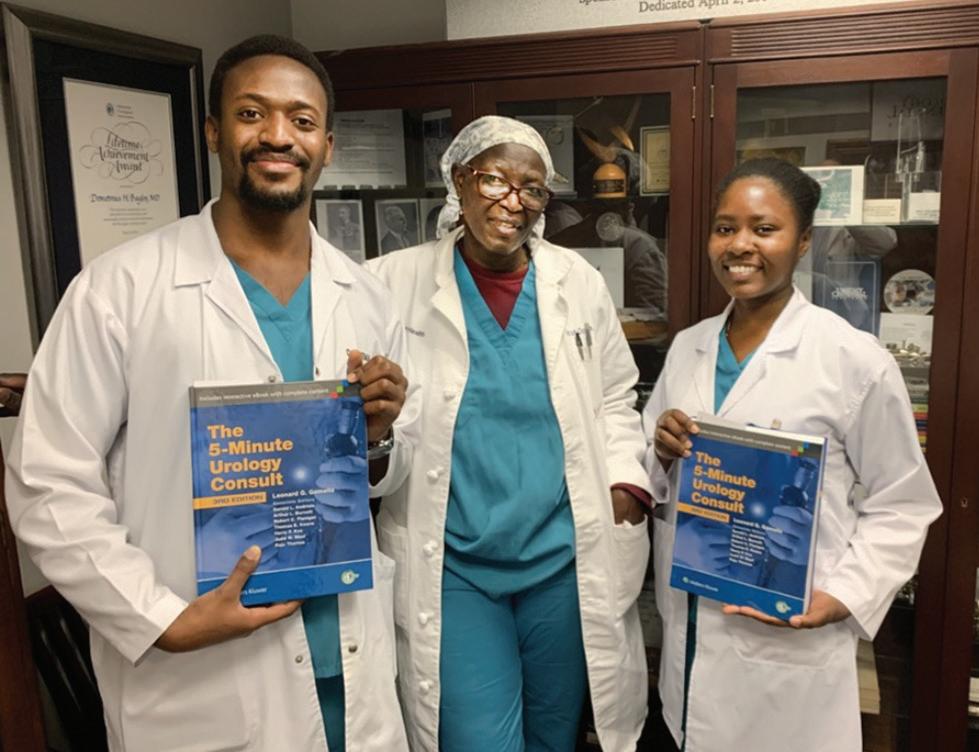
Drs. Derrick Shema and Josiane Izere, visitors from Rwanda who participated in the Jefferson Consortium for African Partnerships (JCAP), with our urology NP Fatuma Doka. They received copies of the “5-Minute Urology Consult” as part of their time in the Department of Urology.
nurse practitioners and participated in our conferences. They spent time in the operating room to observe urology surgeries, they rounded with the team on both the inpatient and consult services. Drs. Shema and Izere The Department of Urology was pleased to interact with several international trainees over the past year.

were grateful to have observed firsthand robotic and endourology cases, having only previously read about them.
In addition to Jefferson’s main Italian partners, Cattolica University and Gemelli Hospital, another partner is a prominent private university located in Milan, Humanitas University. Based on a recommendation of Dr. Ignazio Marino, Professor Emeritus of Surgery at SKMC who is now a Member of the European Parliament, we welcomed Abdallah Alshatali. Abdullah was visiting student in the summer of 2024 from Humanitas, a fourthyear student pursuing a double degree in both Medicine (MD) and Biomedical Engineering (BSE).
Humanitas University 4th year student Abdallah Alshatali (yellow lead apron) with Urology residents Drs. Carlos Perez and JY Leong and SKMC student, Anushka Gosh.
Dr. Leonard Gomella was invited to visit the Martini Clinic in Hamburg, Germany, in the spring of 2024. The Martini Clinic is among the highest volume HIFU centers in Europe. It is part of the University Medical Center Hamburg-Eppendorf (UKE).
Recent data shows the Martini Clinic had become the largest prostate cancer program in Europe with their focus strictly on prostate cancer diagnosis and treatment.
Dr. Gomella is shown here with Martini Clinic HIFU expert Dr. Yamini Nagaraj.


Each year, a select group of medical students from the Jawaharlal Nehru Medical College, part of KLE University in Belagavi, India, complete a formal program at Jefferson. Students are assigned to specialty rotations and in 2024 Aditya Raji and Sanjivini “Vinny” Patil were our primary urology students. Their specialty rotation time at Jefferson also includes exposure to public health lectures, simulation labs, health design labs, JeffSTAT ambulance helicopters, and much more including cultural experience trips to New York, Washington and the Jersey shore.
KLE students rotating on Urology, Aditya Raji and Sanjivini “Vinny” Patil, with Chief Urology Resident Dr. JY Leong in the OR during a robotic radical prostatectomy.
Olivier Traxer, MD, MS
Professor of Urology and Chairman
Urology Department
Sorbonne University Tenon Hospital (Paris, France)
Dr. Olivier Traxer is Professor of Urology and Chairman of Urology at the Sorbonne University Tenon hospital (Paris-France). He is the Director of the GRC#20 (Clinical Research Group #20). He did a research-fellowship at Southwestern Medical School, University of Texas-DallasUSA (Drs. Charles Y.C Pak & Margaret Pearle) to subspecialize in Endourology and kidney stone management.
As an endo-urologist, his main goal is to improve the knowledge on urinary stone disease and endourology. Dr. Traxer has published more than 475 peerreviewed papers.
Dr. Traxer is a board member of the Endourological Society, the French Association of Urology (AFU) and European Association of Urology (EAU) board member of the European Urolithiasis Society (EULIS) and EAU Section
of Uro-Technology (ESUT). He is an active member of the American Association of Genito-Urinary Surgeons and Association of Academic European Urologists (AAGUS & AAEU). He was also the treasurer of Société International d’Urologie. In 2010 at the Chicago-World Congress of Endourology (WCE) he received the Arthur Smith Award, and the Ralph Clayman Mentor Award in 2020.
In 2022, he received the St. Paul Medal at BAUS annual meeting. He was also the president of the World Congress of EndoUrology in Paris 2018 (WCE2018) and became a member of the French Academy of Surgery in 2022. In 2023, he became Honorary Member of the UAA in Dubai.
Dr. Traxer has also compiled magnificent photos of the most beautiful stones from his personal collection and amazing comments

from the 60 most renowned key opinion leaders in the world in endourology and published in a book by Coloplast. Our residents were each given individual copies of the book, Calculi, as a courtesy of Dr. Traxer and supported by Coloplast.
In addition to patient presentations and discussions with

Drs. Scott Hubosky and Leonard Gomella presenting our 2024 DM Davis Visiting Professor, Dr. Olivier Traxer, with a commemorative plaque.
our residents, Dr. Traxer presented two talks: “LASER and Safety!” and “Metabolic Evaluation of Stone Patient: What a Urologist Must Know.”
The DM Davis visiting professorship is held along with our year-end Department of Urology Graduation and Awards Ceremony Graduation (see page 68).
As an endo-urologist, Dr. Olivier Traxer’s main goal is to improve knowledge of urinary stone disease and endourology.




Dr. David Melvin Davis was Chairman of the Department of Urology at Jefferson Medical College from 1935 to 1951. Under Dr. Davis’s leadership, advanced training in Urology was established. The first residencies at Jefferson started in 1937 in Obstetrics, and the Department of Urology established one in 1939. World War II caused a delay in increasing the number of residents, but a second residency position was created in 1946 and a third in 1947. In 1948, an arrangement with Professor John H. Gibbon, Jr. provided a year of training in General Surgery before beginning three years in the Urologic Residency.
Dr. Davis greatly improved the standard of care in the Urology Ward and Curtis Clinic. In addition to more than 130 journal articles, after academic retirement Dr. Davis wrote a textbook Mechanisms of Urologic Disease (1953). He designed a cystoscopic-roentgenographicfluoroscopic table constructed in Philadelphia by the Franklin X-ray Corporation. His interests were in hypospadias, hydronephrosis, and early diagnosis and radical operations for carcinoma of the prostate and the famous "Davis Intubated Ureterotomy."
In 1946, a Professorship in Urology was established under the bequest of Henry Reed Hatfield as a memorial to his father, Nathan Lewis Hatfield. Dr. Davis was its first recipient and he was also the first recipient of the AUA Hugh Hampton Young Award in 1969.
According to Dr. Traxer, The book, Calculi, contains magnificent photos of the most beautiful stones from my personal collection and amazing comments from the 60 most renowned clinicians in the world specializing in Endourology and Coloplast.”

The P. Kenneth Brownstein Lectureship is held annually in honor of Dr. Ken Brownstein, who is Clinical Assistant Professor of Urology and The Harold A. Honickman Physician Director of Jefferson Signature Services. He is a graduate of Hahnemann University School of Medicine (now Drexel University College of Medicine). Dr. Brownstein began his Urology residency in 1972 and has been at Jefferson ever since. The first Brownstein Lectureship was held in 2012 in recognition of his long-time service to Jefferson.
November 13-14, 2024
Jay D. Raman, MD, FACS
Professor and Chair of the Department of Urology
Penn State Health, Milton S. Hershey Medical Center
Jay D. Raman, MD, FACS is Professor and Chair of the Department of Urology at Penn State Health, Milton S. Hershey Medical Center. He received his undergraduate degree from the Massachusetts Institute of Technology (MIT) and graduated AOA from Cornell University Medical College. Dr. Raman completed his Urology Residency at New York Presbyterian Hospital - Cornell Medical Center followed by a Fellowship in Laparoscopic and Robotic Surgery at the University of Texas Southwestern Medical Center in Dallas.
Dr. Raman's clinical practice focuses on robotic-assisted surgery for upper and lower tract urologic cancers, having completed over 2,500 cases. His clinical research centers on quality of care for prostate cancer patients, novel treatments for upper-tract urothelial carcinoma, biomarkers for urinary tract cancers, prostate biopsy infections, as well as complications of urologic surgery.
To date, he has co-authored more than 350 manuscripts, book chapters, and editorials and serves on the editorial board for three journals and as a reviewer for 12 journals.
Dr. Raman is currently Chair of the American Urologic Association (AUA) Office of Education and Past-President of the Mid-Atlantic AUA section. He currently serves as on the Urology Advisory Council for the American College of Surgeons.
The Brownstein Lectureship includes an evening program and a formal grand rounds presentation. On Wednesday evening, Dr. Raman presented a “mini lecture” on “Emotional Intelligence what are not taught during residency” along with a Journal Club. On Thursday, November 14, his lecture was titled: “Intravesical Recurrence Following Surgery for UTUC-Incidence, Predictors & Strategies for Prevention.”

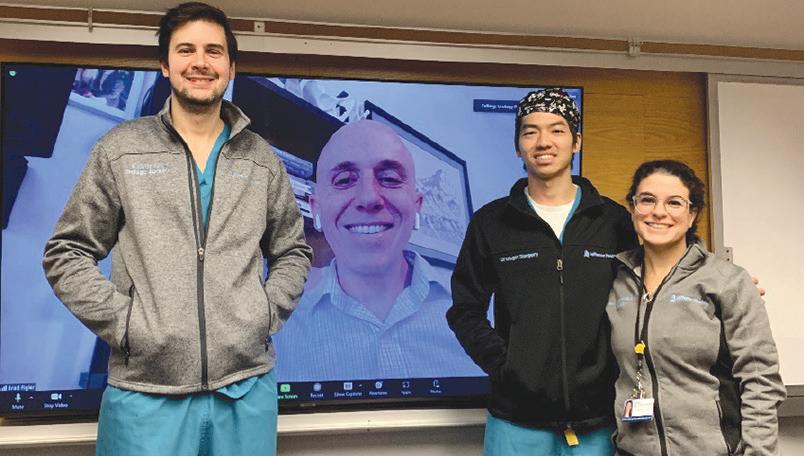

1 “TRANSGENDER HEALTH AND BOTTOM SURGERY”
DR. BRAD FIGLER, UNC CHAPEL
HILL Dr. Figler received his medical degree from Case Western Reserve University School of Medicine, completed residency training in Urology at Emory University, and completed fellowship in GenitoUrinary Trauma and Reconstructive Surgery at the University of Washington. In 2013, Dr. Figler joined the faculty at Thomas Jefferson as Assistant Professor in the Department of Urology.
In 2016, Dr. Figler joined the faculty at UNC-Chapel Hill, where he currently serves as Associate Professor of Urology and Plastic Surgery, Director of the UNC Transgender Health Program, and Director of the Fellowship in Genito-Urinary Reconstruction and Gender Affirming Surgery.
2 “MRI FOR RENAL MASSES AND PREDICTIVE HISTOLOGY”
DR. JEFFERY CADEDDU, UT SOUTHWEST Dr. Jeffrey Cadeddu received his Bachelor of Science in Biomedical Engineering from Johns Hopkins University, and in 1993 received his Doctor of Medicine from Johns Hopkins University School of Medicine, where he also completed his urology and surgery residencies. He then
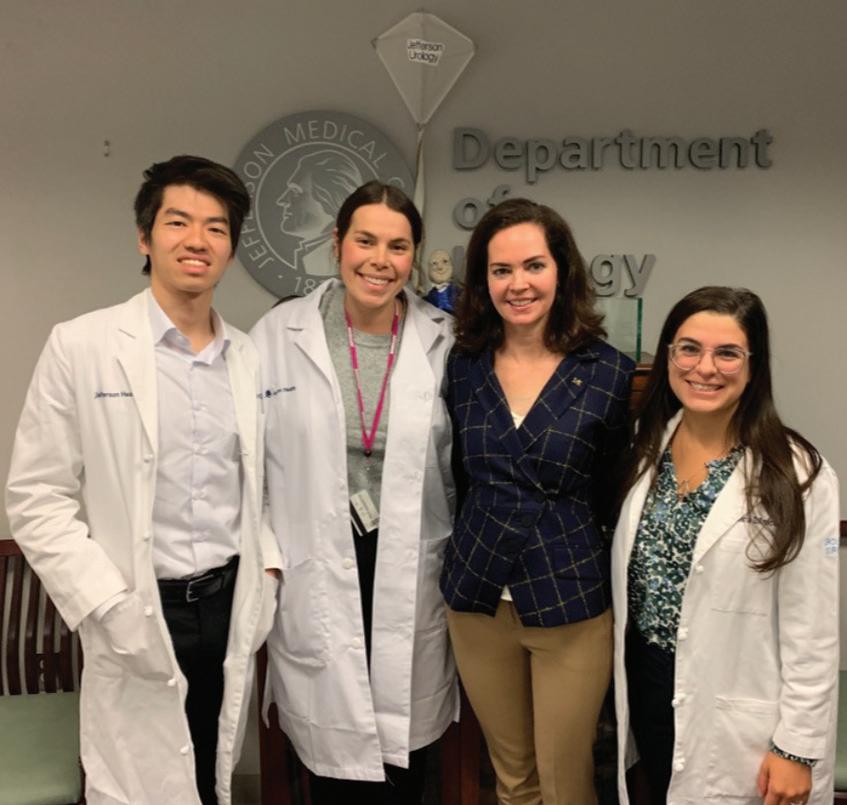
joined The University of Texas Southwestern Medical Center in 1999, and currently holds the dual appointments of Professor of Urology and Professor of Radiology at that institution. In addition, he holds the Ralph C. Smith, MD, Distinguished Chair in Minimally Invasive Urologic Surgery and serves as the Director of the Clinical Center for Minimally Invasive Urologic Cancer Treatment.
His publications include more than 240 peer-reviewed articles; more than 75 invited articles and book chapters; numerous editorial comments, book reviews and original videos. He is the recipient of the American Urological Association’s 2007 Gold Cystoscope Award. Dr. Jeffery Cadeddu was elected for membership in the American Association of GenitoUrinary Surgeons (AAGUS), has served as co-president of the Engineering and Urology Society, served as member for the AUA small renal mass and localized prostate cancer guidelines.
3 “DEI
COMMITMENT
COMMUNITY” DR. KATE H. KRAFT, UNIVERSITY OF MICHIGAN After her participation in the L. William Ferris, MD, Memorial Lectureship in Pediatric Urology at Nemours Children’s

“PSMA
DR. STEPHEN ROWE, UNC-CHAPEL HILL
Health (see page 19), Dr. Kraft joined us for Jefferson Urology grand rounds on October 10, 2024. Kate H. Kraft, MD, MHPE, FACS, FAAP is Professor in the Department of Urology and the Mark C. McQuiggan, MD and Carolyn A. McQuiggan Research Professor at the University of Michigan, Ann Arbor, Michigan. She received her undergraduate degree from Harvard University and medical degree from Columbia University College of Physicians & Surgeons. She completed her urology residency at Emory University and fellowship in pediatric urology at the Children’s Hospital of Philadelphia.Dr. Kraft is chief of the Division of Pediatric Urology at the University of Michigan C. S. Mott Children’s Hospital. Her clinical interests include minimally invasive urologic surgery and endourology in children, pediatric andrology, and disorders of sex development. Her primary research interests include pediatric kidney stone disease, pediatric uroradiology, cryptorchidism, and surgical education. She has published numerous peer reviewed journal articles in these areas and has earned the Clinical Research Prize Award from the American Academy of Pediatrics Section on Urology for her work in undescended testis histology.
Steven Rowe, MD, PhD, is Professor and Chief of the Molecular Imaging and Therapeutics Division in the UNC School of Medicine Department of Radiology. Dr. Rowe received his medical degree and PhD in chemistry from the University of Michigan. He completed residencies in radiology and nuclear medicine at Johns Hopkins University School of Medicine. Most recently, he was an Associate Professor of Radiology and Radiological Science at Johns Hopkins University in Baltimore, Maryland.
He clinically focuses on nuclear medicine, and his research work has been centered around applications of novel molecular imaging agents for positron emission tomography (PET) and single-photon emission computed tomography (SPECT). He is particularly interested in the use of prostate-specific membrane antigen (PSMA)-targeted PET agents in prostate cancer and renal cell carcinoma, as well as the clinical utilization of 99mTcsestamibi SPECT for noninvasive characterization of renal masses. He and his colleagues recently developed and validated a structured reporting system for delineating and codifying findings on PSMA PET known as PSMA Reporting and Data System (PSMA-RADS).
Dr. Rowe’s October 17th, 2024 CME Grand Rounds presentation was supported by a unrestricted grant from Lantheus.

Some of the members of the SKCCC and Department of Urology
at the ribbon cutting and dedication of the new Dietz and Watson/SKCCC screening
A collaboration between the Department of Urology, the Sidney Kimmel Comprehensive Cancer Center Mobile Cancer Screening Unit, and the Prostate Conditions Education Council (PCEC) provides free prostate cancer screening in community settings across the Greater Philadelphia region. Our program also receives funding from Janssen. The team offers educational information about prostate cancer and shared decisionmaking for prostate cancer screening, in line with current screening guidelines. PSA blood draws are provided by a mobile phlebotomist who joins the on-site team at events. Men complete brief questionnaires about their personal and health history, providing additional insight into screening impact. Since
launching the collaboration two years ago, nearly 1000 men have been provided free prostate cancer screening. The majority of men (>80%) are African American, and roughly 15% of those screened each year have an abnormal PSA result. To date, we know of three men who have had prostate cancer detected because of this effort.
The Department of Urology would like to thank our Nurse Practitioners Fatuma Doka and Suzanne Barron, along with our protocol coordinators Alex Kolesnikov, and Jordan DeHoratius for their continued commitment to the community screening program.
Our screenings are IRB compliant and contribute to local and national data assessing the impact of these screening
efforts. Amy E. Leader, DrPH, MPH, Professor, Medical Oncology and the College of Population Health, is the Associate Director for Community Outreach & Engagement in the SKCCC and leads our overall community cancer screening efforts.
Our mobile screening vans have been supported by our friends at Dietz and Watson. On December 3, 2024, the second SKCCC and Dietz & Watson Mobile Cancer Screening Unit was dedicated. The original larger van features a mobile mammography unit, and our new smaller van allows more convenient outreach vehicle for our prostate cancer screening and other awareness programs.

To learn more about all of our SKCC community cancer screening events, including prostate cancer, visit www.jeffersonhealth.org/clinical-specialties/cancer/ community-outreach-engagement/mobile-cancerscreening.

SKCCC members Joe Meehan, Cynthia Pegan, and Kristine Pham and Alex Kolesnikov, from the Department of Urology, are some of the screening team members who provide educational information on prostate cancer that is language appropriate for the site along with the opportunity to have a free PSA test. This event was September 18, 2024 at the Community College of Philadelphia.
Prostate and Ovarian Cancer share the month of September to increase public awareness of the diagnosis and treatment of these fairly common cancers.


Alex Kolesnikov, Clinical Research Project Manager in the Department of Urology, was interviewed by ABC News at the Community College of Philadelphia screening event on September 18, 2024.

Prostate cancer screening and free PSA testing at the Enon Tabernacle Church on April 20, 2024. Tanya JohnsonColeman from the SKCCC is obtaining the PSA blood sample as part of the program.

COMMUNITY SCREENINGS IN 2024 TOOK PLACE AT THE FOLLOWING SITES:
George Washington Carver Center, Norristown PA
Enon Tabernacle Baptist Church, Philadelphia, PA
ChenMed/Providence Life Assurance, Philadelphia, PA
Camden Fire Department, Camden NJ
Mi Salud Wellness Center, Philadelphia, PA
Walk to Save Black Men’s Lives, Phila PA
Salem Baptist Church, Philadelphia, PA
Fred Beans Car Dealership, Doylestown PA
Phila Police Dept 25th District Block Party, Philadelphia, PA
Bucks County Emergency Homeless Shelter, Levittown PA
Septa Employee Headquarters, Phila PA
Fujian Association of Chinatown, Philadelphia, PA
Morivivi/Taller Puertorriqueno, Phila PA
Grow-A-Pair Foundation, Doylestown PA
Jefferson Health Men’s Breakfast, Philadelphia, PA
Community College of Phila,

Sharon Baptist Church, Philadelphia, PA
Department of Urology and SKCCC BCAN Walk team members who were recognized as the top team for the 2024 event. Andrea MaddoxSmith, CEO of the Bladder cancer Advocacy Network is on the right and congratulated our team members.
The SKCCC BCAN Team was the tops in the 2024 Bladder Cancer Walk. The Bladder Cancer Advocacy Network (BCAN) is a community of patients, caregivers, survivors, advocates, and medical and research professionals united in support of people impacted by bladder cancer. Our thanks to Crystal Sypherd, GU Multidisciplinary Clinic
(MDC) care coordinator, who led our cancer center team and our current GUMDC physicians, Drs. Mihir Shah and Adam Metwalli in particular, and their families who supported the event. Our team was congratulated by Andrea Maddox-Smith, CEO of BCAN.

The Department of Urology maintains an active clinical trial division. In addition to our department clinical trials program, we are involved in collaborating and supporting Sidney Kimmel Comprehensive Cancer Center (SKCCC) clinical trial development and recruitment. The department is also involved in the SKCCC Biome program, a program designed to support preliminary innovative cancer trials (see page 58).
Our clinical trial coordinators can provide additional information about these and other clinical trial opportunities. Contact Alex Kolesnikov <oleksandr.kolesnikov@ jefferson.edu> or Jordan DeHoratius <jordan. dehoratius@jefferson.edu>, our Department of Urology clinical trials coordinators.
The department has a portfolio of trials in follow up, actively recruiting trials and pending trials with only the open and pending trials listed here.

For a complete listing of additional SKCCC trials visit: www.jeffersonhealth.org/ clinical-specialties/cancer/ clinical-trials.



DEPARTMENT OF UROLOGY CLINICAL TRIALS PENDING ACTIVATION DECEMBER 2024
PIVOT-006
Indication: Intermediate risk - Non muscle invasive bladder cancer (NMIBC) Agent: novel adenoviral vector
SeaGen/Pfizer Bladder
Indication: BCG- Unresponsive High Grade Non muscle invasive bladder cancer (NMIBC)
Agent: intravesical enfortumab vedotin (EV), an antibody-drug conjugate (ADC)
UTOPIA
Indication: Low grade intermediate risk Non muscle invasive bladder cancer NMIBC
Agent: investigational mitomycin-based formulation
QUILT-2.005
Indication: BCG- Naive High Grade Non muscle invasive bladder cancer (NMIBC)
Agents: FDA-approved agent Anktiva combined with BCG
EG110A
Indication: Neurogenic Detrusor Overactivity in Spinal cord injured patients
Agent: non-replicating HSV-1 vector designed to selectively silence the signals of key bladder sensory neurons responsible for the bladder muscle overactivity
PRISM-II
Indication: PSA Reflex Test
Agent: diagnostic test for prostate cancer detection using semen analysis
UROTHELIAL CANCER VPAC
Indication: Upper tract and bladder urothelial cancer detection
Agent: Diagnostic VPAC Assay for cancer detection
PCa Vision Trial Indication: Biopsy for PCa
Agent: Ultrasound-based computer-aided diagnosis for prostate cancer
The Philadelphia Prostate Cancer Working group (PPCWG) is sponsored by the Sidney Kimmel Comprehensive Cancer Center (SKCCC) and is also supported by the Philadelphia Prostate cancer BIOME project. The Working Group Lecture series is held on the third Wednesday of the month in BLSB 602 at 4-5 PM with 45 minutes of the presentation and 15 minutes dedicated to questions and comments. The goal of the presentation is to facilitate development of collaborative innovative research initiatives, clinical trials, multi-PI and PO1 grant submissions and educate the community on the field of prostate cancer and beyond. The audience is comprised of basic scientists, population health scientists, clinical faculty, staff, and trainees associated with the Sidney Kimmel Comprehensive Cancer Center Consortium of Thomas Jefferson University and Drexel University. In addition, there is representation from a broad spectrum of specialties including Pathology, Medical,

Radiation, and Urologic Oncology. This series enables the group to attract nationally and internationally recognized speakers and allows us to continue our high standard of prostate cancer education and research.
One of our recent speakers was Dr. Natasha Kyprianou, a Professor in the Departments of Urology and Oncological Sciences at the Icahn School of Medicine at Mount Sinai and a member of the NCI-designated Tisch Cancer Institute in New York. Dr. Kyprianou is a translational researcher in urologic oncology with expertise in the pathobiology of prostate, bladder and kidney cancer and with a specific focus on dissecting mechanisms of therapeutic resistance in advanced lethal disease. Pioneering studies by Dr. Kyprianou’s team first established the novel effect of microtubuletargeting chemotherapy on the localization of the androgen receptor (AR) and activity in prostate cancer enabling a novel insight into therapeutic cross-resistance.
The PPCWG is co-led by Marja T Nevalainen, MD, PhD, Professor of Pharmacology, Physiology and Cancer Biology and Urology who is also Associate Director of Translational Research for the SKCC and Kayvan Zarrabi, MD Assistant Professor in the Department of Medical Oncology, SKCCC.

Dr. Natasha Kyprianou, Professor in the Departments of Urology and Oncological Sciences at the Icahn School of Medicine in New York, was a recent speaker at the Philadelphia Prostate Cancer Working group.
If you are interested in being on the PPCWG mailing list or would like additional information, please contact Jessica Tustin (Jessica.Tustin@jefferson.edu) or Collen Katen (Colleen.katen@jefferson.edu).
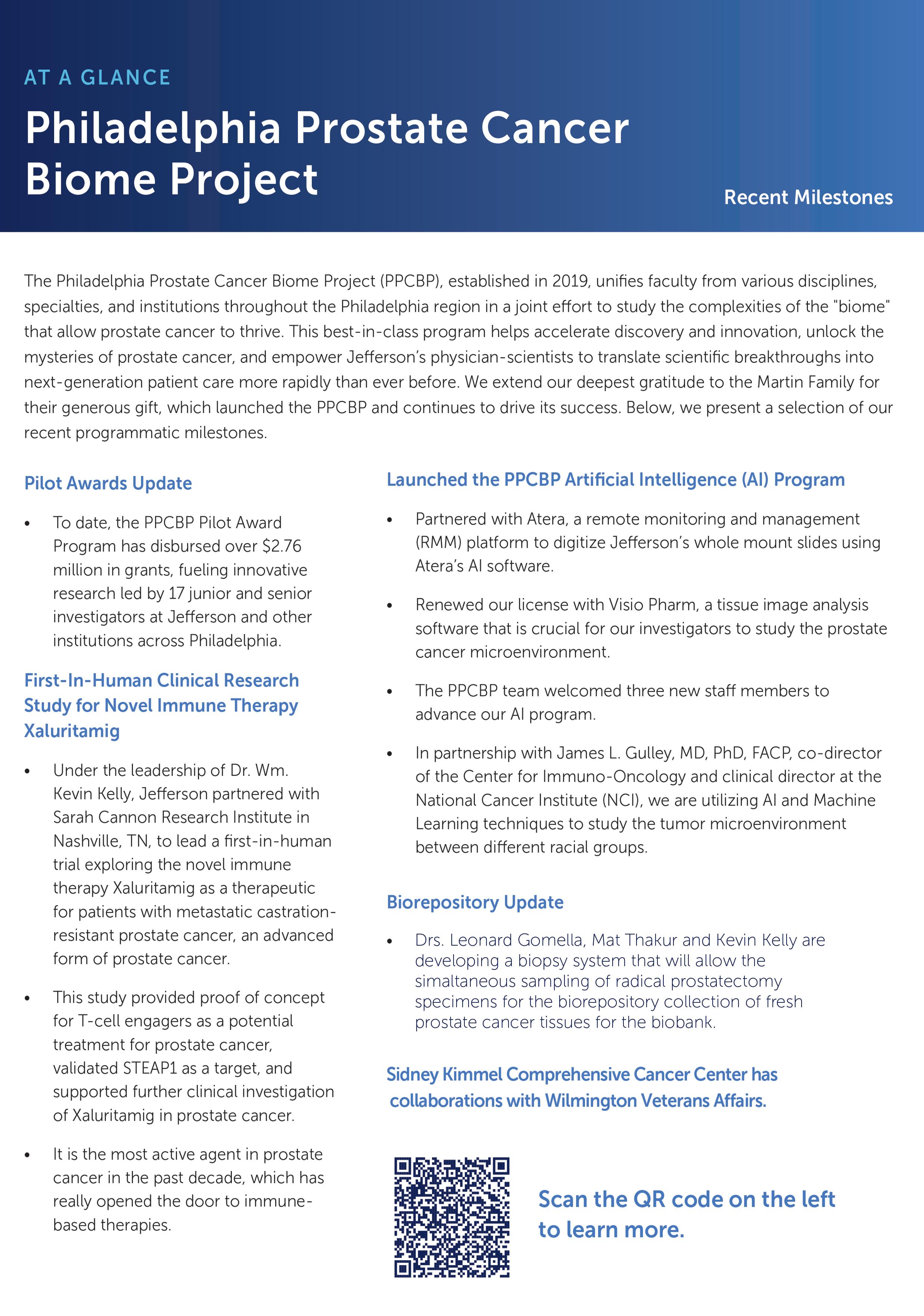
CANCER CENTER AND COMMUNITY ENGAGEMENT ENHANCE RESEARCH OPPORTUNITIES
The summer 2024 publication “Research at Thomas Jefferson University” highlighted how our Jefferson SKCCC cancer researchers and community members have come together to address racial disparities in prostate cancer at the molecular and patient level. “The reasons why African American men are more likely to develop and die from prostate cancer compared to white men continue to baffle us,” says researcher and clinician Leonard Gomella, MD, the Bernard W. Godwin, Jr. Professor of Prostate Cancer, who chairs the department of urology and is a senior director for clinical affairs at the Cancer Center. “While we’ve come a long way, we haven’t been able to definitively identify the root of this disparity.”
Moriah Cunningham is a PhD Candidate in the Sidney Kimmel Comprehensive Cancer Center. She has previously worked in a Department of Urology Research Lab and now is a PhD
Candidate studying prostate cancer, PARP and p53 under the mentorship of Dr. Steven McMahon, Chair, Department of Biochemistry & Molecular Biology. Throughout her training, one issue Moriah has recognized is the pronounced scarcity of data on black prostate cancer patients in clinical and basic science research. Moriah has been proactive in combining community engagement with basic science research.
The Cancer Center will continue to build on outreach to at-risk communities, providing evidence-based solutions for community engagement in research. You can also read about our SKCCC community outreach prostate cancer screening programs on page 54. “Moriah stepping out of the laboratory and into the community sends a powerful message,” says Dr. Gomella. This research magazine provides an in-depth story about Moriah and how she is making a difference in our world of cancer research.
The reasons why African Americans develop and die from prostate cancer compared to white men continue to baffle us.



Download the magazine by visiting: https://research. jefferson.edu/magazine.html

Nemours Children’s Hospital in Orlando has installed this plaque in honor of Dr. Erhard’s career.
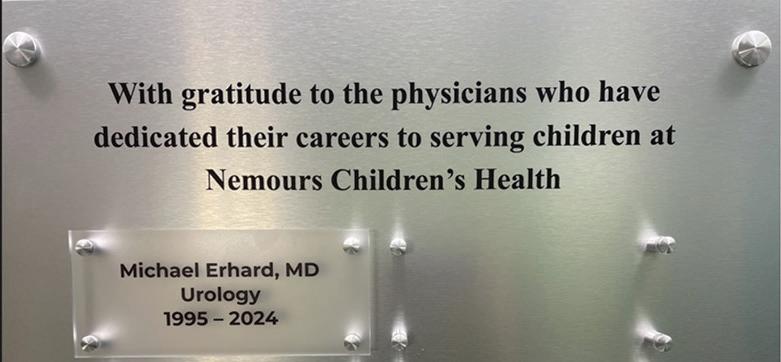

Since graduating from the Jefferson Urology Residency Program in 2016, I have had the privilege of continuing my career in urology at Weill Cornell Medicine. After completing my training, I joined the faculty at Weill Cornell’s Urology Department and currently practice at New York-Presbyterian/ Queens, where I hold the position of Assistant Professor of Urology. In addition, I am Director of Endourology & Stone Disease and Site Director, and Urology Residency Program site director.
Reflecting on my time at Jefferson, I am deeply grateful for the training I received under the leadership of Chairman Dr. Leonard Gomella, as well as the guidance of esteemed endourologists, the late Dr. Demetrius Bagley and the current Bagley Professor, Dr. Scott Hubosky.
Now at Weill Cornell, I have focused my clinical efforts on the complex management of kidney stone disease, an area in which I have built a robust and growing practice. I am fortunate to work alongside esteemed colleagues, including Dr. Larissa Rodriguez, Chair of Urology at Weill Cornell, and Dr. Gerald Wang, Chief of Urology at NYPQ, whose mentorship and support have
Dr. Michael Erhard has dedicated nearly three decades to Nemour’s Children’s Health, where he significantly impacted pediatric care. Completing his urology residency at Jefferson in 1995, and a peds fellowship in 1997 at the University of Florida and Nemours in Jacksonville, he spent 27 years with the Nemours Children’s Health organization, holding leadership roles throughout including CMO and Enterprise Vice President. Michael has been instrumental in expanding Nemours Children’s presence in Florida, with a particular emphasis on North Florida over the last few years as President of that region. Mike officially retired in August 2024 to spend more time with his family, and was a past recipient of our Jefferson Urology Alumni Achievement Award.
been instrumental in my development. With their guidance, I have been honored to take on the role of Director of Endourology and Stone Disease, where I lead a multidisciplinary team dedicated to providing state-of-the-art care for patients with complex stone diseases.
In addition to my clinical work, I have embraced the opportunity to contribute to the academic and educational mission of our department. Jefferson instilled in me a deep commitment to teaching, and I was fortunate to be shaped by the dedication of the attendings there, including Program Director Dr. Patrick Shenot. Inspired by their approach, I have taken an active role in resident training at Weill Cornell and NYPQ. I currently serve as the Site Director for the Urology Residency Program, where I help guide and mentor the next generation of urologists in their clinical and surgical education.
I am truly grateful for the experiences and relationships I built during my time at Jefferson, which continue to shape my professional journey. Thank you to my mentors, colleagues, and fellow alumni for your ongoing support!

“Papi” Jose and Grandma Debbie Moreno with their granddaughter, Ollie.
I vividly remember taking a lucky call from Dr. Gomella 35 years ago as I stood in our kitchen in Long Beach, California –“Yes, of course I will take the urology residency offer.” It meant uprooting my wife, Debbie, and our one-year-old son, and moving across the country, away from all our family and friends. We swore that we would return to SoCal. I broke my promise, and we dropped anchor in Pennsylvania. So what happened?
Completed an awesome Jefferson Urology Residency (1995) topped with prostate circulating tumor (CTC) cell PSA RT-PCR research that was awarded 4 U.S. patents. This research first reported in 1991 and published in Cancer Research 1992 is generally recognized as the first “liquid biopsy” for prostate cancer.
Joined Tri-County Urology private practice (now MidLantic Urology) in 1995 surrounded by salt-of-the-earth staff and partners who allowed me to do research on my day off Wednesday. Through Dr. Lenny Gomella’s support (Associate Professor of Urology at that time), we worked with a start-up company, Immunicon, which developed a second-generation CTC CellSearch™ platform that became FDAapproved and cited in Nature in 2020 as contributing one of the 20 most important milestones in cancer research.
Excellent staff support at the local hospitals allowed me to do robotic cancer surgery and female pelvic reconstruction.
I had the privilege of serving as president of Pottstown Hospital medical staff, Pennsylvania Urology Association, and now in 2024 Philadelphia Urologic Society.
God blessed us with three children and a granddaughter. Ben, our oldest child now works for SpaceX and lives with his wife, Emily, and our granddaughter, Olivia, ironically in SoCal. Charlotte completed law school and is doing a clerkship for a judge in Baltimore. Will works for Hopkins Applied Physics Laboratory and lives with his wife, Victoria, in Maryland.
Today, we still live in the same house we occupied during residency, and we commute to LA as often as we can to be with our aging parents and budding granddaughter. It’s bittersweet, a blessing and all made possible with Debbie’s enduring support.
Our Jefferson urology alumni including students, residents, fellows, and faculty, should let us know if you have any personal or professional news announcements to share. If you do, please contact Dr. Paul Chung, Director of Jefferson Urology Alumni Association (paul.chung@ jefferson.edu). We are committed to keeping connected to our urology alumni across the United States and internationally. Update your contact and other information by using the following link https://tinyurl.com/ jeffersonurology or by using the QR code below on your cellphone. Alumni may also directly contact our office by phone (215-955-6961) or email janice.harper@ jefferson.edu to update your contact information. Specific questions on the Department of Urology or the Jefferson Urology Alumni Association can be directed to Dr. Paul Chung (paul.chung@jefferson. edu) or Dr. Leonard Gomella, Chair of the Department of Urology (leonard.gomella@ jefferson.edu).

Based on the recommendation of the Department of Urology Alumni Committee, Dr. Judd W. Moul (Jefferson/SKMC 1982) received the 2024 Martin L. Dresner, MD Jefferson Urology Alumni Achievement Award. The decision was based on Dr. Moul’s longstanding contributions to urology and specifically to our understanding of the diagnosis and treatment of prostate cancer. He is a noted authority on prostate cancer in AfricanAmerican men, biochemical recurrence of prostate cancer, prostate specific antigen (PSA) testing, nerve-sparing radical prostatectomy and prostate screening biomarkers.
Dr. Moul is the James H. Semans MD Professor of Surgery at Duke University Medical Center and the Duke Cancer Institute. He is a retired colonel from the United States Army Medical Corps and was the director of the Center for Prostate Disease Research from 1992-2004 at Walter Reed Army Medical Center.
Dr. Moul is a 1982 AOA graduate from Jefferson/Sidney Kimmel Medical College and completed residency training at Walter Reed Army Medical Center. He served as the Division Chief of Urology at Duke from 2004 through 2011. During this time, the program was continuously ranked in the top 10 nationally by U.S. News and World Report, he initiated a collaboration with the Department of Defense to train an Army urologist each year and established the Duke Prostate Center.
In 1995, Dr. Moul was the recipient of the AMA Young Physicians Section Community Service Award for his national involvement in prostate cancer patient support groups. He also received the Sir Henry Wellcome Medal and Prize from the Association of Military Surgeons of the United States. In 1996, he was named a Fellow for the American Urological Association/European Association of Urology International Academic Exchange Program in 1994, and was the recipient of the 1997 Gold Cystoscope Award from the AUA. Numerous other awards include the Baron Dominique Jean Larrey Military Surgeon Award for Excellence in 1998 and the Presidential Award from the Uniformed Services Urology Research Group in 2000. He was awarded the Castle Connelly Physician of the Year for Clinical Medicine in 2009 and the Penn State Eberly College of Science awarded him the Distinguished Alumni Award in 2019.
Jefferson Urology Alumni Achievement Awards have been previously presented to Drs. Ken Brownstein, Steve Strup, Marty Dresner, Michael Erhard, David Rivas and Gerry Andriole. In 2022 the award became the Martin L. Dresner, MD, Jefferson Urology Alumni Achievement Award in honor of Dr. Martin Dresner, Jefferson Medical/SKMC graduate. The formal award presentation took place during our year-end David M. Davis Visiting Professor Program on Friday June 7, 2024. We were honored that our new Thomas Jefferson University president, Dr. Susan Aldridge participated in the event along with Dr. Moul’s wife, Ellen.

the

I graduated from my Thomas Jefferson University urology residency in 2008. I took a rare one month off, got married to my amazing wife, and then started working the following month. I took my first and only job at a well-established private practice of four other urologists. The practice, the New Jersey Urologic Institute, is located in Eatontown, New Jersey, on the Jersey shore. We cover and operate at Monmouth Medical Center in scenic Long Branch, a small hospital with great staff and amazing ocean views. I have been lucky to work with a supportive and cohesive group of urologists that felt like home right from the start.
Over the years, the group evolved, partners moved and retired, and new ones joined, but the overall collaborative and cooperative feel of the group has remained. As the landscape of health care has changed, we too have transitioned to a partnership with our hospital and are now formally affiliated with the Barnabas Health System. Our practice is a general urology small group practice, serving a diverse community. We cover bread and butter urology, heavy on endourology with some laparoscopy and robotics. The practice has been very busy (we feel the urologist shortage acutely) but we have strived to maintain a work-life balance. While there’s plenty of work to be done and long hours, my group has prioritized adequate family time, flexibility, and days off. With four young kids, and a plethora of hobbies (all pretty much involving food) I have found taking the time to “recharge the batteries” essential. As time has gone on, I found myself recharging best by getting closer to nature and the simple things. My family spends time together enjoying the outdoors, hiking, fishing, paddling, riding quads, and quite a bit of gardening.
Hopefully, by working with great partners who make coming to work enjoyable, continuing to enjoy support from our partnership with our hospital system, and taking the time to enjoy life and family, I can continue to ride the ups and downs of health care in America, and strive to provide quality compassionate care to my patients for many years to come (four young kids are expensive after all!).
I graduated from the Jefferson Urology program in 2011 and I’m in my 14th year at Lehigh Valley Health Network, now part of Jefferson. My wife, Mary, and I are busy keeping up with the schedules of our three children. Professionally, my practice is heavily influenced by my Jeff mentors. I’ve started our region's only comprehensive stone center and have a robust HOLEP practice. I maintain an academic presence despite a busy clinical practice by mentoring medical students, teaching physicians HOLEP, and participating in clinical trials. Most recently, I am a PI for the SOUND trial. We are one of seven U.S. sites evaluating in-office, low amplitude ultrasound for fragmenting stones.
Dr. Jim and Mary Johannes with their children.


I graduated from Jefferson in 2000. After residency in Boston, my wife Lauren (JMC '98) and I moved to Portland, Maine. We have been here since 2005. I started a private practice
with one other urologist, and we have grown our group to seven urologists. Private practice has allowed me the flexibility to maintain my personal interests and to coach my sons’ sports teams. I have remained active in the New England Section of the AUA. I spent six years as Treasurer of the NE-AUA, and I just finished a year as President of the NEAUA in September. At the NE-AUA annual meeting in Providence, I was able to re-connect with Dr. Gomella who was there to present clinical research trial results (See page 36). I am grateful for my time at Jefferson to get me started in this great field.
I owe much to Drs. Mulholland, Gomella, Bagley, Strup, and McGinnis, as well as a large cadre of outstanding residents at that time.
Courtney Capella, MD
Medical School: Sidney Kimmel Medical College
Undergraduate: Dickinson College
Interests: Plants, National Parks, and Peloton

Mauro Dispagna, MD
Medical School: SUNY
Upstate Medical University's College of Medicine, Syracuse
Undergraduate:
University of Central Florida Interests: Soccer, Formula-1 racing, traveling, wine
Matthew Buck, MD
Medical School: Frank H. Netter MD
School of Medicine at Quinnipiac University
Undergraduate: University of Connecticut Interest: U Conn basketball, hiking, coffee, urological oncology, observational research

Daniel Inouye, MD
Medical School: University of Southern California
Undergraduate: University of California Santa Barbara Interest: Cooking, craft, cocktails, volleyball, rock climbing

Alexander Hirsch, MD
Medical School: Virginia Commonwealth University
Undergraduate: Yale University Interests: Cooking, baking, cycling, rock climbing
Maria D'Amico, MD
Medical School: Boston University School of Medicine
Undergraduate: Columbia University
Interests: Yoga, Peloton, traveling, the beach

Zachary Prebay, MD
Medical School: Medical College of Wisconsin in Milwaukee
Undergraduate: University of Michigan
Interests: Michigan football, reading, coffee, running
David Fu, MD
Medical School: University of Nebraska Medical Center
Undergraduate: Boston College Interest: Golf, basketball, cooking

Joon Yau (JY) Leong, MD
Medical School: Sidney Kimmel Medical College
Undergraduate: International Medical University Kuala Lumpur, Malaysia Interests: Hieroglyphics, being "nice"

Afzal Shakir, MD
Medical School: University of Oklahoma College of Medicine
Undergraduate: University of Oklahoma Interest: Trivia night, table tennis, bass guitar, flight simulators, 3D printing, movie character impersonations

Carlos Perez, MD., PhD
Medical School: Minnesota
Undergraduate: University of Puerto Rico at Cayey Interest: Long-distance running, anything related to reggaeton and Latin trap (merengue, salsa, bachata), cooking Puerto Rican food/trying to blend with midwest cuisine, a good beach day with friends

Michael Panagos, MD
Medical School: University of Maryland School of Medicine
Undergraduate: University of Michigan College of Engineering Interest: Michigan hootball, history, my two cats


Adam Schneider, MD
Medical School: Sidney Kimmel Medical College
Undergraduate: Loyola University
Maryland Interests: Traveling, baking, volleyball, foodie
Alice Linder, MD
Medical School: Columbia University Vagelos College of Physicians & Surgeons
Undergraduate: Harvard University Interests: Bicycling around Philadelphia, bikepacking, tennis, cooking, finding the best ice cream in Philadelphia

Courtney Stewart, MD
Medical School: UTMB John Sealy School of Medicine
Undergraduate: Lipscomb University
Interests: Pottery, reading, running, family, beginner piano player
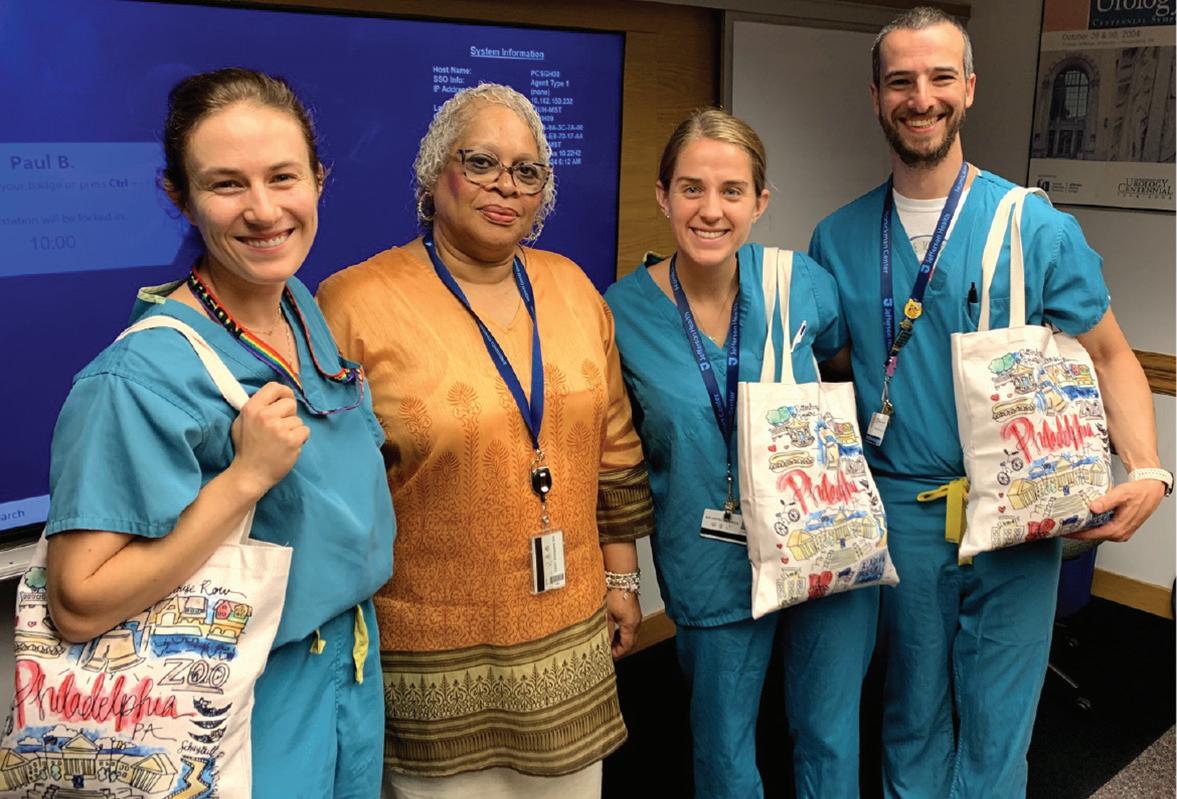
Welcome to Philadelphia gift bags for our new Urology Interns provided by Dr. Tricia Gomella. From left to right: Dr. Alice Linder from Columbia Vagelos College of Medicine, New York, Jefferson Residency Program Coordinator Janice Harper, Courtney “Coco” Stewart from the University of Texas Medical Branch John Sealy School of Medicine in Galveston, Texas, and Dr. Alexander Hirsch from Virginia Commonwealth University School of Medicine in Richmond Virginia.

WELCOME
DR. EITAN GLUCKSMAN 2024-2025 Endourology Fellow

Dr. Glucksman is our new Robotic Urologic Oncology & Minimally Invasive Surgery Fellow. Dr. Glucksman is a graduate of New York Medical College in Valhalla, New York, and is a member of the Touro University System. Eitan completed his urology residency at the Westchester Medical Center under the leadership of Drs. Mo Chaudhry and John Phillips. He is appointed at SKMC as an instructor in Urology and has full attending privileges. His primary mentors will be Drs. Costas Lallas and Scott Hubosky, our Endourology Society Fellowship program directors. Our fellowship is formally certified by the Endourology Society.

CONGRATULATIONS TO DR. ADAM SCHNEIDER AS CLINICAL EDUCATOR OF THE MONTH
Dr. Adam Schneider, PGY2 in the Department of Urology, has been recognized as a Housestaff Awardee for the “Clinical Educator of the Month” in September, 2024. The formal notification was made by Dr. John Spandorfer, Professor of Medicine and the Roger B. Daniels Associate Dean of Professionalism in Medicine. Adam received many wonderful student evaluations with just a few of them summarized here:
“Truly one of the best residents I have worked with. Adam went out of his way to make me feel included and provide me with opportunities to excel on my surgery rotation”
”Adam is very kind and always approachable. He was an excellent student mentor.
“He brought his awesome urology knowledge to us, explained things, and was very helpful with foley techniques!”
We are honored to have Adam as one of our outstanding Urology residents.
Residents
Drs. Courtney Capella & Maria D’Amico attending the SWIU (The Society of Women in Urology) meeting in New Orleans, January 2024. They were also asked to write an article for AUA News to report on the meeting. (See right.)


Dr. Zack Prebay attended the 3rd annual course on Robotics Reconstruction at Northwestern. Zack received a scholarship from Northwestern to attend based on an application demonstrating his interest in the field. Shown are the other scholarship winners Drs. Hwang and Valovska with Dr. Pebay and the Course Host Dr. Ziho Lee from Northwestern (and SKMC graduate!)


Chief resident Dr. JY Leong has been participating in our ongoing VPAC prostate cancer detection project. In addition to several poster presentations, he presented the work at the 2024 Philadelphia Urologic Society annual residents essay competition for a Second Place Prize.

Drs. Matthew Buck and David Fu participated in an endourology training program at Tulane in New Orleans this past year. Their instructor for this hands on station was Dr. Raju Thomas, Chair of Urology at Tulane and Past President of the AUA. Dr. Thomas also takes credit for training our pediatric urologist, Dr. Sonny Figueroa, as a urology resident at Tulane.
NEW CJUI EDITORIAL BOARD MEMBER
The editorial board of the Canadian Journal of Urology International has chosen our resident, PGY4 Dr. Zachary Prebay, for a two-year term on the CJUI Board as resident representative. According to George Geogieff, Publisher of the Journal: "The Canadian Journal of Urology International editorial board has included a resident representative for many years. These urology residents have helped enhance the content of the Journal and have also personally benefited from understanding the medical journal review and publishing process. We look forward to working with our newest editorial board member Jefferson Urology senior resident Dr. Zack Prebay". Dr. Prebay takes over the resident board position from Dr. JY Leong who completed his 2-year term in 2024. Dr. Prebay will be doing a reconstructive urology fellowship after graduation in 2026.
Our annual Jefferson Urology Graduations and Awards ceremonies were held during the David M. Davis year-end visiting professor program.
This year’s event was held on Friday, June 7, 2024, in the Hamilton Building.
You can read about our 2024 Visiting Professor Program on page 50.
Our graduating chief residents all receive a special keepsake signed by all residents and faculty.


Dr. Calio was born and raised in Wilmington, Delaware where he attended high school at the Charter School of Wilmington. His interests included Philly sports, movies, and golf, playing at the varsity level throughout high school. He has a younger brother who lives in the Philadelphia area where he works in finance. Brian has wanted to be a doctor since he was six years old, and never strayed from that goal. After graduating high school, Brian attended the University of Delaware where he graduated with honors and obtained a degree in biology, double minoring in Spanish and biochemistry.
At Delaware, Brian’s passion for medicine was strengthened by his many hours shadowing surgeons at Christiana Hospital and working in a basic science lab at Nemours Children’s Hospital in Wilmington. After college, Brian attended Sidney Kimmel Medical College at Thomas Jefferson University. He had always wanted to pursue a surgical specialty, and it was in his third-year rotation in urology, watching Dr. Lallas perform robotic surgery, that his decision to become a urologist was solidified. He then completed one year of research at the National Institute of Health in Bethesda, Maryland under Drs. Marston Linehan and Peter Pinto, working in the prostate cancer lab, prior to returning for his fourth year of medical school. Brian stayed at Jefferson for his residency training. It was here that he met his fiancé, Ally, an OR nurse in neurosurgery. Brian will be completing a one-year fellowship in robotic surgery at Duke University Medical Center in Durham, North Carolina.

RADHIKA RAGAM, MD, CHIEF RESIDENT
Dr. Ragam was born and raised in Flemington, NJ, alongside her parents, Venkateswara (Rags) and Kamala Ragam, and sister Ashwinee. She is the youngest of her family, with her mother being the youngest of 12 siblings! Radhika attended Hunterdon Central Regional High School where she played on the varsity girl’s golf team for four years, becoming captain her senior year and obtaining two state championships while on the team. Radhika stayed in New Jersey for college where she attended The College of New Jersey’s 7-year BS/MD program. During this time, she completed her undergraduate degree in Biology in 3 years graduating cum laude and was able to study abroad for a half year at King’s College in London.
Radhika completed her medical school training at Rutgers New Jersey Medical School in Newark, New Jersey. Here, she found fulfillment in her clinical rotations, however she found a perfect fit with the field of Urology due to the variety of conditions, personalities within the field, and surgical interventions. Radhika is headed to California for a oneyear fellowship in Minimally Invasive Surgery at University of Southern California’s Keck School of Medicine. Dr. Indy Gill, our Jefferson Urology 2025 DM Davis Visiting Professor, will be her mentor at USC.

HALLE FOSS, MD, CHIEF RESIDENT
Dr. Foss was born and raised in the suburbs of Minneapolis, MN. Growing up she loved playing tennis and developed a passion for music, learning piano, violin, guitar, and singing in choir throughout high school and college. Outside of this she always had an interest in the sciences and went on to attend St. Olaf College in Northfield, MN where she graduated Summa Cum Laude with a B.A. in Biology. During college, she worked as a medical scribe in an emergency department which inspired her to pursue a career in medicine.
Following undergrad, Halle attended the Medical College of Wisconsin in Milwaukee, WI. Here, her interest in urology was sparked after her third-year rotation. She graduated with honors in the Alpha Omega Alpha society and was ultimately matched at Jefferson for residency. Following residency, she will be moving back to Minnesota for a one-year fellowship in Endourology and Minimally Invasive Surgery at The Mayo Clinic in Rochester.

RAJIV RAGHAVAN, MD ENDOUROLGY FELLOW
Dr. Rajiv Raghavan was born in Schenectady, New York and grew up in Glenville, New York 45 minutes West of Albany. He attended The Albany Academy where he graduated as Salutatorian in 2009 and next attended Dartmouth College and the Thayer School of Engineering where he completed a 5-year combined degree in Biomedical Engineering.
At Dartmouth, Dr. Raghavan had a research interest in medical devices and biomaterials engaging in research on orthopedic biomaterials. Dr. Raghavan next enrolled in the Geisel School of Medicine at Dartmouth from which he graduated with honors. There, he developed an interest in Urology after rotating on the service and through his friend, Benjamin Dropkin, MD (now Assistant Professor of Urology at University of Kentucky). He completed his residency training with the Temple Urology residency program program and then did a oneyear clinical fellowship in Robotic and Minimally Invasive Urologic Oncology in our Department. Dr. Raghavan will be joining St. Luke’s Healthcare Network in Bethlehem, PA.
Aaron Hochberg, BS, and Brian Im, BA, had a very productive year as our Jefferson Urology Research Scholars for the 2023-2024 academic year. They combined their efforts into 24 different research projects ranging from oncology studies, to work involving penile prosthesis, infections and work on various opioid considerations in urologic surgery to name a few. Through the end of their scholar year in June 2024 they completed an amazing number of academic products including 7 manuscripts and 15 meetings abstracts and had the opportunity to present at many regional and national meetings. Their work continues after their formal year as they finish up several projects and pass others on to the current year’s scholars. Aaron and Brian are applying to urology programs for the July 1, 2025 intern year.
The Jefferson Urology Research Scholar program was established in 2017 to prepare medical students for a urology residency and to encourage careers as a physician/scientist. Intended as a “gap year” before Year 4 of medical school, the one-year, full-time program provides students with opportunities to work alongside clinical leaders in the field, garnering invaluable insight while obtaining a career-changing experience. In addition to their research programs, they have the opportunity to participate in all Department of Urology grand rounds and lectures. The Scholars program is coordinated by Dr. Costas Lallas, Vice Chair for Education, with 1 to 2 scholars chosen each year. For information on our Jefferson Urology Scholars Program, contact Dr. Lallas (costas.lallas@ jefferson.edu). You can read about our new scholars for the 2024-2025 year on page 79.

Martin L. Dresner, MD Jefferson Urology Alumni Achievement Award
Judd W. Moul, MD, FACS
(See Alumni News on page 60)
Paul Chung , MD
Presented annually by the Department of Urology residents in recognition of the attending physician who has demonstrated exceptional teaching and mentorship.
Dr. Paul Chung, Associate Professor of Urology, with Chief Residents Drs. Halle Foss, Brian Calio and Radhika Ragam, receiving the 2024 Urology Faculty Teaching Award.

Max Koppel, MD, MPH Resident

Dr. Zachary Prebay receiving the Max Koppel, MD, MPH Resident Achievement Award from Dr. Patrick Shenot (left) and Dr. Max Koppel (right). The award is based on the fall 2023 in service exam scores with Dr. Prebay a previous awardee.
The Koppel Award is given annually to the resident who achieves the highest score on the annual Urology in service exam. The award is given to honor Dr. Max Koppel who completed his residency at Jefferson in 1964. While in private practice in the Philadelphia area, Dr. Koppel participated as an officer in the
United States Public Health Service, serving in many deployments. After retirement from practice, he became a Clinical Associate Professor in the Department of Urology assisting in a variety of educational and philanthropic activities.

DOLORES SHUPP BYRNE, PhD
SENIOR UROLOGY AWARD
KERITH WANG, MD, SKMC CLASS OF 2024
Kerith Wang, MD, SKMC Class of 2024, recipient of the Dolores Shupp Byrne, PhD Senior Urology Award. Dr. Wang has begun her Urology training at the Jefferson Einstein Philadelphia program.
The Dolores Shupp Byrne Award is given in honor of Dr. Dolores Byrne who has been a member of the Department of Urology Faculty since 1987. This named award acknowledges her dedication to student teaching and mentorship. Dr. Byrne supervised research time before our program reduced the basic lab time transitioning from a 6 to a 5-year residency program. She serves as Associate Director of Urology Education, is a member of the SKMC admission Committee and supports SKMC students through their 4th year urology rotations. While still active in supporting our medical student experience in Urology, she now primarily serves as the Program Director of the Post-Baccalaureate PreProfessional (P4) program at Thomas Jefferson University. The senior student awardee is chosen by the Department of Urology faculty for their commitment to our specialty and exceptional contributions during their medical student years.

“Jefferson
As part of our Department of Urology “Jefferson 200” celebration, we were honored to have Dr. Susan Aldridge participate in our 2024 Urology Graduation and Awards ceremonies. In addition to participating in our Alumni Award presentation to Dr. Judd Moul (see page 60), she presented the evolution of Thomas Jefferson University from it’s beginnings in 1824 as Jefferson Medical College through our 200th anniversary year and what the future holds for our historic institution.
Dr. Aldridge is widely recognized internationally as a seasoned university leader, educator, and strategist. Prior to her appointment as Jefferson’s 7th and first female President, Dr. Aldridge served on Jefferson’s Board of Trustees. Dr. Aldridge has held leadership positions in some of the nation’s largest universities. She served as President of the University of Maryland Global Campus, Vice Chancellor of Troy University and President of Drexel University Online. She is passionate about creating opportunities for students to access higher education. Twice she was selected as one of Washington DC’s

Dr. Aldridge presenting during our Graduation and Awards Ceremony a Special Bicentennial Lecture titled: “Jefferson 200: Creating Our Third Century”
Top 100 Most Powerful Women, and she has received Outstanding Service Awards from the US Department of Health and Human Services, from the US Veteran’s Administration and from the US Social Security Administration. She was recognized by the Governor of Colorado for exceptional leadership in healthcare planning and delivery.
Her doctoral research, funded by the US Department of HHS, was on the impact of Medicare prospective reimbursement on patient care outcomes. Dr. Aldridge received her Bachelor’s Degree from Colorado Women’s College and her Master’s and Doctorate degrees from the University of Colorado.
A special graduation celebration was held in honor of Jefferson’s 200th year anniversary. Graduates, residents, friends and family along with our 2024 Jefferson Urology Alumni awardee Dr. Judd Moul and his wife, Ellen, enjoyed a beautiful day in Chadds Ford, PA. This year featured a special on site “restaurant service” from the Brazilian restaurant, “Fogo de Chao.”






From a very young age, Yash Shah, BS, always knew he wanted to become a doctor who could help people overcome cancer. But it wasn’t until his first year of medical school that he found his ideal specialty.
one such study, he joined a team analyzing how social factors like income, education and insurance impact metastatic testicular cancer patterns. Outside of Urology, Yash has partnered with David Nash, MD, MBA, and the Jefferson College of Population Health in research exploring how transportation, safe housing and access to nutrition could impact patient outcomes in value-based care settings.
Yash Shah distinguished himself for his interest in Urology that began in his freshman year and has continued throughout his 4 years at SKMC. What is significant about Yash is that his contributions to urology go far beyond his medical school activities. This includes being the social media manager for the "Back Table Urology" Podcast and his work with the American Urologic Association (AUA) as the founder and chief editor of the medical student column and AUA news. We are pleased to present this first ever Department of Urology Medical Student Spotlight to review many of Yash’s accomplishments he has made over the last 4 years even before he starts his formal urology residency training in 2025.
“I met Dr. [Costas] Lallas [Associate Director of the Urology Residency Program] early in medical school. I remember we first met at Di Bruno’s in Philadelphia to discuss my interest,” Yash recalls. “He told me all about urology, and I loved his approach to patient care. So, I spent lots of time shadowing him. He was one of my first mentors and a role model for how he interacts with patients and staff.”
Now, Yash is on track to follow in the footsteps of his mentors and teachers and become a urologist in an academic setting. A fourthyear medical student at Sidney Kimmel Medical College (SKMC), Yash ranks in the top 10 among his class of 270. He serves as President of the Jefferson Urology Society and leads The Journal of Urology’s Urologic Review Survey, a monthly series focused on education and simulation in urology. Perhaps most impressively, he was recognized as a Top 20 “Who to Follow” by the American Urologic Association (AUA) in his junior year.
Yash’s involvement in the AUA was inspired by his lifelong love of writing. “I noticed that there was no easy way for medical students to submit articles to the monthly AUANews publication,” Yash says. At the time, the article submission was by invitation only. So, Yash worked with the AUA editorial team and joined three other medical students to create a regular medical student column for AUANews. “More than 100 students nationwide have applied to be editors,” Yash says.
Yash has already authored numerous scholarly works, including 46 peer-reviewed publications and 53 abstracts. He’s also amassed extensive research expertise, including a study on patient factors impacting localized renal cell carcinoma that earned him a 2022-23 Summer Medical Student Fellowship Award from the AUA.
“Our study determined that increasing partial nephrectomy usage for patients with T1b-T2 renal cell carcinoma is well-advised, although certain scenarios may warrant risk-based management or radical nephrectomy use,” Yash says.
One of Yash’s research interests is studying social inequities, both in urology specifically and in the healthcare system at large. In
Yash is passionate about improving health literacy, and one of his most personally fulfilling research experiences thus far is a study comparing ChatGPT to traditional patient education materials in men’s health. “We compared ChatGPT outputs to AUA patient education and found that AI can produce high-quality, accurate material at a lower grade level with the right prompting,” Yash says. “Now, we’re researching which prompts patients can use to generate the best responses.”
One of Yash’s other professional interests is scientific communication. To that end, he’s served as social media coordinator for BackTable Urology, a podcast that offers tips, techniques and practical advice to urologists. “As our medical knowledge grows exponentially, formats like the BackTable Podcast will play a key role in disseminating information about breakthrough clinical trials and major changes in practice guidelines,” Yash says. “The podcast enables urologists worldwide to hear directly from a study’s author and use that information to provide the most up-to-date care.”
Jefferson, Yash says, has set him up for success through its emphasis on clinical medicine, extensive research opportunities and strong scholarly inquiry program. In addition to Dr. Lallas, Yash mentions Mihir Shah, MD, as one of his mentors at SKMC.
A Philadelphia native who grew up in Phoenixville, Yash is grateful to have had the chance to start his medical training in this community and give back to patients locally. Following Match Day in February 2025, “I would ideally like to treat patients inside an academic medical center, with a goal of becoming an excellent surgeon while furthering my interests in science communication and health policy,” he says.
As for incoming medical students at SKMC, Yash offers three pieces of advice: “Shadow the doctors and residents you admire, find a specialty where you enjoy the bread-andbutter work—not just the most challenging cases—and get involved in whatever other areas interest you to contribute to medicine at large.”
The Jefferson Urology Research Scholar program was established in 2017 to prepare medical students who are primarily interested in urology for a urology residency and to encourage careers as a physician/ scientist. Intended as a “gap year” before Year 4 of medical school, the one-year, full-time program provides students with opportunities to work alongside clinical leaders in the field, garnering invaluable insight while obtaining a career-changing experience. In addition to their research programs, they have the opportunity to participate in all Department of Urology grand rounds and lectures. Jefferson urologists have a long history of
RASHEED THOMPSON
contributing to the field. Some examples include inventing the first uroflowmeter, pioneering the earliest uses of laparoscopy and minimally invasive surgery in urologic practice, performing the first research in detecting circulating micrometastasis in prostate cancer using molecular techniques, establishing multidisciplinary clinics to care for GU malignancies, and performing the first adult bladder augmentations in the world using bladder tissue engineering. The Scholars program is coordinated by Dr. Costas Lallas, Vice Chair for Education. For information on our Jefferson Urology Scholars Program, please contact Dr. Lallas (costas.lallas@ jefferson.edu.)
HOME INSTITUTION: HOWARD UNIVERSITY, WASHINGTON, DC
I was born and raised in Cross Keys, South Manchester, Jamaica, and I am the first male in my family and hometown to graduate from college in the United States. As a medical student at Howard University College of Medicine, I am on the path to becoming the first physician in my family. My interest in Urology stems from the field’s dynamic nature, offering a wide variety of procedures and skills that directly enhance patients’ quality of life. This, combined with a longstanding desire to improve men’s health and wellness in the Caribbean and West Indian populations, has deepened my interest in the specialty. Outside of academics, I enjoy all sports, particularly football, basketball, and MMA, as well as cooking, music, and spending time with loved ones. I am excited to join the Urology Research Scholars Program at Thomas Jefferson University, where I look forward to building strong mentor relationships, gaining valuable research experience, and further solidifying my passion for Urology.

Our 2024-2025 Jefferson Urology Research Scholars Rasheed Thompson and Francisco (Frank) Aguire.
FRANCISCO (FRANK) AGUIRE
HOME INSTITUTION: MEDICAL COLLEGE OF WISCONSIN, MILWAUKEE, WI
Originally from the Los Angeles area, I've called Milwaukee home while in medical school. During my clerkship year at the Medical College of Wisconsin, urology was my favorite rotation, but dermatology also has interested me. My academic interests span a wide range, including health systems, health disparities, skin cancer, autoimmune blistering diseases, kidney/upper tract cancer, and endourology. When I'm not studying, I enjoy exploring architecture, cycling, and attending live music events, especially of the classical and house genres. I'm thrilled to delve deeper into urology and I am honored to be designated as the Weiner Family Foundation research scholar. Frank is supported as the 2024-2025 “The Weiner Family Foundation Urology Research Scholar” and will assist with our work in the identification of biomarkers and immune response in the treatment of bladder cancer.
Tyrique Grant is a student at Lincoln University of Pennsylvania, located in Lincoln University, PA and was with the Department of Urology during the summer of 2024. He participated in all our educational conferences and grand rounds and had exposure to both the outpatient office and operating room.
Pre-Medicine Enrichment Program (PEP) aims to diversify the urology workforce by providing direct financial support to academic programs offering support for first-generation underrepresented minority students through mentoring and support in the core areas of academic study, career planning, personal growth, and scientific research. We were fortunate to be able to sponsor these PEP students three years in a row with grant support from Mid-Atlantic American Urologic Association (AUA’s) PEP program.
Department of Urology 2024 PEP student Tyrique Grant receiving his certificate of program completion with faculty mentor Dr. Whitney Smith, Assistant Professor of Urology.

The Jefferson Urology Society is a student-run organization that provides medical students with the opportunity to learn more about the exciting and dynamic field of Urology. The goal of the society is to promote interaction among students, residents and faculty via informational sessions, research, shadowing opportunities and charitable events. The organization also works to provide interested students with faculty mentors who serve as role models and advisors for students, who are interested in pursuing a career in Urology.
According to Dr. Costas Lallas, Faculty Advisor, “The Jefferson Urology Society is an effective way to introduce students to our Urology specialty early in their medical school careers. It also engages students at all levels with faculty mentors who can guide students in research, rotation electives and ultimately residency program selection”. Any questions or comments can be directed to urology.society@ jefferson.edu.
In 2024, the Jefferson Urology Society (JUS) hosted a variety of events, including the annual Intro to Urology seminar, Robotic Surgery Demo (see below), Journal Club, and Post-Match Panel. We began a new research skills series with an "Intro to Abstract Writing" session. We also introduced a new surgical skills workshop series, where the first
workshop taught the no-scalpel vasectomy on models. Finally, we represented the department at the SKMC Career Fair and Phase 3 Specialty Open House reaching around 50 unique students through our in-person events. The Urology Society leadership continue to connect students with research and shadowing opportunities with the department of Urology, acts as liaisons for the research scholars, and offers informal mentorship to our junior students.
In April, 2024, the Jefferson Urology Society (JUS) student interest group held its annual Robot Demo featuring Dr. Costas Lallas, the faculty mentor for JUS and the Director of Robotic Surgery for Thomas Jefferson University Hospital. Dr. Lallas presented the history of robotic surgery to 25 mostly 1st and 2nd year SKMC students and then gave the students a spin on one of the da Vinci robots that sits in the TJUH ORs. In a separate room, JUS held a concomitant suturing clinic with materials supplied by the Jefferson Rector Simulation Center. It has been demonstrated that institutions with a robust student interest group such as JUS matriculate some of the highest numbers of students into the Urology match every year, and Jefferson is a leader in encouraging students’ interest in the specialty of Urology.


Dr. Costas Lallas serves as faculty mentor for the society.
President Yash Shah Year M4
VP Clinical Aaron Hochberg Year M4
VP Research
Brian Im Year M4
Secretary Josh Wahlstedt Year M3
Treasurer Anushka Ghosh Year M3
Upper Class Liaison Sohan Shah Year M3
Sean Horan Year M3
Lower Class Liaisons
Analyse Giordano Year M2
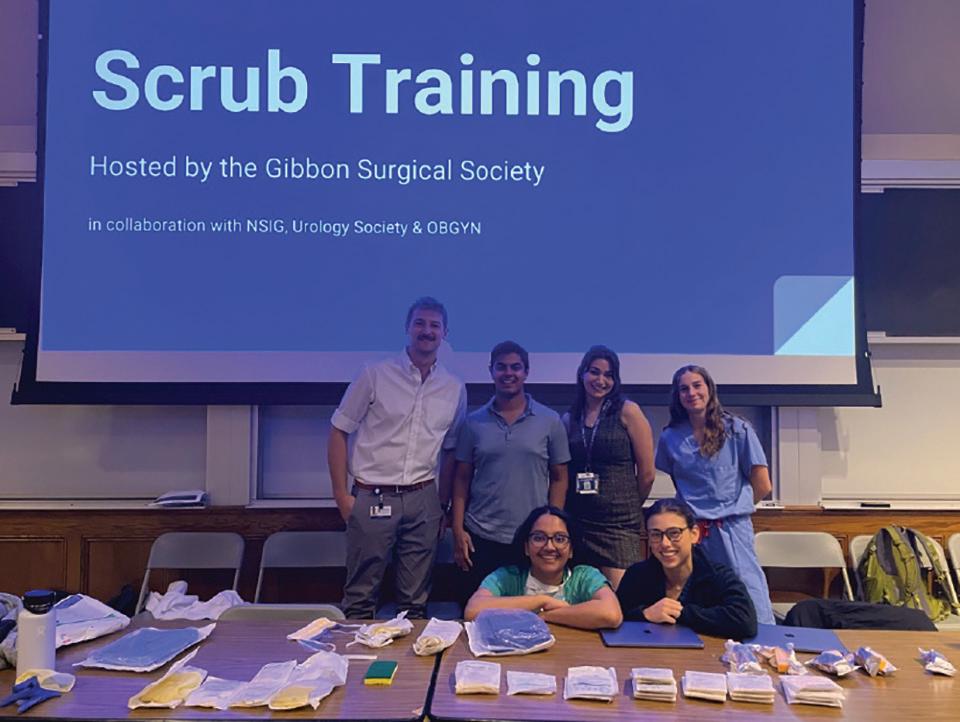
1 Dr. Costas Lallas demonstrating the DaVinci surgical robot to interested SKMC students as part of the Jefferson Urology Society activities.
2 Jefferson Urology Society members participated in the recent SKMC Career Fair and Phase 3 Specialty Open House.
3 The Jefferson Urology Society collaborated with other SKMC student surgical societies to review surgical scrub training for the operating room.
Sohan Shah, BS (SKMC 2026) received a Urology Care Foundation research award. Working with faculty mentor Dr. Paul Chung, associate professor of Urology, the grant was titled: “Novel Method to Reduce Penile Implant Infections Using Inflation and Ultrasound In Vitro.”

Sohan was selected as one of only thirteen 20232024 AUA Medical Student Research Fellows and was the Nathirmal N. Lalchandani, MD Research Fund awardee. This award supported his basic science research under the guidance of Dr. Paul H. Chung. The lab researched methods to reduce the incidence of inflatable penile prosthesis (IPP) infections through various prophylactic and intraoperative antimicrobial solutions. Sohan’s research resulted in two manuscripts published in the Journal of Sexual Medicine, two podium presentations at Mid-Atlantic AUA and Sexual medicine Society of North America (SMSNA), and multiple abstracts accepted to national conferences. In addition, an article was published in AUA News about his experience and the mentorship he received while working in the department (see below). Here are examples of Sohan’s articles published to date:
Im BH, Giordano A, Shah S, Guillame S, Evans R, Hickok NJ, Chung PH. Minocycline-rifampin-impregnated penile prosthesis surfaces retain antimicrobial activity following irrigation with 0.05% chlorhexidine gluconate and antibiotic solutions. J Sex Med. 2024 Sep 3;21(9):823-826.
Simhal R, Im BH, Shah S, Guillame S, Kerkvliet CP, Evans R, Hickok NJ, Chung PH. Antibiotic dip and irrigation solutions confer increased antimicrobial efficacy of inflatable penile prosthesis hydrophilic surfaces compared with 0.05% chlorhexidine gluconate. J Sex Med. 2024 Sep 3;21(9):816-822.

The full text of this AUA News Article can be found at: https://auanews. net/issues/articles/2024/january-extra-2024/the-urology-carefoundationt-summer-medical-student-fellowship-helps-fosterlongitudinal-interest-in-urology

Jefferson Urology 2023-2024 research Scholar Brian Im with residents Drs. Maria D’Amico and Courtney Capella presenting at Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction (SUFU) in Fort Lauderdale.

Dr. Glassman with PA students rotating on Urology Mandy Lojek and Senuri Pathiranage.
The Department of Urology offers a 4-week clinical rotation in collaboration with the Physician Assistant Studies Program, Center City Campus in the College of Health Professions, Thomas Jefferson University. Students spend time both in the outpatient and inpatient setting, including the OR. PA students also attend all Department of Urology educational conferences and meetings. Dr. Deborah Glassman is the Departmental coordinator for the PA rotations. So far, over a dozen Physician Assistant Students have rotated on the Center City Urology service.

Leonard G. Gomella, MD, FACS
Chairman, Department of Urology
The Bernard W. Godwin Jr. Professor of Prostate Cancer Sr. Director Clinical Affairs, Sidney Kimmel Cancer Ctr.
Enterprise Vice President Urology, Jefferson Health Medical School: University of Kentucky
Residency: University of Kentucky Fellowship: Surgical Oncology, National Cancer Institute, Bethesda, MD
Paul Bloch, MD
Assistant Professor
Site Director, Fishpond Office
Medical School: Sidney Kimmel Medical College
Residency: University of Tennessee Health Science Center
P. Kenneth Brownstein, MD, FACS
Clinical Assistant Professor
The Harold A. Honickman Physician Director of Jefferson Signature Services
Director of Development
Medical School: Hahnemann University (now Drexel University College of Medicine), Philadelphia, PA
Residency: General Surgery – UCLA, Harbor General HospitalSan Diego, CA
Urology Residency: Thomas Jefferson University, Phila., PA
Dolores E. Shupp-Byrne, PhD
Assistant Professor
Associate Director of Medical Student Education Director Jefferson’s Postbaccalaureate Pre-Professional Program (P4)
Graduate School: University of Pittsburgh, Pittsburgh, PA
Post-Doctoral Fellowship: Jefferson Medical College, Thomas Jefferson University, Philadelphia, PA
Paul H. Chung, MD, FACS
Associate Professor
Director Men’s Health Program, Reconstructive Urology
Trauma and Prosthetics, and Jefferson Urology Alumni Association
Site Director Honickman Office
Medical School: Sidney Kimmel Medical College
Residency: UT Southwestern Medical Center, Dallas, Texas
Fellowship: Male Genito-Urinary Reconstructive Surgery and Trauma, University of Washington, Seattle, WA
Deborah T. Glassman, MD, FACS
Clinical Associate Professor
Director Telehealth Program, APP Committee Chair, Chief Urology Wellness Officer
Medical School: NYU School of Medicine, New York, NY
Residency: University of Maryland, Baltimore, MD
Patrick T. Gomella, MD, MPH
Assistant Professor Urology and Surgery
Co-Director Prostate Cancer Focal Therapy Program
CME Coordinator
Site Director Asplundh Pavilion
Medical School: Sidney Kimmel Medical College
Residency: George Washington University Fellowship: Urologic Oncology, National Cancer Institute, Bethesda, MD
Irvin H. Hirsch, MD
Clinical Professor
Co-Director Men’s Health Program
Medical School: Mount Sinai School of Medicine, NY
Residency: Beth Israel Medical Center, New York, NY
Fellowship: Male Reproductive Medicine & Surgery/ Urodynamics & Uroprosthetics
Baylor University Medical Center, Houston, TX
Scott G. Hubosky, MD
Demetrius H. Bagley Jr. MD Professor
Vice Chair Quality Improvement & Safety
Director Division of Endourology/Co-Director Fellowship Program Endourology & Laparoscopy
Medical School: Loyola University, Stritch School of Medicine, Chicago
Residency: Thomas Jefferson University Hospital Fellowship: Robotic Surgery and Endourology, Eastern Virginia Medical School, Norfolk, VA
Joseph K. Izes, MD, FACS
Clinical Assistant Professor
Medical School: Jefferson Medical College, Thomas Jefferson University, Philadelphia, PA
Residency: Lahey Clinic Foundation, Burlington, MA Fellowship: Urologic Oncology, Lahey Clinic, Burlington, MA
Costas D. Lallas, MD, FACS
The Nathan Lewis Hatfield Professor of Urology Vice Chair, Education
Co-Director Fellowship Program Endourology & Laparoscopy Program Director
Einstein Urology Residency Program Director
Medical School: Sidney Kimmel Medical College
Residency: Duke University Fellowship: Robotic Surgery, Mayo Clinic, Scottsdale, AZ
Masaya Jimbo, MD, PhD
Assistant Professor
Medical School: Sidney Kimmel Medical College
Residency: Mayo Clinic, Rochester, MN
Fellowship: Andrology and Men’s Health, University of Utah, Salt Lake City, UT
Jeanne V. Llenado, DO, FACOS
Clinical Assistant Professor, Vice Chair Regional Urology
Site Director, South Philadelphia Campus
Medical School: UMDNJ-School of Osteopathic Medicine, Stratford, NJ
Residency: UMDNJ, Stratford NJ
Adam R. Metwalli, MD
Professor
Co-Director Prostate Cancer Focal Therapy Program
SKCCC Urology Liaison
Medical School: Wake Forest University School of Medicine
Residency: General Surger–University of Louisville Hospital
Urology – Oklahoma University Health Science Center
Fellowship Training: Urologic Oncology: National Institutes of Health and University of Texas MD Anderson Cancer Center
Alana M. Murphy, MD, FACS
Associate Professor
Associate Director Urology Residency Program
Director Female Urology
Medical School: College of Physicians & Surgeons at Columbia University, New York
Residency: Columbia University Medical Center, NY, NY
Fellowship: Female Pelvic Medicine and Reconstructive Surgery, Cleveland Clinic, Cleveland, OH
Mihir S. Shah, MD, FACS
Clinical Assistant Professor
Vice Chair for Research
Associate Director Urology Residency Program
Social Media Coordinator
Medical School: Rutgers, The New Jersey Medical School, Newark, NJ
Residency: Thomas Jefferson University Hospital
Fellowship: Advanced Robotics, Laparoscopy and Urologic Oncology, USC Los Angeles, CA
Patrick J. Shenot, MD, FACS
Professor
Deputy Chair
Residency Program Director
Chair, Faculty Affairs Committee
Medical School: State University of New York Stony Brook
Residency: Thomas Jefferson University Fellowship: Neurourology, Thomas Jefferson University
Whitney R. Smith, MD
Assistant Professor
Director DEI, Department of Urology
Chief of UROGYN for Jefferson, NJ
Medical School: Rutgers, The New Jersey Medical School, Newark, NJ
Residency: Thomas Jefferson University Hospital
Fellowship: Female Pelvic Medicine and Reconstructive Surgery Wake Forest Baptist Health, Winston-Salem, NC
Perry R. Weiner, DO, MSc, FACOS
Clinical Associate Professor
Co-Director and Founding Director, Men’s Health Program
Clinical Director, Urology Practice Operations
Site Director, Cherry Hill, NJ
Medical School: New York College of Osteopathic Medicine, Old Westbury, New York
Residency: Philadelphia College of Osteopathic Medicine, Philadelphia, PA
DEPARTMENT OF UROLOGY ADMINISTRATOR
Pamela Yong, MBA (Interim)
JOINT DEPARTMENT OF UROLOGY FACULTY
SIDNEY KIMMEL MEDICAL COLLEGE
Karolynn Echols, MD, FACOG, FPMRS, FABOIM
Associate Professor, Obstetrics and Gynecology and Urology
Director, Female Pelvic Medicine & Reconstructive
Medicine
Department of Obstetrics and Gynecology
Ethan J. Halpern, MD
Professor of Radiology and Urology
Vice Chair for Research
Department of Radiology
William Kevin Kelly, DO
Professor, Medical Oncology and Urology
Chairman Department of Medical Oncology
Marja T Nevalainen, MD, PhD
Professor, Pharmacology, Physiology and Cancer Biology and Urology
Associate Director of Translational Research and Co-Director, Prostate Cancer Working Group
Sidney Kimmel Comprehensive Cancer Center, SKCCC
Mathew L. Thakur, PhD, FSNMMI, FNAI, FACNM, FICNM, FARR
Professor of Radiology, Radiation Oncology and Urology Director, Laboratories of Radiopharmaceutical Research, Molecular Imaging and Biofluid Diagnostics
duPONT NEMOURS PEDIATRIC UROLOGY FACULTY
Jennifer Hagerty, DO, FAAP
Clinical Associate Professor of Urology and Pediatrics
Chief, Division of Urology at Nemours/Alfred I. duPont Hospital for Children
Fellowship: Northwestern University, Ann & Robert H. Lurie Children's Hospital, Chicago, IL
Pasquale “Pat” Casale, MD, FACS
Professor
Medical School: Albert Einstein College of Medicine
Residency: Thomas Jefferson University Hospital Fellowship: Seattle Children’s Hospital and Medical Center
Keara N. DeCotiis, MD
Clinical Assistant Professor of Urology Fellowship: The Hospital for Sick Children, Toronto, Canada
T.E. (Sonny) Figueroa, MD, FAAP, FACS
Professor of Urology and Pediatrics
Fellowship: Children’s Hospital of Michigan, Detroit, MI
Puneeta Ramachandra, MD
Clinical Assistant Professor of Urology and Pediatrics Fellowship: Rady Children’s Hospital of San Diego, San Diego, CA
VOLUNTEER FACULTY
Mohammed Ismail, MD
Assistant Professor
Chief of Urology, VA Medical Center Wilmington, DE
Edouard J. Trabulsi, MD, MBA, FACS
Professor
Chair, Department of Urology Jefferson Einstein Medical Center, Philadelphia, PA

Jefferson’s convenient Navy Yard location at 3 Crescent Drive, with our Department of Urology and Men’s Health Program offices.
Abington/Asplundh Cancer Pavilion
Sidney Kimmel Comprehensive Cancer Center
Site Contact: Noreen Wielgus, MSN, RN 3941 Commerce Avenue, Willow Grove, PA 19090 215-481-4668 | Fax: 215-481-8056
GU Multidisciplinary Clinic
Sidney Kimmel Comprehensive Cancer Center
Site Contact: Crystal Sypherd, CPhT 215-503-0581 Honickman Center, 14th Floor 1101 Chestnut Street Philadelphia, PA 19107 215-955-6700 | Fax: 215-955-0412

New Honickman Center located on 11th and Chestnut Sts., Philadelphia
Jefferson Urology Center City Honickman Center
Site Contact: Janelle Browning 1101 Chestnut Street, 11th Floor Philadelphia, PA 19107 215-955-1000 | Fax: 215-503-2066
Jefferson Urology Cherry Hill
Site Contact: Beverly Scarlett 2211 West Chapel Avenue, #301 Cherry Hill, NJ 08034 844-542-2273 | Fax: 856-667-2428
Jefferson Urology Navy Yard
Site Contact: Tammy Aversa 3 Crescent Drive, 2nd Floor Philadelphia, PA 19112 215-503-7124 | Fax: 215-503-3191

The Department of Urology has urologic oncologists who participate in the Sidney Kimmel Comprehensive Cancer Center at the Asplundh Cancer Pavilion in Willow Grove.
Men’s Health Program at the Navy Yard 3 Crescent Drive, 2nd Floor Philadelphia, PA 19112 215-890-1090 | Fax: 215-503-3191
Jefferson Urology Sewell
Site Contact: Rachel Petrillo 354 Hurffville Crosskeys Road Building 3 Sewell, NJ 08080 844-542-2273 | Fax: 856-667-2428
For Pediatric Urology Care Division of Pediatric Urology Nemours Physicians: 302-651-4200 Locations in Delaware, Philadelphia, Main Line and New Jersey
Jefferson NE Urology Bucks 240 Middletown Boulevard Langhorne, PA 19047 267-560-1001
Jefferson NE Urology Torresdale 3998 Red Lion Road Philadelphia, PA 19114 215-632-8882
Jefferson NE Urology Cottman 1342 Cottman Avenue
Jefferson NE Urology Welsh Road 2137 Welsh Road
Buxmont Urological Specialists 125 Medical Campus Drive Lansdale, PA 19446 215-361-2304
Buxmont Urological Specialists
Einstein Urology Philadelphia
Main number: 610 402 6986 or 1-833-587-6564
LVPG
LVPG
LVPG Urology Carbon 2226 Blakeslee Blvd Dr E, Suite 200 Lehighton, PA 18235 610-402-6986
LVPG Urology Hazelton 50 Moisey Dr. Suite 212
LVPG

1 Congratulations to Dr. Jennifer Hagerty who was selected as Nemours Children’s Health “2024 Physician of the Year”. Dr. Hagerty is Chief, Division of Pediatric Urology at Nemours and SKMC Associate Professor Urology. Shown is Dr. Hagerty is accepting the award from Mark Marcantano, JD, President, Delaware Valley Nemours Children’s Health and Meg Frizzola, DO, FAAP, Chief of Medical Staff and SKMC Associate Professor of Pediatrics Nemours Children’s Health, Delaware Valley. See more about Dr. Hagerty career on page 18.
2 Department of Urology Urologic Oncology attending physicians who participate in the SKCCC GU Multidisciplinary Clinic, gathered for a group photo in the new Honickman Center. Each member has completed formal fellowship training in urologic oncology or robotic surgery with their fellowship institution as noted. From left to right: Dr. Adam Metwalli (MD Anderson Cancer Center, Houston, TX and the NCI, Bethesda, MD), Dr. Patrick Gomella (NCI, Bethesda, MD), Dr. Leonard Gomella (NCI, Bethesda, MD), Dr. Costas Lallas (Mayo Clinic, Scottsdale), and Dr. Mihir Shah (University of Southern California, Los Angeles). (Missing Dr. Joe Izes, Lahey Clinic, Burlington, MA)
3 Enjoying the Jefferson NJ Gala February 24, 2024, at the Borgata in Atlantic City. Rick and Marlene Vallett, and Dr. Franklin and Beverly Scarlett. Beverly is our Urology Practice Manger in New Jersey, and Marlene is our Department of Urology Enterprise Ambulatory Operations Manager.
4 Jefferson Health has a new, multiyear partnership with the Philadelphia Eagles. The partnership makes Jefferson the Official Health System of the Philadelphia Eagles. Jefferson’s logo will be displayed on the team’s practice jerseys, and on the Eagles’ home press conference backdrop.
5 Department of Urology residents had the opportunity to be oriented on the new Storz endoscopy equipment that will be used in the TJUH Thompson OR and in the new Honickman Center operating rooms.
6 Chief residents Drs. Courtney Capella and JY Leong with our rotating medical student finding their “happy place” in the TJUH OR.
7 Chief Resident Dr. Courtney Capella gives a thumbs up as our new Urology Intern, Dr. Alexander Hirsch works with the DaVinci robot simulator in the Hamilton Building. The surgical skills center is part of Jefferson’s Dr. Robert and Dorothy Rector Clinical Skills Center.
8 Our Urology residents enjoying a Phillies game, May 2024.
9 Dr. Jason Aronovitz, Dr. Leonard Gomella, Department of Urology Chair, and Dr. Paul Chung, Director of Men’s Health, recently visited the Independence Blue Cross headquarters in Philadelphia to discuss developing a “Digital Tool to Improve Men’s Health Literacy”. Dr. Aronovitz is Director of Population Health Analytics and Informatics at the Jefferson Einstein Healthcare Network, and Executive Director of the Einstein Care Partners ACO in the Medicare Shared Savings Program, who is developing the Men’s Health program app along with Dr. Chung.
10 Jefferson Department of Urology residents at all levels of training enjoy a celebratory brunch after completing the annual AUA in-service exam (ISE). The ISE is an educational tool offered by the American Urological Association (AUA) to assist residency programs with objective knowledge assessment for residents in training.

11 April 25, 2024, was National Bring Your Child to Work Day. Pictured is Dr. Scott Hubosky, the Demetrius Bagley Jr. Professor of Urology, with his son, Gabriel, a recent graduate of New Jersey’s Cherokee High School Class of 2024. Gabriel is attending Seton Hall University in South Orange, NJ, in pursuit of a Bachelor of Science degree in Nursing.
12 Drs. Carlos Perez and Costas Lallas enthusiastically supporting the Phillies just before they were eliminated from playoff contention. By the time this 2024 “Year in Review” publication gets distributed, spring training will be just a few weeks away.
13 Sad news for our Urology alumni. We report on the passing of the MidTown Diner, affectionately known to the Department of Urology as the “MidStream Diner”, formerly located on this location on 11th and Sansom. The “MidStream” was a resident and attending meeting spot and after hours hang out for many years. Some good news is that a new Starbucks is scheduled to open on the first floor of the Thomas Jefferson University Hospital early in 2025. It will be the largest Starbucks in the state of Pennsylvania at 4200 sq. ft.
14 Chief Resident Dr. Maria D’Amico demonstrating the use of the endoscopic transurethral resection (TUR) simulator in the Hamilton building with one of our visiting senior medical students. The URO Mentor™ TUR simulator was a kind gift of Dr. David and Joyce Rivas.
15 Drs. Carlos Perez and JY Leong having some Halloween costume fun.
16 Drs. Costas Lallas, Anne Lizzardi, Tricia and Lenny Gomella attended the Jefferson 200 Gala celebration at the National Constitution Center on Independence Mall in Philadelphia.
17 Jefferson Urology’s Commemorative Centennial book catalogs the first 100 years of the Department from 1904 to 2004. It was one of the items selected to be enclosed in the “Jefferson 200 Time Capsule”, to be opened on the 250th Anniversary of Jefferson in 2074.
18 The Department of Urology recently hosted a Bladder Cancer Education program. In addition to Urology, Medical Oncology and Radiation Oncology faculty, members of our nursing, research staff and residents also participated in the day long program held in Jefferson’s Alumni Hall.
19 Dr. Mauro Dispagna, PGY 4 urology resident, center, working with the laparoscopic trainer while on rotation at Nemours Children’s Hospital in Wilmington. Dr. Andrew Stemberger is a PGY2 rotating from Cooper University Hospital in Camden, NJ and Kate Fitzpatrick is a third year SKMC student.
20 As part of Jefferson Health Wellness initiative, Dr. Deb Glassman, our newly designated Department of Urology Chief Wellness Officer (page 31), arranged an after-hours reception at “Top Tomato” for faculty and residents. Health systems are working to address the systemic causes of burnout for physicians and Jefferson has encouraged these types of “wellness” events. Jefferson Health has received a silver level designation by the AMA “Joy in Medicine Health System Recognition Program”. Jefferson was honored with 62 health systems for their commitment to physician well-being.

22 Our PGY2 residents Drs. Michael Panagos, Daniel Inouye and Adam Scheider are enthusiastic to start our early morning resident didactic conference with donuts.
23 Department of Urology residents and attendings gathered for a relaxing “game of golf” at Five Iron Golf located on Chestnut Street in Philadelphia. This activity is part of our Jefferson Health Wellness initiatives.
24 Dr. Leonard Gomella was a guest speaker at a Cleveland Clinic Prostate Cancer Focal Therapy program in Cleveland, OH. His lectures covered controversies in prostate cancer screening recommendations and the role of precision medicine for prostate cancer treatment decisions. Dr. Ruben Olivares (left), Associate Professor of Urology, leads the Cleveland Clinic Prostate Cancer Focal Therapy Program.
25 Janelle Browning and Kathleen Quinn, RN, setting up the “Jefferson Urology Giant Candy Holiday Party” sponsored by Dr. Tricia Gomella.
26 The perfect donor gift for our new Honickman Center Urology office!!
27 The Jefferson Urology Team at the Fishpond office. From left to right: Tori Stabler RN, Paul Bloch MD, Whitney Smith MD, and Diana Ruiz MA. (Missing Dr. Deb Glassman)
28 Chief resident Dr. JY Leong’s poster presentation with other Jefferson colleagues at the 2024 AUA meeting in San Antonio, Texas (see page 43).
29 Oksana Chupryna, RN, with her prize from the “Jefferson Urology Giant Candy Party” a 5 pound Hershey bar (see page 25 above).
30 Dr. Deb Glassman with Dr. Susan Aldridge at her inauguration as the 7th and first female President of Thomas Jefferson University at the Kimmel Center on Broad Street. It is a tradition that other University Presidents attend or send a representative to these events. Dr. Glassman was invited to represent her undergraduate alma mater, New York University, on behalf of their President, Linda G. Mills, JD, LCSW, PhD. (See also photo 33.)
31 Dr. Jennifer Hagerty with OR Nurse Haley Chambers and PGY-4 resident Dr. Mauro Dispagna having a little fun with Bluey the Australian dog at Nemours Children’s Hospital in Wilmington. Dr. Hagerty is the artist for these custom children’s bandages.
32 Caroline Richards with Shafeeqa Abraham enjoying a center city patient office Valentines Day luncheon.


33 Dr. Glassman in her official New York University regalia during the Dr. Susan Aldridge Investiture as Thomas Jefferson University President. Dr. Glassman was asked to represent the President of NYU at the event. (See also photo 30.)
34 Dr. Patrick Shenot, Professor of Urology, was recognized by Medtronic Corporation for having implanted over 250 Interstim™ devices. Dr. Shenot is shown here with Medtronic representative Chuck Leone and PGY3 resident Dr. Mat Buck.
35 Examples of a generous gift to help support the Department of Urology in the new Honickman Center. Above is an exam room in honor of Dr. Costas Lallas and below is a donor gift to support a conference room in honor of Dr. Ken Brownstein. See page 20 and the inside front cover for details on other ways to support the Department of Urology’s research, teaching and patient care missions.
36 Residents and faculty at a Nemours Children’s Health pediatric urology reception for University of Michigan visiting professor Dr. Kate Kraft, October 2024.
37 As part of the new Honickman Center opening, Dr. Leonard Gomella was featured on a series of promotions on Philadelphia bus kiosks. The images were also displayed on the SEPTA regional rail system trains and platforms.
38 Our intern, Dr. Coco Stewart, with Dr. Joe Izes, celebrating her first week on the TJUH Urology Consult service.
39 In the fall of 2024, our main academic office on 11 College had some cosmetic upgrades including painting and new flooring in the main areas. We also installed a highdefinition monitor near the waiting area to display electronic posters and other pictures of interest. Shown here is our Jefferson Urology research Scholar Frank Aguirre reviewing a Adstilladrin™ SUO-CTC bladder cancer poster presented at the 2024 SUO in Dallas, TX with Dr. Leonard Gomella as a co-author.
40 Members of the Department of Urology celebrate during our December 13, 2024 holiday party December at Top Tomato, 11th and Sansom.
41 Our interns Drs. Alice Linder, Alex Hirsch and Coco Stewart receiving instruction on the DaVinci robot set up in the OR.
42 Dr. Scott Hubosky and Chief Resident Dr. Maria D'Amico using the new CVAC 2.0 System™. The CVAC System™ (Calyxo, Pleasanton, CA) uses laser lithotripsy, irrigation, and vacuum aspiration to optimize kidney stone clearance.
Shah YB, Ghosh A, Hochberg AR, Rapoport E, Lallas CD, Shah MS, Cohen SD. Comparison of ChatGPT and Traditional Patient Education Materials for Men's Health. Urol Pract. 2024 Jan;11(1):87-94.PMID: 37914380.
Prebay ZJ, Shah MS. Editorial Comment. Urol Pract. 2024 Jan;11(1):133-134. PMID: 38117965.
Shah YB, Liu JB, Machado P, Denisenko A, Wessner CE, Wang KR, Simhal RK, Isguven S, Delaney LJ, Hickok NJ, Forsberg F, Chung PH. Addressing the need for preclinical study of penile prosthesis infection: a new animal model and narrative review. Transl Androl Urol. 2024 Feb 29;13(2):342-352. PMID: 38481874; PMCID: PMC10932634.
Shah MS, Wang KR, Shah YB, Ragam R, Simhal RK, Ghodoussipour S, Djaladat H, Mark JR, Lallas CD, Chandrasekar T. A Narrative Review on Robotic Surgery as Treatment for Renal Cell Carcinoma with Inferior Vena Cava Thrombus. J Clin Med. 2024 Feb 26;13(5):1308. PMID: 38592152; PMCID: PMC10932232.
Prebay ZJ, Fu DH, Chung PH. Androgens and Urethral Health: How Hypogonadism Affects Postoperative Outcomes of Patients Undergoing Artificial Urinary Sphincter or Inflatable Penile Prosthesis Placement. Urology. 2024 Feb;184:266-271. PMID: 37972898.
Z Prebay, D Fu, A Hochberg, B Im, S Shah, P Chung, (177) Androgen Deprivation Therapy Does Not Increase Rates for Reintervention, Complication, or Infection in Penile Implant or Artificial Urinary Sphincter Surgery, The Journal of Sexual Medicine, Volume 21, Issue Supplement_1, February 2024, qdae001.167,
Shah S, Im B, Guillaume S, Simhal R, R Evans, NJ Hickok, Chung, PH (130) Antibiotic Solutions are the Ideal Irrigation Choice for Inflatable Penile Implant Hydrophilic Surfaces, The Journal of Sexual Medicine, Volume 21, Issue Supplement_1, February 2024, qdae001.124,
Leong JY, Prebay ZJ, Ebbott D, Li M, Chung PH. Evaluating the management trends for priapism and assessing the risk of priapism after in-office intracavernosal injections: a cross-sectional analysis. Int J Impot Res. 2024 Mar 6. Epub ahead of print. PMID: 38448610.
Shah S, Im B, Hochberg A, Ghosh A, Perlov N, Lallas CD, Shah MS. Concomitant Naloxone and Opioid Prescribing Associated with Increased Rates of Substance Use Disorder and Death Following Urologic Oncologic Procedures, Urologic Oncology: Seminars and Original Investigations, 2024 March, Volume 42, Supplement, 2024, Page S107, ISSN 10781439,
McPartland C, Salib A, Banks J, Mark JR, Lallas CD, Trabulsi EJ, Gomella LG, Goldberg H, Leiby B, Den R, Chandrasekar T. Risk of Secondary Malignancies After Pelvic Radiation: A Population-based Analysis. Eur Urol Open Sci. 2024 Mar 23;63:52-61. PMID: 38558762; PMCID: PMC10979055.
Loeb S, Keith SW, Cheng HH, Leader AE, Gross L, Sanchez Nolasco T, Byrne N, Hartman R, Brown LH, Pieczonka CM, Gomella LG, Kelly WK, Lallas CD, Handley N, Mille PJ, Mark JR, Brown GA, Chopra S, McClellan A, Wise DR, Hollifield L, Giri VN. TARGET: A Randomized, Noninferiority Trial of a Pretest, Patient-Driven Genetic Education Webtool Versus Genetic Counseling for Prostate Cancer Germline Testing. JCO Precis Oncol. 2024 Mar;8:e PMID: 38452310; PMCID: PMC10939575.
Thakur M, Tomar VS, Dale E, Gomella LG, Solomides C, Kolesnikov O, Keith SW, Navarro HT, Dahlgren O, Chaga M, Trabulsi EJ. Targeting genomic receptors in voided urine for confirmation of benign prostatic hyperplasia. BJUI Compass. 2024 Apr 22;5(7):675-680. PMID: 39022663
Gomella LG. Is PSMA PET disrupting traditional prostate cancer staging and treatment? Can J Urol. 2024 Apr;31(2):1181411815. PMID: 38642457.
Ghosh A, Leong JY, Foss H, Ebbott D, Prebay Z, Li M, Chung PH. Evaluating treatment pathways for Peyronie's disease utilizing the TriNetX research registry. Int J Impot Res. 2024 Apr;36(2):168-170. PMID: 38160222.
Mandel AL, Simhal RK, Shah YB, Wang KR, Lallas CD, Shah MS. Racial Disparities in Diagnosis and Treatment of Depression Associated with Androgen Deprivation Therapy for Prostate Cancer. Urology. 2024 Apr;186:75-80. PMID: 38395075.
Simhal RK, Simon DP, Wang KR, Shah YB, Havranek B, Mark JR, Chandrasekar T, Shah MS, Lallas CD. Perioperative and Complication Related Outcomes for RoboticAssisted vs Open Radical Cystectomy: A Comparative National Surgical Quality Improvement Project Analysis. J Endourol. 2024 Apr;38(4):331-339. PMID: 38269428.
Im BH, Hochberg A, Leong JY, Lallas C, Shah M, Gomella P, et al. MP10-19 Management of Chronic Pain and Overall Morality in Metastatic Renal Cell Carcinoma: A Multicenter Investigation from a Large Global Health Research Network (TriNetX). Journal of Urology [Internet]. 2024 May 1;211(5S):e147.
Prebay ZJ, Wahlstedt J, Shakir A, Wahlstedt E, Shah MS, Chung PH. MP06-11 Patients with Hypertrophic Scarring Disorders are at Elevated Risk of Urethral Stricture, Bladder Neck Contracture and Urethroplasty Failure.
Journal of Urology. 2024 May; 211(5S):e55.
Hochberg AR, Ghosh A, Im BH, Shah S, Gomella PT, Shah M, Mark, JR, Izes JK, Metwalli AR. PD58-03 Undercoding of Von Hippel-Lindau in a Multicenter, Large-Scale Global Health Database Limits Informative Investigations: An Assessment of the TriNetX Database. The Journal of Urology 211(5S):p e1215, May 2024. |
Schostak M, Bradbury A, Briganti A, Gonzalez D, Gomella L, Mateo J, Penault-Llorca F, Stenzinger A, Wyatt AW, Bjartell A. Practical Guidance on Establishing a Molecular Testing Pathway for Alterations in Homologous Recombination Repair Genes in Clinical Practice for Patients with Metastatic Prostate Cancer. Eur Urol Oncol. 2024 Jun;7(3):344-354. doi: 10.1016/j.euo.2023.08.004. Epub 2023 Sep 14. PMID: 37714762.
Mutter MJ, Carrion R, Rogers MJ, Carson CC, Chung PH, Henry GD. Society of Urologic Prosthetic Surgeons' Coding and Billing Position Statement on Ancillary/Adjunct Penile Prosthesis Surgical Procedures: Part I. Urology. 2024 May;187:125-130.. Epub 2024 Mar 1. PMID: 38432430.
McPartland C, Salib A, Banks J, Mark JR, Lallas CD, Trabulsi EJ, Gomella LG, Goldberg H, Leiby B, Den R, Chandrasekar T. Risk of Secondary Malignancies After Pelvic Radiation: A Population-based Analysis. Eur Urol Open Sci. 2024 Mar 23;63:52-61. eCollection 2024 May. PMID: 38558762
Satyal U, Valentine H, Liu D, Slifker M, Lallas CD, Trabulsi EJ, Bukavina L, Szeto L, Hoffman-Censits JH, Mouw KW, Faltas BM, Grivas P, Ibragimova I, Porten SP, Van Allen EM, Geynisman DM, Parker DC, O'Neill JP, Drevik J, Christianson SS, Ginzburg S, Correa AF, Uzzo RG, Ross EA, Zibelman MR, Ghatalia P, Plimack ER, Kutikov A, Abbosh PH. Urine Biopsy as Dynamic Biomarker to Enhance Clinical Staging of Bladder Cancer in Radical Cystectomy Candidates. JCO Precis Oncol. 2024 Jun;8:e2300362. PMID: 38865671.
Gomella LG. The digital rectal prostate exam: from useful to useless to controversial. Can J Urol. 2024 Jun;31(3):11864-11866. PMID: 38912935
Ghagane SC, Rangrez S, Nerli RB, Thakur ML, Gomella LG. Use of TP4303 to identify prostate cancer cells in voided urine samples. Can J Urol. 2024 Jun;31(3):11892-11896. PMID: 38912942
Narayan VM, Boorjian SA, Alemozaffar M, Konety BR, Shore ND, Gomella LG, Kamat AM, Bivalacqua TJ, Montgomery JS, Lerner SP, Busby JE, Poch M, Crispen PL, Steinberg GD, Schuckman AK, Downs TM, Mashni J Jr, Lane BR, Guzzo TJ, Bratslavsky G, Karsh LI, Woods ME, Brown G, Canter D, Luchey A, Lotan Y,
Inman BA, Williams MB, Cookson MS, Chang SS, Sankin AI, O'Donnell MA, Sawutz D, Philipson R, Parker NR, Yla-Herttuala S, Rehm D, Jakobsen JS, Juul K, Dinney CPN.Efficacy of Intravesical Nadofaragene Firadenovec for Patients With Bacillus Calmette-GuérinUnresponsive Nonmuscle-Invasive Bladder Cancer: 5-Year Follow-Up From a Phase 3 Trial. J Urol. 2024 Jul;212(1):74-86 Epub 2024 May 5. PMID: 38704840
Gomella PT, Solomon J, Ahdoot M, Gurram S, Lebastchi AH, Levy E, Krishnasamy V, Kassin MT, Chang R, Wood BJ, Linehan WM, Ball MW. Timing, incidence and management of delayed bleeding after partial nephrectomy in patients at risk for recurrent, bilateral, multifocal renal tumors. Urol Oncol. 2024 Jul;42(7):222.e1-222.e7. PMID: 38614921
Mercedes R, Head D, Zook E, Eidelman E, Tomaszewski J, Ginzburg S, Uzzo R, Smaldone M, Danella J, Guzzo TJ, Lee D, Belkoff L, Walker J, Reese A, Shah MS, Jacobs B, Raman JD. Appropriateness of Imaging for Low-Risk Prostate Cancer-Real World Data from the Pennsylvania Urologic Regional Collaboration (PURC). Curr Oncol. 2024 Aug 20;31(8):4746-4752. PMID: 39195337; PMCID: PMC11352630.
Gomella LG. The Centennial Celebration of the CJU Legends in Urology. Can J Urol. 2024 Aug;31(4):11915. PMID: 39217513
Im BH, Giordano A, Shah S, Guillame S, Evans R, Hickok NJ, Chung PH. Minocyclinerifampin-impregnated penile prosthesis surfaces retain antimicrobial activity following irrigation with 0.05% chlorhexidine gluconate and antibiotic solutions. J Sex Med. 2024 Sep 3;21(9):823-826. doi: 10.1093/jsxmed/ qdae093. Erratum in: J Sex Med. 2024 Oct 31;21(11):1094.
Leader AE, Rebbeck TR, Oh WK, Patel AV, Winer EP, Bailey LO, Gomella LG, Lumpkins CY, Garraway IP, Aiello LB, Baskin ML, Cheng HH, Cooney KA, Ganzak A, George DJ, Halabi S, Hathaway F, Healy C, Kim JW, Leapman MS, Loeb S, Maxwell KN, McNair C, Morgan TM, Prindeville B, Soule HR, Steward WL, Suttiratana SC, Taplin ME, Yamoah K, Fortune T, Bennett K, Blanding-Godbolt J, Gross L, Giri VN. Adaptation of the socioecological model to address disparities in engagement of Black men in prostate cancer genetic testing. BMC Public Health. 2024 Sep 18;24(1):2533. PMID: 39289635; PMCID: PMC11409532.
Simhal R, Im BH, Shah S, Guillame S, Kerkvliet CP, Evans R, Hickok NJ, Chung PH. Antibiotic dip and irrigation solutions confer increased antimicrobial efficacy of inflatable penile prosthesis hydrophilic surfaces compared with 0.05% chlorhexidine gluconate. J Sex Med. 2024 Sep 3;21(9):816-822. Erratum in: J Sex Med. 21(11):1094. PMID: 38979774.
Shah MS, Hochberg AR, Prebay ZJ, Shah YB, Im BH, Simhal RK, Givner D, Wang KR, Simon DP, Mark JR, Metwalli AR, Lallas CD. Stent vs Stent-Less Ileal Conduits After Radical Cystectomy: Is There a Difference in Early Postoperative Outcomes? Urol Pract. 2025 Jan;12(1):139-146.
Simhal RK, Wang KR, Shah YB, Lallas CD, Shah MS, Chandrasekar T. Peri- operative outcomes following radical prostatectomy in the setting of advanced prostate cancer. BJU Int. 2024 Sep;134(3):465-472. PMID: 38653516.
Sartor O, Karrison TG, Sandler HM, Gomella LG, Amin M, Purdy J, Michalski JM, Garzotto MG, Pervez N, Balogh AG, Rodrigues GB, Souhami L, Neil Reaume M, Williams SG, Hannan R, Jones CU, Horwitz EM, Rodgers JP, Feng FY, Rosenthal SA Corrigendum to "Androgen Deprivation and Radiotherapy with or Without Docetaxel for Localized High-risk Prostate Cancer: Long-term Follow-up from the Randomized NRG Oncology RTOG 0521 Trial" [Eur. Eurol. 84(2) (2023) 156-163]. Eur Urol. 2024 Sep;86(3):289-290. PMID: 38897867
Ghoreifi A, Gomella LG, Hu JC, Konety B, Lunelli L, Rastinehad AR, Salomon G, Taneja S, Tourinho-Barbosa R, Lebastchi AH. Identifying the best candidate for focal therapy: a comprehensive review. Prostate Cancer Prostatic Dis. 2024 Oct 23. Online ahead of print. PMID: 39443815 Review.
Buraschi S, Xu SQ, Stefanello M, Moskalev I, Morcavallo A, Genua M, Tanimoto R, Birbe R, Peiper SC, Gomella LG, Belfiore A, Black PC, Iozzo RV, Morrione A. Correction: Suppression of progranulin expression inhibits bladder cancer growth and sensitizes cancer cells to cisplatin. Oncotarget. 2024 Oct 1;15:697-698. PMID: 39352802
Ajmal N, Deng Y, Kenyon LC, Curtis MT, Dispagna M, Izes J, Li L. Metastatic Prostate Adenocarcinoma to the Brain - a Clinicopathologic Analysis of 21 Cases. Diagn Pathol. 2024 Oct 1;19(1):132. https:// doi.org/10.1186/s13000-024-01554-6 PMID: 39354583; PMCID: PMC11443825.
Shah YB, Ghosh A, Hochberg A, Mark JR, Lallas CD, Shah MS. Artificial intelligence improves urologic oncology patient education and counseling. Can J Urol. 2024 Oct;31(5):12013-12018. PMID: 39462532.
Ross AE, Zhang J, Huang HC, Yamashita R, Keim-Malpass J, Simko JP, DeVries S, Morgan TM, Souhami L, Dobelbower MC, McGinnis LS, Jones CU, Dess RT, Zeitzer KL, Choi K, Hartford AC, Michalski JM, Raben A, Gomella LG, Sartor AO, Rosenthal SA, Sandler HM, Spratt DE, Pugh SL, Mohamad O, Esteva A, Chen E, Schaeffer EM, Tran PT, Feng FY. External Validation of a Digital Pathologybased Multimodal Artificial Intelligence
Architecture in the NRG/RTOG 9902 Phase 3 Trial. Eur Urol Oncol. 2024 Oct;7(5):10241033. Epub 2024 Feb 1.PMID: 38302323
Im BH, Hochberg AR, Havranek B, Capella CE, D'Amico MJ, Giordano AH, Smith W, Murphy A, Shah MS, Lallas CD. Analyzing Antibiotic Usage Trends in Genito-Urinary Infections and Procedures: Insights from the TriNetX Database. Urology. 2024 Nov 8:S00904295(24)00969-5. Epub ahead of print. PMID: 39522828.
Bryce AH, Agarwal N, Beltran H, Hussain MH, Sartor O, Shore N, Antonarakis ES, Armstrong AJ, Calais J, Carducci MA, Dorff TB, Efstathiou JA, Gleave M, Gomella LG, Higano C, Hope TA, Iagaru A, Morgans AK, Morris DS, Morris MJ, Petrylak DP, Reiter RE, Rettig MB, Ryan CJ, Sellinger SB, Spratt DE, Srinivas S, Tagawa ST, Taplin ME, Yu EY, Zhang T, McKay RR, Koo PJ, Crawford ED. Implementing evidence-based strategies for men with biochemically recurrent and advanced prostate cancer: Consensus recommendations from the US Prostate Cancer Conference 2024.Cancer. 2024 Dec 1. Online ahead of print. PMID: 39616467
Hochberg AR, Gomella PT, Im B, Ghosh A, Shah S, Thompson RAM, Zarrabi KK, Shah MS, Mark JR, Izes JK, Lallas CD, Gomella LG, Metwalli AR. Is the TriNetX Database a Good Tool for Investigation of Real-World Management of Von Hippel-Lindau? J Kidney Cancer VHL. 2024 Dec 10;11(4):28-38.
Gomella LG. My Morning Commute and the Impact of Urology.Can J Urol. 2024 Dec;31(6):12030-12031

Members of our department including faculty, residents and students have been active contributors to the American Urologic Association News over the last year. Dr. Leonard Gomella contributed this article on prostate cancer genetic testing. Chief residents Drs. Maria D’Amico and Courtney Capella contributed an article on the 2024 Society of Women in Urology annual Meeting in New Orleans (see page 66). SKMC 2026 student Sohan Shah contributed an article on his Urology care Foundation Summer Medical Student Research Fellowship (see page 81) and SKMC 2025 student Yash Shah served as AUA News Medical Student Editor and made multiple contributions (see page 78).

American Urologic Association (AUA) 2025
Annual Meeting
April 26 – 29, 2025 in Las Vegas, NV

The dates for the David M. Davis Visiting Professor are May 30 (dinner) and May 31 (educational program, graduation and awards). The event includes the DMD Visiting Professor Events as well as our various Department of Urology Award ceremonies and graduations.
The annual DM Davis Visiting Professor for 2025 will be Dr. Inderbir “Indy” Gill (pictured). Dr. Gill is Distinguished Professor and Chair of the Catherine and Joseph Aresty Department of Urology at the Keck School of Medicine, the University of Southern California in Los Angeles. He is also the founding Executive Director of the USC Institute of Urology and Associate Dean for Clinical Innovation. Dr. Gill is an internationally recognized leader in the field of robotic and laparoscopic surgery for urologic cancers. An acclaimed innovator, he and his team are the world leaders in robotic urologic cancer surgery for prostate, kidney, and bladder cancer, having performed over 15,000 aggregate cases. For his outstanding work, Dr. Gill has received numerous prestigious worldwide awards.

The Department of Urology Awards Committee is pleased to announce the 2025 recipient of the Martin L. Dresner, MD Jefferson Urology Alumni Achievement Award is Dr. Francis “Frank” Keeley. Dr. Keeley is a native of New Jersey and trained in general surgery and urology at Thomas Jefferson University, graduating in 1996. He next completed a 2-year endourology fellowship in Edinburgh Scotland before taking up the post of Consultant Urologist at the Bristol Urological Institute in England in 1998. Bristol is approximately 120 Miles west of London. He has served as Honorary Secretary of the British Association of Urological Surgeons, Honorary Treasurer of the BJU International journal and a member of the Interventional Procedures Advisory Committee of the National Institute for Clinical Excellence (NICE).
This alumni award is in honor of Dr. Martin Dresner, a 1965 Jefferson Medical College (Sidney Kimmel Medical College) graduate. The award was established in 2022 by a generous estate gift.



