




Editors: Malebona Precious Matsoso, Usuf Chikte, Lindiwe Makubalo, Yogan Pillay, Robert (Bob) Fryatt
ISBN: 978-0-6397-2368-6 (print) ISBN: 978-0-6397-2369-3 (e-book)
All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage or retrieval system, without prior permission in writing from the publisher. Subject to any applicable licensing terms and conditions in the case of electronically supplied publications, a person may engage in fair dealing with a copy of this publication for his or her personal or private use, or his or her research or private study. See Section 12(1)(a) of the Copyright Act 98 of 1978.
Typeset in ITC Galliard Std 10.5pt
Printed in South Africa by Trackstar Trading 111 (PTY) LTD
The author and the publisher believe on the strength of due diligence exercised that this work does not contain any material that is the subject of copyright held by another person. In the alternative, they believe that any protected pre-existing material that may be comprised in it has been used with appropriate authority
Chapter 8: Health Emergencies, AMR and Covid-19 Response.......................................... Introduction
Global context in the preparedness and response to health emergencies circa 2012-2015 ... South African preparedness and response to health emergencies 2015-2020
Organisation of responses to COVID-19
Emerging lessons in public health emergency preparedness and response, 2015-2020
Conclusions and way forward
Chapter 9: Non-communicable Diseases
Introduction
Key policy and guideline changes
Challenges experienced during the past 5 years
Risk factors for NCDs
Impact of COVID (good and bad) on NCDs
The New National Strategic Plan (NSP) for NCDs
Conclusions and way forward
Chapter 10: Mental Health
Introduction
Recent crises in SA mental health
Service organisation
Human resources in the mental health professions
Recent research developments for improved mental health systems
Conclusion and way forward
Chapter 11: Occupational Health and Safety ....................................................................
The world of work in South Africa – Governance, Legislation and Policy Occupational Epidemiology ............................................................................................. Occupational Health Services (Prevention, Promotion, Care, Rehabilitation)
Human resources and Professional Societies
Challenges facing South Africa
Conclusions and way forward
Chapter 12: Infrastructure
Introduction
Description of the status-quo
Broad Overview of Infrastructure Challenges in the Health Sector
Other Issues that affect Infrastructure Provision and Efficacy
Reforms by the Government to Resolve Challenges and the extent of Success
Factors that may affect Infrastructure in the Future
Conclusions and Recommendations
Chapter 13: Quality of Care
Introduction
Governance and leadership of quality
Revolutionising quality of care
Private Sector Quality
Measurement of quality Conclusions and way forward
Chapter 14: Legislative framework and the right to health 2015-2020
The Relationship Between Law and the Right to Health The Legal Framework and how it has Changed between 2015 and 2020 A Case Study: What Covid-19 Teaches us about the NHI
Conclusions and way forward
Chapter 15: Governance, Leadership and Management
The relationships and interfaces of health system governance
Governance at the frontline
Leadership and management practice
Conclusions and way forward
Chapter 16: Information and Indicators for Accountability
Introduction
Background to Information and Indicators for Accountability
Innovations and reforms, 2015–2020
Conclusions and way forward
Chapter 17: Human Resources for Health
Introduction
National Strategy on Human Resources for Health in South Africa
Status of the Health Workforce
Moving HRH towards the Centre of Health Systems: Needs, dilemmas and strategies
National HRH Strategic Planning: 2020- 2030
Conclusions and way forward
Chapter 18: Health financing
Introduction
National health insurance (NHI)
Trends in health spending and budgets
Health Market Inquiry
Standardising benefit package and options
Public sector cost pressures
Conclusions and way forward
Chapter 19: Global and Regional Health
Introduction
Global Health Landscape
South Africa’s Role in the Multilateral System for Global Health
South Africa and Health Diplomacy
Specific Initiatives of Regional Importance
Conclusions and way forward
Chapter 20: Looking to the future
Index
Table of contents 269 269 269 272 281 285 291 291 292 295 311 312 320 320 322 325 333 338 338 339 344 347 354 356 361 361 362 368 379 381

The COVID-19 pandemic has highlighted the extreme vulnerability of our national health systems. It has shown once more that investing in health care is key to economic prosperity and to progress in human development. As much as COVID-19 has exposed our weaknesses, it has also brought our strengths to the fore.
There has been unprecedented collaboration between countries and a massive show of solidarity with vulnerable communities and societies. The COVID-19 pandemic has made governments, policy-makers and health practitioners realise that to achieve and sustain Universal Health Coverage we must be prepared to respond quickly in tackling pandemics. The book is timely, as it comes at a stage when we are taking stock of the efforts we have made in the past to make our health system more resilient – some with great effect, and some less so. This publication covers a five-year period dating back from 2015. It reflects major successes but also many remaining challenges with regard to South Africa’s health system. It follows the first publication which covered the period 2009 to 2014.
The health system in South Africa remains divided and maintains its two-tier status more than 25 years into democracy. During 2019, the Lancet Commission released a report on quality of health care in South Africa, with detailed diagnosis, and recommendations to improve the quality of health care in the country and made a case that increase in coverage will not be sufficient to improve health outcomes. The Health Market Inquiry also released its final recommendations, citing many challenges in the private health sector, and market failure.
The policy reforms that ensued over the last decade involved the production of a green paper and white paper, which served as a prelude to the production of the National Health Insurance Bill. This aims to fulfil our constitutional obligation to protect the right to health care for all. It followed a far and wide consultative process through public hearings across all provinces. The public participation included submissions from various stakeholders and ordinary members of the public.
As some commentators have noted, implementation will not be easy, but the National Health Insurance will become a reality and we are committed to ensuring that our people receive quality health care and are not discriminated against based on lack of affordability.
South Africa still has the largest HIV epidemic in the world, with 8 million people living with HIV. South Africa is also still burdened by tuberculosis and accounts for 3% of cases worldwide. While we have made great progress in tackling HIV and TB – focusing on prevention, testing and treatment – we have fallen behind in reaching our 90/90/90 treatment targets and we will be focusing and quickening our pace to meet the 2025 treatment targets.
South Africa has also worked across partner institutions in the continent to tackle obstacles together. For example, we are working with the World Health Organization on the establishment of an mRNA vaccine technology transfer hub in South Africa that will use a hub-and-spoke model to transfer a comprehensive technology package and provide appropriate training to selected manufacturers in other African and low- and middle-income countries. Africa has the ability, the scientists and the industries to provide the vaccines, therapeutics and diagnostics needed to manage the African health challenges. We cannot continue being consumers of medical countermeasures for diseases produced at high prices that are not affordable to the continent.
Over the next five years, the Department has set the target to increase life expectancy to at least 66.6 years, and to 70 years by 2030. Additionally, it aims to progressively achieve Universal Health Coverage, and financial risk protection for all citizens seeking health care, through application of the principles of social solidarity, cross-subsidisation, and equity. These targets are consistent with the United Nation’s Sustainable Development Goals to which South Africa subscribes, and Vision 2030, described by the National Development Plan, that was adopted by government in 2012.
A stronger health system, and improved quality of care will be fundamental to achieve these impacts. The Department’s Strategic Plan 2020/21–2024/25 is firmly grounded in strengthening the health system. The plan lays out our strategies to each of the outcomes geared to strengthen the health system, improve quality of care, and respond to the quadruple burden of disease in South Africa. We will join hands with our Provincial Departments of Health and partners to achieve these outcomes. We will also collaborate with other government departments to reduce the impact of social determinants of health, and forge strong partnerships with social partners to improve community participation to ensure that the health system is responsive to their needs.
The analysis and recommendations that have come from this huge effort, involving so many commentators, experts, managers and policy-makers will surely assist us on the road to achieving the country’s ambitious goals.
Dr Joe Phaahla, Minister of HealthMalebona Precious Matsoso
Director of the Health Regulatory Science Platform, Wits Health Consortium and previously Director-General of the South African National Department of Health, and served on the WHO Executive Board for a three-year term, acting both as Vice-Chairperson and as Chair. Co-chair Intergovernmental Negotiating Body for the WHO convention on pandemic prevention, preparedness and response.
Previously published over 80 journals, articles, book chapters, reports and guidelines on pharmaceuticals, and on South African health policy. Co-editor of The South Africa Health Reforms 2009–2014: Moving towards UHC (Juta, 2015); Co-author of the Independent Panel for Pandemic Preparedness and Response (WHO, 2021). Peer-reviewed journal articles include High-quality health systems in the Sustainable Development Goals era: time for a revolution (Lancet, 2018), COVID-19: how a virus is turning the world upside down (BMJ, 2020).
Lindiwe Makubalo
Assistant Regional Director, World Health
Organization Africa Regional Office. Dr Makubalo has served on numerous scientific and advisory boards, bodies and groups such as the South African Medicines Control Council, national ethics councils, several data systems boards, expert group on Oncocerciasis Control, Strategic advisory group on malaria eradication, and as African representative on the UNITAID Board. Most recently she held a diplomatic role as Minister, Health Expert for the South African Government to the United Nations in Geneva where she participated and led development of important policy and resolutions such as the NCD indicators monitoring and Ebola resolutions as chair, along with other important activities to strengthen global policy for SDGs and health emergencies.
Emeritus Professor in Health Systems and Public Health. The former Head of the Department of Global Health in the Faculty of Medicine and Health Sciences has been a dental practitioner and an academic during a long and very illustrious career, and served on various professional and educational bodies for many years as well. At Stellenbosch University, which he joined in 1996 as head of the Department of Community Dentistry, he has consistently tried to address such inequalities in health care. He became Associate Dean of the Faculty in 2000 and Executive Head of the Department of Interdisciplinary Health Sciences in 2006. Chikte has played a key role in helping to advance this process of transformation, both as an academic, a Senator and a member of the University Council.
Country Director and Extraordinary Professor, Department of Global Health, Stellenbosch University, and previously Deputy Director-General: National Department of Health. Over 100 peer-review journal articles on all aspects of public health and over 40 other publications, including book chapters and public articles. This includes co-author of the book Mental Health Policy Issues for South Africa (MASA, Cape Town, 1997), Textbook of International Health, 3rd ed.
(Oxford University Press. NY, 2009), Textbook of Global Health, 4th ed. (Oxford University Press. NY, 2017). Recent peer-reviewed articles include lead author of Health benefit packages: moving from aspiration to action for improved access to quality SRHR through UHC reforms (Sex Reprod Health Matters. 2020), Towards an AIDS-free generation by 2030: how are South African children, adolescents, caregivers and health care workers coping with HIV? (South African Journal of Psychology. 2021) and co-author of The impact of implementing the 2016 WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience on perinatal deaths: an interrupted time-series analysis in Mpumalanga province, South Africa (BMJ Glob Health. 2020).
Vice President Health Systems and Policy and Global Project Director of the USAID Local Health System Sustainability Project, Abt Associates, MD 20852, USA. Has published over 40 peer-reviewed publications, chapters, editorials, and articles on topics covering health policy, health financing, health systems, HIV and TB; co-editor of The South Africa Health Reforms 2009–2014: Moving towards UHC (Juta, 2015); co-editor of Special Series Experiences in Promoting Health Finance and Governance Reforms (Health System Reform, 2018). Author of chapter on Primary health care and international development assistance in ‘International perspectives to primary care research’ (CRC Press 2015). Recent peer-reviewed articles include lead author of: editorial Tuberculosis control in South East Asia: vignettes from China, Cambodia and Myanmar (Health Policy and Planning, 2017); Commentary Financing health systems to achieve the health Sustainable Development Goals. (Lancet Global Health, 2017); Article Health sector governance: should we be investing more? (BMJ Global Health, 2017).
Professor Gill Walt, Emeritus Professor of International Health Policy, London School of Hygiene and Tropical Medicine.
Professor Craig Househam, Previously Head of Department, Western Cape Department of Health.
Japan International Cooperation Agency (JICA) South Africa Office
Wits Health Consortium (Pty) Limited (WHC), wholly owned by the University of the Witwatersrand
Foreign, Commonwealth and Development Office (South Africa), Government of UK
Board of Healthcare Funders
Andy Gray, BPharm, MSc(Pharm), FPS, FFIP, Senior Lecturer Division of Pharmacology, Discipline of Pharmaceutical Sciences, School of Health Sciences, University of KwaZulu-Natal
Annibale Cois, MEng, MPH, PhD, Researcher Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University
Ashraf Kagee, PhD, MPH, Professor of Psychology Stellenbosch University
Barry Kistnasamy, Mmed Comm Health, Compensation Commissioner National Department of Health
Beth Englebrecht, MbChB, MFam Med, DHA, DCH
Emeritus Head of Health, Western Cape Government; Adjunct Assistant Professor, UCT School of Public Health, UCT, School of Public Health
Boitumelo Mashilo, MCom (Economics of Trade and Investment) Head: Infrastructure Advisory Services, Government Technical Advisory Center
Candy Day, BSc Pharm, MMedSci (Clinical Pharmacology), Technical Specialist Health Systems Trust
Carmen Sue Christian, PhD, Senior Lecturer Department of Economics, EMS Faculty, University of the Western Cape
Crick Lund, MSocSci (Clin Psych), PhD, Professor of Global Mental Health King’s College London and University of Cape Town
Dudu Shiba, Bcur, MPH, Deputy Director: Mental Health and Substance Abuse National Department of Health
Dumisani Hompashe, PhD (Economics), Senior Lecturer Department of Economics, Faculty of Management & Commerce, University of Fort Hare
Eric Buch, MBBCh, MSc(Med), FFCH(CM)(SA), DTM&H, DOH, Professor, Health Policy and Management, School of Health Systems and Public Health, University of Pretoria and The Colleges of Medicine of South Africa (CMSA), Cape Town
Gaurang Tanna, BSc, BSc (hons) Computer Science, MPH Senior Program Officer, TB, South Africa, Bill and Melinda Gates Foundation
Gertrude Mngola, BPharm, MPH, Health Products Grant Specialist South African National AIDS Council
Giovanni Perez, Chief Director, Cape Metro Western Cape Government: Health and Wellness
Gladys Bogoshi, BSc Physiotherapy, MSc Physiotherapy( Neurology), MPH, CEO Charlotte Maxeke Johannesburg Academic Hospital
Helen Schneider, MBChB, MMed, PhD, Professor School of Public Health, University of the Western Cape
Jabulani Mndebele, Chief Director, District Health Service KwaZulu-Natal Department of Health
Jonatan Daven, BSc (Development Studies), MSc (International Relations) MSc (Public Health), Director: Health, National Treasury, GoSA
Kamy Chetty, MD, Masters (Urban and Regional Planning), Chief Executive Officer, National Health Laboratory Service
Keith Cloete, MBCHB(UCT), DCH(SA), DHM(UCT), Head of Department Western Cape Government: Health
Kerrigan Mcarthy, MBBCh, DTM&H, FCPath (Micro), MPhil (Theology), PhD (Pub lic Health), Pathologist, Centre for Vaccines and Immunology, National Institute for Communicable Disease
Kholekile Malindi, PhD, Lecturer Department of Economics, Stellenbosch University
Kwanele Asante, BA, LLB, MSc, Law and Policy Advisor South African Non-Communicable Disease Alliance
Laura Angeletti-du Toit, PhD Eng. La Sapienza, Rome, Italy, SACAP Pr Arch., Italian Engineering Council Pr Building Eng. Western Cape Government Health and Wellness
Leslie London, MB ChB, DOH, M Med (PHM), MD, Professor of Public Health Medicine, University of Cape Town
Lilian Dudley, PhD, FFPHM, MSc, MBChB, Emeritus Assoc Professor in Health Systems and Public Health, University of Stellenbosch, Dept of Global Health
Lindi Makubalo, Assistant Regional Director, World Health Organization
Lucy Gilson, BA (Hons), MA, PhD, Professor, Health Policy and Systems School of Public Health, University of Cape Town and Department of Global Health and Development, London School of Hygiene and Tropical Medicine
Lungiswa Nkonki, PhD, Senior Lecturer, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University
Marc Mendelson, PhD, MBBS, Professor, Infectious Diseases Groote Schuur Hospital, University of Cape Town
Mark Blecher, PhD, M.Med, MPhil, MBBCH, Chief Director: Health and Social Development, National Treasury, GoSA
Marumo Maake, MM Public Policy BTech: Finance and Accounting Chief Director: Public Sector Remuneration Analysis and Forecasting, National Treasury, GoSA
Melvyn Freeman, MA (Clin Psych), Extraordinary Professor Department of Psychology. University of Stellenbosch
Mohamed Jeebhay, MBChB DOH MPhil (Epi) MPH (Occ Med) PhD FCPHM (Occ Med) SA, Professor and Head of Occupational Medicine School of Public Health, University of Cape Town
Muzimkhulu Zungu, MBChB, Mmed Comm Health, FCPHM, DOMH Head of Workplace HIV TB, National Institute for Occupational Health
Nikhil Khanna, BA (Economics), MPP
Programme Manager: Sustainable Health Financing, Clinton Health Access Initiative, South Africa
Nombulelo Magula, PGDip, MBA, MSc, B. Social Science Hons WHO COVID-19 Emergency Response Consultant and Public Health World Health Organization, South Africa
Noxolo Madela, MSSc, Budget Analyst: Health, National Treasury, GoSA
Nwabisa Daniels, Bcom Hons (Economics), Analyst: Capital Project Appraisals Government Technical Advisory Center
Olga Perovic, MD, DTM&H, FCPath (Micro), MMED (Micro) Principal Pathologist, National Institute for Communicable Disease, a division of NHLS
Pamela Naidoo, PhD, CEO; Extraordinary Professor SU Heart & Stroke Foundation SA; Stellenbosch University
Patrick Moonasar, DrPH, Director Malaria and Vector-Borne Diseases Zoonotic Diseases, National Department of Health
Peter Barron, Honorary Professor, School of public Health, University of the Witwatersrand, Johannesburg
Precious Matsoso, BPharm, PDHM, LLM, Honorary Lecturer, Department of Pharmacy and Pharmacology, Director of the Health Regulatory Science Platform, Wits Health Consortium, University of the Witwatersrand
Rajen N Naidoo, MBChB; DOH; MPH (Occ Med); PhD Professor and Head of Discipline: Occupational and Environmental Health School of Nursing and Public Health, University of KwaZulu-Natal
Rajesh Patel, MBChB, FCFP, MPH, Head: Health System Strengthening Board of Healthcare Funders
Ramphelane Morewane, B Dent Ther, B Tech, PG Dip, Msc, Chief Director, National Department of Health
Raveen Naidoo, BTEMC, MSc Cardiology, MSc Emergency Medicine Director: EMS & Disaster Medicine, National Department of Health
Rene English, MBCHB, MMed, FCPHM(SA), PhD , Director: EMS & Disaster Medicine, National Department of Health
Rita Thom, MBChB (UCT); DCH (CMSA); FFPsych (CMSA); PhD (Wits) Visiting Adjunct Professor, Department of Psychiatry, University of the Witwatersrand
Ritika Tiwari, PhD, PGDM, BSc (Hons), Postdoctoral Fellow, Division of Health Systems and Public Health, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University
Robert (Bob) Fryatt, MBBS, MD, MOH, MRCP (UK), FFPH, Vice President Health Systems and Policy, Abt Associates, Abt Associates
Robyn Hayes Badenhorst, MBA expected completion 2024. UP Logistics. Project Management. Head: Group Strategy, Wits Health Consortium
Ronelle Burger, PhD (Economics), Professor, Economics Department, Faculty of Economic and Management Sciences, Stellenbosch University
Russell Rensburg, BCom Finance and Economics, Director Rural Health Advocacy Project
Sandhya Singh, M(Com Path), Director: Non-Communicable Diseases Department of Health
Sasha Stevenson, BA, BA (Hons), LLB, LLM, Head of the Health Rights Programme, SECTION27
Shabir Banoo, BPharm, PhD, Chief Technical Specialist: Pharmaceutical Policy and Pro grammes, Right to Care; Department of Pharmacy and Pharmacology, Faculty of Health Sciences, University of the Witwatersrand
Shoni Mulibana, BPharm, MPharm, MPH, Manager: Pharmaceutical Services Programmes, Right to Care
Shrikant Peters, BA (PPE), MBChB, MMed (Public Health), FCPHM Manager: Medical Services, Public Health Medicine Specialist Groote Schuur Hospital, Western Cape Department of Health Department of Public Health & Family Medicine, University of Cape Town
Sifiso Phakhati, Bcur(I ET A), Advanced Psychiatric Nursing Former Director: Mental Health and Substance Abuse, National Department of Health
Siphiwe Mndaweni, BA, MSc, MBChB, Diploma in Health Systems Management and Executive Leadership, Chief Executive Officer, Office of Health Standards Compliance
Spo M Kgalamono, MBCHB, DOH, FCPHM (Occ Med), MMed (Occupational Medicine), DPH, Executive Director, National Institute for Occupational Health
Steve Letsike, Executive Director, Access Chapter 2 and Chairperson of the Commonwealth Equality Network
Sue Putter, DipPharm, MPharm, MPA, Deputy Chief of Party and Senior Health System Strengthening Specialist, USAID Global Health Supply Chain - Technical Assistance Programme
Sumaiyah Docrat, BSc (Hons) MPH (Health Economics) PhD, Global Health Specialist: Health Economics, Systems and Policy, Independent Scholar
Tamlyn Roman, PhD, Programme Manager, Clinton Health Access Initiative, South Africa
Terence Carter, MBCHB(Natal), DCH(SA), DHM(UCT), Technical Assistant, Clinton Health Access Initiative, South Africa
Theodosia Adom, PhD, Postdoctoral Fellow, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University
Thulani Clifford Masilela, Master of Arts (MA), Clinical Psychology; Postgraduate Diploma in Health Management, Outcomes Facilitator (Senior Sector Specialist) for Health, Department of Planning Monitoring and Evaluation (DPME), Presidency, Republic of South Africa
Thulani Matsebula, BA, MSc, Senior Economist: Health, World Bank, Southern Africa
Thulile Zondi, BNUR, MPH, Chief Director, Health Information, Research, Monitoring & Evaluation, National Department of Health
Tsakani Furumele, BSc (Medical Laboratory Science), MSc (Zoology), MPH (Epidemiology and Biostatistics), Director: Communicable Disease Control, National Department of Health
Usuf Chikte, PhD, Emeritus Professor in Health Systems and Public Health Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University
Vishal Brijlal, BCom Economics, Former Advisor on Health Financing (NDoH) and Senior Director, Clinton Health Access Initiative, South Africa
Wezile Chita, MPH, PhD, Assistant Dean, Faculty of Health Sciences, University of Witwatersrand
Yogan Pillay, PhD, Country Director and Extraordinary Professor Clinton Health Access Initiative, South Africa. Department of Global Health, Stellenbosch University
AfCFTA African Continental Free Trade Area
AGSA Auditor-General of South Africa
AMR Antimicrobial Resistance
AMS Antimicrobial Stewardship
ART Antiretroviral Therapy
ARV Antiretroviral
CCMDD Centralised Chronic Medicine Dispensing and Distribution
CDC Centers for Disease Control and Prevention
CEO Chief Executive Officer
CHAI Clinton Health Access Initiative
CHW Community Health Worker
CMS Council for Medical Schemes
COPC Community-Oriented Primary Care
COVAX COVID-19 Vaccines Global Access
CSG Child Support Grant
CSOs Civil Society Organisations
CUPS Contracting Units for Primary Health Care
CVD Cardiovascular Disease
DBE Department of Basic Education
DCST District Clinical Specialist Team
DDM District Development Model
DEL Department of Employment and Labour
DHIS District Health Information System
DHS District Health System
DM Diabetes Mellitus
DMRE Department of Mineral Resources and Energy
DO District Office
DRG Diagnosis-Related Group
DR-TB Drug-Resistant TB
EML Essential Medicines List
EMS Emergency Medical Services
EMT Emergency Medical Team
EOC Emergency Operating Centres
ESMS Electronic Stock Management Systems
EtD Evidence-to-Decision
GDP Gross Domestic Product
GERMS-SA Group for Enteric, Respiratory and Meningeal Disease Surveillance in South Africa
GFATM Global Fund to Fight AIDS, Tuberculosis and Malaria
GHS General Household Survey
GLASS Global Antimicrobial Resistance and Use Surveillance System
GMP Good Manufacturing Practice
GP General Practitioner
HDI Human Development Index
HE Health Establishment
HIS Health Information System
HMI Health Market Inquiry
HOD Head of Department
HPCSA Health Professions Council of South Africa
HPL Health Promotion Levy
HPRS Health Patient Registration System
HRH Human Resources for Health
HTA Health Technology Assessment
ICRM Ideal Clinic Realisation and Maintenance
ICESCR International Covenant for Economic, Social and Cultural Rights
IHI Institute for Health Improvement
IHR International Health Regulations
ILO International Labor Organization
iMMR Institutional Maternal Mortality Ratio
IMR Infant Mortality Rate
IMS Incident Management System
IMT Incident Management Team
IP Intellectual Property
IPC Infection Prevention and Control
IPCHS Integrated People-Centred Health Service
IUSS Infrastructure Unit Support Systems
IVDs In Vitro Diagnostics
JEE Joint External Evaluation
LE Life Expectancy
MAC Ministerial Advisory Committee
MAC-AMR Ministerial Advisory Committee on Antimicrobial Resistance
MCC Medicines Control Council
MCH Maternal and Child Health
MDGs Millennium Development Goals
MEC Member of the Executive Council
MNORT Multisectoral National Outbreak Response Team
MNS Mental, Neurological and Substance Use
MPTTT Medical Products Technical Task Team
MRC Medical Research Council
MRU Monitoring and Response Unit
NAPHISA National Public Health Institute of South Africa
NATHOC National Health Operations Centre
NATJOC National Joint Operations Centre
NATJOINTS National Joint Operational and Intelligence Structure
NCCC National COVID-19 Command and Control Council
NCD Non-Communicable Disease
NCR National Cancer Registry
NCS National Core Standards
NDMC National Disaster Management Centre
NDoH National Department of Health
NDP National Development Plan
NEMLC National Essential Medicines List Committee
NGO Non-governmental Organisation
NHA National Health Accounts
NHC National Health Council
NHC-Tech National Health Council Technical Committee
NHI National Health Insurance
NHLS National Health Laboratory Services
NIAMM National Infrastructure Asset Maintenance Management
NICD National Institute of Communicable Diseases
NIOH National Institute for Occupational Health
NMRAs National Medicines Regulatory Authorities
NQIP National Quality Improvement Plan
NRAs National Regulatory Authorities
NSC National Surveillance Centre
OECD Organisation for Economic Co-operation and Development
OHS Occupational Health Services
OHSC Office of Health Standards Compliance
OSD Occupation Specific Dispensation
PDoH Provincial Department of Health
PEPFAR
The United States President's Emergency Plan For AIDS Relief
PFMA Public Finance Management Act
PHC Primary Health Care
PHDC The Western Cape Provincial Health Data Centre
PLHIV People Living With HIV/Aids
PMB Prescribed Minimum Benefit
PPE Personal Protective Equipment
PSDP Public Sector Dependent Population
PUPs Pick-up Points
SAHPRA South African Health Products Regulatory Authority
SAM Severe Acute Malnutrition
SDGs Sustainable Development Goals
SDH Social Determinants of Health
SECEDH Social, Economic, Commercial and Environmental Determinants of Health
SOP Standard Operating Procedure
SSP Stop Stockouts Project
STGs Standard Treatment Guidelines
STIs Sexually Transmitted Infections
SVS Stock Visibility System
TAC Treatment Action Campaign
TB Tuberculosis
U5MR Under-Five Mortality Rate
UHC Universal Health Coverage
UMIC Upper-Middle-Income Country
UNICEF United Nations Children’s Fund
USAID United States Agency for International Development
VUCA Volatility, Uncertainty, Complexity and Ambiguity
WBOT Ward-Based Outreach Team
WBPHCOT Ward-Based Primary Health Care Outreach Team
WISN Workload Indicators of Staffing Need
WoGA Whole of Government Approach
WoSA Whole of Society Approach
Figure 2.1 Figure 2.2 Figure 2.3 Figure 2.4 Figure 2.5
Figure 2.6 Figure 2.7 Figure 2.8 Figure 2.9
Figure 2.10 Figure 2.11 Figure 2.12 Figure 2.13
Figure 2.14 Figure 3.1 Figure 3.2 Figure 3.3 Figure 3.4
Figure 4.1 Figure 4.2 Figure 4.3 Figure 4.4 Figure 5.1
Figure 5.2 Figure 5.3 Figure 4.4 Figure 5.5 Figure 5.6
Figure 5.7
Figure 5.8 Figure 7.1
Population age structure by single years, 2020
Population distribution by race, 2020
Life expectancy at birth: South Africa 2002–2021
Number of natural and unnatural deaths: South Africa 2000–2020
Infant Mortality Rate (IMR) and Under-5 Mortality Rate (U5MR): South Africa 2002–2020
Proportion of children under five years born with low birth weight: South Africa 2015–2018, by province
Proportion of children under five years with severe acute malnutrition: South Africa 2015–2018, by province
Number of maternal deaths by underlying cause: South Africa 1997–2017
Prevalence of bacteriologically confirmed pulmonary TB among adults 15 years and older: South Africa 2018, by sex and by age group
Incidence of TB: South Africa 2000–2020
HIV Prevalence: South Africa 2017, by sex and age group
HIV Incidence: South Africa 2017, by sex and age group
Persons suffering from chronic health conditions: South Africa 2015 and 2019, by sex
Proportion of ever-partnered women aged 18 and older who have experienced physical, sexual or emotional violence committed by any partner in the past 12 months: South Africa 2017, by province
Schema of social determinants of health framework
Real Gross Domestic Product 2015–2020, annual percentage change
Health care expenditure 2015–16 to 2019–20 3G/4G LTE/5G population coverage and smartphone penetration in South Africa from 2015 to 2020
Primary health care components
Per capita expenditure on PHC and percentage of total health expenditure on PHC, 2010/11 to 2019/20 2019/20 PHC utilisation rates and average annual change between 2015/16 and 2019/20 by province
Ten elements of Cape Town Metro COPC
Incidence, new and relapse TB cases notified, HIV-positive TB incidence
TB care cascade, South Africa, 2018
Number of new and relapse notified TB cases per year, 2016–2020
Changes in HIV new infections, deaths and incidence/ prevalence ratio in South Africa 2010 to 2019
HIV testing and treatment cascade 2019, South Africa, with gaps to the three 90s targets
HIV tests done by month, in public health facilities, between March and December 2019 and 2020
Maternal mortality in public sector institutions, South Africa 2005 to 2019
National couple year protection rate
Proportion of provincial health expenditure by programme 2004/5 – 2019/20
Figure 8.1a
Figure 8.1b
Figure 8.2
Figure 9.1 Figure 9.2 Figure 9.3 Figure 9.4 Figure 9.5 Figure 9.6
Figure 11.1a-b.
Figure 11.2 Figure 11.3
Figure 12.1 Figure 12.2
Figure 12.3 Figure 12.4 Figure 12.5 Figure 12.6 Figure 13.1 Figure 13.2 Figure 13.3 Figure 13.4
Figure 13.5
Figure 13.6 Figure 13.7
Figure 15.1
Figure 16.1 Figure 16.2 Figure 18.1
Figure 18.2 Figure 18.3
Figure 18.4
Figure 18.5 Figure 18.6
Figure 18.7 Figure 18.8
Structure and functions of joint WHO-RSA listeriosis incident management team
Phase 1, 2 and 3 of the listeriosis public health emergency response plan to halt the listeriosis outbreak and prevent future outbreaks National and provincial structures supporting SARS-CoV-2 responses as of October 2021 The emergency operations centre
Percentage of deaths from various causes of mortality
Mortality from NCDs in South Africa
WHO’s best buys
Trends in selected NCD risk factors
What are South Africans eating?
Percentage of comorbidities among in-hospital COVID-19 deaths, by age group, South Africa
Pulmonary tuberculosis in Black miners and silicosis in Black South African gold miners at autopsy (1975–2019)
Injuries reported in mines for the five-year period (2014–2018)
Injuries reported among women in the mining industry (2001–2019)
Provincial spread of private health care facilities in 2020
Type of health care facilities consulted first by households in 2015 and 2020
State of health infrastructure
Cumulative number of facilities that achieved an Ideal Clinic status
Compliance of health facilities with NCS infrastructure requirements
IUSS users by country and sessions between 2018 and 2020
Conceptual framework for a high-quality South African health system
Proposed National Strategic Framework
The OHSC value chain
Annual returns submissions by hospitals in South Africa’s provinces in 2019/20
The total number of annual inspections by the OHSC per financial year
PDSA Model for Improvement
Themba hospital percentage of patients triaged within 10 minutes of arrival within the maternity admission room
The dominant relationships of everyday governance practice within the South African health system (2015–2020)
Health system accountability relationships Medicine shortages reported by patients
Provincial health spending as a percentage of budgets, 2015/16 to 2020/21
Government health spending as percentage of GDP and as percentage of total government expenditure
Health financing indicators and life expectancy compared to other UMICs, 2017
The Africa Scorecard on Domestic Financing for Health, 2017, UMIC countries
Percentage deviation from the national public health spending per capita (uninsured)
Private medical scheme expenditure by factor of provision, 2009–2019
Main budget balance, Budget 2021
Provincial health budgets, 2000/01 – 2023/24
Table 2.1
Table 3.1
Table 3.2
Table 4.1 Table 4.2 Table 5.1 Table 5.2
Table 5.3 Table 5.4 Table 5.5
Table 6.1 Table 8.1
Table 8.2 Table 8.3
The 10 leading underlying natural causes of death per age groups in South Africa
South Africa’s HDI trends (based on consistent time series data and new goalposts)
List of the key actions in South Africa within the first 14 days (March 5–19) of COVID-19
Core strategic and operational levers for PHC
Operational levers addressed
Key TB indicators in South Africa 2015 to 2020
Key HIV indicators from 2015 to 2022, South Africa (Thembisa Model)
The three 90s, South Africa, 2015 to 2022
Maternal and Child Mortality 2015 to 2020
Deliveries and terminations in adolescent girls aged 10–19 in the public sector, South Africa 2017/18 to 2021/22
Medicines availability data sources
Core capacities required to implement IHR, and South African scores during the JEE process, 2017
Significant communicable disease events and health emergencies, 2015–2020
Strategic framework and activities to preserve effectiveness of antimicrobials, improve use of antibiotics and strengthen effective management of antibiotic resistant organisms according to the National AMR Strategy Framework
Table 9.1 Table 9.2
Table 9.3 Table 11.1 Table 11.2 Table 11.3
Table 11.4
Table 11.5 Table 11.6 Table 11.7 Table 12.1 Table 12.2 Table 12.3 Table 15.1
Table 17.1 Table 17.2 Table 17.3
Goals and targets in the 2013–2017 NCD Strategic Plan
Most frequently reported cancers (National Cancer Registry: 2015–2018)
Guiding principles for the implementation of the NSP
Legislation on Occupational Health and Safety
Legislation on Occupational Health and Safety for specific sectors
Occupational diseases reported to the Compensation Fund for the non-mining sector in South Africa, 2016/17–2019/20
Occupational diseases per commodity reported in annual medical reports by South African mines (2018 and 2019)
Occupational diseases reported and certified for the mining sector of South Africa (2019–2020)
Public sector health worker COVID-19 disease data per province (March 2020–mid August 2021)
Societies of the different OSH professionals
Provincial spread of public health care facilities
Bed capacity rate per 1 0 dependent population
Waiting times per level of care
Strengthening governance through new approaches to managing meetings
Available data sources for HRH planning in South Africa
HRH studies undertaken in South Africa
2019 Public sector health workforce – Inter-provincial variation in staffing ratios per 100 0 public sector population
Table 17.4
Table 17.5
Table 18.1 Table 18.2 Table 18.3 Table 18.4
Table 18.5 Table 18.6
Table 18.7 Table 18.8 Table 18.9 Table 18.10
Table 18.11 Table 18.12
Medical Specialists in South Africa (gender break up) in 2019
Demographics of sub-specialists who were successful in colleges of medicine examinations in South Africa
Progress with NHI
Consolidated health spending (public and private sectors)
Provincial health budgets
Key health financing indicators in upper-middle-income countries, 2018
PHC expenditure per capita in highest and lowest districts (real 2019/20 prices)
Accruals and payables not recognised (unpaid accounts), 2015/16 – 2019/20
PDoH compensation of employees’ expenditure, 2015/16 – 2023/24
Trends in health personnel numbers in public sector
Distribution of critical skills per 100 0 uninsured population
Goods and services spending per capita (uninsured), 2015/16 – 2023/24
Medico-legal claims contingent liability, 2015/16 – 2020/21
Summary of health allocations for COVID-19 in the 2020 special adjustments budget
In the first book covering South Africa’s health reforms between 2009 and 2014, we noted that initiatives in South Africa on universal coverage started in the 1920s. The book reviewed the five-year period to 2014 which coincided with the end of the timeframe of the Millennium Development Goals (MDGs) and concluded that progress had been made in several key areas, but that many challenges remained.
It was also a phase of transition from MDGs to Sustainable Development Goals (SDGs). During this period progress was made in improvement in health outcomes as reflected by significant increases in life expectancy, as well as reduced maternal and child mortality. The country has the largest HIV epidemic in the world with the largest antiviral treatment programme. The period covered in the first book showed a decline in new infections, and was associated with life expectancy at birth increasing. The establishment of the Office of Health Standards Compliance provided for a systematic, independent monitoring mechanism and recommendations for redress where services failed to meet required standards. There had been progress in improving the availability of essential medicines through price reduction and increased availability of life-saving antiretroviral and other medicines. The country had seen improvements in the collection, analysis and use of information and in rolling out reforms across districts and hospitals. On the health workforce, progress had been made in developing certain specialist cadres, increasing production of health workers (doctors) and formalising the policies on community health workers as essential members of the team for primary health care level. The National Department of Health had rolled out frontline service reforms to improve primary health care services and strengthen community participation through ward-based outreach teams (WBOTs).
The authors also noted the many challenges still facing the country in 2014. The country still faced unprecedented challenges in getting over five million people on antiretroviral therapy (ART) and keeping them adherent, and of improving tuberculosis (TB) prevention and control programmes to the point of successfully treating at least 85% of all TB patients diagnosed. There were also
Malebona Precious Matsoso, Usuf Chikte, Lindiwe Makubalo, Yogan Pillay, Robert (Bob) Fryattmany challenges remaining to improve reproductive, maternal and child health and in mobilising a larger workforce, including improving access to general practitioners and in improving the functioning of WBOTs. Progress, however, was described as being slow on improving leadership and management competencies. Many more challenges were identified – around hospital management, further improvement in the provision of quality services, giving greater voice to communities, intersectoral action and the slow pace of reforms related to the implementation of National Health Insurance (NHI). The authors called for increased efforts to document, monitor and evaluate interventions to improve future planning and implementation.
Objectives of this book: Since the first book was completed, the SDGs (2015–2030) were launched. This second edition aims to document key events and initiatives between 2015 and 2020 and consider the future challenges and implications for the different institutions, practitioners and agencies involved in improving the health of people living in South Africa. The book will be a first-hand account of the ongoing story on the transformation of health and health policy in South Africa. As before, we have brought together, for each chapter, a mix of policy-makers and implementers to work with academics and researchers. This approach seeks to strengthen the links between research, evidence and policy and improve the role of science in implementation.
Intended readership: There is considerable attention on South Africa given the HIV/AIDS epidemic, the COVID-19 response, and South Africa’s growing role in global and regional health. The aim is for the book to be used by all major schools of public health that study global health, and in academic centres that host courses and conduct research on comparative social policies.
Structure: The content and structure of each chapter will start with the challenges facing South Africa in 2015; then provide a description of the initiatives that were underway or that were initiated to improve the situation between 2015 and 2020. There will be some analysis of how well these initiatives progressed, with some examples of successes and descriptions of challenges or remaining problems. There will then be a summary of the overall progress by 2020, with the authors providing some recommendations or reflections going forward.
Key themes: Four main themes run throughout the book. These are:
Health Reform: The book is about health reforms in South Africa between 2015 and 2020 – we are not looking simply for a description of the important issues in each chapter, but whether reforms took place or not. Our definition of reform is a traditional one from the World Health Organization (WHO): ‘Health sector reform deals with fundamental change of processes in policies and institutional arrangements of the health sector, usually guided by the government’.
Gender: We see this as important for all chapters, as gender inequality and discrimination faced by women and girls puts their health and well-being as well as that of their families at risk. The United Nations refers to gender as ‘the social attributes and opportunities associated with being male and female and the relationships between women and men and girls and boys’.
Equity: We will highlight the trends on health equity during this period. Again, taken from the WHO: ‘Equity is the absence of avoidable or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, or geographically. Health inequities entail a failure to avoid or overcome inequalities that infringe on fairness and human rights norms’.
Community engagement: We see this as an important ingredient of success for health reforms. The WHO has defined community engagement as ‘a process of developing relationships that enable stakeholders to work together to address health-related issues and promote well-being to achieve positive health impact and outcomes’.
Intersectoral collaboration: We see intersectoral collaboration as a key action government should adopt both to address broader determinants of health and to improve the effectiveness of health programmes. This was at the core of the declaration on primary health care in the Alma-Ata Declaration and in the more recent Almaty Declaration.
Chapter 2: (Demographic and Health Trends: 2015–2020.) The chapter provides a summary on the recent demographic trends in South Africa, including latest data on the various aspects of equity, determinants of health, health status and access to services that are critical to improving health and well-being.
Chapter 3: (Social, Economic and Environmental Determinants.) The chapter focuses on the main challenges facing South Africa in this period, in particular the macroeconomic situation, poverty, income inequality and unemployment, education and social security, nutrition and hunger, built environment, and safety and security. There is then a commentary on the lessons learned from the coordinated and intersectoral actions developed in response to COVID-19, including what the intersectoral structures achieved at national, provincial and local level, using examples that applied a social determinants of health lens. Finally, the chapter considers the role of technology and regulation, ending with some recommendations for the future.
Chapter 4: (Primary Health Care.) The chapter describes the key contextual factors impacting PHC, and then describes the national programmes and interventions on PHC active in the five-year period. These include Ward-Based Primary Health Care Outreach Teams (WBPHCOTs), District Clinical Specialist Teams (DCSTs), Ideal Clinic Realisation and Maintenance, Centralised Chronic Medicines Dispensing and Distribution Programme (CCMDDP), PHC e-health programme, and private sector contracting. The authors then summarise the main PHC performance indicators, covering financing, health workforce and PHC utilisation, and provide case studies of promising bottom-up health system strengthening, including Community-Oriented Primary Care (COPC) in Tshwane, sub-district models (KwaZulu-Natal sub-district management model, and the 3-feet model in Limpopo and Mpumalanga) and the social accountability model of Ritshidze Community-Led Monitoring of PHC. The chapter ends with a summary of remaining challenges, and conclusions on the way forward.
Chapter 5: (National Health Programmes.) In this chapter there is a focus on three health issues which are used to illustrate the successes and failures of the health system’s response between 2015 and 2020. These are HIV/AIDS, TB, and maternal and child health. The review is complemented by two case studies. The first is the Western Cape Department of Health’s response to TB using lessons learnt from the COVID-19 response and incorporating a wholeof-society approach. The second illustrates gender issues in relation to access to health services and human rights.
Chapter 6: (Accelerating Access to Medicines and Health Technologies.) The chapter focuses on three key areas of national policy and implementation, namely: the South African Health Products Regulatory Authority (SAHPRA) and re-engineering the regulatory framework for health products; Scaling differentiated service delivery models for chronic medicines; and Antimicrobial Resistance – Policy solutions for effective governance.
Chapter 7: (Hospital Services.) The chapter provides an update on relevant national legislation and polices, including the role of hospitals envisioned under the NHI. It then goes on to assess in more detail the increased governance responsibilities at hospital level in the context of the NHI purchaser/provider split and the different roles that will be played by provincial and district management. The chapter then explores the need for adherence to the King 4 governance principles, covering ethical organisational culture and the Protocol on Corporate Governance in the Public Sector. Sections then focus on community engagement and accountability and strengthening financial and supply chain management, and decentralisation of management through functional business units. The chapter discusses progress with hospital governance and policy and patient-centred care and clinical governance.
Chapter 8: COVID-19 and Emergencies. In this chapter, we evaluate why disaster risk reduction and preparedness foster health system resilience. We reflect on the global context and review South African preparedness efforts, drawing extensively from South Africa’s participation in, and findings and outcomes of the joint external evaluation of adherence to the International Health Regulations 2005. We identify health emergencies that took place from 2015–2020 and discuss in some depth two South African health emergencies that unfolded over this time. We reflect on health system responses to the unfolding COVID-19 pandemic over 2020, illustrating how these drew on experience gained by stakeholders in earlier South African emergencies. Finally, we offer pointers to support strengthening South Africa’s emergency preparedness and response over the next five years.
Chapter 9: (Non-communicable Diseases.) The chapter provides an overview of the rise in the non-communicable disease (NCD) burden in South Africa, and the main drivers of this major epidemic. The chapter provides a detailed analysis of some of the main NCDs in the country – coronary heart disease, diabetes, hypertension, cancer and asthma – with details of the trends in recent years and the key initiatives in the five-year period aimed at improving prevention, cure and rehabilitation. Conclusions include recommendations on the way forward.
Chapter 10: (Mental Health.) In this chapter we highlight the various successes in the mental health sector for the period 2015–2020, but also raise areas of concern that require urgent attention. The chapter embraces a dimensional approach to mental health, i.e. that mental health exists on a continuum from severe disability to well-being. The chapter covers five areas, starting with two recent crises in South African mental health, namely, the Life Esidimeni trag edy and the COVID-19 pandemic. The second section addresses service organisation. We highlight the importance of making optimal use of scarce resources and bring into focus the need for a comprehensive approach to service provision, including mental health promotion and prevention.
Chapter 11: (Occupational Health.) The chapter provides an outline of progress in the world of work in South Africa and the governance, legislation and policy on occupational health and safety, including the health systems response. The chapter covers the demography of work and a summary of the epidemiology of occupational injuries and disease, and the progress with occupational health services, including relevant human resources and professional societies. The remaining challenges facing South Africa are described with recommendations for the future.
Chapter 12: (Infrastructure.) The chapter provides an overview of the health infrastructure needs of the country, taking into consideration the health needs, and what is available through the public and private sectors. The chapter then reviews progress with various national initiatives aimed at responding to current challenges including the Ideal Clinic Realisation and Maintenance, the Office of Health Standards Compliance, Infrastructure Unit Support Systems, Draft 10-Year Health Infrastructure Plan, the Accelerated Health Infrastructure Roll-Out Programme, Framework for Infrastructure Delivery and Procurement Management, Draft Maintenance Strategy and the National Infrastructure Asset Maintenance Management. We review the achievements and remaining challenges for each, before looking at non-infrastructure-related challenges such as from the COVID-19 pandemic and climate change.
Chapter 13: (Quality.) This chapter reviews developments in the quality of health care in South Africa since 2015. We highlight important policy developments, and several initiatives in the public and private sectors to improve the quality of care. We also describe the key findings and recommendations of the 2019 South African Lancet National Commission report, ‘Confronting the right to ethical and accountable quality health care in South Africa’, and discuss barriers and opportunities for achieving a high-quality health system in South Africa post COVID-19.
Chapter 14: (Legislative Framework and Right to Health.) The chapter provides a summary on the relationship between law and the right to health, explaining why law matters and a human rights approach to health. It then covers the legal framework and how it has changed between 2015 and 2020, covering legislation, policy and regulations, intellectual property policy, notifiable conditions regulations, emergency medical services regulations, control of sugar, tobacco and alcohol products, and legal advocacy and legal processes. A review is provided of the Life Esidimeni crisis, when law and policy is implemented badly, and the Health Market Inquiry. A review of the key litigation includes emergency medical treatment, physician-assisted suicide and euthanasia, and medical negligence claims. A case study covers ‘What COVID-19 teaches us about the NHI’ and the chapter ends with conclusions on the way forward.
Chapter 15: (Governance, Management and Leadership.) Following a brief overview of the governance, leadership and management successes and challenges in the past, we clarify the governance and leadership concepts that underpin the chapter and describe the key governance interfaces and relationships within the South African health system. We then examine the experience of frontline (district-level) governance and subsequently focus on provincial and national levels – considering how they support or constrain frontline governance in the multi-level public health system. We then summarise the critical issues of leadership and management highlighted in earlier sections and close by drawing out key conclusions for the future about the action needed to strengthen governance, leadership and management.
Chapter 16: (Information, Indicators and Systems.) This chapter describes and evaluates advances in the availability of accurate and timely local health information in South Africa between 2015 and 2020 against the backdrop of calls for more community participation, improved health system responsiveness to communi ty needs and priorities, and enhanced provider accountability. The chapter deals with both the public and the private health sectors, although most routine data sources predominantly cover public sector provision of health care services.
Chapter 17: (Human Resources.) The chapter reviews the previous national Human Resources for Health (HRH) strategy, launched in 2011, and reviews progress with implementation, and the likely implications for HRH of future reforms, in particular the NHI Bill. The chapter then reviews the problems related to inadequate HRH data for planning and monitoring progress, with comparisons to other countries. The implications for formalisation of community health workers are considered, as well as progress in strengthening leadership across the health system. A summary of the recently completed HRH strategy is provided and some of the main challenges outlined, including dealing with the implications of the COVID-19 crisis.
Chapter 18: (Health Financing.) This chapter examines trends, problems, challenges and progress in a selection of public and private financing domains. In general, despite some progress on the policy front, inadequate progress was made on the sector’s key reform, namely NHI, and the chapter attempts to explore why this is the case. In addition, the policy focus on NHI detracted focus from several other areas including medical scheme reform, which despite the Health Market Inquiry, made limited progress. At the end of the period, a large health security crisis emerged in the form of COVID-19, which had major implications for sectoral funding. Budget allocations were initially positive to counter the pandemic in 2020/21, but then increasingly negative from 2021/22 as the effect of prolonged lockdowns on the economy worked its way through to public sector revenue and spending. Final conclusions include that the proposed NHI model in the NHI Bill may require some re-evaluation of aspects of the model to get the NHI reforms back on track.
Chapter 19: (Global and Regional Health.) The chapter provides an overview of the global and regional health architecture and the main actors and institutions that are linked to South Africa. An update is given on the main initiatives that have been undertaken of importance for South Africa, and their relative success. The chapter then reviews the role of international actors and donors in South Africa, and the role of South Africa in supporting other countries in the region. The current challenges, including cooperation during the COVID-19 crisis are reviewed with lessons and conclusions drawn out for the future.
Chapter 20: (The way forward.) The editors led the preparation of this final chapter, which takes the conclusions and recommendations made by the different teams in preparing the chapters and puts them into this final section. This chapter therefore identifies a series of operational and strategic opportunities for the country policy-makers, managers, academics, private sector and civil society to champion over the next few years.
Tracking key demographic and health status trends over time provides insights into progress made towards reducing longstanding unfair health differences. Health is commonly defined as ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’,1 and in economic terms it refers to the ability of people to thrive. What determines the realisation of good health however is multifactorial and complex. Importantly, the attainment of good health outcomes cannot be achieved exclusively through the efforts of the health sector. One’s genetic predisposition, along with a range of political, social, economic and environmental factors all influence health and well-being. This includes factors such as the geographic and political contexts within which one lives.
This chapter updates the one from the previous publication, covering the 2009–2014 period. It provides an overview of the main demographic and health trends in the country. It also highlights areas in which progress has been made as well as the challenges that remain, and concludes with a focus on how the country can improve the monitoring of the health status of South Africans in terms of equity.
South Africa is one of the most unequal countries in the world. The inequality in South Africa is rooted in the apartheid era. South Africa has a Gini coefficient of 63.0.2 Key drivers of inequality in South Africa are income, race, gender, geographic location and household composition.3,4 Labour and investment income are the greatest drivers of inequality. In recent years however, social grants have been shown to decrease inequality, as have remittances.3, 5
Rene English, Annibale Cois, Gaurang Tanna, Candy Day, Thuli ZondiExamining health trends through an equity lens requires the application of a moral dimension or judgement when analysing the differences in health across population strata (health inequalities). The judgement considers how much these differences are (1) avoidable (i.e. not the result of biology and genetics but rather consequences of how the society distributes resources and opportunities), and (2) unfair and unjust where factors such as wealth, power or social standing and not need drives unequal distribution of resources.6, 7
In South Africa, various studies have directly or indirectly measured health equity, and produced indicators of health inequality.4, 8, 9, 10, 11, 12 The studies have largely adopted cross-sectional methods to measure health status.13 The analysis of health inequality has also been based on comparisons of health outcomes across population strata defined in geographical, socio-economic or demographic terms accompanied by a composite index.9, 12, 14, 15 While explicit recall of the moral judgement that underlies the definition of health inequity is not absent in the cited literature, in most cases the unfair and unjust nature of socio-economic disparities (after adjustment for biological determinants such as gender and age) is implicit in the approach.
The equity analyses carried out in the South African population have been mostly based on self-reported data from population surveys 9, 10, 12, 15, 13, 14 and sometimes on local epidemiological surveillance sites, and reflects the general weakness of routinely collected aggregate health data and health information systems in providing indicators disaggregated by population strata. This is a problem common in countries with limited resources and often hinders the possibility of measuring inequalities and inequities by using the most suitable indicators from a theoretical point of view requiring the choice of alternative measures as proxies. A case in point is the difficulty in monitoring geographical inequalities in the progress towards universal health coverage in South Africa.16 The District Health Barometer has however made use of socio-economic status by geographic areas as a crude measure of inequity that can be used with aggregate routine data.17
Knowledge of the limitations of existing data collection systems and the implications thereof are however important to highlight here as these are to be considered when reviewing and discussing the health data presented in this chapter where possible. In the following sections, we will accompany our description of the demographic and health trends between 2015 and 2020 with equity considerations. We will do this by presenting and commenting on selected geographic, demographic and socio-economic patterns observed in the data and on how these patterns differ from those that we would expect from an equity perspective.
South Africa’s population was just under 60 million during 2020.18 Over the period under review (2015–2020), the population increased by 8.5%.18 In 2020, females (51.1%) outnumbered males, and 80.8% were classified as African, followed by Coloured (8.8%), White (7.8%) and Indian/Asian (2.6%). In general, urbanisation is increasing.18 More than half the population live in three prov inces, and two-thirds (66.7%) live in urban areas.19 Gauteng, the economic hub, remains the most populous province (at over 15 million people) despite be ing the smallest in size, followed by KwaZulu-Natal (KZN) (19.3% of the total population) and the Western Cape (WC) at 11.7%.18 The remaining primarily rural provinces have much smaller population sizes, with the Northern Cape (NC) estimated to comprise 2.2% of the population.
Internal migration patterns reveal population movements from rural to more urbanised provinces between 2015 and 2020. Internal migration was positive for Gauteng (13.4%), WC (9.9%) and NW (8.9%), but almost negligible for MP and NC and negative for the remaining provinces.18 A positive influx of migrants from outside of South Africa was observed for all provinces between 2016 and 2021. Gauteng province and the WC received the greatest influx of migrants (internal and external), while the EC, LP and KZN had a negative total for migration. The population shifts have implications for resource allocation and health care provision, access and usage and have impacts beyond health to other sectors.
Births are the main driver of population growth in South Africa. The total fertility rate peaked in 2008 at 2.66 and is progressively declining, dropping to 2.33 in 2020.18 Fertility varies across provinces. In 2020, fertility was highest in the rural provinces, namely LP (2.90) and MP (2.85) and lowest in the urban provinces of WC (2.01) and GP (1.90).18
Trends also show that South Africa’s population is growing older as the fertility rate declines overall.18 The rate of annual growth among the elderly (60 years and older) rose from 1.09% in 2002/2003 to 2.99% in 2015/2016 and remained relatively static at 2.97% in 2019/2020. In 2020, 28.6% of the population were aged 0–14 years, with most residing in KZN (21.8%) and GP (21.4%), with the 25–54-years age bracket comprising the largest population proportion (42.5%).18 The median age is also increasing from 23 years in 2002 to 27 years in 2020 (Figure 2.1). The youth (15–34 years) have increased by 4.2 million between 2002 and 2020. The economically active age group (15–64 years) represents 63.5% of the total population.18 Child and old age dependency ratios show a decrease since 2002. In 2020 Statistics South Africa reported that the population under 15 was lowest in WC (27%) and highest in rural provinces, with LP being the highest at 39%. This suggests a greater economic burden on the working-age population in these provinces. Importantly, population profiles also differ according to population group, with higher dependency ratios amongst Africans and Coloureds (Figure 2.2).18


South Africa has observed declines in overall mortality, and mortality among infants, children and women. However, these gains have all reversed over the last year due to the impact of the COVID-19 pandemic. The overall health status of the South African population has improved since 2007 and this trend continued between 2015 and 2020. Life expectancy (LE) has increased and was at an all-time high in South Africa during 2020.
The LE at birth increased between 2015 and 2020, from 60.2 to 62.5 years for males and from 64.3 to 68.5 years for females.18 The increase in LE over the past decade has largely been driven by decreasing child and young adult mortality rates attributable to the scale-up of various health programmes, including the South African antiretroviral treatment programme.20 21
Since early 2020, South Africa was however ravaged by SARS-CoV-2 infections which reversed the LE gains (See chapter on Emergencies and COVID-19). Mid-year estimates for 2021 released by Statistics South Africa estimate the impact of the pandemic on mortality since early 2020.22 The LE for males declined from 62.4 in 2020 to 59.3 in 2021, and for females the decline was from 68.4 to 64.6 years (see Figure 2.3). These declines in LE and increases in mortality reflect the ‘cumulative burden of the crisis’ when compared to recent trends. Excess deaths are defined as the total number of all-cause deaths observed during a crisis that occurs in excess of levels observed under normal conditions, and provides information on the impact of the pandemic in terms of deaths reported due to confirmed COVID-19 infections.22 23 Higher mortality was observed amongst older people and groups with comorbidities, as reflected in the age-mortality profiles.

In South Africa, causes of deaths are recorded on death notification forms completed by medical practitioners and other role players within the health system. These deaths are further categorised as natural or unnatural. Profiles of deaths in South Africa confirm that the country is faced with a quadruple burden of disease and is currently experiencing an epidemiological transition. The trends suggest an ongoing shift towards non-communicable diseases (NCDs) as the predominant cause of death, whereas communicable diseases drive infant and child mortality. Most of these causes are avoidable and have their root causes within an array of social and economic determinants of health.
A steady rise in NCDs as a cause of death has been observed since the late 2000s.24 As of 2018, just under 60% of total deaths were attributable to NCDs compared to 55.5% in 2015. Just over 10% of the population died due to injuries (e.g. homicide, accidents and suicide). A marginal upward trend is observed for the past two years. Non-communicable diseases are the primary broad cause of death amongst adult males aged 30–50 years and women aged 25–39 years, whereas the percentage of deaths due to injuries is high amongst males in the 5–9 years and 15–19 years groups, and peaks at about 65% for those aged 20–24 years.
Tuberculosis (TB) still ranks as the leading natural cause of death in 2018, followed by diabetes mellitus (DM), cardiovascular disease and other forms of heart diseases. HIV ranked fifth overall. Amongst males, TB, HIV and other forms of heart disease, DM and influenza and pneumonia are the primary underlying causes of death. For females, the primary causes are DM, cardiovascular heart disease, hypertensive disease and other forms of heart disease and HIV. For males, trends in underlying causes of death (per cause) have remained static for all causes except for TB, other forms of heart disease, influenza and pneumonia, where increases were noted. For women, increasing trends were noted for TB, other forms of heart disease, and influenza and pneumonia.
The 10 leading underlying natural causes of death for broad age groups (2018) reveal important information for policy-makers (Table 2.1). When exploring the underlying immediate, or contributing causes of death in 2018, TB, DM, cardiovascular disease, other forms of heart disease, HIV, hypertensive disorders, influenza and pneumonia, chronic lower respiratory disease and malignant neoplasms of digestive disorders were ranked amongst the top 10 (descending order). Non-natural causes of death in 2018 (n=54 163) were primarily due to external causes of accidental injury (68.3%), followed by assault (14.5%) and transport accidents (11.4%). The number of unnatural deaths among the 15–59-year-olds showed a constant increase over time, which is of great concern.23
Ages 1–14
Influenza and pneumonia
Intestinal infectious disease TB
Other forms of heart disease
Cerebral palsy and other paralytic syndromes Ages 15–44 TB HIV

Other viral diseases
Other forms of heart disease
Cerebral palsy and other paralytic syndromes Ages 45–64 years TB DM HIV
Cardiovascular Disease
Other forms of heart disease Ages 65+ DM
Cardiovascular Disease
Hypertensive Disease
Other forms of heart disease Ischaemic Heart Disease

Indicators measuring child mortality are good indicators of a population’s health,25 and neonatal mortality is said to reflect the strength of a country’s health system.26 High death rates amongst children reflect policy failures at multiple levels and have broader societal and public health impacts. Overall, infant mortality rates (IMRs) and under-five mortality rates (U5MRs) in South Africa continue to decline. In South Africa, most women access public sector health facilities during the antenatal period and when giving birth. The indicators presented here reflect mortality rates as measured within public sector health facilities.
The early neonatal death in-facility rate, namely infants of 0–7 days who died during their stay, has decreased between 2017/18 and 2019/20 from 10.2 to 9.6 per 1 000 live births, respectively. Similar reductions are reflected for overall in-facility neonatal mortality (infants 0–28 days who died during their stay in-facility per 1 000 live births) and stillbirth rates. Disaggregation by province however reveals inter-provincial differences with poorer outcomes observed in the more rural provinces. The early neonatal death in-facility rate was highest in the NC (13.1 per 1 000 live births) and lowest in the WC (6.5), with increasing rates observed within three predominantly rural provinces (LP, NC and NW). Stillbirth rates were highest in the NC (24) and lowest in the WC (16.5). Neonatal death rates are highest in the FS (15.6) and NC (15.5), and lowest in the WC (8.2). Increasing trends are noted in the FS, LP, NC and NW provinces.
Infant mortality rates (deaths under one-year per 1 000 live births) and U5MRs have significantly improved over the five-year period. The IMR was estimated to be at 28 per 1 000 live births in 2015, compared to 21 in 2020 (according to the Rapid Mortality Surveillance report 2019/2020) and 23.6 in 2020 (according to Statistics South Africa). The U5MR was 39 per 1 000 live births in 2015, compared to 28 per 1 000 live births in 2020 (according to the Rapid Mortality Surveillance report 2019/20 ) and 34.1 in 2020 (according to Statistics South Africa).28
Low birth weight is defined as weight at birth less than 2 500g. The proportions were calculated from the sum of live births under 2 500g divided by the total sum of live births in a facility. Nationally, there was a decrease in the percentage of children with low birth weight between the years 2014 and 2015 (13.1% to 12.9%). Thereafter, there was a steady increase from 12.9% in 2015 to 13.5% in 2017, then a decrease to 12.9% in 2018 reverting back to 2015 levels. The figure below reflects the provincial trends. Northern Cape has consistently recorded the highest percentages of children with low birth weight for all the years. Provinces that have experienced an increase in the proportions of live births under 2 500g over the 2014–2019 period are EC (13.6% to 14.0%) and FS (13.6% to 13.9%).

Malnutrition is a leading cause of death amongst children in South Africa and has significant longstanding effects on those who survive and generations to come. Nationally, proportions of children under five years with Severe Acute Malnutrition (SAM) decreased slightly from 3.6% in 2016 to 2.1% in 2017, and then increased slightly from 2.1% in 2017 to 2.2% in 2018. In 2018, NC, FS and NW had the highest proportion of SAM incidences of 6%, 5% and 4.6%, respectively, while EC, GP and MP had the lowest proportions at 0.7%, 1.6% and 1.7%, respectively. In 2019, the General Household Survey reported that severe food inadequacy was highest in the NC (12.2%) and the NW (11.4%) provinces – higher than the national value of 6.3%.29 It is very likely that the levels of SAM will have been massively worsened by the COVID-19 crisis.
Measuring maternal mortality provides insights into health services and broader societal factors that determine the health of a pregnant woman and her ability to deliver a child. The National Committee on Confidential Enquiries into Maternal Deaths (NCCEMD) has documented the rise and fall of maternal deaths, with the institutional Maternal Mortality Ratio (iMMR) reaching a peak of 189 per 100 000 live births in 2009 and dropping well below 100 per 100 000 live births in 2019 for the first time since the start of the enquiry.30 Nationally, in-facility maternal deaths declined from 1 019 (2017/18) to 928 (2019/20) per annum. This translates into an iMMR of 105.7 to 88.0 per 100 000 live births over the same period. Provincial trends over time reflect similar improvements, except for the NC where the ratio has increased from 65.9 to 109.9 per 100 000 live births over the 2017/18 to 2019/20 period.

* Other refers to ‘previous existing disease or disease that developed during pregnancy and not due to direct obstetric causes but were aggravated by the physiologic effects of pregnancy’
Source: Dorrington R, Bradshaw D, Laubsher R, Nanna N. Rapid mortality surveillance report 2019 & 2020. Cape Town: Burden of Disease Research Unit, SAMRC, 2021

Annually, a representative portion of the South African population are asked to rate their health based on their own definition of health, and where they accessed care and their levels of satisfaction.29 In a 2019 survey, the first type of health care facility accessed by households when members were ill or injured were public clinics (65.4%), private doctors (21.0%), public hospitals (6.9%), private hospitals (3.1%) and private clinics (2.1%). Public health clinic use was highest in LP (74%), MP (81.2%) and the EC (80.9%), whereas usage in the WC (42.3%) and GP (59.4%) were the lowest. Most (77.1%) reported being very or somewhat satisfied with the services received within the public sector, compared to 97.4% for the private sector.
This is also reflected in the medical aid coverage, where it was highest in GP (24.9%) and the WC (24.1%) and lowest in LP (9.9%) and the EC (10.8%).29
Overall, a very small increase in the medical aid coverage was noted in the country since 2002 (15.9%–17.2%), but this value has remained relatively static between 2015 and 2020. The average for those living in metropolitan cities was 25.2%. The population group that reported the highest coverage were those who classified themselves as White (72.4%), followed by the Indian/Asian group (47.2%). Coverage was lowest for the Coloured group (20.6%) and Black Africans, where only one-tenth reported coverage (10.8%).
During 2020, there were no vaccines available for COVID-19 in South Africa, therefore adherence to non-pharmaceutical interventions and a series of stringent national lockdowns were the only methods available for mitigating and containing its spread. (See chapter on Emergencies and COVID-19 for more detailed discussion.) Numerous innovative data systems and reporting tools were developed to track the pandemic, and manage the country’s response. It is important however to note that the official COVID-19 case numbers are considered an under-estimation of the true number of infections32, as the national testing strategy evolved over time and prioritised certain age and disease risk groups when the country experienced a resurgence. By implication, the number of COVID-19-related deaths also reflect an under-estimate, as demonstrated by the high excess death rates. Furthermore, many infected individuals are asymptomatic or do not access testing services.
The association between TB and socio-economic conditions is well-known, with poor social and environmental conditions known to promote high infection rates. As highlighted in this chapter, TB remains a primary cause of death in South Africa and high TB prevalence rates continue to be a major cause for concern. This is discussed in detail in the Chapter on National Health Programmes.
The prevalence peaks in those aged 35–44 years and in those aged 65 years and older and is lowest among those aged 15–24 years (Figure 2.9). The First South African National TB Prevalence Survey34 conducted in 2018 estimated the prevalence of bacteriologically confirmed pulmonary TB in South Africa at 852 (95% CI 679-1.026) per 100 000 population among individuals 15 years and older. Using this survey estimate, the prevalence of TB for all forms of TB and ages in South Africa was calculated adjusting for individuals younger than 15 years (29%), a rate ratio of child to adult TB (0.6) and the proportion of notified cases that are extra-pulmonary TB (9.7%). The estimated prevalence of TB (all ages, all forms) in South Africa in 2018 was 737 (95% CI 580-890) per 100 000 population. Provincial disaggregation of the data reveals that the highest incidences of TB were recorded in KZN (492.8), NC (592.5) and the WC (617.9) per 100 000 population.


Prior to the introduction of antiretrovirals, HIV had a devastating impact on the health and well-being of South Africa’s population. South Africa nevertheless still ranks highest in the world in terms of incident and prevalent HIV cases. The highest prevalence is among young women between 25 and 49 years.34 The HIV prevalence among females is more than double compared to males in the 25–29 age group, compared to much smaller differences in the older population. This is also reflected in the HIV incidence rates. The number of new infections is almost three times higher among females aged 15 to 24 years compared to males in the same age group.34

HIV prevalence by age and sex, South Africa, 2017

The country has been lauded for its successes in rolling out the largest Antiretroviral Therapy (ART) programme in the world, with more than 5 million people living with HIV and AIDS in care, an action that has had a significant positive impact on mortality rates over the past decade. Important to note is that the proportion of AIDS-related deaths has declined by almost half between 2002 and 2020, from 30.6% to just over 15%. Almost 85% of people living with HIV aged 15–64 years knew their HIV status at the time of the survey (first 90).35 Among those who knew their HIV status, 70.6% were on ART (second 90); among this group on ART, 87.5% had laboratory-confirmed suppressed viral load (third 90). More females than males knew their HIV status (88.9% vs 78%), were on ART (72.2% vs 67.4%) and had better viral load suppression (89.9% vs 82.1%). The successes and shortcomings of the HIV programme are discussed in detail in the chapter on National Health Programmes.
Self-reported NCDs saw a decrease in proportion of previous diagnoses of asthma, cancer and stroke, and an increase in hypertension, arthritis and diabetes in females.36 This is covered in more detail in the chapter on Non-Communicable Diseases, and a summary of recent trends is shown below.
Demographic and health trends: 2015-2020
Year
Condition Gender 2015 2020 Change
Asthma Male 502 431 -71 Female 697 595 -102 Total 1199 1027 -172 Diabetes Male 615 588 -27 Female 961 1044 83 Total 1576 1632 56
Cancer Male 103 69 -34 Female 116 91 -25 Total 218 160 -58
HIV/AIDS Male 530 639 109 Female 922 1038 116 Total 1453 1677 224 Hypertension Male 1464 1619 155 Female 2978 3117 139 Total 4441 4737 296 Arthritis Male 245 252 7 Female 905 967 62 Total 1150 1218 68 Stroke Male 118 95 -23 Female 119 117 -2 Total 237 212 -25
Sources Statistics South Africa. GHS 2015. Pretoria, Statistics South Africa 2016 Statistics South Africa. GHS 2015. Pretoria, Statistics South Africa 2020
Figure 2.13 Persons suffering from chronic health conditions: South Africa 2015 and 2019, by sex [in 1 000s]
The prevalence of disabilityi in the population five years and older increased by 1.5 percentage points between 2015 and 2019, from 5.1% to 6.6%.37 In 2016, overall, 20% of the population aged five and older was reported to have some level of difficulty in at least one functional domain. The most common disability was having difficulty seeing (12%), which increased with age. This was followed by having difficulty walking or climbing steps (7%), and difficulty remembering or concentrating (6%). Six percent of the population aged five and older was reported to have a lot of difficulty or that they cannot do one of the functional domains at all, with the highest prevalence in those 60 years and older (23%).38
i In the General Household Survey, disability was assessed using the Washington Group questionnaire. Persons are classified as ‘disabled’ if they self-reported difficulties in two or more of the abilities assessed by the tool or were unable to perform any one activity.

South Africa is among the countries with the highest rates of intimate partner violence experienced by women in the world. However, under-reporting remains a challenge and criticism in terms of the government’s response remains.39
One in four (26%) ever-partnered women aged 18 or older have experienced physical, sexual or emotional violence committed by a partner in their lifetime. The most common form of violence experienced by women is physical violence (21%); 17% of women have experienced emotional violence, and 6% have experienced sexual violence.38 In terms of controlling behaviours, 19% of ever-partnered women report that their current or most recent partner has displayed three or more controlling behaviours.38 With regard to injuries due to partner violence, 37% of ever-partnered women who have experienced physical or sexual violence by their current or most recent partner have had injuries as a result.38
Overall, many of the demographic trends relevant to the health of South Africans have seen positive trends over the last five years, albeit from a high baseline of morbidity and mortality with marked variation across provinces. South Africa still sees a large amount of internal migration with movement from rural to urban provinces and a continuing positive influx of migrants from outside the country, mostly going to Gauteng and WC provinces. Births remain the main driver of growth however, although the overall total fertility rate is now declining.
In line with these overall trends, the health of most South Africans continues to improve, with positive trends in many of the key measures of health, including life expectancy. However, many of these positive trends will have been affected, some severely, by the impact of COVID-19. Whilst it is too early to accurately show all the relevant statistics, early indications, of life expectancy for example, show a significant impact. The substantial lag in the release of causes of death statistics hampers the public health utility of vital registration data. In addition to the immediate impact on health indices, the longer-term impact on health through worsening determinants of health, such as education, are also likely to be severe.
With regard to child health, a South African 2019 review thereof concluded that there is a pressing need to focus beyond childhood mortality to ensure that each child can thrive, focusing on in utero and early-life exposures, environmental conditions (air pollution, contaminated water and sub-optimal sanitation) and access to better-quality diets.40 This would complement efforts to improve immunisation coverage, feeding practices, systems for monitoring child health outcomes, and formalising and supporting the role of community-based health workers.
In terms of causes of death, TB still remains the highest, followed by diabetes mellitus, cardiovascular and heart disease, with HIV now ranked fifth overall following improvements in mortality from the increasing roll-out of life-long treatment. Many of the risk factors behind the rising levels of NCD are not showing signs of improvement, with increasing levels of smoking in men, and only minor declines in women. Data on alcohol intakes is less recent but has showed overall increases since 2010 in younger groups. The levels of disability are increasing as more data becomes available.
It was beyond the scope of this chapter to provide a formal and comprehensive analysis of health inequities in South Africa and it remains important to highlight some of the challenges and potential solutions to ensuring that health inequalities and inequities can be better monitored. Compared to data routinely collected from health facilities, nationally representative surveys usually allow for a finer disaggregation of health indicators across geographic and socio-demographic strata and a more comprehensive evaluation of the population health status, as they include sectors of the population who do not access the health system. On the other hand, with a few exceptions (such as the annual General Household Survey and the National Income Dynamics Study), survey data collections are only carried out with long periodicities, therefore lacking the ability to track rapid changes in the indicators of interest. Moreover, in many cases, health data in surveys are self-reported rather than based on clinical biomarkers, and therefore prone to high levels of bias, in most cases leading to an under-estimation of the real burden of ill-health and disability.
Other approaches are currently gaining traction and offer interesting possibilities to overcome, at least partially, the limitations of the current data sources in use. These include: (1) the use of modelling techniques (such as small area estimation41) to increase the spatial resolution of indicators of interest based on their relationship with other variables available at a local level; (2) the use of multidimensional indices of deprivation (such as, in South Africa, the Index of Multiple Deprivation42 and the COVID-19 Vulnerability Index43) that combine multiple variables to create measures that are robust to missing data44; and (3) the use of patient-level data from Electronic Health Record Systems that track patients who visit different health care providers. A system of this type is only partially available in South Africa, but its completion is planned as an essential step in the establishment of the National Health Insurance.45, 46
In conclusion, whilst South Africa is rich in terms of demographic and health data when compared to many other countries in Africa, there remains a lack of regular surveillance of key indicators, with continued reliance on expensive and sometimes infrequent surveys.
Demographic and health trends: 2015-2020
1. WHO (1948). Constitution. World Health Organization, Geneva. https:// www.who.int/about/governance/constitution
2. World Population Review. Available at: https://worldpopulationreview.com/ country-rankings/gini-coefficient-by-country. (Accessed: 01/08/2021)
3. Hundenborn J, Leibbrandt M, Woolard I. Drivers of inequality in South Africa. WIDER Working Paper 2018/162. 2018. UNI-WIDER 2018. https://doi.org/10.35188/UNU-WIDER/2018/604-3
4. Omotoso KO, Koch SF. Assessing changes in social determinants of health inequalities in South Africa: a decomposition analysis. International Journal for Equity in Health. 2018;17(181):1–13.
5. Maboshe M, Woolard I. (2018). Revisiting the Impact of Direct Taxes and Transfers on Poverty and Inequality in South Africa. UNU-WIDER Working Paper 79/2018. Helsinki: UNU-WIDER.
6. Ontario Public Health Association. Position statement on applying a health equity lens. Ontario Public Health Association. 2014. Available at: https:// cdn.ymaws.com/www.alphaweb.org/resource/collection/822EC60D0D03-413E-B590-AFE1AA8620A9/alPHa-OPHA_Position_Health_ Equity.pdf.[ Accessed: 14/07/2021]
7. Whitehead M, Dahlgren G. Concepts and principles for tackling social inequities in health: Levelling up Part 1. World Health Organization: Studies on social and economic determinants of population health. 2006;2:460–474. Available at: https://apps.who.int/iris/bitstream/ handle/10665/107790/E89383.pdf. (Accessed: 14/07/2021)
8. Obuaku-Igwe CC. Health inequality in South Africa: a systematic review. African Sociological Review/Revue Africaine de Sociologie. 2015;19(2): 96–131.
9. Ataguba JE, Akazili J, McIntyre D. Socioeconomic-related health inequality in South Africa: evidence from General Household Surveys. International Journal for Equity in Health. 2011;10(1):1–0.
10. Benatar S. The challenges of health disparities in South Africa. South African Medical Journal. 2013;103(3):154–155.
11. von Fintel D, Richter L. Intergenerational transfer of health inequalities: exploration of mechanisms in the Birth to Twenty cohort in South Africa. BMJ global health. 2019;4(5):e001828.
12. Nwosu CO, Oyenubi A. Income-related health inequalities associated with the coronavirus pandemic in South Africa: A decomposition analysis. International Journal for Equity in Health. 2021;20(1):1–2.
13. Ataguba JE, Day C, McIntyre D. Explaining the role of the social determinants of health on health inequality in South Africa. Glob Health Action. 2015;8:28865.
14. Zere E, McIntyre D. Inequities in under-five child malnutrition in South Africa. International Journal for Equity in Health. 2003;2(1):1–10.
15. Nkonki LL, Chopra M, Doherty TM, Jackson D, Robberstad B. Explaining household socio-economic related child health inequalities using multiple methods in three diverse settings in South Africa. International Journal for Equity in Health. 2011 Dec;10(1):1–4.
16. Day, C, Gray, A, Cois, A et al. Is South Africa closing the health gaps between districts? Monitoring progress towards universal health service coverage with routine facility data. BMC Health Serv Res 21, 194 (2021). https://doi.org/10.1186/s12913-021-06171-3
17. Gaede B, Eagar D. Progress toward equity. In: Massyn N, Day C, Peer N, Padarath A, Barron P, English R, et al., editors. District Health Barometer 2013/2014. Durban: Health Systems Trust; 2014. p. 316–38.
18. Statistics South Africa. Mid-year population estimates 2020. Statistical Release P0302. Statistics South Africa. 2020. Available at: http://www.statssa.gov. za/publications/P0302/P03022020.pdf. (Accessed: 14/07/2021)
19. https://www.worldometers.info/world-population/south-africapopulation/
20. Statistics South Africa. Mortality and causes of death in South Africa: Findings from death notification: 2018. Statistical Release P0309.3. Pretoria: Statistics South Africa; 2021.
21. Bradshaw D, Dorrington RE, Laubscher R, Moultrie TA, Groenewald P. Tracking mortality in near to real time provides essential information about the impact of the COVID-19 pandemic in South Africa in 2020. SAMJ. 2021
22. Statistics South Africa. Mid-year population estimates 2021. Statistical Release P0302. Statistics South Africa. 2021. Available at: http://www.statssa.gov. za/publications/P0302/P03022021.pdf. (Accessed: 15/08/2021)
23. Dorrington RE, Bradshaw D, Laubscher R, Nannan, N. Rapid mortality surveillance report 2018. Cape Town: South African Medical Research Council; 2018. ISBN: 978-1-928340-30-0
24. Statistics South Africa. Mortality and causes of death in South Africa, 2018: Findings from death notification. Statistical Release P0309.3. Pretoria: Statistics South Africa; 2017. Available at: https://www.statssa.gov.za/ publications/P03093/P030932017.pdf (Accessed: 02/08/2021)
25. Subramaniam T, Loganathan N, Yerushalmi E, Devadason ES, Majid M. Determinants of infant mortality in older ASEAN economies. Soc Indic Res [Internet]. 2016 December 17 (http://link.springer.com/10.1007/s11205016-1526-8 (Accessed 30 July 2017)
26. Hodge A, Firth S, Marthias T, Jimenez-Soto, E. Location matters: trends in inequalities in child mortality in Indonesia. Evidence from Repeated CrossSectional Surveys. Pan C-W, editor. PLOS ONE. 2014 July 25;9(7):e103597.
27. Dorrington RE, Bradshaw D, Laubscher R, Nannan N. Rapid mortality surveillance report 2019 & 2020. Cape Town: South African Medical Research Council; 2021. ISBN: 978-1-928340-58-4.
28. Malukeke R. Mid-year population estimates 2020. Presentation. Pretoria, July 2020. Available at: http://www.statssa.gov.za/publications/P0302/ MYPE%202020%20Presentation.pdf. (Accessed: 14/07/2021)
29. Statistics South Africa. General Household Survey 2019. Pretoria: Statistics South Africa. 2020. Available at: https://apps.who.int/iris/ bitstream/handle/10665/107790/E89383.pdf. (Accessed: 14/07/2021)
Demographic and health trends: 2015-2020
30. Moodley J, Fawcus S, Pattingson R. 21 years of confidential enquiries into maternal deaths in South Africa: reflections on maternal death assessments. Obstetrics and Gynaecology Forum. 2020;30(4). Published Online: 1 Dec 2020. https://hdl.handle.net/10520/ejc-medog-v30-n4-a2
31. WHO. Global Health Observatory. Indicator Metadata Registry List. https://www.who.int/data/gho/indicator-metadata-registry/ imr-details/4622
32. Mutevedzi PC, Kawonga M, Kwatra G, Moultrie A, Baillie V, Mabena N, et al. Estimated SARS-CoV-2 infection rate and fatality risk in Gauteng Province, South Africa: a population-based seroepidemiological survey. Int J Epidemiol [Internet]. 2021 Oct 30 [cited 2022 Apr 13]; Available from: https:// academic.oup.com/ije/advance-article/doi/10.1093/ije/dyab217/6414575
33. Pillay Y, Mvusi L, Mametja LD, Dlamini S. What did we learn from South Africa’s first-ever tuberculosis prevalence survey? SAMJ: South African Medical Journal. 2021;111(4):0.
34. Simbayi LC, Zuma K, Zungu N, Moyo S, Marinda E, Jooste S, Mabaso M, Ramlagan S, North A, van Zyl J, Mohlabane N, Dietrich C, Naidoo I and the SABSSM V Team. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2017. Cape Town: HSRC Press; 2019. Available at: http://repository.hsrc.ac.za/bitstream/ handle/20.500.11910/15052/11091.pdf?sequence=1(Accessed: 15/07/2021)
35. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2017 (last available)
36. Statistics South Africa. General Household Survey 2015. Pretoria: Statistics South Africa. 2016. Available at: https://www.statssa.gov.za/ publications/P0318/P03182015.pdf. (Accessed: 14/07/2021)
37. Kathard H, Padarath A, Galvaan R, Lorenzo T, editors. South African Health Review 2020. Durban: Health Systems Trust; 2020.
38. National Department of Health, Statistics South Africa, South African Medical Research Council, ICF. South Africa Demographic and Health Survey 2016: Final Report. Pretoria: National Department of Health; 2019. Available at: https://dhsprogram.com/publications/publication-fr337-dhs-final-reports. cfm. (Accessed: 14/07/2021)
39. Mthembu, J., Mabaso, M., Reis, S. et al. Prevalence and factors associated with intimate partner violence among the adolescent girls and young women in South Africa: findings the 2017 population based cross-sectional survey. BMC Public Health 21, 1160 (2021). https://doi.org/10.1186/s12889-02111183-z
40. Bamford L, Martin P, Slemming W, Richter L. Improving the early development of children through quality health care. In: Moeti T, Padarath A, editors. South African Health Review 2019. Durban: Health Systems Trust; 2019. URL: http://www.hst.org.za/publications/Pages/SAHR2019
41. Wakefield J, Okonek T, Pedersen J. Small Area Estimation of Health Outcomes [Preprint]. Available at: https://arxiv.org/pdf/2006.10266.pdf. (Accessed 26/08/2021)
42. Noble M, Zembe W, Wright G, Avenel D. Multiple Deprivation and Income Poverty at Small Area Level in South Africa in 2011. Cape Town: SASPI. 2013.
43. Statistics South Africa. Mapping vulnerability to COVID-19 [Internet]. Available at: http://www.statssa.gov.za/?p=13875#:~:text=The%20 South%20African%20Covid%2D19,against%20a%20set%20criteria%20being. (Accessed: 26/08/2021)
44. Peralta, A, Espinel-Flores, V, Gotsens, M, Pérez, G, Benach, J, Marí-Dell’Olmo, M. Developing a deprivation index to study geographical health inequalities in Ecuador. Revista De Saúde Pública. 2019;53, 97. https://doi. org/10.11606/s1518-8787.2019053001410
45. Katurura MC, Cilliers L. Electronic health record system in the public health care sector of South Africa: A systematic literature review. Afr J Prim Health Care Fam Med. 2018;10(1):e1–e8.
46. Naidoo S. The South African national health insurance: A revolution in health-care delivery! J Public Health. 2012;34(1):149–50.
Much of the premature mortality in South Africa is preventable. Given South Africa’s burden of disease, relatively mediocre health outcomes, and persistent health inequalities, addressing social determinants of health (SDH) becomes crucial to understand and address this context. We develop a hybrid framework that describes how human capital, safety, security, built environment, technology, and environmental and economic factors have influenced health outcomes in South Africa over the past five years.
Between 2015 and 2020, the South African economy struggled to achieve meaningful growth, and the economy further suffered a considerable contraction due to the COVID-19 pandemic. Despite these challenges, the government was unwavering in prioritising expenditure and investment in health care. However, the negative macroeconomic outlook and fragile state of the fiscus limits the resources available to address the challenges that hinder progress on socio-economic factors that determine health outcomes.
South Africa suffers from high inequality in health care and health outcomes, which largely stem from social protection, employment, education, housing, and infrastructure disparities. Although strides have been made post-1994 with increasing access to these basic entitlements, they are still lacking and considered poor quality. The United Nations Human Development Index for 2015 –2019 indicates that South Africa was stagnant along the dimensions of longevity, education and income.
Lungiswa Nkonki, Theodosia Adom, Carmen Sue Christian, Kholekile MalindiThe government provides a range of social protection programmes to cushion the vulnerable, including social grants. In 2019, almost 30% of South Africans benefited from social assistance. Furthermore, during the COVID-19 pandemic, the government increased the existing Child Support Grant. In addition, a new grant, the Special COVID-19 Social Relief of Distress (SRD), was introduced and targeted the unemployed and those not on any form of social assistance.
In 2018, South Africa implemented a sugar and beverage tax to prevent and control obesity and non-communicable diseases (NCDs). While the impact of this health promotion levy is not yet known, available evidence from observational studies suggests that the implementation has impacted product reformation, consumer choices and purchases.
Safety and security issues such as crime and substance abuse, specifically alcohol, have played an increasing role in health outcomes in South Africa, particularly mortality and morbidity linked to traumatic injuries. During the pandemic, restricted sale of alcohol resulted in a statistically significant decrease in unnatural deaths, regardless of the length of curfews. Periods where no or limited restrictions on alcohol were in place had no significant effect or resulted in significantly increased unnatural deaths. A positive impact of social cohesion on optimal health in this context is demonstrated in the recent COVID-19 vaccine roll-out in Limpopo. Despite being one of the poorest provinces in South Africa, Limpopo had the third-highest provincial vaccination rate in the country.
COVID-19 has also demonstrated the importance of technology as a determinant of health, especially literacy and internet access. Applications for employment, housing, and other assistance programmes are increasingly accessible online. As of 2020, 99.8% of the population in South Africa had access to the 3G mobile network, and almost nine in ten South African households exclusively used cellular phones in 2018.
The World Health Organization (WHO) defines SDH as: ‘the circumstances in which people are born, grow up, live, work and age, and the systems put in place to deal with illness’ (Commission on Social Determinants of Health, 2007). The recognition of the critical role of the SDH dates back to the 1940s (Kark & Cassel, 2002), and has been articulated in several ways, including the Alma-Ata Declaration (World Health Organization, 1978), WHO Commission on Health (Commission on Social Determinants of Health, 2007), United Nations Millennium Declaration in 2000, and the expanded set of 17 new Sustainable Development Goals (SDGs). These advances recognise the role of global and national political economies in creating and perpetuating health inequities – the ‘unfair and avoidable difference in health status seen within and between countries’. Some have pointed out contradictions within the SDGs and cautioned that they might not only be inadequate but could potentially be dangerous. Of concern is the failure to acknowledge that mass impoverishment is the product of extreme accumulation and overconsumption by a few, which entails processes of enclosure, extraction and exploitation along the way (Hickel, 2015).
Nationally, SDH is a cornerstone in the National Department of Health’s Primary Health Care Re-engineering Strategy and the National Development Plan (NDP). The NDP aims to eliminate poverty and reduce inequality by 2030 (National Planning Commission, 2011). The NDP is broadly aligned with the SDGs and sees national development as a process requiring a combination of increasing employment, higher incomes through productivity growth, a social wage and good-quality public services (National Planning Commission, 2011). Like the SDGs, the NDP has been criticised for its neoliberal agenda. The success of the NDP is premised on the intention to triple the size of the economy by 2030. Some have cautioned that economic growth based primarily on the extraction and export of raw materials such as minerals and agricultural products will drive unemployment, limit the social agenda and undermine decent work, including health (Scott Vera et al., 2017).
The many dimensions of poverty and vulnerability that cut across the 17 SDGs persist in South Africa despite direct government intervention to address this, including a progressive tax system, free essential and social services (electricity, water and sanitation, basic health and education), and a well-established social assistance system. At the same time, South Africa faces a quadruple disease burden, with major HIV and tuberculosis (TB) epidemics, maternal and child mortality levels higher than the global average, a growing prevalence of NCDs, and high levels of violence and injuries. Most recently, the COVID-19 pandemic has added to this burden.
Improvements in health outcomes have been observed over the past decade, and these include the availability of antiretroviral treatments that have had a dramatic impact on adult mortality and consequently increased life expectancy (Dorrington et al., 2019). Under-5 mortality rates have declined from 41 to 32 per 1 000 live births between 2012 and 2017, and infant mortality rates dropped from 27 to 23 per 1 000 live births (Goga et al., 2019). However, there remains room for improvement in this regard. Much of the premature mortality in South Africa is preventable. Given South Africa’s burden of disease, relatively mediocre health outcomes, and persistent health inequalities, addressing SDH becomes crucial to understand and address in this context.
Having reviewed multiple theoretical frameworks used to review progress on the SDH (Bradshaw, 2008; Dahlgren & Whitehead, 1991; Krieger, 2008; Scott Vera et al., 2017), our conceptual framework starts with economic growth as measured by Gross Domestic Product (GDP) (see Figure 3.1). We begin with reviewing year-on-year GDP and expenditure on health. Notwithstanding the challenges of capitalist growth as measured by GDP, we start here because both international (SDGs) and national (NDP) commitments are premised on increasing the size of the economy by 2030. Thus, looking at the public purse first is an excellent place to start, as it provides a ceiling on how much can be dedicated to improving health and well-being.
We have then clustered poverty, income inequality, education, unemployment and social security together because of their impact on human capital. Human capital has undeniable intrinsic value and consists of the knowledge, skills and health that people accumulate over their lives, and enables people to realise their potential as productive members of society. More human capital is associated with higher earnings for people, higher income for countries, and stronger community cohesion. It is a central driver of sustainable growth and poverty reduction.
We have categorised built environment factors that influence health as housing, water, sanitation, and public transportation. In addition to these environmental determinants of health, we have added accessibility of healthy foods as a social determinant of health. Nutrition-sensitive concerns to address food security and nutrition include poverty, water and sanitation, and climate change.
Social cohesion involves building shared values and communities of interpretation, reducing disparities in wealth and income, and generally enabling people to have a sense that they are engaged in a common enterprise, facing shared challenges, and that they are members of the same communi ty. In this section, we focus on safety and security as markers of inadequate social cohesion.

The advent of COVID-19 presented numerous learning opportunities for including health in all policies. Actions developed in response to COVID-19, which adopted the SDH lens, demonstrate how different sectors worked together to produce positive health outcomes and how spheres of government worked together – connecting action across both levels and sectors. We then discuss technology and internet availability as an SDH. Technology and internet availability were not traditionally seen as SDHs; however, COVID-19 has demonstrated the importance of digital literacy and internet connectivity.
This chapter reviews South Africa’s progress, challenges and opportunities with SDH in the period from 2015–2020. We conclude with a summary of key findings and discuss recommendations for the country. It is crucial that public spending is pro-poor. In our assessment of progress in the five years under review, we pay attention to markers of vulnerability in terms of gender, rural, low-income earners and/or unemployed, very young and old, and race.
Expanding access to quality health care for all is one of the goals set by the NDP’s Vision 2030. This goal closely aligns with the SDG goal of ‘ensuring healthy lives and promoting well-being for all at all ages’ (United Nations Children’s Fund, 2020, p. 6). This close policy alignment with the SDG further cements the government’s commitment to improving health outcomes for all South Africans. Noticeable improvements in health outcomes have been achieved since the transition into democracy; these include an improved life expectancy, and declines in mortality for infants, children and women. These gains are mediocre given South Africa’s expenditure in health care. However, the gains come from a low base (due to the legacy of inequitable provision of health care services under the apartheid government) and have likely been eroded by the COVID-19 pandemic. Chapter 13, which covers the quality of care, provides more detail on the important early gains made while highlighting several actions that appear to have stalled, largely due to COVID-19.
This section reviews the social, economic and environmental determinants of health. Empirical evidence has shown that health outcomes are strongly related to socio-economic and environmental factors. Omotoso and Koch (2018) and Ataguba et al. (2016), for example, provide evidence that suggests inequalities in health outcomes are strongly associated with disparities in educational attainment, employment, social protection, housing and infrastructure, area of residence and rate of urbanisation. Consequently, tracking progress in these determinants will indicate whether strides have been made towards achieving better health outcomes for all.
Another critical determinant of health outcomes is how much expenditure and investment is devoted to the health of the population. This, in turn, is dependent on the nature and extent of economic development that a country is able to achieve. Therefore, our review of progress with addressing socio-economic and environmental challenges will be preceded by a review of economic growth over the reference period as measured by annual growth in GDP and expenditure on health care.
The South African government has set an ambitious path for the growth of the economy under the NDP. The performance of the economy in the 2015–2020 reference period has been underwhelming and out of touch with the path envisioned by the NDP. Figure 3.2 shows that the economy has struggled to achieve meaningful growth and has at times endured short spells of negative growth in consecutive quarters during the reference period. With the emergence of the COVID-19 global health pandemic, the economy suffered a deep recession in 2020 that resulted in the South African economy shrinking by almost 7% compared to the previous year.

Figure 3.2 Real Gross Domestic Product 2015–2020, annual percentage change
Source: World Bank – World Development Indicators (2020)
The macroeconomic outlook during the reference period was further worsened by the sharp rise in government debt. The net loan debt as a percentage of GDP increased from 44% in 2015/16 to just over 58% in 2019/20, while the cost of servicing the debt increased from 3.1% to 4%. With the government committed to addressing the health and economic crises caused by the COVID-19 pandemic, government debt along with the debt-servicing costs are projected to increase even further, causing further strain to the fiscus (National Treasury, 2021).
The nature and extent of economic growth that a country is able to achieve sets a limit on how much expenditure and investment can be devoted to the health of the population. Despite the economy not achieving sustained growth and government debt on the rise, the government appears to be unwavering in prioritising expenditure and investment in health care. Figure 3.3 below shows a steadily rising trajectory for health care expenditure.
With regard to how the budget allocation is utilised by the health department, the lion’s share of the budget is allocated to the provincial health departments. The provision of health care services in South Africa is a mandate of provinces. Since each province is tasked with the provision of health care and has some measure of autonomy in executing the task, variation in health care outcomes and quality of service between provinces is likely to appear and may, in turn, contribute to the inequality of health care outcomes in the country.

South Africa suffers from high levels of inequality in health care and health outcomes. These inequalities reflect and largely stem from inequalities in income, labour market outcomes and access to service delivery. Ataguba et al. (2016) provide empirical evidence that identifies social protection, employment, education, housing and infrastructure as key contributors to health inequality. Some of these factors speak to the very core of human development and are captured by the Human Development Index (HDI)2
1 The expenditure values referred to in the figure are based on audited values as opposed to estimates or adjusted values.
2 Measure of human develop ment compiled by the United Nations Development Programme and published under the Human Development Report.
South Africa from 2015 to 2019. The HDI provides an assessment of South Africa’s progress on three variables (‘longevity, education, and income’) and calculates a composite score which is given as the HDI value. While South Africa’s HDI value of 0.709 for 2019 places it in the high human development category, the HDI value showed an improvement of only one percentage point between 2015 and 2019. This indicates that human development along the dimensions of longevity, education and income was stagnant. Moreover, South Africa’s HDI value was lower than the average HDI value among the group of countries in the high human category group (United Nations Development Programme, 2020).
Table 3.1 South Africa’s HDI trends (based on consistent time series data and new goalposts)
Life expectancy at birth Expected years of schooling Mean years of schooling HDI value
2015 62.6 13.8 10.1 0.701
2016 63.2 13.7 10.2 0.703
2017 63.5 13.7 10.2 0.705
2018 63.9 13.7 10.2 0.707
2019 64.1 13.8 10.2 0.709
Source: United Nations Development Programme (2020)
South Africa is categorised by the World Bank as an upper-middle-income country based on its level of gross national income per capita. However, the income in the hands of South Africans is highly unequal and affords the nation the classification of one of the most unequal countries in the world. When the HDI value reported in Table 3.1 is adjusted for inequality within the three dimensions captured by the index, the HDI value falls to 0.468, representing a ‘loss in human development due to inequality’ of 34% (United Nations Development Programme, 2020, p. 4). The corresponding figure for high HDI countries that South Africa is grouped alongside (based on the unadjusted HDI value) is 17.9% (United Nations Development Programme, 2020), which illustrates South Africa’s inequality.
A recent report by Statistics South Africa (2019a) on inequality trends finds that, based on money measures, inequality has only slightly improved over the past few years. The improvement was primarily confined to the middle of the income distribution. When accounting for the sources of income inequality, the report finds that the unequal distribution of income earned from the labour market is the chief contributor, with social grants playing a significant mitigating role in the inequality gap between the poor and the rich.
To cushion the most vulnerable in the nation against social and economic hardships, the government provides a range of social protection programmes (e.g., social grants and no-fee schools). Of these programmes, social grants are arguably the most important based on the number of people reached and the resources invested. According to data from Statistics South Africa, roughly 30% of South Africans in 2019 benefited from social grants (Statistics South Africa, 2020). This figure was around 12% in 2003. Furthermore, roughly 20% of households in the country report that social grants are the primary source of income in their household (Statistics South Africa, 2020). The receipt of these grants has been linked with improvements in many outcomes at the household and individual levels, including better health outcomes (see for example Oosthuizen (2021)). Thus, these social protection programmes have an element of redistribution.
One of the Achilles’ heels of the current government is the high incidence of poverty. South Africa’s level of poverty has historically stood in sharp contrast to the country’s level of income, which places it under the category of upper-middle-income country. The most recent data on poverty trends reported by Statistics South Africa indicates that over half (55.5%) of the population were living below the upper-bound poverty line of R992 per capita per month in 2015 (Statistics South Africa, 2018b). According to the internationally comparable income poverty line of US$1.90 per day3, almost one in five (18.9%) people in the South African population in 2016 lived below this income poverty line (United Nations Development Programme, 2020). To move beyond the narrow focus on income or the lack thereof, the recent trend in the measurement of poverty augments the traditional income-based poverty statistics by adding multiple dimensions of deprivations that capture the quality of health, education and standard of living of people. Based on this measurement, roughly 6% of the South African population are multidimensionally poor (United Nations Development Programme, 2020). The lower incidence of non-income-based poverty versus income-based poverty reflects the positive impact played by social security programmes administered by the government.
Education is an important determinant for long-term economic development. There is increasing evidence, however, that places the emphasis on quality of education as the key policy lever in the promotion of economic development (Van der Berg et al., 2020). An analysis of key education statistics reveals that significant progress towards meeting the goals of the NDP has been achieved (Van der Berg et al., 2020). Data on high school completion, for example, indicate that educational outcomes in South Africa are at the levels that would be expected given the country’s level of income. Furthermore, data from Statistics South Africa indicates that by 2019, the Basic Education Department had been able to achieve nearly universal school attendance (96.6%) for children between the ages of 7 and 15 years old (Statistics South Africa, 2020).
While noticeable gains have been achieved in expanding access to education, ensuring quality of schooling for all still remains a key challenge. According to Van der Berg et al. (2020), the quality of schooling in South Africa is at a level below what would be expected given the country’s level of income. Lack of progress in ensuring quality schooling for all learners undermines education’s role in promoting economic development in the long term. Additionally, low quality of education can have a detrimental impact on labour market outcomes, and this may in turn lead to inferior health outcomes.
Many South Africans are without work, and this is reflected by the alarmingly high unemployment rates. According to data collected by Statistics South Africa (2015), roughly 8 million people were without work in the first quarter of 2015. Over 2 million of these unemployed individuals had given up searching for employment and were considered to be ‘discouraged work-seekers’ by Statistics South Africa. By the end of the last quarter of 2020, the number of people without work was over 10 million and those classified as ‘discouraged work-seekers’ had increased to roughly 3 million (Statistics South Africa, 2021). This represents an increase of roughly six percentage points in the official unemployment rate under the review period.
During the same period, the absorption rate (i.e., number of employed people as a fraction of the total population) fell from 43.2% in the first quarter of 2015 to 38.2% in the last quarter of 2020. This means that less than four people out of ten were employed in the last quarter of 2020 in South Africa.
The unemployment statistics quoted above were without a doubt adversely affected by the COVID-19 health pandemic that sparked a deep economic recession in 2020. However, it is also true that these unemployment statistics were at alarming levels before 2020 and had been in a negative trajectory due to an economy that had been stagnant.
With less than four people out of ten employed, this places severe strain on the resources that the government has available to address the socio-economic challenges faced by the country. This, in turn, brings into question the role of these socio-economic factors in promoting health outcomes.
This section focuses on the accessibility of healthy foods as a social determinant of health while providing insights into the food environment, food security, nutrition, and initiatives on obesity and child hunger in South Africa.
South Africa is food secure at the national level, however, there is some degree of food insecurity at the household level across the provinces, racial groups, and settlements. While in 2015, more than one in four South Africans were living at the level of food poverty, estimates by Statistics South Africa suggest that in 2017, close to 7 million South Africans and 1.7 million households experienced hunger, and a little over 10 million had inadequate access to food (Statistics South Africa, 2019b). These levels of food insecurity and hunger were reflected in the 2019 estimates (National Department of Health et al., 2019) by the South Africa Demographic and Health Survey, where more than a quarter of children under five years were stunted and 13% were overweight, while in adults aged 15 years and older, two-thirds of women and onethird of men were overweight or obese, almost half had high blood pressure, and at least 8% were diabetic.
The current South African food environment is characterised by large transnational and national food and beverage ‘Big Food’ companies that offer large varieties of healthy and unhealthy foods. In contrast, fast-food chains offer unhealthy foods (Claasen et al., 2016). One of the targets of the SDGs Goal 2 is to reduce malnutrition in all its forms, namely: undernutrition, micronutrient deficiencies, overweight or obesity, and diet-related NCDs, and this is only achievable in a supportive food environment where safe, nutritious and diverse foods are widely available and accessible in adequate quantities to contribute to the dietary requirements of the population for health and active life (Lartey et al., 2016).
Given that the NDP recognises food and nutrition security as a key element of poverty and inequality, various departments have intersectoral initiatives to promote and support food security. A number of these reforms predate the review period. For the 2015–2020 period, we focus on the Health Promotion Levy (HPL), the Child Support Grant (CSG), and the Special COVID-19 SRD grant. The HPL was introduced in 2018 to prevent and control obesity. While the impact on obesity is not yet known, available evidence from observational studies suggests that the introduction of the HPL has impacted product reformation, consumer choices and purchases (Stacey et al., 2019, 2021). A previous study in 2016 (Zembe-Mkabile et al., 2016) indicated that the existing CSG was inadequate in improving child health outcomes, particularly stunting. To mitigate the impacts of the COVID-19 pandemic on child hunger, the government increased the CSG to R300 per child in May 2020 and R500 per caregiver from June to October 2020. In addition, a new grant, the SRD, was introduced to target the unemployed as well as those who were not on any form of social support grant, and one in every three households is dependent on the grant.
The built environment plays a major role in the prevention and management of both chronic and infectious diseases. The impact of the built environment on health can be both direct – for example, by influencing the quality of an individual’s physical environment, or indirect by influencing behaviours that impact disease transmission and health (Pinter-Wollman et al., 2018). In this section, we will focus on the role that housing, water, sanitation and public transportation have played in determining health outcomes in South Africa during the period under review. (Chapter 2 takes a cursory look at waste removal, land degradation and social erosion in relation to health outcomes.)
Although strides have been made post-1994 with increasing access to these basic entitlements, they are still lacking and considered to be of poor quality, as evidenced by the increasing number of protests linked to these public goods and services (Alexander, 2010; Mamokhere, 2019; Morudu, 2017; Wasserman et al., 2018).
In the South African context of urbanisation coupled with a chronic backlog of social housing (Turok & Scheba, 2019), overcrowding remains associated with poor health outcomes, particularly acute respiratory infections and gas trointestinal diseases. Survey data from a recent 11-year panel study in Johannesburg, South Africa analysed the relationship between household crowding and respiratory and gastrointestinal symptoms in two low-income communities (Nkosi et al., 2019). The study found that close to 60% of households were overcrowded by international standards4, although this level was lower compared to other African countries. Furthermore, overcrowding was associated with an increase in acute respiratory and gastrointestinal symptoms, as well as fever/chills, even when controlling for confounding variables.
The impact of inadequate water and sanitation on child health is particularly depressing in the South African context. In 2013, after the public outcry over student deaths in pit latrines at underprivileged schools, and upward pressure from civil society organisations, the Department of Basic Education (DBE) gazetted the Minimum Uniform Norms and Standards for Public School Infrastructure (Christie, 2021). However, by 2018, 19% of 23 471 (i.e. 4 460) public schools still had illegal pit latrines and 37 schools had no sanitation facilities at all (Christie, 2021). Even after a recent show of political will from government to improve the situation (brought on by the COVID-19 pandemic – described in more detail in the paragraph below), a 2021 report on water and sanitation at schools showed a lack of significant progress, with 3 297 schools still relying on pit latrines and 366 schools having no water for sanitation (South African Human Rights Commission, 2021).
The COVID-19 pandemic appeared to reignite the DBE’s commitment to their infrastructure norms and standards for public schools, which resulted in a set of non-negotiables for the reopening of schools being declared on April 29 2020, that included access to water and sanitation (pit latrines to be replaced with mobile facilities) (Parliamentary Monitoring Group, 2020). At the same time that water and sanitation featured on the list of non-negotiables for schools to reopen, the DBE also noted that 3 475 schools would require emergency water support to reopen (Christie, 2021). It took a pandemic to highlight the need for
4 The study used the UN-Habitat definition as the benchmark, i.e., when there are more than two people per room (excluding bathrooms but including kitchens and living rooms).
basic water and sanitation at schools, which they were meant to have since 2013 when the minimum norms and standards for public schools were promulgated. At the time of writing this chapter, we could not confirm whether these schools had reopened or not, and whether issues of water and sanitation had been addressed there.
The availability (or not) of transport plays an integral role in people’s ability to access essential goods and services such as health care services (Martens et al., 2012). This does not bode well for South Africa where the public transport system –which the majority of the poor and marginalised depend on – has become increas ingly unreliable and costly (Maharaj, 2020). Even when transport is available, the cost thereof (direct and opportunity costs) has an impact on healthseeking behaviour (delayed care-seeking) which ultimately influences health outcomes. A 2020 study looking at access to health care in post-apartheid South Africa found that in 2009/2010, 73% of the affordability constraints to access was due to travel costs (Burger & Christian, 2020). These findings also showed an anti-poor bias, which further entrenches health inequalities.
The health consequences associated with transport inefficienciesare wide-ranging: from ill-health to maternal mortality and high infant mortality rates; poor access to healthy, affordable food and essential medication; as well as transport-related traumatic injury (Litman,2002; Lucas & Jones, 2012; Pirie, 2008; Vasconcellos, 2011).
Safety and security have been identified as among the major determinants of health in the South African context (Scott Vera et al., 2017). This section will take a closer look at how substance abuse (specifically alcohol abuse) and social cohesion – both of which directly impact safety and security in communities –relate to health outcomes. What emerges from the recent literature is that the health of the most vulnerable in society continues to be negatively affected disproportionately by these determinants (or a lack thereof, in the case of social cohesion).
A silver lining of the COVID-19 pandemic is that it has offered us many unique learnings that otherwise would not have been possible. One such learning is the clear evidence of the harmful effects of alcohol abuse – directly and indirectly – on health outcomes. In a COVID-19 context, conditions favoured a natural experiment that showed how COVID-19 restrictions, in particular the sale of alcohol and curfews, had a major effect on the pattern of unnatural deaths in South Africa. A recent study in South Africa analysed death data over 68 weeks (January 2020 to April 2021) in relation to information on restrictions on the sale of alcohol, as well as the curfew hours (Moultrie et al., 2021). The findings were stark: During periods of complete restriction on the sale of alcohol, there was a statistically significant reduction in unnatural deaths, irrespective of the length of curfew. In fact, during times when no or limited restrictions on alcohol were in place, it had no significant effect or resulted in significantly increased unnatural deaths.
While restricting the sale of alcohol is not a long-term solution and is accompanied by negative economic impacts for related industries, it is clear that alcohol-related harm needs to be addressed in South Africa. When considering the question of the trade-offs of stricter alcohol regulation in South Africa, a 2014 study estimated that the combined total tangible and intangible costs of alcohol harm to the South African economy were 10–12% of the 2009 GDP. Further analysis showed that the tangible financial cost of alcohol abuse alone was estimated at R37.9 billion, or 1.6% of the 2009
GDP (Matzopoulos et al., 2014). The study was successful in showing that the costs of alcohol-related harms were a heavy counterbalance to the economic benefits highlighted by the alcohol industry to avoid stricter regulation.
Diminishing these costs of alcohol abuse through policy interventions would, directly and indirectly, contribute to social well-being, as demonstrated by the study of the impact of COVID-19 alcohol sale prohibitions and curfews on the pattern of unnatural deaths in South Africa. At the same time, policy interventions also need to dig deeper to understand the systemic reasons behind alcohol abuse in the South African context. These studies also underscore the need for implementing evidence-based alcohol control measures. For further reading on trends in alcohol use, please refer to Chapter 2.
Evidence of the lack of social cohesion in South Africa, which may manifest as crime and violence, and how it negatively impacts health behaviours and outcomes, is well documented (Gass et al., 2010; Lamb, 2019; Lippman et al., 2018; Miller et al., 2020; Olamijuwon et al., 2018; Seedat et al., 2009; Shannon et al., 2020). In contrast, this subsection delves into a case that demonstrates how social cohesion supports optimal health. At the time of writing, Limpopo had the third-highest provincial vaccination rate (48%) (National Department of Health, 2021b) in the country despite being one of the poorest provinces in South Africa (Gateway South Africa, 2021). Social cohesion was clearly demonstrated during the recent vaccine roll-out in Limpopo. Their roll-out plan was co-designed with local churches and community leaders because communities in Limpopo trust local leaders and faith-based organisations (Burger et al., 2021). This form of social cohesion was leveraged to advance health outcomes, namely the vaccination rate, and serves as a great example of how health outcomes may be positively influenced in this context of safety and security
South Africa reported its first case of COVID-19 on March 5 2020. Within 14 days (March 5 – 19), we saw a decisive, strong leadership from the president and the significant, essential and necessary coordination between different ministries, including Education, Justice, Health, Trade and Industry, Transport, Public Works and Infrastructure, Finance, Cooperative Governance and Traditional Affairs, and International Relations and Cooperation. Within these 14 days, South Africa rapidly produced and implemented several action items (Table 3.2). This intersectoral action and coordination is something that South Africa has needed for a long time to address SDH in the country (Nkonki & Fonn, 2020). It remains to be seen whether the intersectoral coordination created as a response to COVID-19 will be fully utilised in the long term.
The literature on intersectoral collaboration suggests that success relies on a shared understanding of what can be achieved collectively and whether stakeholders can agree on mutual goals or acceptable trade-offs. COVID-19 has highlighted key policy dilemmas and trade-offs. For instance, in the case of alcohol bans, there is clear evidence that it decreased natural deaths and trauma-related hospitalisation. At the same time however, alcohol bans had a negative economic impact on the food and beverage and hospitality industry and reduced tax revenues (sin tax, company tax and VAT).
Coordinated and intersectoral actions developed in response to COVID-19
Table 3.2 List of the key actions in South Africa within the first 14 days (March 5–19) of COVID-19
President Declaration of a State of Disaster in terms of section 27 of the Disaster Management Act, 2002
Health Establishment of a national hotline and WhatsApp number for the general population
Home Affairs and International Relations and Cooperation
Travel ban on foreign nationals from high-risk countries such as Italy, Iran, South Korea, Spain, Germany, the United States, the United Kingdom and China as from March 18 2020
Health Dedicated website with daily updates from the National Institute for Communicable Diseases, tests conducted, positive and negative results, information on symptoms and prevention (in local languages), list of amended regulations
Defence and Military Veterans ‘Release of resources’ by the Department of Defence, national organs of state, and institutions within national, provincial and local government
Police ‘Prevention and prohibition of gatherings.’ In this case, a gathering of 100 people was prohibited. The assembly of more than 50 persons at premises where liquor is sold and consumed was also prohibited. The Regulation also makes provision for powers of an enforcement officer to disperse a gathering, or in some cases to arrest and detain the organiser of a gathering
Trade and Industry COVID-19 Block Exemption for the Health Care Sector
Health, and Justice and Correctional Services
Public Works and Infrastructure
Trade and Industry
Basic Education and Higher Education, Science and Technology
‘Refusal of medical examination, prophylaxis, treatment, isolation and quarantine.’ This regulation makes provision for the unlikely scenario where a person refuses to (self) quarantine or (self) isolate. The person may then be placed in isolation or quarantine for a period of 48 hours, as the case may be, pending a warrant being issued by a magistrate, on application by an enforcement officer, to perform the medical examination of a suspected or confirmed case
COVID-19 Block Exemption for the Health Care Sector
‘Places of quarantine and isolation’ by the Minister of Public Works and Infrastructure, the Members of the Executive Council in the provinces and the accounting officers of municipalities
‘Closure of schools and partial care facilities’ from March 18 2020 until April 15 2020, which period may be extended for the duration of the National State of Disaster by the cabinet member responsible
Suspension of visits for 30 days to Correctional Centres, Remand Detention Facilities, Holding Cells, Military Detention Facilities and Department of Social Development facilities, including Child and Youth Care Centres, shelters, One-Stop Centres, and Treatment Centres, which period may be extended for any period, but not beyond the duration of the National State of Disaster by the cabinet member responsible Health, Police, Justice and Correctional Services
Justice and Correctional Services
‘Limitation on the sale, dispensing or transportation of liquor.’ In this case, all on-consumption premises selling liquor, including taverns, restaurants and clubs, must be closed with immediate effect, or must accommodate no more than 50 persons at any time: Provided that adequate space is available and that all directions in respect of hygienic conditions and limitation of exposure to persons with COVID-19 are adhered to. It is also notable that no special or events liquor licenses will be considered for approval during the duration of the National State of Disaster. Establishments will also close earlier between 18:00 and 09:00 the next morning on weekdays and Saturdays; and from 13:00 on Sundays and public holidays
Finance/ Treasury ‘Emergency Procurement Procedures’ in line with financial management legislation, regulations and instructions
President ‘Authority to issue directions.’ In this regard the president authorised the Ministers of Health, Justice and Correctional Services, Basic and Higher Education, Police, Social Development, Trade and Industry, and Transport to issue directions where needed to address, prevent and combat the spread of COVID-19 in matters falling within their respective mandates
Justice and Correctional Services
‘Offences and penalties’ for a person when found liable on conviction, to a fine or imprisonment for a period not exceeding six months, or both such fine and imprisonment
Source https://www.gov.za/Coronavirus
Intersectoral action was first proposed by the Alma-Ata Declaration (World Health Organization, 1978) and involves efforts by the health sector to collaborate with other public policy sectors to improve health outcomes, and there is consensus that it is needed to achieve health in all policies and improve health outcomes. However, translation of evidence into effective policy is a particular challenge for intersectoral policies addressing the SDH.
The literature on intersectoral collaboration suggests that success relies on a shared understanding of what can be achieved collectively and whether stakeholders can agree on mutual goals or acceptable trade-offs. The range of obstacles to effective implementation of SDH policies includes: the multifaceted nature of socio-economic factors (Exworthy, 2008), the dominance of biomedical perspective (Phillips et al., 2016), logistics surrounding intersectoral action for health, lack of ownership or territorial ownership (Skeen et al., 2010), lack of accountability (de Leeuw, 2017), limited resources and time to enable collaboration (Crichton, 2008), poor enforcement of legislative processes that demand intersectoral working, and limited dedicated resources towards integrated policy development (de Leeuw, 2017).
Studies looking at whether SDH have been applied to address population health in South Africa have had a programmatic focus. For instance, they have looked at whether and how the intersectoral approach was applied or not applied in addressing mental health (Skeen et al., 2010), child health (Okeyo et al., 2020, 2021), HIV/AIDS (Mahlangu et al., 2018), tobacco control (Sanni et al., 2018), and gender equity (Hargreaves et al., 2011).
Skeen et al. (Skeen et al., 2010) recommend that the National Department of Health (NDoH) should be a critical partner in developing the intersectoral action to achieve population health. We concur with Skeen et al., and propose that the NDoH should take a stewardship role in promoting intersectoral action in addressing social determinants of health. This recommendation is logically sound. However, several factors mitigate against this, namely, current provincial responsibilities (as outlined in the Constitution and National Health Act), equitable share allocations as well as the silo nature of budgets and accountability. Furthermore, Skeen et al. (Skeen
et al., 2010) recommended the following essential steps for achieving intersectoral collaboration, commencing with a high level of political commitment. They targeted awareness-raising to engage various sectors, using current networks between departments as a springboard and creating a communication culture between departments. They also noted that programmes should be backed by legislation and policies. Formal collaborations exist between government departments and agencies at the national, provincial and district levels. However, these collaborations were found to be more efficient at the national level compared to the provincial and local levels. In the context of this study, stakeholders recognised adequate access to essential services such as housing, education, employment, water, sanitation and transport as critical in health promotion. Aside from the lead department, other government sectors included legislations in departmental policies and plans. They recommend the active engagement of local government structures to provide insights on community-level/local issues and responses.
Mahlangu et al. (Mahlangu et al., 2018) propose mainstreaming approaches to addressing health, as it ensures sector commitments to achieve joint outcomes for national targets. At the same time, it avoids overlap and duplication of activities and functions of government and calls for vertical coordination between levels of government (national, provincial and local) within departments and horizontal coordination between departments.
Mahlangu et al. (Mahlangu et al., 2018) identified consultative engagements between different spheres of government and relevant stakeholders and communication and information sharing as factors that facilitate vertical coordination. Baum et al. (Baum et al., 2017) recommend supportive bureaucratic policy networks that include senior and mid-level staff across the sectors as means to bring about action on the SDHs. In addressing the question of how to establish supportive cross-sector spaces of engagement, cross-sector structures that promote dialogue and the negotiation of different views, e.g. interdisciplinary committees, working groups or policy networks are recommended. Consultative engagements with sub-national government stakeholders are important given that the implementation occurs at the provincial and local levels. Ideally, consultative arrangements should help clarify roles and responsibilities and support the implementation of the SDH approach to improving health outcomes. The flow of information across the different spheres with timely and established interdepartmental lines should ensure relevant, timely information to key players. Working in silos between various directorates in departments and non-synchronised reporting systems at the national level hinder vertical coordination.
There is limited evidence of horizontal collaboration and partnership between departments in practice. This is attributed to the lack of clarity of roles and responsibilities, resulting in the overlap. While platforms exist to facilitate collaboration between government departments, the lack of participation at the national and provincial levels and lack of representation of government departments across districts and local levels limit its effectiveness. Moreover, the complexities of measuring impact where contributions of departments may not be acknowledged in collaborative efforts hinder the process.
Examples of coordinated responses to COVID-19 that applied a social determinants of health lens
The COVID-19 pandemic created a context that necessitated innovation. One area of innovation that leapfrogged during this period is telemedicine, supported by the temporary relaxation of telemedicine guidelines by the Health Professions Council of South Africa (HPCSA) (Percept Actuaries and Consultants, 2020). These conditions have sparked a renewed interest in and demand for telemedicine in South Africa. While it must be stressed that telemedicine is a complimentary service in the package of care – and not a substitute – there needs to be a broader appreciation that much scope remains for the full benefits of telemedicine, i.e. increasing access to quality health care for more South Africans, to be realised. Examples of telemedicine innovations in the South African market include clinicians exchanging patient medical information via messaging apps (e.g. Signapps), telephonic/video patient consultations with health care workers (e.g. Stone Three), remote monitoring of patients (e.g. Quro), and surgeons consulting remotely on surgical procedures (eHealth Group) (Percept Actuaries and Consultants, 2020, 2021).
Another innovation during COVID-19 was alternative models for the delivery of medication in the public sector. One example of this is the home delivery of medication service that the Metropolitan Health Services in the Western Cape offered its patients during the pandemic. The innovation aimed to prevent COVID-19 amongst high-risk patients (those with comorbidities) who would be at risk of more severe disease and to decongest primary health care facilities in anticipation of the expected surge in COVID-19 cases. The innovation linked the existing chronic dispensing unit system with a community-oriented primary care approach in the Metro (Brey et al., 2020). Medication was delivered to pharmacies at local facilities as usual, but from there, a range of means was used to distribute the medication parcels to local non-profit organisations, who delivered the parcels to patients using community health workers (CHWs). Delivery models included the use of e-hailers (such as Uber), bicycles and electric scooters. The innovation lent itself to being scaled up, with 200 000 medication parcels delivered per month using 2 500 CHWs (Brey et al., 2020).
Provincial departments of health (PDoHs) across South Africa were also forced to be creative with the vaccine roll-out programmes by leveraging social capital in communities. As described in the section on Safety and Security, Limpopo’s approach of co-designing their vaccine roll-out programme with trusted local leaders resulted in a high vaccine rate relative to other provinces.
These innovations and new approaches experimented with during COVID-19 demonstrated their potential to bypass or mitigate negative SDHs such as a lack of social cohesion, costly and unreliable transport systems and the high opportunity cost of standing in long queues to access care at facilities. These lessons must be learnt and not forgotten, as well as further explored to see how best they can be leveraged to strengthen the health system.
Digital technology was not traditionally seen as an SDH. However, COVID-19 has demonstrated the importance of digital literacy and internet connectivity as capital that positively impacts health outcomes. Recently, digital literacies and internet connectivity have been called the ‘super social determinants of health’ because they address all other SDHs. For instance, applications for employment, housing, and other assistance programmes, each of which influences an individual’s health, are increasingly accessible online. In addition, digital tools and applications can support a range of health information needs such as patient portals, health trackers, remote monitoring devices, and health information communication (Sieck et al., 2021). Research suggests that tools such as health apps and patient portals can foster greater patient engagement, better support patients outside of the clinic visit, and improve health outcomes. Fundamental to the use of mobile technology in health care are internet-enabled devices, affordable broadband internet, access to digital literacy training, quality technical support, and applications and online content designed to enable and encourage self-sufficiency, participation and collaboration. Whilst technology can contribute enormously to well-being, in the absence of universal access to the necessary enabling infrastructure, it also has the potential to marginalise the poor and exacerbate inequalities.
As of 2020, 99.8% of the population in South Africa had access to the 3G mobile network. 4G/LTE coverage increased significantly from 53% in 2015 to 96.4% in 2020. This trend was accompanied by rapidly growing smartphone penetration that more than doubled to 91.2% over the four years from 2016 to 2019. In 2020, only 0.7% of the South African population had 5G coverage (See Figure 3.4).
Source:

In 2013, the South African government introduced the SA Connect programme to improve universal internet access. This programme prioritises access to free public WI-FI to the population and targets schools, clinics and other government facilities through universal, affordable and high-speed broadband access to all. Several metropolitan areas have WI-FI, while most suburban areas have fibre-optic cables. Data from the 2018 General Household Survey suggests that almost nine in ten (89.5%) South African households exclusively use cellular phones. However, only 10.4% of the population have access to the internet at home (Statistics South Africa, 2018a). Between 2019 and 2020, the number of South Africans who have access to the internet increased by over 3% (1.1 million).
We highlight two successful initiatives of digital technology (ehealth innovations) in health care in South Africa – MomConnect and the Stock Visibility System. In August 2014, the South African NDoH launched Mom Connect as a flagship initiative to strengthen maternal and infant health services and improve mortality outcomes. It is universally accessible through all mobile phones and aims to register all pregnant women, provide them with vital health information and create channels for their feedback. MomConnect has been scaled rapidly through strong government stewardship and leverage of existing technology, content and partnerships (Barron et al., 2018). In early 2019, Mom Connect had registered over 2.5 million mothers and now represents a powerful platform for real-time data collection and linkage to additional services to improve patient care. Chapter 13 provides more descriptive information on MomConnect and how it has impacted the quality of care in South Africa. At the onset of COVID-19, the Coronavirus Rapid Mobile Survey team used the Mom Connect platform to collect information from pregnant women, mothers and child pairs on access to maternal and child health services during the hard lockdown, when face-to-face interviewing was not permitted.
The Stock Visibility System (SVS) (Chapter 4 provides details on SVS) serves as an electronic stock management system on the availability of medicines at health facilities. It has been available in more than 3 000 primary health care clinics and over 300 hospitals since its inception in 2015 (National Department of Health, 2021a). In the context of COVID-19, the SVS has been widely used to monitor personal protective equipment availability in public sector hospitals and, where applicable, COVID-19 vaccine storage in health facilities. Refer to Chapter 4 on primary health care ehealth programmes for a detailed description of the SVS.
While the interventions appear to have significantly impacted the technology landscape, critical issues remain and addressing these can ensure success and consolidate the gains made. The prohibitive costs of maintaining internet connectivity, and in some cases the cost of internet-enabled devices, unequal coverage, interoperability, poor network performance – limiting internet usage and access to data, especially in resource-constrained settings, low levels of education and digital literacy, lack of social support and awareness of the applications, language, and age are significant drawbacks to the extensive application of digital technology in South Africa (Matli & Ngoepe, 2020; Petersen et al., 2020; Phokeer et al., 2016).
We have shown throughout the chapter that there is extended existing support for the SDH approach to improving health outcomes. However, translating evidence into effective policy challenges intersectoral policies addressing the SDH Formal collaborations exist between government departments and agencies at the national, provincial and district levels, however, these collaborations were found to be more efficient at the national level. The NDoH should lead the formulation and implementation of intersectoral action with a high level of active and measurable engagement of all stakeholders.
Given that collaborations between provincial- and district-level departments are less efficient, the NDoH must develop guidelines for provinces and districts on creating consultative engagements for sub-national government stakeholders, drawing on structures and processes that were developed to deal with COVID-19 and documented best practices and innovations by the PDoHs before COVID-19 and in response to COVID-19.
To improve horizontal collaboration and partnership between departments in practice, we recommend that PDoHs be the champions of consultative engagements at provincial and local levels, given that policy implementation occurs at the provincial and local levels. Ideally, consultative arrangements should help clarify roles and responsibilities and support the implementation of the SDH approach to improving health outcomes. The flow of information across the different spheres with timely and established interdepartmental lines should ensure relevant and timely information to key players.
In addressing the social determinants of health, there is a need to engage multiple stakeholders – the public sector (government), private sector and civil society, which represent the three critical stakeholders – at all stages. The interactions among the stakeholders should go beyond information sharing to cooperation, coordination or integration, which are likely to strengthen policy implementation. There is limited evidence on:
1. What the costs are (financial and human) of ensuring health in all policies;
2. How to measure and document the impact of collaborative efforts of departments to achieve social determinants of health; and
3. How policy trade-offs and goals are negotiated, and the outcomes of those negotiations communicated.
Alexander P. Rebellion of the poor: South Africa’s service delivery protests – a preliminary analysis. Review of African Political Economy. 2010;37(123): 25–40. https://doi.org/10.1080/03056241003637870
Ataguba JE-O, Day C, McIntyre D. Explaining the role of the social determinants of health on health inequality in South Africa. Global Health Action. 2016;8(1). https://doi.org/10.3402/gha.v8.28865
Barron P, Peter J, LeFevre AE, Sebidi J, Bekker M, Allen R, Parsons AN, Benjamin P, Pillay Y. Mobile health messaging service and helpdesk for South African mothers (MomConnect): History, successes and challenges. BMJ Global Health. 2018;3(Suppl 2): e000559. https://doi.org/10.1136/ bmjgh-2017-000559
Baum F, Delany-Crowe T, MacDougall C, Lawless A, van Eyk H, Williams C. Ideas, actors and institutions: Lessons from South Australian Health in All Policies on what encourages other sectors’ involvement. BMC Public Health. 2017;17(1): 811. https://doi.org/10.1186/s12889-017-4821-7
Bradshaw D. Determinants of health and their trends: Primary Health Care: In context. South African Health Review. 2008;(1): 51–69. https://doi. org/10.10520/EJC35512
Brey Z, Mash R, Goliath C, Roman D. Home delivery of medication during Coronavirus disease 2019, Cape Town, South Africa. African Journal of Primary Health Care and Family Medicine. 2020;12(1): 1–4. https://doi. org/10.4102/phcfm.v12i1.2449
Burger R, Christian C. Access to health care in post-apartheid South Africa: Availability, affordability, acceptability. Health Economics, Policy and Law. 2020;15(1): 43–55. https://doi.org/10.1017/S1744133118000300
Burger R, Maughan-Brown B, Köhler T, English R, Tameris M. A shot in the arm for South Africa—Increased openness to accepting a COVID-1789 vaccine: Evidence from NIDS- CRAM Waves 4 and 5. National Income Dynamics Study – Coronavirus Rapid Mobile Survey. 2021;31.
Christie P. The Pandemic as a Portal for Change: Pushing against the Limits of ‘Normal Schooling’ in South Africa. Education as Change. 2021;25(1): 1–21. https://doi.org/10.25159/1947-9417/8718
Claasen N, Pointer R, van der Hoeven M, Covic N. Food environments, health and nutrition in South Africa: Mapping the research and policy terrain. 2016. https://media.africaportal.org/documents/WP34_Claasen_etal_final_0.pdf
Commission on Social Determinants of Health. Achieving health equity: From root causes to fair outcomes. (Commission on Social Determinants of Health). World Health Organization. 2007.
Crichton J. Changing fortunes: Analysis of fluctuating policy space for family planning in Kenya. Health Policy and Planning. 2008;23(5): 339–350. https://doi.org/10.1093/heapol/czn020
Dahlgren G, Whitehead M. Policies and strategies to promote social equity in health. Institute for Future Studies. 1991.
de Leeuw E. Engagement of Sectors Other than Health in Integrated Health Governance, Policy, and Action. Annual Review of Public Health. 2017;38(1): 329–349. https://doi.org/10.1146/annurev-publhealth-031816-044309
Dorrington R. et al. Rapid Mortality Surveillance Report 2017. Cape Town, South Africa: South African Medical Research Council. 2019. Available at: https:// www.samrc.ac.za/sites/default/files/files/2019-02-06/RapidMortality SurveillanceReport2017.pdf.
Exworthy M. Policy to tackle the social determinants of health: Using conceptual models to understand the policy process. Health Policy and Planning 2008;23(5): 318–327.
Gass JD, Stein DJ, Williams DR, Seedat S. Intimate partner violence, health behaviours, and chronic physical illness among South African women. South African Medical Journal. 2010;100(9): 582–585.
Gateway South Africa. Mapping poverty in South Africa. South Africa Gateway. (2021, June 11). https://southafrica-info.com/people/mapping-povertyin-south-africa/
Goga AE et al. Neonatal, infant and child health in South Africa: reflecting on the past towards a better future. 2019. doi:10.7196/SAMJ.2019.v109i11b.14301.
Hargreaves J, Hatcher A, Busza J, Strange V, Phetla G, Kim J, Watts C, Morison L, Porter J, Pronyk P. What happens after a trial? Replicating a cross-sectoral intervention addressing the social determinants of health: the case of the Intervention with Microfinance for AIDS and Gender Equity (IMAGE) in South Africa. Social Determinants Approaches to Public Health: From Concept to Practice. 2011;147–159.
Hickel J. The Problem with Saving the World. 2015, August 8. Kark SL, Cassel J. The Pholela Health Centre: A Progress Report. American Journal of Public Health. 2002;92(11): 1743–1747.
Krieger N. Proximal, distal, and the politics of causation: What’s level got to do with it? American Journal of Public Health. 2008;98(2): 221–230. PubMed. https://doi.org/10.2105/AJPH.2007.111278
Lamb G. Social cohesion and violence in South Africa: Constructing a puzzle with missing pieces. Crime, Law and Social Change. 2019;72(4): 365–385. https://doi.org/10.1007/s10611-019-09828-7
Lartey A, Hemrich G, Amoroso L, Remans R, Grace D, Albert JL, Fischer CG, Garnett T. Influencing food environments for healthy diets (p. 154). Food and Agriculture Organization of the United Nations. 2016. https://cgspace.cgiar.org/bitstream/handle/10568/80578/InfluencingFood EnvironmentsForHealthyDiets.pdf?sequence=2
Lippman SA, Leslie HH, Neilands TB, Twine R, Grignon JS, MacPhail C, Morris J, Rebombo D, Sesane M, El Ayadi AM, Pettifor A, Kahn K. Context matters: Community social cohesion and health behaviors in two South African areas. Health & Place. 2018;50: 98–104. https://doi.org/10.1016/j. healthplace.2017.12.009
Litman T. Evaluating transportation equity. World Transport Policy and Practice. 2002;8(2): 50–65.
Lucas K, Jones P. Social impacts and equity issues in transport. Social Impacts and Equity Issues in Transport. 2012;21: 4–112.
Maharaj B. South African Urban Planning in the Twentieth and Twenty-First Centuries—Continuities between the Apartheid and Democratic eras? In R. R. Thakur, A. K. Dutt, S. K. Thakur, & G. M. Pomeroy (Eds.), Urban and Regional Planning and Development: 20th Century Forms and 21st Century Transformations (pp. 101–112). Springer International Publishing. 2020. https://doi.org/10.1007/978-3-030-31776-8_6
Mahlangu P, Vearey J, Goudge J. Multisectoral (in) action: Towards effective mainstreaming of HIV in public sector departments in South Africa. African Journal of AIDS Research. 2018;17(4): 301–312.
Mamokhere J. An exploration of reasons behind service delivery protests in South Africa: A case of Bolobedu South at the Greater Tzaneen Municipality. 2019. http://ulspace.ul.ac.za/handle/10386/2669
Martens K, Golub A, Robinson G. A justice-theoretic approach to the distribution of transportation benefits: Implications for transportation planning practice in the United States. Transportation Research Part A: Policy and Practice. 2012;46(4): 684–695. https://doi.org/10.1016/j.tra.2012.01.004
Matli W, Ngoepe M. Capitalizing on digital literacy skills for capacity development of people who are not in education, employment or training in South Africa. African Journal of Science, Technology, Innovation and Development. 2020;12(2): 129–139.
Matzopoulos RG, Truen S, Bowman B, Corrigall J. The cost of harmful alcohol use in South Africa. South African Medical Journal. 2014;104(2): 127–132.
Miller HN, Thornton CP, Rodney T, Thorpe RJ, Allen J. Social Cohesion in Health: A Concept Analysis. Advances in Nursing Science. 2020;43(4): 375–390. https://doi.org/10.1097/ANS.0000000000000327
Morudu HD. Service delivery protests in South African municipalities: An exploration using principal component regression and 2013 data. Cogent Social Sciences. 2017;3(1): 1329106. https://doi.org/10.1080/23311886 .2017.1329106
Moultrie TA, Dorrington RE, Laubscher R, Groenewald P, Parry CDH, Matzopoulos R, Bradshaw D. Unnatural deaths, alcohol bans and curfews: Evidence from a quasi-natural experiment during COVID-19. South African Medical Journal. 2021;111(9): 834–837. https://doi.org/10.7196/ SAMJ.2021.v111i9.15813
National Department of Health. Stock Visibility System Covid-19 Vaccine Instance Information Pack. 2021a. https://www.google.com/search?q=National+Department+of+Health+Stock+V isibility+System+2021&rlz=1C1GCEB_enZA949ZA953&oq=National+De partment+of+Health+Stock+Visibility+System+2021&aqs=chrome..69i57.1 496j0j9&sourceid=chrome&ie=UTF-8
National Department of Health. Latest Vaccine Statistics—South Africa Corona Virus Online Portal. South Africa Corona Virus Online Portal. 2021b, December 2. https://sacoronavirus.co.za/latest-vaccine-statistics/
National Department of Health, Statistics South Africa (Stats SA), South African Medical Research, South African Medical ResearchCouncil, & ICF. 2019. South Africa Demographic and Health Survey 2016. https://dhsprogram. com/pubs/pdf/FR337/FR337.pdf
National Planning Commission. (2011). National Development Plan: Vision for 2030. Government of South Africa.
National Treasury. Estimates of National Expenditure (2019-2021) (Budget Information). 2021. http://www.treasury.gov.za/documents/national%20 budget/default.aspx
Nkonki L, Fonn S. Decisive and strong leadership and intersectoral action from South Africa in response to the COVID-19 virus. South African Medical Journal. 2020;110(5). http://www.samj.org.za/index.php/samj/ article/view/12879/9153
Nkosi V, Haman T, Naicker N, Mathee A. Overcrowding and health in two impoverished suburbs of Johannesburg, South Africa. BMC Public Health. 2019;19(1): 1358. https://doi.org/10.1186/s12889-019-7665-5
Okeyo I, Lehmann U, Schneider H. The impact of differing frames on early stages of intersectoral collaboration: The case of the First 1000 Days Initiative in the Western Cape Province. Health Research Policy and Systems. 2020;18(1): 1–14.
Okeyo I, Lehmann U, Schneider H. Policy adoption and the implementation woes of the intersectoral First 1000 Days of childhood initiative, in the Western Cape province of South Africa. International Journal of Health Policy and Management. 2021;10(7): 364–375.
Olamijuwon EO, Odimegwu CO, De Wet N. Social cohesion and self-rated health among adults in South Africa: The moderating role of race. Health & Place. 2018;51: 89–96. https://doi.org/10.1016/j. healthplace.2018.02.010
Omotoso KO, Koch SF. Assessing changes in social determinants of health inequalities in South Africa: A decomposition analysis. International Journal for Equity in Health. 2018;17(181): 13. https://doi.org/10.1186/s12939018-0885-y
Oosthuizen M. South Africa: Social Assistance Programs and Systems Review (English) (No. 164802). World Bank. 2021.
https://documents1.worldbank.org/curated/en/238611633430611402/pdf/ South-Africa-Social-Assistance-Programs-and-Systems-Review.pdf
Parliamentary Monitoring Group. Schooling during COVID-19 Lockdown: Update with Deputy Minister. 2020. https://pmg.org.za/committee-meet ing/30116/
Percept Actuaries and Consultants. The nurse can see you now: Reflections from the South African telemedicine market in light of Covid-19. 2020. https:// percept. co.za/wp-content/uploads/2021/02/Percept-TelehealthReport-Revisions.pdf
Percept Actuaries and Consultants. Case Notes from the Frontier: Five case studies of South African telemedicine providers. 2021. https://percept.co.za/wpcontent/uploads/2021/03/Telemedicine-Providers-Case-Study-Report.pdf
Petersen F, Brown A, Pather S, Tucker WD. Challenges for the adoption of ICT for diabetes self-management in South Africa. The Electronic Journal of Information Systems in Developing Countries. 2020;86(5): e12113. https:// doi.org/10.1002/isd2.12113
Phillips C, Fisher M, Baum F, MacDougall C, Newman L, McDermott D. To what extent do Australian child and youth health policies address the social determinants of health and health equity? A document analysis study. BMC Public Health. 2016;16(1): 512. https://doi.org/10.1186/s12889-0163187-6
Phokeer A, Densmore M, Johnson D, Feamster N. A First Look at Mobile Internet Use in Township Communities in South Africa. Proceedings of the 7th Annual Symposium on Computing for Development, 1–10. 2016. https://doi.org/10.1145/3001913.3001926
Pinter-Wollman N, Jelic A, Wells NM. The impact of the built environment on health behaviours and disease transmission in social systems. Philosophical Transactions of the Royal Society B: Biological Sciences.
2018;373(1753): 20170245. https://doi.org/10.1098/rstb.2017.0245
Pirie GH. Virtuous mobility: Moralizing vs measuring geographical mobility in Africa. Afrika Focus. 2008;22(1): 21–35. https:// doi.org/10.1163/2031356X-02201004
Sanni S, Hongoro C, Ndinda C, Wisdom JP. Assessment of the multisectoral approach to tobacco control in South Africa and Togo. 2018.
Scott V, Schaay N, Schneider H, Sanders D. Addressing social determinants of health in South Africa: The journey continues. South African Health Review. 2017;2017(1): 77–87. https://doi.org/10.10520/EJC-c80ea0402
Seedat M, Van Niekerk A, Jewkes R, Suffla S, Ratele K. Violence and injuries in South Africa: Prioritizing an agenda for prevention. The Lancet. 2009;374(9694): 1011–1022. https://doi.org/10.1016/S01406736(09)60948-X
Shannon MM, Clougherty JE, McCarthy C, Elovitz MA, Nguemeni Tiako MJ, Melly SJ, Burris HH. Neighborhood Violent Crime and Perceived Stress in Pregnancy. International Journal of Environmental Research and Public Health. 2020;17(15): 5585. https://doi.org/10.3390/ijerph17155585
Sieck CJ, Sheon A, Ancker JS, Castek J, Callahan B, Siefer A. Digital inclusion as a social determinant of health. Npj Digital Medicine. 2021;4(1): 52. https:// doi.org/10.1038/s41746-021-00413-8
Skeen S, Kleintjes S, Lund C, Petersen I, Bhana A, Flisher AJ, Health TM, Consortium, PRP. ‘Mental health is everybody’s business’: Roles for an inter sectoral approach in South Africa. International Review of Psychiatry. 2010;22(6): 611–623.
South African Human Rights Commission. Report on water and sanitation in schools. 2021. https://www.sahrc.org.za/home/21/files/Water%20 And%20Sanitation%20Report%20-%2028%20SeptemberPM.pdf
Stacey N, Edoka I, Hofman K, Swart EC, Popkin B, Ng SW. Changes in beverage purchases following the announcement and implementation of South Africa’s Health Promotion Levy: An observational study. The Lancet Planetary Health. 2021;5(4): e200–e208. https://doi.org/10.1016/ S2542-5196(20)30304-1
Stacey N, Mudara C, Ng SW, van Walbeek C, Hofman K, Edoka I. Sugar-based beverage taxes and beverage prices: Evidence from South Africa’s Health Promotion Levy. Social Science & Medicine. 2019;238: 112465.
Statistics South Africa. Quarterly Labour Force Survey—Quarter 1 (No. P0211). 2015. https://www.statssa.gov.za/publications/P0211/P02111st Quarter2015.pdf
Statistics South Africa. General Household Survey 2018. 2018a. https://www. statssa.gov.za/publications/P0318/P03182018.pdf
Statistics South Africa. Men, Women and Children: Findings of the Living Conditions Survey 2014/15 (No. 03-10-02 (2014/15); p. 65). 2018b. http://www.statssa.gov.za/publications/Report-03-10-02%20/ Report-03-10-02%202015.pdf
Statistics South Africa. Inequality Trends in South Africa: A multidimensional diagnostic of inequality (No. 03-10–19; p. 232). 2019a. https:// www.statssa.gov.za/publications/Report-03-10-19/ Report-03-10-192017.pdf
Statistics South Africa. Towards measuring the extent of food security in South Africa: An examination of hunger and food inadequacy (No. 03-00–14). 2019b. http://www.statssa.gov.za/publications/03-00-14/ 03-00-142017.pdf
Statistics South Africa. General Household Survey 2019 (No. P0318). 2020. https://www.statssa.gov.za/publications/P0318/P03182019.pdf
Statistics South Africa. Quarterly Labour Force Survey—Quarter 4 (No. P0211). 2021. http://www.statssa.gov.za/publications/P0211/P02114th Quarter2020.pdf
Turok I, Scheba A. ‘Right to the city’ and the New Urban Agenda: Learning from the right to housing. Territory, Politics, Governance. 2019;7(4): 494–510. https://doi.org/10.1080/21622671.2018.1499549
United Nations Children’s Fund. Health Budget Brief South Africa—2020. United Nations. 2020. https://www.unicef.org/southafrica/media/4616/ file/ZAF-health-budget-brief-2020.pdf
United Nations Development Programme. The next frontier: Human development and the anthropocene. Briefing note for countries on the 2020 Human Development Report—South Africa (p. 7). 2020. https://hdr.undp. org/sites/default/files/Country-Profiles/ZAF.pdf
Van der Berg S, Gustafsson M, Malindi K. Education and skills for the economy and links to labour markets in South Africa. National Planning Commission. 2020. https://www.nationalplanningcommission.org.za/assets/ Documents/Education%20and%20skills%20for%20the%20economy%20 and%20links%20to%20labour%20markets%20in%20South%20Africa.pdf
Vasconcellos EA. Equity evaluation of urban transport. Urban Transport in the Developing World. 2011. https://www.elgaronline.com/view/ed coll/9781847202055/9781847202055.00022.xml
Wasserman H, Chuma W, Bosch T. Print media coverage of service delivery protests in South Africa: A content analysis. African Studies. 2018;77(1): 145–156. https://doi.org/10.1080/00020184.2018.1426312
World Bank. World Development Indicators. 2020. https://databank.worldbank. org/source/world-development-indicators/Type/TABLE/preview/on World Health Organization. United Nations Children’s Fund. Declaration of Alma-Ata. International Conference on Primary Health Care: Alma-Ata, USSR. 1978, September 6.
Zembe-Mkabile W, Ramokolo V, Sanders D, Jackson D, Doherty T. The dynamic relationship between cash transfers and child health: Can the child support grant in South Africa make a difference to child nutrition? Public Health Nutrition. 2016;19(2): 356–362. https://doi.org/10.1017/ S1368980015001147
Primary health care (PHC), as envisioned by the 1978 Alma-Ata Declaration, has been a key pillar of South Africa’s health system since the advent of democracy. After the political transition in 1994, a number of PHC-related health policy measures were prioritised, most notably removing user fees for women and children under six years of age, subsequently extended to all public PHC services. During its first two terms of office (1994–2004), the new government also implemented an extensive programme of public PHC facility upgrading. The PHC approach was also enshrined in key health policy statements and legislation, starting with the White Paper on the Transformation of the Health System in 1997 and the National Health Act of 2003, which established the district health system (DHS) as the decentralised building block of the health system.
These measures established a sound basis in policy for the PHC system in South Africa, offering a comprehensive package of basic services including maternal, child and reproductive health, HIV and tuberculosis (TB) testing and treatment, screening and care for non-communicable diseases (NCDs) and treatment of common ailments1 South Africa is an outlier amongst low- and middle-income countries (LMICs) in having low levels of out-of-pocket health expenditure2.
Despite these gains, the rapid emergence of a catastrophic HIV/AIDS epidemic in the mid-1990s impacted severely on health system development. For at least a decade, HIV became an all-consuming and singular focus in South Africa, displacing attention away from the earlier processes of health system reform. The first critical gap was in the human resource dimensions of PHC – the failure to realign health professional education towards PHC, weak management and leadership, and inconsistent policy on mid-level and community-based cadres3. The second gap was in the establishment of a coherent and standardised DHS as the governance
Helen Schneider, Mndebele Jabulani, Ramphelane Morewane, Gio Perezmechanism for PHC and district hospitals. Overall, in this period, the PHC system offered an important safety net but was still characterised by highly uneven quality of care, low public participation and accountability, and a focus on disease treatment rather than prevention.
In 2010, following a visit to the Brazilian health system, the Department of Health adopted the national ‘PHC Re-engineering Strategy’ which, amongst others, formalised a national community health worker (CHW) programme referred to as the Ward-Based Primary Health Care Outreach Team (WBPHCOT) strategy4. The PHC re-engineering strategy became an integral part of a further set of comprehensive reforms in the National Health Insurance (NHI) proposals, which once again placed PHC and the DHS at the centre of the health system. An NHI Green Paper was issued in 2011, followed by a White Paper in 2015 and finally an NHI Bill5 tabled in Parliament in 2019. In the period 2012–2017, 11 (of 52) health districts were designated as NHI pilots across the country, where interventions targeting PHC system strengthening were implemented through conditional grants6, and are currently being scaled up to other districts. Reflecting emerging global agendas on the Sustainable Development Goals (SDGs), the social determinants of health also received attention in this period, with regulations on salt in processed foods and a sugar tax introduced.
These interventions formed the main elements of national policy and programming in the period under review (2015–2020). While these national processes were being implemented, nodes of PHC system innovations were emerging in districts and provinces across the country. These sub-national, bottom-up initiatives are rich in system learning that can inform and complement top-down system development and are reported as case studies of promising practices in this chapter.
The advent of the COVID-19 pandemic in March 2020 had major implications for the PHC system, diverting staff and services away from routine prevention and care and reversing health gains7. The pandemic also precipitated a severe economic and fiscal crisis that will impact on future funding. At the same time, the COVID-19 responses have promoted system innovation and catalysed new relationships and intersectoral action on health and new forms of working (including use of technology), which could be leveraged in future.
The chapter examines the significant contextual factors impacting on PHC in the period, key programmes and interventions implemented and the elements they address. Evidence on PHC performance and sub-national case studies of promising practices are then presented. These include the sub-district model in KwaZulu-Natal (KZN), community-oriented primary care, the 3-feet model in Mpumalanga and Limpopo, and a community-led clinic monitoring programme, Ritshidze. The chapter concludes with a summative assessment of PHC in South Africa, based on the core strategic levers of the World Health Organization (WHO), and the way forward.
Developments in South Africa have occurred against a backdrop of renewed global impetus for PHC as part of Universal Health Coverage (UHC) and the SDGs, culminating in the Astana Conference and Declaration on PHC in 2018, com memorating the 40th anniversary of the landmark 1978 Alma-Ata Conference and Declaration. The Astana Declaration reaffirmed the founding values and principles of the Alma-Ata Declaration, asserting health as a human right and PHC as ‘the cornerstone of a sustainable health system for universal health coverage and health-related Sustainable Development Goals’8. The Declaration recognised a vastly changed context and the ongoing challenges confronting PHC systems9, including:
• new disease burdens – while maternal and child mortality has declined, NCDs, mental health, violence and emergence of new pandemics have increased;
• rapid developments in information technology;
• growing environmental pressures from climate change and urbanisation;
• increasingly pluralistic health systems; and
• deepening inequities – between and within countries.
In 2020, the WHO and the United Nations Children’s Fund (UNICEF) launched a follow-up ‘Operational Framework for Primary Health Care’ proposing three factors as the basis of health and well-being (Figure 4.1): (i) integrated primary care and essential public health functions resulting in improved access, utilisation and quality; (ii) empowered people and communities resulting in improved health literacy, participation and care seeking; and (iii) multisectoral policy and action resulting in improved determinants of health10.

Figure 4.1 Primary health care components (copied from: WHO/UNICEF, 2020)
These components are made possible by fourteen ‘core strategic and operational levers’ outlined in Table 4.1.
• Political commitment and leadership
• Governance and policy frameworks
• Funding and allocation of resources
• Engagement of community and other stakeholders
• Models of care
• Primary Health Care workforce
• Physical infrastructure
• Medicines and other health products
• Engagement with private sector providers
• Purchasing and payment systems
• Digital technologies
• Systems for improving quality of care
• PHC-oriented research
• Monitoring and evaluation
This chapter reviews progress and challenges of PHC in South Africa since 2015, taking the Astana Declaration and the PHC Operational Framework as its starting points, namely, that PHC:
• is the core pivot around which the rest of the health system turns;
• has a population orientation – starting with the smallest political unit, the ward;
• includes community-based services, PHC facilities and hospitals in coordinated systems of integrated delivery;
• provides essential public health functions;
• relates to the sub-district and district structures and processes, which provide the governance and support mechanisms, and which are coterminous with local government and other sectors;
• is mandated to interact with other sectors in a place-based approach; and
• is held accountable through community participation.
These are enabled through core strategic and operational system levers outlined in Table 4.1.
The assessment of progress and performance of PHC in the period draws on several sources. We conducted a non-exhaustive search of publications on PHC in South Africa since 2015, consulted websites and submissions to the NHI parliamentary hearings, and reviewed major strategies developed or evaluations conducted in the period. A key report in the period was the evaluation of PHC system strengthening in the NHI pilot sites6. The chapter also draws on a case study of South Africa’s PHC system conducted for WHO’s Alliance for Health Policy and Systems Research in 20161, which formed part of a subsequent multi-country comparative analysis2 .
Developments related to NHI have been the most significant macro-level factor impacting on PHC. The 2015 White Paper considered PHC as the ‘heartbeat of NHI’, and proposed Contracting Units for Primary Health Care (CUPS) and District Management Offices as the basic building blocks of the new health system11. With the NHI Bill still currently under consideration by Parliament, these system reforms remain paper proposals but will have major implications if eventually implemented. The 11 NHI pilot districts referred to earlier were established while these policy and legislative processes were unfolding. Importantly, the NHI pilot sites ‘did not involve developing new funding arrangements for health care in South Africa, but rather piloted various health system strengthening interventions focused at the primary health care (PHC) level’6
The second key development was the announcement of a universal HIV ‘test and treat’ policy in 2016, with expanded budget allocations, and the deployment of donor-funded (principally the United States President’s Emergency Plan For AIDS Relief (PEPFAR) and the United States Agency for International Development (USAID)) partners to support districts. Several of the health system strengthening interventions implemented in the pilot districts were enabled through these partnerships, aimed at mainstreaming the HIV programme while benefiting the PHC system more generally.
After a 15-year period of expanding budgets and per capita expenditure on public sector PHC, the introduction of austerity measures from 2019/20 onwards reversed this pattern of growth. Declining budgetary allocations pose a significant threat to the future development of PHC, especially in the stabilisation of components such as the WBPHCOT, and in ensuring greater equity. Community health workers emerged as key players in the public health response to COVID-19, yet remain poorly managed and remunerated1
A key development in the period was the widely consulted 2030 Human Resources for Health (HRH) Strategy and associated 2020/21–2024/5 HRH Strategic Plan12. This Strategy makes extensive recommendations on all aspects of HRH development in South Africa, emphasising the critical importance of this core system function for the future development of an NHI. The report specifically assesses current availability and distribution of, and models future HRH needs for HRH public PHC, identifying significant shortfalls and inequities.
In 2017, a South African Lancet National Commission on quality of care was launched following the Lancet Global Health Commission on High-Quality Health Systems in the Sustainable Development Goals (SDG) Era. The report13 has helped to elevate the focus on quality in the health system, highlighting, in particular, the role of people in health systems, i.e. their availability, management and motivations.
In 2019 the president launched the District Development Model (DDM). The DDM is ‘an approach by which the three spheres of government and state entities work in unison in an impact-oriented way, and where there is higher performance and accountability for coherent service delivery and development outcomes’, in order to better respond to the major structural challenges of inequality and poverty. The COVID-19 emergency revealed the necessity for intersectoral collaboration and in some localities, mandated mechanisms such as the Joint Operation Centres catalysed local relationships which could serve as a resource for future place-based approaches to the social determinants of health14.
An overarching feature of the period, compounding fiscal constraints, was a general crisis of governance at provincial level, a high turnover of political and senior administrative leadership, and loss of institutional memory and capacity for stewardship of the health system15. This unstable provincial context resulted in the selective centralisation of decision-making to the national level, notably in the systems interventions linked to NHI pilots, but also hampered the coherence, coordination and integration of initiatives in PHC described in the next section.
In this section we review key initiatives to strengthen PHC over the period, including a centrally funded portfolio of interventions introduced through the PHC Re-engineering Strategy and subsequently as part of the NHI pilot sites and other processes.
Over the last decade the WBPHCOTs have emerged as a central component of the PHC system in South Africa. In 2019, there were 54 000 CHWs in the public health system, constituting 22% of the total and 47% of the PHC workforce, respectively12. These CHWs have a comprehensive scope, fulfilling promotive, preventive and adherence support functions, are supervised by nursing cadres (outreach team leaders) and relate closely to the nurse-based PHC system. The CHWs have become a vital part of new systems of community-based distribution and follow-up for chronic diseases (communicable and non-communicable) and are credited in part for the pattern of reduced PHC facility utilisation over the last five years. Community health workers were a highly visible part of the early COVID-19 pandemic response, as the mainstay of community screening and testing, and supporting the home delivery of chronic medication to patients in households to limit their exposure through health facilities16
The WBPHCOTs grew into a CHW programme from an initially unregulated, highly diverse and fluid community-based care and support system that emerged as part of the HIV/AIDS response from the mid-1990s onwards. However, over the ensuing years the community-based sector struggled to shift from a loose and relatively informal, disease-specific infrastructure to a comprehensive CHW programme, adequately funded, supported and integrated into the health system. In the context of a widening fiscal crisis, frequent lip service to the value of CHWs has not been matched by political, budgetary and organisational commitments. Thus, despite their numerical importance (nearly half of all PHC workers), CHWs constituted only one-tenth of the total PHC health workforce expenditure in 2019, coordinated national and provincial governance of the programme has remained weak, and levels of coverage, recognition, training and supervisory and support systems are highly uneven across the country17
Nevertheless, over the 2015–2019 period, a number of developments signalled that the status of WBPHCOTs may be shifting towards greater formalisation and integration into the health system. The teams formed one of the key components of the intervention package in NHI pilot sites, benefitting from additional resources to expand coverage and team leader support. In 2018, the National Department of Health (NDoH) issued, for the first time, a ‘policy framework and strategy’ for WBPHCOTs, seeking to create
a standardised programme design, laying out norms, scopes of work, roles of different players, mandates and monitoring systems for the country18. The training curricula and processes were redeveloped and a CHW unit established within the DHS cluster to steer the programme nationally.
Although the first goal of the WBPHCOT policy framework is to ‘Improve the working conditions of WBPHCOTs’, it remains silent on questions of CHW remuneration and the sources of funding for CHWs. In practice, CHWs have been paid through a variety of short-term contracting arrangements determined at provincial level – whether through non-governmental organisations (NGOs), third party ‘paymasters’ or the government payroll system. In 2018 the national Public Health and Social Development Sector Bargaining Council signed an agreement with the NDoH and unions to standardise remuneration of CHWs across the country at the minimum wage, with the view to eventually integrating CHWs into the public sector. These bottom-up pressures on conditions of service have been a key driver of formalisation.
In South Africa, an emerging evidence base has provided evidence on the effectiveness19, affordability20 and a high benefit-to-cost ratio of 3.421 of an adequately supported CHW programme. A nationally commissioned investment case estimated that ‘a properly resourced, scaled-up WBPHCOT programme could save 200 000 lives and more than five million productive disability-adjusted life years over 10 years. The multiplier effects of saved lives and employment creation would inject billions of rands of additional revenue into the economy’4
District Clinical Teams (DCSTs) were established as a system of clinical governance, mentorship and quality improvement of districts across the country in 2012, first as part of the PHC Re-engineering Strategy and then subsumed under NHI. These teams had a focus on maternal, newborn and child health, and were to include an obstetrician and gynaecologist, a paediatrician, a family physician, an anaesthetist, a midwife, and a professional nurse in each of the 52 districts. Establishment of DCSTs was slow – after 18 months only 56.4% of posts had been filled across the country, with particular challenges in filling medical specialist posts24. Experiences of the DCSTs have been uneven across the country. When linked to wider systems of clinical governance, DCSTs have been credited with significant gains in maternal and child health outcomes23-26. However, an evaluation of the DCST component in the NHI pilot sites found there was uncertainty of roles (especially with parallel maternal-child health programme structures), variable performance, questionable cost-effectiveness, and crowding out of systems of outreach and support from regional hospitals6,26. The teams were initially funded by conditional grants with the expectation that they would be absorbed into district budgets through the equitable share. One KZN district estimated that the seven members of the DCST constituted 15% of the District Health Management Office budget. Some provinces decided to do away with DCSTs, replacing these with specialist outreach and support through regional and tertiary hospitals, and absorbing nurse specialists into programme structures.
The Ideal Clinic Realisation and Maintenance (ICRM) programme is a PHC standardsetting and quality assurance programme, established in 2013 as a system of auditing and response, intended to improve the PHC infrastructure in preparation for NHI. The purpose is to ‘assure the public that the specific Health Establishment is safe and delivers minimum standard of care as measured against the norms and standards set by the NDoH’iii
In 2015, after an initial period of piloting, the highest health sector decision body – the National Health Council – mandated implementation of the ICRM across the public health system. By 2019, audits had been conducted in all districts and 1 501 (43%) of PHC facilities had retained Ideal Clinic status.
A five-year review of the ICRM conducted in 2020 reported the following achievements of the Ideal Clinic programme:iii
• More than 50% of PHC facilities had achieved Ideal Clinic status (even if some had not maintained this status)
• The programme had been aligned with other processes – notably the Office of Health Standards Compliance and District Health Plans
• The auditing processes are supported by software (including mobile applications), and regularly updated. The Ideal Clinic Manual is regularly updated (Version 19 appeared in May 2021)
• The Ideal Clinic portal provides links to a range of handbooks, guidelines and catalogues
• Resources were mobilised for equipment purchases
• Successes had spurred the development of an Ideal Hospital programme
• The process has been supported by funds from partners
The Ideal Clinic runs the risk of all externally mandated audit systems in organisations –that is, becoming a compliance mechanism rather than a driver of real change, especially if the mechanism does not reflect the reality of practice. The evaluation of the NHI pilot districts alluded to this phenomenon when it reported that ‘facilities would purchase equipment irrespective of the need, in order to reach ideal clinic status’6. Such ‘gaming’, producing ‘an illusion of compliance’, has been reported by others28,29 studying frontline practices associated with the Ideal Clinic. The transaction costs of repeated assessments are high with ‘short implementation windows in which facilities have to adapt to new requirements to achieve the desired ideal clinic status’6. The onus on facility managers to resolve problems of resourcing and infrastructure outside of their decision-space is demotivating28
The Ideal Clinic process reflects a general trend towards greater use of audits and expectations of transparency, which is likely to increase with the advent of the NHI
i See for example: https://www.iol.co.za/news/politics/community-health-workers-to-waitanother-year-for-permanent-employment-26cf6114-c3ba-48a0-a502-4c43bfe3bcac
ii Mkhize, NC and Msimango, P. Sub-District Model Presentation to DHMT, King Cetshwayo District, 30 September 2019 (PowerPoint provided by J Mndebele).
iii Morewane, R. ICRM 5-Year Review: Overview. PowerPoint presentation, 26 February 2020 [available at: www.idealhealthfacility.org.za/].
and the introduction of ‘purchaser–provider’ split arrangements. Intensification of audit and compliance can, however, be counterproductive. An inventory of accountability mechanisms for maternal, neonatal and child health in one district counted a total of 19 different direct or indirect mechanisms, often duplicating and generating accountability overloads29
As part of the NHI pilot site intervention package, in 2014, the NDoH introduced a Central Chronic Medicines Dispensing and Distribution (CCMDD) programme to support adherence and retention in care for HIV and other chronic NCDs. The CCMDD enables follow-up and distribution of medication to stable patients through facility fast queues, community adherence clubs, retail pharmacies and other novel ‘pick-up points’ (PUPs).
By 2019, the CCMDD programme had expanded to all the districts (except in the Western Cape which had an existing programme), was present in close to 3 500 facilities, had registered more than 2 000 external PUPs and more than 2 million patients were being followed up through the system30. Just over half of patients were collecting medication from fast lanes in PHC facilities, 13% through adherence clubs and 35% from external PUPs. Project Last Mile supported the development of external PUPs such as ‘smart lockers’ through private sector engagement. Successful implementation of the CCMDD has been attributed to ‘strong political leadership and will’ and ‘reliable data to support continued implementation’6 According to patient evaluations, the CCMDD facilitated access, reduced waiting times in health facilities and created new medicine collection options33. However, patients also indicated receiving inferior care in private facilities compared with paying patients. Another challenge of a contracted-out system of PUPs is the tracking of patients in two parallel systems and the lack of mechanisms to trace those lost to follow-up in the private sector. The reliance on a few central contractors is also regarded as a risk and requires capacity for managerial oversight and monitoring6
During the COVID-19 pandemic, health services in the Cape Town and Tshwane metros further extended their community-based distribution systems for chronic disease care to include home delivery through CHWs16,32. Within one month of the initial lockdown, the Cape Town metro had distributed 184 000 parcels to patients with chronic diseases who were ‘therefore protected from exposure to COVID-19 at health facilities and public transport’16.
In 2012, the national government launched an eHealth Strategy. In the first step, a Health Patient Registration System (HPRS) was developed and introduced into 657 NHI pilot site PHC facilities as part of a broader ehealth programme, that included installation of computers and Wi-Fi connectivity, rationalisation of existing registers and plans for interoperability between electronic systems (e.g. electronic antiretroviral therapy registers and the district health information system). By 2019 close to 3 000 PHC facilities and nearly 70% of the population was registered on the system33
However, at the time of writing, the HPSR has not progressed beyond patient registration in PHC facilities, and has yet to be integrated with other ehealth and hospital information systems or with the WBPHCOTs34. The WBPHCOTs conduct household registrations and are playing increasingly significant roles in chronic disease follow-up, but their activities are not captured in NHI. Other key infrastructural challenges associated with HPSR implementation include inadequate computer supplies and difficulties with maintenance, safety of equipment and poor network connectivity6. In a survey of facility managers in NHI pilot sites, only 30% reported reliable network connectivity, with the remainder reporting either ‘somewhat reliable’ (52%) or ‘completely unreliable’ (18%) network connections6
Another ehealth innovation – the Stock Visibility System (SVS) – was introduced in NHI pilot sites to support real-time monitoring and reporting of essential medicines and vaccines stocks. The SVS connects players across the supply chain and its purpose is ‘to improve oversight of stock through an electronic stock monitoring system, and thereby reduce stock-outs by allowing for appropriate and timely ordering’6. The SVS was scaled up nationally, reaching over 90% coverage of PHC facilities by 2017/18. Nearly half the 49 managers interviewed in NHI pilot sites reported ‘a substantial decrease in stock-outs as a result of SVS’. The SVS, as with the HPRS, remains a siloed innovation, and shares the same broader challenges of other ehealth interventions in PHC – ensuring stable and functioning infrastructure (in this case mobile phones), securing interoperability, and convergence of data sources into an ‘ehealth enterprise architecture’ for NHI33
Although focused on public sector systems strengthening in the first phase, the NHI ultimately aims to integrate private and public sector provisioning into one health system, funded by a single payer (the NHI fund). Primary care in the private sector is provided in the main through private general practitioners (GP), working in solo or small group practices. GPs are widely available in the private sector, estimated to be 3–4 fold that of the public sector35. Private GP practices typically cater to both insured and uninsured (cash paying) populations, and account in part for out-of-pocket payments for health care in South Africa.
The NHI pilot site interventions have experimented with forms of private sector contracting, which include the use of private sector supply chains and providers in the CCMDD programme. A second initiative was to contract-in private GPs to provide care in public sector PHC facilities. By 2018, 330 GPs had been contracted to work in PHC facilities in the pilot sites6. Three contracting mechanisms emerged – direct contracting with the NDoH, contracting via an intermediary (a national GP organisation) and contracting with the district authority35. Despite the establishment of a dedicated national contracting unit, capacity for oversight and monitoring from this level proved to be limited. Uptake of GP contracts was low in many sites, and the monitoring of claims poor, resulting in over-expenditure on this component of the NHI grants6. The most decentralised model worked best but rested on a pre-existing track record of successful contracting by districts35. The GP contracting initiative was thus not extended beyond the pilot phases.
The experiences with GP contracting highlight the inherent complexity of contracting for health care, and the risks facing a future NHI premised on the purchaser–provider spilt model. Engaging the private sector – in whatever capacity –requires high levels of decentralised capacity for monitoring and oversight in public au thorities, which is as yet not present at district level.
During the period under consideration, PHC in South Africa benefitted from significant system strengthening initiatives, supported by ring-fenced budgets under the umbrella of NHI. The consolidation of initiatives in NHI pilot sites, considerable technical and other support from partners and ring-fenced funding through conditional grants resulted in successful implementation of many of the interventions, some beyond the pilot sites. Collectively, these interventions engaged all the operational levers proposed by WHO/UNICEF (Table 4.2) and have contributed to improved access, quality and standardisation of PHC.
This considerable portfolio of new technology and systems was however constrained by weak strategic levers, in particular, the growing fiscal constraints and budgetary and governance crises besetting many provinces. While the centralisation of funding, planning and donor support meant that provinces could be bypassed, this is unlikely to be sustained in the long run. The ultimate success of the interventions rests on background capacity (staffing, infrastructures, governance, etc.) of provincial health systems. In this regard, the next section discusses metrics of overall performance of the PHC system.
The orientations of interventions of this period also reflected the central preoccupations of NHI – namely ensuring the provision of essential primary care. There were no strategies specifically focused on strengthening public participation and accountability or advancing intersectoral collaboration, despite national initiatives such as the DDM. However, while the national strategies described above were being introduced, nodes of innovation and development were emerging across the country that engaged both strategic and operational levers holistically and which themselves provide important lessons for a future NHI (see bottom-up health system strengthening below).
4.2 Operational
addressed
In this section, we review indicators of PHC performance in three areas: financing, health workforce and utilisation of PHC. The indicators are drawn from routine data sources (collated by the Health System Trust and reported annually in the District Health Barometer36), and a modelling exercise on PHC personnel conducted for the 2030 HRH Strategy. The reported indicators are all for the public s ector and for uninsured populations and exclude curative ambulatory services by private providers (GPs, dentists, pharmacies, therapists, traditional healers and others). The public sector is the majority provider (86% of the population), and despite significant resources within the private sector, these have not contributed in any significant manner to PHC for this majority. Indicators of quality and health outcomes are reported in other chapters.
Public sector PHC is funded through taxation and is provided free at the point of use. In a recent comparative analysis of 20 LMIC PHC systems2, South Africa had the lowest out-of-pocket payments for health care, estimated as 8% of total health expenditure in 2018. The PHC system thus forms an important safety net, providing a comprehensive package of services, including a programme of Nurse-initiated and Managed Antiretroviral Treatment (NIMART) to over 5 million people in 2021.
In the 10-year period from 2010/11 to 2019/20, per capita public PHC expenditureiv increased by 40% in real terms, from R910 (US$60) to R1 272 (US$84) (Figure 4.2). In this period, the proportion of total government health expenditure on PHC increased from 25% to 29%, and all district health services increased from 41–45% of total expenditure. However, it is important to note that much of the growth in expenditure was driven by expansion of HIV/AIDS care over the period, which increased its share of total district expenditure from 14% to 22%36. In addition, the rate of growth in expenditure underwent a steady decline from 2017 onwards.
Figure 4.2 Per capita expenditure on PHC (rand real 2019/20 prices) (primary vertical axis) and percentage of total health expenditure on PHC, 2010/11 to 2019/20
Source: National Treasury and Health System Trust
iv Includes provincial and local government expenditure, conditional grants (e.g. HIV/AIDS, NHI), but excludes district hospitals and district management.
In 2019, there was a total of 244 000 health workers employed in the public health system, a ratio of 5/1 000 public sector dependent population (PSDP). This health workforce is predominantly nurse-based, constituting 56% of public sector workers, with doctors making up 8.6% of the total12. The combined availability of doctors and nurses in the public sector was 3.3/1 000 PSDP, which is below the WHO-recommended norm of 4/1 000 population37. However, when the private sector medical/nursing personnel is included, the ratio rises to 6.9/1 000 population, underscoring the considerable inequities in South Africa’s health system2
As part of the 2030 HRH Strategy, the current (2019) and five-year projected (2025) health workforce needs for PHC were determined. In 2019, nurses and CHWs constituted 90% of the workforce, at 43% and 47% of the total, respectively12. In order to achieve universal (equitable) coverage (as laid out in the PHC Re-engineering Strategy and assuming a PHC utilisation of 3.2), the gap in the public sector PHC health workforce was estimated to be 71 000 in 2019, rising to 88 000 in 2025. Bridging this gap would require an additional 34 billion rand.
The investments in PHC, accompanied by changing disease burdens (HIV/AIDS and NCDs), and introduction of new programmes in PHC are reflected in increased utilisation of services. Public PHC utilisation rates – measured as annual PHC head count per capita uninsured person – was 3.0 in 2010 but declined from 2015/16 onwards, reaching 2.2 in 2019/20, and below the target rate of 3.2 referred to in the previous section. Figure 4.3 shows 2019/2020 data reflecting significant inter-provincial variation (ranging from 1.6 to 2.8) but suggests a pro-equity pattern: wealthier provinces with a greater concentration of private ambulatory providers (Gauteng and Western Cape) have lower utilisation rates. These provinces also concentrate regional and tertiary hospitals, and patients may bypass PHC to access specialist care at higher levels36
Figure 4.3 2019/20 PHC utilisation rates and average annual change between 2015/16 and 2019/20 by province
Source: Copied from District Health Barometer 2019/2036
Plausible reasons for the decline in utilisation include the general shift towards community-based service delivery for stable patients on chronic medication – whether through the external PUPs in the CCMDD programme described above or through the Ward-based Outreach Teams (WBOTS)36. Lower demand for care due to improved health status of children and adults may be another factor. Finally, a factor also suggested is greater quality of data following the rationalisation of facility registers and less double counting of activity.
COVID-19 had a dramatic impact on PHC utilisation. PHC head counts dropped from 99.6 million in 2019 to 81.2 million 2020, an 18.4% decline7. Worryingly, HIV testing and GeneXpert tests for TB declined by 22% and 26%, respectively. The initial severe lockdowns, diversion of staff to the COVID-19 response, and closure of facilities because of staff illness and patient fears all played a role in these declines. However, there were also purposeful initiatives to ‘decongest’ PHC through the organisation of home delivery programmes16,32. The collateral impacts of COVID-19 on PHC programmes are likely to be felt for years to come.
In this section, we review significant innovations in the PHC system that have emerged at sub-national level. Some of these innovations build on or extend existing national strategies (community-oriented primary care and sub-district models), while others introduce novel approaches (community-level monitoring). All provide fresh, and to a large extent, holistic perspectives on the ‘what’ and the ‘how’ of PHC system strengthening and are thus uniquely positioned to inform and complement the ‘top-down’ national strategies reviewed earlier in the chapter.
Community-Oriented Primary Care, defined as ‘a continuous process by which primary health care is provided to a defined community on the basis of its assessed health needs, by the planned integration of primary care practice and public health’40 has a long history in South Africa, dating back to the 1940s. Supported by Departments of Family Medicine, a growing number of COPC nodes across the country have re-emerged over the last 10 years, combining the public health, managerial and primary care principles that inspired the original model. The most developed and articulated of the COPC models is in the Tshwane Metropolitan Municipality of Gauteng province. The core features of the Tshwane COPC model22,v, are:
• Community-based teams of CHWs, providing comprehensive care to households in defined and mapped geographical areas;
• Seamless integration between community-based and facility-based (i.e. clinic and hospital) multidisciplinary teams (including clinical associates and GPS), providing support and referral in defined patient care pathways;
• A locally developed ‘ICT-enabled’ (smart phones, tablets, facility ICT infrastructure) information system architecture, integrating community- with facility-based service activity, support functions (e.g. laboratories) and the district health information system; and providing real-time feedback to providers;
• Systems of local planning and resource allocation, based on population characteristics and disease profile for individual facility catchment areas; and
• A partnership with University of Pretoria of service learning, system development, continuing education, research and evaluation of the model.
The Tshwane COPC model is also the basis of community-based services in KZN.vi Although there are no published impact assessments of the Tshwane programme, economic modelling of its application in a rural district of Limpopo has shown a benefit cost ratio (BCR) of 3.4, with high net savings in averted clinic and hospital use21. The COPC model is also being implemented in the Cape Town metro, with a participatory co-design process, resulting in the formulation of a framework of 10 elements – see Figure 4.416.
The COPC models address many of the current weaknesses in the WBPHCOTs programme, in centering populations and community health systems in PHC, rather than treating them as marginal add-ons; through systematic evidence-based public health and clinical approaches; supportive supervision; and ‘21st century’ ICT-enabled information systems.

A health sub-district typically serves between 50 000 and 500 000 people and contains community-based services, clinics and a district hospital (public sector), and private and traditional providers (dependent on degree of rurality), that form a logical service delivery unit.
In practice, the sub-district as a governance and coordination mechanism is under-developed in South Africa, with reporting lines of the different elements running in parallel to district management teams. This creates a fragmented service delivery environment, compounded by the proliferation of vertical health programmes (HIV, TB, NCDs, etc.) extending from the district into facilities and communities. In such a system, implementation of integrated approaches in a continuum of care, as proposed in the COPC model above, is difficult.
v Marcus, TS. COPC integrated healthcare to and from the home = 21st Century UHC (PowerPoint). Presentation to the National UHC Dialogue, 21-22 November, 2019.
vi Shabangu, GC. Community-Based Model – A Service Delivery Model for KZN (PowerPoint). Presentation to the KZN Department of Health, February 2020.
In this section, we describe two initiatives seeking to formalise and strengthen the sub-district as the basic building block of South Africa’s health system:
• The sub-district management model proposed by the KZN provincial health department, variations of which are present or emerging in other parts of the country
• Achieving improved quality and outcomes through a coordinated sub-district approach in districts of Limpopo and Mpumalanga (referred to as the 3-feet model)
The KZN sub-district management model is premised on the rationale that successful implementation of ‘Community-Oriented Primary Care (COPC) with a responsive Community-Based Model’ requires a sub-district governance mechanism. The aim is ‘to develop a standardised, seamless and well-defined sub district management model, with clear boundaries and well-defined supervisory roles and responsibilities for improved efficiency and effectiveness on the health system’.vii The model defines core functions (roles and responsibilities) and a unified reporting line in the sub-district, through the district hospital Chief Executive Officer (or the most senior other manager if there is no hospital in the sub-district).
Echoing the COPC approach outlined above, Box 1 spells out the functions of the sub-district management.
Box 1: Roles and responsibilities of sub-district management
• Coordinate, oversee and manage service delivery for district hospitals, community health centres, clinics, midwifery obstetric units and community-based services
• Institutionalise COPC concept as a service delivery model
• Create an enabling environment for proper health information management and utilisation for decision-making
• Facilitate health programme coordination, integration and supportive supervision
• Ensure that there is a well-communicated referral system from household right up to the district hospitals
• Collaborate with all stakeholders in the promotion of quality of life of all individuals in the sub-district through Operation Sukuma Sakhe (intersectoral) Strategy.
The sub-district is envisaged to become the CUPS mechanism proposed in the NHI, with the CUPs ‘comprised of a district hospital, clinics and, or community health centers and ward-based outreach teams, and private primary service providers, organised in horizontal networks within a specified geographical sub-district area’.
The formalisation of the sub-district will require:
• ‘Right sizing’ of district management structures to fulfil its new mandate of service planning, coordination, monitoring and evaluation
• Reconfiguration of organisational structures of district hospitals and community health centres to be aligned to the responsibility of supporting PHC management
• Integration of PHC and health programmes, with programme managers reassigned as PHC local area managers
• Strengthening the role of family physicians to provide oversight of the quality of clinical services in district health hospitals and PHC.
In 2013, in response to high maternal and child mortality, the NDoH prioritised a number of districts for targeted action. The 3-feet model was thus developed as an approach to improving quality and outcomes, centred on real-time mortality surveillance and responses in the basic unit of service delivery. A local governance mechanism – the Monitoring and Response Unit (MRU) – was established at sub-district level, creating functional coordination between community, clinic and district hospital services, and between line managers, clinicians, and health programme and information managers. The MRU focuses on outcomes and contributory factors, the development of whole systems thinking, integrating real-time evidence and building responses based on the principles of comprehensive PHC and local decision-making. The 3-feet model is supported by a number of reporting and decision-making tools and a training package39
The model was successfully trialed in the Waterberg and Gert Sibande Districts of Limpopo and Mpumalanga, respectively, and was associated with declines in mortality (most notably for severe acute malnutrition) in both these districts25,40. The approach complements well, and provides a methodology for actioning the sub-district structures and roles and responsibilities outlined in the previous section. The 3-feet model is currently being introduced into a number of other districts across the country, with the focus going beyond just maternal-child health and mortality to incorporate morbidity monitoring and response. The model of the MRU has also been incorporated into District Health Planning frameworks.
viii Ndivhuwo Rambau, Data Project Officer. The Ritshidze campaign: Civil society monitoring of PHC performance (PowerPoint). Presentation to the webinar: Revitalising primary health care: promising practices, 5 October 2021.
Ritshidze was established in 2018 as a consortium of organisations of people living with HIV to improve the experience and quality of care in PHC clinics across South Africa. Ritshidze is a rigorous and independent community-led monitoring and advocacy initiative involving over 400 clinics/community health centres across 29 districts of South Africa. The initiative was made possible through a formal Memorandum of Understanding with the NDoH and followed by negotiations with individual provincial governments.viii Using pre-designed tools and entering data onto tablets, Ritshidze members (‘monitors’) carry out structured quarterly interviews and observations of facilities, with a national team collating data on dashboards in real-time on facility, district, provincial and national levels. Indicators assessed include waiting times, medicine availability, patient treatment literacy and qualitative feedback, and are reported publicly on a web portal (http://data.ritshidze.org.za/). Local monitors engage patients, communities and health facility staff to generate solutions from the data, provide quarterly feedback to facility managers and clinic committees (where these exist), and to ‘duty bearers’ at provincial and national level. Over the period of implementation, a number of Ritshidze indicators – patient waiting times, availability of staff and medicines –have improveVIII Drawing on longstanding, home-grown forms of right-based activism, Ritshidze holds what may ultimately be more effective as a tool of participation and accountability than clinic committees and audit systems such as the Ideal Clinic.
As indicated earlier, these various bottom-up systems strengthening innovations provide a rich basis for an approach to PHC in a future NHI. A key issue going forward will be how to ensure that national strategy development is informed by and engages these bottom-up perspectives, recognising that the priorities of NHI (such as public-private partnerships) may not always cohere with the rationales and approaches of these locally embedded models.
This chapter has shown how PHC remains a central organising idea in South Africa’s health system, and continues to receive concerted attention in policies, programmes and interventions, translating into budgetary commitments. However, we have also argued that investment in the operational levers of PHC have not been adequately matched by attention to the core strategic levers, in particular the structures and systems of governance at sub-district and district levels; or to the problems of unstable leadership, deepening fiscal crisis and corruption at provincial level. There is also a lack of alignment between developments in PHC and other strategic processes – such as human resources for health, quality improvement and the DDM. In such an environment, the introduction of a new mechanism such as the CUPS proposed in the NHI bill may compound system fragmentation (especially between PHC and other levels of the health system) and engender a further loss of coherence and accountability.
Another challenge is that the interventions in PHC have tended to be piecemeal and technical under NHI as the umbrella policy, rather than NHI being embedded in a whole system perspective that places communities and PHC at the strategic centre of the health system. The NHI bill also reinforces a curative view of PHC, defining it as ‘the first level of contact of individuals, the family and community with the national health system, bringing health care as close as possible to where people live and work,
and constitutes the first element of a continuing health care process’5. As a financing reform, NHI is naturally more concerned with technical and allocative efficiency, than with public participation and intersectoral action on the social determinants of health. This echoes global critiques of the UHC movement41
A final challenge is that policy-makers and the ‘political elite’ are typically not users of public sector primary care, which may be a disincentive to embarking on complex and politically difficult PHC-related governance or budgetary reforms.
Primary health care has to be approached as a wider system philosophy embracing participation, intersectoral action and comprehensive approaches to health, embedded within coherent sub-district and district systems. While achieving greater system efficiency is key, further development of the PHC system, especially components such as the WBPHCOTs, cannot occur in an environment of austerity and disinvestment. Emphasis also needs to shift from the ‘what’ of policy to the ‘how’ of implementation, focused on learning through deliberation and by doing, keeping a finger on the pulse of ground realities (‘at 3-feet’), adapting or de-implementing ineffective or harmful strategies, supported by partnerships and embedded and co-produced evaluation and research. The reasons for declining patterns of PHC utilisation need to be better understood.
Going forward, further development of PHC in South Africa will require:
1) A willingness to tackle the governance weaknesses in PHC, starting with the formulation of a coherent sub-district system, and beyond this, establishing meaningful community participation and intersectoral collaboration;
2) The shift from a curative, disease orientation (the focus of NHI proposals) to a more expansive approach, centred on prevention, promotion and action on the social determinants of health;
3) Aligning developments in PHC with other system developments, in particular around HRH development and financing;
4) A commitment to establishing stable, skilled and public-interested leadership in PHC and district health systems; and
5) Forms of health system learning that rely less on nationally defined audits than on co-produced approaches better able to harness bottom-up participation and innovation.
1. McKenzie A, Schneider H, Schaay N, Scott V, Sanders D. Primary Health Care Systems (PRIMASYS): Case Study from South Africa. Geneva; 2017. https:// www.who.int/alliance-hpsr/projects/alliancehpsr_southafricaprimasys.pdf?ua=1.
2. Langlois EV, Mckenzie A, Mecaskey JW. Measures to strengthen primary health-care systems in low- and middle-income countries. Bull World Health Organ. 2020;98:781–791. doi: http://dx.doi.org/10.2471/BLT.20.252742
3. Ryneveld M Van, Schneider H, Lehmann U. Looking back to look forward : A review of human resources for health governance in South Africa from 1994 to 2018. Hum Resour Health. 2020;18:92:1–10. doi:10.1186/ s12960-020-00536-1
4. Schneider H, Daviaud E, Besada D, Rhode S, Sanders D. Ward-based primary health care outreach teams in South Africa: developments, challenges and future directions. In: Rispel L, Padarath A, eds. South African Health Review 2018 Durban: Health Systems Trust; 2018:59–66.
5. Minister of Health Republic of South Africa. National Health Insurance Bill. South Africa: Government Gazette; 2019.
6. Genesis, The Centre for Health Policy, PWC. Evaluation of Phase 1 Implementation of Interventions in the National Health Insurance (NHI) Pilot Districts in South Africa. Johannesburg; 2019.
7. Pillay Y, Pienaar S, Barron P, Zondi T. Impact of COVID-19 on routine primary healthcare services in South Africa. South African Med J. 2020;epub ahead. doi:10.7196/SAMJ.2021.v111i8.15786
8. WHO; UNICEF. Declaration of Astana. Geneva; 2018. https://www.who.int/ docs/default-source/primary-health/declaration/gcphc-declaration.pdf.
9. Rasanathan K, Evans TG. Primary health care, the Declaration of Astana and COVID-19. Bull World Health Organ. 2020;98(February):801–808. doi:10.2471/ BLT.20.252932
10. WHO, UNICEF. Operational Framework for Primary Health Care: Transforming Vision into Action. Geneva; 2020.
11. National Department of Health. National Health Insurance for South Africa (White Paper). Pretoria: Department of Health, Republic of South Africa; 2015.
12. National Department of Health. 2030 Human Resources for Health Strategy: Investing in the Health Workforce for Universal Health Coverage. Pretoria: Department of Health, Republic of South Africa; 2020.
13. South African Lancet National Commission. Confronting the Right to Ethical and Accountable Quality Health Care in South Africa. Pretoria; 2019.
14. Schneider H, Okeyo I, du Toit A, et al. Intersectoral collaboration before and during the COVID-19 pandemic in the Western Cape: implications for future whole-of-society approaches to health and wellbeing. In: South African Health Review 2021. Durban: Health Systems Trust.
15. Presidential Health Summit. Strengthening the South African Health System towards an Integrated and Unified Health System. Pretoria; 2018.
16. Mash R, Goliath C, Perez G. Re-organising primary health care to respond to the Coronavirus epidemic in Cape Town, South Africa. African J Prim Heal Care Fam Med. 2020;12(1)(a2607):1–4.
17. Murphy JP, Moolla A, Kgowedi S, et al. Community health worker models in South Africa: A qualitative study on policy implementation of the 2018/19 revised framework. Health Policy Plan. 2021;36(4):384-396. doi:10.1093/heapol/ czaa172
18. National Department of Health. Policy Framework and Strategy for Ward-Based Primary Healthcare Outreach Teams. Pretoria; 2018.
19. Assegaai T, Reagon G, Schneider H. Evaluating the effect of ward-based outreach teams on primary healthcare performance in North West province, South Africa: A plausibility design using routine data. South African Med J. 2018;108(4):329–335. doi:10.7196/SAMJ.2018.v108i4.12755
20. Bennett R, Marcus TS, Abbott G, Hugo JF. Scaling community-based services in Gauteng, South Africa: A comparison of three workforce-planning scenarios. African J Prim Heal Care Fam Med. 2018;10(1):1–7. doi:10.4102/phcfm. v10i1.1748
21. Bennett R, Marcus TS, Abbott G, Hugo JF. Modelling cost benefit of community-oriented primary care in rural South Africa. African J Prim Heal Care Fam Med. 2020;12(1):1–8. doi:10.4102/phcfm.v12i1.2225
22. Voce A, Monticelli F, Pillay Y, et al. District Clinical Specialist Teams. In: Padarath A, English R, eds. South African Health Review 2013/2014. Durban: Health Systems Trust; 2014:45–58.
23. Caldwell RI, Grant M, Gaede B, Aldous C. Enabling factors for specialist outreach in western KwaZulu-Natal. African J Prim Heal Care Fam Med. 2018;10(1):1–10. doi:10.4102/phcfm.v10i1.1690
24. Feucht U, Marshall C, Kauchali S, et al. Innovations in the clinical care of mothers and children in South Africa: The contribution of district clinical specialist teams. South African Med J. 2018;108(3):S38–S43. doi:10.7196/SAMJ.2018. V108I3B.12808
25. Schneider H, George A, Mukinda F, Tabana H. District Governance and Improved Maternal, Neonatal and Child Health in South Africa: Pathways of Change. Heal Syst Reform. 2020;6:1(e1669943). doi:10.1080/23288604.2019.1669943
26. Oboirien K, Harris B, Goudge J, Eyles J. Implementation of district-based clinical specialist teams in South Africa: Analysing a new role in a transforming system. BMC Health Serv Res. 2018;18(1):1–14. doi:10.1186/s12913-018-3377-2
27. National Department of Health. Ideal Clinic Manual: Version 19. Pretoria; 2021.
28. Muthathi IS, Levin J, Rispel LC. Decision space and participation of primary healthcare facility managers in the Ideal Clinic Realisation and Maintenance programme in two South African provinces. Health Policy Plan. 2020;35(3):302–312. doi:10.1093/heapol/czz166
29. Mukinda FK, Van Belle S, George A, Schneider H. The crowded space of local accountability for maternal, newborn and child health: A case study of the South African health system. Health Policy Plan. 2020;35(3):279–290. doi:10.1093/ heapol/czz162
30. Liu L, Christie S, Munsamy M, et al. Expansion of a national differentiated service delivery model to support people living with HIV and other chronic conditions in South Africa: a descriptive analysis. BMC Health Serv Res. 2021;21:463:1–8. doi:10.1186/s12913-021-06561-7
31. Dorward J, Msimango L, Gibbs A, et al. Understanding how community antiretroviral delivery influences engagement in HIV care: A qualitative assessment of the Centralised Chronic Medication Dispensing and Distribution programme in South Africa. BMJ Open. 2020;10(5):1–10. doi:10.1136/bmjopen-2019-035412
32. Louw JM, Rantloane B, Ngcobo S, et al. Home delivery of medication as part of reducing congestion in primary healthcare in Tshwane District Health Services. South African J Public Heal (incorporating Strength Heal Syst) 2020;4(2):50. doi:10.7196/shs.2020.v4i2.124
33. Wolmarans M, Solomon W, Tanna G, et al. eHealth Programme reference implementation in primary health care facilities. In: Ashnie P, King G, English R, eds. South African Health Review. Durban: Health System Trust; 2015:35–44.
34. National Department of Health. Annual Report 2018–19. Pretoria: Department of Health, Republic of South Africa; 2018.
35. Mureithi L, Burnett JM, Bertscher A, English R. Emergence of three general practitioner contracting-in models in South Africa: A qualitative multi-case study Int J Equity Health. 2018;17(1):1–18. doi:10.1186/s12939-018-0830-0
36. Massyn N, Day C, Ndlovu N, Padayachee T, eds. District Health Barometer 2019/20. Durban: Health System Trust; 2020.
37. World Health Organization. Health Workforce Requirements for Universal Health Coverage and the Sustainable Development Goals. Geneva: World Health Organization; 2016. https://apps.who.int/iris/bitstream/hand le/10665/250330/9789241511407-eng.pdf.
38. Mash R, Ray S, Essuman A, Burgueño E. Community-orientated primary care: a scoping review of different models, and their effectiveness and feasibility in sub-Saharan Africa. BMJ Glob Heal. 2019;4(Suppl 8):e001489. doi:10.1136/bm jgh-2019-001489
39. Clinton Health Access Initiaitive. Health Systems Strengthening at the Sub-District Level : The Three Feet Model. An Implementation Guide. Johannesburg; 2021.
40. Schneider H, Van Der Merwe M, Marutla B, Cupido J, Kauchali S. The whole is more than the sum of the parts: Establishing an enabling health system environment for reducing acute child malnutrition in a rural South African district. Health Policy Plan. 2019;34(6):430–439. doi:10.1093/heapol/czz060
41. Sanders D, Nandi S, Labonté R, Vance C, Van Damme W. From primary health care to universal health coverage—one step forward and two steps back. Lancet. 2019;394(10199):619–621. doi:10.1016/S0140-6736(19)31831-8
South Africa faces a quadruple burden of disease resulting from communicable diseases such as HIV/AIDS, tuberculosis (TB) and malaria; high rates of maternal and child mortality; non-communicable diseases (NCDs) such as hypertension and cardiovascular diseases, diabetes, cancer, mental illnesses and chronic lung diseases such as asthma; as well as injury and trauma. In this chapter there is a focus on three health issues which are used to illustrate the successes and failures of the health system’s response between 2015 and 2020. These are HIV/AIDS, TB, and maternal and child health (MCH).
For each of these three health issues relevant data are presented, painting a picture that illustrates the epidemiology and performance of the health system. Overall, between 2015 and 2019 there was an improvement in key metrics. Since 2020 we have seen the very negative impact of COVID-19 on socio-economic conditions in general, and the health system in particular, and these metrics have either stagnated or deteriorated since March 2020.
The review of progress on the response to these three health issues is complemented by two case studies. The first is the Western Cape Department of Health’s response to TB using lessons learnt from the COVID-19 response and incorporating a whole-of-society approach. The second illustrates gender issues in relation to access to health services and human rights.
Peter Barron, Yogan Pillay, Keith Cloete, Steve LetsikeSouth Africa faces a quadruple burden of disease resulting from communicable dis eases such as HIV/AIDS, TB and malaria; high rates of maternal and child mortality for the country’s level of development; NCDs such as hypertension and cardiovascular diseases, diabetes, cancer, mental illnesses and chronic lung diseases such as asthma; as well as injury and trauma. In all these areas South Africa has a much greater burden of disease than other comparable middle-income countries. In addition, South Africa has additional structural socio-economic challenges that hamper its efforts to improve health. These include having a very inequitable society economically with one of the largest Gini coefficients in the world, large-scale unemployment and a disproportionately large, well-funded private health system that caters for a small sector of the population. The private health sector consumes around 50% of all health resources yet caters for around 15% of the population. Additionally, it distorts the distribution of scarce human resources for health with disproportionate numbers of skilled health workers in the private health sector.
South Africa has the highest number of people infected with HIV globally with more than eight million people living with HIV. In addition, South Africa is one of the 20 high burden countries for TB. These two diseases, in addition to MCH, are used to illustrate the performance of the public health sector during the period 2015 to 2020 in respect of health programmes. This is not to undermine the performance of other programmes which are equally important. For example, it has been well documented that mental health is under-resourced and this population is under-served, as noted in a separate chapter of the book.
In general, with support from its partners and funders, in particular the United States Presidential Program for AIDS Relief (Pepfar) and The Global Fund to Fight AIDS, Tuberculosis and Malaria, the public health system improved key programme metrics during the period 2015 to 2019. With the advent of COVID-19 in 2020 these subsequently either stagnated or deteriorated.
This chapter discusses these three programmes in detail and augments this with two case studies. The first highlights some of the lessons learned from the responses to the COVID-19 pandemic by the Western Cape Department of Health and how it has started to use these to improve the province’s responses to TB. The second case study illustrates particular issues related to human rights and gender equity and access to health services to marginalised communities.
During the period 2015 to 2020, South Africa had the unenviable record of continuing to be labelled a high burden country for TB by the World Health Organization (WHO), for drug-resistant TB (DR-TB) and for TB and HIV co-infection. It has contributed significantly (3.6% of the global burden) to the global numbers of both drug-sensitive and DR-TB cases. Successive WHO Global Tuberculosis reports from 2015 to 2020 paint a picture of this. 1, 2, 3, 4, 5, 6 At the end of 2019, the world as a whole, most WHO regions and many high TB burden countries were not on track to reach the 2020 milestone of reducing TB incidence by 20% from 2015 to 2020. However, South Africa was one of seven high burden countries that was on track to achieve this indicator of the End TB Strategy. During 2020 the COVID-19 epidemic had a negative impact on key aspects of the TB control programme and negatively impacted both targets and indicators.
During 2016 to 2020 some real progress was made with reducing the overall burden of TB in South Africa. Figure 5.1 illustrates the decreases in the incidence of TB, the incidence of HIV-positive TB and the number of notified cases. Also, as shown in Table 5.1, the estimated number of people who died from TB fell from a high of 124 000 in 2016 to 58 000 in 2019. The number of people with DR-TB dropped by over a third from just over 20 000 in 2016 to a little over 13 000 in 2019. The estimated incidence, numbers and rates dropped steadily from 2015 onwards, but were revised upwards in 2019 as a result of the findings from the first ever TB prevalence survey conducted in South Africa in 2018. ‘Missing’ patients is one of the biggest problems facing the national TB programme and is illustrated by an analysis of the TB programme cascade conducted in 2018, as shown in Figure 5.2. There are leakages of patients at every point in the cascade, for example, with not enough patients being tested and those who are diagnosed with TB not initiated on treatment. It is important to understand who and what contributes to these leakages and ‘missing’ patients so that the appropriate interventions can be put in place.

Figure 5.1 Incidence, new and relapse TB cases notified, HIV-positive TB incidence (Rate per 100 000 population per year)Source: World Health Organization – Tuberculosis profile: South Africa 20196 Table 5.1 Key TB indicators in South Africa 2015 to 2020 National health programmes
Estimated incidence
Proportion
Source: World Health Organization
Tuberculosis Reports – Country Profile South Africa1,2,3,4,5,6
Source: Pren Naidoo (based on TB incidence based on National Prevalence Survey (MRC, NDoH); Accessed TB test back-calculated based on test sensitivity, assumption that 10% FN on Xpert receive culture and empiric treatment; Diagnosed based on National Health Laboratory Services (NHLS) data on case-finding (Courtesy Harry Moultrie, NICD) and National TB Report on empiric treatment; Notified and treated and treatment outcomes based on National TB Report and DR TB report (NDoH, Courtesy Sicelo Dlamini & Norbert Ndjeka); Durable cure rates based on CT data on relapse within 18 months for patients treated in 2018)
Disturbingly, 2020, the year of COVID-19, was characterised by a marked disruption of routine health services, which among other things saw a drop in the number of patients tested for TB; a decrease in the expected patients diagnosed for TB; and a drop in the numbers of patients notified and put on treatment. This is clearly illustrated in Figure 5.3. Based on data available in the routine information system, the number of symptom screenings for TB declined from 87.6 million screenings in 2019 to 70.8 million in 2020 (a 19.2% decline). The NHLS reported that the number of GeneXpert tests conducted declined by 26% between 2019 and 2020 with the percentage of positive tests declining by 18%.10,10 This had the effect of increasing the numbers of ‘missing TB’ patients across the entire TB cascade. All the patients who go ‘missing’ either die from their TB, add to the pool of TB by being chronic and infecting people in proximity to them, or else self-cure.
TB prevention has emerged as an important issue and the WHO guidance recommends TB preventive treatment for people living with HIV and household contacts. Of the 3.9 million people globally who received TB prevention treatment, 14% (509 000) were in South Africa. South Africa has also been at the forefront of innovation in TB prevention and is one of the first countries to start short course, preventive therapy through use of the new 3HP drug6. Similarly, South Africa has also been at the forefront of research into new tools, drugs and vaccines to combat TB and has been an early adopter of new drugs such as Bedaquiline in the treatment of multidrug-resistant (MDR) TB.

The Western Cape Department of Health used its lessons from its responses to the COVID-19 pandemic to strengthen its response to the significant burden of TB disease in the province. The case study highlighting the Western Cape Department of Health’s response to TB using lessons learned from COVID-19 is reflected in Box 1.
The COVID-19 pandemic resulted in significant disruptions, especially to TB services at Primary Health Care (PHC) level. GeneXpert test volumes dropped by 35% in 2020 compared to 2019, with a 40% drop at PHC facilities. GeneXpert positivity increased to 17.8% in 2020, and increased further in 2021, reaching a year-to-date average positivity of 19% by 22 August 2021. TB services were unable to recover, with 10 839 fewer TB diagnoses made in 2020, representing a 22% year-on-year reduction.
Between April 2020 and March 2021 there was a 27.2% year-on-year reduction in the number of people started on TB treatment, a 30.3% reduction in the number of people enrolled in TB treatment programmes at PHC level, and greater reductions in TB treatment initiation compared to the reduction in diagnoses, suggesting a larger treatment gap during this period. The worrying trend in these measures resulted in the launch of a provincial multisectoral emergency response plan to reduce TB, launched on 28 April 2021.3
In responding to the COVID-19 pandemic, the Western Cape Province has illustrated its ability to formulate agile, innovative and effective responses to health challenges, adopting a whole-of-society approach. Many of the lessons and innovations implemented in the response to COVID-19 have been adapted to inform the response to TB.
The Western Cape’s Emergency Response Plan for TB is centred on four focus areas:
1. Strategic communication: This includes a public-facing TB dashboard aimed at increasing public awareness.
2. Prevention of new TB infections and improving case detection: Deliberate efforts will be made to increase the uptake of TB preventative therapy amongst high-risk groups. Joint COVID-19 and TB screening is being conducted at all PHC facilities.
3. Enable early initiation of treatment and provide support to improve treatment completion rates: The province will pilot an SMS notification system, like that used for COVID-19, to inform clients of their TB test results. Other interventions in this focus area include the implementation of Urine-LAM testing as well as piloting, with the intention to expand, mobile digital X-ray services.
4. Implementing a whole-of-society response: Enhanced advocacy for socio-economic im provements, including psycho-social and nutritional support interventions for those living with TB.
The plan calls for a collective recognition amongst all stakeholders (government and civil society) that many of the social determinants that impact on the TB epidemic fall outside the scope of Departments of Health and underscores the need for an integrated and multisectoral response to addressing TB.
The COVID-19 pandemic provided fertile soil within which to innovate alternate means of approaching an infectious disease.
Community Prevention: COVID-19 provided a clear focus on increased public awareness for infection, prevention and control (IPC) measures such as mask wearing, cough etiquette and ventilation. Since both TB and COVID-19 are respiratory illnesses, the IPC measures overlap and will potentially allow for decreased stigma and increased uptake of the measures needed.
Screening: Paper-based, online and mobile screening tools proliferated during COVID-19 and allowed for patient agency in response to the pandemic. These tools offer low to no costs and help direct symptomatic patients timeously to care. Leveraging this approach for TB would provide increased passive detection of the disease with earlier treatment initiation. In addition, it may allow for combined COVID-19 and TB screening with appropriate routing of patients to care. A TB screening WhatsApp bot is already being piloted in accordance with this approach
Hotspot Identification and Response: One of the key lessons that had emerged throughout the COVID-19 pandemic was the importance of adequate, timely and accessible public data to understand the epidemic within one’s local context. This took the form of a public dashboard and has subsequently inspired the development and delivery of a first of its kind public TB dashboard in South Africa. This will allow near-real-time disease surveillance to guide programme managers to identify pitfalls within their geographic context and ensure transparency and public accountability to both citizens and the health department (https://www.westerncape.gov.za/site-page/provincial-tb-dashboard).
Testing and Tracing: COVID-19 PCR and TB Sputum GXP testing suffer similar challenges in terms of turnaround times for results. They both require the patient to be tested and return for the result after 24–48 hours. COVID-19 opened an opportunity to explore efficiencies in this process by sharing results via SMS or by a contact centre agent. Over and above this, dedicated teams were tasked to ensure telephonic contact tracing occurred to contain the spread within households. A similar strategy could be employed to ensure efficient containment of positive TB individuals as well as decreased initial lost to follow-up post sputum testing.
Virtual Case Management: The COVID-19 pandemic provided a springboard for virtual case management through telemedicine consultations. In the Western Cape, this was layered with a data-driven and risk-stratified approach to efficiently utilise clinicians to manage those most at risk of clinical deterioration. Within this project, contact centre agents were also onboarded to ensure high throughput follow-up of cases with clear red flags for escalation to the clinician team. This combination of virtual clinical and non-clinical staff supported by a risk-adjusted data-driven strategy for case identification can certainly be applied to the TB population. This will ensure a sharp directed approach to proactively manage and support patients through diagnosis, linkage to care and treatment completion.
Alternate Means of Medicine Delivery: Lastly, a by-product of restructuring the health platform in response to COVID-19 was the rapid ability to decant facilities and allow for alternate means of medicine delivery. The positive spin-off of this was reduced costs for patients to attend facilities for medication and resultant increased access for those vulnerable, with low socio-economic circumstances or too ill to attend facilities. Consideration should be given to expand this service to TB patients to gain similar benefits as those seen for chronic diseases. In addition, the delivery of chronic medication directly to patients’ homes will also potentially improve adherence to TB treatment and thus impact positively upon overall outcomes.
The Executive Director of UNAIDS, Winnie Byanyima, in the UNAIDS 2020 Annual Report15 stated that ‘the global HIV response was off track even before the COVID-19 pandemic, but the collision of COVID-19 and HIV has set it back further. The Fast-Track Targets, which expire at the end of this year, will not be achieved. Thirty-eight million people are living with HIV, with more than 12 million people waiting for life-saving HIV treatment. In 2019, 1.7 million people were newly infected with HIV and 690 000 people died from AIDSrelated illnesses’. She further stated that: ‘Ending AIDS means closing gaps and ensuring that no one is left behind. The HIV response must end inequality. If over the next five years we meet these new targets, end inequalities in HIV treatment and HIV prevention and reduce the stigma and discrimination that holds back the HIV response, the world will be well on its way to ending AIDS by 2030’.
During the past decade there has been significant progress in key indicators related to the impact of HIV in South Africa. UNAIDS country data15 shown in Figure 4.4 reflect the remarkable progress made in decreases in the annual numbers of new HIV cases and number of deaths caused by HIV between 2010 and 2019, with decreases of 53% and 61%, respectively. On the other hand, Figure 5.5 highlights the considerable way to go to achieve the 90:90:90 targets. South Africa made significant progress in reaching the first 90, viz those who are infected who know their status, and in 2019 the proportion was 92%. Of these, the proportion on antiretroviral treatment (ART) was 72%, leaving a gap of 810 000 to achieve the second 90. In terms of those who are on treatment and are viral load suppressed (the third 90), the Thembisa model (Figure 5.6) estimates that 89.7% of those on treatment were suppressed in 201918.
The Thembisa Project, a mathematical model of the South African HIV epidemic, has been the source on which the official UNAIDS estimates for South Africa are based and produced in partnership with UNAIDS and the South African Department of Health18. Tables 5.2 and 5.3 show indicators for HIV and the three 90s, respectively, for the period 2015 to 2022.
The number of new infections declined by 28.4% (from 301 837 to 216 008) during this time whilst the number of AIDS deaths dropped by 17.7% (from 86 851 to 71 435). The overall incidence rate also declined substantially from 0.87% to 0.59% in 2020. Although these are significant improvements, they are below the Sustainable Development Goal (SDG) 2030 target of ending the AIDS epidemic as well as the UNAIDS targets19 of achieving 95:95:95 by 202514. The net effect is that during the period 2015 to 2020 the number of people infected and living with HIV increased from a little over 7 million to nearly 8 million. This now chronic, lifetime infection will place a significant demand and impact on the resources of the health system for another generation. The Thembisa model predicts that by 2030 the total numbers of people living with HIV will have increased to 8.6 million, indicating a slow increase of less than 10% overall for the decade 2020 to 2030.
Although the prevalence numbers have been increasing, data from the Thembisa Project show that there have been notable successes with decreasing the incidence of HIV i. Recent evidence from the Thembisa model estimated an HIV incidence of 0.84% in 15–49-year-olds at the start of 2019. This represents a 62% reduction relative to 2000, and a 47% reduction relative to 2010. Although this reduction is lower than UNAIDS globally set targets of 75% reduction against the 2010 baseline, it is a significant reduction and in line with reductions seen in other countries in Southern Africa. The reduction in incidence in the period 2010 to 2019 was largely due to an increase in the scale-up of ART and condom distribution and use increase. The incidence reductions differed significantly by age and sex, with condoms having the greatest impact in youth aged 15 to 24. Overall incidence reduction was greater in men than in women. As both of these programmes have scope for further increase in scale, it is feasible to look ahead for further similar reductions in incidence over the next decade.
The impact of COVID-19 will undoubtedly amplify the challenges, and early studies provide evidence for this. In a review of routine data comparing 2020 to 2019 there is a demonstrated decrease in the
to similar months in 201920
of HIV tests conducted every month in 2020
Gap
Number
All
Children (0-14)
Women (15+)
Men (15+)
People
People
92% (85-98%) 70% (64-74%)
79% (60-99%)
94% (87-100%)
91% (81-98%)
Figure 5.5 HIV testing and
Source: UNAIDS DATA 202015
5 231 809 47% (36-58%) 157 330 75% (69-80%) 3 505 194 63% (56-68%) 1 569 285
Gap
75%
50%
25%
0%
64% (58-68%) 34% (26-42%) 69% (64-74%) 58% (51-62%)
cascade 2019, South Africa, with gaps to the three 90s targets
Table 5.2 Key HIV indicators from 2015 to 2022, South Africa (Thembisa model)
2015 2016 2017 2018 2019 2020 2021 2022
AIDS deaths 86 851 84 646 84 486 80 037 75 635 71 435 67 803 64 399
New HIV infections 301 837 285 258 263 725 247 945 232 214 216 008 202 165 194 185
New infections (15-24 years) 113 108 104 427 94 604 86 494 79 383 73 428 69 052 66 353
New infections (15-24 years females)
83 984 78 613 71 977 66 358 61 333 56 974 53 656 51 704
Incidence rate (%) 0.87% 0.82% 0.75% 0.69% 0.64% 0.59% 0.54% 0.51%
Mother to child transmission (number)
Mother to child transmission (rate %)
15 856 13 785 12
11 964 11 243 10 518 9 872 9 338
5.0% 4. 5% 4.1% 3.8% 3.6% 3.5% 3.4% 3.3%
People infected with HIV 7 067750 7 269 930 7 454 680 7 614 980 7 760 790 7 892 070 8 008 080 8 110 600
Prevalence males 15+ (%) 12.7% 12.9% 13.1% 13.1% 13.2% 13.1% 13.1% 13.0%
Prevalence fe males 15+ (%) 20.8% 21.3% 21.7% 22.0% 22.3% 22.5% 22.7% 22.8%
Started ART 557 044 575
750 446 531 390 288 344 881 308 245 282 280
Source: Thembisa Project. Version 4.4 Downloads: National and provincial model outputs18
Table 5.3 The three 90s, South Africa, 2015 to 2022
2015 2016 2017 2018 2019 2020 2021 2022
Proportion of HIV patients who know their status (%) 83.9% 86.4% 88.4% 89.8% 91.0% 92.4% 92.6% 93.3%
Proportion who are HIV positive on treatment (%) 57.6% 61.1% 64.8% 68.2% 70.5% 71.9% 73.7% 74.8%
Proportion of patients on ART with viral load suppression (%) 81.7% 82.8% 85.8% 86.1% 87.4% 89.7% 92.0% 92.1%
Source: Thembisa Project. Version 4.4 Downloads: National and provincial model outputs18
Figure 5.6 HIV tests done by month, in public health facilities, between March and December 2019 and 2020
Source: Pillay et al., South African Medical Journal 20212020
In this section, we focus on maternal and under-five mortality, pregnancy in adolescent girls as well as reproductive health services to illustrate how outcomes generally improved up to 2020. Services also improved generally over the period to 2019, but then stagnated or deteriorated with the onset of COVID-19.
During the period 2015 to 2020 the under-five mortality rate (child mortality) and the under-one mortality rate (infant mortality) both made significant improvements in 2020 after modest improvements in the previous four years. There was no change in the neonatal (under 28 days) mortality rate. This is shown in Table 5.421, which is based on the rapid mortality surveillance reports of the South African Medical Research Council, documenting mortality in the total South African population. The maternal mortality saw a steady improvement, with a decline of around one-third with an especially large decline in 2020.
The declines in child and infant mortality in 2020 can be attributed to the impact of total lockdown on both natural (decrease in pneumonia and other respiratory diseases) and also non-natural deaths (accidents). It is not obvious why maternal mortality declined by so much in 2020.
Source: Dorrington et al (2021), Rapid Mortality Surveillance Report, 2019 and 202021

The decline in maternal mortality over the last decade to 2019 is also clearly shown in Figure 5.7, which illustrates deaths in public sector institutions where more than 85% of deliveries take place.

Source: Massyn et al., District Health Barometer22
However, the advent of COVID-19 in 2020 has changed the situation. An early study of routine public sector data shows that the number of maternal deaths increased by nearly 30% compared to 201924 and the institutional maternal mortality ratio increased from 90.5/100 000 live births for the period March to December 2019 to 106.8/ 100 000 for the same period in 202020. Similarly, there was a reversal in the improvement of neonatal mortality with an increase of 487 (4.8%) in the number of neonatal deaths between March and December 2019 and 2020. The institutional neonatal mortality rate increased marginally from 12.0/1 000 live births in 2019 to 12.2/1 000 in 20202020. Furthermore, routine services for essential maternal, women’s and child health, such as reproductive health services for family planning and immunisation services for childhood illnesses were severely reduced by COVID-19 in 202020
Preventing unintended pregnancies is essential for improving adolescents’ sexual and reproductive health and their social and economic well-being. Ideally pregnancies should be delayed, giving adolescent girls the opportunity to complete their schooling and be educationally, emotionally and physically ready to have children of their own. Pregnancies in this age group are important for monitoring progress towards achievement of universal access to sexual and reproductive health care services. A rise in this indicator is a cause for concern, as it indicates challenges in improving access to sexual and reproductive health care services for this vulnerable group. It also is an indicator of high-risk sex, which is a predictor of increases in sexually transmitted diseases such as chlamydia and gonorrhoea as well as HIV.
Table 5.5 shows the numbers of deliveries, terminations, delivery rates and estimated pregnancy rates by adolescent girls aged 10 to 19 years during the period 2017 to 2021. Contrary to what one would prefer from these data, which is a steady decline, there have been steady year-on-year increases in teenage pregnancies from 2017 to 2021. Part of this is due to the unavailability of routine contraceptive methods and services.
Three key issues are reflected in the routinely collected data. Firstly, there are around 4 000 deliveries each year amongst girls aged 10 to 14 years. This is statutory rape and each of these pregnancies is completely unacceptable. The increase in numbers with a nearly 50% increase in delivery rates over the period 2017 to 2020 is a shocking indictment of South African society and service delivery systems. Clearly, there has been a failure of society to protect these very young girls and their babies, with not only the health system to blame.
Secondly, there has been an overall rising trend at the national level over this time, with most provinces showing increases, with the exception of KZN, off an extremely high base. Thirdly, there is a marked difference between the urban provinces, especially Gauteng and to a lesser extent the Western Cape, having much lower proportions of teenage deliveries than more rural provinces such as Eastern Cape and KZN.
Table 5.5 Deliveries and terminations in adolescent girls aged 10–19 in the public sector, South Africa 2017/18 to 2021/22
Population and number of deliveries & terminations, adolescents 10 19, 2017/18 to 2021/22 (public sector) 2017/18 2018/19 2019/20 2020/21 2021/22* % increase 2017/18 to 2020/21
Mid year population 10 14 2 546 451 2 628 874 2 689 346 2 769 793 2 806 206 8.8 Mid year population 15 19 2 304 256 2 372 843 2 316 027 2 371 690 2 439 133 2.9
Mid year population 10 19 4 850 707 5 001 717 5 005 373 5 141 483 5 245 339 6.0
Number of deliveries 10 14 year old 2 726 3 527 3 870 4 053 2 226* 48.7
Number of deliveries 15 19 year old 114 329 121 059 127 028 134 267 70 656* 17.4
Number of deliveries 10 19 year old 117 055 124 586 130 898 138 320 72 882* 16.8
Terminations 10 19 12 896 14 441 16 301 13 972 7 211* 8.3
Pregnancies 10 19 (Deliveries plus terminations)
129 951 139 027 147 199 152 292 80 093* 16.1
Delivery rate 10 14 year per 1 000 1.1 1.3 1.4 1.5 1.6
Delivery rate 15 19 year per 1 000 49.6 51.0 54.8 55.6 57.9
Delivery rate 10 19 year per 1 000 24.1 24.7 25.8 26.6 27.8
Pregnancy Rate 10 19 year per 1 000 26.8 27.8 29.4 29.6 30.5
*The numbers in 2021/22 for deliveries and terminations are for the period 1 April 2021 to 30 September 2022, a six month period. To enable calculation of annual rates these numbers were extrapolated (doubled).
Source: Barron et al. (in press)ii
One of the ways to prevent and decrease the number of teen pregnancies is to make contraceptives readily and easily available. In Figure 5.8 below the proportion of eligible people who were using a modern contraceptive method decreased over the period 2015 to 2020. This means that they were either obtaining it through the private sector (more likely in urban areas) or simply not using contraceptives at all. The use of condoms is an ideal method for preventing not only unwanted pregnancy but also HIV and sexually transmitted infections. Successive behaviour surveys have shown that the youth generally have low condom use rates. This is a public health intervention that needs to be taken much more seriously.
During 2020, as a result of COVID-19, there was an average decrease of 5% in provision of reproductive health methods compared to 201910. This was most marked during the heavy lockdown in April, May and June of 2020.
Source: Massyn N District Health Barometer 2019/202222

The health system continues to make access difficult and is not particularly patient-centred and responsive to human dignity in general and gender differences in particular. The case study in Box 2 illustrates these issues.
The Ritshidze project (‘Saving our Lives’ in TshiVenda) is run by civil society organisations led by people living with HIV and other community activists monitoring public health clin ics and the experiences of people attending these facilities for HIV and TB services. This project aims to hold the NDoH and aid agencies accountable to improve overall HIV and TB service delivery.
The reports from the project found that patients wait very long times to acquire services with an average wait of more than 4.5 hours. At least two out of five patients do not feel that the staff who attended to them are p rofessional and friendly and there were numerous reports of patients who had missed an appointment being sent to the back of the queue. Between 10 and 20% of patients interviewed said that they left the clinic without the necessary medicines because clinics were out of stock of essential medicines such as contraceptives and antiretrovirals.
The facilities also do not generally follow basic infection control guidelines to prevent the spread of infectious diseases such as tuberculosis. This is now particularly pertinent with COVID-19 as well.
There were many reports in all three of the provincial reports reviewed that the project has reported violations of people’s privacy and health care workers are treating key populations without dignity and respect. In many cases, facility staff focus on key populations’ (e.g., gay men, female sex workers) lifestyles and sexual lives, instead of on goodquality service provision.
Significant limited information gaps remain about the health status of the LGBTI+ community (the acronym LGBTI is used in some areas of the paper as a means of includ ing the broad spectrum of sexual and gender identities and communities). This is because routine health data does not include data on the community despite the Bill of Rights guar anteeing access to health care to all regardless of sexual orientation and gender identity. The reality is that the LGBTI+ community is left behind as far as access to health services that meet their needs is concerned.
In the context of this lack of adequate services for the LGBTI+ community a number of non-governmental organisations have bridged the gap and provided dedicated health services. These include the Triangle Project, OUT and Access Chapter 2, amongst others.
However, it is important that government improves the services it provides to this community. In particular, health care workers should be better trained, appropriate services should be provided and relevant data should be routinely collected on members of the community within a rights-based approach.
During the period 2015 to 2019 there were general improvements in most of the key indicators related to HIV, TB and MCWH. However, most of the improvements were below the goals and targets set up by the SDGs, to which South Africa is a signatory. During 2020 (and up to the time of writing), there have been significant challenges posed by COVID-19, which threatens the performance of the health system and its outcomes. Not only has there been decreased access, through actual closure of facilities, lack of transport and fear of contracting COVID-19, but also the diversion of scarce resources (human and financial) towards the COVID-19 response and away from everything else, as well as declining health budgets generally, with the macro-economic environment less conducive to increasing resources for the public health sector.
The public health system as a whole has less resources to fund frontline staff (including community service doctors and nurses, as well as community health workers) who are essential for improving health programmes.
Great progress has been made in reducing the overall burden of TB in South Africa, however, this has been insufficient to reach all the targets of the End TB strategy. In addition, during 2020, as a result of COVID-19, and a reduction in access to health facilities, this has resulted in a reversal of some of the gains made in the 2015 to 2019 period.
In March 2021, a statement by the Stop TB Partnership estimated that the past 12 months have pushed back global TB progress by 12 years11. In South Africa, as in other countries, availability of health system infrastructure has been prioritised for the COVID-19 response and away from competing illnesses, including TB. Health care access has been constrained due to transport disruptions, restricted movement, reduced opening hours, depleted staffing levels, fear, and stigma. In a presentation of the 2021/22 Annual Performance Plan and Budget to the Parliamentary Committee in May 2021, the Chief Financial Officer stated that the repurposing of funds towards COVID-19 interventions meant future financial years would be difficult, with the implication that this would be to the detriment of other programmes, including TB, HIV and MCH13
There has been a range of suggestions to reverse and catch up on TB services and interventions, including using the COVID-19 crisis and not letting it go to waste.,12. These include: using COVID-19 testing to simultaneously test for TB; and using community-based and community-led responses that take diagnosis, care and support to the doors of those affected by COVID-19 and to also do contact tracing and treatment checking for TB. Other lessons from the COVID-19 response include agile decision-making involving all stakeholders, using mobile technology, real-time surveillance systems and enhanced political leadership. Finding and focussing on the missing patients including the elderly, young people and men will be vital to reduce the leakages from the TB cascade.
During the period 2015 to 2020 there were some remarkable successes, but it is clear that the work is not yet done to eliminate HIV as a public health threat. Progress towards the UNAIDS goals of 90:90:90 has been excellent and by the end of 2020 more than 92% of those infected by HIV knew their status and of those on ART treatment 89.7% were estimated to be viral load suppressed. However, of those who knew their status only 72% were on ART treatment, leaving a significant number of people (estimated at 810 000) who had either never started ART or had started but dropped out of treatment for one reason or another. The number of new infections and the number of deaths from HIV have also declined significantly over this period, with a halving of incidence between 2010 and 2019. However, these declines in incidence were below the UNAIDS and SDG goals and targets to end the HIV epidemic by 2030. HIV therefore continues to be a major epidemic in South Africa at the end of 2020 and has been clearly exacerbated by the negative effects of the COVID-19 pandemic. Given that HIV is associated with other NCDs such as diabetes and hypertension and the move to universal health coverage, it makes more and more sense for HIV to be treated as a long-term chronic disease and integrated with other conditions and programmes in a more patient-centred approach.
As with the other programmes, maternal, child and woman’s health had some successes but also experienced stagnation and deterioration associated with COVID-19. Of great concern is the inadequate uptake of contraceptives and the increasing number of adolescents becoming pregnant. This is also associated with adolescent girls being very susceptible to HIV and other sexually transmitted infections such as chlamydia and gonorrhoea, which are increasing and of epidemic proportions. There continues to be a sub-optimal use of condoms in South Africa, which has the potential to play a major role in improving outcomes for many of these challenges.
The health system continues to be negatively affected by the COVID-19 pandemic and faces a resource-constrained environment for several years. Building on the successes of the past and improving overall performance will require doing things smarter and more cost-effectively. One of the ways is to harness the power of data and improved ability to use this in the digital era. This requires greater attention to improving the quality of the data and making it available transparently and easily. Data should be packaged for the multiple users ranging from patients, community, clinicians and managers – all of whom have different needs in order to make appropriate decisions. Each disease and health programme needs to have a package of core and essential services (e.g. contraceptive services for teenage girls) that need to be available and acceptable and used by the beneficiaries of these and which need to be in place regardless of external circumstances. In other words, these need to be protected against all else and the health system needs to be resilient in doing this.
In addition, as health does not come in single disease packages, health services need to be integrated so that patients can seamlessly have all their needs attended to in a patient-centred and holistic way.
1. World Health Organization. (2015). Global tuberculosis report 2015, 20th ed. World Health Organization. https://apps.who.int/iris/handle/10665/191102
2. World Health Organization. (2016). Global tuberculosis report 2016. World Health Organization. https://apps.who.int/iris/handle/10665/250441
3. World Health Organization. (2017). Global tuberculosis report 2017. World Health Organization. https://www.who.int/tb/publications/global_report/gtbr2017_ main_text.pdf
4. World Health Organization. (2018). Global tuberculosis report 2018. World Health Organization. https://www.who.int/tb/publications/global_report/gtbr2018_ main_text_28Feb2019.pdf
5. World Health Organization. (2019). Global tuberculosis report 2019. World Health Organization. https://apps.who.int/iris/bitstream/hand le/10665/329368/9789241565714-eng.pdf
6. World Health Organization. (2020). Global tuberculosis report 2020 World Health Organization. https://apps.who.int/iris/bitstream/hand le/10665/336069/9789240013131-eng.pdf
7. World Health Organization (2021). Global tuberculosis database. Provisional TB case notifications in 2020. https://www.who.int/teams/global-tuberculosisprogramme/data (Accessed 5 May, 2021)
8. Pillay Y, Mvusi L, Mametja LD, Dlamini S. What did we learn from South Africa’s first-ever tuberculosis prevalence survey? S Afr Med J. 2021;111(5): 402–404. ISSN 2078-5135.
9. Van der Walt M, Moyo S. The First National TB Prevalence Survey, South Africa 2018: Short report. 2021. https://www.knowledgehub.org.za/system/files/elib downloads/2021-02/A4_SA_TPS%20Short%20 Report_10June20_Final_ highres.pdf
10. Pillay Y, Pienaar S, Barron P, Zondi T. Impact of COVID-19 on routine primary health services in South Africa. S Afr Med J [S.l.]. 2021;111(8): 714–719. ISSN 2078-5135.
11. The Stop TB Partnership. 12 months of COVID-19 eliminated 12 years of progress in the global fight against tuberculosis. March 18, 2021. http://www. stoptb.org/news/stories/2021/ns21_011.html (Accessed 8 May 2021)
12. Wingfield T, Karmadwala F, MacPherson P, Millington K, Walker N, Cuevas L, Bertel Squire S. Challenges and opportunities to end tuberculosis in the COVID-19 era. Lancet Respir Med. 2021. Published Online March 24, 2021. https://doi.org/10.1016/ S2213-2600(21)00161-2
13. TimesLive. Health services suffer as budget is prioritised to deal with COVID-19. 7 May 2021. https://www.timeslive.co.za/politics/2021-05-07-health-servicessuffer-as-budget-is-prioritised-to-deal-with-covid-19/ (Accessed 8 May 2021)
14. UNAIDS (2020). Prevailing against pandemics by putting people at the centre. Geneva. https://www.unaids.org/sites/default/files/media_asset/prevailingagainst-pandemics_en.pdf (Accessed 10 May 2021)
15. UNAIDS (2020). UNAIDS Data 2020. Geneva. https://www.unaids.org/sites/ default/files/media_asset/2020_aids-data-book_en.pdf (Accessed 10 May 2021)
16. UNAIDS (2020). COVID-19 and HIV: 1 Moment 2 Epidemics 3 Opportunities. Geneva. https://www.unaids.org/sites/default/files/media_asset/20200909_ Lessons-HIV-COVID19.pdf (Accessed 10 May 2021)
17. UNAIDS (2020). End Inequalities. End AIDS. Global AIDS Strategy 2021–2026 Geneva. https://www.unaids.org/sites/default/files/media_asset/global-AIDSstrategy-2021-2026_en.pdf (Accessed 10 May 2021)
18. Thembisa Project. Version 4.4 Downloads. National and provincial model outputs. https://www.thembisa.org/content/downloadPage/ProvOutput4_4 (Accessed 13 May 2021)
19. United Nations. Sustainable Development Goals. Goal 3: Ensure healthy lives and promote well-being for all at all ages. https://www.un.org/sustainable development/health/ (Accessed 17 May 2020)
20. Pillay Y, Pienaar S, Barron P, Zondi T. Impact of COVID-19 on routine primary healthcare services in South Africa. S Afr Med J. Published online 17 May 2021. https://doi.org/10.7196/SAMJ.2021.v111i8.15786
21. Dorrington RE, Bradshaw D, Laubscher R, Nannan N. Rapid mortality surveillance report 2019 and 2020. Cape Town: South African. Medical Research Council. 2021. https://www.samrc.ac.za/sites/default/files/files/2021-11-25/Rapid%20 Mortality%20Surveillance%20Report%202019%262020.pdf. (Accessed 15 February 2022)
22. Massyn N, Day C, Ndlovu N, Padayachee T, editors. District Health Barometer 2019/20. Durban: Health Systems Trust; December 2020. https://www.hst. org.za/publications/District%20Health%20Barometers/DHB%202019-20%20 Complete%20Book.pdf (Accessed 19 May 2021)
23. May J, Witten C, Lake L (eds) (2020). South African Child Gauge. Cape Town: Children’s Institute, University of Cape Town. http://www.ci.uct.ac.za/ sites/default/files/image_tool/images/367/Child_Gauge/South_African_ Child_Gauge_2020/ChildGauge_2020_screen_final.pdf (Accessed 17 May 2021).
24. Soma-Pillay P, Moodley J, Pattinson R, Fawcus S, Gebhardt S, Niit R. The effect of the first wave of COVID-19 on use of maternal and reproductive health services and maternal deaths in South Africa. Obstetrics and Gynaecology Forum. Published online 1 Dec, 2020. https://journals.co.za/doi/pdf/10.10520/ejc-me dog-v30-n4-a10 (Accessed 24 June 2021)
i Johnson L. Meyer-Rath G, Dorrington R et al. The effect of HIV programmes in South Africa on national HIV incidence trends, 2000-2019. JAIDS Journal of Acquired Immune Deficiency Syndromes. Publish Ahead of Print DOI: 10.1097/QAI.0000000000002927 (Accessed 13 February 2022).
ii Barron P, Subedar H, Letsoko M, Makua M, Pillay Y. Teenage births and pregnancies in South Africa 2017 to 2021 – a reflection of a troubled country: analysis of public sector data. SAMJ, in press April, 2022.
South Africa’s National Drug Policy (NDP) was issued in 1996 and appended to the White Paper on the Transformation of the Health System of South Africa in 1997 (Minister of Health, 1997). The NDP set objectives in three broad categories: health objectives, economic objectives and national development objectives. Although the continued relevance of this policy document has been questioned (Gray et al., 2017), it remains the extant national document guiding reform of the pharmaceutical sector.
Implementing the NDP has required multiple amendments to existing legislation and has elicited strong reactions. A number of provisions have been subjected to Constitutional Court challenges, including the powers of the medicines regulatory authority’s inspectorate (Mistry, 1998), the licence to compound and dispense (Affordable Medicines Trust, 2006; South African Veterinary Association, 2019), and the pricing interventions (New Clicks, 2006). In addition, the scheduling of cannabis has been the subject of a Constitutional Court judgment (Prince, 2018).
This chapter summarises key events and initiatives in the field of pharmaceutical policy between 2015 and 2020, with particular focus on the ongoing process of health reform, efforts to advance equity, community participation, and the extent to which intersectoral collaboration has been achieved. Four aspects are highlighted: the continuing process of strengthening the national medicines regulatory authority, the selection of essential medicines and efforts to introduce health technology assessment (HTA), efforts to improve the availability and accessibility of medicines in the public sector, and the actions taken to address antimicrobial resistance.
Shabir Banoo, Susan Putter, Andy Gray, Shoni Mulibana, Gertrude MngolaThe need to strengthen the National Medicines Regulatory Authority was a prime objective of the NDP. Ensuring effective regulation of medicines and other health products, through strengthening systems and improving performance, has become a priority for governments worldwide (WHO, 2018). The process of reform has been protracted and contested, with multiple Amendment Acts (1997, 2002, 2008, 2015), and one unsuccessful attempt (1998) to replace the Medicines and Related Substances Act (Act 101 of 1965) (the Medicines Act).
The reforms implemented in the 2015–2020 period broadly follow the recommendations of the Green-Thompson Report (2008). The process was again protracted with two Amendment Acts (2008 and 2015) being promulgated in 2017, establishing the new South African Health Products Regulatory Authority (SAHPRA). The new Authority replaced the Medicines Control Council (MCC) in 2018.
The current Medicines Act has been in effect since 1967 and has been amended several times over the years. Both the Law Reform Commission (SALRC, 2016) and the State Law Advisers have expressed the opinion that the existing Act cannot be amended any further, and that a complete replacement Bill is warranted.
The MCC had faced a number of financial and human resource capacity constraints that are common to national medicines regulatory authorities (NMRAs) in low- and middle-income countries (Azatyan, 2009). In particular, the increasing volume of applications for the registration of medicines, with limited resources, resulted in significant delays in the registration of medicines, approval of clinical trials, and other critical regulatory functions (Leng et al., 2016). Regulatory timelines in South Africa were much longer than those in comparable countries and the legislative environment impeded implementation of innovative regulatory pathways, such as reliance on the decisions of other NMRAs (Keyter et al., 2018). These delays had a significant impact on patients’ access to both new and essential public heath medicines. SAHPRA inherited both the backlog and the resource constraints of the MCC at its commencement. It needed, therefore, to address key impediments: under-funding and an inability to retain user fees, limited internal technical and administrative capacity, paper-driven systems, and an over-reliance on part-time, external experts to support routine regulatory activities, including registration decisions.
SAHPRA was established as a Schedule 3A public entity, in terms of the Public Finance Management Act (Act 1 of 1999), functioning outside the public service. The Authority is accountable to the Minister of Health and Parliament through its Board, which has governance, fiduciary and performance oversight responsibilities. Provision is also made for the appointment of the usual Board committees, such as those entrusted with audit and risk responsibilities. The Authority is led by its Chief Executive Officer and has operational and financial autonomy, accountability and responsibility for the regulation of health products. It manages its own staff, and appoints relevant technical advisory committees to support its work.
SAHPRA’s mandate has been extended to include the regulation of medical devices including in vitro diagnostics (IVDs). This poses challenges of coordination with existing provisions in the Hazardous Substances Act (Act 15 of 1973). In addition, SAHPRA has been delegated the responsibility for the regulation of ionizing and non-ionizing radiation-emitting medical devices, and radioactive nuclides. A co-regulatory approach is thus needed with the National Nuclear Regulator, which is itself undergoing legislative reform (Minister of Mineral Resources and En ergy, 2021). SAHPRA retains regulatory oversight and control of human and veterinary medicines (including complementary medicines) and clinical trials.
SAHPRA has attempted to address its systemic weaknesses by developing a new operating model, relying primarily on in-house technical and administrative staff to manage all regulatory functions, with external technical support being engaged only where needed. Despite a new funding model, which encompasses a fiscal allocation as well as retention of user fees from applications assessed and regulatory functions per formed, the Authority remains underfunded and under-resourced. The 2020/2021 SAHPRA Annual Report noted that the audit for that financial year remained qualified, although the number of findings reduced from 88 in the previous year to 23, with only one finding leading to a qualification (SAHPRA, 2021).
The Authority has nonetheless made significant strides through appointing key senior management and technical staff, transforming legacy systems, and streamlining regulatory review procedures, coordination and quality management systems. These interventions have been aimed at preventing the development of new backlogs, and expediting the registration of priority health products. Having completed the transfer of staff from the National Department of Health (NDoH), SAHPRA has prioritised the training and development of new and existing employees. Several key technical and operational positions in new regulatory areas still need to be filled. Significant investments have also been made in new digital platforms such as the Electronic Document Submission System, Digital Variations Portal and the Complementary Medicines Licensing Portal. The development of an integrated Regulatory Information Management System, which will bring all regulatory processes onto one platform with built-in automation, intelligence and reporting capabilities, remains the goal. Key achievements include the provision of a complete medicines register on the redesigned SAHPRA website, and steps to provide a repository of professional information and patient information leaflets for registered medicines.
Globally, NMRAs are increasingly focused on improving transparency, information sharing and reliance models, in order to enhance the quality and speed of regulatory decision-making. Amendments to the Medicines Act have enabled SAHPRA to establish information sharing and work-sharing arrangements with recognised NMRAs globally and to advance the development of reliance models. SAHPRA can conduct full reviews of dossiers submitted for registration of medicines, which entail a complete scientific review for safety, efficacy and quality, including Good Manufacturing Practice (GMP). It is also enabled, in relation to applications for multi-source (generic and biosimilar) medicines, to conduct abridged reviews, assessing specific, pre-agreed areas of critical importance. However, it can also conduct verified reviews, validating that an application has been authorised by a recognised NMRA and relying on that decision for key components of the review.
SAHPRA (and the MCC) has been a member of the Pharmaceutical Inspection Co-operation Scheme (PIC/S) since 2007, which has enabled it to strengthen the in spectorate function by harmonising GMP standards and processes for inspection of quality systems, promoting networks and information exchange with other NMRAs, and supporting training of GMP inspectors. SAHPRA also has observer status at the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH), so is expected to contribute to the development of global, harmonised standards.
The WHO has developed a Global Benchmarking Tool to assess the maturity level of NMRAs, as mandated by WHA Resolution 67.20 on Regulatory System Strengthening for Medical Products (WHO, 2014). NMRAs are assigned maturity levels (ML) from 1 (existence of some elements of regulatory system) to 4 (operating at advanced level of performance and continuous improvement). ML4 is intended to replace the previous designation of stringent regulatory authority, but ML3 and above would be considered WHO-listed authorities. SAHPRA aspires to being assigned ML3 status and is in the process of being assessed. Initial indications of the gaps that will need to be addressed in an institutional development plan have been received and are being considered. One of the key challenges is to revisit the outdated interpretation of the secrecy clause (section 34) in the current Medicines Act (Vawda & Gray, 2017). The chairperson of the Board noted in the 2020/2021 Annual Report that ‘more needs to be done in the field of communication to the public, and this continues to be a prioritised work in progress’ (SAHPRA, 2021).
SAHPRA is supportive of the ratification of the Treaty for the Establishment of the African Medicines Agency, which will require a parliamentary process, but also ‘domestication’ of the African Union Model Law on Medical Products Regulation in a future SAHPRA Bill (African Union, 2019).
Eliminating the backlog of registration applications inherited from the MCC was an urgent public health imperative. The backlog was substantial, with over 16 000 applications, many dating back a number of years. Although comprised primarily of applications for the registration of generic medicines, there were also significant bottlenecks in the completion of post-registration amendment (variation) applications. Previously registered products were not able to be marketed until these variations had been finalised.
SAHPRA’s approach to reducing the backlog took advantage of global and regional regulatory harmonisation initiatives, and in particular the WHO prequalification collaborative procedure. With the financial support of the Bill & Melinda Gates Foundation, a dedicated in-house Backlog Team was established, supported by the Boston Consulting Group. Funding was also secured through a special allocation from the National Treasury, as well as from the US Centers for Disease Control and Prevention (CDC), the President’s Emergency Plan for AIDS Relief (PEPFAR) and the Clinton Health Access Initiative (CHAI). SAPHRA was able to appoint additional external reviewers from a pool of local and international experienced regulatory experts. A phased approach was implemented, with applications prioritised based on public health and unmet medical needs. The team also updated guidelines and redesigned operational and business processes and implemented systems to enable electronic submission, review and tracking of applications, to reduce unnecessary bureaucracy and delays. Through engagement with industry applicants, an ‘opt-in’ process was implemented which allowed applicants to voluntarily withdraw older applications in the backlog that were considered out of date or of less interest. All applicants were required to resubmit updated, consolidated electronic applications within a given timeframe in line with SAHPRA’s new guidelines and requirements. Poor-quality applications were rejected if these did not meet strict predefined administrative or quality criteria.
SAHPRA planned to clear the backlog within a two-year period. The 2020/2021 SAHPRA Annual Report showed that 78% of the backlog had been cleared by March 2021 (SAHPRA, 2021). Of 5 320 applications for the registration of medicines, 2 819 (53%) had been finalised. Of 7 440 variation applications, 7 185 (96%) had been cleared. Of 38 new GMP licence applications, 29 (74%) had been issued. Of these 29 new GMP licences, 17 (59%) were issued within 125 working days of receipt of an application.
The approach taken by SAHPRA to clear its inherited backlog of work required a fundamental re-engineering of its procedures and processes, and this new methodology and approach was also introduced into SAHPRA’s ‘business as usual’ work.
SAHPRA is responsible for the monitoring, detection, assessment, understanding and prevention of adverse effects or any other medicine-related problems. An important aspect of pharmacovigilance comprises the systems and processes that holders of certificates of registration employ to ensure that safety-related data is collected, analysed and reported, with mitigations, corrective and preventive actions where required. SAHPRA aims to strengthen capacity within the inspectorate to assess the pharmacovigilance systems of holders of certificates of registration against established guidelines. By 2020, out of the 86 health product safety signals identified, all 86 (100%) had been investigated and finalised (SAHPRA, 2021). Of the 86 health product safety signals actioned, 37 (43%) were actioned within 20 working days.
With the numbers of new products, new technologies and new manufacturers continuously expanding, there is an urgent need to focus on a strengthened approach to post-marketing surveillance and vigilance to ensure that medicines and medical devices are safe and of good quality once introduced into the marketplace. Proactive post-market surveillance is required to reduce the risk of substandard or falsified medicines entering the local market. SAHPRA does not operate its own quality laboratory, and relies on contracted capacity. It also does not yet report on the number of products identified as potentially problematic.
The introduction of the various information technology initiatives has allowed employees to work remotely during the COVID-19 pandemic and has resulted in increased productivity for core business activities. SAHPRA has made significant strides in partnering with relevant stakeholders to reach the public through its public awareness programmes, including providing information on new therapeutics, regulatory approaches for various health products as well as health products safety. The Authority’s redesigned website, use of social media and other communication tools has positioned it as a trusted source of information. The key contributions have been the use of rolling reviews, tied to reliance on section 21 approval, to enable conditional access to COVID-19 vaccines even as the data required for full registration were being developed and submitted. SAHPRA approval has also enabled access to quality-assured IVDs, protecting the health system and the public from exposure to sub-standard products.
In the period 2015–2020, the public sector has continued to rely on the existing structures for the selection of essential medicines. The NDoH Essential Drugs Programme (EDP) provides the secretariat for the ministerially appointed National Essential Medicines List Committee (NEMLC), which is supported by three expert review committees, each focused on a level of care (combined primary health care (PHC) and adult hospital, paediatric hospital and tertiary/quaternary care). The NEMLC continually updates and refines the national Essential Medicines List (EML) and Standard Treatment Guidelines (STGs). The selection of essential medicines is based on assessment of available evidence for efficacy, safety, cost-effectiveness and
affordability. The EML is organised and published per level of care (primary, secondary and tertiary/quaternary), and lists those medicines that should be available in the public health system. There are associated STGs for primary and secondary levels of care, providing guidance to health care professionals. In the 2015–2020 period, updated editions of the Paediatric Hospital EML/STGs were issued in 2017, of the Adult Hospital EML/STGs in 2019, and of the Primary Health Care EML/STGs in 2020. Rather than being issued in printed form,these documents are available on the Knowledge Hub (https://www.knowledgehub.org.za/) and also as a mobile application.
One of the ongoing challenges to the entire medicines selection process is fiscal federalism. Although developed at the national level, the EML/STGs are not automatically applicable in the provinces. They remain subject to agreed cooperative governance provisions, as negotiated in the National Health Council. However, the NDoH has limited leverage, except where specific programmes (such as the antiretroviral treatment programme) are funded by conditional grants from the national budget. The provinces retain considerable autonomy in relation to expenditure funded from the equitable share allocation from the fiscus. The other major challenge is the coordination of selection and procurement processes. Although individual chapters of the EML/STGs are now updated, once approved by NEMLC, rather than waiting for an entire ‘book’ to be completed that does not address the problem of the set tender cycles for particular medicine types or therapeutic groups, newly selected medicines may not be available immediately, and medicines that have been replaced or removed from the EML/STGs may still be subject to ongoing contractual commitments to procure.
In response to the COVID-19 pandemic, a sub-committee of the NEMLC was created and a process of rapid reviews developed (Leong et al., 2020). These rapid reviews, which are now produced by the NEML Ministerial Advisory Committee (MAC) on COVID-19 therapeutics, are placed in the public domain (http://www.health.gov. za/covid-19-rapid-reviews/) and inform the development of the national guidelines for the management of COVID-19. The rapid review process enabled the refinement of an evidence-to-decision (EtD) framework, which documented the basis for each recommendation. Elements considered in the EtD were the scale of health benefits and harms and the certainty of the evidence for each element, the resource implications, eq uity considerations, acceptability and feasibility (Leong et al., 2021).
The promise of health technology assessment
Health technology assessment has been defined as ‘a multidisciplinary process that uses explicit methods to determine the value of a health technology at different points in its lifecycle’ (O’Rourke et al., 2020). The definition also states that the ‘purpose is to inform decision-making in order to promote an equitable, efficient, and high-quality health system’. Health technology assessment has been identified as a key enabler of universal health coverage (UHC) (Wirtz et al., 2017).
Although expected to be an important part of the process for determining the benefit package for National Health Insurance (NHI) in South Africa, HTA processes in South Africa remain fragmented (Siegfried et al., 2017; Wilkinson et al.,
2022). The National Health Insurance Bill (Bill 11 of 2019), which is currently before Parliament, makes mention of various structures that will rely on HTA. The description of the Benefits Advisory Committee (to be entrusted with developing ‘detailed and cost-effective treatment guidelines’) and the Office of Health Products Procurement (tasked to ‘determine the selection of health-related products to be procured’, ‘develop a national health products list’ and ‘coordinate the supply chain management process and price negotiations for health related products’) has been described as confusing (Gray & Vawda, 2019). Further, it was pointed out that the Bill defines ‘health-related products’ as excluding medicines and medical devices, but that ‘health products’ are not defined, whereas ‘health goods’ are, and appear to include medicines and medical devices. Lastly, the Health Care Benefits Pricing Committee must ‘recommend the prices of health service benefits to the Fund’. Section 38(4) of the Bill describes the selection process as follows: ‘The Office of Health Products Procurement must support the Benefits Advisory Committee in the development and maintenance of the Formulary, comprised of the Essential Medicine List and Essential Equipment List as well as a list of health-related products used in the delivery of health care services as approved by the Minister in consultation with the National Health Council and the Fund’. Congruence with the proposals made by the Competition Commission’s Health Market Inquiry (HMI) in 2019 is also unclear (Competition Commission, 2019). The HMI proposed an independent supply-side regulator for health care, as well as an Outcome Measurement and Reporting Organisation (OMRO). The OMRO is described as ‘a platform for providers, patients and all other stakeholders in the provision of healthcare to generate patient-centred and scientifically robust information on outcomes of healthcare’.
This last proposal highlights a key weakness of current medicines selection and nascent HTA processes – the lack of provision for public participation. The same could be said of SAHPRA, which is endeavouring to communicate more directly with the public, but has as yet not explored the potential role of patients, patient organisations and the general public in regulatory processes. Transparency has an inevitable and virtuous consequence, namely, increased demands for access and engagement, and a ‘voice’ in decision-making processes.
The NHI Bill also includes consequent amendments to other legislation. One of the proposed amendments would change the definition of the Single Exit Price (SEP) in section 22G of the Medicines and Related Substances Act from the only price at which manufacturers shall sell medicines ‘to any person other than the State’ to read ‘to the National Health Insurance Fund …. or any other person’. This change, if effected, would have enormous consequences for the current strict separation between state stock procured on contract and private sector medicines.
The first health objective in the 1996 NDP was ‘to ensure the availability and accessibility of essential drugs to all citizens’. Significant successes have been achieved in expanding access to treatment and care services for priority public health diseases, including HIV, through task shifting initiatives (see Chapter on National Health Programmes).
An ongoing challenge for the country is ensuring that its workforce is capacitated to handle the demands of service delivery in a changing environment with a large disease burden. The ongoing shortage of pharmacy personnel in the country, particularly in the public sector, has created significant challenges for the delivery of pharmaceutical services, with supply chain disruptions, long waiting times and delays becoming the norm, especially at high-volume facilities. Whilst it is unlikely that the human resources issues in pharmaceutical services will change appreciably in the near future, strategies are needed to ensure the best possible utilisation of existing pharmacy personnel to provide quality pharmaceutical services.
The NDoH has implemented a number of initiatives aimed at addressing some of these challenges, including implementation of core standards for service delivery, improving coordination of district health services, strengthening PHC services, and integrating the management of chronic diseases. In addition, current initiatives to strengthen the medicines supply chain, implement information management systems, and centralise medicine distribution and dispensing, are also intended to improve availability and access to medicines. These strategies are closely aligned with government’s universal health care objectives under the planned NHI. The NDoH continues to encourage engagement with private sector providers and partners to support efforts at developing best practice service delivery models, particularly for chronic disease patients.
Between 2015 and 2020, a number of reforms were implemented, aimed at improving the availability of medicines at public sector health establishments. These included the establishment of the National Surveillance Centre (NSC), the introduction of the Stock Visibility System (SVS) and the roll-out of the RxSolution stock management system.
The NSC was conceptualised in 2015 to provide visibility of medicine availability throughout the public sector supply chain, coupled with key performance indicators. Medicine availability is measured at various levels in the supply chain – provincial depots, hospitals, community health centres and PHC clinics. Data is also monitored at Centralised Chronic Medicine Dispensing and Distribution (CCMDD) service providers, as well as other health establishments that provide services on behalf of the public sector. To assist in monitoring and evaluating the performance of suppliers, medicine availability is monitored at the level of the pharmaceutical manufacturers who are contracted via transversal contracts to supply medicines to the state. Given the
variety of systems operated in different provinces, the NSC needs to draw on a variety of data sources, shown in Table 6.1. One of the supply chain challenges highlighted by the introduction of the NSC is the lack of a uniform set of master data relating to the medicines used in the public sector. The Medicine Master Data System (MMDS), which is under development, will provide a centralised, uniform set of data to support improved efficiencies at all levels and facilitate visibility via the NSC.
Supplier Management (PAT, Age Analysis)
Provincial warehouses
Hospitals, community health centres and some PHC clinics
PHC clinics
CCMDD and other providers of health care services on behalf of the state
RSA Pharma (supported by CHAI)
MEDSAS, gCommerce, Oracle, PDSX
RxSolution and other electronic stock management systems (ESMS)
SVS
Various ESMS in use by service providers
The information in the NSC is visualised on 154 dashboards, including an integrated dashboard which consolidates all provincial medicine availability views. Users are able to drill down to district and facility level, per province, and can also access the supplier performance dashboard. Root cause analyses can be undertaken to determine reasons for stock shortages identified and apply escalation procedures at health establishment, district/sub-district, provincial or national level, to enable appropriate action where needed. Escalation processes include confirmation of whether the medicine is actually on the formulary of the relevant health establishment, whether an order has indeed been placed, whether stock can be borrowed from another health establishment or whether an alternative medicine is available for use. The NSC is thus able to support effective and informed decision-making, including mitigation of challenges related to medicine availability across the supply chain. Accountable process owners are able to monitor medicine availability routinely and take preventive and corrective action as needed.
Reporting to the NSC has been included in the Annual Performance Plan of the NDoH, with targets related to the number of sites reporting being monitored. In addition, reporting is aligned to the Ideal Clinic framework. By the end of 2020, 3 783 facilities were reporting stock availability to the NSC. There was also an increase in NSC reporting compliance, improving from 80% in November 2019 to 93% in September 2020. Enhanced utilisation of the NSC was one of the unexpected outcomes of the COVID-19 outbreak, with stakeholders embracing the ability to use the NSC to monitor availability of medicines used in the management of COVID-19 as well as those used in the management of chronic conditions, while also providing data to support supply chain planning. In the absence of patient-level consumption data, optimised minimum and maximum stock levels are being calculated and loaded onto RxSolution and SVS.
The SVS was developed to monitor medication stock on hand at PHC level and is a web-based tool with a mobile application used to capture and monitor medicine availability. The tool is an early warning system to support better management of stock availability for essential medicines, particularly those used in HIV and tuberculosis. Each health establishment using the system is allocated a smartphone with the application pre-loaded. The application is designed to work even in remote areas. The data captured is synchronised in real time to a cloud-based server, where it is available to view on the designated SVS web portal by approved users as well as being visualised on the NSC. The portal generates automated emails and short messages (SMSs) that enable web users at all levels of the supply chain to monitor and manage medicine availability at facilities under their control. The SVS was first introduced to 703 sites in 2014, increasing to 3 321 by 2020.
A key finding highlighted in the 2010 Medical Products Technical Task Team (MPTTT) report was that South Africa lacked the capacity to determine a national pharmaceutical budget necessary to address its health needs (MPTTT, 2010). In 2018, the NDoH commenced with the development of a new demand planning process and set of tools, which aimed at improving future medicine demand modelling at national and provincial levels, and the forecasting that underpins the tender system. The new approach was first rolled out in two provinces, with an additional two provinces using the new process in 2019. Challenges relating to pharmaceutical budgets were again highlighted at the Presidential Health Summit held in 2019. One of the immediate actions identified was ‘to ring-fence pharmaceutical budgets and insulate them from being overridden to avoid budgets being redirected to non-medical expenditure which result in stockouts’ (Presidency, 2018). Although some progress has been achieved in the budgeting process for medicines, limited progress has been made in ring-fencing the pharmaceutical budget as recommended by the Presidential Summit Commission.
COVID-19 has placed additional pressure on the public sector medicines supply chain. Among the factors that impacted the supply chain were the lockdowns in countries such as India and China from which many medicines, medical devices, active pharmaceutical ingredients and excipients used in the manufacture of medicines are im ported. An additional challenge was the uncertainty early in the pandemic regarding which medicines would be required for the management of COVID-19 at the various levels of care. Patients at most risk of complications from COVID-19 needed continued access to medicines, with minimal visits to health establishments. The NDoH worked with various implementing partners including the USAID-funded Global Health Supply Chain – Technical Assistance programme, CHAI, and the Africa Resource Centre to respond to changes in the demand for medicines. The first step was to establish a preliminary list of items required for the management of patients presenting with COVID-19, as well as those items where supply challenges were being experienced or were anticipated. Critical care specialists provided input regarding global and local trends and insight into the selection of medicines. The national COVID-19 EPI modelling team provided data on expected patient projections. These inputs were brought together to add a volume lift to the standard baseline forecasts already prepared for all nine provinces. The first demand forecast was published by the end
of March 2020. The forecast was updated weekly until the situation stabilised, and then every two weeks thereafter, based on three components – anticipated medicine requirements, patient projections, and baseline demand forecasts. These were adjusted to take the number of sector patients into account and the duration of hospital stay, updated as new information became available. By the beginning of April 2020, a replenishment planning tool was in use to determine the shortfall in supply of COVID-19 priority items as well as those medicines needed by patients with chronic diseases. An important consideration was that in many instances patients were recipients of multi-month dispensing, as more patients were placed on the CCMDD programme and the length of validity of a prescription was extended to 12 months by means of an exclusion notice published in terms of section 36 of the Medicines Act. The output from the tool was a replenishment plan at the national and provincial levels. This model informed the volumes of medicines that needed to be sourced to fulfil the forecasted demand, taking the stock-on-hand at depots and health establishments and supplier pipeline into account. The recommended orders were shared with provinces to help inform the orders that the provinces needed to place on suppliers. In cases where supply was severely constrained, allocations per province were done. By the end of April 2020, COVID-19 dashboards were published on the NSC providing stakeholders with information about the availability and location of medicines on the COVID-19 priority list. Reporting compliance was also monitored carefully with follow-up taking place as needed. These interventions resulted in a steady supply of medicines in the country despite the challenges caused by the pandemic.
Several early initiatives to improve access to chronic medicines were piloted and implemented in a number of provinces, including using spaced, fast-lane appointments, where chronic medications were pre-dispensed for a patient on an appointment schedule or delivered to a location closest to the patient. Both the Western Cape and Gauteng provinces had also implemented centralised dispensing units (CDUs) that distributed packaged medicines to health facilities for collection by patients (Magadzire et al., 2015).
With funding from the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM), the NDoH implemented the CCMDD programme in 2014, initially in the 11 NHI pilot districts. The programme was aimed at increasing access to medicines, particularly for patients on chronic medication, while decongesting public sector clinics. The programme was implemented as an NHI initiative, with centralised dispensing operations and distribution contracted to private providers. Packaged medicine parcels were distributed for collection to a health facility via a fast lane or adherence club (facility pick-up point (PUP)), or other convenient external PUP identified in the community or at private sector pharmacies (Liu et al., 2021).
The CCMDD can be characterised as a form of differentiated service delivery. HIV treatment programmes have been challenged to manage an increasingly diverse group of patients’ needs as national guidelines have evolved. The need to ensure both long-term adherence and retention in care demands differentiated service delivery options that suit the needs of patients. The CCMDD programme was expanded as a national programme in 2016, in eight provinces and 46 districts, excluding the Western Cape. More importantly, it was implemented as part of the minimum package of interventions to support linkage to care, adherence and retention in care based on
patients’ needs and context. By October 2019, there had been a significant increase in the number of public health establishments enrolled on the CCMDD programme (3 436 in total) and 2 037 external PUPs, with 2.99 million registered patients, of which 2.07 million were active. A total of 76% of active patients were on antiretroviral therapy and 24% on medicines for non-communicable diseases. As more alternative external PUPs are contracted, patients are provided with more convenient options for collecting their medicines closer to their homes or places of work. The CCMDD programme also offers opportunities for patients to have their medicine parcels delivered to their homes, either through a contracted bicycle model or by a community health worker as part of the Ward-Based Outreach Teams (WBOTs).
A further two technological innovations supporting differentiated service delivery models have been trialled – the remote automated dispensing unit (Pharmacy Dispensing Unit or PDUTM) and smart locker systems (e.g., Collect & GoTM and ‘Pelebox’).
The PDUTM, developed and piloted at fixed sites in Gauteng and the Free State by Right to Care, used robotic automation integrated with cloud-based information systems, SMS messaging and telepharmacy support. The system enabled real-time dispensing of prescriptions and allowed public sector patients to collect their chronic medication from any of a number of conveniently located sites in shopping malls, with extended access to services provided after hours, including weekends and public holidays (Firnhaber et al., 2018). Despite high levels of satisfaction from users, the technology was best suited to high-volume facilities and urban centres given the infrastructure requirements (trained support staff, logistics and IT systems, network and electricity) needed and dependence on high utilisation rates for cost-efficiencies (Strydom et al., 2018).
Integrated smart lockers, implemented by Right-ePharmacy and Technovera, were also expanded to facilitate collection of safely stored, pre-dispensed medicine parcels under the CCMDD programme. Patients receive a one-time-PIN (OTP) via SMS, enabling access to the locker. Smart lockers were also COVID-19 friendly in that patients do not have to queue or wait to collect their medicine parcels and support personnel are not required.
The scale-up of the Ideal Clinic Realisation and Maintenance (ICRM) programme also introduced a package of services to improve process flows at facilities as well as quality of clinical care. Scheduling of patient appointments enabled pre-dispensing of patients’ prescriptions which could be supplied from the facility pharmacy, a dedicated CDU or by the CCMDD programme.
The NDoH has embarked on a re-branding campaign intended to improve awareness of the CCMDD programme, making it more relatable to a larger audience. The campaign was branded DABLAPMEDS, a colloquial term for ‘shortcut’, making reference to CCMDD as a timesaving method for chronic medication collection.
Overall, the CCMDD programme has adapted quickly to resolve some of the early implementation problems. However, infrastructure challenges such as network and connectivity issues continue to hamper implementation of web-based platforms to enable online patient registration at health facilities, electronic submission of prescriptions and scanning capability for medicine parcels received and issued at collection points. Additionally, improved systems for prescriptions renewal, multi-month dispensing, expanding differentiated delivery programmes for rural communities and better regulation of private pharmacies to ensure confidentiality and flexible collection times are still needed.
During the COVID-19 pandemic, the NDoH expanded the eligibility criteria for differentiated models of care to strengthen linkage, adherence and retention in care. Extending the validity of chronic medicine prescriptions during this period enabled reduced visits to health facilities, limiting contact and protecting both patients and health care workers. Patients were also encouraged to collect their medicine parcels at external collection points, including through expanding availability of smart collection lockers, as these remained accessible during lockdown periods.
Despite the publication of the WHO Global Strategy for Containment of Antimicrobial Resistance (AMR) in 2001, the slow and fragmented implementation of the recommended interventions in countries continue to contribute to the inadequate response of slowing the spread of AMR (WHO, 2001). Nonetheless, the publication of the Global Action Plan (GAP) has improved the visibility of AMR on a global scale (Leung et al., 2011).
South Africa’s National Action Plan, the Antimicrobial Resistance National Strategy Framework 2018–2024, has embraced a ‘One Health’ approach in an attempt to overcome the fragmented approach in human and animal health, across the public and private sectors (NDoH, 2017). The 2018 strategy updated a 2014 version, incorporating the South African Veterinary Strategy 2016–2026, developed by the then Department of Agriculture, Fisheries and Forestry. An intersectoral Ministerial Advisory Committee (MAC) on AMR was appointed, which drew from both human and animal health sectors. The MAC-AMR established Surveillance, Education, One Health Stewardship, and Infection Prevention and Control Technical Working Groups.
An example of multisectoral action was provided by the efforts to improve the use of colistin, a last-resort antimicrobial used in both human and animal health (Mendelson et al., 2016). A multisectoral, multidisciplinary working group was established in 2016 co-chaired by the MAC-AMR and MCC chairpersons. The working group reviewed the use of colistin in both humans and animals and made various recommendations, including supporting restricting the use of colistin only on the basis of laboratory-confirmed sensitivity testing. The South African Veterinary Council, at the time, also warned veterinarians that any conduct contrary to these recommendations would be considered unprofessional conduct.
The MAC-AMR established two National Training Centres in 2016 to provide health care workers with practical tools required to set up antimicrobial stewardship (AMS) structures, and provide an alternative to the conventional model that relied on infectious disease specialists or clinical microbiologists (Brink, 2017). The AMS model adopted in South Africa needed to take account of the application of task shifting, specifically nurse prescribing at PHC level (Chetty et al., 2019). Guidelines have been published, providing implementers with practical tools to establish robust AMS programmes using quality improvement methodologies (NDoH, 2017b; NDoH, 2018; NDoH, 2019; NDoH, 2019b). Provincial AMR workshops have provided an opportunity for shared learning, encouraging adoption and implementation of best practices. An online AMR module has been targeted at health care workers in both the public and private sectors, in both human and animal health. Engagement is continuing
with all statutory health councils to develop standardised AMR training programmes in the undergraduate curricula for all health care professionals in human and animal sectors, to address the knowledge gaps identified (Chetty et al., 2019). Under the leadership of the MAC-AMR, the Infection Prevention and Control (IPC) working group was established to update the National Infection Prevention and Control Policy and Strategy (2007) and align it to the WHO core components. In 2020, the National Health Council approved the IPC strategy framework, and the practical manual developed to guide health care workers to successfully implement IPC in clinical settings.
South Africa has well-developed surveillance systems for AMR. Programmes operated by the National Institute for Communicable Diseases (NICD) include the Group for Enteric, Respiratory and Meningeal Disease Surveillance in South Africa (GERMS-SA) and the Centre for Healthcare-Associated Infections, Antimicrobial Resistance and Mycoses, which tracks blood culture isolates at sentinel sites for Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter species (the ESKAPE pathogens). The NICD has published these data as percentage-resistance heat maps, disaggregated to provincial and district levels. Consolidation of public and private sector data at national level has been prioritised by the MAC-AMR, and memoranda of understanding have been concluded between the NDoH and private sector laboratories. South Africa contributes some resistance data to the WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS). Some antimicrobial consumption data were provided in 2017 (Shellack et al., 2017), and included in a national report produced in 2018, disaggregated by AWaRe (access, watch and restrict) category (NDoH, 2018). South Africa has not yet provided antimicrobial consumption data to GLASS. COVID-19 has exposed the limitations of existing antimicrobial consumption surveillance, with only national data on volumes of antimicrobials (such as azithromycin) being easily accessible (Leong et al., 2021). Disaggregating data to provincial, district and facility level, especially across both the public and private sectors, remains challenging.
In order to raise awareness of AMR and mitigate inappropriate antimicrobial use, the NDoH added the World Antibiotic Awareness Week (WAAW), now World Antimicrobial Awareness Week (WAAW), to the South African health calendar, which runs from 18–24 of November every year. Through the UK–SA twinning programme, a collaboration with Public Health England, the NDoH launched the Antibiotic Guardian campaign, with a South African-specific website (www.AntibiocGuardian.com/ South-Africa) developed to host pledges specific to the South African context for human health and veterinary professionals. In 2019, the Minister of Health took a public pledge to become an antibiotic guardian.
As described in this chapter, the process of reform of the pharmaceutical sector, first initiated with the publication of the NDP in 1996, continues apace. Fundamental changes have been made to the operating model of the NMRA, with the establishment of SAHPRA in 2018. Several innovations have been introduced to improve the visibility of medicines availability in the public sector, but these remain invisible to the general public. That there is still concern about stockouts is evident from civil society efforts, such as the Ritshidze reports on the performance of the public health sectors in all of the provinces apart from the Western Cape (https://ritshidze. org.za/). The limitations of existing methods are evident in the paucity of data, at disaggregated and patient level, regarding antimicrobial consumption. Antimicrobial consumption in the agricultural sector remains poorly characterised. As efforts progress to rewrite the Medicines Act, attention will need to be paid to the appropriate regulation of medicines used in animals. The following specific recommendations in the areas of focus are offered:
SAHPRA: The Authority remains severely underfunded for its expanded mandate and the demands of maturity level 3. Overcoming the constraints of lack of access to specialist regulatory expertise will demand greater use of reliance models, especially for the assessment of applications for the registration of complex new chemical and biological entities. The legislative reform process needs to be accelerated, specifically to address the relationship with the NDoH, the necessary amendments to the Hazardous Substances Act, the co-regulatory approach to be applied with the National Nuclear Regulator, and the regulation of medicines for animal use (in veterinary care and in agriculture). Intersectoral coordination will be key. An equity focus is needed, especially in relation to methods to prioritise particular applications and ensure that they are expedited. Improving transparency of the entire regulatory enterprise is essential.
Medicines availability: Although there have been major advances made in relation to visibility of medicines availability data in the public sector, consideration needs to be paid to how these can be made patient-accessible and patient-friendly.
Access to chronic medication: The CCMDD programme has enabled a differentiated service delivery approach to chronic medication supply. The programme will need to continue evolving, making it more equitable, in particular for rural areas. However, as the division between state and private stock is altered by NHI, the very raison d’être of a centralised dispensing model will need to be carefully considered.
AMR: South Africa’s national action plan is well designed, on paper, but requires additional financial and human resources to be effectively implemented. Securing funding through the National Treasury is key and developing a business case for AMR is urgently needed. Particular attention needs to be paid to developing routine data systems that can report on antimicrobial consumption at all levels, and across both the public and private sector, in human and animal health.
Affordable Medicines Trust and Others v Minister of Health and Another; 2006 (3) SA 247 (CC).
African Union (2019). Treaty for the Establishment of the African Medicines Agency. https://au.int/sites/default/files/treaties/36892-treaty-0069_-_ama_treaty_e. pdf.
Azatyan S (2009). Overview on Medicines Regulation: Regulatory Cooperation and Harmonization in the Focus. Presented at: Forecasting global ARV demand 20102012 and improving access to adult and pediatric treatment. World Health Organization, Geneva. https://www.who.int/hiv/amds/who_overview_medicines_reg ulation_azatyan.pdf.
Brink A (2016). Antimicrobial Stewardship: From Theory to Practice. https://www. ampath.co.za/pdfs/antibiotic-guidelines/Antimicrobial-Stewardship.pdf.
Chetty S, Reddy M, Ramsamy Y, Naidoo A, Essack S. Antimicrobial stewardship in South Africa: a scoping review of the published literature. JAC-Antimicrobial Resistance. 2019;1(3): dlz060. doi: 10.1093/jacamr/dlz060.
Competition Commission South Africa. Health Market Inquiry. Final Findings and Recommendations Report. September 2019. https://www.compcom.co.za/ wp-content/uploads/2020/01/Final-Findings-and-recommendations-reportHealth-Market-Inquiry.pdf.
Firnhaber K, Banoo S, Mokobori M, Strydom B. Creating the pharmacies of the future – Innovation through the appropriate use of technology. African Journal of Public Sector Development and Governance. 2018;1(1):76–87. doi: 10.10520/ EJC-1724b50ee5.
Gray A, Suleman F, Pharasi B. The National Drug Policy – 20 years and still going? In: Padarath A, Barron P, editors. South African Health Review 2017. Health Systems Trust, Durban.
Gray A, Vawda Y. Health Legislation and Policy. In: Moeti T, Padarath A, editors. South African Health Review 2019. Health Systems Trust, Durban.
Green-Thompson Report (2008). Report of the Ministerial Task Team on the restructuring of Medicines Regulatory Affairs and Medicines Control Council.
Keyter A, Banoo S, Salek S, Walker S. The South African regulatory system: past, present, and future. Front Pharmacol. 2018;9:1407. doi: 10.3389/fphar.2018.01407
Leng HMJ, Pollock AM, Sanders D. The impact of the Medicines Control Council backlog and fast-track review system on access to innovative and new generic and biosimilar medicines of public health importance in South Africa. S Afr Med J 2016;106(4):350–3. doi: 10.7196/SAMJ.2016.v106i4.10237.
Leung E, Weil DE, Raviglione M, Nakatani H, on behalf of the World Health Organization World Health Day Antimicrobial Resistance Technical Working Group. The WHO policy package to combat antimicrobial resistance. WHO Bulletin. 2011;89(5):390–392. doi: 10.2471/BLT.11.088435.
Leong TD, McGee SM, Gray AL, de Waal R, Kredo T, Cohen K, et al. Essential medicine selection during the COVID-19 pandemic: Enabling access in uncharted territory. South African Medical Journal. 2020;110(11):1077–80. doi: 10.7196/SAMJ.2020.v110i11.15271.
Leong TD, Gray AL, Kredo T, de Waal R, Cohen K, Parrish AG, Dawood H. Managing therapeutic uncertainty in the COVID-19 pandemic: rapid evidence syntheses and transparent decision-making. In Govender K, George G, Padarath A, Moeti T (eds). South African Health Review 2021 (pp 41–49). Health Systems Trust, Durban (ISSN 1025-1715; ISBN 978-1-928479-09-3).
Liu L, Christie S, Munsamy M et al.. Expansion of a national differentiated service delivery model to support people living with HIV and other chronic conditions in South Africa: a descriptive analysis. BMC Health Serv Res. 2021;21:463. doi. org/10.1186/s12913-021-06450-z.
Magadzire BP, Marchal B, Ward K. Improving access to medicines through centralised dispensing in the public sector: a case study of the Chronic Dispensing Unit in the Western Cape Province, South Africa. BMC Health Serv Res. 2015;15:513. doi: 10.186/s12913-015-1164-x.
Medical Products Technical Task Team (MPTTT). Medicines Procurement Reform in the Public Sector: Challenges and Opportunities for Improvement of Medicines Procurement in South Africa’s Public Sector. March 2010. National Department of Health, Pretoria. http://ipasa.co.za/Downloads/Policy%20and%20Reports%20 -%20Medicines/procurement/Medicines%20Procurement%20Task%20Team%20 Report-%20Final%2029%2004%202010.pdf.
Mendelson M, Brink A, Gouws J, Mbelle N, Naidoo V, Pople T, Schellack N, van Vuuren M, Rees H, South African One Health Stewardship Sub-Committee of the Ministerial Advisory Committee on Antimicrobial Resistance. The One Health stewardship of colistin as an antibiotic of last resort for human health in South Africa. Lancet Infectious Diseases. 2016;18(9):e288–e294. doi: 10.1016/S14733099(18)30119-1.
Minister of Health (1997). White Paper on the Transformation of the Health System of South Africa. Department of Health, Pretoria.
Minister of Health and Another v New Clicks South Africa (Pty) Ltd and Others; 2006 (2) SA 311 (CC).
Minister of Health (2019). National Health Insurance Bill (Bill 11 of 2019).
Minister of Justice and Constitutional Development and Others v Prince (Clarke, Stobbs and Thorpe Intervening) (Doctors of Life International Inc as Amicus Curiae); National Director of Public Prosecutions and Others v Rubin; National Director of Public Prosecutions and Others v Acton and Others; 2018 (6) SA 393 (CC).
Minister of Mineral Resources and Energy (2021). Draft National Nuclear Regulator Amendment Bill.
Mistry v Interim National Medical and Dental Council of South Africa and Others 10; 1998 (4) SA 1127 (CC).
National Department of Health (NDoH) (2017). South African Antimicrobial Resistance National Strategy Framework: A One Health Approach 2017 – 2024. https://www.knowledgehub.org.za/elibrary/south-african-antimicrobialresistance-national-strategy-framework-one-health-approach.
National Department of Health (NDoH) (2017b). Guidelines on Implementation of the Antimicrobial Strategy in South Africa: One Health Approach & Governance. https://www.knowledgehub.org.za/elibrary/guidelines-implementationantimicrobial-strategy-south-africa-one-health-approach.
National Department of Health (NDoH) (2018). Surveillance for antimicrobial resistance and consumption of antibiotics in South Africa. https:// www.knowledgehub.org.za/system/files/elibdownloads/2020-03/AMR%20 Surveillance%20report%20South%20Africa%20-%20Nov2018.pdf.
National Department of Health (NDoH) (2019). Guidelines for the Prevention and Containment of Antimicrobial Resistance in South African Hospitals. https://www. knowledgehub.org.za/elibrary/guidelines-prevention-and-containmentantimicrobial-resistance-south-african-hospitals.
National Department of Health (NDoH) (2019b). Antimicrobial Resistance Background Document. https://www.knowledgehub.org.za/elibrary/ antimicrobial-resistance-background-document.
O’Rourke B, Oortwijn W, Schuller T. The new definition of health technology assessment: A milestone in international collaboration. International Journal of Technology Assessment in Health Care. 2020;36(3):187–90. doi: 10.1017/S0266462320000215.
Presidency of the Republic of South Africa (2018). Presidential Health Summit. Presidency of the Republic of South Africa, Pretoria.
Republic of South Africa (1973). Hazardous Substances Act (Act 15 of 1973).
Republic of South Africa (1997). Medicines and Related Substances Control Amendment Act (Act 90 of 1997).
Republic of South Africa (1998). South African Medicines and Medical Devices Regulatory Authority Act (Act 132 of 1998).
Republic of South Africa (1999). Public Finance Management Act (Act 1 of 1999).
Republic of South Africa (2002). Medicines and Related Substances Amendment Act (Act 59 of 2002).
Republic of South Africa (2008). Medicines and Related Substances Amendment Act (Act 72 of 2008).
Republic of South Africa (2015). Medicines and Related Substances Amendment Act (Act 14 of 2015).
Schellack N, Benjamin D, Brink A, Duse A, Faure K, Goff D, Mendelson M, Meyer J, Miot J, Perovic O, Pople T, Suleman F, van Vuuren M, Essack S. A situational analysis of current antimicrobial governance, regulation, and utilization in South Africa. Int J Infect Dis. 2017;64:100-106. doi: 10.1016/j.ijid.2017.09.002. Epub 2017 Sep 8.
Siegfried N, Wilkinson T, Hofman K. Where from and where to for health technology assessment in South Africa? A legal and policy landscape analysis. In: Padarath A, Barron P, editors. South African Health Review 2017. Health Systems Trust, Durban.
South African Health Products Regulatory Authority (SAHPRA) (2021). Annual Report 2020/2021. https://www.sahpra.org.za/wp-content/uploads/2021/10/ SAHPRA-202021-Annual-Report.pdf.
South African Law Reform Commission (SALRC) (2016). Statutory law revision: legislation administered by the Department of Health. Project 25: Discussion paper 145. 10 December 2016. https://www.justice.gov.za/salrc/dpapers/ dp145-prj25-DOH-01Aug2017.pdf.
South African Veterinary Association v Speaker of the National Assembly and Others; 2019 (2) BCLR 273 (CC); 2019 (3) SA 62 (CC).
Strydom B, Hendriksz F, Banoo S. Innovation to solution – the Remote Automated Dispensing Unit journey. South African Pharmaceutical Journal. 2018 July;85(3). ISSN: 2221-5875.
Vawda Y, Gray A. Transparency in medicines regulatory affairs – reclaiming missed opportunities. South African Journal of Bioethics and Law. 2017;10(2):70–4. doi: 10.7196/SAJBL.2017.v10i2.00607.
Wilkinson M, Gray AL, Wiseman R, Kredo T, Cohen K, Miot J, et al. Health technology assessment in support of National Health Insurance in South Africa. International Journal of Technology Assessment in Health Care. 2022;38(1):e44, 1–8. https://doi.org/10.1017/S0266462322000265.
Wirtz V, Hogerzeil H, Gray A, Bigdeli M, de Joncheere C, Ewen M, et al. Essential medicines for universal health coverage. Lancet. 2017;389(10067): 403–76. doi: 10.1016/S0140-6736(16)31599-9.
World Health Organization (WHO) (2001). WHO Global Strategy for Containment of Antimicrobial Resistance. https://www.who.int/drugresistance/WHO_Global_ Strategy_English.pdf.
World Health Organization (WHO) (2014). Regulatory System Strengthening for Medical Products (EB134.R17). World Health Organization, Geneva. http://apps. who.int/gb/ebwha/pdf_files/EB134/B134_R17-en.pdf.
World Health Organization (WHO) (2018). Improving the Quality of Medical Products for Universal Access. World Health Organization, Geneva. http://www.who.int/ medicines/regulation/fact-figures-qual-med/en/.
The health system inherited by the current government in 1994 was relatively well resourced for a middle-income country, yet there were significant inequalities present between the private and public sectors, and even within the latter the resources were skewed geographically as well as between levels of care. The performance of South Africa’s health system since the end of apartheid and the establishment of a democratic government in 1994 has been mixed. It has been argued that many good new policies were adopted, but implementation has been poor and inequitable access to hospital services remains a challenge in South Africa as a result of the two-tier health system (Michel et al., 2019). Currently there are approximately 814 hospitals in South Africa, of which 405 are in the public sector and 409 are in the private sector. The public health care facilities serve approximately 83% of the population, who are largely without medical insurance (Competition Commission, 2019).
Hospitals in particular are characterised by multiple resource requirements, processes and interactions, all of which operate within a broader health system context. All of these components require planning and coordination, and therefore sound hospital management at facility, provincial and national levels is essential.
A cascade of authorities starting from national, through provincial, to the facility level govern and manage hospitals. The National Department of Health (NDoH) is responsible for determining the strategic vision of the health system and for enacting policies to be implemented nationwide. The Provincial Department of Health (PDoH) is responsible for the implementation and oversight of service delivery at all facilities.
In 2011 the NDoH adopted the National Policy on Management of Hospitals to ensure effectiveness, efficiency and transparency in the management of public hospitals (NDoH, 2011). It provides directives for the classification of hospitals, which is based on their respective roles and functions, the size of communities served, the nature and level of their health service provision, and the hospitals’ accordance with national norms and standards.
Terence Carter, Tamlyn Roman, Wezile Chita, Gladys Bogoshi, Shrikant PetersIn this classification, a hierarchical relationship exists between levels of care based on the provision of a defined package of services. Regional, tertiary, central and specialised hospitals are charged with rendering specialised tertiary and quaternary services; providing specialised referral units for other hospitals; and providing a platform for the training of health workers and research. Within each hospital, management of different functional areas is organised into functional departments. These include both clinical departments and crosscutting support service departments such as the human resource, supply chain and procurement, finance and logistics departments.
The policy also makes provision for the appointment of competent and skilled hospital managers, including the Chief Executive Officer (CEO), and calls for the development of an organisational framework for accountability to communities served, including guidelines for the establishment of hospital boards.
The national vision and policies for health are interpreted through strategic plans at national and provincial levels, which not only aim to guide implementation at a functional level, but also act to promote alignment with the requirements of a national health system by coordinating the activities of actors.
More specifically, the NDoH’s Strategic Plan outlines the strategic directions to be taken by the Department over a defined period. The overall goals for national health are embedded in the strategic plan which targets, among others, improvements in quality of care, human resources and financial management. These overarching strategies provide the direction, guidelines, norms and standards to be taken into account in provincial strategic planning for health services, and prescribes what should be done at facilities, including central hospitals where relevant. The most recent NDoH Strategic Plan 2020/21–2024/25 is grounded in strengthening the health system, with specific attention to quality improvement (QI) in the provision of care, including hospitals. While human resources for health is identified as a priority, there is limited mention in this period’s strategic plan of the requirements for improved management of hospitals.
In terms of national financing, in 2019/2020, R35 billion was spent on district hospitals alone, making up 33.8% of the total district health expenditure. Add to this that central and provincial hospital services consistently contribute more than 40% to provincial health expenditure (see Figure 7.1), hospitals absorb a significant share of overall public health expenditure (Devan et al. in District Health Barometer, 2020). The implication is that the importance of making hospital services more efficient and effective cannot be ignored, given that these institutions often constitute the largest expenditure category in the health system budget.
Figure 7.1 Proportion of provincial health expenditure by programme 2004/5 – 2019/20
Source: Devan et al. in District Health Barometer 2019–2020
While the national strategy for hospitals and tertiary services ascribes overall responsibility for policies and guidelines governing the management, service standards and human resources for hospitals to the national health department, provincial needs and realities dictate the resourcing and implementation of these proposals and are thus currently the mandate of the provincial health authorities.
The challenges facing the health system were acknowledged in the National Development Plan as follows: ‘The management of the health system is centralised and top-down. Poor authority, feeble accountability, the marginalisation of clinicians, and low staff morale are characteristics of the health system’ (National Planning Commission, 2010: pg. 332). These sentiments apply to all parts of the system, including the public hospital system.
In South Africa, the capacity for hospital management has been a longstanding critical area of concern (Engelbrecht & Crisp, 2010; von Holdt, Smith et al., 2010; Gilson & Daire, 2011; Doherty, 2014; GDoH, 2014).
The health system continues to face the underdevelopment of hospital services and chronic shortage of health professionals, which in turn affects the development of hospital support services in management, operations, administration, and clinical support (Barron & Padarath, 2017). The available resources to provide quality hospital services are compromised by the burden of disease, increasing demand, reducing budgets and the impact of a high medico-legal liability (Auditor-General of South Africa, 2021).

Recent research conducted on quality variability in the health care sector points to the failure of hospital boards and management in governing their establishments as a contributing factor (Brown, 2019). While issues of management and governance may not be the only shortcoming of the system, they are certainly significant contributing factors and it is argued that they should be the starting point for planned reform (Rispel, 2016).
Steward and Wolvaardt (2019) investigated hospital management and health policy in South Africa, and in the study recommended the professionalisation of hospital management, and the promotion of competency and transparency. The study further asserted that health workers must be held accountable for their actions and that hospital boards must be regulated. This was consistent with various studies that emphasise the importance of good corporate governance in the health system to ensure quality service delivery (Fusheini, Eyles, & Goudge, 2017; Govender, Proches & Kader, 2018).
Currently, hospital management capacity is prescribed in the context of the National Policy on the Management of Public Hospitals and the Regulations Relating to the Categories of Hospitals (Government Gazette No R; 185, 2 March 2012) as prescribed by the National Health Act 61 of 2003 (NDoH, 2011; NDoH, 2012). The regulations for the hospital management policy not only define the general categories of hospitals, but also make recommendations for their management in terms of the appropriate management structures, post levels and salary scales, as well as delegations of functions.
The regulations include guidelines for the appointment of competent and skilled managers, but explicitly define the job description and minimum requirements for appointment of the hospital CEO. The educational requirement for this position is a degree or diploma in a health-related field, with a degree or diploma in management as an added advantage, and five years of management experience in the health sector.
There are no formal competencies listed for hospital managers; instead, generic competencies for public sector management are defined in the regulations for Public Service and Administration. Their application to the role of the hospital CEO was benchmarked in a competency framework developed by the Department of Public Service and Administration (DPSA, 2008), and this formed the basis of an assessment of hospital management competencies undertaken by the Development Bank of Southern Africa, which focussed on competencies related to leadership and management, organisational responsibilities, and interpersonal engagements.
Although this assessment found that many hospital CEOs were not fit for the job, and the revised policies have since led to appointments of hospital managers who meet the minimum requirement for the post, the framework used for the detailed assessment of competencies was not formally adopted.
In June 2017, the South African NDoH released its plan for a National Health Insurance (NHI) – see Chapter on Health Financing, which is a financing system intended to facilitate better access to quality and affordable health service for all South Africans (NDoH, 2017). The NHI represents the latest step in a journey towards a
Responses to improve governance of hospitals 2015–2020
public health system that would allow the entire population to realise the right to access health care services that is embedded within the South African Constitution (RSA Constitution, 1996). This plan has been designed in response to a health system that is not without challenges and will require significant reforms to, amongst other things, the management of central hospitals.
The NHI policy gazetted in June 2017 lays out the intention to make some hospitals, including central hospitals, semi-autonomous and to allow complete decentralisation of management functions. Significant decentralisation of authority and decision-making to hospital management is envisaged within the management and governance system of the NHI. The exercise of such authority must be guided by the basic values and principles governing public administration as set out in Chapter 10 of the Constitution.
In order to make these hospitals more effective, efficient and responsive, the NHI proposes that hospital managers will have ‘full delegations and decision-making powers including control over financial management, human resources management, infrastructure and technology, as well as planning and decision-making’ (NDoH, 2017: pg. 38).
This ambitious intent of the NHI recognises that there are existing gaps in ethical and values-based leadership in South Africa, which contributes to poor quality of care through lack of accountability, corruption and fraud (South African Lancet National Commission, 2019). The prevailing management culture reflects the strong emphasis on centralisation, compliance, adherence to centrally determined processes, rigid classification of tasks, and an entrenched hierarchy (Health Ministerial Task Team, 2017).
At this time, and in response to the intentions of the NHI policy, development of a revised governance model for hospitals is in progress and, while this reform has gained much traction, there are still many questions regarding the respective governance roles of the national and provincial health departments, the accountability mechanisms that will be implemented, the financing, CEO competencies and the development of hospital performance indicators (Hendricks, Buch et al., 2015; Waterhouse, Mentor-Lalu et al., 2017).
Several lessons for management of a hospital were learned during the COVID-19 pandemic. The box below reflects some of the lessons reported by the CEO of Groote Schuur Hospital, which are applicable to any hospital both during times of crisis and for effective management on a daily basis.
Box 1 Lessons on and for Management: Personal reflections of a hospital CEO
• Caring for our staff must be a top priority:
o Creating a culture of engagement, listening to and supporting the staff
• Being adaptive and responsive
• Using Artificial Intelligence, Information Technology and Information Management to do business differently
Maximise fiscal discipline and efficiency
Provide leadership
Visible leadership
Responsive leadership
Adaptive leadership
Communication, Communication, Communication
Source: Dr Bhavna Patel, Hospital Annual Operational Planning Presentation, 2021
Improved accountability is often called for as an element in improving health system performance. At first glance, the notion of better accountability seems straight forward, however, it contains a high degree of complexity. For accountability to serve effectively as an organising principle for health systems reform, conceptual and analytical clarity is required.
Using an accountability lens can: a) help to generate a system-wide perspective on health sector reform, and b) identify connections among individual improvement interventions. These results can support synergistic outcomes, enhance system performance, and contribute to sustainability.
Political/democratic accountability also relates to building trust among citizens that government acts in accordance with agreed-upon standards of probity, ethics, integrity, and professional responsibility. These standards reflect national values and culture, and bring ethical, moral, and on occasion religious issues into the accountability equation at both agency and individual levels.
The governance and accountability requirements within a decentralised management framework place a greater onus of meticulous adherence and compliance to the rules and regulations related to financial management and reporting as required by the Public Finance Management Act (PFMA) and its Regulations to be followed and observed.
In this context, the hospital board will have the responsibility of an accounting authority, which must be accountable for the purposes of the PFMA. Accounting authorities must ensure that accurate books and records are kept and that financial statements and other statutory reports are prepared. In addition to obligations contained in the PFMA, the members of the hospital board will be required to carry out their fiduciary duties in accordance with the com mon law and to meet the same obligations as directors of private sector companies.
In addition to its fiduciary responsibilities, the hospital board also has responsibility for evaluating and improving health care quality performance, setting and oversight of strategic quality priorities, promoting leadership and culture, and ensuring effective systems and processes are in place to maintain and improve quality. Such oversight responsibilities will include a quality and safety reporting framework as well as oversight of broad strategic health care quality priorities. This implies moving beyond symbolic acknowledgement of specific planned priorities into quality planning mechanisms overseen by the governing body (Brown, 2019).
Within a complex health care environment, these fiduciary and health care quality performance oversight responsibilities will require board members to have specific training in analytic capabilities and sophistication, particularly in the evolving era of ‘big data’ (Mountford & Wakefield, 2017).
Building the capacity of members of hospital boards must therefore include the ability to analyse, understand and interpret quality and safety data, and routine morbidity reporting (Mannion et al., 2015). Quality improvement is a hospital board priority. This includes balancing a short-term focus with a long-term strategic focus on QI. Critical to achieving this is using data for improvement as well as patient and staff engagement and clinical leadership (Jones et al., 2017).
One of the foundational requirements of the NHI is to ensure health facility readiness and to improve the quality of care by establishing national norms and standards and strengthening clinical governance. However, hospitals in South Africa have faced challenges from insufficient funding, inequitable human resource distribution and poorly maintained infrastructure.
In response to these challenges, and building off of the foundation previously established through the Ideal Clinic Realisation and Maintenance (ICRM) programme (see Chapter on Quality Health Care), the NDoH has developed the Ideal Hospital Realisation and Maintenance Framework (IHRM-F) to facilitate improved quality service delivery. The framework was designed to ‘serve as a benchmark mechanism to monitor Health System Strengthening activities, to improve efficiency gains in service provision and to improve patient experiences’ (NDOH, 2018).
The definition of an ideal hospital is one with:
• Good infrastructure
• Efficient patient management administration processes
• Adequate and appropriately managed staff
• Evidence-based service delivery aligned with the defined package of service for
• that level of care
• Uses patient experience feedback for continuous QI across clinical and administrtive services
• Compliance to standards for corporate governance and accountability to the community and stakeholders.
The IHRM-F framework is based on the ICRM framework which was developed in response to the challenges to providing quality primary health care services, identified by the Office of Health Standards Compliance (OHSC) in a 2013 audit.
The OHSC was created by Parliament as an independent body charged with ensuring that the health and safety of users of all health establishments are protected. Established in terms of the National Health Amendment Act of 2013, it assesses, monitors and enforces compliance by health establishments with prescribed safety norms and standards.
The IHRM-F was designed in alignment with the standards defined by the OHSC and includes both outcome and process assessment for all functional areas of the hospital. This capacitates hospital management to identify and address comprehensive service delivery challenges and benchmark performance against a standardised assessment framework.
An Ideal Hospital Manual was developed to outline the minimum requirements for a facility and to provide detailed guidance on how to assess and satisfy these requirements. A multidisciplinary team made up of clinical, support service, diagnostic and para-clinical service representatives should be appointed every year to lead the completion of the facility assessment against the Ideal Hospital framework. Each functional departmental area in the hospital is to be scored as having achieved, partially achieved or not achieved the minimum standards required and defined by the framework. On the basis of the outcome of this assessment, a facility can then be categorised as not having achieved Ideal Hospital status, or as attaining silver, gold or platinum status. The expectation is that by identifying the areas in need of intervention, the facility management is capacitated to develop and implement a QI plan that will allow for attainment of Ideal Hospital status.
The roll-out of the IHRM-F began with implementation at district hospital level, with staggered deployment to other levels of hospital care expected to follow, but was delayed due to the COVID-19 pandemic. By the start of 2022, 42% of district hospitals nationally had conducted status self-assessments and of those that were assessed, 52% did meet the requirements for Ideal Hospital status. Of this group, 43% achieved silver status, 3% gold and 2% platinum.
The lowest performing functional areas in the assessments were infrastructure, namely, the availability of essential equipment, and operational management, including disaster and emergency preparedness. The recommendation from the NDoH is to increase the number of facilities that have completed status assessments and that PDoHs use the information generated to implement QI plans.
One of the risks of poor clinical governance and poor provision of quality clinical care is the increase in medical negligence and related litigation. There has been a proliferation of medical negligence litigation against the NDoH, leading to large payouts which have put further strain on the health budget (see Chapter on Health Financing). Medical negligence impacts on access to quality health care. The Medical Protection Society estimated that ‘the long-term average claim frequency for doctors in 2015 was around 27% higher than that in 2009’, while the amounts claimed had escalated by an average of 14% per year from 2009 to 2015 (Dhai, 2015).
At a medico-legal summit in Pretoria (9–10 March 2015), Health Minister Dr Aaron Motsoaledi described these claims as reaching ‘crisis’ level: ‘The nature of the crisis is that our country is experiencing a very sharp increase – actually an explosion in medical malpractice litigation – which is not in keeping with generally known trends of negligence or malpractice’ (Kollapen et al., 2017:3).
In a report indicating medico-legal claims paid by government in each province in South Africa (presented at the summit by the acting Chief Litigation Officer of the Department of Justice and Constitutional Development), the total amount paid out for litigation in 2015 was R498 964 916.72; the Department of Health in KwaZulu-Natal led with total claims paid amounting to R153 612 355.49 and with over 5 billion rand in pending claims against the province (Kollapen et al., 2017:16; Maphumulo & Bhengu, 2019).
In 2020–21, the provincial health departments paid out R1.76 billion for medical negligence claims, while the estimated settlement value of unpaid claims at year-end was R124.15 billion (75% of the total claims against the state). Seven provincial health departments had unpaid claims at year-end that exceeded their entire operational budget for the next year (Auditor-General of South Africa, 2019).
Following the medico-legal summit, a comprehensive strategy was developed and implemented to deal with the challenges identified. Key areas of the strategy included improving overall communication and administration, dealing with occupational stress, effective clinical governance, morbidity and mortality monitoring and clinical audits, sharing the outcomes of cases of misconducts/ malpractice, and introducinga mentoring programme in all councils.
One of the key recommendations of the Ministerial Summit was the establishment of provincial medico-legal units. Such units have now been established in seven provinces and the next step is to assess the implementation and impact of these units.
Planning, budgeting, the award of funding and the financial management of a hospital are based on a cascade of laws, policies, auditing mechanisms and processes at both national and provincial levels, with sources of funding for PDoHs and their facilities, such as central hospitals, being both national and provincial.
At the level of the hospital, the responsibility for financial management is assigned to a financial manager, while the responsibility for managing the annual audit process lies with another manager. Annual budgets are prepared according to the Treasury guidelines for the annual performance plans for both national and provincial health departments. These plans identify the performance indicators and targets for the strategies that the facility will seek to achieve in the upcoming budget year, guide the budget, and form the basis of annual reports. Guidance on the structure of the annual performance plan, its targets and indicators and timeframes, and the planning, reporting and auditing processes are set out in the PFMA and the Treasury Regulations.
National Treasury awards every province an amount of funding called the provincial equitable share, which is a constitutionally required distribution of money from the na tional government to the provinces (Blecher, Kolliparna et al., 2010). It is based on a formula that aims to advance national equity.
The division of the equitable share between provinces takes into account the provinces’ need to provide basic services and therefore relates directly to the demand for education, health and welfare services (Treasury, 2016). The equitable share provided by national government to the provinces does not prescribe allocations to these service areas.
A second National Treasury allocation is made to the provinces through conditional grants earmarked for specific projects through the Division of Revenue Act No 1 of 2005 (National Treasury of RSA, 2016). Conditional grants ring-fence budgets for the provision of health services. Although there is no stipulation regarding how the funding should be distributed between organisations, the NDoH is authorised to freeze allocations when spending is slow or mismanaged (Blecher, Kolliparna et al., 2010). The conditional grants received by central hospitals include the health facility revitalisation, the national tertiary services and the health professions training and development grant.
Funding for central hospitals comes from the provincial equitable share, conditional grants and provincial finances, and in theory, the pooled funding is allocated on the basis of need. Each facility submits a projected budget to the province for consideration as part of the financial cycle, but for the most part, budgets are set by historical precedent, with marginal increases allowed to compensate for inflation.
A further source of funding is facility-generated revenue from sources such as patient fees, and although these are collected at the hospital, they cannot be retained for use at that level, and have to be returned to provincial authorities.
Given the context for financing sources, in line with international trends in improving the financial management of hospitals, the approach currently being explored is to make hospital expenditure more effective and efficient. The reform will require hospitals to move away from global budgets towards case-mix-based funding (payment by activity), so that public and private commissioning agencies or purchasers can assess the volume and quality of hospital production.
This calls for more effort on the recording, coding and detailed costing of activities, requiring the following:
a. Providing funds according to a case-based formula (typically adjusted diagnosis-related groups (DRGs)) and, increasingly, tying those payments to activity and/or performance levels
b. Improving management efficiency and accountability with the implementation of cost centre management at a decentralised level
c. Revised delegations to CEOs to be consistent with the accounting of ficer system
d. Training of CEOs and hospital managers to develop capacity to execute the new delegations.
It is envisaged that hospital financial management under an NHI system will address costing, contracting, contract management, use of DRGs and ensuring audit compliance. The use of DRGs as a fee-for-service model under the NHI for costing of health care services would impose a total overarching cost charge per event, such as an admission for a cerebrovascular accident, myocardial infarction or mid-shaft femur fracture requiring operative intervention. Such charges would need to be costed based on an accurate determination of all cost inputs related to a patient’s hospital stay and would also need to factor in the variability of patient management, frequency of presentations and possible resulting economies of scale. Accurate costing is vital to mitigate the risk borne by funders and providers for variability in cost beyond the amount set for remuneration.
Medium- to long-term workforce planning and management for the whole national health system is the responsibility of the NDoH and is governed by the Human Resources for Health (HRH) strategy (NDoH, 2011) (see Chapter on Human Resources for Health). However, the PDoH is responsible for operationalising that plan, which is then implemented by the hospital.
In this respect, while the human resources plan for the hospital is determined externally and is implemented through a centralised decision process with which the hospital must comply, there is some opportunity for flexibility in human resources management at the hospital.
One major challenge is that, at present, the determination of the human resource capacity of the hospital is based on historical establishments and not on empirical data of the current need for health services. In 2009, consultants were contracted by the Gauteng Department of Health to determine an ideal staff structure for all provincial hospitals based on number of beds per hospital. To date, this organisational plan has not been updated to reflect changing demand for services and the related human resource requirement.
However, while the workforce planning for the hospital resides in the provincial authority, which also determines the staff complement and post structure for the facility, where sufficient motivation is provided based on function and purpose, and availability of budget, recommendations may be made for additional staff, or for a shift in staffing positions.
Across the national health system, there is currently a process being led by the NDoH to develop staffing norms and standards using the Workload Indicators of Staffing Need (WISN) tool (WHO, 2014). This tool determines health worker requirement by type and workload, and provides the basis for management of staff establishment. However, until the outcomes of the use of this tool have been finalised, there are no generalisable staffing norms and standards available.
The absence of such national norms and standards does not directly influence the audit practice at the hospital, as they would not inform the annual monitoring conducted by the Auditor-General, whose oversight responsibility is outlined in the section that follows and whose remit largely applies to ensuring compliance with the broad human resources policies and the regulatory mandates.
The state of many health care facilities results in ever-decreasing faith in the health care system. Millions of rands over many years have been dedicated to infrastructural improvements and maintenance (see Chapter on Infrastructure).
The HSR notes that the NDoH ‘has a health infrastructure plan, but to date the country has had neither the expertise nor adequate funding to implement the plan. In some cases, health infrastructure construction that has been successfully completed has either cost more than the initial budgeted amount or facilities have been constructed that fail to meet the need for the service required’. It also states that in most cases there is insufficient capacity for project implementation, monitoring and evaluation.
Over the next three years, R19.2 billion has been allocated to the health facility revitalisation grant and a further R4.3 billion has been allocated to the health facility revitalisation component of the NHI indirect grant. Additional allocations have been added to fund the new academic hospital in Polokwane. However, in order for provinces to access this grant, a two-year planning process is needed in which provinces are assessed and required to obtain a minimum score of 60% in order to qualify for the incentive. Only three provinces qualified in the 2019/20 financial year, these being KwaZulu-Natal, Eastern Cape and Western Cape.
South Africa continues to be plagued by a growing burden of disease, worsening social and commercial determinants of health, and an access-inequitable two-tier health care system, now compounded by the systemic disruptions imposed by the COVID-19 pandemic.
This has in turn led to a sharper diminishment of the resource envelope for funding of health care facilities in the foreseeable future. Within this difficult financial context, it is even more important to bring to fruition the initiatives aimed at defining and capacitating structures for the efficient, decentralised management of health care services.
Upon this foundation, further improvement in the quality and efficiency of health care services is predicated on an ethical leadership which gives spirit to the practice of corporate and clinical governance through continuous improvement and commitment to monitoring and evaluation of inputs, processes and outcomes.
This in turn will allow for transparent interactions with served communities, and encourage engagement with, and ownership of public health care services, to create shared resources for health generation. This will also decrease the drain on the fiscus represented by considerable medico-legal litigation, linked to poor-quality health care and a lack of trust from communities.
An overarching coordinated national commitment to quality improvement and continuous learning, both in the clinical and corporate running of health care services is required to effect the necessary changes to the system.
Auditor-General of South Africa. 2021. Consolidated General Report National and Provincial Departments. Pretoria: Auditor-General of South Africa.
Barron P, Padarath, A. Twenty years of the South African Health Review. South African Health Review. 2017(1):1-10.
Brown A. Understanding corporate governance of Health Care Quality in eight Public Hospitals in Australia. Brown BMC Health Services Research. 2019;19:725.
Competition Commission South Africa, 2019. Health Market Inquiry. Pretoria: Competition Commission of South Africa.
Conmy A. South African health care system analysis. Public Health Review. 2018;1(1). Department of Public Enterprises. Protocol on Corporate Governance in the Public Sector. Pretoria: National Government of South Africa. 2002.
Dhai A. Medico-legal litigation: Balancing spiralling costs with fair compensation. South African Journal of Bioethics and Law. 2015;8(1):2-3.
Fetter RB, Freeman JL. Diagnosis related groups: product line management within hospitals. Academy of Management Review. 1986;11(1):41-54.
Fusheini A, Eyles J, Goudge J. The place of private care governance in the South African health care system. The International Journal of Health Planning and Management. 2018;33(4):e999-e1013.
Govender S, Proches CNG, Kader A. Examining leadership as a strategy to enhance health care service delivery in regional hospitals in South Africa. Journal of Multidisciplinary Healthcare. 2018;11:157.
Health Ministerial Task Team, 2017. Health Ministerial Task Team on Hospital Mismanagement and Poor Service Delivery – Closure Report. Pretoria: National Department of Health.
Jones L, Pomeroy L, Robert G, Burnett S, Anderson JE, Fulop NJ. How do hospital boards govern for quality improvement? A mixed methods study of 15 organisations in England. BMJ Quality & Safety. 2017;26(12):978-986.
Kollapen JJ, Carnelly M, Jaichand V, Lawrence MI. Issue Paper 33, Project 141, Medico-Legal Claims, 20 May 2017 edn., South African Law Reform Commission, Cape Town, South Africa. 2017
KPMG, 2016. The King IV Report on Corporate Governance for South Africa 2016, Institute of Directors of South Africa. Johannesburg: KPMG.
Mannion R, Davies H, Freeman T, Millar R, Jacobs R, Kasteridis P. Overseeing oversight: governance of quality and safety by hospital boards in the English NHS. Journal of Health Services Research & Policy. 2015;20(1 suppl):9-16.
Maphumulo WT, Bhengu BR. Challenges of quality improvement in the healthcare of South Africa post-apartheid: A critical review. Curationis. 2019;Jan 1;42(1):1-9.
Mountford J, Wakefield D. From stoplight reports to time series: equipping boards and leadership teams to drive better decisions. BMJ Quality & Safety. 2017;26(1):9-11.
National Department of Health, South Africa, 2009. User Guide – UPFS 2009 (version 1). South Africa: Pretoria: National Department of Health.
Office of the Presidency of the Republic of South Africa, 2018. Presidential Health Summit Report: Strengthening the South African Health System towards an integrated and unified health system. 19-20 October, 2018. Johannesburg: Birch wood Conference Centre.
Patel B. Lessons on and for Management: Personal reflections of a Hospital CEO. Hospital Annual Operational Planning Presentation. Groote Schuur Hospital, Cape Town. 2021.
South African Lancet National Commission, 2019. Confronting the right to ethical and accountable quality health care in South Africa: A Consensus Report. Pretoria: National Department of Health.
Statistics South Africa, NCD Statistics.
Stewart J, Wolvaardt G. Hospital management and health policy—a South African perspective. Journal of Hospital Management and Health Policy. 2019;3(14):1-7.
Health emergencies, defined as ‘any situation whose scale, timing or unpredictability threatens to overwhelm routine capabilities’1, cause disruption and derail the usual functioning of health systems, and thus set back gains made towards universal health care2. In this chapter, we evaluate why disaster risk reduction and preparedness foster health system resilience. We reflect on the global context emerging from the 2012–2014 Ebola outbreak in West Africa which set the international agenda for emergency preparedness and response in South Africa, 2015–2020. We then review South African preparedness efforts, drawing extensively from South Africa’s participation in, and findings and outcomes of the joint external evaluation of adherence to the International Health Regulations (IHR) 2005. We identify health emergencies that took place from 2015–2020 and discuss in some depth two South African health emergencies that unfolded over this time. We reflect on health system responses to the unfolding COVID-19 pandemic over 2020, illustrating how these drew on experience gained by stakeholders in earlier South African emergencies. Finally, we offer pointers to support strengthening South Africa’s emergency preparedness and response over the next five years.
Kerrigan McCarthy, Kamy Chetty, Marc Mendelson, Patrick Moonasar, Tsakani Furumele, Olga Perovic, Raveen NaidooNot only do health emergencies disrupt services, but they may also precipitate crises in other areas of the health system, and/or lead to a broad range of poor health outcomes in unrelated areas, sometimes for extended periods after the emergency2. Typically, health emergencies disproportionately affect disadvantaged groups who may have limited resources or access to supportive services3. It is the re sponsibility of public health systems to reduce risks and the impact of emergencies in the short and longer term2. ‘Preparedness’ is defined as ‘the capacity of the public health and health care systems, communities and individuals to prevent, protect against, quickly respond to and recover from health emergencies, particularly those whose scale, timing or unpredictability threatens to overwhelm routine activities’1. With adequate preparation, disruptions can be minimised and their impact mitigated through actively managed and effective preventive programmes (such as immunisation), policy and legislative frameworks and through coordinated response efforts. Effective disaster risk management through investment in preparedness contributes to sustainable development4.
In the wake of the 2003 SARS crisis, the World Health Assembly revised the IHR (2005)7 and obtained commitment by member states to create and sustain systems for health emergency preparedness and response by 20128. This included development and adherence to ‘core capacities’9 (Table 8.1) grouped around prevention, detection response, other IHR-related hazards and points of entry. However, the process was severely criticised8. By 2014, only 78 out of 196 member states had submitted their IHR core capacity self-assessments to the WHO10. The self-assessment process did not require external verification, allowing countries to report their capacities without accountability8. Countries unable to implement core capacities because of weaker infrastructure and human resource constraints were not provided with financial or other support8. International leadership to prioritise capacity development of member states was weak8. In the wake of these criticisms, the WHO in consultation with member states developed the joint external evaluation (JEE) process to support assessment of member state adherence to IHR, identify areas that require strengthening and develop structured plans to achieve adherence11. Key components of the JEE were self-evaluation, a ‘whole-of-government approach’, peer review and voluntary external evaluation. By 2017, the process had gained considerable momentum and widespread acceptance, with participating countries identifying new ways of collaborating, and ownership over the process12
Following the lessons learnt from the emergency response to the earthquake in Haiti, in January 2010, the WHO implemented the Emergency Medical Team (EMT) Initiative13. The purpose of the EMT initiative is twofold: firstly, to improve the timeliness and quality of health services provided by national and international EMTs; and secondly, to enhance the capacity of the affected nations health systems in
Health emergencies, AMR and Covid-19 response
leading the activation and coordination of this response in the immediate aftermath of a disaster, outbreak and/or other emergency. Teams may include public health expertise and logistics support either within the team or as specific public health or logistics rapid response teams. Presently, this initiative is at various stages of accreditation by the WHO globally. South Africa has subscribed to the general principles of the EMT Initiative, however, the establishment and accreditation by WHO has been delayed by the current COVID-19 pandemic.
Included in the IHR (2005) ‘core capacities’ is the requirement to create and utilise emergency operating centres (EOC). The concept of a public health EOC was developed by the WHO following the 2003 SARS crisis, and refined over subsequent years with the creation of a framework and handbook for EOC14,15. EOCs use the incident management system (IMS) which is a scalable, flexible and adaptable, command-and-control system for coordinating resources and responses during public health emergencies. Following the successful functioning of the EOC in Nigeria during the West African Ebola crisis, member states were encouraged to create these centres and implement the IMS during EOC activations16
By October 2021, 47 out of 52 AFRO region countries had submitted JEE reports17. Critical evaluation of the JEE process seems to show high levels of concordance between JEE scores, assessments and outbreak response18,19.
Table 8.1 Core capacities required to implement IHR, and South African scores during the JEE process, 201720. (Scores: 1=No capacity; 2=Limited capacity; 3=Developed capacity; 4=Demonstrated capacity; 5=Sustainable capacity)
1 National legislation, policy and financing
Legislation, laws, regulations, administrative requirements, policies, or other government instruments in place are sufficient for implementation of IHR (2005)
The state can demonstrate that it has adjusted and aligned its domestic legislation, policies, and administrative arrangements to enable compliance with IHR (2005)
2 Assess legal framework and policies to ensure all are aligned with IHR (2005); Enact IHR and NAPHISA Bills; Map national health risks and resources with other departments/sectors.
2
2 IHR coordination, communication and advocacy
Functional mechanism is established for the coordination and integration of relevant sectors in the implementation of IHR
4 Evaluate and strengthen the INR national focal point to support IHR coordination, communication and advocacy within and across sectors; Conduct simulation exercises or evaluate past events.
3 Antimicrobial resistance Antimicrobial resistance (AMR) detection
Surveillance of infections caused by antimicrobial-resistant pathogens
Health care-associated infection (HCAI) prevention and control programmes
4 Zoonotic diseases Surveillance systems in place for priority zoonotic diseases/pathogens
3 1Develop and implement a ‘One Health’ national AMR strategy; Develop and implement a national multisectoral plan for HCAI and AMR prevention.
3
1
Antimicrobial stewardship activities 2
Veterinary or animal health workforce 4
Mechanisms for responding to infectious and potential zoonotic diseases are established and functional
5 Food safety Mechanisms for multi sectoral collaboration are established to ensure rapid response to food safety emergencies and outbreaks of foodborne diseases
6 Biosafety and biosecurity
Whole-of-government biosafety and biosecurity system is in place for hu man, animal and agriculture facilities
7 Immunisation
Vaccine coverage (mea sles) as part of national programme
4
4 Develop and approve a national policy for ‘One Health’; Conduct training and joint simulation exercises on recognition and response to zoonotic emergencies; ensure ongoing improvement through evaluation of simulation exercises and past responses; Strengthen laboratory coordination between animal and hu man health; ensure training of veterinar ians in FETP courses.
3 Conduct monitoring and evaluation of places/institutions with high risk for foodborne outbreaks; Link surveillance and response staff and focal points for food safety and animal health; Conduct multisectoral risk assessment and management of foodborne outbreaks; ensure ongoing improvement through evaluation of simulation exercises and past responses with documentation of lessons learnt; strengthen timeliness of reporting and responses.
Biosafety and biosecurity training and practices 3
3 Establish a national biosafety and biose curity committee; Review and harmonise legislation and policies; Develop a ‘dual use’ policy; Strengthen and resource governmental oversight activities; Consolidate national lists of pathogens and laborato ries; standardise and deliver training in biosafety and biosecurity.
National vaccine access and delivery 5
3 Fully implement ‘reach every district’ strategy in provinces through resourcing national EPI oversight, developing health facility micro plans including tracking of defaulters, involving the private sector; Strengthen EPI disease surveillance; Strengthen data quality through validation of coverage data with an EPI coverage survey, includ ing public sector data.
8 National laboratory system
Laboratory testing for detection of priority diseases
5
Specimen referral and transport system 4
Effective modern point-ofcare and laboratory-based diagnostics
3
Laboratory quality system 3
9 Real-time surveillance Indicator- and event-based surveillance systems
Interoperable, interconnected, electronic real-time reporting system
Strengthen ICT systems to link labora tory information systems with public health surveillance systems; increase availability of basic testing and improve turnaround times; link NHLS, strengthen NHLS procurement and supply chain mechanisms; veterinary and private sector laboratories; establish a national laboratory quality framework; support pathology residents and intern scientists/ technicians to complete training.
2
Integration and analysis of surveillance data 4
3 Resources for NMC at provincial level should be increased; Submission of surveillance data should be electronic; Event-based and indicator-based surveillance needs to be interoperable and linked; data collation at each level should be strengthened; community-based surveillance should be strengthened.
Syndromic surveillance systems 4
10 Reporting System for efficient reporting to FAO, OIE and WHO
Reporting network and protocols in country 3
11 Workforce development Human resources available to implement IHR core capacity requirements
3 Simulation exercises should be done; Electronic sharing of surveillance and other data between animal and human health sectors needs to be made available.
12 Preparedness
13 Immunisation
FETP1 or other applied epidemiology training programme in place
4 Workforce strategy 2
National multi-hazard public health emergency preparedness and response plan is developed and implemented
Priority public health risks and resources are mapped and utilised
Capacity to activate emergency operations
3 Assess public health workforce requirements, map existing resources and include mechanisms for increasing workforce in HRH strategy; Fast-track institutionalisation of epidemiology as a specialisation; Strengthen epidemiology training through provision of courses and finances.
2
3
EOC operating procedures and plans 2
Emergency operations programme 4
Case management procedures implemented for IHR relevant hazards
Develop one overarching multisectoral national public health emergency preparedness and response plan; conduct a national risk assessment; prioritise development of the public health emergency committee; advocate for full-time operation of NATHOC.
2 Establish a legal framework with clear roles and responsibilities of EOC and its relationship with the National Disaster Management Centre; Increase human resources of PHOC and conduct training and simulation using the IMS; update EOC SOPs, cascade EOC/IMS to lower levels.
4
14 Linking public health and security authorities
Public health and security authorities (e.g. law enforcement, border control, customs) are linked during a suspected or confirmed biological event
4 Conduct national emergency scenarios and simulation exercises with all stakeholders; ensure procedures address interdepartmental cooperation in response to biological incidents, establish communication channels during non-crisis events; review policy on management of chemical, biological, radiation and nuclear incidents.
15 Medical countermeasures and personnel deployment
System in place for sending and receiving medical countermeasures during a public health emergency
System in place for sending and receiving health personnel during a public health emergency
16 Risk communication Risk communication systems (plans, mechanisms, etc.)
2
2
Finalise a comprehensive plan to send and receive medical countermeasures and personnel; review experiences and conduct simulation exercises of the above; examine the regulatory framework for sub-regional exchange of medical countermeasures and personnel.
17 Points of entry (PoE)
18 Chemical events
3 Develop national-level risk communication preparedness and response plans including surge support and sustainability; perform risk communication simulation exercises.Internal and partner communication and coordination
3
Public communication 4
Communication engagement with affected communities
3 Dynamic listening and rumour management 4
Routine capacities established at PoE
Effective public health response at PoE
Mechanisms established and functioning for detecting and responding to chemical events or emergencies
Enabling environment in place for management of chemical events
19 Radiation emergencies Mechanisms established and functioning for detecting and responding to radiological and nuclear emergencies
Enabling environment in place for management of radiation emergencies
4
4 Review HR capacity for PoE; finalise memoranda of understanding for safe referral and transport of ill travellers; review, evaluate and disseminate public health contingency plans for all sectors at PoE and establish mechanisms to improve compliance.
3 Develop mechanism for timely and sys tematic information exchange between appropriate chemical units, surveillance units and other relevant sectors about urgent chemical events and potential chemical risks and their response; Conduct simulation exercises; formalise agreements between government and private institutions to collaborate and share information.
3
2 Finalise comprehensive national plan for detection, assessment and response to radiation emergencies; Link radiological and nuclear regulatory bodies with DoH/IHR NFP; Establish improved health surveillance and case management for radio-nuclear emergencies.
2
1See section on antimicrobial resistance below. IHR=International Health Regulations (2005); FAO=Food and Agriculture Organisation of United Nations, OIE=World Organisation for Animal Health; ICT=information and communication technology; FETP=Field epidemiology training programme; NMC=notifiable medical conditions; IMS=Incident Management System
South Africa entered 2015 with the West African Ebola crisis abating, and finding itself equipped with legal, policy, laboratory and public health structures well able to support health emergencies.
The right to health and the broader legal framework for public health were ensured by the Constitution21, the National Health Act 61 of 200322, including the notifiable medical conditions regulations23, the National Health Laboratory Services Act24 and the Disaster Management Act25. The International Health Regulations (IHR) Bill26 had been proposed in 2013 and was awaiting enactment.
South African structures for health emergencies in 2015 included the National Joint Operational and Intelligence Structure (NATJOINTS) and the associated National Joint Operations Centre (NATJOC), the Multisectoral National Outbreak Response Team (MNORT), the National Disaster Management Centre (NDMC) and the National Institute of Communicable Diseases’ (NICD) Public Health Emergency Operation Center (PHEOC). NATJOINTS is a structure convened by the South African Police Service with the task of securing lives and livelihoods from internal and external threats, including political and social unrest, environmental hazards and health emergencies. NATJOINTS has representation from all tiers of government including health. This structure is replicated in each of the nine provinces by the Provincial Joint Operational and Intelligence Structures and Provincial Joint Operations Centres. In addition, local government authorities provide for coordination of disasters including health emergencies at municipal level as provided for under the Disaster Management Act 57 of 2002. The MNORT was convened in the late 1990s and constituted with the aim of supporting multisectoral collaboration and response to communicable dis ease outbreaks. Monthly MNORT meetings were attended by national and provincial health authorities (including those responsible for communicable diseases, tuberculosis (TB), HIV, maternal and child health, environmental health and port health), laboratory services, animal health, civil aviation, international relations and cooperation, private sector hospitals and emergency medicine. A significant development was the signing of a memorandum of agreement between the NDoH and the NHLS/NICD to delegate responsibility for creation of an EOC in January 2015. In 2015, the NICD employed an EOC manager, developed operating procedures including criteria for activation and introduced the IMS. The NICD was tasked with development of an electronic notifiable medical conditions surveillance system (the NMC-SS) through a memorandum of agreement between the NDoH and the NHLS in October 2015.
At a provincial level, responsibility for communicable disease control and response was assigned to the Communicable Disease Control Coordinator aided by a data capturer, who worked with the Expanded Programme of Immunisation team, and the vertical TB and HIV programmes where necessary. The NICD Outbreak Response Unit27 provided technical support to the provinces in event of outbreaks, often providing staff including field epidemiologists with training in a crisis.
Over the course of the 2013–2016 West African Ebola outbreak, these structures, and a new structure, the National Health Operations Centre (NATHOC) were integrally involved in supporting South African health responses, which included direct assistance through provision of laboratory diagnostics28, restriction of non-essential travel to the affected region, screening of returning travellers29, training of health care workers in recognition of Ebola Virus Disease (EVD) cases, health system readiness through designation of hospitals for management of EVD cases and health promotion.
A collaborative process commenced in 2016 when the Director General Health initiated a JEE of IHR preparedness in accordance with IHR (2005). The process required an internal self-evaluation, which was to be reviewed collaboratively with external partners in November 201711. Scores and recommendations of the JEE team are tabulated in Table 8.1. The JEE process identified a key weakness in actualising IHR requirements at a legislative and resource level in that the IHR Bill was yet to be enacted, and that IHR functions at the NDoH were under-resourced (Table 8.1, Capacity 2). A second key weakness was identified as the absence of integration of different response sectors, institutions and structures (including the NDMC, NATHOC and EOC) in an overarching legislative and policy framework (Table 8.1, Capacity 1) and that there was no integrated and overarching emergency response plan (Table 8.1, Capacity 12 and 13).
In 2017, regulations relating to the surveillance and control of notifiable medical conditions regulations30 were updated to include an expanded list of notifiable conditions (including listeriosis and antimicrobial resistant organisms), and introduced compulsory reporting by diagnostic laboratories, medical schemes and clinicians.
Table 8.2 lists communicable disease events and health emergencies that occurred in 2015–2020. NATHOC continued to operate in 2015 until restrictions on travel to West Africa during the Ebola outbreak eased. The NICD’s EOC was activated on two occasions: in 2017 to support relocation of mental health care users following the Life Esidimeni crisis in Gauteng province, and in 2018 with the support of the WHO to respond to a national listeriosis outbreak following contamination of a ready-to-eat (RTE) meat production facility in Polokwane, Limpopo Province31
Health emergencies, AMR and Covid-19 response
Nature of event Affected persons
April 2015 Northern Cape Diarrhoeal disease CD >600 NCP DoH, NICD
July 2015 KwaZulu-Natal Diphtheria outbreak CD 15 KZN DoH, NICD, NDoH
August 2015 Western Cape Leptospirosis CD 2 WCP DOH, NDoH, NICD
October 2015 Gauteng Enteroviral meningitis CD >30 Gauteng DoH
November 2015 Lesotho Dysentery outbreak CD >500 Technical advice to Kingdom of Lesotho
May 2016 Eastern Cape XDR-TB CD >100 ECP DoH, NICD
July 2016 Eastern Cape Influenza CD >200 ECP DoH, NICD
July 2016 KwaZulu-Natal Diphtheria outbreak CD 2 KZN DoH, NICD, NDoH
August 2016 Eastern Cape Clostridium difficile CD 8 Local hospital level
December 2016 KwaZulu-Natal Norovirus outbreak CD >600 KZN DoH, NICD
January 2017 Gauteng Sindbis CD 56 NICD
January 2017 Western Cape Measles CD 22 WCP DoH, NICD
February 2017 Gauteng Life Esidimeni Health Services >1 500 GDoH, NDoH, NICD
June 2017 Western Cape Knysna wildfire Fire >10 000 Fire Services, WC EMS
June 2017 Gauteng Measles >200 Gauteng DoH, NICD
June 2017 Limpopo, Gauteng H5N8 avian influenza outbreak CD >50 Multisectoral, led by DAFF
August 2017 Western Cape Diphtheria outbreak CD 4 WCP DoH, NICD
August 2017 South Africa Listeriosis CD >1 500 NDoH, NICD, WHO
September 2017 KwaZulu-Natal Measles CD >30 KZN DoH
October 2017 Gauteng Foodborne illness CD >90 Gauteng DoH, NICD
October 2017 Gauteng Group A streptococcus with necrotising fasciitis CD >20 Gauteng DoH
November 2017 Limpopo Typhoid CD >100 Limpopo DoH, NICD
November 2017 Western Cape, Eastern Cape Enteroviral meningitis CD >3 400 WCP and ECP DoH, NICD
November 2017 Gauteng Staphylococcus aureas CD >350 NICD and institution
December 2017 Western Cape Pseudomonas contamination of water CD >2 000 WCP
January 2018 Western Cape Vaccine-derived poliovirus CD 1 WCP, NDoH, WHO, NICD
February 2018 KwaZulu-Natal Cholera case CD 1 Single case, led by NDoH, KZN DoH and NICD
April 2018 Gauteng Multidrug resistant Klebsiella CD >50 Gauteng DoH, NICD
July 2018 Mpumalanga Wasterborne illness outbreak CD >1 500 MPU DoH, NICD
October 2018 Gauteng Vaccine-derived poliovirus CD 1 Gauteng DoH, NDoH, WHO, NICD
October 2018 Eastern Cape Pertussis CD >250 ECP DoH, NICD
October 2018 Gauteng Foodborne illness outbreak CD >200 Gauteng DoH
November 2018 Limpopo, Gauteng Cholera cases CD <10 cases Imported from Zimbabwe, led by Limpopo and Gauteng DoH
March 2019
Gauteng, Mozambique, Malawi, Madagascar and Zimbabwe
Cyclone Idai Flooding, CD <2.2 mil lion
Government response to request for health and humanitarian aid to affected neighbouring countries
Gauteng DoH, NDoH, NICD
May 2019 Gauteng Presidential Inauguration Mass gathering >35 000 All government departments
May 2019 North West Province Mumps CD >150 NW DoH, NICD
January 2021 Limpopo, Gauteng, Mpumalanga, Free State, Northern Cape, North West
Tropical Storm Eloise Flooding, CD >175 000 NDMC, NDoH, affected provinces Health and Local Government structures
*DAFF=Department of Agriculture, Forestry and Fisheries
Following alerts from public hospitals of increases in listeriosis cases in July and August 2017, an outbreak investigation was initiated by the NICD. Molecular typing identified an outbreak clone ‘ST6’. A total of 937 cases were reported during the outbreak period from June 11, 2017 until April 7, 2018, with case numbers peaking at 41 per week in mid-November 2017 (epidemiologic week 46)31, making the outbreak the largest global listeriosis outbreak ever reported32. In March 2018, the outbreak strain was found to be contaminating an RTE meat production facility in Polokwane, Limpopo province. Cases decreased dramatically after recall of the implicated products on March 4, 2018. In April 2018, the NDoH activated the NICD EOC. On 28 March 2018, the WHO increased their internal risk assessment of the listeria outbreak from grade 1 to grade 2, making provision for deployment of a WHO Country Office incident management team (IMT), repurposing of the WHO staff and deployment of additional resources and surge teams (including food safety, risk communications and EOC experts and epidemiologists). The joint RSA-WHO IMT, described in Figure 8.1a, coordinated drafting and implementation of an emergency response plan (Figure 8.1b). Activities supported by the IMT included real-time surveillance and molecular typing of all Listeria monocytogenes (Lm) isolates and prospective patient food-history interviews to support early detection of clusters, strengthening of food and environmental testing for Lm through development and validation of test methodology, training of almost 900 environmental health practitioners in all South African health districts in inspection procedures, food safety systems, legislative aspects of food control, inspection of all RTE production facilities (n=158), amendment of food legislation to require RTE producers to be Hazard Analysis Critical Control Points (HACCP) certified by externally accredited agencies, and health promotion and risk communication activities. The outbreak and response efforts illustrated the impact and capacity of collaborative, multisector and international efforts to strengthen food safety, to safeguard public health and prevent future listeriosis outbreaks.

Antimicrobial resistance (AMR) has been identified as a ‘global crisis that threat ens a century of progress in health and achievement of the Sustainable Development Goals’33. Although described as an ‘invisible pandemic’ which is evolving over the last 50 years, AMR fulfils the definition of a health emergency because it has capacity to overwhelm our existing armamentarium of lifesaving treatments for common bacterial infections, and may result in 10 million deaths per year by 2050 if unchecked34. Only in May 2015, the 68th World Health Assembly adopted the Global Action Plan (GAP) to combat AMR using the ‘One Health’ approach. By introducing the ‘One Health’ concept into the GAP, WHO succeed in engaging the spectrum of sources of AMR, namely veterinary, agricultural and environmental sources in the fight against AMR. Also in 2015, the WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS) was launched with the aim of monitoring AMR and consumption and use (AMC/U) globally so as to support strategic responses to contain AMR. Presently, an AMR indicator (the proportion of bloodstream infections due to selected types of resistant pathogens) is included in the Sustainable Development Goals (SDGs) linked to target 3.d: ‘Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks’35
Already in 2011, in a situation analysis, South Africa recognised a quadruple burden of resistant infectious disease, including multidrug-resistant tuberculosis, drug-resistant HIV, resistant malaria and antibacterial/antifungal resistance36. In October 2014, the Minister of Health launched the National AMR Strategic Framework, which was updated in 2018 to increase the focus on a One Health
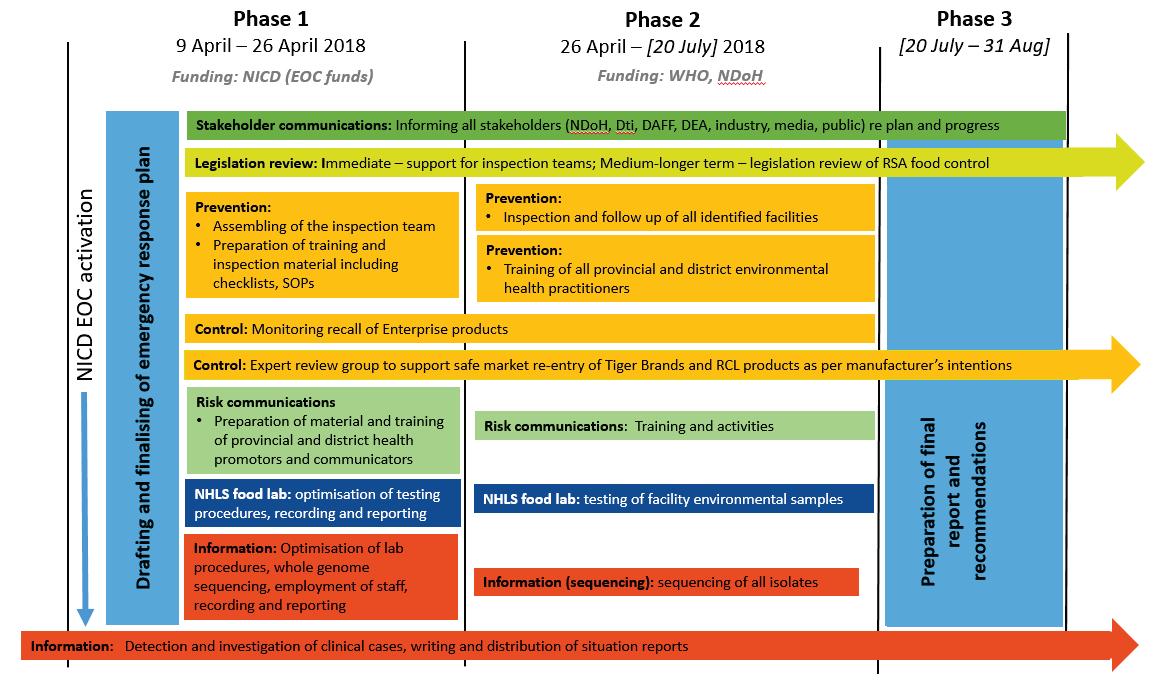
response37. This current framework spans seven years (2018–2024) and outlines the country’s plan for the management of AMR, the improvement of patient outcomes, and mitigation strategies for AMR in animal and environmental health (Table 8.2).
Notable achievements over 2015–2020 include: convening of a ministerial advisory committee (MAC) on antimicrobial resistance20, developing the framework for antimicrobial governance regulation, and utilisation at national, provincial, institutional and district levels38, scaling up of AMR surveillance programmes39,40, development of national training centres and train-the-trainer programmes to support provinces with limited stewardship human resources, implementation of facility and provincial antimicrobial stewardship programmes41, reporting of AMR and antimicrobial usage data to WHO’s GLASS initiative42 (from 2016 onwards), and a toolkit to enable antimicrobial stewardship in South African hospitals43. The surveillance report issued by the AMR MAC in 2018 represents currently available information relating to AMR in humans and antimicrobial consumption in animals and humans in South Africa44.
The current South African AMR surveillance system in humans was built through collaboration between public and private sector laboratory services and reports on AMR in blood cultures for the WHO-required pathogens (Klebsiella pneumonia, E. coli, S. aureus, P. aeruginosa, A. baumannii, and enterococci). In addition, infection prevention and control (IPC) is a cornerstone for combating healthcare-associated infections and AMR. The South African IPC framework45 and manual are linked to the AMR programme and endorsed by the MAC.
Table 8.3 Strategic framework and activities to preserve effectiveness of antimicrobials, improve use of antibiotics and strengthen effective management of antibiotic resistant organisms according to the National AMR Strategy Framework37
1 Strengthen interdisciplinary efforts through One Health governance structures
2 Improving diagnostics to guide patient and animal treatment
3 Optimise surveillance and early detection of AMR
Establish an interdisciplinary national advisory committee
Establish governance structures at operational levels of province, district, health establishments and veterinary services
Provide timely microbiological data to allow delivery of safer, more effective and efficient treatment
Strengthen surveillance of local and national resistance patterns and antimicrobial use
Develop early warning systems of sentinel organisms and outbreaks
Participate in international databases on AMR and antimicrobial use
4 Enhance infection prevention and control, and biosecurity to prevent spread of resistant microbes amongst patients, between animals, farms and countries
5 Promote appropriate use of antimicrobials in human and animal health
Prevent new infections through vaccination programmes and effective water, sanitation and hygiene (WASH) services
Prevent and control the spread of resistant micro-organisms in humans and health institutions
Strengthen and monitor biosecurity and hygiene from farm to retailer
Ensure environmental health and water quality monitoring
Ensure access to safe, effective and affordable antimicrobials
Institutionalise antimicrobial stewardship in human and animal health
Shortly after the identification of SARS-CoV-2 in Wuhan on the 5th of January 202046, preparedness activities commenced in South Africa with activation of the EOC (30 January 2020) and convening of an incident management team (IMT). Following detection of the first South African laboratory-confirmed case of SARS-CoV-2 on March 5, 2020,47 an ‘inter-ministerial committee’ comprising the entire cabinet was formed to coordinate government responses on 15 March 2020 and named the ‘National COVID-19 Command and Control Council’ (NCCC)48. A National State of Disaster was declared on 18 March 202049. On 27 March a nationwide ‘level 5’ lockdown was implemented50, halting non-essential business and confining all persons to their residences until easing of restrictions on 30 April 2020. Within the first eight weeks following importation of SARS-CoV-2, over 270 000 diagnostic tests had been conducted, and over 7 800 cases identified51. A National Plan for COVID-19 Health Response was formally adopted in May 202048, and comprised nine strategic priorities, namely: 1) to provide effective governance and leadership; 2) to strengthen surveillance and strategic information; 3) to augment health systems readiness including emergency medical services; 4) to enhance community engagement; 5) to improve laboratory capacity and testing; 6) to clarify care pathways; 7) to scale-up infection prevention and control measures, 8) to boost capacity at ports of entry; and 9) to expedite research and introduce therapeutics, diagnostics and vaccines.
Pre-existing health structures to support outbreak response were configured around the NCCC (Figure 8.2), and new structures were created, namely the COVID-19 Ministerial Advisory Committee, the project management office (responsible for finance and administration) and the COVID-19 Ministerial Advisory Committee. The MNORT was not convened during the COVID-19 pandemic, as including intersectoral decision-making was assumed by the NCCC. The National IMT was responsible for health sector responses only and was organised into functional areas that aligned to the nine strategic priorities in the National COVID-19 Response Plan. Each province convened their own IMT to support provincial and district health service delivery. Communication with provinces was formally conducted through the NATJOC and provincial joint operations committee and through the National Health Council as in pre-COVID-19 operations. Other structures, such as NATHOC and the EOC were not formally utilised.
Two key developments supporting COVID-19 responses were the creation of a National COVID-19 Response Plan52,48 and data systems to support epidemiological intelligence and case management53. The national response plan identified and delineated key activities in nine strategic priority areas, as outlined above. Systems were created for immediate transmission of laboratory diagnostic test results from public and private sectors to a central data repository at the NICD, as well as mechanisms for electronic and manual geocoding and data cleaning. A second data management system, DATCOV was also set up by the NICD early in the outbreak to support data collection on hospitalisations, bed occupancy and outcomes54.




The years 2015–2020 have seen a gradual increase in number, intensity and severity of health emergencies, culminating in the SARS-CoV-2 pandemic. The foundations for South Africa’s current response capacity were laid through the preparations for potential imported EVD cases from the West African Ebola outbreak in 2014–2016. These led to improvements in preparedness at ports of entry, diagnostic laboratories, infection prevention and control guidelines and training, and hospital-level service delivery. The listeriosis outbreak allowed key stakeholders to gain experience from the WHO in utilising and working within an incident management structure. Surveillance for antimicrobial resistance and antimicrobial stewardship programmes were strengthened through policy and guideline development.
For South Africa, as with other AFRO regional countries55, the JEE process in 2017 was instrumental in supporting multisectoral collaboration and preparedness planning as well as identifying areas requiring additional support. Globally, the JEE process has been shown to correlate with effectiveness of COVID-19 control when adjusting for country income, population density and human development56. Therefore, the recommendations identified by South Africa’s JEE and other opportunities for strengthening, which have been made apparent by the COVID-19 pandemic, need to be addressed if health services are not to be further disrupted and appreciable achievements in universal health coverage are not lost. We highlight six areas for focused attention as follows:



Firstly, governance and the role of legislation and policy is key to bring countries in line with IHR requirements57. The absence of a legislative framework supporting IHR implementation across sectors and at all levels of government, and the absence of a multisectoral health response plan were identified by the JEE process in 2018. The creation of new emergency response structures and reconfiguration or dropping of existing structures to support the COVID-19 response illustrated the inadequacy of pre-COVID-19 preparedness and response plans to address an event of pandemic proportions. South Africa will need to reformulate and enact the IHR Bill26 to ensure progress towards IHR (2005) implementation.
Secondly, the disruption of services reported across many health sectors during lockdown illustrated a key deficiency of continuity of care in emergency planning and response. Primary health care service delivery has been severely impaired during COVID-19 as evidenced by a 19% decline in persons tested for TB, a 22% decline in HIV testing and an 18% decline in PHC facility visits over 2020 compared with 201958. Persons with TB have a two to five times greater risk of death following COVID-19 infection59, and these outcomes are likely exacerbated by service delivery impairment60. The use of antimicrobials for the patients in health care facilities is high and likely to exacerbate AMR61. Nyasulu et al. have created a conceptual framework which may support the next phase of preparedness and response planning62.
Thirdly, SARS-CoV-2 has led to appreciable loss of human resources63, whilst also requiring integration and formal career paths for new cadres of staff including community health workers64 and epidemiologists. The burden of disease, the speed of SARS-CoV-2 transmission, high number of institutional and facility outbreaks and overwhelming requirements for contact tracing, have all highlighted the key role of and requirement for skilled epidemiologists with field experience. Already, the JEE process identified the need to fast-track institutionalisation of epidemiology as a specialisation and strengthen epidemiology training through provision of financial sup port20. Van Ryneveld et al. have identified the key role of governance and capacitation of the NDoH to support alignment of policy, regulatory bodies and human resource requirements65 .
Fourthly, the success of NHLS/NICD’s data management pertaining to SARS-CoV-2 tests, cases, admissions and deaths have highlighted the absence of such systems for other communicable and non-communicable disease across human and animal sectors. Investments across all levels of the health sector are required to support ICT requirements of data management. Significant challenges exist in this space, ranging from digital illiteracy, poor infrastructure, the high cost of installing ICT infrastructure, security concerns and irregular electricity supply66. However, the impact of integrating ICT may yield a wide range of benefits across health programmes and sectors.
Fifthly, the emergence and entrenching of anti-vaccine sentiment in South Africa67 may be ascribed to deficient social listening, delayed roll-out of health promotion and communication campaigns48, and inadequate attention to ‘peace time’ efforts to promote trust in science, government and health authorities. Effective communications and leadership are central to the management of pandemics and their rapidly changing societal and economic landscapes68. Government health communications require ongoing engagement in an interactive process of exchange of information with communities, whilst considering the evolving technical knowledge of the pathogen and its epidemiology and relevant social dynamics, socio-cultural diversity, and a rapidly changing media. Key principles of effective communication strategies68 include
proactive, empathetic, clear, credible messages that recognise uncertainty, account for levels of health literacy and numeracy, consider diverse community needs, appeal to social norms and empower people to act.
Lastly, measures to address the mental health care needs of health practitioners, vulnerable persons and the public, and the inclusion of psychosocial services in response planning was a crucial omission from the National COVID-19 Response Plan69 Siphelele et al.69 believe that the psychology profession should be integrated into preparedness planning and response measures for individual and community mental health sequelae. Psychologists can contribute to pandemic responses by provision of services and training of mental health professionals in immediate and responsive treatment measures.
What is evident is that each of these six areas for focussed attention over the next five years contribute not only to health emergency response, but also to health systems strengthening and provision of universal health coverage. Many interventions to address SARS-CoV-2, with minimal adaption and if applied consistently, also have potential to strengthen specific disease control programmes70
The Independent Panel for Pandemic Preparedness and Response, appointed by the WHO Director-General in response to the World Health Assembly resolution 73.1, has provided the WHO and global community with a comprehensive, evidence-based review of global and WHO responses to the COVID-19 pandemic71. Amongst the most urgent of their recommendations for national governments are that these update their national preparedness plans against predetermined WHO targets and benchmarks within six months, that they ensure appropriate and relevant skills, logistics and funding are available to cope with future health crises and that they appoint national pandemic coordinators accountable to the highest levels of government with the man date to drive whole-of-government coordination for both preparedness and response. South Africa will do well to support and implement these recommendations, as well as the outstanding recommendations from the 2017 JEE recommendations. If addressed, these measures and the six recommendations outlined above will ensure robust, effective containment and response to the next pandemic.
What is certain on review of South Africa’s response to health emergencies over 2015–2020 is that health security requires more than a narrow focus on infectious disease preparedness, detection and response. Universal health coverage and health systems strengthening both support and are supported by health emergency planning and response72
1. Nelson C, Lurie N, Wasserman J, Zakowski S. Conceptualizing and defining public health emergency preparedness. Am J Public Health 2007; 97 Suppl 1(Suppl 1): S9–11.
2. Khan Y, O’Sullivan T, Brown A, et al. Public health emergency preparedness: a framework to promote resilience. BMC Public Health 2018; 18(1): 1344.
3. Kaye AD, Okeagu CN, Pham AD, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pract Res Clin Anaesthesiol 2021; 35(3): 293–306.
4. UNISDR. Sendai framework for disaster risk reduction 2015-2030. 3rd United Nationals World Conference on Disaster Risk Reduction; 2015; Sendai, Japan: UNISDR; 2015.
5. Arnold C. 10 Years on, the world still learns from SARS. Lancet Infect Dis 2013; 13(5): 394.
6. Kirsch T, Sauer L, Guha Sapir D. Analysis of the international and US response to the Haiti earthquake: recommendations for change. Disaster Med Public Health Prep 2012; 6(3): 200–8.
7. WHO. International Health Regulations. In: WHO, editor. Geneva; 2005.
8. Moon S, Sridhar D, Pate MA, et al. Will Ebola change the game? Ten essential reforms before the next pandemic. The report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Lancet 2015; 386(10009): 2204–21.
9. WHO. IHR Core Capacity Monitoring Framework: Checklist and Indicators for Monitoring Progress in the Development of the INR Core Capacities in the States Parties. Geneva: WHO; 2013.
10. WHO. Implementation of International Health Regulations. Geneva: WHO, 2015.
11. WHO. Development, monitoring and evaluation of functional core capacity for implementing the International Health Regulations (2005). Geneva: WHO, 2015.
12. Kandel N, Sreedharan R, Chungong S, et al. Joint external evaluation process: bringing multiple sectors together for global health security. The Lancet Global health 2017; 5(9): e857–e8.
13. WHO. Classification and minimum standards for emergency medical teams. Geneva: WHO; 2021.
14. WHO. Handbook for developing a public health emergency operations centre part A: policies, plans and procedures. Geneva; 2018.
15. WHO. Framework for a public health emergency operations centre. Geneva: WHO; 2015.
16. Ma J, Huang Y, Zheng ZJ. Leveraging the Public Health Emergency Operation Center (PHEOC) for pandemic response: opportunities and challenges. Global health journal (Amsterdam, Netherlands) 2020; 4(4): 118–20.
17. WHO. Strategic Partnership for Health Security and Emergency Preparedness (SPH) Portal. 2021. https://extranet.who.int/sph/jee (accessed 4 October 2021 2021).
18. Garfield R, Bartee M, Mayigane LN. Validating Joint External Evaluation reports with the quality of outbreak response in Ethiopia, Nigeria and Madagascar. BMJ global health 2019; 4(6): e001655.
Health emergencies, AMR and Covid-19 response
19. Boyd MJ, Wilson N, Nelson C. Validation analysis of Global Health Security Index (GHSI) scores 2019. BMJ global health 2020; 5(10).
20. WHO. Joint external evaluation of IHR core capacities of the Republic of South Africa: mission reoport, 27 November - 1 December 2017. Geneva: WHO, 2018.
21. The Constitution of the Republic of South Africa. 1996.
22. National Health Act. South Africa; 2003.
23. Schedule of notifiable medical conditions. 1989.
24. The Republic of South Africa. The National Health Laboratory Services Act, 37 of 2000. Government Gazette 2000.
25. Disaster Management Act. Republic of South Africa; 2002.
26. International Health Regulations Bill. 2013.
27. Blumberg L, de Jong G, Thomas J, Archer B, Cengimbo A, Cohen C. Outbreaks in South Africa, 2004-2011, the outbreak response unit of the NICD and the vision of an inspired leader. South African Journal of Epidemiology and Infection 2011; 26(4): 195–204.
28. Paweska JT, Jansen van Vuren P, Meier GH, et al. South African Ebola diagnostic response in Sierra Leone: A modular high biosafety field laboratory. PLoS Negl Trop Dis 2017; 11(6): e0005665.
29. Weyer J, Blumberg LH. Ebola virus disease in West Africa--South African perspectives. S Afr Med J 2014; 104(11): 754–5.
30. Regulations relating to the surveillance and the control of notifiable medical conditions., in terms of the Nationla Health Act, 2003 (Act 61). In: Health Do, editor. Pretoria: Government Gazette; 2017.
31. Thomas J, Govender N, McCarthy KM, et al. Outbreak of Listeriosis in South Africa Associated with Processed Meat. N Engl J Med 2020; 382(7): 632–43.
32. Kaptchouang Tchatchouang CD, Fri J, De Santi M, et al. Listeriosis Outbreak in South Africa: A Comparative Analysis with Previously Reported Cases Worldwide. Microorganisms 2020; 8(1).
33. WHO. No time to wait: securing the future from drug-resistant infections. Geneva: WHO, 2019.
34. Meyers J. his is how many people antibiotic resistance could kill every year by 2050 if nothing is done. 2016. https://www.weforum.org/agenda/2016/09/this-ishow-many-people-will-die-from-antimicrobial-resistance-every-year-by-2050-ifnothing-is-done/ (accessed 3 October 2021 2021).
35. UN. Department of Economic and Social Affairs- Sustainable Development Goals. 2016. https://sdgs.un.org/goals (accessed 3 October 2021 2021).
36. Winters C, Gelband H. Part I. the Global Antibiotic Resistance Partnership (GARP). S Afr Med J 2011; 101(8 Pt 2): 556–7.
37. DAFF N. South African antimicrobial resistance national stragegy framework; a hone health approach. Tshwane: NDOH, 2018.
38. Schellack N, Benjamin D, Brink A, et al. A situational analysis of current antimicrobial governance, regulation, and utilization in South Africa. Int J Infect Dis 2017; 64: 100–6.
39. Ismail H, Lowman W, Govind CN, et al. Surveillance and comparison of antimicrobial susceptibility patterns of ESKAPE organisms isolated from patients with bacteraemia in South Africa, 2016 - 2017. S Afr Med J 2019; 109(12): 934–40.
40. Perovic O, Ismail H, Quan V, et al. Carbapenem-resistant Enterobacteriaceae in patients with bacteraemia at tertiary hospitals in South Africa, 2015 to 2018.
Eur J Clin Microbiol Infect Dis 2020; 39(7): 1287–94.
41. Engler D, Meyer JC, Schellack N, Kurdi A, Godman B. Antimicrobial Stewardship Activities in Public Healthcare Facilities in South Africa: A Baseline for Future Direction. Antibiotics (Basel, Switzerland) 2021; 10(8).
42. WHO. Global antimicrobial resistance and use surveillance system (GLASS). Geneva: WHO, 2021.
43. NDOH. Guidelines for the Prevention and Containment of Antimicrobial Resistance in South African Hospitals Pretoria: NDOH; 2019.
44. NDoH. Surveillance for Antimicrobial Resistance and Consumption of Antibiotics in South Africa. Pretoria: NDoH, 2018.
45. NDOH. National Infection Prevention and Control Strategic Framework Pretoria: NDOH; 2020.
46. WHO. Timeline: WHO’s COVID-19 response. 2020. https://www.who.int/ news-room/detail/29-06-2020-covidtimeline (accessed 21 September 2020 2020).
47. Abdool Karim SS. The South African Response to the Pandemic. N Engl J Med 2020; 382(e95).
48. Moonasar D, Pillay A, Leonard E, et al. COVID-19: lessons and experiences from South Africa’s first surge. BMJ global health 2021; 6(2).
49. Regulations issued in terms of Section 27 (2), Disaster Management Act, 2002, 18 March 2020. In: Affairs DoC-oGaT, editor. Pretoria: Government Gazette; 2020.
50. Amendment of Regulations issued in terms of Section 27 (2) of the Disaster Management Act, 2002, 26 March 2020. In: Affairs DoC-oGaT, editor. Pretoria: Government Gazette; 2020.
51. McCarthy KM, Tempia S, Kufa T, et al. The importation and establishment of community transmission of SARS-CoV-2 during the first eight weeks of the South African COVID-19 epidemic. EClinicalMedicine 2021; 39: 101072.
52. NDOH. National Plan for COVID-19 Health Response: South Africa. Pretoria: NDOH; 2020.
53. Mccarthy K, Tempia S, Kufa T, et al. The importation and establishment of community transmission of SARS-CoV-2 during the first eight weeks of the South African COVID-19 epidemic. eClinicalMedicine 2021.
54. Jassat W, Cohen C, Masha M, et al. COVID-19 in-hospital mortality in South Africa: the intersection of communicable and non-communicable chronic diseases in a high HIV prevalence setting. medRxiv 2020: 2020.12.21.20248409.
55. Talisuna A, Yahaya AA, Rajatonirina SC, et al. Joint external evaluation of the International Health Regulation (2005) capacities: current status and lessons learnt in the WHO African region. BMJ global health 2019; 4(6): e001312.
56. Wong MC, Huang J, Wong SH, Yuen-Chun Teoh J. The potential effectiveness of the WHO International Health Regulations capacity requirements on control of the COVID-19 pandemic: a cross-sectional study of 114 countries. J R Soc Med 2021; 114(3): 121–31.
Health emergencies, AMR and Covid-19 response
57. Clemente J, Rhee S, Miller B, et al. Reading between the lines: A qualitative case study of national public health institute functions and attributes in the Joint External Evaluation. Journal of public health in Africa 2020; 11(1): 1329.
58. Pillay Y, Barron P, Zondi T. Impact of COVID-19 on routine primary healthcare services in South Africa. S Afr Med J 2020; 111(8): 714–9.
59. Boulle A, Davies MA, Hussey H, et al. Risk factors for COVID-19 death in a population cohort study from the Western Cape Province, South Africa. Clin Infect Dis 2020.
60. Matatiele M, Stiegler N, Bouchard JP. Tri-infection: Tuberculosis, HIV, COVID-19 and the already strained South African health system. Brain Behav Immun 2021; 96: 5–6.
61. Chibabhai V, Duse AG, Perovic O, Richards GA. Collateral damage of the COVID-19 pandemic: Exacerbation of antimicrobial resistance and disruptions to antimicrobial stewardship programmes? S Afr Med J 2020; 110(7): 572–3.
62. Nyasulu J, Pandya H. The effects of coronavirus disease 2019 pandemic on the South African health system: A call to maintain essential health services. African journal of primary health care & family medicine 2020; 12(1): e1–e5.
63. Chersich MF, Gray G, Fairlie L, et al. COVID-19 in Africa: care and protection for frontline healthcare workers. Globalization and health 2020; 16(1): 46.
64. Ray S, Mash R. Innovation in primary health care responses to COVID-19 in SubSaharan Africa. Prim Health Care Res Dev 2021; 22: e44.
65. Van Ryneveld M, Schneider H, Lehmann U. Looking back to look forward: a review of human resources for health governance in South Africa from 1994 to 2018. Human resources for health 2020; 18(1): 92.
66. Bakibinga-Gaswaga E, Bakibinga S, Bakibinga DBM, Bakibinga P. Digital technologies in the COVID-19 responses in sub-Saharan Africa: policies, problems and promises. Pan Afr Med J 2020; 35(Suppl 2): 38.
67. Cooper S, van Rooyen H, Wiysonge CS. COVID-19 vaccine hesitancy in South Africa: how can we maximize uptake of COVID-19 vaccines? Expert review of vaccines 2021; 20(8): 921–33.
68. Hyland-Wood B, Gardner J, Leask J, Ecker UKH. Toward effective government communication strategies in the era of COVID-19. Humanities and Social Sciences Communications 2021; 8(1): 30.
69. Siphelele N, Douglas W. Mental health and COVID-19 in South Africa. South African Journal of Psychology 2021; 51(2): 304–13.
70. Loveday M, Cox H, Evans D, et al. Opportunities from a new disease for an old threat: Extending COVID-19 efforts to address tuberculosis in South Africa. S Afr Med J 2020; 110(12): 1160–7.
71. The Independent Panel for Pandemic Preparedness and Response. COVID-19: Make it the last pandemic. Geneva: WHO; 2021.
72. Sharp A, Jain V, Alimi Y, Bausch DG. Policy and planning for large epidemics and pandemics - challenges and lessons learned from COVID-19. Curr Opin Infect Dis 2021; 34(5): 393–400.
Non-communicable diseases (NCDs), also known as chronic diseases, are usually of long duration and can be caused by genetic, physiological, environmental and behavioural factors, but more typically a combination thereof (WHO, 2021). Examples of NCDs include cardiovascular diseases (CVDs), cancers, chronic respiratory diseases and diabetes.
NCDs are on the rise globally. It is estimated that the global NCD burden will increase by 17% in the next 10 years with a 27% increase in Africa (Wang & Wang, 2020). Additionally, the International Diabetes Federation (2021) predicts an increase of people with Diabetes mellitus (DM) by 129% to 55 million by 2045 in Africa.
In South Africa, NCDs contribute more to the national burden of disease than communicable diseases. A Statistics South Africa Mortality Report (2017) showed a three-year trend analysis for selected main groups of underlying causes of deaths for the years 2015 to 2017. Among NCDs, diseases of the circulatory system increased in proportion from 17.8% in 2015 to 18.4% in 2017 in contrast to infectious diseases, which declined from 19.5% in 2015 to 17.6% in 2017. According to the International Diabetes Federation (2021), South Africa ranks highest, in the Africa region, with the largest increase in the number of people with DM from 1.9 million in 2011 to 4.2 million in 2021.
As the figure below shows, from 2009 onwards the percentage of deaths from NCDs (group II) exceeded that from communicable diseases (group I). This coincides with the scaling up of access to antiretroviral therapy for people living with HIV (Johnson et al., 2017). Notably, as the contribution of communicable diseases as a percentage of total deaths declined, the contribution of NCDs increased sharply. Group III in Figure 9.1 refers to external causes of mortality such as accidents, homicides and suicides. This chapter will not cover road accidents, interpersonal violence and suicides as causes of both morbidity and mortality. The rates of these ‘external causes’ are around 10% of all
Sandhya Singh, Nombulelo Magula, Pamela Naidoo, Kwanele Asante, Yogan Pillayand show a marginal increase
2015.
in
will also not
9.1 Percentage of deaths from
of mortality (STATS SA, 2021)
major causes of death related to NCDs between 2016 and 2018 according to Statistics South Africa are: DM, cerebrovascular diseases, other forms of heart disease, and hypertension (STATS SA, 2021). These conditions may occur as co- or multi-morbidities with other NCDs or communicable diseases including HIV and AIDS and tuberculosis (TB).
common modifiable and unmodifiable risk factors for NCDs, such as diabetes type 2, hypertension and CVD and some of the cancers are largely known. These range from genetic and metabolic factors to what have become known as ‘lifestyle factors’. However, it is clear that characterising NCDs as a lifestyle issue places the blame on the individual and absolves environmental, social and commercial issues that relate to NCDs. In addition, the term lifestyle camouflages the contribution of unhealthy behaviours, which are not only ‘voluntary’ but also associated with negative living environments that are not conducive to adopting pro-healthy behaviours. As stated by Marmot and Bell (2019, pg. 10), ‘social determinants encompass the “causes of the causes” of health inequality: the unequal conditions in which people are born, grow, live, work, and age; and the inequities in power, money, and resources that give rise to them’. The WHO (2021) has recently acknowledged the importance of the commercial determinants of health and defined the commercial determinants as activities of the private sector that can negatively or positively affect health.
The guiding documents for NCDs programmes during the 2015–2020 period were the National Strategic Plan (NSP) for the Prevention and Control of Non-Communicable Diseases (2013–2017) as well as the Strategy for the Prevention and Control of Obesity (2015–2020). The NCD Strategic Plan 2013–2017 reflected government’s response to NCDs, which contribute towards the quadruple burden of disease experienced in the country. However, implementation of the strategy was uneven and performance towards attaining targets could not be measured due to the lack of baseline data and overall ineffective surveillance of NCDs in South Africa. Given the lack of routinely collected data on NCDs through the District Health Information System (DHIS) and the infrequency with which the Demographic and Health Survey has been conducted, it has been difficult to systematically evaluate the implementation of the NSP 2013–2017. Additionally, the poor implementation revealed the negative impact of an inadequate policy cohesion within the NDoH and between other government departments and sectors.
A process to draft the follow-on NCD strategic plan was initiated in 2018 and was completed in 2021. The reasons for this document being delayed is a result of ongoing consultation with stakeholders and lack of agreement on the type of document that would make a real difference. Civil society organisations preferred that the NCD strategic plan followed the format used for the HIV, STIs (sexually transmitted infections) and TB strategic plan, which they considered was the major reason for the relative success of these programmes. The HIV, STI and TB strategic plan placed significant emphasis on human rights as well as a multisectoral approach with defined roles for different sectors. In addition, the HIV, TB and STI strategic plan is co-owned by government, organised labour, business and civil society through the South African National AIDS Council.
In order to address the growing NCD burden of disease, the 2013–2017 NCD strategic plan adopted 10 goals and targets. These are reflected in the table below.
Table 9.1 Goals and targets in the 2013–2017 NCD Strategic Plan (NDoH, 2013)
Goal
Target to be reached by 2020 unless otherwise indicated
1. Reduce relative premature mortality (under-60 years of age) from NCDs Reduce by at least 25%
2. Reduce tobacco use Reduce by 20%
3. Reduce per capita consumption of alcohol Reduce by 20%
4. Reduce the mean population intake of salt Reduce by up to <5g per day
5. Reduce percentage of people who are obese and/or overweight Reduce by 10%
6. Reduce prevalence of raised blood pressure through lifestyle and medication Reduce by 20%
7. Increase prevalence of physical activity (150 mins of moderate activity per week) Increase by 10%
8. Every woman with STIs to be screened for cervical cancer
Every five years or three screens during her lifetime
9. Increase percentage controlled for hypertension, diabetes and asthma Increase by 30% in sentinel sites
10. Increase the number of people screened and treated for mental disorders Increase by 30% by 2030
Like many low- and middle-income countries (LMICs), routine surveillance systems to monitor NCDs in South Africa are sub-optimal. This compromises the ability of the NDoH to fully understand the burden of disease, its determinants as well as the impact of interventions.
While NCD outcomes remain poor, the country effected a range of legislative, regulatory and policy reforms aimed at addressing modifiable risk factors, including:
• A Regulation on Trans Fats in Foodstuffs was passed in 2011 (R127). According to this Regulation, the trans-fat content of any oils and fats cannot exceed two grams per 100 grams and products with higher trans fats levels are prohibited from entering or being sold in the country.
• The Human Papilloma Virus (HPV) vaccination programme was launched in 2014 by the NDoH, in partnership with the Department of Basic Education, as part of primary prevention against cervical cancer. The aim was to target an estimated 550 000 girls in grade 4, aged 9 years and 17 000 public and special schools, before they were exposed to HPV infection.
• In line with targets of the Strategic Plan, a Regulation on reduction of sodium in 13 categories of foodstuffs that are the most common source of sodium for the majority of South Africans was passed in 2013 (R214) and amended in October 2017.
• In February 2016, South Africa became the first country on the African continent to announce plans to introduce a tax fixed at 2.1 cents per gram of the sugar content of sugar-sweetened beverages that exceeds 4g per 100ml. The tax became law in April 2017.
• Regulations regarding warning labels on alcohol products were introduced in 2007 and amended in 2017.
• The Tobacco Products Control Act, Act no. 83 of 1993. South Africa was a global leader in tobacco control until the 2000s. In 2005, South Africa ratified the World Health Organization Framework Convention on Tobacco Control (WHO FCTC). The country is therefore a signatory to the WHO FCTC, thus it has an obligation to implement the WHO FCTC. The Tobacco Products Control Act was amended in 1999, 2007 and 2008. The amendments include a ban on tobacco advertisements and smoking in public places (but permit smoking in designated smoking areas) as well as an increase in the age of sale from 16 to 18 years.
• The NDoH is currently finalising development of the Front-of-Pack (FoP) labelling regulations as a tool to simplify nutritional information for consumers, in addition to making nutritional information mandatory on most food labels, irrespective of whether a claim is made or not. The nutrients are the same as those identified by the WHO in their global strategies which aim to reduce obesity and NCDs, namely added salt, sugars and saturated fat.
South Africa was one of the first countries to introduce mandatory salt reduction regulation for processed foods. A preliminary study by Strauss-Kruger et al. (2021) found that mandatory salt reduction in processed foods lowered the salt intake in young adults by 0.82 g salt/day. Consumer appreciation of the limitation of the use of these products after the legislation came into effect was assessed by Koen et al. (2021). They
found that over three-quarters of their sample did not notice any change in the taste of products after the law come into effect. However, these authors also found that only one-third of their study participants looked at the salt content of products before purchasing, which means that much more education around salt is required.
Research shows a significant positive impact of the levy on sugar-sweetened beverages. Stacey et al. (2021) found that sugar from taxable beverages declined from 16.25 grams per capita per day to 10.63 grams per capita per day post implementation. In addition, they found that this decline was larger in low-income households relative to higher-income households – similar to findings in Mexico. Moreover, Hofman et al. (2021) cite a number of other local studies that show the impact of this levy on the consumption of sugar-sweetened beverages.
Box 1: Impact of salt and sugar legislation
Salt intake has decreased in young people by 0.82g/day after the introduction of mandatory salt regulation for processed foods.
While both low- and high-income households reduced their sugar intake from sugar-sweet ened beverages, the reduction was higher for low-income households after the introduction of the levy.
In addition to related existing policies, action plans, guidelines and user guides, the following have been developed since 2015.
• Framework and Strategy for Disability and Rehabilitation Services in South Africa 2015–2020
• Strategy for the Prevention and Control of Obesity in South Africa 2015–2020
• National Cancer Strategic Framework 2017–2022 (2017)
• Cervical cancer policy (2017)
• Breast cancer policy (2017)
• Updated Management of type 2 diabetes in Adults at Primary Care Level (2017)
• National Policy Framework and Strategy on Palliative Care 2017–2022 (2017)
• National User Guide on the Prevention and Treatment of Hypertension in Adults at PHC Level, 2021.
In addition, a number of health systems changes were introduced that have benefitted persons with NCDs.
• An Integrated Clinical Services Model that incorporates all chronic diseases, whether communicable or non-communicable, was introduced through the Ideal Clinic Initiative. This means that patients are seen for whatever chronic disease they have, including for multiple conditions, during the same visit. As of 2018, 97.2% of clinics had reorganised services with designated consulting areas for management of chronic conditions and had patient appointment systems for people with chronic conditions.
• NCDS were fully included in the Primary Health Care Service Package drafted in 2015. The most common NCDs have also been included into the Adult Primary Care package including asthma/COPD, screening for breast and cervical cancers, cardiovascular disease, diabetes, mental health conditions, epilepsy, and musculoskeletal disorders.
• Medicines for many patients who have controlled NCD conditions are provided through the Centralised Chronic Medicines Dispensing and Distribution (CCMDD) model.
• Training of community health workers on NCDs including on screening for hypertension and diabetes at a community level.
The case for investing in NCDs has been made globally. The WHO estimates that investing an additional 1 US dollar per person annually can save 7 million lives by 2030 in LMICs (WHO, 2021).
Investment in NCD programme implementation is channelled to the provinces and calculated through the equitable share formula as per the Division of Revenue Act and through dedicated conditional grants for oncology and mental health, as well as for NCD-related services provided at tertiary hospitals through the National Tertiary Services Grant. It is not possible to estimate how much provinces invest in NCD implementation using the equitable share as this is not itemised in provincial or facility-level budgets. In addition, the NDoH received a small allocation from the revenues raised from the health promotion levy for use to strengthen health promotion.
A criticism has been that of the R3.195 billion collected in 2018 only R100 million – less than 5% of the total revenue raised – was allocated for health promotion activities (van Rensburg, 2020).
Despite some progress in the development and implementation of strategies, policies and guidelines, South Africa, like many other LMICs, is not on track to meet the Sustainable Development Goal (SDG) Target 3.4 by 2030 – which is to reduce by one-third premature mortality from NCDs through prevention and treatment and promote mental health and well-being. It is therefore not surprising that advocating for the prioritisation of NCDs globally and locally now mainly pertains to equity and human rights. People in LMICs are disproportionally affected by NCDs and the poorest and most vulnerable communities continue to be at highest risk for disease, experience greatest barriers to accessing essential health care and are experiencing the impact of the commercial determinants of health. The poor and vulnerable are less likely to appreciate the impact of commercial determinants of health, due to lack of exposure to education and the appropriate knowledge into the role of the private sector in driving unhealthy behaviours through the marketing of products such as tobacco, and increased levels of salt, sugar and trans fats in food products. This reality highlights the urgency with which SDG Target 1, to end poverty in all its forms everywhere, must be attained, in order to accelerate progress to achieve SDG Target 3.4.
Challenges experienced during the past five years relate to inadequate priority given to the co-existence of NCDs and communicable diseases such as HIV, AIDS and TB. The attention to multi-morbidities has not kept pace with the attention to detection, treatment and care as was the case with HIV and AIDS. There needs to be both high-level political support and resources to address this burden of diseases. This is an issue that civil society organisations have raised, noting that simply acknowledging the escalating burden of NCDs at political and strategic levels fails to translate into desired action on patient engagement and empowerment as well as along the entire continuum of NCD prevention and control (South African Non-Communicable Diseases Alliance and the Cancer Association of South Africa, 2021).
In addition, the importance of involving people living with NCDs in the development of strategies, policies and guidelines at global and national levels has been acknowledged from a rights perspective and has been accepted by policy-makers (Asante, 2021; WHO, 2021). In recognition, the NDoH included a number of civil society representatives to participate in the development of the NSP. This is in line with the efforts by the WHO to convene and partner with civil society organisations in policy and guideline development (WHO, 2021).
At a population level, the significant impact of the social, economic and commercial determinants of health is observed, resulting in an escalation of preventable diseases related to, for example, obesity. According to UNICEF (2019), South Africa has the largest percentage of overweight children under the age of five years and between 10 and 19 years in Eastern and Southern Africa. The South African Demographic and Health Survey (SADHS) (2019) found that a significant percentage of men and women who perceived themselves to be either underweight or of normal weight were overweight or obese. Similarly, the survey found that self-reports of diabetes and hypertension were lower than tested prevalence. Of concern is that the survey reported that among people with hypertension, 80% of women and 87% of men have uncontrolled hypertension. These results strongly suggest that awareness of the risk factors as well as NCDs is low in many communities.
Despite the NCD Declaration of the first UN High-Level Meeting on Noncommunicable Diseases held in 2011 urging all governments to commit to adopting an ‘all of government’ and ‘all of society approach’, South Africa has not established mechanisms to ensure intersectoral collaboration across government and with civil society to combat the growth of NCDs. The lack of coordinating mechanisms to enable policy cohesion and implementation between government departments and with other sectors not only perpetuates the escalating burden of NCDs, but more importantly results in lack of accountability for meeting global and national targets.
During the five-year period provinces such as Gauteng, KwaZulu-Natal, Limpopo and Mpumalanga experienced challenges with the provision of radiation oncology services due to shortage of staff and equipment breakdowns (Schutz, 2020). This was especially acute in KwaZulu-Natal, which led to a South African Human Rights Commission investigation, for example. A number of interventions were implemented to address these challenges, including procurement of equipment and the contracting of private sector oncologists to treat public sector patients. However, many challenges related to long waiting times for oncology services remain and were exacerbated by the COVID-19 pandemic (Cancer Alliance, 2020).
The approach used for the control of the HIV epidemic at municipal ward level through Ward AIDS committees, Ward-based Outreach Teams and Operation Sukuma Sakhe in KwaZulu-Natal brings together different sectors of government as a multisectoral strategy to ending the HIV epidemic as a public health threat. An integrated approach to disease control would benefit control of NCDs leveraging experiences gained using this ward-based multisectoral approach. This approach would accelerate education, screening, testing, early detection and access to care, supported by health promotion and disease prevention interventions through multisectoral structures. Potential benefits would include reducing waiting times for appropriate oncology interventions, improved access to mental health services – which in turn improves outcomes for other diseases such as for those living with HIV and other chronic diseases, prevention of end-stage kidney diseases which require dialysis or renal transplantation, and disabilities from stroke and amputations.
One of the major challenges with data on NCDs is that very little is collected routinely through the DHIS (Wandai et al., 2017). Thus, both programme planning and review of progress relies largely on survey data.
As illustrated above, by 2018 NCDs contributed almost 60% of all deaths, with communicable diseases contributing about 30% and external deaths such as accidents and suicides contributing the remainder. Between 2015 and 2018 (the most recent year for which data is available from STATS SA) the portion of deaths from NCDs increased from 55.4% to 59.3%.
The only survey data that collected data on NCDs during this period was the SADHS which reported in 2019 on data collected in 2016. While the data from the SADHS cannot be used to report about the targets in Table 9.1, it provides some idea of key indicators. The following reflects the data on selected NCDs from the SADHS (2019).
• High blood pressure was the most common self-report condition reported: women (23%) and men (13%).
• The prevalence of measured hypertension nearly doubled since 1998, from 25% to 46% among women and from 23% to 44% among men.
• The prevalence of asthma symptoms in adults was between 3% and 4% with symptoms of COPD at less than 2%.
• 13% of women and 8% of men 15 years and older had an HbA1c level of 6.5% or above, indicating that they were diabetic.
• High proportions of women (64%) and men (66%) were pre-diabetic with HbA1c levels of between 5.7% and 6.4%.
• While 5% of women and 4% of men self-reported being diabetic, 10% of women and 6% of men who were not previously diagnosed were found to be diabetic and 67% of both women and men were found to be pre-diabetic.
• While 13% of children were found to be overweight, 27% of children under five years of age were stunted with 3% wasted, and a further 6% underweight.
• Only 30% of women and 59% of men were found to be within the normal BMI range – with a significant percentage being either overweight or obese.
(There are no comparable data for 2020.)
Avoidable mortality from NCDs: The WHO’s best buys


Figure 9.2 shows estimates of mortality from NCDs. These estimates suggest that the probability of premature death in both males and females will not meet global targets by 2025, although the possibility of females reaching global targets appears to be more likely.
The WHO (2018) also suggests that by adopting the WHO’s best buys 67 800 deaths can be averted in the country by 2025. The best buys (Figure 9.3 below) include: re duce tobacco use, reduce harmful alcohol use, decrease unhealthy diets, increase physical activity, and focus on CVDs, diabetes and cancers.
Data on the cancer programme is largely laboratory based through the National Cancer Registry (NCR). The most recent data from the NCR is for 2018. The table below reflects the number of cancers reported by type and gender. As can be seen from Table 9.2, the most frequently reported cancers in women are: breast, cervical, basal cell carcinoma, squamous cell carcinoma, colorectal and uterus, whilst the most frequently reported male cancers are prostate, basal cell carcinoma, squamous cell carcinoma, colorectal and lung cancers. The picture has not changed over the last four years for which data is available. The quality of the data collected through the NCR depends on clinicians at facility level reporting data required against all data elements. A study at Chris Hani Baragwanath Hospital found that of 398 records of breast cancer from the hospital’s registry, all but one were matched to the NCR, giving a catchment rate of 99.75% (Ndlovu et al., 2022). Whilst this study focused on only one type of cancer and one tertiary facility, it does provide some level of assurance of the completeness of data.
Routine data on cervical cancer screening is available from the DHIS. The national target for screening is 60% which has not been reached. In 2017 the national average was 42.7% (ranging from 30.6% to 57.1%). However, this was worsened by the COVID-19 pandemic – the national average in 2020 was 39.1% (range of 18.1% to 45.9%).
Table 9.2 Most frequently reported cancers (National Cancer Registry: 2015–2018)
Type Female Male
Primary
According to the SADHS (2019), 37% of men and 7% of women use tobacco products. With respect to tobacco smoking, South Africa is on track to meet global targets for females but not males (see Figure 9.4 below). According to Tobacco Tactics (2021), smoking prevalence declined from 33% in 1993 to 20% in 2017, however, the majority of the decline was in the 1990–2010 period. They also estimate that about 44 000 South Africans die annually from tobacco-related diseases.
Alcohol consumption is another major contributor to NCDs, such as cardiovascular diseases. According to the WHO (2016), consumption of pure alcohol in people over 15 years of age was 7.1 litres per person per year; however, if only those who drink alcohol were included, this increases to a staggering 29.9 litres per year. Both the WHO and others report that binge drinking especially among the poor and young people is a major issue (Marx et al., 2021).
Levels of physical inactivity are high in the country, with one report suggesting that 57.4% of the population is inactive, 14.8% are moderately active and 27.8% are very ac tive (Mlangeni et al., 2018). South Africa’s 2018 Report Card on Physical Activity for Children and Youth suggests that the country is making insufficient progress with regard to the promotion of physical activity opportunities that are safe and accessible for the greatest number of children and adolescents (Draper et al., 2018).
According to the World Obesity Federation (2020), 21% of South African women over the age of 20 years have a BMI greater than 35kg/m2, implying severe obesity. This puts South Africa in the top 20 countries in the world with such high rates of female obesity. The Federation rates South Africa’s chance of meeting the UN global obesity targets by 2025 as ‘very poor’.
For obesity, the trajectory for both males and females is upwards and the country is not on target to meet global goals for both sexes. The country is also likely to miss the 2025 global targets on blood pressure as well

South Africa has both significant under-nutrition as well as over-nutrition (more accurately, poor eating habits). Apart from the high levels of obesity reflected above which is more severe in women than men, many children are underweight and stunted. The causes of both under- and overweight are different, with the former largely a result of poverty and food insecurity, while the causes of the latter are largely due to eating either the wrong types of food (or in the wrong combination) or eating too much and/ or inadequate physical activity.

The pandemic has exposed an intimate relationship between communicable and non-communicable diseases, placing a sharp focus on inequalities globally and in South Africa and is an important determinant in clinical outcomes. Those with comorbid NCDs were more likely to develop moderate to severe COVID-19 or die. A lack of pandemic preparedness saw disruption in health services in the process of flattening the COVID-19 pandemic curve at the early stages of the pandemic. Although lockdown regulations did not restrict access to health care facilities, access to facilities was reduced for various reasons including fear of contracting COVID-19, and reduced access to transportation or income. Consequently, screening and testing for NCDs was reduced during the pandemic, including access to treatment and assessment for disease control.
The pandemic reveals significant shortcomings in the country’s response towards the prevention and control of NCDs. According to the hospital-based surveillance system, as of 10 April 2021, 231 237 COVID-19 admissions were reported from 644 facilities (393 public sector and 251 private sector) in all nine provinces of South Africa. There were 121 918 (52.7%) and 109 319 (47.3%) admissions reported in public and private sector hospitals, respectively. On multivariable analysis, factors associated with in-hospital mortality, among other, were patients having comorbid hypertension, diabetes, chronic cardiac disease, chronic renal disease, malignancy, HIV, current and past TB, and obesity.
The approach taken in developing the NSP was to be inclusive, involving NCD stakeholders, and to prioritise those NCDs that contributed the greatest to the burden of disease. The term NCD+ has been adopted in the NSP to signify the importance of the determinants of health (social, economic and commercial) as well as its disproportionate impact on the poor (CANSA, 2020).
The Box below illustrates the process used to develop the NSP in line with WHO guidance on the need for inclusivity and the slogan of ‘nothing about us, without us’.
Box 3: Lessons from the participatory process in developing the NSP 2022–2027

The target for South Africa in the newly adopted NSP, in compliance with the SDG Target 3.4, is to reduce, by one-third, premature mortality from NCDs+ through prevention and treatment and promote mental health and well-being by 2030. The overall aim for the NSP is to progressively improve wellness and reduce premature morbidity, disability and mortality from NCDs+ through the continuum of care across the life course.
The NSP promotes critical reforms, including the adoption of the WHO’s Integrated People-Centred Health Service (IPCHS), the development of a high-level multisectoral governance structure and the initiation of the cascading approach to NCDs. Based on the lessons learnt from the 90-90-90 cascading approach for HIV/ AIDS, the NSP outlines a similar approach for NCDs+, beginning with cascades for diabetes and hypertension. Experience in the HIV response has demonstrated that time-bound targets drive progress, promote accountability, and unite diverse stakeholders – motivating both behaviour and investments (Zuniga, 2018).
A 90/60/50 model is proposed to be applied to blood pressure and blood glucose screening treatment and monitoring as a first step to improving early detection and treatment of NCDs+.
• 90% of all people over 18 will know whether they have hypertension and/or raised blood glucose or not;
• 60% of people with raised blood pressure or blood glucose will receive intervention; and
• 50% of people receiving interventions will be controlled.
Whilst the actual implementation of the NSP lies within the remit of stakeholders that include but go beyond the NDoH, clearly defined guiding principles will be used to ensure the implementation of this NSP is underpinned by core values and principles that apply across the full burden of disease and require a robust health system. These guiding principles for action were identified as critical following a review of the Strategic Plan for the Prevention and Control of Non-Communicable Diseases 2013–2017 and are also identified as important principles in the WHO Global Action Plan 2013–2020. The six guiding principles are described in Table 9.3.
Non-communicable diseases
The Bill of Rights in Chapter 2 of the Constitution lists 39 rights, apart from the right to health (Section 27) which influence the prevention and care for PLWNCDs+. These are: equality (9), dignity (10), life (11), health care, food, water and social security (27), children (28), environment (24 a) and just administrative action (33). Additionally, the constitutional values and principles governing public administration, i.e. transparency, participatory policy-making and accountability are relevant and important. This NSP aims to reinforce these rights through progressive realisation of equitable access to quality and affordable health care and interventions irrespective of ethnicity, gender, language, religion, political or health condition.
PLWNCDs+ experience significant inequities through financing, benefits packages and service delivery across the health sector. This NSP aims to raise the profile of NCDs+ as a priority in South Africa, through the prioritisation of NCDs+ from policy to service delivery and ensuring equitable access to NCD+ services for PLWNCDs+ and vulnerable populations therein.
UHC is linked to SDG Target 3.8 and the South African government’s commitment to UHC, through the delivery of NHI, is an important consideration in the formulation and delivery of this NSP. This NSP, developed during the health sector transition, and the implementation of NHI, endeavours to make its objectives align with the incremental achievement of UHC.
It must be noted that the NHI policy remains in draft form with ongoing implementation occurring in stages, many of which may occur after the expiration of this NSP.
Taking account of the structural and governance challenges that maintain siloed approaches and whilst we await the completed health sector transition, this NSP embraces the spirit of working in an integrated manner across directorates and within the health sector.
This integration occurs in various ways, including:
a) National Policy Alignment
b) Multisectoral and Multi-Stakeholder Engagement
c) Integration within the NDoH
d) Integration of Health Service Delivery
e) Integration across Health Conditions
The critical need for integration of NCDs+ with health programmes, in health systems, across levels and continuum of care, into service delivery platforms and care pathways, and across levels of government and with sectors and stakeholders is underpinned by the IPCHS framework which provides a basis for the goals within this NSP.
The Ottawa Charter (WHO, 1986), Alma-Ata Declaration and most recently, the IPCHS framework (WHO, 2016) all recognise the vital need to engage with and empower individuals and communities. This NSP aims to provide individuals and communities with opportunities, skills and resources as a means to participate actively and meaningfully in their health and health care in order to ensure the co-production of health espoused by the IPCHS model.
The life-course approach focuses on how multiple determinants interact to affect health throughout life and across generations. Health is considered as a dynamic continuum rather than a series of isolated health states. The approach highlights the importance of transitions (linking each stage to the next), of defining protective risk factors, of prioritising investment in health care and social determinants of health, and of gender equality and the promotion of human rights early in the life-course.
Whilst this NSP acknowledges the importance of the first 1000 days in addressing risk to the unborn child, the health status of the woman prior to conception presents a risk to both mother and baby and therefore requires monitoring throughout.
South Africa has made some progress in reducing NCDs, largely through the implementation of legislation. Legislative changes have impacted positively on several of the factors for NCDs, including those for sugar-sweetened beverages and salt. Whilst the decline in the use of tobacco products appears to have stagnated, the recent lockdowns in reaction to the COVID-19 pandemic and the ban on the sale of all tobacco and vaping products between 27 March and 17 August 2020 were found to have resulted in 9% of smokers successfully quitting (Filby et al., 2021).
While the NSP 2013–2017 included all the elements of interventions to respond to the burden of disease from NCDs, it suffered from a range of challenges. These included the lack of sufficient intersectoral collaboration as well as the means to measure progress or lack thereof and for course correction during the period 2013–2017. In addition, the hiatus between 2017 and 2020 – with no plan to guide intervention as a result of a protracted period of consultation for the drafting of the new NSP – also resulted in inadequate progress.
The COVID-19 pandemic illustrated the importance of a multi-modal approach to diseases and the need to be able to deal with patients holistically, given the range of comorbidities that patients are increasingly presenting with. Hence the importance of designing programmes and systems that place the patient/person at the centre, as described in the IPCHS Framework produced by the WHO.
The new NSP, which uses a cascade approach for diabetes and hypertension and which calls for the establishment of a coordinating mechanism similar to that for HIV and TB, holds much promise. However, unless there is high-level political support and additional funding to implement the NSP, progress in reducing the burden of NCDs in the country may be slow.
Asante K. The right to participate: An under-utilised component of the right to the highest attainable standard of health. BMJ. February 16, 2021 https://blogs.bmj. com/bmj/2021/02/16/the-right-to-participate-an-under-utilised-componentof-the-right-to-the-highest-attainable-standard-health/ (Accessed 24 January 2022).
Cancer Alliance (2020). Cancer Treatment Challenges During COVID-19; Letter to Minister Mkhize, 29 April 2020. https://cansa.org.za/cancer-treatment-challenges-during-covid-19/ (Accessed 12 January 2022).
CANSA (2020). Time to ACT on NCDs and Build Back Better. https://cansa.org.za/ time-to-act-on-ncds-and-build-back-better/ (Accessed 20 January 2022)
Department of Health (2013). National Strategic Plan for the Prevention and Control of Non-Communicable Diseases (2013–2017). Pretoria. https://www. iccp-portal.org/system/files/plans/South%20Africa_NCDs%20STRAT%20 PLAN%20%202013.pdf (Accessed 28 November 2021).
Filby S, van der Zee K, van Walbeek C. The temporary ban on tobacco sales in South Africa: lessons for endgame strategies. Tobacco Control. Published Online First: 20 January 2021. Doi: 10.1136/tobaccocontrol-2020-056209 (Accessed 17 January 2022)
Ganju A, Goulart A, Ray A, Majumdar A, et al. Systemic Solutions for Addressing Non-Communicable Diseases in Low-and Middle-Income Countries. Journal of Multidisciplinary Healthcare. 2020;13:693-707. 10.2147/JMDH.S252300. https://www.researchgate.net/publication/343224853_Systemic_Solutions_for_ Addressing_Non-Communicable_Diseases_in_Low-and_Middle-Income_ Countries (Accessed 6 December 2021).
Hofman K, Stacey N, Swart EC, Popkin BM, Ng SW. South Africa’s Health Promotion Levy: Excise tax findings and equity potential. Obesity Reviews. 2021;22(9). https://onlinelibrary.wiley.com/doi/epdf/10.1111/obr.13301 (Accessed 20 January 2022).
International Diabetes Federation (2021). IDF Diabetes Atlas, 10th edition. https:// diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_ Edition_2021.pdf (Accessed 12 January 2022).
Johnson LF, May MT, Dorrington RE, Cornell M, Boulle A, Egger M, Davies MA. Estimating the impact of antiretroviral treatment on adult mortality trends in South Africa: A mathematical modelling study. PLoS medicine. 2017;14(12): e1002468. https://doi.org/10.1371/journal.pmed.1002468 (Accessed 12 January 2022).
Koen N, Marais M, Smit Y, Nel D, Engelbrecht L. Sodium reduction regulations in South Africa – the consumer perspective. Journal of Consumer Science. 2021;6. Knorr. Plate of the Nation: A look at what South Africans are eating. March 2020. https://www.knorr.co.za/content/dam/unilever/knorr_world/south_africa/ print_comms_/knorr_plate_of_the_nation_report-2033974.pdf (Accessed 1 December 2021)
Marmot M, Bell R. Social determinants and non-communicable diseases: time for integrated action. BMJ. 2019;365: Suppl 1. https://www.bmj.com/content/ bmj/364/bmj.l251.full.pdf (Accessed 6 December 2021).
Marx MF, London L, Harker N, Ataguba JE. Assessing Intertemporal Socioeconomic Inequalities in Alcohol Consumption in South Africa. Front. Public Health, 11 May 2021 | https://doi.org/10.3389/fpubh.2021.606050 (Accessed 17 January 2022).
Mlangeni L, Makola L, Naidoo I, et al. Factors Associated with Physical Activity in South Africa: Evidence from a National Population Based Survey. The Open Public Health Journal. 2018. https://openpublichealthjournal.com/ VOLUME/11/PAGE/516/FULLTEXT/ (Accessed 1 December 2021).
National Department of Health, Statistics South Africa, South African Medical Research Council and ICF (2019). South Africa Demographic and Health Survey, 2016. Pretoria.
National Institute for Communicable Diseases National Cancer Registry. https:// www.nicd.ac.za/centres/national-cancer-registry/ (Accessed 3 December 2021).
Ndlovu BC, Sengayi-Muchengeti, Kellett P, Kuonza L, Cubasch H, Singh E, Chen WC. Completeness of reporting of breast cancer data in the National Pathology-Based Cancer Registry in South Africa. Journal of Registry Management. 2021;48(2).
Schutz E. Cancer care in the public sector: Are things getting better? 2020. https:// www.spotlightnsp.co.za/2020/12/08/cancer-care-in-the-public-sector-arethings-getting-better/ (Accessed 12 January 2022).
South African Non-Communicable Diseases Alliance and the Cancer Association of South Africa (2021). Communities to Act on Non-Communicable Diseases (NCDs). https://cansa.org.za/communities-to-act-on-non-communicablediseases-ncds/ (Accessed 12 January 2022).
Spotlight, 13 November 2020. https://www.spotlightnsp.co.za/2020/11/13/ finding-the-money-the-case-for-raising-the-health-promotion-levy/ (Accessed 20 January 2022).
Stacey N, Edoka I, Hofman K, Swart EC, Popkin B, Ng SW. Changes in beverage purchases following the announcement and implementation of South Africa’s Health Promotion Levy: an observational study. The Lancet Planetary Health. 2021;5(4): e200-e2008. https://www.thelancet.com/action/showPdf?pii =S2542-5196%2820%2930304-1 (Accessed 17 January 2022).
Statistics South Africa (2021). Mortality and causes of death in South Africa: Findings from death, 2018. (Accessed 3 December 2021). notificationhttps://www.statssa. gov.za/publications/P03093/P030932018.pdf (Accessed 28 November 2021).
Strauss-Kruger M, Wentzel-Viljoen E, Ware LJ, Van Zyl T, Charlton K, Schutte AE. Early evidence for the effectiveness of South Africa’s legislation on salt restriction in foods: the African-predict study. Journal of Hypertension. April 2021;39: e391e392. doi: 10.1097/01.hjh.0000749104.76735.72 9 (Accessed 17 January 2022).
Tobacco Tactics (2021). South Africa – country profile. https://tobaccotactics.org/ wiki/south-africa-country-profile/ (Accessed 17 January 2022).
UNICEF (2019). Poor diets damaging children’s health worldwide, warns UNICEF. https://www.unicef.org/southafrica/press-releases/poor-diets-damagingchildrens-health-worldwide-warns-unicef (Accessed 12 January 2022).
van Rensburg R. Finding the money: The case for raising the Health Promotion Levy. 2020.
Wandai M, Aagaard-Hansen J, Sartorius B, Hofman KJ. Available data sources for monitoring non-communicable diseases and their risk factors in South Africa. S Afr
Med J. 2017;107(4):331-337. DOI:10.7196/SAMJ.2017.v107i4.11438
Wang, Y., Wang, J. Modelling and prediction of global non-communicable diseases. BMC Public Health 20, 822 (2020). https://doi.org/10.1186/s12889-02008890-4 (Accessed 12 January 2022).
World Health Organization (1978). Declaration of Alma-Ata: International Conference on Primary Health Care, Alma-Ata, USSR, 6-12 September 1978. https://cdn.who.int/media/docs/default-source/documents/almaatadeclaration-en.pdf?sfvrsn=7b3c2167_2 (Accessed 17 January 2022).
World Health Organization (1986). Ottawa Charter for Health Promotion. https:// www.euro.who.int/__data/assets/pdf_file/0004/129532/Ottawa_Charter.pdf (Accessed 17 January 2022).
World Health Organization (2016). Framework on integrated, people-centred health services. https://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_39-en.pdf (Accessed 17 January 2022.
World Health Organization (2016). South Africa. Alcohol consumption, levels and patterns. https://www.who.int/substance_abuse/publications/global_alcohol_ report/profiles/zaf.pdf?ua=1 (Accessed 17 January 2022).
World Health Organization. (2018). Noncommunicable diseases country profiles 2018. World Health Organization. https://apps.who.int/iris/handle/10665/274512. (Accessed 1 December 2021).
World Health Organization. (2019). Global status report on alcohol and health 2018. World Health Organization. https://www.who.int/publications/i/ item/9789241565639 (Accessed 1 December 2021).
World Health Organization (2021). Commercial determinants of health: key facts. 5 November 2021. https://www.who.int/news-room/fact-sheets/detail/ commercial-determinants-of-health (Accessed 12 January 2022).
World Health Organization (2021). Investing 1 dollar per person per year could save 7 million lives in low- and lower-middle-income countries. 13 December 2021. https://www.who.int/news/item/13-12-2021-investing-1-dollar-per-personper-year-could-save-7-million-lives-in-low-and-lower-middle-income-countries (Accessed 12 January 2022).
World Obesity Federation (2020). Obesity: missing the 2025 global targets: Trends, Costs and Country Reports. https://data.worldobesity.org/publications/WOF-Missingthe-2025-Global-Targets-Report-FINAL-WEB.pdf (Accessed 17 January 2022).
World Health Organization (2021). Non-communicable diseases: key facts. https:// www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (Accessed 20 January 2022).
WHO (2021). Nothing for us, without us. Opportunities for meaningful engagement of people living with NCDs: meeting report. Geneva: World Health Organization (Accessed 24 January 2022)
Zuniga JM. UNAIDS 90-90-90—Opportunity in Every Difficulty. J Int Assoc Provid AIDS Care. 2018 Jan-Dec; 17. doi: 10.1177/2325958218809075) (Accessed 27 December 2021).
According to the latest estimates, more than 90% of uninsured people living with a mental, neurological or substance use condition in South Africa do not have access to evidence-based mental health care (Docrat, Besada, et al., 2019). Even though there have been some advances in service delivery, research and policy, the mental health gap is unacceptably high and the quality of care is often inadequate. In this chapter we highlight the various successes in the mental health sector for the period 2015–2020, but also raise areas of concern that require urgent attention. We call attention to system failures and other challenges, which are imperative for government decision-makers and the mental health community to address.
This chapter embraces a dimensional approach to mental health, i.e. that mental health exists on a continuum from severe disability to well-being, as defined in the Lancet Commission on Global Mental Health (Patel et al., 2018). The chapter covers five areas. We begin with two recent crises in South African mental health, namely, the Life Esidimeni tragedy and the COVID-19 pandemic. These crises were moments when radical changes could have been implemented to expand and improve mental health services. The second section addresses service organisation. We highlight the importance of making optimal use of scarce resources and bring into focus the need for a comprehensive approach to service provision, including mental health promotion and prevention.
Third, we address concerns related to human resources in the context of the inequitable distribution of specialist mental health professionals and facilities across the country. We discuss the merits of task-sharing in the context of a resource-constrained environment and identify issues that should be considered to ensure the success of such an approach.
Ashraf Kagee, Sumaiyah Docrat, Melvyn Freeman, Crick Lund, Sifiso Phakathi, Dudu Shiba, Rita ThomFourth, we focus on the depth of research on public mental health conducted in South Africa. It is fortunate that the country has a highly trained and committed cadre of researchers in public mental health. We showcase some of the pioneering work that has been conducted on low-cost intervention delivery methods for mental health. Finally, we address the issue of mental health service costs and needed investments in the context of the National Health Insurance (NHI) transition and the post-pandemic fiscal climate.
Two major crises have been enormously destructive to the mental health of individuals and to the system of service provision in South Africa. These are the Life Esidimedi tragedy of 2016/17 and the COVID-19 pandemic of 2020/21.
The LE tragedy involved the death of 144 persons with mental health conditions in 2016. To conserve costs, the Gauteng Department of Health terminated a contract with Life Esidimeni, which resulted in 1 711 patients being transferred to the care of their families, NGOs and other institutions. The NGOs were not capacitated to provide the necessary specialised care to service users and 144 died due to starvation and neglect. At the LE Arbitration in 2017, former Deputy Chief Justice Dikgang Moseneke referred to the ‘inhumane treatment and torture of mental health care users’ that led to these deaths (Durojaye & Agaba, 2018).
Opposition parties, the media and members of the public sought to hold decision-makers and public servants accountable. They campaigned for compensation, mainly for family members (rather than those who survived the experience) and discussed how similar disasters could be prevented in the future. However, the fundamental questions of where and how people with severe and long-term psychosocial disabilities should be cared for, and how this tragedy could influence potential improvements in mental health care, were not addressed. The human rights of people with psychosocial disabilities, such as the right to liberty and to live in a community, rather than in institutional care, were given very low prominence.
The response of the Health Minister, Dr Aaron Motsoaledi, was to get every person who had been transferred out of the LE institutions back into facilities where they would be safe and where their basic and health care needs would be met. Unfortunately, this approach meant returning to a largely discredited status quo. Instead, what was required in the short term was investment in developing and supporting community-based services and facilitating access to specialist support in the District Health Services (DHS). The Department’s Mental Health Policy Framework states that there is currently an over-reliance on psychiatric hospitals and that community mental health services should be scaled up (Department of Health, 2013). Thus, simply getting people back into institutions was retrogressive. The LE crisis would have been the perfect opportunity to start adequately resourcing and training community facilities and thereby give persons with psychosocial disabilities more humane and more normal lives than is currently the case. Importantly, service users were returned to institutions without
consultation. The state was prepared to pay for institutional care, and in fact increased the daily amount from prior to the crisis (M. Freeman, personal communication, 20 October 2021). However, it was not prepared to invest the same amount for care provision within the community.
Following the LE tragedy, the South African Human Rights Commission held hearings in 2017 into the status of mental health care in South Africa and recommended improvements in services and legislation (SAHRC, 2017). The National Department of Health (NDoH) is currently working on how best to implement these recommendations that include, inter alia, reduced reliance on institutions and building community mental health care. However, thus far progress has been minimal, and the opportunity created by the huge public interest in mental health following the tragedy appears to have been squandered. It is critical that every effort is made to move rapidly to strengthen community mental health services.
The COVID-19 pandemic of 2020 and 2021 brought the realities of poor mental health and the need for mental health promotion and care into focus for millions of South Africans and people globally. A Lancet review of mental health effects of COVID-19 in low- and middle-income countries (LMICs) showed an increased prevalence of psychological distress and mental disorders (Kola et al., 2021). These may be attributed, inter alia, to continued uncertainties about the spread of the disease, the consequences of containment strategies, bereavement, and uncertainty about when and how everyday life would return to normal. The lockdown, aimed at mitigating the spread of COVID-19, has increased peoples’ isolation and has had huge negative economic impacts such as job loss and business closures, which in turn have impacted mental health. Family violence including gender-based violence has also increased (Clark, 2020). In South Africa the volume of calls to the South African Depression and Anxiety Group helpline doubled during the pandemic. An average of 1 400 people reached out every day, reflecting the added mental health burden from COVID-19 (Pijoos, 2021). In March 2021 the results of an innovative methodology to assess the impact of the pandemic on mental well-being across diverse global settings demonstrated that South Africa and the United Kingdom scored the lowest in terms of mental well-being. South Africans were estimated to be facing the highest levels of financial distress due to COVID-19, with the impact experienced mainly by younger people (Newson et al., 2021).
Vulnerable groups, such as persons in psychiatric hospitals or social care homes, people with disabilities, and women experiencing domestic violence or abuse, have been at even greater risk of psychological distress, because pre-existing failures in human rights protection have worsened. Persons living with mental health conditions (as well as other health conditions) were afraid or unable, for example, due to lack of transport, to receive ongoing treatment. Further fuelling the risk of widespread relapse and the need for inpatient care, between April and June 2020, medications for mental health conditions represented 3% of the stock-out reports received by the Stop Stockouts Project. By August, this figure increased to nearly 30% (Lopez Gonzalez, 2020).
The pandemic has also had significant effects on health care workers, who were already at high risk of burnout and psychological distress prior to the COVID-19 pandemic (Liebenberg et al., 2018; Roomaney et al., 2017). Witnessing large
numbers of COVID-19-related deaths has likely added to already high levels of trauma and burnout among health workers (Johnson et al., 2020), resulting in the development of trauma and stress-related mental disorders. The pandemic has brought into focus the need for attention to employee well-being more broadly.
The NDoH has been cognisant of the mental health impacts of COVID-19 and has introduced important interventions and guidelines. For example, a toolkit was developed and distributed aimed at helping people cope with emotional distress and to enhance well-being during COVID-19. The toolkit focussed on topics such as managing stress, identifying mental health symptoms, advising people on the need to keep in touch with others and continue with psychiatric medication, and assisting children during COVID-19. Guidelines were also developed on how to respond to COVID-19 in mental health facilities. Fortunately, and unlike several other countries, these facilities were not scaled down to make way for the hospital treatment of COVID-19 service users. However, the initiatives introduced fell short of using the opportunity to implement the recommendations of the WHO to invest in mental health services.
The United Nations has indicated that humanitarian crises such as natural disasters and conflict situations are opportunities to develop sustainable mental health services (Guterres, 2020). The COVID-19 pandemic has also been such an opportunity. There has been a clear need for government to step up services and assist people with mental health conditions or those in psychological distress. Such an initiative would have filled the gap between the existing need and actual services. If mental health was truly perceived as integral to health, then funding would have been found for these services, particular at the community and primary care level. All age groups, all disorders, and all levels of the health system require strengthening, which is what the investment case aims to do.
The COVID-19 pandemic has yielded the benefit of expanding the use of telemedicine. The ethical rules of the Health Professions Council of South Africa (HPCSA) have changed to allow the use of remote methods of providing mental health care. This approach can provide specialist mental health support to rural districts where it is not possible to attract suitably trained professionals. However, such services should include a large component of training and supervision of less qualified providers, as well as a consultation service for people with complicated conditions. Budgeting for information technology, including budgeting for data costs, is integral to making this approach a workable solution to providing access to specialist care. Simple infrastructure constraints (i.e. working telephones) in government facilities and a lack of digital infrastructure development have resulted in rural communities benefitting the least from such innovations (Wooyoung Kim, 2020). Some shifts such as the drafting of the Gauteng Province Mental Health Strategy and Action Plan 2019 – 2023 (Robertson et al., 2021) and the responses to COVID-19 outlined above have resulted from the LE and COVID-19 crises and from the opportunities for change presented by them. However, neither crisis has thus far sparked fundamental and long-lasting reform in the mental health system.
In the democratic era, South Africa has advanced considerably in policy and legislation aimed at transforming the mental health system and improving access, equity and quality of mental health services. Before 1994 under the Mental Health Act of 1973, mental health services were largely custodial, followed a medical and paternalistic approach, were vertically organised, and were largely not aligned with human rights principles. The thread of the improvements can be traced back from the White Paper on the Transformation of the Health System in South Africa which was adopted in 1997 to the promulgation of the Mental Health Care Act, Act No 17 of 2002 in 2004 and subsequently to the adoption of the National Mental Health Policy Framework and Strategic Plan 2013–2020.
The National Mental Health Policy Framework and Strategic Plan (2013–2020) (NDoH, 2020) and the Framework and Strategy for Disability and Rehabilitation Services in South Africa (NDoH, 2016) promote a comprehensive approach to mental health. This comprehensive approach should include the promotion of mental health, the prevention of mental health conditions and disability, early identification of disorders, and interventions with a disability-inclusive recovery-oriented approach. These services are to be implemented in a community-based framework, with task-sharing as a strategy for addressing the scarcity and maldistribution of resources.
The National Mental Health Policy Framework and Strategic Plan 2013–2020 recommends the establishment of District Mental Health Specialist teams. These teams are intended to plan services in each district in a way that makes use of local resources and provides access to care through the primary health care (PHC) system. The South African Mental Health legislation is regarded as one of the most progressive internationally.
However, weaknesses are experienced at implementation level (SAHRC, 2017). The clauses of the mental health legislation dealing with the promotion of community care, and the mental health policy framework that similarly emphasises community care, have hardly been implemented within provinces, which is where service delivery takes place. Both the mental health legislation and policy are now in need of updating due to developments such as the adoption of the Convention on the Rights of Persons with disabilities. It is unfortunate that the guidance provided in these documents, that should have resulted in a community-based approach to mental health, have largely been ig nored.
The Mental Health Care Act of 2002 and Mental Health Policy Framework (2013–2020) prescribe how the mental health system should be organised, in keeping with the WHO optimal mix of services model. Currently, mental health services are provided through PHC, community-based mental health services, mental health services in general hospitals, specialised psychiatric hospitals, and care and rehabilitation centres in the public, private and not-for-profit organisations. Mental health services are also provided in a range of other sectors, including the South African Police Services, the South African Military Health Services, Correctional Health Services, Employee Health and Wellness Programmes in workplaces, and in Basic Education and Higher Education.
However, in the current model, resources remain largely concentrated in inpatient care and in psychiatric hospitals, with relatively under-developed primary care and community-based services (Docrat, Besada, et al., 2019). There is also an inequitable distribution of mental health services, with most specialised services being unevenly distributed across provinces and concentrated in urban areas, and with little or no access to specialised care in peri-urban and rural areas.
Figure 10.1 displays the organisation of publicly funded mental health services in South Africa. Figure 10.2 displays the organisation of privately funded mental health system, and Figure 10.3 shows the WHO optimal mix of services model.

All PHC facilities in South Africa are mandated to provide basic mental health services, including screening, detection, treatment and/or referral for mental disorders, and dispensing and management of psychotropic medication for those on long-term medication. School health nurses are expected to conduct screening for mental health as part of the school health services. Again, implementation appears to be uneven given the shortage of nurses and is difficult to assess due to lack of data. Unfortunately, existing District Health Information System (DHIS) indicators for monitoring service utilisation of mental health care in the country are not disaggregated at the patient level. Only the total number of outpatient visits and inpatient admissions are enumerated for a given time period. For example, 75% of overall outpatient visits for mental health clients in 2016/17 took place at the PHC level. However, in the absence of data that reflect the number of visits per client for mental, neurological and substance use (MNS) disorders as well as patient-level outcomes, coverage cannot be determined (Docrat, Besada, et al., 2019).
The PHC re-engineering project of the NDoH includes the integration of mental health care into chronic disease management. This inclusion has been a major step forward in terms of making mental health care accessible to people with common mental disorders as well as those with severe mental illness. However, primary care providers need the support of specialist mental health professionals to be able to deliver an acceptable level and quality of service. The package also does not address the acute need for appropriate services for children and adolescents.
Specialised community mental health services are key to ensuring that specialist support is funded by and provided by the DHS. The establishment of District Mental Health Specialist Teams (who plan and organise services and provide a
specialist consultation/intervention service and a supportive/mentoring/teaching role for generalist primary care providers) is included in the policy document and strategic plan. Only 11 teams have been appointed in four of the nine provinces. Budgetary constraints have been cited for this state of affairs. If these services could be established as envisaged in the policy document and strategic plan, it is likely that at least some inpatient admissions could be prevented, in particular, readmissions (which are a proxy for relapse and are unacceptably high in South Africa) (Dreyer & Viljoen, 2019).
The latest available data indicate that there are 355 community-based mental health services that are licensed in terms of Regulation 43 of the Mental Health Care Act, 2002 Regulations. Of these, 261 are residential and 94 are day care facilities. These are largely run by non-governmental organisations with subsidies from the provincial departments of health and social development. Little has been published on their capacity, costs per patient, and subsidies received from government.
Forty general hospitals in South Africa have a psychiatric unit attached, with a total of 1 665 beds. The units attached to district and regional hospitals are largely run by medical officers with support provided by psychiatrists from specialised psychiatric hospitals. Units attached to tertiary and central hospitals have psychiatrists and other members of the multidisciplinary team providing mental health services. These hospitals are mandated to provide services by mental health care practitioners such as psychologists, social workers, psychiatric nurses and occupational therapists. All other general hospitals that are without dedicated units attached are also mandated to provide outpatient and inpatient mental health services for less complex mental health problems and emergency cases. However, the implementation of these mandates is uneven across provinces. The latest information submitted by provinces in terms of the Regulation 12 of the Mental Health Care Act 2002 General Regulations as amended indicate that there are 188 general hospitals designated to conduct 72-hour assessment of involuntary mental health care users. A national study released in 2019 showed that most of these facilities do not meet the required specifications outlined by the Mental Health Care Act (2002). For example, 62% of designated district hospitals sampled across the country indicated that adult mental health inpatients are kept in general wards with other service users. There is a dearth of facilities for adolescents requiring inpatient care and they are usually admitted to general adult medical wards. Similar to medicines for physical health, lack of access to psychotropic medications has also been reported and rural provinces often bear the brunt of stock-outs and a limited range of available medications (Sunkel & Viljoen, 2017).
There are 25 specialised psychiatric hospitals and care and rehabilitation centres in South Africa with a total of 10 732 beds. These hospitals are unevenly distributed among provinces with one province, Mpumalanga, having no specialised psychiatric hospital and KwaZulu-Natal and the Western Cape having as many as five. The role of these facilities includes:
• Provision of inpatient and limited outpatient care
• Provision of sub-specialist services
• Provision of ongoing routine training and supervision of secondary and primary health care services.
The South African Police Service and the South African Military Health Service subsidise mental health services for their members through membership of medical insurance. Most universities provide some form of mental health services to students through their student counselling programmes. However, services are inadequately provided to those in other higher education institutions such as technical and vocational training institutions, which approximately half of all post-school students attend. These health services are currently being transformed to provide comprehensive health services under Higher Health, a non-government organisation working closely with the Department of Higher Education and Training.
Data from the NDoH indicate that there are 41 private hospitals licensed to provide inpatient mental health services in terms of Regulation 42 of the Mental Health Care Act, 2002 General Regulations, with a total of 755 beds. Most psychiatrists and inpatient beds are concentrated in urban areas at the expense of rural regions. In the private sector, of 270 conditions that form the prescribed minimum benefits (PMBs), only two are explicitly psychiatric conditions. These are major affective disorders, including unipolar and bipolar depression, and schizophrenia. The PMBs include a range of other conditions including epilepsy, sexual abuse/rape (counselling), HIV counselling and testing, acute stress disorder, and attempted suicide. Many of these conditions are treated in hospital. Most mental health admissions are due to mood disorders, even though it is possible to treat these patients out of hospital. Funding by private health insurance (i.e. medical aids) for schizophrenia is limited to inpatient treatment only, and therefore individuals and families incur significant out-of-pocket expenses in order to receive appropriate ambulatory care. This arrangement encourages costly, hospital-centric care and most often members incur large co-payments for out-of-pocket medication. An unpublished South African Society of Psychiatrists (SASOP) study has called attention to the uneven distribution of psychiatrists and the need for the involvement of professionals such as nurses, occupational therapists, social workers and others in delivering mental health services (SASOP, 2020).
According to data obtained from Discovery Health which dominates the medical aid market, based on the number of claiming members in 2019 and 2020, depression claims were among their top 10 disease spends (Quantium, 2021). This figure
represents a prevalence of 8.5% and contributes 52% of Discovery’s overall psychosocial spend in 2020. Pharmaceutical claims for mental health increased by 3.5% in 2020, with claims for antidepressants in particular exceeding 6.5% of claims in 2020. Of the 29 000 Discovery Health members who were admitted for inpatient care as at December 2020, those without specified comorbidities stayed in hospital for an average of 6.6 days whilst those with depression spent an average of 9.3 days as an inpatient (Quantium, 2021).
During the trajectory of the COVID-19 pandemic, critical mental health services were suspended in tandem with a higher demand than ever for these very services across all segments of the South African population (Docrat, Besada, et al., 2019).
The lifespan of the Mental Health Policy Framework and Strategic Plan (NMHPF) 2013–2020 (the Policy) ended in 2020. It is apparent that most aspects of the Policy were either poorly implemented or not implemented at all in some provinces due to a lack of dedicated resources and technical capacity to develop costed implementation plans (Docrat, Lund, et al., 2019). This state of affairs has been heightened by weak information systems to support service planning. However, the content of the Policy remains relevant, and its proper implementation and resourcing will improve the quality of and access to mental health services. The NDoH is undertaking an update of this policy, taking into account recent developments such as the COVID-19 pandemic and the need for specific targets to justify the allocation of resources.
The South African mental health system is organised in a manner that facilitates integration of mental health into the general health services environment as prescribed by the Mental Health Care Act of 2002. It is necessary that the barriers that have impeded the implementation of the NMHPF are identified as part of the development of the post-2020 follow-up policy to the NMHPF, the phased implementation of the NHI scheme, and the post-pandemic response. We are at a critical juncture in which to seize the opportunity to leverage existing government efforts to integrate mental health in the post-pandemic response whilst concurrently solidifying its comprehensive inclusion in the South African NHI agenda. Part of the challenge is service organisation that ensures maximum reach to the widest range of the population.
An important barrier to improving the quality of mental health services in under-served areas in South Africa is the lack of measurable indicators. Indicators which would be helpful to monitor services include the following:
• Number of district mental health specialist teams established in each province
• Indicators of evidence-based mental health promotion and prevention activities in each district
• Service utilisation of inpatient and outpatient mental health care services disaggregated by MNS disorder
• Number of people attending primary care clinics identified with an MNS disorder per district
• Post-hospitalisation PHC utilisation
• Monitoring of stock-outs of antidepressant, antipsychotic and anti-epileptic drugs.
Human resources are a critical instrument for the delivery of mental health care, and therefore are a crucial consideration in planning mental health services in South Africa. Opportunities for collaboration among health care workers should be actively sought, with a view to expanding opportunities for service provision. Funding for positions for counsellors, including lay counsellors, along with training, infrastructure, and ongoing supervision are of considerable importance if services are to be made available to all who require them.
Transformation to redress historical injustices in the helping professions is a challenge facing South African society following decades of apartheid education, when Black students and those with disabilities had limited training opportunities. Transforming the mental health professions is rooted in the transformation of training at institutions of higher education. Universities have made strenuous efforts to recruit, train and graduate Black students (Meela et al., 2021). However, enrolment of Black students in graduate training in psychology, psychiatry and other mental health professions is uneven. The cadre of mental health professionals still does not reflect that of the South African population. Further, decolonised pedagogical transformation reflecting African values, cultures and literacy need to be incorporated into our largely Westernised biomedical mental health curricula.
There is an inequitable distribution of specialist mental health professionals and facilities across the country. Most specialists in all mental health professions work in urban and private settings. To illustrate this, the national ratio of public sector psychiatrists to the population was 0.31 per 100 000 (ranging from 0.08 in Mpumalanga to 0.89 in the Western Cape) (Docrat, Besada, et al., 2019). It is estimated that at least 1.9 psychiatrists per 100 000 population will be required in sub-Saharan Africa by 2050 (Charlson et al., 2014). To achieve this number in rural areas and for people who are not members of a medical aid scheme, a redistribution of personnel will be essential.
The South African Society of Psychiatrists reported that in October 2020, 785 psychiatrists were registered with the HPCSA (SASOP, 2020). However, not all of these are active practitioners. Over 84% of psychiatrists are based in three provinces: Gauteng (302), Western Cape (251) and KwaZulu-Natal (209) and 73% of psychiatrists work in the private sector (Miric & Thom, 2021). While the inequitable distribution of psychiatrists is a key consideration, by drawing on psychiatrists in the public and private sectors, this combined workforce would result in an estimated ratio of psychiatrists to population of 1.3 psychiatrists per 100 000 – a significant step closer to the 2050 target. Similar shortages and disparities exist for other specialist mental health professionals including psychologists, registered counsellors and mental health nurses. It is vital that they are prioritised alongside psychiatrists to build multidisciplinary teams. There is also inefficient utilisation of human resources. Most specialist mental health professionals in the public sector work in inpatient units, resulting in insufficient community-based specialist mental health professionals.
Task-sharing, also referred to as task-shifting, refers to the delivery of mental health services by non-specialist health care providers, who are trained and supervised by a mental health specialist. We prefer the term ‘task-sharing’, as it implies a collaborative approach between specialists and non-specialists and is more than just shifting tasks. Task-sharing provides an opportunity for psychologists and counsellors to collaborate in ways that may expand the range and scope of mental health services. As a strategy, task-sharing has been widely endorsed, including by the WHO’s flagship mhGAP programme, as a means of narrowing the treatment gap for mental health conditions (WHO, 2010).
The rationale for task-sharing is the need for an integrated care approach, in addition to limited numbers of highly trained mental health specialists to provide care to all those in need at a population level. Task-sharing represents an opportunity to use available resources efficiently and increase the coverage of mental health care. Typical settings for task-sharing include primary care clinics and community settings, where non-specialist health care staff should be available and can provide care that is accessible and close to the places where most people live and work.
The approach of task-sharing has been endorsed in the National Mental Health Policy and Strategic Plan (2013–2020) (Department of Health, 2013) which strongly advocates for the training of non-specialist primary care and community health workers in basic mental health care. Unfortunately, during the course of the policy’s implementation period, there has been little evidence of systematic scaling up of task-sharing approaches in South Africa.
The main arena in which task-sharing has been implemented and evaluated during the 2015–2020 period has been in research through initiatives such as the Programme for Improving Mental Healthcare (PRIME) (Lund et al., 2015; Petersen et al., 2016), the Mental Health Integration (MhINT) programme (Reiss-Brennan, 2014), Project MIND (Myers et al., 2018), the Africa Focus on Intervention Research for Mental Health (AFFIRM) (Lund et al., 2015) and the Health Systems Strengthening in Sub-Saharan Africa (ASSET) study (Boisits et al., 2021), described in more detail below.
These studies have identified the following challenges in implementing tasksharing. First, training needs to be carefully tailored to the skills and competencies of the non-specialist providers and should be scheduled at a time that fits in with providers’ already busy clinical work. Second, it is vital that systems of ongoing supervision and support for non-specialists are established following training. Staff require ongoing supervision and support as they are likely to face service users with challenging issues. Without this supervision and support, knowledge and skills are frequently forgotten and the quality of service deteriorates. In addition, with rapid turnover of staff in primary care settings, training of new staff is often required. Third, there are several implementation challenges. As existing staff are frequently very busy with their current workload, they may not be motivated to take on additional mental
health tasks, and new referral pathways frequently need to be established to manage complex patients and provide the right level of care. Fourthly, and finally, there are several regulatory challenges associated with task-sharing. For example, scope of practice guidelines may need to be modified by the Health Professions Council of South Africa, the South African Nursing Council, and the South African Pharmacy Council, both to allow specialists to provide supervision, and to allow non-specialists to take on certain tasks, such as psychological counselling and prescription of psychotropic medication.
Nonetheless, some important breakthroughs have been demonstrated in task-sharing approaches, which have been shown to be effective in improving care and clinical outcomes. For example, in the PRIME study, primary care nurses were able to achieve a significant improvement in detection of depression (from 5.8% to 16.4%) and alcohol use disorders (from 0% to 13.8%), and 55.2% of people with depression showed a clinically significant improvement, compared to 23.4% in the control group when supported by trained primary care nurses (Petersen et al., 2019). Three strategies have been key to these successes. First, training and supervision materials that are tailored to the relevant non-specialists need to be developed. Second, roles and scope of practice need to be carefully developed. Third, overall health systems strengthening strategies such as continuous quality improvement and establishing referral pathways are essential.
The Academy of Science of South Africa consensus study report (Academy of Science of South Africa, 2021) has made specific recommendations for providing core competencies that will allow for improved mental health care. These include: (1) training of community health workers in screening for mental disorders and managing chronic mental disorders; (2) integrating traditional healers into the health care system so that they may collaborate more formally with the formal health care system; (3) including mental health into the nursing curriculum so that nurses can have greater competencies in mental health service provision; (4) addressing concerns related to scopes of practice, legal issues of accountability, requisite training and the need for ongoing supervision of community health workers; (5) training existing mental health professionals in mentoring persons with less specialised skills; and (6) scaling up prevention and management of substance use disorders by combining medical and psychosocial interventions. Implementing these recommendations will play an important role in increasing task-sharing opportunities in the provision of mental health care.
Task-sharing holds enormous potential as a means of narrowing the treatment gap for mental health conditions in South Africa. However, it is a complex undertaking, requiring careful planning and consideration of the research evidence. In the context of resource constraints, good data on the efficacy and effectiveness of interventions, including task-sharing approaches, are necessary.
Several studies over the past few years have focused on delivering low-cost, high-quality evidence-based interventions in resource-constrained settings. The Programme for Improving Mental Health Care (PRIME, 2011–2019) studied the integration of mental health services into primary care settings, by developing and implementing district mental health care plans in five countries: Ethiopia, India, Nepal, South Africa and Uganda (Lund et al., 2012). The South African district site was located in the Dr Kenneth Kaunda district in the North West province. Researchers worked closely with the Department of Health at district, provincial and national levels to develop and implement a district mental health care plan focusing on integrating care for depression and alcohol use disorders into primary care for chronic health conditions (Petersen et al., 2016). Significant improvements were shown in both detection and clinical outcomes for depression and alcohol disorders (Petersen et al., 2019).
The Mental Health Integration programme (MhINT), building on the experience of PRIME, sought to develop the model further and replicate it in districts in Mpumalanga and KwaZulu-Natal (Reiss-Brennan, 2014). The work has emphasised the importance of health systems strengthening and continuous quality improvement as cornerstones of integrating mental health into general health care systems. It has focused on providing care for depression comorbid with chronic health conditions such as diabetes, hypertension, HIV and TB.
Project MIND has focused its work on urban and rural areas of the Western Cape in a large cluster randomised controlled trial, led by researchers at the Medical Research Council and the University of Cape Town, in partnership with the Western Cape Department of Health and numerous non-profit organisations (Myers et al., 2018). The study focused on comparing two models of integrating mental health into primary care for depression and alcohol use disorders comorbid with HIV and diabetes. The trial included 24 primary care clinics, eight for each model and eight for a control condition (Myers et al., 2018).
The Africa Focus on Intervention Research for Mental Health (AFFIRM, 2011–2016) study evaluated a task-sharing psychological counselling intervention for maternal depression in Khayelitsha, Cape Town (Lund et al., 2014). The study was an individual-level randomised controlled trial, which compared psychological counselling delivered by community health workers to enhanced usual care (supportive telephone calls to study participants). While the study did not show a significant improvement in the primary outcome of clinical depression, it found a significant reduction in psychological distress in the treatment arm compared to the control arm (Lund et al., 2020). The study showed the need for ongoing sustained su pervision and support for non-specialist community health workers.
It is vital that research is conducted in close collaboration with public sector services, chiefly the NDoH, as well as relevant non-profit organisations. This will allow findings to be taken up in routine practice, at scale, to benefit the many thousands of South Africans who currently have no access to care. Currently, although the NDoH has been very involved in these studies, translation into practice has not yet occurred.
Furthermore, researchers involved in these studies do not have clear communication channels with clinicians working in the private and public sectors, nor are these findings being actively taken up by universities involved in the training of psychiatrists and psychologists in the country. For example, many universities involved in the training of clinical psychologists continue to teach highly individualised long-term psychodynamic psychotherapies, which are both expensive and do not make use of the evidence from task-sharing approaches. Such approaches have the potential to meet the needs of many thousands more people living with mental health conditions. The integration of research findings into training curricula for mental health professionals is a matter that requires continuous programme renewal based on a scientist–practitioner model of professional training. To enhance success in this regard, clinical training programmes in psychology, nursing, psychiatry, social work and counselling will need to place a greater emphasis on evidence-based practice including research methodology, statistics and systematic reviews in the context of population health. This will increase the likelihood of lecturers and clinicians being research literate and thus being more amenable than at present to adapt training curricula in response to research findings.
Despite ongoing research, there remain areas that require investigation. First, there is an enormous gap in research on interventions for children and adolescents, taking low-cost models of service provision to scale. Second, health systems need to be strengthened to create the capacity for integrating mental health into existing primary care and community health systems. Third, while important strides have been made in evaluating mental health interventions, there are still large gaps in our knowledge about interventions that address the social determinants of mental health in South Africa, including poverty and gender-based violence. Rural mental health, a largely neglected area, is a further issue that requires investigation.
The 2018 Lancet Commission on Global Mental Health and Sustainable Development Goals emphasised the inclusion of mental health care in the universal health coverage (UHC) agenda (Patel et al., 2018). Both the WHO and World Bank endorsed investments in mental health as humanitarian and development priorities (Mnookin, 2016). It has been estimated that US$5–17 trillion in lost output is expected by 2030 without significant investment in the treatment of mental disorders. Promisingly, a growing body of evidence for cost-effective options to reduce the burden of mental disorders and improve outcomes for physical health problems, particularly in LMICs, is emerging. One analysis estimates that for every $1 invested in the treatment of depression and anxiety a return of $3–5 can be expected through improved productivity and instrumental benefits of improved mental health over the 15 years of the Sustainable Development Goals (Chisholm et al., 2016).
An explicit pledge to transform mental health services was outlined in the South African National Mental Health Policy Framework and Strategic Plan 2013–2020 (MHPF) (Department of Health, 2013). However, barriers to implementation of the MHPF include weak health information systems to understand the local burden of illness, uneven patterns of service access, inadequate human and financial resources for mental health, as well as a lack of technical capacity to generate costed and budgeted strategic plans for mental health services in all provinces (Docrat & Lund, 2018; SAHRC, 2017). Financial incentives to increase efficiency or resource allocation for mental health services in provinces are minimal (Bateman, 2015). Hence, the struggle to actively fund existing services continues.
In pursuit of UHC, financial protection and health system efficiency, the South African government has committed to the phased implementation of an NHI system (South African National Department of Health, 2017). However, evidence from the NHI pilot districts has raised concerns that mental health priorities have not been explicitly addressed and reflected in the policies and activities supporting its overall implementation. This omission is likely to make future prospects for the South African mental health system uncertain (Schneider et al., 2016).
Until recently, there has been inadequate information about existing resources for mental health care, taking into account the variability across districts and provinces, the degree of policy implementation, and availability and existing uptake of services for mental health at all levels of the health system (Docrat, Besada, et al., 2019). The NDoH has acknowledged these concerns and in 2017 supported a study to evaluate the full costs of mental health services and programmes. Findings revealed that South Africa’s public mental health expenditure fell in the lower recommended bound of 5% of the total public health budget, that the treatment gap was approximately 92%, and that under 1% of the uninsured population were receiving inpatient care (Docrat & Lund, 2018). One reason for the treatment gap was that most expenditure occurred at the inpatient and specialised hospital levels. In 2016/17, 86% of mental health care expenditure was on inpatient care, 50% of which was directed at the psychiatric hospital level. Furthermore, readmission rates of nearly 25% consumed 18% of overall mental health expenditure, indicating a lack of service provision following discharge from hospitals (Docrat & Lund, 2018). Understanding the current inequities in resources, access to services, and inefficiencies in the use of resources provides the foundational tools to promote the redistribution of budgets towards more cost-effective responses to mental health needs.
It has been suggested that UHC should involve the explicit inclusion of mental health services within reimbursement and mandatory insurance schemes as a standard, not as a complementary option (Patel et al., 2018). The NHI is an opportunity rather than a threat to the improvement of mental health services, but its success depends on how the system is managed. If mental health professionals are brought on board collaboratively and adequately remunerated for their work, then NHI could be an opportunity to improve services. The South African government is currently moving towards developing and defining the mechanisms by which the NHI fund will operate. A significant opportunity exists to generate the economic evidence to support decision-making regarding the mental health service benefits for all South Africans, as well as the complementary system reforms and capacity-building efforts that will be needed to realise successful implementation and scale-up. Beyond raising the global profile of mental well-being, with all sectors of society recognising its importance, the COVID-19 response has brought best practices that may be leveraged to improve mental health outcomes for all South Africans under the future NHI. As evidenced by collaborative efforts to respond to the COVID-19 pandemic, a culture of data-sharing (integrating utilisation and clinical records) and standardised treatment ap proaches grounded in public (mental) health care paradigms and broader reciprocity and alignment across the public and private sectors serves as an opportunity to automate systems for integrating utilisation and clinical records delivered through all facilities in the country, towards NHI-led purchasing mechanisms that incentivise quality of care and integration in broader NCD service packages.
In 2019, an Investment Case for Mental Health was commissioned by the NDoH which indicated its intentions to strengthen financing for mental health services (Besada, Docrat, & Lund, 2021). Such an exercise aimed to provide a clear quantification of and integrated case for investments to transform mental health services in line with international and local evidence by estimating the expected return-on-investment (ROI) over a 15-year period from scaling-up interventions targeting anxiety, depression (including perinatal depression), psychosis, bipolar disorder, epilepsy, idiopathic developmental intellectual disability, behavioural disorders, dementia and alcohol and substance-use (opioid and non-opioid) disorders. Further, in acknowledgement of the need for preventative efforts, the ROI associated with (1) early interventions for those exhibiting risky alcohol and substance-use behaviours and (2) the development and roll-out of social-emotional learning programmes delivered in schools to learners (aged 12–17 years) represented a key component of the initiative. Building on global guidelines, and driven by insights from the NDoH, the approach to this work innovatively introduced methodology that reflects the importance of engagement with multisectoral, national and sub-national structures, clinicians, academic experts, and service-user organisations in addition to the National Treasury throughout the modelling process. Decisions of clinical, policy and systems interventions that were prioritised and modelled reflected the diverse perspectives and priorities of a variety of stakeholders, beyond only those responsible for the existing and future allocation and prioritisation of funds and resources.
Return on investment can change significantly due to systems constraints. The approach goes a step beyond global guidelines for examining the costs and benefits of scaling up packages of interventions for priority MNS disorders, by quantifying the infrastructural (capital), human resource and programmatic requirements that must be complementary for the achievement of mental health service scale-up. This means that
services delivered under the future NHI will adhere to requirements for quality and humane mental health care. The key financing streams, roles and responsibilities of sectors beyond health will thus be leveraged.
Released in October 2021, the South African Mental Health Investment Case provides practical methodologies for LMICs, particularly those transitioning to mandatory health financing mechanisms to improve the likelihood that cases for investment in mental health translate into committed bridge and long-term, sustainable mental health care financing. The Investment Case provides a synthesis of the increasing burden imposed by MNS disorders and quantifies the significant cost of inaction on the economy and population well-being. It provides an explicit treatment package to be provided at each level of care to address population needs, thereby serving as a tool for which the NHI benefits package can draw on (Besada, Docrat, & Lund, 2021). Ultimately, beyond the positive returns on investment demonstrated by the Investment Case, the initiative has unequivocally shown that the cost of inaction to the South African economy far outweighs the cost of investing in the mental health of our country. Even when accounting for existing rates of unemployment and labour force participation, lost workforce productivity due to unaddressed mental health well-being translates into an annual economic loss of R161 billion annually (approximately 4% of the country’s gross domestic product per year).
In contrast, the projected needed spend for a paced, rational approach to service scale-up and progressive decentralisation across all sectors is estimated in the region of R26 billion per year, though this average does not account for the gradual increase in coverage and associated investments. For example, in the first year of scale-up, the costs associated with direct service provision, training, supervision, governance and behaviour change campaigns, falling within the mandate of the NDoH, would translate to an amount of R6.74 billion; in comparison, currently estimated expenditure on mental health services amounts to R8.12 billion. For the modelled community-based service platform, the Department of Social Development is mandated to provide subsidies for individuals living with mild to moderate intellectual disability, in addition to the provision of substance-use rehabilitation. Together, these investments would assume a marginal 0.02% of the Department of Social Development’s current resource envelope. It is expected that the Department of Basic Education will finance the social and emotional learning programmes modelled in the Investment Case, translating to only 1% of its allocated budget of R28.59 billion in the 2022/23 period.
Finally, in light of the mandate of the Department of Human Settlements to provide housing needs for vulnerable populations, capital costs estimated for the establishment of community-based residential units would amount to just under 3% of its allocated budget.
Many of these aggregates include upfront investments related to infrastructure development for rehabilitation, recovery, and prevention of disability through a community-based residential and day-care service platform and for revitalising dilapidated hospital infrastructure for mental health. These represent a long-term investment and are not anticipated to contribute to recurrent costs.
Due to research and return on investment calculations, a great deal is known about what needs to be done to strengthen mental health services in South Africa, and much of this has in fact been included in the current legislation and policy. As a consequence of Life Esidimeni and the COVID-19 pandemic there have also been several opportunities to introduce changes and reforms. However, implementation, especially by the provinces has been slow. Even without additional resources, or with some transitional funding, much can be accomplished with sufficient buy-in and prioritisation of mental health care. While greater investment is required, in the current economic climate, few resources will go into mental health unless it is part of the current crisis response or part of ‘building back better’. The last five years have shown us a great deal about what can be done, but the next five will have to show more in terms of real changes in systems and services. Moves towards greater emphasis on community care will be essential. Moreover, though not dealt with in any detail in this chapter, reducing the social and economic determinants of mental health, giving greater emphasis to prevention and promotion programmes, and working across sectors will need to be prioritised if population mental health is to truly change.
Academy of Science of South Africa. (2021). Provider core competencies for improved Mental health care of the nation. https://doi.org/http://dx.doi.org/10.17159/ assaf.2019/0067
Bateman C. Mental health under-budgeting undermining SA’s economy. SAMJ: South African Medical Journal. 2015;105(1): 7–8.
Besada D, Docrat S, Lund C. Mental Health Investment Case for South Africa. Final Report of the Mental Health Investment Case Task Team. 2021.
Boisits S, Abrahams Z, Schneider M, Honikman S, Kaminer D, Lund C. Developing a task-sharing psychological intervention to treat mild to moderate symptoms of perinatal depression and anxiety in South Africa: a mixed-method formative study. International Journal of Mental Health Systems. 2021;15(1): 1–14.
Charlson FJ, Diminic S, Lund C, Degenhardt L, Whiteford HA. Mental and substance use disorders in sub-Saharan Africa: predictions of epidemiological changes and mental health workforce requirements for the next 40 years. PloS One. 2014;9(10): e110208.
Chisholm D, Sweeny K, Sheehan P, Rasmussen B, Smit F, Cuijpers P, Saxena S. Scaling-up treatment of depression and anxiety: a global return on investment analysis. The Lancet Psychiatry. 2016;3(5): 415–424.
Clark B. Gender-based Violence and COVID-19 in South Africa The Clash of Pandemics. 2020. file:///C:/Users/skagee/OneDrive - Stellenbosch University/ Desktop/LN_ROL_CAFE_White_Paper_20201202.pdf
Department of Health. (2013). National Mental Health Policy Framework and Strategic Plan.
Department of Health. (2016). Framework and Strategy for Disability and Rehabilitation Services in South Africa.
Department of Health. (2020). NATIONAL MENTAL HEALTH POLICY FRAMEWORK AND STRATEGIC PLAN (2013-2020). file:///C:/Users/ skagee/OneDrive - Stellenbosch University/aaaAshrafs Manuscripts II/2017/ a-Manuscripts in preparation/SA Health Reforms Book chapter/National-MentalHealth-Policy-Framework-and-Strategic-Plan-2013-2020 (1).pdf
Docrat S, Lund C. Evaluation of the Health System Costs of Mental Health Services and Programmes in South Africa 2016/17 Financial Year. 2018.
Docrat S, Besada D, Cleary S, Daviaud E, Lund C. Mental health system costs, resources and constraints in South Africa: a national survey. Health Policy and Planning. 2019;34(9): 706–719.
Docrat S, Lund C, Chisholm D. Sustainable financing options for mental health care in South Africa: Findings from a situation analysis and key informant interviews. International Journal of Mental Health Systems. 2019;13(1): 1–11. https:// doi.org/10.1186/s13033-019-0260-4
Dreyer R, Viljoen AJ. Evaluation of factors and patterns influencing the 30-day readmission rate at a tertiary-level hospital in a resourceconstrained setting in Cape Town, South Africa. South African Medical Journal. 2019;109(3): 164–168.
Durojaye E, Agaba DK. Contribution of the Health Ombud to accountability: The life Esidimeni tragedy in South Africa. Health and Human Rights. 2018;20(2): 161.
Guterres A. Launch of the policy brief on COVID-19 and mental health. 2020. https:// www.un.org/en/coronavirus/mental-health-services-are-essential-part-allgovernment-responses-covid-19
Johnson SU, Ebrahimi OV, Hoffart A. PTSD symptoms among health workers and public service providers during the COVID-19 outbreak. PloS One. 2020;15(10): e0241032.
Kola L, Kohrt BA, Hanlon C, Naslund JA, Sikander S, Balaji M, Benjet C, Cheung EYL, Eaton J, Gonsalves P, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: Reimagining global mental health. The Lancet Psychiatry. 2021.
Liebenberg AR, Coetzee JFJ, Conradie HH, Coetzee JF. Burnout among rural hospital doctors in the Western Cape: Comparison with previous South African studies. African Journal of Primary Health Care & Family Medicine. 2018;10(1): 1–7.
Lopez Gonzalez L. Mental health: are medicine shortages fuelling a shadow epidemic? Mental Health Matters. 2020;7(4): 26–29.
Lund C, Alem A, Schneider M, Hanlon C, Ahrens J, Bandawe C, Bass J, Bhana A, Burns J, Chibanda D, Cowan F, Davies T, Dewey M, Fekadu A, Freeman M, Honikman S, Joska J, Kagee A, Mayston R, … Susser E. Generating evidence to narrow the treatment gap for mental disorders in sub-Saharan Africa: Rationale, overview and methods of AFFIRM. Epidemiology and Psychiatric Sciences. 2015;24(3). https://doi.org/10.1017/S2045796015000281
Lund C, Schneider M, Davies T, Nyatsanza M, Honikman S, Bhana A, Bass J, Bolton P, Dewey M, Joska J, Kagee A, Myer L, Petersen I, Prince M, Stein DJ, Thornicroft G, Tomlinson M, Alem A, Susser E. Task sharing of a psychological intervention for maternal depression in Khayelitsha, South Africa: study protocol for a randomized controlled trial. Trials. 2014;15. https://doi.org/10.1186/17456215-15-457
Lund C, Schneider M, Garman EC, Davies T, Munodawafa M, Honikman S, Bhana A, Bass J, Bolton P, Dewey M, et al. Task-sharing of psychological treatment for antenatal depression in Khayelitsha, South Africa: Effects on antenatal and postnatal outcomes in an individual randomised controlled trial. Behaviour Research and Therapy. 2020;130: 103466.
Lund C, Tomlinson M, De Silva M, Fekadu A, Shidhaye R, Jordans M, Petersen I, Bhana A, Kigozi F, Prince M, et al. PRIME: a programme to reduce the treatment gap for mental disorders in five low-and middle-income countries. PLoS Med. 2012;9(12): e1001359.
Meela MM, Libhaber E, Kramer B. Transformation of a health sciences postgraduate population (2008-2017) at a higher education institution in South Africa: has this occurred? South African Journal of Higher Education. 2021;35(1): 209–230.
Miric A, Thom R. Unpublished report prepared for the South African Society of Psychiatrists. 2020.
Mnookin S. Out of the shadows: Making mental health a global developmental priority. 2016. http://documents1.worldbank.org/curated/ en/270131468187759113/pdf/105052-WP-PUBLIC-wb-background-paper. pdf
Myers B, Lund C, Lombard C, Joska J, Levitt N, Butler C, Cleary S, Naledi T, Milligan P, Stein DJ, et al. Comparing dedicated and designated models of integrating mental health into chronic disease care: study protocol for a cluster randomized controlled trial. Trials. 2018;19(1): 1–13.
Newson J, Pastukh V, Sukhoi O, Taylor JTT. The Mental State Of The World Report. 2021.
Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, Chisholm D, Collins PY, Cooper JL, Eaton J, Herrman H, Herzallah MM, Huang Y, Jordans MJD, Kleinman A, Medina-Mora ME, Morgan E, Niaz U, Omigbodun O, … UnÜtzer Jü. The Lancet Commission on global mental health and sustainable development. The Lancet. 2018;392(10157): 1553–1598. https://doi. org/10.1016/S0140-6736(18)31612-X
Petersen I, Bhana A, Fairall LR, Selohilwe O, Kathree T, Baron EC, Rathod SD, Lund C. Evaluation of a collaborative care model for integrated primary care of common mental disorders comorbid with chronic conditions in South Africa. BMC Psychiatry. 2019;19(1): 107.
Petersen I, Fairall L, Bhana A, Kathree T, Selohilwe O, Brooke-Sumner C, Faris G, Breuer E, Sibanyoni N, Lund C. et al. Integrating mental health into chronic care in South Africa: the development of a district mental healthcare plan. The British Journal of Psychiatry. 2016;208(s56): s29–s39.
Petersen I, Lund C, Bhana A, Flisher AJ, Health M, Consortium PRP. A task shifting approach to primary mental health care for adults in South Africa: human resource requirements and costs for rural settings. Health Policy and Planning. 2011;27(1): 42–51.
Pijoos I. Help! Lockdown sees calls to SA Anxiety and Depression Group double. Times Live. 2021. https://www.timeslive.co.za/news/south-africa/2021-03-24-helplockdown-sees-calls-to-sa-anxiety-and-depression-group-double/ Quantium. (2021). Insights from the Discovery Health data.
Reiss-Brennan B. Mental Health Integration Programme. Journal of Primary Care & Community Health. 2014;5(1): 55–60. https://doi. org/10.1177/2150131913508983
Robertson LJ, Moosa MYH, Jeenah FY. Strengthening of district mental health services in Gauteng Province, South Africa. South African Medical Journal 2021;111(6): 538–543.
Roomaney R, Steenkamp J, Kagee A. Predictors of burnout among HIV nurses in the Western Cape. Curationis. 2017;40(1): 1–9. https://doi.org/10.4102/curationis. v40i1.1695
SAHRC. Report of the National Investigative hearing into the status of mental health care in South Africa. 2017.
SASOP. Equality in mental health hampered by lack of access, lack of investment. 2020. https://www.sasop.co.za/equality-in-mental-health-hampered
Schneider M, Baron E, Breuer E, Docrat S, Honikman S, Onah M, Sorsdahl K, der Westhuizen C, Lund C, Kagee A, et al. Integrating mental health into South Africa’s health system: current status and way forward. South African Health Review. 2016;2016(1): 153–163.
South African National Department of Health. (2017). Government Notices - National Health Insurance Policy. Government Gazette, 7(40955): 1–70. https://www.gov. za/sites/default/files/gcis_document/201707/40955gon627.pdf
Sunkel C, Viljoen M. Shortage of psychiatric medications in South Africa. The Lancet Psychiatry. 2017;1(4): 15–16.
Wooyoung Kim A. Is it time to rethink how we deliver mental healthcare services? Mental Health Matters. 2020;7(3): 30–32.
World Health Organization. (2010). mhGAP Intervention guide for mental, neurological and substance use disorders in non-specialized health settings: version 2.0. https://doi.org/10.1590/0047-2085000000206
World Health Organization. (2003). Organization of services for mental health. World Health Organization.
Occupational health in South Africa still has a fragmented policy, legal, administrative and service delivery framework. Occupational health services (OHS) are under-developed in many sectors of the economy coupled with the lack of trained occupational health personnel in the public sector and no uniform funding model for occupational health. The surveillance system for occupational injuries and diseases is non-existent and there is no reporting system across the Departments of Mineral Resources and Energy, Employment and Labour, and Health. Where data on occupational injuries and diseases is provided, it is mainly numerator data and thus difficult to interpret, compare and assess trends across sectors.
Migrant labour persists both within South Africa and cross-border with some progress on tracking and tracing workers with occupational lung diseases and ensuring their compensation payments. Informal sector workers face multiple barriers including the low wage subsistence economy and no access to OHS and other services. Class action compensation settlements for silicosis and tuberculosis (TB) in the gold mining sector were welcome developments notwithstanding the need for preventive interventions.
Some gains were made with OHS provision with specialist referral services in occupational medicine in the major metropolitan areas, expansion of the Occupational Health Information System (OHIS) in some Provincial Departments of Health (PDoHs), provision of One Stop Services for ex-mineworkers and limited health services to informal traders, use of the HealthWise tool (ILO / WHO) and incorporation of domestic workers into the compensation system. The COVID-19 pandemic, while galvanising partnerships across public and private sectors, highlighted the gaps in OHS provision especially in public sector health facilities, small and medium enterprises and the informal sector. The Department of Employment and Labour (DEL) and Department of Mineral Resources and Energy (DMRE) took the
Barry Kistnasamy, Spo M Kgalamono, Muzimkhulu Zungu, Mohamed Jeebhay, Rajen N Naidoo, Robyn Hayes Badenhorstlead on workplace interventions in COVID-19 and COVID-19 infection in workplaces was designated a compensable disease.
South Africa’s many academic institutions and professional societies play a significant role in capacity-building initiatives of the different disciplines within OHS. They assist with technical advice to government, employers and trade unions and serve on multiple governance structures. Of note is their participation in OHS initiatives across the continent and other international bodies.
Multilateral agencies such as the International Labour Organisation (ILO), the World Health Organization (WHO) and the International Social Security Association (ISSA) provide global governance and support to occupational health and safety activities at supra-regional and country levels.
South Africa’s occupational health and safety legislation is derived from Chapter 2, Section 24(a) of the Constitution of South Africa, Act 108 of 1996, which states that everyone has the right to an environment that is not harmful to their health or well-being. Section 27(2) places an obligation on the state to take reasonable legislative and other measures, within its available resources, to achieve the realisation of each of the rights in the Bill of Rights. South Africa as a member state of the WHO and ILO has ratified their conventions and adopted instruments in occupational health and safety. Occupational health and safety in South Africa is a tripartite arrangement, and is in line with the International Labour Organization Convention C144 – Tripartite Consultation Convention, 1976 (No. 144). Employers, employee representatives and government contribute on decisions that affect occupational safety and health policy, Acts, Regulations, and implementation. The Mine Health and Safety Act established the tripartite structures, namely the Mine Health and Safety Council and the Mine Qualification Authority, which are led by stakeholders. These institutions coordinate and direct research and training to improve health and safety performance of the mining industry. The Occupational Health and Safety Act (OHSA) established an Advisory Council for Occupational Health and Safety, which is also a tripartite institution. These institutions ensure that there are political, economic and social systems to influence policy and legislation on occupational health and safety (Myeni, 2020).
The legislation on occupational health and safety is progressive and enforceable. In addition, there are voluntary technical standards that, whilst not legally enforceable, are part of the health and safety management systems in many companies. However, the legislation governing occupational health is complex and spans general economic sectors and specifically mining, maritime, aviation, railway, transport and nuclear/ energy sectors. Notably, the fragmented legislative framework falls under different ministries and departments. The main pieces of legislation on occupational health and safety are in Table 11.1.
Occupational Health and Safety Act, Act No. 85 of 1993
Department of Employment and LabourCompensation for Occupational Injuries and Disease Act, Act No. 78 of 1973
Mine Health and Safety Act, Act No. 29 of 1996
Department of Mineral Resources and Energy
Occupational Diseases in Mines and Works Act, Act No. 78 of 1973 National Department of Health
National Energy Regulator Act, Act No. 47 of 1999
Railway Safety Regulator Act, Act No. 16 of 2002
South African Maritime Authority Act, Act No. 5 of 1998
Act of Civil Aviation Authority Act, Act No. 3 of 2009
National Nuclear Energy Regulator
Railway Safety Regulator
Provides for the protection of persons, property and the environment against nuclear damage in South Africa
Provides for safety standards and regulatory practices for the protection of persons and property
South African Maritime Authority Safety provisions for staff on board ships, appliances and equipment
South African Civil Aviation Authority Regulates civil aviation safety and security in support of the sustainable development of the aviation industry
The overall policy framework for occupational health and safety is weak given the fragmentation across the three major departments governing occupational health and safety. The National Department of Health (NDoH) covered aspects of occupational health in the White Paper on National Health Insurance (NHI) but lacks the administration and funding to support occupational health initiatives. The National Institute for Occupational Health (NIOH), an agency of the NDoH, conducts research and provides education and training and specialised laboratory and clinical services in occupational health. The Medical Bureau for Occupational Diseases and the Compensation Commissioner for Occupational Diseases have narrow mandates under the Occupational Diseases in Mines and Works Act, 1973 and cover medical assessments and compensation for cardio-respiratory diseases in mineworkers. There are academic departments of occupational health at a few medical schools and nursing colleges while occupational hygiene and safety is also taught through a few universities and technical institutes. There is a programme on ergonomics at one university. The DMRE and DEL have components of their departments dealing with inspections of workplaces and enforcement under their respective health and safety Acts. In addition, the DEL has a component dealing with compensation for occupational injuries and diseases other than that covered by the NDoH.
The mining sector and major manufacturing sector companies have OHS standards that play a substantial role in occupational health and safety initiatives in the workplace. Of note is the multiplicity of ‘wellness’ services covering health promotion in the workplace that cover chronic diseases including HIV and AIDS. Some of the major trade union federations and larger unions have health and safety focal persons, but in general have not placed occupational health and safety high on the agenda in workplace interactions with management. The COVID-19 pandemic response resulted in some trade unions, especially those covering health workers, raising concerns on OHS and personal protective equipment (PPE) for workers. Various professional societies and associations are also active in occupational health and safety.
The prevention, promotion, curative, rehabilitative and compensation services are fragmented with no overall and uniform health system response. Injured workers are managed within the public and private health care systems depending on the nature and extent of their injury. Except for the system of assessments for cardio-respiratory diseases in mineworkers, there are few cases of occupational diseases reported annually. Owing to latency, many workers with occupational diseases present long after they exit the workplace and in many instances owing to a lack of education and training of health professionals, their diagnosis may not be linked to their work exposures. Injured workers are often cared for in public hospitals with no recovery of funds from the different compensation funds.
Demographic changes to the South African workforce during the period under review were marginal, largely defined by economic imperatives that occurred in the previous decade. The changes impacted on in 2020, because of the COVID-19 pandemic, have yet to be fully described, but immediate effects, such as unemployment, have already been recorded. At the end of the previous decade, economic growth in South Africa fell sharply. The impressive growth rate of 5% in 2007 gave way to almost 2% by 2009 (Organisation for Economic Co-operation and Development, 2010). Similarly, unemployment, hovering at a stable (but high) rate of 20% from 2002 through to 2007, increased to 25% by 2010 (Organisation of Economic Co-operation and Development, 2010). These economic indicators set the stage for the 2015–2020 period.
The ILO estimates that 2.78 million of the world’s 2.7 billion workers die annually from occupational accidents or diseases (International Labour Organisation, n.d.). It is estimated that a large proportion (>80%) of occupational fatalities and disease burden are due to occupational diseases. Furthermore, the economic burden of poor occupational health and safety practices is estimated to be 3.94% of global gross domestic product each year. Similarly, occupational injuries and diseases pose an enormous cost to the South African economy, individual workers, and their families. An earlier South African Demographic and Health Survey conducted over two decades ago suggested that 8.9% of adults reported staying away from work due to disease or injury related to work (Kielkowski, 2004).
Current official data on the spectrum of occupational injury and diseases in the South African workforce is incomplete, unreliable and for a large proportion of the workforce not available. The spectrum of occupational diseases is partially obtainable from the annual reports and the Occupational Diseases in Mines and Works Act. The Compensation Fund in the DEL, legally established through contributions of employers, currently covers 15 million workers employed by 1.08 million employers, which includes the Rand Mutual Association (covering mining, iron and steel) and Federated Mutual Association (covering construction) (Presentation, Milly Ruiters, Compensation Fund, ILO workshop, June 2021) in the formal sector, but excludes public sector workers (exempted employers). Compensation for occupational lung diseases is covered by the Medical Bureau for Occupa tional Diseases and its Compensation Commissioner administered by the NDoH.
Occupational diseases in the non-mining sector reported to the Compensation Fund by the DEL show a downward trend over the past two decades, from over 5 000/ year claims reported in 2003–4 (Adams, 2007) to less than 1 000/year over the past five years (Myeni, 2020). In the non-mining sector, TB (among health care workers), noise-induced hearing loss, diseases due to chemical agents and occupational asthma claims submitted in the 2019/20 period are shown in Table 11.3. Visibly absent from this list is post-traumatic stress disorder, dermatitis and pneumoconiosis that featured over a decade ago (Adams, 2007). Recent data from the Occupational Medicine Clinic at Groote Schuur Hospital in Cape Town indicates that occupational asthma is the most common diagnosis, followed by pneumoconiosis and work-related upper limb disorders and contact dermatitis (personal communication, S Adams, GSH, Cape Town). These trends need to be interpreted with caution in a setting of poor diagnostic capacity for occupational diseases, under-reporting of occupational diseases and overall lack of occupational health service provision in most workplaces in both the private and public sector (Jeebhay & Jacobs, 1999).
Table 11.3 Occupational diseases reported to the Compensation Fund for the non-mining sector in South Africa, 2016/17–2019/20
Occupational Diseases 2016/17 2017/18 2018/19 2019/20
Noise-induced hearing loss 145 279 249 118 Tuberculosis in health workers 141 184 257 191
Occupational diseases associated with chemical agents 64 68 35 41 Occupational asthma 24 28 27 20
COID Injuries* 104 232 252 161
Source: Myeni and Ngcobo, 2020; *probably refers to non-traumatic organ insults
Data from the mining sector (547 847 employees in 2019) indicate that occupational lung diseases comprise the largest portion of the disease burden (70–75%). The five most frequently reported occupational diseases are pulmonary TB, noise-induced hearing loss, silicosis, and coal workers’ pneumoconiosis (see Table 11.4) (DMRE, 2019/20). The relative prevalence of occupational disease among workers in the sector is highest in the gold mining industry. The common commodity sectors reporting these outcomes are gold, platinum, chrome and coal mining. Among these diseases, TB comprised 50% of the occupational disease burden. This is also reflected in autopsy findings of miners conducted for compensation purposes where the reported rate for TB was 138/1 000 (2018). For Black miners, where the rates are extremely high, the rate increased consistently from the early 1990s and peaked at 368/1 000 in 2007, but have since declined annually to 168/1 000 in 2018, before rising again to 234/1 000 in 2019 (Figure 11.1a-b). However, the recent Masoyise report of the industry’s TB incidence was at 220/100 000 for 2020, which is below that of the general population, at 260/100 000. Silicosis rates based on autopsy results have also shown an increase particularly in the gold-mining industry, which accounts for 83% of cases (2018). Silicosis rates in Black gold miners increased over the years from 39/1 000 in 1975 and peaked at 416/1 000 in 2016, thereafter declining to 368/1 000 in 2019, while the rate in White gold miners increased from 176/1 000 in 1997 to 309/1 000 in 2019 (Figure 11.1a-b). During the year 2020, the Medical Bureau for Occupational Diseases certified 7 924 claims (47%) of 16 968 claims received (Table 11.5). The two largest components of claims certified were for TB (50%) and silicosis with/without TB (42%). A steady decline of new cases has been reported in living miners with silicosis. However, there is a risk of under-diagnosis and reporting especially in former miners. A recent study has suggested that the annually reported levels of exposure to respirable crystalline silica suggest a decline, however, the actual levels were not reported over the last few years (Brouwer, 2020). The authors concluded that there was insufficient evidence of progress towards achieving the silicosis elimination target that the country had set.
Figure 11.1
Figure 11.1b
Figures 11.1a-b. Pulmonary tuberculosis in Black miners and silicosis in Black South African gold miners at autopsy (1975–2019)

Source: Mhlongo L, Wilson K, Kgokong N, et al. Pathology Division Surveillance Report 2018. NIOH Pathology Report 1/2021

No.
Pulmonary TB 3 512 3
3 603 52 604 793 43 067 787
Silicosis 1 974 2 067 870 797 40 740 551 40 964 682 Silico-TB 1 213 1,286 925 940 86 486 134 99 496 938
Asbestos-related disease 316
Coal workers pneumoconiosis 85
275 4 088 972 4 612 847
38 2 652 757 1 977 605
Obstructive Airways Disease 141 126 99 90 6 543 612 6 407 787 Cancers (mesothelioma, lung cancer) 35
31 37 2 706 000 3 175 660
Platinum salt sensitivity 0 2 4 1 243 374 36 156
Other 9 20 104 100 1 641 295 1 976 716
Non-compensable disease 7 213 9 044
Total claims received 14 498 16 968 16 968 5 881 197 707 487 201 716 178
Infectious diseases, COVID-19 and vulnerable occupational groups
Tuberculosis in health workers and occupational lung diseases in mining and associated industries continue to be a key priority for the NDoH (Adams, 2012/13; Grobler, 2016). This has been evident in the recent COVID-19 pandemic, which illustrated the vulnerability of the health workforce. Earlier in the epidemic, the WHO estimated that health workers accounted for up to 14% of all COVID-19 cases (WHO, 2020).
A total of 2.3% of COVID-19 hospitalisations at a national level were health care workers (HCWs) as of March 2022 (NIOH, 2022). An estimated 44 406 cases of COVID-19 were reported in the Western Cape (n=12 329), Gauteng (n=15 282) and KwaZulu-Natal (n=16 795) by mid-April 2021 in both the public and private sector. Most infections (86%) were in the public sector, which employs most HCWs in the country (Table 11.6). Among the HCWs, 11.8% experienced moderate to severe disease requiring hospitalisation and 0.9% had demised. Nurses and administrative workers were the most affected job category at all levels of the health care system (Rees, 2021). This could have been due to the large numbers of patients admitted to hospitals with limited facilities for case isolation, limited access to rapid and reliable diagnostic testing in the early stages of the outbreak, and the challenges around access to and best use of PPE (Read, 2021).
Eastern Cape 11 440 1 237 10.8 93 0.8 Free State 3 526 434 12.3 29 0.8
Gauteng 15 971 1 842 11.5 103 0.6
KwaZulu-Natal 10 629 1 772 16.7 158 1.5
Limpopo 4 549 514 11.3 78 1.7
Mpumalanga 3 001 463 15.4 54 1.8
North West 3 664 627 17.1 32 0.9
Northern Cape 1 273 158 12.4 17 1.3
Western Cape 4 604 499 10.8 37 0.8 National 2 923 500 17.1 30 1.0
Total 68 212 8 046 11.8 631 0.9
Source: NDoH (Personal communication, Dr Nicholas Crisp, Deputy Director-General NHI, NDoH)
The impact of COVID-19 on the overall mining community mirrored the pandemic in the rest of the country. In provinces with considerable mining activity, a high proportion of community cases and fatalities emanated from the mines. Mining-related cases were concentrated in areas that are situated close to provincial borders, implying an increased interprovincial transmission risk, possibly exacerbated by work-related transmission. Occupational categories with high dust exposures such as rock drill operators in platinum and gold mining were also reported to have the most SARS-COV-2 infections (Naidoo & Jeebhay, 2020). Data is being collected on a dynamic basis to monitor the trends in other industrial sectors through the Occupational Health S urveillance System (OHSS) for COVID-19. This data reports the mortality rate among reporting workplaces as 1.5%, while 7.5% of workers had moderate to severe disease requiring hospitalisation (NIOH, 2021).
Analysis of workers’ compensation claim data for the period ending 31 March 2021 indicated that there were 20 525 claims for work-related COVID-19 submitted to the Compensation Fund. Most claimants were women workers, with a large proportion originating in the health care sector (75%). Mining contributed 23% of claims and the building industry 2.5%. Data from the Western Cape suggested that about 20% of COVID-19 claims originated from the non-health sectors such as retail, finance and transport (Jeebhay et al., 2021).
In July 2020, the DEL issued a direction on compensation for workplace-acquired COVID-19, addressing workplace-acquired COVID-19 resulting from work-related exposures, exposure to suspected or confirmed cases of COVID-19 in the workplace, or while travelling on an official trip. South Africa is one of a few countries that has taken this step of making COVID-19 infection a compensable disease.
The patterns of occupational injuries in the country are disaggregated according to economic activity. In the non-mining sector occupational injuries have historically accounted for more than 99% of all claims submitted under the Compensation for Occupational Injuries and Diseases Act (Myeni, 2020). According to DEL reports, over a four-year period annual claims declined from 184 100 (2017/18) to 82 526 (2019/20). The largest proportion of claims originated from the more industrialised and urbanised provinces of Gauteng followed by the Western Cape. Compensation claims affecting women ranged between 40 and 45% despite 50% of the working population being women. No data is available for current injury rates, however, the rates of 42 per 1 000 workers in 2006 were 27% higher than in 1994. This suggested a worsening of occupational health and safety standards over time (Adams, 2007). Furthermore, the lack of more detailed data has resulted in an inability to identify the important sectors contributing to these injuries. As previously observed, hand injuries are the most common (Myeni, 2020). This has major implications for the rehabilitation of workers in this country since a substantial proportion are manual workers.
In the mining sector there were 2 350 occupational injuries reported in 2018, which represents an injury rate of 514 per 100 000 workers. As has been the trend over the past three decades, gold mining is the most hazardous and accounts for half of all reported fatalities (2018). Both injury and fatality rates (Figure 11.2) in mines have indicated a downward trend from 1984 and the number of injuries has halved since 2007 (Myeni, 2020; Adams, 2007). This is likely related to the contraction of the mining industry as well as improved safety measures in mines due to improved regulation of mine health and safety since the early 1990s (Jeebhay, 1999; Adams, 2007).
The number of women working in the mining sector has increased significantly in the past 15 years – from around 11 400 in 2002 to 56 691 in 2019, representing 12% of the mining workforce (2019). There has been an increase in the number of injuries involving women since entering the mining workforce (Figure 11.3). Two-thirds of these injuries are due to accidents associated with slipping and falling, material handling and being struck by objects. The Minerals Council has attributed these accidents to all forms of equipment (overalls, PPE, boots or tools) that have been designed and manufactured with men in mind (Minerals Council, 2019).
Figure11.3 Injuries reported among women in the mining industry (2001–2019)

Source: Department of Mineral Resources and Energy, Mine Health and Safety Inspectorate Annual Report 2019/20
For decades now, South Africa continues to report fragmentation, scarcity, paucity and inadequacy of the delivery of occupational health services (Kistnasamy, 1987; Zwi et al., 1988; Lowe et al., 1990; Jeebhay & Jacobs, 1999; Adams et al., 2007). This is despite, among others, the Erasmus Commission and the Abdullah report, which identified and described the gaps in OHS in South Africa (Erasmus Commission 1976; Department of Health 1996).
In South Africa, OHS is mostly delivered using one of three service delivery models, namely: 1) in-house, 2) outsourced and 3) the hybrid model. Large enterprises and the public sector, particularly the PDoHs mostly use an in-house model with multidisciplinary occupational health professionals delivering the OHS on behalf of the employer. Some enterprises use an outsourced model wherein a private entity provides OHS, often with primary health care (PHC). Some enterprises have a hybrid model where the traditional occupational health (occupational hygiene and occupational medicine) is provided in-house, and employee wellness services are outsourced (Michell, 2012; Department of Health 1996).
The ILO (International Labour Organization, 1985), WHO (World Health Organization, 1995), ICOH (International Commission on Occupational Health, 2021), SASOM (South African Society of Occupational Medicine, 2007), the South African Government (Republic of South Africa, 1993; National Department of Health, 1997; Department of Health, 1996), and peer-reviewed publications (Rantanen et al., 2017) have all defined some package of OHS. Mostly, the OHS package in these resolutions and guidelines are adaptations of the ILO Convention 161 (International Labour Organization, 1985).
OHS is intended for the prevention of sickness absenteeism, premature disability and mortality from occupational accidents and diseases, promoting health and longer working careers, work ability and better work organisation (Rantanen et al., 2017). The WHO advocates for a realistic long-term objective to provide all workers access to a competent OHS (World Health Organization, 1995). South African workers face precarious working conditions, and have been grappling with low and inadequate access to OHS for workers particularly in small and medium enterprises (SMEs) and the informal economy (Word Health Organization, 2021; Moyo et al., 2015; Moodley & Bachmann, 2002; Michell, 2012; Lwando Maki, 2019).
Over the past decade, there have been several reforms to the South African health system and occupational health legislation, which had implications for improved access and coverage with OHS. The NDoH introduced the PHC re-engineering policy (NDoH, 2010), National Public Health Institutes of South Africa Bill (Republic of South Africa, 2017) and the NHI bills (Republic of South Africa, 2021), as well as reforms at the Medical Bureau for Occupational Diseases. These reforms have and will impact OHS equity, particularly by improving demand and provision of public sector OHS. The impact is expected primarily for vulnerable workers in the informal economy, SMEs, ex-mine workers and migrant workers who are dependent on the public health system in the management of the interplay between occupational risk and access to health services and the blurred boundary between community and workplace health issues.
While there is a paucity of data, coverage and access to OHS in South Africa is reported to be between 11 and 18%, and mostly in large enterprises (Sitas et al., 1988; Jeebhay & Jacobs, 1999). However, an emphasis on vulnerable workers (informal economy, agricultural, SMEs, ex-mine and migrant workers) is needed, as workers in large enterprises (mining, banking, construction, transport, auto-industry, health sector, etc.) have reasonable access to OHS (Sitas et al., 1988; Moodley & Bachmann, 2002). Since 2015, progress in OHS health reforms has been on policy with limited implementation other than in mining. However, historically and including the past decade, numerous examples of OHS have been implemented in South Africa, including:
• Provision of referral specialist occupational medicine and hygiene services by the NIOH, University of Cape Town (UCT) and Groote Schuur Hospital, and University of KwaZulu-Natal (UKZN) Occupational and Environmental Health department.
• Provision and utilisation of a web-based comprehensive and integrated Occupational Health and Safety Information System (OHASIS) for the health sector to enter and track essential safety, health and environment indicators in the workplace, through the NIOH. OHASIS is fully implemented in the National Health Laboratory Services (NHLS), is undergoing early roll-out in Gauteng PDoH, was recently acquired by the Western Cape PDoH, and the Mpumalanga and North West PDoHs are in negotiations to acquire the system.
• The NDoH’s One Stop Services (OSS) for ex-mineworkers under the Compensation Commissioner for Occupational Diseases and the Medical Bureau for Occupational Diseases. The OSS was initially developed in 2013 to improve equitable access to Benefit Medical Examinations (BMEs) and compensation of eligible ex-mine workers with occupational diseases covered by the Occupational Diseases in Mines and Works Act 78 of 1973. This service has since been utilised as a blueprint for OHS in South Africa and the Southern African region.
• While informal economy workers are excluded from the provisions of the OHS Act, the Phephanathi Platform, an ongoing collaboration between street trader organisations working in Warwick Junction, in the inner city of Durban, South Africa, and their support organisations, Women in Informal Employment: Globalizing and Organizing, Asiye eTafuleni, and the UKZN Occupational and Environmental Health department, has attempted to link traders to various parts of the health system – local government, occupational health professionals (UKZN) and the public health system. The platform focuses on two key pieces of work – the design and roll-out of first aid stands into the markets, and attempts to institutionalise occupational health and safety for informal workers operating in urban public space (Alfers et al., 2016). While the abovementioned programme can be cited as best practice in the informal economy, most informal economy workers will never experience OHS or even standard health services.
• While there are no specified OHS requirements for domestic workers, the landmark decision by the Constitutional Court to uphold the High Court’s declaration that domestic workers were to be included in the Compensation for Occupational Injuries and Diseases Act, and as such receive compensation for occupational diseases and injuries has potential to improve OHS for domestic workers (Atrey, 2021).
• The NDoH PHC re-engineering is delivered through the Ward-Based PHC outreach team consisting of a professional nurse, health promoter, environmental health officer and community health workers. The environmental health officers can provide basic health promotion, and diseases and injury prevention information in workplaces. However, the full potential of this programme in OHS has not been realised owing to lack of conscious collaboration between District Health Services, PHC services and OHS at national, provincial and local government level (NDoH 2013, 2010).
• Implementation of the ILO and WHO-developed HealthWISE tool, to improve work conditions, performance, occupational health and safety for health workers, and the quality of health services provided. Improvements are introduced and sustained by the combined efforts of management and staff, brought together in a dedicated team. This project is led by the NIOH and adopted by the Gauteng and Mpumalanga PDoHs is implemented in selected health facilities within the two PDoHs (International Labour Organization & World Health Organization 2014; Wilcox et al., 2020).
• In the fishing industry, ‘South Africa has measures to ensure worker health on abalone and trout farms including training and annual medical examinations. Monthly OHS meetings are organised to discuss worker health. The industry often implements safety recommendations made by external consultants’ (Cavalli et al., 2019).
• The Masoyise Health Programme, the goal of which is to reduce the impact of TB, HIV, occupational lung diseases and NCDs as occupational health threats in the mining sector, is a multi-stakeholder initiative with representatives of Minerals Council member companies, trade unions (NUM, Solidarity, AMCU, UASA), government (NDoH and DMRE, the Mine Health and Safety Council, NHLS and NIOH), SABCOHA and multilateral organisations including UNAIDS, ILO and WHO. The precursor to the Masoyise Health Programme was Masoyise iTB (‘Lets Beat TB’), the aim of which was to increase counselling for HIV and screening for TB in the industry (Minerals Council South Africa, 2021).
While tragic, the COVID-19 pandemic has thrown the spotlight on the lack of OHS and provided an opportunity for increased OHS coverage. The DEL Directions on OHS measures in workplaces included guidelines on symptom monitoring and management of workers for SARS-CoV-2 and submission of COVID-19-related health data, while the NDoH provided workplace guidelines (Department of Employment and Labour 2020; National Department of Health 2021, 2020). These instruments have led to awareness training, health promotion activities, health risk assessments, workplace screening and referral services, as well as the development of the NIOH’s OHSS for COVID-19.
South Africa still lags on OHS and overarching comprehensive occupational health and safety policy through the DEL is critical for improving equitable access and coverage with OHS. The general lack of OHS provision within the public health sector is an opportunity to adopt and implement the workers’ health interventions in PHC, and the development and/or strengthening of the occupational health units / clinics associated with medical schools / secondary-level hospitals to improve OHS coverage and access. The occupational health inspectorate should strengthen enforcement for OHS, and the informal economy and SMEs should access OHS within the public sector and where possible through the support of large enterprises. An awareness campaign on OHS rights and responsibilities should be considered on a large scale by enforcement authorities, trade unions and employers.
Occupational health professionals include occupational health doctors and nurses, occupational hygienists, environmental health professionals, workplace inspectors, employee assistance practitioners, occupational therapists, ergonomics practitioners and health and safety practitioners. These practitioners can be categorised in three broad sections, namely: those directly involved in service provision, those involved in inspections and enforcement and those involved in social protection.
The total number of certified occupational hygiene professionals is currently 836 (Southern African Institute for Occupational Hygiene). There are 404 (Myeni, 2020) occupational medicine practitioners registered with SASOM, 58 occupational medicine specialists and 1 679 occupational health nurses registered with SASOHN. According to the WHO, the ratio of 1:1 000 population is recommended as best practice. Our proportions in South Africa are very low at 1 occupational health nurse to 5 657 formal sector employees excluding agriculture. However, the doctors’ numbers are a gross under-estimation, especially for occupational medicine practitioners, as a large proportion is not affiliated with SASOM. Registration with professional bodies is voluntary, the result being that there are many more doctors practising occupational health without affiliation to SASOM. For nurses however, due to the incentive of a professional insurance cover, the numbers are a true reflection.
A large proportion of inspectors are employed by the DMRE for the mining sector and the DEL for the remaining industries. There are also other inspection agencies and regulators that perform specific inspections and are highly legislated. For example, the Railway Safety Regulator regulates the railway sector, and the National Nuclear Regulator is responsible for enforcing regulatory radiation safety standards. Currently there is approximately 1 inspector per 3 689 mining employees and 1 per
25 690 employees in the non-mining sector. This is after the recruitment of 500 inspec tors in the DEL in 2019. Of note, over the past three years, more women inspectors have been employed, attempting to bridge the gender divide.
Social protection agencies such as the Medical Bureau for Occupational Diseases and the Compensation Fund together with its mutual assurances employ different cadres of professionals including administrators, nurses, doctors and occupational therapists, among others, depending on their mandate.
The majority of OHS personnel are concentrated in the private sector. Those in the public sector, although qualified as occupational health professionals, are often re-purposed for other duties that are deemed a priority in hospitals, for example, maternity services. One of the main reasons for this is poorly functioning public OHS that lacks the appropriate operational structure.
There are at least 10 different professional bodies for different categories of OHS as per Table 11.7. The direct service provision group, namely, nurses, doctors and occupational hygienists have organised themselves into professional societies.
Table 11.7 Societies of the different OHS professionals (Source Myeni, 2020)
Name of Professional Body
Acronym Professionals represented
South African Society of Occupational Medicine SASOM Occupational Health Doctors
South African Society of Occupational Health Nursing Practitioners SASOHN Occupational Health Nurses
South African Institute of Occupational Hygiene SAIOH Occupational Hygiene Professionals
Southern Africa Institute for Occupational Safety and Health SAIOSH Health and Safety Professionals
South African Qualifications and Certification Committee – Fire SAQCC-Fire Fire Service Technicians
South African Qualifications and Certification Committee – Gas SAQCC-Gas Gas Practitioners
Institute for Working at Heights Professional Body IWH Working at Heights Professionals
Employee Assistance Professionals Association EAPA Employee Assistance Practitioners Ergonomics Society of South Africa ESSA Ergonomics Practitioners
Mine Medical Professionals Association MMPA Medical and Health Professionals in Mining Industry
South African Council for the Project and Construction Management Professions SACPCMP Occupational / Construction Health and Safety Practitioners
These societies are used as a networking platform for members to engage in matters of interest and provide guidance for practice. Continuing education is often a major priority activity of societies to strengthen and promote sound occupational health knowledge and practice as well as to further professional interests of members of these societies.
Training of occupational health professionals happens at various levels in South Africa depending on the roles that one needs to fulfil. Formal courses offered through various universities range from postgraduate diplomas to PhD. For doctors, a Fellowship qualification is offered by the Colleges of Medicine of South Africa through the University of Cape Town, University of the Witwatersrand, University of KwaZulu-Natal and Stellenbosch University. Over the past five years, the number of trained occupational medicine specialists has been increasing by an average of two specialists per year. The total of specialists trained since the speciality was gazetted in 2007 is 56 in the country, including three non-South Africans.
For nurses, various institutions offer postgraduate courses up to Masters and PhD level. It is important to note that the majority of courses are offered in the Gauteng province and none are offered in Mpumalanga, Free State, Northern Cape, Eastern Cape, Limpopo and North West.
Of note, the South African Nursing Council is currently restructuring and has drafted a new curriculum that replaces all courses with a postgraduate diploma and a BCur at NQF8 level. All institutions are in the process of being accredited and the process is rather slow, hence it will be noticed that training has been halted in institutions such as the University of the Witwatersrand. Currently, only Cape Peninsula University of Technology and Durban University of Technology have been accredited thus far for intake in the 2022 academic year of 60 and 15 students, respectively. Institutions such as the Foundation for Professional Development continue to offer short courses (e.g. audiometry, spirometry and vision screening) while awaiting accreditation for two-year courses.
Occupational hygiene consists of professionals emerging from various relevant disciplines. The majority of occupational hygienists stem from the Environmental Health stream that is still offered at a number of tertiary institutions (e.g. Tshwane University of Technology and University of Johannesburg). Many others graduated with a BSc in Physiology from universities such as the North-West and Limpopo. The North-West University recently restructured the formal training of occupational hygienists by introducing specific programmes from undergraduate to PhD level in Occupational Hygiene.
The Southern African Institute for Occupational Hygiene, being the regulatory professional body governs professional examinations that must be successfully completed to demonstrate competence at various certification levels, and continual professional development is required to ensure that occupational hygiene professionals maintain their knowledge and expertise as well as to remain up to date with new knowledge.
Other programmes for occupational hygienists are postgraduate degrees (MSc, MPH, M-Tech and PhD) offered by various universities such as Wits, UP as well as universities of technology.
Furthermore, the Wits School of Public Health has introduced new qualifications (MSc Medicine: Exposure Science & MPH Exposure and Health) which also aim to train occupational and environmental health professionals including occupational hygienists. The new qualifications begin at postgraduate level with no specific undergraduate degree to direct their academic progression. Although the qualifications aim to be specific for exposure scientists, it is however still not clear how placement of graduates will be pursued in terms of employment and career pathing.
It is important to note that South Africa also provides postgraduate occupational health training for the rest of the continent. A recent study confirms that there is still a shortage of occupational health professionals in Zambia, Lesotho, Mozambique and Malawi (Moyo, 2015).
South Africa faces multiple economic challenges such as jobless growth especially affecting young people and the need to transition to a green and climate resilient economy. The elements of an advanced industrial economy and the Fourth Industrial Revolution together with primary, secondary, tertiary and informal sectors cover important models for innovations in OHS that should ‘leave no worker’ and their families and communities behind.
Between 2015 and 2020, there was heightened awareness on occupational health and safety driven in part by occupational health professionals and trade unions. The COVID-19 pandemic exposed some of the shortcomings in occupational health and safety (especially in public health facilities) and provision of PPE. Development of a database for occupational lung diseases in mineworkers, innovations in service delivery for certain sectors of the economy and partnerships across public and private sectors and occupational health professionals in the COVID-19 workplace programme were some of the initiatives during this period. The class action settlements amounting to billions of rands for silicosis and TB allowed for introspection by the mining sector and occupational health and safety preventive interventions such as the Masoyise TB project in the mining sector. Education and training initiatives across the continent were undertaken in partnerships with occupational health professionals and institutes in different countries. The TB project in the mining sector funded by social partners raised awareness on occupational health and safety in the Southern African Development Community region using TB in current and ex-mineworkers as an entry point.
There remains a fragmented policy, governance and legislative framework for occupational health and safety. Attempts to integrate the two compensation systems failed despite substantive work over two years to develop one uniform compensation system. Surveillance data cannot be collected for occupational injuries and diseases and where available covers mainly numerator data. Thus, comparisons across sectors and monitoring of trends are not possible. The funding model for occupational health and safety is mainly driven by private sector resources especially in large companies with many sectors, including the informal sector bereft of services.
Leadership in occupational health and safety is needed and re-visiting the different commission reports and their recommendations would be an important initial step. The legal frameworks, although fragmented, can assist with driving an agenda for reform linking prevention and enforcement. Data that incorporates denominator and numerator can assist with epidemiological surveillance, the OHIS and interventions.
This chapter focused on the difficult legacy of neglect of occupational health and safety in South Africa with some innovations in service delivery. The COVID-19 pandemic provides an impetus of working together to deliver a safe and healthy workplace environment for workers.
• An approach to funding of the medical services may include the transfer of funds for medical care including rehabilitation costs to the proposed NHI fund to cover the costs of health care for occupational injuries and diseases.
• Increased investment in training should be considered to increase the numbers of trained OHS professionals to meet the needs for occupational health and safety especially in the public sector.
• Retention strategies should be developed for trained OHS professionals already in the system.
• A funding model should be developed to support OHS delivery across sectors and provide employment opportunities for occupational health and safety professionals.
Abdullah Report on Occupational Health. South Africa, 1996b.
Adams S, Ehrlich R, Quail Z, Jeebhay MF, Ismail N. Occupational health challenges facing the Department of Health: Protecting employees against tuberculosis and caring for former mineworkers with occupational health disease. South African Health Review. 2012/2013(1).
Alfers L, Xulu P, Dobson R. Promoting workplace health and safety in urban public space: reflections from Durban, South Africa. Environment and Urbanization. 2016;28: 391–404.
Anon. Women in Mining Factsheet. s.l. Mineral Council of South Africa. 2020.
Anon. World Health Organization. Prevention, identification and management of health worker infection in the context of COVID-19. 2020. [Online] [Accessed 2021].
Anon. Masoyise Health Programme Annual Report for 2020. 2021.
Atrey S. Beyond discrimination: Mahlangu and the use of intersectionality as a general theory of constitutional interpretation. International Journal of Discrimination and the Law. 2021;21(2): 168–178.
Brouwer DRD. Can the South African milestones for reducing exposure to respirable crystalline silica and silicosis be achieved and reliably monitored? Front Public Health. 2020; 8: 107.
Cavalli L, Jeebhay M, Marques F, Mitchell R, Neis B, Ngajilo D, Watterson A. Scoping global aquaculture occupational safety and health. Journal of Agromedicine. 2019; 24: 391–404.
Department of Employment and Labour. Compensation for Occupational Injuries and Diseases Act 130, s.l.: s.n. Government of South Africa. 1993.
Department of Health. Report of the Committee on Occupational Health. In: DOH (ed.). Pretoria (South Africa): Government Printers. 1996.
Department of Health, Government of South Africa, Act 33 of 2005. Nursing Act 2005
Department of Labour and Employment, Government of South Africa. COVID-19 Occupational Health and Safety Measures in Workplaces. 2020.
Department of Mineral Resources, Government of South Africa. Mine Health and Safety Act 29. 1996.
Department of Mineral Resources and Energy. Government of South Africa. Mine Health and Safety Inspectorate Annual Report 2019/20. 2020.
Erasmus Commission. The Commission of Enquiry on Occupational Health. Erasmus Commission. Pretoria (South Africa): Government Printers. 1976.
Grobler L, Mehtar S, Dheda K et al. The epidemiology of tuberculosis in health care workers in South Africa: a systematic review. BMC Health Serv Res. 2016;16: 416.
International Commission on Occupational Health. Seoul Statement on Occupational Health Services, Milano, 2021.
International Labor Organization. Health and Safety at Work. https://www.ilo.org/ global/topics/safety-and-health-at-work [Accessed Online 2021].
International Labour Organization. Convention 161 – Occupational Health Services in ILO, Geneva: 1985.
International Labour Organization and World Health Organization. HealthWISE Work Improvement in Health Services, Geneva. 2014
Jeebhay M, Adams S, Morar R, Kolbe-Alexander TL. Health and Healthcare in the South African Workplace. South African Health Review, 13th edition. 2007;13: 103–121.
Jeebhay M, Jacobs B. Occupational health services in South Africa. In Crisp N and Ntuli A, eds. South African Health Review, 5th edition. Durban, South Africa: Health Systems Trust, 1999;19: 257–276. http://www.hst.org.za/sahr/99/chap19.htm
Kielkowski D, Rees D, Bradshaw D. Burden of Occupational Morbidity in South Africa: Two large field surveys of self-reported work-related and work-aggravated disease: research letter. South African Journal of Science. 2004;100(7).
Kgokong N, Mhlongo L, Vorajee N et al. National Institute for Occupational Health. Pathology Division Surveillance Report. 2018.
Kistnasamy MB. Occupational Health in South Africa. Dissertation, MPH, University of KwaZulu-Natal. 1987.
Lowe R, Barron P, Steyn S, Malekela L. Occupational Health and Randburg. SAMJ 1990;77: 581.
Maki L. Occupational Health Services in the South African Construction Industry: Prioritising Health. MMed, University of Pretoria. 2019.
Michell KE. Occupational Health Service Delivery in South Africa. Workplace Health & Safety. 2012: 60, 63–66.
Minerals Council South Africa. 2021. www.mineralscouncil.org.za/work/health-andsafety/masoyise-healthprogramme. [Online] [Accessed 7 June 2021].
Moodley P. Buchmann M. Inequity in Occupational Health Services for Government Hospital Workers in South Africa. Occupational Medicine. 2002: 52, 393–399.
Moyo D, Zungu M, Kgalamono S, Mwila CD. Review of Occupational Health and Safety Organization in Expanding Economies: The case of Southern Africa. Annals of Global Health. 2015: 495–502.
Myeni SS. The Profile of Occupational Health and Safety in South Africa. National Department of Employment and Labour (RSA) and the International Labour Organization. 2020.
Naidoo RJM. COVID-19 – A new burden of respiratory disease among South African miners. Curr Opin Pulm Med. 2021 Mar 1;27(2): 79–87.
National Department of Health. White Paper for the Transformation of the Health System in South Africa. Government Gazette. 1997.
National Department of Health. The Re-Engineering of Primary Health Care in South Africa. 2010.
National Department of Health. OHS within the PHC Re-engineering: The integration of occupational health services within the primary health care health system. Johannesburg, South Africa: NDoH. 2013.
National Department of Health. Guidelines for Symptom Monitoring and Management of Essential Workers for COVID-19-related infection. 2020.
National Department of Health, n.d. National Health Act 61 of 2003. Government Gazette.
National Department of Health. Guideline on the submission of COVID-19-related health data from workplaces to the National Department of Health. 2020. www. nicd.ac.za/wp-content/uploads/2020/08/Workplace-Data-SubmissionGuideline. [Online] [Accessed 20 June 2021].
National Institute for Occupational Health. OHSS Report for COVID-19 in South African workplaces for the period 1 October 2020 – 31 March 2021. 2021.
National Institute for Occupational Health. COVID-19 hospital surveillance –monthly update on hospitalized healthcare workers. Johannesburg (South Africa): NIOH / NHLS; 2022 [updated March 19, 2022; cited 2022 April 05]. Available from: https://www.nioh.ac.za/wp-content/uploads/2022/04/COVI_-HCW_ Report_week11of2022-1.pdf
Organisation of Economic Co-operation and Development. OECD Economic Surveys: South Africa 2010. 2010.
Rantanen J, Lehtinen S, Valenti A, Iavicoli S. A Global Survey on Occupational Health Services in Selected International Commission on Occupational Health (ICOH) Member Countries. BMC Public Health. 2017: 17, 787.
Read JM. Hospital-acquired SARS-CoV-2 Infection in the UK’s first COVID-19 pandemic wave. Lancet. 2021 Sep 18;398(10305): 1037–1038.
Rees K, Dunlop JL, Patel-Abrahams S, Struthers H, McIntyre JA. Primary healthcare workers at risk during COVID-19: An analysis of infections in HIV service providers in five districts of South Africa. S Afr Med J. 2021 Jan 18;111(4): 309–314.
Republic of South Africa. Medicines and Related Substances Act 101. 1965.
Republic of South Africa. Occupational Diseases in Mines and Works Act No 78. Government Gazette. 1973.
Republic of South Africa. Occupational Health and Safety Act No 85 Department of Employment and Labour. 1993: 15–16.
Republic of South Africa. National Public Health Institute of South Africa Bill. 2017. Republic of South Africa. National Health Insurance (NHI) Bill. 2021.
Sitas F, Davies J, Kielkowski D, Becklake M. Occupational Helth Services in South African Manufacturing Industries: A Pilot Survey. Am J Ind Med. 1988;14(5): 545–57.
South African Society of Occupational Medicine (SASOM). Organisational Health Services. 2017.
Wilcox E, Chimedza I, Mabhele S, Romao P, Spiegel J, Zungu M, Yassi A. Empowering Health Workers to Protect Their Own Health: A Study of Enabling Factors and Barriers to Implementing HealthWISE in Mozambique, South Africa and Zimbabwe. Int J Envron Res Public Health. 2020;17.
World Health Organization. Prevention, identification and management of health worker infection in the context of COVID-19. 2020. www.who.int/publications/i/ item/10665-336265. [Online Accessed 2021].
World Health Organization. Occupational Health. The Global Occupational Health Network [GOHNET] Newsletter, 2009 (15) [Online]. Geneva (Switzerland): WHO. 2021. Available: https://www.who.int/occupational_health/network/ gohnet_15.pdf?ua=1 [Accessed June 15 2021].
World Health Organization. Global Strategy on Occupational Health for all: the way to health at work. Recommendation of the Second Meeting of the WHO Collaborating Centres in Occupational Health, Beijing: WHO. 11–14 October 1994.
Zwi A, Fonn S, Steinbert M. Occupational Health and Safety in South Africa: The perspectives of capital, state and unions. Social Science & Medicine. 1988: 691–702.
The National Core Standards (NCS) for Health Establishments are the set benchmark for quality care in South Africa and delivery of health services is measured against this standard. This chapter provides an overview of available health infrastructure in the country, its condition and adequacy. It also highlights the broader infrastructure and non-infrastructure challenges that hamper the delivery of quality health care in the country. Thereafter, it reviews progress by various national initiatives aimed at responding to current challenges including the Ideal Clinic Realisation and Maintenance (ICRM), compliance with the NCS, Infrastructure Unit Support Systems (IUSS), Draft 10-Year Health Infrastructure Plan (10YHIP), and the Draft Maintenance Strategy. For each initiative, we review the achievements and remaining challenges, before looking at trends that will affect the provision of health infrastructure in the foreseeable future such as lessons from the COVID-19 pandemic and climate change.
Health care systems are concerned with the pooling of various inputs including human capital, medicine and medical supplies, laboratory and radiology services, and support services needed to deliver a quality service. These inputs are required in a holistic, integrated and complementary manner. Infrastructure in the form of facilities, health technology1 and equipment plays a critical role as an input that enables the provision of a quality health care service. Its provision enables access to the capacity to prevent, diagnose and treat diseases, and an environment that promotes healing. Without it, access to and quality of health care are compromised.
1 The chapter does not cover Health Technology, but it has many similarities with facilities whereby lessons on the latter may also be applied to the former.
Boitumelo Mashilo, Laura Angeletti-du Toit, Nwabisa DanielsHowever, the health care system in South Africa is plagued by vast disparities in the quality of care and infrastructure across the private and public health sectors. Thus, plans are underway to implement Universal Health Coverage (UHC) that will transcend socio-economic lines and equitable access to quality health care services will be a key outcome. The experience from COVID-19 already demonstrated the need for cooperation between the private and public sectors and this lays a strong foundation for UHC. It can therefore be argued that unless the health sector as a collective finds a way to leverage all available resources (both public and private) in a complementary and integrated manner, UHC will not be realised. However, there is a long path towards this end and many trade-offs must be balanced.
Infrastructure is important in the provision of quality health care because it is the visible interface between health care professionals and the public (Erasmus et al., 2012). Key to this is the availability of infrastructure (access), its location (proximity) and state (acceptable standards). Table 12.1 depicts that the public health care system had about 3 702 Primary Health Care2 (PHC) facilities and 403 hospitals in 2020. Compared to 2015, the number of PHC facilities declined by 63 while the number of hospitals increased by one. Important to note though is that visiting points and health points were not counted as PHC facilities in the 2020 statistics. A breakdown of the available capacity in PHC facilities shows that most of these were in the Eastern Cape, KwaZulu-Natal and Limpopo. For hospitals, most of these were in the Eastern Cape, KwaZulu-Natal and the Western Cape, however, the most bed capacity was in the Eastern Cape, KwaZulu-Natal and Gauteng due to the size of the facilities.
Table 12.1 Provincial spread of public health care facilities
Province
Eastern Cape
State
2015 2020 Number of Hospitals Number of Beds Number of PHC Facilities Number of Hospitals Number of Beds
4 908
Number of PHC Facilities
Cape
Source: Various including the District Health Information System, provincial data and the SA Health Review
2 In this chapter, PHC facilities
health care centres.
In addition to availability of infrastructure, a common measure of access to hospital services is the inpatient bed capacity ratio, which is the number of hospital beds per 1 000 dependent population. The National Tertiary Health Service Plan (NTHSP) set an overall benchmark of 0.37 beds per 1 000 dependent population, made up of different benchmarks per level of care (0.66 beds for district beds; 0.33 beds for regional beds; and 0.13 beds for tertiary beds). Using the NTHSP benchmark ratio, the inpatient bed capacity ratio for South Africa’s uninsured population was 1.7 beds per 1 000 population in 2020, down from 1.9 beds per 1 000 population in 2015. For both these periods, the ratios were above the prescribed benchmark, suggesting that access is generally not a challenge. However, the decline in bed capacity ratio when the population continues to grow is a source of concern. This is because most people in South Africa are dependent on the public health care system and the number of dependents increases with population growth due to poor socio-economic conditions (high inequality, poverty and unemployment) which limit people’s choices based on affordability constraints.

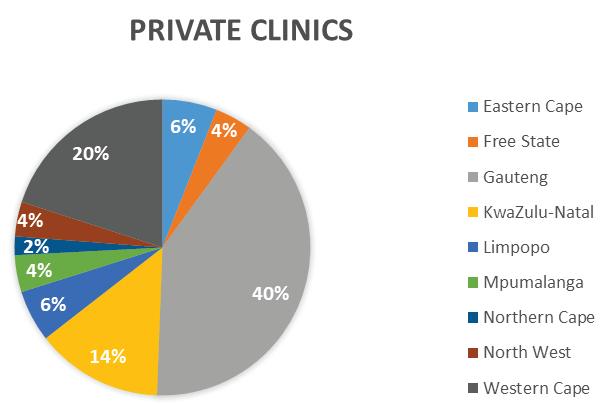
Bed capacity rate per 1
Province
Eastern
KwaZulu-Natal
Limpopo
Northern
TOTAL
Source:
dependent population
Public
2
Public beds
2.19
1.96
11 789 1.47
2.03
1.40
095 1.21
089 1.47
1.29
1.80
For PHC facilities, an appropriate measure of access is the number of consulting rooms available per 1 000 dependent population. However, there is no set benchmark for PHC facilities in the country and public information on the number of consulting rooms in South Africa is limited. The National Department of Health (NDoH) estimated the national average ratio to be 0.29 consulting rooms per 1 000 dependent population in 2015. It is not possible to compare this with 2020 due to data constraints. The World Health Organization (WHO) uses the number of health centres3 per 100 000 population as a benchmark and set this at 10 health centres per 100 000 population in 2018. Using the WHO benchmark, South Africa had an estimated 7.3 PHC facilities per 100 000 dependent population in 2020, a decline compared to 7.5 PHC facilities per 100 000 dependent population in 2015. For both 2015 and 2020, the number of facilities was below the recommended WHO threshold, suggesting that access to PHC is a challenge in South Africa. It must be noted though that the WHO indicator does not specify the size of the health centres and therefore the benchmark is skewed if facilities are not rightsized for the catchment population.
An additional measure of access is the proximity to health care facilities (distance and time) and the costs associated with the access. This is key in a country whose spatial form is known to be exclusionary. The WHO recommends that health care facilities should be available within a five-kilometre radius. According to McLaren et al. (2014), two-thirds of South Africans were found to reside less than two kilometres from public clinics and about 90% reside within a seven-kilometre radius. In terms of time, the 2019 GHS estimates that 41.6% of households can access health care facilities in less than 15 minutes and 43.2% of households can access health care facilities within 15 to 29 minutes. It is important to note that there are notable differences in urban versus rural areas, and across races. Further, the costs associated with accessing health care are prohibitive for the poor particularly in non-urban areas. Lastly, there are long waiting times associated with accessing free public health care, which results in people seeking private health care at costs that are unaffordable to them or opting to not seek medical care. These waiting times do not reflect people who due to inaccessibility challenges do not even attempt to seek medical care.
Table 12.3 shows the average waiting times associated with each level of care in 2015. Overall, specialised hospitals had the shortest total time spent by a patient at two hours per visit, while regional and tertiary hospitals had the longest total time spent by a patient at four hours per visit. This does not include the long waiting lists associated with access to some medical treatments in the public health care system. An example of this would be the Chris Hani Baragwanath Hospital, which in March 2015 had a waiting list of 4 846 patients waiting for a variety of procedures. Most of these patients were awaiting ophthalmic (1 919), orthopaedic (1 326), urology (1 200), general surgery (357) and plastic surgery (44) procedures. This phenomenon is widely prevalent and points to factors that deter patients and disincentivise them from seeking any medical care.
3 These are facilities that provide health care services but have no beds other than those needed for emergencies and maternity care.


Specialized Hospitals 1 2 PHC facilities 2 3 District Hospitals 2 3 Regional Hospitals 3 4 Tertiary Hospitals 3 4
Source: National Department of Health
Notwithstanding the challenges in the public health care system, 62.7% of households first consulted a public clinic for illnesses or injuries and 23.5% of households first consulted a private doctor in 2015. The remaining proportion of households first consulted either a public or private hospital, traditional healer or pharmacy, etc. By 2020, the proportion of households that first consulted a public clinic improved to 65.4% while those who first consulted a private doctor declined to 21%. The dependence on public clinics is consistent for all provinces except for the Western Cape, where the proportion of households that first consult a private doctor (37.2%) was almost as high as those who first consulted a public clinic (42.3%). The trend demonstrates an increasing reliance on public clinics as the first port of call when family members are ill or injured for those who were part of the sampled population. This could indicate that government efforts to strengthen the PHC system are bearing results or that due to changes in the socio-economic status, private health care is no longer affordable or accessible for those who previously relied on it.
Figure 12.2 Type of health care facilities consulted first by households in 2015 and 2020
Source: GHS, 2016 and 2020
Users of the public health care system recorded lower levels of satisfaction compared to those who use private health care according to the 2018 General Household Survey. The survey reported that 80.3% of users of public health care facilities were somewhat satisfied or very satisfied compared to 97.6% of us ers of private health care. This highlights the shortfall in expectations in the overall health care system, albeit more so in the public than the private health care system.
In as far as the state of infrastructure is concerned, public hospitals were rated D+ and clinics D according to the 2017 South African Institution of Civil Engineering (SAICE) Infrastructure Report Card. The ratings indicate that these facilities are at a risk of failure – the infrastructure is not coping with demand and is poorly maintained. The Infrastructure Report Card states that any condition of ‘C’ and below in the context of health care facilities adversely affects patient care and safety, and places the facility and the staff at increased risk.
Further, the 2019/20 Annual Inspection Report of the Office of Health Standards Compliance (OHSC) indicated that only one in seven inspected health facilities complied with the NCS. These condition outcomes point to the need to prioritise maintenance, preventative or backlog, in order to avoid further deterioration in the condition of the current facilities, barring the need to expand access.
Compared to other countries in the continent, the state of South Africa’s public health infrastructure is among the poorest. As illustrated in Figure 12.3, South Africa has an index score of 0.13, which is significantly below the regional average score of 0.40. The poor outcome is despite the country’s high total health spending, which is ranked second on the continent at US$1 148.37 per capita according to the World Bank (2018).
Overall, the analysis in this section points out that notwithstanding the availability of infrastructure, access is a challenge from waiting times and cost perspectives. There are also quality of service issues, and these are reflected in the expectations shortfalls. The National Treasury (2021) reported that medico-legal claims increased from R265 million in 2012/13 to R1.7 billion in 2019/20. Further, contingent liabilities5 increased from R28.6 billion in 2014/15 to R111.5 billion in 2019/20. Dhai (2015) indicated that the rapid increase in medico-legal claims is

indicative of deteriorated levels of care in the public health care system. Expectation shortfalls are also experienced in the private sector, however, the extent is not the same as the public sector and in some cases, there is limited publicly available information to conduct comparative analysis. In regard to medico-legal claims, these are also rising in the private sector but are predominantly driven by medical malpractice. The quality of the infrastructure is a major contributor to the shortfall in expectations for patients.
As such, inadequacies highlighted in this section undermine the quality of health care provided. A quality health care system must have the capacity and capability to respond adequately and timeously to evolving demographic and epidemiological needs of the total population.
The health sector faces several challenges and infrastructure is a contributor. Unless the challenges are adequately resolved, the health sector will continue to deliver sub-optimal outcomes. As such, to the extent that infrastructure contributes to sub-optimal outcomes, this must be pointed out and resolved, in addition to addressing the need for new infrastructure where it is needed. Below are the key infrastructure challenges that contribute to inadequacies in the health care system of the country.
1. Poor condition of health care facilities: As stated in the previous section, a large proportion of public health care facilities are non-compliant with the NCS. These facilities exhibit defects, deep wear and tear, and signs of deterioration such as breakdowns in building structures.
2. Facilities are not fit-for-purpose: Health care facilities are seldom retired, repurposed or refurbished at the end of their economic life, some have inefficient layouts and others were built with inappropriate materials (i.e. asbestos). These factors adversely affect their usability and desirability.
3. Facilities are unresponsive to evolving patterns: The demographic and epidemiological patterns evolve with time, yet health care facilities remain static. The sector seldom rationalises health care facilities to ensure that the size, location and service coverage is appropriate for the needs of the catchment population.
4. Facilities have insufficient, old and dysfunctional health technology: There are facilities that do not have the requisite equipment for their levels of care. This is mainly caused by failure to replace damaged or obsolete equipment, and the inability of staff to operate the health technology where this is available.
5. Maintenance neglect: This is a multi-pronged challenge wherein budgeting for maintenance is generally not done, and even in cases where there are budgets, these are either not used (fully or partially) or are reprioritised to other cost pressures. The deterioration of facilities over time requires major refurbishments at a much higher cost.
4 The health status scores measure the general readiness of facilities to provide essential services and considered the availability of basic amenities and equipment needed for service provision; the total number of beds; and total hospitals, health posts and health centres per 100 000 population.
5 Total medico-legal claims against the state.
To remedy the challenges in this section, we propose that the sector prioritises maintenance as a matter of urgency by ensuring that sufficient maintenance budgets are allocated and ring-fenced for recurrent maintenance. Even when budgets are inadequate, recurrent maintenance programmes must be done to the extent possible. We focus on recurrent6 maintenance because we believe this should take precedence over capital7 maintenance, and certainly new build. Further, maintenance of PHC facilities and hospitals should be differentiated by the hub and spoke model8 managed by the District Office as opposed to a centralised model. The sector must also prioritise the appointment of maintenance personnel at facility level and provide for the required goods and services.
Further, it is common knowledge that there are capacity constraints in the Provincial Departments of Health, health districts and the Department of Public Works and these are major contributors to challenges in the health infrastructure delivery value chain. However, capacity and capability varies across provinces. We propose therefore that the NDoH directs its efforts towards strengthening capacity and capability in a targeted and customised manner according to the needs of each province. Where pockets of excellence exist in the sector, these should be leveraged for the greater good. It is also critical that the sector aims to build capability internally and institutionalise this to reduce reliance on consultants regarding responsibilities that officials should retain and tap into with respect to institutional knowledge, memory and expertise.
It cannot be overemphasised that strategic planning should be done correctly and regularly to inform any new capital work that is to be embarked upon. This should inform the suitability, fit for purpose, and right sizing of facilities. The catchment population and recommended bed norms per level of care, patient audits, referral patterns and occupancy statistics should inform the planning of upgrades and additions, replacements, and new hospitals. The practice of planning public beds independent from private beds should also be changed.
The IUSS guidelines, norms and standards (GNS) that were developed about 10 years ago must be used to support infrastructure planning and delivery in the sector, as they directly influence the size and cost of the health facilities (more on the IUSS in later sections). Adherence to norms and standards must be enforced and deviations without acceptable motivation reported to competent authorities such as the Auditor-General.
The inefficiencies highlighted in previous sections are largely due to systemic challenges that must be tackled to improve the sub-optimal outcomes including in infrastructure. The challenges also contribute to the high cost of infrastructure. These include:
1. Poor planning and coordination: The health sector dedicates very little time to project development and fails to identify the interdependencies between this phase and the operations phase. This is exacerbated by insufficient capability, skills and
6 Recurrent maintenance includes day-to-day maintenance; term contracts for specialist installations and statutory maintenance which is prescribed by the OHS Act.
7 Capital maintenance includes rehabilitation, refurbishment and replacement of obsolete assets, and addressing the backlog maintenance.
8 This is a maintenance model where the maintenance team is employed by the hospital and attends to surrounding PHC facilities.
experience amongst those responsible for planning, specifying, procuring and overseeing the implementation and maintenance of infrastructure in the sector (Human Science Research Council, 2019). The infrastructure directorates in health departments have been hollowed out, institutional knowledge is lost and as such, these directorates are no longer ‘informed clients’. This is partly the reason for appointment of implementing agents, who also do not have the capacity and have to outsource the work to consultants with varying degrees of experience.
There is also no criteria currently to guide the public sector on project prioritisation and selection, which has resulted in subjective and inconsistent selection of projects. There is limited coordination between and within health departments and related public sector structures, and no coordination between the public and private health sector.
2. Inadequate capacity and capability of personnel in public health facilities: The facility managers and Chief Executive Officers appointed tend to not have infrastructure skills and experience to lead or manage infrastructure projects in their facilities. This is exacerbated when infrastructure personnel are either unavailable or incapable. This results in facilities neglecting maintenance and exposing staff and patients to an unconducive work/healing environment. There are also many cases where it is known that health facilities are underfunded and understaffed and the outcomes continue to be poor-quality service.
3. Inadequate funding and poor quantity of spending: The health sector is faced with a trichotomy of inadequate budgets, underspending and sub-optimal spending. Infrastructure budgets have declined over the last 10 years, which has limited public health infrastructure investment and widened the gap between public health infrastructure needs and total investment. The sector has also over the years been underspending on the allocated budget (e.g. inconsistent trend of underspending in the sector at an average 5% per annum between 2015/16 and 2018/19). Lastly, the trend of cost overruns and escalations, significant variation orders, over-specified and expensive designs and other cost inefficiencies is prevalent in the public health sector. These factors undermine value for money, make infrastructure provision costly, and undermine the rationale for additional infrastructure allocations.
4. Non-adherence to industry norms, standards and procurement legislation and processes: In addition to lower levels of compliance to the NCS, there is also noncompliance with building norms and standards, procurement legislation and processes, and bed capacity ratios. In relation to procurement of goods, works and services, the Special Investigating Unit report (2020) under the National State of Disaster indicated that within provincial government departments, procurement was non-compliant with minimum prescripts that regulate public sector procurement. This was effectively a contravention of the Constitution and the Public Finance Management Act principles of fairness, equity, transparency, competitiveness and cost-effectiveness. The Auditor-General (2020) conducted a special audit for COVID-19 and found irregular procurement and contract management to the tune of R3.3bn in the public health sector. The biggest contributors were deviations in awarding of contracts without approved reason (R1.1bn) and non-declaration of interest by successful bidders (R1.1bn).
5. The disjuncture between infrastructure planning and operations: The lack of consideration of full lifecycle costs in the provision of infrastructure combined with poor asset management practices undermine the sector’s ability to be effective, let alone efficient. This is evident in the maintenance neglect once the infrastructure is built, facilities that are unresponsive to the needs of the catchment population, and the limited and outdated information on existing facilities and their condition.
6. Inappropriate use of consultants: There is an overreliance on consultants in the public sector even for functions that should ideally fall on officials. This is largely due to inadequate internal capacity and weak capability by officials in some cases. This results in professional services providers (PSPs) and other consultants being used for the planning, execution and oversight of infrastructure projects on behalf of government. The issue is not the use of consultants, but rather the excessive use, particularly on responsibilities that should fall on officials. Furthermore, there are cases where the segregation of duties between officials and consultants is unclear, resulting in PSPs not being managed or their work unchecked by officials. This evades accountability and good governance principles.
Given the myriad challenges in the sector, we recommended that changes be initiated starting with improving the quality of spend. Measures in this regard could include tighter cost benchmarks and control measures, adherence to infrastructure norms and standards, and introducing an objective criterion to prioritise interventions based on available budgets. In parallel, the request for additional funding in the public sector can be done in line with increases in capacity and capability within the health departments.
The ICRM programme was conceptualised in 2013 to systematically improve and correct deficiencies in PHC facilities in the public sector. The programme was officially launched in 2015 to standardise the requirements for all clinics and provide a benchmark against which all clinics will be measured to enhance the PHC system towards universal health access.
An Ideal Clinic is defined as a clinic with good infrastructure (i.e. physical condition and spaces, essential equipment, and information and communication tools), adequate staff, adequate medicines and supplies, good administrative processes, and sufficient adequate bulk supplies (i.e. clinic uses applicable clinical policies, protocols and guidelines, and partner and stakeholder support) to ensure the provision of quality health services to the community. The sector has developed Ideal Clinic and Community Health Centre Frameworks. These frameworks introduced a weighted ranking criterion that determines whether facilities meet the minimum requirements for ideal status. The infrastructure component has four indicators assessing whether facilities have: (1) suitable and adequately maintained physical space, (2) sufficient and adequately maintained equipment and furniture, (3) availability of bulk supplies and (4) reliable ICT infrastructure and hardware.
The cumulative number of facilities that achieved the Ideal Clinic status increased from 322 in 2015/16 to 2 100 in 2020/21. The improvement means that about 60% of PHC facilities in 2020 met the required percentage compliance with the criteria. The SAICE report (2017) acknowledges improvements in the condition of PHC facilities because of the ICRM programme. Waiting times and availability of medical stock have also improved due to the programme. Egbujie et al. (2018)9 indicated that waiting times in KwaZulu-Natal reduced by four minutes between patient arrival and taking of patient vitals, and by 17 minutes between the taking of vitals and patient consultation since the introduction of the programme.
The programme initially suffered from divergent perceptions on the roles and responsibilities across national, provincial and local government stakeholders. This was exacerbated by the weak intergovernmental relations that limited cooperation and authority. Lastly, the programme had insufficient resources from a human capital and funding perspectives. As a result, there was the unintended consequence of neglect of facilities that were not part of the programme. Muthathi and Rispel (2020) indicate that approximately 25% of all PHC facilities that were ICRM programme compliant had lost their Ideal Clinic status in a four-year period. The Health Systems Trust posits that infrastructure deficiencies; inadequate equipment, consumables and furniture; and emergency medical service response times were some of the contributing factors that resulted in the loss of Ideal Clinic status.
9 Bonaventure Egbujie, Goeffrey Fatti, Ashraf Grimwood and Sameera Allie, ‘Impact of ‘Ideal Clinic’ implementation on patient waiting time in primary healthcare clinics in KwaZulu-Natal Province, South Africa: A before-and-after evaluation’, 2018, https://www.researchgate.net/
The OHSC was established in 2013 through the National Health Amendment Act, with the key objective of protecting and promoting the health and safety of users of health care services. The OHSC executes its mandate by ensuring that health establishments comply with the NCS. In addition, it ensures that complaints about health care are investigated and, where necessary, that action is taken.
The role of the OHSC includes the monitoring and enforcing of compliance by health establishments, both public and private, to the standards and norms approved by the Minister of Health; and ensures consideration, investigation and disposal of complaints relating to non-compliance with the said standards and norms. Further, there are several mandatory norms and standards that guide the implementation of all infrastructure projects across the development cycle including the areas of clinical services, health care environment, support services and procurement and operation. Approval is required should there be a need to deviate from these norms and standards. Infrastructure in both the public and private health sectors must meet the requirements of the OHSC.
The OHSC provides the public with information on acceptable quality standards that should be provided by health establishments and ensures that non-compliance complaints are investigated (Health Standards, 2022). In addition, it is a regulator with the legislative authority to regulate norms and standards, investigate non-compliance and support the implementation of the NHI by certifying facilities as compliant or non-compliant with the NCS (National Health Act, 2013). It also introduced a quality assurance mechanism through the development of the NCS, which regulates the quality of health facilities. Part of the areas assessed by NCS include the operational management, public health, and facilities and infrastructure. Lastly, the OHSC evaluates the quality of services and can improve accountability in the PHC system.
The percentage of health establishments that complied with the NCS increased from 16% of the 730 sampled facilities in 2017/18 to 43% of the 647 sampled facilities in 2019/20. Similarly, the percentage of health establishments that were non-compliant with the NCS reduced from 84% to 48% over the same period.
Figure 12.5 below provides a summary of compliance levels of health establishments with the NCS in the 2016/17 and 2018/19 financial years. It is worth noting that there has been an improvement in the compliance levels in provinces for both PHC facilities and hospitals. In terms of PHC facilities, both KwaZulu-Natal and Gauteng met the compliance levels for PHC facilities compared to 2017/18, when only Gauteng’s PHC facilities were compliant. In terms of hospitals, four provinces met the compliance levels, namely the Western Cape, Mpumalanga, KwaZulu-Natal and Gauteng in 2018/19. This was also the case in 2017/18, with improvements noted for Mpumalanga in 2018/19. This demonstrates that since the establishment of the OHSC, there has been an overall improvement in compliance levels for both PHC facilities and hospitals during the period.
Figure 12.5 Compliance of health facilities with NCS infrastructure requirements
Source: OHSC 2018/19 Annual Inspection Report
The OHSC has been criticised by the Portfolio Committee on Health (2014) for failing to provide solutions to challenges identified in health establishments. The committee wanted the OHSC to provide remedial actions for each facility and make recommendations to provincial stakeholders, as this is where the majority of the challenges were. Further, there are no consequences for provincial and national departments of health on facilities that are non-compliant, and no follow-ups are done on previously non-compliant facilities in subsequent annual inspections or other reports provided by the OHSC (Parliamentary Monitoring Group, 2014).
The Parliamentary Monitoring Group has also criticised the OHSC of having ‘a poor relationship with the private sector’, which hindered its oversight of the sector. The Group also highlighted that there were challenges of limited knowledge and resources available to the OHSC to fully execute its mandate.
The IUSS project was initiated by the NDoH in 2010 to develop national GNS for health infrastructure. The duration of the project was four years and the GNS were gazetted on 17 February 2014 (no. R116); 30 June 2014 (no. 512) and 8 May 2015 (no. R414). The GNS documents covered various aspects of public health infrastructure including:
• Building Engineering Services and Professional service provider instructions
• Various facilities e.g. Paediatric and Neonatal, TB Services, Mental Health and Critical Care
• Support facilities e.g. Catering, Linen and Laundry, Administration and related services
• Information Technology and Infrastructure
• Primary Health Care
• Maintenance and Decommissioning
• Order of Magnitude Estimators for New Clinics; New Hospitals; Upgrade and additions to clinics; Upgrade and additions to hospitals
• Sustainable and climate resilient building technologies
• Project planning and briefing guide
The IUSS further provided data sheets which enabled briefing of consultants to simplify their work. The detail estimator for hospitals was also provided in draft format, allowing for disaggregated costing of all the sub-components of a hospital.


The frameworks developed through the IUSS can be utilised in the project brief particularly where the design-and-build procurement option is selected. They also assist in the development of the design, the monitoring and evaluation of proposals, planning of health technology and the operation of facilities. The proposals based on client briefs can be evaluated in terms of targets enabling optimum solutions to be developed. In addition, performance targets can be set and tracked from an early conceptual design stage through to operation of the facility. The order of magnitude estimators were updated quarterly with the Bureau of Economic Research escalation indices, meaning that they were kept updated up to October 2021. Lastly, the IUSS was widely used by the public and private sector with 42 529 users and 109 951 page views between 2018 and 2020. These users were not only local but included other users from six other countries including India, the United States and France (see Figure 12.6 below for details).
The NDoH did not enforce compliance with the GNS developed through the IUSS project. This was even the case for projects implemented by the Department, where consultants were not compelled to comply with these. It was the same case for benchmarks for gross building areas and cost, which were meant to ensure value for money. The IUSS website was hosted by the Council for Scientific Research and Industry and was grant funded from various sources. The website was subsequently discontinued after two years when the grant funding came to an end and the information has thus not been updated since to reflect the latest technology and treatment protocols.
There was no gradual transition away from the IUSS and the available information does not provide detail on whether the sector has reverted to the South African Health Norms and Regulation 158 for private hospitals. Despite the IUSS project coming to an end, some of the challenges that the project was meant to resolve remain, such as the gap between PSPs and clinical staff, and the lack of cost benchmarks for health infrastructure.
The Draft 10YHIP is a national plan to overhaul the health care system between 2015 and 2025 and was completed in October 2016. The plan was developed to facilitate the planning, resourcing, delivery and maintenance of the physical environment conducive to quality health care services. It was developed with the objective of equitable access requirements based on catchment population and contains the estimates of the value of all existing infrastructure, annual maintenance estimates (adjusted for facility per average condition), refurbishment and replacement value (adjusted per facility based on average condition), and new capacity requirements (based on access and population to bed/ consulting room ratios).
The Draft 10YHIP assisted the sector to develop an objective system of prioritising facility projects based on their condition. It encompasses objective and sound principles for portfolio and priority planning. This is an effort by the NDoH to ensure uniformity in the application in the prioritisation of projects in the sector. In addition, the initiative assisted the sector in establishing a baseline in terms of the number of facilities in the public and private sectors, their location and the generic conditions of public facilities, quantifying the backlog and determining the financial costs associated with the infrastructure needs of the public sector.
The initiative did not gain much traction within the sector and the 2015 Draft 10YHIP remains an informal policy document, which was never approved and enforced. However, there is a collaboration between the NDoH and the Development Bank of Southern Africa to update the plan and enhance it into an online platform. The goal is to enable a more accurate identification of infrastructure requirements based on real-time information on the condition of health facilities.
The NDoH in collaboration with the Development Bank of Southern Africa finalised a Draft Maintenance Strategy in 2015. The strategy focussed on the principles of life-cycle costing, proactive maintenance, and maintenance excellence hierarchy. As part of the life-cycle costing, a strong emphasis was put on utility consumption, collecting data, and planning interventions to reduce consumption costs. Among proposed interventions were developing annual provincial maintenance plans and making maintenance statutory to address some maintenance backlogs; to ensure maintenance of new assets – ring-fencing funds for personnel and goods and services; and move responsibility for maintenance to the provincial health departments (from the relevant implementing agents). Order of magnitude estimators were developed for the maintenance of clinics and hospitals and shared on the IUSS website.
The document was drafted and consulted with all provincial health departments, thereby providing for a pragmatic approach to maintenance. Most concepts were further developed in the One IDMS Operations and Maintenance Module (currently still in draft version).
Limited financial and human capital resources adversely affected the aspiration to reduce the maintenance backlog. The principles proposed in the document were sound and pragmatic, however, the document has remained in a final draft version since 2015.
The COVID-19 pandemic demonstrated the strategic relevance of occupational health and safety in terms of infrastructure and facility management (see Chapter on Occupational Health). The need to protect health staff from contracting COVID-19 highlighted the direct link with the general status of maintenance, ventilation, and general flow in health facilities. The established aerosol transmission requires reviewing the norms and standards for natural and mechanical ventilation. Occupational health and safety capacity building is also needed mainly at the PHC level.
Medical service is not only provided at health facilities. With Artificial Intelligence, information technologies and remote-monitoring technology, some clients will not need to attend physically at a service point. Soon, health care facilities will not need extensive waiting areas, medical records, and outpatient consulting and counselling rooms. Preventative health services can be provided at a community level, reducing the pressure currently experienced at the facility level. Lastly, COVID-19 has also brought the need for an agile and flexible response. Overall, COVID-19 has shown the extent of the inadequacies in the health sector and the response by the sector was also revealing.
Africa is the continent most vulnerable to the impacts of climate change. Already experiencing temperature increases of approximately 0.7°C over much of the continent, predictions are that temperatures will rise further. Africa faces a wide range of impacts, including increased drought and floods. Soon, climate change will contribute to decreases in food production, changes in natural ecosystems and loss of biodiversity, floods and inundation of its coastal zones and deltas, the spread of waterborne diseases and the risk of malaria.
South Africa, the highest producer of greenhouse gasses in the African continent, is also one of the geographical areas most affected by climate change. Desertification along the western area, and extreme weather and flooding along the central and eastern part of the country require resilient health infrastructure. As an adaptation strategy, facilities will have to be carefully located and constructed with technologies capable of resisting extreme weather events.
Reducing the carbon footprint of the health infrastructure portfolio is one way to mitigate the increasing temperature in the atmosphere. It is recommended to design, build, upgrade and convert engineering systems to reach the Net Zero target – the state in which the greenhouse gasses going into the atmosphere are balanced by removing them out of the atmosphere. The Net Zero achievement requires concerted government efforts, as described in the signed Paris Agreement in 2015.
There is no doubt that health care facilities in the future will be very different from the current ones: the use of robots, telehealth, 3D printers and Artificial Intelligence will likely require less space, as most of the care is provided away from them. Facilities in planning now must be designed to allow flexibility, adaptability and expandability.
South Africa requires a health service redesign to address inequality. This should provide the foundations for effective implementation of the Universal Care Coverage, requiring people-centred PHC, which focuses on treatments, prevention, community well-being, and quality of life.
The Western Cape government required a new clinic in Beaufort West, in the Karoo district, of approximately 1 000 m2. The brief for the project was for the design and construction of a green building that would make use of alternative building systems and technologies. In addition, this facility would serve as a pilot in the province for climate resilient and sustainable facilities. The provincial Department of Public Works implemented the project at a total project cost of R26 million and construction commenced in June 2015, and practi cal completion was reached in May 2017.
The building was designed to try and encourage a feeling of wellness. It took into consideration natural light, space, colour, transparency, ease of route finding, and views to the outside. Some of the features that were included in the facility include:

• Energy efficiency: The building harvests natural lighting and enhances this with colour. In addition, the facility uses rock store technology to temper hot summer air and cold winter air to achieve the clinical environment standards without air-conditioning. The system works cyclically, with hot air being drawn in over the rocks during the day, where the rocks cool the air. In the evening, the warmed-up rocks have the cold night air drawn over them, and they cool down. In addition, the dropped eave blocks of the building are done such that they block the hot summer sun but allow the low-angled winter sun to penetrate the building.
• Indoor environmental quality enhancement: The wings are accessed along glazed ‘veranda’-like walkways, which helps to merge the facility with the natural landscape of the location. Furthermore, the facility uses appropriate orientation, calculated overhangs and integrates outward views, which offer spaciousness. Moreover, the roofs reflect the vernacular origin of the adjacent houses, which is done such that they provide internal

This project was done with set community participation targets for the contractor that would ensure secondary objectives of the project were met. This was done through continuous engagements with the local community, incorporating the Expanded Public Works Programme in the building process, sourcing materials locally where possible and subcontracting some of the work to small, medium and micro enterprises in the area. Furthermore, the construction of the facility deliberately made use of labour-intensive technologies, in particular for the construction of the rammed earth external walls. Post-construction, it is clear that the facility is an improvement of previous facilities and is a positive contribution to the community.
The South African health care system faces a plethora of issues and infrastructure is but one of these. Inadequacies associated with the existing infrastructure combined with the need for more highlights how infrastructure contributes to sub-optimal health outcomes. This partially explains the expectations shortfall that patients and others experience when accessing or seeking to access the health care system. For those who can afford to pay for medical services, they can change service providers, however, those who cannot afford to, which constitutes the majority of the population due to unfavourable socio-economic conditions, have no choice but to access health services closest to them irrespective of the quality of service. This is the primary reason why UHC is proposed to transcend socio-economic lines and ensure equitable access to quality health care services. However, UHC will not be achieved in the short term and, although the NCS prescribes the benchmark for quality services, the number of facilities that comply with the benchmark is low and there are no consequences for those that do not.
The demographic and epidemiological patterns are evolving, and the health care system must respond with capacity and capability that is adequate and timely. To do this means that both symptomatic and systemic challenges must be addressed effectively and efficiently. The reforms already initiated in the sector have achieved varying degrees of success, but challenges remain. The case for more interventions is thus self-evident, over and above a need for follow-through on current reforms, including a review and improvement on these.
Catering for future health care needs requires that lessons be drawn from current developments and trends, as these will affect the way health infrastructure is provided. Already with COVID-19, we learnt that medical services may not be provided only at health facilities, but rather remotely enabled by Artificial Intelligence, information technologies, and remote-monitoring technology, amongst others. As such, the need for extensive waiting areas, medical records, and outpatient consulting and counselling rooms will abate over time. The use of robots, telehealth, and 3D printers, etc., will become prevalent, implying less space needed at health facilities as care is provided away from them. Designs must thus allow for flexibility, adaptability and expandability. With respect to climate change, the sector must reduce its carbon footprint by designing, building, upgrading and converting engineering systems to reach the Net Zero state.
Given the critical role that infrastructure plays as an enabler of quality health care service, its improvement bodes well for health care outcomes. This chapter proposes infrastructure-specific improvements, which when combined with enhancements proposed in other chapters around other inputs and the combination of these inputs in a holistic, integrated, complementary and optimal manner, mean that the health sector will be more responsive and advance towards UHC aspirations.
The government needs to maintain and strengthen its efforts to provide and maintain health care infrastructure as an enabler of quality health care. For this to happen, the following actions are recommended:
• Ensure that infrastructure plans are aligned with service improvement plans. This will ensure that the PHC platform is prioritised, given that 90% of client only need to access these facilities.
• Apply quality management and continuous improvement to provincial 10-year infrastructure plans and streamline the infrastructure delivery process by not overburdening implementation through too many reporting requirements (i.e. ‘red tape reduction’). Moreover, differentiate between managing systems and reporting systems (Pharmaceutical Management Information System and Infrastructure Reporting Model). As health care facilities are complicated buildings, use Building Information Management in the design and construction phases, as this will alleviate coordination issues among designers and extensive variations on site.
• Standardise the Service Delivery Agreements between provincial health departments and implementing agents and keep monitoring the implementation thereof.
• Update the IUSS guidelines and keep the portal as originally intended: a platform for all the stakeholders involved in health care infrastructure – i.e. standardised layouts and functional units, as is currently done by the private sector.
• Update the South African Cost Norms for providing effective management of cost versus budget. Consider the entire life-cycle cost per project and prioritise maintenance.
• Capacitate training of the state human resource capacity to deliver health care infrastructure (i.e. to have educated clients). Engage Higher Education Institutes in reviewing their curricula for ensuring alignment between the new professional and technical workforce and the health care service demand.
• Use a dual mode for delivery of infrastructure (centralised approach) where provincial health departments are supported by NDoH, National Treasury, other pockets of excellence in the sector and the private sector when planning and delivering a new hospital. However, leave to provinces the implementation of projects related to PHC, based on standard layouts (decentralised approach).
• Use NEC term service contracts for maintenance and emergency work.
• Use the procurement method described in the Construction Industry Development Board (CIDB) Standard for Uniformity (design and construct, develop and construct, and management contractor), and disincentivise the professional fees linked to the work cost.
Council for Scientific and Industrial Research. Introduction to IUSS guidelines norms and standards. Available: https://slide player.com/slide/17463340/ Council for medical schemes. 2015. Council for medical schemes annual report 2015/16. Available: https://www.medicalschemes.co.za/publications/#20092014-wpfd-2015-16-annual-report
Dhai A. Medico-legal litigation: Balancing spiralling costs with fair compensation. 2015. [Online]. Available: https://www.ajol.info/index.php/sajbl/article/ view/120167/109651
Egbujie B, Fatti G, Grimwood A, Allie S. Impact of ‘Ideal Clinic’ implementation on patient waiting time in primary healthcare clinics in KwaZulu-Natal Province, South Africa: A before-and-after evaluation. 2018. [Online]. Available: https:// www.researchgate.net/publication/324355467
Erasmus L, Poluta M, Weeks R. Integrated assessment and management of healthcare infrastructure and technology. 2012. [Online]. Available: https://www.up.ac.za/ media/shared/Legacy/sitefiles/file/44/1026/2163/8121/innovate7/ integratedassessmentandmanagementofhealthcareinfrastructureandtechnology.pdf Health Standards. Why standards matter. 2022. [Online]. Available: https:// healthstandards.org/ standards/why-standards-matter/ Health Systems Trust. South African Health Review 2017. 2017. [Online].
Available: https://www.hst.org.za/publications/South%20African%20Health%20 Reviews/HST%20SAHR%202017%20Web%20Version.pdf Health Systems Trust. South African Health Review 2020. 2020. [Online].
Available: https://www.hst.org.za/publications/South%20African%20Health%20 Reviews/SAHR_NO_BlankPages_3_8_Artifacts_07052021.pdf
Hunter JR, Asmail S, Ravhengani NM, Chandran TM, Tucker J, Mokgalagadi Y. The Ideal Clinic in South Africa: progress and challenges in implementation. 2017. Available: https://www.hst.org.za/publications/South%20African%20Health%20 Reviews/11_The%20Ideal%20Clinic%20in%20South%20Africa_progress%20 and%20challenges%20in%20implementation.pdf
KPMG. 2016. Universal healthcare: One place, many paths. [Online]. Available: https://assets.kpmg/ content/dam/kpmg/pdf/2016/07/za-universalhealthcare-one-place-many-paths.pdf
McIntyre D, Ataguba J. Access to quality health care in South Africa: Is the health sector contributing to addressing the inequality challenge? 2017. [Online]. Available: https://www.parliament.gov.za/storage/app/media/Pages/2017/october/ High_Level_Panel/Commissioned_reports_for_triple_challenges_of_poverty_ unemployment_and_inequality/Diagnostic_Report_on_Access_to_Quality_ Healthcare.pdf
McLaren ZM, Ardington C, Leibbrandt M. Distance decay and persistent health care disparities in South Africa. BMC Health Serv Res. 2014 Nov 4;14:541. doi: 10.1186/s12913-014-0541-1. PMID: 25367330; PMCID: PMC4236491. Medpages. Medpages Database. 2021. [Online]. Available: https://www.medpages. info/sf/index. php?page=stats
Muthathi IS, Rispel LC. Policy context, coherence and disjuncture in the implementation of the Ideal Clinic Realisation and Maintenance programme in the Gauteng and Mpumalanga provinces of South Africa. 2020. [Online]. Available: https://health-policy-systems.biomedcentral.com /articles/10.1186/ s12961-020-00567-z
Office of Health Standards Compliance. Annual inspection report 2018/19. 2019. [Online]. Available: https://ohsc.org.za/wp-content/uploads/AnnualInspection-Report-_2018-19_Report_02-Mar-20-1.pdf
Office of Health Care Standards Compliance. Mandate. Available: https://ohsc.org. za/who-we-are/#mandate
Rensburg R. Healthcare in South Africa: how inequity is contributing to inefficiency. University of the Witwatersrand. 2011. [Online]. Available: https://www.wits. ac.za/news/latest-news/opinion/2021/2021-07/healthcare-in-south-africahow-inequity-is-contributing-to-inefficiency.html
Sanogo N, Fantaye A, Yaya S. Universal Health Coverage and facilitation of equitable access to care in Africa. 2019. [Online]. Available: https://www.frontiersin.org/ articles/10.3389/fpubh. 2019.00102/full
Shohan M, Rubayet Ul, Alam ASM, Rakhi N, Kabir M. Onset, transmission, impact, and management of COVID-19 epidemic at early stage in SAARC countries. 2020. [Online]. Available: https:// www.researchgate.net/publication/343734542
South Africa. Auditor-General. Second special report on the financial management of government’s COVID-19 initiatives. 2020. Available: https://www.agsa.co.za/ Portals/0/Reports/Special%20Reports/Covid-19%20Special%20report/ Second%20special%20report%20on%20financial%20management%20of%20 government’s%20Covid19%20inititatives%20-%20FINAL%20PDF%20 (interactive).pdf
South Africa. Department of Health. Towards quality care for patients. National Core Standards for health establishments in South Africa. 2011. Available: https://static. pmg.org.za/docs/120215 health0.pdf
South Africa. Department of Health. National policy on management of patient waiting time in outpatient departments. 2015. [Online]. Available: https:// www.knowledgehub.org.za/system/files/elibdownloads/2019-07/Patient%2520 Waiting%2520time%2520Policy%252014%2520November %25202016%2520PDF.pdf
South Africa. Department of Health. 2015 Draft 10-Year Health Infrastructure Plan. 2015.
South Africa. National Treasury. Provincial budgets and expenditure review 2015/16 – 2022/23. 2021. [Online]. Available: http://www.treasury.gov.za/publications/ igfr/2021/prov/Chapter%204%20-% 20Health.pdf
South Africa. Special Investigating Unit. 2021. Investigation into the procurement of, or contracting for goods, works and services, including the construction, refurbishment, leasing, occupation and use of immovable property, during or in respect of the National State of Disaster. Available: https://www.siu.org.za/wp-content/ uploads/2021/02/R23_of_2020_Final_report_on_matters_finalised_for_public_ release_05022021.pdf
South Africa. Statistics South Africa. 2016 General Household Survey (P0318). 2017. Available: http://www.statssa.gov.za/ publications/P0318/P03182020.pdf
South Africa. Statistics South Africa. 2018 General Household Survey (P0318). 2019. Available: https: //www.statssa.gov.za/publications/P0318/P03182018.pdf
South Africa. Statistics South Africa. Annual quarterly and regional fourth quarter report 2018 (P0441). 2019. Available: http://www.statssa.gov.za/publications/ P0441/P04414thQuarter2018.pdf
South Africa. Statistics South Africa. Quarterly labour force survey quarter 4: 2019. 2020. Available: https://www.statssa. gov.za/publications/P0211/P02114th Quarter2019.pdf
South Africa. Statistics South Africa. Mid-year population estimates 2020. 2021. Available: http:// www.statssa.gov.za/publications/P0302/ P03022020.pdf
South Africa. Parliament of the Republic of South Africa. National Health Amended Act of 2013. 2013. Available: https://ohsc.org.za/wp-content/uploads/2017/09/ NationalHealthAmendmentAct12of 2013.pdf.
South Africa. Parliament of the Republic of South Africa. National Health Act of 2003: Norms and standards regulations applicable to different categories of health establishments. 2018. Available: https://www.gov.za/sites/default/files/gcis_ document/201802/41419gon67.pdf.
South Africa. Portfolio Committee on Health. Committee calls on Office of Health Standards Compliance to suggest remedial action. 2014. Available: https://www. parliament.gov.za/news/ committee-calls-office-health-standards-compliancesuggest-remedial-action
South African Institute of Civil Engineering. SAICE 2017 infrastructure report card for South Africa. 2017. [Online]. Available https://saice.org.za/wp-content/ uploads/2017/09/SAICE-IRC-2017.pdf
United Nations. World Population Prospects. 2019. Available: https://population. un.org/wpp/Down load/Standard/CSV/
Van Dyk J. Is trust earned or given? Five COVID lessons for the NHI. Bhekisisa Centre for Health Journalism. 2020. Available: https://bhekisisa.org/health-newssouth-africa/2020-10-07-is-trust-earned-or-given-five-covid-lessons-for-the-nhi/
World Bank. The state of health in the WHO African Region: An analysis of the status of health, health services and health systems in the context of the Sustainable Development Goals. 2018. [Online]. Available: https://apps.who.int/iris/ handle/10665/275292
World Health Organization. Hospital beds (per 1,000 people). 2010. [Online]. Available: https://data. worldbank.org/indicator/SH.MED.BEDS.ZS
World Health Organization. A vision for primary health care in the 21st century towards universal health coverage and sustainable development goals. 2018. [Online]. Available: https://www.who.int/ docs/default-source/primary-health/vision.pdf
Young M. Private versus public healthcare in South Africa. Western Michigan University. 2016. [Online]. Available: https://scholarworks.wmich.edu/cgi/ viewcontent.cgi?article=3752&context= honors_theses
High-quality health systems are necessary for the achievement of Universal Health Coverage (UHC) and the United Nations Sustainable Development Goals (SDGs). UHC and the SDG goal 3, focusing on healthy lives and the promotion of well-being for all people, have renewed the impetus to address quality of care within health systems.1 In South Africa, the proposed National Health Insurance (NHI) system, which aims to improve access to quality health services for all South Africans, has renewed scrutiny of the quality of health care.2 More recently, the COVID-19 pandemic has further exposed the inequities and weaknesses in quality of care across health systems in South Africa.
Chapter 5 on ‘Improving Quality’ in the previous edition of South Africa Health Reform (2009 – 2014) reported on the development of National Core Standards (NCS), the establishment of the Office of Health Standards Compliance (OHSC) as promulgated by an Amendment to the National Health Act 2003 (NHA) in 2013, the findings of the National Baseline Health Facility Audit of 2010, the inspections of health establishments undertaken by the OHSC up to 2014, and briefly described a few quality improvement (QI) initiatives in South Africa.3
This edition of the South Africa Health Reforms reviews developments in the quality of health care in South Africa since 2015. We draw on the findings and recommendations of the 2019 South African Lancet National Commission (‘the Commission’) report, ‘Confronting the right to ethical and accountable quality health care in South Africa’, describe important developments since the publication of the report, and discuss barriers and opportunities for achieving a high-quality health system in South Africa post COVID-19.4
Lilian Dudley, Rajesh Patel, Siphiwe Mndaweni, Thulani MasilelaThe Commission defined a high-quality health system as one which ‘achieves equitable health outcomes and a long and healthy life for all’, and developed a conceptual framework for a high-quality health system, underpinned by the values of human rights, equity and social justice for South Africa. The framework described a quality health system as being responsive to the South African context, and ensuring the achievement of key impacts and outcomes through the mobilisation of appropriate inputs, and service delivery under effective leadership and governance4 (Figure 13.1).
Source: Adapted from: van Olmen et al. (2012) and South African Lancet National Commission4,5
To complement this overarching health systems’ framework, the National De partment of Health (NDoH) developed a National Quality Strategic Framework which specified the main domains of service delivery across the life-course, and the required inputs, processes, outputs, outcomes and impact to inform planning and assessment of such a quality health system. The NDoH framework also emphasised the importance of quality planning, quality control and assurance, and quality improvement, the three components of the Juran Triad6 (Figure 13.2).
Figure 13.1 Conceptual framework for a high-quality South African health system
The Commission found an enabling legal and policy environment, numerous QI initiatives, increased life expectancy and decreased mortality rates in South Africa. The report however identified significant challenges and threats, in particular: i) Gaps in ethical leadership, management and governance; ii) Poor quality of care costs lives; iii) Malpractice cases and medical litigation are threats; iv) the Human Resources for Health (HRH) crisis will undermine high-quality UHC; v) Health information system gaps, and vi) Fragmentation and limited impact of quality of care initiatives. Four overarching recommendations were to: i) Enhance governance and leadership for quality and equity; ii) Revolutionise quality of care; iii) Invest in and transform human resources in support of a quality health system; and iv) Measure, monitor and evaluate to ensure high-quality UHC.
The following sections summarise the Commission’s findings and recommendations, and review progress in moving the agenda of a high-quality health system in South Africa forward in a post COVID-19 pandemic context. Definitions of key concepts are provided below.
• Quality Control is used to determine where and when corrective action is required. It seeks to ensure that outcomes and services are of acceptable quality, free of errors and defects.
• Quality Improvement (QI) is broadly defined as a change process which should lead to better patient outcomes (health), better system performance (care) and better professional development (learning).7

• Certification is a process by which a recognised authority evaluates and recognises an individual provider, or an organisation as having met predetermined requirements.
• Accreditation is a formal process carried out by a recognised body and involves detailed and critical assessment of all aspects of a health care facility against a predetermined set of standards and criteria; and accreditation can be awarded if found to comply to a substantial degree.
The Commission’s 2019 report concluded that the country had accomplished a strong legal dispensation and policy framework for enabling the development of a high-quality health system to generate good health outcomes and has seen political commitment to these ideals.4 These include the NHA of 2003, which was amended in 2013 to create the OHSC as an independent regulator to monitor compliance with national norms and standards, promulgated by the Minister of Health in 2017, in both public and private health establishments (HEs).8 On the downside, the Commission articulated persistent impediments including gaps in ethical leadership, management and governance. The high cost of fraud and corruption to the health system was highlighted, with provincial health departments alone carrying in excess of R40 billion in contingent liabilities in medico-legal claims.9
The report highlighted findings of the Health Market Inquiry (HMI) on failures of governance of the private sector10, as well as findings on weaknesses in governance of the Health Professions Council of South Africa11, the South African Nursing Council12, and challenges in community-led governance structures. The Commission acknowledged the HRH strengths in South Africa, but noted that the sustained HRH crisis has the potential to undermine the achievement of high-quality UHC and recommended the development of a transformative HRH plan.
Enhancing governance and leadership at all levels of the health system to achieve quality and equity ranked the highest of the four overarching recommendations of the Commission. Specifically, this meant preventing fraud and corruption, strengthening community health governance structures, investing in and enhancing the capacity of the OHSC, enhancing the capacity and effectiveness of the Council for Medical Schemes (CMS) and strengthening the governance, effectiveness and efficiency of health professions councils.
The commitment to institutionalise quality health systems, characterised by effective governance and appropriate management, remains enshrined in key government policy prescripts for the period 2019–2024. The National Development Plan (NDP) 2030 prioritised access to health services and improving the quality of services.13 The Medium-Term Strategic Framework (MTSF), government’s five-year programme for ensuring implementation of the NDP 2030 linked to each electoral cycle, accentuated the need for effective governance of the health system to ensure that systematic milestones are attained towards transforming into a quality health system.14 To achieve this, the MTSF 2019–2024 includes an imperative to develop and implement a National Quality Improvement Plan (NQIP) to ensure that public health facilities meet the requirements for the OHSC certification and NHI accreditation. Very steep goals are set in the MTSF 2019–2024, including targets that 80% of public sector facilities should implement the NQIP by 2022/23, and this should improve to 100% by 2024.14
Other MTSF 2019–2024 quality-related requisites are that the health sector’s Ideal Clinic Realisation and Maintenance Programme (ICRM), which by 2018/19 had successfully transformed 1 920 Primary Health Care (PHC) facilities into Ideal Clinics, should increase to 3 467 PHC facilities by 2024.15,16 The health sector was also
required to finalise and implement the HRH Strategy 2030, and HRH Plan for 2020/21–2024/25 to enhance existing capacity to deliver quality health care, through provision of adequate numbers of appropriately skilled and competent health workers, with the right attitudes to patients. A comprehensive policy and legislative framework were also to be developed to mitigate the risks related to medical litigation in order to reduce contingent liability of medico-legal cases by 80% (under R18 billion) by 2024.9
The emphasis placed by the MTSF 2019–2024 on a quality health system is consistent with other health sector policy documents, including the NHI Policy of June 2017 and the NHI Bill 2019.2,17
Progress towards better governance of a quality health system reflects a mixed bag consisting of a modicum of successes and a larger magnitude of impediments.
The implementation of the Medico-legal Intervention project through four contracted service providers resulted in a reduction of the contingent liabilities by R32 billion through the identification of cases for forensic investigations, and deceased claimants and fraudulent cases. A Health Sector Anti-Corruption Forum (HSACF) was launched in October 2019 following the signing of the Presidential Health Compact which mandated government and social partners to work together to reform the health care system. The HSACF, comprising various stakeholders and convened by the Special Investigating Unit, successfully dealt with at least 20 allegations of serious maladministration, fraud and corruption in 2020, providing an effective model of a multisectoral collaboration to address fraud and corruption in the health sector.
As a regulatory entity, the OHSC has a legislative obligation to monitor and assess whether all HEs in South Africa are consistently implementing health norms and standards to assure patients’ health, rights and safety.8 The Health Ombud, currently located within the OHSC, also has a mandate to manage complaints related to the quality of health care from the public and media.8 The OHSC functions under the oversight of a board appointed by the Minister of Health. Ongoing governance challenges faced by the OHSC include inadequate resourcing relative to the scope of its mandate and a perception of lacking true independence from government.
The health sector produced an HRH Strategy 2030, and an HRH Plan 2020/21–2024/25 by October 2020 which was approved by the National Health Council.18 This is discussed further in Chapter 17.
The Council for Medical Schemes (CMS) as a statutory body established by the Medical Schemes Act (131 of 1998) (MSA) regulates the 78 medical schemes registered in South Africa.19 The governance of the Council is vested in a board appointed by the Minister of Health. The CMS’s report provided a constructive response to governance concerns raised by the HMI and the Commission and is summarised in Box 1.
The statutory health professional councils are responsible for licensing of health professionals against prespecified standards, thus ensuring that health workers have the required knowledge and competencies to provide quality health care.20,21 The Commission recommended that the health professionals councils fulfil their legislated mandates for HRH to support the delivery of quality health care by setting appropriate requirements for pre-service training, in-service training and continuous professional development in quality of health care and ethical behaviour for health professionals; and ensuring accountability of health professionals for unethical behaviour. The 2020 HRH strategy specified goals and objectives for improved governance of HRH, including the revitalisation of the HRH regulatory structures to enhance the education, performance and accountability of the health workforce.18 This is discussed further in Chapter 17.
The NHA 2003 provides for governance structures to be established for all public health establishments, including clinics, community health centres and hospitals, as well as for the establishment of district health councils.22,23 It was envisaged that these governance structures would contribute to monitoring the quality of health care, and ensuring transparency, accountability and responsiveness to communities. However, they remain an area of weakness in the health system, as demonstrated in a 2017 national survey which found that only 17.9% of clinic facilities had functional clinical committees.24
The MTSF 2019–2024 set goals to develop and implement an NQIP in response to the Commission’s recommendations.14 An NQIP was adopted for implementation by the NDoH in 2019.25 Implementation has however been slow, with little uptake by provinces.
The period since 2019 has thus seen a further consolidation of policy and plans which support quality health systems. However, progress towards implementation of these plans has been slow, raising concerns about the engagement with implementing stakeholders in the policy development process. Efforts to address corruption have been made though the problems persist. The responsiveness of the health profession councils remains a concern, and community participation in governance remains weak and ineffectual.
A summary of the CMS response to seven specific recommendations of the Commission4: -
1. Implementation of the provisions of the Medical Schemes Act (as amended)19
The CMS has been implementing the provisions of the MSA 131 of 1998 through its various regulatory activities, and contributed substantially to identifying legislative shortfalls in the MSA and its regulations and to the draft amendments to the MSA published in 2018, currently pending the finalisation of the NHI Bill.
The protection of member interest forms a key element of the legislated mandate of the CMS. CMS’s performance of relevant regulatory activities, reported on a monthly, quarterly and annual basis, have been relatively successful and are reported in the Annual CMS and Industry Reports.
The creation of a dedicated data and quality unit at the CMS has not been possible due to uncertainty with respect to this mandate, and a lack of resources. CMS’s funding model through member levies is a limiting factor, but ways to increase annual revenues are being explored to support the establishment of this unit.
The CMS has made progress in collecting information to measure the quality of the health services funded through the medical schemes. Currently, reporting is largely of input data on chronic diseases that are funded in the industry. The next step is to start collecting the process and output data, to provide a better perspective of the health care quality, and to look at these outputs relative to the costs in order to determine the value proposition of health care programmes and services to the scheme members. The CMS has a partnership with Health Quality Assessment (HQA), to ensure that there is one industry report on all key quality elements published annually.
The CMS has several publications that are shared with the industry on a regular basis, mainly to inform members about their benefit entitlements under the broad banner of the Prescribed Minimum Benefits (PMBs). The Annual and Industry reports illustrate the industry trends on key measures and best practice.
The CMS undertook a roadshow in 2018 and 2019 and visited all the entities that it regulates to promote compliance with the CMS’s regulatory directive. The CMS also embarked on a process to coordinate all industry efforts aimed at combatting Fraud, Waste and Abuse, resulting in (a) Industry agreements on definitions of Fraud, Waste and Abuse; (b) an Industry Charter on Fraud, Waste and Abuse, and (c) Codes of Good Practice for schemes, scheme members, service providers and regulators on Fraud, Waste and Abuse as well as the dispute resolution Tribunal.
7. NDoH ensuring that CMS governing body executes its mandate
The Minister of Health has appointed the members of the governing body, and the most recent assessment indicated that the Council was executing the mandate that they had been appointed to do.
Source: CMS feedback report on the SA Lancet Commission Recommendations, 2 April 2021
Box 1: Case Study of the Council for Medical Schemes (CMS) response to the Commission
The Commission reported high levels of preventable morbidity a nd mortality which were associated with poor quality of care in South Africa.4 Gains in immunisation coverage and the establishment of the largest antiretroviral therapy (ART) programme in the world had contributed to a substantial decline in mortality in adults, in under-fives and in pregnant women. However, around 60% of institutional maternal deaths were potentially preventable, and excess neonatal deaths were associated with health system and provider failings. Gaps in ART care quality were identified as inadequate coverage of children, and poor retention in care of all age groups. Underdiagnosis and poor control of chronic diseases such as diabetes, hypertension and mental health as a result of poor access to and quality of care, further contributed to high levels of preventable morbidity and mortality. These findings highlighted the need for a radical transformation of the approach to quality of health care in South Africa.
A critical step was the establishment of the OHSC and its norms and standards, to serve as a national quality control system by monitoring compliance and patient safety at health establishments. The OHSC had, however, conducted a limited number of inspections of public health establishments and none of private health establishments. Findings of these inspections reflected poor performance scores for quality of care at public health facilities across all provinces (OHSC 2014/15 – 2016/17). The Commission identified a compelling need to capacitate the OHSC to allow expansion of inspections in both the public and private sector.4
The Commission also recognised the gains made by the Operation Phakisa ICRM Programme established in 2014 to address deficiencies in the quality of PHC services as described in Chapter 4. This QA programme facilitated monitoring and improvements in quality of care in public sector PHC facilities16, and was adapted for extension to public sector hospitals as the Ideal Hospital Realisation and Maintenance Programme (IHRM).
Several private health care groups and facilities had participated in voluntary health care facility accreditation programmes such as ISO (International Standards Organisation) and the not-for-profit Council for Health Service Accreditation of Southern Africa (COHSASA), the only ISQua (International Society for Quality in Health Care) recognised accreditor of public and private health establishments in South and Southern Africa. The Commission recognised the critical role of these quality assurance (QA) programmes in assessing quality of care against standards for certification or accreditation. The overall impact of these QA programmes on health outcomes was however not clear. An evaluation of the ICRM found significant improvements of health facility scores against the ICRM standards, but not in overall PHC quality outcome measures.26 Systematic reviews of hospital accreditation also found improvements in achieving QA standards, but limited evidence that accreditation improved broader quality or health outcomes.28,29
The Commission identified a wide range of innovative QI projects delivered by government, NGOs, academic and research institutions, the private sector, international partners and funders. These were however fragmented and had limited overall impact, failing to facilitate the implementation of QI across sectors and levels of the health system.4 The Commission recommended that a national integrated, QI Programme of Action be designed in consultation with stakeholders to mainstream QI in the health system.4
The next section reflects on efforts to revolutionise quality of care since the publication of the Commission report.
The Office of Health Standards Compliance (OHSC)
The OHSC undertakes seven key activities with an ultimate goal of improving health service outcomes, as reflected in Figure 13.3

Provinces have largely complied with the submissions of Annual Returns for HEs (Figure 13.4), which are considered alongside reports from the Early Warning System (EWS), an electronic safety and quality surveillance system implemented in public sector clinics and hospitals in 2018/2019. The EWS monitors 11 indicators where there is an immediate risk to safety and quality in HEs to facilitate a rapid response.
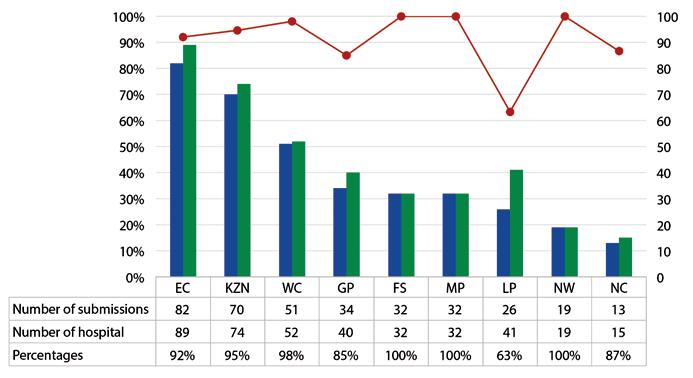
The planned incremental expansion of OHSC inspections from public sector PHC services, followed by district hospitals, referral provincial and tertiary hospitals before being extended to the private sector has however not been realised. A notable decline in the number of annual inspections undertaken by the OHSC since 2016/17 has been attributed to budgetary constraints31 (see Figure 13.5).
The HE inspection findings revealed low levels of compliance with the norms and standards, with less than 20% of HEs meeting compliance levels.32 Leadership and governance, patient safety and security counted amongst the lowest in performance.32,33 To date, no certificates of compliance have been issued, nor any enforcement actions undertaken, but Compliance Notices have been issued.
The NHI Bill (No. 42598 of 26 July 2019) requires HEs to provide proof of certification by the OHSC to be accredited with the proposed NHI fund, placing further pressure on the OHSC to increase the inspections coverage of public and private health establishments.2 The OHSC currently works on a four-year cycle for inspections and certification, and will therefore have to scale up to approximately 10 000 inspections a year to cover the estimated total of 40 000 HEs within such a four-year cycle. With its current capacity and inspection processes, the OHSC is unlikely to meet this demand for inspections, and drastic changes are needed to its inspection and funding models to achieve its regulatory mandate.
Despite reservations about its independence, prominent investigations by the Health Ombud, in particular the Life Esidimeni investigation into the circumstances surrounding the death of mentally ill patients in Gauteng province, have illustrated the importance of this office in responding to serious failures in quality of care.34
By 2020, a total of 3 368 out of 3 481 (97%) of PHC facilities had conducted ‘status determinations’ using the web-based Ideal Clinic dashboard of 208 elements organised in 10 components, and 1 535 out of 3 481 (44%) of PHC facilities achieved Ideal Status, ranging from 15% in the Northern Cape and 21% in the Eastern Cape to 75% in KwaZulu-Natal and 82% in Gauteng.35 Urban provinces performed better than their more rural counterparts, reflecting ongoing inequities in the quality of PHC across the country. Status determinations using adapted ICRM tools had also been conducted in more than 70% of public sector district, regional, tertiary and specialised hospitals by 2020.
Early lessons from the ICRM included that: i) the worst performing facilities had extensive infrastructure, staff and supply-chain management problems, ii) the absence of a clinic manager correlated with poorer performance, and iii) peer reviews functioned well as learning opportunities.36 Responses included the development of a ‘blueprint’ for PHC facility infrastructure to guide the refurbishment of or building of new PHC facilities; the use of national Workload Indicators of Staffing Needs (WISN) and PHC staff normative guidelines to prioritise the filling of vacant posts, particularly clinic managers; and the establishment of a national supply chain management forum.36
The NQIP, adopted at a Presidential Health Summit in December 2018, set a five-year goal to prepare health facilities for OHSC certification and NHI accreditation.25 A key element of this plan was the establishment of four Quality Learning Centres (QLCs) in each province as focal points of learning and capacity development in QA and QI. Each QLC would include a regional, district and private hospital, three PHC facilities, family practitioners, and emergency medical services to facilitate shared learning across multidisciplinary teams. By 2021 a total of 16 QLCs had been identified, consisting of 80 hospitals and 64 PHC facilities, a fraction (1.85%) of the 3 467 public PHC facilities in South Africa.
The slow uptake of the NQIP could be partially attributed to the COVID-19 pandemic. However, it was also critiqued as ‘vague’, out of sync with QI principles and approaches, and failing to clarify how it addresses gaps in, strengthens or complements the ICRM programme.37 The NQIP may have benefited from broader stakeholder engagement, particularly from frontline health care providers and QI experts and practitioners.
Most QI initiatives have focused on priority diseases and programmes such as Maternal and Child Health (MCH), HIV and tuberculosis (TB), and have been developed and implemented with external partners such as the Institute for Health Improvement (IHI), CDC and USAID and external funders. A range of QI approaches including the IHI Improvement model and Quality improvement collaboratives, Lean Management, Six sigma, and Kaizen have been applied across projects. One such MCH QI project, the Mphatlalatsane (‘the first star before dawn’ in Setswana) Project, has provided important lessons for applying QI in South Africa, and is described in a case study below.
In 2018 the NDoH, with the Clinton Health Access Initiative (CHAI) and other partners, launched the Mphatlalatsane Project for Quality Improvement in Sexual, Reproductive, Maternal and Neonatal Health to improve the quality of health care to reduce maternal and neonatal mortality by 50% by 2022.
The project used the IHI Model for Improvement (MFI)38 following three steps of i) setting project aims for improvement; ii) selecting measures to determine if improvement occurs; and iii) testing if self-identified strategies change the existing process and result in changes in outcomes39. QI advisors support local QI teams across the three steps, and continuous improvement is effected through Deming’s Plan-Do-Study-Act (PDSA) cycle40 (see Figure 13.6).

PDSA Model for Improvement
Each change idea is tested on a small scale at facility level, and then iteratively over a few weeks by increasing the scale and reach until significant change is evident in the data. Run charts are used as a tool to monitor progress and measure change. We describe one of the case studies below.
Case Study: Hospital – Labour and Delivery: Triaging of labour ward patients in Themba Hospital in the Ehlanzeni District
Themba Hospital, a regional hospital which performs a large number of monthly deliveries (N=675), reported an increase in the number of birth asphyxia cases, contributing to acute complications and morbidity in infants.42 A root cause analysis suggested that pregnant women in Themba Hospital were only seen when already in advanced labour. The hospital had no standard triaging system nor any triaging space. Labour complications were not addressed in time because of poor monitoring during the first stage of labour. The aim was to triage 80% of pregnant women admitted to the labour ward from a baseline of 0%.
Intervention: A triage stamp was designed, and an admission midwife or doctor assigned to the admission room daily to manage the triaging process. One bed in the admission room was allocated for triaging. The admission register was redesigned to indicate arrival, triage, and admission time to assess progress and to check if the changes implemented were effective.
Results: Triaging improved from 0% to 90% until March 2020 when a COVID-19 pandemic hard lockdown was introduced (see Figure 13.7).
Figure 13.7 Themba hospital percentage of patients triaged within 10 minutes of arrival within the maternity admission room (Source: CHAI South Africa Team: Degratia Masenya, Azukile Nzuzo, Sunette Pienaar, Daniel Nhemachena and Yogan Pillay, 2021)
There was a noted reduction in birth asphyxia cases between July and September 2019 (N=14) and the same period in 2020 (N=3). The decline in triaging from March 2020 (69%) was attributed to COVID-19 and the resultant staff shortages and increased workload.
Lessons learned: The following lessons were identified from the case studies:
• Stakeholder engagement, including clinicians at the forefront of patient care as well as patients, is important in QI project implementation and sustainability.39
• A multidisciplinary team approach assists in facilitating change.43 QI projects are collaborative by design, and involving health care workers at all levels contributes to successful implementation.
• ‘Participative innovation’ can be stimulated by creating enabling environments, providing safe spaces, increasing responsibility and acknowledging the efforts of all team members to improve motivation.44
• Staff need competency in clinical skills to implement QI projects.45
• The leadership of senior management is key for the progress and sustainability of QI projects.46
• Reliable data is important to accurately assess performance, to identify problems and to measure progress. QI projects also create an opportunity to improve the quality of data.
The case studies demonstrated the viability of the MFI in maternity and neonatal care at different levels of care. Facilities should consider QI as an integral approach to service delivery rather than as an add-on activity.
eHealth, defined as the use of Information and Communication Technology (ICT) in health care, includes the use of mobile phone technology (mHealth), computer information systems for data management systems or as clinical decision support systems, and telemedicine or remote care.
An important example is MomConnect, a national digital health initiative which reached 1.5 million pregnant women by 2017, one of the largest mHealth deployments as a proportion of target population in the world47; see also the coverage of this in Chapter 5 on National Health Programmes. Its three main features are: 1) registration of women who are pregnant into a national pregnancy registry, (2) weekly informative text messages, and (3) an interactive help desk for pregnant women and mothers of infants using the public sector. Virtually all (95%) public sector clinics have MomConnect in place, and registrations as a percentage of all antenatal clinic first visit attendees was 64% in 2017.47 User acceptability was very good, with women expressing confidence in the messages received, reporting improved health behaviours and excitement about their role.48 Complaints and feedback from women highlighted health systems quality problems such as shortage of drugs and vaccines, long wait times,47 clinical abuse, and patient neglect by health care professionals.49 Services used this feedback to address quality problems, with the available evidence suggesting that MomConnect has had an overall positive effect on end-users and contributed to a national increase in antenatal clinic visits.50
The Commission reiterated the findings of the HMI on the failures of governance in the private health sector, noting that the NDoH had failed to use ‘existing legislated powers to manage the private health care market, to ensure regular reviews by law, and to hold regulators sufficiently accountable’.10 It also noted the sharp increase in insurance for private medical practitioners associated with a rise in medico-legal claims in the private sector, and reports of nursing malpractice in private hospitals.
The CMS has a mandate to advise the Minister of Health on criteria for measurement of quality and outcomes of health services provided by medical schemes, and to collect and disseminate information about private health care.19 The CMS has access to extensive claims data on private sector health care, but has provided limited analysis of quality of health care through medical schemes. The CMS’s annual reports show poor overall compliance by medical schemes with management of chronic diseases, with low rates of testing, screening and preventative interventions, e.g. aspirin in Ischaemic Heart Disease patients. The CMS also reported a rate of caesarean deliveries of 76.9% in the population covered by medical schemes, amongst the highest rates in the world, reflecting inefficient use of health care resources.52
Citing a lack of resources and capacity to fulfil its mandate to collect and disseminate information on the quality of health care in the private sector, the CMS has utilised a partnership with HQA for the purpose of reporting on quality.
HQA is a non-profit company that has been conducting annual quality of care surveys using mainly medical scheme claims paid data for the past 17 years.53 HQA membership includes 18 medical schemes, and 80% of all insured beneficiaries. HQA provides reports to its members and presents industry-level survey results at a Clinical Quality Conference annually. It provides industry-level benchmarks for each of 174, largely input and process quality indicators for chronic diseases that managed health care organisations, schemes and health care providers can use to monitor quality. This currently represents the only source of collated and analysed data on the quality of care across a wide section of the private sector. However, the data is ‘owned’ by the members, and is not accessible in the public domain for policy-makers, funders or service users.
The 2020 HQA report indicates a slow but progressive improvement in monitoring interventions for high blood pressure, accompanied by a progressive increase in hospital admissions, adjusted for age, gender and chronic disease, for stroke.
Private sector hospital groups are increasingly measuring quality of care and adopting QA and QI processes. Reports of QA and accreditation of private health establishments through COHSASA or ISO are however not available in the public domain. Examples of QI within private hospital groups include the use of IHI’s Triple Aim methodology (best patient experience, best outcomes, and cost effectiveness), and QI for reducing hospital-acquired infections through implementation of care bundles (‘Better Care Always’), hand hygiene programmes, and antimicrobial stewardship.54
The Hospital Association of South Africa (HASA), representing the private hospital sector, commissioned research on the measurement and reporting of quality of care by hospitals in South Africa. The report made recommendations to ensure a fair and effective quality measurement framework and provided a sample set of indicators for private hospitals, including measures of performance outcomes, as well as process measures.55,56
The Board of Healthcare Funders, a representative body for health care funders, developed and piloted an ‘Effective Coverage’ monitoring tool to enable medical schemes to measure the extent to which an at-risk population receives key interventions and remains free of adverse outcomes in preparation for UHC.57,60
The Commission advised that a high-quality health system requires accurate, reliable and timely health information. It found an enabling environment for health information systems (HIS) created through a longstanding commitment to measuring quality expressed in various health policy documents. However, numerous shortcomings included that HIS were only partially electronic, lacked patient-level data, and were fragmented systems incapable of reporting aggregated data across levels of care or care pathways, or across public and private sectors. The South African HIS also focussed largely on input and process measures, with insufficient reporting of outcomes and impacts. Data quality remained a concern, and utilisation of the data by health care professionals and managers was sub-optimal.4
Recommendations included defining national performance targets which measure quality outcomes; and prioritisation of a process of analysis, interpretation and feedback of key indicators. The Commission also recommended strengthening the stewardship role of the national HIS of South Africa.4
Very little has changed in the state of HIS since the publication of the Commission’s Report. Of note is that the initial separate and parallel developments of the OHSC and the IHF programmes, which contributed to an overwhelming volume of audit processes at health facilities, data collection and information systems, have since been aligned to improve efficiency and reduce the reporting burden on health facilities.26,59 Remaining challenges include the ongoing emphasis on input and process measures, with insufficient assessment of quality of care outcomes and impacts, and a lack of transparency of information, with public reporting of quality of care only occurring at an aggregate level, with limited access to the information by clients and communities served by health establishments.
The OHSC measures have not been formally applied to the private sector yet. The HQA and CMS quality of care reports at medical scheme and managed care levels remain largely limited to input and process measures for chronic diseases and are not publicly available.
Although HASA reported that private hospitals have the capacity to measure aspects of quality, and that many are, there does not seem to be any aggregated data at private hospital and clinic level. Private hospitals measure quality largely for internal processes, while some share information within and across groups, or share results at the individual hospital level with funders. The main focus has been on value for money, based largely on input, process and output measures with little assessment or reporting of outcomes of clinical care. The distinct approaches have not been designed to enable comparability across the sector.56
Within primary care in the private sector, the need to improve the quality of health care in relation to the cost of fee for service has prompted the development of a plethora of performance tools to hold providers accountable for the quality of health care delivered. However, there is no uniformity in methodology, data collection, analysis and interpretation of results, and clinicians are adjudged to be at different levels of ‘quality’ by different funders.
The South African National Lancet Commission on Health Systems Quality reported some achievements and numerous challenges to the delivery of quality health care, with clear recommendations to achieve a quality health system for South Africa. Important early gains have been made since, but several key actions have stalled.
National plans were finalised, and actions initiated to reduce and manage fraud, corruption and the cost of medical malpractice; to address the HRH crisis; to support QA and QI; and for the expansion of the ICRM programme into public sector hospitals. The OHCS and the IHF made progress in aligning information systems, and almost 50% of PHC facilities achieved Ideal Clinic status. Innovative QI projects for priority health programmes provided valuable lessons from the field, and the use of ICTs created innovative ways of supporting quality of care. In the private sector, the CMS responded constructively to the Commission’s recommendations with intentions to assess and report on quality of care.
The COVID-19 pandemic contributed to delays in the implementation of plans for quality of care, in particular the HRH plan and the NQIP. The OHSC struggled to meet a mandate beyond its resource capacity using a model for inspections and certification which appeared neither efficient nor effective. Fraud and corruption continued to plague the health sector, particularly with respect to COVID-19 supplies and services. No apparent responses were forthcoming from health professions councils, nor processes to strengthen community engagement with quality of care. Although the CMS and other private health sector stakeholders demonstrated a willingness to assess and improve the quality of care, this has not translated into sector-wide plans or actions. The COVID-19 pandemic further exposed weakness in health systems quality in areas such as supply chain management, infection prevention control and occupational health. The higher excess deaths during the COVID-19 pandemic in provinces such as the Eastern Cape, Northern Cape, KwaZulu-Natal and Free State further demonstrated inequities in the quality of health care across the country.60
Looking ahead, sustained and effective governance and leadership is essential for the attainment of quality health systems in South Africa. Governance should not only focus on the development of legal and policy frameworks for improving quality, but should establish collaborative processes and strengthen management to better coordinate and support implementation across sectors and levels of the health system.61 There is an urgent need for leadership and stewardship from government, the various health regulatory bodies and private sector leadership to drive QA and QI in the public and private health sectors to achieve the desired UHC objective by 2030. The key milestones attained towards reducing medico-legal claims in 2021/22 should be sustained. It is also imperative for the health sector to rebuild, revive and strengthen structures for community participation in governance of quality of care, particularly hospital boards, clinic committees and ward health committees.
The OHSC needs to review and extensively revise its funding and operational models if it is to achieve its regulatory mandate and meet the NHI requirements. At a national level, greater emphasis should be placed on assessing fewer measures, refocusing on outcomes of quality to better assess actual performance, with less emphasis on national reporting of inputs and processes. Health districts, sub-districts and health facilities should be empowered to monitor inputs and processes which are relevant and meaningful to frontline providers to improve the quality of care. There is little evidence to date that the extensive national quality control processes are able to improve the quality of care in the absence of a strong groundswell of district and facility-based quality improvement.
Although the ICRM is being successfully expanded, frontline health managers felt excluded from the planning and not in control of quality aspects that they were held accountable for, often leading to ‘malicious’ compliance which undermined the objectives of the ICRM.62 Greater efforts are needed to involve frontline health managers in the planning and implementation of QA and QI systems, to strengthen their capacity and expand their ‘decision space’ to enable them to respond to gaps in quality.62
The lack of transparency and access to information on quality of care in both the public and private sectors, with insufficient feedback to providers and communities, is a further impediment to initiatives to improve the quality of care. Evidence shows that disclosing information to the public about hospital quality of care encourages hospitals to implement QI strategies.63 Within the private sector, reducing information asymmetry, i.e. the lack of information available to health care consumers (i.e., patients), but which applies also to institutional purchasers (e.g., medical schemes), is seen as a mechanism that advances quality through the effects of improved market functioning.56 PHC initiatives such as the Ritshidze community-led monitoring and evaluation of HIV care are also demonstrating that access to locally relevant information can support improvements in quality of care.64
In conclusion, some progress has been made to ‘revolutionise quality’, but overall implementation of the Commission’s recommendations has been limited. The proposed plan of action for improving the quality of care was not achieved through the current top-down version of an NQIP. There remains a need for an overarching national QI strategy which engages all stakeholders, including frontline health workers, civil society and the many current quality of care players who operate within separate health programmes or sectors. Such a strategy should build on the extensive experience and expertise in QA and QI in South Africa to support efforts to improve the quality of care across sectors and levels of care. More transparency and communication of the state of quality of care in the public and private sectors can contribute to stimulating QI initiatives. Finally, failures in governance and leadership by key partners need to be addressed.
1. Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health. Elsevier Ltd; 2018;6: e1196–252.
2. Government Gazette SA. National Health Insurance Bill [Internet]. 2018. Available from: www.gpwonline.co.za
3. Matsoso MP, Fryatt RJ, Andrews G. The South African health reforms, 2009-2014: moving towards universal coverage. 2015. 302 p.
4. National Department of Health. South African Lancet National Commission. Confronting the right to ethical and accountable quality health care in South Africa. Pretoria; 2019.
5. Olmen J van, Criel B, Bhojani U, Marchal B, Belle S van, Chenge MF, et al. The Health System Dynamics Framework: The introduction of an analytical model for health system analysis and its application to two case-studies. Health, Culture and Society. 2012 Mar 23;2(1):1–21.
6. Begg K, Andrews G, Mamdoo P, Engelbrecht J, Dudley L, Lebese L. Development of a national strategic framework for a high-quality health system in South Africa. South African Health Review. 2018.
7. Batalden PB, Davidoff F. What is ‘quality improvement’ and how can it transform healthcare? Quality and Safety in Health Care [Internet]. 2007 Feb 1;16(1):2 LP –3. Available from: http://qualitysafety.bmj.com/content/16/1/2.abstract
8. Government Gazette no. 36702 R of SA. National Health Amendment Act, 2013. 2013.
9. South African Law Reform Commission. Issue Paper 33, Project 141 Medico-Legal Claims [Internet]. 2017. Available from: http://salawreform.justice.gov.za
10. Competition Commission SA. Health Market Inquiry: Provisional Findings and Recommendations Report. 2018.
11. Mayosi BM, Adam M, Maserumule M, Matlala N, Mgijima R, Mtukushe L. Report of the ministerial task team (MTT) to investigate allegations of administrative irregularities, mismanagement and poor governance at the Health Professionals Council of South Africa (HPCSA): a case of multi-system failure. Pretoria; 2015.
12. Rispel L, Bruce J. A Profession in Peril? Revitalising nursing in South Africa. Padarath A, English R, editors. South African Health Review. 2015;115–26.
13. Government of South Africa. National Development Plan – 2030, Chapter 10, Promoting health. 2013.
14. Department of Planning Monitoring and Evaluation (DPME). Medium Term Strategic Framework 2019–2024. 2018.
15. Department of Health. Annual Report 2018/19.
16. Department of Health SA. Ideal Clinic Framework: Definitions, Components and Checklists. 2020.
17. National Department of Health South Africa. National Health Insurance Policy. 2017.
18. National Department of Health SA. 2030 Human Resources for Health Strategy: Investing in the health workforce for Universal Health Coverage. 2019.
19.The Republic of South Africa. Medical Schemes Act NO. 131 of 1998. 1998.
20. Government Gazette SA. Health Professions Amendment Act. 2008.
21. Republic of South Africa. Nursing Act 2005, Regulations regarding the scope of practice for nurses and midwives [Internet]. 2020. Available from: www.gpwonline.co.za
22. National Health Act [No. 61 of 2003], Republic of South Africa. Government Gazette. 2004.
23. Government Gazette RSA. National Health Act, no. 61 of 2003. 2004.
24. Health Systems Trust. Assessing patient experiences of care in primary health care facilities in South Africa. Durban; 2017.
25. Draft National Quality Improvement Plan. 2018.
26. Department of Health. Ideal Hospital Realisation and Maintenance Framework Manual Version One. 2018.
27. Stacey N, Mirelman A, Kreif N, Suhrcke M, Hofman K, Edoka I. Facility standards and the quality of public sector primary care: Evidence from South Africa’s ‘Ideal Clinics’ program. Health Economics (United Kingdom). 2021 Jul 1;30(7): 1543–58.
28. Brubakk K, Vist GE, Bukholm G, Barach P, Tjomsland O. A systematic review of hospital accreditation: The challenges of measuring complex intervention effects. BMC Health Services Research [Internet]. 2015;15(1). Available from: http:// dx.doi.org/10.1186/s12913-015-0933-x
29. Araujo CAS, Siqueira MM, Malik AM. Hospital accreditation impact on healthcare quality dimensions: A systematic review. International Journal for Quality in Health Care. Oxford University Press; 2020;32: 531–44.
30. Department of Health SA. National Quality Improvement Guide. 2012.
31. Office of Health Standards Compliance. Annual Report 2019/20. 2021.
32. Office of Health Standards Compliance. Annual Inspection Report 2018/19. 2020.
33. Office of Health Standards Compliance. Annual Report 2017/18. 2018.
34. Office of the Health Ombud. The report into the circumstances surrounding the deaths of mentally ill patients: Gauteng Province, No guns: 94+ Silent deaths and still counting. Pretoria; 2017.
35. Department of Health. Ideal Clinic Dashboard. https:// www.idealhealthfacility.org.za. 2020.
36. Hunter J, Thoovakkunon M, Asmall S, Tucker JM, Ravhengani N, Mokgalagadi Y. The Ideal Clinic in South Africa: progress and challenges in implementation. South African Health Review [Internet]. 2017;111–24. Available from: http://www.hst. org.za/publications/South African Health Reviews/11_The Ideal Clinic in South Africa_progress and challenges in implementation.pdf
37. Deochand E. Vote4Health: Is the National Quality Improvement Plan for health good enough? Spotlight. 2019 Mar.
38. Crowl A, Sharma A, Sorge L, Sorensen T. Accelerating quality improvement within your organisation: Applying the Model for Improvement. Journal of the American Pharmacists Association. 2015;55(4):364–76.
39. Silver SA, Harel Z, McQuillan R, Weizman AV., Thomas A, Chertow GM, et al. How to begin a quality improvement project. Clinical Journal of the American Society of Nephrology. 2016;11(5):893–900.
40. In the beginning, there were Deming and Juran. The Journal for Quality and Participation. 1999;22(6):59–61.
41. Creswell JW. Research design: Qualitative, quantitative and mixed methods approaches. 2014. 398 p.
42. Workineh Y, Semachew A, Ayalew E, Animaw W, Tirfie M, Birhanu M. Prevalence of perinatal asphyxia in East and Central Africa: systematic review and meta-analysis. Heliyon. 2020;6(4).
43. Robinson TE, Janssen A, Harnett P, Museth KE, Provan PJ, Hills DJ, et al. Embedding continuous quality improvement processes in multidisciplinary teams in cancer care: Exploring the boundaries between quality and implementation science. Australian Health Review. 2017;41(3):291–6.
44. Heath CB, Clark EC, Howard J. 10 Ways To Keep Your Quality Improvement Team Motivated. Family Practice Management. 2018;25(5):23–6.
45. Staines A, Amalberti R, Berwick DM, Braithwaite J, Lachman P, Vincent CA. COVID-19: patient safety and quality improvement skills to deploy during the surge. Int J Qual Health Care. 2021;33(1):1–3.
46. Twum-Danso NAY, Akanlu GB, Osafo E, Sodzi-Tettey S, Boadu RO, Atinbire S, et al. A nationwide quality improvement project to accelerate Ghana’s progress toward millennium development goal four: Design and implementation progress. International Journal for Quality in Health Care. 2012;24(6):601–11.
47. Barron P, Peter J, LeFevre AE, Sebidi J, Bekker M, Allen R, et al. Mobile health messaging service and helpdesk for South African mothers (MomConnect): History, successes and challenges. BMJ Global Health. 2018;3.
48. Skinner D, Delobelle P, Pappin M, Pieterse D, Esterhuizen TM, Barron P, et al. User assessments and the use of information from MomConnect, a mobile phone text-based information service, by pregnant women and new mothers in South Africa. BMJ Global Health. 2018;3.
49. Engelhard M, Copley C, Watson J, Pillay Y, Barron P, LeFevre AE. Optimising mHealth helpdesk responsiveness in South Africa: Towards automated message triage. BMJ Global Health. 2018;3.
50. LeFevre AE, Dane P, Copley CJ, Pienaar C, Parsons AN, Engelhard M, et al. Unpacking the performance of a mobile health information messaging program for mothers (MomConnect) in South Africa: Evidence on program reach and messaging exposure. BMJ Global Health. 2018;3.
51. Heekes A, Tiffin N, Dane P, Mutemaringa T, Smith M, Zinyakatira N, et al. Self-enrolment antenatal health promotion data as an adjunct to maternal clinical information systems in the Western Cape Province of South Africa. BMJ Global Health. 2018;3.
52. Council for Medical Schemes. Annual Report 2019/20: For the benefit of the member [Internet]. 2020. Available from: www.medicalschemes.co.za
53. Health Quality Assessment (HQA). https://www.hqa.co.za.
54. Richards GA, Brink AJ, Messina AP, Feldman C, Swart K, van den Bergh D. Stepwise introduction of the Best Care Always central-line-associated bloodstream infection prevention bundle in a network of South African hospitals. Journal of Hospital Infection [Internet]. 2017 Sep 1;97(1):86–92. Available from: http:// dx.doi.org/10.1016/j.jhin.2017.05.013
55. Hospital Association of South Africa (HASA). https://hasa.co.za.
56. Carvounes A, Childs B, Dreyer K, Kantor G, Ranchod S. Quality measurement and reporting in the South African private hospital industry. 2017.
57. Board of Healthcare Funders (BHF). https://www.bhfglobal.com.
58. Ng M, Fullman N, Dieleman JL, Flaxman AD, Murray CJL, Lim SS. Effective Coverage: A Metric for Monitoring Universal Health Coverage. PLoS Medicine. Vol. 11. Public Library of Science; 2014.
59. Office of Health Standards Compliance. Annual Performance Plan 2021/22. 2021.
60. Bradshaw D, Laubscher R, Dorrington R, Groenewald P, Moultrie T. Report on weekly death rates in South Africa. 2021 Nov.
61. Emerson K, Nabatchi T, Balogh S. An integrative framework for collaborative governance. Journal of Public Administration Research and Theory. 2012 Jan;22(1):1–29.
62. Muthathi IS, Levin J, Rispel LC. Decision space and participation of primary healthcare facility managers in the Ideal Clinic Realisation and Maintenance programme in two South African provinces. Health Policy and Planning. 2020 Apr 1;35(3):302–12.
63. Herrera C, Lewin S, Paulsen E, Ciapponi A, Opiyo N, Pantoja T, et al. Governance arrangements for health systems in low-income countries : an overview of systematic reviews. Cochrane Database of Systematic Reviews. 2017;(9).
64. Ritshidze ‘Saving our Lives’. Community-led clinic monitoring in South Africa.
Law plays an outsized role in South African health advocacy. This is despite some misgivings about the utility of law and policy in meeting the constitutional imperative to ensure that ‘everyone has a right of access to health care services’. In this chapter we consider the reason for the focus on law and the right to health care services as a determinant of health, and the development of law and policy in the past five years (both through legislation and legal advocacy). We go on to reflect on one of the biggest potential legal interventions to realise the right to health – National Health Insurance (NHI) – and how the experience under COVID-19 has demonstrated both the need for health financing and systems reform, and lessons for NHI.
An often-repeated lament in South Africa is that we have good law and policy but fail on implementation. The implication is that it does not really matter what the law says if it does not result in the realisation of rights. Why, then, write a book chapter on the legislative framework and the right to health?
Yamin describes health as ‘perhaps the most radical of subjects for human rights because, more than any other topic, it challenges the boundaries of what is “natural”. There can be no right to be healthy… [b]ut much of population health is indeed subject to social control through laws, policies, and programmes that influence exposures and mitigate effects…’1
LEGISLATIVE FRAMEWORK AND THE RIGHT TO HEALTH 2015–2020
Law in itself cannot realise the right to health. However, without it we lack the framework for rights realisation. Law can also negatively impact the social determinants of health, and result in discrimination in access and treatment. The report of the Lancet Commission on the Legal Determinants of Health states:
‘By establishing the rules and frameworks that shape social and economic interactions, laws exert a powerful force on all the social determinants of health. Well-designed laws can help build strong health systems, ensure safe and nutritious foods, evaluate and approve safe and effective drugs and vaccines, create healthier and safer workplaces, and improve the built and natural environments’.2
In other words, ‘law can turn vision into action’,3 whether that is through requiring universal access to health care services, or setting standards for the registration of medicine or the quality of services or training. It can strengthen governance of health institutions and decision-making structures.4 It can also create the space for civil society to hold state and non-state actors accountable for realisation of health rights.5
Thus, while good laws alone do not equate to the realisation of the right to health, they are, globally and in South Africa, an important framework for the development of a health system that is capable of realising the right.
Health law and the right to health care services is thus a site and a tool of, and not a substitute for struggle.6
Law has particular importance in health advocacy in South Africa. Activists use the constitutional right of access to health care services, together with supporting rights, as the basis for claims.
One of the ways to use the law for the realisation of rights is through litigation. Yamin notes that ‘the propriety of judicial intervention is at least to some degree inherently related to how one assesses the capacity of the political branches of government to maintain health systems that respond rationally to the population’s needs’.7 Perhaps due in part to the failure of political branches to maintain a responsive health system, litigation on the right to health in South Africa, while not as common in comparison to some other rights or as frequent as in some other countries, continues to be used as a tool to secure realisation of the right. Reflecting on the utility of right to health litigation, Yamin notes further ‘the overall evidence suggests that health rights litigation is neither a dangerously infectious trend to be urgently contained nor a panacea for health inequity’.8 Courts can facilitate and prompt democratic deliberation by bringing neglected voices into public fora, unblock channels for problem-solving and reorganise the structural dimensions of social problems.9
The most famous example of the use of law in health advocacy in South Africa is the campaign for access to antiretrovirals (ARVs) to prevent mother to child transmission of HIV. HIV prevalence among pregnant women attending antenatal clinics grew from 7.6% in 1994 to 30.2% in 2005.10 In the absence of treatment, an estimated one-fifth to one-third of children born to mothers living with HIV would have contracted the virus, but the chance of transmission would be halved through the use of nevirapine.11 The Treatment Action Campaign (TAC), a social movement comprised mostly of people living with HIV, initiated a campaign of rights awareness and treatment literacy, advocacy, mobilisation and litigation to secure access to such treatment. Educating people about HIV, its treatment, and the right to access health care services, including treatment, was the foundation of the struggle, and skilful litigation together with out of court legal and other advocacy won an ARV roll-out that became the world’s biggest
ARV programme.12 The movement around and prompting the litigation emboldened affected people to understand their claims as underpinned by demands for justice rather than charity.13
Almost 20 years later, health advocacy in South Africa continues to draw on legal claims and uses a combination of research, education, mobilisation, assistance to government and litigation to secure the realisation of health rights.
While health advocacy (from civil society, academia and others) and progressive government policy and implementation has improved access to health care services, huge problems remain. Access to services and the quality of services that a person receives depend largely on socio-economic status, geography, race, gender and other factors that should not be determinative of whether one has access to life-saving or enhancing care. The inequality of funding between public and private health services is well known. Access to services between provinces and between urban and rural areas varies significantly. Furthermore, medication out of stock14 or health worker objection to the provision of health services such as termination of pregnancy15 means that access to the treatment or service required can be secure in a health facility one day and absent the next.
The right to health is not merely a principle. It can be applied in an operational, systematic and sustained manner,16 which is how both international and South African law require it to be.
The right to health care services has a constitutional basis in South Africa, with the Constitution providing that ‘Everyone has a right of access to health care services in cluding reproductive health care’ and requiring that the state must take ‘reasonable legislative and other measures within its available resources’ to progressively realise that right.17 Children are guaranteed a further right to ‘basic health care services’ which is immediately realisable and is not subject to progressive realisation or available resources.18
The constitutional right has been interpreted by the courts to include the provision of antiretroviral therapy to pregnant women19 and to people in prison20 , and the right to access to affordable medicines.21
The Constitution recognises rights to be indivisible, interrelated and mutually supporting, which means that it is necessary to achieve the realisation of some rights in order to fully enjoy other rights. For example, without realisation of everyone’s rights to health care services, basic education, food and water, the rights of some to dignity and equality are infringed.22 The National School Nutrition Programme, which feeds around 9.3 million learners every day in South Africa is intended both to ensure the realisation of the right to basic nutrition and children’s rights to basic education, recognising that one cannot learn on an empty stomach.23 In short, the right to health is not fully realisable unless other rights are realised.
South Africa is also a signatory to several international covenants including the International Covenant for Economic, Social and Cultural Rights (ICESCR)24 which it signed in 1994 but only ratified in 2015. The ICESCR provides for the right of everyone to the ‘enjoyment of the highest attainable standard of physical and mental health’ and requires states to take steps for its realisation. Additionally, the Committee on Economic, Social and Cultural Rights’ General Comment 1425
recognises that health is more than just access to health care, but is determined by a range of social factors such as access to decent housing, safe water, adequate sanitation, nutritious food, education, health-generating employment and numerous other factors. Most of these factors are also rights contained in our Bill of Rights in Sections 26, 27 and 29, amongst others.
The legal status of health rights in South Africa is therefore clear. The question then is what they mean or how the right to health care services can be made ‘operational’?
The right to the highest attainable standard of health is an individual and a community right and has, at its core, a health system that is responsive to needs and accessible to all.26 It is in furtherance of this element of the right to access health care services that health rights litigation in South Africa, unlike in other countries, has been pursued to develop the health system in a way that enables the realisation of rights rather than purely to meet individual needs.27
The right to health requires that we adopt an understanding of the health system as a core social institution.28 Hunt and Backman compare an effective health system to a fair justice system.
‘The right to a fair trial is widely recognised to have strengthened many court systems. It has helped to identify the key features of a fair court system [such as independent judges, legal aid and trials without undue delay]. In much the same way, the right to the highest attainable standard of health can help to establish effective, integrated, and accessible health systems’.29
A focus on realising the right to health therefore strengthens health systems, ensuring health coverage that is truly universal and meets the needs of people.30
A right to health approach to strengthening health systems requires the application of human rights principles to each of the World Health Organization’s health system ‘building blocks’. These building blocks are services; workforce; information systems; medical products, vaccines and technologies; financing; and leadership, governance and stewardship.31
The building blocks should themselves be built using the right to health principles of transparency, participation, a focus on process along with outcomes and on the underlying determinants of health as well as medical care. Incorporating right to health principles requiring the centring of the well-being of individuals, communities and populations, equity and non-discrimination, and respect for cultural difference into the building blocks creates a health system that caters to the needs of the country. The right to health principles of quality and progressive realisation (which includes a plan for improvement with benchmarks and monitoring and evaluation) ensure improvement within the building blocks. Finally, recognising health as a public good and as a right informs and serves as a foundation for the health system building blocks.32
If law can be used to build a health system that realises and protects human rights, has law developed and been used in the period between 2015 and 2020 to do just that?
The health system in South Africa is governed by the National Health Act 61 of 2003 (NHA), which was enacted in furtherance of the state’s obligations under section 27 of the Constitution to take reasonable legislative and others measures to realise the right of access to health care services. The NHA sets out the structure of the health system, laying out the powers and responsibilities of national, provincial and local spheres of
The legal framework and how it has changed between 2015 and 2020
government, and providing for both public and private components to the system. The NHA creates a framework for the delivery of health care services and provides for the rights and duties of health care personnel, governance of health facilities, the quality of health care services, and human resource planning, among others.
The NHA includes a provision for the Minister to make regulations on a range of issues, and other pieces of legislation and policy deal with particular aspects of the health system and health law.
Between 2015 and 2020, while only one Act within the purview of the Minister of Health has been passed (although this Act is not yet in effect), there have been some significant enacted and proposed changes in the legal framework for health and health-related matters. Here we review some of these changes, before considering the impact of litigation, legal advocacy and other legal processes in this period.
The National Public Health Institute of South Africa Act 1 of 2020, not yet in force, was the only Bill introduced to the legislature by the Minister of Health in this period that has been signed into law.
The Act provides for the establishment of the National Public Health Institute of South Africa (NAPHISA), which is intended to coordinate and conduct disease and injury surveillance, and to provide for specialised public health services, interventions, training and research on the major health challenges in the country. It is expected that NAPHISA will fill an important gap in the public health landscape in South Africa. While there are some excellent surveillance systems in the country, they are managed by different institutions and there is no coordination or integration. This means that the data that should inform health policy is fragmented.33 NAPHISA is intended to change this; to become South Africa’s version of the Centre for Disease Control in the United States. NAPHISA will include divisions dealing with communicable and non-communicable diseases, occupational health, cancer surveillance, injury and violence prevention, and environmental health.
When it is established, NAPHISA should contribute to the realisation of the right of access to health care services through the creation of an evidence base for health rights-protective policy. Until such time, South Africa remains without coordinated surveillance and research, to the detriment of rights realisation.
Many medicines and medical devices are prohibitively expensive, largely because of the intellectual property (IP) rights accorded to those who make or produce them. Intellectual property rights are the incentive currently used to encourage the development and production of these lifesaving substances and tools. However, such rights neither need to be the incentive used, nor should they trump the health rights of their users.
In the late 1990s, South Africa recognised the limitation on access to antiretroviral treatment that wide-ranging IP protection caused and amended its legal framework governing the regulation of medicines to enable access to generic medicines.
This move was strenuously opposed by the pharmaceutical industry supported by the United States government, which litigated against the South African government. Following significant public pressure led by the TAC, the matter was settled.34
Despite this early pushback against public health damaging IP protection, at present there is no substantive examination of patents in South Africa, including patents on medicines and medical devices. If the right paperwork is filed and a filing fee is paid, a patent can be granted. This results in far more poor-quality patents being granted in South Africa compared to other countries. There is also no process for an affected person to oppose the granting of a patent, either before or after it is granted. Finally, there are no criteria for patentability to ensure genuine innovation through the patent system. This allows for what is called ‘evergreening’: re-patenting essentially the same invention with small changes, such as turning a tablet into a capsule. Evergreening a patent results in a further 20-year monopoly on its production and sale.
The result of the current IP regime is the creation of monopolies on the production and sale of medicines and medical devices over long periods without certainty that there has been any or substantive innovation that requires protection.
The Intellectual Property Policy of the Republic of South Africa Phase 1 (IP Policy)35 was approved by Cabinet on 30 May 2018 and envisages a change to the IP regime in South Africa. The IP Policy is intended to be implemented in phases, with Phase 1 focusing on IP and public health and the implementation of commitments undertaken in international agreements. The IP Policy recommends IP law reform, including provision for substantive examination of patent applications, for opposition, and for criteria for patentability, among others. The IP Policy also commits to the introduction of a ‘more effective and efficient’ system to obtain compulsory licenses for medicines. Compulsory licenses ensure that medicine is more readily available by requiring the licensing of producers when a patent is granted. In so doing, the IP Policy introduces the use of flexibilities contained in the Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS).
The IP Policy is framed in terms of the Constitution and acknowledges the importance of considering the health impact of economic policy. This framing and acknowledgement, and indeed the eventual adoption of the IP Policy, was the product of sustained advocacy and activism over many years.36
Unfortunately, amendments to IP law in line with the IP Policy have not yet been made. While draft bills have been produced, nothing has yet been introduced in the legislature. This means that in practice, nothing has yet changed in the lives of people in South Africa who need medicines, but which remain unaffordable due to IP regime barriers to access. The IP Policy, while creating the promise of an improvement in the realisation of the right of access to health care services, has not delivered on this promise. Government’s inaction on this issue is somewhat in contrast to South Africa’s international diplomacy, which has seen South Africa at the forefront of global negotiations to secure a waiver of IP related to technologies needed to address COVID-19 at the World Trade Organisation.37
On 15 December 2017, 10 years after the first draft of regulations for the control of notifiable conditions was published for comment, the Minister of Health promulgated the Regulations Relating to the Surveillance and the Control of Notifiable Medical Conditions (Notifiable Conditions Regulations). A public health imperative, the Notifiable Conditions Regulations provide for the responsibilities of officials, institutions and health care providers at different levels and within different sectors of the health system to notify the relevant structures about any diagnosed case of a notifiable medical condition. The most serious notifiable medical conditions include cholera, listeriosis and respiratory disease caused by a novel respiratory pathogen such as SARS-CoV-2. There are three lists of notifiable medical conditions attached as Annexure A to the Notifiable Conditions Regulations, each of which includes a category of notifiable medical condition that must be treated in a particular way.
The Notifiable Conditions Regulations provide for the prevention and control of notifiable medical conditions through voluntary (or, where necessary, mandatory) medical examination, prophylaxis, treatment, isolation and quarantine. Mandatory medical intervention may only take place upon application to a High Court and in particular circumstances. This ensures the appropriate balance of the rights of the individual and the demands of public health.
The Notifiable Conditions Regulations were not yet in place to guide the response to the listeriosis outbreak in 2017–2018, however, the classification of SARS-CoV-2 as a category 1 notifiable medical condition meant that there was a process in place for reporting, examination and treatment of COVID-19 when it was first diagnosed in the country in March 2020.
Section 27(3) of the Constitution provides that no one may be refused emergency medical treatment. Despite this clear right that accords to everyone in South Africa, emergency medical services (EMS) have long been a weakness of the health system in many provinces.
Access to EMS in the Eastern Cape, for example, remains limited, with dire health consequences for many, particularly in the rural parts of the province.38 This has been the case for many years39 and there are no signs of improvement. Part of the problem is the poor use of the EMS budget,40 as well as the significant pressure on the overall budget.
EMS has also been a site of corruption, with as yet incomplete Special Investigations Unit investigations into EMS service provision across a range of provinces.41
On 1 December 2017, the Minister of Health promulgated the Emergency Medical Services Regulations.42 The EMS Regulations apply to public and private EMS and require licensing, minimum staffing and equipment for ambulance, and appropriate management of EMS. Existing EMS providers had until 1 December 2018 to comply with the EMS Regulations, however, it is unclear whether the EMS Regulations are currently in force.
Despite being amongst the leading causes of death, data on diabetes prevalence and treatment coverage is scant. While diabetes was included in the last two South Africa National Health and Demographic Surveys43, the manner in which the sample was constructed did not allow for extrapolation to the general population. Models suggest that between 2008 and 2017, national prevalence rates almost doubled from 5.6% to 10.6%, while treatment coverage of the same period declined from 44.4% to 35.8%.44
Excess sugar is a major cause of obesity and is a risk factor in diseases such as type 2 diabetes, hypertension and heart disease.45
In April 2018, a Health Promotion Levy on sugar-sweetened beverages was introduced. South Africa was the first country in Africa to introduce such a tax, which aims to reduce the consumption of sugar-sweetened beverages. The first four grams of sugar per 100 millilitres of liquid are free, and thereafter, a levy (currently of R0.21 per gram of sugar) is charged. The levy amounts to around 11% of the price per litre of sugar-sweetened beverage.
Research published three years after the introduction of the levy found that the levy36 coincided with large reductions in purchases of sugar-sweetened beverages, in terms of both volume and sugar quantities. This is good news for health and the health system and demonstrates a clear example of law as a determinant of health.
Other measures targeting non-communicable diseases (NCDs), particularly related to tobacco products and alcohol have failed to progress. For example, the Control of Tobacco Products and Electronic Delivery Systems Bill37 was published in the Government Gazette on 9 May 2018 for public comment and sought to bring vaping and other electronic devices delivering nicotine under the purview of tobacco product regulation. However, intensive lobbying and what has been described as an orchestrated misinformation campaign and attempt to buy media influence48 has been used by the tobacco industry to undermine the Bill, which is still to be presented to Parliament.
Similarly, two bills proposing evidence-based measures to reduce alcohol-related harm remain suspended. The Control of Marketing of Alcohol Beverages Bill,49 intended to control harmful marketing of alcohol, particularly affecting children, though approved for release for public comment in 2013, and having undergone three regulatory assessments, remains unpublished. Research has identified the key role of the alcohol industry in lobbying against the bill and its strategies for impeding its progress.50 The Department of Trade and Industry also released a Draft Liquor Amendment Bill51 in 2016 for comment, but no Bill has yet been presented to Parliament or subject to public hearings. In fact, a report52 of draft bills receiving priority attention in 2020 mentioned none of the three bills cited above.
The uneven success of legislative measures to address NCD is both a major concern for a country grappling with a massive burden of NCDs and reflective of the extent to which government struggles to keep industry influence out of the policy process where their products and profits are at stake.53
The impact of law goes beyond legislative, regulatory and policy changes. Legal advocacy and legal processes in health have also impacted health rights realisation between 2015 and 2020.
The National Mental Health Policy Framework and Strategic Plan 2013–2020 provides for the deinstitutionalisation of mental health care users where appropriate for the individual user and where community residential care facilities have been developed and capacitated to care for mental health care users. It acknowledges that, in South Africa, as elsewhere in the world, deinstitutionalisation has progressed at a rapid rate without the development of community-based alternatives, and has led to homelessness, people with mental illness in prisons, and revolving doors of care.
Despite these warnings, from March 2016, the Gauteng Department of Health moved in the region of 2 000 mental health care users out of Life Esidimeni (facilities in which some people had lived for over 20 years as a result of a contract the facilities had with government) into NGOs that were ill-equipped, ill-prepared and (for a few months) not paid to care for them. The move happened in the midst of a cold winter during which 144 people died of causes varying from cold, hunger and thirst to sepsis from bedsores.
In addition to the warnings contained in the policy itself were warnings from psychiatrists, experienced NGOs, activists, families of the mental health users and lawyers about the likely ‘devastating impact on the health and social well-being of mental health users, the health care system and members of our community’54. Two court cases, multiple protests and countless letters were ignored.
In an arbitration award, issued after 45 days of evidence and legal argument from October 2017, former Deputy Chief Justice Dikgang Moseneke described the ordeal as ‘a harrowing account of the death, torture and disappearance of utterly vulnerable mental health care users in the care of an admittedly delinquent provincial government’55
The arbitration resulted in information emerging about the decision to terminate the contract with Life Esidimeni and the implementation of that decision, the award of compensation to bereaved families and survivors, and regulations containing standards for the licensing of residential facilities catering to mental health care users.
Following the arbitration, the Gauteng Department of Health developed the Mental Health Recovery and Strengthening Plan, intended to reform mental health care provision in the province. The extent to which the plan has been implemented remains in question, with periodic reports of non-payment of NGOs and difficulties experienced by NGOs in complying with new licensing regulations, which require a very high level of care to be provided – beyond what is ordinarily expected within such facilities. Mental health services remain severely underfunded, with most of the funding concentrated at tertiary level rather than community-based care.
In November 2013, the Competition Commission initiated an inquiry into the private health sector in South Africa (the ‘Health Market Inquiry’ or ‘HMI’) to enquire into the high and rising costs of health care and whether any features in the private health care market prevent, restrict or distort competition.56 During its initial investigation, the Commission identified several features of the private health sector that could negatively impact competition and which had an impact on the determination of pricing, quality of service and health outcomes. These included information asymmetries, regulatory frameworks possibly undermining competition and monopolisation of critical areas of the market, including hospitals and medical schemes.
The HMI covered much of the private health sector, including hospitals and medical schemes, but also reviewed the regulatory frameworks, statutory bodies and the organisations representing health practitioners. The inquiry included submissions from a wide variety of stakeholders, including civil society. The focus of the civil society submissions was the framing of the HMI in terms of the right to health and the obligations that this right created for both the private health sector and government in regulating it.57
The HMI panel finalised its findings in September 2019.
In the final report, the HMI panel stated: ‘We have identified features that alone or in combination, prevent, restrict or distort competition. The market is characterised by highly concentrated funders and facilities markets, disempowered and uninformed consumers, a general absence of value-based purchasing, practitioners who are subject to little regulation and failures of accountability at many levels’.58
The panel recommended, among others, greater regulation of mergers in the sector, management of risk pooling through regulation, and the introduction of a standardised benefit option to be offered by all schemes that covered primary health care (PHC) services. The panel recommended the review of rules to promote multidisciplinary practices to give users access to improved care at lower cost.
Despite it coming at a reported cost to the fiscus of just under R200 million, the recommendations of the HMI have not been implemented. The opportunity to reduce some of the inefficiencies and inequities of the private health sectors was, therefore, not taken up.
Development of the law in ways that may expand or contract access to health care services also occurs through litigation.
Section 27(3) of the Constitution provides that no one may be refused emergency medical treatment. One of the first cases relating to the right to health care services that reached the Constitutional Court was Soobramoney v Minister of Health KwaZulu-Natal 1998 (1) SA 765 (CC). This case was partly argued on the basis of the right not to be refused emergency medical treatment, but the court found that the treatment that Mr Soobramoney was seeking (renal dialysis in the final stages of chronic renal failure) did not constitute emergency medical treatment. The court decided against Mr Soobramoney and he died without the dialysis that he needed.
In 2016, the Constitutional Court was faced with another matter concerning the right not to be refused emergency medical treatment in the form of Oppelt v Department of Health, Western Cape 2016 (1) SA 325 (CC). Mr Oppelt suffered a dislocation of vertebrae that compressed the spinal cord and interfered with blood supply, in the course of a game of rugby. The treatment required is to reduce the dislocation by stretching the spine and realigning the vertebrae. In one theory, if this treatment is applied within four hours of the injury, the chance of complete recovery is 64%. Mr Oppelt did not receive the treatment until more than 12 hours later and was paralysed from the neck down. He sought damages against the Western Cape Department of Health. Mr Oppelt was successful in the High Court, unsuccessful in the Supreme Court of Appeal, and successful in the Constitutional Court.
In considering the breach of the right of Mr Oppelt not to be refused emergency medical treatment, the majority judgment in the Constitutional Court found that ‘[p]roficient health care entails providing urgent and appropriate emergency treatment whenever a medical condition requires it’.59 In this case, the court found that the Western Cape Department of Health’s employees and their slavish adherence to a transfer protocol (that did not need to be so adhered to) was substantially short of the standard of practice that a member of the public is entitled to expect and caused the harm. The Western Cape Department of Health was ordered to pay damages to Mr Oppelt. The case has potentially far-reaching implications for access to emergency treatment and the obligations on the state.
Although not decided on the basis of the right to access health care services, physician-assisted suicide and euthanasia are contentious issues involving health professionals and have been subject to litigation in the relevant period. In 2015, Robert Stransham-Ford, who was terminally ill, applied to the Gauteng High Court for an order permitting his physician-assisted suicide or euthanasia and protecting any physician who assisted him from prosecution. Fabricius J granted the order but declined to extend the possibility of lawful physician-assisted suicide or euthanasia to other cases. This meant that it was only those assisting Stransham-Ford who would be protected by the order.60 As it happened, Stransham-Ford died shortly before Fabricius J handed down his order, although the judge was not told this. The judge gave his reasons for the order some days later, by which time he knew that Stransham-Ford had died. Even though the order related only to Standsham-Ford, Fabricius J refused to recall his order on the grounds that his judgment has broader societal implications.
On appeal, the Supreme Court of Appeal (‘SCA’) set aside the High Court order,61 both because the issue before the court had been moot at the time of the order and because it found the order wrong in law. The SCA considered the possibility of a development of the common law in relation to physician-assisted suicide, as Fabricius J had ordered (but only in relation to Stransham-Ford), but disagreed that Fabricius J had evidence or the legal argument before him to consider this. The court found that the erroneous approach to the law in the High Court rendered it impossible to consider whether any limitation of a constitutional right was reasonable and justifiable in terms of section 36 of the Constitution.
While the SCA’s decision reversed the High Court order, this is not the end of the road for physician-assisted suicide and euthanasia. Another matter has been launched by two terminally ill people (one of whom is also a palliative care specialist) seeking the decriminalisation of physician-assisted suicide and euthanasia.
Much of the litigation relating to health in the past five years has been in the form of claims for damages for medical negligence. In 2017, the South African Law Reform Commission released an Issue Paper on Medico-legal claims62 in which it laid out in some detail the problem with the explosion of medical negligence claims (in what they suggest is about poor treatment of patients, poor record keeping that makes it difficult to counter such claims, dishonest and predatory lawyers, and the impact on the health budget of ever-increasing medical negligence claims).
While it is not necessary to go into the detail of the reported cases in this period, it suffices to say that government has committed to taking various steps to curb such claims both relating to the health system (prioritising improvements in areas where claims are more prevalent and improving record keeping) and to the administrative and legal handling of such claims (through the Special Investigation Unit’s investigations into fraud and the strengthening of medico-legal units in provinces).63 Alternative means for dealing with medico-legal claims are likely to be an area of development in the coming five years.
The NHI Bill, gazetted in 2019, is a significant legislative development concerning the right to health. The Bill envisages substantial health financing shifts with the pooling of public and private resources to improve equity in health service access.
Before the parliamentary discussion on the Bill could get underway, a pandemic that required intra-governmental cooperation, transparency and good governance, solidarity and collaboration between public and private health sectors hit our shores. Along with the devastation it brought, the COVID-19 pandemic provided an opportunity to test and advance some of the tenets of NHI and the reformed health system that it is intended to bring about. The extent to which this opportunity was taken up, and lessons that it may provide for legislative and health system change, are the subject of this final section.
South Africa’s NHI first started its legislative development with a Green Paper in 2011, outlining how an NHI would provide universal health coverage and expression of the state’s obligations to realise the right to health. Subsequent iterations through two White Papers (201564 and 201765) involving substantial public consultation processes, often highly contested and challenging,66 culminated in the gazetting of the NHI Bill in 2019.
Central to the NHI is the commitment to unlock access to care for people who lack resources to purchase care, and to bring the private sector’s resources into one harmonised system for population health care – with an emphasis on equity and the constitutional entitlement to access to health care services. The NHI Bill seeks to do this through the establishment of an NHI Fund – which would become the single payer for all covered health care services – and various structures that would determine what services would be covered, who would provide them, and how much would be paid for them. The Bill therefore encompasses a change to health financing as well as broader change to how the health system would work.
In relying on the pooling of resources (financial, human and other), NHI demands social solidarity. This is a significant shift from the current system in which those who can afford to do so can pay for their health services in the well-resourced private sector while everyone in South Africa contributes through tax to an under-resourced public health sector to cater to the vast majority of people in the country. It also requires coordination between the public and private health sectors where, for the first time at scale, a centralised fund would be used to pay private health care providers to serve people who would ordinarily be served by the public health system. Finally, the NHI envisages both centralisation and decentralisation of decision-making power in that the funds would be centralised in the NHI Fund, but local-level structures would decide on prioritisation of health services to be delivered and paid for by the Fund. This too represents a change from the current system in which, in the public sector, most decisions on service provision and funding are made at the provincial level.
If ever circumstances were to arise to test these foundational principles of a future NHI, the COVID-19 pandemic was it.
An easily transmissible virus, deadly in particular to vulnerable people, required individuals to take action in their own interests and also in the interests of others. Just as South Africans were asked to undertake practices to protect others at high risk or in need (e.g. quarantine and practicing non-pharmaceutical interventions to control COVID-19 spread) or to forsake personal benefits for a greater good (e.g. restrictions on freedom of movement and recreational opportunities), so too will the NHI be an
experiment in persuading South Africans to see their own best interest lying in solidarity with others, through the cross-subsidisation at national scale of the poor by the rich and the sick by the healthy.
Hospitals potentially running out of beds in the public and private sectors called for cooperation between those sectors. COVID-19 tested the state’s ability to harmonise the operations of the private sector under national leadership, as will be required for the NHI to work.
Moreover, a scared population needed both honest and good faith national stewardship and local-level action, just as under NHI, institutional arrangements and decision-making and implementation power are intended to shift.
So how did we do, and what does it mean?
To the extent that South Africans cooperated with lockdowns, quarantine, restrictions on recreational activities and non-pharmaceutical interventions to help contribute to the control of COVID-19, we saw the effect of short-term regulations significantly slow the expansion of the pandemic. However, there was also widespread resistance to many of these measures, particularly as pandemic fatigue set in and as the impacts on livelihoods became increasingly intolerable. Regulatory and programmatic interventions to enable adherence to these measures were only partial (e.g. social security support). Low rates of mask usage in public despite high awareness and resistance from industry to lockdowns were evident, exacerbated by public anger over revelations of corruption in procurement of personal protective equipment (PPE).67 It was mainly non-state actors, operating outside of any regulatory support, such as community action networks,68 that were able to mobilise solidarity contributions at community level. Private sector actors (in collaboration with government) mobilised financial resources from business and the general public through a Solidarity Fund to enable flexibility in COVID-19 response.
Some of the solidarity deficit could have been remedied by decentralised delivery and control at the local level (as proposed under NHI), to facilitate a community-led response. State action to support communities was somewhat lacking, and there was weak utilisation of community participation structures such as health committees provided for in the National Health Act.69 Health committees and hospital boards will be essential to making NHI function in an accountable manner. A future NHI will have to achieve a better legislative solution for harnessing community-based action to address upstream determinants of health and accountability for quality care under UHC.
The COVID-19 pandemic also illustrated clearly how transparency is key to building public trust in health systems70 – both private and public – required for achieving UHC.71 The meme of an inept72 or frankly criminal state73 undermines the willingness of people to commit to a system that requires social solidarity74 and belief in a state able to deliver quality care in an equitable manner.
The failure of systems to prevent corruption during COVID-19 has raised alarm bells about the ability of our health system to secure the integrity of a future NHI that will depend on large-scale contracting and procurement.75 Both widespread PPE-procurement corruption and the Digital Vibes scandal in which R150 million of spending intended for initially NHI and then COVID-19 communications was paid to
a company with alleged links to high-level National Department of Health (NDoH) officials, including the Minister, give us reason to be concerned about the safeguards in place to prevent corruption and mismanagement of funds.
Much of the commentary on the NHI Bill has highlighted deficient governance structures, particularly as they relate to the NHI Fund. Power is concentrated in the hands of the Minister and there are insufficient checks on this power, given the sums of money and decision-making requirements involved.76 There are various suggestions for the strengthening of the governance structures, including through securing the independence of the NHI Fund Board and the panel that appoints it; setting criteria for appointment; facilitating public participation in appointments; and tightening provisions for removal from or dissolution of the board. Appropriately defining the roles, membership and process for appointment of advisory committees is also an important step to improving governance and management of NHI funds.77
Government has itself recently published a governance arrangement for a proposed National Social Security Fund that meets many of the concerns raised about the governance arrangement contained in the NHI Bill. While it was withdrawn following a furore, the Green Paper on Comprehensive Social Security and Retirement Reform (2021)78 is useful for its detailed treatment of governance. The Green Paper lays out a structure for governance of the National Social Security Fund and processes for appointment of members, qualifying criteria, nominations, suspensions, and ways of ensuring that the board is independent of, while not being totally removed from, government and the Minister. It is an approach that should be used in amending the NHI Bill to better secure the integrity of the NHI Fund.
Transparency and the requirement of good governance also apply to the private sector and to the contracting arrangements79 that will be required under a future NHI.
As Jerome Singh points out in relation to managing the COVID-19 epidemic, ‘all relevant information about a pandemic and its decision-making processes ought to be communicated or made accessible to the public to uphold its trust’.80 The same principles apply beyond COVID-19 to the NHI introduction.
With regard to the state stewardship role, the COVID-19 experience was also somewhat uneven.
Responding effectively81 to COVID-19 required a strong, coordinated and integrated health service at its centre.82 Use of the disaster management regulations presented an opportunity to lay the basis for the operationalisation of centralised funding that could have facilitated better coordination and contracting of private sector actors. However, efforts to negotiate contracts with the private sector and to share resources across one platform were only of limited success, despite it being described as a ‘learning lesson’83 by a senior NDoH official. Reportedly, key lessons included a failure to reach agreement on pricing, and the obstacle posed by the inherent fragmentation of the private sector, which includes independent hospital groups on the one hand and individual practitioners who deliver services in these hospitals on the other. Paradoxically, regulations issued by the Minister of Trade and Industry to respond to the emergency and which provided for exemptions from measures in the Competition Act84 to allow private health care actors to enter agreements or practices to assist control of the pandemic may have served as a disincentive to collaborate.
As a result, negotiations with the private sector were conducted on a province-byprovince basis with only one province managing to complete negotiations. Any intention to bring the public and private health sectors together as one coordinated and centrally managed health service, which was effected in Ireland and Spain to dif fering extents,85 could not be implemented in South Africa, where public–private inequalities remain persistent determinants of health outcomes. In line with this, Jassat et al. investigated COVID-19-related mortality in hospitalised cases and reported significant differences in mortality rates in publicly funded facilities, with deaths in the public sector often occurring within three days of admission, pointing to delayed access to care impacting on increased risk of death.86 The inequity of the health system inevitably translated into inequity in health outcomes.
Cairncross and colleagues warned that during COVID-19 joint coordination could not take the form of ‘renting’87 high care and ICU beds at rates solely determined by the private sector when there is a desperate and urgent need. Identifying what has been described as ‘a tolerable margin’ of profit88 that is also fair and which will not bankrupt the public health system remains a key challenge for future NHI implementation and its regulatory framework. To what extent the state will be able to steward a unified health system across public and private providers, making choices that may not be palatable to some influential actors, remains to be seen.
In addition to requiring cooperation between public and private sectors, the NHI is premised on inter-governmental collaboration under changed powers and functions. Under NHI, a centralised single payer is established to purchase services, while district-level structures will decide on the prioritisation of services locally. Provinces will likely be delegated some of the service-provision obligations that they currently hold. Such changes in functions constitute a big change from the current decision-making and implementation model and envisage the simultaneous centralisation and decentralisation of power and function.
The COVID-19 experience has alerted us to the possible pitfalls of the kind of decentralisation and centralisation that we are likely to see under NHI. Loosening of public sector finance management procedures intended to facilitate decentralised flexibility in urgent purchasing of PPE was exploited by unscrupulous predators to enable looting of public funds. Highly centralised decision-making simultaneously led to slow initial roll-out of vaccines, opacity in decision-making and limited scope for public participation across all aspects of the COVID-19 response.
That being said, centralised price setting for medicines and devices, as anticipated under NHI, could have limited the price inflation that we saw in the purchase of PPE.
COVID-19 demonstrated both the shortcomings of a divided and inequitable health system and the difficulty that we will have in changing it through law. We will need a regulatory framework that works to reduce rather than entrench inequality, by requiring transparency, fostering participation and building trust; exercising stewardship over what should be a single health system; and clarifying (having properly tested) power and decision-making structures. South Africa should use the pitfalls and lessons of COVID-19 to inform legislative change (and the mobilisation and buy-in that must go with it) on NHI and the move to UHC.
While not a period of much legislative development, 2015–2020 has seen various changes to health and the health system brought about through legal advocacy, litigation and some legislative and regulatory change. It is also a period from which many lessons can be learned: the need for Intellectual Property law change to secure access to medicines and vaccines; the urgency of emergency medical services reform and the reform of the private health sector; the benefit of NCD control; and the risk of poor policy implementation (including to the lives of vulnerable people). The failure to progress some important legislation on social determinants of health is also instructive for efforts to strengthen the health system in the future. COVID-19 provided an unwelcome but perhaps useful test of some of the principles of NHI: a potentially system-changing legislative change in the next five years. The law is not the sole determinant of health. It cannot create the kind of health system that South Africa needs to realise the right of access to health care services. However, in combination with advocacy, activism and the contributions of those both in and outside the system, it can contribute to that aim.
1. Yamin AE. ‘Power, suffering and courts: reflections on promoting health rights through judicialisation’ in A Yamin and S Gloppen (eds) Litigating health rights: Can courts bring more justice to health. (2011) Harvard University Press at 365.
2. Gostin L et al. The legal determinants of health: harnessing the power of law for global health and sustainable development. Lancet. 2019; 393:1857–910 at 1857.
3. Gostin L et al. The legal determinants of health: harnessing the power of law for global health and sustainable development. Lancet. 2019; 393:1857–910 at 1860.
4. Gostin L et al. The legal determinants of health: harnessing the power of law for global health and sustainable development. Lancet. 2019; 393:1857–910 at 1860.
5. London L. What is a human-rights based approach to health and does it matter? Health and Human Rights 2008;10(1):65–80. Accessible at URL: http:// www.hhrjournal.org/2013/09/13/what-is-a-human-rights-based-approach-tohealth-and-does-it-matter/
6. Hunt P, Backman G. Health systems and the right to the highest attainable standard of health. Health and Human Rights Journal. September 2013 at 19.
7. Yamin EA. ‘Power, suffering and courts: reflections on promoting health rights through judicialisation’ in A Yamin and S Gloppen (eds) Litigating health rights: Can courts bring more justice to health. (2011) Harvard University Press at 335.
8. Yamin AE. ‘Power, suffering and courts: reflections on promoting health rights through judicialisation’ in A Yamin and S Gloppen (eds) Litigating health rights: Can courts bring more justice to health. (2011) Harvard University Press at 335.
9. Gargarella R. ‘Dialogic justice in the enforcement of social rights: some initial arguments’ in A Yamin and S Gloppen (eds) Litigating health rights: Can courts bring more justice to health. (2011) Harvard University Press at 344.
10. South African Department of Health. National HIV and Syphilis Prevalence Survey – South Africa 2006
11. Kapczynski A, Berger J. ‘The story of the TAC case: The potential and limits of socio-economic rights litigation in South Africa’ in Human rights advocacy stories eds D Hurwitz and M Satterthwaite, 43–79. (2009) New York: Foundation Press, p47, 50, 55, 57.
12. Minister of Health and Others v Treatment Action Campaign and Others 2002 (5) SA 721; M Heywood ‘Preventing mother-to-child HIV transmission in South Africa: Background, strategies and outcomes of the Treatment Action Campaign case against the Minister of Health’. (2003) 19 SAJHR 278.
13. Yamin AE. ‘Power, suffering and courts: reflections on promoting health rights through judicialisation’ in A Yamin and S Gloppen (eds) Litigating health rights: Can courts bring more justice to health. (2011) Harvard University Press at 349.
14. https://ritshidze.org.za/wp-content/uploads/2021/06/Ritshidze-North-WestState-of-Health-2021.pdf
15. Harries J, Cooper D, Strebel A, Colvin CJ. Conscientious objection and its impact on abortion service provision in South Africa: a qualitative study. Reproductive Health. 2014;11(1):16–26.
16. Hunt P, Backman G. Health systems and the right to the highest attainable standard of health. Health and Human Rights Journal; September 2013 at 2.
17. Section 27.
18. Section 28.
19. Minister of Health v Treatment Action Campaign No. 2 2002 (5) SA 721 (CC).
20. Van Biljon v Minister of Correctional Services 1997 (4) SA 441 (C).
Legislative framework and the right to health 2015-2020
21. Minister of Health & Another v New Clicks SA (Pty) Ltd & Others (Treatment Action Campaign and Innovative Medicines SA as Amici Curiae) 2006 (1) BCLR 1 (CC) at para 514.
22. See further Stevenson The National Health Act Guide (3 ed) https://section27. org.za/wp-content/uploads/2019/07/Stevenson-National-Health-ActGuide-2019-1.pdf at 5.
23. Equal Education and Others v Minister of Basic Education and Others 2021 (1) SA 198.
24. https://www.ohchr.org/en/professionalinterest/pages/cescr.aspx
25. https://www.refworld.org/pdfid/4538838d0.pdf
26. Hunt P, Backman G. Health systems and the right to the highest attainable standard of health. Health and Human Rights Journal. September 2013 at 3.
27. Yamin AE, Gloppen S (eds). Litigating Health Rights: Can court bring more justice to health? (2011) Harvard University Press.
28. Yamin AE. ‘Power, suffering and courts: reflections on promoting health rights through judicialisation’ in A Ely Yamin and S Gloppen (eds) Litigating Health Rights: Can court bring more justice to health? (2011) Harvard University Press at 369.
29. Hunt P, Backman G. Health systems and the right to the highest attainable standard of health. Health and Human Rights Journal. September 2013 at 3.
30. Gostin et al. The legal determinants of health: harnessing the power of law for global health and sustainable development. Lancet. 2019;393:1857–910 at 1857.
31. https://www.who.int/healthsystems/strategy/everybodys_business.pdf
32. For a description of the broad outlines of a right to health approach to health systems, see Hunt and Backman ‘Health systems and the right to the highest attainable standard of health’. Health and Human Rights Journal. September 2013 at 4–13.
33. https://www.nioh.ac.za/naphisa-the-fight-against-a-quadruple-burden-ofdisease/
34. For a short history of this episode and its lasting implications, see https://www. dailymaverick.co.za/article/2020-04-16-medicine-patent-victories-fromhiv-fight-are-now-more-relevant-than-ever/
35. https://www.gov.za/sites/default/files/gcis_document/201808/ippoli cy2018-phasei.pdf.
36. Much of the advocacy and activism on Intellectual Property law reform has been led by the Fix the Patent Laws Coalition, a broad coalition of health rights focussed civil society organisations. For a full list of member organisations, see https://www. fixthepatentlaws.org/
37. https://docs.wto.org/dol2fe/Pages/SS/directdoc.aspx?filename=q:/IP/C/ W669R1.pdf&Open=True
38. https://section27.org.za/2019/08/double-trauma-as-ambulance-fails-toarrive-again/
39. https://section27.org.za/2015/10/ems-in-the-eastern-cape/
40. https://www.dailymaverick.co.za/article/2020-10-27-better-spending-can-transform-emergency-medical-services-in-the-eastern-cape/
41. https://section27.org.za/2019/07/siu-investigation-into-buthelezi-ems-signalsa-move-to-greater-accountability/
http://section27.org.za/wp-content/uploads/2018/02/EMSRegulations-2017.pdf
43. National Department of Health, Statistics South Africa, South African Medical Research Council, and International Children’s Fund. South Africa Demographic and Health Survey 2016. Pretoria: NDoH; 2017.
44. Cois A, Kengne AP. ‘Non-communicable diseases’ in Massyn N, Barron P, Day C, Ndlovu N, Padarath A, editors. District Health Barometer 2018/19. Durban: Health Systems Trust; February 2020 at 135.
45. https://pubmed.ncbi.nlm.nih.gov/30882235/
46. https://www.thelancet.com/journals/lanplh/article/PIIS2542-5196(20)303041/fulltext
47. https://841e1e5c-cd4b-4521-abe7-8d810b959f2b.filesusr.com/ugd/0a15f0_ b87dd015df084a3a97d725b894269088.pdf
48. https://tobaccotactics.org/wiki/south-africa-industry-interference-with-the-control-of-tobacco-products-and-electronic-delivery-systems-bill/
49. https://www.polity.org.za/article/the-new-control-of-marketing-of-alcoholbeverages-bill-2013-10-02
50. Bertscher A, London L, Orgill M. Unpacking policy formulation and industry influence: the case of the draft Control of Marketing of Alcoholic Beverages Bill in South Africa. Health Policy and Planning. 2018;33:786–800. doi: 10.1093/heapol /czy049; URL: https://academic.oup.com/heapol/article/33/7/786/5042203
51. Minister of Trade and Industry. Draft Liquor Amendment Bill. Government Gazette, 30 September 2016; https://www.gov.za/sites/default/ files/gcis_document/201609/40319gon1206.pdf
52. https://www.dailymaverick.co.za/article/2020-11-05-draft-laws-back-up-incrammed-calendar-dominated-by-must-dos-leaving-key-legislation-dangling/
53. Reeve B, Gostin L. ‘Big’ Food, Tobacco, and Alcohol: Reducing Industry Influence on Noncommunicable Disease Prevention Laws and Policies; Comment on ‘Addressing NCDs: Challenges From Industry Market Promotion and Interferences’. International Journal of Health Policy and Management. 2019;8(7): 450–454. doi: 10.15171/ijhpm.2019.30.
54. http://healthombud.org.za/wp-content/uploads/2017/05/ FINALANNEXURES.pdf at p45.
55. Life Esidimeni Arbitration Award, para 1 https://section27.org.za/wp-content/ uploads/2020/10/LifeEsidimeniArbitrationAward.pdf
56. https://www.compcom.co.za/healthcare-inquiry/
57. https://section27.org.za/2016/02/make-private-healthcare-more-accessible/; https://section27.org.za/wp-content/uploads/2016/02/SAFMH-OralSummary-For-HMI.pdf
58. https://www.compcom.co.za/wp-content/uploads/2020/01/Final-Findingsand-recommendations-report-Health-Market-Inquiry.pdf at 30.
At [56].
60. Stransham-Ford v Minister of Justice and Correctional Services and Others 2015 (4) SA 50 (GP).
61. Minister of Justice and Others v Estate Stransham-Ford 2017 (3) SA 152 (SCA).
https://www.justice.gov.za/salrc/ipapers/ip33_prj141_Medico-legal.pdf
63. http://www.treasury.gov.za/documents/national%20budget/2019/review/Full BR.pdf at 83.
64. https://www.gov.za/sites/default/files/gcis_ document/201512/39506gon1230.pdf
65. https://serve.mg.co.za/content/documents/2017/06/29/whitepaper-nhi2017compressed.pdf
66. https://businesstech.co.za/news/government/494239/experts-warn-that-southafricas-nhi-plan-has-a-major-flaw-its-not-going-to-work/; https:// www.dailymaverick.co.za/article/2017-08-28-op-ed-has-the-national-healthinsurance-process-been-captured/; https://www.dailymaverick.co.za/ article/2019-08-14-ambitious-national-health-insurance-plan-stalked-by-theshadow-of-state-capture/
67. https://mg.co.za/news/2021-02-08-siu-to-recoup-some-of-the-r13-3-billionspent-on-corrupt-ppe-contracts/; https://www.agsa.co.za/Portals/0/Reports/ Special%20Reports/Covid-19%20Special%20report/2020%20Covid-19%20 Media%20Release%20FINALISED.pdf
68. van Ryneveld M, Whyle E, Brady L. What Is COVID-19 Teaching Us About Community Health Systems? A Reflection from a Rapid Community-Led Mutual Aid Response in Cape Town, South Africa. International Journal of Health Policy and Management. 2020. doi: 10.34172/ijhpm.2020.167.
69. Jeranji T. Are clinic committees an overlooked but vital missing link in SA’s Covid-19 response? Daily Maverick. 30 July 2020. https://www.dailymaverick. co.za/article/2020-07-30-are-clinic-committees-an-overlooked-but-vital-missinglink-in-sas-covid-19-response/
70. Stevenson S. What a lack of transparency and PPE corruption means for National Health Insurance. Spotlight Op-Ed. 9 September 2020. https:// www.dailymaverick.co.za/article/2020-09-09-what-a-lack-of-transparencyand-ppe-corruption-means-for-national-health-insurance/
71. https://www.afro.who.int/news/restoring-peoples-trust-medical-facilitiesessential-prescription-achieving-universal-health
72. Everett D. South Africans are revolting against inept local government. Why it matters. The Conversation. 23 Feb 2021. https://theconversation.com/southafricans-are-revolting-against-inept-local-government-why-it-matters-155483
73. Sibanda SO. Corruption Perceptions Index: Covid-19 PPE procurement scandals cement South Africa’s global ranking below 50. Daily Maverick. 21 January 2021. https://www.dailymaverick.co.za/opinionista/2021-01-28-corruptionperceptions-index-covid-19-ppe-procurement-scandals-cement-south-africas-glob al-ranking-below-50/
74. Douwes R, Stuttaford M, London L. Social solidarity, human rights and collective action: Considerations in the implementation of the National Health Insurance in South Africa. Health and Human Rights. 2018;20(2):185–196. URL: https:// cdn2.sph.harvard.edu/wp-content/uploads/sites/125/2018/12/Douwes.pdf
75. Stevenson S. What a lack of transparency and PPE corruption means for National Health Insurance. Spotlight Op-Ed. 9 September 2020. https:// www.dailymaverick.co.za/article/2020-09-09-what-a-lack-of-transparencyand-ppe-corruption-means-for-national-health-insurance/
76. Detailed submissions on this issue can be found here: https://section27.org. za/wp-content/uploads/2019/11/SECTION27-and-TAC-NHI-Billsubmission-29-November-2019.pdf
77. https://section27.org.za/wp-content/uploads/2019/11/SECTION27and-TAC-NHI-Bill-submission-29-November-2019.pdf; https://dullahomarinstitute.org.za/women-and-democracy/board-members-of-state-owned-enterprises-towards-transparent-appointments/reports/nhi-bill-dullah-omar-institute-submission-with-endorsements-nov-2019.pdf
78. https://www.gov.za/sites/default/files/gcis_document/202109/45076gon789. pdf
79. As above https://www.dailymaverick.co.za/article/2020-04-22-it-is-urgentto-integrate-sas-private-and-public-healthcare-systems-now/
80. Singh JA. How South Africa’s Ministerial Advisory Committee on COVID-19 can be optimised. SAMJ, S Afr Med J. 2020 June [cited 8 July 2021];110(6). Available from: http://www.scielo.org.za/pdf/samj/v110n6/20.pdf
81. Cairncross L, Reynolds L, Rensburg R, London L. It is urgent to integrate SA’s private and public healthcare systems now. Daily Maverick. Op-Ed 22 April 2020. https://www.dailymaverick.co.za/article/2020-04-22-it-is-urgent-to-integratesas-private-and-public-healthcare-systems-now/
82. Nkinki L, Fonn S. COVID-19 shows that where there is political will there is away to work across sectors. The Conversation. April 29 2020. https:// theconversation.com/covid-19-shows-that-where-there-is-political-will-there-isa-way-to-work-across-sectors-134999
83. https://sacoronavirus.co.za/2020/07/28/the-lessons-of-covid-19-for-nhi/
84. https://www.spotlightnsp.co.za/2020/04/03/covid-19-minister-mkhize-is-responsible-for-coordinating-with-private-sector/
85. Kringos D, Carinci F, Barbazza E, et al. Managing COVID-19 within and across health systems: why we need performance intelligence to coordinate a global response. Health Res Policy Sys. 2020;18:80. https://doi.org/10.1186/ s12961-020-00593-x; https://health-policy-systems.biomedcentral.com/track/ pdf/10.1186/s12961-020-00593-x.pdf
86. Jassat et al. Increased mortality among individuals hospitalised with COVID-19 during the second wave in South Africa. 2021. Available from: https:// www.medrxiv.org/content/10.1101/2021.03.09.21253184v1.full-text.
87. https://www.dailymaverick.co.za/article/2020-04-22-it-is-urgent-to-integratesas-private-and-public-healthcare-systems-now/
88. https://mg.co.za/special-reports/2020-11-04-nhi-and-covid-19-lessons-fromthe-pandemic-and-the-way-forward
Review of the first 25 years of democratic governance in South Africa highlights achievements in post-apartheid social and economic transformation, including health system successes (RSA, 2019). Improvements in life expectancy and maternal and child health outcomes in the 2014–2019 period demonstrate that collective action across provinces has been harnessed for positive results.
However, the 25-year review also notes a range of governance challenges. One health system experience has come to symbolise a ‘system of public governance that is broken’ (Kruger, 2019): the Life Esidimeni tragedy in Gauteng province. The 2015–16 death of 144 mentally ill patients due to neglect, after being transferred to unlicensed and ill-equipped non-governmental organisations (NGOs), is recognised as a failure of ethics, process and oversight (Freeman, 2018; Office of Health Ombud, no date). Supply chain and financial management irregularities across the public and private health sectors also indicate longstanding accountability failures and were further revealed in the 2020–21 COVID-19 responses (Auditor-General, 2020–21; Rispel et al., 2016). Meanwhile, for patients and their families, governance failure can be experienced as preventable death and disease, as well as drug shortages, long waiting times, and disrespect (Rispel et al., 2019). Such quality of care weaknesses have generated medical negligence claims that threaten the resourcing of the public health system (RSA, 2019; Rispel et al., 2019).
Contextual factors only exacerbated the challenges of health governance in 2015–20. The VUCA context (of volatility, uncertainty, complexity and ambiguity) included ‘austerity budgets’ that impacted directly on public health spending and staffing (Harding et al., 2020), service delivery protests in poorly served communities and growing economic inequality (Visagie et al., 2021). Meanwhile, conflict and change within the ruling African National Congress party had varied consequences within the health system. The COVID-19 pandemic was yet
another element of the VUCA context that demonstrated the impact of globalisation on population health across countries.
However, it is also important to acknowledge and learn from the pockets of positive health system governance experiences demonstrated in this period. In this chapter, we examine both the challenges and the positive experiences in order to consider how to strengthen governance to deliver better outcomes, especially for the most vulnerable. Our specific focus is on the processes and practices of governance, which are intertwined with leadership and management. These were identified as areas of weakness in a 2009–2014 review of South African health reforms (Levendal et al., 2015).
In section 2 we clarify the governance and leadership concepts that underpin the chapter and describe the key governance interfaces and relationships within the South African health system. Section 3 examines the experience of frontline (district-level) governance; section 4 focusses on provincial and national levels – considering how they impact on frontline governance in the multi-level health system; and section 5 summarises critical issues of leadership and management highlighted in earlier sections. Finally, section 6 draws out key conclusions for the future about the action needed to strengthen governance, leadership and management.
The chapter is founded on a set of 15 anonymous in-depth interviews and group discussions with senior health managers from across the country1 . It also draws on relevant, empirical research reported in peer-reviewed publications from the 2015–20 period, documentary material and media reports. International literature provides the conceptual foundations of the chapter.
Globally, the critical role of governance in attaining health system goals has been recognised since the publication of the World Health Organization’s landmark 2000 Health Systems report (WHO, 2000). Understanding governance as ‘stewardship’ – a ‘function of a government responsible for the welfare of the population, and concerned about the trust and legitimacy with which its activities are viewed by the citizenry’ (WHO, 2000: 129) – this report also noted that governance ‘percolates’ across all levels of the health system. In a successor document (WHO, 2007), ‘leadership and governance’ was considered in relation both to health services and the wider action needed to tackle the social determinants of health. It was defined as ‘protecting the public interest by influencing all actors that impact on health, through an array of instruments, processes and “institutions”, such as other ministries, parliament, statutory bodies, NGO “watchdogs” and the “free media”’ (WHO, 2007: 24).
More than 20 years after the WHO 2000 report, understandings of health system governance are still evolving in response to experience and ever-changing health and socio-political contexts.
1 This work received ethics clearance from the University of Cape Town, Faculty of Health Sciences Human Research Ethics Committee (HREC) REF 265/2021.
Attention has been paid, first, to three sets of critical health system governance actors (Bigdeli et al., 2020):
(1) Policy-makers – at central and sub-national levels, including the legislative and executive branches, elected politicians and professional civil servants;
(2) Health service providers – both public and private (for profit and not for profit), clinical and non-clinical, labour organisations, professional bodies, health professional training organisations and more;
(3) People – citizens, residents, patient groups, NGOs and civil society organisations (CSOs), and the media.
Recognising this array of actors, the early WHO frameworks have been criticised for seeing governance as an internal function of government, paying too much attention to national ministries of health, and ignoring other governance actors (Abimbola et al., 2017).
Second, a relational view of governance has gained prominence, focused on the formal and informal rules that shape the relationships between actors, through which governance is exercised (Abimbola et al., 2017).
From this perspective, governance, especially in decentralised systems, is acknowledged as a multi-level and polycentric process, rather than solely the function of the national sphere of government. Policy change, for example, entails complex processes of interactions between the centre and periphery, rather than being a centrally-controlled, top-down process (Gilson et al., 2017a). Whilst ‘dependent on arrangements set at political or national level’, governance must ‘be operationalized by individuals at lower levels in the health system’ (Pyone et al., 2017: 720). The everyday practice of decision-making is, consequently, a critical governance concern. Actors such as mid-level managers, local-level managers and frontline health workers are acknowledged to play key governance roles, alongside social actors, such as community actors, CSOs, trade unions and professional bodies, and local political actors. Their decision-making is influenced both by governance hardware (e.g. governance structures and the delegations of formal decision-making power) and by the software of personal values, communication practices and power or trust relationships (Abimbola et al., 2017; Gilson et al., 2017).
Third, whole-of-society (WoSA) and whole-of-government (WoGA) approaches have been recognised as key to tackling ‘wicked’ problems, such as disease outbreaks, growing economic inequality and climate change. Kickbusch and Gleicher (2012) argue that the interdependence and complexity of these problems demands networked and system-wide responses in which governance is ‘co-produced’ by multiple actors. Rather than focusing only on the governance of health care, it is critical, then, to think about governance for health – that is, as ‘the attempts of governments or other actors to steer communities, countries or groups of countries in the pursuit of health as integral to well-being through both whole-of-government and whole-of-society approaches’ (Kickbusch & Gleicher, 2012: vii).
Such approaches demand what has been called collaborative governance: ‘the processes and structures of public policy decision-making and management that engage people constructively across the boundaries of public agencies, levels of government, and/or the public, private and civic spheres in order to carry out a public purpose that could not otherwise be accomplished’ (Emerson et al., 2012: p.3). Although influenced by contextual factors, such governance is enabled by principled engagement among actors, shared motivations (for example, mutual trust and shared commitment), procedural and institutional arrangements, incentives to engage and leadership.
Collective action for health and well-being, moreover, requires approaches to leadership that move beyond the dominant command and control managerial styles of public sector bureaucracies. Systems leadership is, instead, a ‘collective form of leadership’ concerned with ‘the concerted effort of many people working together at different places in the system and at different levels’ (Bigland et al., 2020).
It entails both vertical and horizontal governance relationships. Within health care it embraces staff in all levels, professions and sectors, as well as service users and carers (Vize, 2016). Exercising such leadership requires both the individual skills that ensure actions are adapted to issue and context, as well as a wider authorising and enabling system environment (Bigland et al., 2020).
With these concepts in mind, Figure 15.1 presents a detailed view of health system governance actors and relationships in South Africa, considering those of most importance in the everyday practice of governance 2015–20 (drawing on interviews). It highlights, first, the multi-level and polycentric nature of governance. The three levels of public governance (national, provincial, local) are integrally connected, as the South African state is a unitary, albeit quasi-federal state, in which health is constitutionally defined as a ‘concurrent’ (shared) responsibility across levels. The current funding flows to the public health system reflect this shared responsibility. With oversight from the Financial and Fiscal Commission, the National Treasury allocates resources directly and separately to provincial and local governments, which then determine budget allocations to health activities and the other functions for which they are responsible. At the same time, the National Department of Health (NDoH) funding for specific purposes is through conditional grants to Provincial Departments of Health (PDoHs). Some PDoHs also enter into service-level agreements with large metropolitan municipal authorities (in the local sphere), providing resource support against clearly defined health service targets.
Figure 15.1 The dominant relationships of everyday governance practice within the South African health system (2015–2020)
The figure also reveals four other overall elements of everyday health system governance practice. First, given their particular and strong influence in the South African health system, ‘oversight actors’ (yellow boxes) are added as a category separate from ‘policy-makers’ (black and blue boxes). These include international organisations (e.g. WHO), the legislatures at national and provincial levels, specific national government actors, such as the Auditor-General’s (AG) office, established in the Constitution, and the Office of Health Standards Compliance (OHSC). Organised Labour (trade unions) is also included as an oversight actor, although outside government. Second, across levels, most relationships (black and yellow lines) are those among Bigdeli et al’s (2020) ‘policy-makers’, considering political, public service and oversight actors. This suggests that governance is primarily seen as an internal function of government and the public health system in South Africa. Third, few formal relationships (pink lines) with social actors (the ‘people’ actors, pink boxes) exist, although provincial- and district-level oversight bodies do include some that offer spaces of engagement with such actors (e.g. clinic committees and hospital boards). Fourth, governance relationships with public ‘health care providers’ (solid green lines) are most important at district/provincial level, and across levels there are, currently, few formal relationships with private sector actors (dotted green lines).
The District Health System (DHS) represents the base and frontline of the South African health system, with responsibilities for effective and equitable service delivery and the development of a District Health Plan (National Health Act, Act 61 of 2003).
As Figure 15.1 shows, the DHS lies across the provincial/local government interface, and health district boundaries are contiguous with municipality boundaries. This section discusses the governance relationships of, and everyday governance practice within, the DHS – illuminating both challenges and pockets of positive experience.
The District Office (DO) manages a wide span of governance relationships, which can be considered in three groups (Bigdeli et al., 2020):
1. Policy Accountability relationships – Within the DHS the key concern is policy implementation, and relationships with political leaders and health managers across governance levels are particularly important in current practice, in contrast to those with other government sectors. Relationships between the DO and politicians are, in principle, mediated through the PDoHs, with respect to the Member of the Executive Council (MEC) for Health (provincial Minister of Health), and through the municipality, with respect to mayors and municipal councils. In practice, however, district managers may find themselves engaging with political leaders at all levels, including ward councillors, around community-level health and health care challenges (interviews). Although shielded by the PDoHs from the full weight of their demands, the DO and health facility staff also interact with two sets of national-level actors: staff from the NDoH and national oversight organisations (specifically, the AG’s Office and the OHSC).
2. Service Provision relationships – The DO, through sub-district offices, has governance responsibility for public health service delivery across all provincially-managed facilities, from the district hospital to community-based services offered by community health workers. It must also coordinate with higher-level hospitals and the Emergency Medical Services (EMS), for example. The governance relationship with local government (municipalities) for service provision is important, as municipalities are responsible for environmental health services (National Health Act, Act 61 of 2003) and may also manage other PHC services. The DO sometimes also engages with private health care providers as well as, in some settings, higher education institutions involved in research and health professional training. Finally, health facility managers engage with organised labour groupings in employer–employee negotiations, with support from district managers as needed.
3. Public Accountability relationships – Relevant district-level relationships include interactions between the DO and the provincial legislature, which has oversight over all provincial activities. Where functional, district managers may also interact with the District Health Council (DHC) in the development and implementation of District Health Plans to meet the needs of communities (National Health Act, Act 61 of 2003). At facility level, District Hospital Boards and Clinic Committees are assigned governance roles. However, a 2017 survey found that only 17.9% of 168 clinics sampled across the country had functional committees (RSA, 2019). Wider research illustrates that the functionality and influence of clinic committees is undermined by legislative weaknesses, skills’ limits, facility manager and ward councillor attitudes, limited resources and lack of recognition (Haricharan et al., 2021a, b). Finally, there may be relationships between the DO and NGOs/ community-based organisations. Some are public accountability relationships. For example, Ritshidze, a community-led monitoring system developed by organisations representing people living with HIV/AIDS, is collecting facility-level data on critical aspects of primary care experience in facilities spread across provinces. It uses the information collected to engage community members and clinic staff in generating solutions to the problems identified, engaging also with clinic committees, provincial and national health managers, as well as conducting wider advocacy work (https://ritshidze.org.za). However, when NGOs are contracted to support service provision, they are more appropriately categorised as service delivery governance relationships (Mukinda et al., 2020a; Nxumalo et al., 2018a; Orgill et al., 2021).
Managing these relationships is challenging in practice. Although there are excellent examples of district managers, inadequate delegation of key financial and human resource management decision-making authority may constrain their work. In some provinces, managers may not be appointed at commensurate levels of seniority within the public service or have the necessary skill sets (interviews). Empirical studies of experience across the country (such as the Gauteng experience around emergency obstetric care, see Box 1 below) demonstrate that district-level governance relationships can also be problematic (e.g. those with organised labour; see also: Fana & Goudge, 2021; Nxumalo et al., 2018a, b; Mukinda et al., 2020b).
Background: EmOC services were managed by the PDoH, through different directorates, and clinical governance was supported by the District Clinical Specialist Team, managed by the NDoH.
• Limited communication and coordination of EmOC services: routine district management team meetings did not include all relevant health managers
• Weak provider accountability: indicated in late arrival at work and absenteeism
• Resource shortages: inadequate drugs, ambulances and infrastructure
• Staff shortages at primary care level: led to delays in attending to patients, under-qualified staff members dealt with patients
• Quality of care weaknesses: patients queueing for obstetric emergencies and unsatisfactory patient monitoring turned smaller complications into emergencies; patients experienced poor maternal and neonatal outcomes leading to medico-legal challenges
Underlying governance, leadership and management weaknesses:
1. At district and sub-district levels
• Budget constraints impacted on staff recruitment and led district managers to appoint senior staff into acting positions, limiting their authority and commitment
• Labour organisations frustrated staff disciplinary processes, discouraging managers from holding staff accountable
• Vacant posts, including CEO posts, took long to fill because of slow provincial approval processes
• Budgeting and expenditure data were not sufficiently disaggregated to allow efficienct EmOC management
2. At higher governance levels
• EmOC was not adequately funded by national or provincial government, despite being a national policy directive
• Inadequate communication between PDoH and NDoH managers and lack of clarity over managers’ roles led to duplication of efforts
• Unstable PDoH leadership, with three acting heads of department over a five-year period, led to changing EmoC priorities over time, undermining implementation
• Weak accountability of the provincial procurement office led to stock-outs of drugs and life-saving equipment
In addition, governance challenges at the district level often stem from higher levels. This may reflect the dominance of vertical lines of accountability within the public system – to the PDoH, NDoH, including health programme managers, to oversight actors such as the AG’s Office and OHSC, as well as to key provincial/local government political actors. A rich body of recent research reports experience from the frontline and makes clear the continuing presence of ‘the inverted pyramid’ of power within the public health system (see Figure 15.2; Gilson & Daire, 2011). At every level actors feel subject to the top-down, command and control exercise of power by those at higher governance levels. This exercise of power translates into huge reporting and meeting burdens that undermine district support for service delivery (for example, 19 maternal and child health accountability mechanisms were identified in one district, involving 22 reporting meetings a month: Mukinda et al., 2020a; see also Gilson et al., 2017b). In addition, the top-down exercise of power has generated a culture of compliance to audit demands (Mukinda et al., 2020a; Nxumalo et al., 2018a; Scott & Gilson, 2017)
and a climate of fear, blame and responsibility shifting. The knock-on consequences include punitive personal performance processes (Nxumalo et al., 2018b), and a failure to report problems when identified (which might in turn lead to medico-legal claims: Thwala et al., 2019). Vertical accountability processes, therefore, limit the development of organisational quality of care improvement strategies and prevent proactive consideration of how to strengthen public accountability (Mukinda et al., 2020a). They undermine policy implementation by stifling the local creativity, innovation, and frontline agency needed to implement policy changes and meet local needs (Kawonga et al., 2016; Nxumalo et al., 2018a; Scott & Gilson, 2017). The culture of avoiding responsibility and accountability has, finally, been identified as underlying the Life Esidimeni tragedy (Kruger, 2019).
Figure 15.2 The inverted pyramid of power in the South African health system, 2015–20 (adapted from the Local Government and Health Consortium, 2004)
Despite the challenges, there are positive district-level governance experiences. Four examples are presented in Boxes 2–5, focusing on service delivery (quality improvement in Limpopo and Mpumalanga, and hospital leadership in the Eastern Cape) and intersectoral action (in KwaZulu-Natal and the Western Cape). For governance of health, these experiences highlight the importance to service provision governance of relationships between clinicians and managers for (Box 2), and between primary care facilities and hospitals (Box 2 and 3). Box 3 also highlights the value of constructive relationships with the hospital boards that serve as a bridge to communities (see also: Nxumalo et al., 2018a; Mukinda et al., 2020b; Schneider & Nxumalo, 2017). Collaboration across government sectors is, meanwhile, central to governance for health. However, multiple relationships are entailed in such collaboration – cutting across the three sets of governance actors and the multiple governance levels (Box 4 and 5; van Rensberg et al., 2018; Marais & Petersen, 2015). Purposefully crafting new institutional arrangements to support and manage these relationships is essential (Box 4 and 5).
Box 2: Improving maternal, neonatal and child health (MNCH), experience from Mpumalanga and Limpopo provinces (Source: Schneider et al., 2020)
Background: A new governance mechanism for MNCH care was implemented in two districts to improve outcomes, with no additional budgetary resources. An experienced external facilita tor supported the districts through regular visits, deliberately making connections with other district-level initiatives and key persons, such as the District Clinical Specialist Teams (DCSTs). After three years there was a steep drop in cause-specific under-five mortality in both districts and maternal mortality had halved in one of them. Many frontline actors felt that the monitoring and response unit (MRU) was a key contributor among the various relevant interventions implemented.
Key features of the MRU:
• Principles: a systems approach, comprehensiveness and a focus on leadership and governance
• A ‘triangle’ of actors worked together across community to district levels: managers as ‘drivers’, clinicians as ‘experts’, and information officers as ‘navigators’
• A monthly meeting brought a wider range of district and sub-district actors together to define and implement priority actions for achieving the MNCH targets, using a set agenda for reporting, analysis and response to MNC deaths
• A system of 24-hour reporting and 48-hour review of MNC deaths by district programme managers and the DCST, who consequently supported frontline staff to implement agreed solutions
Governance relationships and practices supporting achievements:
• A collective vision for MNCH allowed alignment of all actors towards shared goals, and collective action across levels was also driven by interdependence and shared responsibility
• New relationships supported implementation, e.g. between PHC actors and district hospitals at sub-district level, between sub-district and district managers, between units within hospitals, and between clinicians and managers
• Collaboration between hospital heads and senior medical/nursing managers was key; nursing managers and dieticians remained in post even as senior managers and doctors
• Mid-level managers at the district and sub-district levels were purposefully engaged in driving change, rather than bypassed by higher-level programme managers
• A systems-level perspective was developed through multi-level teamwork, so staff could see the link between preventive actions and hospital outcomes
• A new culture of engaging with clinical guidelines was established, increasing ownership and accountability of managers and professionals, and intensifying in-service training
• New systems of meaning around data and actor roles were constructed that supported implementation: staff better understood the rationale behind data collected; senior clinicians better understood their public health and governance roles
• National-level endorsement and engagement (through the facilitator) increased the credibility of the MRU
• Supportive problem-solving by the DCST and programme managers increased staff willingness to report and account for deaths
• The external facilitator, specifically: engaged district, sub-district and facility actors in a process of collective sensemaking, and developed supportive relationships with actors outside the district; built consensus on problems to be prioritised and appropriate responses to them; and employed metaphors to provide the rationale for collaboration between PHC and hospitals
Background: Two district hospitals in the Eastern Cape province, both located in the same district, with largely similar resources, caseloads and patient demographics, were compared.
Over the previous seven-year period, perinatal mortality had fallen more significantly in one of the hospitals. A supportive yet firm leadership style characterised this hospital, in contrast to the more traditional, hierarchical leadership practices in the other hospital.
Factors enabling stronger performance in better performing hospital
1. Enabling leadership practices:
• Staff considered senior managers as supportive, approachable, friendly and firm
• Hospital managers valued and consciously assembled diverse staff teams, emphasising ‘listening’, open and continuous communication
• Staff contributions were valued and good suggestions implemented and acknowledged, empowering staff and enhancing trust among them
• Managers were proactive and innovative in problem-solving
• Senior staff made frequent and supportive ward supervision visits
2. Organisational practices and culture:
• A collective approach to finding organisational solutions was adopted, with all staff invited to meetings (including support staff, e.g. cleaning staff).
• An inherent culture of learning from mistakes existed, recognising that learning is part of professional development, and a continuous process – this supported a willingness to discuss mistakes and problem-solve for them
• Meetings were used as learning platforms, in which a collective and systems approach to accountability was established, without blaming individuals
• One adverse event was discussed at each perinatal meeting: staff were broken down into small groups to discuss mistakes made and lessons learnt; feedback sessions included in-service training on relevant topics
• Scheduled meetings always occurred and meeting minutes were actively used to increase accountability: actions and responsible persons were noted; at subsequent meetings, feedback was given on progress made on previous action points
• Good performers were acknowledged, while those who had performed less well were encouraged and given suggestions for how to improve responses to challenges
• Data were used in meetings to identify areas that needed improvement and to track action; they were (well) captured, and graphs were created and publicly displayed
• Staff were proactive in reporting low levels of stock, with one staff member dedicated to coordinating procurement of equipment for all departments
• Hospital managers sustaining relationships with all key partners working in maternal health in their catchment areas
• Hospital managers actively involved their board: using board members to bridge across sectors: to youth, traditional leadership, business and local community; board members also lobbied at provincial level to help speed up otherwise slow bureaucratic processes
• Hospital managers frequently engaged with district managers to address hospital challenges, and also directly contacted provincial/ national managers, bypassing district/ provincial levels, to tackle problems, e.g. to unfreeze posts or order drugs/equipment
The WoSA approach is a place-based collaborative governance approach, initiated in 2016, that mobilised local, provincial and national government actors, as well as civil society, business and community-based organisations to collaborate in tackling the multiple and multi-generational determinants of vulnerability (‘the stories of the lives of people’).
• Working in four learning sites, a trusted, independent, external facilitator assisted in building relationships between government/sectoral actors, whilst data from various sectors were integrated to create a shared vision and monitoring frame of improving dignity and quality of life along the life-course
• A WoSA coordinating committee in each learning site was supported by cross-sectoral working groups to address specific community needs, engaging community-based workers in community interactions. For example: in one site the ‘first 1000 days’ (conception to two years of age), including early childhood development, was the unifying target. Two wards were selected for more intense collaborative action with the approval of the mayoral council which included ward councillors. Members of the WoSA working groups addressing particular issues accompanied the Integrated Development Plan officers during scheduled evening sessions to listen to community inputs, and supported proactive communication with communities. They also engaged with the ward councillors, who, together with community health workers, were offered training to support them in their community engagement role
• Community-level impacts were observed from reports on local priorities (tackling community safety and policing concerns, infrastructural and refuse removal problems and spatial development and early childhood development)
• Lessons about how to work differently across sectors and levels of governance informed new activities, initiated in 2021 across multiple geographical areas, to tackle the critical issues of unemployment and community safety within the province
• The Premier and extended Cabinet authorised and held departments, political leaders, and municipalities accountable for intersectoral engagement
• The Cabinet-endorsed PSPs of 2014–2019 and 2019–2024 enabled intersectoral and intergovernmental collaboration, as did the Integrated Development Plan process, a policy imperative for municipalities
2. Governance mechanisms and decision-making practices supporting WoSA teams
• A politically-led steering committee of clustered departments developed focus areas for WoSA implementation, indicators of improvement, and action plans, and reported to Cabinet at six-monthly intervals
• The PDoH played a leading role, as steward of provincial population health and well-being
• At municipal level, the mayoral executive committee held the municipal manager, WoSA coordinating committee and ward councillors accountable for improvement work in communities
• At local level, decision-making entailed listening to community voices and using evidence in the identification of priority places and levers for impact
3. Leadership practices and capabilities enabling intersectoral collaboration:
• Leadership behaviours that reflected the values of respect, humility, cultural sensitivity, being responsive, collaboration, learning, adaptiveness, serving the goals of others
• Leadership actions that demonstrated support for investing in partnership development towards shared goals that address community needs, rather than pursuing sectoral interests, as well as for co-creation, joint learning and authorising frontline staff to network outside their organisations – including with communities
• Leadership mindsets that support comfort with uncertainty, and the disruptive realities of community dynamics and innovative approaches, whilst important leadership practices were supporting collective sensemaking and applying systems-thinking approaches in identifying the interconnected, root causes of vulnerability and community challenges
• The shift from vertically-directed governance to horizontal governance interactions was problematic, given differing levels of decentralised autonomy and authorisation for decision-making across departments, and the vertical lines of accountability for annual performance plans, and their auditing by the Auditor-General
• Poorly aligned strategy and policy across provincial departments, and fragmented provincial data management
• Political cycles and election processes across government levels (local, provincial and national) stall progress towards intersectoral collaboration over time
Box 5: Operation Sukuma Sakhe (Sources: Interview material; Ndlovu & Msweli, 2016; Phakati, 2019; Tshishonga, 2016)
Background: Operation Sukuma Sakhe (OSS), meaning Stand up and Build in isiZulu, is a multilevel, multisectoral governance approach implemented across KwaZulu-Natal province since 2009 in response to a directive of the South African National Aids Council. Over time, OSS has been institutionalised and expanded to address various social determinants of health, as well as, most recently, the COVID-19 vaccination programme. Overall, OSS seeks to leverage the skill of various sectors and com munities to address community-level challenges impacting on health and well-being.
Health care delivery is also strengthened through the OSS, e.g. the PHC outreach programme is strongly aligned with the ward war room, ward councillors support clinic and hospital advisory boards, ensuring that members on these structures are of good standing. However, the District Health Council stands separate from the district-level OSS structure, as it focuses only on health and oversees the District Health Plan.
• The principal design feature is ward-level localised governance, involving all sectors and civil society actors in a ‘war room’
• The ward councillor acts as the war room champion, and an administrator appointed by the Cooperative Governance and Traditional Affairs Department supports the councillor, also coordinating field workers within the local community (also accountable to their line departments)
• The field workers conduct home visits to explore household needs, and channel to relevant government departments for action
• District health managers nominate health ward officials, who account to the war room on progress in tackling problems on a weekly/two-weekly basis and also report back to the district health managers
• Ward-level activities are reported to the District HIV/AIDS/TB Council, which is co-chaired by the district health manager and a representative of civil society, and supported by the district health manager
• The district mayor, supported by the district health manager, reports to Cabinet meetings, alongside the Health HOD
• the provincial Cabinet regularly visits 20 wards in one district once per month to obtain feedback from ward councillors and to meet directly with communities to obtain feedback about delivery issues
• The provincial premier mandates the OSS, and holds district council mayors and Cabinet MECs accountable within it
• A cascade of accountability pivots around district council mayors, who receive feedback from ward councillors through local municipalities and are supported by the district health managers
• The ward councillors monitor the extent to which community problems have been resolved, reporting to district councillors
• Despite the frequency of elections associated with the political cycles across local, provincial and national and government levels, the continuity of the OSS system has been sustained over time due to entrenched administrative processes
• War room attendance is inconsistent, given the range of competing demands, and variable across departments, as not all have staff located at this level
• The large number of meetings and linked reporting demands pose a considerable administrative load and has impacted on time to deliver care
• There is an imbalance between reactive work and the systematic, intersectoral actions of system strengthening that tackle the root causes of ill-health and can generate health and social system resilience
• A particular challenge is the speed with which interventions need to be implemented which negatively impacts on the required administrative processes, as well as equity and fairness in service delivery
• The functionality of war rooms depends on the calibre and leadership capability of ward champions, which is uneven
• The cascaded accountability mechanism also relies on leadership capabilities, which are variable, to coordinate a range of actors (politically and administrative), and make sense of a large set of information
These experiences all demonstrate how the forms of governance and leadership that focus on building relationships create collaborative cultures of reflection, problem-solving and action (Boxes 2–4). Such cultures enable strengthened governance practices – such as teamwork within and across levels of care, coordinated action across governance interfaces and horizontal accountability to peers and the public (Nxumalo et al., 2018a, b; Mukinda et al., 2020a; Scott & Gilson, 2017). Meetings were identified as particularly important spaces of collaborative problem-solving, also allowing proactive engagement with available data (e.g. Box 2 and 3). Table 15.1 summarises wider district-level experiences about how routine meetings can become spaces that bring people together across hierarchies and silos in order to collaborate around shared goals. Small changes can have significant governance impacts (Gilson et al., 2020; Orgill et al., 2021).
• Institutionalise use and engagement with data to develop sensemaking skills, to diagnose problems, monitor progress and support forward planning e.g. by creating new routines to produce reports covering core indicators which are shared prior to the meeting and expected to be read by all
• Develop a systems approach by including NGOs, community representatives and all service providers in district management team meetings, and extending the planning processes to longer than the usual one-year cycles
• Recognise the power of words e.g. change the names of existing meetings to orient attention, encourage a proactive focus and break with historical associations
• Establish key principles to drive meetings (e.g. be positive; value people; listen to others and ask questions which allow others to contribute; share own challenges)
• Streamline meetings to encourage more proactive engagement (e.g. by introducing a focused agenda, oriented to the district’s core functions; managing time proactively by allocating a set time for each agenda item and a dedicated time-keeper)
• Encourage participation and share power (e.g. by rotating the chair of the meeting to share power and responsibility; asking challenging questions and using ‘rounds’ where each person present responds to a common question)
• Create opportunities to share ideas/knowledge and to learn from and challenge one another (e.g. by adapting existing meetings to allow space for team work among health facility managers, and with col leagues working in support functions; discussing what enables and prevents progress and developing collective responses to challenge)
• Strengthen collective sensemaking through encouraging investigation of problems (e.g. by collecting information ‘on the ground’ and engaging with solutions; presenting problems and proposed solutions at meetings, with regular follow-up reports of progress on the issues; presenting resolved problems to build capacity and provide for collective learning)
• Develop practical habits in meetings to support strong, positive organisational relationships and diffuse power (e.g. by using information and data purposively; allowing reflection in pairs and small groups on issues and problems)
‘Mid-level’ DHS managers play critical roles in creating new cultures, mediating top-down imperatives and bottom-up realities. Through their values, behaviours and actions these managers support frontline providers to re-orient their work better to meet the needs of their populations (e.g. Box 3; Gilson et al., 2020; Orgill et al., 2021). Such managers must be empowered, skilled and have sufficient confidence to practice governance differently. Beyond knowledge of public sector procedures and processes, they need the leadership skills required to: navigate relationships; challenge rules upwards as appropriate, even whilst respecting vertical reporting and accountability; instil new ‘just’ cultures, of collective inquiry and mutual accountability; encourage data and evidence use; and motivate and enable those they work with and nurture leadership in others (Boxes 2–4; Gilson et al., 2014, 2017b, 2020; Mukinda et al., 2020b; Nxumalo et al., 2018a, b; Orgill et al., 2021; Scott & Gilson, 2017). Such skills are also important in supporting policy implementation, such as for mental health care (van Rensberg et al., 2018; Marais & Petersen, 2015), going to scale with CHW programmes (Schneider & Nxumalo, 2017) and integrating HIV monitoring within the DHS (Kawonga et al., 2016).
Table15.1 Strengthening governance through new approaches to managing meetings (Sources: Gilson et al., 2020; Orgill et al., 2021)
The multi-layered nature of health system governance means that provincial and national governance experience impacts on frontline governance. This section discusses in more detail the governance challenges at higher levels that undermined frontline governance in the 2015–20 period. It also highlights experiences that demonstrate how governance at higher levels could be strengthened to support relational governance at the frontline.
A critical influence over all aspects of provincial health governance is widely acknowledged to be the specific relationship between the MEC and Head of Department (HOD), i.e. the ‘executive interface’ (Public Service Commission, 2019). Instability in this relationship undermines service delivery and policy implementation across levels (see Box 1), as well as the long-term visions required for provincial health system development.
Several interviewees noted that the division of powers between these two positions is a ‘structural design flaw’ in governance. Although the HOD is the formal accounting officer, responsible for financial management, the MEC is responsible for the internal organisation of the department and has power over human resource decisions (Public Service Commission, 2019). Despite expectations, MECs have often not delegated these powers to the HOD and, in some instances, have even been involved in appointments at the lowest levels. This blurring of political and administrative decision-making (commonly called ‘political interference’, and rooted in political party loyalties) is a key governance challenge (interviews), only compounded by regular turnover in MECs and HODs. Several interviewees suggested, however, that HODs must develop the political skills to navigate their relationship with the MEC – paying attention to political goals and imperatives and holding fast to public sector regulations and long-term health system visions. Shared health system visions between the MEC and HOD are also important in supporting governance action. Further, PDoHs must work proactively to strengthen and deepen health system leadership at district and hospital level, as a foundation for leadership stability. Interviewees hailed the Western Cape PDoH, for example, for its smooth HOD transitions in 2015 and 2020.
Two other provincial relationships that impact on the DHS are those between the PDoH and provincial and national treasuries and between the PDoH and AG’s Office. Both can challenge frontline governance, as described earlier. However, constructive relationships allow PDoHs, for example, to clarify the context of health care as the AG’s Office conducts audits and, in the case of treasuries, support collaboration around budgets and budgeting. Positive relationships can both buffer demands on the system and support system development (interviews).
Current experience suggests three other areas of action to strengthen provincial support for district governance. First, the exercise of facilitatory and participatory leadership approaches at higher levels is needed to enable similar leadership at DHS level. Such approaches support frontline actors to modify and adapt policies, to experiment and innovate, to better meet population needs (Nxumalo et al., 2018a; Mukinda et al., 2020b; Scott & Gilson, 2017). Although holding frontline managers accountable for the responsibilities assigned to them remains important, PDoH managers might therefore best be seen as facilitators of the frontline (Box 2), role modelling leadership practices that are enabling (Box 4).
Second, intersectoral collaboration at district and local levels requires provincial authorising mandates, provincial-level collaboration across sectors and provincial–municipal government engagement (Box 4, 5). The provincial premier’s leadership is crucial in securing provincial cabinet support for WoGA and WoSA initiatives. A new mindset is also required so that PDoHs become stewards of population health and support investments of time and resources beyond the formal boundaries of health care (Box 4, interviews). However, as shown in Figure 15.1, the governance relationships and practices important for WoGA and WoSA are not fully prioritised in everyday governance practice at the frontline, including relationships with ‘people’ actors, such as CSOs. Boxes 4 and 5 highlight that structural challenges to intersec toral collaboration within the public sector must be offset through provincial action.
Third, improving health care quality at district and primary care levels requires adequate delegation of decision-making power and clarification of organisational roles, relationships, responsibilities and accountability lines (Box 2, 4 and 5; Kawonga et al., 2010; Moosa et al., 2017; Schneider & Nxumalo, 2017). A 2015 WC DoH departmental policy statement, for example, clarifies and aligns roles and responsibilities across the PDoH in order to improve staff accountability and strengthen service delivery, emphasising the inter-connectedness of different components of the provincial health system (WCG:H, 2015: 3-4). Although other provincial health departments have also sought to revise their overall governance framework and structures in order to strengthen the DHS for improved service delivery they have faced political challenges (interviews).
The relationship between PDoHs and the NDoH is central to health system governance nationwide (Figure 15.1). The National Health Council (NHC), chaired by the national Minister of Health, is the mechanism for cooperation among political heads across levels/provinces. It must advise the national minister on, for example, policies, proposed legislation, norms and standards, and integrated plans for the country (National Health Act, Act 61 of 2003). The NHC has established the NHC Technical Committee (NHC-Tech, chaired by the NDoH Director General) as its advisory body, also serving as the main governance interface between PDoHs and the NDoH senior management team. Draft policies, strategies, performance and planning matters, underpinned by sound technical work, are intended to be considered in its quarterly meetings. Technical advisory sub-committees and ad hoc committees of the NHC-Tech also conduct technical work, involving provincial department staff and technical experts, and making recommendations to the NHC-Tech.
In practice, however, interviewees indicated considerable frustrations about the provincial–national relationship in recent years. Weak follow-up of decisions made at either level and the lack of an agreed long-term national health vision to drive a coherent nationwide policy and reform agenda for health system development were identified as governance challenges (interviews). The implementation challenges resulting from the disjuncture between national decisions and realities on the ground was another widespread concern (interviews; see also: van Rensberg et al., 2018; Marais & Petersen, 2015 (mental health); Schneider & Nxumalo, 2017 (CHW programmes); G:ENESIS/CHP/PWC, 2019 (NHI pilot sites)). The Ideal Clinic
policy (Box 6), for example, highlights weak policy coherence, poor coordination and communication challenges, as well as frontline governance challenges similar to those discussed earlier (Box 1). Interviewees suggested that limited consultation with provincial HODs during policy development meant that inadequate attention was given to conflicting policy priorities, levels of system preparedness, and resource requirements across contexts. The common complaint of ‘unfunded mandates’ was seen as an indicator of this problem, i.e. PDoHs being tasked to implement new policies from within their existing budgets, regardless of the policies’ additional resource needs (see Box 1, 6).
The underlying factors identified as contributing to the problems included the limited functionality of the NHC and NHC-Tech as mechanisms of cooperation, the lack of shared understandings about the role and purpose of each governance level, or the features and values of an effective inter-level relationship, and the high rate of provincial MEC and HOD turnover. The NDoH capacity weaknesses were another factor. These ranged from an inability to attract and retain adequate numbers of skilled technocrats and to hold them accountable for their work, leadership tensions and styles that were de-motivating, to limited succession planning. The NDoH weaknesses were reflected in, for example, weak HRH stewardship (van Ryneveld et al., 2020), as well as the failure to tackle problems such as medico-legal challenges and budget accruals across provinces (interviews).
It is also important to recognise that provincial and national departments work within multiple regulatory frameworks that influence their scope of responsibilities and decision-making power, and establish the vertical lines of accountability dominant within the health system. Many of these are government-wide frameworks that make no allowance for this system’s specific needs (interviews).
Despite the challenges, there were experiences of collective action across the national–provincial levels in the 2015–20 period that offer suggestions for how to strengthen this relationship for improved system-wide governance. The clustering of provinces and their HODs, for example, enabled collaborative learning, although challenged by HOD turnover. Experience around strategic planning, monitoring and evaluation processes over 2015–20 was particularly positive. It shows how constructive and well-managed relationships within the NHC-Tech, drawing on frontline experience, can support governance practice and service delivery improvements across provinces.
Box 6: Policy implementation challenges across health system levels: Ideal Clinic Realisation and Maintenance (ICRM) policy experience (Sources: Muthati & Rispel, 2020; Muthati et al., 2021)
The aim of the ICRM was to support the achievement of national core quality standards in primary health care
• Conceptualise the policy and develop policy documents to support implementation
• Communicate the idea to other levels of government
• Establish a delivery unit, with funding
• Set targets for provinces and establish teams to oversee provinces
• Develop memoranda of understanding across departments in other sectors e.g. between provincial health and education
• Support the districts
• Implementation: support PHC facilities and maintaining ‘ideal clinic’ standards by providing resource motivation
• Contestation about whether national or provincial governments should allocate the funding
• National policy actors consulted more amongst themselves than with provincial actors who are the main implementers
• Provincial government experienced the ICRM as an unfunded mandate
• Conditional grant funding was only allocated for two years and the conditions did not fully consider ICRM implementation needs
• Provincial actors perceived national actors to be slow to produce supporting policies for the ICRM implementation
• Districts communicated directly with the NDoH, bypassing provincial managers
• Provincial government criticised local government for not cooperating and refusing to implement provincial instructions
• Provincial actors did not engage adequately with local actors, neither in giving advice nor in gaining advice from local government
• Lack of ownership and sense of exclusion due to insufficient involvement of implementers
• District actors felt that provincial actors did not take ownership of the ICRM programme and districts lacked support
• Infrastructure challenges to implementing ICRM; lack of consideration of the difference between rural and urban facilities
• Delays in procuring equipment and confusion of task execution due to poor role clarity
• Nature of communication across government considered hierarchical, uncoordinated and rigid, often excluding local actors
• PHC facility managers experienced disempowerment as a result of unfulfilled roles and responsibilities by various departments and levels of government
• PHC facility managers penalised for non-compliance with prescribed standards that were either Provincial or National Department of Health responsibilities, as a result of inad equate support
• Poor relationships across government spheres
• Perceived top-down approach of NDoH
• Mismatched goals and ambitions and poor policy coherence between Ideal Clinic and National Core Standards led to duplication of effort, demotivation and frustration
• Confusion regarding overlapping roles and responsibilities and poor accountability
• Ineffective and weak communication
• Poorly developed sense of power and agency at lower system levels to influence implementation
The national Director General (DG) and provincial HODs are required by the National Health Act (Act 61 of 2003, sections 21 and 25) to prepare strategic, medium-term and annual performance plans across the national and provincial levels. Section 33, meanwhile, obliges district managers to table annual District Health Plans with the DHC and MEC. District Health Plans roll into provincial annual performance plans, which in turn link to the national annual performance plan. The DG is tasked to integrate the health plans of the national department and provincial departments and submit the integrated health plan to the NHC. Practically and coherently com plying with these directives is complex due to the various processes across a range of administrative offices at different system levels (NDoH, nine PDoHs, 52 districts –eight of which include metropolitan municipalities’ PHC plans) and differing contexts, including various political aspirations at national and provincial levels. Uneven capabilities in data governance, leadership, and strategic planning capabilities exacerbate the difficulties. Reducing fragmented planning, and meeting various deadlines related to health and budget planning have been challenging.
• Planning should be approached in a synchronised, systematic and structured way.
• Planning from the top needs to connect to planning from the bottom and the District Health Plan should be prioritised as the basis of health system planning for the country.
• District managers should be empowered with the necessary information and tools to execute their responsibility to govern for health and not only to manage district health services. Monitoring and evaluation, and planning processes need to therefore reflect the interconnections and interdependencies with other components of the system, other sectors and communities – by, inter alia, incorporating data from downstream contexts into district data, e.g. hospital mortality.
• Indicators and target setting should be iterative, starting from the bottom, and linked to problems to be solved.
• Publication of annual district health profiles (that show a colour-coded, district-based, data matrix by condition, indicator set and age group) at national level.
• Providing a practical guide to support district teams in using the profiles to i) consider coverage and quality of facilities as equally important, and ii) identify geographic area and age groups to prioritise for interventions.
• Provincial teams using district health profiles to identify districts with less than provincial average performance, as areas where to target interventions.
• Stronger joint planning involving managers and clinicians to generate shared understanding both of the problems and of the modifiable factors around which the system can take action (related to patients, providers or the system), generating improvements to test.
• Action was taken to streamline the burdensome National Indicator Data Set (NIDS) to focus exclusively on the data sets needed for the district health profiles.
• The NIDS and official population figures, disaggregated to sub-district level, are also now formally agreed and signed off at NHC-Tech level by October every year to ensure provinces and districts have sufficient time and necessary data to craft their annual performance plans.
To address these concerns, the NHC-Tech subcommittee responsible for health planning (the National Strategic Planning Committee) coordinated efforts with the subcommittees for District Health Systems and information systems (the National Health Information System for South Africa). Over the 2015–20 period, annual planning showed increasing maturity, building on a set of principles agreed within the NHC-Tech (Box 7). The subcommittee’s work was also enabled by active and facilitatory chairing, consultations with district and provincial managers and national programme managers, and purposefully drew from district-level experience with mortality audits and monitoring processes (see Box 3). Over time, the subcommittee’s leadership systematically tabled sound and well-argued recommendations that enabled decision-making at the NHC-Tech.
As Figure 15.1 makes clear, the NDoH sits in a web of international and national, cross-level governance interfaces, all of which are policy and oversight relationships. The lack of engagement with public health service providers is not surprising, given the constitutionally defined roles of the different governance levels. In terms of the private health sector, the Medical Schemes Council, an oversight body, represents a national governance interface with health insurers, but there is no equivalent for private health care providers. It is also noteworthy that there are no current, formalised spaces for health governance interactions at national level with the broad array of ‘people’ actors, such as CSOs. However, the National Health Summit of 2018 (only the third since 1994) was judged to generate value through engagements with multiple stakeholders from across the country (interviews).
Given the current experience, Box 8 highlights the critical governance roles that the NDoH could, in future, further develop in order to strengthen frontline governance.
Box 8: The critical roles of the NDoH in governance (Sources: interview material; see also G:ENESIS/CHP/PWC, 2019; Muthati & Rispel, 2020; Muthati et al., 2021; Njau et al., 2021)
• A national political champion for health and well-being
• Establishing long-term national health visions and planning to support alignment and coherence across levels within the sector
• Developing new national-level governance relationships to strengthen governance for health, such as with other sectors, CSOs, organised labour, academics, and the private health sector
• Coordinating action in supporting Business Cases for Health System Investment submitted to National Treasury
• Taking action nationally in managing the regulatory context for health (e.g. interceding on behalf of the health system with government departments that stablish and implement national regulatory frameworks impacting across provinces) and to support the delegation of decision-making powers across the system to enable frontline governance
• Supporting action to foster connectedness across spheres of governance
• Supporting and enabling provincial and district health system development
• Supporting and enabling the strengthening of key governance processes across the system e.g. annual planning, leadership development
• Enabling policy implementation through new approaches to policy development, monitoring and evaluation approaches linked to outcomes and supporting experimentation and learning
• Coordinating action across provinces to tackle critical health system governance problems e.g. medico-legal claims bills
As highlighted in previous sections, leadership and management practice has a critical influence on the form and strength of governance relationships at every level of the health system, with consequences for quality of care, intersectoral collaboration and cross-level collective action. Reflections on the Life Esidimeni tragedy and patterns of health system corruption also highlight the critical need to strengthen system leadership and stewardship practices to improve governance and accountability (Kruger, 2019; Rispel et al., 2016).
Interviewees judged that governance interfaces were undermined where leadership practice was regarded as autocratic and excluded professional groups, clinicians, organised labour, civil society actors or other government actors within and across levels. They also identified a tendency for government officials and managers to hold on to power in the face of challenging or complex circumstances, leading to decision-making without adequate information and experience.
In contrast, trusting relationships were judged to underpin robust governance relationships across the health system, as well as enabling innovative and creative responses to challenges. Strong teams and teamwork were identified as critical, and as based on: open communication, mutual respect, recognition of shared humanity and the offering of support in any way or form required (interviews). Boxes 2–4 clearly highlight the critical enabling practices and capabilities of system leadership that underpin both governance of health (for quality improvement, for example) and governance for health (collaboration within and beyond government boundaries).
Finally, interviewees reflected on the importance of robust leadership, working within established government procedures and sensitive to legitimate political pressures, but able to withstand illegitimate pressures. They expressed strong concern about the evidence of unethical and corrupt practices across the health system and within the wider public sector.
Strengthening health leadership and management is a longstanding government priority that was recognised in pre-2015 efforts to establish a country- and system-wide leadership development approach (Levendal et al., 2015). Although there were no national-level related developments in the 2015–20 period, the Western Cape PDoH published a leadership behaviours charter, leadership competency framework and leadership development strategy (WCG:H, 2016a,b). These documents continue to shape and influence a wide range of leadership development activities, and reflect the central role of leadership development within the WCG: health system transformation vision. They indicate that comprehensive plans and broad-ranging activities are needed to encourage, incentivise and support managers across the health system to develop relevant leadership competencies across their careers. The wider importance of public sector leadership development was also noted in this period (National School of Government, 2020), picking up the demands for a professional public service made in the National Development Plan, Vision 2030 (RSA, 2012). However, the specific needs of health system leadership are not clearly recognised. Interviewees noted, for example, the specialised nature of health care and the particular sets of critical stakeholders, including clinicians, health professional groups and private health sector actors, who must work together to achieve collective health system goals.
The structural and legislative foundations of governance in the South African public health system are well established. However, across sectors, the everyday practice of governance is weak. In the public health system, the consequences are seen in access inequities and disrespectful experience, as well as in large-scale crises such as the Life Esidimeni tragedy. The development of a capable state, founded on strong ethical practice, is therefore necessary to address the country’s social, economic and well-being needs. It is the most critical challenge currently facing the country (Kruger, 2019; Heywood 2021a, b; RSA, 2012).
Pockets of positive governance experience within the health system show that there is capability within this system, but this capability must be deepened, spread and sustained. Four governance re-sets are needed: one requires action outside the system, and three address health governance specifically.
It is essential that the broader governance environment is recognised as having a critical influence over health governance. New public management (NPM) practices, such as centralised control of lower-level public managers through target-setting and audit processes undermine public administration across sectors; as does the undue politicisation of public governance (Chipkin & Lipietz, 2012). As noted in the health system, NPM practices have worked to create a ‘system of regulatory compliance’ that ‘paralyses service delivery and decision-making, makes it difficult if not impossible for the state to work with informality, sets government apart from communities, undermines cross-sector partnering, stifles innovation and prevents system change’ (Boraine, 2021). These practices have ‘deprofessionalised major areas of public service’, and heightened policy accountability at the expense of public accountability (Cronin, 2021).
Some currently proposed reforms tackle at least some of these challenges. The draft National Implementation Framework towards the Professionalisation of the Public Service (NSG, 2020), for example, presents proposals that seek to ‘insulate’ the public service from politics and political parties. They include reforms to the terms of office and process of appointing senior public servants, recognition of specialist competencies and new efforts to manage the political-administrative interface. Such proposals could bring the leadership stability globally acknowledged as necessary for health system development (Balabanova et al., 2013). However, until such changes in current regulatory frameworks are achieved, senior health leaders at different levels must work to buffer the frontline from regulatory demands as well as heighten public accountability.
In looking to the future, three health system governance re-sets are also needed. First, communities and the DHS must be placed at the heart of the health system, with frontline governance strengthened to support quality improvement and local, place-based intersectoral action. This requires adequate and appropriate authority delegations to district managers, nested within coherent and aligned roles and responsibilities across the multi-level system. This re-set will require PDoH and NDoH managers to offer enabling leadership for frontline actors, even as they hold them to
account for outcomes – supporting them to work towards health and well-being goals. PDoH officials could, for example, become coaches for district health managers, whilst those in the NDoH must act as overall system facilitators (see Box 7). Deepening the already initiated bottom-up health planning processes will also be important. As is globally recognised (Hallsworth, 2011; Kickbusch & Gleicher, 2012), policy-making to address complex issues must combine appropriate central (national/provincial) guidance and accountability mechanisms (for example, in terms of monitoring outcomes), with the local-level flexibility needed to respond to implementation realities (G:ENESIS/ CHP/PWC, 2019; Kawonga et al., 2016; Muthati & Rispel, 2020; Schneider & Nxumalo, 2017).
Within this re-set, the PDoH/NDoH interface demands specific attention. One interviewee suggested co-creating a health governance charter that clarifies the values underpinning this interface, the roles of various actors, the spaces of engagement, and forms of reciprocal accountability. Nested within, but more detailed than, the existing legal frameworks, such a charter could provide the basis for maintaining stable structural relationships over time, despite provincial and national leadership turnover. Previous positive experiences of collaboration and coordination within the NHC-Tech also illustrate the everyday governance practices important in sustaining constructive governance relationships across levels. Consultation, engagement and holding actors to account for following through on agreed actions, are key.
Second, given the complex nature of future health and well-being challenges, as previewed by COVID-19, intersectoral collaboration and deepened engagement with social actors at local levels are essential. This will require that provincial health departments, specifically, adopt a new mindset of stewardship for health. They must look beyond health care as they seek, and work within, provincial government mandates for WoSA and WoGA approaches, to enable intersectoral action for health at district level (van Rensberg et al., 2018; Marais & Petersen, 2015). Political support from local government is also needed, and the Integrated Development Planning process could assist in institutionalising collaboration. However, collaborative governance requires flexibility, working across structural boundaries and the boundaries of formality/ informality, and being willing to engage openly with other actors rather than pre-determining the terms of engagement (Bigland et al., 2020; Bolden et al., 2019; Emerson et al., 2012).
Greater openness to civil society is also important in strengthening accountability to patients and the public. Simply recognising ‘people actors’ as legitimate governance actors, as well as becoming less defensive towards them, could be first steps in engagement. This could entail inviting, supporting and learning from local-level initiatives addressing specific needs, such as the Ritshidze initiative. Provincial and District Health Councils might thereby be opened beyond current mandates as spaces for engagement with civil society, even as strengthening the functionality of clinic committees and hospital boards remains important. More regular engagements with a wide range of ‘people’ governance actors through provincial and national health summits could, moreover, support relationship-building, and draw in the multiple forms of evidence needed for decision-making. Strengthened, productive relationships with organised labour would ideally be part of this effort.
Third, implementing these health governance re-sets requires both new mindsets and deepened skillsets, including those of ethical practice. Kickbusch and Gleischer (2012)
specifically stress the importance of ‘systems thinking’ skills, drawing on complexity science and interdisciplinary insights, in governance for health. These skills are integral to the concept of system leadership (Bolden et al., 2019). Formal leadership and management training programmes have a role to play in developing such leadership (Bolden et al., 2019; Doherty & Gilson, 2015), and can be guided by relevant frameworks – such as those of the Western Cape DOH (WCG:G 2016a,b).
Establishing a national institutional home for health leadership and management development could support relevant programming. However, it is even more important that everyday governance practice both nurtures and supports the deepening of health system leadership. Appropriately managed meetings (see Table 15.1) and group coaching interventions (Cleary et al., 2018) are relevant practices. New quality improvement (Box 2) or WoSA initiatives (Boxes 4–5) that pay attention to governance relationships and practices offer opportunities to deepen system leadership.
Formally-designated managers across the system play vital roles in role-modelling relevant leadership practices, such as respectful and active listening, putting oneself in the shoes of others, having robust and difficult conversations and acting ethically. Senior managers can also be held accountable, through their performance agreements, for enabling the spread of system leadership.
A final consideration is whether and how these governance re-sets fit with the macro health system reforms proposed in the 2019 NHI Bill. On the one hand, governance strengthening is needed to support implementation of the reforms, as noted in the NHI pilot site evaluation (G:ENESIS/CHP/PWC, 2019). On the other hand, the reforms may work against the governance re-sets. More specifically:
• the proposed, centrally-controlled purchasing and contracting mechanisms may enhance the existing top-down audit and accountability approaches that undermine frontline governance, and new sub-district-level structures may fragment health care governance;
• there is no clear place for PDoHs in the reforms proposed, ignoring their important roles of enabling and coaching lower system levels, and acting as stewards for health;
• the potential influence of the national Minister of Health over the NHI Fund’s governance structures ignores wider concerns about political/administrative interfaces;
• the reforms focus on health care financing and related structures, inadequately considering how to address the social determinants of health or support the required intersectoral collaboration.
In conclusion, strengthening governance for health is a long-term endeavour in every setting (Kickbusch & Gleischer, 2012). Past experience as well as the needs of the future demand that the lessons of 2015–20 drive a new South African health governance, leadership and management agenda. The health system must work better, and especially for those who are most vulnerable. Existing positive experiences offer ideas of what is possible. Governance re-sets must build on these experiences and embrace regular reflection on experience through the lens of system stewardship. Implementation of the NHI reforms must also work to support, not undermine, the re-sets. Recognising that some of the roots of health system governance challenges lie outside the health system, wider political and public service action must, finally, accompany health system reform.
Governance, leadership and management
Abimbola S, Negin J, Martiniuk AL, Jan S. Institutional analysis of health system governance. Health Policy and Planning. 2017;32(9):1337–1344.
Auditor-General, South Africa. Consolidated general report on national and provincial audit outcomes PFMA 2020-21. (2020-21). https://www.agsa.co.za/Reporting/ PFMAReports/PFMA2020-2021.aspx
Balabanova D, Mills A, Conteh L, Akkazieva B, Banteyerga H, Dash U, ... McKee M. Good Health at Low Cost 25 years on: lessons for the future of health systems strengthening. The Lancet. 2013;381(9883): 2118–2133.
Bigdeli M, Rouffy B, Lane BD, Schmets G, Soucat A. Health systems governance: the missing links. BMJ Global Health. 2020;5(8): e002533.
Bigland C, Evans D, Bolden R, Rae M. Systems leadership in practice: thematic insights from three public health case studies. BMC Public Health. 2020;20:1735.
Bolden R, Evans D, Jarvis C, Mann R, Patterson M, Thompson E. Developing Systems Leadership in Public Health: A scoping report. Bristol Leadership and Change Centre, Centre for Public Health and Wellbeing, University of the West of England. (2019) ISBN 9781860435546. Downloaded from https://uwe-repository. worktribe.com/output/1492816/developing-systems-leadership-in-publichealth-a-scoping-report, 25 October 2021
Boraine A More than a new path and a more capable state: we need a new institutional and political culture. ASSAf webinar: What must be done if the state is to be capable of poverty and inequality reduction? 22 July 2021.
Chipkin I, Lipietz B. Transforming South Africa’s Racial Bureaucracy: New Public Management and Public Sector Reform in Contemporary South Africa. PARI Long Essays, Number 1. (2012). Downloaded on 25 October 2021, from: https://47zhcvti0ul2ftip9rxo9fj9-wpengine.netdna-ssl.com/wp-content/ uploads/2017/05/PARI-L.E.-1.-Transforming-Racial-Bureaucracy-Feb2012.pdf
Competition Commission, South Africa. Health Market Inquiry Final findings and recommendations report. (2019) Downloaded on 25 October 2021, from https://www.compcom.co.za/wp-content/uploads/2020/01/Final-Findingsand-recommendations-report-Health-Market-Inquiry.pdf
Cronin J. Why the South African state is incapacitated. New Frame, 25 August 2021. Downloaded 25 October 2021, from https://www.newframe.com/why-thesouth-african-state-is-incapacitated/
Doherty J, Gilson L. Workplace-based learning for health system leaders. Practical strategies for training institutions and governments. Lessons from a consultative workshop 17-19 August 2016, Cape Town, South Africa. (2016) Downloaded, 25 October 2021, from https://resyst.lshtm.ac.uk/resources/workplace-basedlearning-for-health-system-leaders-practical-strategies-for-training
Emerson K, Nabatchi T, Balogh S. An integrative framework for collaborative governance. J Public Adm Res Theory. 2012;22:1–29.
Fana T, Goudge J. Austerity, resilience and the management of actors in public hospitals: a qualitative study from South Africa. BMJ Global Health. 2021;6(2): e004157.
Freeman, MC. Global lessons for deinstitutionalisation from the ill-fated transfer of mental health-care users in Gauteng, South Africa. The Lancet Psychiatry. 2018;5(9): 765–768.
GENESIS/Centre for Health Policy (CHP)/Price Waterhouse Cooper (PWC). Evaluation of Phase 1 implementation of interventions in the National Health Insurance (NHI) pilot districts in South Africa NDOH10/2017-2018. (2019) Downloaded, 25 October 2021, from https://www.hst.org.za/publications/ NonHST%20Publications/nhi_evaluation_report_final_14%2007%202019.pdf
Gilson L, Daire J. Leadership and Governance within the South African health system. Chapter 6 in Padarath A and English E (eds) South African Health Review 2011. (2011) Durban: Health Systems Trust.
Gilson L, Elloker S, Olckers P, Lehmann U. Advancing the application of systems thinking in health: South African examples of a leadership of sensemaking for primary health care. Health Research Policy and Systems. 2014;12(1):1–13.
Gilson L, Lehmann U, Schneider H. Practicing governance towards equity in health systems: LMIC perspectives and experience. Int J Equity Health. 2017a;16:171. https://doi.org/10.1186/s12939-017-0665-0
Gilson L, Barasa E, Nxumalo N, Cleary S, Goudge J, Molyneux S, ... Lehmann U. Everyday resilience in district health systems: emerging insights from the front lines in Kenya and South Africa. BMJ Global Health. (2017b);2(2): e000224.
Gilson L, Ellokor S, Lehmann U, Brady L. Organizational change and everyday health system resilience: Lessons from Cape Town, South Africa. Social Science & Medicine. 2020;266:113407. DOI: 10.1016/j.socscimed.2020.113407
Harding M, Baduza M, Chaskalson J. Socioeconomic rights and austerity. A SECTION27 Report. (2020) Downloaded on 1 November at http://section27. org.za/wp-content/uploads/2020/08/S27-final-austerityreport-2020-13082020.pdf
Haricharan HJ, Stuttaford M, London L. Effective and meaningful participation or limited participation? A study of South African health committee legislation. Primary Health Care Research & Development. 2021a;22(e28):1–8. doi: 10.1017/ S146342362100032
Haricharan HJ, Stuttaford M, London L. The role of community participation in primary health care: practices of South African health committees. Primary Health Care Research & Development. 2021b;22(e31):1–10. doi: 10.1017/S146342362100027X
Heywood M. Social justice needs a capable state – so what is civil society doing about it? Daily Maverick 7 September 2021. (2021a) Downloaded 25 October 2021, from https://www.dailymaverick.co.za/article/2021-09-07-social-justice-needsa-capable-state-so-what-is-civil-society-doing-about-it/
Heywood M. (Association of Former Directors-General launched to address scourge of corruption and bolster governance. Daily Maverick 29 September 2021. 2021b). Downloaded 25 October 2021, from https://www.dailymaverick.co.za/ article/2021-09-29-association-of-former-directors-general-launched-to-addressscourge-of-corruption-and-bolster-governance/
Hallsworth M. System stewardship. The future of policymaking? Working Paper, Institute for Government. (2011) Downloaded 25 October 2021, from https://www.instituteforgovernment.org.uk/sites/default/files/publications/System%20Stewardship.pdf
Kawonga M, Blaauw D, Fonn S. The influence of health system organizational structure and culture on integration of health services: the example of HIV service monitoring in South Africa. Health Policy and Planning. 2016;31(9):1270–1280.
Kickbusch I, Gleicher D. Governance for health in: the 21st century. World Health Organization. (2012). Regional Office for Europe.
Kruger N. ‘Instructions from above’: Advocate Adila Hassim on the Ethical and Systemic ramifications of the Life Esidimeni disaster. 2019 David Sanders lecture on Public Health and Social Justice, University of the Western Cape. (2019) https:// www.uwc.ac.za/news-and-announcements/news/instructions-from-above-advocate-adila-hassim-on-the-ethical-and-systemic-ramifications-of-the-life-esidimenidisaster-317
Levendal E, English R, Schneider H, London L, Haricharan H. Health Governance. Ch 12 in Matsoso MP, Fryatt RJ and Andrews G (eds). The South African Health Reforms 2009–2015: Moving towards universal coverage. (2015). Cape Town: Juta.
The Local Government and Health Consortium. Decentralising Health Services in South Africa: Constraints and Opportunities. (2004) Durban: Health Systems Trust. ISBN 1-919743-79-0
Marais DL, Petersen I. Health system governance to support integrated mental health care in South Africa: challenges and opportunities. International Journal of Mental Health Systems. 2015;9(1):1–21.
Mathole T, Lembani M, Jackson D, Zarowsky C, Bijlmakers L, Sanders D. Leadership and the functioning of maternal health services in two rural district hospitals in South Africa. Health Policy and Planning. 2018;33(suppl_2): ii5–ii15.
Moosa S, Derese A, Peersman W. Insights of health district managers on the implementation of primary health care outreach teams in Johannesburg, South Africa: a descriptive study with focus group discussions. Human Resources for Health. 2017;15(1): 1–9.
Mukinda FK, Van Belle S, George A, Schneider H. The crowded space of local accountability for maternal, newborn and child health: a case study of the South African health system. Health Policy and Planning. 2020a;35(3):279–290.
Mukinda FK, van Belle S, Schneider H. Perceptions and experiences of frontline health managers and providers on accountability in a South African health district. International Journal for Equity in Health. 2020b;19:110.
Muthati IS, Rispel LC. Policy context, coherence and disjuncture in the implementation of the Ideal Clinic Realisation and Maintenance programme in the Gauteng and Mpumalanga provinces of South Africa. Health Research Policy and Systems. 2020;18(55).
Muthati IS, Kawonga M, Rispel LC. Using social network analysis to examine intergovernmental relations in the implementation of the Ideal Clinic Realisation and Maintenance programme in two South African provinces. PLoS ONE. 2021;16(5): e0251472.
National School of Government (NSG). A National Implementation Framework towards the Professionalisation of the Public Service. Draft. Government Gazette, 24 December 2020 No.44031. (2020) Downloaded on 25 October 2021, from https://www.gov.za/sites/default/files/gcis_ document/202012/44031gon1392.pdf
Ndlovu NI, Msweli P. Theorizing and institutionalizing operation Sukuma Sakhe: a case study of integrated service delivery. Environmental Economics. 2016;7(4): 161–169.
Njau J, Silal SP, Kollipara A, Fox K, Balawanth R, Yuen A, White LJ, Moya M, Pillay Y, Moonasar D. Investment case for malaria elimination in South Africa: a financing model for resource mobilization to accelerate regional malaria elimination. Malaria Journal. 2021;20:344.
Nxumalo N, Gilson L, Goudge J, Tsofa B, Cleary S, Barasa E, Molyneux S. Accountability mechanisms and the value of relationships: experiences of front-line managers at subnational level in Kenya and South Africa. BMJ Global Health. 2018a;3(4): p.e000842.
Nxumalo N, Goudge J, Gilson L, Eyles J. Performance management in times of change: experiences of implementing a performance assessment system in a district in South Africa. International Journal for Equity in Health. 2018b;17(1): 1–14.
Republic of South Africa (RSA). Department of the Presidency. (2012) The National Development Plan (NDP) 2030. Pretoria: Government Printers.
Republic of South Africa (RSA). Department of the Presidency (2019). Towards a 25-Year Review 1994–2019. Downloaded on 25 October 2021, from https:// www.dpme.gov.za/publications/20%20Years%20Review/20%20Year%20 Review%20Documents/20%20Year%20Review.pdf
Office of Health Ombud (no date) The report into the circumstances surrounding the deaths of mentally ill patients: Gauteng province. No guns. 94+ silent deaths and still counting. Downloaded 25 October 2021, from http://healthombud.org.za/ wp-content/uploads/2017/05/FINALREPORT.pdf
Orgill M, Marchal B, Shung-King M, Sikuza L, Gilson L. Bottom-up innovation for health management capacity development: a qualitative case study in a South African health district. BMC Public Health. 2021;21(1):1–19.
Phakathi M. Exploring trust in intergovernmental relations: the case of Operation Sukuma in KwaZulu-Natal. Journal of Public Administration. 2019;54(4): 558–566.
Pyone T, Smith H, van den Broek N. Frameworks to assess health systems governance: a systematic review. Health Policy and Planning. 2017;32(5):710–722.
Public Service Commission. Guide on Governance Practice for Executive Authorities (EAs) and Heads of Department. Pretoria: Public Service Commission. (2019) Downloaded on 25 October 2021, from http://www.psc.gov.za/documents/ reports/2019/PSC%20Report%20175x250-B5-Final%2009052019%20HoD%20 Guide-Printer-3mm%20bleed-20191107.pdf
Rispel LC, De Jager P, Fonn S. Exploring corruption in the South African health sector. Health Policy and Planning. 2016;31(2):239–249.
Rispel L, Shisana O, Dhai A, Rensburg R, Wolvaardt G, Dudley L, Patel RH, ... Whittaker S. Achieving high-quality and accountable universal health coverage in South Africa: a synopsis of the Lancet National Commission Report. South African Health Review. 2019;2019(1):9–80.
Schneider H, Nxumalo N. Leadership and governance of community health worker programmes at scale: a cross-case analysis of provincial implementation in South Africa. International Journal for Equity in Health. 2017;16(1):1–12.
Schneider H, George A, Mukinda F, Tabana H. District Governance and Improved Maternal, Neonatal and Child Health in South Africa: Pathways of Change. Health Systems & Reform. 6(1):e1669943.
Scott V, Gilson L. Exploring how different modes of governance act across health system levels to influence primary healthcare facility managers’ use of information in decision-making: experience from Cape Town, South Africa. International Journal for Equity in Health. 2017;16(1):1–15.
Tshishonga N. Operation Sukuma-Sakhe as a Service Delivery Model at UGU District Municipality, KwaZulu-Natal Province. (2016). South African Association of Public Administration and Management (SAAPAM) Limpopo Chapter 5th Annual Conference Proceedings, p.186–194.
Thwala SBP, Blaauw D, Ssengooba F. ‘It needs a complete overhaul…’ District manager perspectives on the capacity of the health system to support the delivery of emergency obstetric care in an urban South African district. Global Health Action. 2019;12(1):1642644.
Visagie J, Turok I, Swartz S. What lies behind social unrest in South Africa and what might be done about it? The Conversation. August 18 2021. Downloaded on 1 November at https://theconversation.com/what-lies-behind-social-unrest-insouth-africa-and-what-might-be-done-about-it-166130
van Rensburg, AJ, Khan R, Wouters E, van Rensburg D, Fourie P, Bracke P. At the coalface of collaborative mental health care: A qualitative study of governance and power in district‐level service provision in South Africa. The International journal of health planning and management. 2018;33(4):1121–1135.
Van Ryneveld M, Schneider H, Lehmann U. Looking back to look forward: a review of human resources for health governance in South Africa from 1994 to 2018. Human Resources for Health. 2020;18(1):1–10.
Vize R. Stories from Leadership for Change. A report for the Leadership for Change Steering Group. (2016).
Western Cape Government: Health (WCG:H) Health governance and accountability framework. Policy statement. 3 August 2015.
Western Cape Government: Health (WCG:H) (2016a) Leadership Competency Framework.
Western Cape Government: Health (WCG:H) (2016b) Leadership Development Strategy.
World Health Organization. The World Health Report 2000: Health Systems: Improving Performance. Geneva: World Health Organization. (2000). Downloaded 25 October 2021, from https://www.who.int/whr/2000/en/ whr00_en.pdf
World Health Organization. Everybody’s business – strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: World Health Organization. (2007). Downloaded 25 October 2021, from https:// www.who.int/healthsystems/strategy/everybodys_business.pdf
People have a right to play an active role in maintaining, promoting and restoring their health and to participate in the planning, organisation, operation and control of primary health care (PHC). These rights were recognised in the 1978 Declaration of Alma-Ata and updated in the 2018 Declaration of Astana (WHO, 1978; WHO, 2018). The Alma-Ata declaration promotes a people-centred approach to health systems that celebrates ‘the spirit of self-reliance and self-determination’ and acknowledges that the people ‘have the right and duty to participate individually and collectively in the planning and implementation of their health care’ (WHO, 1978). Community participation, meaning ‘involvement in decision-making with regard to priority-setting, planning, implementation, and evaluation at local, national, and global levels’ (Haricharan et al., 2021: 2) is instrumental in service delivery governance and can encourage the accountability and needs-responsiveness of a health system (WHO, 1978; WHO, 2015). Such participation enhances equity and social justice. Similarly, health workers and policy-makers, because they are appointed to serve citizens, need to be responsive and accountable to those citizens. The Astana Declaration expands on the original Alma-Ata Declaration by describing the responsibilities of health providers more explicitly and mentioning the aspiration to ‘increase community ownership and contribute to the accountability of the public and private sectors for more people to live healthier lives in enabling and health-conducive environments’ (WHO, 2018). This also resonates with the recommendation by Kruk et al. (2018), in the Lancet Global Health Commission on High-Quality Health Systems, to promote health system quality by empowering people to hold systems accountable and actively seek high-quality care.
The post-apartheid South African government introduced a number of reforms to create channels for health system accountability and to expand the role of communities, but these channels did not function well in practice. The post-apartheid
Ronelle Burger, Andy Gray, Dumisani Hompashegovernment adopted community participation as part of a broader, continuing health system reform. The new, decentralised, preventative health system was intended to be a departure from the previous centralised, curative system (Haricharan et al., 2021). The White Paper for the Transformation of the Health System in South Africa (1997) stresses the importance of ‘the active participation and involvement of all sectors of South African society in health and health-related activities’, and the National Health Act 61 of 2003 provides for the establishment of health committees, hospital boards and district health councils. However, despite these reforms, the system remains centralised and top-down and often does not value and prioritise the needs of communities (NPC, 2012). The South African experience with hospital boards and clinic committees has been mixed, but the consensus in the literature is that in most cases the impact of these committees has been minimal (Haricharan et al., 2021). Complaints have been heard about the lack of political commitment, poor participation by facility managers, negative attitudes of health workers, inadequate resources, insufficient capacity and skills of committee members, and lack of clarity about the role and mandate of committees (Schneider et al., 2017).
In South Africa, the need for enhanced community ownership and provider accountability has become more urgent and pertinent after an era of government corruption and bureaucratic inaction under President Jacob Zuma. Commentators have interpreted the rising number of service delivery protests –reaching a peak between 2009 and 2013 – as evidence that communities are disgruntled and the available accountability channels are not perceived to be effective (Botes, 2018; Chenwi & Tissington, 2010).
There are at least three binding constraints (i.e. conditions that must be remedied or they will delay progress) that impede efforts aimed at making these channels more effective: the limited devolution of decision-making and power in the public health system, citizens’ feelings of disempowerment and low expectations of health providers, and the lack of timely access to information on local facilities, providers and environmental health local indicators. Devolution of power is crucial for local accountability, as hospitals and health facilities cannot be held to account when they do not have the authority to deal with citizens’ complaints. Citizens can only make effective use of the available accountability channels if they know their rights, know what they can expect of health services and environmental health standards, and feel empowered to speak out, knowing that their voices matter and can make a difference (Zwama et al., 2019). Accountability requires transparency, and accurate and updated local indicators to help communities and patients assess and evaluate local service provision and environmental health (Ebrahim & Weisband, 2007; Potts, 2008).
This chapter focuses on the third of these three binding constraints. The Lancet Global Health Commission on High-Quality Health Systems (Kruk et al., 2018) concluded that measurement is key to accountability and quality improvement. Many of the available indicators globally do not capture the processes and outcomes that matter most to people. In their report, the Commission called for fewer, but better, health system indicators. They found that information systems generate many metrics that produce inadequate insight at a substantial cost, including those on public expenditure and health worker time. Indicators on inputs are widely available but weakly related to the quality of care that patients receive. Similarly, indicators such as the percentage of births with skilled attendants do not reflect the quality of childbirth care and the Commission warns that this can encourage unwarranted complacency about progress in maternal and new-born health. To enhance accountability, they recommend that governments should provide a dashboard with a
broad set of health system performance indicators, updated annually. They propose that the set should cover health outcomes, people’s confidence in the health system, user experience, financial protection (such as out-of-pocket expenditure and affordability ratios) and measures of health inequality, equity and social justice. The Commission omitted environmental health indicators from their list, but this is clearly vital to include.
This chapter describes and evaluates advances in the availability of accurate and timely local health information in South Africa between 2015 and 2020 against the backdrop of calls for more community participation, improved health system responsiveness to community needs and priorities, and enhanced provider accountability. The chapter deals with both the public and the private health sectors, although most routine data sources predominantly cover public sector provision of health care services.
The term ‘accountability’ is now widely used in health policy statements and documents, as this concept is universally accepted as essential for good governance. However, the meaning of the term has been diluted through overuse and by imprecise and vague use as a proxy for good governance. The literature on accountability explains the concept as a provider’s obligations to the people who need its services, such as the obligations of a government to the country’s citizens, or a hospital to the patients. The government’s obligation derives from its election by citizens as their representative. In the case of medical service providers appointed by government, the obligation then is derived indirectly and stems from the government’s appointment of such providers, the providers’ contractual obligation to the government, the government’s obligation to the citizens, and the patients’ health needs. Providers can be contracted via salaried employment or via services rendered for a fee. The important point here is that while the government can contract out the delivery of a service, the responsibility for this service remains that of the government.
This responsibility implies that citizens (in the case of this chapter, patients) have the right to ask the state to explain why it made specific decisions and took certain actions. Citizens (patients) can assess and evaluate the decisions and actions of the state and use their voice to complain and call for reform, but also to give positive feedback, call for penalties or mobilise communities to demand reforms. Figure 16.1 illustrates these roles and relationships. In line with the framework proposed by the Lancet Global Health Commission on High-Quality Health Systems, we have placed citizens and patients at the centre of this diagram (Kruk & Pate, 2020).
Various institutional accountability support mechanisms can support, enhance and strengthen these accountability relationships. Media reporting can help to assess whether government and providers are meeting their responsibilities and giving prominence to patients’ grievances and reform agendas, making it more likely that their voices will be heard. Non-governmental organisations play a similar role, but using dif ferent channels. Both civil society and the media can make patients aware of their rights and what they can expect (and demand) from providers and the government. The ju dicial system can enforce accountability in cases where responsibilities and obligations have been acknowledged as legal rights. In South Africa, all three mechanisms have been used well and effectively (Levy, Hirsh, Naidoo & Nxele, 2021; Raith Foundation, 2020; Wasserman, 2020; Heywood, 2009; Pieterse, 2008).
Source: Authors’ diagram representing an overview of the literature
The framework shown in Figure 16.1 makes it clear how responsibilities and rights are linked to information. The information, in turn, allows for evaluation and assessment against selected indicators, by citizens, civil society and media. Transparency ensures that there is a firmer and more credible basis for these assessments and evaluations, enabling the verification of the empirical claims motivating grievances and demands.

Examining information and indicators from the point of view of governance and accountability is very different to simply considering whether the information and indicators are adequate for planning or decision-making purposes.
Table 16.1 explores the overlap between information and accountability. It first lists five criteria that information and indicators must meet to facilitate and promote the assessment and evaluation function of accountability. Firstly, the information or indicators need to be perceived as credible, reliable and accurate. Secondly, they need to be available regularly (at least yearly) to enable tracking over time. Thirdly, the timely release of data is crucial to ensure early detection of problems and a rapid response, and ideally there should be alignment between an indicator’s geographical aggregation and the likely sphere of influence for patients and citizens (such as facility or sub-district level). Fourthly, the indicators should ideally identify problems at the point where they emerge. For example, it is better to identify bad eating habits in children by an increase in child obesity than by an increase in diabetes 30 years later or cardiovascular disease 40 years later. The fifth, and possibly most demanding criterion is facility-level accountability. To satisfy this criterion we need indicators that capture facility performance. The concern here is that most health system indicators are influenced by the feeder community’s profile and are thus affected by poverty and social problems, making it difficult to find indicators that can assess health facility performance. For instance, if a facility has a high percentage of pregnant women accessing antenatal care late, this might be attributable to supply-side factors, such as long waiting times or nurses turning pregnant women away, or to demand-side factors, such as cultural beliefs or patients postponing pregnancy testing, or to a combination of demand- and
supply-side factors. Indicators with a large range of potential drivers are therefore less useful for promoting accountability.
The second group of accountability dimensions in Table 16.1 lists two criteria relating to patient voice. When patients share their assessments and evaluations of service delivery, their voices are more likely to be heard and their stories to travel further when they focus on indicators that are easy to interpret and understand and that matter to most people. An increase in a composite measure such as an index would, for instance, be difficult to interpret, while a rise in avoidable deaths among children under five is easily recognised as an indicator that matters.
Table 16.1 Required attributes of health system indicators to enhance accountability
Widely viewed as credible, reliable and accurate
Available at regular intervals, enabling tracking over time
Assessment and evaluation of provider quality and environmental health
Patients’ voices
Timely availability and available at local level to identify facilities that need support at an early stage
Indicators that allow early identification of health system weaknesses (e.g. proportion of people living with HIV/Aids on treatment who have undetectable viral load)
For assessing facility effectiveness: Clear measures of facility effectiveness that partly reflect community factors
Easy to understand and interpret meaning of the indicator
Clarity on why this indicator matters to communities and patient groups, and on how to improve it
Source: Authors’ diagram representing an overview of the literature
The South African health system has a large number of data sources. Routine adminis trative data, predominantly from the public sector, is collected via the District Health Information System (DHIS) to support decentralised decision-making (Heywood & Rohde, 2001). The DHIS was designed to provide facility staff with local-level feedback on service provision and changes in service needs and to track key targets (William son & Stoops, 2001). The system draws on the Core Health Indicators as summarised in the National Indicator Data Set (NIDS), including data on maternal health, child health, HIV and tuberculosis (TB). Information on TB was initially captured in parallel vertical electronic TB registers (ETR.net, and EDR.net for drug-resistant TB patients), but in 2014 the National Department of Health (NDoH) decided to integrate TB information into TIER.net (Three Integrated Electronic Registers),1 which was initially used for HIV services (Myburgh et al., 2020). Data from TIER.net are now integrated into the DHIS. Most of the information in the DHIS is available every month and at the facility level. Processing delays introduce lags in the availability of the DHIS data. Public access to the data is via formal request. Other data sources are PERSAL, an integrated personnel and salary system; Vulekamali (the National Treasury’s budget tracking data site and application programming interface); and Vulindlela, which tracks non-staff expenditure.
1 As proposed by the WHO’s three-tiered ART patient monitoring and evaluation strategy, the three tiers were a paper-based system, a non-networked electronic system and a networked electronic system.
Information and indicators for accountability
The data on the private health sector is patchy and fragmented. It is often not comparable across providers and its indicators are rarely comparable to those of the public sector. Its key indicators, such as surgery success rates or mortality rates, are rarely publicly accessible. Much of the routine data produced by providers and medical schemes is generated for accounting or billing and not primarily clinical purposes. An important private health markets data source is the Council for Medical Schemes, which provides aggregated membership and claims data (CMS, 2020). One of the intermediaries, Mediscor, provides public access to the pharmaceutical utilisation data of a large subsample of medical scheme beneficiaries (Mediscor, 2020). The pharmaceutical industry relies on sales volumes data provided by companies such as IQVIA. The Medicines Price Registry website tells consumers the maximum fee they should be paying for medicines (based on government fee schedules) and lists more affordable generic alternatives.
In addition to these administrative data sources, several household surveys provide useful information on access to health services and health outcomes from a citizen and patient perspective. These include demographic surveys such as the 1998, 2003 and 2016 Demographic and Health Surveys, nutrition surveys such as the 2013 SANHANES (South African National Health and Nutrition Examination Survey), and general household surveys with health modules such as the longitudinal National Income Dynamics Study 2008 to 2017, the Statistics South Africa General Household Surveys 2002 to 2018, the 2001 and 2011 Census and the 2007 and 2016 Community Surveys.
The rest of this section outlines six significant information innovations or reforms that can strengthen the health system and make it more accountable: the rapid local data release in response to the pandemic, the Stock Visibility System (SVS), the Centralised Chronic Medicines Dispensing and Distribution (CCMDD) programme, the public release of Office for Health Standards Compliance inspection reports, the Western Cape Provincial Health Data Centre, and the Ritshidze project.
While routine data sets from the above sources are traditionally released only after a considerable time lag, during the COVID-19 pandemic when timely information was vital, information systems were adjusted and innovated to enable rapid collation, cleaning, analysis and release of data into the public domain. The National Institute for Communicable Diseases (NICD) has been developing its electronic app for national surveillance of Notifiable Medical Conditions since 2017, but the COVID-19 pandemic provided an opportunity to showcase the benefits of monitoring trends with minimal delays. The NICD’s DATCOV hospital surveillance system was developed in response to the need to track trends in COVID-19 hospitalisations and study COVID-19 hospitalisation risk. These efforts to provide timely and reliable evidence for public decision-making demonstrate the value of transparency, ease of access, timeliness, and the integration of public and private health systems. It is, however, concerning that the Medical Research Council’s estimation of excess deaths (i.e. the share of deaths that is above expectation based on previous data) suggests that the system could be missing a large share of COVID-19 mortality (MRC, 2021). While not all excess deaths would be COVID-19 deaths, the strong correlation between these excess deaths and the official
COVID-19 mortality statistics provides a compelling case for interpreting the majority of the excess deaths as being due to the pandemic. Assuming such an interpretation, missed cases would be attributed mainly to misreporting or patients not being tested for COVID-19.
In addition to innovative surveillance systems, there were rapid social surveys tracking hardship and unemployment during the pandemic. Surveys such as the National Income Dynamics Study Coronavirus Rapid Mobile Survey (NIDS-CRAM) and the Human Sciences Research Council and University of Johannesburg COVID-19 Democracy Survey generated rapid but credible aggregated data on how the pandemic and the lockdown affected unemployment and social problems and changes in life circumstances, health beliefs and health behaviour. They helped to amplify the voices of citizens and enhanced responsiveness to citizens and their needs during the pandemic. Surveys such as this normally take three years from conceptualisation to public release, going through the stages of procurement of funding, ethics application, questionnaire design, contracting of survey firms, data gathering, data cleaning and curation, and writing of reports. However, in the case of NIDS-CRAM, tight deadlines, high levels of commitment and running parallel processes enabled the team to plan, fund, conduct, analyse and release their survey in less than four months. Such rapid surveys have been helpful in shaping the social policy response to the increased hardship following the pandemic and lockdown.
Since the initiation of the COVID-19 vaccination programme in May 2021, daily updates on the number of vaccine doses administered per province, in both the public and private sectors, have been posted on the South African Coronavirus website,2 and the South African Health Products Regulatory Authority (SAHPRA) has provided reports on adverse events after immunisation with the COVID-19 vaccines.3
The NDoH’s SVS is another example of how improved information can facilitate responsiveness. Since its launch in 2014, this cloud-based reporting system has been rolled out to more than 3 500 clinics. Designed to track the availability of medicines, it is paired to a smartphone mobile app that can capture and upload information on the availability and expiry rates of a facility’s medicines. The aim of this system is early detection to minimise drug stock-outs. It sends the staff reminders about weekly stock updates and flags problems according to an escalation protocol. The app can also be used to order and receive medicine. There are no data costs associated with using the app, as it works via a zero-rated channel. The system has now been combined with stock management data, under the overarching system referred to as the National Surveillance Centre. This data can be used to assess the use of particular medicines. For example, the National Policy Framework and Strategy on Palliative Care (2017–2022) includes an indicator of morphine consumption per district health service headcount. The indicator’s usefulness was demonstrated by a pharmacy student project at the University of KwaZulu-Natal (Dhoodat et al., 2017), which showed that public sector oral morphine use in 2016 ranged from 2.8mg per 100 of those visiting the public sector for ambulatory care (in the rural Umzinyathi district) to 156.2mg (in the urban uMgungundlovu district). Subsequent student projects (Akoonjee et al., 2019;
1 See https://sacoronavirus.co.za/latest-vaccine-statistics/
2 See http://aefi-reporting.sahpra.org.za/
Andrew et al., 2020) have shown how antimicrobial use has varied between districts in KwaZulu-Natal and how tramadol use has changed over time, using the same data sources (depot and direct delivery issues to health facilities, normalised by the estimated uninsured population per district).
The then Minister of Health, Aaron Motsoaledi, reported that in 2014 and 2015 the number of stock-outs for antiretrovirals, TB medicines and vaccines decreased in KwaZulu-Natal by 46%, 49% and 14%, respectively, and in Limpopo by 66%, 49% and 42%%, respectively (Motsoaledi, 2016). By August 2019, more than 90% of facilities were regularly reporting their stock levels on the SVS (McKenzie & McCann, 2016).
Given this chapter’s focus on health system responsiveness, it is important to note that the SVS was introduced by the NDoH in response to persistent advocacy by non-profit organisations (NPOs), under the umbrella of the Stop Stockouts Project (SSP).4 The NPOs involved in this programme were Section27, Médecins Sans Frontières, the Southern African HIV Clinicians Society, the Rural Doctors Association of South Africa, the Rural Health Advocacy Project, and the Treatment Action Campaign. The NPOs drew attention to the frequent stock-outs of vital medicines and the adverse consequences of these stock-outs. As part of the SSP, the NPOs trained community members on their health rights, set up a hotline to report local stock-outs and persuaded the NDoH to run an annual survey to track the levels of drug stock-outs at their facilities (McKenzie & McCann, 2016).
The launch of the CCMDD programme was also a notable milestone for patient-centred care. This programme is a dispensing operation that allows stable chronic patients to collect their medication from a public health facility express queue, a private provider, or designated community-based pick-up points (PUPs) such as churches, community halls or a Pelebox. The Pelebox is a smart locker technology which uses the patient’s mobile phone number and a one-time PIN sent to the mobile phone as a security measure. It flags patients who have failed to collect their medicine and are at risk of defaulting, which facilitates improved patient management. The centralised dispensing function is performed by a contracted pharmacy, using state tender stock funded by the participating provinces (all except the Western Cape, which had previously contracted its own centralised dispensing unit). Although the number of patients served by the programme can be shown per disease, these data are difficult to interpret, as the percentage of patients referred to the centralised service is unknown.
The programme was first trialled at 10 of the 11 National Health Insurance (NHI) pilot districts in 2014 (excluding Eden). In 2016 it expanded nationally. By 2019, 3 436 facilities had registered as part of the programme. At this point, the programme covered 88% of South Africa’s districts, with the remainder covered by the Western Cape Chronic Dispensing Unit. Patients were collecting medication from more than 2 000 external PUPs by the end of 2019. More than 2 million patients were enrolled in the programme, of whom 76% were on ART (Liu et al., 2021).
4 Previously the District Health Information System (DHIS) had an indicator, now no longer collected, which was based on the availability of a tracer list of drugs at health facilities. Day (2014) showed that the data from the two sources were correlated.
The programme has yielded substantial benefits for both patients and the health system. Long waiting times and inconvenient opening times can impede medicine collection and treatment adherence (Dorward et al., 2020). Thus, by dramatically reducing the time cost associated with collecting chronic medication, the programme is removing the obstacles to patient adherence. Private providers often have extended hours of operation, allowing working patients to collect their medicine over weekends. Better adherence should affect disease progression, quality of life, the demand for acute care, and particularly hospitalisation. This decanting lightens the load on overburdened public health facilities and is expected to benefit patients who use these facilities.
The OHSC was established in 2013 as an independent quality regulator mandated to assess the quality structures, processes and outcomes of health establishments against pre-determined standards. It has three functions: it inspects facilities, certifies them, and enforces compliance with prescribed standards. It publishes the scores from its facility inspections in its annual inspection reports, providing both facility-level scores and aggregates from functional areas, per province.
The release of the OHSC’s inspection reports since 2016 represents a significant stride ahead in the pursuit of quality health services and accountability (OHSC, 2016). The 2016/2017 inspection report found that only seven of the 649 public sector facilities visited complied with standards. A score of 80% was the cut-off point for compliance (OHSC, 2017). By 2019, there had been little improvement, with nine of the 730 public sector facilities complying with standards without any qualification or condition, and a further 155 facilities (21%) being classified as compliant with a qualification or condition. It is concerning that 248 facilities (34%) were non-compliant and 103 (14%) critically non-compliant (OHSC, 2020). As from 20225, the OHSC will include private hospitals in its compliance investigation schedule. The target in 2022/23 is to inspect 52 private health facilities (12% of the total number).
The South African Lancet Health Commission report on Health System Quality (2019) positioned the OHSC as an important role player in promoting the quality of care in the South African health system. However, the report acknowledges that the understaffed OHSC would require more teeth to fulfil this role effectively. The OHSC has faced considerable scrutiny and criticism, and much of this may be due to its prominent and expanded role under the NHI. The OHSC will monitor compliance with the standards by public and private health care practitioners who contract with government to provide services to members of the public. In monitoring compliance, it will issue certificates to health care facilities as a public guarantee of compliance.
There are concerns that the indicators tracked by the OHSC do not have a clear link to health outcomes (Mabaso, 2016), and a disproportionate share of these are bureaucratic tick boxes that represent inputs and necessary conditions – or ‘structure variables’ in the Donabedian (2005) framework for measuring health care quality. This is a concern, because health systems should not be assessed on the basis of inputs such as the number of doctors or the number of clinics or the number of medicines dispensed.
Inputs rarely matter to patients. What matters is how well systems perform and whether they meet needs. What matters to patients is recovering from illness and being treated with care and respect (Kruk, 2018; The Lancet, 2018). Currently, the OHSC inspectors only interview a small sample of patients per facility (OHCS, 2016).
Although administratively linked to the OHSC, the Office of the Health Ombud has a distinct and independent responsibility to receive complaints from members of the public about the quality of service they receive from medical facilities and to carry out a systematic inquiry. The South African Lancet Health Commission report on Health System Quality (2019) flagged the lack of independence of the Health Ombud, who relies on the staff of the OHSC, as a concern.
The PHDC supports clinical care by providing transparent real-time clinical data to providers, and indicators to track treatment adherence and patient management. To set up the centre, patient-level clinical data across various information systems had to be consolidated. Patient registration was digitised, a unique identifier was implemented across the various data systems, and there was standardisation of the capture of information across core administrative systems in hospitals and clinics (Boulle et al., 2019). The data centre links almost two dozen sources of data to track the patient’s health journey over time. During the pandemic, this rich data set was used to administer a telemedicine service, identifying and managing high-risk COVID-19 cases with comorbidities (David et al., 2021). The PHDC enabled the early assessment of the association between HIV and severe COVID-19 outcomes, at the time a key uncertainty on how COVID-19 would be experienced in the region, as well as the exploration of COVID-19 in diabetic patients (WCDoH & NICD, 2021; Dave et al., 2021). The centre links data on case detection, laboratory assessments, treatment access and outcomes and can access this data with minimal delays, which allows it to function as both a shared electronic health record (through a web-based Single Patient Viewer application) and as a surveillance system for specific diseases (Boulle et al., 2019).
The PHDC team ascribes the success of the centre to the prioritisation of clinical care support. This enabled them to demonstrate, at an early point in the project, the centre’s value to clinical teams at the facilities. This is vital, as it is these teams who are doing the work of capturing patients’ clinical data, and it ensures continual improvement of the systems due to the ongoing scrutiny of consolidated records at an individual patient level. This approach is in contrast to the typical data improvement project, driven by researchers or funders, where data completeness and fidelity are often uncertain, and new data collection is frequently a once-off aggregate exercise providing no direct benefit to patients or providers
Although the Ritshidze project was not motivated by the pandemic (launched in December 2019), it deserves a mention because it is also innovative. The initiative has the primary aim of using data to boost citizen voices to hold government and aid agencies accountable for inadequacies in TB and HIV prevention, diagnosis and treatment. Community members collect information on TB and HIV public primary care services from local sites. The data is analysed, solutions are explored for the problems identified, and the proposed problems and solutions then serve as a platform for advocating for improved health services in the community. At the time of writing this chapter, the Mpumalanga, Free State, Limpopo, North West, Eastern Cape, KwaZulu-Natal and Gauteng provincial reports had been released.6
The Ritshidze project is based on a community-led monitoring system that takes place quarterly at 400 clinics and community health care centres across 27 districts in 8 provinces. The project looks at several health care indicators that include facility hours and waiting times, clinic conditions, access to medicines and shortages, contraception services and access, and HIV-related services. Figure 16.2 shows responses from patients regarding indicators of medicine shortages. The data for the figure is based on 1 037 responses from public health care facilities in seven provinces (Eastern Cape, Free State, Gauteng, KwaZulu-Natal, Limpopo, Mpumalanga, and North West). From the graph, it is clear that contraceptives (43%) are most often reported to be in short supply, followed by HIV medicine (14%) and vaccines (13%).
The six information innovations or reforms outlined above have helped to improve South Africa’s health system, moving it towards the gains anticipated by government’s ambitious 2019 National Digital Health Strategy. The response to the COVID-19 pandemic has shown not only that rapid data collection can promote transparency and evidence-based decision-making, but also that timely indicators are feasible and may have helped to shift expectations and norms. Despite the Promotion of Access to Information Act 2 of 2000 (PAIA), too few public and private health data sets are made available to the public in a timely manner. In South Africa, many data sets of public importance are accessible in principle, but effectively protected from widespread scrutiny by long-drawn-out or unpredictable bureaucratic processes. In many other countries the same data is downloadable from government websites without any paperwork being required. As much as legislation can enable access, it can also hamper needed access when interpreted too narrowly. The Protection of Personal Information Act 4 of 2013 (POPIA) has specific provisions that enable the ‘further processing’ of personal information gathered for one purpose, for example to ‘to prevent or mitigate a serious and imminent threat to … public health or public safety’. Despite this, the Act is frequently cited as a reason to deny access to personal information. In South Africa, data is sometimes released only after a lengthy waiting period. Recent examples of long delays in data release have been the Demographic and Health Survey (25 months), the National TB Prevalence Survey (19 months) and the National Immunisation Coverage Survey (not yet released, although the fieldwork ended in June 2019). The rapid surveys and surveillance systems set up during the pandemic demonstrated not only the value of timely data, but also that the processes of data cleaning, preparation, curation and analysis can be compressed.
The SVS and the CCMDD programme support the management and dispensing of medicine and yield useful information on the availability of medicine and collection of prescriptions. However, there is still no information on the percentage of patients receiving the right medication. In 2017, the Lancet Commission on Essential Medicines Policies called for the establishment of ‘independent pharmaceutical analytics units’, specifically to ‘focus on generating information for action to promote quality use’. The Commission highlighted the lack of attention to access to essential medicines, their affordability and quality, and their correct use, in the reports on the Millennium Development Goals and Sustainable Development Goals, and also in the World Health Statistics. A set of 24 indicators were proposed to measure progress. Nationally, we have seen some progress with the National Surveillance Centre data, which is reported to district level and is being used in at least some provinces. However, this data is rarely placed in the public domain, hence its quality has not been the subject of independent review. The Centre’s work does, however, show how greater reliance on routine data can be facilitated by new technologies, including mobile applications (Simão et al., 2018).
Arguably the most serious shortcoming of the current set of health system indicators is the shortage of information on health system performance: the components that would be called ‘process and outcomes variables’ in the Donabedian quality of care model (2005). Overwhelmingly, the health information available provides a window
on health system inputs – or ‘structure’ in the Donabedian model. Very little data is available on outcomes. For instance, despite myocardial infarctions being a large part of the country’s disease burden, we do not have public data on how many occur each year, what percentage are fatal and how well hospitals manage them. The shortage of data on the process and outcomes dimensions of health care is a serious deficiency in an era of evidence-based decision-making. It often means that performance management and planning and policy processes are blind to these dimensions.
The CCMDD programme provides some indirect information on chronic diseases, but more is needed. Except for HIV, where we have the ART cohort data set, there is also little information on control of chronic diseases. Modelled estimates of the extent of hypertension and diabetes control have been included in the Universal Health Coverage Service Coverage Index (UHC SCI), calculated for South African provinces and districts (Day et al., 2021). The CCMDD data can be used to track the dispensing and collection of hypertension medication, however, without a suitable denominator, the percentage of patients diagnosed with hypertension who are on medication cannot be determined. Moreover, aggregated data on the use of medicines cannot be used to assess drug adherence, evaluate drug safety, or compare outcomes for different drug treatments. Longitudinal data is essential to track patients across the system to examine continuity of care and the quality of patient management. The Western Cape PHDC has demonstrated the benefits of such capability. The Depart ment of Health has been investing in an electronic health record system since 2014 and has also committed to system interoperability with its 2014 National Health Norma tive Standards Framework for Interoperability in eHealth. More than 44 million people have been registered on the government’s electronic health record system (Ramaphosa, 2020).
Aggregate data can also obscure differences at small area level, such as sub-districts or individual facilities. We thus need to disaggregate the available data in various ways, as noted by the Lancet Commission report on the future of health in sub-Saharan Africa, in order to enable local accountability and monitoring processes.
Finally, there is also a shortage of data on the contribution of social and environmental factors to health outcomes, including education, social development, nutrition, water quality, air quality, sanitation and housing. It is crucial to invest in intersectoral data systems to promote and deepen the understanding of the social determinants of South Africa’s burden of disease. The planned revival of the Blue Drop and Green Drop reporting systems on water and sewerage, respectively – launched in 2009 but disbanded in 2014 – is an example of such an initiative. According to the Department of Water and Sanitation’s 2019 Water and Sanitation Masterplan, 44% of the water treatment works and 56% of the waste water treatment works were classified as not working properly (DWAF, 2019:19).
The projects and initiatives described in this chapter show how information system improvements, the public release of data and rapid local data can create pathways to strengthen accountability and enhance the responsiveness of the health system. The provision of information to communities is vital for promoting accountability. Rapid and credible data can help amplify patients’ voices and make the health system more responsive. Such data will empower patients and raise their expectations regarding the quality of care. These improvements inspire optimism, and chart the way forward.
The following are some reforms that should take priority in future. Greater transparency could be achieved by introducing norms and standards about expected delays in the public release of data. Obstacles to easy public access to data should be eliminated. There should be intersectoral collaboration in tracking social and environmental determinants of disease. The Core Health Indicators should be expanded to include more indicators that can track health system performance and more indicators of chronic disease prevalence and chronic disease patient management (such as hypertension and diabetes control, and treatment adherence). Expansion of the Core Health Indicators would imply a strategic commitment of the NDoH to invest in systems that can collate different data sets to make it possible to track patients across the health system. Today’s innovations in digital health records and rapid data have made it possible to access more timely feedback on how users are experiencing policies and programmes, thus helping to detect design and implementation problems at an early stage and fine-tune these initiatives.
In this chapter we mapped the progress with expanding the information available to document and track local health services and outcomes. Such information will however only strengthen downward accountability if local stakeholders (such as civil society groupings or patient organisations) are aware of it, and use it effectively to draw attention to local problems and lobby for solutions. In this way the information can then empower communities to ensure that primary health care facility staff and district-level decision-makers are held accountable. However, it is vital to acknowledge that this will not happen automatically, and will require substantial effort and investment by advocacy groups and community leaders.
Akoonjee A, Ali M, Jhazbhay A. Antimicrobial utilisation in the KwaZulu-Natal public sector – differences between districts. BPharm project, UKZN, 2019.
Andrew E, Gwamanda S, Haniff A, Magwaza S, Mnisi N. Teeluck S. Tramadol utilization within the districts of the KwaZulu-Natal public healthcare sector. BPharm project, UKZN, 2020.
Boulle A, Heekes A, Tifin N, et al. Data Centre Profile: The Provincial Health Data Centre of the Western Cape Province, South Africa. International Journal of Population Data Science. 2019;4(2):05. DOI: 10.23889/ijpds.v4i2.1143.
Botes L. South Africa’s Landscape of Social Protests: A Way Forward for Developmental Local Government? African Journal of Public Affairs. 2018;10(4):214–256.
Chenwi L, Tissington K. ‘Engaging Meaningfully with Government on SocioEconomic Rights: A Focus on the Right to Housing.’ Socio-Economic Rights Project, Community Law Centre, University of the Western Cape 7. 2010.
CMS (Council for Medical Schemes). Annual Report Council for Medical Schemes. 2020. Pretoria: Council for Medical Schemes. Available from: https:// www.medicalschemes.co.za/publications/#2009-3506-wpfd-2019-20-annualreport.
Dave JA, Tamuhla T, Tiffin N, Levitt NS, Ross IL, Toet W, Davies MA, Boulle A, Coetzee A, Raubenheimer PJ. Risk factors for COVID-19 hospitalisation and death in people living with diabetes: A virtual cohort study from the Western Cape Province, South Africa. Diabetes Res Clin Pract. 2021 Jul;177:108925. doi: 10.1016/j.diabres.2021.108925. Epub 2021 Jun 21. PMID: 34166703; PMCID: PMC8215881.
David NJ, Brey Z, Ismail M. Telemedicine in the Western Cape Department of Health during the first peak of the COVID-19 pandemic: Leveraging data to save lives by activating a telemedicine response. Afr J Prim Health Care Fam Med. 2021 May;20;13(1):e1–e4. doi: 10.4102/phcfm.v13i1.2954. PMID: 34082548; PMCID: PMC8182462.
Day C, Gray A, Cois A, Ndlovu N, Massyn N, Boerma T. Is South Africa closing the health gaps between districts? Monitoring progress towards universal health service coverage with routine facility data. BMC Health Services Research. 2021;21(Suppl 1):194.
DWAF (Department of Water and Sanitation). Water and Sanitation Masterplan. 2019. Pretoria: Department of Water and Sanitation. Available: https://www.gov.za/ sites/default/files/gcis_document/201911/national-water-and-sanitationmaster-plandf.pdf
Dhoodat N, Limalia N, Moloto C, Magubane M, Pillay M. Opioid utilization in the public sector of KwaZulu-Natal in 2016. BPharm project, UKZN, 2017.
Donabedian A. Evaluating the Quality of Medical Care. The Milbank Quarterly. 2005;83(4):691–729.
Dorward J, Msimango L, Gibbs A, et al. Understanding how community antiretroviral delivery influences engagement in HIV care: a qualitative assessment of the Centralised Chronic Medication Dispensing and Distribution programme in South Africa. BMJ Open. 2020;10:e035412. doi: 10.1136/bmjopen-2019-035412
Information and indicators for accountability
Ebrahim A, Weisband E. Introduction: Forging Global Accountabilities. In Ebrahim, A. & Weisband, E. (eds). Global Accountabilities: Participation, Pluralism and Public Ethics Cambridge, U.K.: Cambridge University Press. 2007.
Haricharan HJ, Stuttaford M, London L. Effective and meaningful participation or limited participation? A study of South African health committee legislation. Primary Health Care Research and Development. 2021;22(e28):1–8. https://doi. org/10.1017/S1463423621000323.
Heywood A, Rohde J. Using information for action. A manual for health workers at facility level. Arcadia, Pretoria: The Equity Project, 2001.
Heywood M. South Africa’s Treatment Action Campaign: Combining Law and Social Mobilization to Realize the Right to Health. Journal of Human Rights Practice. 2009;1(1):4–36. https://doi.org/10.1093/jhuman/hun006
Kruk, M.E. 2018. Q&A: Margaret Kruk, Improving Health Care Quality in ResourcePoor Countries. Harvard Public Health Magazine.
Kruk ME, Gage AD, Arsenault C, et al. High-quality health system in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health Commission. 2018;6(11): e1196–e1252.
Kruk ME, Pate M. The Lancet Global Health Commission on High-Quality Health System 1 year on: Progress on a Global Imperative. The Lancet Global Health. 2020;8(1): e30–e32.
The Lancet. Editorial: Putting quality and people at the centre of health systems. The Lancet. 2018;392(10150):795. doi: 10.1016/S0140-6736(18)32064-6.
Levy B, Hirsch A, Naidoo V, Nxele M. South Africa: When Strong Institutions and Massive Inequalities Collide. March 2021. https://carnegieendowment.org/ files/202103-Levy_etal_SouthAfrica.pdf
Liu L, Christie S, Munsamy M, Roberts P, Pillay M, Shenoi SV, Desai MM, Linnander EL. Expansion of a national differentiated service delivery model to support people living with HIV and other chronic conditions in South Africa: a descriptive analysis. BMC Health Serv Res. 2021 May 17;21(1):463. doi: 10.1186/s12913-02106450-z. Erratum in: BMC Health Serv Res. 2021 Jun 4;21(1):549. PMID: 34001123; PMCID: PMC8127180.
Mabaso K. External Quality Assessment of health facilities in South Africa: Strengths appraised and gaps identified. PhD dissertation, University of Oxford. 2016. McKenzie A, McCann T. Evaluation of the Stop Stockouts Project (SSP), South Africa. 2016.
MRC (Medical Research Council). Report on Weekly Deaths in South Africa. 2021. Mediscor. Medicines Review. Centurion: Mediscor. 2020. Available from: https://www. mediscor.co.za/wp-content/uploads/2020/09/Mediscor-MedicinesReview-2019.pdf
Motsoaledi A. Address by Minister of Health, on the occasion of the Stock Visibility System for the improved access and availability of essential medicines in South Africa launch, Midrand (14/07/2016).
Myburgh H, Peters RPH, Hurter T, Grobbelaar CJ, Hoddinott G. Transition to an in-facility electronic Tuberculosis register: Lessons from a South African pilot project. South Afr J HIV Med. 2020;21(1):1025. Published 2020 Jan 16. doi:10.4102/sajhivmed.v21i1.1025.
NDoH (National Department of Health). The White Paper for the Transformation of the Health System in South Africa. 1997. Available from: https://www.gov.za/ sites/default/files/gcis_document/201409/17910gen6670.pdf
NPC (National Planning Commission). National Development Plan 2030: Our future - make it work. Pretoria: National Planning Commission. 2012.
OHSC (Office of Health Standards Compliance). National Core Standards Part 2: Assessment tools and methods. 2016.
OHSC. Annual Inspection Report 2015/16. Pretoria: Office of Health Standards Compliance; 2017.
OHSC. Annual Inspection Report 2016/17. Pretoria: Office of Health Standards Compliance; 2018.
OHSC. Annual Inspection Report 2018/19. Pretoria: Office of Health Standards Compliance; 2020.
Pieterse M. Health, Social Movements, and Rights-Based Litigation in South Africa. Journal of Law and Society. 2008;35(3):364–388. https://www.jstor.org/ stable/40206853
Potts H. Participation and the Right to the Highest Attainable Standard of Health. Colchester: Human Rights Centre; University of Essex. 2008.
Raith Foundation. Critical Reflections on the Social Justice Sector in the Post-Apar theid Era. 2020. Available from https://tinyurl.com/SJSReviewReport.
Ramaphosa C. State of the Nation Address by President Cyril Ramaphosa, Parliament, Cape Town, 13 Feb 2020. Available: https://www.gov.za/speeches/ president-cyril-ramaphosa-2020-state-nation-address-13-feb-2020-0000.
Schneider H, McKenzie A, Schaay N, Scott V, Sanders D. Primary Health Care Systems (PRIMASYS): Case study from South Africa. Geneva. 2017.
Simão M, Wirtz VJ, Al-Ansary LA, Hill S, Grove J, Gray AL, Nannei C, Hedman L, Das P, Hogerzeil H. A global accountability mechanism for access to essential medicines. Lancet. 2018;392(10163):2418–2420.
South African Lancet National Commission. Confronting the Right to Ethical and Accountable Quality Health Care in South Africa: A Consensus Report. 2019. Pretoria: National Department of Health.
South African National Department of Health. National Digital Health Strategy for South Africa, 2019–2024. 2019. Available from: www.health.gov.za Wasserman H. 2020. The state of South African media: a space to contest democracy. Publizistik. 2020 Jul;2:1–15. doi: 10.1007/s11616-020-00594-4
WHO (World Health Organization). Declaration of Alma-Ata. The International Conference on Primary Health Care in Alma-Ata, USSR. Geneva. 1978. Available from: https://www.who.int/publications/almaata_declaration_en.pdf
WHO (World Health Organization). WHO Global Strategy on People-Centred Integrated Health Services: Interim Report. In Service Delivery and Safety. 2015. Retrieved from www.who.int
WHO (World Health Organization). Declaration of Astana. The Global Conference on Primary Health Care in Astana, Kazakhstan. 2018. Available from: https://www. who.int/docs/default-source/primary-health/declaration/gcphc-declaration.pdf
Zwama G, Stuttaford MC, Haricharan HJ, Douglas J. Rights-Based Training Enhancing Engagement of Health Providers with Communities, Cape Metropole, South Africa. Frontiers in Sociology. 2019;4(April):1–12. https:// doi.org/10.3389/fsoc.2019.00035
Western Cape Department of Health (WCDOH) in collaboration with the National Institute for Communicable Diseases, South Africa (NICD). Risk Factors for Coronavirus Disease 2019 (COVID-19) Death in a Population Cohort Study from the Western Cape Province, South Africa. Clin Infect Dis. 2021 Oct 5;73(7):e2005–e2015. doi: 10.1093/cid/ciaa1198. PMID: 32860699; PMCID: PMC7499501. Williamson L, Stoops N. Using information for health. In: Ijumba P (ed), South African Health Review 2001. Durban: Health Systems Trust, 2001: 101–116.
The chapter touches on the previous national Human Resources for Health (HRH) strategy, launched in 2011, reviews progress with implementation of HRH interventions and reflects on the likely implications for HRH of future health system reforms, in particular the National Health Insurance (NHI) Bill. The chapter then reviews the problems related to inadequate HRH data for planning and monitoring progress. The implications for formalisation of Community Health Workers (CHWs) are considered, as is progress in strengthening leadership across the health system. A summary of the recently completed HRH strategy is provided. Some of the main HRH challenges are outlined, including dealing with the consequences of the COVID-19 crisis.
In 2016, the Global Strategy on Human Resources for Health: Workforce 2030 was adopted by the 69th World Health Assembly (WHA69.19), which explicitly highlighted equitable access to health workers. This was followed by the report of the United Nations High-Level Commission on Health Employment and Economic Growth (HEEG) in September 20161, which highlighted that investments in education and job creation within the health and social sectors result in a triple return of improved health outcomes, global health security, and inclusive economic growth. The HEEG report made the following recommendations:
(1) stimulate investments in creating health sector jobs (for women and youth) with the right skills, numbers and location;
(2) maximise women’s economic participation and foster their empowerment through leadership and addressing gender biases and inequities in education and the health labour market;
(3) scale up transformative, high-quality education and lifelong learning to match skills with the health needs of populations;
(4) reform service models that focus on hospital care and focus on underserved areas;
(5) harness the power of cost-effective information and communication technologies to enhance health education, services and information systems;
(6) ensure investment in the International Health Regulations core capacities with skills development of national and international health workers along with protection and security of all health workers and facilities.
The plan proposes goals and the strategic approach and activities with which the International Labour Organization (ILO), Organisation for Economic Co-operation and Development (OECD) and World Health Organization (WHO) can support and facilitate country-driven implementation of the Commission’s recommendations, reinforce the implementation of the Global Strategy on Human Resources for Health: Workforce 2030, and concomitantly optimise the path for achieving the 2030 Agenda for Sustainable Development, including Universal Health Coverage (UHC).
However, there has been limited progress on HRH globally and the world’s health workers bear undue impact of the pandemic. It has only become more evident how critical the health workforce is to health systems and achieving improved coverage. Additionally, simple availability of health workers does not ensure accessibility. It is only when there are enough health workers who are adequately skilled and equipped (with right tools and technologies), equitably distributed and who are motivated and empowered to deliver quality health care that is appropriate, that they adequately support the health system.
In 2011, the Minister of Health launched the South African Human Resources for Health (HRH) Strategy for the Health Sector 2012/13–2016/17. She stated: ‘Improving human resource planning, development and management is instrumental in the overhaul of the health system. It is a strategic intervention whose activities will contribute significantly to improved health outcomes. Compensation of employees is one of the biggest cost drivers in any institution ... Therefore, as the most expensive asset, we have to manage human resources prudently ... this means that the health sector has to be staffed by an appropriately skilled workforce that is able to respond to the burden of disease and citizens’ expectations of quality service’ 2
HRH planning is intricate because it is dependent on a range of factors, including what services need to be provided (e.g., community vs facility-based; fixed vs mobile) and how and who will provide them and what skills are required. HRH planning, estimation and forecasting is crucial to planning training pipelines, service delivery and budgets, each of which comes with challenges. Planning of training pipelines is difficult due to the long lead times to graduate professionals, interdigitating with the choices on scope of practice, the changing epidemiology and technology and the rate of turnover of staff.
Projections of the total numbers per category required and their unit costs are important for budgeting purposes. The way in which wages are set or determined is a crucial consideration which affects government’s control over unit costs. Planning
numbers faces the complexity in giving empirical content to health needs. Benchmarks or standards and norms are therefore often used in HRH planning to provide comparators for adequate provisioning. Ono et al. have found that the Netherlands, Australia, United Kingdom and especially Japan are incomparable in their HRH planning, data collection approaches, and models used.3 However, their conclusions are not generalisable to South Africa. The usefulness for South Africa of the few documented HR planning case studies and literature from comparable peer countries, such as other African or upper-middle-income countries3 has been contested, as such ratios are always conditional on modes of delivery and services packages. However, local and context-specific engagement on adequate health worker ratios, which involves multiple stakeholders and experts can overcome this problem. The wide disparities in vulnerability and remoteness between South African communities should lead to some variation based on the community.
In the quinquennium under review there was important formative work on HRH planning, estimating need and forecasting, particularly in the preparation of the South African HRH Strategy 2030.
Reliable data is essential for effective HRH planning. While there are several sources that have databases available for the health workforce in South Africa, unfortunately none are complete (Table 17.1). Thus, an HRH planning exercise may require compilation and analysis of more than one database. A big challenge is that, barring the Statistics South Africa population statistics, none of the databases are available in the public domain. In the 2015–2020 quinquennium an initiative to merge data sources into a useable tool was initiated.
Table17.1 Available data sources for HRH planning in South Africa
Data Sources Database variables available Database variables absent
Health Professions Council of South Africa (HPCSA)4 and other pro fessional councils
Personnel and Salaries management system (PERSAL)
Board of Healthcare Funders (BHF)
Colleges of Medicine of SA (CMSA)
Council for Medical Schemes (CMS)
District Health Information System (DHIS)
Demographic and Health Surveys (DHS)
Registration data of health work force – Age, location, race, gender, etc.
Public–private split absent. Includes non-practicing professionals and those overseas
Government payroll information Does not identify any field of specialisation
Practice numbers (enabling health care providers to claim from health funders)
Examination data on specialist fellowships. Includes demographic data
Information on use of professionals in the private sector
Information on nurse workloads, hospital volumes and disease profiles
Helpful for population health needs and for triangulation of visits
National Income Dynamics Survey (NIDS) Data on factors such as visits to clin ics, and private sector consultations
No other HRH data
--
Department of Higher Education and Training (DHET)
Stats SA – General Household Survey (GHS)
Data on number of enrolments and graduates
Social determinants of health; access and use of health services
Stats SA – Population Statistics5 Demographic indicators
The HRH planning studies that have been undertaken previously tended to be limited to a few major health workforce categories, such as doctors, medical specialists, CHWs and nurses (Table 17.2). There has been no study estimating or forecasting the entire health workforce of South Africa (especially not for the support staff such as cleaners, laboratory technicians and ambulance drivers).
Human Resources for Health in South Africa –A draft strategy
Updated General Practitioner (GP) and Specialist Numbers for SA
The Human Resource Supply Constraint: The Case of Doctors
The Human Resource Supply Constraint: The Case of Nurses
Human Resources for Health South Africa (HRH Strategy for the Health Sector: 2012/13 –2016/17)6
Staffing Norms for Primary Health Care in the context of PHC Re-engineering
National Tertiary Health Services Plan and Clinical Teaching and Training of Health Professionals
Implementation guideline of health workforce norma tive guides and standards for fixed PHC facilities
Year Health worker disciplines considered
2001 Nursing, dietetics, pharmacy, radiogra phy, laboratory, physiotherapy, occupa tional therapy, dental, social work
2010 GPs, Specialists
2010 Medical Specialists, Medical
Primary Strategy
All levels Estimate
All levels Forecast
2010 Registered and Enrolled nurses and Nursing assistants All levels Forecast
2011 Medical, Medical Specialists, Dental, Nurses Community health and home-based workers
2012 Medical Specialists, Medical Nursing Counsellors, Pharmacy Admin support
2013 Infrastructure and health facility based: Pop/Consult Room, Hospitals – Public, Hospitals – Private, Beds – Public, Beds – Private
2015 Medical Nurses, Nursing, Pharmacy, Dental Clinical Associate, Admin sup port, Operational Facility Manager, Counsellor, Groundsman, Security, Cleaner
All levels Estimate + Forecast
Primary Estimate + Forecast
Tertiary Estimate + Forecast
Primary Normative Guidelines
Medical specialist planning Report with results for reference group input
2030 Human Resources for Health Strategy: Investing in the Health Workforce for Universal Health Coverage
2019 Medical Specialists by discipline Tertiary Estimate + Forecast
2020 Plan 1: Medical specialists, Medical, Den tal, Nursing, Pharmacy, Occupational therapy, Physiotherapy, Psychology, Radiography, Environmental health, Clinical associates
Plan 2. Primary health care workers
Plan 3. Medical specialists
Estimate + Forecast
There have been huge transitions in the journey of HRH estimation and forecasting in South Africa, beginning with the report of the HRH Task Team chaired by Professor William Pick (2000) to the current WISN Tool which has been gazetted by the South African government.
The WISN tool was developed by the WHO to determine staffing norms. The National Department of Health (NDoH) is currently using WISN for developing and implementing health workforce staffing norms and standards for health facilities7. In 2017, the NDoH reported that the activity standards for district hospitals had been completed7. However, the NDoH was unable to meet its target of approving HRH norms for district and specialised hospitals due to the unavailability of data on district hospital service activities7. Failure to set HRH norms for district and specialised hospitals in turn affected the development of HRH norms for regional, tertiary and central hospitals7. Furthermore, the WISN approach seems to be the only method adopted by the NDoH for HRH planning, but several limitations have been reportedon its methodology. These limitations include dependence on the accuracy of annual service statistics used to assess workloads; possible overreporting of annual service statistics; inability to differentiate when the same activity is performed by two different staff categories; and insufficient consideration of the unique circumstances and HRH needs in rural areas8–10. Nonetheless, the WISN has identified the shortfalls in PHC staff in South Africa. In line with proposals from some health economists, it may be more appropriate to use a combination of integrated needs-based HRH planning methods. These methods should include consideration of: demographic and epidemiological changes; impact of health policies on service delivery; quality and equity; prioritisation of underserved areas; workforce and health expenditure; level of services; and the productivity of health care workers11–13
The non-generalisability of WISN may be affected by the topography, climate, and population densities of different areas14, 15. Wrong decision making based on WISN results may also pose an impact. In certain health facilities, due to a lighter workload – WISN calculations may show lower need for the health staff. Moreover, if service statistics are incomplete, human resource needs will be under-estimated. Furthermore, given the changing environment and its impact on health programmes, factors such as emergence of new tasks and services should also be considered in the calculation of human resources needed16 and the norm obtained should be reviewed as
far as possible17. Additionally, as reported by Smith et al.18, work has been done to value the cost South Africa’s PHC system using WISN to determine the mix and number of staff. Staffing levels that comply with WISN requirements are very low (7% of clinics in March 2016)19. A study done by the Medical Research Council (MRC) in North West province found the WISN model to be significantly more expensive than norms suggested by the MRC. This example illustrates the importance of linking staffing norms to broader HRH planning processes and modelling20. Thus, South Africa implemented WISN for PHC workforce planning but found the skills mix and staff determinations to be unaffordable due to the financial, infrastructure and technical challenges associated with WISN21
Most of the HRH models prepared in South Africa have included factors which impact the productivity of physicians, including technological changes. In recent years, some HRH models have started to account for task-shifting, for example, substitution of doctors by mid-level staff such as nurses or trained assistants (called clinical associates in South Africa)22. Foreseeing South Africa’s shortage of medical professionals, these substitutions are very relevant when planning for NHI. Task shifting may mean that the production of mid-level health workers needs to be increased, some new cadres created, or the scope of existing cadres expanded.
Health workforce planning needs to take migration into account. Labonte et al. (2015) found that there has been an overall decrease in emigration of skilled health workers from South Africa since the early 2000s, driven by a reduced need for foreign-trained skilled health workers in destination countries, including generalist and specialist doctors, nurses, dentists and pharmacists23. However, 10% of the survey sample reported that they were very likely to migrate within the next two years. This migratory intent varied by professional groups – 60% of dentists and just over 40% of nurses reported some likelihood of seeking work in another country within the next five years23. One-third of survey respondents were return migrants, showcasing the concept of ‘circular migration’ as discussed in previous studies24, 25 .
Public spending is calculated using spending by government expenditure and schemes, social health insurance and private insurance. The OECD reported in 2020 that more than 70% of health spending across OECD countries was funded from public sources. On average, 8.8% of Gross Domestic Product was dedicated to health in 2018. Countries such as Columbia (74%) and Chile (60%) had higher proportional expenditure through government/compulsory schemes than South Africa at 43%26 Thus, in South Africa where government provides subsidies for voluntary health insurers, the proportion of total spending from public sources is higher (54%) than government/compulsory schemes (43%)26. In South Africa there has been an increase of 53% in overall provincial and local government health expenditure from R100 759 million in FY2011/12 to R215 755 million in 2020/21. The annual average increase over the past nine years has been 8.8%27. (See Chapter on Health Financing for more detail.)
The health workforce inequities at several levels in South Africa were stark and the workforce inequity between the public and private health sectors is projected to worsen without concerted policy intervention. For example, the overall national density of medical specialists was calculated as 16.5 per 100 000. However, there are an estimated seven specialists per 100 000 user population employed in the public sector and 69 per 100 000 in the private health sector. There are also inequities within the public health sector. Rural provinces have significantly lower densities of more skilled health professionals. The inequities for medical specialists, nurses and CHWs are marked. For example, the Western Cape has 25.8 medical specialists per 100 000 public sector population compared to only 1.4 per 100 000 in Limpopo. Although the location of public sector tertiary and central hospitals influence this maldistribution, in practice this means that accessing specialist services in Limpopo is extremely difficult in comparison to other provinces28.
The urban–rural inequalities in the health workforce also deny equitable access to health care in South Africa, mostly discriminating against the poor29. The disparities vary in urban areas, while resourcing is consistently poorer in rural areas29 Furthermore, the shortage of drugs, equipment and infrastructure often mitigate against attracting highly trained professionals to rural and underserved urban areas30.
The provincial inequalities in health worker densities also reflect the variation in skills mix across the country. The public health sector in South Africa is predominantly nurse-driven, with nurses making up 56% of health care providers, reaching 63.9% in the Eastern Cape. While medical doctors constitute around 8.6% of the public health workforce, the proportions are lower in Limpopo (4.3%), Mpumalanga (6.1%) and the North West (6.1%), but higher in Gauteng (11.6%) and the Western Cape (14.6%). CHWs play a critical role in the health systems of the Northern Cape (36.8%), Mpumalanga (35.3%), North West (34.9%) and Limpopo (31.1%), as compared to lower proportions in more urbanised provinces (Eastern Cape – 14%, Western Cape –15%, KwaZulu-Natal – 18%, Free State – 19%, Gauteng – 19%). The maldistribution of health workers within provinces by district and level of care requires further analysis and policy attention28
There has been an overall increase in the number of doctors who have been trained in the last two decades in South Africa. The HPCSA registrations show an increase from 21 378 doctors (2000) to 46 420 (2020), an overall increase of 117%.
There was a 31.1% increase in the South African population over this period, during which the ratio of male doctors per 10 000 population only increased from 3.52 in 2000 to 4.69 in 201931, compared to an increase in female doctors per 10 000 population from 1.25 in 2000 to 3.21 in 201931
The recently completed National HRH Strategy 2030 provided a more detailed breakdown of the current ratios of health practitioners in South Africa, including projections of needs into the future28. Most of the ratios show impressive gains since the 2011 HRH Strategy, although this may in part be due to higher levels of inclusion in the PERSAL HR information system. (See Chapter on Health Financing for more discussion of this.)
Table17.3 2019 Public sector health workforce – Inter-provincial variation in staffing ratios per 100 000 public sector population
Province with the:
HW Category Year best ratio 3rd best ratio 5th best ratio 9th best ratio
Medical Practitioners 33.11 NC – 45.25 KZN – 37.42 GP – 31.89 LP – 25.94
Medical Specialists 9.96 WC – 25.81 FS – 12.99 NW – 3.66 LP – 1.36
Professional Nurses 147.95 EC – 189.67 LP – 174.60 NW – 140.56 FS – 93.60
Enrolled Nurses 64.04 KZN – 97.81 GP – 65.12 WC – 51.76 NC – 24.43
Nursing Assistants 69.78 EC – 90.57 LP – 88.19 WC – 82.23 MP – 36.03
Pharmacists 11.89 WC – 19.54 FS – 14.52 LP – 11.30 MP – 7.85
Pharmacy Assistants 3.68 KZN – 10.59 NW – 4.66 NC – 3.50 WC – 0.00
Occupational Therapists 2.64 NC – 5.88 FS – 3.22 EC – 2.51 KZN – 1.94
Physiotherapists 3.10 NC – 6.29 FS – 3.38 WC – 3.05 MP – 2.63
Speech Therapists & Audiologists 1.51 NC – 2.99 MP – 1.72 GP – 1.52 NW – 0.86
Psychologists & Vocational Counsellors 1.47 LP – 2.34 NW – 1.96 GP – 1.16 KZN – 0.81
Radiographers 5.94 WC – 9.36 EC – 6.55 GP – 6.21 MP – 3.42
Community Health Workers 111.79 NC – 263.14 NW –178.77 KZN – 99.21 WC – 69.36
Clinical Associates 0.77 MP – 1.65 KZN – 1.23 FS – 0.78 WC – 0.00
Source: PERSAL32 for all the selected categories except CHWs, which were obtained from the CHW register, as reported in the DHB 2017/1833
Population: Calculated from Thembisa model34, StatsSA GHS35
An OSD for remuneration was introduced in 2007 for public sector employees in South Africa in an effort to better recruit, retain and motivate professionals for public service. Each identified occupation has its own differentiated OSD scales to cater for the unique needs of an occupation, prescribing job grading, structures and job profiles to eliminate inter-provincial variations. The OSD also provides clear salary progression and career-pathing opportunities36. While the salaries are lower than in advanced industrial countries, OSD has closed this gap but widened the gap with African countries37. Questions have been raised about how effective OSD has been to drive commitment in health professionals to public service.
Compulsory community service of 12 months was introduced in 1998 for health professionals, starting with medical practitioners38 so that those who had benefitted from state largesse (government heavily subsidises health professional education) could offer a period of service back to where the needs are greatest. Community service is required before full professional registration can be obtained. The experience of community service for doctors over the first one-and-a-half decades was successful and largely met its original objectives of redistribution of health professionals
and professional development39. Community service requires more attention to orientation, management support and clinical supervision, and a focus on professional development opportunities38. Additionally, it has been suggested that community service initiatives should integrate mental health into PHC for decentralising mental health services40. While the benefits have been shown, the community service programme has been subjected to immense funding pressure, with under allocation of provincial resources to support the increased number of health professional graduates.
Globally, CHW programmes gained prominence in the 1970s with WHO’s Declaration of Alma-Ata, which saw CHWs as a key mode of delivery for PHC and as a strategy to expand the supply of health care workers. In many low- and middle-income countries, CHW programmes have been driven by non-governmental organisations (NGOs) reaching the doorstep of marginalised and rural populations.
The evidence of the effectiveness of CHW programmes is based on cost-benefit analyses and randomised control trials of CHW programmes on child and maternal health, or communicable diseases or single health issues. More recent evidence suggests that programmes designed around multiple health issues may be more cost-effective and better suited for the multiple disease burden of low-income and middle-income countries. The studies highlight design and implementation issues that hinder CHW programmes from reaching their expected outcomes, namely: under-resourcing, affordability, short and varied quality of training, inadequate integration with the formal health system, poor management and supervision practices, and an informal CHW workforce that is often subjected to unfavourable working conditions. However, in several other countries such as Ghana (unpaid) and Rwanda (not entitled to salary), the remuneration levels would not be at this level41
The experience with CHW programmes in South Africa echoes that of other low-income and middle-income countries. There were few CHW programmes until a rapid upscaling of AIDS-focussed NGO programmes. In 2011, the NDoH shifted to a comprehensive CHW policy focus on the disease burden presented by HIV/ AIDS and TB, maternal and child health42. There is strong emerging evidence of the effectiveness of CHWs43. However, there is also evidence that policy-makers need to contend with career pathing, variation in educational qualifications and training, retention, leadership and governance issues. There has been important progress in this regard with the formalisation of CHW programmes into the public sector, providing better salaries and job security.
Moreover, large-scale, comprehensive CHW programmes have been introduction in the context of implementing UHC, which has improved access to social support and health services at household and population level43. CHWs provide a range of health and psychosocial services in households and poor communities, especially in support of maternal and child health (MCH) services; TB, HIV/AIDS; and core areas of health promotion for nutrition, sanitation, and healthy living in South Africa44.
Diplomatic relations between South Africa and Cuba resulted in a bilateral agree ment to establish the Nelson Mandela - Fidel Castro medical student training pro gramme in 1994, aiming to promote PHC45. The programme began in 1996. In 2012, the programme was rapidly scaled up and peaked when 1 000 students were sent to study in Cuba. At that stage South Africa’s eight medical schools were graduating about 1 200 doctors a year. Experience with the programme showed that the medical students should be better supported for ease of transition into the local settings via a well-structured orientation and intervention programme in clinical skills46. This led to greater involvement of the South African Committee of Deans and provincial representatives. While the benefits of the increased medical training are not in question, there have been suggestions that at least some of the funds might have been better spent on increasing local capacity to scale up medical training47
During the COVID-19 crisis, health workers faced several consequences including mental health stresses. It is evident that to build a resilient workforce, occupational and environmental factors must be addressed. Therefore, the psychological well-being of the health workers continues to be a priority. Female nurses being in close contact with COVID-19 patients had the most to gain from efforts aimed at supporting psychological well-being. Further research including on social care workers and analysis of wider societal structural factors is recommended48. (See Chapter on Mental Health for more discussion of this topic.) Due to increased workplace stress and vulnerability associated with working during the COVID-19 pandemic, South Africa’s health care workers experienced anxiety, depression, burnout, resilience and coping strategies during lockdown levels 2 and 349
Health is a labour-intensive, labour-dependent sector. Without sufficient health workers who are well trained, supported and distributed a health system cannot be successful. It is therefore imperative that HRH is moved towards the centre of health systems development. There has been movement on this over the past quinquennium, but this momentum must not be lost.
It is important with massive reforms to begin with the end in mind. The NHI Bill describes what the NHI will look like. Health planners and managers need to document what the starting point is and plot the voyage to that destination. This includes estimating how long it will take, what it will it cost, how the money will flow, and a host of other institutional and service delivery issues.
Nelson Mandela - Fidel Castro Medical Collaboration Programme
Moving HRH towards the centre of health systems: needs, dilemmas and strategiesHuman resources for health
The essence of the NHI Bill is that there will be ONE health system for everyone, albeit with many parts and that everyone who lives in South Afr ica will have access to the system, irrespective of ability to pay, and appropriate care for their needs. This means that HRH planning needs to be reworked for the requirements of the NHI and will need to revisit the number of health workers and skills mix required, scale up education given the long lead times to produce professionals and plan for improved workplaces and better distribution. This includes addressing the public–private dichotomy.
Under the NHI, the fragmented, poor, inefficient, understaffed and ill-equipped public sector (serving about 85% of the population) and the fragmented, over-serviced, over-specialised, expensive private sector (serving about 15% of the population) will together serve 100% of the population. This huge reform requires both systemic change and local change. These are many and complex and will take place over many years until 2030, including in HRH. A start has been made and HRH needs to be at the centre of this planning and evolution.
Quality national and sub-national data on the health workforce is a pre-requisite for developing evidence-informed policy. Most governments face challenges in reporting and publishing a full account of their HRH situation50. As in South Africa, the information is often dispersed and there are capacity constraints in data collection, analysis and utilisation. Governments do engage in multiple efforts and partnerships to improve minimum, inter-operable data sets; enable their national authorities to develop strategic intelligence on HRH; and to inform health workforce projections in relation to population needs and health systems priorities50. The efforts to do this in South Africa are evolving and should result in the development of National Health Workforce Accounts (NHWA) to improve the availability, quality and use of data on the health workforce through monitoring of a set of indicators to support achievement of UHC, Sustainable Development Goals (SDGs) and other health objectives. There is a need for developing and maintaining health workforce data sources such as the National Census, Labour Force Surveys and key administrative national and regional sources50
The Presidential Health Summit (2018) brought together key stakeholders from a wide range of constituencies in the health sector to deliberate and propose solutions to address the challenges facing the South African health system. The summit realised some practical, prioritised and realistic action plans with immediate, short-term and medium-term interventions. The HRH actions included a Review of Remuneration of Work Outside Public Sector (RWOPS) and validation and optimisation of the Integrated Human Resource, Personnel and Salary System (PERSAL) and HR management information systems, and most importantly, that staffing and funding policy must meet the needs of the health system51. The summit recognised that HRH challenges of governance and control hamper implementation of HRH plans and strategies and that provincial processes on allocation of funds also work against central planning and prioritisation, including issues with provincial budget negotiations resulting in poor provinces performing badly. The lack of a planning unit that works in collaboration with intergovernmental departments, such as the
Department of Labour, Treasury, NDoH, HPCSA and the Job Seekers Exemption Certificate (JSEC) (medical training planning committee) are hamstrung due to lack of a comprehensive HRH model. The summit was able to garner unanimous support for the implementation of NHI including universal quality health care, social solidarity and equity in health access52 and HRH planning and interventions should be geared towards this.
In 2014, the Competition Commission of South Africa instituted a market inquiry into the South African private health sector in order to ascertain whether there were features preventing, distorting or restricting competition53. (See Chapter on Health Financing for more discussion of the HMI.) The final 2019 HMI Report flagged a range of regulatory and systemic issues that need to be addressed, including key HRH-related challenges. These include the disparity in the availability of specialists and general medical practitioners between the public and private health sectors, and between rural and urban communities54. The Commission made recommendations regarding the payment models and structure of private health care that need to be addressed to achieve greater equity. The report also identified concerns regarding the market power of health practitioners, incentives and relationships that may drive the high costs in the private sector. The report also mentioned that three big companies dominated the South Africa job market by offering doctors, who have admission rights over patients, attractive opportunities to practise in their facilities, thus indirectly influencing admission rates53
No accurate database exists on the number of practitioners active in the private sector. Using claims data, the HMI reaffirmed the challenges of the distribution and structure of private medical practice. The HMI found that there are 1.75 private practitioners per 1 000 insured population. While general practitioners are evenly distributed across the insured population (just under 1 per 1 000), specialists are concentrated in provincial capitals and metropolitan areas54. Most doctors work in solo practices, except for single-discipline group practices, such as radiologists, some anaesthetists, and corporate pathology groups. Multidisciplinary groups that allow for up- and down-referral are notable by their absence and the framework that serves as an impediment to this needs to be addressed. This kind of organised care is not well supported by funders and some practitioner associations and is limited by the current HPCSA ethical rules54
The value of research in HRH to support policy-making and operational success needs to be understood and acknowledged through increased funding to enable the small pool of HRH researchers in South Africa to grow. New avenues of research need to be opened up.
There is a need for explanatory research to examine the roles and responsibilities of each category of health workers and determine who is defined as a health worker, in addition to research efforts that seek to descriptively count health workers in a more inclusive manner55
There is also a need for research to conceptualise the important aspects of social relations that may otherwise be hard to recognise, and how to measure and address these56, for instance, the lack of gender disaggregated data57. The science of HRH, which offers a deeper understanding of how UHC and the SDGs are dependent on health workers, has the potential to overcome outdated and ineffective orthodoxy about health workers globally57.
Strategic leadership capability for the health workforce is essential, and there are many examples of innovation and good practices in the health system. However, leadership competency gaps remain at all levels of the health system and there are shortfalls in strategic, technical and managerial competence, capability and accountability. The prevailing health system culture acts as a barrier to the new styles of leadership needed. Gaps in ethical and values-based leadership contribute to poor quality of care through lack of accountability, corruption and fraud58. This prevailing management culture reflects the strong emphasis on centralisation, compliance, adherence to centrally determined processes, rigid classification of tasks, and an entrenched hierarchy. Consequently, there is a reluctance to question higher authority. These mitigate against decentralisation, individual agency, innovation, active engagement, and accountability. Consequently, many health leaders and managers feel unsupported, isolated and unpre pared, with reportedly high levels of burnout, stress, low morale and poor motivation impacting staff, especially at the frontline of service delivery59
People management is a core function, yet HRH management practices tend to be weak, with wide variations across provincial health departments and insufficient accountability. Underlying these broader HRH management shortcomings is the limited state of readiness of national and provincial HRH divisions for both strategic and technical functions, with insufficient numbers of competent managers, a general low prioritisation of strategic HR within health departments and the persistent narrowing of HRH to a mainly administrative and operational function with little strategic and decision-making authority.
South Africa has numerous laws, well-established frameworks, policies and procedures that guide the governance, leadership and management of the health system and its human resources. However, the implementation of these remains sub-optimal. Health systems and HRH governance, leadership and management are priority areas that will determine the effectiveness and functioning of South Africa’s health system, and its outcomes. Although two-thirds or R133 billion of the public health sector budget is spent on the health workforce, limited attention is given to its optimal governance, planning, financing and management. At national and provincial government levels, more attention is needed on how this monetary investment translates into measurable gains, implementation efficiencies, and improved health outcomes
The lack of management capacity within the public sector indicates a great need for further development of managers, and provinces need to identify managers who need training and make resources available for such60. The capacity to provide such programmes has grown but requires support to ensure their sustainability. The NDoH identified the training of managers of public hospitals for improving efficiency in health service delivery. Thus, the NDoH in collaboration with the universities of KwaZulu-Natal and the Witwatersrand launched a Master’s programme to train hospital managers61. The majority of the participants from this programme are working in the public health sector61
In a workforce forecasting exercise undertaken in 2021, it was estimated that if the status quo is maintained for male doctors (namely, 4.69 per 10 000 population), then by 2030 it will have increased to 4.76 per 10 000 population. In contract, if the status quo is maintained in the production of female doctors (namely, 3.21 per 10 000 population), then by 2030 the density of female doctors will increase to 4.35 per 10 000 population.
However, if an attempt is made to achieve equity with male doctors, then an additional 2 242 female doctors will be needed by 203031 (Table 17.4).
Medical Specialists
Anaesthesiology 1 216 638 1 854 1:0.5
Cardiology 1 0 1 1:0
Cardiothoracic Surgery 139 9 148 1:0.1
Clinical Pharmacology 9 11 20 1:1.2
Community Health 47 30 77 1:0.6 Dermatology 139 129 268 1:0.9
Diagnostic Radiology 693 314 1 007 1:0.5
Education Pathology (Microbio logical) 1 0 1 1:0
Emergency Medicine 83 51 134 1:0.6
Family Medicine 714 255 969 1:0.4
Fast Track – Paediatrics 1 1 1:0
Medical Genetics 1 10 11 1:10 Medicine 1 340 479 1 819 1:0.4
Neurology 110 81 191 1:0.7 Neurosurgery 217 11 228 1:0.1 Nuclear Medicine 41 41 82 1:1 Obstetrics and Gynaecology 875 436 1 311 1:0.5
Occupational Medicine 21 16 37 1:0.8
Ophthalmology 433 127 560 1:0.3
Orthopaedics 910 48 958 1:0.1 Otorhinolaryngology 318 49 367 1:0.2
Paediatric 628 761 1 389 1:1.2
Paediatric Surgery 17 17 34 1:1 Pathology 506 486 992 1:1
Physical Medicine (Closed) 2 5 7 1:2.5 Plastic and Reconstructive Surgery 196 34 230 1:0.2
Preventive Medicine (Closed) 10 2 12 1:0.2 Psychiatry 440 476 916 1:1.1
Public Health Medicine 19 54 73 1:2.8
Radiation Oncology 121 118 239 1:1 Radiology 0 1 1 1:0 Surgery 922 144 1 066 1:0.2
Urology 284 15 299 1:0.1 Venerology (Closed) 2 0 2 1:0
The number of women undertaking CMSA examinations for sub-specialists is consistent. However, the trend for African sub-specialists is increasing as compared to other population groups (Table 17.5).
Table17.5 Demographics of sub-specialists who were successful in colleges of medicine examinations in South Africa
Demographics 2012–16 2017–21 2012–21
Men 82 (43.2%) 303 (45.6%) 385 (45%)
Women 108 (56.8%) 362 (54.4%) 470 (55%)
South African
African 70 (36.8%) 317 (47.7%) 387 (45.3%)
Coloured 11 (5.8%) 45 (6.8%) 56 (6.5%)
Indian 51 (26.8%) 161 (24.2%) 212 (24.8%)
White 58 (30.5%) 142 (21.4%) 200 (23.4%)
Source: CMSA, 2022
Technological innovations may radically reshape the health sector, as evidenced by the creation of a fully virtual care facility, where health care personnel exclusively provide ‘telehealth’ services to patients, whereby medical advice and provision is given remotely through telecommunication technologies62. Advances in this field have also been driven by the COVID-19 pandemic. The National Digital Health Strategy for South Africa (2019–2024) mentions development of a Human Resource Information System (HRIS) to provide information necessary to support the health workforce. The HRIS aims to address the availability, completeness and quality of health workforce data63
Health care organisations will need to account for a wide range of implications related to technological advances, including the virtual delivery of services and the integration of robotics and Artificial Intelligence. However, the health sector must evaluate the added benefits of technology for patients and workers and enhance its usefulness through improved policy and practice. While health technology can contribute to cost containment, it has added to health care expenditure growth in recent years in OECD countries. Evidence of the effectiveness and utility of new technologies is not always clear, and policy-makers must balance innovation with value62
South Africa’s commitment to attaining UHC for all its citizens through NHI recognised the need for adopting a strategic approach to HRH which is critical to HRH-related reforms. Sufficient numbers of well-skilled, enabled and supported health workers are central to the achievement of an affordable, accessible and quality health care system for all as envisaged in the NHI. Thus, a Ministerial Task Team was constituted in 2019 which in collaboration with the NDoH and in consultation with stakeholders delivered the28 2030 Human Resources for Health Strategy. Its release by the NDoH sets out the overall vision, goals and actions required to address persistent issues of inequity and inefficiencies in the health workforce. The Strategy provides insights on the numbers of health workers of different categories needed to provide for health promotion and disease prevention, and curative, therapeutic, rehabilitative and palliative services. It informs the training and education reforms that are needed in South Africa’s public universities, nursing colleges and health worker training institutions to supply adequate numbers of all cadres of the health workforce, from CHWs to sub-specialists28.
The Strategy laid down five basic HRH strategic goals28:
Goal 1: Effective health workforce planning to ensure HRH is aligned with current and future needs.
Goal 2: Institutionalise data-driven and research-informed health workforce policy, planning, management and investment.
Goal 3: Produce a competent and caring multidisciplinary health workforce through an equity-oriented, socially accountable education and training system.
Goal 4: Ensure optimal governance; build capable and accountable strategic leadership and management in the health system.
Goal 5: Build an enabled, productive, motivated and empowered health workforce.
The Strategy concludes with commitments to work immediately to:
• Mainstream gender and ensure diversity so that all health workers feel they belong and are treated with dignity, recognising that the health workforce must feel and be safe and treated fairly. This includes integrity in human resource practices, reasonable workloads, rapid recruitment, effective occupational health and wellness programmes and the necessary resources to perform their roles.
• Revise rural recruitment and retention strategies required to ensure that South Africa achieves its health system goal of equity in access to health professionals.
• To implement a shift in organisational culture and strategies to boost morale and give effect to the commitment to caring and quality. This should be rooted in competency frameworks and a more effective performance management and development system that facilitates full productivity from all health workers.
• Embark on an NDoH review of RWOPS, its interpretation, application and management.
• Strengthen the HRH function in the NDoH and conduct an economic analysis of the costs and benefits of internship and compulsory community service programmes, and the cost of employment of health professionals.
• Have the health sector work more closely with other sectors of government impacting on the practice environments of health workers (e.g., their conditions of service, living and working arrangements and safety).
The strategy was launched in March 2020 and coincided with the declaration of 2020 as the International Year of the Nurse and Midwife, and the launch of the first ever report on the State of World Nursing 2020 by the WHO. Nursing and midwifery being at the forefront of managing the COVID-19 pandemic has highlighted the need for dedicated attention to and decisive action towards the plight of this professional workforce, as nurses are the backbone of any health care system. The disease burden has placed an additional stress on nursing. Increasing nurse turnover is widening the patient‐to‐nurse ratio, adding to workload and leading to a deterioration in the quality of care and patient satisfaction and health care outcomes64. The turnover of nurses in South Africa is not known, but recruitment of younger nurses and succession planning require attention.
The National Strategic Direction for Nursing Education and Practice: A Road Map for Strengthening Nursing and Midwifery in South Africa (2020/21–2025/26) was released by the NDoH in 202065. The Strategy’s overall objective is to harness nursing education and practice in support of UHC and the vision of the National Development Plan 2030 for ‘a health system that works for everyone and produces positive health outcomes’. It seeks to optimise nursing workforce planning, embrace digital technologies for education and clinical practice, as wellas advance socially accountable education programmes and systems, leadership and governance towards better nursing services.
The Strategy65 is underpinned by the need to:
a) Provide a framework for organising and coordinating the nursing workforce contribution towards the goals of UHC against the backdrop of the 2030 Human Resources for Health Strategy;
b) Build on gains made in the implementation of the recommendations of the previous nursing strategic plan that was mostly focused on nursing education; and
c) Enable a focus on the implementation of core HRH-relevant strategies to the nursing sector with targets and measurable outputs.
This chapter has provided evidence of important achievements in HRH in the past quinquennium, but has also shown up the fault lines in HRH today and what is needed to gear HRH in the next quinquennium for better availability of HRH and UHC.
The HRH Strategy 2030 ends with a detailed five-year Strategic Plan that focuses on key implementation activities, for the period from 2020/21 until 2024/25 and this should be the core of the way forward on HRH in South Africa. The Strategy highlights the specific actions needed to achieve each of its five goals and should be the central focus of HRH development for the next five years.
Key focus areas are:
• Coordination: Coordinated efforts from all stakeholders will be required to support implementation of HRH plans. Better coordination between the NDoH, the Department of Higher Education and Training, National Treasury, provincial departments, professional bodies and training institutions will be needed as will the financial instruments. Furthermore, engagement between the public and private health sectors along with social partners and with the Ministry of Employment and Labour will be required. Key to the way forward is:
• Planning: For more effective and comprehensive HRH planning, a functional National Health Workforce Analysis and Planning Function should be established to institutionalise and strengthen planning. It should draw on national and international health workforce planning expertise, including labour market analysts.
• Information driven: HRH planning and policy-making should be information driven using data from various sources such as PERSAL, health professional council registers (HPCSA, South African Nursing Council (SANC) and South African Pharmacy Council (SAPC)), District Health Information System (DHIS) and WHO National Health Workforce Accounts. This will create the data science opportunities for more predictive and intelligent analytics and decisions.
• Health workforce education: Globally, South Africa’s health education and training system is one of the most advanced and sophisticated. However, the existing health workforce supply pipeline is not fully configured and does not support optimum skills mix of the health workforce. Curriculum realignment with population health needs, specifically of vulnerable, under-served and rural and remote populations, is needed to lead changes towards transformative and sustainable outcomes.
• Leadership and management: A major investment is needed in leadership and management development. Performance standards for HRH leadership and management need to be institutionalised, revitalised continuously, and applied at every level of the system. The HRH regulatory structures need revitalisation to ensure good and accountable governance (e.g. HPCSA, SANC and SAPC). Strengthened systems of oversight of key professional regulatory bodies are needed, as is an effective Forum of Statutory Health Professions Councils.
• Conditions of service and positive workplaces: Positive conditions of service and workplaces to ensure the health, safety and well-being of the health workforce are fundamental drivers of quality health care and the overall performance and efficiency of the health system. This must be a priority. As an initial step, mainstreaming gender and ensuring diversity at all levels would help to ensure that health workers are treated with dignity and fairness.
1. ILO, WHO. Health Employment and Economic Growth: A Five-Year Action Plan (2017–21). 2016. [cited 2021 14 October]. Available from: https://www.who. int/hrh/com-heeg/com-heeg_actionplan2016.pdf?ua=1.
2. National Department of Health. Human resources for health for South Africa: Strategy for the health sector 2012/13–2016/17. Pretoria 2011.
3. Ono T, Lafortune G, Schoenstein M. Health workforce planning in OECD countries. 2013.
4. Database [Internet]. HPCSA. 2018 [cited 28 March, 2019].
5. Statistics South Africa. Mid-year population estimates. Pretoria: Stats SA; 2018 [cited 2019 March 3]. Available from: http://www.statssa.gov.za/publications/ P0302/P03022018.pdf.
6. Department of Health – South Africa. Human Resources for Health South Africa: HRH strategy for the health sector: 2012/13–2016/17. Department of Health Pretoria; 2011.
7. South African National Department of Health. Annual Report of the National Department of Health. Pretoria: NDoH; 2017 [cited 2019 August 6].
8. World Health Organization. WISN - Workload Indicators of Staffing Need User Manual. Geneva: WHO; 2010.
9. Namaganda G, Oketcho V, Maniple E, Viadro C. Making the transition to workloadbased staffing: using the Workload Indicators of Staffing Need method in Uganda. Human Resources for Health. 2015;13(1):89.
10. McQuide PA, Kolehmainen-Aitken R-L, Forster N. Applying the workload indicators of staffing need (WISN) method in Namibia: challenges and implications for human resources for health policy. Human Resources for Health. 2013;11(1):64.
11. Soucat A, Scheffler R, Ghebreyesus TA. The labor market for health workers in Africa: a new look at the crisis. The World Bank; 2013.
12. Birch S. Improving the Fiscal and Political Sustainability of Health Systems through Integrated Population Needs-Based Planning: Seminar briefing #17 London: Office of Health Economics Research; 2015.
13. Academy of Science of South Africa. Reconceptualising health professions education in South Africa: Consensus study report. Pretoria: ASSAf; 2018.
14. Abdideh M, Jannati A, Asghari Jafarabadi M. Standard development of family physicians to the population defined by WISN. Bull Env Pharmacol Life Sci. 2014;3(12):89–96.
15. Jocom PA, Massie RG, Porotu’o JP. Kebutuhan riil tenaga pemasak di instalasi gizi dengan menggunakanmetode workload indicators of staffing need (WISN) di RSU Pancaran Kasih GMIM Manado. Jurnal Biomedik. 2017;9(1).
16. Daviaud E, Chopra M. How much is not enough? Human resources requirements for primary health care: a case study from South Africa. Bulletin of the World Health Organization. 2008;86:46–51.
17. Doosty F, Maleki MR, Yarmohammadian MH. An investigation on workload indicator of staffing need: A scoping review. Journal of Education and Health Promotion. 2019;8.
18. Smith A, Ranchod S, Strugnell D, Wishnia J. Human resources for health planning and National Health Insurance: the urgency and the opportunity. South African Health Review. 2018;2018(1):23–31.
19. Hunter JR, Chandran TM, Asmall S, Tucker J-M, Ravhengani NM, Mokgalagadi Y. The Ideal Clinic in South Africa: progress and challenges in implementation. South African Health Review. 2017;2017(1):111–23.
20. Daviaud E. Strengthening PHC Services in the North West Province 2015. Available from: http://www.mrc.ac.za/sites/default/files/files/2016-07-14/ StrengtheningPHC.pdf.
21. Mabunda SA, Gupta M, Chitha WW, Mtshali NG, Ugarte C, Echegaray C, et al. Lessons Learnt during the Implementation of WISN for Comprehensive Primary Health Care in India, South Africa and Peru. International Journal of Environmental Research and Public Health. 2021;18(23):12541.
22. Veller M. Public Health system in dire straits. Cape Times; 2018. Available from: https:// www.pressreader.com/south-africa/cape-times/20180601/281861529185604].
23. Labonté R, Sanders D, Mathole T, Crush J, Chikanda A, Dambisya Y, et al. Health worker migration from South Africa: causes, consequences and policy responses. Human Resources for Health. 2015;13(1):92.
24. Agunias DR. From a zero-sum to a win-win scenario. Literature review on circular migration Washington, DC. Migration Policy Institute. 2006.
25. Kingma M. Nurses on the move: a global overview. Health Services Research. 2007 Jun;42(3 Pt 2):1281–98. PubMed PMID: 17489915. Pubmed Central PMCID: 1955376.
26. Organisation for Economic Co-operation and Development. Public funding of health care 2020 [cited 2021 19 October]. Available from: https://www.oecd. org/health/Public-funding-of-health-care-Brief-2020.pdf.
27. Day C, Gray A, Padayachee T, Cois A. Health and Related Indicators. South Africa Health Review. 2021.
28. National Department of Health (NDoH). 2030 Human Resources for Health Strategy: Investing in the Health Workforce for Universal Health Coverage. Pretoria: Government Printers, 2020.
29. le R Booysen F. Urban–rural inequalities in health care delivery in South Africa. Development Southern Africa. 2003;20(5):659–73.
30. Espinet X, Aliyev S, Stanton-Geddes Z, Bun V. The road to healthier communities: Rethinking rural accessibility amid a health crisis. World Bank Blogs; 2020 [cited 29 March 2022]. Available from: https://blogs.worldbank.org/transport/roadhealthier-communities-rethinking-rural-accessibility-amid-health-crisis.
31. Tiwari R, Wildschut-February A, Nkonki L, English R, Karangwa I, Chikte U. Reflecting on the current scenario and forecasting the future demand for medical doctors in South Africa up to 2030: towards equal representation of women. Human Resources for Health. 2021;19(1):1–12.
32. Personnel and Salary Information System (PERSAL) [Internet]. 2019 [cited 4 April 2019]. Available from: http://www.vulindlela.gov.za/.
33. Community Health Worker Information System, [Internet]. South African National Department of Health.
34. Johnson LF, May MT, Dorrington RE, Cornell M, Boulle A, Egger M, et al. Estimating the impact of antiretroviral treatment on adult mortality trends in South Africa: A mathematical modelling study. PLOS Medicine. 2017;14(12):e1002468.
35.StatsSA. General Household Survey 2018. Pretoria: StatsSA, 2019.
36. NCOP Health and Social Services. Occupational Specific Dispensation: Health Department briefing South Africa: Parliamentary Monitoring Group; 2009 [cited 2021 9 December]. Available from: https://pmg.org.za/committeemeeting/10658/.
37. George G, Rhodes B. Is there really a pot of gold at the end of the rainbow? Has the Occupational Specific Dispensation, as a mechanism to attract and retain health workers in South Africa, leveled the playing field? BMC Public Health. 2012;12(1):1–8.
38. Reid SJ, Peacocke J, Kornik S, Wolvaardt G. Compulsory community service for doctors in South Africa: A 15-year review. South African Medical Journal. 2018;108(9).
39. Erasmus N. Slaves of the state-medical internship and community service in South Africa: forum-issues in medicine. South African Medical Journal. 2012;102(8): 655–8.
40. Swarts B. A community (dis) service: Reflections of a community service clinical psychologist. South African Journal of Psychology. 2013;43(1):105–15.
41. Ballard M, Westgate C, Alban R, Choudhury N, Adamjee R, Schwarz R, et al. Compensation models for community health workers: comparison of legal frameworks across five countries. Journal of Global Health. 2021;11.
42. Assegaai T, Schneider H. National guidance and district-level practices in the supervision of community health workers in South Africa: a qualitative study. Human Resources for Health. 2019;17(1):1–10.
43. Thomas L, Buch E, Pillay Y, Jordaan J. Effectiveness of a large-scale, sustained and comprehensive community health worker program in improving population health: the experience of an urban health district in South Africa. Human Resources for Health. 2021;19(1):1–11.
44. Thomas LS, Buch E, Pillay Y. An analysis of the services provided by community health workers within an urban district in South Africa: a key contribution towards universal access to care. Human Resources for Health. 2021;19(1):1–11.
45. Seakamela S. Mandela – Castro Medical Program Continue To Transform South Africa. Fair Planet.
46. Motala MI. Exploring the impact of experience-based medical learning on students’ clinical preparedness: a case study of the South African–Cuban medical training collaboration programme at the University of KwaZulu-Natal, South Africa 2014.
47. Baggott R, Lambie G. Hard currency, solidarity, and soft power: the motives, implications, and lessons of Cuban health internationalism. International Journal of Health Services. 2019;49(1):165–85.
48. De Kock JH, Latham HA, Leslie SJ, Grindle M, Munoz S-A, Ellis L, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health 2021;21(1):1–18.
49. Cook LJ, Hassem T, Laher S, Variava T, Schutte E. Mental health experiences of healthcare professionals during COVID-19. SA Journal of Industrial Psychology. 2021;47(1):1–10.
50. World Health Organization. Improving health workforce data and evidence. Geneva: WHO; 2021 [cited 2021 9 December]. Available from: https://www. who.int/activities/improving-health-workforce-data-and-evidence.
51. Presidential Health Summit. Strengthening the South African health system twards an integrated and unified health system. 2018.
52. Hamilton PJ. A Commentary on The National Health Summit 2018 Report. South Africa: Helen Suzman Foundation; 2019 [updated March 26, 2019; cited 2022 29 March]. Available from: https://hsf.org.za/publications/hsf-briefs/acommentary-on-the-national-health-summit-2018-report.
53. Nkonki L, Bhengu N, Fonn S, Ramokgopa M. The Health Market Inquir y and its potential contribution to improving health systems functioning in South Africa. South African Health Review. 2019;2019(1):81–8.
54. Competition Commission of South Africa. Health Market Inquiry – Final Findings and Recommendations Report. Pretoria: Competition Commission; 2019.
55. Part A. Health worker profiles: boundaries, metrics and modelling. A HEALTH POLICY AND SYSTEMS RESEARCH READER ON.31.
56. Part A. Social contexts and relations shaping health workers. A HEALTH POLICY AND SYSTEMS RESEARCH READER ON.43.
57. George A, Campbell J, Ghaffar A. Advancing the science behind human resources for health: Highlights from the Health Policy and Systems Research Reader on Human Resources for Health. Health Research Policy and Systems. 2018;16(1): 1–8.
58. Commission SALN. Confronting the right to ethical and accountable quality health care in South Africa: A Consensus Report. Pretoria: National Department of Health. 2019.
59. Health Ministerial Task Team. Health Ministerial Task Team on Hospital Mismanagement and Poor Service Delivery – Closure Report. Pretoria 2017.
60. Pillay R. Managerial competencies of hospital managers in South Africa: a survey of managers in the public and private sectors. Human Resources for Health 2008;6(1):1–7.
61. Naidoo S, Mothagae M, Kistnasamy B, Jinabhai C, Basu D. A hospitalmanagement training programme in South Africa. Southern African Journal of Public Health. 2017;2(2):34–9.
62. International Labour Organization. The future of work in the health sector. Geneva: ILO; 2019 [cited 2021 22 September]. Available from: https://www.ilo. org/wcmsp5/groups/public/---ed_dialogue/---sector/documents/publication/ wcms_669363.pdf.
63. National Department of Health. National Digital Health Strategy for South Africa 2019–2024. 2019. Available from: https://www.health.gov.za/ wp-content/uploads/2020/11/national-digital-strategy-for-south-africa2019-2024-b.pdf.
64. Jones T, Heui Bae S, Murry N, Hamilton P. Texas nurse staffing trends before and after mandated nurse staffing committees. Policy, Politics, & Nursing Practice 2015;16(3-4):79–96.
65. National Department of Health. National Strategic Direction for Nursing and Midwifery Education and Practice. Pretoria, South Africa: NDoH, 2020.
The period 2015 to 2020 was characterised by several developments relating to health financing reforms towards Universal Health Coverage (UHC). This chapter examines trends, problems, challenges and progress in a selection of public and private financing domains.
The chapter starts with an analysis of progress with National Health Insurance (NHI) and examines why progress has been slow. We also present research findings on building a consensus on the way forward. The chapter then examines trends in health spending at national and provincial level and spending through the private sector. It next looks at some of the pressures on future financing of health and the impact of COVID-19.
The chapter ends with a discussion of the status of financing reforms, suggesting some re-evaluation of aspects of the model to get NHI reforms back on track.
Mark Blecher, Vishal Brijlal, Jonatan Daven, Sasha Stevenson, Marumo Maake, Noxolo Madela, Thulani Matsebula, Nikhil KhanaNational Health Insurance is about a common, central fund, which will purchase quality health care services that are needed by the people of South Africa. This must be done in a way whereby access is equitable and without prejudice. The White Paper represents government’s statement of intent on achieving UHC to ‘provide all people with access to a common set of comprehensive health services of sufficient quality, while also ensuring that the use of these services does not expose the user to financial hardship’. As such, it is important that there is progressive realisation of this principle over the transition period. Over time, all people will access a common set of comprehensive benefits.
Although an admirable reform in principle, it has progressed poorly in implementation. In 2017, Cabinet approved the White Paper on NHI,1 almost six years after the publication of its precursor, the Green Paper, in 2011.2
Previous publications have shown that NHI reforms made slow and insufficient progress in the period 2015–2020.3
Table 18.1 shows a brief summary of progress on NHI over the five-year period. While some progress was made with the release of a White Paper in 2017 and an NHI Bill was developed and introduced to Parliament4, there has been little progress with implementation. This is surprising given that NHI Pilots were launched already in 2012/13, and NHI discussions have been taking place since 2008 and indeed long before, noting that a Social Health Insurance was already proposed as government policy in the White Paper of 1997, more than 20 years prior to the release of the NHI white paper.5
New taxes No Some tax options in White Paper, but no progress in implementation
Other sources of revenue
Partial Medical tax credit capped and partially redirected to NDoH
Funding/ alloca tions Partial Indirect and direct NHI conditional grants put in place
Pooling No
Complexities pertaining to powers and funding of provinces
Integration of Government medical schemes: GEMS, Parmed, Polmed, Transmed
No Besides the NHI Bill, no practical process has been put forward on how functions would be transferred to central government and delegated back to provinces for delivery
No No practical work done on scheme alignment or consolidation
Medical Schemes reform No Medical Schemes Amendment Bill published for comments in 2018 but not taken forward and introduced to Parliament
Re-imbursement reform: DRGs for hospital reimbursement
Reimbursement for PHC: capitation and contracts
No Despite funding allocated for DRG development, only limited coding of diagnoses done. Overall, project did not proceed, although some progress in Western Cape province
No Very good actuarial project to determine capitation rate and develop contracts, but never taken forward
Purchasing from public providers No No piloting of purchasing with public sector
Purchasing from private providers No Minimal progress: COVID-19 critical care and COVID-19 vaccine programme has potential to build collaboration
i Source: Authors
Treasury unlikely to support until current underspending is addressed and more progress is made on mixed provision model and strategic purchasing
This reform was enacted to make medial scheme tax subsidy dispensation more equitable
Low spending on NHI indirect grant
Funding previously earmarked on NDoH budget for capitation development but not utilised
CUP purchasing model
No No progress with development
There seems to be resistance within the public health sector for strategic purchasing, despite being the inherent feature of NHI model
Institutions e.g. hospitals as semi-autonomous providers
Legislative or regulatory framework for contracting
No No progress in this area
No No progress except NHI Bill
Contract development Limited Draft GP capitation contracts developed, but not taken forward
IT systems Limited Some progress on Health Patient Regis tration system, but limited modules and integration with other systems
Governance Limited
Policy Yes White Paper published in 2017
NHI Bill Yes Very long delays in Parliament
Establishment of pre-cursor to NHI Fund
No NHI Fund has not been established, and interim structure not built in NDoH
Provision Limited
Private GPs Limited Some contracting on sessional basis, but no strategic purchasing
Pharmacies Partial Centralised Chronic Medicine Dispensing and Distribution (CCMDD) model has had some successes but limited in scope
Other private No No progress in contracting private sector, except limited contracting under COVID-19
Quality of care Partial Ideal clinics and some other initiatives, Office of Health Standards Compliance established
NHI indirect grant partly reformed to focus on CUPs from 2022/23
NHI has been delayed in Parliament for over two years
Funding allocated for this from 2018 and onwards but no progress and no spending
Table 18.1 shows limited progress in many areas pertaining to NHI, particularly in strategic purchasing, pooling and developing a mixed provider platform. Many of the transition steps during the second phase of NHI preparation (2017–2022) outlined in the White Paper (Chapter 9) have not been accomplished.
While COVID-19 has indeed delayed NHI work, this is relevant only for the final year of the period. A previous paper laid out a set of obstacles and solutions.3 Looking further into underlying causes, we deliberate on several probable reasons for slow progress:
• Weak management and capacity
• Inability to build compromise and consensus across interest groups
• Complexity and politics around provincial vs national powers and political interests
• Weak economic growth since 2010
In many instances, progress on NHI has been stymied by managerial inability to deliver on key technical reforms as part of a transitional process. Some examples include:
• Inability to develop a Diagnostic-Related Group (DRG) system for hospital reimbursement, despite funding allocated for several years and access to diagnostic groupers at no cost. Many similar-income countries have drawn far ahead, e.g. Thailand has implemented DRG payments for over a decade.6
• Inability to implement a capitation system of reimbursement for private general practitioners or Contracting Units for Primary Health Care (CUPs), despite funding and enabling research which developed a financing model and capitation formula for South Africa.7,8,
• Inability to put in place an NHI interim management structure despite funding being allocated for this purpose since 2018/19.
• Inability to make progress with purchasing priority services for NHI funded through the indirect NHI Grant, such as school health, mental health, oncology and maternity care for high-risk pregnancies.
However, some areas where progress has been made, upon which further developments can be built are as follows:
Centralised Chronic Medicine Dispensing and Distribution programme (CCMDD): (see Chapter 5 on Accessing Access to Medicines and Health Technology).
Health Patient Registration System (HPRS): The HPRS contains over 50 million individual person records. Although the system is currently narrow in scope focussing mainly on patient registration, it provides an electronic tool on to which a capitation system could be built. Additional modules, such as patient diagnoses, laboratory tests and medicine prescriptions need to be added or linked over time. To date it is also largely limited to public sector facilities. Furthermore, some limited progress was made on Primary health care re-engineering, such as with the Ideal Clinic initiative (see Chapter 4 on Primary Health Care).
Progress in these areas demonstrates that where some management capacity exists for reforms, it is possible to innovate and make changes that can improve service delivery, make a difference to client experience and demonstrate benefits from NHI.
Successful health reform globally is dependent on a balance of forces and the ability of reformers to bring various stakeholders onboard. The NHI is a highly redistributive reform and given that South Africa is one of the most inequitable countries in the world, several scenarios can potentially be perceived to threaten the interests of some sections of the population.
While NHI has the potential to greatly benefit the country, some of the approaches that have been taken to it have the risk to turn potential allies into powerful opponents and jeopardise and endlessly delay the reforms. Some examples include:
• The inclusion of Section 33 in the NHI Bill,9 which states that medical schemes will only be able to provide top-up insurance once NHI is fully established, has been perceived as threatening by some. This provision does not exist in many countries and may be premature, as medical scheme members have not yet been able to build any trust in the NHI.
• The failure to demonstrate successful pilots of contracting private general practitioners and specialists has not built confidence among private sector users that they will be able to continue using service providers which they trust. It has also not brought private practitioners into the system, who are a powerful constituency.
• Low quality in the public sector (c.f. OHSC reports10), weak accountability, budget cuts, long queues, corruption, etc. can be perceived as obstacles, where users do not trust that the model being proposed is of acceptable quality and choice.
Addressing these kinds of challenges is a potential route for resolving constraints to reform.3 Prior to 2008, policy reforms had suggested a path of social health insurance focussing on the formally employed, which might have been an easier reform path, albeit less redistributive. After 2008, policy direction changed towards a universalist approach, echoing an emerging global direction towards UHC. However, given huge inequities, this shift potentially entails far greater redistribution (medical scheme spending exceeds government spending per capita more than five-fold). Addressing the needs of gaining as well as potentially losing parties is essential to build consensus around an implementable path.
The model selected for NHI (i.e. a centralised NHI Fund) requires legally shifting health services, which has been a provincial competency for almost a century, to become a national function (potentially delegated back to provinces). It is not only extremely complex administratively, but also threatens provincial power bases, noting also that health comprises almost 30% of provincial expenditure. These may not be stated explicitly, but nevertheless may be powerful underlying forces. In addition to natural reluctance of decentralised administrations to cede power to the centre, party political dynamics such as the Western Cape being governed by an opposition party and Gauteng having a narrow political majority in recent elections also complicate the reform.
Questions have been asked whether there is coherence across government on health financing reform for NHI. For its part, the Treasury is supportive of NHI financing reform, but is concerned by the slow pace of progress as described above and with on-the-ground reforms that citizens can see as improving options and services. The pace of funding and financing increases needs to be matched by performance and service improvements and good use of funds already allocated.
Recognising lack of progress and lack of consensus on health system and health financing reform, health and education rights law centre, SECTION27 sought to determine the views of different stakeholders across the system about the problems that exist currently and the kind of reforms that are needed. SECTION27 worked with Concentric Alliance, a conflict resolution and consensus-building company, to develop a questionnaire and to interview 34 people across the public and private health sectors, regulators and professional associations, civil society and labour. Interviews were conducted between November 2020 and August 2021 and dealt with the participants’ views on the foundational principles of a health system; what is most wrong with South Africa’s system at present; priority areas for reform; NHI as it is currently proposed; transitional steps in reform efforts; the potential of partnerships across the sector; and areas of consensus and divergence.
The interviews revealed important consensus on health and access to health care services as a right and that this requires both government provisioning and regulation. The inequality between public and private health sectors was recognised to be a problem by all participants. Many participants raised the need for greater investment in primary health care (PHC) services, both directly and through the training of professionals to work at this level. Almost all participants identified the absence of a universal system to monitor service provision, individual patients and health outcomes as a weakness.
In relation to NHI as it is currently formulated, the primary concerns related to its failure to address the problems in the public sector, such as NDoH capacity, weak governance, management and accountability, and in the private sector, in particular inefficiency and waste, and inadequate regulation. There was also a lack of clarity on priority issues including pricing, purchasing of services, financing and accreditation. They also identified as problems its targeting of medical schemes (largely through Section 33), which was described by people within both the public and private sectors as ideological and unnecessary and with insufficient consideration of transition (with reference to lack of evidence from piloting and lack of preparedness). Interestingly, nearly all participants felt that there is an important role for the private sector within NHI. While there was significant support for some form of NHI in South Africa amongst participants, the dominant view was that many questions remain unanswered, and this was seen as a problem by most participants.
Participants viewed the COVID-19 experience as instructive on what South Africa should expect with NHI. Some participants were impressed with the ‘reaching out’ of the private sector and expressed frustration (mostly from within the public service) with the public sector’s delays and lack of urgency in developing working relationships with the private sector. Others in the public sector had a different experience of private sector duplicity and unwillingness to contribute genuinely in the COVID-19 crisis. This recent experience coloured the participants’ views of NHI, its prospects and South Africa’s health system reform path.
Research undertaken by
Recommendations included focussing on strengthened governance and accountability mechanisms, the improvement of public sector infrastructure, training and retention of appropriate human resources for health, and the establishment of monitoring and evaluation systems based on health outcomes. A number of participants mostly supported piloting of interventions at district level to build systems and processes that enable accountable implementation of the NHI locally. National government participants tended to favour provincial-level piloting. Some participants proposed focussing on particular types of services to demonstrate success. Importantly, almost all participants, including those from the private sector, recommended a focus on private sector reform, including in relation to pricing, market concentration and a lack of transparency (key issues identified in the Health Market Inquiry).
The research demonstrated that health stakeholders want to help. There is broad appetite for health system and health financing reform and a willingness to talk. There remains a lack of trust between many stakeholders, which hampers open engagement, and a feeling that ideological lines have been drawn. The role of the private sector is an area of conflict, as is the role of provinces. Stakeholders in both of these areas have not been properly engaged, further entrenching distrust and opening the health reform process up to years of litigation and other delays.
The importance of engaging and building trust with key stakeholders is also evident from international reform processes. For example, in Turkey, assuring existing scheme beneficiaries that their entitlements would not be reduced was essential in building support. Further, consolidating pools into a single national scheme was only done at the end of the reform process, following practical progress in the areas of standardisation of benefits, increased provider payments and enrolment of informal sector beneficiaries. In Mexico, the Minister of Health engaged closely with legislators, including from other political parties, to help usher the reform through legislative process, but also had to be willing to reach compromises with key stakeholders in order to move the reform forward.11 In Malaysia, on the other hand, several past attempts at health financing reforms have failed, partly due to a lack of openness and inclusiveness in the reform process.12
South Africa’s most recent National Health Accounts (NHA) data is for 2016/17 and showed that total health expenditure in the country was R392.6 billion. This translates to 8.86% of GDP, of which government health expenditure was 5.1% of GDP and 14.95% of total government expenditure. The latter two percentages are higher than estimates often reported, because the NHA methodology adds government tax subsidies and employer contributions (for public servants) to medical schemes (together amounting to around R40 billion per annum) to public as opposed to private financing. Interestingly, the latter figure is close to the Abuja target of 15%, although using alternate measurement approaches and definitions yields various estimates varying from 12.6%–16% of government expenditure.
More recent data bringing together public and private spending is shown in Table 18.2, using data available to the National Treasury. Notably, the total health expenditure number for 2016/17 of R392.3 billion is virtually identical to that reported by the NHA for that year. Total health spending is estimated to have risen to R540 billion by 2020/21, with some of the increase in the latter year due to the COVID-19 response. Table 18.2 covers different areas of expenditure in South Africa’s two-tiered health system from 2015/16 to 2020/21. The table also indicates
expenditure from the private sector, which is made up of medical schemes, out-ofpocket expenditure, and medical insurance as well as expenditure by donors.
Table18.2 Consolidated health spending (public and private sectors)
Public health spending is largely funded by general tax revenue raised nationally, which is divided among the national, provincial and local spheres of governments. Given that health is currently largely a provincial function, provinces receive the bulk of the health budget, averaging 92% since 2015/16 of total health expenditure. The provincial health budgets are funded via provincial equitable share formula allocations via provincial governments and direct conditional grants (transferred via the NDoH).
The average annual growth rate in provincial health expenditure was 8.1% from 2015/16–2019/20, similar to the growth rate of 8.6% observed from 2011/2012 to 2014/15. Budget 2020/21 was substantially higher due to special allocations for the COVID-19 pandemic. However, in the subsequent years from 2021/2022 to 2023/2024 budgets have been substantially reduced with annual growth rate projected at only 1.8%, from R210.9 billion in 2019/20 to R226.4 billion in 2023/24. The financially constrained period post COVID-19 is discussed in more detail in a latter section.
Some of the reforms during the 2015–2020 period include additional allocations in support of NHI and health promotion for non-communicable diseases (NCDs), following introduction of a sugar-sweetened beverages tax. An additional R4.2 billion over three years from 2018/19–2020/21 was allocated for strengthening the health system and contracting priority services in preparation for wider NHI roll-out. These funds were obtained through capping growth on the medical tax credit. In 2018, a health promotion levy on sugary beverages was initiated. Although these funds were not earmarked for use by the health sector only, a portion of revenue generated from this
was to further support prevention programmes related to NCDs. However, there was significant underspending in these areas, most likely due to management constraints and difficulties in conceptualising how to use the NHI indirect grant in the absence of NHI legislation and an independent NHI Fund.
Overall spending performance by provincial health departments was above 99% between 2015/16 and 2019/20. Underspending was somewhat higher in 2020/21, amounting to R3.2 billion. While spending on conditional grants also performed fairly well during this period, there was under-expenditure mainly of the Health Facility Revitalisation Grant, attributed mainly to slow contractor performance and other problems in infrastructure delivery. A significant portion of the under-expenditure emanated from KwaZulu-Natal (KZN) (R1.9 billion) and Gauteng (R1.1 billion).
Between 2015/16 and 2020/21, provincial spending on health grew from R154 billion to R210 billion, an average annual rate of increase of 8.2% (Table 18.3). There are several factors that influenced the increase in expenditure in the sector over the period under review. The first is growth in the general population, which increased by over 4 million over the same period (at an annual growth rate of 1.6%). Secondly, expenditure on core goods and services items such as medicine and medical supplies are affected by medical inflation and by exchange rate fluctuation, which puts pressure on provincial budgets for these items. Despite the overall underspending, medicines and medical supplies were overspent by over R2 billion in total between 2015/16 and 2019/20. Furthermore, large amounts of accruals and payables not recognised were incurred by the sector during the same period, reflecting unpaid bills which increased from R10.2 billion at the end of 2015/16 to R15.3 billion at end of
2020/21, a strong signal of pressure on these budgets. This is likely to reflect both a degree of under-budgeting and inappropriate use and management of resources, e.g. over-prescribing, inadequate laboratory gatekeeping and inadequate controls over personnel costs.
Spending is expected to reach R226.4 billion in 2023/24 at an annual average growth rate of 4.9% since 2015/16. However, there is a declining trend between 2020/21 and 2023/24 which is partly attributed to once-off additional funding that was available for COVID-19 response in both 2020/21 and 2021/22. Furthermore, there were significant reductions in the baseline allocations for compensation of employees across national and provincial departments due to the anticipated zero increase in the salaries of public servants over the 2021 medium-term expenditure framework (MTEF) period. Reductions were also effected on other items as part of government-wide fiscal consolidation.
While the growth in provincial expenditure may seem favourable, there remains budget pressures and threats such as accruals, medico-legal claims (both discussed later in this chapter), widening and changing pattern of disease burden (because of NCDs), corruption, and poorly funded training of medical students, among other issues.
District health services make up approximately 46.3% of total provincial spending over the observed period, followed by central hospital services at 20.4% and provincial hospital services at 17.9%. It is also worth noting that significant investments in district health services, consequently PHC, is consistent with the country’s focus on achieving UHC through implementation of the NHI, which is highly embedded on the PHC service platform13. Sustainable financing of PHC is fundamental in achieving goals such as equity, improved access to health care services, reduced financial risk for users and providing care at low cost.14,15 However, achievement of these is not solely contingent on availability of funds but on other components as well such as availability of health workforce, medicines and supplies, leadership and governance, and good financial management.
While the focus is on strengthening investments in PHC services (housed under district health services), the central hospital services programme had a rapid growth at an annual average growth of 10.9% compared to 8.9% for overall district health services. In PHC services, the main driver of expenditure is the HIV/AIDS sub-programme,
also with the highest annual average growth rate of 15.6% from 2015/16 to 2019/20. This is largely due to additional allocations to the HIV/AIDS conditional grant from 2017/18 onwards, in support of the implementation of the universal test and treat policy, in line with the targets set by the United Nations Programme on HIV/AIDS16 (see also Chapter on National Health Programmes).
According to the World Health Organization (WHO), countries may find it difficult to achieve UHC with health spending less than 4–5% of GDP17 . In 2001, heads of state of the African Union pledged that 15% of the government annual budget should be allocated to the health sector, a target commonly referred to as the Abuja Declaration target18. As shown in, total government health expenditure has remained relatively stable at approximately 4.2% of GDP over the period under review and around 14% of the overall government budget. This is close to the Abuja Declaration target and higher than several other upper-middle-income countries’ (UMIC) spend (see Table 18.4 and), indicating significant political commitment in prioritising health.
As shown in Table 18.4 and, South Africa’s level of public health financing compares fairly well with other UMICs, in terms of current health expenditure (CHE) and domestic general government health expenditure (GGHE-D) per capita, and as percentages of general government expenditure (GGE) and of GDP. Out-of-pocket (OOP) expenditure as a percentage of health expenditure is amongst the lowest in this group at 7.7%, far below the UMIC average of 32.6%. Catastrophic health expenditure is not routinely monitored, but a recent study by Koch and Setshegetso found that the share of household expenditure going to health increased between 1995 and 2010, but that catastrophic health expenditure was still relatively rare, and that very few households were impoverished due to health care costs. However, it may be more common for certain groups, such as chronic patients. South Africa does have a high burden of disease especially due to HIV/AIDS and has unit costs of personnel that exceed most comparable-income countries , and life expectancy is considerably below that of UMIC peer countries. Under NHI it has been projected that public financing will rise from 4% to 6% of GDP.
Figure 18.2 Government health spending as percentage of GDP and as percentage of total government expenditure
Table 18.4 Key health financing indicators in upper-middle-income countries, 2018
CHE per capita in US$
GGHED per capita in US$
CHE as % of GDP
GGHED as % of GDP
GGHED as % of CHE
OOP as % of CHE
GGHED as % GGE
GDP per Capita in US$
Argentina 1 128 693 9.6 5.9 61.4 27.7 15.2 11 719
Cuba 987 877 11.2 9.9 88.9 11.0 15.2 8 822
Brazil 848 354 9.5 4.0 41.7 27.5 10.3 8 917
Romania 687 548 5.6 4.4 79.7 19.5 12.7 12 368
Russian Federation 609 362 5.3 3.2 59.5 38.3 9.8 11 456
South Africa 526 284 8.3 4.5 54.0 7.7 13.3 6 373
Mexico 520 260 5.4 2.7 50.1 42.1 10.5 9 673
Ecuador 516 268 8.1 4.2 52.0 39.8 11.4 6 345
Colombia 513 367 7.6 5.5 71.6 15.1 19.6 6 717
China 501 283 5.4 3.0 56.4 35.8 8.9 9 364
Iran 484 222 8.7 4.0 45.9 35.8 21.8 5 591
Dominican Republic 462 204 5.7 2.5 44.3 44.7 15.4 8 051
Malaysia 427 219 3.8 1.9 51.2 35.1 8.5 11373
Turkey 390 302 4.1 3.2 77.4 17.5 9.3 9 453
Peru 369 231 5.2 3.3 62.6 29.2 15.3 7 046
Thailand 276 210 3.8 2.9 76.3 11.0 15.0 7 274
Kazakhstan 276 168 2.9 1.8 60.8 33.5 9.1 9 440
Guatemala 260 93 5.7 2.1 36.0 57.5 16.7 4 549 Venezuela (Bolivarian Republic of) 257 123 3.6 1.7 47.8 38.2 3.7 7 212
Algeria 256 168 6.2 4.1 65.8 32.6 10.7 4 115 Iraq 239 115 4.1 2.0 48.1 51.4 6.2 5 830
Sri Lanka 157 65 3.8 1.5 41.1 50.7 8.3 4 190
UMIC simple average 477.5 280 7.5 3.9 56.4 32.6 12.4 7 364
Acronyms: CHE = current health expenditure (including public and private); GDP = gross domestic product; GGHE-D = domestic general government health expenditure; GGE = general government expenditure; OOP = out-of-pocket expenditure
Source: Global Health Expenditure Database, accessed 29 August 2021
Figure 18.3 Health financing indicators and life expectancy compared to other UMICs, 2017
* South Africa shown as blue dot, other UMICs as grey dots and UMIC average as black line
Figure 18.3 is sourced from the Africa scorecard on domestic financing for health using 2017 data (https://scorecard.africa/23) and the countries presented here are African countries in the UMIC group. The figure indicates that South Africa is doing fairly well in terms of prioritising health in government expenditure, e.g. spending 13.3% of government budget in 2017 (their definition), which was an improvement from 2015, despite a low growth in revenue (from 5.7% in 2016/17 to 5.1% in 2017/18). The numbers also suggest that as government prioritises health expenditure (with a percentage of health expenditure against total government expenditure moving closer to 15%), performance in the UHC coverage index improves. Generally, countries that have a high proportion of domestic sources in financing health tend to perform better in the UHC service coverage index, e.g. South Africa, Namibia and Botswana. Countries such as Mauritius nevertheless scored fairly well, although domestic funding share is lower than 50%, and their government spending per capita is fairly high ($244), being closer to that of Namibia ($249). The WHO suggests that significant investments in domestic funding for health care is essential to achieve UHC24. In general, while public funding for health care in South Africa compares well with other UMICs, health outcomes such as life expectancy are much worse than most income comparable UMICs, such as Brazil, Vietnam, Thailand, Turkey and Indonesia. This is partly due to HIV/AIDS, but also due to significant levels of household poverty, unemployment and inequality, high input costs, substantial inequities betweenpublic and private spending and inefficiencies and management weaknesses.

Source: https://scorecard.africa/25
In the previous edition of this publication, McIntyre, Brijlal and Nkosi26 highlighted inequitable level of health care expenditure across provinces as a major challenge in the health system, with the lowest spending province per capita in 2012/13 (Mpumalanga) spending around 15% below the national average and the highest (Western Cape) more than 30% above this average. They recommended that these inequities be addressed by directing additional funds towards relatively under-resourced provinces (and districts) rather than ‘robbing Peter to pay Paul’ within a stagnant funding envelope.
As seen elsewhere in this chapter, real per capita expenditure has indeed increased over the past five years (although not so going forward – see Figure 18.8 below. Our estimates presented in show that while considerable differences remain, it seems as if the variations between provinces have narrowed, with both lower- and higher-spending provinces moving closer to the national average between 2015/16 and 2019/20. It thus seems that progress has been made in line with the aforementioned authors’ recommendations. This is likely the result of a combination of factors, including the provincial equitable share (PES) funding formula, annual benchmarking exercises with provincial treasuries, and the HIV conditional grant making up an increasing share of health expenditure and in many cases benefiting otherwise under-resourced provinces. The health component of the PES formula has been revised for Budget 2022 and onwards to further improve equity in inter-provincial resource distribution. It is also important to note that some variation between provinces may be warranted due to differences in demographics and disease burden, and that tertiary hospital services tend to be concentrated in urban centres with patients from more rural provinces often being referred to these.

Figure 18.4 The Africa Scorecard on Domestic Financing for Health, 2017, UMIC countries
Source: Author calculations based on data from National Treasury27
Health expenditure per capita varies, not only between provinces, but even more so between districts, often even within the same province.
Table 18.5 shows, for each province and for the whole country, PHC expenditure per capita in the lowest and highest spending districts and the ratio between the two.28 The highest spending district in the country in 2019/20 (Namakwa in Northern Cape) spent 2.5 times more than the lowest spending district (Joe Gqabi in Eastern Cape), which is a smaller ratio than in 2012/13 when the same ratio was 2.9. This ratio differs considerably between provinces with some provinces, e.g. Limpopo and Mpumalanga, having relatively small internal variation and others, e.g. Northern Cape and Western Cape, having a relatively high ratio of 2.2 and 2.0, respectively. More systematic and evidence-based approaches to allocating funding across districts would likely improve equity and could form the basis for the capitation reimbursement mechanism envisaged under NHI. The National Treasury and Western Cape Province have worked with actuaries to develop an equitable district allocation formula, which is under discussion.
The private health care industry in South Africa is substantial, consuming large proportions of the country’s available resources in the form of general practitioners, specialists, nurses, hospitals, and hospital beds.
Medical schemes are at the front and centre of the private health care industry due to their role as the main vehicle for providing financing. The medical schemes industry is broad and fulfils the roles of financing, pooling, managed care and administration30 Notwithstanding the contribution made by medical schemes towards private financing for health care, they are perceived partly as drivers of the inequality and inefficiencies that have been and remain a key feature of the South African health care system. The Health Market Inquiry (see below), discussed elsewhere in this chapter, has brought into focus a range of factors that are leading to affordability problems in the medical scheme environment.
According to the NHA exercise done in 2013/2014, South Africa invests 8.7% of its GDP on health expenditure. The proportions of health expenditure covered in both the public and private sectors were split almost evenly at 47% and 43%, respectively, despite more than 80% of the population relying on the public sector. This is notwithstanding the observed ‘maldistribution of resources between the public and private health sectors relative to the population each serves’31. The amount spent by a medical scheme beneficiary translates to a multiple of five times the amount per capita compared to that available to a patient funded by tax in the public sector. Annual contributions paid by members to medical schemes increased from R151.6 billion in 2015 to R205.8 billion in 2019, but the total number of medical scheme beneficiaries has on average either stagnated or declined over the same period,
showing negative growth between 2014 and 2017 and a slight increase in 2019. There is evidence to suggest that members are migrating to lower-cost benefit options or deregistering dependents as a result of affordability pressure.
The amount paid in contribution in terms of beneficiaries per capita has increased from R17 272 in 2015 to R22 891 in 2019, vs R4 667 per capita in the public sector. The rate of contribution increases has consistently exceeded the Consumer Price Index during the past 20 years. Medical schemes are subject to limited income cross-subsidisation through a tax credit applied to partially offset contributions. It has been argued by some that the tax credit is a subsidy to higher-income earners and that it must be removed. A counter argument is that the tax credit has the effect of alleviating pressure from health facilities in the public sector, and after introducing caps it is now smaller per person than the public sector subsidy. As NHI evolves it is likely that this tax subsidy will be progressively phased down, although this is partly dependent on acceptable alternate arrangements being put in place under the NHI.
The largest share of expenditure in the private sector goes to private hospitals, followed closely by pharmaceuticals and medical specialists, as illustrated in Figure 18.6 below.

The Health Market Inquiry published its final report and recommendations in September 2019. The Inquiry had been instituted by the Competition Commission of South Africa in 2014 to investigate factors that were preventing, distorting, or restricting competition in the private health sector.32 The Inquiry was established after concerns from the national government that the nature of price determination and lack of competition were resulting in excessive pricing. A review of the HMI report shows that even though its focus was the private health care market, it covers many areas that are key to health system reform and has implications for the roll-out of the NHI. The HMI report provides a systematic and comprehensive documentation of issues plaguing the South Africa health system, albeit with a private health care sector focus.
The Inquiry notes that ‘the South African private health sector suffers from multiple market failures. The sector comprises a complex set of interrelated stakeholders who interact with one another in an imperfect environment replete with information asymmetry, a lack of transparency and moral hazard’.
The HMI makes important findings on the supply of practitioners, who are important for successful roll-out of the NHI. In particular, the inquiry concludes that better use of available practitioners could result in improved access and costs. While there are valid concerns on the shortage of practitioners in the country, there is sufficient indication that practitioners are concentrated in the private sector despite the medical scheme population remaining stagnant for a sustained period. The HMI found that practitioners are concentrated in the private sector at a rate of 1.75 per 1 000 population for specialists and just under 1 per 1 000 population for general practitioners. This is in stark contrast to the public sector where these ratios are 0.1 for specialists and 0.4 for general practitioners. Of interest to the NHI is that most doctors are concentrated in provincial capitals and metropolitan areas, which has implications for access for the population outside of these areas. The design of the NHI would either need to introduce incentives for doctors to consider relocating to undersupplied areas or put in place innovative referral mechanisms that enable the population in remote locations access to doctors. Another observation made by the inquiry is that doctors are accustomed to working in solo practices, except for single-discipline group practices such as radiologists, some anaesthetists, and corporate pathology groups (Nkonki et al., 2019). For health care service delivery under the NHI to function as envisaged, the introduction of multidisciplinary groups that allow for more efficient referral of patients would be necessary.
The inquiry identifies behaviour that contributes to wastage of resources such as inappropriate use of services of specialists by patients and unnecessary referrals to high care wards and ICUs. Hospital admission rates were observed to be increasing at 1.99% on a yearly basis between 2010 and 2014. The increase in hospital admissions is associated with the concentration of specialists, a finding which led the inquiry to conclude that supplier-induced demand existed.
The Inquiry recommended amongst others:
• changes to the way scheme options are structured to increase comparability between schemes and increase competition in that market;
• a system to increase transparency on health outcomes to allow for value purchasing;
• a set of interventions to improve competition in the market through a supply side regulator.
One of the key recommendations of the HMI is the introduction of a standardised benefit structure, as follows:
‘Alongside the standardisation of benefits, a risk adjustment mechanism must be implemented. The risk adjustment mechanism will “equalise” risk associated with the standard benefit option across all schemes. Risk adjustment would be of little use if it is not applied to a standard basket of benefits. In the absence of a standard package, it would be impossible to measure the risk across schemes fairly. Therefore, as indicated above, the HMI proposes that a risk adjustment mechanism be implemented for the base benefit package to be offered by all schemes.’
Importantly, the recommendation to introduce a risk adjustment mechanism was not new and earlier in 2005, the Council for Medical Schemes had started a process to simulate implementation of such an intervention. The effort was abandoned when implementation of the NHI was announced in 2009. A key concern with the medical schemes’ environment is the fragmentation of risk pools through the proliferation of numerous benefit options. The recommendation to formulate a standardised benefit package on which a risk-adjustment mechanism would be applied is a plausible option to alleviate this concern.
The HMI report has been characterised as the most systematic and comprehensive investigation carried out into the South Africa private health sector.33 Since publication of the report however, there has not been extensive debate of the key findings and recommendations and the NDoH has not yet given any signal that it would seek to investigate implementation of any of the recommendations.
The HMI recommended that the role of the Council for Medical Schemes be extended and that it should define a new base benefit package which would be part of the foundation to create a basic package for the NHI. The creation of a new base benefit package is recommended alongside the creation of a risk-sharing mechanism.
Currently, both the public and private sectors struggle with the provision of a comprehensive set of services.
In the public sector, the challenges can be summarised as:
a) Service delivery is organised in terms of levels of care, however, facilities of equal level of care do not provide the same set of services.
b) Access to resources – financial, human, medicines, equipment and supplies, are all contributors to inequity in access to services.
c) Quality of care and ability to maintain service delivery standards is another indicator of poor, or inequity in access.
The lack of providing people with equal treatment is not unique to the public sector. Private sector challenges include:
a) Every year, benefits are reduced, in terms of benefit limits or types of interventions that will be funded.
b) Primary health care is largely discretionary and not a prescribed minimum benefit, and used more from a competitive advantage perspective as opposed to ensuring access to care.
Inequity in access tends to be driven by income and contribution levels as compared to geographic access in the private sector. A costed service benefit framework, that is provided within both the public and private sectors is critical to ensuring the NHI is able to transition towards UHC. The key question is how to get there. During the time period covered by the review, the following key activities were initiated that began the movement towards a single common set of services and other financing reforms:
a) Approval of the White Paper on NHI
b) Draft NHI Bill was approved by Cabinet and submitted to Parliament for consideration
c) Draft Medical Schemes Act Amendment Bill was published for public comment.
In addition, various transition processes were initiated:
• In the public sector, the National Treasury commissioned development of a new formula for the health component of the Provincial Equitable Share formula, which takes into account population weighted by age and sex, deprivation index, rurality and premature mortality, amongst others. The new formula has now been adopted and is being phased in from 2022/23 and onwards and will contribute to more equitable provincial allocations. A potential district allocation formula was also developed, complementing regular reviews of district spending.28
• In the private sector, whilst the amendment to the Medical Schemes Act is required, the Council for Medical Schemes has started a process of drafting new regulations that replace the prescribed minimum benefits with a standard set of services that every benefit option provides for.
Although public sector health budgets increased in real terms and per capita during the period of review, these increases were to a large extent offset by growing cost pressures and other challenges in the sector, such as accruals, medico-legal claims, increasing personnel costs, and pressures in the goods and services budgets. These areas are discussed below.
Table 18.6 shows the total value of unpaid accounts/invoices between 2015/16 and 2020/21. The total value of these accounts increased from R10.2 billion in 2015/16 to R15.3 billion in 2020/21. However, there has been a notable year-on-year reduction between 2018/19 and 2019/20, mostly in Gauteng, Limpopo and Mpumalanga. There are large differences between provinces when looking at the annual growth rates of accruals, with the Eastern Cape (23%), Western Cape (18%) and North West (14%) showing the largest annual increases in the period. The year-on-year increase in 2020/21 amounted to R2.4 billion, with Gauteng and Eastern Cape as the main drivers.
Table 18.6 Accruals and payables not recognised (unpaid accounts), 2015/16 – 2019/20
To understand the budget impact of accruals it is useful to show them as a percentage of expenditure, as described in the table per province. One can note that the Eastern Cape is particularly badly affected by the unpaid accounts, as accruals was equivalent to around 16% of total provincial expenditure in 2019/20.
Spending on health personnel increased from R96.7 billion in 2015/16 to R131.2 billion in 2019/20, representing an annual average growth rate of 7.9% over the period (Table 18.7) (see also discussion in the Chapter on Human Resources for Health). The most significant increases were in the North West, Northern Cape and Gauteng. Personnel numbers overall were, however, on a declining trajectory between 2015/16 and 2018/19 before increasing significantly in 2019/20. However, some categories, such as doctors, have increased consistently during this period (Table 18.8). The main driver in expenditure growth in human resources relates mainly to wage increases, as the average CoE expenditure per employee increased from R312 874 in 2015/16 to R412 220 in 2019/20iii. There was a decline from 2021/22 to 2022/23 due to the once-off funding allocated for COVID-19 response and a reduction in budgets for compensation of employees over the 2021 MTEF.
Limpopo spends close to 70% of its budget on compensation of employees, which crowds out spending on medicines, medical supplies and other key service delivery costs, and moving forward the province needs to better control its personnel spending.
iii Authors’ calculations based on data presented in Tables 18.6 and 18.7.
The public sector provincial personnel numbers started increasing in 2019/20 driven mostly by increases in medical practitioners and professional nurses. The increase in the number of employees in the Free State, KZN, Limpopo and the North West relate to community health workers (CHWs). The Free State and Limpopo added over 2 000 and 8 000 CHWs from May 2019, respectively, but this reflects more the addition of these cadres to the government PERSAL system, as opposed to more feet on the ground. Further increases in 2020/21 were driven by additional appointments as part of the COVID-19 response.
There is a skewed distribution of medical specialists across provinces (e.g. 24 per 100 000 in Western Cape vs 1 per 100 000 in Limpopo), with a high concentration in Gauteng and the Western Cape, partly since six of the country’s 10 central hospitals are in these two provinces (Table 18.9). The average number of medical specialists per 100 000 uninsured population has decreased from 11 per 100 000 in March 2016 to 10 per 100 000 in March 2020. The decline emanates mainly from Gauteng and the Western Cape, which account for the highest number of specialists. The number of doctors has increased between 2016 and 2020, but there are many provinces that experienced fluctuations over the same period. The number of professional nurses per 100 000 population declined from 153 to 151 during the same period (Table 18.9). Despite uninsured population increases, the number of nurses decreased in absolute terms in provinces such as the Free State and Limpopo.
As shown in Table 18.10, goods and services spending per capita (uninsured population) increased by 8.5% per year between 2015/16 and 2019/20 and is expected to increase by 4.6% per year between 2015/16 and 2023/24. The highest increases were in Limpopo and the Eastern Cape, though the two provinces are still spending below the national average. The Northern Cape has the highest spending per capita compared to other provinces followed by Gauteng, KZN and the Western Cape.
The high spending in the Northern Cape could be partially attributed to population sparsity, which is one of the factors driving health expenditure across many countries. Spending per capita is projected to decline significantly in real terms between 2020/21 and 2023/24, mainly due to the once-off additional funding made available for COVID-19 response and fiscal constraints over the MTEF. These numbers will need to be continuously re-evaluated as the budget reductions over the MTEF are substantial in key goods areas.
Table 18.10 Goods and services spending per capita (uninsured), 2015/16 – 2023/24
The sector saw an explosion of medico-legal claims during the period. Table 18.11 shows that, between 2015/16 and 2020/21, the contingent liability on medico-legal claims more than doubled from R43.1 billion to R120.3 billion. Actual expenditure on settlements is much lower, but grew from R985 million to R1.7 billion during the same period. Eastern Cape accounts for the highest share of the contingent liability at 37.7% followed by Gauteng and KZNiv. The average annual growth rate of medical legal liabilities is around 23%, meaning that even though payments are less than 1% of liabilities, their budget impact is growing exponentially. Generally, provincial budgets for medico-legal payments are conservative or not budgeted for at all during the period under review and many reforms are required in the area of medico-legal.
Table 18.11 Medico-legal claims contingent liability, 2015/16 – 2020/21
iv It is important to note that each province uses its own ‘method’ to measure contingent liabilities, which makes cross-provincial comparison difficult.
Cerebral palsy-type claims make up around 50% of all claims and 60% of total liabilities. Effective interventions targeted at obstetrics and gynaecology would therefore likely demonstrate significant return on investment. The problem is also highly skewed to a set number of facilities, with around 4% of facilities representing 84% of the claims.
Although quality of care in the public sector is often inadequate and is one of the root causes, this escalation cannot be explained merely by an increase in malpractice and negligence. There are several and often complex reasons, including increasingly litigious behaviour from law firms that target the sector. Many provincial health departments have struggled to cope with this pressure and are left partly defenceless due to weak legal capacity, inadequate processes for managing claims, poor record keeping (with some cases relating to incidences more than a decade old), and in some instances fraudulent claims and allegations of corruption. The South African Law Reform Commission has made some recommendations for coming to terms with this problem. The NDoH has established a central expert medical specialist team to assist provinces with medico-legal matters. Amendments to the State Liability Act of 1957 have been proposed to provide for periodic payments (rather than lump sums) and for future medical treatment to be provided by the state in kind instead of paying high private sector rates. Other reforms, which have been implemented by other countries and need to be explored in more detail in South Africa include a no-fault compensation system, capping of claims and defined schedules, mediation, doing away with once-and-for-all payments, and focusing more on rehabilitation and other interventions.
The health sector with National Treasury and the provincial treasuries initiated a Joint Health Action Plan to assist the sector to devise accrual intervention strategies; better align procurement plans with approved budgets and cash flow projections; and address procurement, supply chain, medico-legal and infrastructure issues. Joint projects are being undertaken in some provinces in the sector in order to improve financial management and human resources. Such projects include the piloting of the approved post lists and budget monitoring tools for hospitals in Mpumalanga and Free State which are working with the Western Cape to roll these out. A health system review is being undertaken in North West province.
National Treasury is drawing from international experience in attempting to introduce some aspects of gender-responsive budgeting. The new provincial equitable share formula, used to allocate funds to provinces contains elements which include age and sex and fertility, to take into account differential costs such as for maternity. Health service utilisation rates tend to be higher amongst women. More attention may need to be given to a number of specific reproductive health and other services.
The last year of the period in focus was marked by the global health security crisis caused by the COVID-19 pandemic (see Chapter on Emergencies and COVID-19).
A special adjustments budget was tabled in June 2020, allocating or reprioritising more than R21 billion to the health sector’s response (Table 18.12), the vast majority going to provincial departments of health which together received a net budget increase of R17 billion, with further amounts reprioritised internally.
Table 18.12 Summary of health allocations for COVID-19 in the 2020 special adjustments budget
South Africa initially chose to procure vaccines via COVAX, with agreements signed in December 2020, but shortly thereafter also sourced vaccine supply directly from manufacturers, primarily Pfizer and Johnson & Johnson. To this end, a total of R15.3 billion has been allocated over 2021/22 and 2022/23 for purchasing and administering vaccines. Amounts of R8 billion in 2021/22 and R7.4 billion in 2022/23 have also been allocated to the sector for responding to further waves of infections.
The economic impact of the pandemic and the ensuing lockdown measures were massive, with GDP contracting by -7% in 2020.34 Revenue in 2020/21 dropped considerably and coupled with the fiscal response package, it resulted in a government deficit of approximately 15% of GDP in that year Error! Reference source not found. The carry-through implications of the economic contraction on government budgets are severe, with Budget 2021 containing budget reductions of R264 billion over three years to stabilise debt by 2024/25 and avoid a sovereign debt crisis.35
Source: National Treasury
These reductions impact all sectors, including health, with R76.4 billion of reductions in provincial health departments between 2021/22 and 2023/24.v For the first time in over two decades, real per capita expenditure on health is expected to decline between 2020/21 and 2023/24 (Figure 18.8), even compared to pre-pandemic levels.

Figure 18.8 Provincial health budgets, 2000/01 – 2023/24
A considerable share of these reductions could be absorbed by savings from a public sector wage freeze, given that over 60% of health budgets are spent on compensation of employees. However, the total reductions exceed these potential savings and will have to be managed carefully so as not to harm frontline services. As revenue projections improved somewhat for Budget 2022, additional allocations were made to the sector to partially reduce the impact of the previous budget reductions. These additions are not reflected in the tables presented in this chapter.
It is possible that the NHI model envisaged in the current NHI Bill may have been significantly challenged by the events that unfolded in 2021, when financial irregularities and capacity constraints emerged in the NDoH, especially around the Digital Vibes sagavi. This matter is likely to weaken public confidence in a monopolistic central NHI Fund controlled substantially by a small number of individuals. It would be a pity if this derailed the entire NHI permanently. However, spill-over effects of the scandal might prompt re-examination of aspects of the model, noting that there are many successful but different models of NHI internationally, including single vs multiple funds, centralisation vs decentralisation (c.f. Australia, Canada, Netherlands and German models) and the location, nature and balance of powers. For example, the Thai Universal Care Fund is under a diverse board with multiple different stakeholders from different constituencies providing a balance of powers.
Trust needs to be built for NHI, through manifest improvement in options and services. Compromise might be required around sections of the Bill such as Section 33 to avoid endless legal challenges. Attention needs to be given to building compromise around the Bill and subsequent reforms. Part of this is giving users greater rather than fewer choices and includes building mixed provider platforms in an effective and efficient way, using smart strategic purchasing and systems.
Confidence of provinces needs to be retained, through rapid re-introduction of delegation of responsibilities for service delivery (noting that legal shift of function to national sphere is required to centralise funding). Without this not only will provincial powerbases obstruct the reforms, but major risks arise in which parts of the health service could collapse in an interregnum in which functions and funds are transferred to the centre. NHI continues to offer major opportunities for the sector, however, opportunities in this regard have not been used to best advantage over the period reviewed.
COVID-19 and its associated lengthy lockdowns have caused severe damage to the fiscus, which is likely to take at least three years to fully recover36. As shown above, although health budgets were augmented for COVID-19 in 20/21, as the effect of the pandemic and prolonged economic lockdowns fed through to the fiscus, health budgets over the MTEF were substantially reduced by R76 billion in Budget 2021, as a result of the economic recession, weaker fiscal position and worsening debt position following COVID-19 and prolonged lockdowns37. In this context, funding major new policies such as NHI is likely to be difficult, also noting competing spending pressures. Because of this, if major new system reforms are not very well managed, are not building trust and consensus, and not showing evidence of strong performance, they are unlikely to compete effectively.
vi https://www.gov.za/speeches/minister-joe-phaahla-response-release-investigation-reportdigital-vibes-communication
1) The Portfolio Committee on Health and Government should review aspects of the model of NHI, including in the NHI Bill, to rebuild confidence, noting that a range of successful NHI models exist internationally. This might include reviewing single vs multiple funds, balance of centralisation vs decentralisation and vesting and balance of powers. Substantial improvements in managerial capacity to implement NHI reforms are required, since progress on this key reform has been jeopardised by poor progress and insufficient managerial capacity for implementation.
2) The COVID-19 pandemic has substantially threatened the fiscus and placed health and other social sectoral budgets at risk over the MTEF. This will require continued budgetary evaluation. Health outcomes after years of improvement have been significantly threatened by COVID-19 and service disruptions and backlogs have occurred. Widespread roll-out of COVID-19 vaccinations and addressing services backlogs will be required to get health outcome improvements back on track.
3) The new health component of the Provincial Equitable Share formula has provided an important update to the formula and improved equity, benefiting poorer provinces such as Eastern Cape and Limpopo. Progress in its implementation should be monitored.
1. Department of Health. National Health Insurance policy towards universal healthcare. Government Gazette 2017; 627: 30 June 2017.
2. National Department of Health. National Health Insurance in South Africa – Policy Paper. Pretoria: National Department of Health, 2011.
3. Blecher MS, Daven J, Harrison S, et al. National Health Insurance: Vision, Challenges and Solutions. In: Moeti T, Paradath A, editors. South African Health Review 2019. Durban: Health Systems Trust; 2019. Available at: http:// www.hst.org.za/publications/Pages/SAHR2019
4. Minister of Health. National Health Insurance Bill, 2019. Government Gazette; 209: B11.
5. Department of Health. White Paper on the transformation of the health system in South Africa. Governmet Gazette, Pretoria: 1997.
6. Blecher MS, Pillay A, Patcharanarunamol W, et al. Health financing lessons from Thailand for South Africa on the path towards universal health coverage. South African Medical Journal. 2016;106(6):533–6.
7. Ramjee S. Support for National Health Insurance and Infrastructure investment. National Treasury. Government Technical Advisory Service; Pretoria: 2018.
8. Moosa S. Support to the implementation of NHI capitation reforms contract model National Treasury, GTAC, Pretoria: 2018.
9. Minister of Health. National Health Insurance Bill, 2019. Government Gazette; 209: B11.
10. Office of Health Standards Compliance. Annual Inspection Report, 2018/19. Pretoria: OHSC, 2019. Available at: https://ohsc.org.za/wp-content/uploads/ Annual-Inspection-Report-_2018-19_Report_02-Mar-20-1.pdf
11. Sparkes SP, Bump JB, Özçelik EA, Kutzin J, Reich MR. Political economy analysis for health financing reform. Health Systems & Reform. 2019 Jul 3;5(3):183–94.
12. Croke K, Mohd Yusoff MB, Abdullah Z, Mohd Hanafiah AN, Mokhtaruddin K, Ramli ES, Borhan NF, Almodovar-Diaz Y, Atun R, Virk AK. The political economy of health financing reform in Malaysia. Health Policy and Planning. 2019 Dec 1;34(10):732–9.
13. Matcoso MP, Hunter JR, Brijlal V. Embedding quality at the core of universal health coverage in South Africa. Lancet Glob Health. 2018;6(11). Available: https:// www.thelancet.com/journals/langlo/article/PIIS2214-109X(18)30323-1/ fulltext
14. World Health Organization. The world health report 2008: Primary health care now more than ever. 2008. Geneva, Switzerland: World Health Organization. Available: http://www.who.int/whr/2008/whr08_ en.pdf.
15. Wong ST, Browne AJ, Varcoe C, et al. Development of health equity indicators in primary health care organizations using a modified Delphi. PLoS One. 2014;9(12). Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4257722/pdf/ pone.0114563.pdf
16. Joint United Nations Programme on HIV/AIDS. Fast-track ending the AIDS epidemic by 2030. [Internet] Available: https://www.unaids.org/sites/default/ files/media_asset/JC2686_WAD2014report_en.pdf
17. World Health Organization. Spending targets for health: no magic number. 2016. [Internet] Available: https://www.who.int/health_financing/documents/ no-magic-number/en/
18. World Health Organization. The Abuja Declaration: ten years on. [Internet] Available: https://www.who.int/healthsystems/publications/abuja_report_ aug_2011.pdf?ua=1
19. Koch SF, Setshegetso N. Catastrophic health expenditures arising from out-of-pocket payments: Evidence from South African income and expenditure surveys. PloS One. 2020 Aug 11;15(8):e0237217.
20. Mutyambizi C, Pavlova M, Hongoro C, et al. Incidence, socio-economic inequalities and determinants of catastrophic health expenditure and impoverishment for diabetes care in South Africa: a study at two public hospitals in Tshwane. Int J Equity Health. 2019;18:73.
21. Serje J, Bertram MY, Brindley C, Lauer JA. Global health worker salary estimates: an econometric analysis of global earnings data. Cost Effectiveness and Resource Allocation. 2018 Dec;16(1):1–9.
22. Hernandez-Peña P, Poullier JP, Van Mosseveld CJM, et al. Health worker remuneration in WHO Member States. Bulletin of the World Health Organization 2013;91:808–815.
23. The Global Fund. The Africa Scorecard on Domestic Financing for Health. 2017. [internet] Available: https://scorecard.africa/
24. World Health Organization (WHO). Health Systems Financing: The Path to Universal Coverage. World Health Report 2010, WHO, Geneva. 2010. [Internet] Available: https://www.who.int/whr/2010/en/
25. The Global Fund. The Africa Scorecard on Domestic Financing for Health. 2017. [internet] Available: https://scorecard.africa/
26. McIntyre D, Brijlal V, Nkosi, M. Chapter 6: Health systems financing. In: Matsoso MP, Fryatt RJ, Andrews G (eds). The South Africa health reforms 2009–2014: Moving towards universal coverage. Cape Town: Juta and Company; 2015.
27. National Treasury. Estimates of Provincial Revenue and Expenditure. [Internet] Available: http://www.treasury.gov.za/documents/provincial%20budget/ default.aspx
28. Massyn N, Day C, Ndlovu N, Padayachee T. District Health Barometer 2019/20 datafile. Durban: Health Systems Trust; 2020. Available: https://www.hst.org.za/ publications/Pages/DHB2019-20.aspx
29. National Department of Health. National Health Insurance White Paper. Pretoria: NDoH; 2017.
30. Ramjee S, Vieyra T, Abraham M, Kaplan J, Taylor R. National Health Insurance and South Africa’s Private Sector. In: Padarath A, English R, editors. South African Health Review 2013/14. Durban: Health Systems Trust; 2014. Available: http:// www.hst.org.za/publications/south-african-health-review-2013/14
31. McIntyre D. How can we best achieve a universal health system? A public conversation. In. Moeti T, Padarath A, editors. South African Health Review 2019 Durban: Health Systems Trust; 2019. Available: http://www.hst.org.za/ publications/Pages/SAHR2019
32. Nkonki L, Bhengu N, Ramokgopa M, Fonn S. The Health Market Inquir y and its potential contribution to improving health systems functioning in South Africa. In: Moeti T, Padarath A, editors. South African Health Review 2019. Durban: Health Systems Trust; 2019. Available at: http://www.hst.org.za/publications/ Pages/SAHR2019
33. Solanki GC, Wilkinson T, Cornell JE, Besada D, Morar RL. The Competition Commission Health Market Inquiry Report: An overview and key imperatives. South African Medical Journal. 2020 Feb 1;110(2):88–91.
34. StatsSA. Gross domestic product: Fourth quarter 2020. Pretoria: StatsSA, 2021. Available at: http://www.statssa.gov.za/publications/P0441/P04414th Quarter2020.pdf
35. National Treasury. Budget Review 2021. Pretoria: National Treasury, 2021. Available at: http://www.treasury.gov.za/documents/national%20budget/2021/ review/FullBR.pdf
36. National Treasury. Budget Review 2021. National Treasury, Pretoria: 2021. www.treasury.gov.za
37. Blecher MS, Daven J, et al. COVID-19 Lives and Livelihoods. Annual Health Review 2021. Heath Systems Trust; Durban: in press.
This chapter provides an overview of the global health context and main health issues facing the African region and the rest of the world. The overview includes the main actors and institutions that influence health in South Africa, and those which South Africa influences globally. The responsibilities for the health of the people of South Africa are laid out in the South African Constitution and in the National Health Act, no 61, 20031. Whilst most of the provisions of both these require accountability within South Africa, it is common currency that the health of people within the country is influenced by factors beyond the borders of the country, both in terms of the determinants of health and in interventions to improve health. Global health transcends national borders and links people and other living species together beyond states, continents or regions, making particular health problems central for the whole world, within the context of security imperatives and humanitarian values2
Usuf Chikte, Ritika Tiwari, Precious Matsoso, Yogan Pillay, Robert (Bob) Fryatt, Lindiwe Makubalo
Over the last three decades, the global health landscape has undergone rapid transformation in terms of the disease focus, health actors, funding and architectural arrangements. One of the significant features of the current health landscape has been a major epidemiological and demographic transition with increased life expectancy giving rise to growing and aging populations. At a policy level the Sustainable Development Goals (SDGs) or Agenda 2030 introduced, at a level of health and wellness, aspirations targeting Universal Health Coverage (UHC) through Primary Health Care (PHC). The World Health Organization (WHO) has translated this aspiration to the Triple Billion programme targets on protection from emergencies, healthier lifestyles and prevention3
Emerging diseases and outbreaks have become more dominant, posing major threats which are accompanied by significant social, public health and economic consequences.
The period under review in this chapter has been characterised by the rise in global public health threats. Ebola emerged as a global threat to public health in 2015 and continues to be a threat in the African region. In 2019, an unprecedented pandemic, COVID-19, shook the world and brought the entire globe almost to a standstill. COVID-19 spread across 215 countries and territories claiming lives, with dire social, economic and health consequences as well as laying bare the fragility of health systems, and the worlds’ ability to produce and distribute countermeasures against COVID-19. The shortcomings of international instruments and mechanisms to respond to widescale epidemics and pandemics were laid bare. The COVID-19 pandemic also generated a greater cooperation between scientists, institutions and agencies to find rapid solutions, underscoring the need to intensify and invest in research and development with the view to understand rapidly the new variants and embark on a race to discover a vaccine, therapeutics, appropriate diagnostics tools and public health prevention measures with calls for greater investments in these areas. South Africa played a major political role during this period and contributed significantly through sharing information and discoveries and collaborating on the scientific front. The COVID-19 pandemic has reiterated the value of international cooperation and collaboration. When the World Health Assembly convened in May 2020, member states passed a resolution emphasising the need for solidarity, resource redistribution, and collective action4.
The global health institutional system has seen expansion over the past few decades in the form of a continued increase in both the number and diversity of actors5-7. The increasing number of health agencies has its pros and cons. Concerns have been raised that non-multilateral agencies could weaken the multilateral approach and undermine the more democratic approach to global policy-making. However, the interactions between global health actors are influenced by the actors themselves, the internal arrangements within the system, and external forces, such as actors and arrangements from other important global policy domains8. Multilateralism is an important tool for ensuring inclusive global policy. Organisations such as the WHO have provided low- and middle-income countries an opportunity to participate in framing global health policy and to some extent influence the flow of resources. During this period, South Africa played an important role in the global multilateral system.
During the period under review, South Africa as a member of the Foreign Policy and Global Health Group led resolution on UHC to the United Nations General Assembly. In addition, South Africa co-chaired the Health Employment and Economic Growth initiative, led by the WHO, International Labour Organization and Organisation for Economic Co-operation and Development. South Africa served on the WHO Executive Board for a three-year term and chaired for a year. This was during the most crucial time of WHO reform. South Africa played a stewardship role in the Stop TB initiative as its chair, in the BRICS initiative advocating for the combatting of TB in 2016. The Stop TB Partnership has been key in advocating for an enhanced response to the global burden of tuberculosis. The Stop TB Partnership represents a coalition of over 1 600 government, civil society and donor organisations and is currently hosted by the United Nations Office for Project Services and was previously hosted by the WHO. South Africa led the resolution of the United Nations General Assembly for the convening of a High-Level Meeting on TB in September 2018 as part of the Global Health and Foreign Policy member countries which included Brazil, France, Indonesia, Norway, Senegal, South Africa and Thailand.
The significant role played by South Africa as the G20 member was led by President Ramaphosa with its role as founding member of the WHO Access to COVID-19 Tools Accelerator (ACT-A) initiative, and as a member of the G77 which strongly advocated for stopping TB. The South African Health Minister co-chaired the Facilitation Council with Norway, guiding the work of ACT-A, leading to the establishment of the Manufacturing Task Force on vaccines, which has been instrumental in advancing negotiations on technology transfer to Africa and other developing countries.
Assuming African Union chairpersonship in 2020 was a significant development as it placed the country in the forefront of COVID-19 activities globally and on the continent. In 2020 South Africa chaired the African Union Commission and initiated and supported programmes on COVID-19 such as the AVAT Africa Vaccine Acquisition Platform9, the development of the Africa Taskforce for Novel Coronavirus (AFTCOM), African Medicines Supplies Platform (AMSP) COVID-19 Response Fund, and envoys led to the President being nominated COVID-Champion by African Union heads of states in 2021.
South Africa made several other significant contributions to global initiatives. Largely led and guided by the South African Mission to the UN, South Africa was able to contribute to the framing of declarations and global policy resolutions on an extensive list of critical areas. This included antimicrobial resistance, the Global Vaccine Action Plan, primary health care, neglected tropical diseases, Ending TB, maternal, infant and young child nutrition, and initiating and leading negotiations on Ebola which led to a significant global response. South Africa also played a significant role on the International Health Regulations (IHR), establishing the WHO Emergencies programme, and chairing the Independent Oversight and Advisory Committee (IOAC) for the WHO Emergency Programme. In 2020 South Africa in collaboration with India proposed and has been negotiating for a waiver on some provisions of the Trade Related Aspects of Intellectual Property Rights (TRIPS
agreement) for preventing and containing COVID-19. South Africa also represented Africa on the UNITAID Board, the Global Fund Board, the IHR Committee, and other key initiatives.
In addition to this diplomacy and advocacy, South Africa has continued to be a significant contributor to the research, science and technical developments through science institutions and contributions by South African scientists on a large number of technical advisory groups and committees.
Civil Society in South Africa has also been a major influence and inspiration to many areas of health. Perhaps most important has been its influence in tackling HIV. In 2006, international and African scientists and politicians gathered to identify and discuss the main drivers of the HIV epidemic in Southern Africa, which led to the identification of key drivers which included multiple concurrent sexual partnerships, gender power inequities, high population mobility, and cultural norms and belief systems10. The consensus among scholars about the main drivers is that the social context in high-prevalence communities in South Africa plays a major role in the way in which sexual risk-taking is configured in the country.
Historically, the role of communities in places with people living with HIV (PLHIV) and peers in service delivery, research and drug development, as well as groups responsible for advocacy, social and political accountability, resource mobilisation and social and human rights protection have also been recognised as some of the crucial drivers for HIV. Their leadership and engagement have contributed significantly to improved outcomes in access to HIV treatment, prevention, and support and care services around the world. Their continued and expanded role is especially important for the future success of HIV responses in sub-Saharan Africa, where the HIV burden remains the greatest. The lessons learned from the leadership and involvement of communities of PLHIV and peers in the HIV response hold value beyond HIV responses. The models and approaches they have efficiently and effectively utilised have relevant applications in addressing shortfalls in health systems in the COVID-19 era, as well as broader, more integrated health challenges as countries move to develop and operationalise UHC11
Public–private partnerships in health offer significant opportunities for strengthening health care systems, especially in Africa where the health financing gap is a major issue. The development and implementation of the Bioko Island Malaria Elimination Project is a case in point. Loss in productivity through absenteeism as well as high health costs motivated this 15-year project. This partnership between the government of Equatorial Guinea and three private sector partners (Marathon Oil Corporation, Noble Energy and Atlantic Methanol Production Company) has been reported to have reduced the prevalence of malaria by 75%. The results have been substantial, with 1 000 infected mosquito bites per capita annually in 2004, down to three bites per capita in 2018. Lessons learned from this example include acknowledging the challenges caused by different management and operational styles between partners that can cause conflict, continuity of funding, and different expectations of potential outcomes and responsibilities. In addition, a potential weakness on the part of governments is the development of national health plans without considering or including the participation of the private sector in the process, thus ignoring the symbiotic role companies can play in bolstering the services offered by the public health system14
In an increasingly interconnected world, the AfCFTA agreement will play an important role in facilitating trade of health products and medicines on the continent, including through reduced tariffs among member countries and will cover policy areas such as trade facilitation and services, as well as regulatory measures with reference to sanitary standards and technical barriers to trade. In general, the agreement is expected to create the largest free trade area in the world measured by the number of countries participating. AfCFTA can lift an additional 30 million people from extreme poverty (1.5% of the continent’s population) and 68 million people from moderate poverty15. The pact aims to connect 1.3 billion people across 55 countries with a combined gross domestic product (GDP) valued at US$3.4 trillion16. With the global economy in turmoil due to the COVID-19 pandemic, the creation of the vast AfCFTA regional market is a major opportunity to help African countries diversify their exports, accelerate growth, and attract foreign direct investment15
South Africa is party to international laws and agreements such as the United Nations Convention on the Rights of Persons with Disabilities53. In 2018, almost 600 000 children with disabilities remained out of school. Most children with disabilities attend specialised schools or classes. Children with psychosocial disabilities are frequently placed in poorly regulated special service centres, based on long-term institutionalisation, often located far from their families and communities, and lack properly trained staff. No legislation exists to give full effect to the right to inclusive education for all children with disabilities. Across South Africa, a high number of cases continued to be reported of corporal punishment, violence, abuse, neglect and inequality involving children with disabilities, especially children with autism spectrum disorder and children with psychosocial and/or intellectual disabilities, by teachers and peers in schools and school hostels17
As in previous years, the government has still not implemented key aspects of the 2001 national policy to provide inclusive education for all children with disabilities, nor adopted legislation to guarantee the right to inclusive education. However, the government continued to implement the Screening, Identification, Assessment and Support (SIAS) policy designed to ensure that children with disabilities are provided full support when accessing education. The majority of the government’s limited budget for learners with disabilities continued to be allocated to special schools rather than to inclusive education17.
Historically, during the transition to democracy, the international community supported President Mandela’s nation-building process by channelling all development assistance via the new democratic government. The first years of the democratic dispensation saw the establishment of the Reconstruction and Development Programme (RDP), with a dedicated ministry under the presidency. Through the use of the fiscus and extra budgetary resources from donors and the private sector, the government constructed low-cost housing and extended access to water and electricity to millions of poor18 Management of foreign aid was led by the RDP Ministry under the presidency, but under President Mbeki this was shifted to the National Treasury and managed by the International Development Cooperation unit in the Budget Office. Official development assistance (ODA) from donors was now aligned to government priorities, and used in a more strategic way to support development planning, apparatus building and public policy. As attention shifted to state building, less funding went to civil society, causing a gradual non-governmental organisation (NGO) crisis over the next years with many organisations obliged to shut down.
South Africa was never an aid-dependent country, as ODA never exceeded 1% of the government’s own budget. Technical support, however, continued and was used primarily to address the capacity gaps in the government and improve delivery of services. South Africa has to a large extent received funding and technical support through multilateral sources, mostly the WHO. Much of development assistance was therefore provided through bilateral engagements in the form of resources, capacity development, exposure visits, dialogue, and knowledge exchange with other countries. An important global debate at present is the extent to which upper-middle-income countries such as South Africa can expect development assistance. Increasingly, upper-middle-income countries are not receiving assistance. This was evident, for instance, during the COVID-19 pandemic, when South Africa was one of the few countries in Africa that did not qualify for support from COVID-19 Vaccines Global Access (COVAX) to purchase vaccines and had to purchase from domestic resources. Most middle-income countries, South Africa included19 nevertheless have high poverty rates and a weak capacity of the public service to deliver appropriate services, which thus justified donor engagement. It is also argued that COVID-19 and the measures that were put in place have had a significant impact on most economies.
At the same time, South Africa has been fortunate as it attracted many donors because of its strong macro-economic stability and a world-class public financial management system18.
In the past, South Africa had a major national human resource deficit and this was addressed with the import of technical skills – engineers, doctors, teachers, and other specialised personnel from Europe and North America, as well as from Cuba, Iran, Uganda and other African countries with higher levels of education18. Prior to democracy, most development assistance from foreign donors would flow via civil society, churches, student organisations and the private sector20. Major institutions that acted as conduits of foreign aid included the Kagiso Trust, Urban Foundation, Gerald Foundation, Rural Foundation, Cofuka Steps, Joint Education Trust, South African Chamber of Commerce, and the United Democratic Front18
Today, South Africa’s largest donors include the United States, the European Union, Germany, the United Kingdom, France, Netherlands, Belgium, various Nordic countries, and United Nations programmes and funds18. The ODA is provided through a mixture of budget support (provided through the RDP Fund), technical cooperation and concessionary loans. The bulk of foreign aid goes to the health and education sector, where South Africa still has major deficits and the largest HIV-infected population in the world21
Significant amounts of US funding (mostly from the United States President’s Emergency Plan for AIDS Relief or PEPFAR, the US Centres for Disease Control and Prevention, and other HIV-related funds) are channelled largely through NGOs, research centres, universities and public entities18. The collaboration of the NDoH with the US government resulted in the development of important programmes such as the ‘Dreams programme’22, which uses a multisectoral approach to prevent HIV/AIDS among adolescent girls and young women and their male sex partners.
Whilst South Africa is not a recipient country because of its middle-income status, GAVI receives a modest contribution from South Africa as a donor country. From 2020, GAVI’s mandate as a member of the ACT-A means that South Africa now indirectly benefits from GAVI through the COVAX facility negotiation.
South Africa has been shaped by, and is actively shaping the world through global trends on the determinants of health, and formal collaborations with global and regional institutions. The influence of South Africa in the response to COVID-19 in the region exemplifies this – with the President’s role in the African Union, the pivotal role of South African scientists in tracking and researching interventions, and the breakthrough in planning for the mRNA COVID-19 vaccine production in the country. South Africa needs to continue to examine and expand on its role in the region and globally, both to improve the health of the people of South Africa, and to play its role in improving health globally. The country is constantly striving for the betterment, harmonisation and coordination of Africa’s global health system with investment through sustainable financing initiatives and ensuring that aid goals are continuously aligned with the regional health needs and priorities. At the same time, there is a critical need to develop thought leadership for effective decision-making, for implementation of the most appropriate global health programmes, and for strengthening global health initiatives to enhance regional alliances and efficient functioning at a governmental level.
1. Government of South Africa. National Health Act 61. Cape Town 2003.
2. World Health Organization. The Triple Billion Targets. Geneva: WHO; 2020 [cited 2022 4 April]. Available from: https://www.who.int/news-room/ questions-and-answers/item/the-triple-billion-targets.
3. Holder J. Tracking Coronavirus Vaccinations Around the World. The New York Times. April 1, 2022.
4. World Health Organization, editor. Seventy-third World Health Assembly. A73/ CONF/1 rEV; 2020.
5. Bump JB, Friberg P, Harper DR. International collaboration and COVID-19: What are we doing and where are we going? Bmj. 2021;372.
6. Peel M GA, Cookson C. WHO struggles to prove itself in the face of COVID-19. Financial Times 2020 Jul 11.
7. World Health Organization. The access to COVID-19 tools (ACT) accelerator. 2020 [cited 2021 6 July]. Available from: https://www.who.int/initiatives/ act-accelerator.
8. Liverpool School of Tropical Medicine. Sub-Saharan Africa and the 2019 Global Burden of Disease Study: Celebratory with a note of caution. LSTM; 2020 [cited 2021 2 July]. Available from: https://www.lstmed.ac.uk/news-events/ blogs/sub-saharan-africa-and-the-2019-global-burden-of-disease-studycelebratory-with-a.
9. Frenk J, Moon S. Governance challenges in global health. New England Journal of Medicine. 2013;368(10):936–42.
10. Gostin LO, Mok EA. Grand challenges in global health governance. British Medical Bulletin. 2009;90(1):7–18.
11. Moon S, Szlezák NA, Michaud CM, Jamison DT, Keusch GT, Clark WC, et al. The global health system: lessons for a stronger institutional framework. PLoS Medicine. 2010;7(1):e1000193.
12. Hoffman SJ, Cole CB. Defining the global health system and systematically mapping its network of actors. Globalization and Health. 2018;14(1):1–19.
13. United Nations Children’s Fund. The African Union’s African Vaccine Acquisition Trust (AVAT) Initiative. Unicef; 2021 [cited 2022 4 April]. Available from: https://www.unicef.org/supply/african-unions-african-vaccine-acquisitiontrust-avat-initiative.
14. US department of State. DREAMS Partnership 2014 [cited 2022 4 April]. Available from: https://www.state.gov/pepfardreams-partnership/#:~:text=DREAMS%20provides%20a%20 comprehensive%2C%20multi,of%20access%20to%20secondary%20school.
15. Besharati NA. South African Development Partnership Agency (SADPA). Strategic Aid for Development Packages for Africa? 2013.
16. The World Bank. South Africa 2021 [cited 2021 March 18]. Available from: https://data.worldbank.org/country/ZA.
17. Guilbaud A. Business partners: firmes privées et gouvernance mondiale de la santé: Presses de Sciences Po; 2015.
18. The Global Fund. Results & Impact. 2021.
19. World Health Organization. Joint COVAX Statement on the Equal Recognition of Vaccines. WHO; 2021 [cited 2 July 2021]. Available from: https:// www.who.int/news/item/01-07-2021-joint-covax-statement-on-the-equalrecognition-of-vaccines.
20. Eboko F, Baxerres C. The era of global health: The policies, the actors, and the dynamics. Politique africaine. 2019 (4):5–20.
21. Koplan JP, Bond TC, Merson MH, Reddy KS, Rodriguez MH, Sewankambo NK, et al. Towards a common definition of global health. The Lancet 2009;373(9679):1993–5.
22. Lachenal G. The Dubai stage of public health. Revue Tiers Monde. 2013 (3):53–71.
23. UNAIDS. Who we are
24. Hanson S, Zembe Y, Ekström AM. Vital need to engage the community in HIV control in South Africa. Global health action. 2015;8(1):27450.
25. Caswell G, Dubula V, Baptiste S, Etya’ale H, Syarif O, Barr D. The continuing role of communities affected by HIV in sustained engagement in health and rights. Journal of the International AIDS Society. 2021;24:e25724.
26. United Nations. The Sustainable Development Goals Report 2019. New York. 2019.
27. World Health Organization. Global health initiatives. Available from: http:// www.emro.who.int/health-topics/global-health-initiative/index.html.
28. Ki-Moon B. The millennium development goals report 2013. United Nations Pubns. 2013;365:366.
29. Hernández-Peña P. Global Spending on Health: A World in Transition [Global Report 2019]. WHO/HIS/HGF/HFWorkingPaper/. 2019 (19.4).
30. James C. Health and inclusive growth: Changing the dialogue. Health Employment and Economic Growth: An Evidence Base. Geneva: World Health Organization. 2016.
31. Summan A, Stacey N, Birckmayer J, Blecher E, Chaloupka FJ, Laxminarayan R. The potential global gains in health and revenue from increased taxation of tobacco, alcohol and sugar-sweetened beverages: a modelling analysis. BMJ global health. 2020;5(3):e002143.
32. Marquez PV, Dutta S. Taxes on tobacco, alcohol, and sugar-sweetened beverages reduce health risks and expand fiscal space for Universal Health Coverage post-COVID-19. World Bank; [cited 2021 6 July]. Available from: https:// blogs.worldbank.org/health/taxes-tobacco-alcohol-and-sugar-sweetenedbeverages-reduce-health-risks-and-expand-fiscal.
33. World Health Organization. Weekly Epidemiol Record. Global distribution of measles and rubella genotypes update. 2006;81:474–9.
34. Centre for Global Development. CASE 17: Eliminating measles in Southern Africa. 2021 [cited 2021 14 July]. Available from: https://www.cgdev.org/sites/ default/files/archive/doc/millions/MS_case_17.pdf.
35. Global Polio Eradication Initiative. The man who kicked polio out of Africa. 2013 [cited 2021 14 July]. Available from: https://polioeradication.org/news-post/ the-man-who-kicked-polio-out-of-africa/.
36. Measles & Rubella Initiative. Measles in the African Region: Progress and Focus on Elimination 2020. 2020 [cited 2021 14 July]. Available from: https:// measlesrubellainitiative.org/measles-in-the-african-region-progress-and-focuson-elimination-2020/.
37. University of Cape Town. Major vaccine success stories. 2017.
38. Omnia Health. Focusing on Africa’s challenges and opportunities in digital health 2020 [cited 2021 July 14]. Available from: https://insights.omnia-health.com/ hospital-management/focusing-africas-challenges-and-opportunities-digitalhealth.
39. National Department of Health. National Digital Health Strategy for South Africa 2019 – 2024. 2019. Available from: https://www.health.gov.za/ wp-content/uploads/2020/11/national-digital-strategy-for-south-africa2019-2024-b.pdf.
40. GBC Health. Case Studies: Successful African Health Public–Private Partnerships. GBC Health; 2019 [cited 2021 28 July]. Available from: https://gbchealth.org/ case-studies-successful-african-health-public-private-partnerships/.
41. Barchiesi F. Rethinking the Labour Movement in the ‘New South Africa’ Routledge; 2019.
42. Vickers B. Towards a new aid paradigm: South Africa as African development partner. Cambridge Review of International Affairs. 2012;25(4):535–56.
43. Wikipedia. New Partnership for Africa’s Development. 2018 [cited 2021 28 July]. Available from: https://en.wikipedia.org/wiki/New_Partnership_for_Africa%27s_ Development#cite_note-1.
44. Landsberg C. The quiet diplomacy of liberation: International politics and South Africa’s transition. Jacana Media; 2004.
45. Partner A, An A. World AIDS Day—December 1, 2014. Vital Signs. 2013;2005.
46. Maliszewska M, Ruta M. The African Continental Free Trade Area: Economic and Distributional Effects. World Bank Group; 2020.
47. The World Bank. The African Continental Free Trade Area. The World Bank; [cited 2021 28 July]. Available from: https://www.worldbank.org/en/topic/trade/ publication/the-african-continental-free-trade-area.
48. South African Institute of International Affairs (SAIIA). South African Development Partnership Agency (SADPA): Strategic Aid or Development Packages for Africa? Available from: https://saiia.org.za/research/south-africandevelopment-partnership-agency-sadpa-strategic-aid-or-development-packagesfor-africa/.
49. Virani A, Wellstead AM, Howlett M. The north-south policy divide in transnational healthcare: a comparative review of policy research on medical tourism in source and destination countries. Globalization and Health. 2020;16(1):1–15.
50. African Union. Statement of the African Union (AU) Labour Migration Advisory Committee (LMAC) on the novel Coronavirus Disease COVID-19 and the condition of African Migrant Workers. 2020 [cited 2021 28 July]. Available from: https://au.int/en/pressreleases/20200414/statement-lmac-condition-africanmigrant-workers-covid-19.
51. African Union. Mobility and migration of african health workers post COVID-19. African Union; 2020 [cited 2021 28 July]. Available from: https://au.int/sites/ default/files/documents/39884-doc-mobility_and_migration_of_african_health_ workers_post_covid-19.pdf.
52. World Health Organization. A dynamic understanding of health worker migration World Health Organization, Geneva. 2017.
53. South African Human Rights Commission. Human rights and persons with disabilities. Johannesburg. SAHRC; 2018 [cited 2022 4 April]. Available from: https://www.sahrc.org.za/home/21/files/FINAL%20Human%20Rights%20 and%20Persons%20with%20Disabilities%20Educational%20Booklet.pdf.
54. Human Rights Watch. South Africa Events of 2018. 2018 [cited 2021 28 July]. Available from: https://www.hrw.org/world-report/2019/country-chapters/ south-africa#.
The book has reviewed progress in various dimensions related to health in South Africa over the period 2015 to 2020. In this chapter we provide a summary of the progress and challenges raised by the authors, and a set of recommendations taken from the various chapters to strengthen health reform in the South African health system.
The health of most South Africans continues to improve, with positive trends in many of the key measures of health, including life expectancy. However, many of these positive trends have been affected, some severely, by the impact of the COVID-19 pandemic. In addition to the immediate impact on health outcomes, the longer-term impact on health through worsening determinants of health, such as poverty, inequality, unemployment, natural disasters and education, are also likely to be severe.
Recommendation (1) Surveillance: There remains a lack of regular surveillance of some key indicators, with a continued reliance on expensive and sometimes infrequent surveys.
• Child health surveillance: there is a pressing need to focus beyond childhood mortality to ensure that each child can thrive, focusing on in utero and early-life exposures, environmental conditions (air pollution, contaminated water and sub-optimal sanitation) and access to better-quality diets.
• Disabilities: The country must consider the additional data needs in terms of realisation of the socio-economic rights in the Constitution and monitoring the Sustainable Development Goals (SDGs) regarding disabilities.
• Inequalities and inequities: It remains important to highlight some of the challenges and potential solutions to health inequalities and inequities through better monitoring, including of non-communicable diseases (NCDs), as well as investments in areas where the greatest impact of narrowing the gaps can be made.
Malebona Precious Matsoso, Usuf Chikte, Lindiwe Makubalo, Yogan Pillay, Robert (Bob) FryattRecommendation (2) Improved data: A number of approaches are recommended to overcome the limitations of the current data sources; these include:
• Local analyses: The use of modelling techniques (such as small area estimation) to increase the spatial resolution of indicators of interest based on their relationship with other variables available at a local level;
• Deprivation indices: The use of multidimensional indices of deprivation that combine multiple variables to create measures that are robust when corrected for missing data;
• Linking data systems: The use of patient-level data from Electronic Health Record Systems once they are implemented that track patients who visit different health care providers which can also be linked to other data systems such as vital registration.
To improve sub-national horizontal collaboration and partnership between departments we recommend that Provincial Departments of Health (PDoHs) be the champions of consultative engagements at provincial and local levels, given that policy implementation occurs at the provincial and local levels. Ideally, consultative arrangements should help clarify roles and responsibilities and support the implementation of the social determinants of health approach to improve health outcomes. There is the need to engage critical stakeholders – the public sector (government), private sector and civil society – at all stages and for direct engagement of communities at ward level. The interactions among the stakeholders should go beyond information sharing to cooperation, coordination or integration, which are likely to strengthen policy implementation.
Recommendation (3) National leadership for SECEDH: The National Department of Health (NDoH) should urgently lead the formulation and implementation of intersectoral action with a high level of active and measurable engagement of all stakeholders, in line with the district development model.
Recommendation (4) Sub-national collaboration on SECEDH: The NDoH should develop guidelines for provinces and districts on creating consultative engagements for sub-national government stakeholders building on structures and processes that were developed to deal with COVID-19 and documented best practices and innovations by PDoHs before COVID-19 and in response to COVID-19.
PHC should be approached as a wider system philosophy embracing participation, intersectoral action and comprehensive approaches to health, embedded within coherent sub-district and district systems. While achieving greater system efficiency is key, further development of the PHC system, especially components such as the Ward-Based Primary Health Care Outreach Teams, cannot occur in an environment of austerity and disinvestment. Emphasis also needs to shift from the ‘what’ of policy to the ‘how’ of implementation, focused on learning through deliberation and by doing, adapting or de-implementing ineffective or harmful strategies, supported by partnerships and embedded and co-produced evaluation and research. The reasons for declining patterns of PHC utilisation need to be better understood, including the need to better understand the role of communities as well as community, household and personal health and to strengthen these.
Looking to the future
Recommendation (5) Strengthened PHC governance: The governance weaknesses in PHC need to be tackled by the formulation of a coherent sub-district system, and beyond this, establishing meaningful community participation and intersectoral collaboration, shifting from a curative, disease orientation to a more expansive approach, centred on prevention, promotion and action on the social and other determinants of health. This should be accompanied by a commitment to establishing stable, skilled and public-interested leadership in PHC and district health systems.
Recommendation (6) Aligned PHC reforms with the National Health Insurance (NHI): Developments in PHC need to be aligned with other system developments, in particular Human Resources for Health (HRH) development and financing and the NHI. This could be achieved through forms of health system learning that rely less on nationally defined audits than on co-produced approaches better able to harness bottom-up participation and innovation. There also is a need to be clear about the role of the private health sector, including the role of traditional healers.
During the period 2015 to 2020 there were some remarkable successes, however, declines in incidence were below the global targets, e.g., those set by WHO, UNAIDS, Stop TB Partnership Board and the SDG goals to end the HIV and TB epidemics by 2030. As with other programmes, maternal, child and woman’s health had some successes but also stagnation and deterioration associated with COVID-19. Of great concern is the inadequate uptake of contraceptives and the increasing number of adolescents becoming pregnant. There continues to be a sub-optimal use of condoms in South Africa, which has the potential to play a major role in improving outcomes for many of these challenges. As improved health often does not come from single disease interventions, health services need to be integrated so that patients can seamlessly have all their needs attended to in a patient-centred and holistic way.
Recommendation (7) TB: There has been a range of suggestions to reverse and catch up on TB services and interventions, including using the lessons from the COVID-19 crisis and response and not letting it go to waste. These include using COVID-19 testing to simultaneously test for TB and using community-based and community-led responses that take diagnosis, care and support to the doors of those affected by COVID-19 to also carry out contact tracing and symptom checks for TB.
Recommendation (8) HIV: It makes increasing sense for HIV to be treated as a long-term chronic disease and integrated with other conditions and programmes in a more patient-centred approach.
Recommendation (9) Package of essential services: Each disease and health programme needs to have a package of essential services (e.g. contraceptive services for teenage girls) that is affordable, available and acceptable to beneficiaries and which need to be in place regardless of external circumstances. In other words, these need to be protected against shocks such as pandemics, thus the importance of resilient health systems.
The South African Health Products Regulatory Authority (SAHPRA) continues to improve its performance, although this is held back due to the constraints of lack of access to specialist regulatory expertise. The Centralised Chronic Medicine Dispensing and Distribution programme provided a paradigm shift to differentiated service delivery and will need to continue to evolve, building on the high number of local innovations, and making the programme more equitable, in particular for rural areas where connectivity and internet access is a major barrier. Some successes in the fight against antimicrobial resistance (AMR) have been achieved but efforts need to be scaled up.
Recommendation (10) SAHPRA: Efforts will need to be scaled up to overcome the constraints to strengthen specialist regulatory expertise. Furthermore, approval times for various regulatory activities must be shorted.
Recommendation (11) Pharmacists: Strategies are urgently needed to ensure the best possible utilisation of existing pharmacy personnel to provide quality pharmaceutical services.
Recommendation (12) Anti-microbial resistance: Securing funding through the National Treasury is key and urgently requires developing a business case for scaling up efforts for tackling AMR.
South Africa continues to be plagued by a two-tier health care system, based on the socio-economic status of its users. This is now compounded by the systemic disruptions imposed by the COVID-19 pandemic. This has in turn led to a sharper decline in the resource envelope for funding of health care facilities in the foreseeable future. Further improvement in the quality and efficiency of hospital services is predicated on ethical leadership which gives spirit to the practice of corporate and clinical governance through continuous improvement and commitment to monitoring and evaluation of inputs, processes and outcomes. This in turn will allow for transparent interactions with served communities, and encourage engagement with, and ownership of public hospital services, to create shared resources for improving health outcomes. This will also decrease the drain on the fiscus represented by considerable medico-legal litigation, linked to poor-quality health care and a lack of trust from communities. In the context of NHI, development of an integrated hospital platform across the public and private health sectors will be necessary.
Recommendation (13) Decentralised management of hospital services: It is important to bring to fruition the initiatives aimed at defining and capacitating structures for the efficient, decentralised management of hospital-level services.
Recommendation (14) Quality of services: An overarching coordinated national commitment to quality improvement and continuous learning, both in the clinical and corporate management of hospital-level services is required to effect the necessary changes to the system.
What is certain on review of South Africa’s response to health emergencies over 2015–2020 is that health security requires more than a narrow focus on infectious disease preparedness, detection and response. Universal health coverage (UHC) and health systems strengthening are a critical component of health emergency planning and response. The number of reviews including the Independent Panel for Pandemic Preparedness and Response, appointed by the WHO Director-General in response to the World Health Assembly resolution 73.1, has provided the global community with a comprehensive, evidence-based review of responses to the COVID-19 pandemic.
Recommendation (15) Pandemic preparedness: South Africa should update its national preparedness plans against the WHO and country adopted targets and benchmarks within six months and ensure appropriate and relevant skills, logistics and funding are available to cope with future health crises. It should also appoint national pandemic coordinators accountable to the highest levels of government with the mandate to drive whole-of-government coordination for both preparedness and response. South Africa should also implement outstanding recommendations from the 2017 Joint External Evaluation recommendations.
Legislative changes have impacted positively on several of the factors contributing to NCDs, including those for sugar-sweetened beverages and salt. While the National Strategic Plan (NSP) 2013–2017 included all the elements of interventions to respond to the burden of disease from NCDs it suffered from a range of implementation challenges. These included the lack of sufficient intersectoral collaboration as well as the means to measure progress or lack thereof and for course correction during the period 2013–2017. In addition, the hiatus between 2017 and 2020 – with no plan to guide intervention as a result of a protracted period of consultation for the drafting of the new NSP, also resulted in inadequate progress. The NDoH should design programmes and systems that place the patient/person at the centre, as described in the WHO’s Integrated Person-Centred Health Services Framework.
Recommendation (16) Non-Communicable Disease National Strategic Plan: The NDoH should rapidly implement the new NSP which recommends the use of a cascade approach for diabetes and hypertension and which calls for the establishment of a coordinating mechanism similar to that for HIV and TB. High-level political support and additional funding is required to implement the NSP and reduce the rising burden of NCDs in the country.
The last five years have shown us a great deal about what can be done for mental health, but the next five years will have to show more progress in terms of real changes in systems and services. Moving towards a greater emphasis on community care will be essential. Moreover, reducing the social and economic determinants of mental health, giving greater emphasis to prevention and promotion programmes, and working across sectors will need to be prioritised if population mental health is to be strengthened.
Recommendation (17) Increased investment in mental health services: Greater investment is required for mental health services as part of the current ‘building back better’ response to the crisis. To improve mental health in South Africa, moves towards greater emphasis on community care will be essential.
There is a legacy of neglect of OHS in South Africa, although with some more recent innovations in service delivery. The COVID-19 pandemic provides the required impetus for working together (government and the private sector) to deliver a safer and healthier workplace.
Recommendation (18) Funding occupational health services: A funding model to support occupational health service delivery across sectors is required in South Africa. Funding of the health services under the NHI could include medical care and rehabilitation for occupational injuries and diseases. Increased investment in supporting OHS professionals is required to meet the needs for OHS especially in the public sector as well as retention strategies for trained OHS professionals already in the system.
South Africa requires a health service redesign to address inequality and to build the foundations for effective implementation of UHC. This will enable government to maintain and strengthen its efforts to provide and maintain health care infrastructure as an enabler of the provision of quality health care.
Recommendation (19) State capacity for improving health infrastructure: Human resource capacity to deliver health care infrastructure must be strengthened either by improving required capacity in the various Departments of Public Works across the provinces or moving the function to PDoHs along with the necessary capacity. Institutions of Higher Education must be engaged to review their curricula for ensuring alignment between the new professional and technical workforce demands in health infrastructure.
Looking to the future
Recommendation (20) Health infrastructure priorities and efficiencies: Infrastructure plans must be aligned with plans for improving services focused on the PHC platform. The infrastructure delivery process should be simplified by: not overburdening implementation from too many reporting requirements; using BIM (Building Information Management) in the design and construction phases; standardising the Service Delivery Agreements between PDoHs and relevant Implementing Agents; updating the Infrastructure Unit Support Systems guidelines and keeping the portal as a platform for all the stakeholders involved in health care infrastructure; update the South African Cost Norms for providing effective management of cost versus budget; and using the procurement method in the Construction Industry Development Board (CIDB) Standard for Uniformity to reduce cost of professional fees.
The South African National Lancet Commission on Health Systems Quality reported some achievements and numerous challenges to the delivery of quality health care, with clear recommendations to achieve a quality health care system for South Africa. Some progress has been made to ‘revolutionise quality’, however, overall implementation of the Commission’s recommendations has been limited. There remains a need for an overarching national quality improvement (QI) strategy which engages all stakeholders, including frontline health workers, civil society and the many current quality of care role players who operate within separate health programmes or sectors.
Recommendation (21) Office for Health Standards Compliance: The OHSC needs to be provided with the necessary resources to achieve its regulatory mandate and to support the NHI requirements as these evolve. It should also review its modus operandi with fewer measures and a greater focus on outcomes rather than inputs and processes to assess performance. It should also segregate the Office of the Health Ombudsman into a separate entity.
Recommendation (22) Continuous quality improvement: Health districts, sub-districts and health facilities should be empowered to monitor the inputs and processes relevant to frontline quality of care. Greater efforts are needed to strengthen the capacity of frontline health managers in the planning and implementation of quality assurance and QI systems, and to expand their ‘decision space’ to enable them to respond to gaps in quality.
Recommendation (23) Quality data: Information should be provided to the public about hospital quality of care to help encourage hospitals to implement QI strategies. Within the private sector, data on quality should be made available to health care users (i.e., patients) and institutional purchasers (e.g., medical schemes) to advance quality through improved market functioning.
While not a period of much legislative development, 2015–2020 has seen various changes to health and the health system brought about through legal advocacy, litiga tion and some legislative and regulatory change. It is also a period from which many lessons can be learned: the need for Intellectual Property law change to secure access to affordable medicines and vaccines; the urgency of emergency medical services reform; the need to reform the private health sector; the benefit of NCD control; and the risk of poor policy implementation. The reasons for the failure to progress some important legislation on determinants of health are instructive and can inform future efforts. COVID-19 provided an unwelcome but perhaps useful test of some of the principles of NHI: a potentially system changing legislative change in the next five years.
Recommendation (24) Urgent legislation: The government should fast-track the passage of the NHI Bill alongside strengthening capacity for its implementation. The government should also implement the recommendations of the Health Market Inquiry.
The structural and legislative foundations of governance in South Africa are well established. However, the everyday practice of governance is weak, across sectors. The development of a capable state, founded on strong ethical practice, is therefore necessary to address the country’s social, economic and well-being needs. Communities and the district health system must be placed at the heart of the health system, with frontline governance strengthened to support quality improvement and local, place-based intersectoral action.
Recommendation (25) PDoH/NDoH roles and relationships: The PDoH/NDoH interface demands specific attention by co-creating a health governance charter that clarifies the values underpinning this interface, the roles of various actors, the spaces of engagement, and forms of reciprocal accountability. As shown possible by COVID-19, provincial health departments must look beyond health care as they seek, and work within, provincial government mandates for whole of society and whole of government approaches.
Recommendation (26) Civil society: Provincial and District Health Councils should be opened beyond current mandates as spaces for engagement with civil society, in addition to strengthening the functionality of clinic committees and hospital boards.
Recommendation (27) Leadership development: Implementing improvement in governance requires new mindsets and deepened skillsets, including those of ethical practice and ‘systems thinking’. Formal leadership and management training (in teams) and mentorship programmes have a role to play in developing such leadership. Senior managers can also be held accountable, through performance agreements, for enabling the spread of system leadership.
Progress is being made in South Africa to expand the information available to document and track health services and outcomes. Such information will however only strengthen downward accountability if local stakeholders (such as civil society groupings and patient organisations) are aware of it and use it effectively to draw attention to local problems and advocate for solutions. This will not happen automatically and will require substantial effort and investment by advocacy groups and community leaders.
Recommendation (28) Improved access and use of data: The government should introduce norms and standards for the public release of data to achieve greater transparency and better use of existing data. In addition, core data sets need to be expanded to cover social, commercial and environmental determinants of disease and chronic disease prevalence and chronic disease patient management (such as hypertension and diabetes control, and treatment adherence). The NDoH should invest in systems that make it possible to track patients across the health system and access more timely feedback on how users are experiencing health service provision.
Recommendation (29) Private sector accountability: Accountability for information is not only required from the public sector, and upcoming legislation on the NHI provides an opportunity to bring accountability from other sectors especially the private sector.
The NDoH has produced an updated Human Resources Strategy for the health sector. Implementation of the plan has been slow largely due to fiscal constraints. However, HRH should be a central focus of health sector reform even amidst fiscal constraints.
Recommendation (30) Implementation of the HRH strategy: The NDoH should coordinate efforts from all stakeholders across national government to support the implementation of the HRH plans effectively. In addition, engagement with the private health sector and with the Ministry of Employment and Labour Relations is required to assess and address future needs. To take on this role, a functional National Health Workforce Analysis and Planning Unit should be established drawing on national and international health workforce planning expertise, and utilising data science opportunities for more predictive and intelligent analytics and decisions.
Recommendation (31) Prioritised recommendations of the HRH strategy: Other actions identified as necessary in the HRH strategy include: curriculum realignment with population health needs; revitalised HRH regulatory structures; performance standards for HRH leadership and management; attention to service and positive workplaces to ensure health, safety and well-being of the health workforce, and main streaming gender and ensuring diversity at all levels for health workers.
The real challenge for health financing in South Africa is to be able to function within the budget allocated and provide the best-quality services possible. To achieve this there must be a rational balance between personnel, goods and service allocations. However, additional finances will be required for health as the cost of providing services as well as burden of disease increases. COVID-19 and its associated lengthy lockdowns have caused severe damage to the fiscus, which is likely to take at least three years to fully recover.
The NHI continues to offer major opportunities for the sector, however, opportunities in this regard have not been used to best advantage over the period reviewed. Trust needs to be built and there needs to be compromise around the Bill and subsequent reforms to avoid endless legal challenges. This includes building mixed provider platforms in an effective and efficient way, using smart strategic purchasing and systems. Confidence of provinces needs to be retained, through rapid re-introduction of delegated responsibility for service delivery (noting that the legal shift of function to national sphere is required to centralise funding). Without this not only will provincial powerbases obstruct the reforms, but major risks arise which may result in parts of the health service collapsing as functions and funds are transferred to the centre.
Recommendation (32) Health financing-related legislation: The Portfolio Committee on Health and the NDoH should review aspects of the model of NHI, and the need to revise the NHI Bill, to rebuild confidence, noting that a range of successful NHI models exist internationally. Moreover, recommendations arising from the Health Market Inquiry need to put back on track for implementation.
Recommendation (33) Strengthened NDoH capacity for health financing reforms: It will be useful to rebuild a health economics and financing unit in the NDoH. As well as assisting with NHI implementation, the unit should help monitor the new health component of the Provincial Equitable Share formula which has improved equity, benefiting poorer provinces such as Eastern Cape and Limpopo.
South Africa has been shaped by, and is actively shaping, the world through global trends on the determinants of health, formal collaborations with global and regional institutions and through the expanding knowledge on health technology and public health interventions. The influence of South Africa in the response to COVID-19 in the region exemplifies this – with the President’s role in the African Union, the pivotal role of South African scientists in tracking and identifying new COVID variants and researching interventions, and the breakthrough in planning for mRNA COVID vaccine production in the country.
Looking to the future
Recommendation (34) South Africa’s role in global and regional health: South Africa needs to continue to examine and expand on its role in the region and globally, both to improve the health of the people of South Africa, and for improving health regionally and globally. This should include striving for the betterment, harmonisation and coordination of Africa’s global health system, sustainable financing initiatives, aligning aid goals with the regional health needs and priorities, providing thought leadership on global health programmes, and strengthening global health initiatives through regional alliances.
Whilst there has been progress with some health reforms and health outcomes in the period before the COVID-19 pandemic, there is still much to be done to strengthen the health system and in the provision of equitable and quality care. Major reforms, such as the introduction of NHI, seem to have stalled. The recommendations from the analyses of the 2015 – 2020 period in this book provide some light on where attention, mainly by government, is required for the South African health system to be rejuvenated and to respond optimally to future challenges.
Most such reforms require political will, stewardship and the exercise of vigilance on corruption. Equally important is the attention required to address gender inequality and discrimination faced by women and girls; a particular low point is the increasing levels of adolescent pregnancy – a signal of many failings in the health system and beyond that require urgent attention. Successful reforms often also require changes in the way communities are engaged in order that different stakeholders can work together to achieve positive health impact and outcomes. Finally, the government should continue to expand intersectoral collaboration to both address broader determinants of health and to improve the effectiveness of health services, in particular the quality of primary health care. However, it is not only the government but also an active citizenry that is required to keep the government accountable in all spheres of government.
A
accountability definition 322 health system performance 150, 320, 321, 234, 251, 278, 298, 321, 366, 368 in health standards compliance 129 information and indicators for 322–325 longstanding failures 291 private sector 415 accountability dimensions information and indicators’ requirements 324 accruals 370, 382 acountability relationships in health system 323 AfCFTA African Continental Free Trade Area 400 African Continental Free Trade Area (AfCFTA) 400 AIDS prevalence 21, 22, 88 Alma-Ata Declaration 46, 58, 60, 320, 346 annual health planning maturing process 309–310 anti-microbial resistance scaling up needed 410 Astana Declaration 60, 61, 320
B Beaufort West Clinic green building 240 bed capacity provincial spread 224, 225 Bioko Island Malaria Elimination Project 400
C
capacity constraints effect on public confidence 391 financial and human resource 230 of data on workforce 348 capitation system of reimbursement inability to develop 365
CCMDD Centralised Chronic Medicines Dispensing and Distribution programme 66, 114,163, 327–328 Centralised Chronic Medicines Dispensing and Distribution programme (CCMDD) patient-centred care 66, 114,163, 327–328 child health district clinical specialist teams 64–65 child health improving 299 need for improved 25, 41, 42, 407 climate change implications for health planning 293 clinical associates importance of 343 clinics antenatal 270 dependence on 227 extent of reliance on 18, 227–228 Ideal Realisation and Maintenance 232–233 infrastructure ratings 228 patients’ proximity to 226 Stock Visibility System (SVS) 326–327 collaboration intersectoral 306 collaborative governance definition 293 community health workers effectiveness of programmes 346 community service compulsory 345 cost pressures public sector 382 role in maintenance neglect 229 COVID-19 financing 388–389 global response shortcomings 397 impact on economic growth 389–390 impact on mental health of workforce 347 South Africa’s role in global responses 398 COVID-19 infrastructure lessons impact of technology 238 importance of flexibility 238 improving ventilation 238 COVID-19 Tools Accelerator (ACT-A) initiative South Africa’s role in 398
COVID-19 vaccines
Manufacturing Task Force on 398
D data collection value of rapid 331 data innovations driven by COVID-19 150, 325–326 data shortages effect on health care 262, 329, 332 data sources for human resource planning 340–341 need for improved 348, 408 DDM
District Development Model 62, 76 declarations of Alma-Ata improving health outcomes 46, 58, 60, 320, 346 development assistance international 401–402
Diagnostic-Related Group (DRG) inability to develop a 365 district clinical specialist teams 64 District Development Model (DDM) 62, 76 district health interventions 295, 296, 302, 305, 321
Draft 10-Year Health Infrastructure Plan 237 Draft Maintenance Strategy 238 DRG
“Diagnostic-Related Group” 365
Eemergency obstetric care (EmOC) Gauteng Province 297 EmOC emergency obstetric care 297 expenditure declining 62 health care 36-37, improving efficiency 132 mental health 193–195 primary health care 70 total district 124 workforce 63
G gender and human rights 97
gender equity in medical workforce 351 gender issues in budgeting 388 global and regional health South Africa’s role in 417 global health initiatives South Africa’s contributions 398–399
Global Strategy on Human Resources for Health: Workforce 2030 equitable access to health workers highlighted 338 goods and services spending per capita 385 governance at provincial level 63, 69 challenges 250, 291, 297, 348 challenges in hospitals 125–126, 129 community participation in 251, 312 implementation of improved 250 importance of good leadership and management for 311 improving 251, 263, 270, 283, 414 policy and planning 249 positive experiences 298 relational view of 293 relationships and interfaces 292, 294, 295, 296, 298, 303, 305 SA Lancet Commission’s findings on 249 weaknesses 77, 130, 283, 312, 409, 414 governance practice dominant relationships in 294 governance relationship district-province 305 provincial-national 306
H
health accounts data national 368 health budget trends 370–372 provincial 370 health care expenditure inequitable 375 health care facilities access to 266
infrastructure planning shortcomings 230–231 waiting times 226 health care needs for the future 241
health channels need for greater efficacy 321 health data improved access and use of 415 health expenditure per capita variations 376 health financing legislation need 416 reforms 416 health financing reform building consensus around 367 lessons from COVID-19 367 health governance critical roles in 310 health governance charter need for 414 health indicators core 324 health infrastructure capacity constraints 230 challenges 229–230 improving 412 priorities and efficiencies 413 ranked against other African countries 228–229 health infrastructure planning impact of climate change 239 health infrastructure provision asset management shortcomings 232 compliance issues 231 funding and spending inadequacies 231 inadequate capacity and skills 231 overreliance on consultants 232 recommendations 232
Health Market Inquiry (HMI) findings 110, 249, 278, 349, 379–380 health ombud 250, 255, 329, 413 health partnerships public-private 76, 201, 218, 348, 400 Health Patient Registration System (HPRS) 67, 365 health personnel trends 383–385 health practitioners staffing ratios 344–345 Health Products Regulatory Authority (SAHPRA) need for scaled up efforts 104–118, 410 health providers 262, 264, 281, 304, 320, 321, 322, 344, health reforms political economy 366
health service managers further development of 351 health services inequitity 381 standardising 381 health spending provincial 369, 376 reforms 369 compared with international benchmarks 228, 372–375 public 291, 369 trends in 368–370 health standards compliance accountability for 129 health system culture impact on the health system 350 health system governance dominant relationships 294–295 re-sets needed 312–314 health system governance actors 293 health workforce migration 343 need for strategic leadership capability 350 HEEG
United Nations High-Level Commission on Health Employment and Economic Growth (HEEG) report 338–339 high-quality health system conceptual framework 247 definition 247 HIV
Advocacy and Health Delivery 399 co-infection 83, 164, 191 lessons from 165, 172 Masoyise Health Programme 214 prevalence 21-22, 58, 62, 82, 88–92, 99, 270 rights-based access to 97 targets set by the United Nations 372 treated as a chronic disease 409 Treatment Action Campaign (TAC) 270 HIV/AIDS burden on health system 82 co-morbidities 159 expansion of care 70 impact on health system development 58 unequal response 88 HMI
Health Market Inquiry 110, 249, 278, 349, 379–380
hospital boards minimal impact on community needs 321 hospital services decentralised management 410 hospitals accountability 128 community engagement 128 definition of ideal 129 financial management reforms 387 funding 131–132 human resources 132–133
Ideal Hospital Realisation and Maintenance Framework (IHRM-F) 129–130 infrastructure 133, 228–230 leaders and management 126–127 mental health services in 185 of the future 239
Office of Health Standards Compliance (OHSC) 129 persistent challenges 125–126 private for mental health services 186 psychiatric 186 ratings 228 role of specialised 124 strengthening governance 129 waiting times 226 workforce 132–133 household surveys provide data from a citizen perspective 325 HPRS
Health Patient Registration System 67, 365 Human Resource Information System (HRIS) aims 353 human resource planning data sources 340 strategic intervention 339 human resources performance studies 341 human resources for health digitisation 353 research 350 skills mix 343 task shifting 343 human resources for health management practices shortcomings 350 Human Resources for Health Plan for 2020/21–2024/25 250
Human Resources for Health Strategy 2030 immediate commitments 354–355 strategic goals 354 vision, goals and actions 354
human resources health strategy implementation 250, 415 prioritiesed recommendations 415 human resources management information systems 348 human resources studies undertaken in South Africa 341–342
Ideal Clinic Realisation and Maintenance (ICRM) implementation challenges 232–233, 256, 307–308 successes 249 inequalities and inequities need for improved monitoring 407 infrastructure provincial spread 224 infrastructure planning health care facilities 230 Infrastructure Unit Support Systems (IUSS) project achievements 235 challenges 237 Integrated Human Resource, Personnel and Salary System (PERSAL) 348
Joint Health Action Plan 387
Lancet Global Health Commission on High-Quality Health Systems holding systems accountable 320, 321 leadership in Eastern Cape hospitals 300 development 311 leadership and governance WHO definition 292 leadership development need for 414 leadership practices autocratic 311 enabling 300 legislative development health 414
Masoyise Health Programme 214 maternal mortality 17–18 maternal-child health 3-feet Model 75 programme structures 64 maternal, neonatal and child health (MNCH) experiencing improvement 299 medical workforce gender equity 351 medico-legal litigation challenges and reforms 386–387 meetings new approaches 304 mental health services increased investment needed in 412 MomConnect 50, 259 mothers living with HIV 270 mothers of infants MomConnect 259
N
National Digital Health Strategy moving towards anticipated gains 331 National Health Insurance limited progress 363–365, 381, 391 National Health Insurance Bill data requirements for implementation planning 348 potential for alienation 366 resources for health planning 347–348 National Indicator Data Set (NIDS) summary of Core Health Indicators 324 National Policy on Management of Hospitals see hospitals 123 National Quality Improvement Plan (NQIP) 249, 256
National Quality Strategic Framework proposed structure 248 mandate 247 National Strategic Direction for Nursing Education and Practice: A Road Map for Strengthening Nursing and Midwifery in South Africa (2020/21–2025/26) objectives 355 NDP 2030 implementation of 249
Nelson Mandela-Fidel Castro Medical Collaboration Programme
impact on medical student training 347 Non-Communicable Disease National Strategic Plan rapid implementation needed 411 non-communicable diseases (NCDs) data needs for 165–166, 407 nursing strategy recruitment and succession planning 355
O obstetric deaths causes 18
Occupation Specific Dispensation (OSD) remuneration scales 345 occupational health and safety challenges 218 occupational health services funding 412 Office for Health Standards Compliance (OHSC) inspection reports made public 328–329 value chain 254 OHSC
see The Office of Health Standards Compliance (OHSC) ombud health 255 Operation Sukuma Sakhe KwaZulu-Natal province 302–303 oversight actors separate from policy makers 295
P
package of essential services importance of 409 pandemic preparedness need to update responses 411 payables 382 performance studies in human resources 341 pharmaceutical analytics units independent called for 331 pharmaceutical utilisation data Mediscor provides public access to 325 pharmacists deployment efficiencies needed 410
Western Cape Provincial Health Data Centre 329
policy accountability relationships within the district office 295 political interference governance challenge 305 polycentric process 293 practitioners community service 345 environmental health 147 failures of accountability 278 shortage of 379 Presidential Health Summit human resources for health challenges 348–349
primary health care challenges confronting 60 shortcomings to be addressed 408–409 people’s rights 320 primary health care facilities benchmarks 226 measure of access 266 private financing medical aids 377–378 private health care regulatory and systemic issues 349 private health data fragmented 325 provincial and district health councils extended mandates 414 provincial equitable share (PES) funding formula 375 Provincial Equitable Share formula improving equity 391
public accountability relationships nature of at district office level 296 public health spending 343–344 public health system inverted pyramid of power 297 public health system governance view of 295
Q quality measurement of 262 private sector 260-261 quality health system interventions community participation in governance 251 Council for Medical Schemes (CMS) report 251
fighting corruption 250 Human Resources for Health (HRH) Plan 250
National Quality Improvement Plan (NQIP) 251 Office of Health Standards Compliance (OHSC) 250 quality health system interventions statutory health professional councils implementation of mandates 251 Quality Improvement Plan (QI) projects 257–259 quality of care recommendations 413 revolutionising 253 quality of services
national commitment to 410
Rrelational view of governance prominence of 293 relationships policy and oversight 310 Ritshidze Community-led Monitoring 76
S SAHPRAHealth Products Regulatory Authority 104–118, 410 SECTION27 interviews recommendations 368 views on current and ideal health system 367 service provision relationships of the district office 296
Social, Economic, Commercial and Environmental Determinants of Health (SECEDH) recommendations 408
South African Human Resources for Health (HRH)
Strategy for the Health Sector
South African Lancet National Commission 2019 governance findings 249 high-quality health system definition 247 accreditation 248 certification 248 quality control 248 quality improvement 248 Council for Medical Schemes (CMS) response to 252
SSP
Stop Stockouts Project 327 staffing needs workload indicators 342 Stock Visibility System (SVS) aim of the system 326 in clinics 326–327 preventing stockouts 327 Stop Stockouts Project (SSP) non-profit organisations involved in 327 Stop TB initiative South Africa’s role in 398 strengthening governance through relationship building 303 Sustainable Development Goals (SDGs) health and wellness aspirations 397 system-wide governance collective action 307 systems leadership description 294
T TAC
Treatment Action Campaign 270 TB
leading natural cause of death 13, 19–20, 25, 33
South African National TB Prevalence Survey 19 policies and programmes 58, 235, 257, COVID-19 impact on 72, 81, 82, 98, 152, 409 national health programmes and support 83–87, 143, 160, 164 co-morbidities 159, 170, 191 occupational disease 201, 205, 206, 214, 218 data 324, 330, 331 stock-outs for medicines 327 community health workers 346 Stop TB initiative 398, 409 technological advances implications 353 telehealth reshaping the health sector 353 training pipelines planning challenges 339 Treatment Action Campaign (TAC) 270 Triple Billion programme 397 tuberculosis
See TB
United Nations Convention on the Rights of Persons with Disabilities
South Africa’s response 401 United Nations High-Level Commission on Health Employment and Economic Growth (HEEG) report recommendations 338–339 universal health coverage addressing needs 9, 224, 339, 366 financing reforms needed 361 HIV 99 mental health 193 provided by National Health Insurance 281
W waiting times for access to health care facilities 226–227 Western Cape Provincial Health Data Centre (PHDC) 329 WHO
State of World Nursing 2020 355 WHO frameworks early, criticised 294 whole-of-government (WoGA) key approach 293 whole-of-society (WoSA) key approach 293 achievements 301–302
Western Cape province 301 WISN 255, 342–343
Workload Indicators of Staffing Needs (WISN) Workload Indicators of Staffing Needs 255, 342–343