5 minute read
Ambulatory Surgery Center Development in an Academic Medical Center—Is It Possible?
The Ambulatory Surgery Center Association defines ambulatory surgery centers, or ASCs, as “modern healthcare facilities focused on providing same-day surgical care, including diagnostic and preventive procedures.”[1] Indeed, ASCs have transformed the outpatient surgical experience for many millions of Americans by providing them with a patient-centric, efficient, and cost-conscious alternative to overnight hospital-based outpatient procedures. Since the advent of ASCs (first established in 1970 in Phoenix, AZ), there has been substantial evidence supporting that spine procedures can be successfully completed with high-quality care and positive patient outcomes.[1] The benefits of ASCs specifically for surgeons are incremental; they allow surgeons the ability to perform specific procedures more safely, efficiently, and conveniently compared to hospital-based operating rooms.
The Agency for Healthcare Research and Quality states that nearly 75% of all surgeries in the United States are done in an ambulatory setting, often at an ASC.[2] As the concept gained traction and with broad partnerships between management companies, physicians (surgeons and anesthesiologists), and financial entities, ASCs are now the preferred site of service for many spine procedures, including decompressions, endoscopic cases, and select fusions (eg, anterior cervical discectomy and fusion). It is reasonable to expect that the patient and surgeon benefits, quality control, and cost-consciousness in the private sector make ASCs attractive options for academic medical centers that traditionally provide quaternary care to a sicker patient population. By definition, an academic ASC is defined as an ASC that operates under the management of an educational institute and is located within or outside the institutional buildings. A hospital outpatient department (HOPD) is typically owned by a hospital and is managed by its management team. The physical location of the HOPD could be within a 35-mile radius of the main hospital.
The question is, can the benefits of privately owned ASCs translate to academic medical centers? What needs to be done differently in an academic ASC to achieve similar success?
What are the differences between non-academic vs academic ASCs?
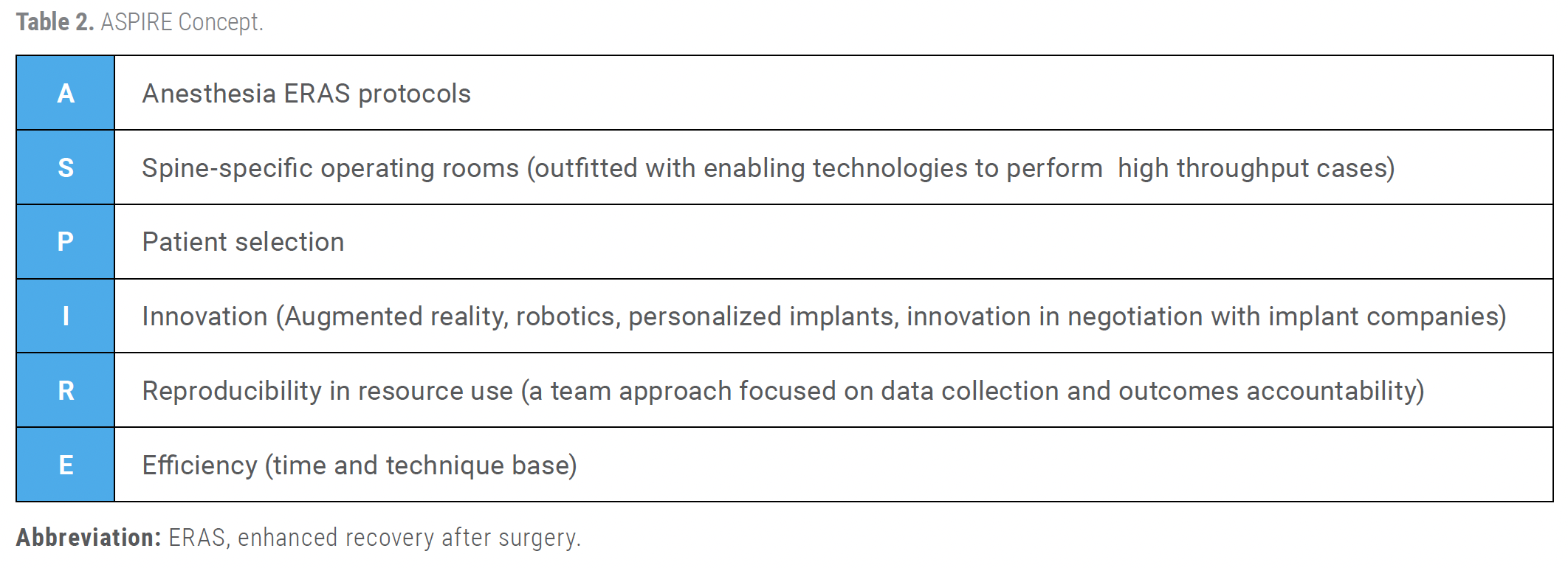
Nonacademic ASCs are typically managed by externally hired teams with physician board oversight, promoting cost-conscious decision-making and fostering culture change through physician ownership. In contrast, academic ASCs, which can be ASCs or HOPDs, are under hospital administration jurisdiction, require inspections from the Joint Commission on Accreditation of Healthcare Organizations, and potentially need accreditation if trainees are involved. Medicare/Medicaid payments can also differ between ASC and HOPD entities. Table 1 outlines some of these differences.
What factors do academic institutions need to keep in mind when opening an ASC?
Culture Shifts
The quaternary-level care model of traditional academic medical centers often leads to inefficiencies and restrictions in terms of access to cost and time-conscious care. In an environment that will only be successful if there is protocolized care, procedural fluidity, and rapid turnover, staffing models (physician, nursing, operating room teams) will need to include individuals with a highly flexible mindset. Constant communication is key to rapid corrections of any issues that may lead to inefficiency.
Partnerships and Joint Ventures
Academic medical centers may collaborate with private practices, healthcare systems, or investment groups to form ASCs. These joint ventures allow academic centers to leverage external expertise and investment while expanding their outpatient capabilities. The Johns Hopkins Model (JHM) is an excellent example to study.[3] Its Surgery Coordinating Council (SCC) was established to integrate its eight ASCs with its HOPDs. With culture change, partnerships, and a constant cycle of improvement, they have created a superb model of academic center ASC integration. Some factors in their success have been (1) promoting multidisciplinary interactions among JHM-employed and non–JHM-employed physicians; (2) setting approaches for ASC quality and safety efforts; and (3) constantly identifying, implementing, and evaluating best practices.
Focus on Efficiency and Innovation
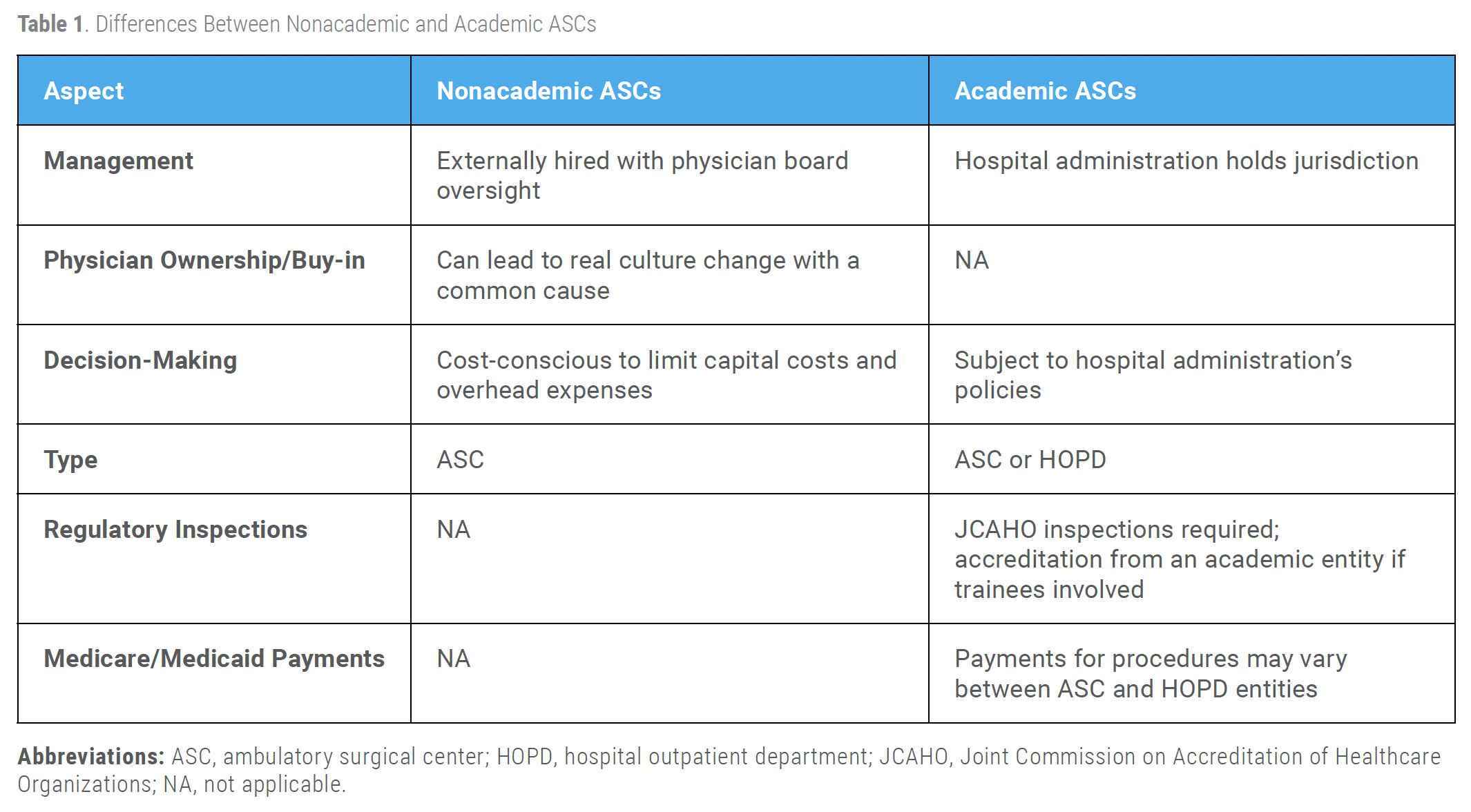
ASCs allow academic centers to offload routine or less complex surgical cases from traditional hospital settings, which are often more expensive. This separation increases the efficiency of hospitals for complex surgeries and allows the ASC to specialize in high-volume, lower-risk procedures. The ability to invest in enabling technologies creates an exciting set of principles, including surgery-specific operating rooms—outfitted at the ASC to only take care of specific service lines. We believe the ASPIRE concept (Table 2) allows academic centers to create success for spinal procedures in the ASC environment.
Training and Research
Since academic centers are teaching institutions, having an ASC can offer medical residents and students exposure to outpatient surgeries, giving them hands-on experience. It also provides a setting to explore new surgical techniques and technologies in a controlled, cost-effective environment. Fellows who are being recruited to an ASC-heavy practice can get a head start on managing their training and creating their practice.
Improved Patient Experience
ASCs can streamline the patient experience with shorter wait times, lower costs, and a less intimidating atmosphere compared to large hospitals. This aligns with academic institutions' missions to advance patient-centered care.
Financial Incentives
Operating an ASC can be a more profitable venture compared to a full-service hospital, due to lower overhead costs and better insurance reimbursement rates for outpatient services. Academic centers often pursue these ventures to help offset other more costly areas of care.
Summary
Academic centers can and often do create ASCs. These centers, which are designed for outpatient surgeries, allow academic institutions to expand their surgical services, improve patient care, and create a more efficient and cost-effective environment for certain procedures. The ASPIRE concept can guide spine-specific success in academic ASCs.
References
1. Ambulatory Surgery Center Association. What is an ASC? https://www.ascassociation.org/asca/about-ascs/surgery-centers
2. Wier LM, Steiner CA, Owens PL. Surgeries in Hospital-Owned Outpatient Facilities, 2012. HCUP Statistical Brief #188. Agency for Healthcare Research and Quality; 2015.
3. Ishii L, Pronovost PJ, Demski R, Wylie G, Zenilman M. A model for integrating ambulatory surgery centers into an academic health system using a novel ambulatory surgery coordinating council. Acad Med. 2016;91(6):803–6.
Contributors:
Safdar N. Khan, MD[1]
Hania Shazad, MD[1]
Richard L. Price, MD, PhD[2]
From the [1]Department of Orthopaedic Surgery and [2]Department of Neurological Surgery, both at UC Davis Health in Sacramento, California.