
11 minute read
Augmented Reality
Transforming the Future of Spine Surgery
In the rapidly evolving field of medicine, augmented reality (AR) has emerged as a transformative technology that seamlessly integrates virtual images into the real world. When compared to virtual reality (VR), which immerses users entirely in a synthetic virtual realm, and mixed/merged reality (MR),[1] which represents a fusion of a virtual environment with haptic feedback through physical models, AR technology stands out as a compelling choice for applications in spine surgery. AR offers real-time applications in surgical procedures, surpassing the primarily training-focused utilities of VR and MR in nonoperative settings.[2]
AR navigation in spine surgery delivers accuracy and enhances workflow compared to conventional navigation and freehand techniques. This is particularly crucial in spine surgeries, where precision is vital due to the proximity of the operative field to delicate neurovascular structures. AR support also improves surgical comfort, particularly in reoperations where anatomical landmarks are lacking. Additionally, AR-based patient registration reduces radiation exposure for both patients and medical staff. It also provides a safe platform for trainees to practice complex surgical procedures through stepby-step interactive learning, minimizing the risk of patient harm and achieving higher success rates with reduced tissue trauma. Additionally, the collaborative nature of AR fosters multidisciplinary teamwork during surgery and facilitates global expertise expansion through telementorship. Moreover, its cost-effectiveness and adaptability make it a valuable tool for surgical training and practice, especially in resource-limited settings.[3–5]
AR-Based Surgical Set-up
An AR-based surgical procedure comprises three key components: patient registration, instrument tracking, and display (Figure 1). The radiological images of the patient’s anatomy are used to construct a 3-dimensional (3D) model using advanced software. Patient registration involves aligning computer-generated images with the surgical area utilizing markers strategically positioned within the surgical field to maintain continuous tracking. The markers play a critical role in maintaining constant tracking of both the surgeon’s instruments and the patient’s anatomy. Markers ensure that the superimposed 3D images remain in the correct position and orientation, even as the instruments move. The display device allows the visualization of the holographs during surgery. As the surgeon operates, the display overlays an image of the vertebral spine onto the surgeon’s operating field, which enables precise identification of the optimal trajectory for procedures, such as an accurate screw placement.[6]
Display devices offer a diverse range of user interfaces tailored to meet the distinct demands of spine surgical procedures. These include monitor-based AR, in which a C-arm with embedded cameras displays real-time video with AR enhancements on an operating room monitor, head-mounted display AR (with AR integrated into surgeons’ goggles), microscope AR (with predefined AR elements seen through the microscope), and projector-based AR (with holographic overlays on glass screens). Comparing these interfaces is complex due to differing study metrics. Selection depends on surgical needs and technological advancements.

Clinical Applications of AR in Spine Surgery
AR technology has undergone extensive investigation in preclinical settings within the domain of spine surgery, exhibiting significant potential to augment accuracy, safety, and training in this specialized field (Table). Investigations into clinical studies and live patients are painting an exciting picture of its potential benefits.[6] The scrutiny surrounding the safety and efficacy of AR navigation in thoracic pedicle screw placement has yielded highly promising results. Researchers have achieved an overall accuracy rate of an impressive 94.1%, notable for its absence of severe errors or device-related adverse events.[7,8] Of equal significance is the seamless integration of AR into hybrid operating room setups, marked by the inclusion of intraoperative imaging and patient tracking. This technological integration has successfully eliminated the necessity for traditional fluoroscopy, thereby not only mitigating radiation exposure but also substantially enhancing the precision of screw placement.[9,10]
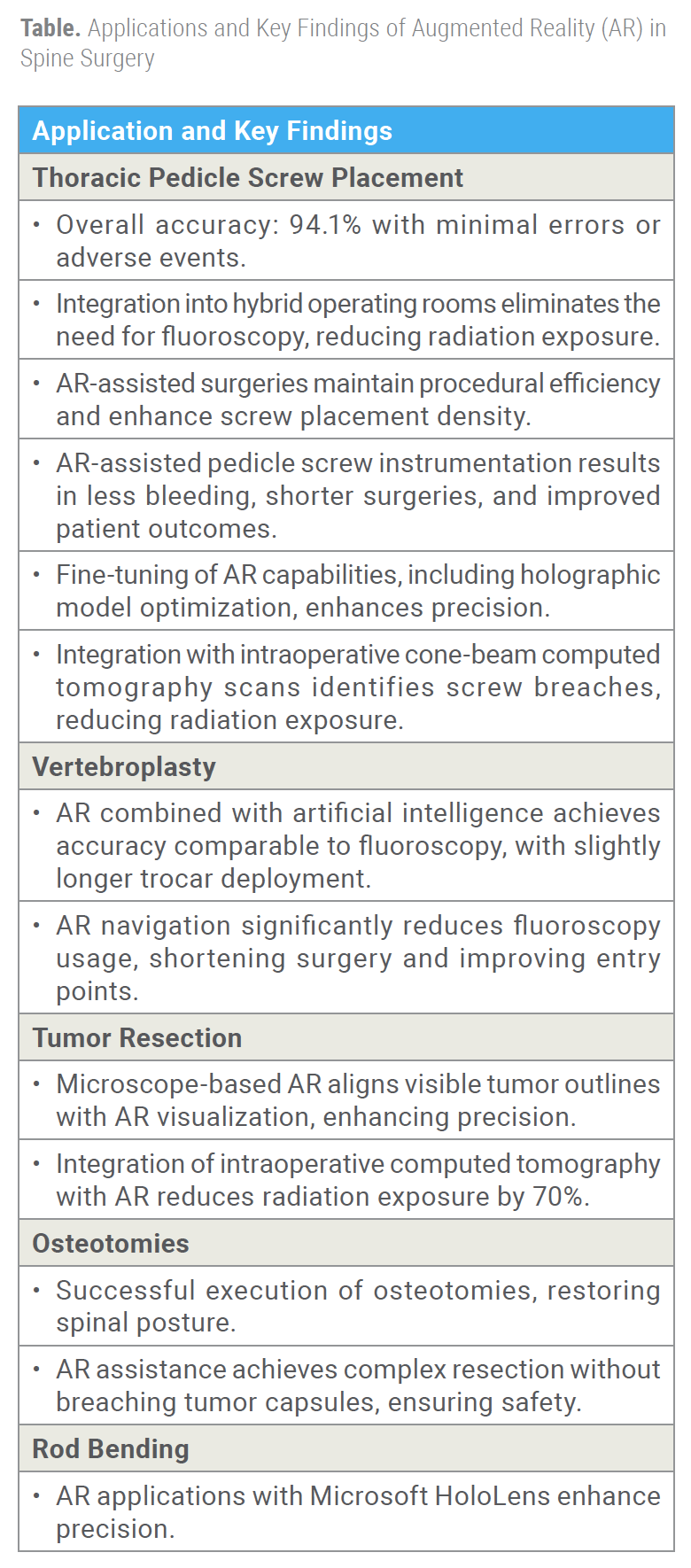
Remarkably, the introduction of AR into the operating theater does not impede the efficiency of surgical procedures. AR-assisted spinal surgeries do not lengthen the duration of operations but, rather, they augment the density of pedicle screw placements, particularly in intricate deformity cases.[9,10] The advantages of AR-assisted pedicle screw instrumentation continue to accumulate, with research indicating reduced intraoperative bleeding, shorter surgical durations, and notably superior patient-related outcomes compared to conventional methods.[11] Moreover, meticulous fine-tuning of AR’s capabilities, including the optimization of an intraoperative holographic model pipeline, has resulted in pinpoint precision through the utilization of patient-specific
landmarks.[12] The synergy of intraoperative cone-beam computed tomography scans with AR-assisted systems has proven highly effective in identifying pedicle screw breaches,[13] rendering routine postoperative CT scans obsolete while simultaneously reducing the overall radiation exposure burden on both patients and medical staff. These findings collectively underscore the transformative potential of AR in the field of spine surgery, offering an intriguing glimpse into the future of precision, safety, and patient care in this specialized domain.
The dynamic combination of AR with artificial intelligence in vertebroplasties achieves accuracy on par with traditional fluoroscopy, albeit with a slight extension in trocar deployment time.[14] Furthermore, AR-assisted navigation substantially reduces the reliance on fluoroscopy, thereby curtailing operative durations and significantly enhancing the proportion of “optimal” entry points.[15] The introduction of a microscope-based AR navigation system into tumor resection surgery has illuminated a close alignment between the visible tumor outline and AR visualization. This alignment translates into a remarkable boost in surgical precision. The amalgamation of intraoperative computed tomography (CT) with AR has yielded a staggering 70% reduction in effective radiation exposure.[16,17] The early pioneers of AR application in osteotomies, led by the work of Kosterhon et al, deserve commendation for laying the foundational groundwork. They executed osteotomies in the thoracic and lumbar regions, restoring spinal posture with surgical finesse.[18] Similarly, Molina et al executed a complex resection of a chordoma margin without breaching the tumor capsule. Their posterior-only approach, bolstered by AR head-mounted displays and integrated tracking cameras, underlined the precision and safety offered by this pioneering technology.[19] Additionally, AR applications employing Microsoft HoloLens head-mounted displays have unlocked a new level of precision, particularly in rod bending.[20]
Legal and Ethical Implications
In terms of protecting data, new technologies pose new challenges that have both legal and ethical implications.[21] In general, the use of new technologies has opened new paths for fraud, scams, and data trading. A special threat is created using technologies that track cognitive or decision-making processes, or augmented intelligence, which gathers very personal data, for example, on the functioning of someone’s brain. In the United Kingdom, current legal requirements, including common law, the Data Protection Act 1998, and the Freedom of Information Act 2000, establish the framework for data protection and confidentiality. The holding organizations, such as hospitals, should have governing bodies or a designated “Caldicott guardian” responsible for enforcing data security and protecting personally identifiable data as highlighted by the General Medical Council. While regulations like the General Data Protection Regulation in the European Union serve as foundational pillars for data protection, they must be complemented by specific guidelines tailored to the unique challenges posed by AR technologies. Fur-thermore, the National Health Service (NHS) adheres to the NHS code of practice for confidentiality, which is underpinned by 7 principles governing the collection and transfer of identifiable information.[22] Healthcare professionals engaging with patient data through AR technology must possess a deep understanding of these principles to ensure compliance.
Surgeon autonomy may be influenced by marketing efforts promoting AR, potentially impacting unbiased decision-making. Patients, too, can be swayed by advertising, potentially influencing their choice of surgeons or facilities offering AR-assisted procedures and affecting their autonomy in healthcare decisions. Ensuring informed consent and transparency about AR’s role in surgery is paramount, alongside managing conflicts of interest that may arise from financial relationships between technology providers and healthcare professionals. The development of these groundbreaking technologies has ignited concerns about the potential introduction of biases into their design and implementation, particularly when the development teams lack diversity. Biases embedded within technology can have far-reaching consequences, disproportionately affecting specific user groups based on factors such as gender, race, age, or social background.[23]
Future Directions
To fully unlock AR’s potential in the field of spine surgery and facilitate its widespread adoption, it becomes imperative to prioritize aspects such as standardization of protocol and outcome measures, improving the ergonomics of AR headsets,[24] forging ethical frameworks, and investing in comprehensive education and training programs. AR technology continues to redefine the boundaries of what can be achieved in the world of spine surgery, transcending its role as a mere tool and emerging as a transformative force that pushes boundaries and elevates the standards of precision, safety, and patient care.
References
1. Yuk FJ, Maragkos GA, Sato K, Steinberger J. Current innovation in virtual and augmented reality in spine surgery. Ann Transl Med. 2021;9(1):94.
2. Sakai D, Joyce K, Sugimoto M, et al. Augmented, virtual and mixed reality in spinal surgery: a real-world experience. J Orthop Surg. 2020;28(3):2309499020952698.
3. Shahzad H, Bhatti NS, Phillips FM, Khan SN. Applications of augmented reality in orthopaedic spine surgery. J Am Acad Orthop Surg. 2023;31(17):e601.
4. Cofano F, Di Perna G, Bozzaro M, et al. Augmented reality in medical practice: from spine surgery to remote assistance. Front Surg. 2021;8:657901.
5. Carl B, Bopp M, Saß B, Voellger B, Nimsky C. Implementation of augmented reality support in spine surgery. Eur Spine J. 2019;28(7):1697-1711.
6. Burström G, Persson O, Edström E, Elmi-Terander A. Augmented reality navigation in spine surgery: a systematic review. Acta Neurochir (Wien). 2021;163(3):843-852.
7. Elmi-Terander A, Burström G, Nachabe R, et al. Pedicle screw placement using augmented reality surgical navigation with intraoperative 3D imaging. Spine. 2019;44(7):517-525.
8. Molina CA, Sciubba DM, Greenberg JK, Khan M, Witham T. Clinical accuracy, technical precision, and workflow of the first in human use of an augmented-reality head-mounted display stereotactic navigation system for spine surgery. Oper Neurosurg. 2021;20(3):300-309.
9. Elmi-Terander A, Burström G, Nachabé R, et al. Augmented reality navigation with intraoperative 3D imaging vs fluoroscopy-assisted free-hand surgery for spine fixation surgery: a matched-control study comparing accuracy. Sci Rep. 2020;10(1):707.
10. Edström E, Burström G, Nachabe R, Gerdhem P, Elmi Terander A. A novel augmented-reality-based surgical navigation system for spine surgery in a hybrid operating room: design, workflow, and clinical applications. Oper Neurosurg. 2020;18(5):496-502.
11. Gu Y, Yao Q, Xu Y, Zhang H, Wei P, Wang L. A clinical application study of mixed reality technology assisted lumbar pedicle screws implantation. Med Sci Monit Int Med J Exp Clin Res. 2020;26:e924982-1-e924982-12.
12. Buch VP, Mensah-Brown KG, Germi JW, et al. Development of an intraoperative pipeline for holographic mixed reality visualization during spinal fusion surgery. Surg Innov. 2021;28(4):427-437.
13. Burström G, Nachabe R, Persson O, Edström E, Elmi Terander A. Augmented and virtual reality instrument tracking for minimally invasive spine surgery: a feasibility and accuracy study. Spine. 2019;44(15):1097.
14. Auloge P, Cazzato RL, Ramamurthy N, et al. Augmented reality and artificial intelligence-based navigation during percutaneous vertebroplasty: a pilot randomised clinical trial. Eur Spine J. 2020;29(7):1580-1589.
15. Hu MH, Chiang CC, Wang ML, Wu NY, Lee PY. Clinical feasibility of the augmented reality computer-assisted spine surgery system for percutaneous vertebroplasty. Eur Spine J. 2020;29(7):1590-1596.
16. Carl B, Bopp M, Saß B, Nimsky C. Microscope-based augmented reality in degenerative spine surgery: initial experience. World Neurosurg. 2019;128:e541-e551.
17. Carl B, Bopp M, Saß B, Pojskic M, Voellger B, Nimsky C. Spine surgery supported by augmented reality. Glob Spine J. 2020;10(2 suppl):41S-55S.
18. Kosterhon M, Gutenberg A, Kantelhardt SR, Archavlis E, Giese A. Navigation and image injection for control of bone removal and osteotomy planes in spine surgery. Oper Neurosurg (Hagerstown). 2017;13(2):297-304.
19. Molina CA, Dibble CF, Lo SFL, Witham T, Sciubba DM. Augmented reality–mediated stereotactic navigation for execution of en bloc lumbar spondylectomy osteotomies. J Neurosurg Spine. 2021;34(5):700-705.
20. Wanivenhaus F, Neuhaus C, Liebmann F, Roner S, Spirig JM, Farshad M. Augmented reality-assisted rod bending in spinal surgery. Spine J. 2019;19(10):1687-1689.
21. Parsons TD. Ethical challenges of using virtual environments in the assessment and treatment of psychopathological disorders. J Clin Med. 2021;10(3):378.
22. Donaldson A, Walker P. Information governance—a view from the NHS. Int J Med Inf. 2004;73(3):281-284.
23. Wójcik M. Augmented intelligence technology. The ethical and practical problems of its implementation in libraries. Libr Hi Tech. 2020;39(2):435-447.
24. McKnight RR, Pean CA, Buck JS, Hwang JS, Hsu JR, Pierrie SN. Virtual reality and augmented reality—translating surgical training into surgical technique. Curr Rev Musculoskelet Med. 2020;13(6):663-674.
Authors: Hania Shahzad, MD, and Safdar N. Khan, MD
From The Ohio State University, Wexner Medical Center, in Columbus, Ohio.










