
12 minute read
A Comparative Review of Lumbar Bone Density Measurement Techniques and Additional Applications
The evaluation of vertebral bone density prior to spinal instrumentation is a critical component of the preoperative assessment. Instrumentation of osteoporotic bone can result in complications such as pedicle screw pullout, device subsidence, or device migration.[1-5] A growing area of research focuses on screening lumbar bone prior to spinal surgery and may yield great benefits to patients in reducing instrumentation complications.
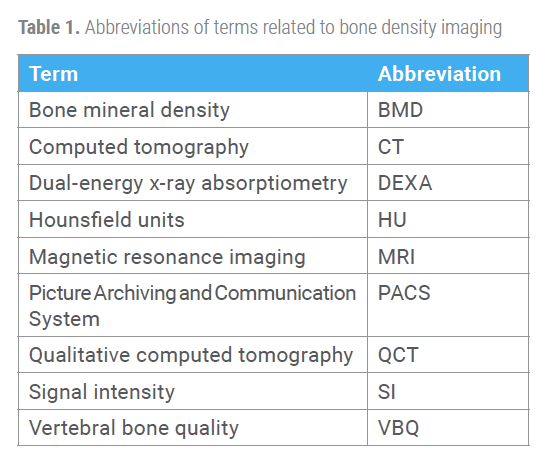
Dual-energy x-ray absorptiometry (DEXA) has been the gold standard for assessing lumbar bone density and classifies bone as either normal, osteopenic, or osteoporotic.[6,7] In light of potential shortcomings in DEXA’s lumbar composite values, alternative imaging for bone density measurements have been investigated, such as computed tomography (CT) Hounsfield units (HU), quantitative computed tomography (QCT), and magnetic resonance imaging (MRI) vertebral bone quality (VBQ).[8,9]
In a previous issue of Vertebral Columns,[10] we explained how to acquire and interpret these lumbar bone density measurements. In the present article, we discuss the literature comparing lumbar bone density measurement techniques and present additional applications of these measurements for spinal surgery. A considerable number of studies have provided evidence that indicate promising alternatives to DEXA for measuring lumbar bone quality.
CT HU and QCT Lumbar Measurements
Multiple studies have tested CT HU as a measure of bone density in comparison to DEXA bone mineral density (BMD) values. Viswanathan et al reported a significant correlation between CT HU and DEXA T-scores at the upper lumbar levels (L1-L3) in patients who underwent 1-2 level lumbar fusions.[11]
The opportunistic availability of CT measurements may provide reasonable identification of osteoporosis, but not all studies agree. Kohan et al found a low to moderate correlation between CT HU measurements and femoral neck DEXA BMD values in patients with adult spinal deformities.[12,13] In addition, the cutoffs for defining osteoporotic versus osteopenic or normal bone are still debated, with normal bone around 160 and 179 HU and osteoporotic/ osteopenic bone closer to 100 and 110 HU.[14-16]
Other studies have researched correlations between CT HU measurements and incidences of postoperative complications. Murata et al experimented with CT measurements and the incidence of vertebral fractures in an elderly population. They found that CT HU measurements of the anterior one-third of the vertebral body can predict the occurrence of postoperative vertebral fractures.[17]
Li et al calculated CT HU measurements for the planned screw position on preoperative CT and found these measures to better predict screw loosening than any other vertebral CT HU measurement. They concluded that using specific CT measures of bone density will reduce the risk of screw loosening and their complications in future patients.[18] Zaidi et al found that CT HU, when compared to DEXA BMD values, correlated with successful lumbar interbody fusion, cage subsidence, adjacent segment fractures, and pedicle screw loosening.16 As a result, CT HU could be a promising measure of bone density.
St. Jeor et al conducted research regarding CT HU to propose a more comprehensive “expanded spine” criteria to refine the classification of spine surgery patients with potentially low bone density.[19] The expanded spine criteria diagnosed osteoporosis on the basis of a CT HU score less than 110 and/or the National Bone Health Alliance (NBHA) guidelines and/or degraded DEXA trabecular bone scores with osteopenic T-score. Retrospectively applying the expanded spine
criteria to lumbar spine surgery patients, the authors found that 70.4% of patients with normal or osteopenia DEXA BMD scores were reclassified with osteoporosis. The expanded spine criteria may be especially useful for patients of older age, as men and women older than 70 years were more frequently classified with osteoporosis based on the CT HU criteria than via DEXA or NBHA.
Quantitative computed tomography (QCT) is a specialized CT scan that transforms the CT signal in HU based on a calibration phantom using an analytical software.[20] Due to the ability of the QCT to separate cortical from trabecular bone, which is a known shortcoming of DEXA, some physicians have ordered QCT to assess bone quality.[21] Lin et al used a QCT-derived volumetric BMD to compare against DEXA T-score values in an older population, finding that QCT was more helpful than DEXA for detecting osteoporosis and predicting vertebral fractures.[22]
MRI VBQ Lumbar Measurements
A number of studies have tested MRI VBQ as a measure of lumbar bone density. Ehresman et al found that MRI VBQ is an important piece of information in order to assess risk for instrumentation failure.[23] Similarly, Roch et al found that VBQ is significantly correlated with CT bone quality values, although they used a different equation for VBQ measurements. 24 Cutoffs for MRI VBQ are also still debated, but lower scores indicate normal bone (<2.41) and greater scores indicate osteoporotic/osteopenic bone quality (>3.0).[25,26]
Kadri et al identified a VBQ threshold above which patients should undergo screening for osteoporosis,[25] and Hu et al reported an association between VBQ and cage subsidence after transforaminal lumbar interbody fusion.[27] Kale et al found a moderate correlation between their measure of VBQ and DEXA, which is consistent with some previously established literature.[28,29] They concluded that this MRI measure has the potential to be a predictor of decreased bone density, specifically pertaining to higher VBQ values.
In a recent study, Courtois et al compared lumbar MRI VBQ and CT HU scores to DEXA BMD scores and found that MRI VBQ scores had a much weaker correlation with DEXA than CT HU composites scores.[14,30] This study also used receiver operating characteristic area under the curve analyses to discern that CT HU demonstrated a greater ability to differentiate patients between normal and osteopenic/osteoporotic bone than MRI VBQ. Thus, CT HU may be a more reliable measure for lumbar bone mineral density compared to MRI.
Additional Applications: Lumbar Periendplate or Pedicle Measurements
Additional applications using CT HU, QCT, and MRI VBQ have recently been proposed such as at the lumbar endplate or the anticipated pedicle screw trajectory. These other methods may be used to help evaluate complication risks.
Cage Subsidence
Using QCT, Okano et al measured lumbar endplate bone density to assess the risk of subsidence and determined that endplate measurements were a better predictor of subsidence than trabecular bone density measurements after standalone lateral lumbar interbody fusions.[31] Jones et al found this to be congruent with their study, noting that significantly elevated endplate measurements using MRI was predictive of severe cage subsidence after the same lumbar procedure.[3]
Pedicle Screw Loosening/Pullout
Numerous studies have linked low HU values from CT pedicle screw bone density measurements with increased levels of pedicle screw loosening or pullout.[18,32-34] These studies confirmed that low bone density predisposes patients to pedicle screw pullout and also showed that this method of measuring bone density using alternative imaging techniques may aid in additional screening prior to lumbar instrumentation. Ishikawa et al described a method of measuring S1 pedicle screw trajectory bone density on CT and its ability to predict screw loosening six months postoperatively.[35] This method defined the HU region of interest (ROI) as a rectangular box where the screw was to be placed intraoperatively, and the authors concluded that lower CT HU correlated with screw loosening, suggesting that pedicle screws be placed in an area of the bone with high HU values. Another study examining the S1 pedicle screw trajectory bone density using MRI instead of CT and concluded that VBQ scores moderately correlated with DEXA T-scores and could be a beneficial tool to utilize in addition to the DEXA report.[36]
In some cases, especially if there is a concern for artificially increased DEXA values, utilizing these other techniques may provide more bone quality information prior to spinal surgery.
Conclusion
Recently, a number of alternative techniques have emerged to measure spine bone density in an effort to address the shortcomings of DEXA. Despite a number of studies comparing these methods, there is an overall lack of standardization within spine surgery. Some studies would argue that CT seems more closely correlated than MRI with DEXA BMD, while other studies found VBQ to be an adequate tool for assessing osteoporosis.[8,23,25]
Complimenting DEXA with alternative methods for measuring bone density prior to spinal instrumentation surgeries may lead to less hardware-related complications. The continued development of this field of study will aid spine surgeons in their decision-making process.
References
1. Bertagnoli R, Zigler J, Karg A, Voigt S. Complications and strategies for revision surgery in total disc replacement. Orthop Clin North Am. 2005;36(3):389-395.
2. Ouyang H, Hu Y, Hu W, et al. Incidences, causes and risk factors of unplanned reoperations within 30 days of spine surgery: a single-center study based on 35,246 patients. Spine J. 2022;22(11):1811-1819.
3. Jones C, Okano I, Arzani A, et al. The predictive value of a novel site-specific MRI-based bone quality assessment, endplate bone quality (EBQ), for severe cage subsidence among patients undergoing standalone lateral lumbar interbody fusion. Spine J. 2022;22(11):1875-1883.
4. Soliman MAR, Aguirre AO, Kuo CC, et al. Vertebral bone quality score independently predicts cage subsidence following transforaminal lumbar interbody fusion. Spine J. 2022;22(12):2017-2023.
5. Sakai Y, Takenaka S, Matsuo Y, et al. Hounsfield unit of screw trajectory as a predictor of pedicle screw loosening after single level lumbar interbody fusion. J Orthop Sci. 2018;23(5):734-738.
6. Link TM. Osteoporosis imaging: state of the art and advanced imaging. Radiology. 2012;263(1):3-17.
7. Krugh M, Langaker MD. Dual-Energy X-Ray Absorptiometry. StatPearls Publishing LLC; 2023.
8. Kim AYE, Lyons K, Sarmiento M, Lafage V, Iyer S. MRI-based score for assessment of bone mineral density in operative spine patients. Spine. 2023;48(2):107-112.
9. Ahmad A, Crawford CH III, Glassman SD, Dimar JR II, Gum JL, Carreon LY. Correlation between bone density measurements on CT or MRI versus DEXA scan: a systematic review. N Am Spine Soc J. 2023;14:100204.
10. Courtois EC, Satin AM, Rogers-LaVanne MP, Derman PB. Lumbar bone density measurements: using CT and MRI scans as alternatives to DEXA. Vertebral Columns. Summer 2023:16-19.
11. Viswanathan VK, Shetty AP, Rai N, Sindhiya N, Subramanian S, Rajasekaran S. What is the role of CT-based Hounsfield unit assessment in the evaluation of bone mineral density in patients undergoing 1- or 2-level lumbar spinal fusion for degenerative spinal pathologies? A prospective study. Spine J. 2023;23(10):1427-1434. doi:10.1016/j.spinee.2023.05.015
12. Kohan EM, Nemani VM, Hershman S, Kang DG, Kelly MP. Lumbar computed tomography scans are not appropriate surrogates for bone mineral density scans in primary adult spinal deformity. Neurosurg Focus. 2017;43(6):E4.
13. Kim KJ, Kim DH, Lee JI, Choi BK, Han IH, Nam KH. Hounsfield units on lumbar computed tomography for predicting regional bone mineral density. Open Med (Wars). 2019;14:545-551.
14. Courtois EC, Ohnmeiss DD, Guyer RD. Assessing lumbar vertebral bone quality: a methodological evaluation of CT and MRI as alternatives to traditional DEXA. Eur Spine J. 2023;32(9):3176-3182.
15. Yaprak G, Gemici C, Seseogullari OO, Karabag IS, Cini N. CT derived Hounsfield unit: an easy way to determine osteoporosis and radiation related fracture risk in irradiated patients. Front Oncol. 2020;10:742.
16. Zaidi Q, Danisa OA, Cheng W. Measurement techniques and utility of Hounsfield unit values for assessment of bone quality prior to spinal instrumentation: a review of current literature. Spine. 2019;44(4):E239-E244.
17. Murata K, Fujibayashi S, Otsuki B, Shimizu T, Matsuda S. Low Hounsfield unit values at sagittal section on computed tomography predicts vertebral fracture following short spinal fusion. J Orthop Sci. Published online March 21, 2023. doi:10.1016/j.jos.2023.03.008
18. Li J, Zhang Z, Xie T, Song Z, Song Y, Zeng J. The preoperative Hounsfield unit value at the position of the future screw insertion is a better predictor of screw loosening than other methods. Eur Radiol. 2023;33(3):1526-1536.
19. St Jeor JD, Jackson TJ, Xiong AE, et al. Osteoporosis in spine surgery patients: what is the best way to diagnose osteoporosis in this population? Neurosurg Focus . 2020;49(2):E4.
20. Link TM, Lang TF. Axial QCT: clinical applications and new developments. J Clin Densitom. 2014;17(4):438-448.
21. Adams JE. Quantitative computed tomography. Eur J Radiol. 2009;71(3):415-424.
22. Lin W, He C, Xie F, et al. Discordance in lumbar bone mineral density measurements by quantitative computed tomography and dual-energy X-ray absorptiometry in postmenopausal women: a prospective comparative study. Spine J. 2023;23(2):295-304.
23. Ehresman J, Ahmed AK, Lubelski D, et al. Vertebral bone quality score and postoperative lumbar lordosis associated with need for reoperation after lumbar fusion. World Neurosurg. 2020;140:e247-e252.
24. Roch PJ, Çelik B, Jäckle K, et al. Combination of vertebral bone quality scores from different magnetic resonance imaging sequences improves prognostic value for the estimation of osteoporosis. Spine J. 2023;23(2):305-311.
25. Kadri A, Binkley N, Hernando D, Anderson PA. Opportunistic use of lumbar magnetic resonance imaging for osteoporosis screening. Osteoporos Int. 2022;33(4):861-869.
26. Ehresman J, Schilling A, Yang X, et al. Vertebral bone quality score predicts fragility fractures independently of bone mineral density. Spine J. 2021;21(1):20-27.
27. Hu YH, Yeh YC, Niu CC, et al. Novel MRI-based vertebral bone quality score as a predictor of cage subsidence following transforaminal lumbar interbody fusion. J Neurosurg Spine . Published online May 13, 2022. doi:10.3171/2022.3.Spine211489
28. Kale H, Yadav S. Can routine MRI spine T1 sequences be used for prediction of decreased bone density? Acta Radiol. 2023;64(1):164-171.
29. Li W, Tong T, Zhu H, et al. Hounsfield units value is a better predictor of bone mineral density than the vertebral bone quality score of magnetic resonance imaging in patients with lumbar degenerative diseases. Research Square Preprint posted online January 3, 2022. doi:10.21203/rs.3.rs-1110968/v1
30. Zou KH, Tuncali K, Silverman SG. Correlation and simple linear regression. Radiology. 2003;227(3):617-22.
31. Okano I, Jones C, Salzmann SN, et al. Endplate volumetric bone mineral density measured by quantitative computed tomography as a novel predictive measure of severe cage subsidence after standalone lateral lumbar fusion. Eur Spine J. 2020;29(5):1131-1140.
32. Xu F, Zou D, Li W, et al. Hounsfield units of the vertebral body and pedicle as predictors of pedicle screw loosening after degenerative lumbar spine surgery. Neurosurg Focus . 2020;49(2):E10.
33. Chen Z, Lei F, Ye F, et al. Prediction of pedicle screw loosening using an MRI-based vertebral bone quality score in patients with lumbar degenerative disease. World Neurosurg. 2023;171:e760-e767.
34. Wichmann JL, Booz C, Wesarg S, et al. Quantitative dual-energy CT for phantomless evaluation of cancellous bone mineral density of the vertebral pedicle: correlation with pedicle screw pull-out strength. Eur Radiol. 2015;25(6):1714-20.
35. Ishikawa Y, Katsumi K, Mizouchi T, Sato M, Yamazaki A. Importance of computed tomography Hounsfield units in predicting S1 screw loosening after lumbosacral fusion. J Clin Neurosci. 2023;113:1-6.
36. Huang W, Gong Z, Wang H, et al. Use of MRI-based vertebral bone quality score (VBQ) of S1 body in bone mineral density assessment for patients with lumbar degenerative diseases. Eur Spine J. 2023;32(5):1553-1560.
Authors: Emily C. Courtois, MS
Mary P. Rogers-LaVanne, PhD
Peter B. Derman, MD, MBA
Alexander M. Satin, MD
From the Texas Back Institute in Plano, Texas.










