How to reduce the risk of choking
General advice to help someone eat and drink safely and reduce their risk of choking

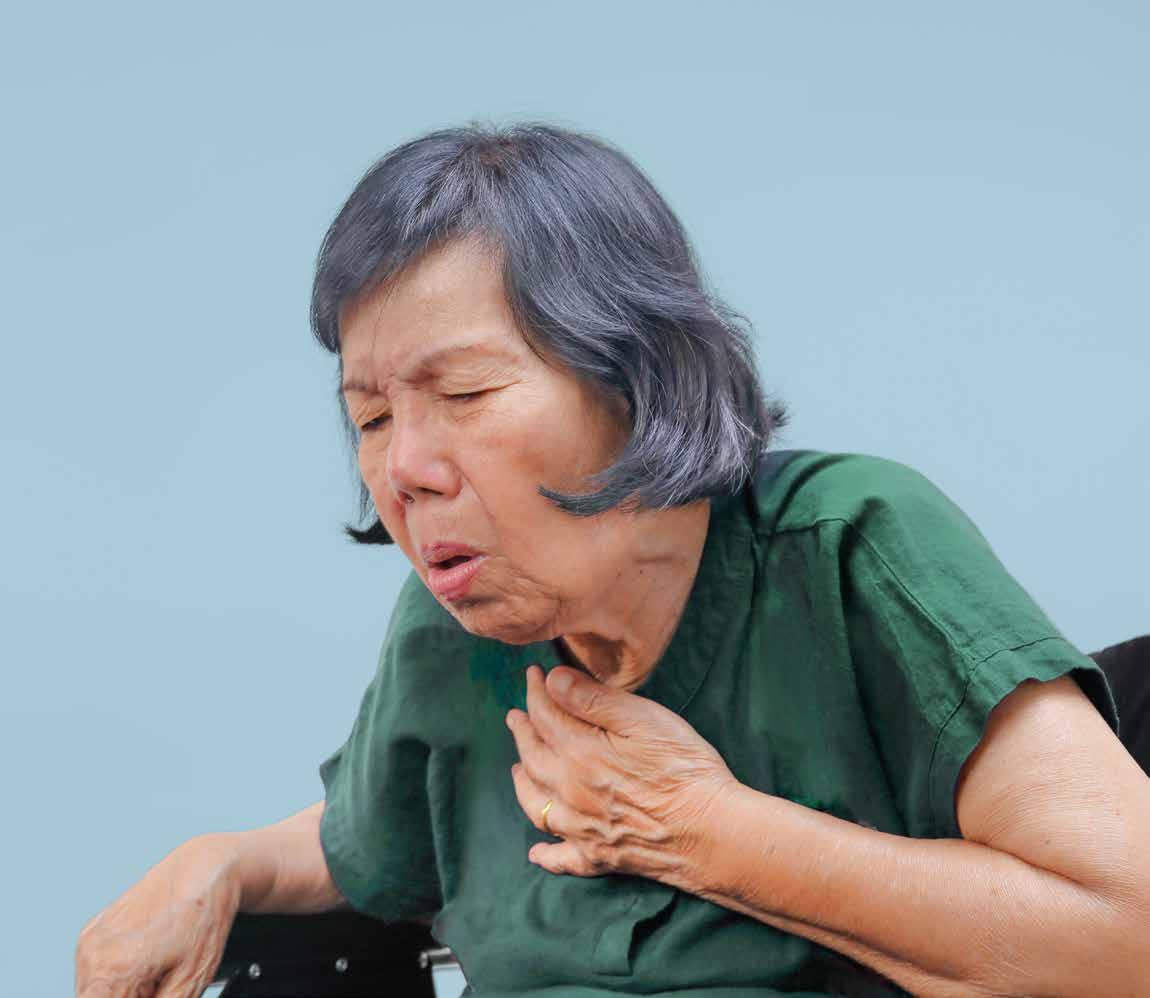
Anyone can choke at any time. The risk of choking increases when someone is eating or drinking.
“Choking happens when someone’s airway suddenly gets blocked, either fully or partly, so they can’t breathe or breathe properly… If the airway is partially blocked, the person will usually be able to speak, cry, cough or breathe… When choking is severe, the person won’t be able to speak, cry, cough or breathe. Without help, they’ll eventually become unconscious.
(NHS, online, 2022)
At Iris Care Group we promote safe eating and drinking throughout all our services. We know from research that people with swallowing difficulties and/or learning disability have a further increased risk of choking. For example, every year people with a learning disability die from choking. In a lot of these cases, death is likely to have been preventable (Hampshire Safeguarding Adults Board, online, 2012).
Everyone is at risk of choking and it is important that all staff are aware and implement safe swallow strategies when supporting people to eat and drink as safely as possible.
It is important that information on choking is discussed with staff in supervisions and included on risk assessments. Training on choking will also be provided through eLearning and as part of First Aid training.
We know that many of the people we support require ongoing support to recognise and/or understand the health and safety aspects of eating and drinking and the risks of choking (e.g., the amount of food placed in their mouth at a time, the temperature of the food, the rate of intake and presence of inedible items). Some individuals may also rely solely on support from staff to encourage and remind them of safe swallow strategies.
It is important to ensure that people who have identified swallowing difficulties (dysphagia) or who are at a risk of choking are supported by staff when eating and drinking and appropriate eating and drinking plans/PBS plans and safety and support plans are followed.
If the person has an Eating and Drinking care plan (written by the Speech and Language Therapy team following an assessment of the person’s swallow), they may have been recommended a texture modified diet or prescribed thickened fluids (International Dysphagia Diet Standardisation Initiative). Food and drink needs to be prepared in line with the care plan. Instructions on how to prepare thickened fluids can be found on the tin. It is important that fluids are prepared in a specific and accurate way if prescribed thickener.
Incidents of choking must be recorded and reported as soon as possible. Training on what to do when a person chokes is available via the Learning and Development Department. Training around specific swallowing difficulties (dysphagia) is available via the Speech and Language Therapy team.
Below are some safe swallow strategies that can help reduce the risk of a person choking. Look at the list of ‘risks’ in the left side of the table and consider the ideas on the right side to help reduce the risk.
What is the problem?

Person is easily distracted

Person is unable to maintain a stable and upright position while eating
Ideas to consider to help reduce the risk of choking
• Supervise the person when they are eating and drinking.
• Promote a calm, quiet and relaxed environment.
• Reduce distractions (e.g., turn TV off, clear the table from unnecessary clutter).
• Consider eating at quieter times (e.g., when less people are in the room).
• Serve one course at a time (e.g., if the person is distracted by dessert, place this on the table once the previous course has finished).
• Supervise the person when they are eating and drinking.
• Support the person to sit as upright as possible with their feet on the floor and buttocks towards the back of the seat. Do the same if the person uses a wheelchair and utilise the wheelchair tray as needed.
• Do not let the person eat or drink while lying down.
• If the person needs to eat or drink in bed, ensure that they are supported to be as upright as possible. Adjustments may need to be made if they use a profile bed.
• Encourage the person to remain seated whilst eating and drinking.
• Encourage the person to remain upright for approx. 30 minutes after eating or drinking as food/drink may fall into their airway.
• Consider a referral to Occupational Therapy for a seating assessment.
What is the problem?

Ideas to consider to help reduce the risk of choking
• Supervise the person when they are eating and drinking.
• Support the person to cut the food up into bite sized pieces (1.5cm x 1.5cm).
• Use smaller utensils (e.g., teaspoon rather than tablespoon).
• Offer to help the person remove excess food from the fork/spoon.
• Offer to load the spoon/fork for the person. This can be done hand over hand if appropriate.
• The person may have a visual difficulty and is unable to see how much they are putting on their fork/spoon. Ensure glasses are worn if prescribed and that they are clean. Consider using a plain coloured plate.
• Remember that lots of small mouthfuls without swallowing is just as dangerous as one large mouthful. Encourage the person to swallow in between mouthfuls.
• Consider a referral to Occupational Therapy for an independent feeding skills assessment if the person has difficulty cutting up their food or putting food onto their fork/spoon.
What is the problem?

Ideas to consider to help reduce the risk of choking
• Supervise the person when they are eating and drinking.
• Remove the need to rush by allowing plenty of time to eat before activities, trips out, etc.
• Demonstrate a slow pace of eating.
• Encourage the person to chew their food properly before swallowing it.
• Agree on a single word or phrase that everyone will use to prompt the person to slow down (e.g., ‘steady,’ ‘slow,’ ‘slowly’). Support this using non-verbal means if needed (e.g., Makaton, gestures).
• Encourage the person to take regular sips of fluids throughout the meal.
• Place a small amount of food on the plate at a time, or a small amount of fluid in a cup at a time.
What is the problem?

Talking
when eating and drinking

Moving around when eating and drinking
Ideas to consider to help reduce the risk of choking
• Supervise the person when they are eating and drinking.
• Discourage talking when swallowing. Talk before, after or in between courses. Mealtimes can still be social. If the person wants to talk, encourage them to swallow what is in their mouth first.
• Don’t be tempted to start a conversation yourself.
• Don’t give any prompts that require an answer when the person is eating and/or drinking.
• Supervise the person when they are eating and drinking.
• Encourage the person to remain seated when eating and drinking. Staff should do the same.
• Make sure everything is available to the person before they sit down to eat and drink (e.g., the drink, meal, cutlery, napkin, any sauces, any specialist equipment).
• Reduce distractions in the environment.
What is the problem?

Swallows food without adequate chewing (no dentition, ill fitted dentures, limited dentition, broken/ missing dentition)
Ideas to consider to help reduce the risk of choking
• Supervise the person when they are eating and drinking.
• Soft, moist foods are generally easier to swallow.
• Consider adding sauces to dry foods to make them easier to chew.
• Ensure dentures are fitted correctly.
• Be aware of high risks foods (see page 9) as these can increase the risk of choking.
• If a person is not managing their current diet, consider a referral to Speech and Language Therapy for a dysphagia assessment.
• Consider a referral to the dentist/oral hygienist.
What is the problem?

Person is drowsy, sick, upset or agitated

Ideas to consider to help reduce the risk of choking
• Supervise the person when they are eating and drinking.
• If the person gets sick, it can cause a sudden change in their eating and drinking, discuss with the GP.
• It is important that the person is fully alert while eating and drinking so they can swallow as safely as possible. Encourage them to eat and drink when they are most alert and at their best.
• Check side effects of medication and discuss with prescriber (e.g., some medications can cause a dry mouth which may impact the person’s ability to swallow safely).
• Give the person gentle prompts to draw their attention to the food and/or drink.
• Consider offering the meal at a later time.
• Supervise the person when they are eating and drinking.
• Be aware of the person’s diagnoses and how these can/may present (e.g., COPD, asthma).
• Encourage the person to visit their GP to investigate any concerns.
• If the person is showing difficulty breathing whilst eating and/or drinking, encourage them to stop and recover before continuing.
• Consider a referral to Physiotherapy for advice.