











































































































































































































































































A step in the right direction Podiatry Review The Institute of Chiropodists and Podiatrists News SPRING ISSUE Volume: 79 No: 2 Apr/May/Jun 2022 The Institute of Chiropodists and Podiatrists FREE 4 Page CPD Article Principles of Gait: Creating the Lever for Acceleration Products & Procedures under the microscope - UREA Pages 19 - 22 Pages 24 - 26 SafeTPen ™ Exciting New Product launch Pages 10 -13 Pages 30 - 34 Anatomy in Motion (AiM)

Podiatry Review
Published by The Institute of Chiropodists and Podiatrists

150 Lord Street Southport
Merseyside PR9 0NP
Tel: 01704 546141 Email: info@iocp.org.uk Website: www.iocp.org.uk
Editor: Andrew Williams, MInstChP, CFPodM
Academic Editor: Martin Harvey, PGCert, BSc, MInstChP, MCPodS
Academic Advisor: David M Holland, BSc, CSci, FFPM - RCPS(Glasg).
No:
Academic Review Team
Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP
Mr S Miah, CFPodM, MInstChP
Mr A Williams, MInstChP, CFPodM
Media and Publicity Contact: Doctor Bharti Rajput, MBE PhD
Email: media@iocp.org.uk
Medicines and Procedures Panel (MaPP)
Chair: Gaynor Wooldridge, MInstChP, CFPodM
Andrew Williams, MInstChP, CFPodM
Abid Ali, CFPodM, BSc, MInstChP
Somuz Miah, CFPodM, MInstChP
Martin Harvey, PGCert, BSc, MInstChP, MCPodS

Contents
Podiatry Review Spring Apr/May/Jun 2022
Volume: 79
2 ISSN 1756-3291 Annual Subscription £20 UK / £30 Overseas
© The
Disclaimer:
CONTACTS 4 IOCP Contacts 5 Editorial ARTICLES 6 5 minutes with your CEO 9 2022 Mid Wales Diary 10-13 SafeTPen™ New Product Launch 14-16 Footnotes: Foothealth Practitioner News 17 Obituary:
18 Fellowship Awards 19-22
24-26 Products
28-29
30-34
35 Obituary:
COURSES 7 Dermal Filler & Podriatric Ultrasound NEWS 37 Branch News 38 Classified Adverts 39 Diary of Events 24-26 @IOCP_Chiropody @IOCPChiropody Podiatry Review Spring Issue 2022 | 3 10-13 30-34
Institute of Chiropodists and Podiatrists
The Editor and the Institute of Chiropodists and Podiatrists accept no responsibility for any opinions expressed in the articles published in the journal, and they do not accept any responsibility for any discrepancies in the information published. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying or otherwise, without the prior written permission of the publishers.
Arthur George Holland
4 page CPD articlePrinciples of Gait: Creating the Lever for Acceleration
and Procedures under the microscope: Urea - the magic substance?
IOCP AGM - Nominations
AiM - an introduction
Colin J. Craig
IOCP Contacts
Executive Committee
President: Mrs L Pearson, FInstChP, BSc Pod Med
Chair Executive Committee: Mr M Harvey, PGCert, BSc, MInstChP, MCPodS
Vice-Chair Executive Committee: Mr A Ali, CFPodM, BSc, MInstChP, BSc
Chair Board of Education: Mr A Williams, BSc(Hons), CFPodM, FFPM RCPS(Glasgow)
Vice-Chair Board of Education: Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP
Chair Board of Ethics: Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP
Honorary Treasurer: Mr S Miah, CFPodM, BSc (PodM), MInstChP
Regional Director (Ireland): Mr S Preston, MInstChP
Regional Director (Scotland): Mrs H Jephcote, MInstChP Regional Director (England North): Mrs C McCartney, MInstChP Regional Director (England Midlands): TBC
Regional Director (England South): Ms B Wright, MSc BSc (Hons), PGCE PGDip, FInstChP Regional Director (Wales): Mrs L Pearson, FInstChP, BSc Pod Med`
Academic Advisor: David M Holland, BSc, CSci, FFPM-RCPS(Glasgow)
Medicines and Procedures Panel (MaPP): Gaynor Wooldridge, MinstChP, CFPodM Chief Executive Officer: Mr Anthony Hubbard, CSci CChem FRSC
Company Secretary: Miss A J Burnett-Hurst, HonFInstChP Standing Orders Committee: Mr M Franklin, MInstChP Birmingham
Branch Secretary Telephone Email
4 | www.iocp.org.uk CONTACTS
& the Shires
Harrison
Cheshire & North Wales Michele Allison
700027
Essex Beverley Wright 01702 460890
Leeds Caroline McCartney 07583 934468
Irish Janette Pegley-Reed 00353 8627 31371
Sarah Bowen 07790 717833
West
Marsden
Wales &
135 6485
716607
Kate
01789 612959 kathrynharrison87@gmail.com
07766
missminou@hotmail.co.uk
solespirits@hotmail.com
hello@chiropodyandfoothealth.co.uk
jpegleyreed@gmail.com London
footwoman@gmail.com North
Alison
01772 623180 alison.marsden@hotmail.com Sheffield Helen Rawse 07789 025022 hrawse@live.co.uk South
Monmouth Esther Danahar 01656 740772 estherdanahar@yahoo.co.uk Scottish John Stott 0780
jls@stottland.com Wolverhampton David Collett 01785
djcollett@hotmail.co.uk
(Acting secretary of)
Branch Secretary Contacts
Dear Colleagues














Welcome to the spring issue of the Podiatry Review which again is full of interesting and thoughtprovoking material. It is always satisfying to see a wide contribution of articles from both regular and new authors. The diversity of material from biomechanics to the use of urea in clinical practice indicates the wealth of knowledge available within our profession.
















We are finally moving from restrictions of the global covid pandemic and hopefully we can now look forward to more face-to-face contact with our patients and colleagues. I have continued to provide occasional remote consultations with patients but virtual meetings with colleagues although vital, has never been as conducive as direct social interaction. Our CPD program planned for the forthcoming year as well as our AGM at the Primary Care meeting in May is testimony to that. I would welcome as many of you to attend that meeting and be active as possible at the AGM. The Institute of Chiropodists and Podiatrists are a truly democratic organisation, and we need as much in interaction with members as possible.





On this note I would like to discuss the use of professional terms within our organisation, namely, Chiropodist and Podiatrist. We get on occasion members and individuals outside of the organisation querying the continued use of the title Chiropodist. I have attended several branch meetings where there has been quite a significant majority wanting to continue with its use. This is mainly because patients are still familiar with this term and in some members the term Podiatrist is seen as a more advanced practitioner.











I must say my own position has flip flopped over past years but I do feel quite strongly that it should be kept. The term is a protected title after all. I qualified from Northampton in 1988 and my diploma was in Chiropody but obtained a BSc in Podiatry as a top up a year later with diplomas being phased out during this time. It is also true that other organisations within the Podiatry arena have dropped the title but it is a fact that our patients, particularly the elderly, continue to relate to this title and may impact on potential business if withdrawn. However, on the democratic aspect of our organisation I think it’s time for this to be discussed and the membership to decide. I would welcome any thoughts direct to me or the board on this important matter. In conclusion, let me have your thoughts and hopefully we can have good democratic discourse at the AGM. Hopefully we can continue to have your contributions to the journal and welcome any thoughts on CPD for the future.
Stay safe.




















































































































































 Andrew Williams Chair Board of Education
Andrew Williams Chair Board of Education
Guidelines for new and established authors






































































































Content of your article should be Podiatry or foot health-related. Podiatry Review is mostly in easy-to-read format, and articles for submission should reflect this. CPD Certificates are issued for Case Studies and Articles. Please ensure that your name and title (ie - FHP, Podiatrist, or other) are included with your article. Please proof-read and spell-check your article before submission. It would be helpful to the Editorial Committee if you could reference any books or Papers mentioned in your article. If you are not sure how to do this we are happy to assist.

Podiatry Review Spring Issue 2022 | 5 Editorial
Executive Officer
Having met and worked with the Head Office team, I can see the hard work that goes into adding a very personal touch to looking after our members. We have a very passionate and enthusiastic crew who provide the base from which we can grow.
It is very encouraging to hear the number of new people that are contacting us for our FHP course; listening to the reasons why they are coming to the Institute for training tells me that we are doing all the right things. We are really making a difference and adding value to education through the type of training and support that we are offering, and we are looking to improve that throughout 2022.
We are also in the process of extending our lease for 150 Lord Street, to further develop that as our HQ and our clinical training base and are working to add new tutors to our team to provide more training. It is quite exciting to see the people who are passionate about developing others that we are working with.
I am extremely delighted to let you know that we are looking at building our members knowledge beyond conventional podiatry, moving us firmly in to new areas of treatment; we will be doing this with a leading foot and leg health clinician who is making a big difference in our industry. Afni Shah-Hamilton is a pain management specialist, who focuses on the biomechanics of the entire body. Afni has helped a large number of patients with unresolved (or in some cases previously undetected) problems with the toes, foot
Two months into the role and the excitement grows!
or ankle that were causing long term knee, hip, back or neck pain. Afni also has a keen interest in the role of podiatry in cancer treatment and this is reflected in the fact she sits on the Macmillan Cancer Support Allied Health Advisory Board and are delighted to welcome Afni as the IOCP lead for cancer care in podiatry. She brings a wealth of knowledge and experience to our educational offer and will be working with us to develop our members knowledge and skills as we ask her to Chair an education working group entitled ‘Advancing IOCP Education’.
Tremendous work by Gaynor!
It has also been good to start to get to know the Executive Team better and to be working with them as our leadership team; we are starting to build a longterm development plan which will focus on furthering education, enabling networking and providing business support and advice for our members.
On a final note for this month, it is also very pleasing to see that we have three people standing for the President’s role this year, showing the growing level of interest and pride in our organisation. May I take this opportunity to wish Bill, Caroline and Linda all the very best in the election and to ask you, our members to take the time to vote for your preferred candidate.
It is also very pleasing to report that we have been heavily involved in developing an innovative new product for podiatry;

As you are aware bottles of liquified Phenol were the subject of an NHS elimination notice due to a number of incidents relating to spills and injury. This caused some concern for many members who regularly use the product for nail surgery. Gaynor Wooldridge, Chair of Medicines for the IOCP, immediately recognised this concern and began investigating and exploring other safe alternatives.
Gaynor has worked alongside a fantastic team at Canonbury to review the SafeTPen and we are delighted to have been part of the product development process and the first podiatry body to endorse the product.
Within the next twelve months, you will be seeing a lot of activity which I hope will also provide the stimulus for more of you to get involved in our Institute, either at branch, regional or national level. It is a great time and a great opportunity to get involved and make a difference for the IOCP.
I will be at the NEC event and also at the AGM. If you are going to be there in person and would like to have chat, you can either look out for me there or contact me to book a time for a chat on our stand. Otherwise, you can always email me on anthony@iocp.org.uk
6 | www.iocp.org.uk ARTICLE
Keep putting your best foot forward, explore new ground and enjoy the journey!
We are really making a difference
‘‘ ‘‘
Chief
Anthony Hubbard CSci CChem FRSC



Podiatry Review Spring Issue 2022 | 7 Podiatric Ultrasound (Imaging) Date: Saturday & Sunday, 18th and 19th June 2022 Time: 8.45am - 5.15pm both days Location: The Wiggin Training Centre at Sir Robert Peel Hospital, Mile Oak, Tamworth B78 3NG TUTORS: Consultant MSK Podiatrist Mr Abid Ali, CFPodM, MFPM RCPS(Glasg) Adrian Burman - BSc (Hons), PGDip, PGCert COST: Theory only (online) Members £150 Non-Members £175 Theory and Practical Members £550 Non-Members £625 *Sponsored by COURSES These courses are all approved and certified by The Institute of Chiropodists and Podiatrists Course places are limited -For further info phone Sam on 01704 790405 or email: sam@iocp.org.uk Go to www.iocp.org.uk/courses-events/ to book your place
The aim of the programme is to educate and train suitably qualified Podiatrists in the safe and competent use of basic diagnostic ultrasound imaging for musculoskeletal conditions. Dermal Filler of the Feet Course Date: Saturday 23rd April 2022 Time: 9.00am - 5.00pm Location: The Institute of Chiropodists and Podiatrists Training Centre, 150 Lord Street, Southport, Merseyside PR9 0NP TUTORS: Martin Harvey - FPodM, MCPodS PGC IP BSc Somuz Miah - CFPodM, BSc (PodM), Cert HTox, Dip Sp.I, PGCE IP, MFPM RCPS (Glasg) COST: Members £365 Non-Members £425
COURSE You are encouraged to bring a patient of along to the afternoon practical for free treatments by delegates, these appointments need to be pre-booked with Head Office as soon as possible, phone Sam on 01704 790405 to pre-book. This course is open to all podiatrists with POM-A Maximum 10 delegates
COURSE AIM
ABOUT THE
• Network through local member branches, situated throughout the United Kingdom and the Republic of Ireland for peer support and CPD events
We’ve teamed up with Community, a modern trade union you can choose to opt into! Offering additional industry support, advice, and training.
Members also receive discounted rates on health plans from the Health and Medical Care Association (HMCA)


Head to our website: www.iocp.org.uk or contact our team: info@iocp.org.uk
our growing podiatry
become a member Run by members for the members! We are a truly democratic organisation where your voice is heard. We strongly believe in working together to build a stronger future for podiatry
Support
The Institute of Chiropodists and Podiatrists are proud to offer our members comprehensive, market leading support and unrivalled insurance packages, tailored to suit your needs! Including insurance to colleagues in the Republic of Ireland, we’ll never leave you stranded! Join
family -
• Quarterly issues of Podiatry Review, contributing to your Professional Development
• Continuing Professional Development Support – Guidance and assistance with the members continuing professional development portfolio for HCPC audits & 20% discount on Elsevier academic books • Business Support and special discounts from our trade and advice partners • Access to the members area of the Institute website including a private discussion forum • Member rates on all our CPD courses and access to our free CPD webinars!
• Join the IOCP ‘Find a practitioner’ service to promote your business to members of the public finding the IOCP website through search engines.
• Access our confidential advice service, including advice from the IOCP medicines and procedures panel (MaPP) on the use of drugs and therapeutics as well as appropriate podiatric procedures.
8 | www.iocp.org.uk
PLUS…
Mid Wales Diary
David Holland BSc(Hons) Pod-Med, CBiol, CSci, FFPM-RCPS(Glasg).

2021 was a busy year for me. Work carried on at a slightly slower pace than in 2020 - good thing too! I finally submitted a paper to The Foot - a peer-reviewed journal which enjoys a multi-profession international readership, and we should be in print this year - open-access too. My co-author is a widely-published PhD, and Honorary Research Associate at the Institute for Human Evolution at the prestigious University of Witwatersrand of South Africa.
Things have been moving apace at Wyvern. As I write this, on December 18th, the river has already been into the garden. This is normally a January incursion. Sign of things to come for 2022 perhaps? Otherwise the upstairs interior at Wyvern is almost complete, and Alison has designed and prepared, with some professional help, a new bed in the back garden for fruit trees and shrubs.
As you read this, it’s well worth remembering that Spring is just around the corner!

I came across two topics in late 2021 which may be of professional interest to the readership:
The first concerns cocaine the street drug. There is little doubt that vast quantities of this drug are being used throughout the UK. I’m not about to moralise on this. I’ve never taken it myself, and I regard the taking of street drugs a matter of choice. I assume the consumer has weighed up all the pros and cons. After that, well, it’s up to them.
You may already be aware, whether Podiatrist or FHP, that cocaine can initiate vascular disease. This includes accelerated atherosclerosis (1) which I didn’t previously realise. It can affect seemingly healthy young people I’ve just given a medicolegal opinion on such a case. The Podiatrist in question made an assumption about health and circulatory status based on the patient’s age and lifestyle. The patent (now minus one of his legs from the knee down) neglected to mention a habitual cocaine use.
The second topic of interest equally important and much more uplifting is a possible answer to growing antibiotic resistance. We all know that antibiotics are necessary, but there is an acknowledged problem growing bacterial resistance. In 2018 it was estimated that approximately 28% of bacterial infections were resistant to antibiotics. By 2050 it is estimated this will rise to 40%, leading to an additional 10 million deaths a year world-wide.
One answer to antibiotic-resistant bacteria is naturallyoccurring nanoscopic viruses called phages which can infect and kill bacteria. Phages have been used clinically since the early 1920’s. However their use nearly died out with the advent of antibiotics (2)
With phage therapy there is a need to isolate the infecting organism, then choose the phage which is specific in its action against that organism. Antibiotics can be applied fairly indiscriminately broad-spectrum antibiotics work against a host of bacteria, not just one type. There is also a commercial advantage to antibiotics after the very considerable cost of development they are easy to produce and market.
Exeter University is building up a library a phage biobank which, it is hoped, will eventually take the place of much antibiotic prescribing. The advantages of modern phage therapy over antibiotic therapy are clear:
Much lower development costs (hopefully under a commons licence, meaning the development cannot be patented for profit), much faster development, increased clinical safety (less side-effects than antibiotics), and most importantly an ability to mutate, as all viruses do, to overcome bacterial resistance. In addition, because phages target specific bacteria, the good bacteria those in the gut for example are unaffected. In some cases phage therapy can also be used in conjunction with antibiotic therapy.
However we do need the right phage for each infecting organism hence the need for a phage biobank.
Some newly-identified phages have weird and wonderful names (the phage discoverer can name their own phage)LemonAid discovered in the River Lemon in Devon specific against Acinetobacter baumannii, KylieMinegg - discovered in a chicken coop, and specific against Psudomonas aeruginosa a bug associated with Cystic Fibrosis.
Phages are natural - and everywhere. If you would like to learn more about the Exeter University phage project, or become a phage-hunter yourself (Exeter Uni will provide the kit) visit www.citizenphage.com.
REFERENCES
1. Keren Bachi et al. Vascular disease in cocaine addiction (2017) (open-access).
2. Ben Templeton. The hunt for ‘holes of hope’ in The Biologist, Vol 68 No 4. Winter 2021.
Podiatry Review Spring Issue 2022 | 9 ARTICLE
Product launch
Introducing the Phenol SafeTPen™
Since the publication of the article Phenol: past, present and future (Wooldridge, 2021) there has been a National Patient Safety Alert issued around the use of Liquid Phenol 80% (NHS 2021). The safety alert requires all bottles of multi-use Phenol with concentrations of 80% and above being removed from Podiatry clinics and safer alternatives to be sought for nail matrix ablation. The alert was published after 5 years of investigations into incidences which required some patients to be hospitalised.
 By
By
Nail pathologies make up a large part of a podiatrist’s workload, with 5% according to Moda and Latham (2016) being onychocryptosis. The requirements for the surgical removal of a toenail can have many aetiologies shape of the nail (involution, fan shaped); poor footwear causing pressure; teenager hyperidrosis; and the most common factor being poor cutting techniques by patients or carers (Moda and Latham, 2016; Institute of Chiropodists and Podiatrists (IOCP 2022)
See Figure 1
Figure 1 - Schematic illustration of the adolescent type of ingrown toe nail as cited in Haneke (2012)

Onychocryptosis can be presented at different stages to a podiatrist: Stage 1 often only requiring conservative treatment (e.g. packing, nail brace or gutter treatments), with Stage 2 to 4 often requiring surgery (Martínez-Nova, SánchezRodríguez, and Alonso-Peña, 2007) and Stage 4 is (where the skin from around the nail plate can cover the entire nail) requiring a Zadek’s procedure and referral to a Podiatric surgeon (Abbot, Maher and Wilkinson 2012).

See Figure 2
Figure 2 - Stage 1 – 3 of onychocryptosis
Eekhof et al., 2012)
Stage 2 and 3 can generally be managed with nail surgery and ablation within either NHS or private practice, as long as the suitably qualified Podiatrist has kept up to date with their local anaesthesia certificate, cardiopulmonary resuscitation and anaphylaxis training (IOCP 2022) (Royal College of Podiatrists RCoP2021).
The decision to remove the nail is often through the assessment of pain, reoccurring onychocryptosis, surgical relapse and failure of conservative treatment requiring the ablation of the nail matrix during surgery (Martínez-Nova, Sánchez-Rodríguez, Alonso-Peña 2007). This can be done as mentioned by Wooldridge (2021) and Eekhof et al., (2012) with phenolisation in conjunction with surgical removal of part or the whole nail; a Zadek’s; Vandenbos; or terminal Syme and Winograd procedures.
However Eekhof et al., (2012) concluded their report stating that phenolisation of the nail matrix combined with a surgical procedure to remove the nail was the preferred procedure, rather than purely a surgical procedure on its own. Following auditing of Phenolisation of the nail matrix it has been found that there is a minimal proportion of patients that report regrowth 1 year post op where the phenolisation has been carried out effectively (Eekhof et al., 2012; Kannegieter and Kilmartin, 2010).
Traditionally phenol has been applied through the decanting of phenol into a gallipot from a bottle, which leaves the practitioner and patient open to inhalation of the fumes, as well as possible spillage when decanting. Bottled phenol has the ability to take in the atmosphere’s moisture diluting its strength and reducing its reliability of its action as a nail ablation agent (RCoP, 2021). (RCoP 2021) T raining 30 years ago taught students to drop the phenol from an orange stick or dropper onto the blacks file within the nail sulci (IOCP 2022) and then to be rubbed in for 3 x 1 minute.
10 | www.iocp.org.uk
Michelle Gibson Training & Education Manager, Canonbury Products Ltd
Figure 3 – Galipot containing decanted phenol
Since this time practice has been adapted into using cotton wool tipped orange sticks. However, both of these methods require a careful hand when applying across the toe / foot from a clean field or the holding of the gallipot above the area of surgery and then delivery into the sulci, ensuring that the phenol doesn’t drip onto any other skin or seep under the tourniquet. Any drips onto the surrounding skin or seepage under the tourniquet could result in other tissue damage from a phenol burn.


Figure 4 - Traditional method of phenolisation
With all of this in mind, and the only available alternative safe phenol product available on the market being the Swab-it (EZ Swab), Canonbury Products Ltd are launching a safer alternative delivery device for nail ablation combined with phenolisation. Working in collaboration with practicing podiatrists and the Institute of Chiropodists and Podiatrists (IOCP) the SafeTPen™ was conceived.
What is it?
SafeTPen™ contains blue coloured 89% Phenol USP in a 0.4ml quantity for professional use during nail matrix ablation. SafeTPen™ comes with an 18 month shelf like, is registered with the MHRA as a Medical Device and is UKCA marked – the UK equivalent of the CE mark for Europe.


SafeTPen™ contains a glass ampoule within a plastic outer coating. Use of a glass ampoule was chosen to prevent evaporation of the phenol when stored as well as prevent absorption of moisture, thereby allowing the end user to be guaranteed to have 0.4ml of phenol at 89% to use during a partial or total nail avulsion. The glass ampoule and plastic outer is designed to prevent any splash back of phenol onto the practitioner, which can happen when piercing the membrane with other devices, or spillage through decanting prior to the procedure.
The decision was made to blend a blue dye with the phenol to make it more visible to the practitioner, allowing then to easily see if the tube has been damaged prior to use; to see where the phenol has been applied correctly; and, more importantly, if any phenol has been administered by mistake to the surrounding tissue, therefore reducing the potential burning of intact skin on the patient.
Podiatry Review Spring Issue 2022 | 11
Figure 5 - SafeTPen™ logo and SafeTPen™ device
Figure 4 shows leakage onto the base of the sulci during the application and figure 6 where the skin is white around the sulci post-phenol application.
Figure 6 - Post- phenolisation using the traditional method – 3 x 1minute applications
To use SafeTPen™ it is a quick “Snap, Snap and Squeeze” (figure 7) through snapping the 2 ends of the glass ampoule (proximal to distal) and a gentle squeeze of the plastic tube phenol is loaded into the compressed polyester tip of the device ready for use.

Once the tip has turned blue, you know it is impregnated with phenol (see Figure 8), a further gentle squeeze will allow phenol to be dropped from the tip.

Figure 8 SafeTPen™ ready for use
The compressed polyester was chosen for the tip so that there was no possibility of leaving cotton wool fibres within the nail matrix area, therefore reducing the chance of post-op infection due to the cotton wool fibres contributing as a foreign body. The tip is tapered and smaller overall in diameter compared to the current swabs available on the market, allowing the practitioner to have more accurate positioning and application of phenol to the site where it is needed.
Usage of SafeTPen™
SafeTPen™ doesn’t require pressure from the practitioner or aggressive rubbing into the matrix to undertake the ablation, compared to the traditional method using cotton wool or a blacks file. Excessive pressure on the SafeTPen™ tip may cause the tip to retract, at which point it is advised to discard the device to prevent excessive phenol flow rate. Recommended use of the phenol within SafeTPen™ is as per your university training or guidance through your Institute / College membership.
Gold standard practice for the use and timing of phenolisation for nail ablation is through patient assessment. Although the 3 x 1 minute application is ideal for a well perfused hallux, the actual time of the phenol applied should be related to the surface area of the nail bed that requires ablation and healing time, in which case the time should be adjusted downwards (IOCP, 2022; RCoP 2021).


Figure 7 How to activate the SafeTPen™
NB: Please see the bottom of page 22 for the REFERENCES for this article
Figure 9SafeTPen™ in use
For each procedure undertaken, phenolisation time and amount used should be taken into consideration and recorded on the patient’s notes (IOCP, 2022 and RCoP 2021). SafeTPen™ can be used for more than 1 minute application.
12 | www.iocp.org.uk ARTICLE (continued)
Once you have applied one minute application of phenol dry if required or as per local protocol and then reapply the same SafeTPen™ into the area for the next 1 minute ablation as long as there is still phenol contained within the SafeTPen™ delivery device.
Kannegieter and Kimartin (2010) cited Giacalone (1997) in the treatment of diabetic patients with phenolisation. Giacalone (1997) is cited as saying there was no post-op infection or ischaemia from the procedure of nail surgery using phenolisation and saw an average healing time of 5 weeks. The SafeTPen™ is not contra-indicated for use in the immune-compromised patients, patients on anti-coagulants, diabetes etc., however it is the responsibility of the practitioner to have thoroughly assessed the patient’s understanding of the procedure, medical history, contra-indications to LA, tourniquet and phenol as well as the assessments of the lower limb (neurological and vascular) to ensure it is safe to proceed (IOCP, 2022; RCoP 2021) . NHS (2009) issued a National Patient Safety Alert recommending the use of CE marked, coloured and labelled tourniquets (e.g. Tournicot/Unicot from Canonbury Products Ltd.) to prevent patient injury / amputation through tourniquets being left in situ following toe and hand surgery.

The use of SafeTPen™ is required to be documented in the patient’s notes recording the batch number, the strength and the time it was applied during ablation. However, it is good practice to record the approximately volume used within the surgery e.g. using 2 x SafeTPen™ during the surgery can be recorded as 0.4ml of liquid phenol 89% (1 pen) per sulci via the SafeTPen™ delivery device or 0.8ml of liquid phenol (2 pens) via the SafeTPen™ delivery device used in total.
Following phenolisation with SafeTPen™, as with bottled phenol and the alternate swab, there is no requirement to wash the sulci out with 5% chlorhexidine spray, saline, or glycerine (RCoP 2021). It has been discussed that washing of the sulci / nail matrix areas can cause the phenol to contaminate surrounding tissue and possibly seep under the tourniquet if not protected adequately, it is also possible that the use of a post-op wash could lead to dilution and increased risk of regrowth, however this decision is the practitioner’s choice through following their training / local guidelines.
Dressing the toe on completion of the nail surgery procedure, when using SafeTPen™, doesn’t require any special dressings techniques, again the dressing choice is left to the practitioner’s knowledge / local or national guidelines.
Following the surgical procedure, the SafeTPen™ should be disposed of as medical waste, and disposed of as per clinical guidelines and the local medical waste policies.
If you have any further questions about the new alternative, safer delivery device SafeTPen™ for using phenol within surgery, please contact Canonbury Products Ltd. via info@canobury.com
 of Medicines
of Medicines
There were a number of possible safe alternatives already available for chemical matrixectomy, including some well-known brands, Sodium Hydroxide or Trichloroacetic Acid.
As Chair of the Medicines and Procedures Panel (MaPP) for the IOCP, I led a team to immediately begin researching safe phenol alternatives for members and, in August 2021, we had discussions with a US provider of single-use phials. Four members trialled the new product, but we quickly decided that it was very similar to another product already available in its handling and application.
In September 2021, we began talks with Canonbury about what seemed like an exciting potential new product development, and we entered into discussions on what we, as Podiatrists, actually needed from a single-use phenol. That was incredibly easy. We all know, in our profession, what the disadvantages of the current products are:
1. The ability to access the phenol easily and safely
2. Seeing the product we’re actually using
3. Not running short of the phenol during nail surgery
4. Safely being able to apply the product with an applicator that is too large
The prototype was available at the end of November 2021, and handling it was a ‘wow’ moment. It felt so easy, safe and comfortable, and came with an applicator tip that truly suited its purpose. Yes, this was exciting!
So, here we are today with the launch of this amazing new product, that I absolutely believe will be a game-changer for the world of podiatry.
A huge thanks to Canonbury, we are proud to have been part of this innovative new product that we now know as SafeTPen™.
Podiatry Review Spring Issue 2022 | 13
Gaynor Wooldridge Chair
and Procedures Panel (MAPP) for IOCP writes:
Footnotes
Foot Health Practitioners News - Issue 9


Hi Everybody.
It’s hard to believe, but April is upon us once again. The last twelve months have been very difficult for many people, but thankfully Spring is just around the corner. We saw a reduction of Covid regulations at the end of February, Hurray! But I am still wearing a mask. The clocks will go forwards on the 27th of March giving us longer evenings, more time to enjoy with friends and family.
So many things to look forward to.
As I type this it is the end of February. It is now 4 days since Russia invaded the Ukraine, this makes me realise what a very fragile planet it is that we live on.
We all struggle to make a living, to enjoy the better things in life, and suddenly they can all be taken away in seconds.
My heart goes out to the people of Ukraine and the millions of Russians, who don’t want this war. I hope that by the time you are reading this, certain people may have come to their senses and a cease fire has been brokered.
In February I was involved in the very sad closure of the Leicestershire and Northamptonshire Branch of the Institute. This was due to the lack of attendance by Members.
A case of ‘If you don’t use it, you lose it.’ At the final meeting there were 6 attendees, of which I was the only FHP.
It is such a shame as I used to use the meetings to get to know some of the more established Chiropodists. The wealth of knowledge that these people possess is incredible, and they were very happy to share it. Unfortunately, this has now gone.
We had 25 Foot Health Practitioners in the branch, all of whom have been transferred to other branches.
Most meetings are at this current time being held on the Zoom platform. When you get your invitation from which ever branch you belong to, log on and take part. You never know you might enjoy it!
I am just off now to buy my Easter eggs before the shops run out. Have a great Spring.
Ian Fenton
Is there a specific element of your industry that you are passionate about?
Maybe it’s working with people?
Maybe it’s a certain product or treatment?
Then why not share your knowledge and expertise with your peers and feature an article in our footnotes section.
Footnotes is specifically included to share the work of our FHP community and raise the profile of all the great work you do in foot health. Content of the article should be foot health related and in an easy-to-read magazine style format.
Contact julie@iocp.org.uk for more details.
14 | www.iocp.org.uk
CALLING ALL ASPIRING FHP AUTHORS
JoySewell








Podiatry Review Spring Issue 2022 | 15
Somuz and the Graduation Group
Alison Graham
Mirela Ene
Jessica Hindley
Louise Johnson
Day
December 2021 The podiatry instrument packs given to students are sponsored by Heeley Surgical
Graduation
21st
IOCP Chair of Ethics
Health regulators Support the Government Equalities Office
I was interested to learn about many health regulators supporting the Government Equalities Office (GEO) consultation, which is proposing a ban on conversion therapy practices in England and Wales (HCPC, 2022).
The primary purpose of this Memorandum of Understanding (MoU) which forms this proposal is for the protection of the public. This is through a commitment of ending ‘conversion therapy’ practices in the UK.
“...an umbrella term for a therapeutic approach, or any model or individual viewpoint that demonstrates an assumption that any sexual orientation or gender identity is inherently preferable to any other, and which attempts to bring about a change of sexual orientation or gender identity or seeks to suppress an individual’s expression of sexual orientation or gender identity on that basis.”
(BACP, 2022).
It may not be commonly discussed in foot health practitioner’s clinics or domiciliary practice, but the GEO has proposed a ban on talking therapies for minors and adults. Particularly, if any individual was considering a change of sexual/ gender orientation or transformation; or a practitioner were to consider changing any service user’s sexual orientation or gender identity. This is something even as a parent with school children and teachers themselves could raise as a talking point in practices, seeking support.
The GEO has also proposed other measures in the MoU to stop harmful, coercive and, perhaps at times, violent practices which may be interpreted as conversion therapy. Whereby, there could be various practices linked to being a conversion therapy practice, which is likely to become a criminal offence.
However, there are practices relating to “Gender Identity Development Services”, which are not linked to the definition of conversion therapy. Particularly, the gender identity therapies that are evidence-based, effective and beneficial therapies for a patient or service user. These therapies would not be controversial to the MoU, nor would health practitioners be contravening their regulatory or professional standards.
This maybe an unusual format to bring to the attention to our CoFH members. However, as a professional body, we think it is sometimes useful to bring information which becomes available to regulated health professionals, to our CoFH foot health practitioners.
All the best,
Beverley Wright Chair of Ethics

REFERENCES
BACP, 2021. Available at: http://bacp.co.uk/media/13265/memorandum-of-understanding-onconversion-therapy-in-the-uk-september-2021.pdf. [Accessed. 20th February 2022].
HCPC, 2022. Available at: http.//www.hcpc-uk.org/news-and-events/blog/2022/conversiontherapy-ban-what- registrants-need-to-know/15-February-2022. [Accessed. 20th February 2022].

16 | www.iocp.org.uk
Beverley Wright
Foot Health Practitioners News - continued
Arthur
George
Holland
- 30th August 1926 - 5th February 2022
It was with great sadness that we learnt of the passing of Arthur Holland on 5th February 2022.

Arthur George Holland was born on 30th August 1926 in Rotherham, South Yorkshire. His upbringing was influenced by the Salvation Army and as he grew older, he was proud to play in the cornet section of their Rotherham band. He was also a member of the St John’s Ambulance brigade from boyhood.
Arthur commenced training as a nurse but with the intervention of war, he did his duty and joined the army where his basic training as a nurse was acknowledged. As a result, he was assigned to The Royal Army Medical Corps. Subsequently, he joined several regiments, one of which was the Cameroon Highlanders where he was made an honorary kilt wearer. An honour he accepted with pride and which continued throughout his life. The army took him to many places including the Far East, Java, Singapore, Burma and India. He witnessed may atrocities but also made many friends along the way, not only colleagues but also the native people especially in India.
Arthur enjoyed recounting his personal experience in the army to visitors. It clearly was a special time in his life. His Burma Star took pride of place at home.
After the war Arthur took any job he could find to provide for his family, including Parkgate Iron and Steel works and the coking plant at Canklow Colliery. This didn’t particularly suit Arthur but an opportunity arose for him to obtain a position of medical room attendant, which saw him treating miners underground and where necessary administering morphine. He also joined the Order of the Moose, an organisation that raised money for charities and proudly took his turn as President of the Rawmarsh Lodge.
It was from there that Arthur branched out into chiropody later becoming a state registered chiropodist, in fact one of the first chiropodists in the UK to train to administer anaesthesia. He worked for the NHS and in private practice.
He was a member of Sheffield branch and attended branch meetings. He particularly enjoyed the Institute’s annual general meetings and the dinner dances.
Arthur was utterly devoted to his wife, Eunice, his daughter Elaine and his grandsons, Graham and Stuart. He was a loving uncle to his nieces and nephew. He loved family life and family holidays especially Christmas. Arthur remained sociable all his life despite in recent years losing his sight and much of his hearing. Regardless of these health challenges Arthur remained independent and as active as possible. He learnt Braille and computer skills and continued to tend his garden as much as he could.
Rest in Peace Arthur. A true Gentleman with arguably the most interesting life of anyone I have met. You will be missed by all.
Condolences to Elaine, Graham and Stuart.
 Stephen Willey Ex Chairman, Board of Ethics IOCP and Sheffield Branch
Stephen Willey Ex Chairman, Board of Ethics IOCP and Sheffield Branch
OBITUARY
Podiatry Review Spring Issue 2022 | 17
Award of Consultant Fellowship of the IOCP
The Institute of Chiropodists and Podiatrists
Award
Submissions are invited from members or academic fellows of the Institute pursuant to granting them additional recognition as a Consultant Fellow of the Faculty of Podiatric Medicine of the Institute of Chiropodists and Podiatrists (CFPodM). This allows fellows to progress to further advanced training and practice indemnified by the IOCP.
Consultant Fellowship is a clinical award for senior members of the profession, recognising and demonstrating their seniority and an advanced scope of clinical practice. The minimum attainments of individuals seeking the award must be as follows:
• They must be current registrants of the Health and Care Professions Council, in good standing, at the time of application without pending disciplinary action.
• They must be current full members or academic fellows of the Institute of Chiropodists and Podiatrists with current IOCP Option 4 professional indemnity insurance.
• They must have a degree in Podiatry or Podiatric Medicine awarded by a UK university
• They must have Local Anaesthesia (POM-A) and Prescription Medicine (POM - S) annotations recorded on their HCPC registration entry OR have POM-A and Supplementary Prescribing/ Independent Prescribing recorded on their HCPC annotations.
• They must have a minimum of 12 years of clinical practice as a podiatrist.
• They must submit evidence of a pattern of continuing professional development throughout their career to date in subjects appropriate to podiatric medicine.
• They must submit a curriculum vitae, showing their journey through the profession to the date of application and this must demonstrate how they believe themselves to have a scope of practice that merits the title ‘advanced/Consultant’
• They must agree to submit a presentation/lecture to the IOCP Annual Conference demonstrating their advanced knowledge/ practice/research.
The award is via the agreement of the panel of the Consultant Fellowship board of the IOCP who will ensure that all of the minimum standards have been met. Applicants will also be required to successfully undertake an interview and provide two professional references including a statement/sponsor of support. Once the criteria has been met and the appropriate application paperwork submitted to the registered offices of the Institute, the award will then be formally issued upon payment of the nominal administration fee of £150.
Award of Academic Fellowship
The Institute of Chiropodists and Podiatrists
Award
Submissions are invited from members of the Institute pursuant to granting them additional recognition as an Academic Fellow of the Faculty of Podiatric Medicine of the Institute of Chiropodists and Podiatrists (FPodM).
Application is by way of completion of the appropriate paperwork and submission of a 5000 word dissertation containing previously unpublished material on a relevant podiatric subject that meets the approval of the Review Board of the Faculty of Fellows. Such dissertation is to be constructed on sound academic principles and be adequately referenced in an accepted academic style.
For members who have not previously published, the Board is happy to give informal and friendly guidance to members wishing to develop this interesting new area of their professional career. A nominal fee of £100 is payable to cover the necessary administration by Head Office. Certificates of Fellowship will be awarded to successful Fellows and their names recorded on the Roll of Fellows maintained by the Faculty.
Accepted dissertations will be published in Podiatry Review and be added to The Fellows Library which will be an electronic knowledge bank available online to registered members. Such activity is also held to be Continuing Professional Development (CPD) by the IOCP and is suggested as being suitable to record in the event of HCPC audit.
Applications will be accepted from current members who are HCPC registered, annotations such as POMs or LA are not a condition of application as this is an academic award open to all HCPC registered full members of the Institute.
For further information and an application form please contact Head Office by emailing info@iocp.org.uk.
18 | www.iocp.org.uk
AWARDS
Essentials of Biomechanics
Principles of gait: Creating the Lever for Acceleration
By Andy Horwood Visiting Lecturer & Fellow Staffordshire University

INTRODUCTION
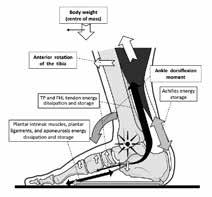
Impact and braking forces of deceleration during the initial contact and loading response of gait generates two spikes of vertical force (at heel strike and forefoot loading) and also one peak of horizontal force. The energy these impulses create must be dissipated safely and spread across multiple tissues within the lower limb to avoid injury. Damage may occur if energy and forces concentrate repetitively into a specific structure. Therefore, the lower limb is required to provide mechanisms of shock attenuation. These shock absorbing techniques were reviewed in the last edition of this journal and the mechanisms of energy dissipation discussed. The processes of protecting the body from impact collisions at heel strike and at forefoot loading leaves the foot relatively flexible and thus in its most compliant state at the start of single-limb support. Being compliant has advantages for support of the body by improving foot-to-ground contact when the body weight is vaulting over the foot at the ankle. However, higher compliance within the foot is a disadvantage for acceleration at the end of stance phase.
The Advantages of Compliance During
Early Midstance
By permitting more compliance to develop out of relative stiffness during forefoot loading the foot is able to act as a shock absorber. It acts much like a spring, albeit one that can adjust its springiness to terrain circumstance. The foot is able to absorb impact energies by (relatively) freely straining (lengthening and widening) under increasing loading stress as the full body weight is transferred onto the foot at the start of single-limb support. The foot stiffens under increased loads and at faster loading rates, reflected by changes demonstrated by the foot vault’s (arch’s) height that occur during gait (Stolwijk et al, 20014; Bjelopetrovich and Barrios, 2016; Takabayashi et al, 2020). Initial flexibility during early midstance phase allows the foot to become increasingly prone to the support surface so as to reach lowest foot vault profile at the heel lift boundary (Hunt et al, 2001). By doing so, the contact area of the foot’s plantar surface expands to improve stability with the ground. This pronation effect also reduces peak plantar pressures via forces spread out over an enlarging surface contact area. The flexibility the foot retains throughout midstance allows energies to be dissipated to protect the anatomical structures within the foot. This is achieved by straining all the connective tissue structures that bridge the vault, such as the plantar ligaments and the plantar aponeurosis (fascia), as joints across the vault move and glide under load. The connective tissues are protected from overstraining by muscular contractions that actively adapt the level of stiffness of the foot (and lower limb) by controlling and limiting joint motions. Muscle contractions also protect bone from high tensile and shear stresses, creating more compression forces within the bones, which their tissue structure can tolerate well.
Thus, foot compliance during early midstance helps dissipate forces from impact and body weight-induced loading of the lower limb. However, compliance must be limited to prevent excessive deformation of anatomy. Increasing connective tissues stiffness is a response to increasing strains within the foot. The foot’s stiffness is further increased via muscular activity that helps to protect its anatomy from the body weight overly straining tissues during single-limb support. As midstance progresses forces upon the foot rise, requiring muscle and tendon-induced stiffening within the plantar vault to help resist the strains associated with the ankle dorsiflexion moments of late midstance. These ankle extension forces are directed into the foot’s vault via anterior tibial rotation, concurrent rearfoot plantarflexion, and midfoot dorsiflexion. This midfoot motion primarily occurs at the talonavicular and 4th and 5th tarsometatarsal joints (Wolf et al, 2008). However, it is important to moderate this foot motion, for too much foot flexibility (compliance) during the later stages of stance is a problem for the mechanics of acceleration. By allowing the foot vault to sag downwards (sagging deflection) throughout midstance, energy can be dissipated. However, foot vault deflection also induces relative stiffening of the soft tissues of the foot vault, particularly once muscle activity increases during late midstance.
Podiatry Review Spring Issue 2022 | 19 CPD 4 page article
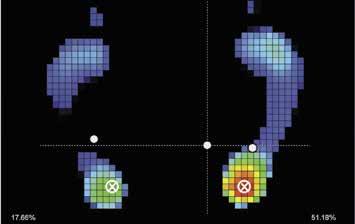
Figure 1
The foot flattens, lengthens, and widens (pronates) during late midstance as the body’s centre of mass (CoM) passes forward over the foot via anterior tibial rotation. This creates the ankle dorsiflexion moment that is resisted by triceps surae, which provides an effort force (E) that acts as a brake on anterior tibial rotation, decelerating the forward progression of the CoM. This strong muscular braking by eccentric triceps surae contraction stretches the Achilles, storing energy within it to be release later for acceleration. The ankle dorsiflexion moment also causes articular compression on the dorsal aspect of the foot as part of sagging deflection of the vault. This is expressed as rearfoot (talar and distal calcaneus) plantarflexion and midfoot dorsiflexion, particularly medially at the talonavicular joint. Vault depression stretches the plantar connective tissues to dissipate and store energy within them. Muscular contraction from tibialis posterior (TP), flexor hallucis longus (FHL), and peroneus longus (not shown) work with other plantarflexion extrinsic muscles and the plantar intrinsic muscles to control and moderate vault sagging deflection that flattens the arch (pronation). The combined stretching of the connective tissues and increasing muscle activity stiffens the foot (initially within the transverse profile of the vault), giving it a property that enhances the ability to initiate heel lift and acceleration off the foot during terminal stance. (Permission www.healthystep.co.uk)
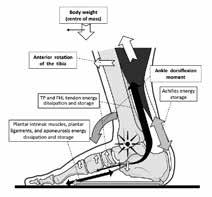
Gaining Stiffness Throughout Midstance
Therefore, early midstance utilises a more compliant foot (mobile adaptor) as a leftover feature of the impact shock absorbing phase of walking. As soon as forefoot loading is completed at foot flat (and toe flat via the reversed windlass mechanism), the foot begins a cycle of stiffening. As is demonstrated on a force-time curve, from the F1 peak of peak vertical force during initial limb loading, forces start to decrease.
This occurs because the lower limb starts a cycle of limb lengthening via hip and knee extension to lift the centre of mass (CoM) away from the ground. Force is mass x acceleration, so if the body weight accelerates away from the ground then ground reaction forces (GRF) decrease. This limb extension occurs with the foot pronating further onto the ground at its most rapid rate under strain-deformation, but fortunately during a time of decreasing force. This improves the contact stability of the lower limb as the CoM lifts up and the opposite limb starts its swing phase.
Thus, the vertical forces on the force-time curve start to form a trough (see figure 2).

Stiffening the Foot Against Gravitational Forces
The trough reaches its peak depth around the same time as the centre of mass (CoM) achieves its highest point in the middle of stance phase, which is referred to here as absolute midstance. After absolute midstance, the CoM of the body starts to fall forward as the tibia rotates anteriorly on the ankle, increasing the vertical GRF component again (mass x increasing acceleration towards the ground).
This anterior fall of the CoM on the extended leg should initially be controlled (braked) by the activity of the ankle plantarflexor muscles, primarily the triceps surae. This muscle, working through the Achilles tendon, moderates extension (dorsiflexion) moments at the ankle.
Gastrocnemius activity within triceps surae also prevents knee hyperextension during late midstance. The rotation
Figure 2
Early midstance starts at the F1 peak that signifies the beginning of single-limb support. The foot is now at its most compliant during stance phase because it has flexibility that was required for foot deformation for acting as a shock absorber. The lower limb now starts to extend under extensor muscle contraction at the hip and knee, accelerating the CoM away from the ground, thus reducing the vertical component of the GRF. This process ends with the CoM at its highest point during gait around the middle of midstance. Thus, absolute midstance point is where the vertical and horizontal force components are at their lowest. The dip in the vertical force trace is known as the F2 trough. During this period the foot is linearly elastically (stretching at a consistent rate) but from the F2 trough the rate of stiffening of the foot increases, although the vault of the foot continues to flatten. (Permission www.healthystep.co.uk)
20 | www.iocp.org.uk CPD 4 page article Principles of Gait: Creating the Lever for Acceleration (continued)
of the tibia at the ankle resisted by the calf muscles (mainly soleus), stretches and store energy within such tendons as those of tibialis posterior, peroneus longus, flexor hallucis longus, but most significantly within the thick Achilles tendon. Elastic potential energy is thus stored within these tendons until the moment of heel lift, but this process also stiffens the foot during late midstance via these tendons that run under the vault.
The foot beneath the ankle still needs to be able to dissipate some energy through connective tissue stretching during late midstance to prevent tissue injuries within it. However, the priority during late midstance begins to become the storage of energy under the foot for use during heel lift and for acceleration at the end of stance. Connective tissues (indeed all biological material) are viscoelastic. Such materials via their collagen content, stretch easily at first, then show linear elasticity before they start to stiffen exponentially for further changes in length. The foot vault continues to lower (pronate) until just after heel lift.
However, the more pronated it becomes the stiffer the connective tissues behave. This stiffness can be moderated by muscular activity of the extrinsic calf muscles via tightening their tendons and also via the plantar intrinsic muscles that now become increasingly active.
During late midstance the centre of the GRF moves increasingly into the forefoot and moves off the heel. This means that the forefoot connective tissues are now stretching more and those of the rearfoot have started offloading. Thus, ligaments within the rearfoot such as the short plantar ligament and spring ligament should start to recoil while those that cross the rearfoot into the forefoot, such as the long plantar ligament and also the plantar aponeurosis, continue to elongate (Welte et al, 2021).
The deep transverse metatarsal ligament will stretch and
stiffen between the metatarsal heads, preventing excessive intermetatarsal splay which stiffens the foot across its transverse profile. This is very important, as transverse foot stiffening is easier to achieve than longitudinal foot vault stiffening, but the latter couples to the former (Venkadesan et al, 2017a, 2017b, 2020). To aid transverse plane foot stiffening during late midstance, the tibialis posterior and peroneus longus become very active and together stiffening the foot (Kokubo 2012). The foot is gradually turning into a semi-rigid beam that can lever the heel off the ground, rotating at the metatarsophalangeal (MTP) joints.
The anterior fall of the CoM of the body reduces the forces on the heel. When the forces of elastic recoil stored within the Achilles are greater than the body weight derived forces keeping the heel on the ground, heel lift will initiate. Both the acceleration of the CoM downwards and forwards and the active ‘pushing’ of the plantarflexor force released into the ground at heel lift, generate an increasing vertical GRF that creates a second peak of vertical force known as the F3 peak. This peak of force is heavily influenced by how stiff the foot is at heel lift and thus indicates the mechanical efficiency of acceleration.
The Advantage of Creating a SemiStiffened Beam
Having a compliant foot at the start of midstance means that loading energies can be safely dissipated within the foot anatomy. By creating a stiffer foot during midstance, energy can be stored, but by remaining semi-flexible some energy can still be dissipated. Moderating muscle activity to adjust the levels of foot stiffness means that more or less energy can be dissipated or stored during every step, depending on the need of that particular step. The capacity to moderate and provide adaptable foot stiffening is the key to avoiding injury during locomotion.
Figure 3
From absolute midstance at the depth of the F2 trough and throughout late midstance represents a period of increasing vertical forces. This creates an up-slope from the F2 trough to another peak of vertical force associated with acceleration at heel lift. This is known as the F3 peak and requires a stiffened foot to generate the high GRF. The F3 peak is associated with positive work and increased momentum for the body weight. It reflects the size of the GRF generated by ankle plantarflexion power around heel lift that derives from elastic recoil energy released from the Achilles tendon. (Permission www.healthystep.co.uk)

Podiatry Review Spring Issue 2022 | 21
Principles of Gait: Creating the Lever for Acceleration (continued)
Summary
The amount the foot is stiffened at the end of walking midstance effects how efficient the foot will be during acceleration (Takahashi et al, 2016, 2017). Stiffness of the foot enables utilisation of both lever arm mechanical advantages and also increased energy storage that is released for creating power for maintaining the body’s CoM momentum onto the next step. However, sometimes energy dissipation at acceleration will be more important than energy efficiency and the momentumdriving power. This means that retaining the ability to moderate foot stiffness remains an important ability within the foot to provide the right locomotive approach to terrain conditions or gait perturbations, and thus avoid injury.
In the next edition we will consider how foot stiffening levels influence the type two lever mechanics of the terminal stance phase of gait during acceleration biomechanics.
REFERENCES:
Bjelopetrovich A, Barrios JA. (2016). Effects of incremental ambulatory-range loading on arch height index parameters. Journal of Biomechanics. 49(14): 3555-3558.
Hunt AE, Smith RM, Torode M, Keenan A-M. (2001). Inter-segment foot motion and ground reaction forces over the stance phase of walking. Clinical Biomechanics. 16(7): 592-600.
Kokubo T, Hashimoto T, Nagura T, Nakamura T, Suda Y, Matsumoto H, et al. (2012). Effect of the posterior tibial and peroneus longus on the mechanical properties of the foot arch. Foot & Ankle International. 33(4): 320-325.
Stolwijk NM, Koenraadt KLM, Louwerens JWK, Grim D, Duysens J, Keijsers NLW. (2014). Foot lengthening and shortening during gait: A parameter to investigate foot function? Gait & Posture. 39(2): 773-777.
Takabayashi T, Edama M, Inai T, Nakamura E, Kubo M. (2020). Effect of gender and load conditions on foot arch height index and flexibility in Japanese youths. Journal of Foot and Ankle Surgery. 59(6): 1144-1147.
Takahashi KZ, Gross MT, van Werkhoven H, Piazza SJ, Sawicki GS. (2016). Adding stiffness to the foot modulates soleus force-velocity behaviour during human walking. Scientific Reports. 6: 29870.
Takahashi KZ, Worster K, Bruening DA. (2017). Energy neutral: the human foot and ankle subsections combine to produce near zero net mechanical work during walking. Scientific Reports. 7: 15404.
Venkadesan M, Dias MA, Singh DK, Bandi MM, Mandre S. (2017a). Stiffness of the human foot and evolution of the transverse arch. https://arxiv.org/ abs/1705.10371
Venkadesan M, Mandre S, Bandi MM. (2017b). Biological feet: Evolution, mechanics and applications. (Chapter 7, Section 7.1.) In: Bioinspired Legged Locomotion: Models, Concepts, Control and Applications. [Eds.: Sharbarfi MA, Seyfarth A.] Butterworth-Heinemann, Elsevier Science. pp. 461-486. www.researchgate.net/profile/Madhusudhan-Vankadesan/publications/32.
Venkadesan M, Yawar A, Eng CM, Dias MA, Singh DK, Tommasini SM, et al. (2020). Stiffness of the human foot and evolution of the transverse arch. Nature. 579(7797): 97-100.
Welte L, Kelly LA, Kessler SE, Lieberman DE, D’Andrea SE, Lichtwark, et al. (2021). The extensibility of the plantar fascia influences the windlass mechanism during human running. Proceedings of the Royal Society B: Biological Sciences. 288(1943): 20202095.
Wolf P, Stacoff A, Liu A, Nester C, Arndt A, Lundberg A, et al. (2008). Functional units of the human foot. Gait & Posture. 28(3): 434-441.
REFERENCES FOR THE SafeTPen™ ARTICLE ON PAGES 10 - 13
Abbot, P., Maher, A., Wilkinson, A. (2012) Case Report. Complicated chronic ingrowing toe nails Podiatry Now Feb, 14-16. https://www.researchgate. net/publication/261359432_Clinical_Case_Report_Complicated_chronic_ingrowing_toe_nails (accessed February 17th, 2022)
Eekhof, J., Van Wijk, B., Knuistingh Neven, A., van der Wouden, J. (2012) Interventions for ingrowing toenails. Cochrane Library. https://doi. org/10.1002/14651858.CD001541.pub3
Institute of Chiropodists and Podiatrists (2022). Nail surgery guidelines. Members area iocp.org.uk

Kannegieter, E., Kilmartin, T. (2010). Critical Review The conservative and surgical management of ingrowing toenails. Podiatry Now. Dec. 11-18. https://www.researchgate.net/publication/270899548_Critical_Review_The_conservative_and_surgical_management_of_ingrowing_toenails (accessed February 24th, 2022)
Martínez-Nova, A., Sánchez-Rodríguez, R., Alonso-Peña, D. (2007) A New Onychocryptosis Classification and Treatment Plan. J. Am Podiatric Assoc. 97 (5), 389-393
Moda, R,K., Latham, A. (2016) Evaluating clinical outcomes of Nail surgery. Podiatry Now. June 10-13 https://www.researchgate.net/ publication/307853049_Evaluating_Clinical_Outcomes_of_Nail_Surgery_A_Retrospective_Audit (accessed February 24th 2022)
National Health Service. (2021) National Patient Safety Alert Elimination of bottles of liquefied phenol 80%. https://www.england.nhs.uk/ publication/national-patient-safety-alert-elimination-of-bottles-of-liquefied-phenol-80/ (accessed October 10th, 2021)
National Health Service, (2009) Reducing risks of tourniquets left on after finger and toe surgery. https://webarchive.nationalarchives.gov.uk/ ukgwa/20180501163609/http:/www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=65568&p=2 (accessed 28th February 2022)
Royal College of Podiatry (2021) Nail surgery guidelines. https://membersarea.rcpod.org.uk/podiatric-practice/professional-resources-area/ guidelines (accessed December 2021)
Wooldridge, G. 2021. Phenol: past, present and future. Podiatry Review. https://iocp.org.uk/about/podiatry-review/ (accessed February 18th, 2022)
22 | www.iocp.org.uk
CPD 4 page article
PODARICK NAILS IT!
Podarick can you help me?
I am a foot health practitioner (FHP) and I’m finding it hard to advertise my services as an FHP. Google and Facebook only have listings for chiropody and podiatry, not FHP, can I advertise on these sites as an FHP?

Podarick says:
It is a struggle for many professions to advertise under the correct listings. Particularly, as some listings require evidence of registration of your profession such as HCPC registration number to advertise as a “chiropodist” or “podiatrist”. If you cannot find the relevant FHP listing, then you must decide what other listing to place your advertisement under. Many FHPs advertise under “Health”, “Beauty”, “Hairdressing”, or another listing that associates the other services practitioners offer. However, unregistered practitioners cannot use the protected titles in any form of advertising under the banner of “chiropodist”, “chiropody”, “podiatrist” or “podiatry” because it is illegal. This includes an advert, brochure, business card, directory entry, invoice, leaflet, letterhead, logo, poster, or website. Facebook, Instagram, Twitter, or other social media site, FHP have control of what they write and post on these sites. Anyone found to be using these protected titles who are not HCPC registered are liable to prosecution, which can result in a fine and a criminal record.
“Article 39(1) of the Health Professions Order 2001 makes it a criminal offence for a person, with intent to deceive (whether clearly or by implication) to:
• say that they are on the HCPC Register;
• use a designated title to which they are not entitled; or
• say falsely that they have qualifications in a profession we regulate.
The words “by implication” mean that an unregistered person may be committing an offence even if they do not use the designated title directly (for example, if they describe the service they provide as “chiropody” or “physiotherapy”).” (www.hcpc-uk.org)
For further information of misuse of protected titles, please go to: Misuse of title | (hcpc-uk.org).
Send your Nail Clippings to Podarick: c/o The Institute of Chiropodists & Podiatrists 150 Lord Street, Southport, PR9 0NP
Apology to Mr Iain B McIntosh
In the January issue (Vol. 79 No.1) the attribution for the author of the Cold Foot Syndrome article (pages 28-30) was incomplete and inaccurate. The author was Iain B Mcintosh, former chiropody school inspector and ICP medical adviser. We would like to apologise to Mr McIntosh for any upset caused.
Podiatry Review Spring Issue 2022 | 23 ARTICLE
Products & Procedures under the microscope
With Gaynor Wooldridge Chair of the Medicines and Procedures Panel (MaPP) at the Institute of Chiropodists and Podiatrists

UREA – THE MAGIC SUBSTANCE?
INTRODUCTION
As podiatrists and foot health practitioners we are in a prime position to assess patients’ skin, and to also advise on the most appropriate course of action for maintaining skin integrity and the treatment of dry skin conditions. This article will have a closer look at the history of urea, it’s properties, the wider global uses, and current applications in skin care of this amazing substance.
What is it?
All of our patients know what urea is, don’t they? When we recommend cream containing urea, they all have something amusing to say! “I went to the doctor after drinking a litre of food colouring. I was diagnosed with having a case of dye urea.”
But what actually is the physiology of urea? Urea, (molecular formula NH2CONH2, Fig. 1), is also known as a carbamide, and is a polar, hygroscopic molecule produced by the human body. It is the chief nitrogenous end product of the metabolic breakdown of proteins in all mammals, and some fish, and occurs in their urine, blood, bile, milk and perspiration (Kerrapati and Mehendale, 2014); this urea, or ornithine, cycle, (Fig. 2), is also known as the Krebs-Henseleit cycle (Oxford dictionary, 2006). Grether-Beck et al. (2012) hypothesised that urea was not merely a passive metabolite, but also a small-molecule regulator of epidermal structure and function.
Early discoveries
In Asia, Africa and Europe the therapeutic use of urine (urotherapy) has been documented for centuries (Savica et al. 2011). Pliney the Elder discussed the use of urine for treating sores and burns, as well as skin rashes and more, in his Naturalis Historia (AD 77)
It is the largest single work to have survived from the Roman Empire to modern day. The book of Proverbs (5:15), purportedly written and complied approximately 700 BC and attributed to King Solomon, advised:
Fig. 1 Fig. 2
2016).
24 | www.iocp.org.uk ARTICLE
“...drink water from your own cistern, flowing water from your own well...” (Motola,
Urea was first isolated from urine in 1727 by Herman Boerhaave (Kyle, 2018). Rouelle is commonly cited as its discoverer in 1773 (Verzi, 2020), but Boerhaave beat him by almost 50 years. The first ground -breaking laboratory synthesis was produced by Friedrich Wohler in 1828, which followed William Prout’s extraction of pure urea from urine (1817); Prout also identified that hydrochloric acid was contained in gastric juices and classified food components as water, fats, carbohydrates and proteins (Rosenfeld, 2003).
The first use of urea in modern medicine was the topical treatment of wounds due to its proteolytic and antibacterial properties (Verzi, 2020). Robinson (1936) discussed the healing effects of urea on chronic, purulent wounds. He reported that a 2% solution of urea in water, on saturated gauze dressings which were applied to the wound, had remarkable cleansing and healing properties.
These healing effects of urea on chronic, purulent wounds were also discussed by Robinson (1936). Robinson was a senior entomologist, and he demonstrated how local granulation tissue was stimulated by allantoin; this is produced during the breakdown of uric acid produced by maggots. He also carried out successful clinical tests to show that the ammonia/urea produced by the maggots was sufficient to increase wound pH to neutral, or slightly alkaline; this promoted the healing of purulent and indolent wounds. Elmore (1938) also discussed the use of urine to improve wound healing in horses.
Modern medicine
Until the early part of the 19th century, it was believed that the synthesis of urea required a living organism, or some part of a living organism, such as a kidney (Ramberg, 2000). In 1828, Friedrich Wöhler, as previously mentioned, challenged this view by synthesising urea in a laboratory, thus disproving the concept of Aristotle’s vitalism theory (Coulter et al. 2019). Wöhler is now known as a pioneer of organic chemistry - even though he never actually intended to make urea!
Because urea is a naturally occurring substance found on the surface of the skin, it is an active part of our natural moisturising factor (NMF), and makes up 7% of these water binding, skin substances (Fowler, 2012). Over time, urea decreases with age, trauma from harsh ingredients and environmental factors, all of which makes the skin more susceptible to dryness, aging and inflammation (Fig. 3, reproduced from clinic photographs, 2022). As podiatrists, we frequently see alterations in barrier function, often associated with several skin diseases. At a lower dose (≤ 10%), urea containing topical formulations act as a skin moisturiser, whilst higher concentrations (≥ 10%), urea based preparations exert a keratolytic action (Cellano, 2018). See Fig. 3

Piquero-Casals et al. (2021) reviewed the properties of urea, and reported that it was hygroscopic, present in the epidermis as a component of the natural moisturising factor (NMF) and essential for adequate hydration and integrity of the stratum corneum. There have been multiple clinical trials in the use of urea-containing formulations. The results have all shown significant improvement in atopic dermatitis, ichthyosis, xerosis, seborrheic dermatitis and psoriasis; it has also been shown to improve skin penetration and optimise the action of topical drugs (Pan et al. 2013).
Neuropathy can also refer to autonomic compromise, as well as sensory and motor dysfunction, as in anhidrosis. The Rochester Diabetic Neuropathy Study (Dyck et al. 1992) found that 6% of the study population presented with autonomic neuropathy, and that this autonomic defect was evident in the eccrine sweat glands of the skin. The study compared the efficacy of 10% and 25% urea cream on participants (male and female) with type 1 and type 2 DM. The results indicated that both creams significantly hydrated the skin, but 25% hydrated it more significantly.
Ivan Bristow (2013) also discussed the use of emollients in the care of the diabetic foot, and supported the benefits of urea and emollients in maintaining skin integrity. He also suggested how the creaming also serves as a means of daily foot inspection for people with diabetes and at-risk feet.
Other current uses
Fig. 3
There are many varied uses of urea. It is now prepared commercially in vast amounts from liquid ammonia and liquid carbon dioxide. These two materials are combined under high pressures and elevated temperatures, to form ammonium carbamate; this then decomposes at much lower pressures to yield urea and water (Sigurdasen et al. 2018). Kumar (2013) investigated how urea can now be used as a source of electric power, as urine eating bacteria are able to create a current strong enough to power a mobile phone. In 2013, Cai et al. published their results demonstrating that stem cells harvested from human urine were able to be reprogrammed into neurones, and then used to grow tooth-like structures.
Globally, 90% of synthetically produced urea, with production at approximately 220m tonnes/year, is now used in fertilisers and as an additive (AdBlue) for diesel fuel emissions. Demand and supply has continued to push up fertiliser prices 3-fold between 2021 and 2022 (Outlaw et al. 2022).
Podiatry Review Spring Issue 2022 | 25
Continued overleaf
Products & Procedures under the microscope
(continued)
The United Nations Food and Agriculture Organisation’s index of food prices is already at its highest level since 2011. China and Russia are the biggest producers of industrial urea, and they have restricted exports to ensure supply to their own farmers. An energy crunch in China has also led to fertiliser production to be slashed, and the food-grade carbon dioxide, which is a by-product of the ammonia production process, was also dramatically affected during the COVID pandemic (Nelson, 2022).
And finally…
Urea is a small, but vitally important, compound in the body. As practitioners working within foot care, we are constantly looking to improve and maintain the quality and integrity of patients’ skin. Urea plays a fundamental role in regulating keratinocyte proliferation, the skin’s barrier function and antimicrobial defence (Piquero-Casals, 2021). The key to healthy skin must surely be hydration, and urea seems to be this ‘magic’ ingredient.
REFERENCES
Bristow, I. 2013. Emollients in the care of the diabetic foot. The Diabetic Foot Journal. Vol 16 No. 2
Cai, J et al. 2013. Regeneration of tooth-like structures from integrationfree human urine induced pluripotent stem cells. Cell Regeneration Journal volume 2 no. 1
Cellano, L. 2018. Topical urea in skincare: A review. Dermatol Therapy. Nov Coulter, I et al. 2019. Vitalism A world view revisited: a critique of vitalism and it’s implications for integrative medicine. Integrative Medicine: A Clinicians Journal. 18(3): 60-73
Dyck, PJ et al. 1991. The Rochester Diabetic Neuropathy Study Design. Criteria for types of neuropathy, selection bias and reproducibility of neuropathic tests. Neurology Journal 41(6)
Elmore, CJ. 1938. Urea for wound healing. JAMA 110(10): 758
Fowler, J. 2012. Understanding the role of natural moisturising factor in skin hydration. Practical Dermatology
Grether-Beck, S et al. 2012. Urea uptake enhances barrier function and antimicrobial defence in humans by regulating epidermal gene expression. The Journal of Investigative Dermatology 132(6): 1561-1572
Kligman, A. 1957. Dermatologic uses of urea. Acta Dermato-Venereologica Korrapati, MC and Mehendale, HM. 2014. Urea. Encyclopedia of Toxicity. 3rd ed: pp 885-888
Kumar, M. 2013. From gunpowder to teeth whitener: the science behind historic uses of urine. Science Smithsonian Magazine
Kyle, RA and Steensma, DP. 2018. Herman Boerhaave Master Clinician and Humanist. Mayo Clin Proc. Nov; 93(11): 119-120
Motola, J. 2016. The history of urine as healing. The journal of Urology. Vol.195, Iss 4S
Nelson, A. 2022. CO2: will there be another carbon dioxide gas shortage in the UK, and how it could impact on supplies. National World.
Outlaw, JL et al. 2022. Economic pact of higher fertiliser prices in AFPCs. Representative Crop Farms Briefing Paper 22-01
(Kligman, 1957).
Oxford Dictionary of Biochemistry and Molecular Biology (2nd Ed). 2006. Edited by Cannock, R et al. Oxford University Press.
Pan, M et al. 2013. Urea, a comprehensive review of the clinical literature. Dermatol Online Journal; 19: 20392 [PubMed] Accessed 15th February 2022
Piquero-Casals, J et al. 2021. Urea in dermatology: a review of its emollient, moisturising, keratolytic, skin barrier enhancing and antimicrobial properties. Dermatol Ther (Heielb); 11(6): 1905-1915
Pliney the Elder. AD77. Natural History LCL392: 50-51. Book XX. Natural Art Library.
Robinson, W. 1936. Use of urea to stimulate healing in chronic, purulent wounds. The American Journal of Surgery. Vol 33, Iss 2 pp 192-197
Ramberg, PJ. 2000. The death of vitalism and the birth of organic chemistry: Wohler’s urea synthesis and the disciplinary identity of organic chemistry. Ambix 47(3): 170-95
Rosenfeld, L. 2003. William Prout: Early 19th century physician chemist. Clinical Chemistry 49: 699-705
Savica, V et al. 2011. Urine through the centuries. Journal of Nephrology 24 Suppl 17: S123-5
Sigurdasen, JJ et al. 2018. The molecular processes of urea hydrolysis in relation to ammonia emissions from agriculture. Reviews in Environmental Science and Biotechnology 17; 241-258
Verzi, AE et al. 2020. History of urea as a dermatological agent in clinical practice. Int J Clin Practice
FIGURES
Fig.1 National Centre for Biotechnology Information (2022). PubChem compound summary for CID 1176, Urea. Retrieved February 15 2022 from https://PubChem.ncbi.nlm.nih.gov compound/Urea
Fig.2 Krebs, H and Hanseleit, K. 1932a. Untersuchungen uber die. Harnstoffbildung I’m Tierkorper I, Klinische Wocheschrift 11(27): 1137-1139
26 | www.iocp.org.uk ARTICLE
“It often happens in the search for new therapeutic agents that some old stand-by is overlooked, whose lustre has worn off, but which may have useful applications in moments where miracle drugs falter. In the world of topical therapy, urea is such a drug. Youthful skin with a visible glow –it’s the holy grail of skincare.”

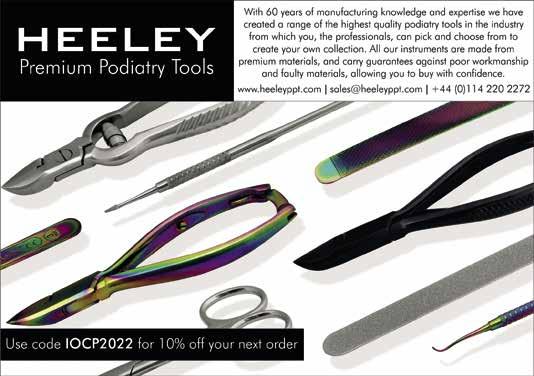
Podiatry Review Spring Issue 2022 | 27
NOMINEES
Annual General Meeting Nominations



President

Vice-Chair,



28 | www.iocp.org.uk
Executive Committee
Abid Ali Elected unopposed
Linda Pearson
Caroline McCartney
William Liggins
Andrew Williams Elected unopposed
Chair, Board of Education
>>
Beverley Wright Elected unopposed
Vice Chair, Board of Education
for National Office - 11th May 2022

Taking place at the Arden Hotel, Birmingham on the evening of Wednesday, 11th May 2022 in the Millennium Room from 7.30pm, after the Institute of Chiropodists and Podiatrists Annual General Meeting.






It has been a long time since we last got together, so book your place at the IOCP’s Networking Event, enjoy a buffet whilst meeting up with members and acquaintances, time to swap ideas and socialise.
Pre booking is required via the website in the members area, along with a deposit of £20, which is fully refundable upon attendance after the event.
If you are attending Primary Care, The Arden Hotel is a 5–10 minute walk.
There is limited availability, book your ticket early to avoid disappointment
No attendance - No refund.
Podiatry Review Spring Issue 2022 | 29
our
FREE
Don’t miss
first
Members Networking Event/Buffet
Regional Director: England North
Caroline McCartney Elected unopposed
William Liggins Elected unopposed
Regional Director: England Midlands
Joseph Olivelle Elected unopposed Regional Director: Ireland Stephen Preston Elected unopposed
Helen Jephcote Elected unopposed
Regional Director: Scotland
Linda Pearson Elected unopposed
Regional Director: Wales
Michael Franklin Elected unopposed
Standing Orders Committee
Regional Director: England South
FOREWORD by Afni Shah-Hamilton
Ask a member of the public what a podiatrist is and you are most likely to hear “Is that the same as a Chiropodist?” or “Oh they cut toe nails!”, when in fact we all know there is so much more to our profession.
Other professions already have a strong working relationship with one another, for example: physiotherapists, chiropractors and osteopaths. The role of a podiatrist in the biomechanics of the body and overall well-being of a patient is crucial and needs to be recognised by other professions. In a series of articles for the Podiatry Review, we will be looking beyond the ‘conventional’ podiatry box with Afni Shah-Hamilton, who already incorporates a wide range of therapies and treatments to enhance her overall patient experience.
Afni Shah-Hamilton graduated from University College London in Podiatry BSc (Hons) and completed her master’s degree at Kings College London. Afni established a successful clinic in North London, Tiptoe Foot Care, where she specialises in pain management. Afni has helped a large number of patients with unresolved (or in some cases previously undetected) problems with the toes, foot or ankle that were causing long term knee, hip, back or neck pain.

Afni has further broadened her knowledge by studying a range of related areas including systematic kinesiology and Anatomy in Motion (AiM), to identify the root cause of long term joint pain and mobility issues.
The first therapy in review is; Anatomy in Motion. Founded by Gary Ward who explains the philosophy of AiM, how it was developed and introduces its key principles. This extension of biomechanics and traditional anatomic training could be used by podiatrists to enhance their treatments and give patients better outcomes.

Beyond Podiatry:
An Introduction to the principles of Anatomy in Motion (AiM)
TThe act of re-aligning the feet is second nature to many podiatrists, and when advising on insoles you will no doubt consider the impact on the arches, ankles and knees. However, the connections go much further than this and for many the detailed explanation of how the feet communicate movement to the whole body still remains an enigma.
This isn’t unique to podiatry, I have found that the vast majority of healthcare practitioners are aware that the whole body is connected. As a result, they understand that working with just one part of the body in isolation will never quite cut the mustard; and yet they have rarely been shown in detail how it’s connected or how the various parts of the body move together to provide efficient long chains of movement.
By Gary Ward Founder of Anatomy in Motion
Anatomy traditional biomechanics training to understand the full picture. It is based on the gait cycle but for podiatrists it provides an opportunity for you to widen your existing knowledge and use this greater understanding to lead to improved patient outcomes.
How can AiM help your clinical practice?

What if you could be presented with what is essentially a roadmap that explains these connections in full detail? Biomechanics has the chance to move from observation of isolated structures toward observation of the whole body, once you recognise and acknowledge that each part of the body is able to communicate movement to all other parts.
For instance, how does a foot communicate movement to the opposite shoulder? We may have seen a foot - shoulder relationship many times but can you explain and predict it? By studying AiM you can learn the interplay between all bones and joints and their subsequent impact on the soft tissue system, and, as a result, better understand and resolve physical problems that your patients are experiencing in their day to day lives.
30 | www.iocp.org.uk ARTICLE
To work with the human foot is to work with the whole body
Such an understanding can also help resolve a common bug bear of practitioners where some patients inexplicably don’t respond to the standard treatment. Perhaps orthotics work for one collapsed arch but does very little for another. Or one patient’s back pain goes away, but another person’s remains the same. By re-assessing our thinking and asking a few (better) questions we can obtain deeper insight and identify where bespoke solutions are needed. Is the foot position the underlying problem here or is it being caused by something else? An underlying structural issue that may not even be obvious to the patient? The clues are often all there once you know where (and how) to look for them.
What is Anatomy in Motion?

Anatomy in Motion is a movement oriented education system that provides an alternative approach to biomechanics. It is based simply on what the joints of the human body do and when they do it during the human gait cycle. It takes into account how upper body biomechanics can be influenced greatly by lower body biomechanics and vice versa.
Each bone and joint are connected in long chains that create clear and predictable patterns of movement that are both learnable and simple to work with. Importantly though, there is no single direction of influence. For instance, did you know that somebody’s neck posture can affect the state of a person’s feet? Looking only at the feet in this instance may not provide an adequate or lasting solution as the underlying cause potentially remains unresolved. By taking a wider view and then using our knowledge of the connections through the body, perhaps we could be in a better position to help?
Anatomy in Motion was created out of a personal curiosity to uncover exactly how we as human beings walk. It was founded on the line of questioning: if I move joint A, what happens at joint B? If I move joint B in that way then what happens at joint C? And therefore if I move joint A, can we always predict what will happen to joint C?
Of course, it doesn’t stop at C, it keeps on going until you can see exactly how the foot and neck are communicating with each other through their movements. AiM documents specifically how these structures connect and the key to it all was movement, joint surface anatomy and the gait cycle.
Joining the dots – the Flow Motion ModelTM
The documentation process that underpins AiM began when I met a Biomechanics expert called Hamish Wolfenden, who specialised in the Windlass Mechanism (explains arch function in static positions, when the arch is able to deform without resistance). Our mutual interest at the time was ski
boot fitting and he introduced me to the gait cycle and how he used it to help formulate the perfect orthotic for ski boots and running shoes.
As he shared his theories and experience, I was able to structure my own thinking and explain to him what the whole body is doing at any particular moment in the gait cycle. This is how I came to document the movement patterns that occur in the whole body at each of his four key stages in the gait cycle. I then went a step further to document a fifth grounded phase and two swing phases before completing the model with an additional five phases that were taking place between the seven. This comprehensive twelve phase analysis is AiM’s central Flow Motion ModelTM.
I thought I knew my biomechanics of human movement before I built the model and yet the act of doing so opened my eyes to a world of undiscussed information and perhaps some falsehoods as well. The world of closed chain biomechanics (analysis when weight bearing) is very different to the open chain biomechanics (examination when non weight bearing) that the majority of us are being taught. For me, it began to break the mould of traditional anatomical thinking.
To give an example, let us think about general rehab for a sprained ankle. What’s the advice? The front page of a google search simply states “Rest, Ice, Compress, Elevate” (other than recommendations to visit a local podiatrist of course!). However, it’s more than likely that a sprained ankle will have involved some structural damage to the area, which will then continue to prevent the affected joints from moving in the way they once could. If so, this is likely to have a natural knock-on effect up the kinetic chain and appropriate rehab needs to address this.
If it doesn’t, you may find years down the line that the ankle sprainee visits your clinic with knee and low back pain. It’s unlikely you would take the, by now, age old ankle sprain into account (the patient may even have forgotten about it by then) and yet it could hold the key to everything.
So how would AiM help? If following an ankle sprain you can no longer pronate your foot very well, the limitations in movement will lead to a consequential effect throughout the leg all the way up into the pelvis and onto the spinal column as well. As a result, the body can become very one sided, leading to physical discomforts across the body and a string of potential clues to lead you to the underlying issue, even if the restriction in the foot is not immediately obvious.
S Podiatry Review Spring Issue 2022 | 31
Fundamentally, the body organises itself in a particular way when it is moving and if part of that movement is taken away or restricted then a whole range of movement opportunities for that person are also taken away from them.
I have long seen my role as an AiM practitioner being: 1) To uncover what movements are lacking in the system 2) To determine what the knock-on effect has been to surrounding structures using the links established in the Flow Motion Model and 3) To then restore those movements to reflect the natural movements we see in the gait cycle through specific AiM exercises.
So, when the foot is flat on the floor we know: What we would like the foot bones to be doing What the ankle, knee and leg should be doing How the pelvis would respond What its impact on the spinal column would be and how that would affect the shoulder girdle, cervical spine and carriage of the skull.
The model therefore describes one whole body shape per gait phase that we should all be able to achieve in that moment.
A great question then to check is whether or not our body is capable of achieving that shape? And are we in balance i.e. does our body access the equal and opposite shape when the other foot is on the ground? If you consistently access a phase differently on your left foot to your right foot then this will have far reaching consequences for your whole body. They may not be noticed today but could be predicted, once you have identified the restriction.
Before AiM treatment,left, & after AiM treatment, right. Pressure is more balanced especially in the left heel.
What does the Flow Motion Model tell us?


The Flow Motion model takes a snapshot of the gait cycle, call it a phase, and details each and every joint motion and direction of bone motion that should be taking place simultaneously throughout the whole body. By breaking this down into each plane of motion at each joint we obtain a very detailed and informative ‘photograph’ of that moment in the cycle.
As an example, a pronated leg is likely to incorporate a flexed knee, push a pelvis away in both the frontal and transverse planes while creating a greater amount of anterior tilt in the same side ilium. The Flow Motion Model allows us to predict that this will naturally contribute to changes in the spinal column such as lumbar extension and counter rotation to the pelvis and call the opposite shoulder to internally rotate. If you are capable of accessing this equally on both sides you will notice that you are free to move your pelvis, spine and shoulder girdle in both directions in all planes of motion. Balance and freedom in the body achieved

A race against time
A single footstep lasts between 0.6 and 0.8 seconds, this is not a lot of time for a lot of movement to take place. Yet we know that in a single footstep, each and every bone and joint must travel toward both ends of its movement potential (e.g. flexion and extension) and in all three dimensions at least once.
So, if you over rotate something in one direction, the chance of mirroring this in the other direction within such a small window of time is virtually impossible. Thus, excess movement in one direction is always balanced by lack of movement in another.
F 32 | www.iocp.org.uk ARTICLE (continued)
Plane Colour Sagittal Red Frontal Green Transverse Blue KEY
For example, if one foot pronates more than the other then this affects the timing of the movement through the other phases of the gait cycle. This in turn changes the movement possibilities at the different structures as we go up the chain. It’s likely for instance that the pelvis rotates more in one direction than the other direction (away from the pronating foot) and may as a result be experiencing lower back discomfort. Whilst they might first notice the back pain, AiM tells us that they really need to pay attention to their feet.
This is just an example of the type of whole body insight that can come from observing the body in motion and studying the Flow Motion Model. It’s the subtle changes in joint alignment as the whole body compensates for small changes that can highlight where the real need for treatment lies.

particular motion. For instance, your adductors are perfectly set up to join in and decelerate hip extension too.
Joints ACT: Muscles React
This rule states that, in motion, joints act but muscles react. As a result, it is the quality of joint motion that determines the effectiveness of the muscle. For instance, if your hip doesn’t flex very well, it will fail to create a decelerative demand on the glute muscle and the contraction response will be negligible. Working that glute harder and harder into extension is unlikely to have the desired goal as the act of glute contraction fails to teach the hip to flex. Educating the hip to flex, then, which is simply part of a whole-body motion, coupled with foot pronation, is what will eventually remind the glute of its responsibilities around that hip.
Joints give muscles something to do
Joints give muscles something to do… it’s a key term I have lived by for years and is highly impactful. Now consider all of the joints in the human foot. How likely is it that they are capable of accessing all of their movement potential and creating an opportunity for those foot muscles to get back on board? Observing the feet in the closed chain, when the foot is on the ground and the body is moving above it, as well as in the open chain whilst sat on your podiatry chair brings about a whole different level of appreciation for what the foot has to undergo in every step that it takes.
For a full understanding of the process including a treatment example visit https://www.youtube.com/watch?v=EBHCvy9PHnc
AiM’s key rules
We have some key rules underpinning AiM, the first two of which oppose conventional wisdom.
Muscles lengthen before they contract
This rule states that, in motion, muscles lengthen before they contract. Muscles lengthen to decelerate the opening of a joint in a bid to protect it from excess. It is from this lengthened position that the muscle then begins to contract and bring the joint back towards its midline and beyond. As it approaches the opposite end range, the opposite set of muscles will now become responsible for decelerating this new dimension of motion.
In motion, think about the glutes decelerating hip flexion while the psoas decelerates the extension. Together they work as a team to achieve that outcome. You will also find that more than one muscle is involved in the deceleration of any joint motion even if they are not known for that
Next time…
I’ll be discussing more specific information on this approach for the feet in the next issue but some key takeaways worth considering beforehand is that the majority of the muscles in the foot are supinator muscles. Given that muscles must lengthen before they contract in motion, it makes sense that we must pronate the foot to give these muscles their best opportunity for a supinatory contraction.
To create the perfect environment for a foot pronation to take place we must teach the bones of the foot to move into the optimal position of pronation. This will kickstart the muscles of supination and these muscles will contract against the movement to initiate a shortening from their lengthened state. This decelerates the motion of pronation. Remember that the better a foot is at moving from a pronated foot shape to a supinated foot shape the more likely the foot will become more centred in its resting state.
Podiatry Review Spring Issue 2022 | 33
Allied to these two key rules are a set of wider (but fundamental) observations:
A joint rests centred only when it can access both end ranges of its anatomical structure
A hip that can flex but not extend will rest flexed
A foot that pronates but cannot supinate, will rest pronated
Only when a joint is centred at rest, can it have no tension or compression placed upon the structure
As soon as movement away from its resting centre is experienced, joint closure and joint opening takes place which knocks on to shortening and lengthening the surrounding tissues
Resting in non-centred spaces, leads to compromised joint and muscle function

Naturally the further away from centre you rest, the greater the risk to the structures.
As you can see, it’s potentially a different way of thinking about biomechanics and gait and it’s apparent in all movement even something as simple as a squat. Lowering into a deep squat demands a deceleration from the glute muscles as they move into a lengthened position. They then contract back as you return to a standing (rest) position.
In summary
So, to summarise what we have been talking about, AiM provides an alternative approach to biomechanics based on what the joints of the human body do and when they do it during the gait cycle.
Some of its key elements are:
1 Flow Motion Model – 12 detailed phases of joint mechanics through the gait cycle
2 Joint surface anatomy determines the movement possibilities from one bone to the next resulting in a clear explanation of one structure c ommunicates movement to the next
3 Muscles lengthen before they contract muscles contract fully from a lengthened position and as such serve to decelerate eccentrically structures as they move away from centre
4 Joints ACT: Muscles REACT the ability for a joint to move optimally is what optimises muscle function (not the other way around)
5 Re-educating joints to move well and in sequenced movement patterns enables a person to reorganise their own structure and move through problems they may have been stuck in for years.
When we apply these ideas to the human body, we can use the Flow Motion Model to help us understand the global movement patterns that a person is unable to access (or accessing too much) that is causing their problem. This allows us to identify a restricted gait phase and we can then use that phase to guide us to specific joint interplay that is problematic in the system. Finally, we can use human movement (in the form of specific AiM exercises) to restore or re-educate the lost patterns so that the person can reorganise their system to take pressure off the joints and soft tissue that was flashing the alarm bells of concern. We will explore some of these exercises further in my future articles.
Ultimately, a deeper understanding of biomechanics opens up a new perspective that can help practitioners from all branches of the healthcare industry, including podiatrists who wish to venture beyond podiatry.
AiM is a specialist therapy and individuals should undertake and qualify in the course before any treatment commences.
About Gary Ward
Gary Ward is the founder of Anatomy in Motion and creator of the Flow Motion Model. As well as treating patients directly, including a number of professional athletes, he has been teaching AiM for the past fifteen years, to bodyworkers from all areas of the industry in all corners of the world.
Through mapping AiM’s Flow Motion Model he has given hundreds of practitioners and thousands of patients the opportunity to better understand the cause of their problems and to overcome them using three-dimensional movement to restore any lost or forgotten movement patterns.
Gary has written a book all about the AiM philosophy entitled ‘What the Foot?’ and has contributed to a number of other books and articles on the subject. In 2016, he took part in an episode of ‘Doctor in the House’ for the BBC assisting his friend Dr Rangan Chatterjee.
For more information and to undertake either a lower limb or upper body courses, see website: www.findingcentre.co.uk instagram: GaryWard_AiM
34 | www.iocp.org.uk ARTICLE (continued)
A
Colin J. Craig - husband, Dad, chiropodist & podiatrist
On 25th August 2021 Colin Craig, devoted husband, Dad and chiropodist/podiatrist went safely home.

‘Mr Craig’ as his patients referred to him was in private practice in Antrim for over 50 years, having established his surgery in May 1966. He was a much-loved chiropodist/ podiatrist and many of his patients became his friends and then family friends. He was always enthusiastic about chiropody/podiatry and dedicated to the Institute of Chiropodists & Podiatrists undertaking the role of Chairman of the Northern Ireland Branch for many years. He thoroughly enjoyed his working life, only stopping through illness.
My Mum and I were blessed to have the most amazing Dad and husband, who we loved absolutely. He was a character who made everything colourful and lived life to the full, enjoying every minute. He was passionate about Italy, painting, Alfa Romeos and so much more. Life has lost its sparkle without him.

It is with Great sadness we share the news of the death of our esteemed colleague Colin Craig. Colin was a lifelong member of the Northern Ireland Branch of which he dedicated his time serving as chairman on numerous occasions and most recently until his retirement in late 2019.

Colin was always a very funny, positive man. We will miss his humorous stories and will always remember him with fondness. Our thoughts and prayers are with his wife and daughter. Rest in peace Colin.
Former Northern Ireland Branch Secretary
OBITUARY
Paula McDonnell
Podiatry Review Spring Issue 2022 | 35

36 | www.iocp.org.uk
Wolverhampton Branch Meeting - Sunday 9th January 2022

The meeting went well, and for the educational part one of our branch members (Kim Averall), gave us an inter esting and informative PowerPoint presentation entitled “Occupational Therapy (its influence on my practice)”.
Those present found it interesting as we were told how you should not just look at the patient’s problems but asses the whole patient and their surroundings, looking for trip hazards, steps and stairs.
Also, are they able to look after themselves at home, checking their psychological state (depression, aggression and short- and long-term memory).
We were told how to correctly set walking sticks to the correct height to help with balance and walking. We were shown what disability aids were available to help and were given contact details for groups that can also be of help.
After the meeting finished, we had our post-Christmas get together at a local restaurant in the village.
David Collett Wolverhampton Branch Secretary
Podiatry Review Spring Issue 2022 | 37 BRANCH NEWS
Wolverhampton Branch held their Branch AGM and first meeting of the year on Sunday 9th January 2022.
SVTS Chiropody Drill repair and sales
We offer an excellent competitive and efficient repair service for all makes of Podiatry/chiropody Nail drills. Berchtold, Hadewe, Suda, Footman, Podiacare, Podo Tronic and Podo Pro EVO-30,40&50 drills. We sell Berchtold S35/ S30, Hadewe, EVO 30,40.50 Dust Bags from £1.25 – £2 each. WE ALSO BUY UNWANTED DRILLS.
Unit 255 Stratford Workshops, Burford Road, London E15 2SP Contact us on 0208 5190044 or www.chiropodydrillrepair.co.uk
Chiropodist/ Podiatrist required in Heswall, Wirral
We are situated in Heswall, Wirral. We are a busy multi-discipline clinic in the heart of a thriving village.
Our clinic is exceptionally busy with five chiropodists and full-time reception staff. The position is offered with hours to suit applicant.
The successful candidate must be personable, not afraid of being busy and have great attention to detail. In return they can earn £200-300 per day.
This is a self-employed position and payment is on a fee sharing basis.
Tel: 01513 429665 for further information
Podiatrist required for busy clinic near Lahinch, Co. Clare, Ireland
Immediate start for a person with a BSc in Podiatry. The preferred candidate should be experienced and have an ambition to run their own practice.
There will be an opportunity to lease this thriving clinic in the near future, thus offering the right person, a fantastic chance to own this already well-established business and to live in an area of outstanding natural beauty.
Lahinch on the Wild Atlantic Way, with its slow pace of life, offers a great place to live, work and play. It has fantastic beaches, golf courses, shops and restaurants. All the pubs offer local Irish food and traditional music evenings with lots of Craic. Close by are the Cliffs of Moher, the Burren National Park, a world heritage site renowned for its rare native plants and flowers. Experience the enthralling beauty of the limestone pavements and curious rock formations and explore the hiking trails of Caher Valley, Lochavalla Hoop or picnic on Mullaghmore after a hearty climb.
Salary package or lease terms negotiable. Please apply via e-mail with up-to-date CV to Phil McMahon at macmahon.phil@gmail.com or ring me for an informal chat on 00353871617697
38 |
CLASSIFIED ADVERTS
www.iocp.org.uk
Please
all products advertised in the Podiatry Review and on the Website are accepted by the
and
on the basis of a commercial advertising
and purchasers
out
as to the suitability of such products for their
the
does not imply our
To place an advert here or for more information please email julie@iocp.org.uk Diabetic Foot Module Course 10th – 14th October 2022 At The Wellcome Collection Euston Road, London Intensive update course for specialist practitioners. For more information, please email diabeticfootmodule@gmail.com
note:
Institute of Chiropodists
Podiatrists
service
should carry
their own assessment
own specific needs. Acceptance of the advertisement by
Institute
endorsement or approval of the product.
APRIL 2022
3 Cheshire, North Wales Branch Meeting
The Dene Hotel, Chester
Contact Michele Allison on 07766 700027 or email missminou@hotmail.co.uk
7 Sheffield Branch Meeting
At 7.30pm Via Zoom
Contact Helen on 07789 025022 or email hrawse@live.co.uk for further information
10
Leeds Branch Meeting
9.30am at St Mary’s Social Club, Melton Street, Batley. WF17 8PT
Contact Caroline on 07583 934468 or email hello@ chiropodyandfoothealth.co.uk
24 Wolverhampton Branch Meeting and AGM
At 10am at the Reading Rooms, Market Street, Penkridge, Staffs. ST19 5DH
First aid training
Contact: David on 01785 716607 or email djcollett@hotmail.co.uk
27 London Branch
At 7.30m via Zoom
JUNE 2022
26 Cheshire, North Wales Branch Meeting
Venue TBC
Contact Michele Allison on 07766 700027 or email missminou@hotmail.co.uk
JULY 2022
14 Sheffield Branch Meeting
At 7.30pm Via Zoom
Contact Helen on 07789 025022 or email hrawse@live.co.uk for further information
17 Wolverhampton Branch Meeting and AGM
At 10am at the Reading Rooms, Market Street, Penkridge, Staffs. ST19 5DH
Speaker to be arranged
Contact: David on 01785 716607 or email djcollett@hotmail.co.uk
27
London Branch Meeting
At 7.30pm Via Zoom
Contact Sarah on 07790 717833 or email footwoman@gmail.com
SEPTEMBER 2022
NOVEMBER 2022
17 Sheffield Branch Meeting
At 7.30pm Via Zoom
Contact Helen on 07789 025022 or email hrawse@live.co.uk for further information
JANUARY 2023
8 Wolverhampton Branch Meeting & AGM
At 10am at the Reading Rooms, Market Street, Penkridge, Staffs. ST19 5DH
Contact: David on 01785 716607 or email djcollett@hotmail.co.uk
25 London AGM Meeting
At 7.30m via Zoom.
Contact Sarah on 07790 717833 or email footwoman@gmail.com
SOUTH WALES AND MONMOUTH BRANCH
Meetings are taking place via zoom, members who would like details of the next meeting and wish to attend please contact Esther on 01656 740772 or email estherdanahar@ yahoo.co.uk
Please email julie@iocp.org.uk with information about Branch
Meetings whether face to face or via zoom etc.
Keep your Branch members up to date so they can attend.
Meeting
Contact Sarah on 07790 717833 or email footwoman@gmail.com
MAY 2022
11 IOCP AGM at Primary Care
At the Birmingham NEC at 6:00pm
11 & 12 Primary Care
At the Birmingham NEC
29
Leeds Branch Meeting
9.30am at St Mary’s Social Club, Melton Street, Batley. WF17 8PT
Contact Caroline on 07583 934468 or email hello@ chiropodyandfoothealth.co.uk
11 Cheshire, North Wales Branch Meeting
Venue TBC
Contact Michele Allison on 07766 700027 or email missminou@ hotmail.co.uk
OCTOBER 2022
9 Wolverhampton Branch Meeting and AGM
10am at the Reading Rooms, Market St, Penkridge, Staffs. ST19 5DH Speaker to be arranged
Contact: David on 01785 716607 or email djcollett@hotmail.co.u
26 London Branch Meeting
7.30pm via Zoom.
Contact Sarah on 07790 717833 or email footwoman@gmail.com
Podiatry Review Spring Issue 2022 | 39
DIARY OF EVENTS


























































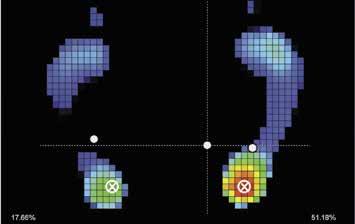






































































 Andrew Williams Chair Board of Education
Andrew Williams Chair Board of Education


























 By
By











 of Medicines
of Medicines













 Stephen Willey Ex Chairman, Board of Ethics IOCP and Sheffield Branch
Stephen Willey Ex Chairman, Board of Ethics IOCP and Sheffield Branch