MARCH-APRIL 2025

Winners of the Healthcare Design Awards 2025 are revealed
Experts predict healthcare property market trends for 2025
Trailblazing community hospital voted best in England by patients








MARCH-APRIL 2025

Winners of the Healthcare Design Awards 2025 are revealed
Experts predict healthcare property market trends for 2025
Trailblazing community hospital voted best in England by patients







2025 has kicked off with two major announcements impacting the healthcare estate — the results of the review of the New Hospital Programme (NHP), and the publication of the latest Estates Returns Information Collection (ERIC) data.
The NHP — a pledge by the previous government to deliver 40 new or improved hospitals by 2030 — will now take more than a decade to deliver after the Labour-ordered review found the original plan was ‘behind schedule’, ‘unfunded’ and, therefore, ‘undeliverable’.

This admission, and the subsequent reordering of projects as part of a new three-wave, 10-year delivery plan, has led to criticism from trust chiefs who fear that already-dilapidated buildings will continue to deteriorate while they wait their turn.
You can read more about this in our news section ( p6).
We also cover the publication, late last year, of the 2023/24 Estates Returns Information Collection (ERIC) data.
The mandatory data collection is a critical instrument for collecting information related to the costs and operations of the NHS estate.
And it makes grim reading, showing a growing backlog maintenance crisis, with £13.8bn needed just to restore buildings and equipment to ‘acceptable’ levels.
In our report, we speak to Charlotte Wickens, policy adviser at The King’s Fund, about the issues facing healthcare estates managers who are having to balance a lack of funding with tough targets such as achieving net zero carbon ( p10).

About Jo: Jo is the editor of Healthcare Property, having joined Nexus Media in November 2023.
She has been specialising in design and construction best practice for the past 16 years, working on the Building Better Healthcare Awards and editing both
These issues are more evidence, if needed, that the healthcare estate needs capital investment — and quickly.
But that £13.8bn backlog maintenance figure is higher than the entire Department of Health and Social Care capital budget for this financial year.
This means tough questions will have to be asked and healthcare operators will need to work with the private sector moving forward.
But, despite this, innovation is still happening.
In this edition of Healthcare Property, we reveal the winners of the 2025 Healthcare Design Awards ( p44) and speak to the team behind Heatherwood Hospital, which has been named the best elective care centre in England by patients ( p36).
We also look at the impact of colour on healthcare environments ( p40), and explore why the UK is falling behind on the adoption of ‘rightsizing’ when developing senior living facilities.
Throughout 2025, Healthcare Property magazine will continue to bring you all the news and views from the sector, including, in this edition, a special report predicting the likely direction of travel for the property sector over the next 12 months ( p22).
Coming up in the next edition we will be looking more closely at infrastructure procurement and the NHS net zero carbon journey.
To contribute to these features, or to get in touch with us, please email joanne.makosinski@nexusgroup.co.uk
Jo Makosinski Editor, Healthcare Property
Building Better Healthcare and Healthcare Design & Management magazines.
She has a special interest in the design of public buildings, including schools, nurseries, colleges, hospitals, health centres, and libraries.

Chief executive officer
Alex Dampier
Chief operating officer
Sarah Hyman
Chief marketing officer
Julia Payne
Editor
Joanne Makosinski
joanne.makosinski@nexusgroup.co.uk
Reporter and subeditor
Charles Wheeldon
Advertising & event sales director
Caroline Bowern
Business development executive
Kirsty Parks
Head of content
David Farbrother
Head of marketing
Carrie Lee
Publisher Harry Hyman

We round up the latest big stories, including the results of the annual Estates Returns Information Collection (ERIC) data, and the findings of the government review into the New Hospital Programme
News on the latest design and construction projects from across the health and social care sectors

The critical role of ‘rightsizing’ for an ageing population, and how expanding the use of private patient units (PPUs) could help drive NHS efficiencies
34-35


Health think tank, reform, reveals its vision for the Hospital of the Future, plus the Centre for Mental Health calls for a radical reform of psychiatric inpatient care
Investor Publishing Ltd, 3rd Floor, 10 Rose & Crown Yard, King Street, London, SW1Y 6RE
Tel: 020 7104 2000
Website: www.healthcare-property.com
3029-0627 © Investor Publishing Limited 2025
The views expressed in Healthcare Property are not necessarily those of the editor or publishers.

36-42
We speak to the architects behind Heatherwood Hospital, which was recently named the best in the UK by patients; explore the impact of colour in healthcare settings; and look at how modern methods of construction are delivering topquality facilities, faster

22-27
Real estate leaders predict what is in store for the health and care property sector in 2025
Unveiling the winners of the 2025 Healthcare Design Awards
NHS Shared Business Services launches new soft facilities management procurement solutions, and why fire safety should not be overlooked
48-50 Environmental
Exploring Scotland’s approach to net zero carbon in the NHS estate

Health leaders respond to the findings of a government review of the beleaguered New Hospital Programme
Hospital leaders were ‘right to be sceptical’ over funding for 40 new hospitals as the Government describes the original timetable for the New Hospital Programme (NHP) as ‘unrealistic’ and admits it may take more than a decade to deliver the much-needed improvements.
In a statement last month following an urgent review of the NHP ordered after Labour’s victory at the General Election, ministers admitted that delivery of all planned schemes could take far longer than the previous government’s 2030 target.
And this has led to criticism from trust leaders who fear further degradation of buildings and a negative impact on staff and patients.
A new, ‘credible’ timeline for delivery will ensure staff and patients around the country have access to the facilities they desperately need as soon as possible, the
Government said.
It follows a review of the scheme, which found that the previous government’s commitment to deliver 40 new hospitals by 2030 was ‘behind schedule’, ‘unfunded’ and, therefore, ‘undeliverable’.
In its annual report, published last week, the Infrastructure Projects Authority (IPA) also deemed the previous scheme ‘unachievable’, rating the programme as ‘red’ and highlighting major issues including with the schedule and budget.
But an independent IPA review has upgraded the programme from a ‘red’ to an ‘amber’ rating, thanks to the action being taken to improve deliverability.
In May 2023, for example, the previous government announced that the programme was backed by over £20bn of investment.
However, this funding was never delivered. Labour’s new plan will be backed with £15bn of new investment over consecutive five-year waves, averaging £3bn a year.
Wes Streeting, Health and Social Care Secretary, said: “The New Hospital Programme we inherited was unfunded and undeliverable.
“Not a single new hospital was built in the past five years and there was no credible funding plan to build 40 in the next five years.
“When I walked into the Department of Health and Social Care, I was told that the funding for the New Hospital Programme runs out in March.
“We were determined to put the programme on a firm footing, so we can build the new hospitals our NHS needs.
“Today we are setting out an honest, funded, and deliverable programme to rebuild our NHS.”


investment during the 2010s leaving some hospitals with roofs that have fallen in and leaking pipes which freeze over in winter.
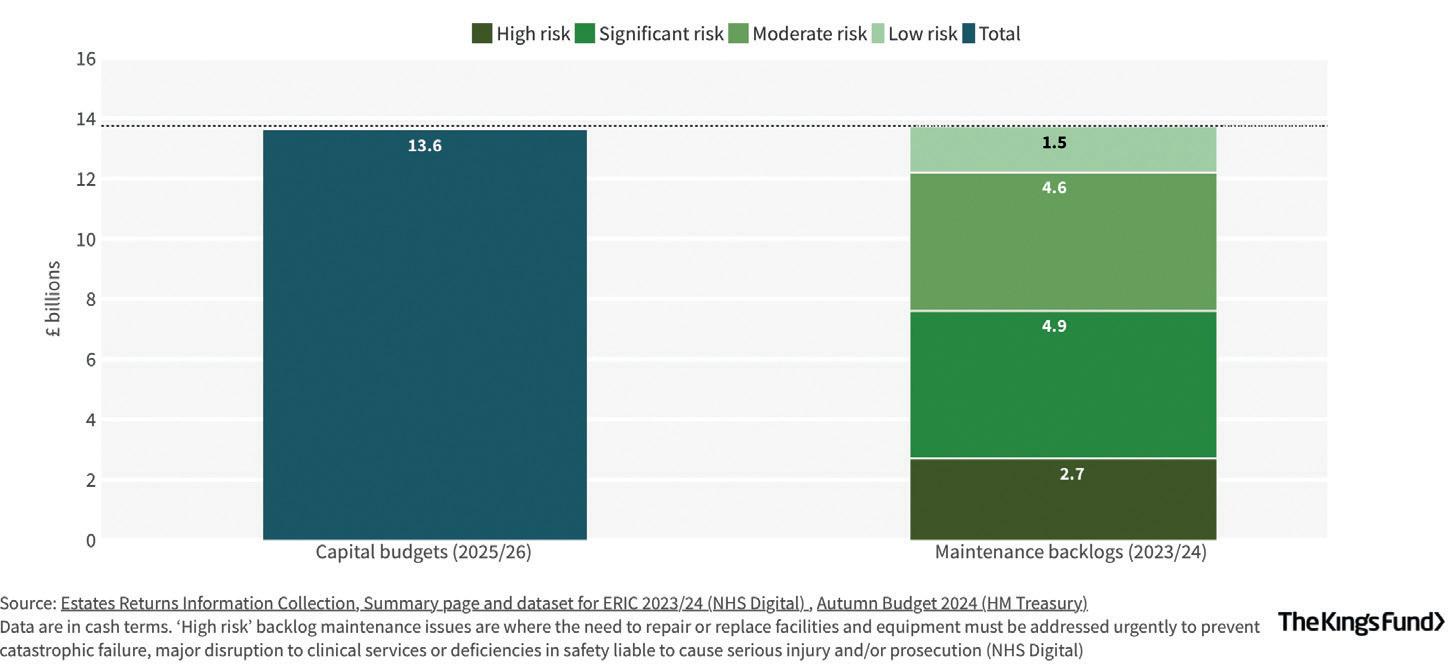
At the Budget in November, the Chancellor, Rachel Reeves, announced that health capital spending in the NHS is set to increase to record levels of £13.6bn in 2025/2026.
For schemes that were out of scope of the review, those already with approved full business cases will continue as planned and are already in construction (wave 0).
The remaining schemes will be allocated to one of three wave groups:
• Schemes in wave 1 are expected to begin construction between 2025-2030. These schemes include hospitals constructed primarily using reinforced autoclaved aerated concrete (RAAC), and have been prioritised as patient and staff safety is paramount
• Shemes in waves 2 are expected to begin construction between 2030-2035
• Schemes in wave 3 are expected to begin construction between 2035-2039 Hospitals in later waves will be supported on their development and early construction work before then to ensure they are ready for main construction.
And the plan for implementation sets out a clear pipeline of schemes to be delivered over the next decade and beyond.
The NHP will continue to work closely with industry to support construction, develop relationships, and secure investment within the supply chain, the Government said.
Morag Stuart, chief programme officer for the New Hospital Programme, added: “This provides certainty on the next steps for the New Hospital Programme.
With one of the largest reported maintenance backlogs in the country (amounting to £439m), the NHP investment is desperately needed, and sooner rather than later, as the current condition of our estate limits our ability to provide the environment that our patients and staff deserve
“We will continue to work with local NHS organisations to deliver improvements to hospitals across England, including making best use of new technology and improving layouts and ensuring future hospitals are designed to meet the needs of patients and staff.”
The New Hospital Programme is just one part of the Government’s wider commitment to transforming the NHS estate.
Over £1bn has been set aside to make inroads into the existing backlog of critical maintenance, repairs, and upgrades; while £102m has been dedicated for upgrades to GP surgeries across England as a first step towards transforming the primary care estate.
Among the hospitals impacted by the review are the Royal Preston Hospital, operated by Lancashire Teaching Hospitals NHS Foundation Trust; and Royal Lancaster Infirmary, run by University Hospitals of Morecambe Bay NHS Foundation Trust.
Following the review, construction work on a replacement Royal Lancaster Infirmary is due to begin between 2035-2038; while
work on the new Royal Preston Hospital is expected to start between 2037-2039.
Aaron Cummins, chief executive of University Hospitals of Morecambe Bay NHS Foundation Trust, said of the announcement: “Any delay to the delivery of a replacement new hospital for the Royal Lancaster Infirmary is disappointing, but we accept the need for a fully-costed and deliverable timeline of investment through the New Hospital Programme.
“While this may not be the news local communities wanted, we hope that the outcome brings some certainty that patients and NHS colleagues will get the new hospital that they deserve.”
Nottingham University Hospitals NHS Trust (NUH) also has two projects within the programme — the National Rehabilitation Centre and ‘Tomorrow’s NUH’.
The National Rehabilitation Centre was not included in the review as it is already under construction and it will continue to go ahead as planned.
But the Government has announced that the Tomorrow’s NUH programme will face considerable further delays and

commencement of the main scheme of work will not be allowed to begin until at least 2037.
The news was met with ‘disappointment’ from trust bosses who fear the impact on staff and patients.
Anthony May, trust chief executive, said: “While we welcome the Government’s ongoing commitment to Tomorrow’s NUH (TNUH), we are very disappointed that the review of the New Hospital Programme means significant delays to the scheme.
“This will not only considerably impact our patients and staff for the coming years, but will also have a huge impact on our wider communities across the region.
“This will mean a significant delay to building a new Centre for Women, Children and Families for Nottingham and our cancer patients will have to wait an additional decade to receive treatment in a bespoke cancer care building.
“Nottingham will also continue to be one of the only acute hospitals in the country without a helipad and we will not be able to build the much-anticipated multi-storey carparks at NUH for many years.
“With one of the largest reported maintenance backlogs in the country (amounting to £439m), the NHP investment is desperately needed, and sooner rather than later, as the current condition of our estate limits our ability to provide the environment that our patients and staff deserve.”
Health think tank, The King’s Fund, also weighed in on the announcement, with its director of policy, partnerships, and events, Siva Anandaciva, telling Healthcare Property:
“This review confirms that hospital leaders were right to be sceptical that there was enough funding to deliver the 40 new hospitals by the 2030 deadline.
“The construction industry has not been immune from rising inflation and labour shortages over recent years, and it is welcome that new plans announced today aim to be more realistic, including a long-term outline for how the programme will be funded.

economy — many hospitals are already spending significant amounts of taxpayers funding trying to maintain sub-standard buildings — and they will have to keep doing so in the years to come.
“Additionally, the scale of the crumbling NHS estate is far wider than the 40 rebuilds on the New Hospital Programme.
“Much of the mental health estate is some of the oldest within the NHS and it is reported that an estimated one in five of England’s GP premises pre-date when the NHS was formed in 1948.
‘However, it will be devasting to staff and patients to hear that plans to rebuild many local hospitals will be kicked so far into the long grass.
“It is clear that the knackered condition of some NHS buildings and equipment in both hospital and out-of-hospital settings is harming patients and staff and hampering attempts to improve NHS productivity.
“Pausing or delaying plans to rebuild hospitals is also very likely to be a false
“And, while £1bn was earmarked in the recent Budget for the most-critical maintenance issues in NHS hospitals, there is a £13.8bn maintenance backlog for buildings and equipment.
“The result is poorer patient care and staff experience because of multiple IT failures, flooded corridors, dangerous roofs, unreliable diagnostic equipment, and substandard layouts that create overcrowding in A&E departments.” n
It is clear that the knackered condition of some NHS buildings and equipment in both hospital and out-of-hospital settings is harming patients and staff and hampering attempts to improve NHS productivity


In this article we look at the findings of the latest Estates Returns Information Collection (ERIC) data, which reveals the true state of NHS buildings
The poor physical state of NHS buildings has become ‘a severe hindrance’ to plans to increase productivity, according to health think tank, The King’s Fund.
Responding to the release, in December, of the Department of Health and Social Care’s latest Estates Returns Information Collection (ERIC) data — a critical instrument for collecting information related to the costs and operations of the NHS estate — Charlotte Wickens, policy adviser at The King’s Fund, said patients and healthcare leaders were ‘in limbo’, with NHS maintenance backlog data showing £13.8bn will need to be invested to restore buildings and equipment to acceptable levels.
This figure is higher than the entire Department of Health and Social Care capital budget for this financial year.
Wickens said: “The scale of the
maintenance backlog means there will have to be some difficult decisions about which buildings and what equipment is prioritised for investment at the upcoming comprehensive spending review.”
The provisional ERIC data for 2023/24 is a mandatory data collection for all NHS
trusts, including ambulance trusts, and comprises information relating to the costs of providing and maintaining the NHS estate, including buildings, maintaining and equipping hospitals, the provision of services such as laundry and food, and the costs and consumption of utilities.
The scale of the maintenance backlog means there will have to be some difficult decisions about which buildings and what equipment is prioritised for investment at the upcoming comprehensive spending review
Key takeaways from this year’s collection include:
• The total cost of running the NHS estate was £13.6bn — up 9.25% on the previous year
• The total cost to eradicate backlog maintenance (BLM) is £13.8bn — up 18% on previous year. The estimated cost to eradicate ‘high risk’ BLM is £2.7bn, ‘significant risk’ BLM is £4.9bn, ‘moderate risk’ is £4.6bn, and ‘low risk’ stands at £1.5bn, all showing an increase on the previous figures
• The number of trusts with an Estate Development Strategy is down from 211 to 209
• Estates and Facilities RIDDOR (The Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 2013) incidents were up by 3.8% to 7,966. Those related to critical infrastructure risk stood at 1,584, down nearly 2% on the previous year. In particular, flood occurrences triggering a risk assessment increased by 28% to 358
• The number of fires recorded was down 19% to 1,102, but false alarms were up by nearly 5% to 23,651. 6,049 of those led to emergency services callout and there was one reported death and 21 injuries, though no patients sustained injuries during evacuation
• Gross internal floor area of NHS buildings stands at 27.5 million sq m — up 1.2%, while occupied floor area is 25.3 million sq m, an increase of 1.1%
• There has been no change in the number of single patient ensuite bedrooms, with 40,012 recorded, but a slight increase in isolation rooms from 1,892 to 1,907
• The cost of water and sewage was £101m — up 9%
• Waste costs were £180.5m — up 9.5%
• On a more-positive note, clinical service incidents due to infrastructure failures decreased by 4.8%
Commenting on the figures, Issy Whitelock, senior consultant at construction and facilities management specialist, Sewell Group, told Healthcare Property: “The newly-released provisional NHS ERIC data gives us a telling snapshot of the NHS estate’s current state. And, as you might expect, managing buildings, infrastructure, and costs is a growing challenge for NHS trusts.
“Total running costs increased, continuing the sizeable upward rising trend seen over the last four years, with these outpacing revenue growth and intensifying the financial strain on the service.
“Despite an increase in capital spending, reaching £11.2bn in 23/24, this only returns capital investment levels to where they were

Despite an increase in capital spending, reaching £11.2bn in 23/24, this only returns capital investment levels to where they were in 2010, after years of underfunding
in 2010, after years of underfunding.
“Compounding these pressures, the IFRS 16 accounting standard now requires leases to be included as capital expenditure, putting restrictions on an already-stretched capital budget, limiting available funds, and impacting NHS trusts’ financial flexibility.”
Wickens adds: “Many patients and staff alike will be familiar with the issues that come with the poor condition of the NHS estate, such as slow scanners, broken lifts, leaking roofs, and the relocating of services to work around dilapidated buildings.
“The neglect of the NHS estate led to 751 dangerous incidents to patients and staff, such as through equipment failures or infection outbreaks.
“The latest NHS maintenance backlog data shows £13.8bn will need to be invested to restore buildings and equipment to acceptable levels. That figure is higher than the entire Department of Health and Social
Care capital budget for this financial year. And this data only covers hospitals, much more would be needed to restore outdated GP practices and other primary and community care buildings.”
The figures reveal that the top 20 trusts with the highest BLM account for 30% of the total BLM across the NHS estate.
However, only nine of the 20 trusts with the most-critical infrastructure risks are included in the New Hospital Programme (NHP), highlighting a significant funding gap for urgent repairs and upgrades.
A welcome sign, according to Wickens, is that ministers have set about changing how NHS capital budgets are planned and set.
She said: “The recent budget earmarked a rise in capital spending, including £1bn for critical maintenance issues with NHS buildings, and a promise to set longer-term capital budgets so that NHS organisations can better plan for future modernisation.”
The neglect of the NHS estate led to 751 dangerous incidents to patients and staff, such as through equipment failures or infection outbreaks
• The total energy usage from all energy sources across the NHS estate was 11.1 billion kWh — down 0.86% on the previous data return
• Total energy costs stand at £1.4bn — up 16%. Total cost of electricity was £769m — up 21%
• The number of CHP units operated on site remains unchanged at 223
• The number of trusts operating a waste reuse scheme increased by 11% to 93. 155 trusts now have a waste manager and 125 have an energy manager Whitelock said: “Energy remains one of the NHS’s largest financial burdens, with costs rising by 13% this year, an additional £185m.
“While the proportion of these energy costs resulting from gas and oil dropped by 2% compared to previous years, these sources still make up a substantial 40% of total energy spending.
“This highlights the NHS’s continued heavy reliance on traditional energy sources, even as it seeks to move toward moresustainable options.”
She added: “Sustainability remains a key goal, with 76% of trusts creating estates development strategies to support some of these ambitions.
“However, many trusts face a tough choice: improve energy efficiency or manage rising costs.
“Progress is visible in some areas, with solar panel investments, EV fleets, and energy upgrades, though budget constraints limit larger-scale green projects.
“Seven Integrated Care Boards (ICBs) saw a reduction in their trust’s gas emissions by over 10%, and there’s been a 38% rise in trust-owned solar power consumption, which is promising.
“LED lighting is also expanding, though 1,778 sites still have less than 50% LED coverage. This could offer substantial benefits, but will need capital investment.”
And she warned that, with the added pressure of backlog maintenance costs, the challenge of achieving net-zero emissions across the healthcare estate could
be in jeopardy.
“This data paints a vivid picture of an NHS estate under growing strain, with rising costs across almost every area,” she said.
“Trusts are making difficult choices: fix urgent issues or invest in long-term transformations like digital upgrades and sustainability.
“It’s a tough call, and the risk is that sustainability projects may be sidelined in the short term and the forthcoming risks associated with the rising BLM and critical infrastructure risk continue to grow.”
• The total cost for cleaning services was £1.5bn — up 10.5%
• The number of cleaning staff rose by 0.4% to stand at 42,000
• The total cost of providing inpatient food was £0.8bn — up 5.6%
• Inpatient food ingredients cost increased by 21% to £291.7m
• The number of inpatient main meals requested increased by 3% to 143 million; meals provided to A&E and urgent care patients increased by 10% to 5.2 million; and staff/visitors meals served stood at 43 million, an increase of 10%
• The number of catering staff rose by 5.8% to stand at 17,900
• Food waste — the first time this had been recorded as part of the ERIC return — was 11,800 tonnes
• Parking costs rose by 6% to £77m.
Income generated from patient and visitor parking was £172m — up 18.5%; while income from staff parking fees was £70.5m — up by 51%
According to Whitelock and Wickens, the data shows a need to look more long-term at the NHS estate and to embrace technology.
Whitelock told Healthcare Property that Sewell Group had devised a tool to support trusts, adding: “One of the key takeaways from the 2023/24 ERIC data is that while estates costs are rising, many trusts struggle to pinpoint exactly where efficiencies can be made.
“This is where data can make a tangible difference in managing the estate and making data-driven decisions.
“We have developed a tool which allows trusts to make sense of their ERIC data to help tackle estate management and cost control challenges — by taking a deep dive into their ERIC data, our estates dashboard can help trusts benchmark performance both between their own sites and nationally, and identify opportunities for cost-saving or operational improvements.
“For instance, we recently worked with an NHS trust in England helping them uncover discrepancies in their data reporting, which were skewing their performance metrics.
“By correcting this, and advising them on how to better utilise their space, we were able to cut down their estates spend while improving the quality of care offered to patients.
“These kinds of insights are vital at a time when NHS funding is tight, and making sure every pound is used effectively can have a direct impact on patient services.”
The King’s Fund has also teamed up with Epsom and St Helier University Hospitals NHS Trust to shine a light on what the capital backlog means for them on a local level.
Every year the trust invests millions in improving its buildings so that staff can provide safe care to patients.
However, its estate is deteriorating faster than the trust can fix it, and the outdated infrastructure causes significant disruption to teams and patients.
In the last year the trust has had to postpone hundreds of operations due to ventilation issues in its theatres.
Even though the trust has now fixed the issue, it anticipates this happening repeatedly due to the deteriorating buildings.
Working with The King’s Fund the trust has devised a plan which will help deliver on the recommendations in Lord Darzi’s review to shift care closer to home and cut surgery waiting times faster. This includes:
• 85% of services staying at Epsom and St Helier hospitals with care closer to home, including urgent treatment, frailty, and ambulatory care services, which will better support the population immediately around St Helier
• Reducing waiting lists faster because Epsom and St Helier theatres will be dedicated to planned surgeries
• The trust’s new specialist emergency care hospital will be located next to The Royal Marsden hospital, helping to improve access to specialist oncology services and reduce the need for local patients to travel n
The Government has announced the biggest capital investment in hospices in a generation.
Over the next two years £100m in funding will help hospices provide the best care to patients and their families in a supportive and dignified physical environment.
Hospices for children and young people will also receive a further £26m revenue funding for 2025/26 through what was, until recently, known as the Children’s Hospice Grant.
Health and Social Care Secretary, Wes Streeting, said: “Hospices provide the care and support for patients and families at the mostdifficult time, so it is only right they are given the financial support to provide these services.
“This package will ensure they will be able to continue to deliver the compassionate care everyone deserves as they come to the end of their life in the best-possible environment.
“This investment will go towards helping hospices to improve their buildings, equipment, and accommodation. That will include refurbishing bedrooms and bathrooms for patients, providing comfortable overnight facilities for families, and improving IT systems to make it easier for GPs and hospitals to share vital data on patients.
“The money will also help towards improving garden and outdoor spaces so patients and their families can spend time outdoors in greener and cleaner spaces.”
Dr Amanda Doyle, NHS national director of primary care, added: “It’s absolutely right

that staff are able to provide high-quality and compassionate care to people at the end of their life in the best-possible environment, and this package will help them to do that.”
As part of the 10 Year Health Plan, the Government wants to shift healthcare out of hospitals into the community to ensure patients and their families receive personalised care in the most-appropriate setting.
And the palliative and end-of-life care sector, including hospices, will have a big role to play in that shift.
The capital funding will also support the Government’s shift from analogue to digital, through digital upgrades.
There are currently around 170 hospices that provide end-of-life care for adults, and around 40 which provide hospice care for children and young people in England, with some hospices providing care to both.
Toby Porter, chief executive of Hospice UK, said: “The announcement will be hugely welcomed by hospices, and those who rely on
their services.
“Hospices not only provide vital care for patients and families, but also relieve pressure on the NHS.
“This funding will allow hospices to continue to reach hundreds of thousands of people every year with high-quality, compassionate care.
“We look forward to working with the Government to make sure everyone approaching the end of life gets the care and support they need, when, and where, they need it.”
Responding to the announcement Ralph Coulbeck, chief executive at Haven House children’s hospice, called for the Government to support local decision-making on where the money should be spent.
He said: “It will be a relief to everybody in the children’s hospice sector to hear that the Children’s Hospice Grant is being maintained next year; this will help to support the vital care we provide to seriously-ill children and their families.
“It is also very positive to hear about the Government’s plans to invest significantly in the wider hospice sector; and we hope there will be as much flexibility as possible to determine locally how this new money is spent.
“This investment shows how government recognises the importance of integrating services to improve the treatment patients receive.”
Dudleys Consulting Engineers has secured four contracts with Torsion Projects to provide structural and civil engineering support for new care home developments in Durham, Chesterfield, Bradford, and Worksop.
The latest instructions follow the successful delivery of new care home and retirement living projects for parent company, Torsion Care, in Shipley, Bingley, Brighouse, Sleaford, Lincoln, and York, for which Dudleys provided full engineering consultancy support.
In Durham, Torsion Care has just completed the purchase of land at Mount Oswald in partnership with Banks Group.
Having supported the project through planning stages, Dudleys is now working onsite to deliver a purpose-designed, three-and-a-half storey care home offering 74 en-suite bedrooms with care facilities.
Torsion Care is also poised to deliver a new 72-bedroom care home in Chesterfield after securing planning consent subject to conditions.
Dudleys is supporting the redevelopment of the former Walton Works, including Grade II-listed mill buildings for the care home alongside new housing.
And, in Bradford, Torsion is redeveloping a brownfield site at Eccleshill to build a new 72-bedroom care home with associated ancillary services. Dudleys is providing engineering solutions to raise the site level by

Works are also due to commence on site next month in Worksop, where Torsion is building a new 70-bed care home within the expanding development at Gatefold Toll Bar in Worksop.
Watson Batty Architects is designing the scheme.
Paul Brownlow, director at Dudleys, said: “We are delighted to secure these further contracts with Torsion Care, cementing our role as a valued advisor for its fast-growing development plans.
“Our team is highly skilled in working with challenging brownfield sites that need varying levels of remediation from historic use or local environmental impact and we admire Torsion’s commitment to rejuvenating often-difficult sites to provide much-needed new community-focused facilities.”
Mercian Group will deliver a 68-bedroom care home development in Somerset for growing not-for-profit provider, Amica Care Trust.
abrdn will fund the development on behalf of a segregated client.
The 1.35-acre site is located within the Orchard Grove masterplan in the expanding town of Taunton in Somerset.
Mercian Developments identified the site’s potential for elderly care and achieved consent for a care home facility which, once built, will comprise 68 bedrooms with ensuite wetrooms.
Designed by KWL Architects, communal amenities will include a selection of lounge and dining spaces, flexible dayrooms for hobbies and activities, a hair salon, café, cinema/bar, sensory room, feature terraces on the first floor, and generous landscaped gardens.
The home will also have exceptional sustainability credentials, being 100% electric powered, and is expected

And it will meet a muchneeded demand for marketstandard wetroom beds in a catchment area which currently has a shortage of modern, quality provision.
Chris Towers, managing director of Mercian Developments, said:
“Mercian has been working with Amica to identify and deliver a flagship scheme for the trust in the Taunton area and is delighted to have completed this acquisition in partnership with abrdn, which will be funding the scheme.
“We can’t wait to get cracking on building what will be a fabulous new home for Amica and the surrounding communities.”
Keren Wilkinson, chief executive
are delighted to get this beautiful state-of-the-art care facility over the line, being so close to our head office, and are looking forward to offering our outstanding care services to the local Taunton community and beyond once completed.
“We are acutely aware of the pressures on the local authority and health services and are excited to be able to offer these modern facilities that will be able to offer excellent services to all.
“By integrating cutting-edge technology, we aim to empower residents to maintain their independence while ensuring they remain safe, comfortable, and well cared for.”
The deal was facilitated by
St George’s University Hospitals NHS Foundation Trust has received planning consent from Wandsworth Council for the development of one of the country’s largest renal units.
The plans will bring together specialist inpatient kidney care from across St Helier Hospital in Sutton and St George’s Hospital in Tooting, while strengthening outpatient services in local hospitals, clinics, and at home, where 95% of patients will continue to receive care and treatment.
Building the new unit, and freeing up space at St Helier, will help pave the way for St George’s, Epsom and St Helier University Hospitals and Health Group (gesh) to deliver on plans to build a new Specialist Emergency Care Hospital in Sutton and modernise Epsom and St Helier Hospitals, part of the government’s New Hospital Programme.
Designed by BDP Architects, the six-storey building will deliver high-quality inpatient, outpatient, and dialysis facilities. This will include inpatient services for people on long-term dialysis, and more-complex care for

individuals needing specialist surgery such as a kidney transplant.
It has been designed following extensive engagement with patients and staff and will feature:
• A building of the highest environmental standards
• 81 beds, including enhanced care and daycare beds
• 72% single rooms with ensuite bathrooms
• 24 acute dialysis stations, including eight single rooms
• Landscaped gardens, including spaces for people with reduced mobility
• Dedicated ambulance parking bays
Closely-located blue badge parking spaces
Jordan Rundle, director of healthcare development and investment at Christie & Co, who said: “We are delighted to have worked with Mercian again on another successful turnkey care home development.
“This scheme has been thoughtfully designed to provide best-in-class accommodation for the growing elderly population in Taunton, with very high energy efficiency and environmental credentials.
“Amica Care Trust is well placed to operate the scheme, having an excellent reputation in the local community and being committed to providing the best care and support through its dedicated and highly skilled team.
“We are looking forward to seeing the scheme come forward for construction and becoming a landmark development in Orchard Grove masterplan.”
Christie & Co acted for Mercian and JLL acted on behalf of abrdn. The property was transacted at an undisclosed price.
and drop-off spaces
New footpaths and a widened pedestrian entrance will also be built, as well as curative spaces for public, patients, and staff.
The purpose-built, modern healthcare facility will be designed to offer better experiences for patients and staff, with improved access to other specialist services.
And the building will enable enhancements to be made to the main entrance and accessibility to St George’s from Blackshaw Road, leading up to the renal unit, ITU, and the Atkinson Morley Wing.
Dr James Marsh, group deputy chief executive and renal consultant at gesh, said: “Reaching this milestone is a huge achievement and means we’re a big step closer to transforming the care we provide to our kidney patients.
“This is a once-in-a-generation opportunity to bring together the best of our two excellent renal services in a state-of-the-art, purpose-built renal hospital at St George’s — and we’re ready to press forward and deliver on our plans.”
Construction has begun on an energyefficient Community Diagnostics Centre (CDC) in Hereford, which will provide a calming and reassuring environment for diagnostic imaging and testing.
Designed by Architype and Medical Architecture for Wye Valley NHS Trust, and being constructed by Speller Metcalfe, the £18m centre is part of a national initiative to boost NHS diagnostic capacity by providing CDCs in local communities across the country. By conveniently locating the new facility close to people’s homes, the service will be more accessible and will reduce the need for hospital visits.
It will also relieve capacity pressures and waiting times at hospital-based diagnostic facilities.
Alongside expertise in healthcare design, the design team members were selected for their knowledge and experience in designing to Passivhaus standards.
Passivhaus design standards combine principles such as high thermal efficiency, airtightness, and mechanical heat recovery to reduce carbon emissions and greatly improve a building’s energy performance.

Rooms are arranged using a set of standard templates, both for improved efficiency and so the building can be easily and cost-effectively adapted to accommodate future changes to service requirements.
This has the benefit of significantly reducing the operational costs of the building, providing long-term savings to the NHS estate.
These principles also provide a robust framework to easily achieve the trust’s other sustainability targets, including exceeding the NHS Net Zero Carbon Building Standard and achieving a BREEAM ‘Excellent’ sustainability rating.
In consultation with a wide range of NHS stakeholders, the building’s internal spaces have been designed to meet the specific technical and safety requirements of a cuttingedge diagnostic facility.
Spaces for MRI, CT, and X-ray imaging, which require protective shielding and heavy, vibration-sensitive items of equipment, are located on the ground floor. This ensures an efficient structural engineering solution can be adopted and enables easy access for patients from the public waiting and reception area.
Spaces for patients to consult with clinicians are provided on the first floor, alongside staff welfare facilities, where generous views and natural daylight create a positive environment for wellbeing.
A double-height atrium directs visitors towards the entrance with its bright, welcoming reception and waiting space.
This area is defined by natural finishes and a large-scale artwork creating an internal landmark which aids orientation on the ground and first floors.
This supports the use of simple and intuitive signage and wayfinding, removing unnecessary visual clutter and enabling the interior to adopt a more-familiar and lessinstitutional character.
The building’s interior has been designed with a calming palette of materials and finishes to support positive patient experiences, subtly comforting those who may otherwise be anxious.
Attention has also been paid to details that create a high-quality workplace to aid the recruitment and retention of NHS staff.
Externally, a black standing-seam metal cladding has been selected as the primary material for the elevations. This provides a contemporary interpretation of the local industrial context, while creating a distinct identity which aids navigation to the site.
As visitors approach the diagnostic centre, softer timber details become apparent within the outside canopy and the window and door reveals, while vertical timber cladding elements beneath the canopy frame the main entrance and provide a clear destination.
And all materials have been selected for their longevity and their ability to age well as part of a holistic sustainability strategy.
Mark Barry, director at Architype, said: “It is very exciting to be constructing another public building and further improving services in our local city, following a three-year period of innovation in the healthcare sector working alongside Medical Architecture.”
Mark Nugent, associate director at Medical Architecture, adds: “This building reflects the collaborative approach of the client, contractor, and the design team members, who have all strived towards the shared ambition of a moresustainable development approach which has the potential to reduce revenue costs, as well as carbon, across the whole NHS estate.”
And Alan Dawson, strategy and planning officer at Wye Valley NHS Trust, said: “Our patients deserve the highest-quality care, and this centre will be instrumental in speeding up the diagnosis of illnesses like cancer and heart disease to ensure they are treated more quickly.
“There’s no doubt that the new centre will lead to improved patient experience and outcomes and will contribute to shorter waits for people from Herefordshire and beyond.”

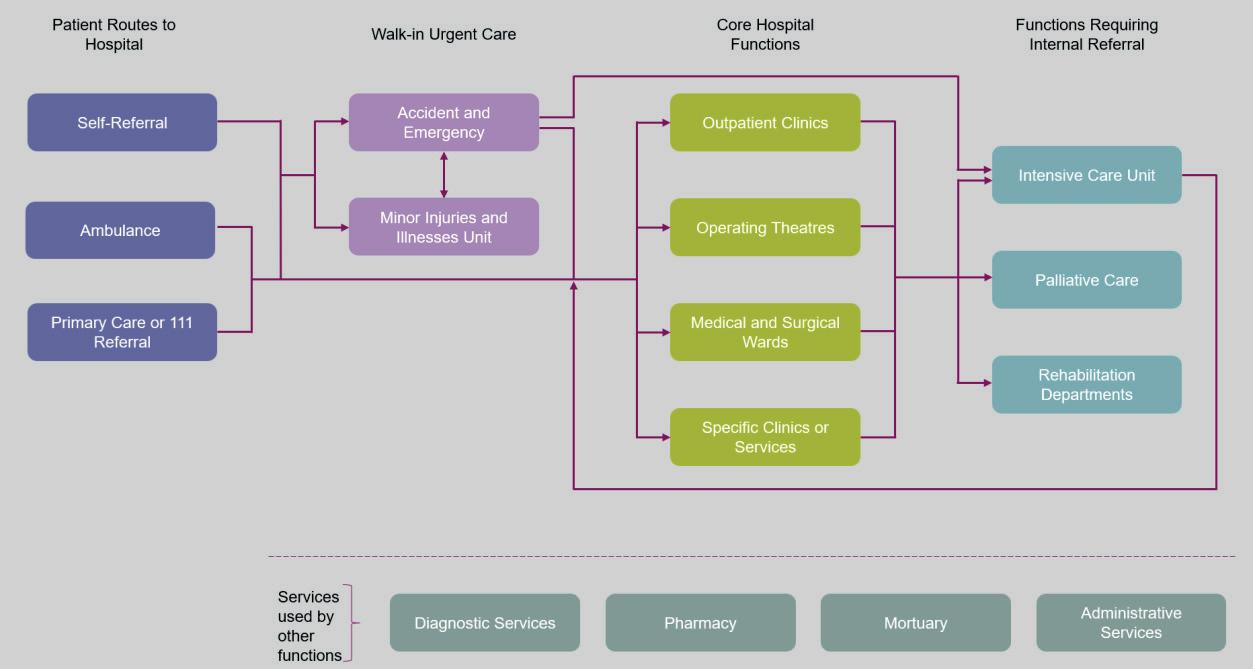
Westminster think tank, Reform, calls for a more-joined-up, preventative approach to medical services and the delivery of the healthcare estate
The current approach to delivering hospital infrastructure needs ‘a fundamental reset’, favouring a more-effective model of system-wide integration, according to Westminster think tank, Reform.
As part of its Reimagining Health workstream, Reform has embarked on a new project to outline a vision for hospitals within a health system that is re-orientated towards prevention and early intervention.
The Hospital of the Future proposes a fundamental reset in the approach to secondary care, providing a long-term vision with a new, revitalised model fit for the 21st Century.
And reform has now published the first in a series of papers diagnosing the problems experienced by hospitals today.
This will be followed by a series of papers outlining a detailed programme of reform to reimagine hospitals for the future.
The paper poses the view that a focus on the need for more resource is the wrong approach without consideration of whether the right resources are being deployed to meet the type of demand.
The model of secondary care, it says, is not changing with the nature of demand.
Furthermore, it should be viewed as a service, not just a building.
Reform aims to challenge how the physical hospital building can change and how the same level of care can be provided outside of the traditional hospital.
And it acknowledges that rethinking the division of care in a hospital raises fundamental questions about economies
of scale, as well as logistical concerns about services, facilities, and rotas.
It also points out that patient flow within hospitals needs a ‘fundamental reset’ and promises to explore a more-effective model of system-wide integration, the role of management and flow co-ordination, as well as the technology infrastructure needed to enhance this.
The paper states: “There are severe problems facing hospitals in the immediate
term: financial deficits in NHS trusts, a reliance on locum working, outdated equipment, and a growing maintenance backlog, to name a few.
“But, underlying these shortterm problems, is a profound set of structural questions as to how a hospital fundamentally operates and whether this is the right model.
“This framing paper will diagnose the problems in hospitals today — what they are, why they exist, and the longterm prognosis.”
The paper says that, since the creation of the hospital, the logic of the physical hospital building has always been that it enables substantial economies of scale.
These arise from being able to achieve high levels of utilisation of specialist capacity, both human and technical. For example, health systems have high fixed infrastructure costs, in that they must pay for diagnostic and operating theatre equipment as well as hospital beds and staff. These high costs become substantially more cost efficient the larger the patient base that uses them.

Thus, the core logic of hospitals is that they provide a range of services that draw on economies of scale, providing different forms of care to high volumes of patients using the same underlying infrastructure base.
The paper states: “With this said, it is still not clear what the optimal size and scope of a hospital is if it is to make the most use of its available expertise, infrastructure, and equipment.
“Hospitals that are too large can depart from the optimal level of efficiency and exhibit diseconomies of scale.
“But, at the other end of the scale, small hospitals might be inefficient because the fixed infrastructural and administrative costs are shared across too small a caseload.
“How hospitals achieve economies of scale is also evolving. Many large regional hub hospitals are seeking to increase volumes in specialised services to deliver high-quality care affordably, while smaller hospitals are forming networks to invest in infrastructure, share back office costs, and retain staff who want to undertake a range of clinical work.”
Problems which need addressing, according to the report, include poor understanding of patient flow; hospitals being internally incoherent and fragmented; a bias towards specialism within the workforce; poor integration between primary, secondary,

The different types of hospitals
and social care; insufficient management; complicated funding models; and an absence of communication and technological infrastructure.
Low capital investment is also cited.
The paper states: “Over the past 15 years, levels of capital investment have grown dramatically, but this is partially to compensate for the fact that from 2014-15 to 2019-20, funds from capital budgets were transferred to support dayto-day spending and relieve the growing pressures in the NHS.
“The dire state of NHS England’s hospital estates contributes to poor
secondary care productivity.
“In 2023-24, the cost to resolve the backlog of maintenance for all ‘risky’ NHS England buildings was estimated to be just over £13.75bn.
“Worryingly, over 55% of those costs would be needed just to tackle high-risk and significant-risk building issues.”
It adds: “There are numerous negative consequences, for patients and staff, resulting from poor NHS hospital estates.
“Perhaps, most obviously, shut or disused facilities caused by unsafe buildings or unusable equipment reduces the capacity of secondary care.
…it is still not clear what the optimal size and scope of a hospital is if it is to make the most use of its available expertise, infrastructure, and equipment
Over the past 15 years, levels of capital investment have grown dramatically, but this is partially to compensate for the fact that from 201415 to 2019-20, funds from capital budgets were transferred to support day-today spending and relieve the growing pressures in the NHS
“Broken lifts, unfit-for-use or outdated equipment, and finding workarounds for estate issues causes major inefficiencies, similarly reducing secondary care capacity.”
In its vision for the future, the paper reimagines hospitals as if they were being designed from scratch today, posing four questions:
• How should the patient journey through the hospital change?
• How would hospitals interact with the rest of the healthcare system?
• How would the entire configuration and location of secondary care services look different?
• How would this change the scale, clinical portfolio, workforce, infrastructure, and funding model of secondary care?

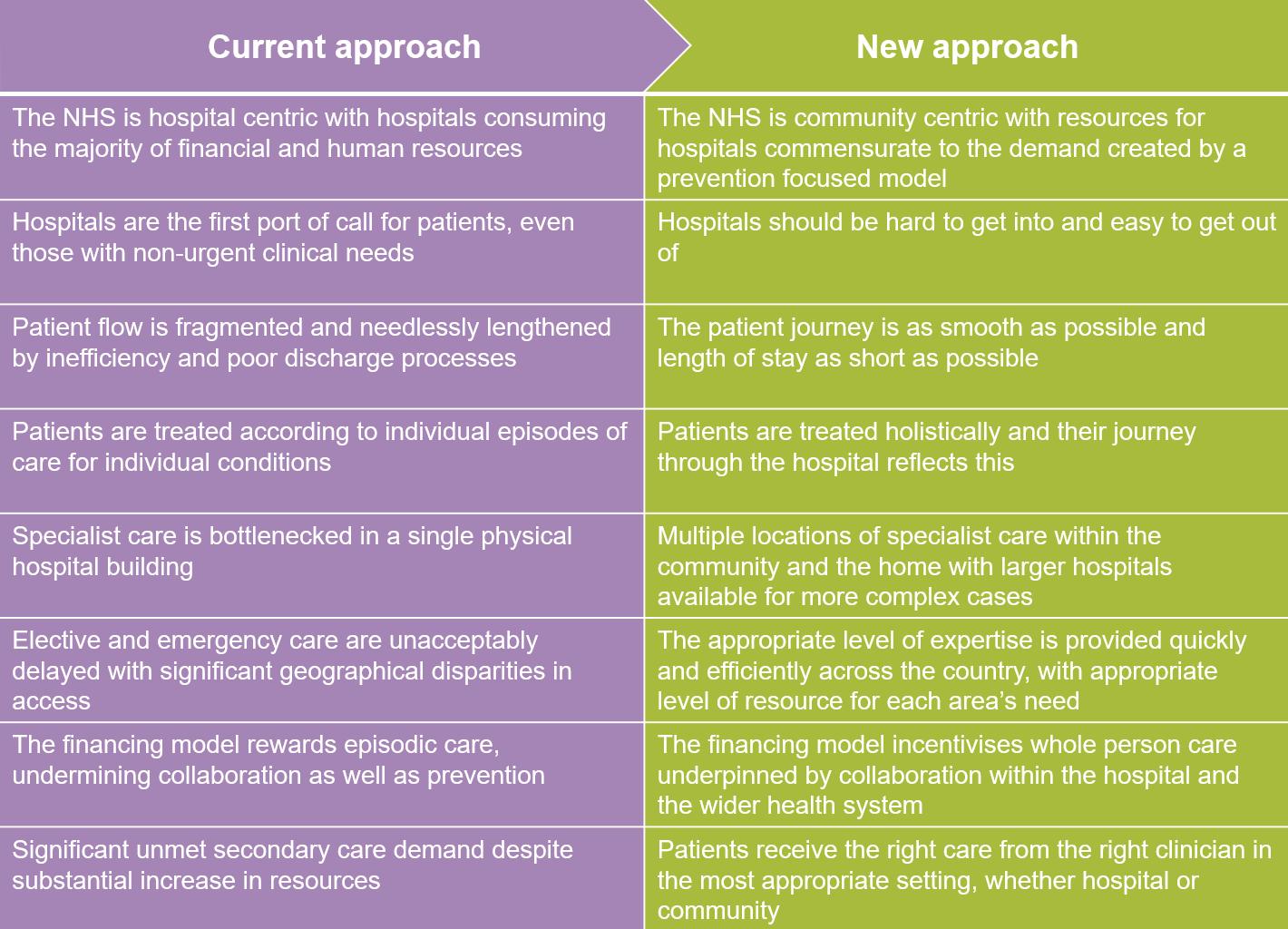
It concludes: “Policymakers have paid lip service to prevention for decades, but realising the prevention ambition will always be unachievable if there is not a coherent plan for what the role of the hospital is, and how it can achieve this.
“Otherwise, the modus operandi that has existed for decades — a hospitalcentric health system — will continue, draining resource out of the health
service and forcing costs to increase in perpetuity.
“As the healthcare landscape continues to evolve, the pressure to overhaul hospital systems will only intensify.
“The decisions made today will shape the future of healthcare delivery, and with mounting pressure on the system, the imperative for reform has never been more obvious.” n
Policymakers have paid lip service to prevention for decades, but realising the prevention ambition will always be unachievable if there is not a coherent plan for what the role of the hospital is, and how it can achieve this
EACH EDITION COVERS...
Environmental
Sustainability, carbon reduction, and energy efficiency news, features, insight, and case studies
Projects
The latest building projects in health and social care
Finance
Key drivers behind the health and care property investment markets and procurement insight
Property news
The latest property deals
Market insight
An overview of the key issues impacting the property sector (construction figures, reports, industry comment etc)


Design & Build
Best practice approaches to the design and construction of the health and social care estate
Estates & Facilities
The latest issues impacting estates and facilities management practices in health and care settings
Product
Focus on building products which are helping to boost health and social care environments
People overs and shakers within health and social care
SCAN HERE TO SUBSCRIBE


A‘radical overhaul’ of mental health inpatient care is needed to achieve the Government’s goal of shifting treatment from hospitals to communities, according to a new report from the Centre for Mental Health.
Care beyond beds finds that inpatient care is too often characterised by unsafe levels of bed occupancy, chronic staffing shortages, and dilapidated facilities which risk retraumatising patients.
Patients reported wards with mouse infestations and faeces on floors and walls and many said they did not feel safe.
Black people, neurodivergent people, and children are among the most poorly served.
The report says that the NHS’s 10year Plan must boost investment across the mental health system to drive a ‘safe and sustained shift’ towards community care and to provide inpatient care which
is high quality, close to home, and adequately staffed.
And it finds that limited community support means that people struggling with their mental health are ‘funnelled’ towards the more-acute end of the system. This causes more distress and upheaval and incurs higher costs.
This is especially the case for out-of-area placements, with patients being sent miles from their homes and support networks to get a hospital bed.
The report points out that inpatient services are an important part of the mental health care system, but that comprehensive investment in alternatives to inpatient care, such as crisis cafes and houses, would enable more people to get effective care closer to home.
…too many inpatient services are in outdated buildings that make safe and therapeutic care harder to provide
It also calls for a ‘fair share’ of NHS capital funding to be dedicated to psychiatric services so that outdated facilities can be updated or replaced.
Service users quizzed as part of the report described mental health services in general as ‘fragmented’, ‘difficult to navigate’, and ‘under resourced’.
Strikingly, many wards are not fit for purpose and are ill equipped to deliver good-quality care.
Some participants talked about a pervasive sense of monotony, marked by uninspiring settings and a scant selection of activities which can contribute to a detrimental environment.
Andy Bell, chief executive at the Centre for Mental Health, said: “The NHS spends as much on inpatient services as it does on community mental health care, even though the vast majority of people access their support through community settings.
“As the Darzi report says, too many inpatient services are in outdated buildings that make safe and therapeutic care harder to provide.
“Small-scale and incremental change will be insufficient to deliver the system-wide change that’s needed.
“We need to redesign our mental health system with a wider range of options, including from community and voluntary sector organisations, and a much bigger say for people using services in the kind of treatment and support they can get.
“The new Mental Health Bill promises to modernise mental health care. It must go hand-in-hand with investment in services, staff, and better facilities so that people can receive compassionate and effective support in a mental health crisis close to home, wherever they live.” n





In this special report healthcare property leaders reveal their predictions for the sector in 2025
The healthcare real estate sector experienced significantly more activity in 2024 compared with 2023, with an approximate doubling of transactional volume, according to Richard Harris, head of healthcare at Colliers.
Multi-billion investment from major US healthcare REITS, such as Welltower and Omega, were the highlight of the year, attracted by a generally-higher yield profile when compared with other sub markets and the lack of competition from domestic REITs due to capital restraints.
Colliers estimates that, overall, UK healthcare real estate transaction volumes for 2024 will exceed £2.5bn, which would be comparable to peak pre-COVID.
Harris said: “Add persistent historic underinvestment in real estate to universal human demand and this is a rich recipe for opportunity.”
CBRE’s UK Real Estate Market Outlook 2025 adds: “Healthcare investment

volumes will continue to increase in 2025 following a surge in activity in H2 2024, driven by increasing demand and needs.
“Strong operational performance, attractive lease features, and improving investment market conditions for a growing buyer pool continue to attract investors to the sector.”
Key takeaways from the report include:
• Investment activity will increase as economic conditions continue to improve and buyer and seller pricing expectations align
• Healthcare will be a focus for real estate
Add persistent historic underinvestment in real estate to universal human demand and this is a rich recipe for opportunity
investors due to its resilient inflationary characteristics and robust returns
• The prime healthcare market will be increasingly competitive into H1 2025, while value-add investors are targeting the mid-market to access higher returns through operational performance and active asset management
• New sources of capital focusing on operational real estate have been key to driving healthcare investment activity within a new interest rate environment. At the core returns end of the spectrum, liability-matching insurance capital has enhanced pricing across the capital stack, and this will be a key driver of investment activity in 2025. Global strategic investors including PE, wealth managers, and REITs are focusing on larger-scale operational platforms
And Colliers predicts that technology and sustainability will continue to underpin property market decision-making over the coming months, with hybrid spaces that accommodate both virtual consultations and in-person visits expected to expand significantly, with providers adopting smaller footprints and adaptable layouts.
The market, Harris adds, will also favour smaller, decentralised facilities located closer to residential areas to improve access to care while reducing operational costs.
Here, we look at some of the predictions for each sub sector of the market. n

Growing demand from institutional investors and global private equity firms
CBRE’s UK Real Estate Market Outlook
2025 reveals that primary care property investment activity returned in 2024, with Assura and USS announcing a £250m joint venture in Q2, demonstrating the growing demand from institutional investors for healthcare assets.
And there was new interest from global private equity investors.
The report predicts this increasing demand will continue in 2025, maintaining the current level of investment activity.
It states: “Relatively-slow rental growth and high construction costs have created a barrier to new developments in the primary care market.
“However, we expect upwards pressure on rental levels as third-party investors seek to improve and increase primary care capacity in line with NHS sustainability targets.”
Eddison’s valuer and regional director, David Hayton, adds: “Together with the training and recruitment of more GPs, the need for better-quality GP surgeries and medical centres is seen by many doctors as one of the biggest challenges that the primary healthcare sector faces.
“Where an old GP surgery cannot be adequately modernised or extended, obtaining the land with planning consent on which to build a new medical centre, not to mention the challenges of selecting a contractor and arranging finance, present a considerable obstacle to many GP practices, particularly those with only a small number of partners, some of whom may be approaching retirement.
“As a result, the two largest primary care PLCs — Assura and PHP — have become the main drivers of new medical centre development.
“This trend is likely to continue as the GP sector attempts to address the problem of a decline in the appeal of the traditional partnership structure, resulting in fewer doctors willing to take on the ever-morecostly challenge of improving their surgery premises or developing new facilities.
“2025 will be a challenging year for the primary care sector and is likely to experience ongoing media attention, given the importance to most people of a successful, fully-resourced primary care sector, operating from modern, fit-forpurpose surgeries.”
Primary Health Properties PLC (PHP) is predicting a year of strategic growth and opportunities in 2025.
Mark Davies, chief executive, told

Together with the training and recruitment of more GPs, the need for better-quality GP surgeries and medical centres is seen by many doctors as one of the biggest challenges that the primary healthcare sector faces
Healthcare Property: “As we approach our 30th anniversary we celebrate our marketleading position in primary care in the UK and Ireland.
“It has been a challenging start to the calendar year as UK Gilts have been volatile and it makes investment decisions more challenging when the cost of capital is moving around.
“However, we are confident that our commitment to secure long-term income streams, supported by a high-quality portfolio with increasing demand for space will deliver continued success for PHP.
“Our confidence was demonstrated by a 3% increase in our dividend that we
announced on 2 January 2025 and, looking ahead, PHP sees a range of interesting and accretive opportunities as the market adjusts to the new interest rate environment and we are well set to announce a strong set of results on 28 February.
“Finally, we have the strongest political momentum we’ve seen for primary care for a long time and, combined with the demographic tailwinds we see day in, day out, we are well set to benefit from a 10year plan for healthcare, with more care in the community and we will continue to campaign for reform of the rental system in the UK at a time the Government has committed itself to NHS reform.” n
Increasing investor interest against the backdrop of rising patient demand and improving operational performance
New figures published by LaingBuisson show strong, sustained demand for private health cover as record numbers of individuals and employers continue to turn to private medical insurance (PMI), health cash plans, and dental cover.
This has led to a record high of £7.59bn for the UK health cover market – up £825m year on year.
And this will have an impact on property values and appetite among investors and financiers.
Knight Frank’s 2024 Healthcare Capital Markets report featured insight from Nicholas West, head of UK at Northwest Healthcare Properties REIT.
He revealed the performance in the private medical market was being underpinned by the growing NHS waiting list backlog, growth in the self-pay market, and higher levels of PMI.

The firm is also seeing an emerging trend of operators reinvesting profits into major capital expenditure projects at their hospitals, such as the construction of new operating theatres, upgrading of diagnostic equipment, and other building fabric improvements.
For example, in 2023 Spire undertook £2.8m of capital expenditure to repurpose admin space for a new minor operations theatre at its asset in Sheffield.
And Knight Frank anticipates these improvements will boost operator profitability and energy performance credentials going forward into 2025.
West said: “Location is critical to the operational performance of a hospital.
“Access to top-quality consultants, proximity to NHS feeder sites, and patient affluence profiles are some of the key criteria which are important to hospital operators.
“For this reason, operators in highquality locations seek long-term leases,
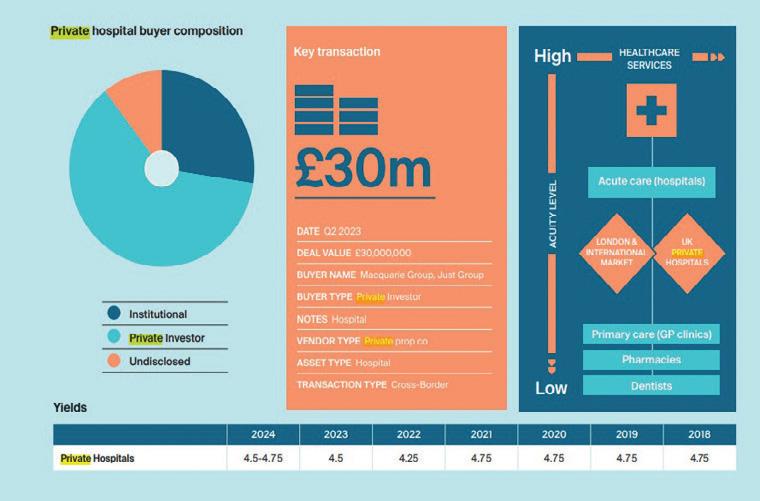
typically 20-30 years in duration, with index-linked rent reviews.
“In the short-to-medium term, we forecast that the NHS backlog will remain high, due to the unprecedented levels of doctor and NHS staff strikes, which will continue to drive private hospital revenue streams.
“The high levels of staff and energy cost inflation are anticipated to subside, albeit will remain at elevated levels for some time, and EBITDA should therefore grow inline with the revenue performance of the sector.
“On a longer-term basis, we forecast that the private hospital sector will also outperform the all-sector real estate benchmark, due to the structural
In the short-to-medium term, we forecast that the NHS backlog will remain high, due to the unprecedented levels of doctor and NHS staff strikes, which will continue to drive private hospital revenue streams
prevalence of multi-morbidities and the ageing population.”
And CBRE’s UK Real Estate Market Outlook 2025 states: “There has been considerable investment into the private acute hospital sector in 2024.
“Notable deals include Song Capital’s £631m refinancing of MPT’s UK hospital portfolio in Q2, and Assura’s £500m acquisition of Northwest Healthcare’s portfolio of 14 UK hospitals in Q3.
“We anticipate increased investor demand in 2025 against the backdrop of rising patient demand and improving operational performance.
“The long-term structural trend from inpatient to outpatient care will drive demand for specialist diagnostic and postacute rehabilitation services.
“These require specialist real estate, which may create new investment opportunities in the medium-to-long term.
Eddisons’ research points to a healthy pipeline of projects moving into this year.
Valuer and regional director, David Hayton, said: “It takes a long time to develop a new hospital, from obtaining the land and planning consent to completing the construction of highlycomplex buildings.
“There are currently a series of new private hospital developments in the pipeline, most of which are in the early stages and 2025 is likely to see further schemes confirmed as the private hospital sector attempts to capitalise on both the demand coming from the NHS and the anticipation of further demand for private treatment from individuals who are unwilling to wait months and years for NHS treatment.” n
UK care home market expected to experience a year of growth, with an increase in expansions, first-time buyer activity, and deals funded by REITS
The UK’s over-65s make up around 20% of the population and this proportion is expected to grow year on year, with an additional 1.5 million over-65s in the next five years, fuelling demand for retirement housing and social care facilities.
Similarly, in a recent study commissioned by the UK government, it was found that retirement housing units or ‘supported housing’ will need to grow by nearly 1.3 million over the next 15 years to meet the expected levels of demand.
This imbalance presents significant opportunities for developers and investors.
Christie & Co labelled 2024 as a year of growth in the UK care market, with the majority of operators reporting improved occupancy levels, a reduction in agency usage, and a return in buyer confidence, which resulted in an increase in transactional activity across the market.
Small-to-medium-sized groups (groups of three to 19 care homes) were the most-active buyer group in 2024, thanks largely to the return of occupancy – a notable shift from the most active in 2023, which was first-time buyers and independent purchasers.
However, deal times continued to be delayed as issues with the Care Quality Commission (CQC) persisted, according to Christie & Co’s Business Outlook 2025 report.
The report also notes a reduction in the number of closed, vacant care homes in 2024 — which made up 12% of the company’s healthcare sales in 2024 compared with 16% in 2023.
This is largely due to a material reduction in closed care home instructions and not a reflection in declining investor appetite for repurposing this stock, the firm says.
In addition, the land and development market faced stronger headwinds due to construction cost inflation, ongoing challenges in the planning system, and the availability of debt.
However, the need for futureproofed care beds remains undiminished and the underlying ESG credentials, together with future bed demand, remain compelling for investors.
And Christie & Co expects the combination of improved operational trading performance and stabilisation of construction costs to provide increasing confidence to return to the development

for consented sites and transactional activity forecast for 2025.
In particular, a greater number of developments are coming forward in untapped regions including the South West of England, Wales, and London and it is expected that this will continue into 2025.
In the care market in 2025,
Christie & Co expects:
• Increased activity with interest rates easing
• Increased deals funded by REITS
• Continued first-time buyer activity
• Margins squeezed on those dependent on local authority fees
• ESG credentials will become increasingly important for both owners and funders
• Existing operators will continue to expand with a preference for businesses with upside
• Concern around staffing cost increases versus local authority fees
• Healthcare will continue to be a key target sector for investors
Commenting on the report, Richard Lunn, managing director of care at Christie & Co, said: “2024 was another challenging year and the care sector which, like many, employs a significant workforce is notably impacted by the increase in employers’ National Insurance contributions, with little certainty that local authority fee increases will be sufficient to cover the differential.
“However, strong operators are alive to all the challenges and we are sure that appetite for the whole spectrum of care businesses will continue and, therefore, 2025 will see an increase in activity from a range of buyers and REITS.”
Christie & Co’s director and head of healthcare development and investment, Jordan Rundle, adds: “Following a prolonged period of headwinds in the land and development market, momentum is building in the new-build sector and this has been largely driven by stabilisation of costs and improved underlying trade performance in the private pay arena.
“As confidence returns, we are already seeing a noticeable uptick in demand from operators for good-quality, consented care home sites and anticipate greater land deal volumes over the next 12 months.”
Healthcare real estate investment manager, Elevation, is also predicting momentum in the sector through 2025, with operators looking to address the undersupply of quality care beds.
Elevation’s investment director, James Giles, said: “Over the last 12 months, as construction costs stabilised to a new normal, we started construction on 14 development projects for highquality care homes.
“We see this momentum towards new development continuing in 2025 with an encouraging pipeline of projects.
“Our operator partners have ambitious plans to grow their businesses, delivering social value by addressing the undersupply of quality care beds, and we are very supportive to fund such growth.”
The company’s ESG director, Jacob Hurtley, added that ESG was increasingly key for both operators and investors.
“We are seeing a big push towards integrating energy efficiency and renewable technologies to make property more sustainable,” he said.
“This is driven from both operators looking to make efficiency as well as long-term financial savings, and investors who are looking to boost the long-term resilience of their assets by enhancing their ESG characteristics.
“For example, last year we successfully rolled out solar panels and infra-red heating at participating care homes.”
And Eddison’s valuer and regional director, David Hayton, concludes: “While the private elderly care sector continues to enable many operators to generate good profits, this is almost always highly dependent upon being able to charge higher fees to ‘self-funding’ residents than can be obtained from local authorities.
“That ability to consistently generate profit attracts new care home development in parts of the country where operators can charge premium fees to ‘selffunding’ residents.
“The ‘turnkey’ costs of opening highquality homes regularly exceed £150,000 per bed, affirming residential care as an attractive business choice.” n
Demand for real estate remains strong amid a critical shortfall in places
According to Christie & Co’s recentlyreleased Business Outlook 2025 report, children’s social care settings continue to be sought after as demand for placements increases.
And, following a ‘somewhat-frustrating’ 2024, the next 12 months is likely to see a growth year for the sector, with the emphasis on SEN and complex needs.
The report states that ‘throughout 2024, activity in the sector was moderate, with limited acquisition and business expansion opportunities available to buyers due to many operators holding onto their existing businesses and expanding them, where possible, to keep up with the increase in demand for children’s services’.

care transactions in 2024.
And, despite a shortage of small-tomedium-sized businesses being presented for sale, the sector witnessed a handful of major transactions last year.
fostering, residential, and special education for children with high-acuity and complex needs – from the majority shareholder, Graphite Capital.
Moving through this year, Christie & Co expects:
• Increased merger and acquisition activity
• Continued buyer appetite for quality businesses with proven earnings, especially established businesses with experienced management teams
• Properties with the benefit of permitted C2 or C2a use will continue to command premiums over those sold on a vacant possession basis with C3 use
Amid heightened demand for highquality operational businesses and welllocated vacant properties benefitting from C2 use and CLD, Christie & Co achieved 105% of the asking price on children’s social
In May, for example, Cap10 Partners partnered with the existing Compass management to acquire 100% of Compass Community Children’s Services (Compass) — a leading UK provider of therapeutic
• With local authority funding shortfalls, Christie & Co fears that commissioning into services at lower cost points could result in children’s individual needs not being met
• Continued stagnation of the market in Wales in the short-term n
Independent dental sector dominates the market, with practices appealing to first-time buyers and owner-operators
The independent sector continued to dominate market activity throughout 2024, with first-time buyers, existing owners, and smaller groups driving over 80% of agreed transactions, according to Christie & Co.
This sustained momentum in the volume segment was reflected in pricing, with practices achieving an impressive average of 108% of their asking price.
As borrowing costs stabilised over the year, the market gained more confidence, particularly in practice acquisitions.
Viewings surged by 19%, offers received rose by 17%, and the number of agreed deals soared by 26% compared with 2023.
The aggregate value of all offers increased by 1.5% which, when allowing for the increased volume of offers received, reflects the dominance in independent market activity.
Activity levels were further bolstered by a significant 18% rise in the number of practices brought to market in 2024.
This influx of supply provided prospective buyers with a wider range of opportunities, influencing the average number of offers per practice sale. After climbing from 2.2 in 2022 to 4.4 in 2023, the average rose to 4.8 in 2024, reflecting the evolving market dynamics.
The market has experienced a



is showing signs of renewed optimism on the horizon.
While the transactional market in 2024 saw fewer major deals to corporate operators, this shift has opened up exciting opportunities for independent and first-time buyers.
Predictions for 2025 include:
• A continued appetite from independent groups and owner-operator first-time buyers for all practice types
• Increased numbers of sellers wanting to exit before future changes to Business Asset Disposal Relief (BADR)
• Higher National Living Wage (NLW) rates affecting practice profitability along
• Private Equity-backed corporate buyers returning to the market in light of stabilised interest rates and successful periods of integration and divestment
• Continued issues with recruitment, alleviated somewhat by the streamlining of the PVLE & ORE processes
• Due to the financial restrictions placed on NHS-focused practices, such as the ineligibility for the increased employment allowance, acquisitions focused on NHSheavy portfolios might have less appeal to buyers. Buyers may, instead, target practices with a larger private patient base, which are less constrained by the 2024 Autumn Budget’s public sector stipulations n
Bouyant market after a record year for transactions
2024 was a record-breaking year for pharmacy property transactions, with a third of real estate deals involving new market entrants, reveals Christie & Co’s Business Outlook 2025 report.
In the 12 months to the end of November 2024, Christie & Co completed 222 pharmacy sales, more than double the amount for the preceding year. And 36% of these were corporate disposals, which the broker expects to subside in 2025 and be replaced with an increasing volume of independent sales.
First-time buyers were the most-active buyer type in 2024, acquiring 33% of pharmacy businesses on the market with Christie & Co, down from 45% in 2023.
In contrast, large groups and corporate operators made up just 8% of acquisitions last year.
And Christie & Co notes an average decrease of 6.3% in the price per pharmacy businesses sold last year.
While 2024 was a record year for transactional activity, with deal volume at an all-time high despite ongoing operational challenges and cost pressures, the distressed pharmacies that came to the market all generated significant interest from buyers keen to acquire competitivelypriced opportunities on both a local and a regional basis.
This negative price movement, therefore, was a product of the high numbers of smaller pharmacies and corporate disposals sold in the first half of the year.
Encouragingly, the last quarter saw a vast increase in the average value of the pharmacies being added to the pipeline (offers made and deals being accepted), which will no doubt positively impact the price index in 2025.

Pixabay
An average of 91% of asking price was achieved on pharmacy businesses in 2024, which is a decrease on the year before, which saw offers accepted at an average of 2.5% above asking price.
As part of its annual sentiment survey, Christie & Co asked pharmacy professionals across the country for their views on the year ahead.
When questioned about their sentiment in 2025, 22% said they feel positive while 50% feel negative, which can be attributed to the uncertainty around funding in the sector.
When asked about their sale and acquisition plans, 68% stated that they are looking to buy and/or sell this year.
In the pharmacy market in 2025, Christie & Co expects:
• Cost challenges will remain a key factor in the market, none more so than the
Although cost pressures will continue to be a feature for the foreseeable future, market appetite remains strong for well-established, well-run businesses, but it’s likely that market appetite in England will be tempered by the outcome of the much-needed funding settlement negotiations
increase in National Living Wage (NLW) from April 2025
• It is hoped that, with an improved funding settlement, levels of distress in the sector will subside
• A continuation of the improvement seen in Q4 2024 of the volume of independent sales as corporate disposal processes start to subside
• Improved appetite from group operators to acquire as some cost pressures stabilise
• Private equity is expected to renew its focus on the sector, as it is one of the few primary care sectors not to have seen significant investor appetite
Jonathan Board, head of pharmacy at Christie & Co, comments: “2024 was a record year from pharmacy transactions due in part to an increased level of corporate divestments.
“As we move into 2025, the entire sector is waiting with bated breath for an announcement on the outcome of pharmacy’s wider funding agreement which will replace the Community Pharmacy Contractual Framework’s 5-year deal from 2019.
“This will hopefully provide some certainty for all contractors moving forwards and allow them to plan and invest accordingly.
“Although cost pressures will continue to be a feature for the foreseeable future, market appetite remains strong for well-established, well-run businesses, but it’s likely that market appetite in England will be tempered by the outcome of the much-needed funding settlement negotiations.” n


PVictoria Thourgood, head of corporate real estate and the later living practice at Browne Jacobson, untangles various legal and financial hurdles to developing more senior housing and discusses why the adoption of 'rightsizing' remains limited in the UK compared to other countries
rojections indicate that the number of individuals aged over 85 will double in the next 25 years, with a quarter of the UK population expected to be aged 65-plus by 2050.
This demographic shift is set to impact every aspect of society, from the workforce and economy to healthcare, social care, and other public services.
As Britain faces significant challenges arising from its an ageing population, the concept of ‘rightsizing’ presents itself as a vital-yet-underutilised solution to some of these challenges.
Senior housing options support physical and mental wellbeing in later life.
And the health and independence benefits of age-appropriate housing, especially integrated retirement communities (IRCs), are becoming increasingly recognised.
A pivotal study conducted in 2015 by the not-for-profit IRC developer and operator, ExtraCare Charitable Trust, in collaboration with Aston University, highlighted the significant advantages of retirement villages.
The research revealed continuous improvements in depression, perceived health, and memory among residents, alongside a 7% cost reduction to the NHS due to decreased hospital stays and fewer unplanned and routine GP visits.
Further studies have shown enhanced physical activity, reduced anxiety, and, notably, diminished loneliness — a condition the NHS acknowledges as having a profound effect on health.
Despite these clear advantages, though, barriers such as funding, scale, supply, and affordability have impeded the
… the practice of ‘rightsizing’ — choosing a home that fits an individual’s current needs and lifestyle, distinct from downsizing for financial reasons — has yet to become a cultural norm in Britain
broader development of IRCs, with only 3% of new homes being developed for senior living.
Recent recommendations from an Older People's Housing Taskforce report aimed at increasing the availability of later living accommodations include dedicating 10% of affordable housing to later living, favouring senior housing in planning policies, adopting more-flexible design and construction methods, and introducing financial incentives like a capped stamp duty for rightsizing.
These proposals underscore the need for innovative solutions to overcome the challenges hindering the expansion of IRC development.
However, the practice of ‘rightsizing’ — choosing a home that fits an individual’s current needs and lifestyle, distinct from downsizing for financial reasons — has yet to become a cultural norm in Britain.
Rightsizing by retirees can also help alleviate property ladder bottlenecks by freeing up larger family homes for the market.
And new occupants are more likely to invest in energy efficiency improvements to older housing stock, creating a positive domino effect.
This practice is more common in countries like the US, Canada, Australia, and New Zealand, which offer a wider range of independent and assisted living options.
For instance, 6.5% of over-65s in the US reside in IRCs, compared to just 1% in the UK.
There are almost 20,000 retirement community providers in the US, where the later living market is forecast to grow from $113bn in 2024 to $150bn by 2029.
Much progress is still to be made across the Atlantic, but there’s an acceptance the American dream’s latter years can be spent in retirement communities rather than large, detached houses.
For Britain to normalise this practice, providers, intermediaries, government, and the wider sector must consider how to communicate the offer to people not just at retirement age now, but who will be in 20 to 30 years time.
Another key consideration here is making units affordable for their target residents — they can’t only be for those with highvalue homes to sell.
With more than 90% of residents selling their home before moving into retirement housing, according to Knight Frank, there’s some correlation between the value of their
Figure 1.11: Satisfaction with attributes of the current home
To what extent do you agree or disagree with the following statements?
I worry my current home will be too expensive to keep warm in winter
My current home will not be suitable if my/ my households needs change in the future Strongly agree
Figure 1.12: Reasons for moving to their
Satisfaction with attibutes of the current home
You said you moved into your current home within the last five years, which two or three of the following were the most important reasons for moving to your current home?
Moved to a nicer home
Moved to a better neighbourhood/more pleasant area
Moved to a smaller house/flat
Moved to be closer to family or friends
Moved to an area with better local amenities
Moved to a larger house/flat
Moved to a cheaper house/flat
Moved because my friends/family wanted me to Moved to be closer to essential services
Moved to take up a new job or to be in an area with more work
Moved to accommodation with additional care/support services provided
Moved in with family or friends
Something else
Base: All those who have moved into their current home within the last 5 years (1002): Fieldwork dates: 7-13 December 2023
Reasons for moving to their current home
home and what they can afford to live in during their retirement.
With the delivery cost of an IRC being a function of the land cost, build cost, and profit, its integrated services can
mean the outright purchase of a unit is often unaffordable.
This might explain why operators often focus on London, East Anglia, and the South East of England for new locations.
For rightsizing to really become commonplace, a wide range of senior living options are needed across the country, along with plenty of tenure options for those who choose to rent instead of buy when moving into retirement communities.
In December, the Housing Learning and Improvement Network (Housing LIN) published a report titled Older People’s Housing Preferences, funded by UK Research and Innovation.
It provides further insight into the housing circumstances, aspirations, and preferences of older adults in the UK.
Based on a representative survey of over 5,500 UK adults aged 50 and over, it highlighted how location is the mostimportant factor in their decision-making.
It found that almost 60% expect to move into a smaller property, which suggests that more people might be willing to rightsize if they can find a home that meets their needs in their locality.
This aligns with the 2023 Associated Retirement Community Operators (ARCO) manifesto for an IRC in every town, updated last year to include an IRC in every London borough.
Ultimately, for Britain to embrace rightsizing, a concerted effort from providers, intermediaries, government, and the wider sector is essential.
This involves not only communicating the benefits of rightsizing to current and future generations, but also ensuring a sufficient choice of housing options to cater to the diverse aspirations and needs of older people.
We must ensure current and future older generations understand what those options are.
There is a misconception that older people are frail and dependent, and that age-appropriate housing is all about design features such as wider doorways for wheelchairs.
In reality, it is also about freedom to spend your time leading a fulfilling life doing the things you really want to do,

of neighbourhood and surrounding area
A private garden
Proximity to essential amenities
Sufficient space and living area
Off-street parking (front drive or garage)
Energy efficient
Free from hygiene issues
Physically secure
Affordability
Pets are allowed within the home
A fast and reliable internet connection
Space for guests to stay overnight
Good storage space for essential items
Private space in the home to work/for hobbies and be alone
Access to recreational facilities green spaces
Community and social connections
Ability to live with family or extended family
Wheelchair accessible
Access to cultural and/or religious amenities
Access to communal facilities
Other
None of the above
Don't know
Base: All UK adults aged 50+ (5591): Fieldwork dates: 7-13 December 2023
such as volunteering or learning a new skill, rather than worrying about getting the boiler or fence repaired.
All this underscores the critical need for a strategic approach to delivering increased later living options.
And this approach must prioritise collaboration with later living providers, local authorities, and healthcare agencies to
develop strategies that cater to the differing needs of older people.
Such efforts will not only address the challenge of providing appropriate housing, but also contribute to managing other key issues like social care provision and affordable housing supply, marking a significant step forward in Britain’s response to its ageing population challenge. n
For Britain to normalise this practice, providers, intermediaries, government, and the wider sector must consider how to communicate the offer to people not just at retirement age now, but who will be in 20 to 30 years time
Scan to read now
Inside issue 05, September-October 2024
• Contractor appointed to build £15m community health centre
• Keyworker housing model supports recruitment and retention of staff
• Investors and property developers remain interested in health and care sector
Scan to read now
Inside issue 06, November-December 2024
• Why we need to rethink our approach to healthcare design and delivery
• How private capital can bring long-term solutions for the health estate
• RAAC hospitals to be rebuilt despite Labour's spending review
Scan to read now
Inside issue 07, January-February 2025
• New hospital sets standards for future clinical design
• Budget special report — the impact on health infrastructure
• Winners of the National Care Awards and HealthInvestor Power List are revealed

Exploring the role private patients units could play in improving NHS efficiency
The expansion of private patient units (PPUs) within NHS hospitals could help to solve the waiting list backlog as well as generate revenue for struggling trusts, according to healthcare leaders.
Speaking after Prime Minister, Kier Starmer, revealed his plans to develop a closer relationship between the public and private healthcare sectors, Carly Caton, a partner specialising in commercial healthcare at law firm, Browne Jacobson, said PPUs would be provide a long-term
approach to help address long waiting times.
She told Healthcare Property: “The Government’s stated ambition is to make facilities and resources with latent capacity in the private sector available to the NHS where it is most needed or in the ‘national interest’ to cut waiting times.
“But, if the Prime Minister really does want to form a stronger relationship between the private and public sectors, another, longer-term approach with the potential to generate additional revenue
for the NHS itself while delivering better patient outcomes is to encourage NHS trusts to expand their private patient units (PPUs) by partnering with independent healthcare providers.
“Increasing private patient activity within NHS hospitals is also one of the easiest routes to develop further collaboration between the public and private sectors.
“Most trusts already run PPUs but, with the exception of a few, these tend to be relatively small, meaning they provide untapped potential in terms of raising additional income to plough back into NHS services.”
Research from Latchmore Healthcare Associates found that PPUs generated £634m of revenue in 2019 — a 14% share of the private patient market — and identified more than £500m of potential private care within NHS PPUs outside London that is
… if the Prime Minister really does want to form a stronger relationship between the private and public sectors, another, longer-term approach with the potential to generate additional revenue for the NHS itself while delivering better patient outcomes is to encourage NHS trusts to expand their private patient units…


Caton said: “PPUs are ideally placed to serve the high-acuity and complex segment of the market as they can share resources within the NHS facilities. As the NHS is already treating these individuals as NHS patients, providing a private pathway would mean payment from insurers for work they are doing anyway, and effectively very high margins.
“There are numerous ways of expanding PPUs and it doesn’t necessarily require significant capital investment if a trust is willing to partner with a private provider.
“Partnership structures can extend from commercial agreements to developing some form of physical expansion to estates, and all while creating new income streams for NHS patients at no cost to the taxpayer — meaning everyone is a winner.”
Her comments came after Starmer revealed a new agreement had been struck with the independent sector as part of plans to end the hospital waiting list backlog.
As part of the deal, NHS England and the independent sector will:
• Work on aligning NHS and independent sector digital systems around a national set of standards so patients can more easily see appointments and results on the NHS App
• Encourage longer-term contractual relationships to be established, enabling
training occurs consistently in the independent sector
Starmer said: “Mission-led government is about doing things differently.
“When the waiting lists have ballooned to 7.5 million, we will not let ideology or old ways of doing things stand in the way of getting people’s lives back on track.
“As we deliver our Plan for Change to rebuild the NHS, it would be a dereliction of duty not to use every available resource to get patients the care they so desperately need.
“That’s why this agreement will make sure working people get greater choice over when, and where, they receive their treatment and provide more support to the areas in greatest need.”
The deal will set out how independent sector capacity can be used to tackle some of the longest waits in specialist areas of treatment, such as gynaecology, where there is a backlog of 260,000 women waiting more than 18 weeks for treatment.
Orthopaedics will also be a key focus, where over 40% of patients are waiting longer than the 18-week target.
The agreement will also give patients in more deprived areas, where NHS provision is more limited, a greater choice over where they are treated.
failed by 14 years of neglect of the NHS.
“I’m not going to allow working people to wait longer than is necessary when we can get them treated sooner in a private hospital, paid for by the NHS.
“If the wealthy can be treated on time, then so should NHS patients.
“This new agreement will help to cut waiting times faster in parts of the country where the need is greatest, and in gynaecological care, where women are left waiting far too long.”
Welcoming the announcement, David Hare, chief executive of the Independent Healthcare Providers Network (IHPN), said: “This new agreement is a clear statement from Government, the NHS, and independent sector that independent providers are a critical part of the NHS’s long-term recovery and renewal.
“Independent providers already treat millions of NHS patients every year, and this agreement builds on these strong foundations by making full use of existing capacity in the sector, ensuring that patients are offered proper choice of provider, as well as supporting the sector to invest in, and deliver, an even wider choice of high quality services to NHS patients to bring waiting times down — all delivered free at the point of use and paid for at NHS prices.” n
Independent providers already treat millions of NHS patients every year, and this agreement builds on these strong foundations by making full use of existing capacity in the sector
Ward House Nursing Home in Ventnor on the Isle of Wight has been sold for residential development.
Originally a pair of semi-detached houses which were joined together a number of years ago, the former nursing home comprises a three-storey property with 19 bedrooms, of which eight have ensuite facilities.
There is also a passenger lift accessing all floors, with a large and extended lounge/ dining area on the ground floor.
And rooms to the rear of the property and the enclosed garden have panoramic views over the English Channel.
Ward House ceased trading in February 2024 and RSM UK Restructuring Advisory LLP

was appointed as its liquidator shortly after. Following an open sales process with

Capel Grange Care Home in Newport, South Wales, has been sold to Amaya Care Homes for an undisclosed sum.
Built in 2009, the facility boasts 72 bedrooms with wetroom facilities.
Previously owned by Linc Cymru Housing Association (Linc), which merged with Pobl Group in April 2024, Capel Grange was brought to market as part of a strategic divestment of Linc’s care portfolio. Following a confidential sales process with Rob Kinsman at Christie & Co, the home has been sold to Amaya Care Homes as part of its strategic initiative to broaden its assets in the region.
This acquisition effectively doubles its representation in South Wales, following its earlier acquisition of Bryn Celyn Care Home in Maesteg in 2021.
Charles Phillips at Christie & Co, the property has been sold to experienced residential developer, Johann Joubert.
Phillips said of the site: “Due to the property being closed and in such a good location in Ventnor, we obtained interest from a number of applicants looking to use the property for a variety of different planning uses, but mainly from residential developers.
“We are confident that, with Johann’s property development skills, he will be very successful with this one and we look forward to seeing the finished product in the future.”
Ward House was sold for an undisclosed price.

Real estate fund, Elevation Healthcare Properties (EHP), has acquired land and agreed forward funding to support the development of a care home in Otley, Yorkshire, with Torsion Care as developer and operator and Torsion Projects as contractor.
The home is due to open late next year and, once completed, it will be let on a long-term lease with RPI-linked escalator with cap and collar to Torwood Care, an existing operator relationship for EHP.
Torwood currently operates four care homes and has five developments under construction.
The Otley scheme will provide 66 ensuite wetroom bedrooms with communal amenities including a hairdresser, café/bistro, and a family games room.
The development will eradicate gas from its

design to reduce carbon emissions in operation, and will include air source heat pumps, solar panels, and an all-electric design in the laundry and kitchens to target an EPC A rating, BREEAM Construction rating of ‘Excellent’, and a BREEAM In-Use rating of ‘Excellent’.
Martin Hutson, director of Torwood, said: “The scheme will further strengthen our existing care home portfolio and provide much-needed, high-quality care for local people.
“All the Torwood portfolio consists of EPC A and BREEAM excellent-rated homes, which provide high levels of sustainability and carbon reduction.
“This aligns strongly with our fund partners’ strategy and we will continue to innovate the development of our homes to deliver some of the most modern and carbon efficient care homes in the sector.”
Specialist business property adviser, Christie & Co, has announced the sale of the specialist care home, Crystal Hall, in Preston.
Established in 1989, Crystal Hall is an adult mental health and neurological care facility registered for 65 service users, occupying a majority-single-storey property in the Preston village of Whittingham.
It has been owned by Amanda Cummings and her family since its conception. But she recently decided to sell to pursue retirement.
Following a sales process led by Julie Kitson and Hayley Hughes of Christie & Co, the home has been sold to Crestview Care, a new entrant into the sector which bought its first home just a few weeks prior to this purchase.
James Guy, managing director at Crestview Care, said: “I am pleased to have purchased Crystal Hall and look forward to building on the success and maintaining the reputation that Amanda has gained over the years.”
Crystal Hall was sold for an undisclosed price.


Nursing Home in Houghton, Pembrokeshire.
McCarthy said: “Demand remains strong for a range of care assets across the UK and, despite challenges faced by operators across the board, we expect appetite to continue from all buyer types.”
Bryngwy Residential Home was sold for an undisclosed price.
Property developer, Zephyr X, has taken out an £8.8m bridging loan to support the development of a purpose-built 70-bed care home and seven supported living apartments in Blackburn, Lancashire.
The loan was provided by Blackfinch Property, which stated that it will allow Zephyr X to build up occupancy and trading performance, positioning it for a refinance onto a long-term commercial mortgage.
The care home will be energy efficient, with an EPC B rating and electric vehicle charging points and bicycle racks on site.
Jason Wong, assistant investment manager at Blackfinch Property, said: “We are proud to continue our relationship with Zephyr X as it delivers much-needed care solutions in Blackburn.
“This facility addresses an urgent demand for modern, sustainable care homes, while also delivering significant benefits to the local community.
“By supporting developers through every stage of their project lifecycle, we’re helping to ensure that essential infrastructure is in place to meet the growing needs of the UK’s ageing population.”

Just three years after it opened, Heatherwood Hospital in Ascot, Berkshire, has been named the best elective care centre in
Ascot has been home to a hospital at Heatherwood for almost a century, originally serving as a tuberculosis sanitorium for children.
In 2018, with ageing facilities and a growing need for investment, the hospital’s long-term future was in doubt and plans were unveiled for a replacement building.

Sean Woodhead
Designed by multidisciplinary design practice, BDP, and built by Kier Construction, the new £98m Heatherwood Hospital is an elective facility focused on orthopaedic and high-volume, lowacuity procedures, set within picturesque
The 11,500sq m hospital opened in 2022 and its forward-thinking approach to the delivery of health services has since been widely recognised, not least with the recent announcement that it has been named the best elective care centre in England by patients as part of the Care Quality NHS Adult
The annual appraisal looked at the experience of 63,573 patients across 131 NHS trusts who stayed at least one night in hospital during November 2023.
And, between January and April 2024, 1,250 patients at each trust were invited
to give their views, answering 55 questions about hospital admission and discharge, care and treatment, communication with staff, involvement in decisions, respect and dignity, and the hospital ward and environment.
The average score of Heatherwood patients asked to rate their overall experience was 9.7 out of 10, the best of any individual hospital included in the survey.
The aim, architecturally, was to deliver a fantastic experience for both staff and patients, with uplifting public spaces, and access — both visually and physically — to the surrounding woodland, providing therapeutic and wellbeing benefits for everyone using the building.
Outside, there is a large biodiverse pond area, with terraced access down to water level on one side, allowing safe interaction with aquatic life, and nearby nature walks.
The communal courtyard which links the main hospital with the GP hub and administration building includes semi-mature arboretum trees and sensory planting.
Elsewhere, a sheltered roof garden, enclosed on all four sides, offers a pleasant


… we jumped at the opportunity to be involved as it is not often you get the chance to design a hospital in a location like this
and relaxing view from the spaces that overlook it.
Biophilic design was absolutely key to the approach, helping to create a calm and restorative environment that supports wellbeing and recovery.
The simple form of the building and its compact footprint also have important sustainability benefits.
This approach generates a good wall-tofloor ratio which, combined with a highlyinsulated envelope, limited areas of curtain walling, and the use of LED lighting throughout, results in a building which is highly energy efficient.
The use of timber cladding and hybrid curtain wall and window systems has also reduced the quantity of embodied carbon.
And additional energy savings have been realised via the inclusion of two large air source heat pumps and a large PV array at roof level.
Where possible, sedum roofs were included, which help with attenuating storm water run off, while the large biodiverse ‘balancing pond’ has biodiversity benefits on top of wellbeing advantages, with deer using it to cool off in the height of summer.
Unlike other hospitals with A&E departments, Heatherwood is not affected by the demands of emergency care.
Instead, it can operate six days a week, morning to night, without having to manage emergency patients, and clinicians are not taken away from elective work.
In addition to its six ultra-clean theatres, the hospital features a 48-bed inpatient unit and outpatient and diagnostic facilities for orthopaedics, cardiology, radiology, lithotripsy, physiotherapy, and orthodontics.
The hospital was commissioned by Frimley Health NHS Foundation Trust and, since its launch, has reduced waiting times for patients needing knee and hip replacements, with more than 1,000 joint replacements performed in the first 10 months — up 20% on the number of procedures carried out pre-COVID.
The hospital has also successfully reduced the length of time patients stay in hospital, with 40% of patients safely discharged within 24 hours.
Sean Woodhead, architect associate at BDP, said: “When we first bid for the project in 2015 and discovered that the trust was looking at using the existing woodland site with this lovely kitchen garden from the original hospital, we jumped at the opportunity to be involved as it is not often you get the chance to design a hospital in a location like this.”
The design of the hospital and ward environment was one of a number of topics addressed in the National NHS Adult Inpatient Survey and plays a key role in shaping patient experience.
Research (Roger Ulrich) has shown that having a hospital room with a window view of a natural setting has restorative influences, therefore helping to reduce length of stay.


And, at Heatherwood, all rooms have views over woodland, access to terraces, and, therefore, fresh air.
Inpatient accommodation is located on the top floor of the hospital, in what is referred to as a ‘notional treehouse’, with close views into the tree canopy. Corridors are relatively short and, in many cases, single sided, with additional full-height glazing at the ends, allowing access to views and daylight.
Another key plank of BDP’s design approach was to ensure that the layout and arrangement of the hospital was purposefully compact, minimising travel distances, both internally and externally.
The outpatient department, indeed the whole of the ambulatory entrance floor, operates as a digitally-enabled one-stop shop of clinical services for patients, where they can have a consultation, imaging, and procedure all in one visit, delivering patient-focused care with high levels of efficiency and safety — as well as reducing stress and saving on car journeys.
Meanwhile, another floor is entirely dedicated to surgery, optimising the flow, with expansion space designed in to accommodate two more theatres if needed in the future.
And theatres are paired so staff can easily go from one to the other, resulting in optimum efficiency.
This approach to design has enabled the hospital to introduce innovative ways of working to increase the number of operations it performs, such as
It is our belief that this model should form part of the future of healthcare and bringing together specialist services makes absolute sense, rather than combining lots of different services into one site


trialling orthopaedic ‘super weeks’ where surgeons managed to double the number of weekly joint replacement procedures from 40 to 80.
The day surgery unit itself operates on a ‘medi-room’ model of care and its design and layout is informed by Post Occupancy Evaluation analysis from the day surgery unit at Frimley Park Hospital.
Following consent, the patient is allocated a medi-room for the duration of their stay.
From this multi-functional room, they will change, meet with the anaesthetist and surgeon, and wait in a gown ready for their procedure.
Following the operation, and a short time spent in the first-stage recovery unit, the patient will return to their medi-room for second-stage recovery, before changing and being discharged.
There are a number of benefits to this approach, including improved privacy and dignity; larger spaces to make changing easier; and the patient can be accompanied by family members if desired.
Staff were also at the forefront of the design, with staff bases on the inpatient floor naturally lit with access to private terraces, while changing facilities are also provided.
The optimised approach to building layout has supported the trust’s wider goals regarding the rationalisation of services across all of its sites, by centralising elective services in Ascot

emergency care in other locations.
Woodhead said: “By paying careful attention to design, including access to nature, daylight, and fresh air, and an optimised approach to layout with builtin flexibility, patients have better health outcomes and reduced recovery periods, while the wellbeing of all those using the building is supported, including staff.
“Of course, many hospitals have started as a central hospital and grown organically, but where there is the opportunity to step back and take a strategic and holistic view of the wider healthcare system or an individual trust or facility, then we should embrace it.”
It is hoped the hospital will act as a benchmark for delivering out-of-hospital services in more-therapeutic environments.
Speaking to Healthcare Property, Woodhead said: “It is not often you have the opportunity to work on a site like this and what has been really gratifying is that our aim to create a building that is people
and recognised by patients in the National NHS Adult Inpatient Survey
“It is our belief that this model should form part of the future of healthcare and bringing together specialist services makes absolute sense, rather than combining lots of different services into one site.
“By keeping clinical pathways separate, you create efficiencies.
“But, while a number of trusts are looking to do a similar kind of thing, these developments tend to be on acute sites. It is rare you get the opportunity to build on a site such as that at Heatherwood.”
Flexibility and adaptability have been incorporated into the design, which could allow the delivery of additional services in future, if required.
“For example, there is an opportunity to repurpose rooms to deliver additional, lessinterventional treatments, freeing up time in the theatres for more elective surgery”, said Woodhead. n
By paying careful attention to design, including access to nature, daylight, and fresh air, and an optimised approach to layout with built-in flexibility, patients have better health outcomes and reduced recovery periods, while the wellbeing of all those using the building is supported, including staff
Dr Axel Buether, one of the world’s leading colour experts and a pioneer of modern evidence-based colour psychology, has worked in collaboration with flooring supplier, Bona, to develop a new colour collection

Ihave studied the effects of colour for decades, and while a lot of my work has fallen across different industries, much has centred on the healthcare sector.
The impact of colour is astounding, and the colour of our surroundings significantly influences our moods and emotions and, ultimately, our wellbeing.
The applied research projects that I have been involved in focus on the effects of the environmental factor colour, the processing of which takes up more than 60% of the neuronal capacities of our brain, on human experience and behaviour as well as wellbeing and health.
Indeed, the psychology of colour is a fascinating topic.
The use of colour has astonishing results on people and different colours have different purposes.
In a healthcare environment, the colours used need to work in harmony.
There needs to be a balance because too much, or too little, of one colour may have
negative effects, and, as an example, could make people feel anxious or unwell.
Equally, bright red or green are often used to create stimulating environments and therefore are not often found in healthcare.
Colour is an atmospheric environmental factor that can make us tired, listless, and sick, or keep us awake, active, and healthy.
It therefore has the strength to change people’s healthcare journey.
My research has taken me to more than 100 different hospitals in Europe over many years, and has covered a wide and diverse area — all with colour as a core focus.
For instance, I have explored innovative colour concepts which have proven to have a positive impact on the wellbeing and health of patients and staff.
The use of colour is not only about creating great aesthetics, it’s so much more.
It can facilitate positive interactions in a healthcare environment which can, in turn,
lead to many benefits.
Historically, the interior design and feel of healthcare organisations such as hospitals were often referred to as ‘clinical’ — the colour scheme was commonly restricted to white, which, while it makes spaces feel clean, it can also feel sterile, lacking character and warmth.
Today, there has been enormous progress and a move away from how healthcare facilities looked in the past.
Colours are now being factored into the design process to make healthcare settings look, and feel, more appealing.
By incorporating the right colours, spaces can be transformed into warm and welcoming areas that meet the needs of those using the facilities.
The incorporation of colour into design was often focused on the walls, and I was quite fascinated by the positive contribution that a floor’s colour could have on people’s


My latest collaboration, the development of the Bona Resilient Colour Collection, is a brand-new range of flooring products which has been tailored to the unique needs of the healthcare environment.
The collection, which draws inspiration from the natural world, can be successfully applied on resilient floor surfaces in any setting — from nursing and care homes, to therapy centres, hospitals, or children’s clinics.
Resilient surfaces are widespread in healthcare and include materials such as PVC, rubber, vinyl, and linoleum — and hence the impact of flooring colour is vast.
In healthcare, staff are often under enormous stress and pressure, working long-hours, sometimes with little, or no, breaks.
It’s a high-paced, demanding environment where many life-changing decisions are made.
To relieve some of this pressure, and reduce the level of stress and anxiety that people experience, a calming atmosphere is essential, and, remember, colour can evoke positive feelings and be used to elevate our mood.
By incorporating natural elements into interior spaces, starting with the floor colour, it can profoundly enhance wellbeing and improve physical health; increase trust and confidence; and improve staff focus and experience.
Recent research, Colour as a design tool: The design of the effects of light and surface colours in relation to the experience and behaviour of people in the built space, reports that a positive atmosphere can improve the wellbeing of building occupants, visitors, and staff by up to 100%.
The 2020 report also reveals that a colour concept that takes into consideration daylight conditions, structural context, and usability criteria, improves workplace identification by more than 50% and reduces sick leave by around 30%; while the rating of the working environment among staff improved by 40%.
When considering the ongoing difficulties that healthcare faces around workforce recruitment and retention, of which burnout and stress are one of the key drivers, the colour of flooring delivers additional relevance.
As well as supporting everyone’s wellbeing, a relaxing, calm atmosphere can also support the patient recovery process.
Furthermore, by improving the mental health and wellbeing of staff, and relieving the pressure of the hectic work-life for healthcare professionals, it can, in turn, facilitate the delivery of better patient care.
People work and feel their best when they are in a natural environment, and connecting with nature has a myriad of benefits, therefore any design should be developed in harmony with nature.
The best colour schemes in healthcare are those that consist of colours found in nature as these promote a positive atmosphere — soft, natural, earthy shades radiate warmth and comfort and create a calm and healing environment.
The right balance of colours not only makes an area feel more open and spacious; it is crucial for maintaining a professional-yet-comforting atmosphere, without evoking a sense of coldness, and by using earth tone colours on flooring such as a grey-green, or grey-blue range, it projects seriousness and credibility, which is particularly important for patient trust.
The positive effect of carefully-selected surface colours on patients, staff, and visitors has been scientifically proven, and there are hospitals and other healthcare facilities that are setting the standard and successfully demonstrating the innovative impact of colour.
While this has often largely focused on the walls, the colour of flooring can also deliver many benefits; helping to improve our overall experience in healthcare. n

Offsite construction methods underpin delivery of hospital project
Arecent project at Peterborough Hospital highlights the versatility and efficiency offered by modular construction approaches.
With a significant challenge in increasing its bed capacity during the winter, the hospital faced a time when demand for healthcare services peaked dramatically.
To meet this need efficiently, the hospital turned to modular building specialist, Wernick.
The new two-storey building, consisting of 22 modules, added 20 beds with ensuite facilities and included essential hospital infrastructure such as a reception area, pantry, offices, and utility rooms.
To ensure aesthetic harmony with the surrounding buildings, a terracotta rainscreen cladding was incorporated.
The project demonstrated the effectiveness of modular construction in addressing urgent healthcare infrastructure needs, particularly when speed and quality are paramount.
Wernick’s HM Flex modular solution not only met the immediate requirements, but also provided a flexible option for future expansion.
The quick installation process helped minimise disruption to ongoing hospital operations, a crucial factor in a healthcare setting.
Peterborough Hospital required an emergency facility delivered on time, with minimal disruption to hospital activities.


And, where required, modules arrive with interior fixtures and fittings in situ, decreasing the time required at the location further.
Programme reliability and speed are fundamental benefits of modular construction, making it ideally suited to healthcare environments.
David Moss, director of estates and facilities at Peterborough Hospital when the project was commissioned and completed, said: “The reason why we needed to expand our hospital bed base is because we were under real pressure in the winter months.
“The additional 20 beds will be used to alleviate some of the pressures that we will feel in the winter period.
“We needed a solution to be delivered quickly, so we went for a modular option”.
Manufacturing a building in a factory setting while building work takes place onsite cuts construction programmes by approximately 50%.
Modules are taken to the site by lorry and craned into position, a process which can take just one or two days.
As a result, the movement of vehicles and the number of personnel required for each project can be reduced by as much as 90% compared to many ‘traditional’ build programmes.
This means lower noise pollution and disturbance to patients, as well as fewer carbon emissions and diesel fumes from power generators and construction vehicles.
Sites with tight access points or a small footprint also benefit from decreased movements on site.
Modules are constructed to strict standards — Wernick’s modules are manufactured under ISO 9001 and 14001, in a dedicated facility, using a building system which fits the client’s budget and aesthetic.
These systems are also carefully designed to minimise material waste during the construction phase, and any waste produced is fully recycled, all without compromising the performance of the building for its intended use.
The look of the building was an important consideration for the hospital trust, which specified external cladding to match the buildings already on site.
The result is a facility that is indistinguishable from the surrounding hospital building.
A link to the main rehabilitation building, provided using an additional module, further creates the illusion of a building that has always been there.
Mark Carter, commercial director at Wernick Buildings, said: “Our work in Peterborough stands as a testament to how modular buildings can effectively relieve the pressures on healthcare facilities and support the growing demand for accommodation space.
“By employing our modular construction approach, we were able to deliver highquality accommodation swiftly, minimising disruption to ongoing medical services.
“We are proud to deliver a building that helps Peterborough Hospital to continue its vital work in a well-equipped and supportive environment.”n


This month saw the winners of the 2025 Healthcare Design Awards announced at a ceremony in London
The 2025 Healthcare Design Awards was held in London on 13 February, recognising innovation and excellence in the design of health and care facilities.
Celebrating and rewarding projects that do not just demonstrate good design, but have made a real impact on people’s lives, seven trophies were handed out at the event.
Introducing celebrity guest speaker, Jo Brand, to the stage at the event, Jo Makosinski, editor of
construction costs, workforce shortages, and a change in government, to name just a few.
“But, against this backdrop is the fact that the need for health and care services is growing.
“And the importance of the environments from which these services are delivered cannot be underestimated.
“Every person in this room today has contributed to delivering both new and refurbished buildings which will have a long-


“The Healthcare Design Awards aims to recognise these efforts and promote a new approach to delivering health and care infrastructure which truly puts person-centred care at its heart.
“This year the judges had a very difficult time deciding the winners as the standard of entries was particularly high.
“But those they have chosen are projects they believe are changing the way we look at designing health and care buildings and














New research shows that nearly half of the public trust fire doors in hospitals to be fit for purpose, despite an increase in incidents
Despite an 18% increase in fires across NHS trusts—averaging nearly four incidents a day —52% of people still consider hospitals to be among the safest buildings.
A survey of 2,000 adults, conducted as part of the British Woodworking Federation’s Fire Door Safety Week campaign, focused on the theme ‘A False Sense of Safety’.
The campaign aims to bridge the gap between perceived safety and actual fire risk, encouraging the public to engage in fire safety awareness and report any fire door issues, regardless of location or the assumption that fire safety is someone else’s responsibility.
When asked about fire safety in other buildings, 36% of respondents considered schools to be as safe as hospitals, and 26% felt the same about care homes.
This contrasts with recent reports from the East Sussex Fire and Rescue Service, where two care home directors were fined nearly £125,000 for multiple fire safety violations, which included defective fire doors and a lack of detection equipment and alarms, across four premises.
Helen Hewitt, chief executive of the British Woodworking Federation (BWF), said: “Our latest research shows that people often have a greater sense of fire safety in buildings like schools and hospitals.

“Regardless of where you are, it is crucial to be aware of fire safety measures, such as emergency exits and fire doors, because the risk of fire is present in any building.”
When considering building safety, emergency exits were cited as the mostimportant factor in feeling safe by 75% of respondents, followed closely by visible fire safety measures, including alarms and fire doors (70%).
Additionally, 46% of respondents said they always, or often, notice fire doors in the buildings they visit.
Regarding the buildings where respondents believed fire doors are well maintained, 47% felt that fire doors in
Hewitt said: “Fire doors are crucial in
preventing the spread of fire and smoke.
“It’s encouraging that more people are noticing fire doors in the buildings they visit, but there’s still work to be done to ensure people feel confident in spotting and reporting fire door issues.
“Knowing who to report these problems to is key — start with the premises manager or owner, and escalate unresolved issues as needed.
“With the correct information, we can all contribute to maintaining fire safety.”
Fire doors require expert maintenance to remain effective. However, 29% of respondents would trust management and 27% would trust the building owner to handle fire door issues, while 13% would trust a handyman, and 19% a caretaker.
For fire doors to function correctly, they must be installed and maintained by a competent, trained professional.
Gavin Tomlinson, Protection and Business Safety Scrutiny Committee chairman at the National Fire Chiefs Council (NFCC), said: “Fire doors are an essential feature in most buildings, helping to protect both occupants and responding firefighters in the event of a fire.
“When well fitted and properly maintained, fire doors provide vital protection against the spread of fire within buildings.
“While legislation requires those responsible for fire safety to have arrangements for testing and maintaining fire safety measures, people should feel safe in the buildings they visit or work in, and they should feel empowered to report faults and raise concerns, particularly those related to fire doors.” n
It’s encouraging that more people are noticing fire doors in the buildings they visit, but there’s still work to be done to ensure people feel confident in spotting and reporting fire door issues
NHS Shared Business Services (NHS SBS) has launched three new soft facilities management (FM) procurement solutions designed to enhance operational efficiency, save costs, and ensure highquality environments for NHS patients, staff, and visitors.
Together, the new framework agreements for linen and laundry, grounds maintenance, and security services — with a combined value of £375m — provide NHS trusts and other public organisations with a compliant and cost-effective way to source solutions that support the day-to-day running, upkeep, and caretaking of facilities across their estates.
Nick Verburg, head of category management at NHS SBS said: “The framework agreements provide essential services that support clean, safe, and functional environments, aligning with government and NHS national priorities for a resilient and efficient healthcare system.
“Developed with a regional structure to ensure all sizes of suppliers are included, we are delighted to be able to offer a blend and provide a choice of solutions for the NHS, and to work with hospitals, trusts, and Integrated Care Systems to manage their soft FM needs.”



Valued at £150m, the framework agreement provides a comprehensive solution for managed laundry and linen services, including hiring, buying, and decontaminating — critical to the prevention and control of infections in healthcare settings — through to repairing and recycling of old linen, enabling its reuse for cost efficiencies.
Promoting sustainable practices, it aligns with the NHS’s net-zero carbon goals and its regional structure gives buyers the ability to source from local NHS suppliers and small-to-medium-sized enterprises (SMEs), which constitute 56% of suppliers on the framework agreement.
Addressing the critical need for safety, the £125m framework agreement provides access to a range of security services, including manned guarding, keyholding, and emergency response.
By helping NHS organisations protect staff, patients and assets, the framework agreement ensures a secure environment essential for delivering uninterrupted care.
All three framework agreements simplify procurement by providing access to preapproved suppliers, removing the need for lengthy and complex tender processes.
And, with transparent pricing and inclusive access to suppliers, including SMEs, they make procurement more accessible and equitable.
Aligned with the NHS’s net-zero carbon ambitions, the agreements also offer environmentally-conscious solutions, from sustainable laundry practices to energy-efficient equipment.
Verburg said: “By streamlining procurement and ensuring access to highquality sustainable services, we’re helping healthcare organisations save time and money while enhancing patient care.” n


WFiona Schaefer, innovation manager at InnoScot Health, considers the Scottish NHS carbon net zero challenge, looking at what the sector has achieved and what it needs to focus on moving forward
ith the NHS continuing to strive to meet net zero carbon ambitions in the coming years, never has there been greater focus on identifying and integrating greener alternatives.
With activity aimed at meeting NHS Scotland’s 2040 net zero emissions target gathering pace, we have seen tremendous progress made across the country’s healthcare facilities through robust innovation-driven strategies, including the launch of its National Green Theatres Programme.
We also believe that NHS Scotland is now poised to make major strides across 2025 in that vital drive, which is not only reducing health service impact on the environment and generating cost savings, but also — and most importantly — helping to enhance the wellbeing of the very people it is treating.
It is now firmly recognised that climate change exacerbates existing health risks
while posing new challenges which impact the health of the population, healthcare assets, and services.
As Dr Tedros Adhanom Ghebreyesus, director-general of the World Health Organization, put it: “The most-pressing reasons for urgent climate action are the impacts, not in the future, but right now, on health.
“The climate crisis is a health crisis.”
The Scottish Government agrees, stating that ‘NHS Scotland plays a pivotal role in safeguarding the life and health of communities by developing climate-resilient health systems capable of responding to these evolving threats’.
In achieving net zero, the greatest challenge is reducing building energy emissions, resulting chiefly from heating, lighting, and hospital activity.
The good news is that emissions from
the energy used to heat and power NHS Scotland buildings continue to fall steadily — in some cases helped by purposebuilt facilities.
Embodying the cutting-edge green vision, the new University Hospital Monklands in Lanarkshire is being built as a fully-digital and net zero carbon exemplar.
Also falling steadily are medical gas emissions, including the replacement of anaesthetic gas, Desflurane, with a less-harmful gas, which is now saving emissions equivalent to powering 1,700 homes every year.
In fact, NHS Scotland won the European Sustainable Healthcare Project of the Year Award in 2023 after becoming the first national health service in the UK to stop using Desflurane with its high global warming potential and marked contribution to the carbon footprint of healthcare facilities.
In 2022/23, NHS Scotland’s reported emissions from its net zero target areas were 571,000 tonnes of carbon dioxide equivalent, of which 407,000 resulted from building energy use — a huge 70%.
A point of concern, yes, but also a clear picture of where significant effort needs to be concentrated.


Last August, Scotland’s Cabinet Secretary for Health and Social Care, Neil Gray, also noted that a minority of 20 NHS sites were responsible for over 60% of building energy emissions, with decarbonisation plans being prepared for those priority sites, a move rightly considered ‘critical to decarbonising the NHS’.
Gray cautioned that ‘some of these sites will be easier to decarbonise than others due to their age and construction’, but it is encouraging, nevertheless, to note that determined action is now either planned, or is underway, to continue the momentum behind a 31% reduction in NHS Scotland’s total heat and power emissions evidenced between 2015-16 and 2022-23.
Last year’s Annual NHS Scotland Climate Emergency & Sustainability Report echoed the Health Secretary’s sentiments, stating that: “For building energy, much more now needs to be done, but the achievements so far should make us hopeful in realising that further progress can be made.”
Indeed, the report found that NHS Scotland collectively met all of its annual energy targets relating to heating and powering buildings while its primary goals remain focused on:
• Reducing greenhouse gas emissions from NHS buildings by at least 75% by 2030 compared to a 1990 baseline
• Renewable heating systems being integrated into all NHS-owned buildings by 2038
• Net zero emissions being achieved by 2040 or earlier for all of its estate
In order to achieve those goals, the Scottish Government has urged that the country’s health boards ‘must find innovative solutions to reduce their energy emissions’.
To that end, significant sustainable opportunities include the potential for replacement of more-traditional energy forms with biomass boilers, solar panels, air source and ground source heat pumps, and battery storage.
We believe that innovation targeted at lowering buildings' emissions identified by the knowledgeable, insightful Scottish health service workforce can be a huge asset in achieving that desired progress — and there are many opportunities for forward thinkers.
Certainly, staff can play a vital role in decarbonising NHS buildings by identifying, not only lesser-used areas which could benefit from the integration of
We believe that innovation targeted at lowering buildings' emissions identified by the knowledgeable, insightful Scottish health service workforce can be a huge asset in achieving that desired progress — and there are many opportunities for forward thinkers
smart technologies to monitor and respond to usage patterns, but also noting where improved building insulation and upgraded glazing could be most effective, thereby producing marked efficiency savings.
Only recently, staff at NHS Forth Valley revealed their work to optimise building energy usage within high carbon theatre facilities, including adjusting the speed of Heating, Ventilation, and Air Conditioning (HVAC) systems equipped with fans and evaluating the effectiveness of anaesthetic gas scavenging systems while maintaining safe and efficient working conditions.
Sometimes external innovation can be just as effective as internal innovation.
Considering the natural environment around NHS sites, with staff-led initiatives helping to maintain and improve their biodiversity, are also enhancing wellbeing opportunities for both staff and patients.
Hand in hand with that is the continued rollout of eHealth and digital technologies to reduce travel, together with decarbonising fleet vehicles, making NHS sites truly greener places.
NHS teams are also undoubtedly best placed to offer everyday insights into how to manage building waste more effectively and encourage circular economy principles such as motivating patients to return used inhalers and introducing best practice on their wards.
Ultimately, they can be ambassadors for change, pushing for fellow workforce innovators to share ideas, while raising awareness and supporting sustainable action.
And InnoScot Health has a sustainability innovation call seeking forwardthinking ideas from health and social care professionals that can help support NHS Scotland in its green ambitions moving forward. n
Healthcare organisations could save in excess of £200,000 a year by introducing energy-efficient solar carport technology.
Solspan says its research — which spanned multiple sectors including healthcare — ‘underscores the adaptability and widespread advantages of solar car ports’.
The company said: “For healthcare organisations, solar car ports can help power essential medical equipment and reduce energy costs in facilities that operate 24/7, allowing hospitals and clinics to allocate resources more effectively while enhancing their sustainability efforts.
“Beyond cost efficiencies, solar car ports could also play a critical role in reducing carbon footprints and advancing sustainability targets.”
It adds: “By generating renewable energy on site, organisations can slash operational costs, achieve energy independence, and meet increasing environmental regulations.”
The environmental benefits are equally compelling.

Solar car ports could cut the sector’s annual CO2 emissions by over 23 million kilograms, equivalent to 767 round-trip flights between London and New York, and reduce emissions by 230 million kilograms over 10 years.
The EV charging capabilities of solar carports could also power over 427,000 electric vehicles annually, translating to 4.2 million EVs over the same period, according to the research.
To help healthcare businesses realise these benefits, Solspan has launched what it dubs ‘an innovative online calculator’.
A spokesman said: “By simply inputting the
number of car parking spaces, organisations can instantly calculate their potential annual financial and carbon savings.
“This tool provides tailored insights, making it easier for organisations in the healthcare sector to make informed decisions about adopting solar car port solutions.”
The study, based on publicly-available data, evaluates the average number of car park spaces for organisations across different sectors, annual sunlight hours for each area, and current business electricity rates.
Clifford Huntley, research and development director at Solspan, said: “This analysis underscores the immense potential of solar car ports in delivering both economic and environmental advantages.
“Our goal is to support businesses in the healthcare sector in making informed decisions that contribute to a sustainable future while also enhancing their bottom line.
“Our new savings calculator is an invaluable tool for organisations to visualise their potential savings and environmental impact.”
Assura plc has announced the completion of two healthcare development projects, which are its first schemes designed to be net zero carbon.
The company, which is the UK’s leading diversified healthcare REIT, has delivered sustainable healthcare schemes in Fareham and Winchester at a combined total development cost of £13.6m.
At Fareham, a refurbishment of an existing high street building into a specialist children and family development centre for Hampshire and Isle of Wight Healthcare NHS Foundation Trust focused on controlling the internal environment using as little energy as possible.
Significant upgrades were made to the roof, walls, and windows, combined with the installation of an all-electric heat pump system, powered using as much renewable energy as possible from 72 new solar panels installed on the roof.
While, at Winchester, a new-build city centre development for a medical practice serving over 17,000 patients also features an all-electric energy solution as well as maximising solar panels on the roof to minimise the ongoing running costs for the tenant.
Whole-life carbon assessments are now

being updated and finalised for each site to reflect the materials used during construction to calculate the final embodied carbon required to be offset.
In line with UK Green Building Council guidelines, actual energy consumption will be monitored at both sites over the first 12 months of operation to compare performance against design assumptions, with appropriate adjustments and offset credits then acquired to ensure operational net zero has been achieved.
Jonathan Murphy, chief executive of Assura plc, said: “Today’s announcement demonstrates delivery against our commitment to produce sustainable healthcare assets that offer a positive social impact to the communities they serve, while helping our healthcare customers to meet
their net zero carbon aspirations.
“We have a clear, stated ambition to be net zero carbon by 2040 and the number one listed property business for long-term social impact.
“The completion of our first two developments applying the Assura Net Zero Carbon Design Guide marks further progress.
“Our ESG strategy, The Bigger Picture, sits at the heart of our business and decision making and we will continue to deliver impressive buildings that facilitate the delivery of highquality healthcare services.
“As the first FTSE 250 B Corp, Assura is continually focused on prioritising the positive impact we have on all our stakeholders.”
Adding to this achievement, the company has also announced that the Northumbria Health and Care Academy in Cramlington, which opened last summer, has become the first healthcare building in the UK to achieve WELL Building Standard Gold Certification.
The academy, let to the Northumbria Healthcare NHS Foundation Trust on a 30-year lease, provides training to nurses, midwives, and allied health professionals such as physiotherapists, radiographers, podiatrists, and occupational therapists.

EACH EDITION COVERS...
Environmental
Sustainability, carbon reduction, and energy efficiency news, features, insight, and case studies
Projects
The latest building projects in health and social care
Finance
Key drivers behind the health and care property investment markets and procurement insight
Property news
The latest property deals
Market insight
An overview of the key issues impacting the property sector (construction figures, reports, industry comment etc)


Design & Build
Best practice approaches to the design and construction of the health and social care estate
Estates & Facilities
The latest issues impacting estates and facilities management practices in health and care settings
Product
Focus on building products which are helping to boost health and social care environments
People overs and shakers within health and social care
SCAN HERE TO SUBSCRIBE
