In this Issue:
• Challenges in Treatment of a Hyper-Divergent Patient with TM-dysfunction, Maxillary Prognathism, Dento-alveolar Protrusion and Gummy Smile: A Case Study
• The Safety and Efficacy of Fixed Sagittal Appliance Therapy: A Clinical Survey
• Influence of Facial Structures on the Perception of Smile Esthetics between Laypersons and Orthodontists – A Cross-sectional Analytical Study
• Orthodontic Treatment of a Geminated Maxillary Lateral Incisor: A Case Report
International Journal of
VOLUME 35 | NUMBER 1 | Spring 2024 Visit the IAO online at www.iaortho.org
Published Quarterly by the International Association for Orthodontics
Orthodontics
Editorial

Hello fellow orthodontic practitioners, I am writing this editorial thinking about where dentistry and especially Orthodontics will be in the coming years. I do not have a crystal ball I only havethe lessons taught from my past to guide and help improve our profession.
As editor of the journal, I read a lot of articles submitted for publication.The managing editor, Mrs. Allison Hester, and I attempt to produce an interesting quarterly with articles that add to the orthodontic knowledge base so members can research like problems and their treatments when encountered in their practices.
This is a valuable benefit of IAO membership as is the ability topick up the phone and call someone regarding a clinical issue you may encounter. Please know that as an IAO member, you have that opportunity and ability to learn from each other.
The IAO has valuable resources to increase your clinical abilities. CaseworX, for example, is fantastic to record and document your cases. It is used to walk you through your fellowship application and after that your Diplomate. It is valuable to have your cases evaluated by your peers you learn from, and in completing the cases, you will have a broader appreciation of what you can do as an orthodontic health care provider.
As technology improves we will be able to understand when and how treatment needs to be applied to set up the best outcome. We, as general practitioners practicing orthodontics, have a front seat at the growth and development show. Our staff must be aware of this so that they can identify and
point out easily correctable clinical issues that if ignored, may worsen over time.
The common denominator in my years of orthodontic learning has to be the application of timely intervention, so that development does not result in undesirable situations. In the future, artificial intelligence may help guide clinical choices – for the end result of facial and dental beauty starts at a very young age.
I am excited to see what the future of the profession holds; however, this future stands on the shoulders of collegiality and cooperation. My suggestion is to help each other learn and obtain accreditation in this great profession of orthodontic health care.
I am always available for comments, complaints or suggestions regarding the journaI. I thank Mrs. Allison Hester, our managing editor, for her invaluable role in getting the journal completed and looking so good.
I have a request to all who read this, and the ask is to please help each other to write and submit articles or case reports to the journal. The journal is YOUR journal and you can make it reflect what is important to you today. In doing so making the journal better for everyone, now and in the future. Also , send the journal to your friends and share the knowledge.
Yours for accredited GP orthodontic education and better patient care
I remain
Respectfully
Dr. Rob Pasch DDS MSc IBO General Practitioner.
2
Dr. Rob Pasch Editor
Editor
Rob Pasch, DDS, MSc, IBO
Mississauga, Ontario, Canada
E-mail: paschrob@rogers.com
Managing Editor
Allison Hester
8305 Pennwood Dr Sherwood, AR 72120
E-mail: allisonhijo@gmail.com
Consultants
Adrian Palencar, ON, Canada
Michel Champagne, QC, Canada
Dany Robert, QC, Canada
Scott J. Manning, USA
Mike Lowry, AB, Canada
Edmund Liem, BC, Canada
Yosh Jefferson, NJ, USA
G Dave Singh, CO, USA
Monika Tyszkowski, IL, USA
William Buckley, OH, USA
International Journal of Orthodontics, copyright 2020 (ISSN #1539-1450). Published quarterly (March, June, September, December) by International Association for Orthodontics, 750 North Lincoln Memorial Drive, #422, Milwaukee, WI 53202 as a membership benefit. All statements of opinion and of supposed fact are published on the authority of the writer under whose name they appear and are not to be regarded as views of the IAO. Printed in the USA. Periodical postage paid at Milwaukee, WI and additional mailing offices. Subscription for member $15 (dues allocation) annually; $40 U.S. non-member; $60 foreign. Postmaster: Send address changes and all correspondence to:
International Journal of Orthodontics 750 North Lincoln Memorial Drive, #422 Milwaukee, WI, USA 53202
Phone 414-272-2757 Fax 414-272-2754
E-mail: worldheadquarters@iaortho.org
Challenges in Treatment of a Hyper-Divergent Patient with TM-dysfunction, Maxillary Prognathism, Dento-alveolar Protrusion and Gummy Smile: A Case Study, by Adrian J. Palencar, MUDr, MAGD, IBO, FADI, FPFA, FICD
The Safety and Efficacy of Fixed Sagittal Appliance Therapy: A Clinical Survey, by Stephen Deal, DDS, Crispen Simmons, DDS, Soroush Zaghi, MD
Influence of Facial Structures on the Perception of Smile Esthetics between Laypersons and Orthodontists – A Cross-sectional Analytical Study, by Dr. Fizzah Ikram, Dr. Rashna Hoshang Sukhia, and Dr. Mubassar Fida
Orthodontic Treatment of a Geminated Maxillary Lateral Incisor: A Case Report, by Rami Aboujaoude, Lina Aboujaoude, Falah Aboujaoude, Carla Jabre, Jad Nasr
Editorial, by Dr. Rob Pasch, DDS MSc IBO, Editor
Growing Beautiful Teeth Chapter 7: Max the Maxilla, by Estie Bav
Practice Management Tips: How to Achieve Consistent Case Acceptance, by Scott J Manning, MBA; Founder, Dental Success Today
Tips from the Experienced: The Utility Arch, Part 1, by Dr. Adrian J. Palencar, MUDr, MAGD, IBO, FADI, FPFA, FICD
Author’s Guidelines

AUTHOR’S GUIDELINES FOR THE INTERNATIONAL JOURNAL OF ORTHODONTICS POSTED ONLINE AT www.iaortho.org. Past IAO publications (since 1961) available online in the members only section at www.iaortho.org.
SPRING 2024 VOLUME 35 NUMBER 1
Table of Contents
G&H Orthodontics 25 Highland Metals 30
International Journal of Orthodontics
Visit the IAO online at www.iaortho.org 6 16 2 12 26 14 31
Departments Advertisers
FEATURES
32 35
Challenges in Treatment of a Hyper-Divergent Patient with TM-dysfunction, Maxillary Prognathism, Dento-alveolar Protrusion and Gummy Smile:
Adrian J. Palencar, MUDr, MAGD, IBO, FADI, FPFA, FICD
A Case Study
AUTHOR

Dr. Adrian Palencar MUDr Komenski University (Stomatology), Bratislava Slovakia
Recertified 1970 Unversity of Western Ontario.
Master AGD, IBO Diplomate, Fellow Academy of Dentistry International, Fellow Pierre Fouchard Academy, Fellow International College of Dentists.
Recipient of IAO PINSKER Award (2003) IBO Examiner 2005-2014, Master Senior Instructor, IAO education Committee Examiner, IJO and Spectrum Ortho Consultant.
Assistant instructor Rondeau Seminars (21 years).
Authored 14 articles, co-authored 2 articles (with Dr David Pampena), authored 48 IAO Monthly Tips and 389 page “Case finishing and Mechanics” for Rondeau Seminars.
Abstract:
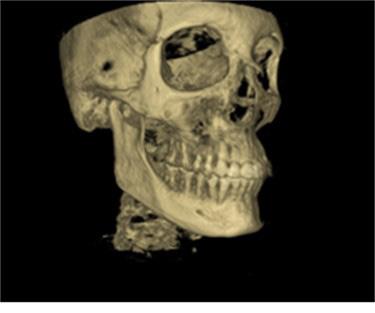
There are many challenges we face in our everyday clinical practice. Some patients have a robust set of problems, while others have few. Regardless of the number and nature of the concerns, we are obliged to diagnose and correct them so that the patient can be healthier and have better self esteem from an improved appearance. This article presents a case of a 31-year-old man with Class II skeletal and Angle Class II, Division 1 dental malocclusion, hyper-divergence, TMdysfunction, maxillary dento-alveolar protrusion, moderate crowding, and gummy smile. This complex case was treated firstly without extractions with Mandibular repositioning splint. However, later in the treatment the patient required odontectomy of two second maxillary bicuspids, and TADs. The total treatment time was 41 months.
Keywords: TAD (Temporary Anchorage Device); Power arm; Translation; Power thread; Third Newton Law; Odontectomy; Regional acceleratory phenomenon; TM disfunction; Anterior repositioning splint; Protrusive appliance; Closing coil spring; Elastomeric chain; Retainer.
Conflict of Interest: None
*This article has been peer reviewed
Introduction:
Skeletal hyper-divergence:
Traits: long lower face, dolichocephalic, high mandibular plane angle, skeletal open bite,and clockwise grower. The cause of hyper-divergence during development of the individual may have been the following:
1. Mouth breathing due to soft tissue dysfunction (enlarged adenoids, tonsils, allergies, nasal obstruction)
2. Incorrect tongue position
3. Tethered oral tissue (tongue and lip tie)
4. Poor oral positions (lips apart, tongue is not resting on the palate)
5. Adverse swallowing patterns
6. Thumb and finger sucking
7. Genetics (only 10%)
The treatment is multifactorial. The first line of action is to eliminate detrimental habits, render the airway patent, implement orofacial and myofunctional therapy, high pull head gear, occlusal bite blocks, repulsing magnets, and TADs for intrusion of maxillary molars. Finally, if there is crowding, the odontectomy of selected posterior teeth would be considered. In extreme cases, orthognathic surgery may be the only solution.1
Dental Crowding:
This is a condition where all teeth do not fit into dental arches. They may be misaligned, rotated, impacted, or ectopically erupted. Causes are narrow arches, habits, premature exfoliation of deciduous teeth, the odontectomy of deciduous teeth, supernumerary teeth, and tooth decay. Treatment depends on a careful analysis and treatment planning for the orthodontic patient. We may create space to alleviate crowding by transverse development of dental arches, distalization of posterior teeth, mesialization of anterior teeth, proclination of anterior teeth, airrotor slenderizing (IPR) and in severe cases, the odontectomy of a selected tooth or teeth.2
4
Featured*
Prognathism
Prognathism is a positional relationship of the mandible and maxilla to the skeletal base, where either jaw protrudes beyond the predetermined imaginary line in the coronal plane (frontal plane) of the skull. Prognathism in humans can be due to normal variation among phenotypes. In the human population where it is not the norm, it may be due to a malformation, the result of an injury, a disease state, or a hereditary condition. 3 In disease states, maxillary prognathism is associated with Crouzon syndrome, Down syndrome, and Cornelia de Lange syndrome.4 Treatment of the mild and moderate maxillary prognathism is orthodontics in combination with surgical plates and TADs. However, the severe true maxillary prognathism requires orthodontic therapy and orthognathic surgery.
Dento-alveolar protrusion is a positional relationship of the alveolar process and anterior teeth to the skeletal base. Not all dento-alveolar protrusions are anomalous, and significant differences can be observed between different ethnic groups. Harmful habits such as thumb sucking, tongue thrusting, and lip biting can result in or exaggerate dento-alveolar protrusion, which causes teeth to misalign. The combination of oro-facial myofunctional therapy, habit breaker, functional appliances, fixed orthodontic treatment, and lifetime retention is required for a successful outcome.
“Gummy Smile”5
It is an appearance, which frequently precipitates a visit (or referral) to an orthodontic clinician. Teenagers (mostly females) may become very concerned about the appearance of their smile. Some of them may even become shy or introverted. A recent survey suggests that 37% - 47% of people say that the first thing that they notice when meeting someone is their smile. If there is more than 2 mm of exposed gingival display during the posed (dynamic) smile, it is considered a “gummy smile.” This condition is quite common. It is found in 10.5% - 29% of the population and it is more common in females. Etiology of “gummy smile” can be multifactorial and therefore must be accurately diagnosed to render the appropriate treatment.
The factors that contribute to the “gummy smile” include:
1. Hypertrophic gingiva
2. Altered passive eruption
3. Excessive incisal wear
4. Short upper lip
5. Lip hypermobility, overactive upper lip muscles, which lift the maxillary lip upward (levator labii superioris and levator anguli oris)
6. Vertical maxillary dento-alveolar excess
7. Habitual mouth breathing
Treatment must be addressed to the etiology of “gummy smile.” The following are some of the options:2
1. Altered passive eruption and Hypertrophic gingivagingivectomy
2. Excessive incisal wear - Crown lengthening and full crown coverage
3. Short upper lip – surgical lip repositioning. This surgical procedure restricts the muscle pull of elevator lip muscles, therefore reducing the gingival display while smiling.
4. Hypermobility – Botulinum Toxin injections, Hyaluronic acid
injections, lip fillers or “gummy tuck.” This surgical procedure involves removal of a small strip of tissue from the inside of the upper lip and the lip is sutured into new lower position.
5. Vertical maxillary dento-alveolar excess – orthodontic treatment, or alternatively, orthodontic treatment with orthognathic surgery
6. Habitual mouth breathing – polysomnogram, evaluation the cause of airway obstruction and appropriate therapy
Some patients have more than one contributing factor; therefore, the treatment must be managed appropriately.
The Case
An Asian male (A. B.), aged 31 years, presented to our office with the following complaints: “I do not like my teeth. I cannot close my lips. My jaw hurts. I sleep with an open mouth. I snore at night.”
Anamnesis
The patient’s medical history reveals allergy to dust and mites, clenching, grinding, and snoring at night. The patient reported TMJ discomfort and a habitual mouth breathing. He was sucking his thumb until age six. Concerning dental history, the patient had good oral hygiene, a moderate number of restorations, generalized Tetracycline stain and failing porcelain veneers on maxillary anterior teeth.
Examination
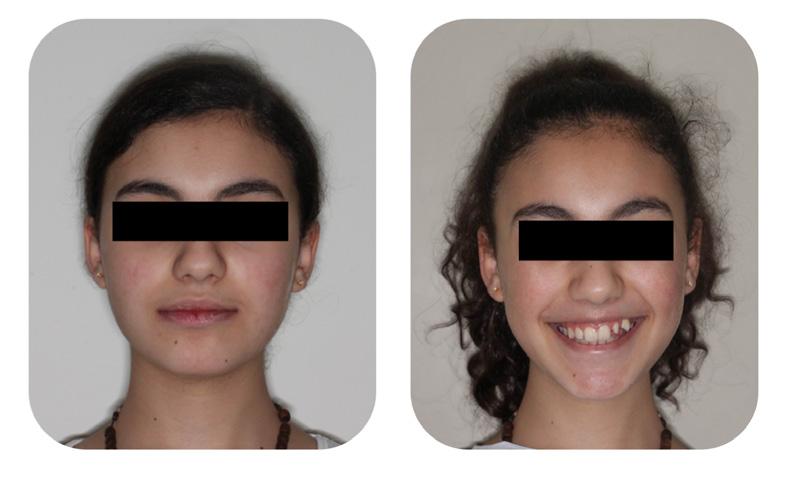
Clinical Macro-esthetic appraisal revealed normal facial symmetry, slightly longer lower face height and prognathic profile. The patient’s upper (+5.0 mm) and lower lip (+8.0 mm) were convex in relation to the “S” line (Steiner), and they were incompetent (Figure 1-A, B, C).
Clinical appraisal of patient’s posture was significant: the frontal view revealed head straight and a high right shoulder, while the lateral view revealed the head in straight position (Figure 1-D, E).

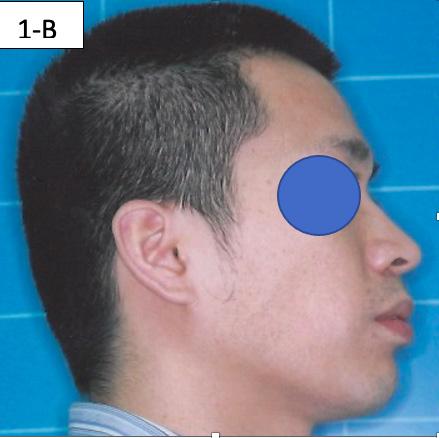
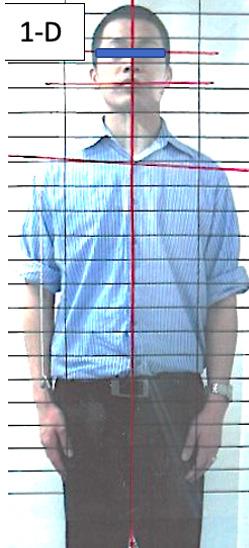
FIG 1A: Pre-treatment, frontal view
FIG 1B: Pre-treatment, lateral view
FIG 1C: Pre-treatment posed smile
FIG 1D: Pre-treatment, posture, frontal view
FIG 1E: Pre-treatment, posture, lateral view


5 5
Clinical Mini-esthetic appraisal revealed full upper and lower lips incompetent and incongruent smile arc to the lower lip. The patient’s posed smile revealed positive buccal corridors and adequate tooth display at lips in repose. (Figure 2-A, B, C).

FIG. 2A: Pre-treatment, lips together
FIG. 2B: Pre-treatment, lips in repose
FIG. 2C: Pre-treatment posed smile


Clinical appraisal of the Airway revealed a patent airway; lower airway -15/18 mm, oropharynx - Mallampati II -III, nasopharynxvery patent (Figure 3-A, B, C).





FIG. 4A: Pre-treatment, frontal view
FIG. 4B: Pre-treatment, right lateral view
FIG. 4C: Pre-treatment, left lateral view



FIG. 4D: Pre-treatment, maxilla, occlusal view
FIG. 4E: Mandible occlusal view
FIG. 4F: Pre-treatment, OB and OJ
TMJ Appraisal:
FIG.3A: Pre-treatment, lower airway
FIG. 3B: Pre-treatment, oropharynx
FIG. 3C: Pre-treatment nasopharynx

Clinical dental appraisal revealed full Angle Class II molar and cuspid relationship. The arches were wide and there was a moderate crowding. The patient had 9.0 mm overjet and 6.0 mm overbite. However, the patient reported SDB symptoms, and he also presented with symptoms and signs of TM dysfunction (Figure 4A, B, C, D, E, F))
Clinical Micro-esthetic appraisal revealed signs of attrition and abrasion. Periodontal health was good, and the patient was devoid of tooth decay. However, there was a moderate number of restorations, generalized Tetracycline stain and failing porcelain veneers on the maxillary anterior teeth.
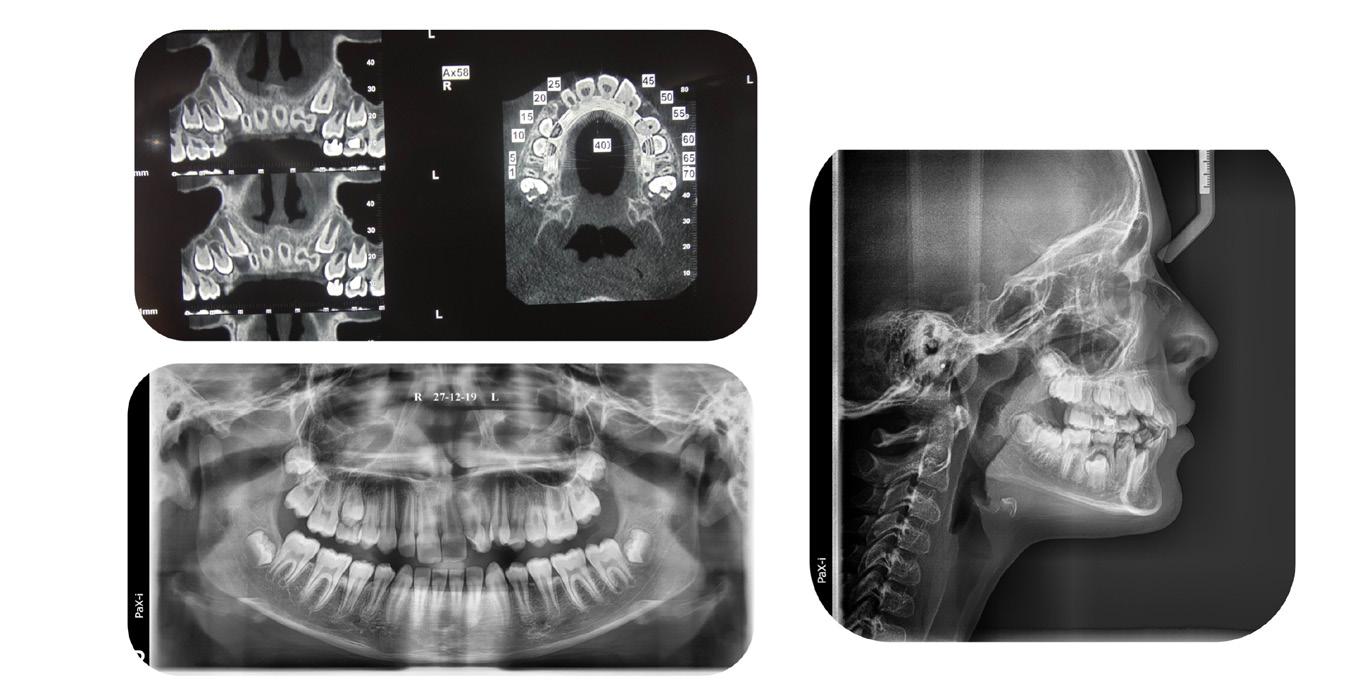
The patient had the following: migraine headaches, sore teeth upon awakening, buzzing in his ears, teeth clenching and grinding, joints locking when opened wide, popping, and clicking, pain and problems sleeping soundly. He had normal range of motion, deviation to the right on opening, clicking, The patient also had a sensitivity to palpation on the right TMJ, Posterior neck left, Trapezius left and Anterior digastric bilaterally. The transcranial TMJ radiogram reveals posteriorly displaced condyles and limited maximum opening on the right side (Figure 5-A).
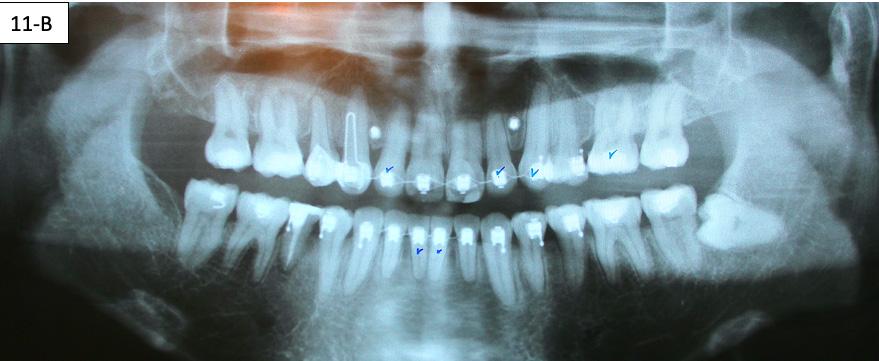
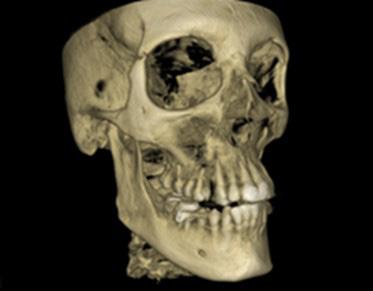
Panoramic radiogram revealed complete permanent dentition with mandibular left impacted wisdom tooth. Roots of the mandibular second bicuspids appeared to be short. There was an excellent bone support and no sign of periodontal or periapical pathology. (Figure 5-B).
Lateral Cephalometric radiogram and tracing revealed robust lower airway (18.0/15mm), CVMS 6, maxilla and mandible are prognathic (SNA - 93° and SNB - 84°), Class II skeletal (ANB –9.0 mm, Witts – 9.0 mm). The patient was hyperdivergent (NS/ GoM – 30°, ALFH - 83 mm!!), protrusive maxillary incisors (U1/ SN – 117.0°), mandibular incisors were within the norm (L1/GoM 95.0°) and Harvold Δ was 30 mm. The soft tissue profile (lips) was convex (Figure 5-C, D).
Diagnosis
The patient exhibited skeletal Class II with mild hyperdivergent tendency, slightly prognathic profile, Angle Class II, division I, with moderately crowded maxillary and mandibular arches. The patient had 9.0 mm over-jet, 6.0 mm overbite and maxillary incisors were protrusive and mandibular incisors were within the norm. The patient exhibited slight “gummy smile” because of the combination of mouth breathing, short upper lip, and vertical maxillary dento-alveolar excess. The soft tissue profile
6
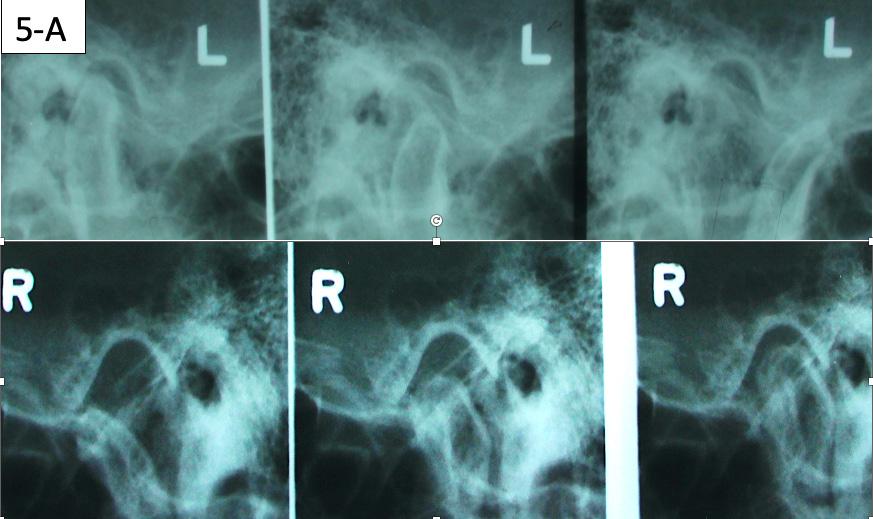
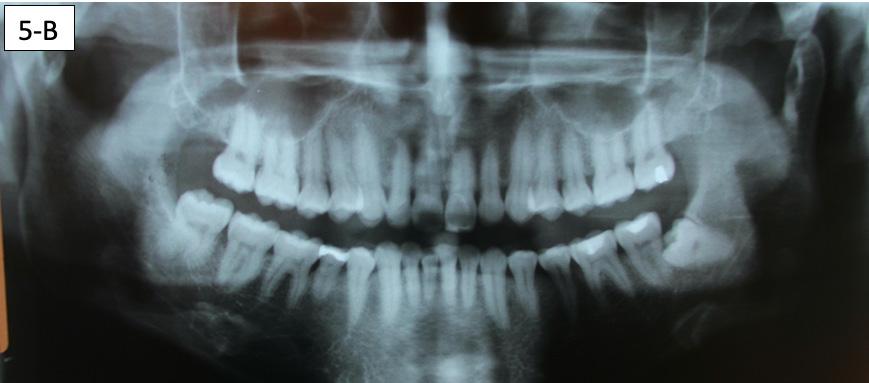

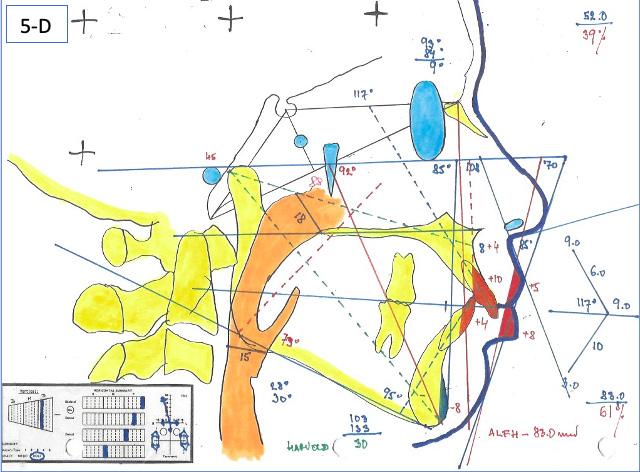
FIG. 5A: Pre-treatment, TMJ radiogram
FIG. 5B: Pre-treatment, Panoramic radiogram
FIG. 5C: Pre-treatment, Cephalometric radiogram
FIG. 5D: Pre-treatment,Cephalometric tracing
was convex. There were signs and symptoms of TM dysfunction -Internal derangement, posteriorly displaced condyles, early reciprocal click, disc displacement with reduction and limited excursion on the right condyle. The patient was a habitual mouth breather with incompetent lips.
Treatment Plan
The author proposed construction and placement of a mandibular anterior repositioning splint – in therapeutic position, where the signs and symptoms would be minimal. The time frame is 3 to 6 months. The second stage – forced eruption of the mandibular posterior teeth, followed by Straight Wire Appliance, odontectomy of #15(4) and # 25(13), placement of TADs, retraction of the maxillary anterior teeth, protraction of the maxillary molars. The third stage – placement of TADs distally to #12(7) and #22(10) and intrusion of the maxillary anterior sextant. The fourth stage – bonded and removable retainers.
Results
Maxillary and mandibular impressions were taken in irreversible hydrocolloid impression material. Both TMJ discs were recaptured in the Phonetic bite,6 which was recorded with the PVS bite recording material (Blue Bite). The therapeutic splint was fabricated, tried, inserted, and verified that the displaced discs were recaptured. This splint must be worn 24/7, except brushing the teeth, eating and sports (6-A, B, C, D, E).


FIG. 6A: Phonetic bite
FIG. 6B: Therapeutic splint
FIG. 6C: Splint in situ, frontal view
FIG. 6D: Splint in situ, right lateral view
FIG. 6E: Splint in situ, left lateral view



After the patient became accustomed wearing the splint, the acrylic was cut off distally to #46(30) and #36(19). A band was cemented on #17(2), #16(3) and #27(15), #26(14) and brackets/ tubes were bonded on #15(4), #25(13), #37(18), and #47(31). A 016 SS sectional wire was inserted in the maxilla bilaterally from the second molar to the second bicuspid and a ¼” - 4.5 oz elastics were placed for forced eruption of the mandibular second molars (Figure 7-A, B).
When the mandibular second molars became in contact with the maxillary molars, the acrylic was hollowed out from the intaglio of the splint above #46(30) and #36(19). Two ¼” –4.5 oz triangular elastics were placed for forced eruption of the mandibular first and second molars (Figure 7-C, D).
After the mandibular second molars became firmly in contact with the maxillary molars, a Maxillary removable protrusive appliance (Twin block II) with hooks was inserted to maintain the therapeutic position with the recaptured disks. Also, composite build-up was bonded to the lingual surface of #11(8) and #21(9), to maintain the mandible in the same position. Three ¼” – 4.5 oz triangular elastics were placed for forced eruption of the mandibular first molars and bicuspids. Separators were placed between the mandibular molars and bicuspids to speed up the elevation of the posterior sextants (figure 7-E, F, G).
The TMJ signs and symptoms have improved, therefore, the next step was to address the chief concerns of the patient, lip incompetence, maxillary incisor protrusion and gunny smile. The
7 7
author decided on odontectomy of #15(4) and #25(13), retraction of the maxillary anterior sextant and protraction of the maxillary molars. The intrusion of the maxillary anterior teeth would follow with the assistance of TADs.
The brackets were bonded on maxillary cuspids, bicuspids and mandibular anterior teeth followed by placement of a 014 SS sectional wire in the maxilla and a .014 SS arch wire in the mandible. Maxillary second bicuspids were extracted, and a 1.6 x 8.0 mm AncorPro (OrthoOrganizers) TADs were inserted just mesially to the first molars. Closing coil springs were attached from the TADs to the first bicuspids (Regional Acceleratory Phenomenon) (Figure 8-A, B, C).7
The brackets were bonded on the maxillary incisors and there was a progression of the arch wires a .014 NiTi, a .016 SS and a .018 SS. The progression of the arch wires in the mandible was a .016 NiTi, a .016 SS, a .018 SS and a .018 x 025 SS with the step-down distally to the cuspids. A 1.6 x 8.0 mm Ancor Pro TADs were inserted on the buccal aspect distally to the maxillary lateral incisors to aid the intrusion of the maxillary anterior sextant.8 Maxillary incisors were laced back, to prevent splaying during the intrusion and two links of an elastomeric chain were attached from the TADs to the arch wire. Power arms were bent from a .016 x 022 SS wire and ligature tied to the bracket #13(6) an #24(12).
Closing coil springs were attached from TADs to the power arms. To prevent an undesirable labial moment (flaring) of the maxillary incisors, Class I (labial intra) elastics (¼” – 4.5 oz) were


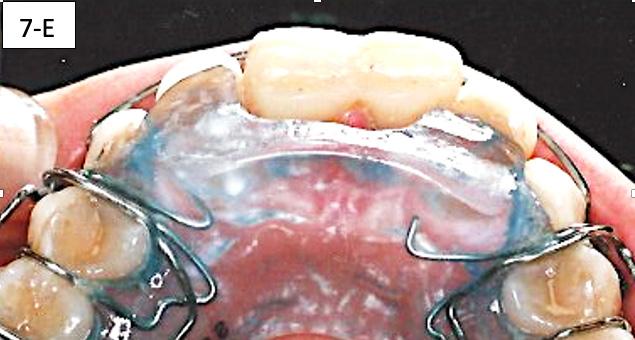
FIG. 7A: Forced eruption of #47(31)
FIG. 7B: Forced eruption of #37(18)
FIG. 7C: Forced eruption of #36(19) & #37(18)
FIG. 7D: Forced eruption #46(30) & #47(31)
FIG. 7E: Protrusive appliance and composite build-ups
FIG. 7F: Forced eruption of mandibular posterior sextants
FIG. 7G: Forced eruption of mandibular posterior sextants




placed from the buccal hook of the maxillary first molar to the helical loop on the arch wire. The helical loop was fabricated just distally to the maxillary lateral incisors on a. 018 SS arch wire (Figure 8-D, E, F, G).
Posterior TADs were removed, when interdigitations of the maxillary cuspids and first bicuspids was achieved, we initiated the protraction of the first molars. Commercial laboratory soldered buccal power arms to the orthodontic bands on #16(3) and #26(14). These power arms allowed us to apply the force close to the center of resistance of the first molars. The TADs inserted distally to maxillary second incisors previously, served two purposes: intrusion of the anterior sextant and protraction of the maxillary first molars. The applied force was delivered with an Elastomeric chain. To prevent excoriation of the attached gingiva a .018 x .025 hand bent tissue shield was bonded to the buccal surface of #13(6) (Figure 9-A, B, C, D).
The side effect of protraction of the first molars is a mesiolingual moment (rotation). To neutralize this, the force must be applied, from the palatal aspect with the Power thread or the Elastomeric chain. The Power thread is attached to the lingual cleat of the molar bands, and it is stretched to the maximum, then tied to the arch wire between the cuspids and lateral incisors. A 3/16” – 4.5 oz Class III elastic was placed on the right side and a ¼”4.5 oz triangular elastic was placed on the left side to ameliorate the interdigitation (Figure 10-A, B, C).



FIG. 8A: Odontectomy of #15(4) & # 25(13)
FIG. 8B: CCS and TAD, right lateral view
FIG. 8C: CCS and TAD, left lateral view
FIG. 8D: TADs inserted, frontal view
FIG. 8E: TADs in situ, radiogram

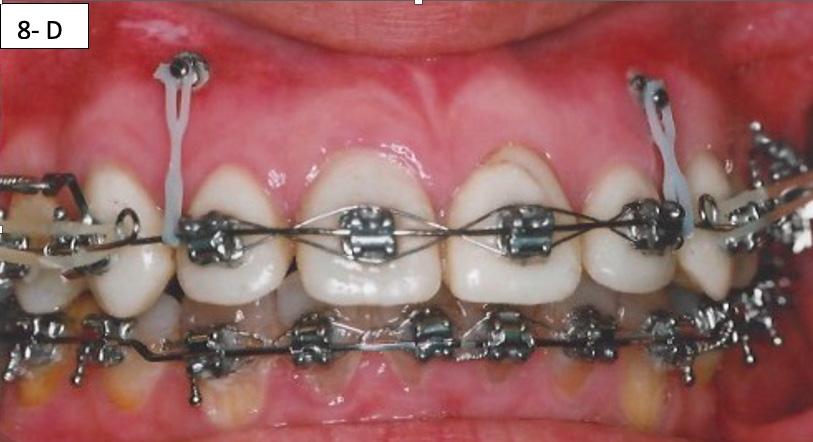


FIG. 8F: Class I elastic, right lateral view
FIG. 8G: FClass I elastic, left lateral view
8


9A: Soldered power arms
FIG. 9B: Excoriation of the







Pre-de-bracketing appraisal
Pre-de-bracketing records comprise of the facial photographs, intra-oral photographs, panoramic radiogram, and study casts. After the prudent appraisal of the bracket position, root angulation, occlusion, lips in repose, posed smile and maxillary incisor display, numerous teeth were re-bracketed. We also evaluated the improvement of the signs and symptoms of the TM dysfunction.
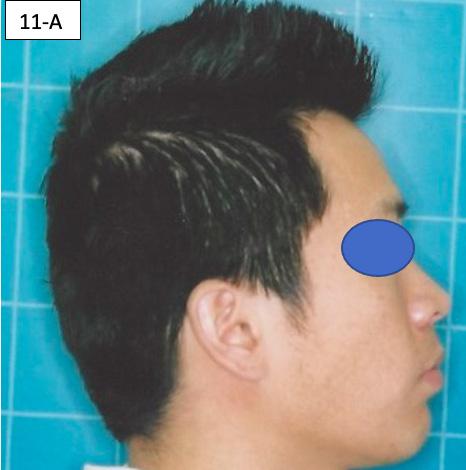
After re-bracketing, the treatment continued with the progression of the arch wires: a .014 NiTi, a .018 NiTi, a .019x025 “V” Force -3 and the final arch wire a .018x.025 SS. These final arch wires were left for three months. After this time, the esthetics, TMJ, airway, occlusion and alignment were evaluated. The patient reported that he was satisfied, and very happy with the result (Figure 11-A, B, C, D, E, F).9
Countdown on retention
One month before de-bracketing, when everyone was satisfied and the patient had a .018 x .025 SS arch wire in the maxilla and the mandible, we appointed the patient for “Countdown on retention.” The TAD’s and Tissue guard were removed and the full arch wire was left in the maxilla. However, in the mandible, it was


11A: Pre-debracketing, lateral view
11B: Pre-de-bracketing, panoramic radiogram
FIG. 11C: Pre-de-bracketing, lips in repose
FIG. 11D: Pre-debracketing, posed smile
FIG. 11E: Pre-debracketing, right lateral view
FIG. 11F: Pre-debracketing, left lateral view


cut and bent in, just distally to the cuspids. Also, two 3/8” – 2.5 oz. elastics were placed, in a letter “W” with tail configuration, for one month. They were zig-zagged from the maxillary cuspids and finished on the mandibular molars and had a slightly protrusive line of action on the mandible (Figure 12 - A, B).10
Retention
The retainers comprised of a maxillary wrap around QCM retainer with a flat pad in premaxilla to dis-occlude the posterior sextants. This also serves as an anterior deprogrammer. Also, there was inserted a bonded retainer #43(27) to #33(22). The mandibular bonded retainer was made of a .0215 flexible spiral (braided) wire, and bonded with Unitec Bond 1, and Tetric Evo (Ivoclar). The patient was instructed to wear her QCM retainer 24/7 (except sports, brushing his teeth and meals) for 12 months, and after this, only at night. The bonded mandibular retainer was recommended to stay indefinitely.
Please view the post-treatment images at the time of insertion of the retainers (Figure 13 – A, B, C. D, E, F, G, H, I, J, K, L).
Six months after the de-bracketing, the patient requested replacement of his eight deteriorating porcelain veneers in the maxillary arch (Figure 14 – A).
9 9
FIG.
oral mucosa
FIG. 9C: Tissue guard, right lateral view
FIG. 9D: Protraction of the first molar, left lateral view
FIG. 10A: Lingual intra – Power thread, occlusal view
FIG. 10B: Class II elastic, right lateral view
FIG. 10C: Triangular elastic, left lateral view
FIG.
FIG.
FIG. 12A: “W” with tail, right lateral view
FIG. 12B: “W” with tail, left lateral view








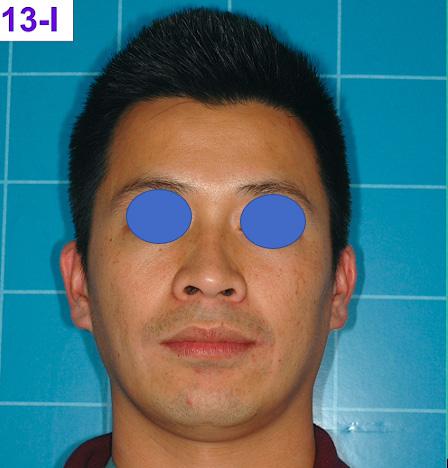

FIG. 13A: Post-treatment, fontal view
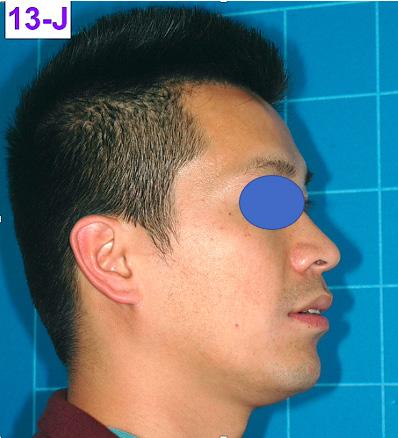

FIG. 13B: Post treatment, right lateral view
FIG. 13C: Post-treatment, left lateral view
FIG. 13D: Post-treatment, maxilla, occlusal view
FIG. 13E: Post-treatment, mandible, occlusal view
FIG. 13F: Maxillary QCM retainer
FIG. 13G: Post-treatment, lips in repose
Fig. 13H: Post-treatment, posed smile
Fig. 13I: Post-treatment, fontal view
Fig. 13J: Post treatment, lateral view
Fig. 13K: Post-treatment, posed smile Text
Fig 13L: Post-treatment, profile





Fig. 15A: Post-treatment, Cephalometric radiogram
Fig. 15B: Post-treatment, Panoramic radiogram
Fig. 15C: Post-treatment, Cephalometric tracing
Fig.15D: Cephalometric superimposition
Table 1: Panoramic and Cephalometric radiograms, and Midsagittal Cephalometric Analysis

10
FIG. 14A: Bonded porcelain veneers, frontal view
Discussion
This orthodontic case involved several functional and esthetic concerns. Of chief concern were:
1. Incompetent lips and protrusive maxillary incisors
2. Short upper lip, vertical maxillary excess and gummy smile
3. Prognathic maxilla
4. Class II division 1 malocclusion
In addition to these problems, the patient presented with habitual mouth breathing and several signs and symptoms of TM dysfunction. He exhibited hyperdivergence. The patient’s lips were severely convex related to the “S” line (Steiner) and incompetent.
Although the treatment was a lengthy one (41 months), our outcome was favourable. The patient was finished with a skeletal class II, and Angle Class I cuspid and a Class II molar relationship with minimal overjet and overbite. ANB improved from 9° to 7°however, Wits improved from 9.0 mm to 5.0 mm. ALFH decreased by 4.0 mm due to the odontectomy of maxillary second bicuspids, which caused favourable autorotation of the mandible. This happened despite forced eruption of mandibular posterior sextants during the TMJ therapy.
The position of the anterior teeth was less favourable, U1/SN 117° to 124°, L1/GoM 95° to 99°. The Naso-labial angle improved to the ideal value from 85° to 102°. The Facial axis (Growth axis –Ricketts) changed to a more ideal value, from 88° to 91°, due to the odontectomy of two maxillary second bicuspids. The soft tissue profile was convex (lips to S line – Steiner) and improved considerably: from +5/+8 to +3/+3.
The final panoramic radiogram reveals impacted mandibular left wisdom tooth, minimal root resorption and acceptable angulation except for #22(10), where the root remained mesially oriented. Root canal therapy was done on the tooth #45(29), because it developed purulent pulpitis during the orthodontic treatment.
Concerning the finishing and esthetics, the patient expressed great satisfaction with the outcome, and we felt the occlusion was acceptable. Therefore, we agreed to end the treatment.
To summarize, the authors presented a case encompassing numerous clinical abnormalities that required a variety of treatment techniques.
The problem list included:
1. Incompetent lips and protrusive maxillary incisors
2. Short upper lip, vertical maxillary excess and gummy smile
3. Prognathic maxilla
4. Class II division 1 malocclusion
5. TM dysfunction
6. Hyper-divergence
7. Habitual mouth breathing
The treatment involved:
1. Placement of TMJ mandibular therapeutic splint
2. Forced eruption of mandibular posterior sextants
3. Placement of maxillary protrusive appliance
4. Straight Wire Appliance
5. Odontectomy of maxillary second bicuspids
6. Placement of TADs
7. Retraction and alignment of the maxillary cuspids and first bicuspids
8. Protraction and alignment of maxillary molars
9. Finishing the case
10.Retention
In conclusion, this case, offered us several opportunities. Firstly, we were excited to be challenged by such a diverse and significant set of problems. Then, it was motivational to apply a varied and unique set of orthodontic techniques towards those clinical concerns. Thirdly, we were able to watch our plan progress towards achieving a successful result. The greatest satisfaction, however, was the gleam from this young man’s greatly enhanced smile when our treatment ended.
References
1. Rasool G, Bibi T, Hasseb ulah Khan M. Comparison of dento-alveolar heights in relation to vertical facial pattern. JKCD, December 2016, Vol.7, No. 1
2. Johal A.S., Battegel J.M., Dental Crowding: comparison of three methods of assessment. European Journal of Orthodontics, 19 (1997) 543-551
3. www.Medline Plus, Medical Encyclopedia
4. Winter R.M: “Cor nelia de Lange syndrome,” J. Med. Genet., 1986;23:188
5. Mahardawi B., Wongsirichat N., Gummy smile: A Review of Etiology, Manifestations and Treatment, Siriraj Medical Journal, 2019, 71(2):168-174
6. Olmos S., Airway Centered Dentistry: (The A, B, Cs of Treatment for Chronic Face Pain/OSA and Closing Anterior Open bite Without Ortho), Oral Health, March (2017) 44-56
7. Teng G.Y.Y., Liou E.J.W., Interdental osteotomies induce Regional Acceleratory Phenomenon and accelerate tooth movement. Journal of Oral and Maxillo-facial Surgery, January 2014, 72-1, Pages 19 -29
8. Palencar A.J., Molar distalization with the assistance of Temporary Anchorage Devices. International Journal of Orthodontics, Spring 2015, Vol. 26, No. 1
9. Palencar A.J., Treatment of Prognathic Maxilla with Dento-alveolar Protrusion in Adult with Assistance of TADs: A Case Study, International Journal of Orthodontics, Spring 2019, Vol. 30,
10. Alexander R.C., The Alexander Discipline, 1986, Batavia IL, Quintessence Publishing, Pages 431 – 432
11 11
Growing Beautiful Teeth
Chapter 7: Max the Maxilla

Estie Bav is an active member and senior instructor of IAO. She graduated BDSc from the University of Western Australia, and practises in her own private family dental surgery in Melbourne Australia. In November 2018 she published her first book titled “Growing Beautiful Teeth,” primarily targeting parents, grandparents, teachers or any child health carer to look out for early signs of dental growth issues. It informs the unaware the importance and impact of teeth and jaw on other areas of health such as breathing, sleep, posture, and even behaviour.
Currently the dental profession tends to “supervise and wait” for growth issues to become complex and expensive to correct….”
“My concern is that most parents miss out on basic and important dento-facial growth information until too late.”
The book was designed to be a helpful resource for your patient to read, and for introducing the subject to younger dentists and allied health professionals who may not be familiar with the teeth-occlusion-airway-TMJ-sleep paradigm.
Her message is to get involved with a child’s dento-facialairway development early.
Growing Beautiful Teeth is available from any major online booksellers, or at
• www.drestiebav.com
• www.growingbeautifulteeth.com
She can be reached at estie@drestiebav.com
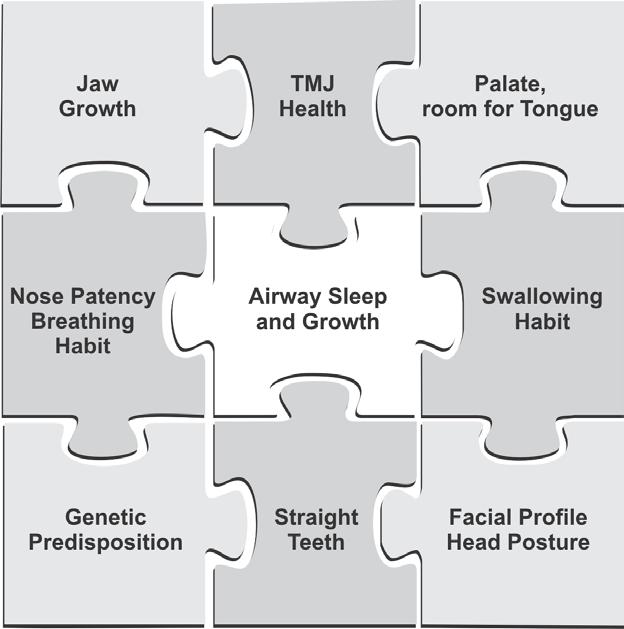
Having read through all the chapters up to here, you will by now understand how important it is to ensure that your child’s jaws develop correctly. Generally, jaw growth deficiency lies in the upper jaw, the Maxilla.
Good Reasons for Maximizing the Maxilla
1. To provide plenty of room for future permanent teeth to align and to lessen the need for any tooth extraction.

2. To have a beautiful and broad smile. When teeth are removed and/or dental arches are small, the results are often dark buccal corridors that detract from a smile. Wide dental arches will fill the smile with teeth displayed from one corner of the mouth to the other.


3. To accommodate the tongue. Often the tongue is too big for the mouth. You cannot shrink the tongue but you can develop the maxilla to accommodate it.
4. To not constrain but allow the mandible to develop forward during growth. Compression in the TMJs must be avoided to reduce the risk of TMD.
How my book can be helpful….
It takes time to educate parents on the benefits of treating dental growth issues early and explaining what signs we look for. In writing this book in simple language I hope to bring an awareness to the larger parent community, which will in turn save my dental colleagues chairside time. This book would be a helpful resource for the waiting room, and for introducing the concept to younger colleagues joining your practice.

12
EXCERPT
Arch too short and flattened… Arch too narrow and tapered… Happy arch….room for everyone
Buccal corridor: dark unfilled space caused by a narrow arch and typically tooth extractions Contrast with this gorgeous smile set in a broad dental arch
The mother has a broader smile. We suspect the daughter may have a narrower palate and dental arches.
small maxilla traps the mandible, like a car being trapped when the garage is not large enough (garage door over closes)
!!
A
Do not constrain
Fig 29: Undersized arch causes tooth crowding.
Fig 30: Broad and narrow smiles.
Fig 31: Do not constrain the mandible
5. To support a wide nasal cavity which facilitates airflow and nasal breathing.
6. To develop a balanced and attractive facial profile by allowing nature to put the lower jaw where it needs to go as the head and midface grow forward.


and When We Need Them
By the age of seven years or even earlier as necessary, the child can have x-rays of the head and jaw taken. Dentists use these to analyse the direction that the jaws, face and teeth are growing.
The two useful ones are the orthopantomogram (OPG) also known as panoramic x-rays of the head, and the lateral cephalogram (or ‘lat ceph’) which are both 2D imaging.
The OPG will show if any teeth may be congenitally missing or if there may be supernumerary teeth present. These are extra teeth above the number that we normally have. It also helps detect any upper canines that may be at risk of being impacted (stuck) due to an undersized maxilla and shortage of space.
The lateral cephalogram which captures the side view of the head and facial profile can be traced, measured, and analysed to assess the direction of the child’s growth in this area. This analysis is called a cephalometric analysis. The measurements are made in relation to a frame of references and compared to a set of average values. There are many analyses taught and used. The ideal ones measure the relative position of the jaws against the base of the cranium to give us a guide to the position of the maxilla. As we have discussed it is important to know if the maxilla may be set back too far and growth guidance therapy may need to be initiated.



There is a new digital 3D imaging known as cone-beam volumetric tomographs (CBVT) which can provide 3D views of the cranium, jaw and teeth. As more of this type of x-ray equipment is developed and released on the market, they will provide improved quality images with lower exposure to x-rays as well as at a lower cost for the patients. CBVT, due to their 3D imaging capability, are particularly helpful for studying the jaw joints, the nasal cavities, sinuses and the airway at the back of the throat.
There are many methods used by dentists to help develop the maxilla, but below are some common ones.
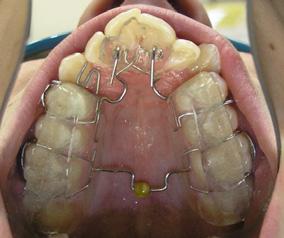
‘Expanding’ Appliances
If the maxilla needs to be expanded, or as I prefer the term ‘developed’, then the dentist will prescribe dental or oral appliances (also referred to as ‘plates’) which are customised to fit the child’s mouth.
The appliance is made to fit inside the palate of the child and this is to be worn for several months. These plates usually will have some screws or springs as components that need to be turned or ‘activated’ every few days. This activation expands the plate, which in turn will press and stimulate the maxilla to develop in the direction that we wish to gain extra growth in. For this reason, they are often known as orthopaedic appliances because they remodel or expand the bony structures to reshape the palate, and prepare and create space for the adult teeth to grow into.
There are myriads of expansion appliances designed by dentists over the years and used to achieve the orthopaedic changes required.
Broadly speaking, the appliance needs to be worn full-time (24/7) for the activation to work satisfactorily and efficiently without relapses.
Removable Appliances have the advantage of being able to be removed for hygiene. However, their correct use will require good compliance by the child and good support and supervision by the parents.
They are removed from the mouth only for cleaning purposes and for activation. As the plate is widened, so will the maxilla as it is gently nudged along. In my experience, the younger patients are usually the most cooperative or adaptive to wearing these appliances. I have made appliances for patients as young as 4 years old with great results.







13 13
Before maxilla expansion
After maxilla expansion
Fig 32: Facial profile improved after maxilla expanHead X-rays: Why
OPG or panoramic scan
Lateral Cephalogram
Ceph’ analysis
Fig 33: OPG and lateral ceph x-rays.
various appliances to max the maxilla
Fig 34: Appliances
Fixed Appliances are bonded to selected teeth and cannot be removed during the whole duration of treatment. They have the advantage of staying inside the mouth full-time for improved and controlled activation. However, mouth and teeth hygiene during the use of these appliances can be a challenge as they cannot be taken out for cleaning. Fortunately, these days new dental hygiene tools such as air or water jet spray cleaners are available and help make the task easier.
Forward-pull Face Mask
The forward-pull face mask, also referred to as a ‘reversed’ head gear, is a frame that fits around the child’s face and provides the attachments for elastic bands to protract the maxilla forward. It is used in conjunction with a palate expansion appliance and is worn mostly during the evening and night. Please be aware that this is not the usual headgear that we commonly see teenagers wear to retract their upper teeth backwards, against growth.
Forward-pull face mask are used in the very young for maximum effectiveness. Ideally, they are prescribed for those between 4–6 years old because that is when bones are very adaptable, and again to nip growth issues at the bud. Despite its appearance, I find that young kids are cooperative with wearing a forward-pull mask, especially when the parents are helpful in supervising its proper use.
Orthognathic Surgery
These are surgical techniques to treat a young adult when growth is finished (typically in the late teens), or later. Parts of the upper or lower jaw or both may be sectioned and moved to correct shape, dimension and alignment.
Again, there are pros and cons which, like all surgical treatment, need to be fully understood and taken into consideration by the patient and parents. This procedure may be avoided if growth problems are picked up and intercepted early.
Twotypesofforwardpullface mask,orreversedheadgear
Two types of forward pull face mask, or reversed headgear


We refer to the group of related issues such as mouth breathing, poor muscle tone or aberrant tongue habits that contribute to the structural deficiency as functional issues and these obviously cannot be ignored. For the best outcomes, treatment maximising the maxilla structure will need to be accompanied by various functional therapy either before, during or after the maxilla development.
There can be some confusion with the term ‘functional’ in this area of dentistry. Note that a ‘functional appliance’ can also refer to an oral appliance that is prescribed for a child with a retracted mandible that needs to grow more forward (once the maxilla has been expanded). Some common removable functional appliances include the Twin Blocks, Bionator and the Biobloc III.
Orofacial Myology
Orofacial Myology (OFM) or Oral Myofunctional Therapy (OMT) are health disciplines that are involved with training the muscles of the jaws and mouth for optimal functioning, and correcting aberrant tongue habits.
Just as orthopaedic surgery treating other parts of the body calls upon physiotherapy and exercises to promote healing, dentofacial orthopaedic changes such as maxilla development or orthodontics will be more effective when the associated muscles are retrained to function optimally as well.
OFM is a natural and essential part of guiding a child’s growth for a beautiful and healthy set of teeth, jaws, head, face and airway.
I first heard of OFM in the late 1980s when Dr John Mew, a British orthodontist (specialist) and founder of the orthotropic premise, came out from the UK to teach his techniques to a handful of general dentists here in Melbourne. He stressed that for an effective treatment outcome, there is a need for the patient to learn to keep their mouth closed and tongue properly postured.
Dr Mew wrote an amazing book titled Biobloc Therapy about his treatment philosophy and maxilla expansion technique – ‘the thoughts that initiated it, the research that founded it and the clinical work that developed it …’ – and each time I pick up the book to read, I feel enormous admiration for and inspiration from his wisdom and passion on the subject.
OFM was such an unknown subject back then and, for many years to follow, few dentists understood why or how to apply any of these exercises for the benefit of their patients.
Fortunately, this important subject has now gained wider recognition, and education in this area is gaining momentum and included in many worthwhile dental health symposium programs around the world. There are, however, too few dedicated OFM therapists in Australia currently.1
Typically, an oral myofunctional therapist (OMT) may be a speech pathologist, or a dental therapist or hygienist who has undergone further training in the subject. Dentists and osteo- or chiro-practitioners also undertake such training to learn how to detect unhelpful muscle patterns and habits that may interfere with jaw expansion treatment, and how appropriate exercises can be included as part of the therapy for their patients.
A course of dedicated OM Therapy may run for a few weeks. Ideally, they should be introduced to complement a course of dentofacial growth guidance and breathing retraining. These exercises aim to achieve the Big 3 as discussed earlier. I have noticed that some progressive ENT surgeons are also including OMT as part of their patient care. We should not be surprised because to improve breathing and airway issues, patients must use the muscles of the face and mouth correctly.
Role of Genetics
Are small maxilla and/or retruded mandible inherited? Parents often comment that the poor child takes after one of the parents
14
Fig 35: Face Mask. Functional Issues
and erroneously believe that nothing can be done to correct the situation.
Although genetic influence does play a role (especially in the Class III strong mandible pattern and the Class II Division 2 short maxilla pattern), we can see that there are many ‘environmental’ influences that are within the control of the parents to deal with, to redirect the child’s growth in the right direction.
So, one may ask what is causing this avalanche of relative underdevelopment of the upper jaw in our modern world? There are several theories offered by dentists, anthropologists, biologists and their published books are certainly well worth reading.2,3,4,5 The consensus points to mouth breathing, poor airway and sleep, poor use of orofacial muscles and making the wrong food choice. We are selecting to eat more processed foods, and this includes baby formula for infants. These types of food are often made to be eaten fast and easily without involving much chewing effort, and often with no consideration for the nutritious content.
An analogy is a child who never had to walk or to exercise the legs but was carried everywhere. The child’s leg muscles would atrophy. As we no longer eat harder and tougher foods, our orofacial muscles are not properly used and the skeletal structures they connect to do not develop as they should.
Orthodontic Teeth Alignment
Once optimal dentofacial growth has been achieved and functional issues controlled, then usually the permanent teeth will come out perfectly with no need for further treatment as nature intended.
However, sometimes it may be desirable at this stage for the young adult to have the teeth alignment idealised and this is where braces or newer techniques such as clear aligners can be used. These are treatment techniques that can fine-tune the alignment, the inclination, and/or rotation of the individual tooth. Orthodontists are especially skilled in this phase of therapy.
Adjunct Complementary Therapy
I have also found that treatment provided to my patient by osteopaths and/or chiro- practitioners who specialise in the fields of the cranium and jaw can enhance my treatment outcome for the child. These practitioners take care of the neural system to ensure good connectivity between the various parts of the body that impact on the growing dentofacial structures.
The conclusion is that your dentist and practitioners from various health disciplines must collaborate to treat the child as a whole patient, and not just the teeth, for a successful outcome.
Burnout?
Parents often ask me, ‘Is my child too young for treatment, or will my child get burnt out if we start at such a young age?’ This thought is often also used as a criticism from opponents to the philosophy of treating early. My opinion based on observation of my patients is that treating the young is a lot easier, because the problem is not so ingrained. The child is still growing and the skeletal structure is adaptable. As we all appreciate, bad habits that are well set is much harder to undo. We certainly cannot sit and watch the child suffer from poor airway, sleep, and growth.
As mentioned before, scientific studies are increasingly finding that maximising the growth of the maxilla can help treat other significant medical conditions in children such as SDB, OSA, ear
infections and nocturnal bedwetting. Indirectly, it has also been found now that poorly developed jaws and the consequences of inadequate airway, breathing and sleep, are associated with childhood obesity, childhood behavioural and social issues, and learning issues paralleling those observed in ADHD.
It is important that for a successful treatment outcome, not only must parents be enrolled in and dedicated to helping the child grow the maxilla to the max, they must also supervise the breathing and orofacial muscle retraining (daily exercises). This is an area I often find that parents, in our modern and busy world, let us down.
What Happens When the Dental Arches Shrink?
Here I want to share with the reader the case of a young oriental adult who I was sitting next to for several days at a publishing workshop. When he heard that I was a dentist, he commented that he had just been paying big sums of money for his dental treatment. He was also suffering from TMD with clicking and painful TMJs during that conference.
I noted he had a flattened midface and a long face shape, and I said to him that perhaps his mandible and tongue are constrained by an undersized and set-back maxilla. His response was interesting. He said, ‘ah ha, that makes so much sense now because ever since I had eight teeth removed with my orthodontic treatment, to have my remaining teeth straightened, my tongue has felt cramped and uncomfortable. I hate how my tongue sits nowadays. It’s like it doesn’t know where to belong.’
Beware of the collateral unwanted outcome of losing tongue space and airway when aiming for straight teeth at all costs including extractions of perfectly sound teeth.
This young man is not alone, and his experience is in fact sadly common based on what I find in my patients who attend my practice for TMD pain treatment and occlusion rehabilitation.
Your child needs more than just straight teeth treatment must seek to improve and benefit but not affect other critical areas of the body
1. For more information, visit: Academy of Orofacial Myofunctional Therapy (AOMT) at https://aomtinfo.org/ and The Australian Association of Orofacial Myology (AOMT) at http://australianassociationoforofacialmyology.org.au/
2 WA Price, Nutrition and Physical Degeneration, Price-Pottinger, 1939
3 R Cor ruccni, How Anthropology Informs the Orthodontic Diagnosis of Malocclusion’s Causes, Edwin Mellen Press, 1999
4 A Fonder, The Dental Physician (2nd Ed.), Medical-Dental Arts, 1985
5 DE Lieber man, The Story of the Human Body, Vintage Books, 2013
15 15
Fig 36:Jig-saw of the bigger picture.
The Safety and Efficacy of Fixed Sagittal Appliance Therapy: A Clinical Survey
Stephen Deal, DDS, Crispen Simmons, DDS, Soroush Zaghi, MD
AUTHORS

Dr. Stephen Deal, DDS University of Arkansas and the University of Tennessee College of Dentistry. Since 2003, his practice emphasizes proper facial growth, orthodontics and dentofacial orthopedics, TMD and Sleep Dentistry. He has completed extensive post graduate training in orthodontics, craniofacial pain, TMD and sleep. Dr. Deal has lectured internationally on the biology of facial growth and incorporating the ControlledArch System into clinical practice.

Dr. Crispen Simmons, DDS
Since graduating from the University of Tennessee Center for Health Sciences in 1977, Dr. Simmons has completed over 5000 hours of continuing dental education (advanced dental instruction). His course work has included studies of craniofacial pain, temporomandibular disorders, pain management, orthodontics, myofunctional therapy and sleep dentistry. Some of the world’s leading authorities in these fields have been his mentors.

Dr. Soroush Zaghi, MD
Dr. Zaghi is a graduate of Harvard Medical School, UCLA Otolaryngology (ENT) residency, and Stanford Sleep Surgery Fellowship. He is very active in clinical research with over 90+ peer-reviewed research journal publications and is a recognized leader on advancing standards of care for sleep-disordered breathing and tongue-tie surgery.
Abstract:
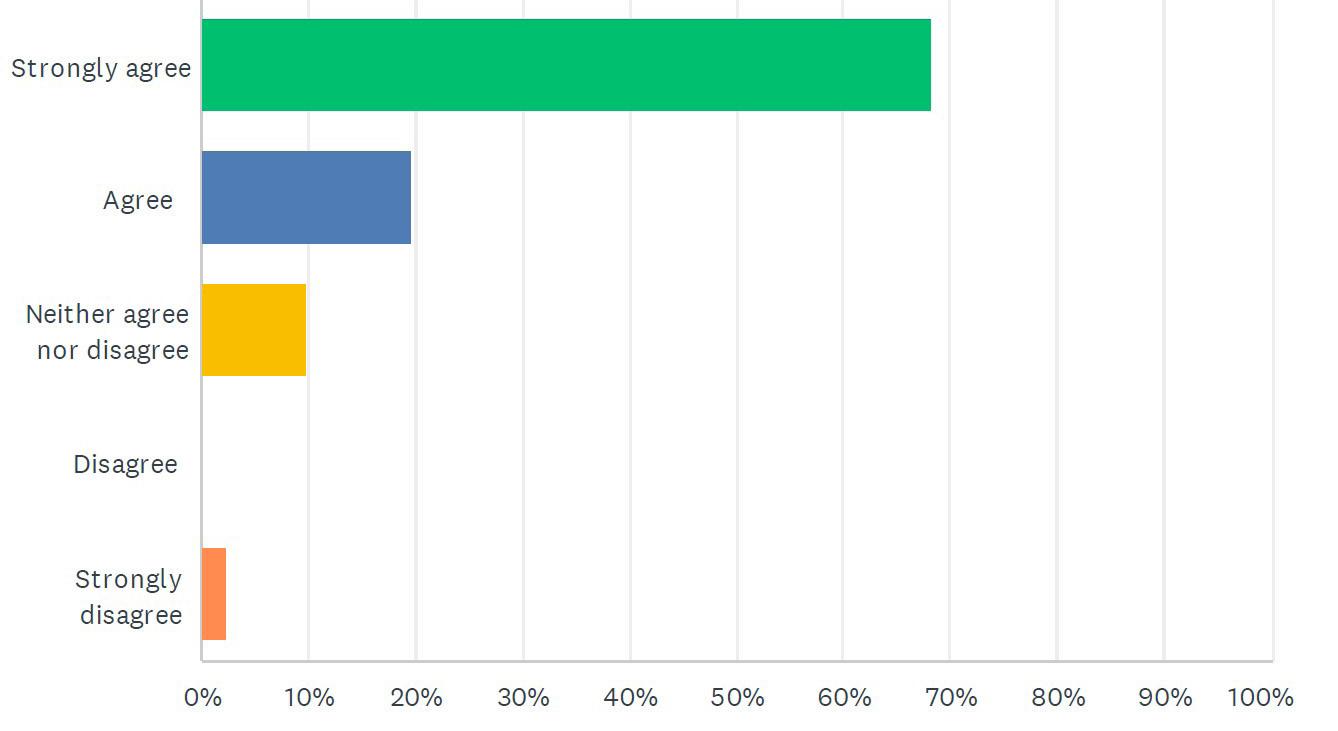
Introduction: Orthodontic/jaw orthopedic appliances have been in use for over a century and have been found to be safe and effective when used correctly. The fixed OsseoRestore™ Appliance (ORA) is a recent innovative appliance that incorporates current scientific understanding of human craniofacial growth and development. This is a clinical survey to ask practicing clinicians about the safety and efficacy of the fixed ORA.
Methods: A 15-question survey was created using SurveyMonkey software and sent to known providers of the fixed Osseo-Restore orthopedic appliance. Responses were collated and these results are reported.
Results: The most common complications reported were mouth discomfort 19.92%, tooth sensitivity 11.21%, gingival inflammation 10.43% and tongue irritation 10.29%, all common orthodontic complications. Severe complications were rare with tooth loss and tooth breakage at less than 1% and 1.36% respectively.
Discussion: Complications during and following orthodontic treatments have been well documented, and no known orthodontic therapies are without risk of undesired complications or side effects. The ORA is no exception and entails risks and benefits no different from any orthodontic/orthopedic treatments that should be weighed by providers and patients prior to implementing any treatment. Pre-existing craniofacial and oral conditions that may possibly contribute to undesirable side effects during and following treatment should be identified, discussed with the patient, and documented to ensure proper informed consent. The importance of patient selection criteria cannot be overstated when considering any recommended surgical, dental, or orthodontic therapy.
Conclusions: The ORA is a safe and effective appliance when used properly and within the biologic range of force. Like all orthodontic appliances, it has risks and benefits that should be weighed prior to treatment. These risks are well within the known complication rates of other forms of maxillary expansion. Proper patient selection criteria and critical thinking skills by the practitioner throughout treatment are essential for achieving the desired treatment responses and goals.
Conflict of Interest: None
16
been peer reviewed
*This article has
FEATURED*
Introduction:
A variety of orthodontic/jaw orthopedic appliances have been in use worldwide for well over a century and a half and, when used correctly, they have been found to be safe, efficacious and often beneficial, although not without risks and limitations in success.1 Most orthodontic/jaw orthopedic appliances currently in use have been developed by a more or less trial and error process concerned with correction or improvement of orthodontic/jaw orthopedic deficiencies presenting in the transverse, vertical, or sagittal planes. The fixed Osseo-RestoreTM appliance (ORA) is a recent innovative appliance that reflects the several previous decades contributions of many clinicians; and it incorporates current scientific understanding of the nature of human postnatal craniofacial growth and development.
The introduction of innovative orthodontic/jaw orthopedic systems or appliances has always been met with skepticism often followed by opposition from those with an opinion to defend. Dissenting opinions are a necessary and valuable component of scientific progress. Sometimes dissenting opinions are founded upon inadequate information or they are only opinions unsupported by facts.
There are many misconceptions regarding the biologic processes of craniofacial growth and development as well as orthodontic movement of teeth. Consider that even though all elements and nuances of tooth movement have not been described, or yet even to be conceptualized, it can be definitively stated that bone remodeling occurs in every case when teeth move through bone regardless of whether the movement is natural, therapeutic, or iatrogenic.2-6 This process is accomplished through a complex system of addition and resorption of bone in response to stress and strain within biologic limits when applied to the system. The change in tooth position is a direct result force amplitude and duration and is independent of the concept and mechanisms of growth. 2-4,6
Based upon the first principles of bone growth, remodeling, and repositioning that are extensively described in the literature, we can infer that any orthodontic device or appliance applying a force that is within the biologic range of force should do no more harm nor good than normal biologic processes.7 This means that if an appliance is placed properly, utilized as designed, and delivers forces within the biologic range of about 3,000 microstrain (µE) or less during growth or 1500 µE or less in adults, then the appliance would likely be safe for the delivery of the desired response to the teeth and bone. Biological loading regimes as provided by functional appliances may subject a bone to such strains and promote size and shape change consistent with the demands of the mechanical environment.8
Achieving the desired treatment responses and goals requires not only clinical experience but knowledge and comprehension of chosen appliance biologic mechanisms, capabilities, and limitations. Essential to the entire treatment process is the application of critical thinking skills by the practitioner throughout treatment. Any orthodontic/jaw orthopedic appliance can be misused resulting in clinical challenges. It is up to clinicians to properly utilize all tools at their disposal and adjust treatment planning when necessary; this includes orthodontic appliances of all types.
Evaluating the performance of any orthodontic appliance should obviously include the best applicable scientific analyses
but should also include the clinical experiences of practitioners who routinely utilize the appliances in question. To gather information regarding clinical experiences, a survey was created to poll practitioners specifically using the Osseo-Restore TM appliance in clinical practice.
Methods:
The authors developed a questionnaire survey utilizing SurveyMonkey software. The survey consisted of 15 questions submitted to 56 clinical dentists known to be experienced in ORA indications and management. The survey was designed to assess the safety and efficacy of the fixed Osseo-RestoreTM appliance and to allow clear, relevant, and timely responses with the intent of increasing participation rate. The complete survey questionnaire is found in Fig.1.
1. The CBS documentary was an unfair, biased, and onesided portrayal of the safety and efficacy of the fixed Osseo-RestoreTM appliance.
2. How many years have you been practicing dentistry?
3. How many years have you been using the fixed OsseoRestoreTM appliance?
4. How many fixed Osseo-RestoreTM appliances do you administer annually?
5. Would you consider yourself an expert, intermediate, advanced or beginner when administering the fixed OsseoRestoreTM appliance?
6. The fixed Osseo-RestoreTM appliance is safe and effective when used in appropriately selected patient candidates.
7. Complications from the fixed Osseo-RestoreTM appliance are possible but rare and infrequent.
8. Have you ever had a patient incur tooth loss that could be directly related to effects of the fixed Osseo-RestoreTM appliance rather than a unrelated pre-existing condition?
9. Have you ever seen permanent damage to oral structures that you could definitively attribute solely to the use of the fixed Osseo-RestoreTM appliance and not a pre-existing condition? If yes, please elaborate.
10.Indicate the frequency of occurrence of the following complications when administering the fixed OsseoRestoreTM appliance.
11. Rank your most common indications for treatment with the fixed Osseo-RestoreTM appliance from most common to least common.
12.Based upon your diagnosis, what is the average maxillary development indicated when using the fixed OsseoRestoreTM appliance?
13.Indicate the frequency of occurrence of the following subjective comments made by your patients following the completion of fixed Osseo-RestoreTM appliance therapy?
14.Do you intend to continue use of the fixed OsseoRestoreTM appliance?
15.Do you feel that the fixed Osseo-RestoreTM appliance is safe and effective when utilizing it to treat your patients?
FIG. 1: Complete survey questionnaire
17 17
Results:
Forty-one of the 56 (41/56) practitioners surveyed responded, yielding a 73% participation rate. This is considered a good survey response rate. On average, the participants had been in practice for 25 years with a cumulative total of 1,014 years of clinical experience. Eighty-three percent of the participants prescribed between 5-80 fixed Osseo-RestoreTM appliances each year. Over 60% of the respondents rated themselves as advanced/expert when administering the fixed Osseo-RestoreTM appliance.
Questions regarding complications yielded the following responses:
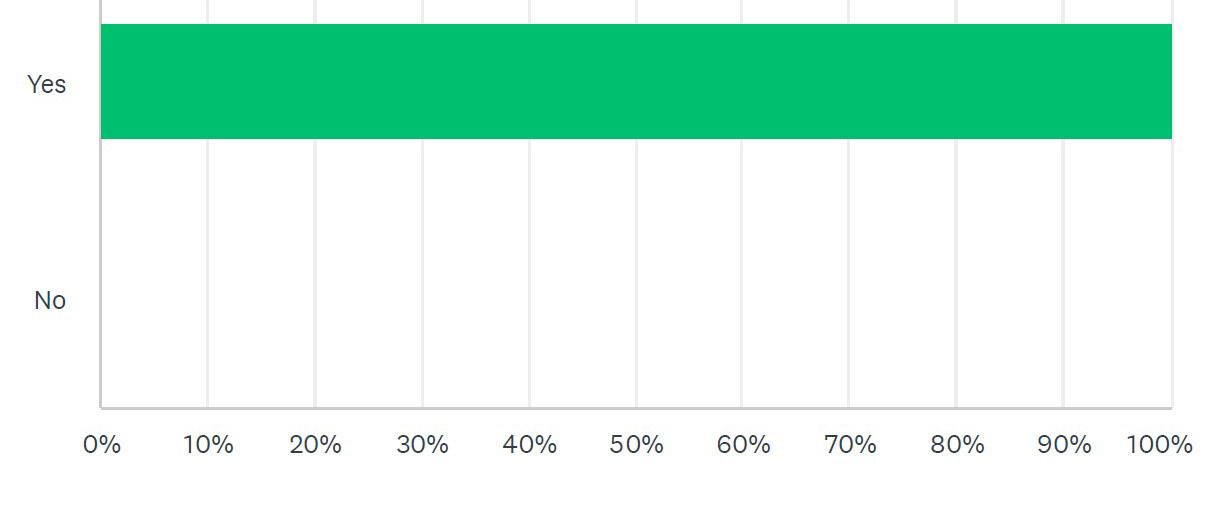
All respondents (100%) rated the fixed Osseo-RestoreTM appliance as safe and effective when used in appropriately selected patient candidates. Most respondents (97%) stated that complications from the therapeutic use of fixed Osseo-RestoreTM are rare and infrequent.
Assessing major complications, 97% stated they had never had a patient lose a tooth attributable to the effects of the fixed OsseoRestoreTM. Many (92%) stated that they had never seen permanent damage to any oral structures that could be attributed solely to the use of the fixed Osseo-RestoreTM.
When ask to access the frequency of complications noted in their clinical experience, participants responded as indicated in Table 1.



18
Fig 2A: The CBS documentary was an unfair, biased, and one-sided portrayal of the safety and efficacy of the Fixed OsseoRestore Appliance.
Fig 2B: How many years have you been practicing dentistry?
Fig 2C: How many years have you been using the Fixed OsseoRestore Appliance?
Table 1: Responses to frequency of complications noted
Fig 2D: How many Fixed OsseoRestore Appliances do you administer annually?

Fig 2E: Would you consider yourself an expert, advanced, intermediate, or beginner when administerin the Fixed OsseoRestory Appliance?
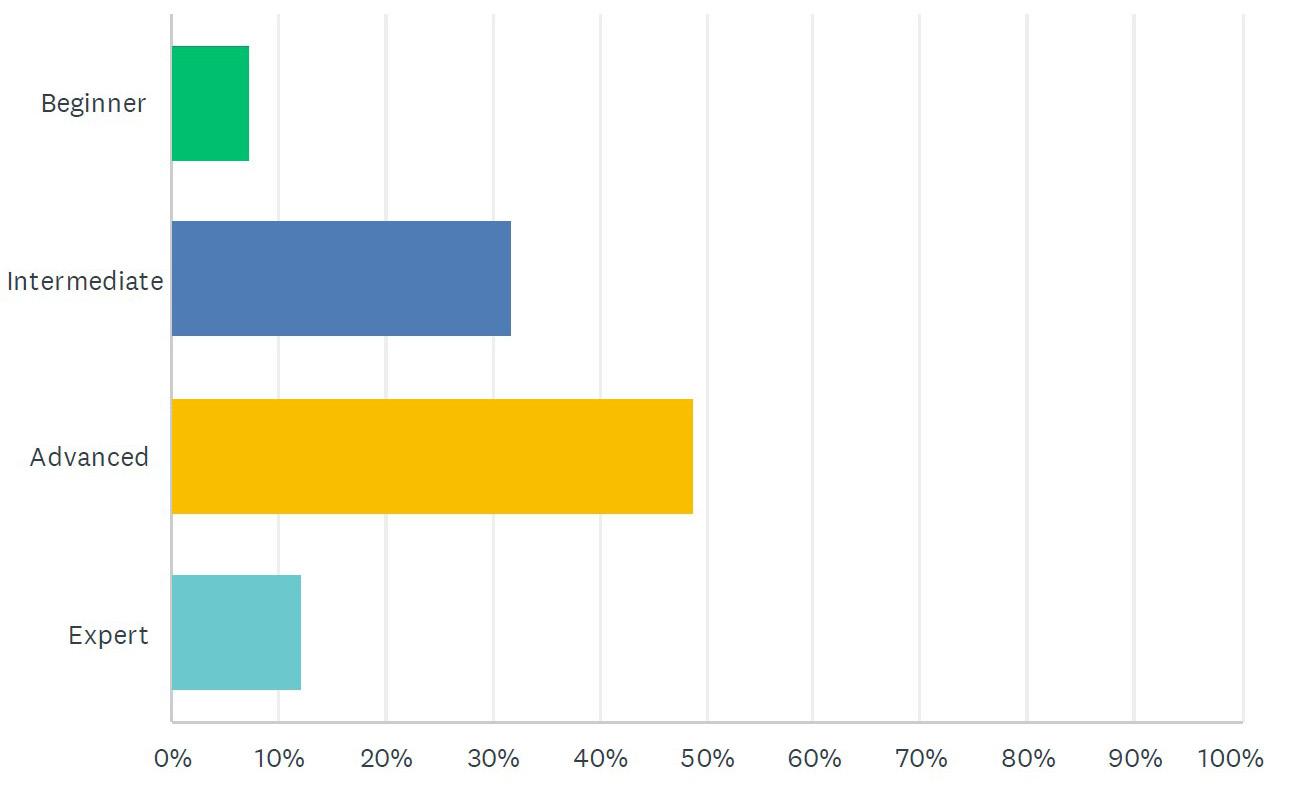
Fig 2F: Complications from the Fixed OsseoRestore Appliance are possible but rare and infrequent.
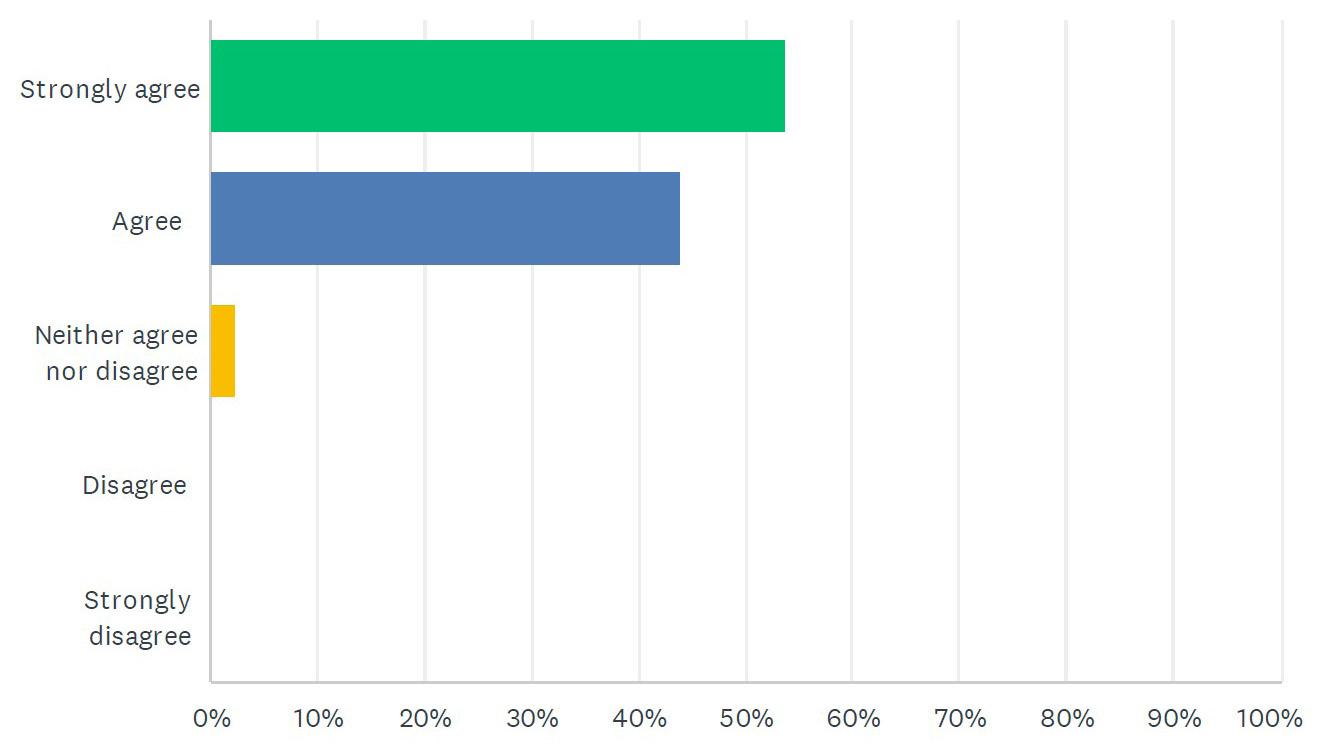
Fig 2g: The Fixed OsseoRestore Appliance is safe and effective when used in appropriately selected patient candidates.

Fig 2H: Have you ever seen permanent damage to oral structures that you could definitively attribute solely to use of the Fixed OsseoRestore Appliance and not a preexisting condition? If yes, please elaborate.

Fig 2I: Have you ever had a patient incur tooth loss, that could be directly related to effects of the OsseoRestore Appliance rather than a unrelated preexisting condition?
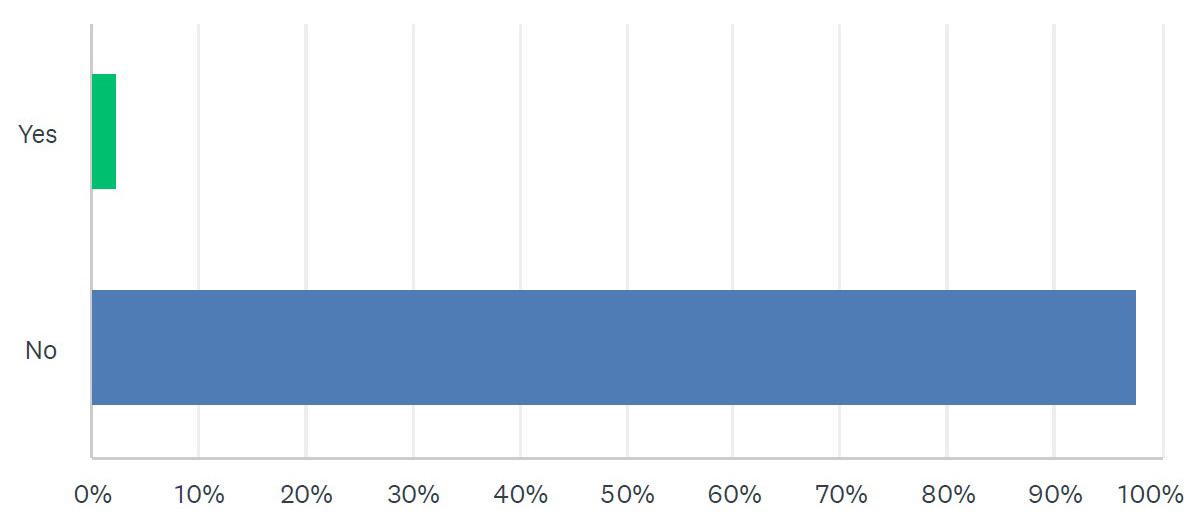
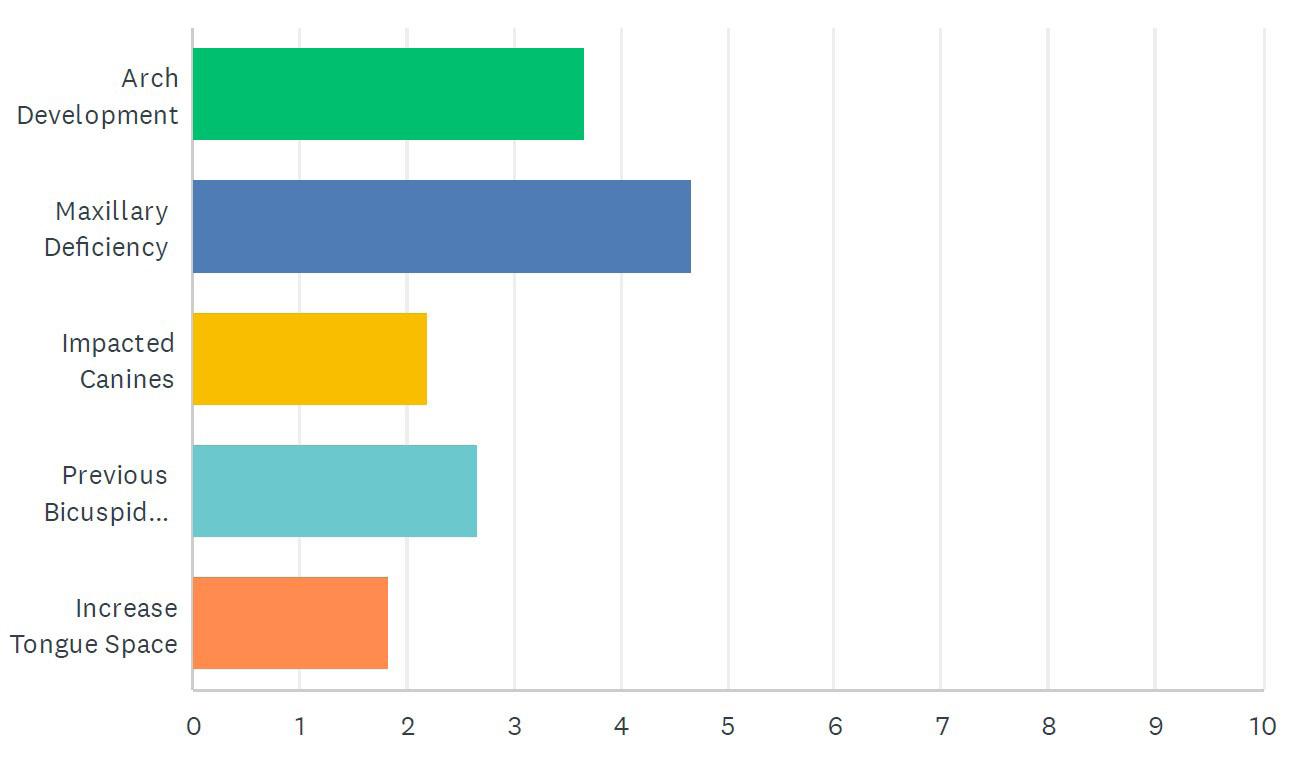
Fig 2J: Rank your most common indications for treatment with the Fixed OsseoRestore Appliance from most common to least common.
19 19
Fig 2K: Based upon your diagnosis, what is the average maxillary development indicated when using the Fixed OsseoRestore Appliance?
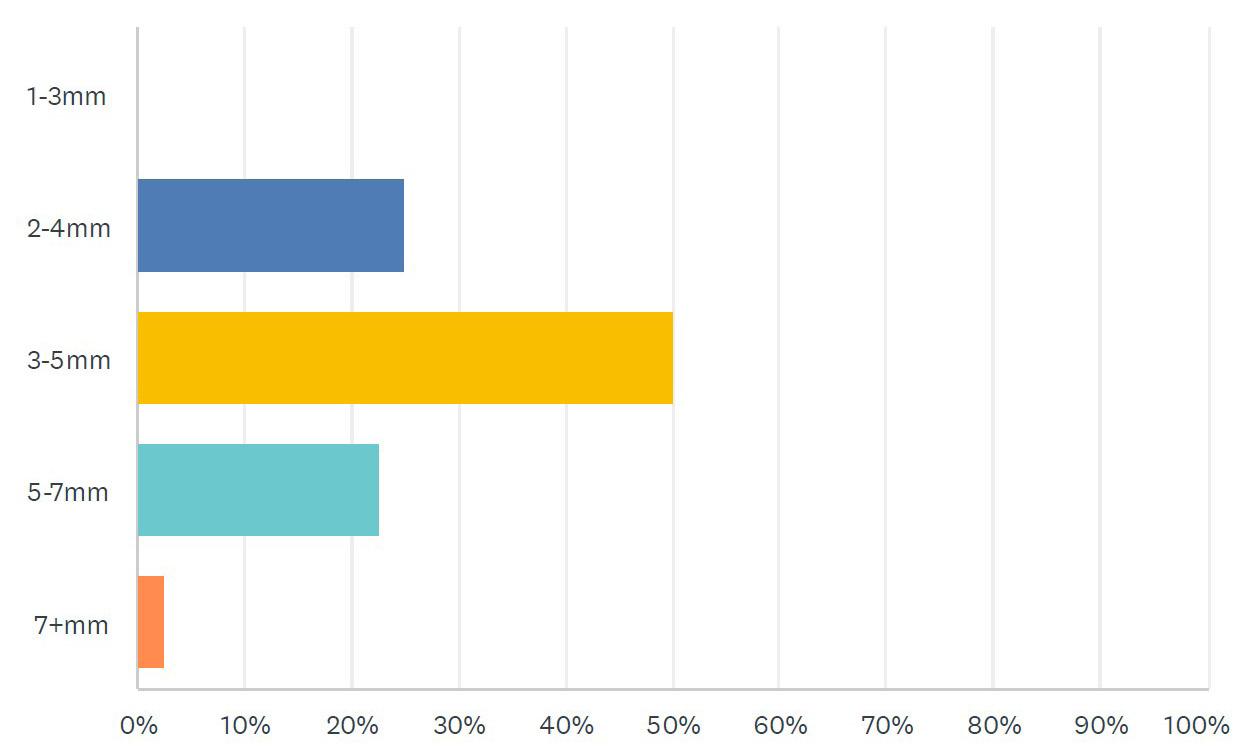
Fig 2L: Indicate the frequency of occurrance of the following subjective comments made by your patients following the completion of Fixed OsseoRestore Appliance therapy?

Fig 2M: Rank your most common indications for treatment with the fixed Osseo-RestoreTM appliance from most common to least common.

Fig 2N: Do you intend to continue use of the Fixed OsseoRestore Appliance?
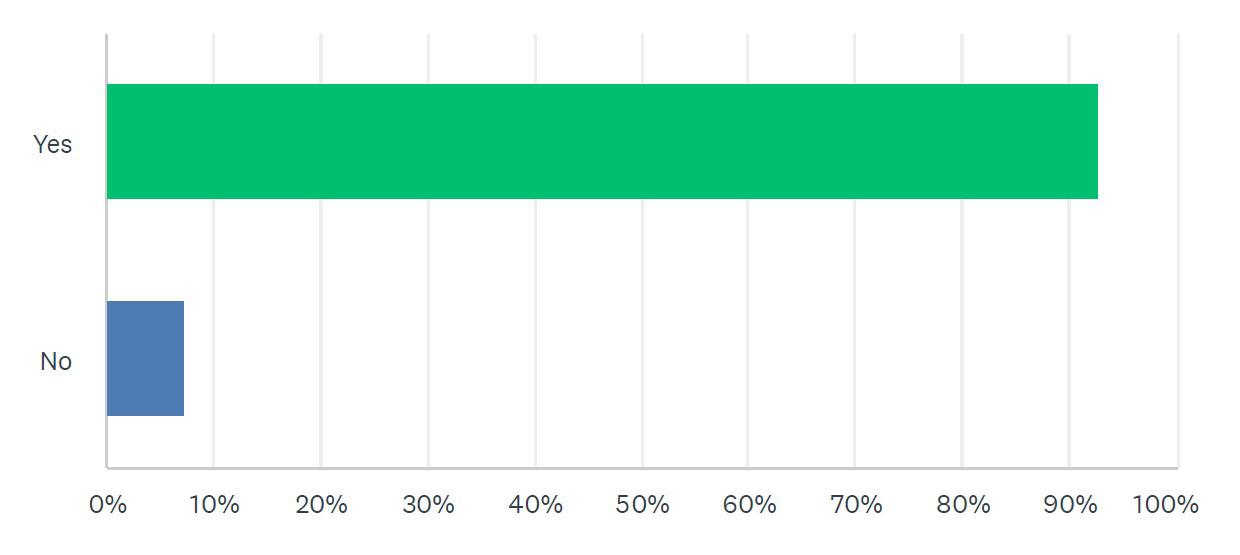
Fig 2O: Do you feel that the Fixed OsseoRestore Appliance is safe and effective when utilizing it to treat your patients?
20
The most common complications reported were mouth discomfort 19.92%, tooth sensitivity 11.21%, gingival inflammation 10.43% and tongue irritation 10.29%, all common orthodontic complications. Severe complications were rare with tooth loss and tooth breakage at less than 1% and 1.36% respectively. Overall complication rate of Osseo-RestoreTM appliances was 6.97%
The most common indications for use of the fixed OsseoRestoreTM as prescribed by practitioners in descending order are:
1. Maxillary deficiency
2. Arch development
3. Previous bicuspid extraction
4. Impacted canine teeth
5. Increased tongue space
Percentages of recommended maxillary development ranges typically indicated in their treatment plans:
2-4mm: 26%
3-5mm: 53%
5-7mm 18%
Over half of the respondents stated that in their patient populations, over 80% of the patients treated experienced subjective improvement in the following categories:
Less pain/decrease in initial symptoms
More pleasing profile
Increased quality of life
More comfortable
More tongue space
Better lip support
More pleasing smile
Most participants (92%) indicated that they would continue to use the fixed Osseo-RestoreTM as an option for their patients. All participants (100%) stated that in their experience, the fixed Osseo-RestoreTM appliance is both safe and effective.
Discussion:
Complications during and following orthodontic treatment are well documented. No known orthodontic therapies are without risk of undesired complications or side effects. Commonly noted examples are sensitive or painful teeth, gingival inflammation, gingival recession, root resorption, enamel decalcification, occlusal discrepancies, and tooth loss.9-19 One common criticism of sagittal expansion is that the teeth are in some way pushed or moved outside the bony housing of the maxilla. Critics have used CBCT imaging in order to validate this point. Although that line of thinking is very popular, it is misguided and is refuted by basic radiological principles. The size of the voxel elements available on all CBCT machines, that is the cubic volume of tissue that can be measured, is 2 to 3 times greater than the size of a thin lamina of alveolar bone (~100 micrometers). As stated previously, bone remodeling occurs in every orthodontic case. In addition, it should also be considered that remodeling bone is in various stages of mineralization depending on the status of bone at that point in the process of remodeling. When these realities are taken into consideration, it becomes clear that the CBCT simply cannot produce an accurate image demonstrating a thin lamina of bone due to the size of the bone cell and the mineral content of the remodeling bone. Providers relying on the visual CBCT as the benchmark for the status of remodeling are deceived. Figure (3) demonstrates pre-treatment CBCT, CBCT immediately following

3: Pre-treatment CBCT, CBCT immediately following the removal of the ORA, and CBCT 16 months later following removal of orthodontic appliances in an adult patient.
the removal of the ORA, and CBCT 16 months later following removal of orthodontic appliances in an adult patient. The bone is not absent, dehisced, or resorbed in the mid-treatment CT, it is simply beyond the current resolution capability of CBCT.
Complications occur in nearly every orthodontic treatment regimen. As examples consider the following papers on complications with routinely performed expansion therapies. A retrospective study on complications with Surgically Assisted Rapid Palatal Expansion (SARPE), Smeets et al, showed an overall complication rate of 52.5% with neurosensory disturbances (NSDs) making up 27.03%. A study of complications associated with MiniScrew Assisted Rapid Palatal Expansion (MARPE), Bud et al reported a greater than 2mm decrease in buccal bone at the first molar in 40.7% of the cases studied and a change in the occlusal plane in 37% of patients. Williams, et al, reported 41 of 120 SARPE cases studied developed at least one complication (34.17%). In 2022, Yoon et al, reported on complication rates of MARPE. They found gingival inflammation in 83.9%, pain during or after expansion in 45% and appliance breakage in 10% of cases studied. The Osseo-RestoreTM is no more or less likely than any other orthodontic appliance currently in use to incur complications. As is the case with all orthodontic appliances, risks and benefits of Osseo-RestoreTM appliances need to be weighed prior to initiating any orthodontic treatment. Fortunately, the more severe expressions of orthodontic side effects are infrequent and often unavoidable. Nevertheless, they do exist and are therefore should be precisely included in consent for orthodontic treatment as a minimum standard of care for every orthodontic patient 20-23 Pre-existing craniofacial and oral conditions which could possibly contribute to undesirable side effects during and after treatment should be identified, discussed with the patient and documented to insure proper informed consent. The possibility of significant treatment complications exists in some patients lacking any presentation of pre-operative risk conditions should also be considered and explained.
The importance of patient selection criteria obviously cannot be overstated regarding any recommended surgical, dental or orthodontic therapy. Individual patient characteristics combine to require each case to be managed uniquely. Clinical findings such as grossly deficient jaw structure, flared teeth or functional challenges such myofascial dysfunction, chronic oral
21 21
Fig.
breathing and lip incompetence pose significant challenges to all orthodontic therapies. Practitioners who are rigorous in data collection and efficient treatment plan development addressing all identifiable patient deficiencies will be rewarded with a greater degree of clinical success. Development of clear, reasonable and individualized treatment objectives guides patient care and improves patient expectations.
Conclusions:
Historically, innovation in dentistry has been met with controversy and resistance. This is certainly true in the orthodontic realm. Over time, innovations are utilized, debated, researched, and accepted or discarded by most practitioners. The final determinates of the destiny of an innovation are its scientific foundations combined with the crucible of clinical application. This survey primarily explores the experiences and opinions of clinical dentists applying the Osseo-RestoreTM appliance for appropriate patient care. Reported patient complaints associated with the Osseo-RestoreTM appear not to differ from those reported generally in other comparable orthodontic treatments. Patient and clinician satisfaction with appliance results were overall high. It is the opinion of the authors that this clinician survey confirms our own extensive experience that the Osseo-RestoreTM appliance is both safe and effective when used as indicated by properly trained and experienced clinicians.
References:
1. Philippe J, Guédon P. L’évolution des appareils orthodontiques de 1728 à 2007. Conférence inaugurale de la 79ème réunion scientifique de la SFODF à Versailles, le 31 mai 2007 [Evolution of orthodontic appliances from 1728 to 2007. Inaugural Conference of the 79th Scientific Meeting of the SFODF at Versailles, 31 May 2007]. Orthod Fr. 2007 Dec;78(4):295-302. French. doi: 10.1051/orthodfr:2007031. Epub 2007 Dec 18. PMID: 18082119.
2. Enlow DH, Hans MG. Essentials of facial growth. Second ed. Ann Arbor, MI: Needham Press, Inc.; 2008.
3. K alina E, Grzebyta A, Zadurska M. Bone remodeling during orthodontic movement of lower incisors: Narrative review. International Journal of Environmental Research and Public Health. 2022; 19(22):15002.
4. Janson G, Valarelli FP. Bone remodeling and orthodontic tooth movement. Journal of the World Federation of Orthodontist.2012; 1(1), e7-e11.
5. Frost HM. (1987). The biology of fracture healing. An overview for clinicians. Part I. Clinical Orthopaedics and Related Research. 1987; (225), 239-253.
6. Singh S, Singh SP, Kaur G. Orthodontic tooth movement and bone remodeling: A comprehensive review. Journal of Oral Biology and Craniofacial Research. 2020; 10(1), 28-34.
7. Frost HM. (1994). Wolff’s Law and bone’s structural adaptations to mechanical usage: An overview for clinicians. Angle Orthodontist. 1994; 64, 175-188.
8. Lanyon LE. Functional strain in bone tissue as an objective, and controlling stimulus for adaptive bone remodelling. Journal of Biomechanics. 1987; 20, 1083-1093.
9. Renkema AM, Sips ET, Bronkhorst E, Kuijpers-Jagtman AM. Gingival labial recessions in orthodontically treated and untreated individuals: A case-control study. J Clin Periodontol. 2007;34(8):633-638.
10. Ng an P, Kess B. Retention and stability in orthodontics. In: Graber LW, Vanarsdall RL Jr, Vig KWL, eds. Orthodontics: Current Principles and Techniques. 6th ed. Elsevier.
11. Rinchuse DJ, Miles PG, Sheridan JJ. Nonextraction orthodontic treatment using clear aligners: A case report. J Orthod. 2003;30(3):223-228.
12. Al-Moghrabi D, Pandis N, Fleming PS. Randomized clinical trials on orthodontic tooth movement techniques: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2019;156(2):153-164.
13. Ren Y, Jongsma MA, Mei L, et al. The effect of orthodontic treatment on periodontal pocket depth: A systematic review and meta-analysis. Clin Oral Investig. 2018;22(4):1589-1599.
14. Al-Moghrabi D, Pandis N, Fleming PS. The impact of orthodontic treatment on dental caries: A systematic review and meta-analysis. Orthod Craniofac Res. 2019;22(2):145-156.
15. Chen YJ, Chang HH, Lin HY, et al. Root resorption associated with orthodontic treatment: A review of the literature. Biomed J. 2014;37(6):350-360.
16. Li J, Li Y, Li X, et al. Comparison of enamel demineralization and bacterial colonization in patients with clear aligners and fixed appliances: A meta-analysis. BMC Oral Health. 2020;20(1):230.
17. González-García E, de Carlos F, Montiel-Company JM, Almerich-Silla JM. Orthodontic treatment and its impact on oral health-related quality of life in patients with fixed and removable appliances: A systematic review. Eur J Orthod. 2016;38(3):241-247.
18. Meeran NA. Iatrog enic possibilities of orthodontic treatment and modalities of prevention. J Orthod Sci. 2013;2(3):73-86.
19. Talic NF. Adverse effects of orthodontic treatment: A clinical perspective. Saudi Dent J. 2011;23(2):55-59.
20. Allareddy V, Elangovan S, Rampa S, Lee MK, Allareddy V. The importance of informed consent in orthodontics. Am J Orthod Dentofacial Orthop. 2017;152(4):423-430.
21. Int J Clin Pediatr Dent. 2014 May-Aug; 7(2): 105–108.Published online 2014 Aug 29. Informed consent for braces.
22. Jharwal V, Terhan M, Rathore N, Rathee P, Aggarwal D. Orthodontic consent form: lsusd.lsuhsc.edu› fdp › wp-content › uploads › 2013 › 06 › fdpconsentortho. pdf
23. Rischen RJ, Breuning H, Bronkhorst EM, Kuijpers-Jagtman AN. Records needed for orthodontic diagnosis and treatment planning: A systematic review, PLoS ONE 8(11): e74186. https://doi.org/10.1371/journal.pone.0074186
24. Maximiliaan Smeets, Oliver Da Costa Senior, Shaheen Eman, Constantinus Politis,A retrospective analysis of the complication rate after SARPE in 111 cases, and its relationship to patient age at surgery,Journal of Cranio-Maxillofacial Surgery,Volume 48, Issue 5,2020,Pages 467-471,
25. Bud ES, Bică CI, Păcurar M, Vaida P, Vlasa A, Martha K, Bud A. Observational Study Regarding Possible Side Effects of Miniscrew-Assisted Rapid Palatal Expander (MARPE) with or without the Use of Corticopuncture Therapy. Biology (Basel). 2021 Mar 3;10(3):187. doi: 10.3390/biology10030187. PMID: 33802266; PMCID: PMC8001817.
26. Williams BJ, Currimbhoy S, Silva A, O’Ryan FS. Complications following surgically assisted rapid palatal expansion: a retrospective cohort study. J Oral Maxillofac Surg. 2012 Oct;70(10):2394-402. doi: 10.1016/j.joms.2011.09.050. Epub 2012 Apr 18. PMID: 22516838.
27. Audrey Yoon, Jacqui Payne, Heeyeon Suh, Linda Phi, Angela Chan, Heesoo Oh,A retrospective analysis of the complications associated with miniscrewassisted rapid palatal expansion,AJO-DO Clinical Companion,Volume 2, Issue 5,2022,Pages 423-430,ISSN 2666-4305,
22
PRACTICE MANAGEMENT
How to Achieve Consistent Case Acceptance Success
 by Scott J Manning, MBA
by Scott J Manning, MBA
In previous articles, we’ve talked about the fastest, most dramatic and sustainable way for you to add profit to your practice. The fact is most practices aren’t anywhere close to their potential. They are playing for minimums, baselines, and daily goals that are by themselves self-limiting.
What’s worse than that is the entire system, process, protocol for patients getting healthy is one that leads to a constant and never-ending plateau you can’t break through because of the four key leverage points of dentistry leaving you stuck in your ways.
Today, my focus is to build on your bottom-line efforts from the past two weeks by going straight to the heart of the matter with diagnosis and case acceptance. You will breakthrough all plateaus, remove the limits, close the gaps, and discover a better way to achieve optimal health for your patients. As a result, you will also maximize your ability to become more profitable because you have maximized your ability to impact your patients’ lives through transformative dentistry.
This is what it’s, what you, what they, are all about.
Today, we are going to talk about creating more opportunity by building better patients by expanding on our principles from last week and ultimately expanding case acceptance.
Let’s start with how to dramatically increase the value of your new patients whether 1, 10 or 100. We’ll build your new patient business inside of your practice that delivers results through valuable dentistry and gets patients to proceed with full, comprehensive treatment plans.
The reality is, if you don’t keep your patients in the practice, in the cycle of treatment, nurtured in hygiene, then you never get the chance to cultivate the real-life changing treatment they need (which also happens to be the dentistry you love to do).
We both know that brand new patients don’t often say yes to everything or at least not right away. This is, of course, relative and depends on your process to get big case acceptance with
new patients.
That said, if you are only relying on this and never planting seeds in order to cultivate treatment in the future, then you are missing the majority of all the opportunity in your practice. Therefore, quite literally, you’re starting back over at zero on the first of every month.
If you want to turn these seeds into profits and your patients into treatment value over time then you have to keep them engaged in your practice. Not just through the new patient process but through enough points of engagement and steps to solidify a real relationship with them so they will stick around.
Every practice says they do a great job taking care of their patients BUT… what they really mean is (and maybe you say this too) that the patients that you keep like you and you take care of them inside of their mouths.
Unfortunately, this is not enough because you also have to take care of them outside their mouths. To do that you have to really embrace knowing your patients and establishing your relationship with them.
Five typical pitfalls that all can be fixed:
First, most practices are too desperate for short-term gratification of getting the easy money or billing insurance and then moving on to the next patient instead of building for the future value of the patient along the way.
Second, most practices have a culture of “busy” and they let that get in the way of actually being productive and working towards tomorrow’s treatment; not just today’s production.
Third, maybe the biggest pitfall is lacking a system that covers all parts of the patient engagement from phone through completion of treatment to follow-up and turning them into referrals. At least we need a system that holds accountable every patient opportunity so we know what happened to them and where they ended up.
Fourth, it’s quite possible your team missed the main point of where they put their focus. It could be they are in such a rush to turn emergencies or grab some same day dentistry that at the end of the day you have some money but you also lost patients that you’ll never see again (maybe without even knowing it). Money today is actually negative returns tomorrow.
Finally, fifth, every doctor once in a while gets in the habit of starting or stopping (depending on how you look at it) at diagnosing the patients’ mouths instead of getting to know the patient. The mouth doesn’t buy from you, trust you, come back to you, refer to you… the person does.
This is a provocative shift and it has to come out in more than just words. It’s about the essence of your practice, the culture inside, the focus of your team, and the conditioning and education of your patients.
You have the ability to mine your patients for gold that will never run out and it will actually build upon itself, leading to a consistent cycle of the highest value A patients coming through referrals.
Therefore, you’ll never reach a point when you get to compounding growth and building the value of your practice for the future. You’ll be making money today to pay last month’s bills instead of out ahead of your practice getting paid for the future and increasing the value of your patients every step of the way.
This will be a game changer for you.
23 23
“You play the most pivotal role in terms of getting patients to say yes. They don’t come into your practice pre-determined to say yes or no. Your job and your responsibility is to move them towards the yes, towards more interest, towards being committed to their health”

Four Pillars of Case Acceptance Success
Using my structure, you can systemize, yet keep personal, your patient flow and outcomes so you are controlling the back end of your practice and building wealth for the future.
The first pillar is creating individualized experiences. The core concept is not every patient should or needs to go through the same type of experience.
You want the phone process to organize properly the patient’s experience so that you can match it to what they need and what is going to be the most personalized experience for them.
The second pillar is all about customized treatment planning. On the surface this sounds silly because of course you customize your treatment plans. You don’t shuffle them up and let the patient pick one and just go with it. Every patient has a treatment plan unique to them.
Here’s the point though… Is it complete? Is it comprehensive? Do they know it’s unique to them? Has it been made personalized, individualized? Is it obvious that is it customized from start to finish?
The best and easiest way to do this is to be certain you are representing the photographs and/or included them with the treatment summary and presentation by the patient concierge or treatment coordinator.
It doesn’t matter what you are doing, it matters what the perception is to the patient.
The third pillar is a triad of tracking, following-up, and following-through. This is the one that every practice does halfway or just doesn’t do at all. There are three things here and you can’t do just one of them.
Track what you want to know… every statistic is not as relevant or important as the next. You want future focused values and numbers that reveal true effectiveness of your systems.
Follow-up… on everything, every patient, every dollar, period. Follow-through… on what you promise, what you say, what you do — this is big.
It could be referred out treatment that you need to know what happened with the patient. Treatment plan follow-through. Phone call follow-through. Clinical question follow-through. Even specific procedures that a patient is interested in moving forward with but not enough time was taken to discuss in the heat of the moment in the midst of the day.
I’d bet every day there are 5 to 10 balls dropped by doctors and teams that would have resulted in patients saying yes but they just weren’t followed through with.
Every single practice on earth has at the very least $5,000 a day and probably more like an hour that is NOT accepted and probably not even presented… all because we are too busy or too bashful or too distracted or too apologetic or too whatever.
Slowing down to ensure this is secured and you net another million dollars. There is only one thing that is required for this to happen — one — and that’s belief, humble belief that it exists and it’s your fault for missing it now.
When you accept that REALITY and own that RESPONSIBILITY you breakthrough and you never look back!
The final pillar is so important and that’s to always remember to set up an actual system and expectation that the experience is never over when the patient leaves.
Now is when you get to really wow them. What happens
24
post-visit, post-check, post-treatment, post-referral, posteverything is really the difference between the good and the great practices.
These are the ones that get the big cases coming back and that have consistent referral streams coming in.
Those four pillars ought to give you some serious aspects of your practice and your team to assess. Constructively look at each one so you can make improvements in what really matters.
So many doctors waste time on things that really don’t matter or will at very best have a insignificant impact. I always loved when Zig Ziglar said, “Let’s keep the main thing, the main thing.” There are so many distractions taking you away from the actions, decisions, strategies, and work that will give you leverage, growth, profit, and satisfaction.
These four are exactly that. The main things. And they should be yours.
All too often people have the wrong perception and understanding about case acceptance and patients saying “Yes.” I’m talking about You and Your Team.
Questions are asked of me and comments made that imply some concept of “black and white.” Where patients either want it or they don’t; patients either say “Yes” or “No.”
The reality is all that does is let you off the hook. Which is what most people want. Not the smart, successful, ambition people, but most. They settle for this idea that “it’s up to the patient.”
It is not (just) up to the patient.
You play the most pivotal role in terms of getting patients to say yes. They don’t come into your practice pre-determined to say yes or no. Sure, some do, but most are on a continuum of interest. Your job and your responsibility is to move them towards the yes, towards more interest, towards being committed to their health.
This whole process, done right, is just that — a process. It requires certain things to happen along the way. Then if everything is aligned properly (the emotional engagement, the desires, and the goals of the patient are being met), then you can achieve the outcome you want… because (and I mean only because) that is also what the patient wants.
You can’t and you aren’t going to sell a patient something they do not want. But, you have to acknowledge the fact that they do not walk in necessary “wanting” what they need right now. Which this is good news for you because if they already wanted it, then they most likely would have already gone somewhere else before and bought it.
Make no mistake about it, it is not your patients’ job to walk in believing or even feeling they deserve any of the life-changing benefits you can deliver. It is your job to bring them to that point.
I could go on and I will.
Case acceptance is a process that is not cookie-cutter or one-size fits all but customized for patients based on how they buy, what they value, their own personal principles, ways they make decisions and how they justify investments (among many other things).
Here is what I want you to know: every single thing you do either takes away from or adds to your patients’ journey down that continuum to case acceptance. You are either moving them forward or pushing them backwards.
Plain and simple, I’m challenging you to take more control and responsibility over every patient “Yes” that you and they deserve to hear.
From top-performing wires and elastomerics to brackets and beyond, G&H craftsmanship and products are continuously improving. Leverage our expertise from start to finish:
25 25
Premium Products Reliable Results Personalized Support You Can Have It All! Tur n to G&H Orthodontics® for a full line of reliable products you can trust.
Scan the QR code to request samples from the G&H Orthodontics portfolio. GHOrthodontics.com +1 317-346-6655 Delivery Testing Materials Inspection Development Distribution
Influence of Facial Structures on the Perception of Smile Esthetics between Laypersons and Orthodontists –A Cross-sectional Analytical Study
Dr. Fizzah Ikram, Dr. Rashna Hoshang Sukhia, and Dr. Mubassar Fida
AUTHORS
Dr. Fizzah Ikram
BDS, FCPS trainee, Orthodontics, Section of Dentistry. The Aga Khan University Hospital
Dr. Rashna Hoshang Sukhia
BDS, MSc, FCPS, FFD Orth RCS (Ireland), MOrth RCSEd (UK), Program Director Orthodontics Residency Program, Department of Surgery, Faculty of Health Sciences, The Aga Khan University Hospital
Dr. Mubassar Fida
BDS, MCPS & FCPS (Orthodontics), MCPS (Periodontology), MCPS (Community Dentistry), PGD HIMS,Consultant Orthodontist/ Professor, Associate Program Director Orthodontics Residency Program, Section of Dentistry, Department of Surgery
ABSTRACT:
Introduction: During social interactions, a person concentrates on facial components, such as the eyes. Therefore, it can be contemplated that factors other than smile parameters can influence an attractive smile. The objective of this study was to compare the role of facial structures in the perception of smile esthetics between laypersons and orthodontists.
Methods: Seventy-four raters evenly distributed across two panels of raters [orthodontic residents, orthodontists (OD), and laypersons (LP)] participated in this cross-sectional study. Frontal smile and frontal close-up smile photographs of adult male and female subjects were shown to the two panels of raters. The raters evaluated those photographs on a visual analogue scale (VAS). Mann-Whitney U test was applied to compare smile attractiveness between the raters. Linear regression was applied to determine the factors influencing smile esthetics.
Results: There was no statistically significant difference between the ratings of the two panels regarding perceived smile esthetics (p ≤ 0.05). There was a significant positive correlation between the perceived smile esthetics of all photographs. Young raters were significantly less critical while rating the photographs.
Conclusions: Female frontal smile photograph was deemed more attractive by orthodontists. Photographs of the female gender received higher rating scores from both laypersons and orthodontists. Orthodontists were most critical while rating the male photographs. The age of the raters had a significant association with the perception of smile esthetics.
Keywords: Smile esthetics, Facial components, Frontal smile photographs, Close-up smile photographs
Conflict of Interest: None
INTRODUCTION:
A pleasing face has been proven to be a stronger indicator of the overall attractiveness of an individual than the rest of the structures of body.1 An esthetic face comprises a balance between the different facial structures. 2 The face can be divided into three verticals and five horizontals to understand the harmony between the structures.3-5 Studies suggest that the components, such as the nose, lips and chin, play an essential role in enhancing the attractiveness of the face.6
The third vertical of the face mainly consists of the mouth, lips and chin, all of which contribute towards a smile.7 An esthetic smile can be described as the harmonious inter-relationship between the teeth, gingiva and lips interplaying within the dynamic display zone of the face. 8 In orthodontics, various variables and ratios are used to evaluate the attractiveness of a smile. 9 These variables include the transverse display of the smile, buccal corridors, the smile arc, incisor and gingival display, and the midlines. Any deviation from the normal range of the aforementioned components may affect the esthetics of the smile. 10 Small buccal corridors, coincident dental and facial midlines and the presence of a smile arc play an essential role in deeming the smile as attractive.11 Correction of smile variables should be made concerning facial structures and features of each individual. An esthetic smile is essential in improving the quality of life of people seeking orthodontic treatment.
Apart from smile variables, there can be components that may influence an attractive smile such as different facial patterns along with gingival display and altered facial components. 12 A balanced facial pattern is considered as most favourable for adequate gingival display, hence, producing an attractive smile.13
Various studies in the past have assessed the influence of facial structures on the esthetics of the face. 14,15 Patusco et al. 16
*This article has been peer reviewed
26
FEATURED*
assessed the attractive face as perceived by women for male individuals. They found that women considered structures, such as the eyes, nose, chin area and mouth, as a contribution towards the esthetics of face. However, the literature is insufficient in assessing the role of facial structures in the perception of an esthetic smile.
This study aimed to evaluate the influence of facial components on the perception of smile esthetics between the two panels of raters. The null hypothesis was that there will be no significant influence of facial structures on smile attractiveness as perceived by laypersons and orthodontists.
MATERIALS AND METHODS:
After obtaining approval from the institutional ethical review committee (2022-8088-23416), a cross-sectional study that included 74 (N) participants was conducted at a tertiary care hospital. The sample size was calculated by Open-epi software using the findings of Ghaleb et al.17, who reported a mean esthetic score of 25.79 ± 12.39 and 35.14 ± 16.07 at -15˚ of alteration of incisor inclination for orthodontists (OD) and laypersons (LP), respectively. Keeping α = 0.05 and the power of study as 80%, a sample size of 37 (n) was calculated. Since we had two groups, a total sample of 74 (N) was required.
We included individuals with ideal skeletal, dental, and soft tissue relationships, orthognathic facial profiles, adequate smile variables, and those who signed the informed consent form. Subjects with a previous history of orthodontic or orthopedic treatment, presence of any craniofacial dental anomaly or syndrome such as hemifacial microsomia, Down’s syndrome, cleidocranial dysplasia and history of trauma or maxillofacial surgery in the orofacial region were excluded from our study. The subjects (one male and one female) who met the ideal requirements were called to the audiovisual department. Frontal smile and frontal close-up smile photographs of both subjects were taken under adequate light with a Canon 720 SDX camera (megapixels 18.2 and maximum resolution 4896×3672). Camera was adjusted on a tripod at a distance of four feet from the subjects for frontal smile photographs and two feet for frontal close-up smile photographs. Subjects were guided to produce a posed smile while looking straight into the camera and keeping their head in a natural position as suggested by the literature.18 The photographs were stored in a JPEG format. (Figure 1 and 2)
Subjective assessment was done by two different panels of raters that were categorized into 37 orthodontists and 37 laypersons. Orthodontists who had a minimum of one year of experience in the field of orthodontics whereas laypersons included in this study belonged to different walks of life, with no knowledge of dentistry and had no previous history of orthodontic treatment. Exclusion criteria for raters included those who had any visual disturbances and raters who were not willing to rate the study. All the photographs were scored on a continuous Visual Analogue Scale (VAS) from 0 to 10, with 0 being unattractive and 10 being the most attractive.
STATISTICAL ANALYSIS:
Data were analyzed using SPSS (version 23.0) and STATA (version 12.0). Shapiro-Wilk test was used to determine the normality of data which showed a non-normal distribution. Frequencies were reported for categorical variables, such as gender. Descriptive statistics for age were reported as mean and



standard deviation. Mann-Whitney U test was used to assess the perception of smile attractiveness between laypersons and orthodontists. Spearman’s correlation was used to determine the correlation among smile esthetics of all photographs. Linear regression was used to assess the factors associated with an esthetic smile. Intra-class correlation (ICC) was applied to determine the intra-examiner reliability. A p < 0.05 was considered statistically significant.
RESULTS:
Demographics: The mean age of the sample was reported to be 28.65 ± 6.02 years. The mean ages of laypersons and orthodontists were 27.24 ± 6.75 and 30.05 ± 4.88 years, respectively. There was a gender distribution of 13 males and 24 females in both groups of raters.
Smile Scores: There was no statistically significant difference between the ratings of the two panels regarding perceived smile esthetics (p ≤ 0.05). Insignificant differences in smile scores were reported for the female frontal smile (p = 0.611), female frontal close-up smile (p = 0.481), male frontal smile (p = 0.331), and male frontal close-up smile (p = 0.085). (Table I) There was a significant positive correlation among smile esthetics of all photographs (p ≤ 0.05). (Table II) Age had a significant influence on perceived smile esthetics of male subject (p ≤ 0.05) while there was no significant association of other factors on perceived smile esthetics of female subject. (Table III, IV) Good inter-examiner reliability was demonstrated by the intra-class correlation data (0.82).
DISCUSSION:
An attractive face is one in which there is a balance between the facial structures.19 Whereas, an esthetic smile is one in which there is harmony among the lips, teeth, and gingiva.20 In our study, we accepted the null hypothesis as there was no significant influence of facial structures on smile attractiveness as perceived by laypersons and orthodontists. There was an insignificant difference between the scores of both panels of raters regarding smile esthetics while young raters had a significant impact on the
27 27
Figure 1: Frontal smile photographs of male and female subjects
Figure 2: Frontal close-up smile photographs of male and female subjects
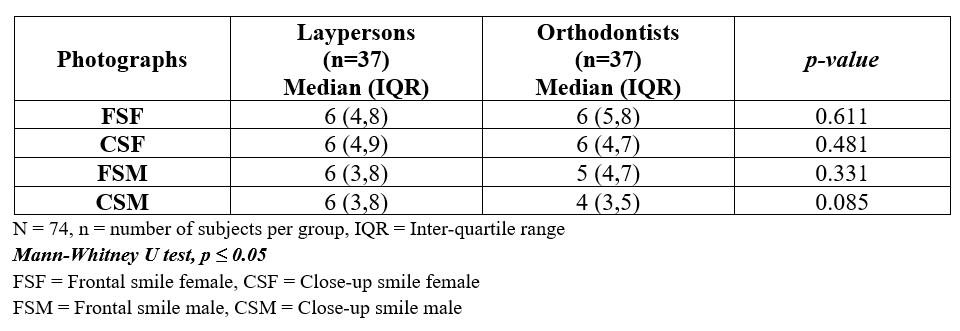



perception of smile esthetics.
Malheiros et al. 21 conducted a study to assess the influence of alterations in dentogingival structures on smile attractiveness. They found that along with the smile parameters, lips may also influence the smile esthetics. In our study, smile parameters or facial structures were not manipulated. Thus, there could have been no influence of modified structures in this study. De lima et al.13 conducted a study to assess the effect of different facial patterns with varying levels of gingival show on smile attractiveness. According to them, orthodontists were more critical and objective towards a gingival show on smile with different facial patterns. We found contrasting results in our study since both orthodontists and laypersons considered frontal smile photographs as more attractive than frontal close-up smile photographs. (Table I) This can be attributed to the contribution of facial structures and the balance between them, however, the difference was not found to be statistically significant.
Patusco et al.16 assessed the role of facial components in the attractiveness of a male smiling face by a panel of female raters only. They found that structures such as the eyes, nose, chin area, and mouth were considered as most attractive. However, our study evaluated the perception of smile esthetics and the impact of facial structures on it including both males and females as raters. Both the groups in our study found the influence of facial structures over smile attractiveness insignificant. The laypersons found both the frontal smile and frontal close-up smile of the male subject equally attractive. It showed that laypersons were less observant and cautious in the judgement of an esthetic smile since they are less aware of objective assessment of smile attractiveness, whereas the orthodontists were more particular and equally critical of both frontal and frontal close-up smile photographs of a male subject. This could be because orthodontists are trained in the correction of smile variables to achieve a perfect smile. Additionally, the presence of facial hair in the lower third of the face of the male subject may have negatively influenced the rating process.
Grimes et al. 22 assessed the role of nasal deviation on smile aesthetics and found a significant influence of deviated nasal structure on the perception of an esthetic smile. However, they did not find any difference between the ratings of
Table 1: Comparison of perception of smile attractiveness between laypersons and orthodontists
Table 2: Association of smile esthetics among photographs
Table 3: Factors influencing rating of female photographs
Table 4: FFactors influencing rating of male photographs
orthodontists, laypersons and general dentists. Singh et al.23 conducted a study to learn the role of asymmetry of the chin towards an attractive smile, they also used the frontal smile and frontal close-up smile photographs and concluded that there was no significant difference between the ratings of orthodontists, oral surgeons and laypersons which is in agreement with our study since there was no significant difference between ratings of frontal smile and frontal close-up smile photographs between the two groups. However, in our study, subjects without any deviation of facial structures were assessed, nevertheless, there was no significant difference regarding perceived smile attractiveness. This finding demonstrated that smile esthetics was not influenced by facial structures. Moreover, specific facial structures were not observed which should be assessed in future studies.
In a study conducted by Horn et al.24 to assess the role of alterations in smile dimensions in the perception of an esthetic smile, they found that young adults were most influenced while rating the most esthetic smile. These results were congruent with our study as we also found a significant association of age with the ratings of the photographs. (Table IV) There was a significant negative influence of age on the rating of the male subject photographs. With the increase in age, the raters in both groups became more critical of the ratings of male photographs. This can be attributed to the fact that Asian females have inherently more attractive features than Asian males as suggested by Wilkins et al.25 This also showed that with an increase in age, the perception of an esthetic smile becomes stringent.
Several studies show increased neuronal activity for a smiling face as compared to a non-smiling face during social interactions, hence, a smiling face is considered more esthetically pleasing.” Previously, there have been studies that assessed the esthetic smiling face and the components most pertinent to it.29-31 Godinho et al.32 conducted a study to assess the contributing factors of an attractive smiling face. They found that in male subjects, the eyes and smile had a significant role while in females, the smile and skin had major contributions towards an attractive smiling face. This was the first study that assessed the role played by facial structures in the perception of an esthetic smile. Keeping rater bias in mind, the immanent facial features may have played a role in the rating and that could have led to a critical rating by the participants. This study had a limitation as both the subjects and raters belonged to the Asian ethnicity, therefore, studies involving more ethnicities should be carried out. Furthermore, there should be studies performed to understand whether specific structures and physiognomy of the face, may have a role in the attractiveness of a smile. This will not only have an impact on orthodontic diagnosis but also will help in treatment planning to achieve a pleasing smile with other facial features.
CONCLUSIONS:
• There was no significant influence of facial components on the perception of smile attractiveness between laypersons and orthodontists.
• Facial structures may not play an important role in the judgement of an esthetic smile.
• Young people are less stringent regarding the judgement of perceived smile esthetics.
REFERENCES
:
1. Ong E, Brown RA, Richmond S. Peer assessment of dental attractiveness. Am J Orthod Dentofacial Orthop. 2006;130:163-69.
2. Ackerman JL, Proffit WR. Soft tissue limitations in orthodontics: treatment planning guidelines. Angle Orthod.1997;67:327-36.
3. Câmara CA. Esthetics in orthodontics: six horizontal smile lines. Dental Press J Orthod. 2010;15:118-31.
4. Bhuvaneswaran M. Principles of smile design. J Conserv Dent. 2010;13:225-32.
5. Mack MR. Perspective of facial esthetics in dental treatment planning. J Prosthet Dent. 1996;75:169-76.
6. Parul P, Kumar M, Goyal M, Mishra S, Shaha K, Abrar M. Impact of facial components on the attractiveness of face: A perception-based study. Am J Orthod Dentofacial Orthop. 2022;162:218-29.
7. Sarver DM. The importance of incisor positioning in the esthetic smile: the smile arc. Am J Orthod Dentofacial Orthop. 2001;120:98-111.
8. Peck S, Peck L. Selected aspects of the art and science of facial esthetics. Semin Orthod. 1995;1:105-26.
9. Soh J, Wang ZD, Zhang WB, Kau CH. Smile attractiveness evaluation of patients selected for a US-based board certification examination. Eur J Dent. 2021;15:630-8.
10. Aldhorae K, Alqadasi B, Altawili ZM, Assiry A, Shamalah A, Addin Al-Haidari S. Perception of dental students and laypersons to altered dentofacial aesthetics. J Int Soc Prev Community Dent. 2020;10:85-95.
11. Işıksal E, Hazar S, Akyalçın S. Smile esthetics: perception and comparison of treated and untreated smiles. Am J Orthod Dentofacial Orthop. 2006;129:8-16.
12. Van der Geld P, Oosterveld P, Van Heck G, Kuijpers-Jagtman AM. Smile attractiveness: self-perception and influence on personality. Angle Orthod. 2007;77:759-65.
13. De Lima AP, Conti AC, Capelozza Filho L, de Almeida Cardoso M, Almeida-Pedrin RR. Influence of facial pattern in smile attractiveness regarding gingival exposure assessed by dentists and laypersons. Am J Orthod Dentofacial Orthop. 2019;155:224-33.
14. Faure JC, Rieffe C, Maltha JC. The influence of different facial components on facial aesthetics. Eur J Orthod. 2002;24:1-7.
15. Reyneke JP, Ferretti C. Clinical assessment of the face. Semin Orthod. 2012;18:172-86.
16. Patusco V, Carvalho CK, Lenza MA, Faber J. Smile prevails over other facial components of male facial esthetics. J Am Dent Assoc. 2018;149:680-7.
17. Ghaleb N, Bouserhal J, Bassil-Nassif N. Aesthetic evaluation of profile incisor inclination. Eur J Orthod. 2011;33:228-35.
18. Bister D, Edler RJ, Tom BD, Prevost AT. Natural head postureconsiderations of reproducibility. Eur J Orthod. 2002;24:457-70.
19. Bergman RT. Cephalometric soft tissue facial analysis. Am J Orthod Dentofacial Orthop. 1999;116:373-89.
20. Ackerman MB, Ackerman JL. Smile analysis and design in the digital era. J Clin Orthod. 2002;36:221-36.
21. Malheiros AS, Brito AC, Gurgel JA, Bandeca MC, Borges AH, Hayashida TM. Dentogingival alterations and their influence on facial and smile attractiveness. J Contemp Dent Pract. 2018;19:1322-8.
22. Grimes K, Fleming PS, Sharma PK. The influence of nasal deviation on the perception of maxillary dental centerline and smile aesthetics. J Orthod. 2022:146;53-125.
23. Singh H, Maurya RK, Kapoor P, Sharma P, Srivastava D. Subjective
29 29



You Deliver the Smiles
Simply great wires at great prices. That’s what Highland Metals has promised, and delivered, for more than 30 years.
Find affordable products manufactured in the USA with the clinical results you demand.
Explore top-performing options including:
and objective evaluation of frontal smile esthetics in patients with facial asymmetry – A comparative cross‐sectional study. Orthod Craniofac Res. 2017;20:8-20.
24. Hor n S, Matuszewska N, Gkantidis N, Verna C, Kanavakis G. Smile dimensions affect self-perceived smile attractiveness. Sci Rep. 2021;11:18.
25. Wilkins CL, Chan JF, Kaiser CR. Racial stereotypes and interracial attraction: Phenotypic prototypicality and perceived attractiveness of Asians. Cult Divers Ethn Minor. 2011;17:427-31.
26. O’Doher ty J, Winston J, Critchley H, Perrett D, Burt DM, Dolan RJ. Beauty in a smile: The role of medial orbitofrontal cortex in facial attractiveness. Neuropsychologia. 2003;41:147–55.
27. Beltran D, Calvo MG. Brain signatures of perceiving a smile: Time course and source localization. Hum Brain Mapp. 2015;36:4287-303.
28. Chen J, Ou Q, Chi Z, Fu H. Smile detection in the wild with deep convolutional neural networks. Mach Vis Appl. 2017;28:173-83.
29. Chang CA, Fields Jr HW, Beck FM, Springer NC, Firestone AR, Rosenstiel S. Smile esthetics from patients’ perspectives for faces of varying attractiveness. Am J Orthod Dentofacial Orthop. 2011;140:17180.
30. Otta E, Abrosio FF, Hoshino RL. Reading a smiling face: Messages conveyed by various forms of smiling. Percept Mot Skills. 1996;82:111121..

31. Reis HT, Wilson IM, Monestere C, Bernstein S, Clark K, Seidl E, et al. What is smiling is beautiful and good. Eur J Soc Psychol. 1990;20:25967.
32. Godinho J, Gonçalves RP, Jardim L. Contribution of facial components to the attractiveness of the smiling face in male and female patients: a cross-sectional correlation study. Am J Orthod Dentofacial Orthop. 2020;157:98-104.




Scan the QR code to order wires from
30
Nickel Titanium Stainless Steel Beta Titanium Molybdenum
.
Enjoy Great Prices and Quality You Can Trust
Highland Metals.

TTIPS FROM THE EXPERIENCED
The Utility Arch, Part 1
By Dr. Adrian J. Palencar, MUDr, MAGD, IBO, FADI, FPFA, FICD
he definition of the Utility Arch from Google: “The utility arch is a two-couple intrusion arch wire used for control of anterior deep overbite. It is commonly made with rectangular wire, attached to the teeth only at the molars and the incisors and is activated for incisor intrusion by a molar tip back bend.”
The definition is succinct; however, it does not describe all functions this appliance can deliver. It can be utilized for intrusion, extrusion, protrusion, retrusion, space maintenance and for molar control. There are two moments of the couple in each sextant, one on the lateral incisor and one on the molar.
The utility arch was first published by Dr. Charles Burstone (1928-2015), the father of Biomechanics and further developed by Dr. Robert M. Ricketts (1920-2003), the pioneer of Bio-progressive orthodontic treatment.
The utility arch is constructed from a .016 x .016 SS wire, and it is undersized in a .022 x 028 slot – it means that it can rotate it in the buccal tube. It is author’s opinion that it is easier to make the bends on the flat surface of the arch wire than on the round one, thus the square wire.
Not too many clinicians are willing to spend time and effort to bend a Utility arch. Therefore, it is available in a prefabricated form a .016 x .016 and a .018, Stainless steel, also in Nitanium super elastic or Bio-kinetix+ Thermally activated.
A simplified prefabricated version of the Utility arch was designed and developed by Dr, Ravindra Nanda – Connecticut Intrusion Arch (CIA). It is available in a .019 x .022 and a .017 x .025 (long and short) – Nitanium super elastic or CNA Beta 3.
Please compare the evolution of the Utility arch. If the material and the thickness of the wire would be the same, the only difference is the length of the wire. The longer is the wire, the gentler is the force, and the function is the same.
References
1. Cerum Ortho Organizers catalogue
2. Rondeau Seminars, Level I, Session 3
3. Palencar A. J. Case Finishing and Mechanics manual
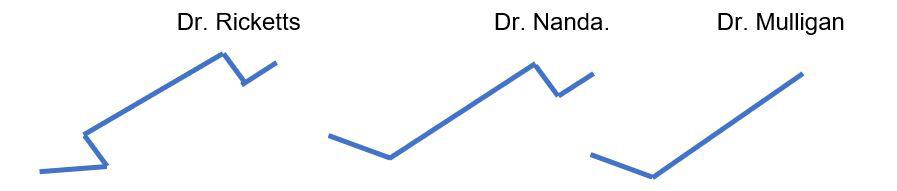
As the readers may notice, the simplest way to fabricate the intrusive (or any other) arch is Mulligan mechanics. The applied force can be titrated by the amount of Tip back (less acute angle than the Utility arch). The force should be measured by the Gram gage. The following pliers may help you bending the Utility arch.



“The utility arch is a two-couple intrusion arch wire used for control of anterior deep overbite. It is commonly made with rectangular wire, attached to the teeth only at the molars and the incisors and is activated for incisor intrusion by a molar tip back bend.”
–Webster’s Dictionary
31 31
Gram Gage
Nance Pliers
Tweed Loop Forming Pliers
Orthodontic Treatment of a Geminated Maxillary Lateral Incisor: A Case Report
by Rami Aboujaoude, Lina Aboujaoude, Falah Aboujaoude, Carla Jabre, Jad Nasr
AUTHORS
Rami Aboujaoude
Department of Orthodontics, School of Dental Medicine, Saint Joseph University, Beirut, Lebanon.
Lina Aboujaoude
Department of Orthodontics, School of Dental Medicine, Saint Joseph University, Beirut, Lebanon.
Falah Aboujaoude
Université Pierre et Marie Curie
Stomatologie et chirurgie maxillofaciale: Hopital Pitie Salpetriere Service Stomatologie et Chirurgie Maxillo-Faciale
Carla Jabre
Department of Endodontics, School of Dental Medicine, Saint Joseph University, Beirut, Lebanon.
Jad Nasr
Department of Pediatric Dentistry, School of Dental Medicine, Lebanese University, Beirut, Lebanon.
ABSTRACT:
Introduction: Tooth gemination is not a very common phenomenon. It occurs most frequently in the primary dentition, with an estimated prevalence of 0.6%, whereas its prevalence in the permanent dentition is even rarer, and is estimated to be around 0.1%. We present a case of a geminated maxillary left lateral incisor that was treated with a multi-disciplinary approach.
Keywords: Gemination; Double Tooth; Dental Anomaly; Multi-Disciplinary.
INTRODUCTION:
AIt is not uncommon for tooth buds to fuse or geminate during the morphodifferentiation stage of development. Various terms have been used to describe such phenomenons, such as “twinning”, “schizodontia”, “concrescence”, etc. 1 Differentiating gemination and fusion can be difficult. Both of them refer to a larger than normal sized tooth, but in the first, there is a normal number of teeth in the arch, whereas in the second, a tooth is missing.2 Due to this ambiguity, some authors prefer using the term “double tooth.”
Double teeth are more frequently observed in the primary dentition, with a prevalence of 0.6%. The prevalence of such teeth in the permanent dentition is even rarer, and is estimated to be between 0.1% and 0.23%.2,3
According to Hamasha and Al-Khateeb, the maxillary central incisors were the most commonly affected teeth (3.6%), followed by the mandibular third molars.4 For Altug et al., the maxillary lateral incisors were the most concered.3 Barbério et al. found that the upper lateral incisors, premolars and molars were the most commonly geminated/fused teeth.5 Both sexes are
equally affected, according to Brook and Winter.6
The etiology of gemination remains unclear. It is clear that genetics play an important role, but environmental factors, trauma, systemic diseases and hypervitaminosis have all also been linked to this phenomenon.1,2
If left untreated, double teeth may have a negative impact on dental arch lengths and occlusions, which might complicate an eventual orthodontic treatment. A multidisciplinary approach should be followed in order to restore function and esthetics.1 In this paper, we report a case of a geminated maxillary left lateral incisor that was treated with a team approach.
MATERIALS AND METHODS:
AA 12-year-old female patient presented to our clinic with a chief complaint of anterior upper crowding. Her medical history was uneventful. Clinical and dental cast examinations showed an oversized maxillary left lateral incisor (15mm in width) that was rotated “mesial-out”, combined with a slight class II relationship on the left side, a symmetrical face and a straight profile. Overbite was 50%, whilst overjet was 3mm (Fig. 1 and 2).
Radiographic evaluation of tooth 22 showed two distinct roots. In addition to the panoramic and the lateral cephalogram, a CBCT exam was done in order to study the canal anatomy; it revealed a small connection between the two pulp chambers at the cervical level (Fig. 3).
It was decided that the tooth would benefit from hemisection, in order to transform it into a regular sized lateral incisor. Brackets were bonded and alignment was initiated.
Then, a root canal treatment of the double tooth was done: after anesthesia
*This article has been peer reviewed
32 FEATURED*

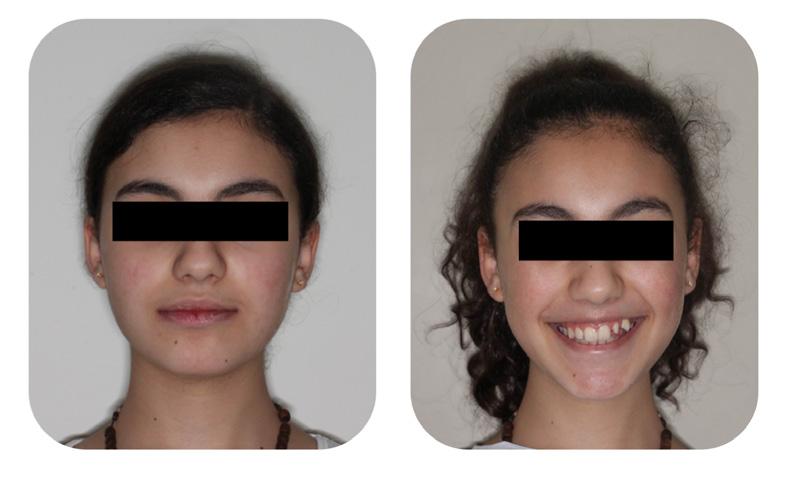


(Mepivacaine 3%, 1/100 000), and rubber dam placement, two distinct access cavities were made from the palatal surface. Working length was established with the use of an apex locator (Root ZX, Mini, J. Morita Corp., Tokyo, Japan) and verified with a periapical radiograph. Shaping was done using Reciproc R25. Copious amounts of sodium hypochloride 6%, with ultrasonic activation (EDDY, VDW GmbH, Munich, Germany), were used to disinfect the root canals and remove the debris. The canals were filled using gutta-percha and zinc oxide sealer (SealiteTM Regular, Acteon, Pierre Roland, France) with the continuous wave technique.
The endodontic treatment was then followed by root separation using a dental burr, then an extraction of the distal root (Fig. 4). Orthodontic treatment was then continued (Fig. 5).
A satisfactory result was obtained. Total treatment time was 18 months. The patient was advised to have a crown restoration on the tooth, but was pleased with the end result and decided to postpone it for the time being (Fig. 6 and 7).

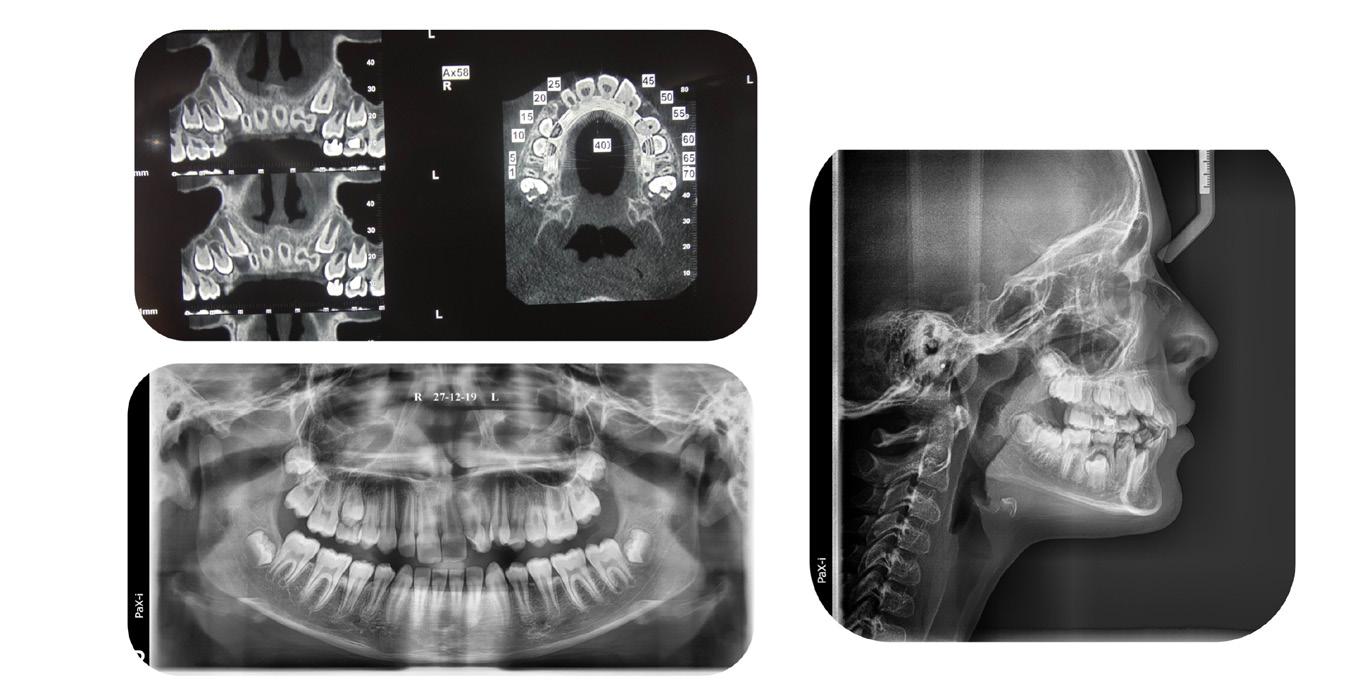





33 33
Figure 3: Initial radiographic exam.
Figure 2: Initial intra-oral pictures.
Figure 1: Initial extra-oral pictures.
Figure 4: Panoramic x-ray during initial orthodontic treatment.
Figure 6: Orthodontic treatment progress pictures.
Figure 5: Orthodontic treatment, root canal treatment and hemisection
Figure 7: End result intra-oral pictures.
DISCUSSION:
Gemination/fusion is a rare phenomenon that occurs in less than 1% of the population. Establishing a differential diagnosis between the two can be challenging. The etiologies are unclear, but include trauma, vitamin imbalances, genetics, environmental factors and some neurological disorders (1–4).
The treatment of double teeth can be quite challenging and requires a multi-disciplinary approach. Hemisection was indicated in this case because two separated roots were observed, with connecting pulp chambers (7).
An alternative option would have been extraction of the giant tooth followed by an implant, but this option was rejected due to the patient’s young age.
CONCLUSION:
Despite being a rare phenomenon, the treatment of a geminated tooth can be quite challenging for the practitioner; a multi-disciplinary team approach should therefore be the gold standard of treatment, ensuring a conservative individualized end result.
REFERENCES:
1. Proffit WR, Fields Jr HW, Sarver DM. Contemporary orthodontics. Elsevier Health Sciences; 2006.
2. Le Gall M, Philip C, Aboudharam G. Orthodontic treatment of bilateral geminated maxillary permanent incisors. Am J Orthod Dentofac Orthop Off Publ Am Assoc Orthod Its Const Soc Am Board Orthod. 2011 May;139(5):698–703.
3. Altug-Atac AT, Erdem D. Prevalence and distribution of dental anomalies in orthodontic patients. Am J Orthod Dentofac Orthop Off Publ Am Assoc Orthod Its Const Soc Am Board Orthod. 2007 Apr;131(4):510–4.
4. Hamasha AA-H, Al-Khateeb T. Prevalence of fused and geminated teeth in Jordanian adults. Quintessence Int Berl Ger 1985. 2004 Aug;35(7):556–9.
5. Barbério G, Costa S, Rios D, Oliveira T, Machado M. Rare Case of Bilateral Gemination in Deciduous Teeth. Int J Morphol. 2013 Mar;31:575.
6. Brook AH, Winter GB. Double teeth. A retrospective study of “geminated” and “fused” teeth in children. Br Dent J. 1970 Aug 4;129(3):123–30.
7. Cetinbas T, Halil S, Akcam MO, Sari S, Cetiner S. Hemisection of a fused tooth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Oct;104(4):e120-124.




34
Figure 8: End result extra-oral pictures.
Figure 9: One year post-treatment panoramic x-ray.
Author Guidelines
MANUSCRIPT SUBMISSION
Manuscripts are to be submitted electronically at www. editorialmanager.com/iaortho. If the manuscript is written in a language other than English, the author(s) must submit an English translation. The author may also submit a copy in his or her native language that will published in the online version only with a mention in the printed issue that the article is available online in his or her own language. The manuscript must be original and submitted exclusively to IJO.
The Journal invites authors to submit:
•Clinical reports
•Technique articles
•Review articles
•Case reports
MANUSCRIPT FORMAT
Abstract. Must include a short abstract no more than 50 words that describe the significance of the article.
Keywords. Must include keywords to help categorize the article.
Length. Manuscript should be no longer than 15 doublespaced pages, excluding figures and illustrations.
Tooth Numbering. The numbering of teeth should be international numbering. (US numbering can be added and put in parentheses.)
Non-English Manuscripts. Authors are encouraged to submit the manuscript in languages other than English for posting on the IAO website. A mention will be added to the English version published in the International Journal of Orthodontics, directing readers online for other translations.
Illustrations. Images must be available electronically as separate files. High quality digital images must be presented in one of the following formats: .tiff, .eps,.jpg, or .pdf with resolution of a minimum 300 dpi. Images must not be embedded in software programs such as Word or Power Point. The names on the digital files for photo/illustration files should match the manuscript reference. For example, if manuscript copy references Figure 1, electronic file should be titled Figure 1.jpg. No more than 16 photographs, figures, & illustrations are recommended; if greater than 16, IJO has the right to select and limit the number if necessary. Figures must be clearly referenced as to their placement in the manuscript. Brief captions for the figures, identified by number, must be provided. All images must be titled. Radiographs must be of superior quality.
References. References must be included and authors are responsible for the accuracy of references. Manuscripts without them will be returned. Cite references in the text as endnotes and number them consecutively. Citations must be referenced in the following style:
Periodical:
1.Sim JM, Jefferson Y, Dillingham SE, & Keller DC. Diagnosing an orthodontic patient using three different analyses. IJO 1990; 1(4):101-106.
Book:
2.Fonder AC. The Dental Physician. 2nd ed. Rock Falls, IL; Medical Dental Arts; 1985:25-82.
World Wide Web site:
3.Health Care Financing Administration. 1996 statistics at a glance. Available at: http://www.hcfa.gov/stats/stathili.htm”. Accessed Dec. 2, 1996.
Products: Any products mentioned in the manuscript should be footnoted disclosing the company name and address.*
*XYZ Orthodontic Co., 123 Main St., Los Angeles, CA 90000.
REVIEW AND EDITING PROCESS
Editor. Articles will initially be reviewed by the editor. If author fails to adhere to the guidelines set forth, manuscript will be returned to the author for revision and correction.
Peer review. Articles in IJO are subject to an anonymous peer review process. Reviews may take up to eight weeks to complete.
Decision. Once the reviewing consultants have completed their critiques, the editor examines their comments and makes a decision to accept, accept with minor revisions, revise and resubmit, or reject.
Editing. IJO reserves the right to edit manuscript for conciseness, clarity, and stylistic consistency. The author has final approval before publication.
Questons? Contact Managing Editor, Allison Hester at allisonhijo@gmail.com, 501-517-1620.
AUTHOR RESPONSIBILITIES
Copyright transfer. IAO holds the copyright for all editorial content published in the journal. All accepted manuscripts become the permanent property of the IAO, and may not be published elsewhere in full or in part, in print or electronically, without written permission from the IAO.
Reprint permission. The author is responsible for obtaining written permission from the publisher, or the person or agency holding the copyright for any material that is reproduced from a published source.
Consent forms. Any patient clearly identified in the article must sign a form indicating his or her consent to be depicted in the article. It is the author’s responsibility to confirm consent.
Author’s photo and bio. The author(s) must submit a headshot (preferably professional) and current biographical sketch. If author holds a teaching position, the title, department, and school should be included. Any position or relationship with a dental manufacturer must be identified. The sketch should include rank or title and station of authors who are in federal service, and should be limited to 60 words or less.
Conflict of interest. The author will identify any conflicts of interest upon submission of any articles.
REPRINTS
The International Journal of Orthodontics provides the corresponding author a final electronic copy of the Journal in which the article appears as well as an electronic copy (.pdf) of the pages where the article appears. Requests for individual reprints of the article should be directed to Chris McKay, IAO, 414-272-2757 or at chris@iaortho.org.
Patients have a right to privacy that should not be infringed without informed consent. Identifying information, including patients’ names, initials, or hospital numbers, should not be published in written descriptions, photographs, and pedigrees unless the information is essential for scientific purposes and the patient (or parent/guardian) gives written informed consent for publication. Informed consent for this purpose requires that a patient who is identifiable be shown the manuscript to be published. Authors should identify Individuals who provide writing assistance and disclose the funding source for this assistance. Identifying details should be omitted if they are not essential. Complete anonymity is difficult to achieve, however, and informed consent should be obtained if there is any doubt. For example, masking the eye region in photographs of patients is inadequate protection of anonymity. If identifying characteristics are altered to protect anonymity, such as in genetic pedigrees, authors should provide assurance that alterations do not distort scientific meaning and editors should so note. (Source: International Committee of Medical Journal Editors (“Uniform Requirements for Manuscripts Submitted to Biomedical Journals”), February 2006).
35 35






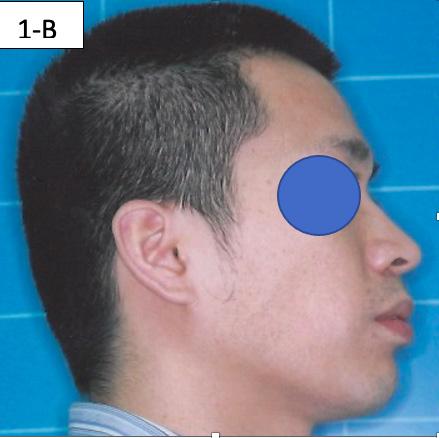
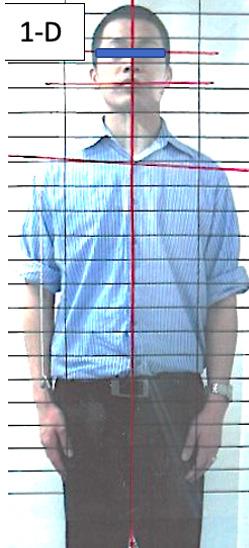














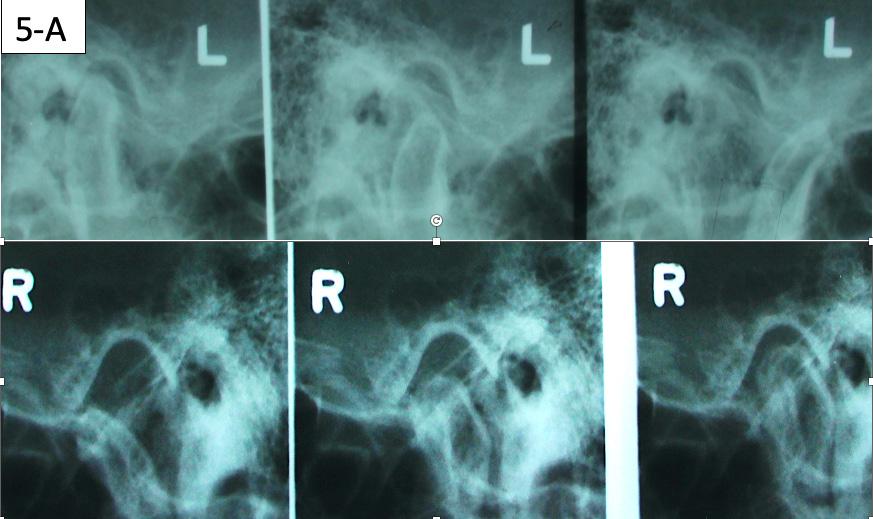
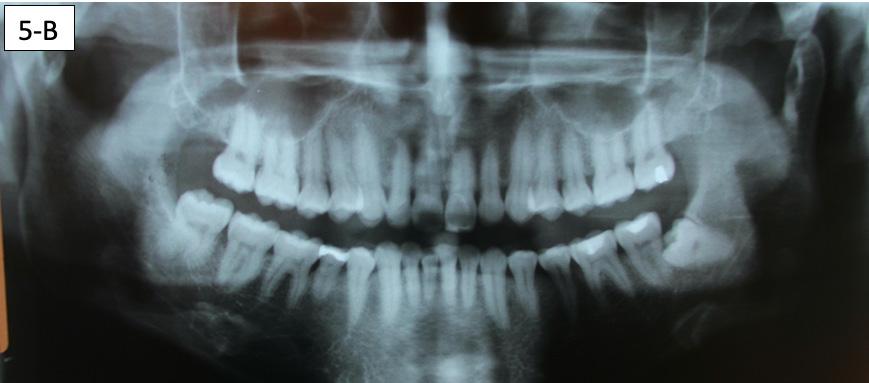

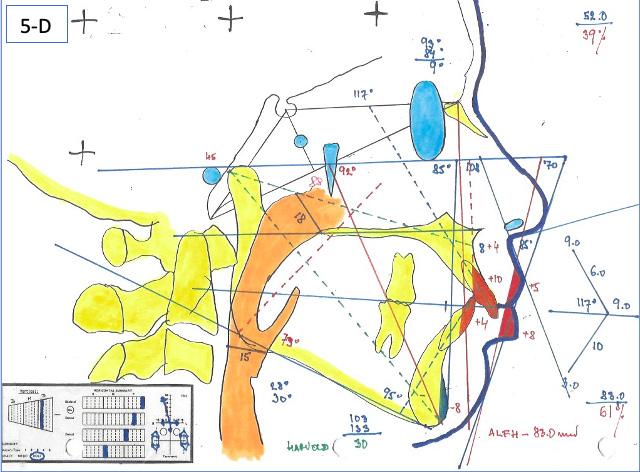







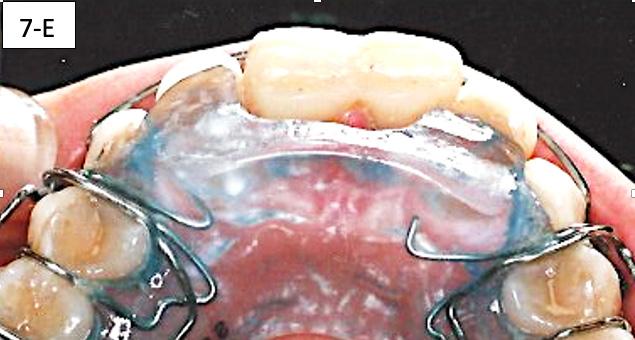








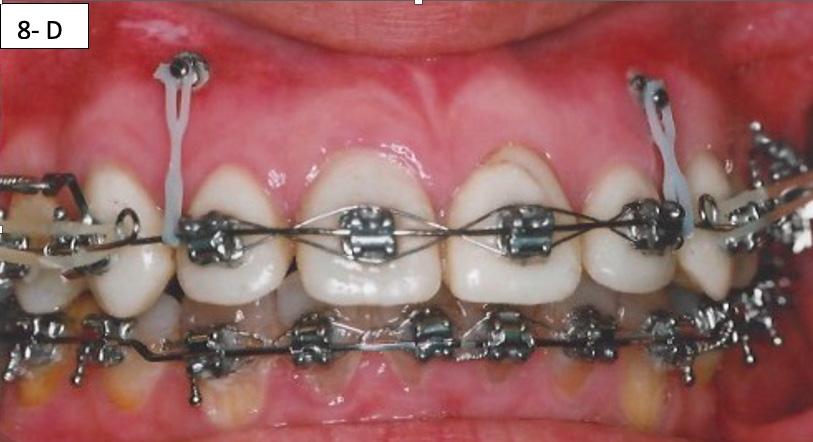







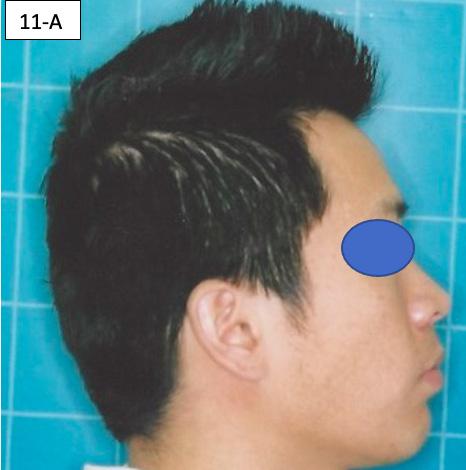
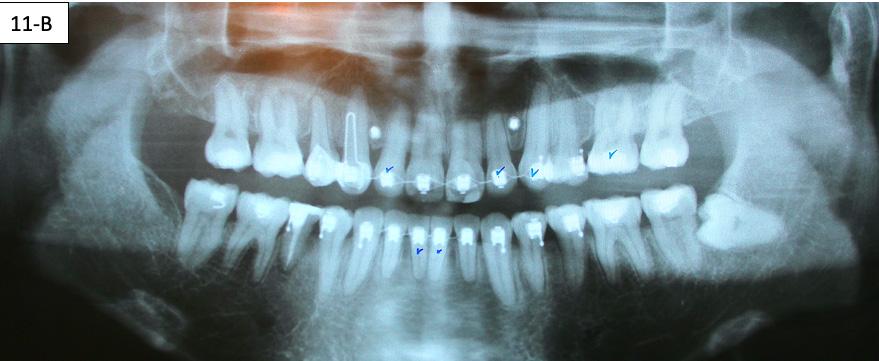
















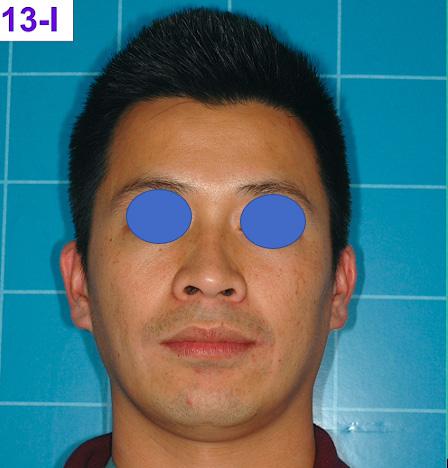

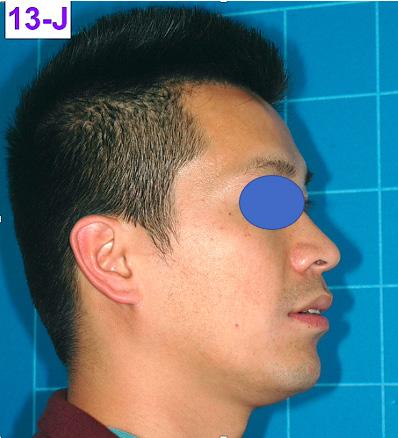








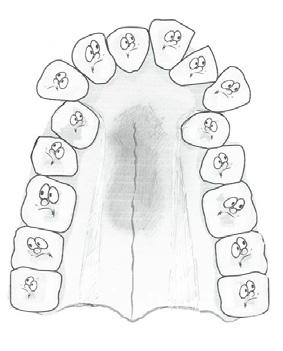


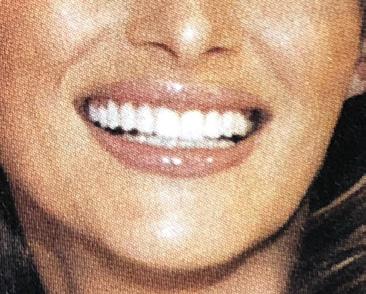













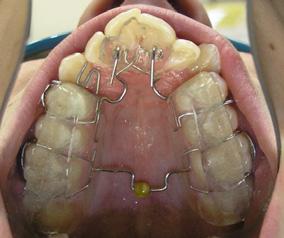



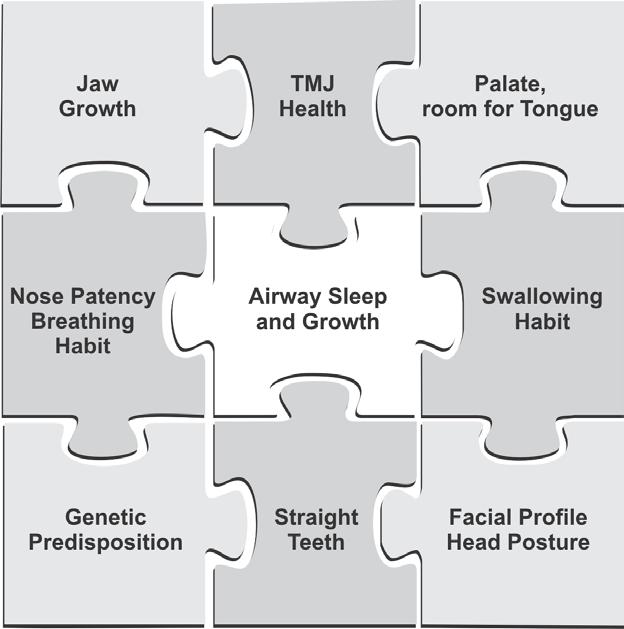




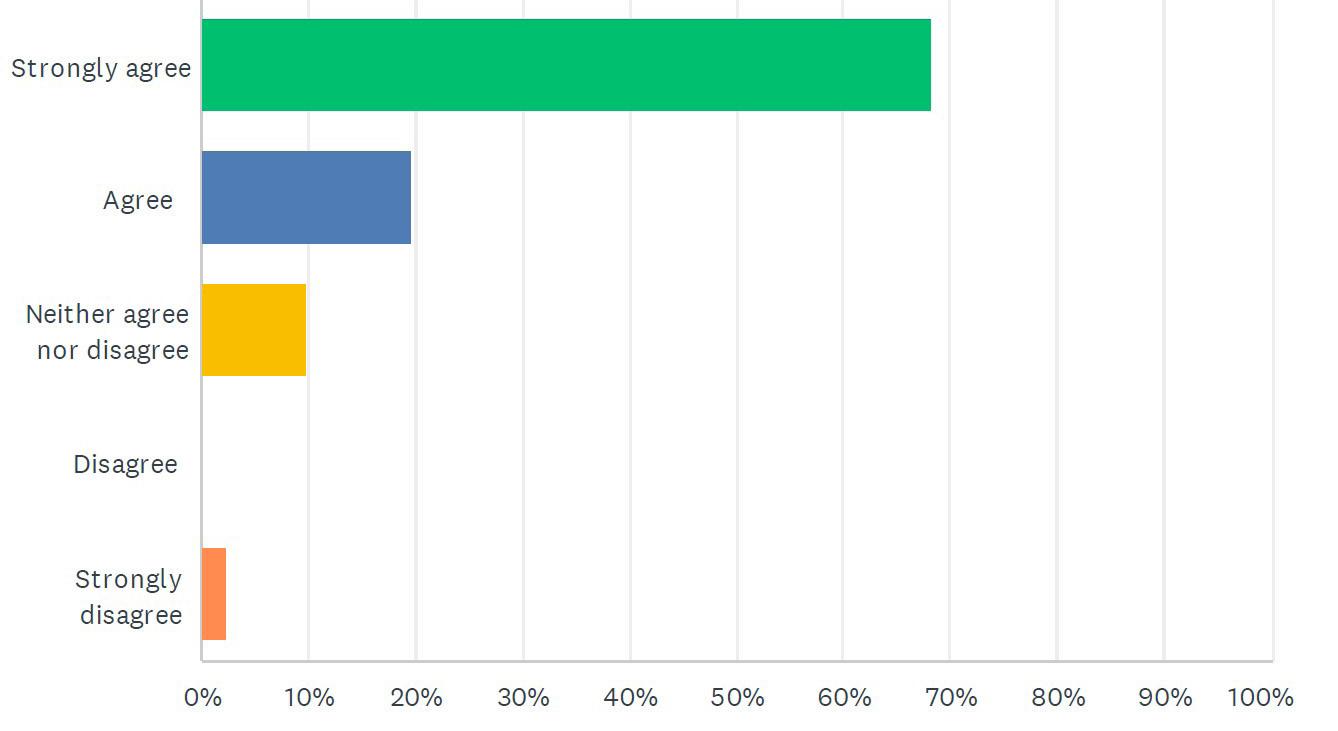


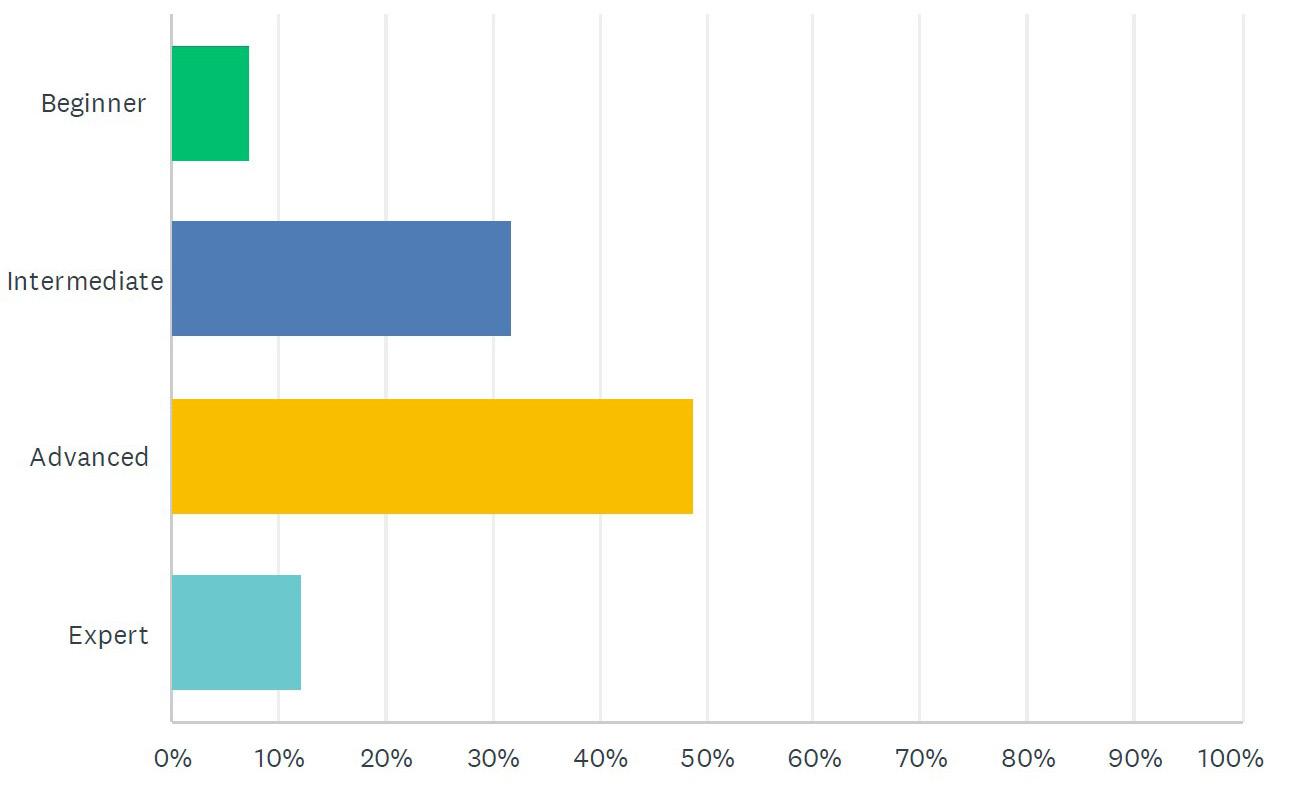
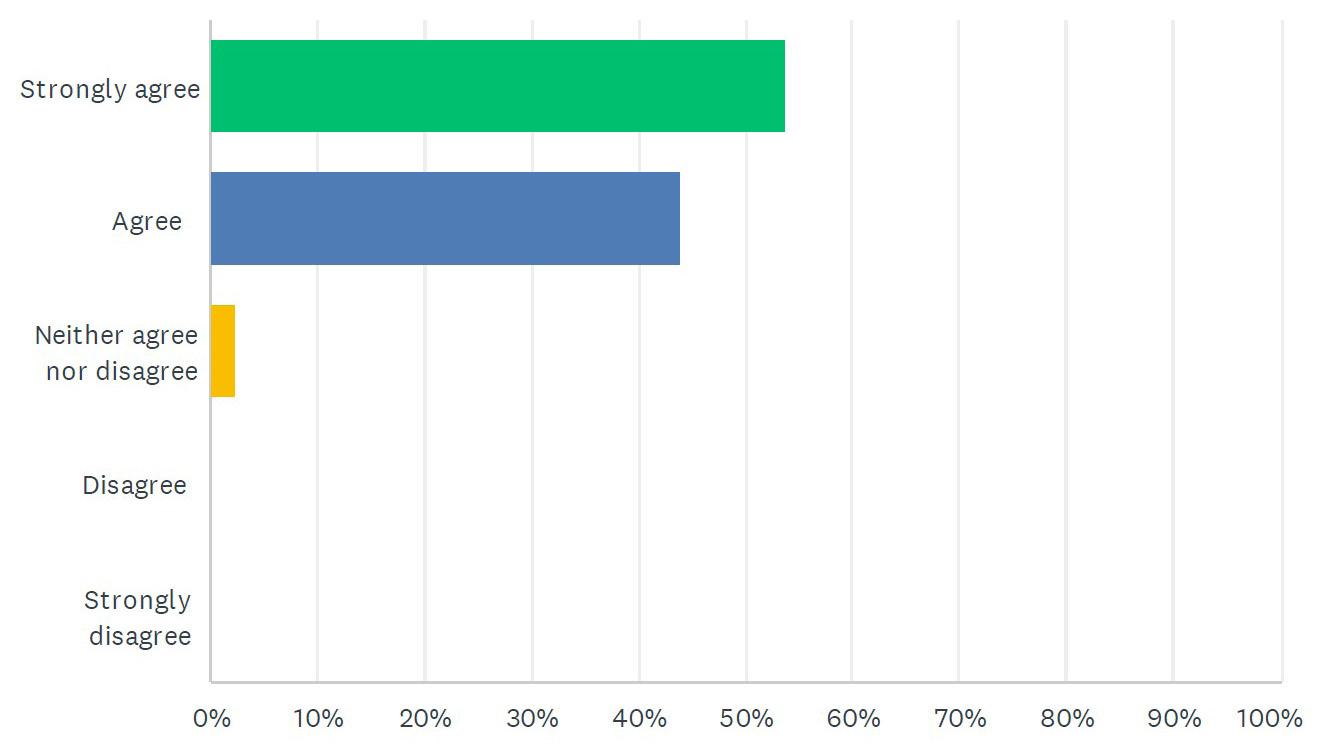


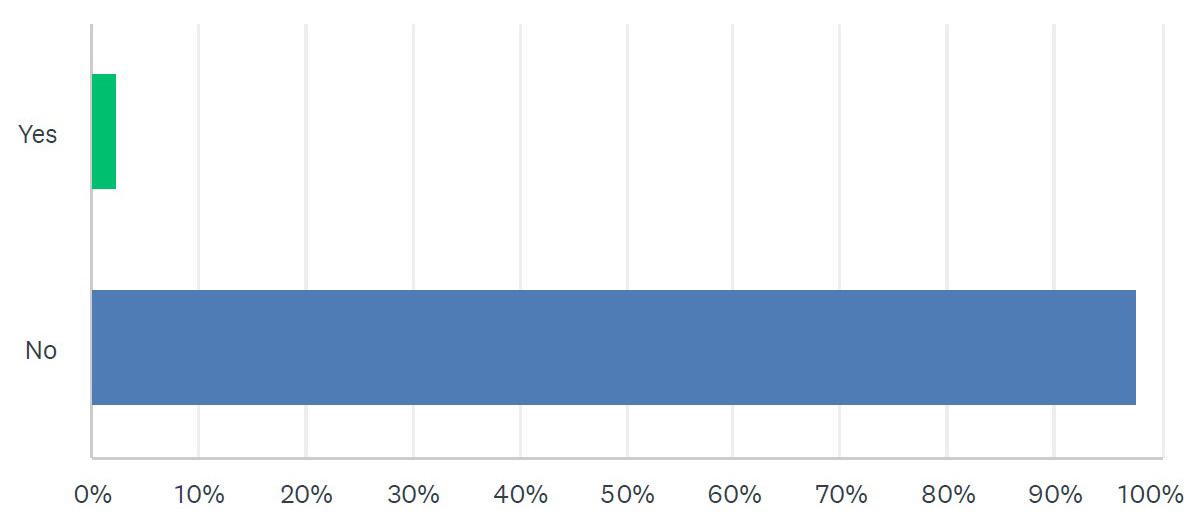
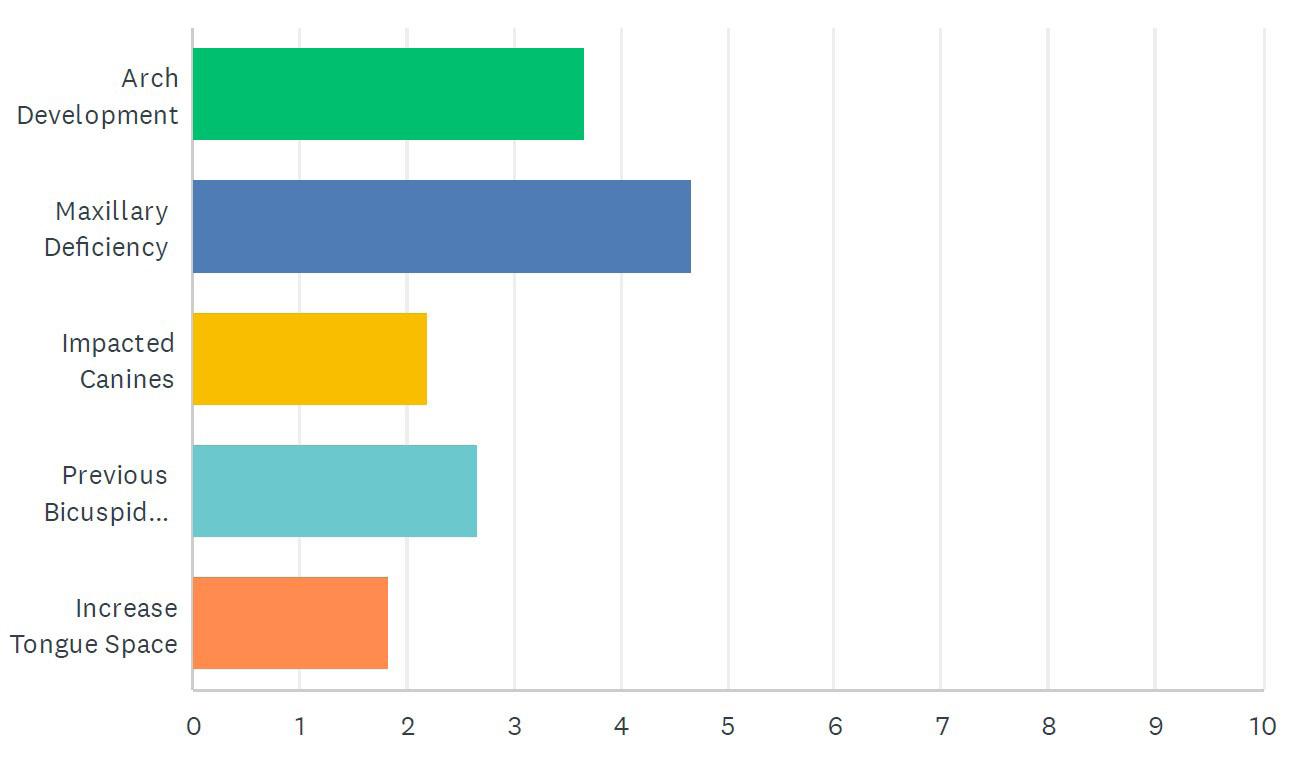
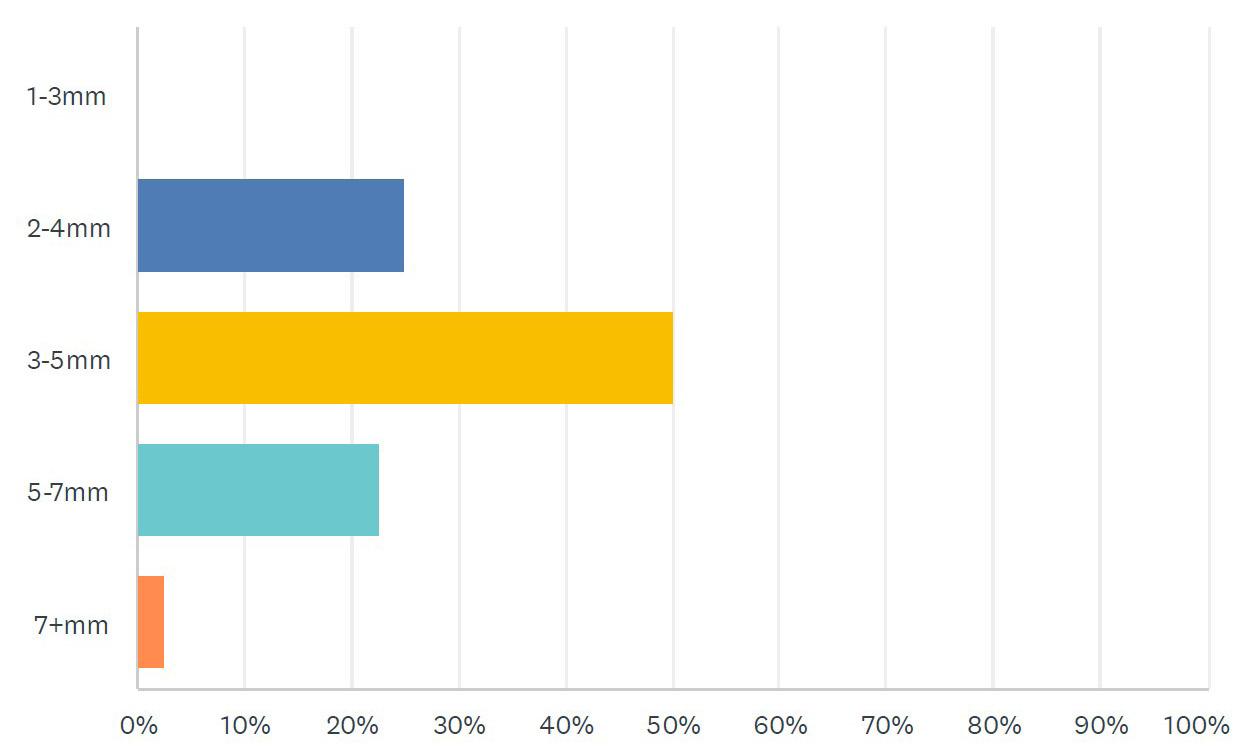


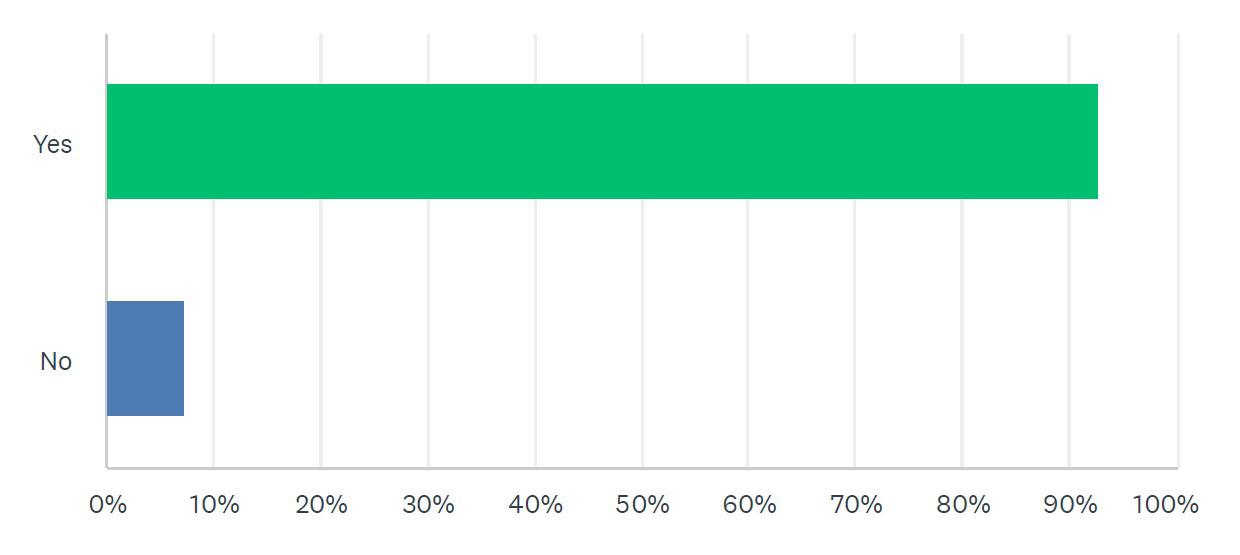
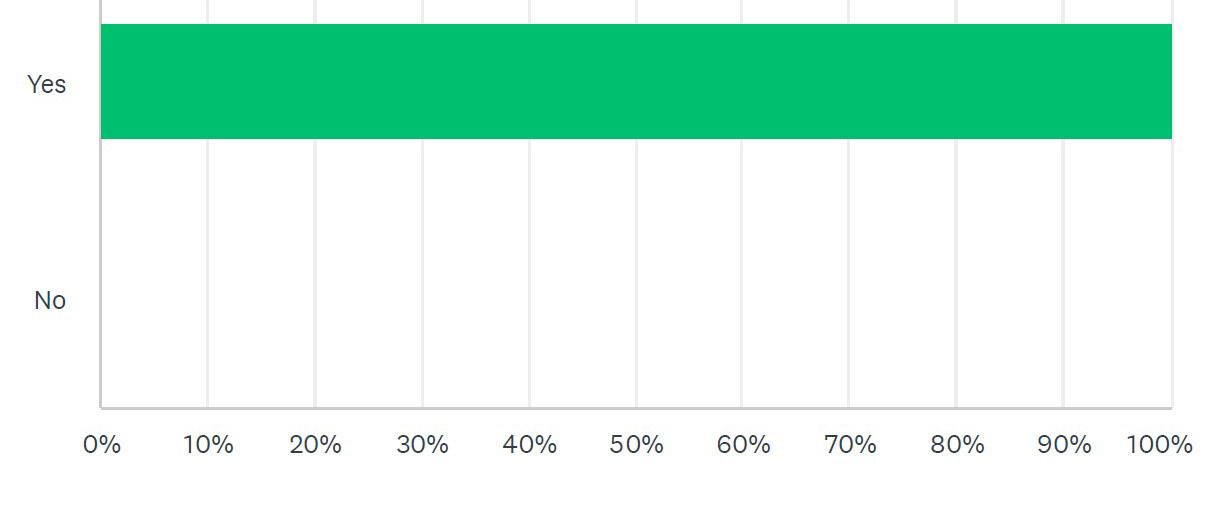

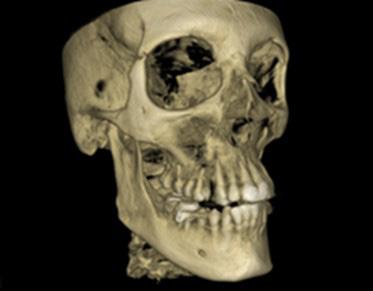
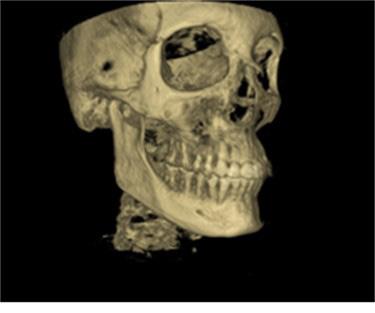
 by Scott J Manning, MBA
by Scott J Manning, MBA