





• The purpose of this guide is to equip our quality committee members with foundational knowledge about Inova’s Our Patients Key Performance Indicators (KPIs)
• This guide will summarize the concept of clinical excellence, our KPI selection and goal setting principles, and each of Our Patients KPIs.
• This guide will not review actual performance.
• Clinical Excellence at Inova: 4-5
• Key Performance Indicator Selection and Goal-Setting Overview: 6-9
• Key Performance Indicator Overview: 11-35

• At Inova, we view patient experience, safety, and quality in a coalesced manner that we refer to as clinical excellence.
• We believe the same organizational mindset, culture, and imperatives positively impact outcomes across all domains of clinical excellence.
• There is no clinical excellence without equity. Therefore, for each of our measures, our analytics tools enable us to understand outcomes by demographic factors and identify disparities.
• We address disparities and inequities into existing clinical excellence improvement efforts.

Quality

Clinical Excellence represents the totality of quality, safety, and patient experience outcomes.
The foundations of quality, safety, and patient experience overlap. Therefore, to achieve the highest levels of clinical excellence, we must fortify these foundations.
Patient Experience Safety

• Key performance indicators (KPIs) are intended to drive focus and prioritization of organizational efforts in improvement.
• We have KPI’s in four categories:
- Our Patients
- Our Team
- Financial Sustainability

- Growth
• We select KPIs in the “Our Patients” category based on our internal drive to excellence and external factors such as Centers for Medicare and Medicaid (CMS) programs, Leapfrog Safety Grade, and Vizient Quality and Accountability Scores.



• “Our Patients” KPIs drive organizational focus and are a reasonable proxy for overall clinical excellence
• We select KPIs in the “Our Patients” category based on several factors:
- Our internal drive to excellence guided by our care mandate and care imperatives
- External factors such as:

o Centers for Medicare and Medicaid (CMS) programs
o Leapfrog Safety Grade
o External Benchmarking Composite Quality Scores (Vizient)
o Value-based care measures
• We select the most critical KPIs to be our Key Results.

• Once we select KPIs, we set goals that reflect our internal drive to excellence and use external benchmarking when available and appropriate
• For measures where external benchmarking, we aim for top decile performance over a three-to-five-year time frame
• For measures where external benchmarking is not available, we aim for improvement “compared to ourselves”
• Our general principle is to set goals that are lofty but attainable
• We stratify our goals by hospital, ambulatory location, and service line


• Inpatient Mortality
• Catheter-Associated Urinary Tract Infections & Central Line-Associated Blood Stream Infections
• Surgical Site Infections
• Likelihood to Recommend Composite
• Hand Hygiene
• Length of Stay

• Serious Safety Event Rate
• Advance Care Planning
• Know Our Patients
• What Matters Most
• Depression Screening and Follow Up
• High Blood Pressure Screening and Follow Up

Why does this measure matter?
Inpatient Mortality is a key indicator of care quality. Preventable hospital deaths highlight opportunities for health systems to enhance inpatient care and avoid system failures. Thus, inhospital mortality is a crucial quality indicator.
How do we define this measure?
Inpatient mortality is risk-adjusted, using the O/E ratio, calculated by dividing observed (O) by expected (E) inpatient mortality. Observed mortality is the actual death rate in hospitalized patients, while expected mortality is influenced by coded diagnoses. When O/E is equal to 1.0, observed mortality was exactly as expected (greater than 1.0, observed mortality is higher than expected; lower than 1.0, observed mortality is lower than expected). Patients in observation, ambulatory, hospice and rehab status are excluded from this measure.
What is the benchmark source?

The Vizient Clinical Database provides risk-adjusted data and comparison based on hospital type.
How do we improve performance?
1 – A systemwide approach to early identification of and intervention on clinical worsening (deterioration) and/or severe infection (sepsis) that is often subtle and may go unrecognized.
2 – Aligning care to patient goals and wishes by implementing hospice care before or during hospitalization.
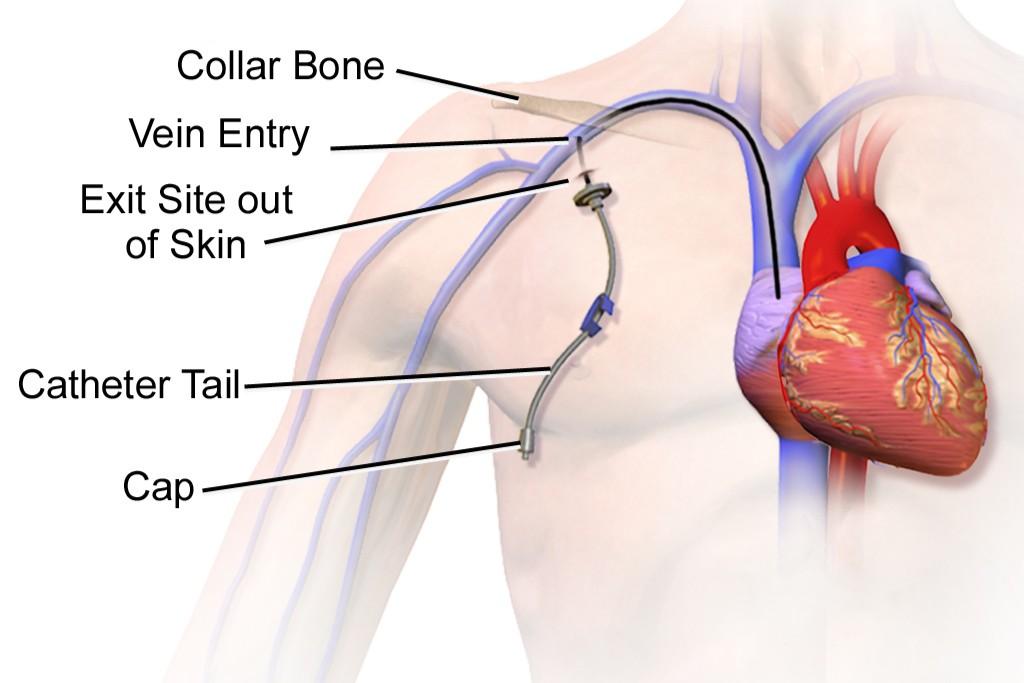
Depiction of a central line
Depiction of a urinary catheter


Why does this measure matter?
Catheter-Associated Urinary Tract Infections (CAUTIs) and Central Line-Associated Blood Stream Infections (CLABSIs) are preventable healthcare complications linked to significant suffering, mortality, and expenses. CAUTI arises when bacteria move along urinary catheters, causing urinary infections. CLABSI emerges when bacteria enter the bloodstream via large intravenous catheters called central lines. Despite previous progress, national rates of CAUTI and CLABSI have risen since the onset of the COVID pandemic.
How do we define this measure?
Our measure is the absolute numbers of these infections collected through our internal surveillance. We utilize the Center for Disease Control (CDC) National Health Safety Network (NHSN) surveillance definitions for defining hospital acquired CAUTI and central line associated blood stream infections CLABSI.
What is the benchmark source?

CDC National Healthcare Safety Network
How do we improve performance?
1 – Hand Hygiene at all applicable moments of care
2 – Inserting a urinary catheter or central line only when necessary, with the safest and cleanest technique
3 – Safely maintain urinary catheters or central lines
4 – Assess necessity daily and remove urinary catheters or central lines when they are no longer necessary


Why does this measure matter?
Surgical site infections (SSI) are complications after surgery, most of which are preventable. These infections can occur at the site of a surgical incision or within the surgical area, and they can lead to complications, prolonged hospital stays, increased healthcare costs and even mortality.
How do we define this measure?
Our measure is the absolute numbers of these infections collected through our internal surveillance after abdominal hysterectomy (removal of the uterus), colon surgery, knee surgery, hip surgery, and coronary artery bypass grafting. We utilize the CDC’s National Health Safety Network (NHSN) surveillance definitions for surgical site infections.
What is the benchmark source?

CDC National Healthcare Safety Network
How do we improve performance?
1 - Administering the correct antibiotic at the correct dose at the correct time before surgery
2 - Blood sugar control around the time of surgery
3 - Temperature control during surgery.
4 - Skin cleaning and preparation before hospitalization and immediately before surgery.


Why does this measure matter?
Patient experience is crucial for clinical excellence, representing patients' perceptions and feelings about their healthcare journey, encompassing communication, access, and overall treatment satisfaction. Prioritizing patient experience ensures patients feel safe, respected, and supported, enhancing care quality, adherence, and outcomes. A patient’s likelihood to recommend, assessed through post-encounter surveys, gauges inclination to suggest a provider or facility to others. High likelihood to recommend ratings reflect healthcare quality and signify trust.
What is the benchmark source?

Press Ganey, an external vendor, provides benchmark data with their network of over 41,000 healthcare facilities.
How do we define this measure?
Our Likelihood to Recommend composite is a composite measure from hospital surveys, emergency department surveys, and medical practice surveys. These surveys account for 15 percent, 15 percent, and 70 percent of the composite, respectively. We review the percentage of patients surveyed who answered with the highest possible choice of their likelihood to recommend.
How do we improve performance?
1 – Decrease friction before and during an encounter
2 - Improve communication between team members and patients
3 – Improve teamwork within the team and between team members and patients
4 – Implement care models in which patients experience teamwork and communication
World Health Organization: 5 Moments for Hand Hygiene


Why does this measure matter?
Hand hygiene is the single most effective action to stop the spread of infection. Most germs that cause serious infections in healthcare are spread by the hands of healthcare workers. Per Centers for Disease Control and Prevention, studies show that on average, healthcare providers clean their hands less than half of the time that they should. These gaps contribute to the spread of healthcare associated infections that affect 1 in 31 hospital patients.
How do we define this measure?
Our Key Performance Indicator is the percentage of total observed hand hygiene encounters performed correctly as measured and tracked by trained observers. Appropriate hand hygiene is achieved through handwashing (cleaning hands with soap and water), antiseptic hand wash, antiseptic hand rub (alcohol – based hand sanitizer including foam or gel), or surgical hand antisepsis. The World Health Organization defines five moments for hand hygiene, our trained observers observe two of these moments - upon entry and exit from a patient room.
What is the benchmark source?

We internally measure and track hand hygiene.
How do we improve performance?
Our gaps are primarily non-technical. We have active initiatives to increase coaching when we observe lapses in hand hygiene and positive reinforcement when we observe hand hygiene performed well. Until hand hygiene becomes an organizational habit, it will require continuous attention at all levels. We collaborate with our support services teams to ensure there is ample supply and location of alcohol-based hand rub dispensers and to address empty soap dispensers.



Why does this measure matter?
Hospital Length of Stay is an indicator of efficiency and effectiveness of care and is a surrogate measure for overall patient flow throughout a hospital. Optimal patient flow and length of stay requires patients to receive the right care in the right place at the right time. Therefore, optimization of length of stay requires evidence-based decision making, teamwork, and coordination of care. Poor hospital wide patient flow puts patients at risk for harm, decreases access to inpatient care, increases costs, and increases the burden on healthcare team members.
What is the benchmark source?
The Vizient Clinical Database provides risk-adjusted data and comparison based on hospital type.
How do we define this measure?
Length of Stay (LOS) is risk-adjusted, using the O/E ratio, calculated by dividing average observed (O) by average expected (E) LOS. The observed LOS is the number of calendar days a patient stayed in the hospital after admission. The expected LOS is the number of expected days a patient stays in the hospital and is influenced by coded diagnoses and conditions. When O/E is equal to 1.0, observed mortality was exactly as expected (greater than 1.0, observed mortality is higher than expected; lower than 1.0, observed mortality is lower than expected). Patients in observation, ambulatory, emergency department, hospice and rehab status are excluded from this measure.
How do we improve performance?
1 - Service lines and sites collaborate on disease-specific care pathways focused on evidence-based resource use and discharge criteria.
2 - Teamwork and communication: multidisciplinary and trio rounds.
3 - Optimize case management. Of note: we measure and intervene on other measures of patient flow such as hours in observation status and total patient boarding hours (boarding refers to patients who are admitted but stay in another setting).
Why does this measure matter?
Serious safety events refer to gaps in care that cause severe harm or death. Eliminating harm is a moral obligation. Addressing errors and patient safety improves care quality, affordability, and equity. Tracking our serious safety event rate aligns with our care imperatives that highlight zero harm, psychological safety and collaboration in teams.
How do we define this measure?
Any event that meets criteria for a National Quality Forum
serious reportable event or The Joint Commission Sentinel Event is included in the numerator of the rate. The denominator of the rate is adjusted patient days. Events are classified as a serious safety event through a system level classification process.
Serious safety events at Inova have included severe hospital acquired pressure injuries (otherwise known as pressure ulcers or bedsores), falls with severe harm, wrong side or site surgery, unintentional retention of foreign objects after a procedure,
maternal harm events, oxygen depletion, workforce safety events, and suicide.
What is the benchmark source?

Serious safety events are detected through voluntary reporting by our teams. We internally measure and track serious safety events.
How do we improve performance?
Culture is essential to ensuring high levels of safety. We have several initiatives aimed at enhancing safety at Inova, some are targeted towards preventing specific complications and some are broader efforts to improve our culture. In the coming months, we will be implementing and socializing a set of behaviors aimed towards improving safety and associated evidence-based tools that reduce the chances of errors.
• The definition of harm has expanded from physical harm to include emotional and financial harm.

• Errors in diagnosis (delayed diagnosis or incorrect diagnosis) are increasingly recognized as an important safety risk across settings
• Ambulatory safety must be considered in addition to hospital safety.
• Safety refers to both patients and team members.
• Safety is a quality and not a quantity – it means so much more than the absence of harm –safety is an attribute that must be ever present to keep our patients and team members safe.
• Most of the time, things go well for our patients and team members. Therefore, our biggest learning opportunity is to learn from everyday work rather than solely from adverse events.

Why does this measure matter?
This measure aligns with our care imperative to “know each patient and honor what matters most to them with empathy and compassion.” Advance care planning involves discussing and preparing for future decisions about your medical care if you become seriously ill or unable to communicate your wishes. Advance care planning impacts other clinical excellence outcomes and is a quality measure in and of itself. We emphasize completion of a specific note type in the electronic medical record, so all advance care planning conversations are easily accessible to care teams across the continuum of care.
What is the benchmark source?

How do we define this measure?
Percentage of adult (18 years or older) inpatients with an Advanced Care Plan note type in Epic. Excludes outpatients and inpatients who are not adults.
How do we improve performance?
We internally measure and track advance care planning. Our improvement initiatives are primarily centered around education of providers and making the note type seamless to use and locate.
Of note: An advance care plan note is one component of a broader set of advance care planning tools such as identification of a healthcare agent and discussion of resuscitation status.
Social Drivers of Health Wheel in Electronic Medical Record


Why does this measure matter?
Collection and documenting social drivers of health (SDoH) and race, ethnicity, and language (REaL) allows for a more holistic understanding of health and is essential to achieve our mission to provide world-class healthcare – every time, every touch – to each person in every community we have the privilege to serve. Awareness of SDoH and REaL helps us understand disparities, promotes equity in healthcare, helps us tailor care to individual needs, and provides direction for future program development.
How do we define this measure?

Percentage of all available Social Drivers of Health (SDoH) risk assessments and Race, Ethnicity and Language (REaL) demographic data collected for adult (18+ years) patients in a hospital inpatient or ambulatory face-to-face encounter. The eleven available social drivers of health are alcohol use, tobacco use, housing needs, depression, intimate partner violence, social connections, stress, physical activity, transformation needs, food insecurity, and financial needs.
We internally measure and track the Know Our Patients measure.
After a comprehensive educational campaign, service lines in collaboration with our system Health Equity Steering Committee, have taken the lead in prioritizing collection of REaL and SDoH. Incorporation into the MyChart check-in process has increased collection of REaL and SDoH. Inova has implemented an online referral program, “UniteUs”, to meet the needs of individual patients based on identified SDoH. Of note: The Centers for Medicare and Medicaid Services (CMS) will institute a requirement for hospitals to collect SDoH starting in 2024. Work is underway to meet this requirement
What is the benchmark source? How do we improve performance?

Why does this measure matter?
In addition to asking “what’s the matter”, asking patients what matters most to them aligns with our care imperative to know each patient and honor what matters most to them with empathy and compassion. placing patients' priorities at the forefront leads to more effective and patient-centered healthcare experiences. When healthcare providers understand what matters to patients, they can tailor their care to better meet these expectations. This approach enhances patient experience, health outcomes, trust in the healthcare system, and the patient-provider relationship.
How do we define this measure?
Percentage of all patients who visited an ambulatory setting in person or were inpatient in the hospital with What Matters Most ever documented in Epic. This documentation could have taken place in an ambulatory setting or in the hospital setting during a past visit.
What is the benchmark source?

We internally measure and track the What Matters Most measure.
How do we improve performance?
In addition to efforts in socializing the importance of this measure, we have created tools in our electronic medical record to make documentation of what matters most seamless. Sharing stories of how honoring what matters most has impacted patients and care teams has served as positive reinforcement of the initiative.


Why does this measure matter?
Depression is an extremely common, underdiagnosed, and treatable condition. Depression is associated with profound suffering and disability, poor status of other chronic medical conditions, poor clinical outcomes, and is a leading cause of suicide. Five out of ten people who commit suicide saw their Primary Care Physician in the preceding four weeks. Therefore, detecting depression through validated screening tools and following up appropriately is expected to improve our community's health. Depression screening normalizes mental health and is the first step in the development of a comprehensive depression care model at Inova.
What is the benchmark source?
We internally measure and track depression screening and follow up.
How do we define this measure?
The percentage of patients aged 12 years and older screened for depression on the date of the encounter at any Inova outpatient site for up to 14 days prior to the date of the encounter using a standardized depression screening tool AND if positive, a followup plan is documented. The follow up options are:
-Treatment and symptom management by their primary care physician
-Connection to an Inova Behavioral Health Therapist
-Community health resources for patient guided therapy and outreach

-Transfer to the nearest Emergency Room
How do we improve performance?
Our primary opportunities to improve depression screening are to integrate screening seamless into the workflow of a clinic visit and to share stories of lives changed due to depression screening in all areas of Inova Health System. Our surgery ambulatory clinics were among the first groups to implement depression screening and provided us with valuable learnings on how to implement depression screening outside of primary care and behavioral health.


High blood pressure is a major risk factor for heart disease and stroke, both of which are leading causes of death in the United States. Commonly referred to as the “Silent Killer,” nearly onethird of all American adults have high blood pressure and more than half of them do not have it under control. Due to the impact on morbidity, mortality, and quality of life, Inova has designated High Blood Pressure Screening and follow-up as a key performance indicator.
Percentage of patient visits at any Inova ambulatory site, for patients aged 18 years and older seen during the measurement period who were screened for high blood pressure AND a recommended follow-up plan is documented in the patient’s chart, as indicated. Follow up plans vary based on severity of blood pressure elevations and include follow up with a primary care physician, a specialist, or in rare circumstances, refer to the emergency department.

We internally measure and track high blood pressure screening and follow up.
Inova launched an initiative to develop universal screening and follow-up for High Blood Pressure in Ambulatory Services. The focus on the project was to create a seamless process for reliably measuring blood pressure and providing a consistent referral process.