Why You Should

Of course you should always thank a nurse, but May is a special month. That's when it's celebrated Nurses Week (May 6-12) and Nurses Month.


FREE GVHEALTHNEWS.COM MAY 2024 • ISSUE 225 P. 2 O!-O!-O!-OZEMPIC! Medicare spent $57 million to cover the drug in 2017. In 2022? It spend $4.6 billion. See 'Healthcare in a Minute' on page 7. Cardiologist Jeffrey D. Alexis has helped grow UR Medicine transplant program, which recently celebrated a record number of heart transplants — 40. He discusses why there have been more transplants locally. P. 4 UR: 40 HEART TRANSPLANTS
Thank a Nurse This Month See releated stories starting on page 12

Cuddly, friendly, fun: Your pet brings so much to your life, but experts warn that, in rare cases, they can also bring illness.
The health benefits of pet ownership are many, noted physician Stacey Rose, an associate professor of infectious diseases and internal medicine at Baylor College of Medicine in Houston.
For example, the presence of a dog or cat in the home can desensitize a child's developing immune system to certain allergens. Pets are also well-known stress busters, helping to lower risks for high blood pressure and depression, Rose noted in a Baylor news release.
But there are hidden health dangers, especially for pregnant women or anyone with an immune system weakened by illness, organ transplant or infection with HIV.
For those people, there's the risk of toxoplasmosis, caused by the toxoplasma germ that can be found in cat feces, Rose said.
Hookworm — this time found in dog feces — is another infectious agent to be wary of, so always wash your hands after picking up after your dog.
Then there's the danger of getting bitten or scratched by a dog, cat or other pet.
Cats, especially, can transmit a



dangerous organism called Pasteurella multocida through a bite, and dog bites can pass along another hazardous germ called Capnocytophaga canimorsus.
Infections with these germs can be dangerous and even fatal for people with compromised immune systems, Rose said.
Cats and dogs who roam outside can also come into contact with rodents, possums, raccoons and other wild critters. Rose said the main health issue there is the insects that live on these animals, such as fleas and ticks — and the illnesses they carry.
For example, Murine typhus is a flea-borne illness that can bring on rash, fever and other symptoms in humans.
“You don't have to have direct
exposure with a rodent to be at risk; if your pets are gallivanting with those other animals and the fleas are transferred from the rodent to your pet, then your pet can help transmit that disease," Rose explained.
Bartonella henselae illness is another flea-borne bacterium that's so associated with felines that it's been nicknamed "cat scratch" disease.
It's most associated with scratches from kittens, Rose said. If the kitten is carrying fleas, the fleas' infected feces can enter your body via a scratch.
According to the Baylor news release, "in kids or adults with a normal immune system, one might develop a big lymph node that will go away on its own," after a scratch, but "with a compromised immune system, that same bug can lead to far-reaching diseases including bloodstream infections or infections of the heart or heart valves, or the eye, liver or spleen."
Then there are illnesses caught from scaly cold-blooded pets such as turtles, lizards or snakes.
The U.S. Centers for Disease Control and Prevention continues to issue alerts about people (often small children) catching salmonella from these animals after handling them.
Elderly people, or those with compromised immune systems, should also avoid handling pet reptiles, or wash their hands thoroughly with soap and water if they do.
“There are plenty of reasons why we can and should have pets, but you just need [to] be aware of your own immune system and the potential risks," Rose said. We have to be conscientious pet owners for our own health and the health of our families and neighbors."



Page 2 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024
Can I Get Sick From My Pet? Live Allergy Free! Excellence in Allergy and Asthma Care - Since 1985 AAIR Brighton 3136 Winton Rd. S., Ste. 203 Rochester, NY 14623 (585) 442-0150 AAIR Canandaigua 3170 West Street, Suite 222 Canandaigua, NY 14424 (585) 396-7280 AAIR Perinton 6800 Pittsford Palmyra Rd. Building 400, Suite 400, Fairport, NY 14450 (585) 425-1650 Asthma, Wheezing, Cough, Recurrent Infections Nasal, Sinus and Eye Allergies Urticaria, Angioedema, Eczema and Contact Dermatitis Food Allergies Mast Cell Activation Allergy Shots Desensitization Insect Allergy Infusion Center Complete Allergy Care While Minimizing Medication Requirements! www.aair.info Board Certified Allergists Providing Specialized Care for Adults and Children


Adult Day Health Care is a medical model day program that serves adults with physical, psychosocial and medical needs. Services include medication assistance, cultural arts and lunch or dinner. Transportation available within Monroe County. Ask about our new afternoon program from 2:00 – 7:00 p.m. Call (585) 784-6570 or visit JSLAdultDayHealthCare.org for more information.
May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 3
A service of Jewish Senior Life
days are filled with friendships and activities, combined with the care I need.” ADULT DAY GUEST
“My

U.S. TB Cases Reach Highest Level in a Decade
Tuberculosis cases are on the rise in the United States, with the number of reported infections in 2023 the highest seen in a decade.
Forty states, including New York, logged an increase in tuberculosis (TB) cases, and rates were up among all age groups, the study from the U.S. Centers for Disease Control and Prevention found. More than 9,600 cases were reported, a 16% increase from 2022 and the highest since 2013.
"Although TB incidence in the United States is among the lowest in the world and most U.S. residents are at minimal risk, TB continues to cause substantial global morbidity and mortality," the researchers wrote in the March 28 issue of the CDC publication Morbidity and Mortality Weekly Report.
"This post-pandemic increase in U.S. cases highlights the importance of continuing to engage communities with higher TB rates and their medical providers in TB elimination efforts and strengthening the capacity in public health programs to carry out critical disease control and prevention strategies," they added.
Experts point to a surge in TB cases internationally — the World Health Organization has said TB was behind only COVID-19 in infectious fatal diseases worldwide in 2022, the Associated Press reported. There have also been big spikes in migration and post-pandemic international travel, which likely fueled the spread of TB.
But other factors are at play, including other illnesses that weaken the immune system and allow latent TB infections to surface.
The 2023 count “was a little more than was expected,” physician Philip LoBue, director of the CDC's Division of Tuberculosis Elimination, told the AP.
Tuberculosis is caused by bacteria that attack the lungs, and is spread through the air when an infected person coughs or sneezes. If not treated properly, it can be fatal, according to the CDC.

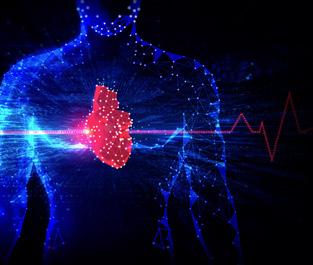
Meet Your Doctor
By Chris Motola
Jeffrey
D. Alexis, M.D.
Cardiologist has helped grow UR Medicine heart transplant program, which recently celebrated a record number of transplants — 40. He discusses why there have been more transplants locally
Q: UR Medicine recently made news for having performed 40 heart transplants in 2023, 82% more than the previous year. What's your role in this?
A: I am one of the heart failure cardiologists. My team has many members. The cardiologists help to manage the patient both before and after the transplants. We manage their heart failure and then, after they get their transplant, help make sure they're taking their medicines correctly, doing their biopsies, keeping an eye on how their progressing. The surgeons do the actual transplant. We also have transplant coordinators who play a very vital role in the post-operative care — seeing the patients in clinics, adjusting their medications. And, of course, we also have financial counselors, dietitian, psychologists and social workers. So it really takes a village, a lot of people working together to make sure patients are getting a benefit from their transplant.
Q: How long have you been with the program?
A: I've been with the program since October 2003. Transplants started in 2001 at the University of Rochester. And we've been growing the program since then. We did 40 transplants last year, which is a record for us. There are several factors that led to increasing numbers of transplants, not just for our center, but across the country. One of the reasons for that is we can now use hearts from patients with hepatitis C. That's a big change because in the past we couldn't use them because that would mean the recipients would get hepatitis C. That comes with a lot of bad side effects like liver disease. Now we have a cure for it, so we're able to use those hearts.
Q: How common of an issue was that?
A: So one of the tragedies is that the opioid epidemic has produced a lot of donors, many of which had hepatitis C as well. So those are hearts that we're able to use now. The relationship with donors has
also changed. Fifty years ago a lot of donors were from motor vehicle accidents. You don't see that as much anymore. So now donations are more commonly from donors who died of stroke or an overdose. You may have also heard of something called DCD, donation after circulatory death. That's also started to be used. That's where patients don't necessarily have to have experienced brain death to become donors. So that's also increased the number of transplants we're seeing around the country.
Q: What are some examples of DCD?
A: So these are patients who have a critical illness and are about to die. They're often on a breathing machine. They're taken off. We wait for them to pass and then we harvest their hearts. Whereas before there was the requirement of brain death that patients had to meet.
Q: What's the prognosis look like for a heart transplant recipient these days?
A: The biggest chal-

have a longer life expectancy. This is sort of old data because it's being updated, but the median survival rate was around 11 years. For those who survived the first year, the median life expectancy was 13 years. There are some signals that suggest that's improving. There are patients who have lived 30 years. We still have ways to go to improve survival. Issues patients may have include rejection and infection, and cancers can be another issue. These can be cancers of different organs or lymphoma. The issue is due to immunosuppression which doesn't necessarily cause the cancers, but doesn't help.
Q: What kinds of conditions are generally treated with heart transplants?
A: Patients may have coronary heart disease. They may have had a large myocardial infarction. There may be a familial process. Some families have multiple members who have needed heart transplants. Some patients may have an inflammatory process called myocarditis. There's a weakness that can develop in the heart related to pregnancy. And, finally, there's congenital heart disease. So patients who are born with heart disease or defects. And while treatment and survival rates for congenital heart disease is improving, their hearts may fail over time, so they may eventually need a heart transplant.
Q: How did you personally become interested in this subspecialty?
A: I always found the mechanics of the heart interesting. Heart failure has high mortality, but with sudden onset heart failure you can potentially get patients better in a short period of time. I always found that fascinating. And then with heart transplants, the fact that you can remove a heart from one patient and implant it into another patient is really remarkable.
Q: Do you do any work with devices?
A: Yes. I'm actually the director of the LVAD (left ventricular assist device) program here at Rochester. They are great devices for patients who have end-stage heart failure. So what we try to do is find the right treatment for each patient. For some, LVAD might be the best treatment, for some it may be a transplant. For some it could be medicine. But some patients do very, very well on LVADs.
Lifelines
Name: Jeffrey D. Alexis, M.D.
Position: Medical director of the Left Ventricular Assist Device Program at University of Rochester School of Medicine and Dentistry
Hometown: Brooklyn
Education: Harvard Medical School
Affiliations: University of Rochester Medical Center
Organizations: American College of Cardiology, Heart Failure Society of America, International Society of Heart and Lung Transplantation, American Heart Association, Association of Black Cardiologists Family: Wife (Christine), three children
Hobbies: Watching sports, bicycling, reading
Page 4 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024

Healthcare in a Minute
By George W. Chapman

O!-O!-O!-Ozempic!
Medicare spent $57 million to cover the drug in 2017. It spent $4.6 billion in 2022
The catchy tune in the commercial might be referring to its price.
Medicare approved the drug to treat diabetes in 2017. Part D spent a sensible $57 million on it for patients in 2018. But due to increased demand, new uses like weight loss and glaring price gouging by manufacturer Novo Nordisk, Part D spending on Ozempic rose to an astounding $4.6
Pharmacist Shortage
Not getting much attention, (like the nurse and physician shortage), is the increasing shortage of pharmacists.
In the past 10 years, the number of applicants to pharmacy schools has declined a precipitous 60%. Some of this decline could be self-inflicted as pharmacy schools unilaterally decided to mandate all students must get a Ph.D. starting in 2000. It has gotten so bad that CVS is offering $20,000 scholarships to 21 needy pharmacy students. While laudable, that won’t even make a dent in the shortage.
Pharmacy is a great career. Pharmacists work in hospitals, supermarket, community retail stores, primary health centers, nursing facilities and research. Salaries are in the $130,000 to $170,000 range. Pharmacists are increasingly involved in direct patient interaction. The shortage of pharmacists and our dependence on
billion (with the “b”) in 2022.
Medicare has been prevented from using its vast purchasing power to negotiate drug prices literally by an act of Congress under George W. Bush. Recently, Congress has magnanimously allowed Medicare to negotiate 10 - yes, just 10 - drug prices in 2026. This shows how much influence and control the drug lobby exerts over Congress. Maybe one of
the “goodwill” of corporations like CVS to mitigate the shortage is just another example of our fragmented and uncoordinated healthcare system where individual components must fend for themselves because there isn’t a national strategic plan or vision.
Health Over Wealth Act
In an effort to control unscrupulous private equity firms notorious for realizing profits over patient safety and community welfare, this proposed bill would require medical groups, nursing homes and hospitals to reveal any PE affiliation.
Struggling healthcare organizations, particularly vulnerable rural nursing homes and hospitals, have resorted to partnering with PE for salvation. Typically, the PE firm will quickly turn around the finances of their client by immediately cutting staff and unprofitable services.
Employers are faced with rising premiums. Consequently, employee contributions and copays are also rising (cost shifting) causing many families to postpone or even avoid seeking care because of high out of pocket expenses. As discussed in previous columns, medical debt is the No. 1 cause of personal bankruptcy. While the goals of the task force are laudable, they should also consider a functioning national healthcare system to replace our enormously expensive, confusing, inequitable, uncoordinated and fragmented healthcare system. Just saying.
Kaiser Permanente acquires Geisinger Health
the 10 prices Medicare negotiates in 2026 will be Ozempic. This is another example of why our care and drugs cost so much and why we need to seriously consider/ study a national plan. As mentioned last month, total healthcare costs in the US are expected to increase from about $5 trillion last year to around $15 trillion in 2030.
Before the facility knows what has hit them, their fledgling hospital or nursing home has been stripped to bare bones, leaving the remaining employees and the community high and dry.
Once the ephemeral profits are gone, so too is the PE firm. PE firms typically get paid a hefty management fee and then first crack at profits. The Health Over Wealth Act is intended to regulate PE in healthcare and to require healthcare organizations to reveal any PE involvement.
Task Force on EmployerSponsored Healthcare
Half of the US population is covered by employer-sponsored healthcare.
The Commonwealth Fund has recently created a task force comprised of representatives from politics, universities and insurers to identify market incentives and regulatory policies that would result in better access, delivery, outcomes and overall population health.
California-based Kaiser has just added Pennsylvania-based Geisinger Health to its vast multi-hospital, multi-system, multi-state healthcare system, Now known as Risant Health, the multifaceted healthcare system boasted revenues more than $100 billion last year. Geisinger brings 10 hospitals (including Guthrie Cortland Medical Center) and 600,000 members to Risant.
Nonprofit hospitals have had to build large networks and capital in order to compete with well- heeled for-profit providers like Walmart, Amazon and CVS. Size helps Risant effectively negotiate with wealthy commercial insurers like United, Aetna, BCBS, Anthem and Humana. The ultimate goal is to further develop Risant’s own health insurance plan (Kaiser Permanente) by adding members which mitigates risk and keeps their premiums competitive. Profits generated by their proprietary insurance plan are then re-invested in the healthcare system and patient care.
Amazon RxPass
Medicare can’t negotiate prices, but Amazon can. Prime members are eligible for the RxPass which promises not only lower drug prices but drone delivery to your doorstep someday soon. This home delivery presents an existential threat to “mom and pop” pharmacies and huge corporate chains like CVS and Walgreens. Between 2009 and 2015, one of eight brick and mortar pharmacies closed, most in depressed and underserved communities. Innovation is great, but once again our lack of a national gameplan is apparent.

George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.
Page 6 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024

Life Expectancy in Rochester Region Falls by 3 Years Since 2013
People of color and people living in ZIP codes with low socioeconomic status affected the most
Spikes in the number of deaths from drug overdoses, homicide, heart disease and COVID-19 led to a three-year drop in life expectancy in the Finger Lakes region from 2013 to 2021.
The average life expectancy for the region peaked at 80.5 years in 2013 before falling to 77.3 years by 2021.
The drop that started in 2013 erased all the gains in life expectancy recorded from 2000 to 2012.
This is according to a new data spotlight on life expectancy for the nine-county Finger Lakes region released in March by Common Ground Health.
The analysis was based on information from the New York State Department of Health Vital Statistics.
Life expectancy declines were largest for people of color and people living in ZIP codes with low socioeconomic status, leading to the largest gap in life expectancies since at least 2000.
In 2021, those living in low socioeconomic status ZIP codes had a life expectancy that was 9.2 years lower than those living in high socioeconomic status ZIP codes. Life expectancies fell 7.5 years for Black non-Latino residents and 6.8 years for Latino residents from their respective peaks. In contrast, the life expectancy of white residents declined only 2.5 years.
“The color of your skin or
amount of resources in your neighborhood should not determine how long you live,” said Wade Norwood, CEO of Common Ground Health.
“We know how to close these gaps: we can reverse overdoses, we can de-escalate violence and we can prevent drug addiction, heart disease and COVID. What we need is continued commitment to public health preventative measures and immediate action to ensure that everyone is able to live a long and healthy life.”
Many of the root causes of the inequities are outline in previous Common Ground Health reports, such as “ Overloaded: The Heavy Toll of Poverty on Our Region’s Health, The Color of Health: The Devastating Toll of Racism on Black Lives.”
“We never forget that these statistics represent loved ones lost too soon,” said Marc Solomon, director of analytics at Common Ground Health. “We encourage the community to read our previous reports, which outline the underlying causes of these disparities. The reports summarize the actions our community has said it needs to address the inequitable outcomes we see reflected in the life expectancy data.”
To read the original study, visit www.commongroundhealth.org/lifeexpectancy24.
Submitted by Common Ground Health
SERVING MONROE AND ONTARIO COUNTIES
A monthly newspaper published by Local News, Inc. Distribution: 33,500 copies throughout more than 1,500 high-traffic locations.
In Good Health is published 12 times a year by Local News, Inc. © 2024 by Local News, Inc. All rights reserved. P.O. Box 525, Victor NY 14564. Phone: 585-421-8109 • Email: Editor@GVhealthnews.com
Editor & Publisher: Wagner Dotto
Writers: Deborah J. Sergeant, Chris Motola, George Chapman, Gwenn Voelcker, Anne Palumbo, Jim Miller
Advertising: Anne Westcott (585-421-8109) • Linda Covington (585-750-7051)
Layout & Design: Angel Campos–Toro • Office Secretary Allison Lockwood
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen.




Power of Eminus Mirus to Your Reiki Practice.

May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 7
ADVANCED FOOT CARE from Andrea’s Foot Care Pino
Andrea Whitcomb-May 585-381-4297 Andreasfootcare.com Call our experienced team for your home foot care service. House Calls Tools are sterilized in a medical grade autoclave. Specializing in diabetic and geriatric care. FEELING TRAPPED IN A CYCLE OF UNEXPLAINED HEALTH ISSUES? The Struggle is Real •
to Break Free Personalized All-inclusive Wellness Programs Natural Wellness – Preventative Health Sandy
ADVERTISE Reach thousands of health-conscious readers in the region. Advertise with In Good Health — Rochester's Healthcare Newspaper Carol McCoon is teaching Eminus Mirus Energy Medicine
Class Location: Wheeler Healthy U, 308
East
RESERVE YOUR SEAT! All interested in energy medicine are welcome to attend. EM is an easy-to-learn, non-touch method. Classes forming for June & July LEVEL 1 IS FREE Carol McCoon, LMT, MS Ed. & EM Level 4 Practitioner. (585) 742-1969 | singingwind00@hotmail.com Listen to Carol’s interviews at her website: www.singingwindsoundtherapy.com
Saggiomo 585-309-9336
It’s Time
Bullard, Owner/Practitioner Call Today • 585-648-1999 www.cornerstonetohealing.com
Add the
Eminus Mirus Energy Medicine teaches how to improve the flow of Qi & restore balance to the body Eminus Mirus addresses: Inflammation, Circulation, Anxiety, and Allergies
Bluff Dr,
Rochester.
Live Alone & Thrive
Practical tips,
advice
By Gwenn Voelckers
and hope for those who live alone
On Your Own: Rediscover Your True Self
Living alone after a divorce or the death of a spouse can be a challenging yet transformative experience.
I know it was for me.
My own path to contentment took some time, some growing pains — setbacks as well as successes — and some aching losses before I could find my way back to my true self.
For many, the transition from married life to being single marks a period of rediscovery and a time to redefine their identity.
After focusing on the needs of a spouse and family, it’s common to feel as if you’ve lost touch with who you are as an individual. However, I’ve come to realize that the key to living alone successfully lies in embracing this opportunity to explore who you really are and who you aspire to be.
My journey began with a set of soul-searching questions to identify and clarify my beliefs, values, likes and dislikes. I was careful to focus on what mattered to me and to steer clear of “shoulds” and other people’s agendas.
This exercise in introspection enabled me to create a life that is authentic, fulfilling and uniquely mine. Contentment followed.
To begin your own journey of self-discovery, you might start by asking yourself some fundamental questions:
1. When have you felt the most fulfilled and alive in your life? What were the circumstances surrounding those moments?
2. What dreams and aspirations did you have when you were younger? Are there any steps you can take now to work toward those dreams?
3. Who are the people in your life that bring out the best in you? What is it about those relationships that are so meaningful to you?
4. What are you curious about? What subjects or topics do you find yourself constantly wanting to learn more about?
5. When do you feel most like your ol’ self again? What are you doing in those moments? (I took up gardening again.)
6. What values are most important to you? Helping the less fortu-
nate? Working toward equal rights? How can you incorporate those values into your daily life?
7. What kind of books, movies or music do you enjoy? Could those subjects hint at a hidden passion or interest?
8. How do you spend your time when no one is watching, when you are just being you? (I like to sing to my cat!)
9. What activities or hobbies did you pursue as a young adult that gave you joy? Are there any ways you can incorporate those activities back into your life now?
10 What are some small, simple pleasures in life that bring you joy? How can you incorporate more of those into your daily routine?
These questions can help you gain a deeper understanding of yourself and your desires. They can also serve as a guide as you navigate this new chapter in your life.
Teresa, a good friend of mine, had spent most of her adult life caring for her family. She wouldn’t have traded that for the world, but after her divorce, she realized that somewhere along the way she had disappeared around the edges. She had lost her own sense of self.
Determined to reconnect with herself, she started exploring her family history through Ancestry.com. As she delved into her roots, she uncovered fascinating stories about her ancestors and their lives. Teresa began to see herself as part of a larger whole, which brought her a deep sense of fulfillment and belonging.
Similarly, Steve, my middle-aged neighbor, found himself at a crossroads after the death of his wife. He had been so aligned with her that he struggled to find his own identity after her passing.
Through therapy and self-reflection, Steve recalled his love of travel. On his first solo trip, he discovered a sense of freedom and adventure that he had been missing. It led to many more trips and a newfound appreciation for life’s possibilities.
Teresa and Steve’s stories highlight the transformative power of reconnecting with your true self. By taking the time to understand who you are and what you want out of life, you can create a new and fulfilling existence for yourself.
Remember, this journey is yours and your alone. Embrace it with an open heart and a curious mind, and you will be amazed at what you discover along the way.

Gwenn Voelckers is the author of “Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own.” She welcomes your thoughts on this column as well as topic suggestion for future essays at gvoelckers@rochester. rr.com.


Page 8 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024
Along with the Blue Cross Blue Shield Association, we’re committed to reducing racial and ethnic maternal health disparities by 50% in 5 years. Join us and take action today: Get the facts in our episode “Reducing Racial Disparities in Maternal Health” with Dr. Cuyler at ExcellusBCBS.com/ podcast or wherever you listen to podcasts. 01 0203 BE AWARE BE ENGAGED BE AN ADVOCATE Childbirth complications are 46% higher among Black mothers. Anyone can help by learning more about this urgent issue. (Tip: start with our podcast episode)1 Every expecting mother should receive unbiased, high-quality care. Examine your own implicit biases. What might need to change? Support policies and organizations that increase access to affordable, culturally sensitive maternal healthcare. Let the expecting mothers in your life know they have a voice, are being heard, AND believed. When every mom receives the care she needs, EVERYBODY BENEFITS 1. Blue Cross Blue Shield Association. Health of America, Maternal Health Data. 2020.
FU.S. Falls Out of Top 20 in ‘World’s Happiest Countries’ List
or the first time, the United States has fallen out of the top 20 spots on the annual world’s happiest nations list.
Americans are now No. 23, far behind the top five countries — Finland (No. 1), Denmark, Iceland, Sweden and Israel.

“The United States of America has fallen out of the top 20 for the first time since the World Happiness Report (WHP) was first published in 2012, driven by a large drop in the wellbeing of Americans under 30,” the World Happiness Report said in a news release. The U.S. placed 15th in last year’s rankings.
This decline may not come as a surprise to many Americans, with U.S. Surgeon General Vivek Murthy citing rising levels of anxiety and mental health issues among the young as a “devastating” crisis as far back as 2021.
The new global happiness tally was issued to coincide with the United Nations’ International Day of Happiness. It’s based on citizens’ responses from more than 140 nations and is “powered by data from the Gallup World Poll and analyzed by some of the world’s leading wellbeing scientists,” the WHP explained.
Rounding out the top 10 countries on the list, beginning with No. 6, are The Netherlands, Norway, Luxembourg, Switzerland and Australia. Canada placed 15th and the United Kingdom, No. 20.
At the bottom of the 143-nation list: Afghanistan.
For the first time, the survey also attempted to assess happiness levels by age.
“In comparing generations, those born before 1965 are, on average, happier than those born since 1980,”
the WHP found. “Among millennials, evaluation of one’s own life drops with each year of age, while among boomers life satisfaction increases with age.”
There was variance between countries when it came to differences in generational happiness, however.
“We found some pretty striking results,” said John Helliwell, emeritus professor of economics at the Vancouver School of Economics at the University of British Columbia in Canada, and an editor of the World Happiness Report.
For example, happiness among the young (ages 15 to 24) has declined across North America, Western Europe, the Middle East and North Africa, and South Asia since 2019, the report found.
But everywhere else, younger people are feeling better now than in years past.
“There is a great variety among countries in the relative happiness of the younger, older, and in-between populations,” Helliwell said in the news release. “Hence the global happiness rankings are quite different for the young and the old, to an extent that has changed a lot over the last dozen years.”
Lithuania is the happiest place to live if you’re age 30 or under, the report found, while Denmark is the happiest spot for folks age 60 or older.
Some countries have seen big improvements in their levels of happiness. For example, Serbia has steadily risen 69 places up the rankings since 2013, to take the No. 37 spot in 2024. Bulgaria charted a similar 63-place rise, to rank No. 81 this year.



May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 9 Scan the QR code or visit HearingLossRochester.org to learn more. Hearing loss. You don’t have to face it alone. Forty Years Strong
Advertise with In Good Health
Confused by the LGBTQ+ Terms? Here’s Some Guidance
By Deborah Jeanne Sergeant
Understanding the “alphabet soup” of LGBTQ+ can challenge people outside of these groups.











Katrina Ehmann, licensed clinical social worker and non institutional care program coordinator and veteran care coordinator for LGBTQ+ Health Program at the Department of Veteran Affairs in Rochester, said that these letters frequently represent the terms that capture “the spectrum of how we relate to others sexually, romantically, emotionally and also how we define who we are by our gender or gender expression. Most commonly known of the acronym are L=Lesbian, G=Gay, B=Bisexual, T=Transgender, Q=Queer. The ‘plus’ signifies the many other identities and sexual orientations.”
She encourages people to ask open-ended questions such as “Who do you live with?” or “Who do you spend most of your time with?” instead of “Are you married?”
“When assessing someone’s overall health, ask if they’re sexually active, how many partners, male, female or other?” she said. “Let the
person know that it’s important for you to understand this aspect of their health for preventive health care and to ensure their health care goals are met.”
Awareness as to why these questions are asked can help prevent misunderstandings.
Ehmann believes that listening and mirroring the other person’s language can help foster a greater level of comfort.
“Use the name or pronouns they’re asking to be called by and if they’re speaking about a relationship and use the term ‘significant other’ for instance, you too should use that same term,” she said. “If you make a mistake, it’s OK, apologize and be sure next time to use the proper language, as they’ve asked you to use.”
Ehmann said that using the correct terms with others may not be possible and that some new terms may develop and older ones may change in meaning, since language is ever-evolving.
But it all hinges upon respect for others.
“Ultimately when interacting with others whether in the healthcare setting or in general, every person deserve to be treated respectful and to feel safe, so approach everyone you meet with an open mind and open heart,” Ehmann said.

Doing so in a healthcare setting is especially important so patients feel heard and so they build a trusting relationship with their healthcare provider. Megan Lytle associate professor of psychiatry at URMC, said that using the correct name and pronouns can reduce suicide risk by 56%.
“It says, ‘I see you and know who you are,’” Lytle said. “It’s like a cisgender person using their new last name after getting married. Language is important with every patient we see.”
She added that it may be helpful to “check in” by asking if you’re using the right language. She views this as a strategy aligning with a patient-centered approach.
“If you’re unsure, a very simple thing is to introduce yourself with your name and pronouns as it cues the person that they’re safe,” Lytle said. “Ask, ‘How may I address you?’”
Recording the correct title helps improve consistency when addressing people.
As further information is needed, it is also alright to ask people to define terms that are unfamiliar or that may be used in ways with which you do not expect.
“The definition of ‘bisexual’ is different from when I was growing up,” Lytle said. “I may say, ‘I’m going to ask you a lot of questions and some may seem obvious but I want to understand you.’ If they tell me something that may not feel as obvious, I may say, ‘I’m somewhat familiar with that but I’d like to know what that means to you.’”
Page 10 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024
D E P AUL
The way to reach thousands of health conscious readers in Rochester and the Finger Lakes GVHEALTHNEWS.COM MARCH 2024 NEW ADDICTIONINTERNETSPECTRUM: WHERE ARE YOU ON THE SCALE? NONPROFIT USES FITNESS AND EXERCISE TO FIGHT ADDICTION When the Big Boss is a Nurse Dan Ireland has tracked a path from bedside nursing to C-level hospital leadership. He is now the president of three Rochester Regional Health hospitals: United Memorial Medical Center, Newark-Wayne Community and Clifton Springs. Jonathan Westfall is the executive director at ROCovery Fitness, a community recovery outreach center. DON’T WAIT ‘TILL SOMETHING HAPPENS TO YOUR HEART P. 11 WHO WINS, WHO LOSES IN THE DISPUTE BETWEEN EXCELLUS BCBS AND WELLNOW? George Chapman: “Unless the stalemate is broken, all three parties — Excellus BlueCross BlueShield, WellNow, consumers — will lose.” 8 Top Concerns for Older Adults Expanding Longevity: $101 Million to the Best Ideas Why You Need to Have Your Hearing Checked Recent studies by top universities suggest taking multivitamins could help prevent memory loss and slow cognitive aging among older adults. Daily MightMultivitamin Help BrainsAging GVHEALTHNEWS.COM FEBRUARY ISSUE 222 EE GOLDEN YEARS SPECIAL ALSO INSIDE HEART HEALTH FREE WNY Mom Bikes Across America Transcontinental bike trek — 3,600 miles from San Diego to New York City —honors the memory of her son, who died by suicide. Page 8. 5 THINGS YOU NEED TO KNOW ABOUT April is Stress Awareness Month. How to keep it in check. Page 19 CHIROPRACTIC CARE NOW CONSIDERED MAINSTREAM Longtime chiropractor recalls that medical doctors were very prejudiced against chiropractic — chiropractic care has come a long way, he says P.13 ORGAN DONATIONS GVHEALTHNEWS.COM APRIL 2024 J. Ryan of the Finger Donor Recovery IT’S WORTH SUPPORTING IT! editor@GVhealthnews.com
others whether in the healthcare setting or in general, every person deserve to be treated respectful and to feel safe, so approach everyone
meet with an open mind
open heart'
'Ultimately when interacting with
you
and

Cancer Cases Set to Soar 77% by 2050, Thanks to Aging Population
As the world's population ages, a new report warns that the number of people with cancer could climb 77% by 2050.
In the report, published in April in the journal CA: A Cancer Journal for Clinicians, researchers from the American Cancer Society found there were about 20 million cancer cases and 9.7 million cancer deaths in 2022, the latest year for which data is available.
However, “we think that number will go up to 35 million by 2050, largely due to an increasing population in the aging population,” physician William Dahut, chief scientific officer for the American Cancer Society, told CNN.
“A lot of the drivers for cancer that we've traditionally seen in high-income countries, such as tobacco and obesity, these same cancer drivers are now moving into the low-income countries,” Dahut noted. “These are countries that do not have the tools to find cancer early, treat cancer appropriately and prevent it in ways that are often being done in other countries.”
The good news is that those risk factors can be minimized with lifestyle changes, experts said.
“With more than half of cancer deaths worldwide being potentially preventable, prevention offers the most cost-effective and sustainable strategy for cancer control,” senior study author physician Ahmedin Jemal, senior vice president of surveillance & health equity science at the ACS, said in a news release. “Elimination of tobacco use alone could prevent 1 in 4 cancer deaths, or approximately 2.6 million cancer deaths annually."
Another expert concurred.
While the causes of cancer can be complex, genetic or environmental, “about 50% of cancers are preventable,” Bilal Siddiqui, an oncologist and assistant professor at the University of Texas MD Anderson Cancer Center, told CNN.






“All patients should talk to their doctors to ensure they receive age-appropriate cancer screenings, and it's important to make the key lifestyle changes that can reduce our risk for cancer, including stopping smoking, reducing alcohol intake and staying physically active,” he said.
In the new report, researchers turned to global data on cancer incidence and death from the Global Cancer Observatory, a World Health Organization database.
What did the data show?
The most common cancer types were lung, breast in women, colon, prostate, stomach, liver, thyroid, cervical, bladder and non-Hodgkin lymphoma, according to the report.
Lung cancer was also the leading cause of cancer deaths, followed by colon, liver, breast in women, stomach, pancreatic, esophagus, prostate, cervical cancer and leukemia.
Tobacco remains “the principal cause of lung cancer,” according to the report.
“While we do see lung cancers that are not related to smoking, the number one cause of lung cancer is smoking. And so obviously, there's still much work to be done in the U.S. and everywhere to continue to address the epidemic of smoking,” said physician Harold Burstein, an oncologist at Dana-Farber Cancer Institute in Boston.
“Other things that people can do to reduce their cancer mortality include screening for early cancer detection and better outcomes. In the U.S., we have very vigorous opportunities for screening with mammography, colonoscopy and Pap smears, but these are still often under-utilized by many parts of our society,” he said. “In the more advanced economies, like the U.S., we have seen remarkable declines in the rates of mortality from breast cancer and colon cancer, probably about half of that due to early detection.”
























• Help an older adult manage day-to-day
• Give a lift to someone who no longer drives.
• Give a caregiver a break.
• Make a friendly phone call.
• Lead fall prevention or healthy living workshops.
• And more!

May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 11
LIFESPAN WELCOMES EVERYONE
nances.
OUR VOLUNTEERS FILL CRITICAL ROLES SUPPORTING OLDER ADULTS AND CAREGIVERS. www.lifespanrochester.org Time exible and ful lling! When you do good, you feel good! Learn more! Join us for our Register Now! MASKS ARE STILL REQUIRED DUE TO COVID-19, STRICT SAFETY POLICIES ARE IN EFFECT AND APPLY TO EVERYONE. WE COVER OUR STYLING CHAIR IN DISPOSABLE VINYL. I ALSO WEAR PROTECTIVE COVERINGS. THERE IS NO WAY AN OPERATOR COULD BE THREE FEET APART FROM A CLIENT WHILE WORKING, WHICH IS WHY THE CLIENT AND I ARE COVERED. YOU WILL RECEIVE FOOT COVERINGS, VINYL GLOVES AND A SHEER VINYL CAPE WHICH YOU WILL WEAR OUT TO YOUR CAR AND DISCARD AT YOUR CONVENIENCE. TEMPERATURE WILL BE TAKEN AT THE DOOR. NO WIGS ARE TOUCHED BY BARE HANDS. ONLY THE CLIENT IS PERMITTED INSIDE! CALL 585-392-7823 NO TEXTING OR EMAILS NO PICTURES TAKEN - ONLY FACETIME BY APPOINTMENT ONLY - ABSOLUTELY NO WALK INS. MUST CALL FOR APPOINTMENT Grasta’s helps individuals with Chemotherapy, Radiation, Psoriasis, Alopecia, Diabetes, Menopause, Childbirth, Lupus, & Burn Victims, Trichotillomania and COVID 19 related Hair Loss. HIGH QUALITY WIGS & HAIR PIECES IN A VARIETY OF STYLES & BLENDS AND TOPPERS ARE AVAILABLE. ASK ABOUT MY NEW AMBIENT FIBER WIGS A+ Rating Grasta’s Beauty And Wig Studio grastasbeautyandwigstudio.com 409 Parma Center Rd. (Rte. 18), Hilton Just minutes from Greece Ridge Mall! Sharon M. Grasta (Russo) - owner & operator LARGEST INVENTORY OF TOP QUALITY WIGS IN WESTERN NEW YORK! CALL 585-392-7823 - NO TEXTING BY APPOINTMENT ONLY - ABSOLUTELY NO WALK-INS. MUST CALL FOR APPOINTMENT. CUSTOM MADE EUROPEAN HUMAN HAIR, WIGS & TOPPERS - HATS & SCARVES TOO We specialize in professional, personal, and confidential service. We enjoy making clients feel beautiful from the inside out. MASKS ARE STILL REQUIRED. Due to Covid-19, strict safety policies are in effect and apply to EVERYONE. We cover our styling chair in disposable vinyl. I also wear protective coverings. There is no way an operator could be three feet apart from a client while working, which is why the client and I are covered. You will receive foot coverings, vinyl gloves, and a sheer vinyl cape which you will wear out to your car and discard at your convenience. Temperature will be taken at the door. No wigs are touched by bare hands. ONLY THE CLIENT IS PERMITTED INSIDE! “She made me feel beautiful...” “Sharon was so kind & understanding and she had lots of hairpieces to choose from. She knew exactly what I needed. I loved her right away because she showed me what was good on me & the ones not good on me. Sharon was always patient Sharon loves her customers and it shows in how wonderful she treats them: like family. - Mrs Ann M. Colarertalo 409 Parma Center Rd. (Rt. 18), Hilton Grastasbeautyandwigstudio.com Sharon M. Grasta (Russo) – owner & operator ONLY THE CLIENT ALLOWED INSIDE
Attracting Male Nursing Students
What can educators do to attract more men to the nursing field?
By Deborah Jeanne Sergeant
From Florence Nightingale onward, nursing has been a female-dominated career. But more men than ever are earning nursing degrees.
According to the Bureau of Labor Statistics, the percent of male nurses has grown by 59% in the past decade. However, that still amounts to only 12% of all licensed practical nurses, registered nurses and nurse practitioners.
One of the barriers to seeking an education in nursing is the need to earn while you learn. It’s tough to hit “pause” on work to focus solely on the rigorous studying required to complete a nursing degree. Pew Research reveals that women are the primary breadwinner in only 16% of US households and men are the primary or sole breadwinner in 55% of them.
Finger Lakes Health College of Nursing and Health Sciences offers
some remote prerequisite classes and evening classes which “help the person who is working full-time,” said Kathy Mills, registered nurse and dean of Finger Lakes Health College of Nursing and Health Sciences and director of Marion S. Whelan School of Practical Nursing.
Many of the resources and textbooks are also online, which can help people who are working to fit in study time when they can.
“We have agreements with several colleges like Keuka and Brockport so their coursework would correlate,” Mills said. “They both have online courses for their bachelor’s. Typically at the associate level that is where they get most of the hands-on and most of the rest is online.”
James Hill, an assistant nurse manager for ambulatory psychiatry at UR Medicine Mental Health & Wellness, believes that the field is “more welcoming of men” than

it used to be and he is seeing more male students coming into clinic than he used to.
“In a traditional sense, making it more flexible for males to go back to school while working part-time or full-time, that is attractive,” Hill said.
He certainly found that true in his academic journey. The flexibility offered him by part-time classes at a community college and accelerated classes at Niagara University helped him scale back his full-time employment to part-time for only a year while earning his BSN in 2016.
“I was still able to financially contribute to the family,” he said. “The flexibility of the program made it more attractive to work while still going back to school. It would’ve been much more difficult to pursue a
career change in nursing if I'd had to go back to school full-time.”
Although he found the accelerated program stressful — one of the toughest experiences of his life, in fact — it was for only a year. The program accepted the general education core from a previous bachelor’s degree and a few classes at community college fulfilled prerequisites like anatomy and biology.
Of course, women who work full-time also benefit from hybrid, weekend and online classes. However, the social stigma of quitting work to go to school is less for women than men, as women often take time away from work for family care giving duties. Traditionally, women aren’t expected to serve as the family’s main wage earner.
To our Thompson Health nurses and nurses everywhere



The nurses at Thompson Health serve as the backbone of our community, embodying dedication, compassion, and unwavering commitment to our mission of caring for others. Day in and day out, these healthcare champions go above and beyond to provide exceptional care, comfort, and support to each and every patient. Their selfless dedication not only improves the health and well-being of individuals, but also strengthens the fabric of our Finger Lakes community. Through their expertise, empathy, and tireless efforts, Thompson Health nurses truly make a difference in the lives of those they serve, personifying the highest standard of healthcare excellence.




Page 12 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024 Nursing
F.F. Thompson Hospital is an ANCC Magnet designated hospital for nursing excellence.

In a Field Historically Female-driven, Men are Making Inroads
Percentage of men in nursing grows from 9.4% to 11.2% between 2020 and 2022
By Deborah Jeanne Sergeant
During the pandemic, 20% of medical personnel left the healthcare industry, including nurses.
Interestingly, the number of males working in nursing has grown since then.
According to statistics published in the 2022 National Nursing Workforce Survey in the Journal of Nursing Regulation, the percent of men in nursing grew from 9.4% to 11.2% between 2020 and 2022.
One of them is Josh Lynch, registered nurse on an acute care floor for Rochester Regional Health, who graduated with a bachelor’s in nursing from Nazareth College in 2021.
Lynch had previously worked as a certified master automotive technician and operated Mer-win Automotive in Rochester. He felt drawn to nursing because of the care his twin girls received after his babies were born 15 weeks early. It was five months until both girls were at home and the neonatal intensive care unit nurses impressed Lynch deeply.
“I said to my wife one day, ‘I can go back to fixing cars; I’m really good at it but I’ll never be happy doing that again,’” he said.
The couple adjusted their working schedules and lives to accommodate Lynch going back to school.
Shifting from a male-dominated career of automotive repair to one that’s traditionally female-oriented wasn’t a huge adjustment to Lynch. But it seems to be at times to others.
“A lot of people say those are so misaligned and they’re really not,” Lynch said of his two careers. “There are so many similarities with critical thinking and diagnostics, only you’re diagnosing people not cars.”
He took the advice of his automotive mentor Chris Whiteman, who told him, “’Josh, sometimes you can’t just put your toe in to test the waters; you have to jump in,’” he said. “If you really want to make a career change, jump in. it’s going to be scary and there will be uncertainty and most of the time, it works out in the end.”
Of his nursing class, 46 started and only about six men completed the class. But hiring agents seem eager to recruit male nurses, as they’re not common candidates. Because of his automotive background, he can “repair a lot of stuff on the unit that’s broken,” he said. “You do what you’ve got to do to get through.”
Lynch has noticed that although stigmas about working as a nurse have not been major, he has noticed that many things such as scrubs and shoes are geared more toward women.
Still, it’s a small matter and he’s glad to work as a nurse.
“I’ve had so many deep life experiences,” Lynch added.
‘Not very welcomed by staff’
A lot has changed for the better for male nurses since the start of the

nursing career of Greg Hoffman-Fragale, doctor of nurse practitioner and interim nursing officer at Finger Lakes Health.
He became interested in nursing at age 18 while working at a fastfood restaurant. Hoffman-Fragale had been accepted at Julliard and was weighing whether he wanted to play clarinet professionally. A relative encouraged him to work as a nursing assistant to test the waters.
Hoffman-Fragale earned his LPN in and later RN and eventually doctor of nurse practitioner. But when he started out in 1992, “I was not very welcomed by staff,” he recalled. “Back then, there was a lot of hazing by staff. They gave us a really hard time. It was quite a challenge, but I was determined to integrate into it. Over the years, I’ve observed more and more men in nursing, especially since the mid- to late-2000s.”
He also noted that many male nurses work in areas of leadership as well.
Hoffman-Fragale worked as a nurse in New York City for a few years and noted that integrating into a healthcare organization was easier there than in Upstate.
“It’s still a female-dominated profession and there are still moments where it’s more difficult,” he said. “There’s a sense of an undertone of unacceptance in some instances.”
Fortunately, he’s had almost never had an issue with patients, except for earlier in his career when a few elderly female patients wanted a female caring for them.
‘How’s Gaylord?’
Rochester Regional Health nurse
Todd Plucknette initially thought that he would work in exercise physiology and earned a degree from SUNY Brockport in 2015.
While seeing patients at the hospital, he observed what nurses do and he realized that’s what he really wanted to do. A fair amount of overlap between the education and


the job skills helped smooth the transition. After taking a few prerequisite courses, he graduated in 2020 with his associate in nursing from Genesee Community College and is hoping to return to school at SUNY Brockport for his bachelor’s degree in nursing.
As for receiving flack for his career choice, Plucknette said that hasn’t happened except for a little good-natured ribbing from his buddies such as “How’s Gaylord?” referencing a male nurse character maligned in the movie “Meet the Parents” (2000). But fortunately, a lot has changed in 24 years.
“I never get any disrespect or anything like that,” Plucknette said. “Our staff is really great, supportive and helpful. It’s a team effort to make sure the patients are well-cared for.”
He advises anyone interested in nursing to shadow a nurse on a unit or work as a tech to see what it’s all about.
May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 13
Greg Hoffman-Fragale, doctor of nurse practitioner and interim nursing officer at Finger Lakes Health
Josh Lynch is a registered nurse on an acute care floor for Rochester Regional Health
Todd Plucknette is a Rochester Regional Health nurse.
Nursing
Like Mother Like Daughter
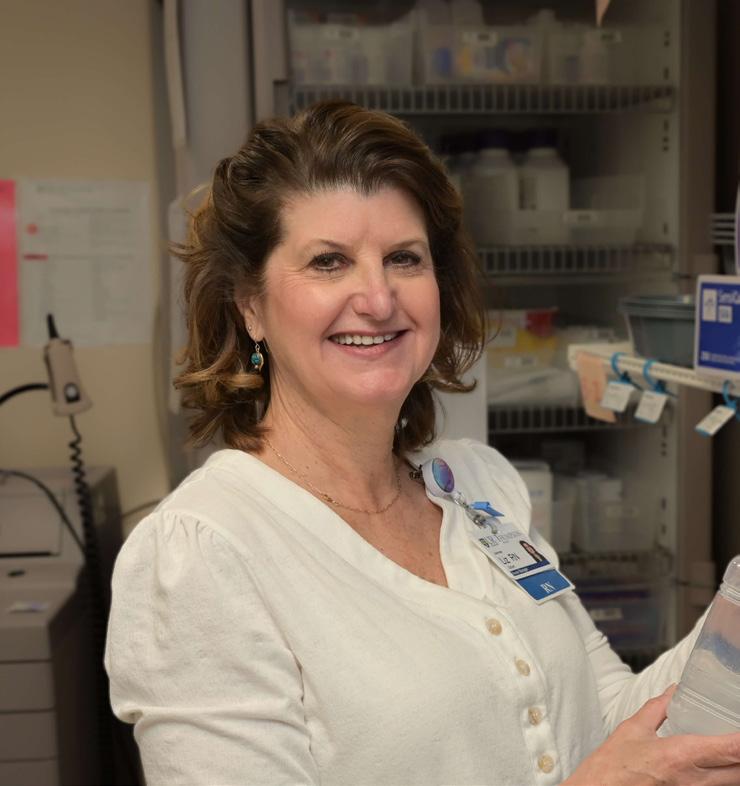
Nurses Diane Nau and Stacie Nestorowycz have both a career and family in common
By Deborah Jeanne Sergeant
Diane Nau, registered nurse, and her daughter, Stacie Nestorowycz, also a registered nurse, are both happy in their chosen professions at Rochester Regional Health.
However, their interest in the profession differed when they were younger.
Nau knew from a young age that nursing was the path for her once she read a “Little Golden Books — Nurse Nancy” book and dressed up as a nurse for Halloween.
“It just stuck with me and I never considered being anything else,” she said.
She began studying at Monroe Community College right out of high school and completed her RN in 1975. In 2013, she completed her master’s degree. She currently works as a labor and delivery nurse at Unity Hospital.
For Nestorowycz, she waffled between wanting to nurse like her much-admired mother and teaching.
New Visions, a high school career exploration program, provided an opportunity to experience teaching and Nestorowycz quickly learned that she hated it.
She completed her bachelor's de-
gree in nursing at Roberts Wesleyan in 2009. At first, she worked in labor and delivery but eventually shifted to surgical nursing, which she loves. She has two certifications in surgery and specializes in post-op nursing.
“Every day is different.”
Nestorowycz said. “People are at their most vulnerable after surgery and I can comfort and support patients to get to a better place. Right after surgery is hard.”
As for Nau, labor and delivery is her jam.
“Ninety-nine percent of the time, it’s happy but it’s challenging,” Nau said. “Women often doubt their ability to do it. It’s my job to empower them to bring their baby from the inside to the outside.
“On the other side, the 2% of the time, helping a family through it when their baby isn’t born in the way they expected is a huge part of the job as well. It takes a lot to help a family heal after that happens.”
Patient education is also a large part of her job.
Nestorowycz believes that although anyone can go to school to become a nurse, not everyone should do so.
“You have to love people for who



TRAIN FOR A NURSING CAREER
The call for nurses has never been stronger. Prepare for licensure and learn to deliver heartfelt, patient-centered care. Choose from two in-demand programs:
• Licensed Practical Nurse (LPN)
• Registered Nurse (RN)
Learn and practice in our Sands Family Center for Allied Health, which replicates a real hospital setting with patient bays, simulation rooms, and modern equipment. Get

they are,” she said. “It has to be in your heart that you want to make a difference to another person. That’s what drives me every single day. I want to be there for my coworkers and patients. I’m not there for the glory or fame.”
She encourages anyone interested in nursing to shadow a nurse or volunteer in some capacity in a healthcare environment to see what it’s like.
Nau enjoys the variety of positions in nursing, from neonatal nursing to hospice. There’s also leadership roles and education. She has also worked as a nursing instructor


at St. John Fisher. Nestorowycz hopes to volunteer in a hospice facility when she retires.
“Having a nurse as a parent really sets you up whether you want to do it or don’t want to,” Nau said. “You know your parents work off shifts, holidays and weekends. You know what it is going into it.
“I’d never dissuade any of my children if they wanted to be a nurse. Nursing is very fulfilling and you can do what you want.”
She has another daughter living in California who works as a nurse. Nestorowycz added that with nursing, “you can go anywhere.”

Page 14 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024
Schedule your complimentary, confidential hair loss evaluation today and see how easy it is to be yourself again! Call now! (585) 272-7320 We specialize in both permanent and non-permanent techniques, gradual hair replacement, and system integration. We can provide topical hair loss treatments and laser hair rejuvenation. Check out Virtual Reality Hair Replacement for men & women at Baldness.com. Serving Men, Women and Children Restoring hair Restoring confidence Affordable Financing. Onsite service and repairs. 1425 Jefferson Rd., Saginaw Plaza, 2nd floor Rochester, NY 14623 • 272-7320 Rochester’s Hair Replacement Specialists Rochester’s Hair Replacement Specialists Schedule your complimentary, confidential hair loss evaluation today and see how easy it is to be yourself again! Call now! (585) 272-7320 We specialize in both permanent and non-permanent techniques, gradual hair replacement, and system integration. We can provide topical hair loss treatments and laser hair rejuvenation. Check out Virtual Reality Hair Replacement for men & women at Baldness.com. Serving Men, Women and Children Restoring hair Restoring confidence Affordable Financing. Onsite service and repairs. 1425 Jefferson Rd., Saginaw Plaza, 2nd floor Rochester, NY 14623 • 272-7320 Rochester’s Hair Replacement Specialists Rochester’s Hair Replacement Specialists
Mother & Daughter: Diane Nau, registered nurse, and her daughter, Stacie Nestorowycz, also a registered nurse, work at Rochester Regional Health.
started
at FLCC.EDU/NURSING
now
How to Become a Nurse Mid-Career
Shifting from a different career to nursing is easier than ever
By Deborah Jeanne Sergeant
After 10 years working in education in Buffalo City Schools, James Hill was looking for a change.
He had always wanted a career that involves helping others.
He filled that desire by becoming a nurse. Hill currently serves as an assistant nurse manager for ambulatory psychiatry at UR Medicine Mental Health & Wellness.
“My main goal in life is to help other people,” Hill said. “I figured nursing was a great option. I also appreciated the flexibility that nursing offered. The world is your oyster. There are many different hats you can wear as a nurse.
“My ultimate goal in life is to be a great father and husband. I don’t want my career to get in the way of my roles as a father and husband.”
Since Hill needed to contribute to his household income while going to nursing school, he initially worked part-time as a nurse’s aide at a hospital while attending a local community college part-time to complete a few
prerequisites. An accelerated class at Niagara University enabled him to graduate with a BSN (bachelor of science in nursing) in 2016, a year after beginning the program.
Hill is currently completing his master’s degree in clinical nurse leader at the University of Rochester School of Nursing.
In a way, his pursuit of a medical career brings his education full circle. Hill had initially enrolled at Canisius University in Buffalo in a premed program, but he had heard that it’s difficult practicing medicine while raising a family. Family — this time, his originating family — also influenced his life and career, as he and wife, Maria, moved back to Rochester to live closer to relatives.
“I’ve loved my nursing career,” Hill said. “I decided to get into psychiatric nursing, as a lot of skills and strategies I used as a special education teacher transferred to psychiatric nursing.”
The biggest adjustment initially was the schedule, going from Monday through Friday, 7 a.m. to 3:30
Where to Get a Degree
Looking for a nursing school? You have plenty of options in the region.
• Finger Lakes Health College of Nursing and Health Sciences
• University of Rochester School of Nursing
• Isabella Graham Hart School of Practical Nursing
• St John Fisher College
• Roberts Wesleyan University School of Nursing
• Bryant & Stratton College-Greece
• Nazareth College, Rochester
• Monroe Community College
• SUNY Brockport
• Keuka College
• Marion S. Whelan School of Practical Nursing
ADVERTISE

p.m. to a schedule that’s “all over the place,” Hill said. “A lot of the skills and strategies working with students were similar in working with patients in a psychiatric setting.”
Making the segue from non-medical career into nursing relies heavily upon the educational opportunities offered by nursing schools. That’s a topic often on the mind of Kathy Mills, registered nurse and dean of Finger Lakes Health College of Nursing and Health Sciences and director of Marion S. Whelan School of Practical Nursing.
In addition to standard daytime classes, Finger Lakes Health College
offers RN program classes in the evening with clinical hours on Saturdays to help people who are currently working to complete their degrees. The program requires students to attend classes on campus two days a week. Many of the prerequisite classes are available online, but the core nursing classes require in-person attendance.
For the remote classes, “all the lectures are recorded online so they get that the week before they come to class,” Mills said. “Then we do a learning activity, so we know they understand it. Like I do a lecture on physical assessment and in class, they can demonstrate on each other. We try to cover all the levels of students, those who learn by hearing or tactile. And we have texts for the reading learner.”
“It’s really focused for the adult learner,” Mills added. “That’s what we focused on when we developed it: the adult learner. That was the true intent for the RN degree.”
Clinic days last 10 hours. The associate program takes four, 15-week semesters to complete.
It’s not easy to complete a nursing degree while working. However, Hill advises those interested to follow your passion: “Ultimately, I made the career change for myself, as much as I like to help people. Nursing offered me the opportunity to help people, whether working at the bedside to help people or in other aeras. If you feel stuck in your career and you feel working in nursing would bring you more joy, pursue that. In the end, the whole journey was worth it.”

At People Inc., our RNs and LPNs build meaningful connections every day. Are you ready to make an impact?

May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 15 Nursing
Kathy Mills is the dean of Finger Lakes Health College of Nursing and Health Sciences and director of Marion S. Whelan School of Practical Nursing.
JOIN THE PEOPLE INC. FAMILY! Consistent Schedules • Outstanding Benefits LPNs: $23-26/hr • Full Time RNs: $70,720-76,960 (annual) Part Time RNs: $34-37/hr
APPLY
NOW
Reach thousands of health-conscious readers in the region. Advertise with In Good Health — Rochester's Healthcare Newspaper

Fighting Burnout
Nurses face unprecedented risks for burnout
By Deborah Jeanne Sergeant
Though the pandemic is now endemic, one of its many lasting effects is even worse staffing issues in healthcare than before.
Add to this combative patients, long hours, changing shifts, emotionally stressful work and plenty of physical challenges and it’s little surprise that nurses face high risk for burnout.
“It’s bad right now,” said Josh Lynch, registered nurse on an acute care floor for Rochester Regional Health. “As terrible as it is to say, you have to become somewhat emotionally detached and pack certain things away and deal with them later.”
He said that some nurses he knows wor kout at the gym, meditate or, as he does, spend time with his kids and binge watch TV shows when not at work.
“I want to sit, zone out and not think about anything,” he said. “I want to be in a different moment.”
Unfortunately, he knows some nurses who turn to substance use to cope.
“If you don’t take care of yourself, this job will eat you alive,” Lynch said. “The things we see and go through and are expected of us will tear you apart if you let it.”
“If you don’t take care of yourself, this job will eat you alive. The things we see and go through and are expected of us will tear you apart if you let it.”
It’s also beneficial for nurses to adjust their perspective. For example, remaining a perfectionist can make each day a drag.
“Some things we found recently is thinking about respecting people where they are and trying not to be a perfectionist,” Blaakman said. “We may feel like we need to have all the answers but patients need to make choices. You can’t fix other people but you can help them reach their own goals.”
2
T
Saturday, July 13th 10:00 am to 6:00 pm Sunday, July 14th 10:00 am to 5:00 pm







Susan Blaakman, founding member of University of Rochester School of Nursing’s Wellness Task Force and director of the psychiatric mental health nurse practitioner program, recommends that nurses practice self-care to combat the stressors inherent to the work.
This includes “enough sleep, good nutrition, and setting boundaries in place,” Blaakman said. “Seek help when you need it. When you have intense feelings, don’t push them away but embrace them and understand what’s happening in your body physiologically.”
Blaakman noted that mindfulness can help, as it can help slow breathing and assist in noticing what’s happening around the person. Gratitude can also help reduce burnout, such as feeling thankful to help patients during their most vulnerable moments.

Greg Hoffman-Fragale, doctor of nurse practitioner interim nursing officer at Finger Lakes Health, takes a week off for a vacation every quarter as well as a mental health day. He also periodically has massage therapy.
“Self-care is helpful because if you don’t take care of yourself, you can’t take care of your employees, your nurses or your patients,” Hoffman-Fragale said. “Self-care is important because often as a leader we are selfless and lose sight or focus on our own needs and put the needs of others first. We have to remember that we’re human beings. Because we’re leaders doesn’t mean we don't require food, rest leisure time with family and pets.”
Hoffman-Fragale added that professional boundaries also help mitigate stress, such as refusing to stay late. Otherwise, “you get short with your loved ones and curt with staff,” he said. “You can get fatigued, cranky and sick.”

Page 16 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024 56th Annual July 13 & 14 2024 PRESENTED BY: Rochester's premier summer arts festival is right around the corner! H a n d m a d e F i n e A r t s a n d C r a f t s
h e 1 4 t h A n n u a l E m e r g i n g A r t i s t E x p o F o o d T r u c k s a n d a B e e r G a r d e n L i v e M u s i c o n M u l t i p l e S t a g e s T h e 1 0 t h A n n u a l F a i r y H o u s e S h o w c a s e
T
n d A n n u a l C o r n H o l e T o u r n a m e n t
h
C o r n H i l l 5 K o n S u n d a y F r e e A d m i s s i o n a n d S h u t t l e B u s S e r v i c e www.cornhillartsfestival.com SPECIAL THANKS TO OUR 2024 SPONSORS
e
Mark Your Calendar! Nursing
Susan Blaakman, is a founding member of University of Rochester School of Nursing’s Wellness Task Force and director of the psychiatric mental health nurse practitioner program.
SmartBites
By Anne Palumbo
The skinny on healthy eating
Cheeky Rhubarb Delivers the Goods
Some vegetables need to be tamed, and feisty rhubarb is one of them. It’s barely edible raw, it looks like celery, its leaves are poisonous, it’s beyond tart, and it thinks it’s a fruit!
With such a rebellious personality, is it any wonder rhubarb gets short shrift at the market?
My advice? Give this imposter fruit a chance!
All it takes is a good recipe and a little sugar to open your eyes to rhubarb’s delicious, nutritious side.
Rhubarb, like most fruits and vegetables, benefits heart health in several ways. Its fiber helps lower cholesterol; its diverse antioxidants keep inflammation at bay; and its potassium helps lower blood pressure. Indeed, a trifecta of nutrients to help keep our tickers in tiptop shape.

In addition, rhubarb teems with vitamin K, an essential vitamin for blood clotting, bone building and heart health. Recent studies from the Perth Longitudinal Study of Aging Women revealed that women who ate more vitamin K-rich foods significantly reduced their risk of bone fractures later in life. What’s more, a growing number of studies have demonstrated that vitamin K may play an important role in slowing, and even preventing, the progression of Alzheimer’s disease.
Rhubarb’s fiber benefits our
bodies in ways above and beyond our bowels. Yes, it promotes regularity and reduces the risk of colon cancer, but it also improves digestion, helps to regulate blood sugar levels, and facilitates weight loss or maintenance because it’s so filling.
On the downside, rhubarb does contain oxalates, which are naturally occurring compounds in plants. Because oxalates can bind to calcium—and to a lesser extent—other minerals in the stomach and intestines, they can reduce the absorption of these beneficial nutrients, as well as increase the risk of kidney stones in some people. What to do? Cook rhubarb to reduce oxalate content; eat in moderation; drink plenty of water to dilute oxalates in urine; and consult your doctor if you have kidney issues.

Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
Helpful Tips
Choose firm, crisp stalks with shiny skin. Remove toxic leaves (if present), then wrap rhubarb in plastic wrap and store in fridge for up to a week. Don’t cut the stalks until you are ready to use or the rhubarb will dry out.

Adapted from dishnthekitchen.com 12 standard muffins
FOR THE STREUSEL TOPPING
3 teaspoons all-purpose flour
2 tablespoons sugar
1 tablespoon brown sugar, packed
1 tablespoon cold butter, cut into pieces pinch salt ¼ cup walnuts
FOR THE MUFFINS
¾ cup + 1 tablespoon white
1. For the streusel topping: Place flour, sugars, butter, and salt into the small bowl of a food processor. Pulse until the mixture resembles coarse crumbs. Add walnuts and pulse until the walnuts are desired size. Set aside.
2. For the muffins: Preheat oven to 425°F and line a standard muffin tin with paper liners.
3. Mix the flours, baking powder, and salt together in a small bowl. Set aside. In the bowl of a stand mixer, cream the butter and sugar together for 3 minutes. Add the eggs one at a time, then add the milk.
whole-wheat flour
½ cup all-purpose flour
1½ teaspoons baking powder
½ teaspoon salt
1 cup sugar
6 tablespoons butter, softened
2 eggs
½ cup 2% milk
½ cup walnuts, chopped
1 cup strawberries, chopped 1 cup rhubarb, chopped
4. Gently add the dry mixture to the bowl until it comes together. Do not overmix.
Fold in the walnuts, strawberries, and rhubarb.
5. Evenly distribute the batter in the muffin cups. Top each muffin with some streusel topping.
6. Bake at 425°F for 15 minutes; then check for doneness with a toothpick. If it doesn’t come out clean, bake a few minutes more until toothpick looks clean. Cool in muffin tin for 10 minutes, then remove and cool muffins on wire rack.

May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 17
STRAWBERRY-RHUBARB MUFFINS
Not a Subscriber? NAME ADDRESS CITY/TOWN STATE ZIP 1 YEAR (12 ISSUES) $30.00 $40.00 2 YEARS (24 ISSUES) Clip and Mail with payment to: In Good Health P.O. Box 525, Victor, NY 14564 Subscribe and get In Good Health: Rochester’s Healthcare Newspaper right to your home or office! ELDER JUSTICE COMMITTEE IS GOING TO THE THEATRE And YOU ARE INVITED SAVE THE DATE EVENT WILL BE HELD AT 240 East Ave. Rochester, NY Ticket Info Online At The Little or At The Door DOCUMNETARY “FIRE THROUGH DRY GRASS” & Discussion with The Filmmakers & Advocates THURSDAY JUNE 13, 2024 MOVIE STARTS AT 1:15 PM Questions Contact Elder Justice Committee of Metro Justice (585-397-3537 (ELDR) ejcontact@elderjusticecommittee.com Poests turned filmmakers document starting their advocacy during COVID by filming their lives in a nursing home. As they faced institutional neglect, they refuse to be abused, confined, and erased. The film shows people with disabilities, nursing home residents and others can continue what started duing COVID to advocate for a life of dignity and purpose, free from neglect and abuse.

AI Detects Sight-robbing Condition in Babies
For premature infants, this early detection can save their sight
By Deborah Jeanne Sergeant
Premature babies and their families face myriad challenges as they navigate a world for which they’re not yet ready.
One area of development that could use medical intervention is vision. An ophthalmologist typically examines the eyes of premature babies in the neonatal intensive care unit to look for issues such as retinopathy of prematurity (ROP).
“It is important to examine the retinas of premature babies to protect their vision and prevent abnormal retinal blood vessel development, which can lead to reduced vision and blindness,” said physician Olachi J. Mezu-Ndubuisi, an associate professor of pediatrics and ophthalmology at University of Rochester.
Preemies have immature retinas that lack all of the blood vessels fullterm babies have. Ideally, these blood vessels develop as they should so they can nourish the photoreceptors that carry visual information to the
brain. When these blood vessels do not develop properly, it can cause blindness. Fortunately, if discovered early, this problem can be corrected with laser surgery or injections. But detection is key. Artificial intelligence has provided tools to help providers detect at-risk babies more accurately and efficiently.
“Artificial intelligence in ROP would involve using algorithms or codes to teach a computer to quickly differentiate between abnormal and normal retinas,” Mezu-Ndubuisi explained. “AI could be a very useful screening tool for ROP. Advances in perinatal and neonatal care have led to increased survival of extremely premature infants at earlier gestational ages. Therefore, ROP remains the leading cause of preventable childhood blindness worldwide despite advances in neonatal care.”
AI can help ease the burden of ROP exams on the few available ophthalmologists, especially in rural
Angry? Venting to Others Probably Won't Help You
Grumbling and grousing to others isn't an effective way of reducing rage, a new review shows.
Folks who vent about a source of anger might feel better in the moment, but that won't diminish their ire, researchers found.
Instead, stress-reducing techniques like deep breathing, mindfulness, meditation and yoga are much more effective alternatives than griping, results show.
“I think it's really important to bust the myth that if you're angry you should blow off steam - get it off your chest,” said senior researcher Brad Bushman, a professor of com-
munication at Ohio State University. “Venting anger might sound like a good idea, but there's not a shred of scientific evidence to support catharsis theory.”
For this analysis, researchers reviewed over 150 studies involving more than 10,000 participants. They discovered that turning down the heat through stress-relieving activities is better at reducing anger because it lowers a person's fight-or-flight response.
On the other hand, venting about anger actually increased a person's agitation, as did physical activities like jogging.
“To reduce anger, it is better to
areas.
Mezu-Ndubuisi added that AI exams are more objective than the human assessment of how abnormal blood vessels look.
“This assessment can vary between different observers,” she added. “Significant differences in diagnosis can lead to delays in treatment of ROP which can pose a threat to vision.
“Artificial intelligence is very promising but needs to be optimized to more reliably use information about the individual baby’s condition or risk factors for ROP to accurately guide diagnosis, treatment and monitoring of infants with ROP.”
Matt Gearinger, pediatric ophthalmologist at Flaum Eye Institute, does rounds at URMC’s NICU to examine babies’ eyes. He said that AI exams can help identify which babies are at risk and need treatment, which “can cut the workload extensively” for rural areas not well served by ophthalmology.
“They don’t have enough people who can do the eye exams,” he said. “Babies born at 30 weeks or earlier or who have low birth weight get screened automatically.”
Low birth weight is 1,500 grams (or about 3.3 pounds) or less.
Physician Luca Zatreanu, chair of ophthalmology at Rochester Regional Health, said that he also examines babies who have experienced an unstable clinical course, like bleeding

Physician Luca Zatreanu, chairman of ophthalmology at Rochester Regional Health: “There are approximately 500 infants annually in the US that can lose vision from retinopathy.” he says. “It’s very treatable, but you have to screen and detect it.”
in the brain, supplemental oxygen in the first week of life and a long NICU stay.
“There are approximately 500 infants annually in the US that can lose vision from retinopathy,” he said. “It’s very treatable, but you have to screen and detect it.”
Currently, AI is capable of identifying with 100% accuracy the most severe cases of ROP and 80% accuracy for those later deemed “more than mild.”
“That’s huge,” Zatreanu said. “It removes humans from the equation from the screening except form providing the images. Someone still needs to take pictures of the babies’ eyes in the NICU and feed them into the platform. It would automatically say ROP is present. You can funnel these babies to the appropriate provider.
“It’s a challenge. We definitely need people to help with screenings with preemies. It’s not easy to find these kinds of doctors so having this as an opportunity in the near future would be huge for us. If we had portable cameras and trained personnel on how to take the photos and upload the photos, that would be a huge help.”

engage in activities that decrease arousal levels,” Bushman said in a university news release. “Despite what popular wisdom may suggest,
even going for a run is not an effective strategy because it increases arousal levels and ends up being counterproductive.”
Page 18 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024
Dangers of Polypharmacy
Taking
a lot of medications? You could experience higher health risks
By Deborah Jeanne Sergeant
People aged 60 to 64 take an average of 13 prescription medications, according to Georgetown’s Health Policy Institute.
That number rises to 20 by age 65.
But just taking five or more daily medications is what Jinjiao Wang, Ph.D., assistant professor of nursing at University of Rochester Medical Center, calls “polypharmacy.”
“Its danger is not because of the number, but the risk of potentially unnecessary or inappropriate medications that increases along with the number of medications one is taking,” Wang said.
Wang is co-editor-in-chief of the research journal JMIR Aging.
Unnecessary polypharmacy or inappropriate polypharmacy happens when a patient is prescribed a medication initially intended for a specific time period or for specific symptom but the patient is still taking it even though the issue it should address is no longer present.
“That this ‘legacy’ medication may no longer be needed or, even worse, causing side effects,” Wang said.
Some patients take medication to treat side effects caused from other

medication which providers may mistake as new symptoms.
Wang calls this phenomenon “prescribing cascade.”
This often happens with older adults who see multiple specialists. They may prescribe medication that the others don’t know about. Even with electronic medical records, if the patient sees providers associated with different health systems, that information may not be shared.
Taking unneeded medication costs patients and insurance companies money. It also takes out of the drug supply medication that someone else may need and in some cases struggle to find. Unnecessary polypharmacy also taxes the patient’s body as it must process yet more prescriptions.
It’s also taxing on the patient. Swallowing numerous pills daily can cause pill fatigue. It can become troublesome to take them at the right time and in the right fashion, such as before breakfast, with food or at bedtime. Taking medication incorrectly can hamper its ability to work correctly and with more medications comes more changes to make mistakes.
Swallowing numerous pills in-
Recommended Vaccines for Medicare Recipients
By Jim Miller
All recommended vaccines for adults, age 65 and older, should be covered by either Medicare Part B or Part D, but there are some coverage challenges you should be aware of.
Here’s a rundown of which vaccines are recommended by the Centers for Disease Control and Prevention (CDC) and how Medicare covers them.
• COVID-19: Even though COVID-19 is no longer a public health emergency, it can still cause severe illness, particularly in older adults. Because the COVID virus continues to mutate, new vaccines are being developed to keep pace, so the CDC recommends that all seniors stay up to date with the latest COVID vaccines, including booster shots.
All COVID-19 shots are covered
100% by Medicare Part B.
• Flu: Considered an annual vaccination, most people of all ages receive flu shots in the fall when flu season begins. The CDC recommends seniors, 65 and older, get a high-dose flu shot for extra protection beyond what a standard flu shot offers. The Fluzone High Dose Quadrivalent, FLUAD Quadrivalent and FluBlok Quadrivalent are your three options. Annual flu shots are covered under Medicare Part B.
• Pneumonia: These vaccines help protect against pneumococcal disease, which can cause pneumonia, meningitis and other infections. The CDC recommends everyone 65 and older get a pneumococcal vaccine. There are several different vaccine options available, so talk to your doctor or pharmacists to find out which
creases risk for drug interactions.
“A lot of drugs interact with other drugs,” said Sarah Phillips, supervision pharmacist at Clifton Springs Hospital. “One drug from one prescriber may interact with drugs from other prescribers. Older adults don’t metabolize drugs in the same way. The liver and kidney function is lower so drugs build up in their systems and have drug toxicity.”
Phillips said that polypharmacy can raise risk for side effects such as confusion, falls, loss of appetite, increased sedation and other contributors to hospitalization.
To reduce polypharmacy, Phillips recommends scheduling an annual medication review with the primary care provider or pharmacist. It can take an hour to go through the list. Phillips reminded that any over-thecounter medication, supplements and herbal preparations used should also be part of the conversation, as these can all interact with prescriptions.
“Once we have the full picture, we can analyze what you’re on,” Phillips said. “We look for indications, outcomes and interactions. We’re talking with the patient and understand what they’re taking, why
is best for you or visit the CDC’s Pneumococcal Vaccination webpage at CDC.gov/vaccines/vpd/pneumo/public/index.html.
Medicare Part B covers both single dose and two-dose pneumococcal shots once in your lifetime.
• Shingles: Caused by the same virus that causes chicken pox, shingles is a painful, blistering skin rash that affects more than 1 million Americans every year. All people over age 50 are recommended to get the two-dose Shingrix vaccine, which is given two to six months apart, even if you previously received Zostavax. In 2020, Shingrix replaced Zostavax, which is no longer available in the U.S.
All Medicare Part D prescription drug plans cover shingles vaccinations, but coverage amounts, and reimbursement rules vary depending on where the shot is given. Check your plan.
• Tdap: Tetanus, diphtheria, and pertussis (whooping cough) are diseases caused by bacteria that can lead to serious illness and death. Therefore, a one-time dose of the Tdap

they’re taking it and how it’s making them feel.”
A meeting such as this can help providers identify prescriptions that are no longer needed or suggest trying a different medication that could reduce side effects.
“Find a pharmacy you like and stay with that one pharmacy,” Phillips added. “If you use multiple pharmacies, we’re all segmented. If you use one, they see your whole drug list and can see if there are any interactions. But it doesn’t remove the need for that medication management session annually.”
Wang wants patients to know more about their medications, including their names, dosage, desired effects and potential side effects.
“Let your providers know when you have symptom changes that may be related to side effects of certain medications; do not be afraid to have an open discussion with your providers, if you have questions or concerns about your medications or simply wonder if some of your medications are still needed,” she said. “One hint, if you don’t know what a medication does for you — that is a good place to start this conversation with your providers.
However, never stop taking a medication without consulting your provider.”
vaccine is recommended to all adults. If you’ve already had a Tdap shot, you should get a tetanus-diphtheria (Td) booster shot every 10 years.
All Medicare Part D plans cover these vaccinations.
• RSV: Respiratory syncytial virus (RSV) can lead to pneumonia or bronchiolitis and can worsen other chronic conditions common among older adults, such as asthma and chronic obstructive pulmonary disease (COPD). The CDC recommends all adults, age 60 and older, talk to their doctor about getting one of the RSV vaccines (either Arexvy or Abrysvo), usually in the fall and winter months when the virus is most prevalent.
• Other vaccinations There are other vaccines you may need depending on your health, lifestyle or travel plans. To help you get a handle on which ones are appropriate for you, take the CDC’s What Vaccines Do You Need? quiz at www2.cdc.gov/nip/adultimmsched. Also, talk to your doctor during your next visit about what vaccinations you should get.
May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 19
Golden Years
Jinjiao Wang, Ph.D., is assistant professor of nursing at University of Rochester Medical Center.

Untreated Hearing Loss Further Linked to Dementia
A large Danish study confirms growing body of evidence
By Deborah Jeanne Sergeant
Arecently released Danish study of 570,000 people over 14 years identified untreated hearing loss as increasing the risk for dementia compared with people with no hearing loss or those with treated hearing loss.
The study doesn’t surprise Carolynne Pouliot, doctor of audiology and owner of Hearing Aide Works Audiology in Penfield, who referenced a 2011 study that stated even a mild untreated hearing loss increases the risk of dementia by 200%; moderate hearing loss and severe hearing loss by 500%.
“People may still ‘get by’ with their hearing loss and be at risk,” Pouliot said. “None of the participants had dementia when they started. At the end, that’s what they found.”
She referenced several other studies that indicate similar results, including a Duke University study by Murali Doraiswamy, which indicated that even people diagnosed with dementia who also have hearing loss find that treating their hearing
loss is twice as effective as medication prescribed to slow cognitive decline.
“Walking around with untreated hearing loss has so many risks,” Pouliot said. “The best thing you can do to prevent cognitive decline or to slow it if you’re diagnosed is to treat any hearing loss present. The hidden benefits of treating hearing loss show up in research again and again.”
Introducing hearing aids at that point can also make their use more effective so that the brain becomes accustomed to their input.
For those who would develop cognitive decline, earlier adoption of hearing aids to treat hearing issues can delay onset of dementia by seven years.
“You can buy yourself seven years by treating hearing loss,” said Matthew S. MacDonald, doctor of audiology and owner of MacDonald Audiology in Rochester.
Hearing loss tends to isolate people as they withdraw from social situations because they cannot participate in conversation and understand
what’s going on around them the way they used to. But MacDonald said that it’s not only the lack of socialization.
“An interesting study done at University of Colorado showed that the brain with hearing loss actually had changed as a result of the hearing loss,” MacDonald said. “Parts of the auditory cortex meant to be used for hearing were being used for pattern recognition. They showed that when those individuals treated their hearing loss, within six months, those people’s brains reorganized themselves to their original designation.
“If you have problems with your hearing, you’ll use other modalities to make up for it, like lip reading. We don’t want this cross-modal brain use. People need to use all of their cognitive resources. Hearing loss can drain your cognitive resources. If you have to struggle to pay attention to what someone is saying, it doesn’t leave resources left for memory and cognitive processing.”
MacDonald wants more people to receive a baseline hearing exam, even before the TV volume creeps up and they feel “everyone mumbles.” Most people who experience hearing loss over time are not aware of its encroachment. But those who receive an exam and are told that they hear just fine can know later if their hearing has changed.


Sarah Hayes, doctor of audiology, Ph.D. and assistant professor of otolaryngology at URMC, said that fewer than 30% of people with hearing loss who could benefit from using hearing aids obtain and use them.
“People with hearing loss typically wait an average of seven years before seeking help,” she added. “As an audiologist, I want people to know that not only is it important to protect your hearing when you are exposed to loud noise, whether you are attending a loud music concert or using your lawnmower, but if you suspect that there has been a change


in your hearing or you’ve noticed that you are struggling to hear what others are saying to you, make sure that you get your hearing tested. Identifying and managing hearing loss is very important for our brain health.”
She hopes that additional study will bring a better understanding of the link between untreated hearing loss and cognitive decline. Her lab is studying how hearing loss alters the brain’s regions that control memory, learning and executive function, all of which dementia negatively impacts.
Joe Kozelsky, retired audiologist, honorary board member of the Hearing Loss Association of America Rochester Chapter in Fairport and author of the book “Hearing, Hearing Loss and Hearing Aids,” thinks that the link between untreated hearing loss and increased risk for dementia should prompt people to take care of their hearing loss. But in addition, improving quality of life should be reason enough.
“Start with a bonafide professional rather than an over-the-counter aid or responding to ads on TV,” Kozelsky said.
Muffled hearing could have other reasons such as a build-up of wax or other problem. Nonetheless, Kozelsky sees merit in treating hearing loss for the reasons the growing body of evidence seems to indicate.
“You want to do what you can to avoid the social isolation of hearing loss,” he said. “That’s harmful and does lead to sensory deprivation and withdrawal.”
Page 20 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024 Golden Years
Carolynne Pouliot is a doctor of audiology and the owner of Hearing Aide Works Audiology in Penfield.
Matthew S. MacDonald is a doctor of audiology and owner of MacDonald Audiology in Rochester.
Highest Prices Paid We BUY TEST STRIPS We will pick up and pay on the spot We pick up 6 days a week. 11am to 6:30pm One Touch Ultra & Freestyle Lite. All Brands Considered. Up to $50. (585)-284-3455
5
Stroke prevention is crucial because strokes can cause significant disability — and death.
Sometimes referred to as a brain attack, stroke occurs when the blood vessel that carries oxygen and nutrients to the brain is either blocked by a clot, bursts or ruptures.
When that happens, part of the brain doesn’t receive the blood and oxygen it needs, so brain cells die.
One in six deaths from cardiovascular diseases are due to stroke and every 40 seconds someone in the United States has a stroke, according to the Centers for Disease and Prevention.
“Stroke prevention is important because the vast majority of strokes are preventable through control of common risk factors and lifestyle choices,” said Adam Kelly, a physician specializing in neurology at UR Medicine Comprehensive Stroke Center.
These include controlling blood pressure, getting regular physical activity, taking in a healthy diet and quitting smoking. Following these recommendations plus some other healthy choices can help people avoid about 90% of strokes.
By managing risk factors such as high blood pressure, diabetes and high cholesterol individuals can reduce their chances of experiencing a stroke.
Kelly explains five aspects about strokes.
1.Know the Symptoms
Common symptoms of a stroke include sudden numbness or weakness in the face, arm or legs — especially on one side of the body. In
Things You Need to Know About Stroke
By Ernst Lamothe Jr

addition, there is confusion, trouble speaking or understanding speech, vision problems, dizziness, loss of balance or coordination and severe headaches.
Strokes are often compared to heart attacks due to their potential for serious and life-threatening consequences. Understanding causes of strokes is slightly complicated considering how it differs by gender, age and ethnicity.
“Stroke symptoms usually come on fast, often without a warning and that is one way we distinguish stroke from other neurologic conditions,” said Kelly. “The specific symptoms we commonly see include weakness or numbness of half of the body, drooping of one side of the face, sudden change in vision, slurring of
Six in 10 Stroke Survivors Will Struggle With Depression Years Later
Six out of every 10 stroke survivors wind up struggling with depression later in their lives, a new study says.
That compares to the 22% depression rate of the general population, results show.
Further, nine of 10 stroke-related depression cases occur within five years of surviving a stroke, researchers found.
“Depression is common in stroke survivors but our research shows it persists for much longer than previously thought,” researcher Yanzhong Wang, a professor of statistics in population health at King's College London, said in a news release.
Biochemical changes in the brain caused by stroke injury can contribute to depression by interfering with a person's ability to feel positive emotions, according to the American Stroke Association.
For the study, researchers reviewed the cases of 6,600 stroke survivors whose data appears in a South London stroke registry.
Results showed that severe depression tended to occur earlier after stroke, lasted longer than expected, and was quicker to recur than cases of mild depression.
Depression among stroke survivors can affect their mobility, hampering simple tasks like walking

speech or trouble getting words out or sudden loss of balance.”
2.Stroke conditions and confusion
Having a stroke means that the blood supply to a part of the brain is interrupted or reduced, leading to damage to brain cells. This can result in various neurological deficits depending on the location and severity of the stroke.
“The most common condition that stroke gets compared to is heart attack or myocardial infarction,” said Kelly. “Both conditions share common risk factors like high blood pressure, high cholesterol, diabetes and smoking. Both can come on quickly with little warning. In both cases, the most common cause is blockage of blood flow to part of the affected organ, which in stroke is the brain and in heart attack is the heart. Finally, in both cases, our initial treatment is usually attempting to reopen blocked or narrowed blood vessels using clot-dissolving medications or surgical procedures.”
3.Time
is of essence
Some misconceptions about stroke include the belief that it only affects the elderly. In fact, it occurs at various ages. Another misconception is that strokes always cause paralysis. However, the symptoms and outcomes vary widely.
“A major misconception we see is that stroke symptoms can wait to be checked out. Stroke symptoms are a medical emergency and one of the most time-sensitive medical conditions we face,” said Kelly. “We have options, either medical or surgical,
and holding objects, Wang said. It also can increase their overall risk of death.
“Quality of life is important for stroke survivors as there is evidence depressed survivors have a reduced survival rate,” researcher Lu Liu, a doctoral candidate at King's College London, said in a news release.
“There are many reasons why this could be, including disruptions to the survivor's social life, reduced physical ability and inflammatory disorders observed in depressed patients,” Liu added.
Doctors need to pay particular attention to stroke survivors who have depression that lasts longer than one year, “because of the high risks of experiencing persistent depression,” Liu said.
'Stroke prevention is important because the vast majority of strokes are preventable through control of common risk factors and lifestyle choices.'
that can reverse or minimize the effects of stroke. They are best delivered in the first few minutes to hours after a stroke occurs. Too often we see people who are having a stroke decide to go to bed and wait to get checked out the following morning if their symptoms persist. Unfortunately, by that point, many of our treatments may no longer be possible. We often use a saying that ‘time is brain,’ meaning that the longer stroke symptoms go on, the more brain tissue is at risk of injury.”
4.Family history
Family history can play a role in stroke risk as genetics can influence certain risk factors such as high blood pressure and heart disease.
“We do see a familial or hereditary tendency toward stroke in some patients,” said Kelly. “This is almost never due to inheritance of a specific gene from one’s parents, but more likely due to a collection of genes that makes a family more susceptible to stroke, similar to how we see some families more likely to suffer from cancer and diabetes.”
5.Vital post stroke information
After a stroke, patients can experience a variety of symptoms including weakness, sensory changes, vision loss or other changes, speech or language dysfunction or other neurologic problems. The nature of the symptoms will depend on the size of the stroke and the particular area of the brain that was affected.
“Stroke patients are also more prone to other post-stroke issues including fatigue, depression, memory problems and anxiety. Fortunately, these can often improve considerably with time and participation in activities like physical, occupational and speech therapy,” said Kelly. “Patients and families should feel empowered to discuss any possible post-stroke concerns with their primary care provider, neurologist or other healthcare team members.”
May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 21
Adam Kelly is a physician specializing in neurology at UR Medicine Comprehensive Stroke Center.
Shortage of Primary Care Doctors Could Bring Crowded ERs: Study
Americans living in areas where primary care doctors and nurse practitioners are in short supply face a greater risk for emergency surgeries and complications, new research shows.
They're also more likely to wind up back in the hospital after they've left it. That's because serious health issues don't get addressed until they become emergencies, said lead study author Dr. Sara Schaefer, a resident in the University of Michigan's Department of Surgery.
"The role of the primary care provider in identifying a potential issue, and referring a patient for diagnostic imaging and surgery, can make a major difference in addressing an urgent problem before it becomes an emergency," she explained in a university news release.
For the new study, her team looked at data for Medicare patients in areas where the federal government has identified a shortage of primary care providers.
Patients had operations for three conditions where timing is critical: colectomy to remove a cancer from the colon; hernia repair; and repair of aneurysms in the the body's largest blood vessel, the aorta.
Nearly 38% of those in areas with more severe shortages required emergency surgery, compared with 30% of those in areas with the least severe shortages, the study found.
They also had a higher risk for serious complications (15% versus about 12%), and hospital readmission (nearly 16% vs. 13.5%).

CALENDAR HEALTH EVENTS of
May 5
EYS event to raise funds for cancer patients
EYS Embrace Your Sisters, a Canandaigua-based nonprofit whose mission is to provide emergency financial assistance for people with breast cancer, is organizing its 17th annual Tea at Two Fashion Show.
According to EYS, this “will be a truly inspirational afternoon” and is the largest fundraising event that Embrace Your Sisters holds. Fashion show models will include breast cancer survivors who will be on the runway showcasing the latest trends.
The event will start at 2 p.m., May 5, at Casa Larga Vineyards & Winery, 2287 Turk Hill Road in Fairport. Tickets are $50 and are available at the organization’s website, www. embraceyoursisters.org.
May 5
Hearing loss group schedules programs
The Hearing Loss Association of America – Rochester Chapter’s feature presentation will highlight officials at Lifespan of Greater Rochester who will explain some of the
more than 30 services it offers for older adults and caregivers — from transportation, to choosing a Medicare plan, to health and wellness programs. The event will take place at noon on May 7 at St Paul’s Episcopal Church Parish Hall, 25 Westminster Road at East Avenue. People may also participate by Zoom (To obtain Zoom link, pre-register at the chapter website hearinglossrochester.org).
For other HLAA programs taking place in May, visit hearinglossrochester.org.
May 15
NCADD-RA presents annual luncheon
The National Council on Alcoholism and Drug Dependence-Rochester Area’s (NCADD-RA) 78th Annual Luncheon will take place from 11:30 a.m. to 2 p.m. on Wednesday, May 15 at the DoubleTree by Hilton in Rochester. Keynote speaker Stephen L. Dewey will present “Understanding the Science of Substance Use Disorder.” Dewey received his Ph.D. from the University of Iowa and completed his postdoctoral fellowship in the neurology department at Stony Brook University. During his 23-year tenure at Brookhaven
National Laboratory, he conducted research on the effects of addictive drugs on the human brain. Dewey has published more than 250 peer-reviewed scientific research articles, book chapters, and abstracts. For more information or to register, contact Elaine Alvarado at ealvarado@depaul.org or call 585-719-3481. You may also visit ncadd-ra.org/ events-trainings/ncadd-ra-annual-luncheon/ to register online.
July 28
Golf tournament to benefit Notre Dame Learning
Center
The Notre Dame Learning Center will holding its annual golf tournament on July 28 at Webster Golf Club, 440 Salt Road, Webster. The tournament begins at 1:30 p.m. with a shotgun start. Golfers will enjoy playing 18 holes of golf (cart included) in a four-person scramble—a guarantee of fun. Awards will be announced at the dinner that follows the conclusion of the round.
All proceeds from the day are used to support the work of the center. With its main campus at the Charles Settlement House, NDLC provides free tutoring to students in grades 1-9 whose families may not otherwise be able to afford such services to support or augment their children’s education.
For more information on being a sponsor or participating in the tournment, contact the Notre Dame Learning Center at 585-254-5110 or online at ndlcenter.org/golf-2024 .

• Rochester Presbyterian Home’s Memory Care Residences offer a different (better!) way of living for people with memory impairment.
• We are not a facility. We are a family.
• Live in a home in a neighborhood with people who truly know you.
• Private bedrooms and bathrooms with a spacious kitchen and living area.
• Beautifully manicured outdoor courtyard space.
• Scheduled social events, outings and spontaneous activities that engage mind, body and soul.
• Variety of freshly prepared meals made on-site to suit every palate.
• Personal laundry service on-site.
• Enhanced services and personal care assistance available.


Page 22 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024
Li v e in a Home ... No t a Facili t Creekstone FAIRPORT Cottage Grove NORTH CHILI 20 Crossing Creek Drive Fairport, NY 14450 585.223.0160 creekstonerochester.org 48 Cottage Grove Circle North Chili, NY 14514 585.594.8720 cottagegroverochester.org
CAN be different!
Memory Care
Visit
and call 585-235-9100 ext. 126
Memory Care Residences in Monroe County.
www.rph.org
to learn more about our
 By Jim Miller
By Jim Miller
Choosing a Senior Community That Offers All Levels of Care
Dear Savvy Senior,
Can you help me identify some good senior living communities that offers all levels of housing and care from independent living to nursing home care? I am in my late 70s and know I need to downsize from my current house, but I want my next move to be my last.
One Move Mary
Dear Mary,
If you want your next move to be your last, an all-inclusive retirement community — also known as a continuing-care retirement community (or CCRC) — is a great option to consider.
Here’s what you should know, along with some tips to help you locate one.
What are CCRCs?
CCRCs are different from other types of senior housing because they provide all levels of housing, services and care in one convenient location.
While the appearance and services of CCRCs can vary greatly, most provide apartments or sometimes single-family homes for active independent seniors. In addition, they also offer onsite assisted living for seniors who require help with basic living tasks like bathing, dressing or going to the bathroom, and nursing home care for residents when their health declines.
CCRCs also provide a variety of resort-style amenities and services that include community dining halls, exercise facilities, housekeeping and transportation, as well as many social and recreational activities.
But be aware that all these services come at a hefty price. Most communities have entry fees that range from less the $100,000 to more than $1 million, plus ongoing monthly fees that generally range from $2,000 to $5,000 for singles ($3,000 to $6,000 for couples) depending on the facility, services and the contract option you choose.
With more than 2,000 CCRCs in operation throughout the U.S, finding a facility that fits your lifestyle, needs and budget will require some legwork. Here are some steps that can help you proceed.
• Make a list: To find CCRCs in the area you want to live go to “MyLifeSite.net” and “Caring.com,” which provide online lists. Once you’ve located a few, call them to find out if they have any vacancies,
what they charge and if they provide the types of services you want.
• Take a tour: Many CCRCs encourage potential residents to stay overnight and have a few meals in their dining hall. During your visit, notice the upkeep of the facility and talk to the current residents to see how they like living there. Also, check out the assisted living and nursing facilities, and find out how decisions are made to move residents from one level of care to another.
• Do some research: While on your tour, find out who owns the CCRC and get a copy of their most recently audited financial statement and review it. Also find out their occupancy rate. Unless it’s a newer community filling up, occupancy below 80 percent can be a red flag that the facility is having financial or management problems.
To investigate the CCRC’s longterm care services call your state long-term care ombudsman (see “LTCombudsman.org” — type “New York” in the search menu) who can tell you if the assisted living and nursing care services had any complaints or problems. You can also use Medicare’s nursing home compare tool at “Medicare.gov/care-compare.”
• Understand the contract and fees: Most CCRCs offer three types of contracts: life-care, or type A contracts, which have the highest entry fee but covers all levels of long-term care as needed; type B, or modified contracts that have lower entry fees but limits long-term care services in the initial fee; and type C, or fee-forservice contracts, which offer the lowest entrance fees but requires you to pay extra for long-term care if you need it.
You also need to find out what yearly price increases you can expect? How much of your entry fee is refundable to you if you move or die? And what happens if you outlive your financial resources?
To help you sort through all this, consult with your financial adviser or lawyer before committing.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.




May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 23
At St. Ann’s, our goal is to get you healthy and home as soon as possible following surgery or a cardiac event. In fact, our average length of stay is 40% shorter than the national average. That means you’ll be back doing the things you enjoy before you know it. Preplan your stay. Call (585)697-6565 or visit stannscommunity.com. The best part of rehab is when it’s over. And ours is over 40% sooner. 1500 Portland Ave. Rochester, NY 14621 InGoodHealth4.7x6.6.indd 1 11/5/18 1:26 PM P. 2 GVHEALTHNEWS.COM MARCH 2024 • ISSUE 223 NEW ADDICTIONINTERNETSPECTRUM: WHERE ARE YOU ON THE SCALE? NONPROFIT USES FITNESS AND EXERCISE TO FIGHT ADDICTION When the Big Boss is a Nurse Dan Ireland has tracked a path from bedside nursing to C-level hospital leadership. He is now the president of three Rochester Regional Health hospitals: United Memorial Medical Center, Newark-Wayne Community and Clifton Springs. Jonathan Westfall is the executive director at ROCovery Fitness, a community recovery outreach center. Rochester Region's Healthcare Newspaper

Ask St. Ann’s

Transitional Care: The Best Place to Heal
By Veena Madiraju
For some of us, a hospital stay is no big deal. We go in, we get treated, we go home.
As we age, however, the process may not be that simple. Our bodies don't recover as quickly, we need more help getting back to normal, and we're at greater risk of something happening that will send us back to the hospital.
To reduce that risk there's transitional care, which helps people make the transition from hospital to home. The goal is to get you back to your pre-hospital level of functioning and ensure you can return home and resume your daily activities safely.
At St. Ann's, we do that by providing short-term, 24-hour care and rehabilitation services that include physical, occupational and speech-language therapy.
Of course, everyone wants to go home ASAP. But a short stay in rehab will ensure you are fully recovered and able to do everything you did before you entered the hospital. In fact, at the Transitional Care Center at St. Ann's, the first thing we do when you arrive is make a plan to ensure your safe discharge—setting goals for improvement while you're with us and outlining what needs to happen once you go home.
Discharge planning is coordinated by an interdisciplinary team that includes doctors, nurses, therapists, social workers, dietitians and case managers. Together they will outline the steps, responsibilities and timelines for your care and discharge. In addition to your personalized rehab goals, this includes education and training for you and your support network on topics such as medication management, self-care techniques, fall prevention strategies, dietary guidelines, coping skills and follow-up care. It's all part of our goal of getting you back to full strength.
It's important to consider the impact of major surgery on our bodies, especially as we age. Our ability to do things we take for granted when
we're in good health — getting up from a sitting position, walking across a room, getting in and out of a car — can be seriously impaired. A fall or other setback can make matters worse, delaying your recovery.
You may have family or friends willing to look in on you, but they can't provide the round-the-clock skilled nursing care the staff at a transitional care center can. Simply put, it's the best place to heal. And you'll leave with sound, medically approved strategies to continue your recovery at home.
Although the hospital may make recommendations, the choice of where to go for rehab is entirely up to you. Look for someplace that offers the “three P's”:
• Personalized care. Therapy should be individualized to meet your specific needs.
• Partnership. Staff engage you and your family in decisions regarding your care.
• Proactive. The care team is able to foresee potential health problems and address them before they occur.
An important tip
Once your surgery is scheduled, do your homework. Look into the options for transitional care — contact the admissions office and find out what they offer. Once you've made a decision, pre-plan your stay. When you're ready to leave the hospital, it's one less thing to worry about. You'll be glad you did!

Veena Madiraju is assistant administrator of the Transitional Care Center at St. Ann's Community. She can be reached at Vmadiraju@ mystanns.com.
The Social Security Office Ask
From the Social Security District Office
How You Can Protect Yourself From Identity Thieves
Identity theft is when someone uses your personal information to impersonate you or steal from you. These crimes can impact your physical, mental and emotional health and lead to lost opportunities that are often hard to measure. Learning more about identity theft can help you keep your personal information safe.
Types of Identity Theft
There are two types of identity theft you should be aware of:
• Thieves stealing your data, physically or digitally, without contacting you directly.
• Thieves contacting you directly and convincing you to provide sensitive information.
In these instances, you may never know how the thief got your information.
How Identity Thieves Use Your Information
Identity thieves steal personal information like your name, address, credit card or bank account numbers, Social Security number (SSN), and medical insurance account numbers. They use this information to:
• Buy items with your credit cards or bank accounts.
• Obtain new credit cards or accounts in your name.
• Use your SSN to get a job.
• Open phone or utility accounts in your name.
• Steal your tax refund.
• Use your health insurance to obtain medical care.
• Pretend to be you if they are arrested.
How to Spot Identity Theft
To spot identity theft:
• Keep track of your mail for missing bills or other documents.
• Review your credit card and bank statements for unauthorized transactions.
Q & A
Q.: What is the estimated average Social Security payment that a person receives each month?
A.: The estimated average monthly Social Security benefit for a retired worker in 2024 is $1,907.00. The average monthly Social Security benefit for a worker with a disability in 2024 is $1,537.00.
Q.: My spouse doesn't have enough work credits to qualify for Social Security retirement benefits. Can they qual-
• Obtain and review your credit reports regularly to make sure they do not include accounts you have not opened.
Ways to Prevent Identity Theft
While no plan is perfect, taking the precautions below can help you better protect your personal information:
• Protect documents that have personal information.
• Ask questions before giving out your SSN.
• Protect your personal information online and on your phone by using a strong password and adding multi-factor authentication when offered.
• Safeguard your information on social networks.
What to Do if You Believe Someone Has Stolen Your Identity
• Report fraud to the company where it occurred.
• Contact a credit bureau to place a fraud alert on your credit report.
• File a complaint with the Federal Trade Commission at www. identitytheft.gov.
• File a police report.
For more information about how to protect your SSN from identity thieves, read our publication,"Identity Theft and Your Social Security Number" at www.ssa.gov/pubs/EN05-10064.pdf. Please report suspected Social Security imposter scams — and other Social Security fraud — on the Office of Inspector General’s website at www.oig.ssa.gov/report.
It’s important to protect yourself against identity theft because it can damage your credit status. Repairing this damage can cost you a great deal of time and money.
Please share this information with your family and friends.
ify on my record?
A.: A spouse receives one-half of the retired worker's full benefit unless the spouse begins collecting benefits before full retirement age. If the spouse begins collecting benefits before full retirement age, the amount of the spouse's benefit is reduced by a percentage based on the number of months before he or she reaches full retirement age. You can learn more by reading our online publication, "Retirement Benefits", at www.ssa.gov/pubs.
Page 24 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024
Health News
Roberts Wesleyan nursing school has new dean
Annemarie Dowling-Castronovo

Annemarie Dowling has recently been appointed as the new dean at Roberts Wesleyan University School of Nursing. She joins Roberts Wesleyan from Monmouth University in New Jersey, where she served as chairwoman of the nursing department, chief academic nursing officer and professor of nursing at the Marjorie K. Unterberg School of Nursing and Health Studies.
“Following an extensive national search, we’re very pleased to welcome Dr. Annemarie Dowling-Castronovo as the next dean for the school of nursing,” said Susanne Mohnkern, interim dean and graduate program director for the School of Nursing at Roberts Wesleyan University. “Dr. Dowling-Castronovo possesses the leadership qualities that will not only promote the mission of the school of nursing and the university but will also enhance educational experiences for students

in our program to pursue rewarding careers in essential health care roles.”
Dowling-Castronovo brings to her new role more than two decades of experience as a practitioner and a leader in academic settings. Board-certified in palliative and gerontological care, her background in health care includes a variety of nursing and clinical positions at hospitals and clinics in the New York City area, including Brooklyn Hospital Center, NYU Downtown Family Care Clinic, Staten Island University Hospital and Northwell Health.
Prior to her tenure at Monmouth University, Dowling-Castronovo held respective academic appointments and professorial roles as a certified nurse educator at several schools along the East Coast, including New York University, College of Staten Island (City University of New York) and Wagner College.
Dowling-Castronovo obtained her Associate in Applied Science and Bachelor of Science from the College of Staten Island, a master’s degree from New York University’s Division of Nursing and her Ph.D. from Rutgers, The State University of New Jersey. She will relocate from Staten Island to the Greater Rochester area this spring as she assumes the role of dean.
RRH recognized as one of the
best systems to work for
Rochester Regional Health announced its inclusion in Becker›s Healthcare Review›s prestigious list of the nation’s 150+ top places to work in healthcare | 2024.
This recognition honors the entire Rochester-based health system covering 13 counties from Genesee County to the northern tip of St. Lawrence County. According to officials, it is a testament to the organization’s unwavering commitment to fostering a supportive, inclusive, and rewarding work environment for its 20,000 team members.
“Being named one of the Best 150 Health Systems to Work for by Becker’s Healthcare Review is a tremendous honor for Rochester Regional Health,” said Richard “Chip” Davis, CEO of Rochester Regional Health. “This recognition underscores our dedication to prioritizing the well-being and professional growth of our employees. We believe that, by investing in our team, we ultimately enhance our ability to embrace our purpose of uplifting humanity through care for our community.”
Becker’s Healthcare Review, a leading source of cutting-edge business and legal information for
healthcare industry leaders, rigorously evaluates health systems across the nation based on workplace culture, employee benefits, professional development opportunities, and overall employee satisfaction. Organizations cannot pay to be featured on this list.
“At Rochester Regional Health, we recognize that our greatest asset is our people. We are deeply committed to fostering a workplace culture that values diversity, equity, and inclusion, where every individual feels respected, supported, and empowered to thrive,” said Charlene Wilson, executive vice president and chief people officer. “Through initiatives including regular merit-based raises, paid training programs, tuition assistance and comprehensive benefits packages, we strive to create opportunities for our team members to excel and advance in their careers.”
Canario joins Thompson Health Primary Care Team
Physician José Canario recently joined The Mary Clark Thompson Family Practice, an affiliate of F.F. Thompson Hospital in Canandaigua.
Board-certified in family medicine, Canario is a Geneva resident who graduated from the Eastern Virginia Medical School in Norfolk, Virginia, completing his family
Frank Guido couldn’t be happier he had a choice for treating his prostate cancer!

To hear more of Frank’s story and learn if CyberKnife is right for you, visit hoacny.com

Frank chose non-surgical CyberKnife® at HOA –offering 5 treatments instead of 35!
“The original diagnosis was to treat my prostate cancer with seven weeks of radiation, five days a week. I was kind of upset that I was never given the option of CyberKnife,” said Frank. “The precise radiation achieved by CyberKnife, far fewer treatments, and the personalized care I received from Dr. Chin and his team made my decision an easy one. Better, the treatment was a real success!”
May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 25

medicine residency at UR Medicine’s Highland Hospital. He later obtained a master’s in medical management from the University of Rochester’s Simon School of Business.
From 2016 through March of this year, Canario served as chief medical officer for the Penn Yanbased Finger Lakes Community Health. He previously treated patients at a family practice in Penn Yan and also served as medical director of both the Keuka College Health Center and the urgent care centers operated by FLH Medical, PC, in Geneva, Clifton Springs, and Seneca Falls.
Canario treats both children and adults at The Mary Clark Thompson Family Practice, which is located at the Sands Family YMCA, 351 North St. in Canandaigua.
Thompson included on top places to work
UR Medicine Thompson Health was recently named to the 2024 edition of the “150 Top Places to Work in Healthcare” list released by Becker’s Healthcare, a Chicago-based media platform serving healthcare decision-makers.
“This is the seventh time since 2015 we have been named to this national list, and we see it as a reflection of our commitment to supporting the professional growth and personal well-being of our
associates,” said Thompson Health President/CEO Michael F. Stapleton, Jr. “Especially at a time when there are workforce shortages within the healthcare industry, attracting and retaining top talent is fundamental to everything we do, so this validation of our efforts is something for which we are incredibly grateful.”
Each year, Becker’s Healthcare develops its “150 Top Places to Work in Healthcare” list based on nominations and editorial research. Organizations cannot pay for inclusion.
Cognivue names Paul W. Estes as president
Neuroscience technology

innovator Cognivue, Inc. recently announced that Paul W. Estes has been promoted to president, ushering in the company’s next stage of market evolution.
According to a company’s news release, he will guide the executive leadership team and oversee the company’s technology roadmap planning, new product expansion, partnership relations, sales and staffing.
His appointment comes after 15 years of serving in increasingly senior positions with Cognivue. Estes joined the company in 2009, helping conceive and develop Cognivue technology, then played integral roles in its de novo 510(k) clearance from the U.S. Food and Drug Administration and subsequent commercialization.

Most recently, he was Cognivue’s chief operating officer.
Estes succeeds Tom O’Neil, who left the company for a non-competitive leadership role in the healthcare infrastructure sector.
“Cognivue is headed into its next chapter of success, making it an even greater privilege to lead so many incredibly talented people throughout the company. Cognivue has several exciting developments ahead, such as the full-scale launch of our FDAcleared next-generation technologies and continued participation in the groundbreaking Bio-Hermes clinical study with the Global Alzheimer’s Platform,” said Estes.
Jewish Senior Life Acquires Home Care Services Agency
Jewish Senior Life has received

approval from the NYS Department of Health to acquire Embrace Care, LLC, a licensed home care services agency, enabling the organization to expand its continuum of services to include in-home nursing services. The new organization will be called Jewish Home of Rochester Licensed Home Care.
“We are committed to offering a full spectrum of services and programs to meet the diverse needs of older adults in our community,” said
Michael S. King, president and CEO at Jewish Senior Life. “We are now able to expand our continuum of services to include in-home nursing services, which are a particular area of need for growing numbers of older adults who prefer to live as independently as possible in their own homes.”
Jewish Senior Life currently provides non-medical, in-home support services through its living well companion care program. With this acquisition, the organization will offer a range of medical and non-medical in-home services, with a focus on geriatric post-acute and palliative home care services in Monroe, Orleans, Wayne, and Livingston counties.
Embrace Care, founded in 2016, provides nursing, home health and personal care services to clients in Monroe and Orleans counties.
“Our organizations share a deep commitment to providing the highest quality care and support that enables older adults to age in their place of choice. I have every confidence that Jewish Senior Life and our skilled and caring providers will continue to serve our clients with exceptional care,”m said David Georgiev, CEO of Embrace Care.
Jewish Senior Life and Embrace Care have entered into a management agreement to finalize details of the ownership transfer to Jewish Home of Rochester Licensed Home Care. Embrace Care’s direct care staff members will be invited to join Jewish Senior Life. Notifications were shared with employees and clients earlier this week.
“We are delighted to welcome new team members and clients to our Jewish Senior Life family,” King says. “Current clients will continue to receive services from us.”


Page 26 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024
Jose Canario
Paul W. Este
Michael S. King
Welcome Change


Prepare for new opportunities that stimulate engagement, feed your curiosity, and inspire a fresh desire for learning. St. John’s full array of service options address evolving needs within compassionate community settings.
• Independent Senior Living
• Enhanced Assisted Living
• Respite Care
• Rehabilitation
• Skilled Nursing Care
• Dementia Resource Center
• Hospice Care
Many life-enhancing choices await you.
SCHEDULE A TOUR TODAY. 585-760-1300 | stjohnsliving.org


Solo Traveling
• Cover In Good Health's columnist Gwenn Voelkers travels to Paris alone — and shares her experience
• Biking Biking around Rochester, Upstate. Cycling: cheaper than therapy
• Activities Table tennis is hot in Rochester (who knew?)
• Romance Penfield author is about to publish 107th book. One sold a million copies
• True Crime Local author pens ancestors' true crime story
• Advocate For Beth Ares it was a song that got her started
• Second Act Tracy Eckstrand: from school psychologist to singer-songwriter
• Music Elderly Brothers: Spreading joy one song at a time
• Retirement Part of it is to learn how to spend money saved over the years
• Summer Area zipline parks offer thrills and birdseye views
so much more!
May 2024 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • Page 27 NAME ADDRESS CITY/TOWN STATE ZIP 1 YEAR (6 ISSUES) $30.00 $40.00 2 YEARS (12 ISSUES) SUBSCRIBE
magazine serving active adults
Don’t miss a single issue. CLIP AND MAIL TO: 55 PLUS P.O. Box 525, Victor, NY 14564 SELECT STORIES IN THE NEW ISSUE OF 55 PLUS
to 55Plus, the only
in Rochester!
Issue 87 – May-June 2024
...and
INSIDE CHECK UP: MEDICAL TESTS YOU NEED WHEN YOU TURN 55 P. X TABLE TENNIS ANYONE? P 24
Gwenn Voelckers, the author and columnist of “Live Alone and Thrive,” recently spent 10 days in Paris. She talks about her solo experience and offers suggestions for women (and men) traveling alone. Plus: she lists her favorites spots in the City of Lights. P. XX
IGH May 2024
Don't Miss the New Issue!
THE TIME
FOR A
AND PLACE

Page 28 • IN GOOD HEALTH – Rochester / Genesee Valley Healthcare Newspaper • May 2024












































































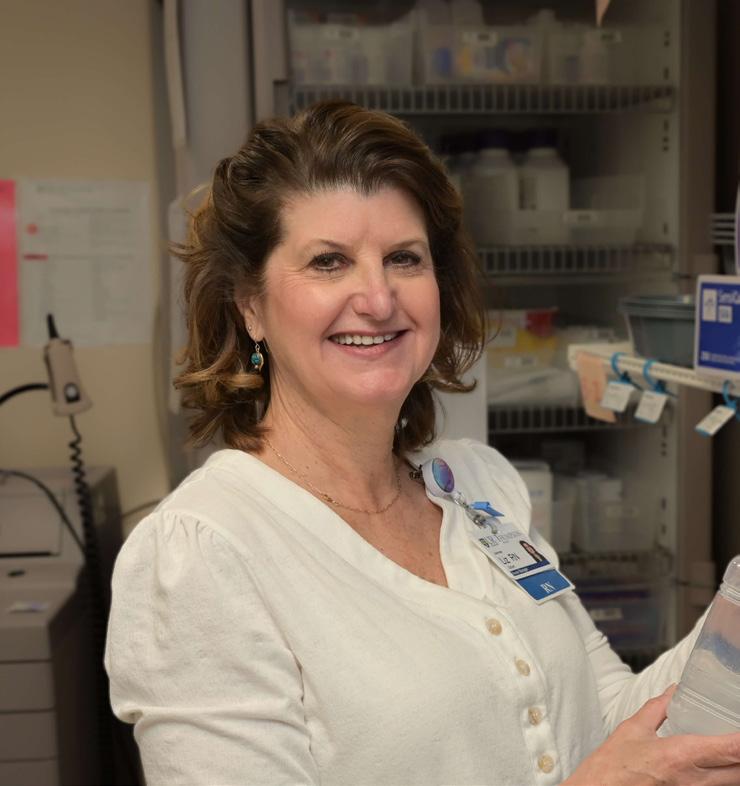
















































 By Jim Miller
By Jim Miller