VOL.17 NO 4 PAGES 44 www.expresshealthcare.in HEALTHCARE IT Prescribing innovation:
revolutionising the healthcare sector Shuba
Managing Director - GE BEL& General Manager- ISC South Asia,GE HealthCare INTERVIEWS INDIA'S FOREMOSTHEALTHCARE MAGAZINE SINCE 2000MAY2024,`50
HowAI is
Nagesh











































Chairman of the Board
ViveckGoenka
Sr.Vice President-BPD
Neil Viegas
Vice President-BPD
Harit Mohanty
Editor
Viveka Roychowdhury*
Editorial Team
Lakshmipriya Nair
Kalyani Sharma
DESIGN
Art Director
Pravin Temble
Senior Designer
Rekha Bisht
Senior Artist
Rakesh Sharma
Marketing Team
Rajesh Bhatkal
Douglas Menezes
Ashish Rampure
Debnarayan Dutta
Production Co-ordinator
DhananjayNidre
Scheduling & Coordination
Pushkar Waralikar
CIRCULATION
Mohan Varadkar



CONTENTS

INTERVIEW

P12: DR NITISH SHETTY CEO, Aster DM Healthcare, India
P13:
VIKRAM THAPLOO CEO-Telehealth, Apollo Hospitals Enterprises
POLICY

15 WILLTHE ABHA-UHI BE AS TRANSFORMATIVE AS UPI?
MEDTECH

27 WHYCLINICIANS NEED THE RIGHT MESSAGING PLATFORMS HEALTHCARE IT
26 PRESCRIBING INNOVATION: HOW AI IS REVOLUTIONISING THE HEALTHCARE SECTOR
P24:
SHUBANAGESH Managing Director - GE BEL & General Manager- ISC South Asia, GE HealthCare
-
and Published byVaidehi Thakar on behalf of The Indian Express (P) Limited and Printed at The Indian Express Press,Plot No.EL-208,TTC Industrial Area,Mahape,Navi Mumbai-400710 and Published at Mafatlal Centre,7th floor,Ramnath Goenka Marg,Nariman Point,Mumbai 400021. Editor: Viveka Roychowdhury.* (Editorial & Administrative Offices: Mafatlal Centre,7th floor,Ramnath Goenka Marg,Nariman Point,Mumbai 400021) * Responsible for selection of news under the PRB Act.Copyright © 2017.The Indian Express (P) Ltd.All rights reserved throughout the world. Reproduction in anymanner,electronic or otherwise,in whole or in part,without prior written permission is prohibited.
May2024 EXPRESS HEALTHCARE 9
Express Healthcare® Regd.With
Regd.No.MCS/162/2022
RNI No.MAHENG/2007/22045.Postal
24.Printed
Pg 16
Will the next PM have the right cure for the healthcare sector?
While various regulators are proposing policy changes to reduce the cost of healthcare services, none of these efforts will have long term impact, for citizens/patients, if they are not sustainable and feasible for the providers of these services.
Take for example, the recent decision by the insurance regulator, the Insurance Regulatory and Development Authority of India (IRDAI), to abolish the age limit for health insurance. A long over due initiative but how soon will this translate into real benefits for senior citizens? India, traditionally considered a younger nation, is now watching a drop in fertility rates. As births drop below the number of deaths, it is only a matter of time before the country's demographic profile gets more silver.
Health insurance is an important part of helping all citizens cope with the increasing cost of healthcare but increasing awareness about insurance coverage has been an uphill task. Certain sections of the population remain underserved, with low or poor coverage. Even after IRDAI removed the entry age barrier of 65 years for purchasing health insurance, there is no guarantee that insurers will find the senior citizen health insurance market attractive enough to design policies which meet the requirements of this category.
For instance, will insurers reduce the waiting period for pre-existing diseases, which most senior citizens would have? Will these policies remain on paper, with stringent terms, exhaustive exclusion criteria and higher premia? Will insurers offer a graded claim pay out in the first three years and full claim post four years of continuous renewal? Current insurance policies for this age category offer relatively smaller sums insured, which are not sufficient to pay the hospital bills which senior citizens have to deal with.
While long overdue, insurers need to find ways to make seniorcitizen health insurance coverage feasible and sustainable from an operationalpoint of view. As the senior citizen population grows, swelling an already substantially large market, one hopes that insurers will re-look their offerings for this category and design more innovative health insurance covers.
A similar well-intentioned but difficult to implement initiative is the diktat from the Supreme Court of India (SC) to rationalise fee structures for private hospitals across India, by mandating that private hospitals implement the Clinical Establishment (Central Government) Rules, 2012. The rationale is that a set fee structure will reduce hospital bills of patients, putting

Good intentions are not enough, we need a well thought out balanced long term blueprint and a solution which is sustainable for all stakeholders. Hopefully the next government and Prime Minister is up to the task
public and private hospitals at par in terms of treatment costs.
The central government's consultations with state governments had mixed results. State governments from Gujarat, Madhya Pradesh, Uttar Pradesh and Uttarakhand were reportedly against the idea, citing concerns that fixing fees might compromise quality of services. However, states like Uttar Pradesh, Bihar, Himachal Pradesh and Telengana, which had adopted the Clinical Establishments Act, 2010 were willing to take the discussion forward with private hospital authorities and asked the ministry for further guidance.
Analysts tracking the sector point out that if the hospital fees are regulated, they would impact smaller hospitals more than the larger chains. Tausif Shaikh, India Analyst - Pharma and Healthcare, BNP Paribas India opines that price regulation would hit standalone hospitals, whose net profit margins are mostly in low single digits.
The analyst note reiterates a positive view on the hospital sector, despite the looming apex court verdict, reasoning that standardising pricing is difficult due to the extremely heterogeneous nature of the healthcare industry with substantial differences in hospital infrastructure, instruments used during surgeries, expertise of medical staff and the complexity of diseases that hospitals deal with.
While implementation of standardised pricing appears highly unlikely, BNP Paribas India states there is a possibility of capping room rents, which could impact hospital chains earning higher average revenue per occupied bed (ARPOB).
With the next date of the next SC hearing fixed on September 10, one hopes that we get more clarity on how this rule can be implemented in a more balanced manner. Capping room rents would go easy on patients' pockets but would hospitals then cut back on clinical services or reduce quality of equipment? These are difficult choices and decisions. While the centre has put the onus on states, this merely prolongs the uncertainty.
Good intentions are not enough, we need a well thought out balanced long term blueprint and a solution which is sustainable for all stakeholders. Hopefully the next government and Prime Minister is up to the task.
VIVEKA ROYCHOWDHURY, Editor viveka.r@expressindia.com viveka.roy3@gmail.com
EDITOR’S NOTE EXPRESS HEALTHCARE May2024 10













INTERVIEW
Technologyholds immense potential to improve healthcare affordability
Dr Nitish Shetty ,CEO,Aster DM Healthcare,India in an interaction with Kalyani Sharma shares his company’s current and future plans and discusses about the role of technology and PPPs in the healthcare sector
What are the current plans of Aster DM Healthcare, and what would you be looking for this year?
The segregation is expected to unlock value for investors in India and we do have some aggressive plans in pipeline to fuel this excitement. We do have some aggressive plans to expand in India in the next 3 years. Currently, we have 19 hospitals spread across 5 states, with most of them in South India. Although this includes nearly 4500 beds across our hospitals, we believe there is room for further growth. Following the segregation, we now represent about 1/3rd of the entity in India.
Compared to our peers, we are on par in terms of size in India, but the market demands a larger share. Our aim is to rank among the top 3 healthcare service providers in India, and we now have the opportunity to achieve this goal. Therefore, we have devised a clear expansion plan for the next 3 years, focusing on organic growth. We plan to add over 1700 beds by FY27, a combination of brownfield and greenfield opportunities to take the total number of beds in India to 6600+.
Our greenfield expansion is slated for Kerala, with projects in Trivandrum and North Kerala. However, a significant portion, 60 per cent of our investment, will go towards expanding existing capacity, primarily in Kerala and Karnataka, with a few additions in other states. This expansion is in anticipation of the market growth expected in the next 2-3 years, aligning our capacity with projected demand.
Expanding northward not

only enhances our margins but also allows for substantial investment in hospital equipment, boosting our competitiveness and visibility in the market. Additionally, we are exploring expansion opportunities in other geographies, notably Maharashtra.
Are you targeting tier 2 & 3 cities for these opportunities?
Yes, we are. Our model has been proven successful in tier 1 & 2 cities, with 70 per cent of our units currently located there, including business in tier 1 cities like Bengaluru. While we’ve performed well in these areas, we are open to opportunities in other metro cities.
Our primary focus, however, remains on expanding and increasing our footprint, replicating successful models established
in Bengaluru and Kerala.
Our mandate is to ensure consistent footprint growth while meeting stakeholder expectations in terms of margins and performance parameters. The evolving healthcare landscape demands a blend of consolidation and expansion efforts, a balance we aim to achieve moving forward.
How do you see technology impacting healthcare affordability?
Technology holds immense potential to improve healthcare affordability. The complexity of healthcare operations, with diverse specialties and data fragmentation challenges, can be effectively addressed through AI integration. While digitalisation and telemedicine have made strides, they have not fully addressed data
fragmentation. AI, however, shows promise in this regard.
Technology adoption, particularly in business aspects, is gaining momentum, driven by benefits such as streamlined data access for clinicians, enhanced patient-doctor interactions, and improved operational efficiency. Integrating technology with insurance systems can lead to seamless processes and improved healthcare outcomes.
Do you foresee challenges in healthcare professionals adopting AI?
While there may be initial hesitancy, healthcare professionals are increasingly embracing technology for its potential to enhance efficiency and augment their capabilities. AI, seen as “Augmented Intelligence,” complements rather than replaces human expertise. As technology matures to offer tangible benefits like streamlined patient data access and improved diagnosis processes, adoption among professionals is likely to grow.
The convergence of clinical expertise and technological advancements will drive widespread adoption, empowering healthcare professionals to deliver better care.
What are Aster DM
Healthcare’s future plans regarding innovation and technology?
We prioritise collaboration with technology firms for innovation and R&D initiatives. Collaborations in both clinical and business domains aim to leverage technology for improved healthcare delivery and
operational efficiency.
Technology plays a crucial role in achieving our goal of being among the top healthcare providers, driving innovation and enhancing patient care experiences.
How do you view Public Private Partnerships (PPPs) in healthcare?
PPPs have been beneficial in leveraging governmentsponsored schemes and expanding healthcare access. While challenges exist, particularly in payment and pricing structures, collaborations between private and public sectors can drive positive outcomes in healthcare delivery. The government’s role as a facilitator and regulator, with private sectors as providers and payers, can lead to improved healthcare access and quality.
What do you see as the biggest challenge and opportunity for the healthcare industry?
The biggest opportunity lies in India’s growing healthcare needs, with significant potential for expansion and innovation. However, deploying talent and infrastructure to tier 2 & 3 cities poses a challenge, albeit one that can be overcome through coordinated efforts among stakeholders. The integration of private insurance, improved connectivity, and government support are key factors in realising the industry’s potential and providing equitable healthcare access across the country.
Kalyani.sharma@expressindia.com journokalyani@gmail.com
EXPRESS HEALTHCARE May2024 12
AI has emerged as a game-changer in healthcare
Apollo Hospitals organised the 11th edition of its International Health Dialogue (IHD),an amalgamation of the International Patient Safety Conference (IPSC) & Transforming Healthcare with Information Technology (THIT) on the 23rd-24th of February. Vikram Thaploo ,CEO-Telehealth,Apollo Hospitals Enterprises in an interaction with Express Healthcare talks about the key outcomes of the conference and more
What were the key outcomes of the 11th Transforming Healthcare with IT (THIT) 2024 conference?
At the THIT conference, luminaries like S. Somanath, Kiran Mazumdar Shaw, and Dumitru Prunariu, former Chair of the UN Committee on Peaceful Use of Outer Space, discussed ‘Transforming Healthcare with IT.’ Other notable participants included Russell Andrews, former Medical Advisor at NASA, and Thais Russomano, CEO of InnovaSpace Ltd., among others, representing diverse expertise from healthcare, technology, and space exploration.
Across the two days, the 11th edition of Transforming Healthcare with IT saw participation from 1500+ health professionals from 30+ countries including healthcare leaders, government officials, students, clinicians, and more. Since the first edition in 2011, the spectrum of participants and range of discussions have magnified. With over 50 sessions and 100 speakers, the sessions in 2024 amplified the patient perspective, put the spotlight on the integration of Artificial Intelligence (AI) in building a futuristic healthcare model, and emphasised the rising importance of data privacy at every step.
A major highlight of the conference was 'Solvathon 2024', a first-of-its-kind healthcare hackathon in collaboration with Indian Institute of Technology –Alumni Centre, Bengaluru that saw 14 enterprising teams 6 problem statements,

and 36 hours of relentless problem solving, with the winning team getting the opportunity to co-implement their solution commercially with Apollo hospitals.
As the conference theme was “A to I, Achievement through Innovation," what are the technologies driving innovations in healthcare that were highlighted at the conference?
The theme for this year’s THIT was centered around the topic of “From A to l, Achievement through Innovation"; exploring the potential of AI in strengthening healthcare services in India. There were deep dive sessions around the role of AI in revolutionising connected medical devices and how India is driving innovation in healthcare on a global scale. Sessions and discussions ranged from the
role of AI in healthcare, fostering patient-centricity, the rise of smart hospitals, the role of mental wellness in patient safety to healthcare in outer space, and prioritising health equity.
Technologies driving innovations in healthcare that were highlighted at the conference included AI in chest X-rays, Healthcare in Outer Space, AI's impact on privacy and security, Cloud Computing and Generative AI, and AI in Cardiology. Apart from that, the "Innovations in Digital Health" session also delved into novel technologies such as telemedicine, wearables, and health-tracking apps, exploring their potential to improve patient outcomes and healthcare accessibility.
The THIT sessions also explored the importance of public-private collaborations, leveraging data for improved
healthcare outcomes while safeguarding patient privacy, and upskilling the healthcare workforce for the digital era.
How can health leaders collaborate to propel digital transformation and pioneer healthcare innovation, across all demographic and geographic locations, especially the underserved locations and populations of India and the world?
Health leaders can collaborate to propel digital transformation and pioneer healthcare innovation by adopting a multifaceted approach that prioritises collaboration, knowledge sharing, and value-based incentives. Firstly, it is crucial to recognise that digital transformation is not solely about implementing technologies but also about fostering a culture of change and empowering individuals
to embrace new ways of working. Leaders should focus on identifying and attracting skilled employees while also investing in the training and development of the current workforce to ensure they are equipped to thrive in a digitalised environment.
Furthermore, collaboration and alignment across different business units are essential to ensure a smooth and cost-efficient transformation. Leaders must work towards breaking down organisational silos and fostering collaboration among teams to better understand priorities and identify potential risks. By creating an environment that encourages open communication and knowledge sharing, health leaders can drive innovation and accelerate the adoption of digital technologies.
Additionally, investing in infrastructure and solutions in a sustained manner is paramount to support digital transformation initiatives. Health leaders should prioritise the allocation of resources towards technology infrastructure and solutions that enable seamless collaboration and data exchange across demographic and geographic locations, especially in underserved areas. Moreover, implementing value-based incentives can incentivise digital adoption and collaboration among healthcare professionals, ultimately driving positive outcomes for patients and communities.
In essence, by prioritising collaboration, knowledge sharing, and value-based incentives, health leaders can
May2024 EXPRESS HEALTHCARE 13
INTERVIEW
spearhead digital transformation efforts that have a meaningful impact on healthcare delivery, particularly in underserved locations and populations. Through sustained investment and a commitment to fostering a culture of innovation, health leaders can drive positive change and improve healthcare outcomes for all.
THIT 2024 saw a larger than usual representation from the IITs, reflecting that many have started Schools of Medicine and have campus innovation incubators serving healthtech startups. How are industry leaders like the Apollo Hospitals group engaging with such academia outside the medical world?
As industry leaders, we at the Apollo Hospitals group actively engage with academia outside the medical world by fostering partnerships and collaborations with institutions, including those within the IIT ecosystem. These partnerships offer a unique opportunity for us to leverage academic expertise and research capabilities to drive innovation in healthcare. By collaborating with IITs and other academic institutions, we co-create solutions, develop cuttingedge technologies, and nurture healthtech startups through innovation incubators. Our goal is to bridge the gap between academia and industry, facilitating the exchange of knowledge, promoting interdisciplinary research, and accelerating the translation of academic innovations into real-world applications that benefit patients and healthcare systems.
What are the recent technological developments that can support future healthcare technology in the industry?
Recent technological developments that can support future healthcare
technology in the industry include AI, Extended Reality (XR), Health trackers, wearables, and sensors, Direct-to-consumer genetic testing, revolutionising drug development, consumer medical robotics, and 3Dprinting & bioprinting.
AI has emerged as a gamechanger in healthcare, revolutionising medical record analysis, treatment planning, and drug development processes. With AI algorithms, medical professionals can access insights and create treatment plans faster than ever before.
Extended Reality (XR), which encompasses virtual reality (VR), augmented reality (AR), and mixed reality (MR), holds promise in various medical applications. VR offers immersive experiences beneficial for mental health care and pain management, while AR assists surgeons in complex procedures, enhancing precision and outcomes.
Health trackers, wearables, and sensors empower individuals to monitor their health and wellbeing actively. These devices provide valuable insights into personal health metrics, facilitating proactive healthcare management and lifestyle changes.
Direct-to-consumer genetic testing offers personalised insights into genetic predispositions for various health conditions. Individuals can leverage this information for preventive measures and early interventions, optimising their quality of life.
Technological advancements in drug development, such as AI and in silico trials, promise to streamline the process, reducing time and costs associated with bringing new drugs to market.
Consumer medical robotics, including surgical robots and exoskeletons, are transforming healthcare delivery by enhancing precision, efficiency, and patient outcomes.
3D-printing and bioprinting technologies are
making strides in healthcare, enabling the creation of biotissues, regenerative heart valves, artificial limbs, and even potential organ printing in the future.
In summary, these technological innovations hold immense potential to reshape the future of healthcare, empowering patients, improving treatment outcomes, and driving efficiencies across the industry.
How is ATNF/HNG/ATH helping healthcare facilities in rural India? Is it affordable and accessible to all?
Apollo Telehealth has revolutionised the healthcare landscape by breaking down geographical barriers and extending quality medical care to over 15 million individuals. With its innovative approach, Apollo Telehealth has made medical consultations easily accessible from any location, significantly reducing travel and wait times. Through just a few clicks, patients can connect with expert doctors, improving healthcare outcomes.
This platform is democratising healthcare by ensuring that individuals lacking access to medical facilities can still receive timely and expert medical attention, leading to improved individual health outcomes and a healthier society overall. With a dedicated team of over 350 clinicians, Apollo Telehealth's command center manages more than 20,000 clinical transactions daily, offering a wide range of services including emergency, primary, secondary, and preventive healthcare, along with quality audits and training sessions. Specialized services such as TeleEmergency, Tele-Radiology, and Tele-Ophthalmology reach even the remotest regions, enhancing the healthcare landscape and improving overall quality of life. Notably, over 10,000 TeleEmergency cases have been successfully stabilized in states like Himachal Pradesh
and Tripura, showcasing the impact of timely interventions. Through partnerships with publicprivate entities, Apollo Telehealth has established over 800 centers in 7 states, activating 350,000 public touchpoints at gram panchayats through Common Service Centres, thus making quality healthcare more accessible to the masses.
Has Apollo Telehealth been running any program under PPP (Public Private Partnership) as it is in trend? If yes, Please share a brief.
Dr Prathap C. Reddy, Chairman, Apollo Hospitals Group, and Dr Sangita Reddy, Joint Managing Director, Apollo, have long championed the vision of universal healthcare access through innovation and technological advancement. Dr Prathap Reddy envisioned leveraging technology to provide highquality medical care even to the remotest corners of the country, leading to the establishment of Apollo Telehealth. Dr Sangita Reddy, passionately committed to transforming healthcare ecosystems, has spearheaded initiatives to integrate cutting-edge technology and patient-centric approaches into healthcare delivery.
In line with their vision and mission, Apollo Telehealth (ATH) has been pioneering initiatives under Public-Private Partnerships (PPP), aligning with the current trends in healthcare.
With over two decades of experience in Telemedicine, ATH stands as the largest and oldest multi-specialty telemedicine network globally. Through strategic PPP collaborations, ATH has significantly contributed to advancing primary healthcare in the country, impacting the lives of more than 20 million individuals across the country.
With a remarkable track record of over 20 million teleconsultations delivered and 20,000 clinical transactions conducted daily, ATH has emerged as India's
foremost turnkey provider in telemedicine. The network operates 500+ public health centers, 100+ franchised teleclinics, and has a presence through 350,000 common service centers, with plans for further expansion.
Notably, ATH has collaborated with the Andhra Pradesh government to provide Tele-Ophthalmology services at 115 centers across the state, extending its reach to underserved communities. Furthermore, its Himachal Pradesh Telehealth Program offers critical emergency, specialty, and super-specialty consultations in the Himalayan Mountain range, ensuring access to quality healthcare even at altitudes of about 14,000 feet above sea level.
In alignment with the vision to harness technology for universal access to highquality medicine, ATH has been entrusted by the government of Uttar Pradesh for Tele-Radiology services in 134 Community Health Centers (CHCs) and Telemedicine services in 120 CHCs.
Moreover, ATH's establishment of Digital Dispensaries across 100 selected PHCs in Jharkhand, equipped with state-of-the-art equipment for vital signs monitoring and screening programs, further underscores its commitment to extending healthcare services to underserved areas.
Recently, ATH expanded its reach to Meghalaya by setting up five Digital Dispensaries and running a mass cancer screening program in collaboration with the state government. These initiatives reflect ATH's dedication to making healthcare accessible to all, in line with its mission to transform healthcare ecosystems through technological advancements and service innovations.
Abbreviations:
ATH: Apollo Telehealth
ATNF: Apollo Telemedicine Networking Foundation
HNG: Healthnet Global
EXPRESS HEALTHCARE May2024 14
POLICY
Will the ABHA-UHI be as transformative as UPI?
Dr Sabine Kapasi,Co-Founder and MD,Enira Consulting feels that ABHAhas what it takes to make a big difference in Indian healthcare,in spite of several challenges that need to be addressed
As we celebrate the strides in healthcare innovation, let us explore how the Ayushman Bharat Health Account (ABHA) and Unified Health Interface (UHI) emerge as transformative pillars, leveraging digital technologies to enhance access and efficiency in healthcare delivery across India. Its importance can be gauged by how starting April 1, the government has made it compulsory to connect the Central Government Health Scheme (CGHS) beneficiary ID with the Ayushman Bharat Health Account ID.
All of us will remember how the Unified Payment Interface (UPI) had brought about a significant transformation in digital payments across India. Launched by the National Payments Corporation of India (NPCI) in 2016, UPI swiftly became the most widely adopted digital payment system in the country. Its seamless interface has simplified transactions, making swiping and tapping through payments a commonplace experience.
Drawing parallels with UPI’s success, ABHA under the Ayushman Bharat Digital Mission (ABDM) aims to revolutionise the healthcare sector. Managed as a key component of ABDM, ABHA acts as a pivotal tool for Indian citizens, offering a multitude of benefits. These include streamlined processes at medical facilities, enhanced access to treatments, and a robust identity system, effectively transforming the landscape of healthcare services. The ABHA initiative provides citizens with convenient access to medical treatments and healthcare facilities, along with user-friendly options for personal health record applications through the ABDM ABHA app, ensuring a reliable and secure healthcare identity for every individual.
Inclusion is one of the core design principles for all ABDM building blocks. For those who
require assistance for the creation of ABHAs, assisted modes have also been rolled out. Further, an offline ABHA generation module has been introduced in rural areas wherein internet connectivity is limited or not available. The most important point to be noted is that health records associated with Health IDs or ABHA numbers can only be accessed with the informed consent of the individual.
The same goes for the UHI, which comprises a set of open protocols designed to facilitate interoperability within health services. It serves as a fundamental component within the ABDM Stack, emphasising the accessibility and delivery of health services. While the existing ABDM components facilitate the exchange of personal health data and maintain registries for doctors, patients, and healthcare facilities, UHI builds upon these elements to offer a seamless, end-to-end user experience. Through applications enabled with UHI, patients can easily discover, schedule, engage in, and pay for services provided by various participating providers, all within their preferred application interface.
The impact of these new initiatives is substantial. Consider the experience of bypassing lengthy queues at the Out Patient Department (OPD) – it significantly improves patient convenience and operational efficiency, akin to a valuable healthcare enhancement. Moreover, the widespread adoption of ABHA and UHI by hospitals nationwide underscores their effectiveness in simplifying processes for both patients and healthcare providers, ultimately enhancing overall healthcare service delivery.
The main objective of ABHA is to reduce the time taken at the OPD registration counter, provide accurate data in the hospital record, and, most importantly, avoid the

wait in the long queues. Ever since the launch, the program has witnessed an increase in adoption among various hospitals across India.
As of February 2024, there are around 36 crore ABHAlinked Health Records, indicating a significant digital footprint of health information. Additionally, there are approximately two lakh registered Health Facilities, highlighting the extensive network available for healthcare services. Furthermore, there are roughly three lakh Healthcare Professionals registered, ensuring a robust workforce to cater to patient needs. The Health Records App has been downloaded approximately 67 lakh times, showcasing the growing adoption of digital health solutions among users. Together, these estimates reflect the progress and adoption of digital initiatives in the healthcare sector.
In Uttar Pradesh’s Gautam Budh Nagar, CMS District Hospital achieved a remarkable feat of implementing this scheme and it helped them in the management of the massive footfall.
ABHA and UHI are part of mobile technology-based health solutions, known as MobileHealth (mHealth), which are increasingly revolutionising healthcare delivery, particularly in low and middle-income countries. According to the World Health Organization (WHO), mHealth encompasses
electronic health services and information delivered via mobile devices like smartphones and personal digital assistants.
In Ethiopia, mHealth applications have significantly improved maternal and child health indicators. These applications provide accessible and effective tools for monitoring pregnancies, tracking immunisations, and ensuring timely healthcare interventions, thereby reducing maternal and child mortality rates.
Along the Thai-Myanmar border, web-based mobile modules have been instrumental in the treatment and follow-up of malaria cases. These modules facilitate real-time data collection, rapid diagnosis, and targeted treatment strategies, contributing to better disease management and control.
In Senegal’s Saraya region, mHealth solutions are empowering communities to manage malaria cases at the grassroots level. Through mobile-based platforms, community health workers can track outbreaks, conduct awareness campaigns, and coordinate with healthcare facilities for prompt treatment, leading to improved health outcomes and reduced disease burden.
Another noteworthy example is the ReMiND (Reducing Maternal and Newborn Deaths) program in Uttar Pradesh, India. Implemented through Accredited Social Health Activists (ASHA) workers in Kaushambi district, this mobile-based application enhances routine healthcare service delivery. ASHAs can efficiently track pregnancies, provide essential antenatal care, promote institutional deliveries, and offer postnatal support, thereby contributing to a significant reduction in maternal and newborn mortality rates.
Challenges that need to be addressed
However, ABHA faces several
challenges that need to be addressed. Firstly, there is a need for more use cases to demonstrate its effectiveness and versatility. Secondly, the literacy rate among the target population poses a challenge, requiring tailored approaches to ensure understanding and usage. Thirdly, technical stability is imperative for the smooth functioning of ABHA and to instill trust among users. Lastly, adoption from the side of doctors is crucial for the widespread implementation and success of ABHA. Addressing these challenges will be essential for the sustainable development and impact of ABHA. Finally, the implementation brings privacy concerns, where the risk of privacy breaches in digital health records can lead to identity theft or discrimination. Cybersecurity risks are also significant, with the increasing digitization of healthcare systems making them vulnerable to attacks like data leaks or ransomware incidents. AI can help prevent these risks and make healthcare systems more resilient against cyber threats. Despite these roadblocks, ABHA has what it takes to make a big difference in Indian healthcare. Using mobile technology smartly, ABHA is set to change how healthcare is delivered. It will help improve the health of mothers and children, deal with disease outbreaks better, and manage community healthcare effectively. Getting an ABHA number isn’t compulsory, but it does make getting timely medical treatment much easier. It simplifies the transmission of patient information between hospitals, in turn improving medical services. As mobile health (mHealth) grows, ABHA goes beyond its usual role, becoming a key tool in achieving global health goals and making healthcare more engaging and impactful for everyone.
May2024 EXPRESS HEALTHCARE 15




Breaking silos of healthcare,insurance and finance,while not an easy task,will be key to ensure healthcare access to all.It requires concerted efforts from all stakeholders with newage approaches and technology
ByKalyani Sharma
EXPRESS HEALTHCARE May2024 16 cover )

May2024 EXPRESS HEALTHCARE 17
India's healthcare landscape is currently experiencing a significant transformation driven by technological advancements, evolving public policies, and dynamic market forces. Central to this shift is the crucial element of healthcare financing, which encompasses an intricate network of funding mechanisms, insurance schemes, public-private partnerships, and innovative models.
Vikram Venkateswaran, Partner, Deloitte India shares, “India's healthcare sector is undergoing a transformation fueled by investments in both public and private domains. Private hospitals, backed by a surge of $14 billion in PE funding in the last 4 years, are embracing technology to streamline operations. This translates to better diagnostics, improved patient experiences, and shorter hospital stays. The average length of stay in large corporate hospitals is down to 3.4 days thanks to these initiatives that are supported by data, analytics on a digital transformation backbone.”
Traditional models vs innovative approach
Traditional healthcare systems in India have historically relied on individuals paying for their own healthcare, placing a heavy burden on them. But this approach has proven unsafe, especially for vulnerable people.
Dr Puneet Khanduja, Lead -Health and Nutrition,MicroSaveConsulting (MSC) shares that the Economic Survey 2022-23 confirms this trend, stating that almost half of all health spending in India is still paid by patients themselves directly at the point of treatment, although this has dropped as the government’s share of spending on health went up significantly after 2013-14. The ES 2022-23 also reported a concomitant decline in out-of-pocket expenditure as a percentage of total health expenditure from 64.2 per cent in 2013-14 to 48.2 per




The average length of stay in large corporate hospitals is down to 3.4 days thanks to these initiatives that are supported by data,analytics on a digital transformation backbone
Vikram Venkateswaran Partner, Deloitte India
Innovative approaches like blended financing,crowdfunding,and healthcare lending are emerging to address affordability gaps and improve access to quality healthcare services
Dr Puneet Khanduja
Lead -Health and Nutrition, MicroSaveConsulting
(MSC)
In India,the decentralised nature of healthcare financing has resulted in a significant disparity in medical funding, leaving approximately 400 million citizens without access to essential healthcare services
Gaurav Gupta Co-Founder & CEO, CarePay
Healthcare financing is not new.But the way it has been done before is broken.It has essentially been a “desperation financing”solution and this needs to change
Chris George CEO & CO-Founder, Qube Health
cent in 2018-19. Households in the lower wealth quintiles are more likely to face catastrophic health expenditure, with the odds of incidence and intensity being higher for these households.”
Gaurav Gupta, Co-Founder & CEO, CarePay opines, “In India, the decentralised nature of healthcare financing has resulted in a significant disparity in medical funding, leaving approximately 400 million citizens without access to essential healthcare services. This exacerbates financial burdens and restricts crucial medical care, a situation compounded by the rise in cash flow challenges faced by hospitals. These challenges often stem from delays in insurance reimbursements, placing significant financial strain on hospitals and limiting their ability to provide quality care and expanded services to all patients.”
Recent years have seen a shift toward new financial models, including health insurance plans, government subsidies, and financial services.
Dr Khanduja shares, “Innovative approaches like blended financing, crowdfunding, and healthcare lending are emerging to address affordability gaps and improve access to quality healthcare services. These new models aim to combine public, private, and philanthropic funding to create sustainable financing structures that cater to the diverse healthcare needs of the population.”
These systems are designed to spread financial risk, increase access to healthcare, and improve overall health.
Sharing his views on this, Chris George, CEO & COFounder, Qube Health said, “Healthcare financing is not new. But the way it has been done before is broken. It has essentially been a “desperation financing” solution and this needs to change.”
“Instead of focusing on providing financing at the point of care, we need to provide financing in the hands of the pa-
EXPRESS HEALTHCARE May2024 18
)
cover
tient. This patient, who is the payor for healthcare then has the power of choice to decide which healthcare option is best for their family. It gives them more control. In these days of app-based payments for almost everything, it is high time that we put the power to pay, in the hands of every Indian”, he added.
Namit Chugh, Principle, W Health Ventures emphasises that over the last decade, the entry of new insurance distributors, better regulatory support, increasing use of technology and COVID-19 has led to the healthcare insurance growing 2x as faster than the general insurance industry
He added, “Start-ups are now making insurance purchase, understanding, and processing simple and fast. Majority of the tech-led innovation has happened in distribution and purchase. Today, it is possible to browse through 10 healthcare plans online, compare them using intuitive visuals and also get an assistant to guide you on the right policy.”
Howtechnologyis revolutionising healthcare financing and delivery
The advent of technology has revolutionised healthcare financing in India. Mobile applications, telemedicine platforms and data analysis tools streamline processes, reduce cost management and provide transparency in financial transactions. With its secure and independent features, blockchain technology is exploring its potential to revolutionise healthcare payments and prevent fraud. By investigating these technological innovations and their impact on healthcare financing and services, we can pave the way for a more efficient, patient-focused ecosystem.
Explaining how technology is revolutionising healthcare financing, Visalakshi Chandramouli, Managing Partner, Tata Capital Healthcare Fund said, “Technology is playing a transformative role in healthcare financing and delivery. For ex-



ample, in the dialysis sector, the government has launched the Pradhan Mantri National Dialysis Programme (PMNDP) technology portal in May 2022. The portal integrates all dialysis centers under one platform, where the patient and dialysis session information is consolidated allowing for creation of a renal registry, faster payments for service providers and also facilitating smooth portability for patients from one center to
Over the last decade,the entry of new insurance distributors,better regulatory support,increasing use of technology and COVID-19 has led to the healthcare insurance growing 2x as faster than the general insurance industry
Namit Chugh Principle, WHealth Ventures
While there have been notable successes of PPPprojects in the diagnostics and dialysis space, segments such as hospitals have seen limited uptake primarily due to the structure and financial viability of the proposed PPPs
Visalakshi Chandramouli Managing Partner, Tata Capital Healthcare Fund
By aligning incentives and sharing risks,PPPs have the potential to drive sustainable development and inclusive growth in the healthcare sector
Siddharth Singhal Co-founder and MD of Vibcare Healthcare
another across the country. On the delivery front, technology is being leveraged for improved access (eg. telemedicine), improved productivity (eg. radiology AI), improved convenience (eg. @ home healthcare).”
Breaking silos of healthcare, insurance and finance, while not an easy task, will be key to ensure healthcare access to all. It requires concerted efforts from all stake-
holders with new-age approaches and technology.
George highlights, “The ability to integrate apayments-infrastructure, healthcare financing, health insurance, and healthcare providers onto one mobile application is the truest example of how technology is revolutionising healthcare financing and delivery of healthcare. The movement of money, between the payor and the provider of
healthcare, is the true ‘lubricant’ in the smooth delivery of healthcare. Especially in India where cell phone access far exceeds healthcare access.”
Fintech platforms are playing a key role in changing the way health insurance is acquired, managed and used. These platforms uses technology to close current gaps of affordability and make the process more transparent. From digital insurance marketing to AI-powered insurance recommendation engines, fintech companies are changing the way people and businesses use health insurance products and programs.
Talking about fintech startups, Dr Khanduja said, “Fintech start-ups are also leveraging technology to offer healthcare lending options, personalised patient engagement, and innovative payment plans, thereby improving the overall efficiency and effectiveness of healthcare financing and delivery systems. Innovative payment plans offered by these players are designed to make healthcare more accessible and affordable for patients. Flexible payment plans allow patients to pay for their medical expenses in instalments, reducing the financial burden of healthcare costs.”
Gupta shares, “Embedded finance has emerged as a catalyst for empowering patients, offering tailored financing options for out-of-pocket health expenses. By providing enhanced patient experiences, fintech platforms offer a range of financing solutions at the point of care, such as zero-cost EMI, curated to cater to diverse portfolios. These solutions, imbued with a completely digital process and quick loan disbursals, make healthcare services more accessible and affordable. As a result, necessary care is not hindered by financial constraints, ensuring a seamless healthcare journey for all.”
“Thus, through a collaborative approach, fintech 2.0 and vertical financing facilitate seamless transactions across
May2024 EXPRESS HEALTHCARE 19
the healthcare landscape, enhancing the end-to-end healthcare journey. Prioritising innovation, customer-centricity, and inclusivity, technology holds the potential to revolutionise healthcare financing and delivery, fostering a brighter and more equitable future”, he added.
Impact of government schemes on healthcare financing
The Government of India has launched several flagship schemes aimed at improving healthcare access and affordability. The Ayushman Bharat - Pradhan Mantri Jan Arogya Yojana (PMJAY) and National Health Mission (NHM) are some of them.
Siddharth Singhal, Cofounder and MD of Vibcare Healthcare mentions, “Government schemes such as Ayushman Bharat and the National Health Mission are pivotal in reshaping the healthcare financing landscape. Ayushman Bharat, the world's largest government-funded healthcare programme, aims to provide health coverage to over 500 million Indians, offering a safety net against catastrophic health expenditures. Similarly, the NHM focuses on strengthening healthcare infrastructure, promoting preventive healthcare, and expanding access to essential services, thereby augmenting the foundation for sustainable healthcare financing in the country.”
George also shares, “These are great initiatives, that are now finding faster traction through partnerships with private companies and start-ups building with their sandbox. Through open APIs and deeper collaborations, these schemes have the ability to have far reaching impact that surpass the impact of schemes in the India stack for payments and finance.”
Chugh believes that it’s an early but great step in the right direction to ensure better healthcare coverage to a larger population base. These welfare
TECHNOLOGYIN HEALTHCARE FINANCING AND DELIVERY
Forthose without insurance: Technology has helped create simpler insurance products (therapy-specific coverage,sachet insurance,OPD/preventive focused plans etc.) and also facilitated faster and cost-effective distribution (surpassing or augmenting human agents with websites,online ads etc.).
For those with insurance: Alarger challenge technology has helped solve today is simplifying existing insurance and financing products by explaining their terms more transparently and recommending the right products for individuals and their needs. Majority of the tech-led innovation has happened in distribution and purchase.Today, it is possible to browse through 10 healthcare plans online,compare them using intuitive visuals and also get an assistant to guide you on the right policy.
During a healthcare event: Technology in India is just picking up in this area by fast tracking claim processing,and also providing immediate term financing to make true cashless experience possible.As an example,companies are now building centralised, NLP-based engines that can parse through case papers,insurance documents and hospital policies simultaneously to adjudicate claim within seconds (this used to take manual processors multiple hours and was still prone to errors).
Source:NamitChugh,Principle,WHealthVentures
SEVERALPPPMODELS OFCARE DELIVERY
Several PPPmodels of care delivery initiated by the Government of India are currently being implemented across the country,such as the Biomedical Equipment Management and Maintenance Program (BEMMP),Free Diagnostics Service Initiative,Pradhan Mantri National Dialysis Programme (PMNDP),and National Mobile Medical Units.
BEMPPfocuses on ensuring the availability and functionality of medical equipment in public health facilities by supporting state governments for outsourcing the comprehensive maintenance of medical equipment across all public health facilities.
The Free Diagnostics Initiative provides a set of essential diagnostics at various levels of care,,which citizens can avail themselves of at the facility.Similarly,PMNDP,a government initiative aimed at providing affordable dialysis services to patients suffering from End-Stage Renal Disease (ESRD) in India,is being implemented in PPP mode in several states such as Uttar Pradesh,Himachal Pradesh,Madhya Pradesh, Telangana,among others.
Source:DrPuneetKhanduja,Lead-HealthandNutrition,MicroSaveConsulting(MSC)
schemes have demonstrated wider reach – now inching towards 600M+ ABHA IDs; promised cover of Rs 5 lakh per family for 12 crore families; and already Rs 1 lakh crore reimbursed till December 2023.
But he also mentions, “However, only approximately 30 per cent insurance in India is via public insurance. And even today, two thirds of Indian patients pay out of pocket (patient side problem) and hospitals suffer from payables and working capital crunch (hospital side problem). Dedicated focus on improving coverage, ensuring ground-level aware-
ness and utilisation, fraud detection and also timely hospital repayments will add further credibility to the noble schemes and help achieve healthcare goals for the country.”
Recently, to widen the market and foster adequate protection from healthcare expenses, insurance regulator Insurance Regulatory and Development Authority of India (IRDAI) has removed the age limit of 65 years for individuals buying health insurance policies. By abolishing the maximum age restriction on purchasing health insurance
plans, IRDAI aims to foster a more inclusive and accessible healthcare ecosystem, ensuring adequate protection against unforeseen medical expenses.
“Outside of this the government has also provided regulatory environment to help health insurance grow. The just announced policy of removing age bar for a healthcare policy is on the same line. IRDAI has welcomed innovation by introducing friendlier guidelines like the sandbox license to pilot new products across the spectrum – distribution, underwriting, manufac-
turing, servicing, and claims”, Chugh added.
The evolving landscape of public-private partnerships in healthcare financing
Public-private partnerships (PPPs) aims to bring together the power of resources by government, initiatives by private sector including community partnerships. PPPs are emerging as an crucial strategy for financing and delivering healthcare in India and expanding coverage in underserved areas.
Singhal opines that by aligning incentives and sharing risks, PPPs have the potential to drive sustainable development and inclusive growth in the healthcare sector.
George believes that we are a long way off in this regard, however any initiative that connects the dots between the India stack for finance, healthcare and insurance, will truly democratise access to healthcare in India.
Chugh explaining the private sector dynamics said, “The health insurance premium in India (gross written premium) for the last 12 months is Rs 1 lakh crore+ already (20 per cent+ up from last fiscal) with 37 per cent coming from standalone health insurance companies. Roughly 1/3rd of this came from the top-5 standalone health insurers (rising at ~26 per cent YoY).
While these insurers are typically legacy companies, the industry growth has encouraged new players to enter as set-up and distribution becomes easier. Recently, Narayana Health (India’s leading hospital chain) obtained an IRDAI license to offer insurance also. This opens up the possibility of fullstack managed care organisations in India where the provider has greater visibility to patient data and is also better incentivised to provide quality preventive care and improve patient outcomes longterm.”
Chandramouli also shares,
“While there have been notable successes of PPP projects in
EXPRESS HEALTHCARE May2024 20
cover )
the diagnostics and dialysis space, segments such as hospitals have seen limited uptake primarily due to the structure and financial viability of the proposed PPPs. The government is working on improving the viability of PPP in the hospital segment for example the super specialty Hospital in Katra, Jammu run by Narayana Health has been successful. We can expect private sector players to actively bid for projects if the financial viability of the projects are addressed.”
Challenges and opportunities
Healthcare financing ecosys-
tem is making a significant progress but challenges still persist. Imbalance in resource allocation, some administrative complexities and 100 per cent accessibility remain challenging problems.
Dr Khanduja also believes that affordability remains a critical issue as healthcare expenses outpace household incomes for many.
He said, “The NITI Aayog's "Health Insurance for India's Missing Middle" report highlights the significant gap in health insurance coverage for a large segment of the Indian population, who are not poor enough to qual-
ify for government insurance schemes but also cannot afford private insurance.”
George said, “Cutting through the silos of healthcare, insurance and finance is a tough challenge for anyone. This however is also the opportunity. Solving the healthcare access problem in India, begins by solving the healthcare payments and financing problem first.”
The pandemic also underlined the need for a sustainable financial system. This in turn creates an opportunities for policy reforms, collaboration and innovation.
Singhal mentions, “Ad-
dressing disparities in access, ensuring financial sustainability, and enhancing regulatory frameworks are critical tasks that require concerted efforts from all stakeholders. However, amidst these challenges lie immense opportunities for innova tion, collaboration, and impact. By harnessing the power of technology, fostering partnerships, and prioritising inclusivity, India can pave the way for a resilient and equitable healthcare financing ecosystem.”
Wayforward
As India's healthcare sector
continues to evolve, the importance of a sound and inclusive financial system cannot be ignored. From traditional to innovative, from government intervention to private sector, from PPPs to technological advancements, all healthcare services play an important role in the future development of healthcare in India. On the path to universal health coverage, affordability, and quality care for all, stakeholders in the world health system must work together.
Kalyani.sharma@expressindia.com journokalyani@gmail.com
Healthcare financing and its role in a complexsystem
Rakshith Rangarajan,Fund Manager,Inviga Healthcare Fund and Karan Kumar,Business Analyst,Inviga Healthcare Fund share their views on healthcare financing in India
As we sat down to write this article one thing was for certain, we were never going to be short of topics to cover. The fabric of the Indian healthcare industry is rich, diverse, multilayered. The emergence of India as one of the fastest growing economies in the world, rising in affluence, gradually alleviating poverty, fostering a free market, bristling with a rich entrepreneurial talent and a robust venture financing system – are making the headlines. Rather than pick up a specific aspect of this “kaleidoscope” and marvel at it for a few hundred words, we felt it may be interesting instead to appraise the Indian healthcare ecosystem very briefly through the lens of Emergent Behaviour and Complex Systems theory. And through this, place with you, some of our views on how Healthcare Financing is responding to the changes ushered in by the government and technology. We hope it helps you appreciate better, some of the “invisible hands” at work as


you navigate through your own microcosms within Indian healthcare!
Complexsystems theory
Let us define complex systems
and emergent behaviour. Complex systems are “highly composite”, built up from a very large set of mutually interacting subunits (often also complex). All these subunits re-
peatedly interact with eachother and result in rich, collective behaviour that feeds back into the behaviour of the individual parts. “Emergence” is said to happen when the ulti-
mate observable macro-behaviour of the entire system is exponentially different and not attributable to any single subunit but to the complex relationships between subunits. “A
May2024 EXPRESS HEALTHCARE 21
Rakshith Rangarajan
Karan Kumar
Whole is greater than the sum of the parts”.
Quite intuitively, one can realise that the Indian healthcare economy is a complex system: what with various subunits, patients (a multitude of demographic/economic/genetic segments), providers (institutions, clinicians, nurses), payers, administrators, suppliers, lenders, investors, educators and many more. Each of these subunits has its own set of unique circumstances, incentives, motivations and objectives and is concurrently optimising for maximising its utility/satisfaction (health or profit or otherwise). And what is emergent from all of these interactions is what one sees in the form of macro indicators of health and healthcare economics.
As we shall see, every rise and fall in one sub-unit materially (sometimes perversely) alters the alignment of the system. For the purpose of this write-up we have considered merely two factors, (1) The Impact of Ayushman Bharat/PMJAY/ National Health Mission on Healthcare Businesses & Financing and (2) How technology is revolutionising healthcare delivery and financing. Let’s evaluate their contribution to emergent behaviour for better and worse!
Impact of Ayushman Bharat/PMJAY/ National Health Mission on healthcare businesses & financing
◆ Prime mover: The administration
◆ The intention: Improved healthcare access and affordability: Universal Health Coverage (UHC) assures protection to India’s vulnerable population (~50 Crore+) and makes catastrophic episodic healthcare financially manageable. Extends across primary, secondary, and tertiary care services, as well as pre- and post-hospitalisation care. Aims to establish 1.5 Lac Health and Wellness Centres (HWCs), in rural and urban areas. Offers annual coverage of Rs 5 lac per family.
◆ The promise offered by
AB/PMJAY/NHM: (1) Egalitarian Health (2) Mitigating the impact of adverse selection in insurance (3) secular contribution to the consumption of health. Induction of 50 Cr people as “consumers” would likely spur demand on an exponential scale especially for front-line care, diagnostics etc. In an ideal world, this should directly imply a win-win for patients and providers alike - Businessmen and their Financiers would be smiling all the way to the bank, thanks to the exponential growth in opportunities driven across every layer of the value stream, with every incremental person enrolled/covered under the scheme.
◆ Has this materialised?
◆ With~27k hospitals covered (out of the total pool of 70k) and 6 crore hospital admissions facilitated the net has been cast wide already. Nearly 50 per cent of the beneficiaries of the scheme used private care, which is encouraging. We estimate that since its launch in September 2018, nearly USD 2 billion of venture capital flows have supported diagnostics and primary care initiatives alone, which underscores the expectations of growth.
◆ On the flipside, there is evidence of hospitals not meeting standards for enrolment (infra + HR), which is decelerating the roll out. This offers clear opportunities for private enterprise and its financiers.
◆ For instance, deficient infra, lack of quality equipment is an oft cited issue. Is this not an opportunity for financiers, medical equipment manufacturers/ leasing services and the like to unlock value? ~ USD 1 billion of private equity flow has supported the Devices space since 2018 and flows are on the rise
◆ Similarly, businesses that help address skilling gaps are welcome. Several start-ups are operating in this niche, well financed by VCs and it would be very interesting to see some of them achieve meaningful scale.
◆ Thematic healthcare funds can play a role in helping entrepreneurs identify sustainable niches and curate investment
opportunities that alleviate infrastructural bottlenecks. The demand is genuine, the Administration’s commitment is genuine and the jigsaw only needs a robust B Plan and acumen.
◆ PMJAY also is shackled by the usual malaise of pilferage, suspicious enrolments, which have decelerated roll out. There are also recurring complaints of delayed payments from the Administration. Health-tech can play a role as described in the next section
◆ Perverse emergent behaviours and remedies: Government sponsored UHC of the gargantuan scale of PMJAY will necessarily impact all participants irreversibly. However certain perverse outcomes are only to be expected despite well-intentioned policy and rollout. Some examples are:
(1) High influx of entrants at the conventional primary care and diagnostics interface:
◆ In a geographically dispersed market, which is accelerating, with low entry barriers, commoditisation is a distinct possibility. With NDHM and data interoperability play, this trend will intensify. All these forces in unison are likely to increase consumer choice, reduce switching costs/lock-ins.
◆ The primary remedies for businesses are to increase efficiencies by leveraging tech, innovative delivery models, harnessing supply chain control and focusing on quality of delivery as a primary non-price source of differentiation. Those that cannot evolve to meet this heightened competitive risk, will face headwinds.
◆ This preference for sophistication and pursuit of “niches” is evident in practice, as VCs/PEs with exposures to these segments have bankrolled (1) advanced diagnostics, bio-informatics of (2) omni-channel play, (3) widening/integrating offerings. Increased VC focus on profitability also indicates a heightened sensitivity to the increased competitive environ.
◆ Responsible investing can ensure value to the entrepreneur by counselling them away from “feeding frenzies”, and training guns on durable profitable need gaps. Capital allocation becomes efficient. Several healthcare funds are doing this admirably well.
(2) Process may sadly trump Quality: Something that healthcare IT can set-right
◆ There is a risk of an inadvertent loss of flexibility in provider-patient interactions. Every instance of care-demanded is unique and the clinical pathways often have a fair divergence. However, Insurers would naturally like predictability, in process, in cost, in delivery. Even more-so if it is Govt. Sponsored health.
◆ Standardization however does not help necessarily in delivering Quality of health, as determined in clinical terms (efficiency in diagnosis, response to treatment, recovery time, postop care, re-admissions, etc).
◆ This trend along with a techled “intrusion” into the provider-patient conversation requires a balancing act (as the next section shall explain)
(3) The rationing of care by providers who have faced delays in payments.
◆ This is certainly not desirable and goes against the principles with which UHC was incepted. Rationing can also be seen as a “reasonable” act of “self-preservation” by private operators, who need to make ends meet, with finite resources.
◆ Often, rationed care is not identifiable, since quality is not measured. In such instances, patients lose first and the society bears an invisible cost of poor-care.
◆ It would be very interesting to see businesses extract viable opportunities in addressing the very “handbrakes” that are impeding UHC currently.
◆ Health-fintech can together with Insurers resolve this by helping agencies identify genuine delivery, make the processing of claims seamless and
credit to providers, with some sovereign backing. This can help ensure continued liquidity in the system.
◆ Other perspectives and musings:
◆ Healthcare insurance is a very powerful tool and creates incentives that shape the behaviour of several actors in this drama. Ensuring a balance between process and novelty is crucial, as is the importance of gradually determining how “quality” is measured and “priced”.
◆ Could the answer to many of the systemic challenges impeding PMJAY be found in a PPP with private insurers? Is there a way to balance insured populations (and iron out asymmetries) through a PPP-esque trade off? Can state-sponsored incentives be created where blind-spot segments (for instance, “middle class senior citizens”) are inducted into private insurer pools?
Impact of technologyin revolutionising healthcare deliveryand financing
◆ Prime movers: Everyone + 1-debilitating-virus
◆ On the consumption side, we’ve witnessed wholehearted adoption of tech (ranging from large private providers signing HUGE cheques for cutting edge equipment to the common man, wielding a smartphone with his healthcare apps of choice and dud-cheap data).
◆ En masse creation of tech by Gen X, Y and Z has provided incredible value to the Industry, with 68k start-ups creating the “new".
◆ The Administration has also supported through schemes that initially facilitated capital good import and gradually now, a Make in India focus and generous allocations of upto Rs 15k crore to support this. But yes, the pandemic has (at a phenomenal, anguishing cost to life and wealth) whipped the entire citizenry up a steep digital learning curve. The healthtech market may well blossom into a USD 50 billion industry in the next 5-7 years.
◆ The impact till date:
EXPRESS HEALTHCARE May2024 22 cover )
◆ Undoubtedly tech (1) has enhanced accessibility, (2) is helping address the urban rural skew by making caregiving possible remotely, (3) is improving productivity of clinical talent, capacity allocations in hospitals, (4) making datadriven care and evidence based care possible in real time (5) increasing transparency and mobility through digitisation
◆ We have seen tech also spur healthcare financing directly:
(1) Subscription and demandbased Insurance models have arisen, (2) Healthcare crowd funding platforms have started getting traction as consumer awareness has arisen, (3) Loans for medical expenses are also becoming prevalent, with zero fee and interest free credit
◆ With improving digital infrastructure, capability to authenticate identities and validate requirements, transact securely
– all within a few taps is now a reality. The healthcare-fintech segment, which we estimate is sized at ~USD 2.5 billion is likely to touch USD 10 billion by the end of the decade.
◆ We believe financing interest in Healthcare IT systems will continue with a preference for platform plays that either (1) cover wider provider networks or (2) a broader set of consumer needs with consequent M&A spin-off activity. There will continue to be churn in protocols chosen as diverse IT systems coalesce. As much as this would result in shakeouts for businesses with limited
“hooks” on the provider, it presents ripe feeding ground for acquisitions and corporate venture capital
◆ Perverse emergent behaviours and remedies:
(1) The risk of over-investment and a motive for increased utilisation
◆ Hospitals, especially in urban settings, often look to raise their market standing and positioning by investing in state of the art facilities. This tendency is evident from the fact that nearly very hospital of repute in such markets projects its “technical sophistication”
◆ A sobering thought here is that not every patient that walks in requires “high end medical equipment”. There is a distinct possibility of an incipient “excess capacity” below the line, on an equipment level – especially in dense urban areas.
◆ And yet, the emergent behaviour puts pressure on other providers to mimic, raise costs to stay competitive on dimensions that may not impact patients as much.
◆ While larger operators attract a wider array of patients from the hinterland and can utilise such infra efficiently, mid-market operators may struggle to complete.
◆ Hospital-owners often break bank and procure the “next big thing”. In the absence of natural demand/patient flows, will this not create pressures where supply “drives” demand and an over-selling of unnecessary
care happens? Especially when there are wage-bills to settle and interests to cough up. Are equipment suppliers inadvertently exacerbating this behaviour through pay-per-use models? Evidence in other developed economies suggests that this is indeed a possibility
◆ The intent is not to cast aspersions on ethics. The most well-intentioned initiatives can unwittingly veer into treacherous territory.
◆ It often takes an experienced hand in the boardroom (often in the nature of a high pedigree investor), to identify these undercurrents and ensure the moral compass of the venture is realigned. Equally the wrong financial partner can unknowingly amplify these issues by creating pressure to increase bottomline without first ensuring the business is pursuing the right objectives.
(2) Over-reliance on tech and defensive medicine
◆ Increased digitisation, EMR, privity of provider-patient interactions has the downside of making clinicians sensitive to every recommendation they make.
◆ Healthcare cannot be reduced to entirely-deterministic protocol. Often, a patient’s context is unique, unpredictable and fuzzy and often cannot be closeted into set-patterns. Clinicians need to exercise novelty in such cases, use heuristics as much as they use data to chart out the road ahead
◆ If provider-systems were to over-enforce tech, it would naturally give rise to a tendency for clinicians to reduce their exposure to scrutiny.
◆ Similarly much like many of us reach for a calculator to do basic math, or google maps to head to our nearest grocery, a clinician that is over-supplied with tech/data may develop an unwholesome dependency on tech.
◆ Even here, healthcare financiers can help, by recognizing the boundaries of what is optimal and excessive.
(3) Ushering in value based care: Development of metrics, measuring and controlling
◆ It is our earnest hope that private players and healthcare investors can take the lead in terms of framing the tenets of value-based care intelligently and in doing so ensure that healthcare is not relinquished to SOPs cast-in-stone.
◆ We will eventually encounter the elephant in the room –namely the “pricing of care” and we believe that if handled responsibly, a societally acceptable answer to this can well emerge from private enterprise. Technology’s role here would be to faithfully reflect healthcare value-additive activities, costs, revenues and outcomes.
In conclusion: Bringing it all together
The purpose of this article was to cast some light on how, in a
complex system such as healthcare, every act of expansion is like throwing a pebble in a pond. The ripples can sometimes be rhythmic and beautiful. In some instances they can induce unintended turbulence of varying scales. It makes good business sense to try to grasp these shifts in behaviours and motivations of various segments and use it to shape strategy and policy. As we observed, even very noble endeavours create adverse behaviours by other actors (who also are acting either in self-preservation or optimising for other positive ends).
Healthcare financiers have a unique vantage point of having visibility of all actors, through their relationships and networks. They can witness, in some instances even prior to the incumbent prime-movers, the response that every stimulus elicits from this complex system. And it endows the healthcare investor with a unique responsibility to inform, educate and sometimes instruct the behaviour of various players so as to encourage behaviours that are socially tenable.
Ourapproachin this articleis surely not comprehensive given the sheer scale of the subject. Ithas beenillustrativeat best. We have placed our thoughts with you, to trigger a conversation that we would love to take forward, for the betterment of our industry.

May2024 EXPRESS HEALTHCARE 23
MEDTECH
INTERVIEW
Making Indian healthcare self-reliant in a global ecosystem
Shuba Nagesh ,Managing Director - GE BEL& General Manager- ISC South Asia,GE HealthCare in an interaction with Express Healthcare talks about the current landscape of medtech manufacturing in India
How has the landscape for local manufacturing in the medtech sector evolved over the years?
As per Invest India, India's medtech market is growing at an impressive 15 per cent CAGR. India’s disease burden is shifting from communicable, maternal, neonatal, and nutritional diseases to noncommunicable diseases like cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes. This shift, in turn, has catalysed a shift from curative healthcare to preventive healthcare. The burden calls for more optimised diagnosis with the use of precision diagnostic tools that integrate AI, big data for more accurate mapping of patient data and personalised treatment protocols.
Traditionally, India relied heavily on imports, but the focus is now shifting towards domestic production to improve affordability and accessibility. The Government is taking proactive steps by incentivising domestic production of high-quality medical devices through PLIProduction Linked Incentive and through Promotion of Research & Innovat ion in the Pharma sector (PRIP), attracting investments in medical devices segments. India’s medical devices manufacturing footprint is developing further in scale and geography, with 250+ organisations engaged in innovations for addressing critical health issues and dedicated medical devices

The evolving landscape for local manufacturing in the medtech sector reflects broader trends towards technological innovation,regulatory adaptation,Supply Chain Resilience,and market demand for more personalised,costeffective,and sustainable healthcare solutions
manufacturing clusters. Additionally, opening foreign direct investment in the medtech sector has facilitated collaborations and technology transfer, bringing global expertise to the Indian market.
The evolving landscape for local manufacturing in the medtech sector reflects broader trends towards technological inn ovation, regulatory adaptation, Supply Chain Resilience, and market demand for more
personalised, cost-effective, and sustainable healthcare solutions. The landscape for local manufacturing in the Indian medtech sector has evolved positively, driven by government support, regulatory reforms, market demand, technological advancements, and increased investment. This trend is expected to continue, further strengthening India's position as a hub for medical device manufacturing in the region.
There are many policies that are now favoring manufacturing in India. As a global medtech company investing in India, what are your views on the current policy ecosystem?
The policy ecosystem in India offers promising opportunities for global medtech companies,addressing challenges related to regulatory compliance, infrastructure, skills development, and intellectual property protection, essential for unlocking the full potential of the Indian market.
Collaborating with government stakeholders, the industry, and local partners, leveraging government programs, and adopting a long-term strategic approach has helped navigate the complexities and maximise the benefits of investing in India's growing healthcare sector. The government’s intervention through incentive schemes and the recent National Medical Devices Policy 2023
strengthens the aspiration of making India the global manufacturing hub and innovation hub for Medical Devices, growing R&D and innovation of futuristic medical technologies.
Many industries, including medical devices, share a common base of subcomponents’ manufacturing, and newer policies should focus on boosting electronics, PCB infrastructure, and raw material availability for the scale of growth that is being targeted. While the policy ecosystem focuses on the public healthcare institutions being encouraged to prioritise the procurement of domestically-manufactured medical devices, 80 per cent of the procurement is currently from the private sector and needs to be incentivised with economic benefit to buy locallymanufactured medical devices. Rebates could be provided to private healthcare providers buying locally manufactured medical equipment in underserved areas and for imported medical devices of similar specifications. Steps like extending Import of Goods at Concessional Rate of Duty (IGCRD) incentives for procurement from EOU (Export Oriented Unit) /EHTP (Electronic Hardware Technology Park) are currently applicable only for imported parts that are used in the local manufacturing of certain medical devices go a long way in strengthening localisation.
The policies aimed at
EXPRESS HEALTHCARE May2024 24
creating a conducive environment for medtech manufacturing, leading to increased domestic production, affordability & accessibility are much appreciated, and while the efforts to harmonise standards, facilitate exports, simplifying the regulatory process are underway, the speed of approvals (especially for products from platforms already approved ) is of the essence.
Even as we manufacture locally, healthcare expenses continue to impact patients. What can be done to address the talk on affordable care?
Affordability for citizens and patients through Government initiatives like Ayushman Bharat and the Pradhan Mantri Bhartiya Janaushadhi Yojana covers today about 37 per cent of the total population, and these health schemes offer standardised benefits and ensure that providers offer the best care to all pockets of our society. While the scheme itself can be strengthened to go deeper and broader, aspects like telemedicine, digital health platforms, and electronic medical records can further streamline processes, improve efficiency, and reduce administrative costs.
Addressing the issue of affordable healthcare requires a multifaceted approach:
Aggressively boosting healthcare infrastructure in government hospitals through advanced medical diagnostic infrastructure— preventative and therapeutic. Doubling down in both scale and quality of healthcare in government hospitals is the need of the hour for the 1.4 billion citizens of our country.
Strengthening policies to encourage local purchases, both in government and private hospitals.
Engaging and involving all stakeholders, including governments, healthcare providers, insurers, pharma companies, and medical
device manufacturers, to step up collaborative efforts through public and private healthcare partnerships, leveraging strengths and addressing gaps. Conscious advancement in services, preventive healthcare schemes, value-based care, healthcare financing, technology, inn ovation, and regulatory reforms can help create strong healthcare infrastructure. These strategies, if executed in a coordinated manner, can work towards making healthcare more affordable and accessible for all individuals, ultimately improving health outcomes and enhancing overall wellbeing.
When we speak about ‘Make in India’, what is GE HealthCare’s vision in India?
India is committed to achieving ‘Universal Health Care for All’ by 2030, and GE HealthCare aims to be at the forefront of that movement by leveraging its global expertise in innovative medical technology to design better tools that combine better clinical outcomes with accessibility and affordability. As a country that has the potential to become the medtech manufacturing hub of the world, India’s greatest strength lies in its dynamic demographic. At GE HealthCare, we are investing in research and development to create innovative medical technologies specifically designed for the needs of the Indian population. This will not only improve access to cutting-edge healthcare but also create intellectual property within the country. Our presence in India, both as one of the largest global engineering and manufacturing hubs, has positioned us to expand and scale up our manufacturing footprint to serve increasing needs production and reduce dependence on imports to make medical devices more affordable and accessible. Our vision for, and in India has always been to bring
together a fragmented medtech ecosystem by leveraging indigenous R&D to curate products and services, manufactured in India for the world to make healthcare more accessible, affordable, precise, and connected.
Nearly three decades ago, we embarked on our manufacturing journey in India through thriving joint ventures in South Asia with Wipro and BEL. Presently, our operations in India are conducted through four manufacturing facilities that produce a wide range of medical technologies, including CT scanners, Cath lab equipment, ultrasound scanners, patient monitoring solutions, ECG machines, and ventilators, including hitech subsystems like X-Ray Tubes, High Voltage Generators, among others.
In 2022, Wipro GE Healthcare launched the Medical Device Manufacturing (MDM) facility in Bengaluru under the Indian government’s Production Linked Incentive (PLI) Scheme, aligning with the National Agenda of Atmanirbhar Bharat. The vision was to encourage local manufacturing of medical devices in the country. The greenfield facility had set up 24/7 operations for manufacturing CT machines, Cath lab equipment ultrasound scanners, patient monitoring solutions, ECG machines, and ventilators.
Could you discuss some of your products or services catering to the country’s local needs?
The organisation’s emphasis on localisation is evident in our product lineup, with landmark achievements such as the Mac 400 ECG Machine (2007) and the Made in India PET CT system for cancer diagnosis (2014). In 2022, we launched Revolution Aspire at Wipro GE Healthcare’s MDM plant, which is an advanced imaging solution designed and manufactured end-to-end in India. Our first Revolution ACT was designed and manufactured
in India, which was more affordable and compact than previous models, making it ideal for smaller hospitals and clinics, in keeping with the needs of the existing Indian healthcare facilities. Our Revolution Aspire CT system was another end-toend Make in India CT Scanner designed for higher clinical efficiency aimed at addressing the needs of tier 2 and 3 cities.
GE HealthCare has been at the forefront in R&D and Engineering since it was established in the John F. Welch Technology Center in 2000, boasting a team of over 1800 engineers and technologists. This center has been instrumental in developing innovative solutions, filing over 1100 patents, and delivering cutting-edge products. Additionally, our commitment to innovation is evident in initiatives such as the establishment of the brand’s first 5G inn ovation lab in Healthcare Technology Centre India (HTCI) Bengaluru – the first for GE HealthCare, globally.
Beyond manufacturing and R&D, our expansive service organisation plays a crucial role in maintaining the quality and reliability of our products. The GE HealthCare team is dedicated to servicing and maintaining equipment in hospitals, ensuring that our products consistently meet the highest standards of performance and reliability.
GE HealthCare offers a range of products and services tailored to address the specific healthcare needs of India. Here are some examples:
◆ Affordable diagnostic imaging solutions: We provide a variety of diagnostic imaging solutions designed to meet the needs of healthcare facilities across India, from large urban hospitals to smaller clinics in rural areas. These solutions include X-ray systems, ultrasound machines, and computed tomography (CT) scanners that are affordable, reliable, and easy to use.
◆ Maternal and infant care solutions: Given the importance of maternal and infant health in India, we offer specialised products and services to support maternal and neonatal care. This includes fetal monitoring systems, incubators, and neonatal intensive care unit (NICU) equipment designed to ensure the health and safety of mothers and newborns during childbirth and the postnatal period.
◆ Cardiovascular health solutions: We provide a range of cardiovascular imaging and monitoring solutions, including electrocardiography (ECG) machines, echocardiography systems, and cardiac stress testing equipment, to help healthcare providers diagnose and manage heart conditions effectively.
◆ Digital healthcare solutions: We offer digital healthcare solutions that leverage technology to improve access to healthcare services and enhance patient care outcomes. This includes telemedicine platforms, remote monitoring systems, and electronic health record (EHR) systems that enable healthcare providers to deliver care more efficiently and effectively, particularly in remote and underserved areas.
◆ Community health initiatives: GE HealthCare is involved in community health initiatives aimed at improving health outcomes and raising awareness about preventive healthcare practices. This includes partnerships with local healthcare organisations, NGOs, and government agencies to provide screenings, vaccinations, health education programs, and other community-based interventions.
By offering innovative solutions, supporting healthcare infrastructure development, and promoting capacity building and community engagement, GE HealthCare aims to make a positive impact on healthcare delivery and outcomes across India.
May2024 EXPRESS HEALTHCARE 25
HEALTHCARE IT
Prescribing innovation: HowAI is revolutionising the healthcare sector
Munira Loliwala,AVP- Strategy and Growth,TeamLease Digital stresses that from revolutionising diagnostic techniques to streamlining administrative processes,the influence of digital solutions is permeating every facet of this critical domain
Technology’s relentless progress has revolutionised businesses across industry verticals and the healthcare sector is no exception. Today, the profound impact of technology and Artificial Intelligence (AI) on healthcare practices is becoming increasingly palpable. In this dynamic landscape, these cutting-edge advancements are poised to redefine the very essence of patient care, transforming it into a more personalised, efficient, and datadriven endeavour.
The healthcare industry, once rooted in traditional methods, is now witnessing a seismic shift as technology seamlessly integrates with medical practices. From revolutionising diagnostic techniques to streamlining administrative processes, the influence of digital solutions is permeating every facet of this critical domain. The burgeoning field of telemedicine, for instance, has bridged geographical barriers, enabling patients to access quality healthcare services from the comfort of their homes, a boon in regions grappling with resource constraints.
AI & data-driven healthcare: Precision & personalisation
Moreover, the advent of AI and machine learning have ushered in a new era of precision medicine, where algorithms can analyse vast troves of data, unravelling intricate patterns and insights that were previously obscured. This data-driven approach not only enhances diagnostic accuracy but also paves the way for tailored treatment plans, optimising patient outcomes and reducing the strain on healthcare resources.

With the total healthcare market in India estimated at a staggering USD 367 billion, and the Indian health technology market projected to grow at an impressive annual rate of 22 per cent, reaching USD 35.8 billion by 2030, the potential for technology to revolutionise healthcare delivery in the country is immense.
As we delve deeper into this transformative journey, it becomes evident that the synergy between technology and healthcare holds the promise of a more efficient, accessible, and personalised healthcare ecosystem, one that prioritises patient well-being while embracing the cutting edge of innovation.
Transforming job roles: The impact on healthcare careers
The proliferation of AI and other disruptive technologies within the healthcare sector is poised to reshape the job landscape profoundly. As these cutting-edge innovations permeate medical practices, a new wave of roles and skill sets is
emerging, redefining the traditional workforce dynamics. Consequently, certain positions are anticipated to be in high demand, commanding lucrative salaries and promising career prospects.
One such role that is gaining traction is that of data scientists. With the healthcare industry generating vast amounts of data, the ability to analyse and extract valuable insights from this information is paramount. Data scientists, adept at leveraging advanced analytical techniques and machine learning algorithms, play a crucial role in uncovering patterns and trends that can inform decision-making and drive precision medicine initiatives. As the healthcare sector continues to embrace datadriven approaches, the demand for these professionals is expected to soar, making it a highly sought-after and wellcompensated career path.
Technology: Catalysing transformation
The impact of disruptive technologies, particularly AI, within
the healthcare sector, cannot be overstated. These innovations are revolutionising virtually every aspect of medical practice, from diagnosis and treatment to patient care and administrative processes. The convergence of health and technology, often referred to as digital health, is driving this profound transformation.
Telemedicine, for instance, has gained significant traction, enabling remote consultations and bridging the gap between patients and healthcare providers. Medical virtual assistants, powered by AI, are enhancing patient experiences by providing personalised support and guidance. Additionally, selfmonitoring healthcare solutions empower individuals to take an active role in managing their well-being, contributing to preventative care efforts.
Further, the integration of big data, blockchain, and epharmacy platforms is streamlining operations, improving data security, and enhancing the accessibility and affordability of healthcare services. These disruptive technologies are not only optimising existing practices but also paving the way for entirely new business models and revenue streams within the industry.
The hiring landscape
With India’s health-tech market expected to grow by an impressive 25 per cent between 2024 and 2028, the demand for skilled professionals in this evolving sector is soaring. With the digital health market projected to expand from USD 12.20 billion in 2023 to USD 25.64 billion by 2027, the hiring landscape is undergoing a significant transformation.
Roles such as data scientists, developers, cybersecurity
specialists, technical development engineers, quality testing professionals, and design experts are anticipated to be in high demand. These positions require a unique blend of technical expertise and industryspecific knowledge, making them highly sought-after in the ever-evolving healthcare ecosystem.
Additionally, the rising adoption of artificial intelligence is expected to surge the growth of tech employees in India by almost 33 per cent as of FY 2025, compared to FY 2024, which witnessed an average rise of 15 to 20 per cent. This surge in demand is driven by the implementation of AI-powered solutions across various healthcare domains, including diagnostics, treatment planning, and patient monitoring.
Fostering growth and unlocking potential
To facilitate the growth of the digital health market and capitalize on the potential of emerging technologies, collaborative efforts from both the public and private sectors are crucial. Government incentives and Production-linked Incentive (PLI) schemes play a vital role in fostering an environment conducive to innovation and investment.
Finally, the monetisation of healthcare educational infrastructure, leveraging digital universities and institutes, and promoting healthcare-focused research and development initiatives will unlock the true potential of this burgeoning sector. By nurturing a skilled workforce and cultivating an ecosystem that embraces technological advancements, India can position itself as a global leader in the digital health revolution.
EXPRESS HEALTHCARE May2024 26
Whyclinicians need the right messaging platforms
Rohit Singh,Managing Director,Feedback Medical India explains how use of public messaging platforms is non-compliant with the Data Protection Act
Digital inn ovation plays a pivotal role in enhancing medical imaging and clinical communication in the rapidly evolving landscape of healthcare. Clinicians, now more than ever, require efficient tools for communication to make timely and well-informed clinical decisions. These tools not only facilitate quick decision-making but also grant clinicians access to clinical data, including vital medical images, anytime and anywhere.
Moreover, such platforms enhance clinicians' ability to collaborate both onsite and remotely, enabling seamless two-way communication with fellow clinicians, patients, and nursing staff. However, despite the convenience these platforms offer, there's a lurking danger when clinicians resort to public messaging platforms for clinical data sharing and communication. This poses a significant risk to patient data safety and may lead to non-compliance with data protection regulations, such as the Data Protection Act 2023.
Howuse of public messaging platforms is non-compliant with the Data Protection Act

When selecting secure messaging platforms,clinicians must consider key factors such as encryption protocols, authentication,consent management mechanisms,and access controls
Whether you're a hospital, running a clinic, diagnostic labs, or any healthcare delivery organisation, communication is key for your team for operational efficiency and productivity. However, the use of public messaging platforms for clinical communication purposes raises the risk of patients’ data safety and noncompliance to the Digital Personal Data Protection (DPDP) Act 2023. Non-compliance has a risk of monetary fines up to Rs 250 Cr (and more in some cases).
The DPDP Act is an Act to provide for the processing of digital personal data in a manner that recognises both the right of individuals to protect their personal data and the need to process such personal data for lawful purposes and
for matters connected therewith or incidental thereto.
In the realm of healthcare, personal data encompasses a broad spectrum, ranging from health records to personally identifiable information. This data is entrusted to hospitals, doctors, and healthcare or-
ganisations, who serve as custodians or data fiduciaries. These fiduciaries, whether acting alone or in collaboration with others, hold the responsibility of determining the purpose and methods of processing this sensitive information.
The data principals, comprising patients of all ages, including adults, children (alongside their parents or lawful guardians), and individuals with disabilities, entrust their personal data to these fiduciaries. This data undergoes various processing activities, including collection, recording, storage, retrieval, and sharing, among others, to facilitate effective healthcare delivery. It is essential that these processes adhere to strict privacy and security standards to safeguard the confidentiality and integrity of individuals' personal health information. Thus, within the healthcare ecosystem, the responsible handling and processing of personal data plays a critical role in upholding patient trust and ensuring the delivery of quality care.
Secure
messaging platforms offer numerous benefits to clinicians and healthcare organisations
Enhancing patient confidentiality: Secure messaging platforms facilitate confidential communication among healthcare professionals, ensuring the privacy of patient data.
Streamlining collaboration and care coordination: Effective communication enables seamless collaboration and care coordination among healthcare providers, leading to improved patient outcomes.
Improving time and cost efficiency: Secure messaging offers a more efficient means of exchanging information compared to traditional methods, reducing operational costs, and enhancing productivity. Healthcare-specific messaging platforms, when integrated seamlessly with other IT systems, ensure patient discussions are documented, accessible, and referenced by relevant clinicians. Public messaging platforms lack this capability, making them unsuitable for secure and comprehensive patient record management. When selecting secure messaging platforms, clinicians must consider key factors such as encryption protocols, authentication, consent management mechanisms, and access controls. Robust encryption protocols ensure the confidentiality of patient data during transmission, while strong authentication mechanisms verify user identity and prevent unauthorised access. Consent management ensures that heath data is processed after disclosing purpose and receiving consent. Defined access controls limit user permissions, mitigating the risk of data breaches and ensuring compliance with privacy regulations.
In today's digital era, protecting patient data and privacy is essential, and secure messaging platforms play a crucial role in achieving this goal. By adopting the right messaging platforms and adhering to best practices in implementation, clinicians can safeguard sensitive patient information, foster trust and confidence among patients, and ultimately advance healthcare delivery.
May2024 EXPRESS HEALTHCARE 27






















BUSINESS AVENUES EXPRESS HEALTHCARE May2024 EXPRESS HEALTHCARE 28


HemantSurgical offersend-to-endturnkeysolutionsfordialysiscentre setup,encompassingeverythingfrominitialplanningtofinalimplementation.




BUSINESS AVENUES EXPRESS HEALTHCARE EXPRESS HEALTHCARE May2024 29
CENTERSETUP
DIALYSIS
24x7Support Team GlobalBiomedical EngineersNetwork 25Yearsof TurnkeyExpertise 4000+Successful Installations www.hemantsurgical.com CONTACTUS +919619484952 Wearecommittedtodeliveringthehigheststandardsofqualityinevery aspectofourwork,fromequipmentselectiontostafftraining,toenhance patientoutcomesandsatisfaction.
RevolutionizeBloodProductVerificationwith InnovativeIrradiationConfirmationMethod

KEYFEATURES:
➨ Simplicitywithin-depthinsights.
➨ FunctionsasaYES/NOdevice,ensuringcompliancewithEuropean/UK/AABBguidelinesfordoseranges.
➨ Adaptabletosyringes,especiallysuitableforneonatalapplications.
➨ AvailableinbothGammaandX-rayversions.
➨ Soleindicatorguaranteeingthatthedelivereddosealignswithrecommendedlimits(25Gyto50Gy) forbloodanditscomponents.
➨ Includesprintedlotnumber(barcode)andexpirationdatefortraceability.
➨ Swiftorderprocessingwithacommitmenttoqualityandexceptionalcustomerservice.

No.127,BussaUdyogBhavan,TokershivrajRoad,SewriWest,Mumbal-400015,Maharashtra, Landline:+91022-24166630/Mobile:+919833286615/Email:support@rosalina.in/Website:www.rosalina.in

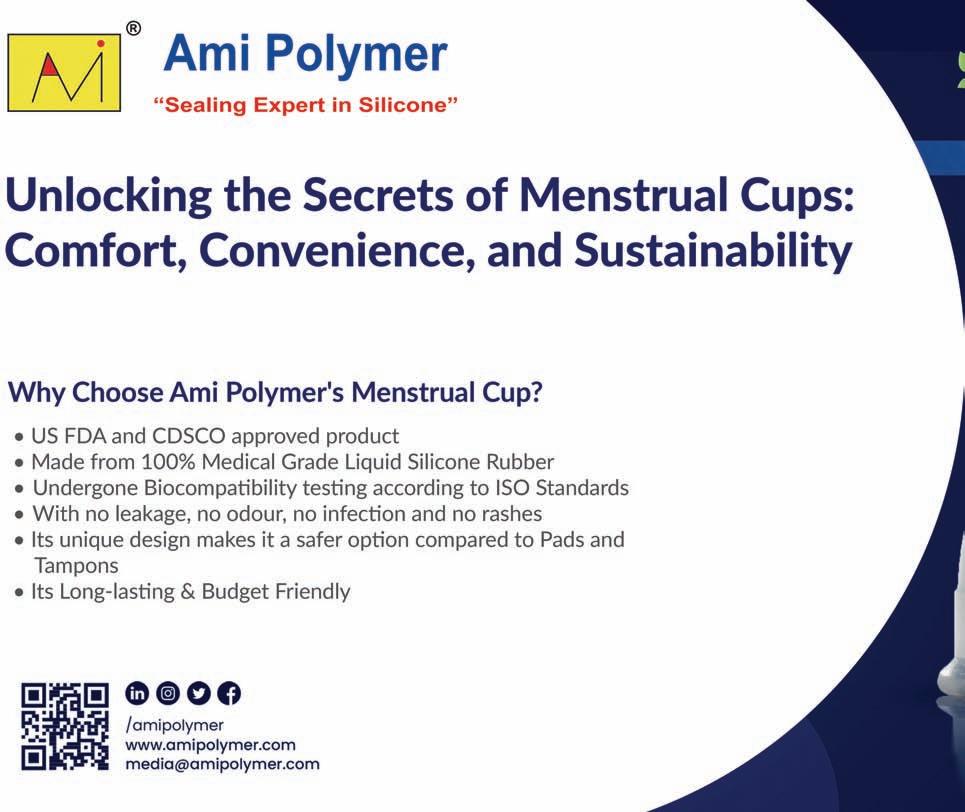
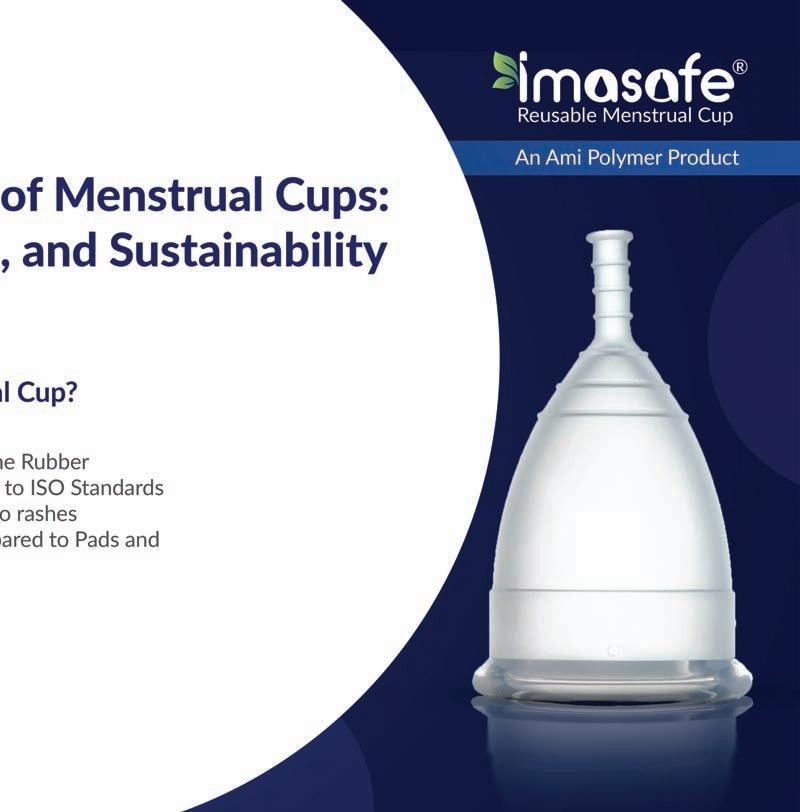




AVENUES EXPRESS HEALTHCARE May2024 EXPRESS HEALTHCARE 30
BUSINESS
























CovertheLengthand BreadthofIndia
India's Largest & No.1 Healthcare Event & Hospital needs Exhibition 234 38th Edition| AUG2024 CHENNAINEWDELHI 39th Edition| OCT2024 567 BUSINESS AVENUES EXPRESS HEALTHCARE EXPRESS HEALTHCARE May2024 31
58,000sqmtofexhibitionspace Forenquiries:+917305789789|www.medicall.in|info@medicall.in
HEALTHCARE TRACKER
Strain echocardiography: Arevolutionary tool in cardiovascular imaging
BN Pandey,National Product Manager-Cardiac Ultrasound,BPLMedical Technologies highlights that in recent years,strain echocardiography has emerged as a revolutionary technique,providing valuable insights into myocardial function,and offering a more comprehensive understanding of cardiac mechanics
Cardiovascular diseases
are a leading cause of morbidity and mortality worldwide, affecting adults of all ethnicities, ages, and sexes, emphasising the need for advanced diagnostic tools to identify, assess, and manage cardiovascular conditions. In recent years, strain echocardiography has emerged as a revolutionary technique, providing valuable insights into myocardial function, and offering a more comprehensive understanding of cardiac mechanics.
Understanding strain echocardiography
Strain echocardiography is a non-invasive imaging test used to measure the deformation or strain of myocardial tissue during the heart’s contraction and relaxation cycle. Unlike traditional echocardiography, which primarily focuses on global and regional wall motion, strain echocardiography provides detailed information about the myocardial deformation in both longitudinal and circumferential directions.
Types of strain
Longitudinal strain: Evaluates the deformation of the my-
ocardium along the long axis of the heart. Longitudinal strain is crucial for assessing the function of the subendocardial layer and is particularly valuable in detecting early changes in myocardial function.
Circumferential strain: Assesses the deformation of the myocardium in the circumferential direction, providing insights into the mid-myocardial layer. Circumferential strain is essential for assessing overall myocardial function and is particularly relevant in conditions such as myocardial infarction.
Radial strain: Measures the deformation of the myocardium in the radial direction, perpendicular to the endocardial surface. Radial strain is crucial for assessing the function of the subepicardial layer and is often used in conjunction with other strain parameters for a comprehensive evaluation.
Clinical applications
Early detection of myocardial dysfunction: Strain echocardiography is highly sensitive in detecting subtle changes in myocardial function, enabling early identification of cardiac

dysfunction before overt symptoms or structural abnormalities occur.
Monitoring cardiotoxicity: In patients undergoing chemotherapy or other treatments that may have cardiotoxic effects, strain echocardiography is a valuable tool for monitoring myocardial function and detecting early signs of cardiomyopathy.
Ischemic heart disease: Strain echocardiography aids in the assessment of ischemic heart disease by providing detailed information about regional myocardial function. It helps identify areas of impaired strain, indicative of myocardial ischemia or infarction.
Valvular heart disease:

Strain echocardiography complements traditional assessments in valvular heart diseases by offering additional information on myocardial mechanics. It aids in surgical decision-making and postoperative monitoring.
Choosing the right tool for cardiac imaging
Strain echocardiography is a powerful technique for assessing myocardial functioning. With the versatile BPL Alpinion ECUBE 8 series of ultrasound system, healthcare professionals can harness the full potential of strain echocardiography and much more.
The BPL Alpinion ECUBE 8 series is equipped with dedicated advanced software for Strain Echocardiography with Bull’s eye, capable of precise and comprehensive assessment of myocardial strain for all 4 chambers of the heart. Suitable for adult as well as paediatric patients, its Single Crystal Phased Array probes provide crystal clear and detailed image quality in very high frame rates in both 2D as well as colour doppler imaging.
Beyond strain echocardiog-
raphy, the ECUBE 8 series offer several advance features in Cardiac Imaging, such as the Auto EF calculation, stress echo, and tissue doppler imaging. With its single crystal convex probe, the ultrasound system can also be used in shared services, making it an adaptable solution for varied imaging needs.
Explore the features of the ECUBE 8 Series by visiting our website. You may also experience the full capabilities of the ECUBE 8 Series firsthand. Book a quick product demo to see it in action.
Strain echocardiography has emerged as a powerful tool in the field of cardiovascular imaging, providing clinicians with a more nuanced understanding of myocardial mechanics. Its ability to detect subtle changes in myocardial function early on makes it an invaluable asset in the diagnosis and management of various cardiac conditions. As technology continues to advance, strain echocardiography is likely to play an increasingly significant role in improving patient outcomes and enhancing our understanding of cardiovascular diseases.
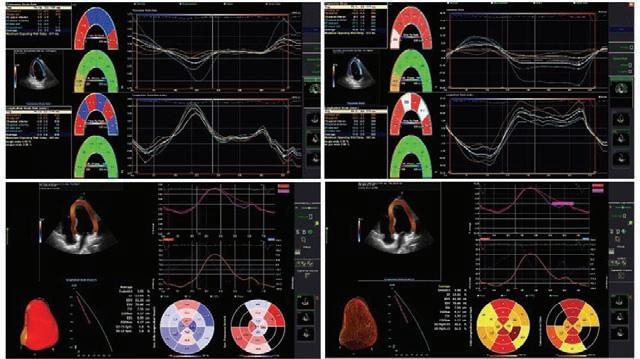
EXPRESS HEALTHCARE May2024 32
Sysmexadvanced technologies enabling tomorrow’s haematologytesting
Sachin Rajguru,Deputy Product Manager – Haematology (XN-L& 3 Part),Marketing Department, Sysmex explains about Sysmex’s technology advancement in XN and XN-LSeries analyzers
Sysmex analysers are known around the world for their reliability, accuracy and quality. Since we were founded nearly half a century ago, we have been driven by the desire to innovate so that both you and we can do our jobs better. To improve the analysis capabilities of our devices so clinicians can help people more effectively. In those near-on fifty years it is fair to say we have changed the haematological analysis landscape. And nowadays we are the global leader in the haematology market. This is largely due to our focus on knowledge and technology-backed up by service and solution-based thinking.
Modern automated blood cell counters use various technologies to determine the parameters of a full blood count. When EDTA blood samples are aspirated by the analyser, blood is aliquoted (separated into small portions before being used in the various channels) and treated with various reagents to support the cellspecific properties. Next the analyser uses a range of technologies to investigate the content of the sample. Modern additions to the workflow include automatic smear-making, staining and digital imaging. Sysmex literally covers all the bases of the haematology laboratory. It offers laboratories a full range of haematology platforms with a depth of clinical focused haematological parameters. These comprehensive solutions provide powerful productivity and efficiency, ensuring the accurate delivery of relevant information to clinicians.
Although the first automated hematology analyzers were launched in the 1950s, the adoption rate of these analyzers was insignificant. The

adoption was slow because of the high operational cost as well as capital expenditure. At that point in time, peripheral smears (PS) were the preferred choice for99 percent of laboratories in India. However, this method was time-consuming, and the results too were not reliable.
Over the years, there has also been an increasing demand for compact, powerful, and affordable analyzers to provide accurate and reliable differential analysis of blood counts. Common requirements include high throughput, simplified testing process, broad parameter ranges, smaller footprint, minimum blood volumes to cater to pediatric and point-of-care applications, reduce manual work and further increase the efficacy and productivity of laboratories.
Moreover, the first analyzers launched and currently available 3-part differential analyzers too are based on electrical impedance technology. In the 1980s, this technology was supplemented with optical flow cytometry to allow differentiation of the white blood cells (WBCs) into their five subgroups (neutrophils, lymphocytes, monocytes, eosinophils, and basophils) in an automated manner.
Our XN-L Series, 6-part dif-
ferential haematology analysers use fluorescence flow cytometry as the prime detection method for white blood cells (WBC), WBC differential, Immature Granulocytes (IG) Reticulocytes (RET), Reticulocytes-Haemoglobin (Ret-He), Immature Platelet Fractions (IPF) and much more.
Sysmex“CORE” Technologies
a. Fluorescence Flow Cytometry (FFC)
Fluorescence flow cytometry is used to analyse physiological and chemical properties of cells. In flow cytometry, cells are examined while they are flowing through a very narrow flow cell. XN-L Series utilises the same core technology as high-end haematology analysers - the proven and reliable laser flow cytometry - to count and analyse cells. After the cells are irradiated by the laser beam, the forward scattered light (FSC), side scattered light (SSC) and side fluorescent light (SFL) of the cells are analysed. The three signals are used to differentiate and count cells with the help of unique digital technology and algorithms. Cells with similar physical and chemical properties form a cluster in a graph known as a scattergram.
b. Hydrodynamic DC sheath flow detection
Sysmex analysers use the DC sheath flow detection method to count red blood cells and platelets. The method reduces interference errors and the possibility of abnormal cell pulse detection, which could be caused by cells passing through the transducer off-centre. As soon as the cells have passed the orifice, they are seized by another, inverse flow and immediately led to the drain. This prevents renewed circulation and a change in the platelet count.
With Sysmex’s technology advancement in XN and XN-L Series analyzers with Fluorescence Flow Cytometry (FFC) method, it allowed the labs to access more cellular information than was ever available before through routine CBC with differential. These analyzers enumerate exclusive clinical parameters in addition to the conventional parameters enumerated by a basic 5-part differential analyzers.
XN-L Series enumerate advanced clinical parameters like Ret, Ret-He, IPF which are of additional clinical relevance for hospitals with multispeciality functionalities like oncology , nephrology etc. Ret-He, IRF along with reticulocyte count is helpful for anaemia management, IG for infections, IPF for screening and monitoring of thrombocytopenic disorders.
These are compact fully-automated 6-part differential hematology analyzer designed to meet today’s laboratory needs by providing enhanced clinical values that only XN-Series were previously able to provide, while improving operational efficiency in the laboratories.
The factor that drives growth of the hematology test-
ing market is the enhanced capabilities of the analyzers, such as expanded range of reported parameters and functionality to create high-value added testing.
Sysmex, a front runner in In-vitro diagnostics in India has acquired market leadership in Haematology with more than 22,000 successful installations across India with customer base starting from smaller stand-alone Pathology laboratories to India’s largest sample processing labs. Sysmex Analysers are preferred choice and used by Pathology labs since 1993, the year in which Sysmex started selling their quality products in India through then distribution network. Over the years and with advance quality products, Sysmex customer base and acceptance increased in India many folds.
XN-LAnalyzers: Benefits at a Glance
✓ US-FDA approved
✓ Fluorescent Flow Cytometry method measures not only cell size, but also the intracellular information and nucleic acid content
- Reliable differentiation of immature and other abnormal cells, such as IG
- Accurate measurement of low WBC / PLT count
✓ Hydrodynamic DC sheath flow detection method eliminates potential errors in cell counters such as coincidence, recirculation and stress changes
✓ Immature granulocytes (IG) with every differential analysis aids in the early prediction of infection and inflammation
✓ iRBC flag for Malaria screening
✓ Upgradability to RET, IPF, Low-WBC, Body Fluids parameters
May2024 EXPRESS HEALTHCARE 33
HEALTHCARE TRACKER
Understanding cervical cancer
Ruchi Sanghavi,Domestic Marketing Executive,Ami Polymer talks about cervical cancer,its causes,symptoms and also throw light on the ways to prevent it
What is cervical cancer?
Cervical cancer is a type of cancer that occurs when abnormal cells grow in the cervix, the lower part of a woman's uterus.
It is one of the more prevalent cancers among women, but if detected early, it can be prevented or effectively treated.
What causes cervical cancer?
◆ Certain types of human papillomavirus (HPV), mainly spread through sexual contact, can lead to cervical cancer if the infection persists.
◆ Smoking can heighten the chances of developing cervical cancer.
◆ Individuals with weakened immune systems are at a higher risk of cervical cancer.
◆ Starting sexual activity early in life can increase the risk.
◆ Having multiple sexual partners or a history of sexually transmitted infections (STIs) can also raise the risk of HPV infection and, consequently, cervical cancer.
Symptoms of cervical cancer
◆ Unusual vaginal bleeding, like bleeding between periods, after sex, or post-menopause.
◆ Pelvic pain unrelated to menstrual cycles or intercourse.
◆ Discomfort during sex.
◆ Abnormal vaginal discharge, which might be watery, bloody, or have a bad smell.
◆ Changes in menstrual patterns, such as heavier or prolonged periods.
◆ Lower back or pelvic discomfort or pain.
Preventing cervical cancer
◆ Being vaccinated against high-risk types of human papillomavirus (HPV) can greatly decrease the likelihood of developing cervical cancer.
◆ Regular Pap smears or cervical screening tests can detect any abnormal cervical changes early, allowing for prompt treatment.
◆ Practicing safe sex by using condoms can lower the risk of
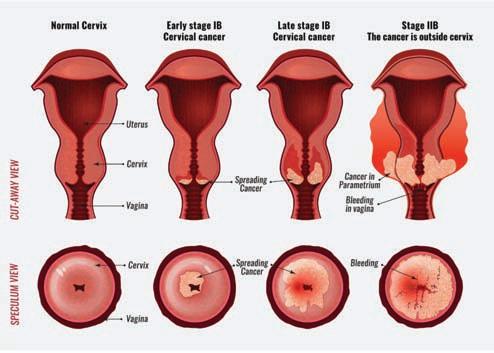


Being vaccinated against highrisk types of HPVcan greatly decrease the likelihood of developing cervical cancer
HPV and other sexually transmitted infections (STIs) associated with cervical cancer.
◆ Quitting smoking or avoiding exposure to second-hand smoke is crucial since smoking increases the risk of cervical cancer.
◆ Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and a healthy weight, supports overall well-being and lowers the risk of cancer.
◆ Using sterilised menstrual cups reduces the risk of introducing harmful bacteria or infections that could contribute to cervical cancer.
◆ Opting for medical-grade silicone in menstrual cups minimises the risk of adverse reactions or complications that could indirectly affect cervical health.
Conclusion
Cervical cancer can be avoided by being vaccinated, undergoing regular screenings, and making healthy lifestyle decisions. Early detection and proactive healthcare are vital for women's health. Collaborative actions to spread awareness and implement preventive measures play a crucial role in effectively fighting against this disease.
 Author – Ruchi Sanghavi Domestic Marketing Executive ruchi.s@amipolymer.com
Author – Ruchi Sanghavi Domestic Marketing Executive ruchi.s@amipolymer.com
EXPRESS HEALTHCARE May2024 34
HEALTHCARE TRACKER
Drager unveils Vista 300 in India
New patient monitoring system revolutionises hospital-wide information flow
Mumbai, 16 April 2024: Dräger, a global leader in medical and safety technology, announces the launch of Vista 300 in India, a groundbreaking patient monitoring system designed to streamline information flow across hospital departments.
The Vista 300 system offers continuous end-to-end data transfer from the patient's bed to the Hospital Information System (HIS), providing medical professionals with access to critical clinical care information along the entire patient pathway, from the Emergency Room (ER) to the Intensive Care Unit (ICU) and Neonatal Intensive Care Unit (NICU).
Keyfeatures of the Vista 300 system include:
Seamless integration of patient data, vital signs, and therapy device data into clinical workstations.
Easy configuration and intuitive user interface for clear display of information from multiple sources.
Extended data management capabilities with additional components such as the Vista spot check monitor, central monitoring station, gateway software, and viewer stations.
Shalin Patel, Managing Di-

New patient monitoring system revolutionises hospital-wide information flow
rector of Draeger India Group, expressed excitement about the launch, stating, "At Dräger, we are committed to innovation and excellence in healthcare technology. The Vista 300 system represents a significant advancement in patient monitoring, enabling medical professionals to provide optimal care while optimising workflows."
"The Vista 300 system is designed to meet the diverse needs of medical professionals in acute care settings. Its seamless integration with therapy devices and hospital networks ensures efficient data exchange and enhances patient care,” said Dhritimay Dhar, Vice President - Sales and Market-
ing, Medical business, highlighting the system's versatility and connectivity.
The Vista 300 system for adults, pediatric patients, and neonates provides not only data from connected devices but also supports cross-departmental workflows within the hospital. Its advanced networking capabilities allow for easy access to patient and therapy information, while ensuring data security through encryption and controlled user authentication.
The Vista 300 is manufactured by Drägerwerk AG & Co. KGaA.
For more information about the Vista 300 patient monitoring system, please visit Vista 300 | Draeger
Dräger.Technologyfor Life®
Dräger is an international leader in the fields of medical and safety technology. Our products protect, support, and save lives. Founded in 1889, Dräger generated revenues of around € 3.4 billion in 2023. The Dräger Group is currently present in over 190 countries and has more than 16,000 employees worldwide. Please visit www.draeger.com for more information.
May2024 EXPRESS HEALTHCARE 35
Hemant Surgical: Pioneers in Turnkey Dialysis Center Solutions for 25 Years
Beyond equipment provision,Hemant Surgical goes the extra mile by offering extensive training and support to healthcare professionals operating the dialysis centers
For over two decades, Hemant Surgical has been the go-to solution provider for dialysis center setup, completing over 80 projects across African countries. Their expertise extends globally, exemplified by their achievement in establishing India's largest 100-bedded dialysis center at a prominent Gurudwara in Delhi. This landmark project underscores their commitment to advancing renal care infrastructure, not only in India but also in underserved regions worldwide.
Setting up a dialysis center
requires meticulous planning, precise execution, and top-notch equipment. Hemant Surgical understands these requirements like no other. Their turnkey solutions encompass every aspect of establishing a dialysis center, from initial planning and layout design to equipment installation and staff training.
One of the key strengths of Hemant Surgical is its team of highly skilled biomedical engineers spread across the globe. These professionals bring a wealth of experience and expertise to every project, ensuring that each dialysis center is
set up to the highest standards and complies with all regulatory requirements.
Moreover, Hemant Surgical’s commitment to quality is unwavering. They partner with leading manufacturers of dialysis equipment to offer state-of-theart machines, ensuring optimal performance and patient safety. Whether it's hemodialysis machines, water treatment systems, or ancillary equipment, Hemant Surgical provides a comprehensive range of products tailored to meet the unique needs of each dialysis center. Beyond equipment provi-
sion, Hemant Surgical goes the extra mile by offering extensive training and support to healthcare professionals operating the dialysis centers. From technical training on equipment maintenance to clinical education on best practices in dialysis care, the company ensures that staff members are well-equipped to deliver exceptional care to patients.
Furthermore, Hemant Surgical’s global presence allows them to serve clients from diverse geographical locations. Whether it's in bustling urban centers or remote rural areas,
the company has demonstrated its ability to deliver turnkey solutions efficiently and effectively, contributing to the advancement of renal care on a global scale.
In conclusion, for those seeking to establish a dialysis center with unparalleled quality and expertise, Hemant Surgical stands out as the ultimate onestop solution provider. With 25 years of industry experience and a global network of biomedical engineers, they continue to set the benchmark for excellence in turnkey dialysis center setup.
AiMeD and DRISPjoin hands to give a boost to bilateral medical device trade
Indian Embassy in Moscow bats for tapping potential of Indo-Russian medical device industry through collaborative efforts
Given the enormous opportunities in the medical device industry for multifaceted bilateral engagements, experts from India and Russia have vouched for faster efforts to give a boost to collaborations to make the most of emerging opportunities in the areas of manufacturing and marketing lifesaving medical equipment and devices.
“The support extended by Indian Embassy in Moscow in our collective efforts to mutually cash in on emerging opportunities in medical device industry will go a long way in giving a further fillip to bilateral trade ties between two nations,” said Rajiv Nath, Forum Coordinator, Association of Indian Medical Device Industry (AiMeD).
Nath informed that experts
from India and Russia at a recently held webinar rightly stressed the need for a dynamic and multifaceted economic engagement, guided by shared interests and a commitment to further deepen bilateral cooperation and the two organisations will contribute in their own humble manner in line with that objective.
The online event was attended by over 70 Indian manufacturers and exporters alongside some key Russian investors. The webinar also saw the attendance of boilerplate organisations “There is a huge scope for partnerships between Indian stakeholders and their Russian counterparts in the field of medical device industry. Centre for the Development of Russia India Strategic Partnership
(DRISP) and AiMeD have joined hands to accelerate the pace of bilateral engagements, he said.
Ved Prakash, First Secretary, Embassy of India in Moscow, in his opening remarks, expressed gratitude for the organisation of the meeting on medical devices. Rohit Neema, Second Secretary, Indian Embassy in Moscow, promised his support for facilitating trade and cooperation in the medical device sector between India and Russia, recognising the sector's potential for economic growth and job creation.Nath through his presentation of a comprehensive analytical document titled ‘Medical Devices –The next big thing after IT and Pharma’ showcased the latest trends and the year-on-year growth in
exports and also introduced the audience to the domestic champions from various segments who have achieved great heights under the guidance of policies enacted by the Indian government.Prasun Prakash, Founder, DRISP, alongside moderating the discussion, pointed out the right timing for the exchange of technology, critical data, knowledge base, human resource and expertise in the sector considering the latest geopolitical trends and the growing interest inside Russia towards establishing strategic partnerships with Indian manufacturers.
Denis Stepanov, General Director, CES Spine Medics, Russia, highlighted the potential for Indian medical device manufacturers entering Rus-
sia. He said that there are opportunities in the market, such as the interest from manufacturers and the need for hightech and high-quality medical products. He also addressed the challenges, including the registration process, competition from Chinese and Turkish manufacturers, and the need for international collaboration.Ashish Rangra from Invest India made a detailed presentation on the Indian medical devices sector, covering its current valuation, projected growth, key segments, import dependency, and the government’s initiatives and incentives. He also discussed the upcoming manufacturing infrastructure, including the introduction of four new parks and success stories of companies investing in India.
EXPRESS HEALTHCARE May2024 36
HEALTHCARE TRACKER
REGD.WITH RNI NO.MAHENG/2007/22045,POSTAL REGD.NO.MCS/162/2022 – 24,PUBLISHED ON 8TH EVERY MONTH, POSTED ON 14TH,15TH,16TH EVERY MONTH,POSTED AT MUMBAI PATRIKA CHANNEL SORTING OFFICE,MUMBAI – 400001




























































































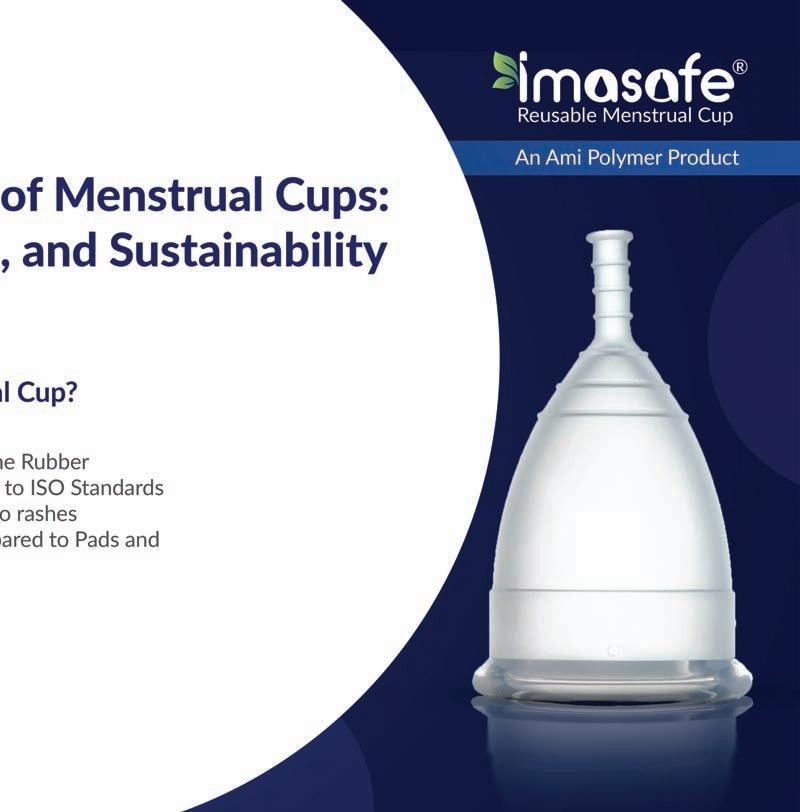























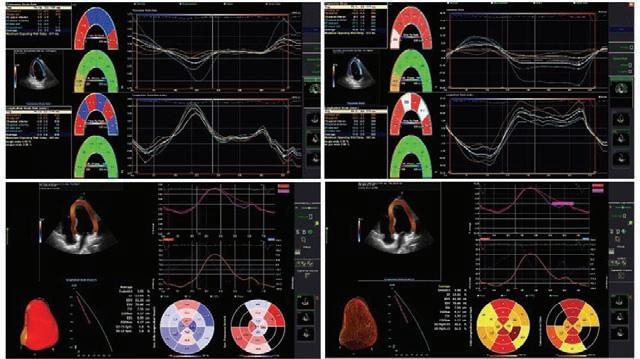

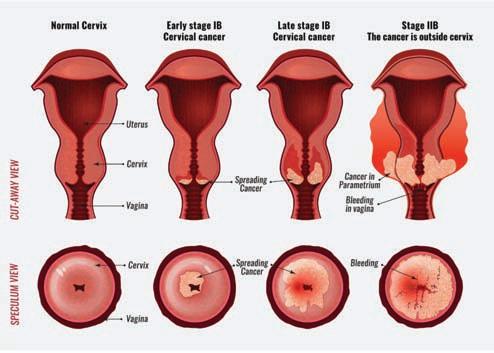


 Author – Ruchi Sanghavi Domestic Marketing Executive ruchi.s@amipolymer.com
Author – Ruchi Sanghavi Domestic Marketing Executive ruchi.s@amipolymer.com