











Findings
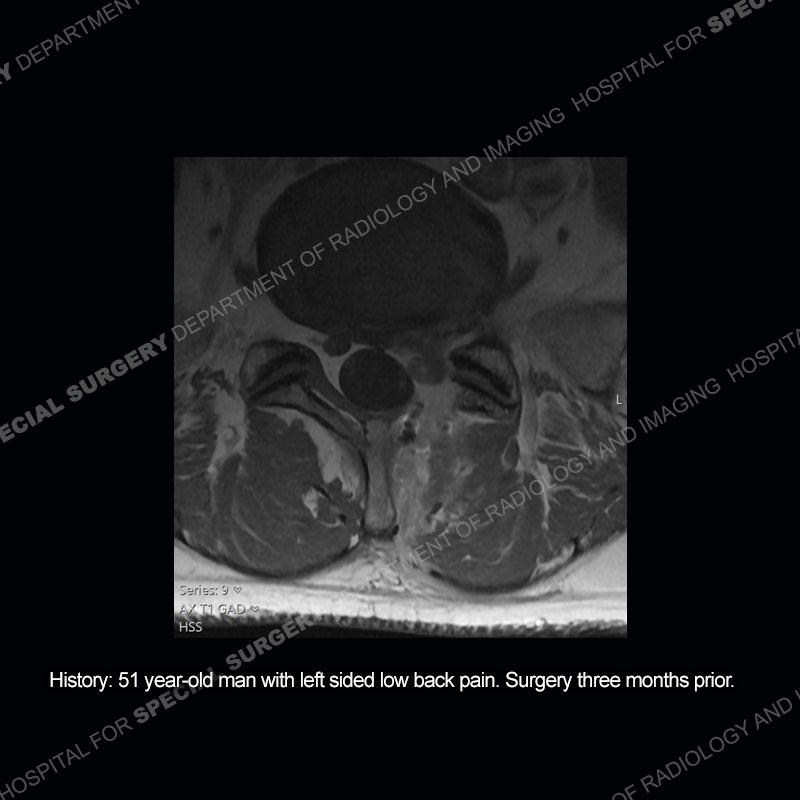
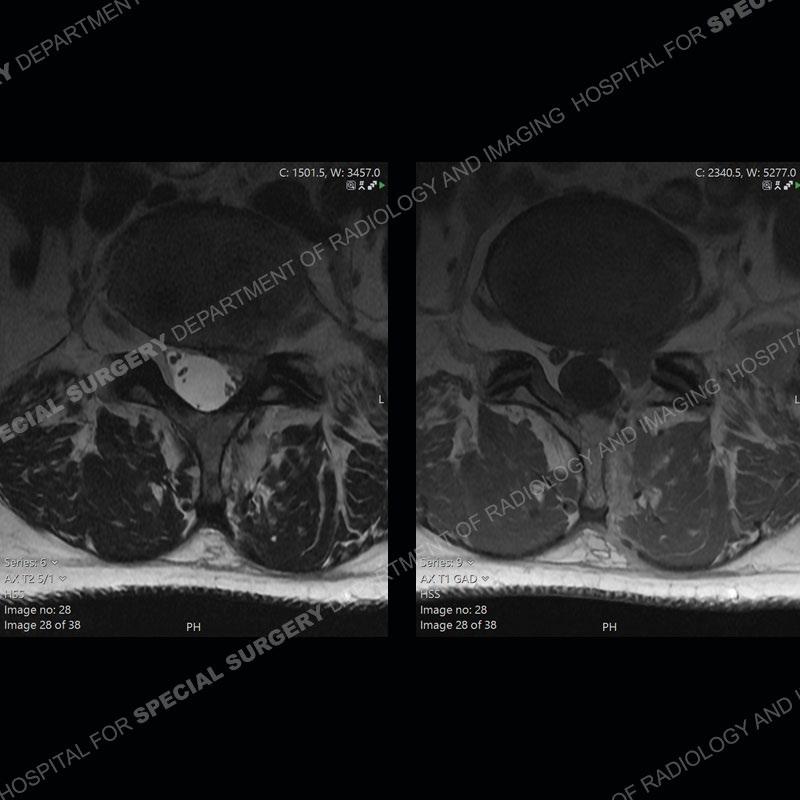
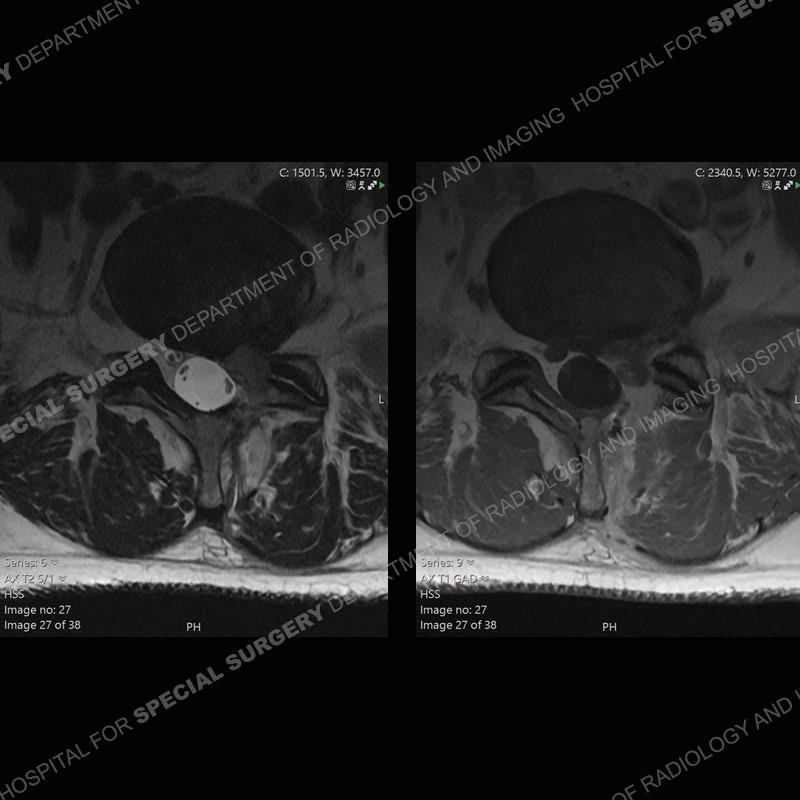
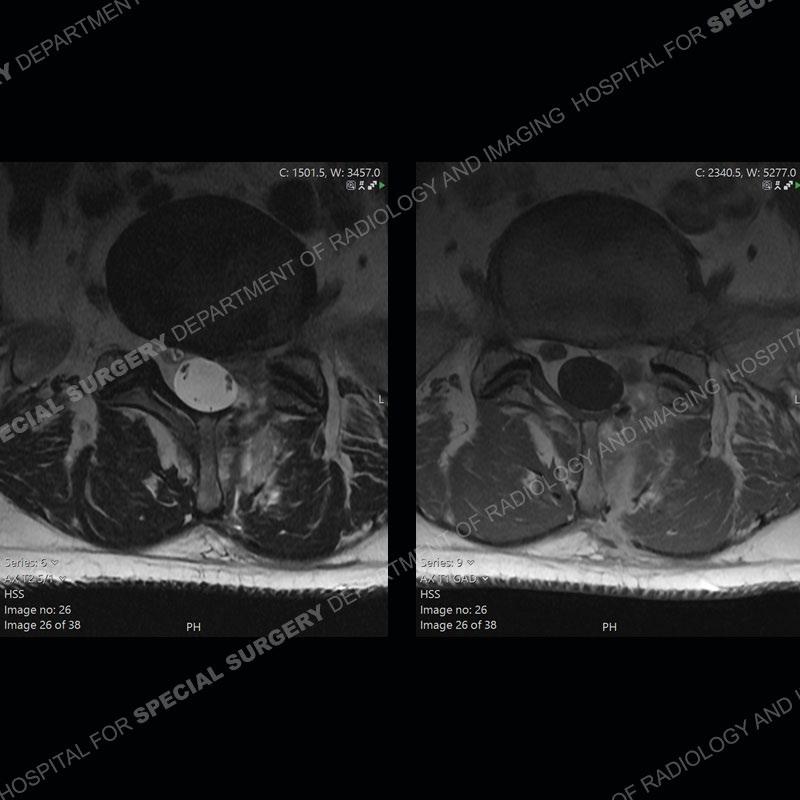
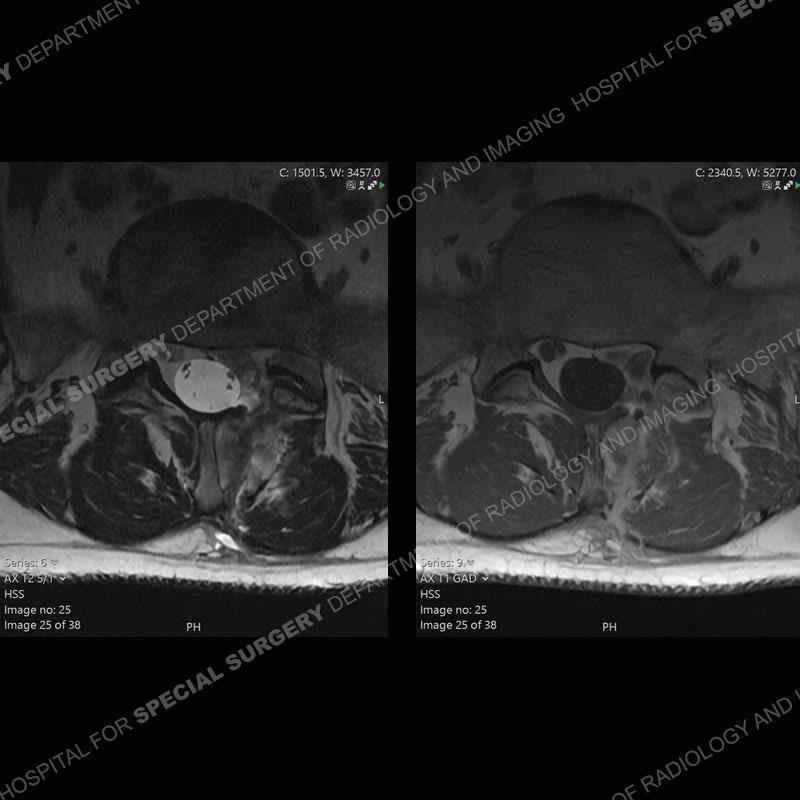
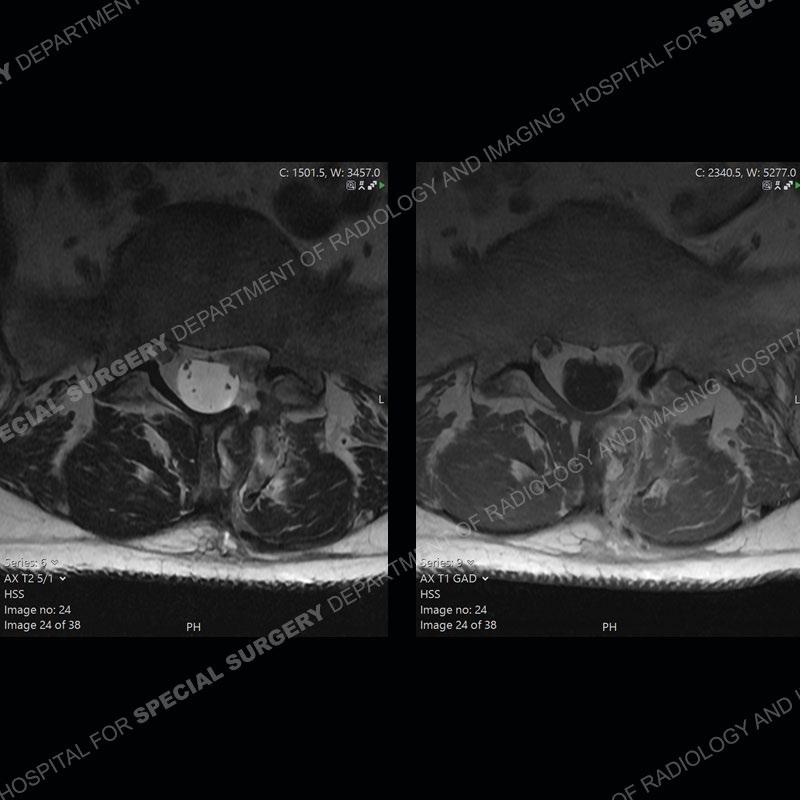
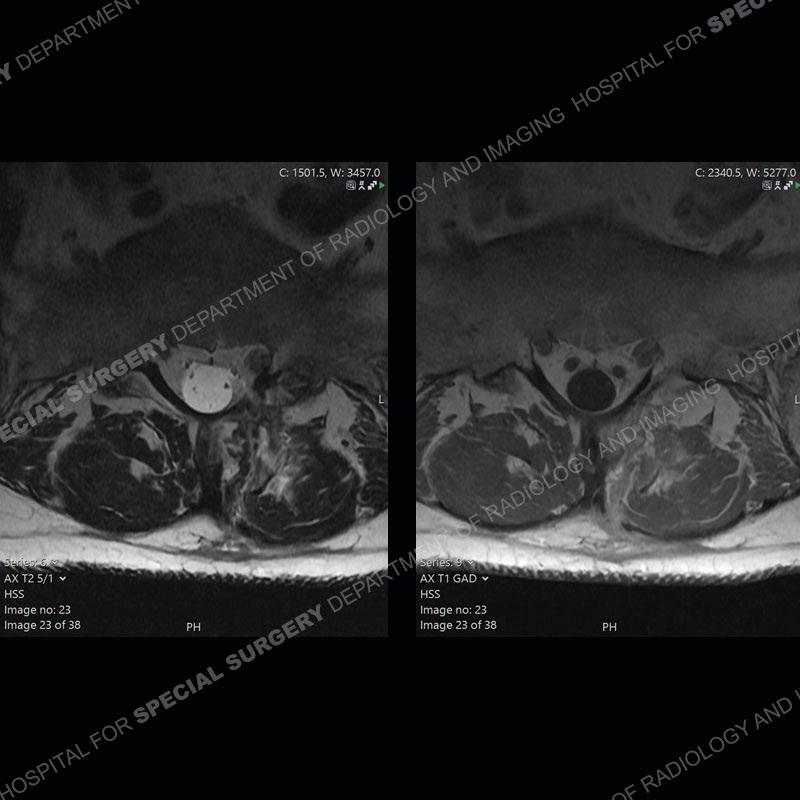
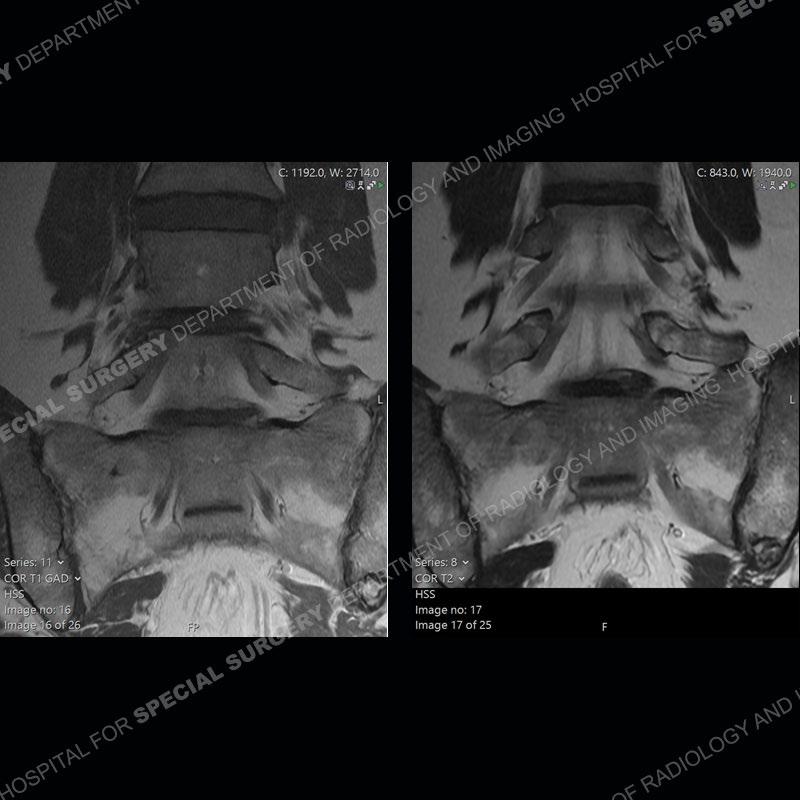
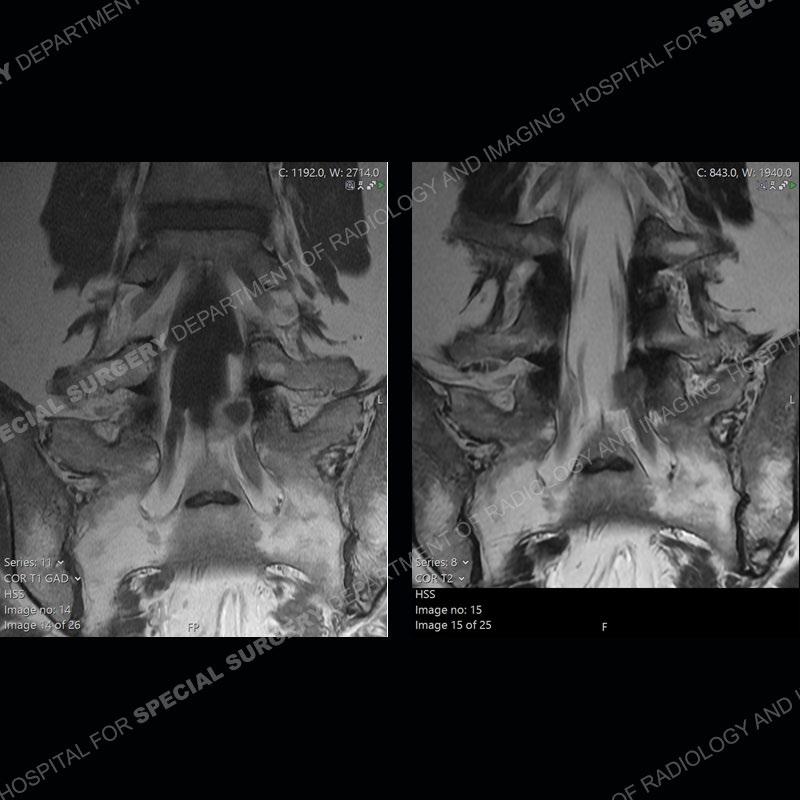
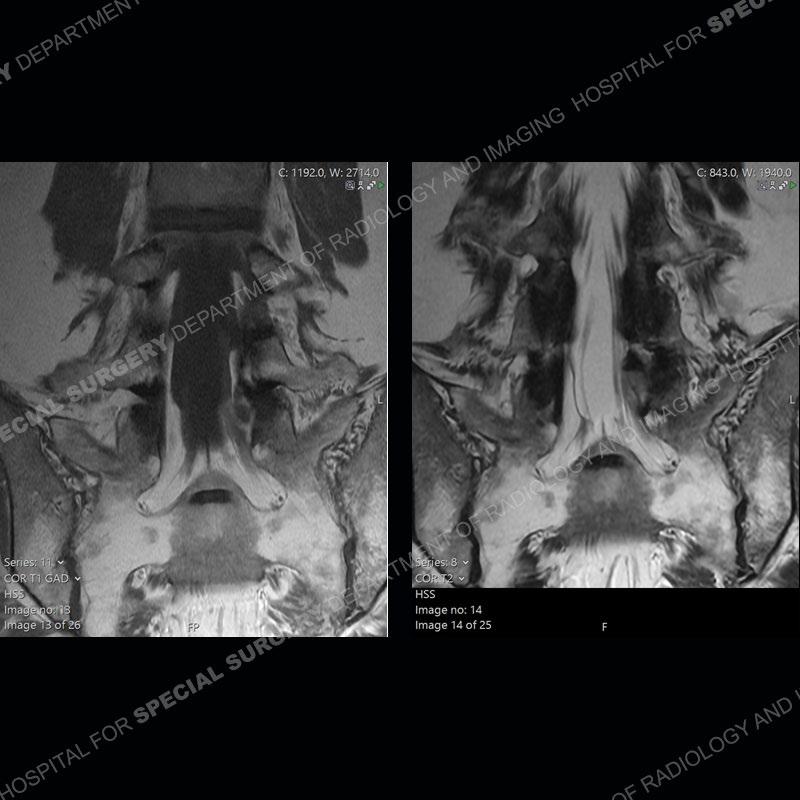
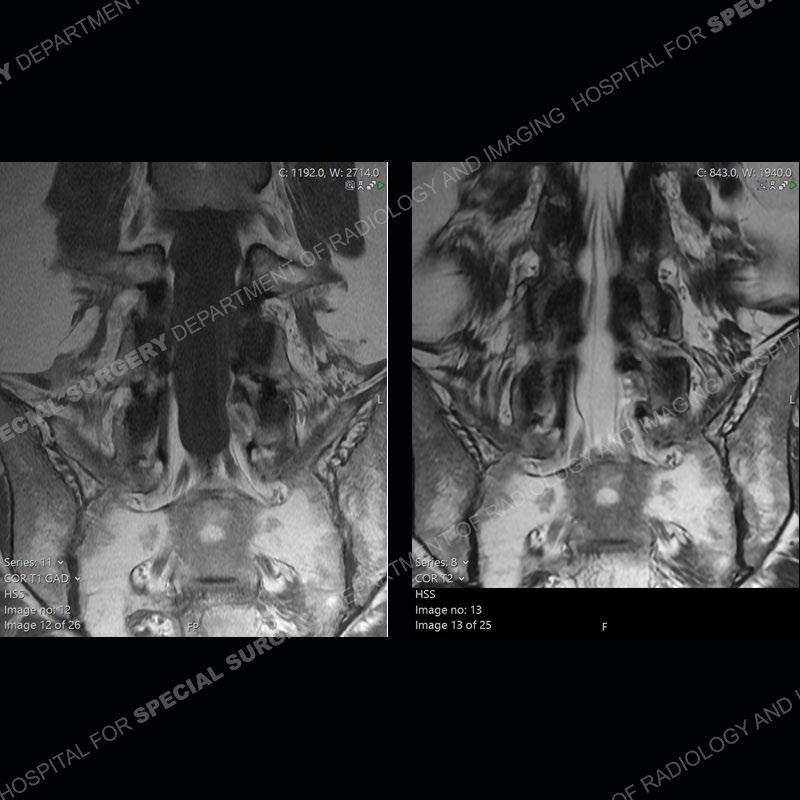
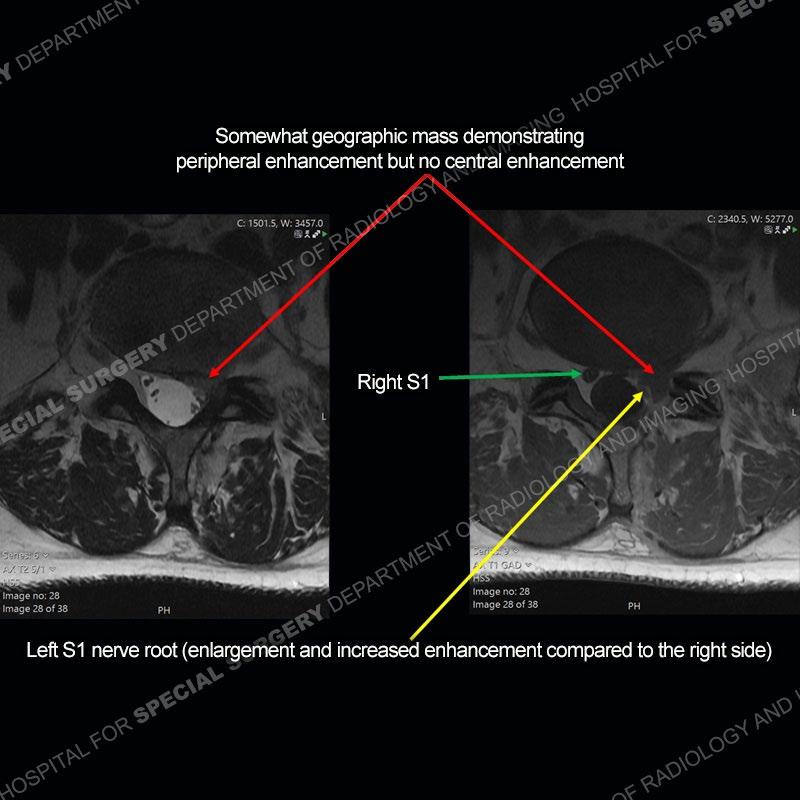
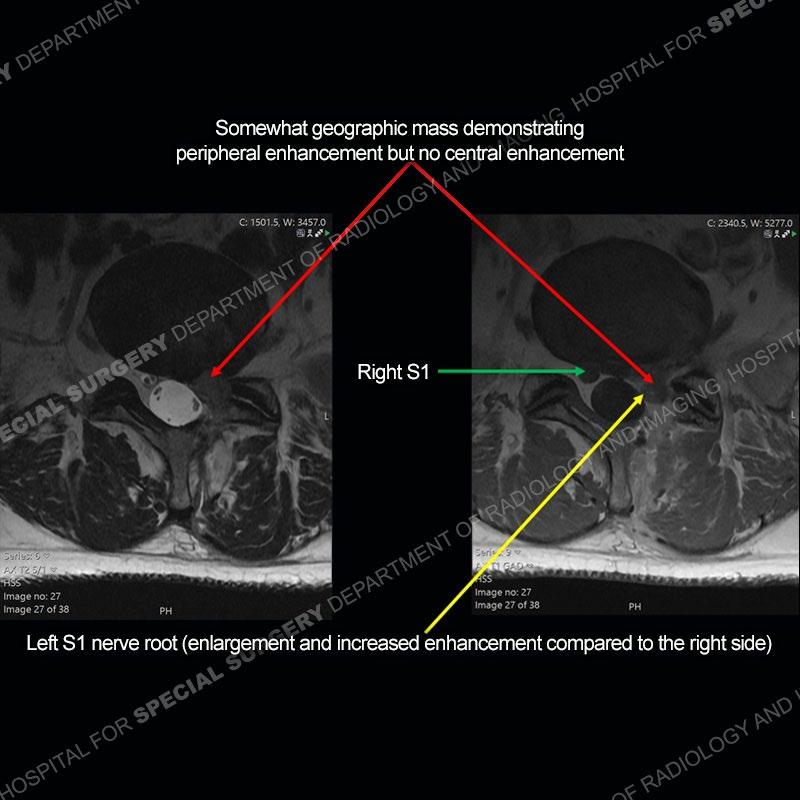
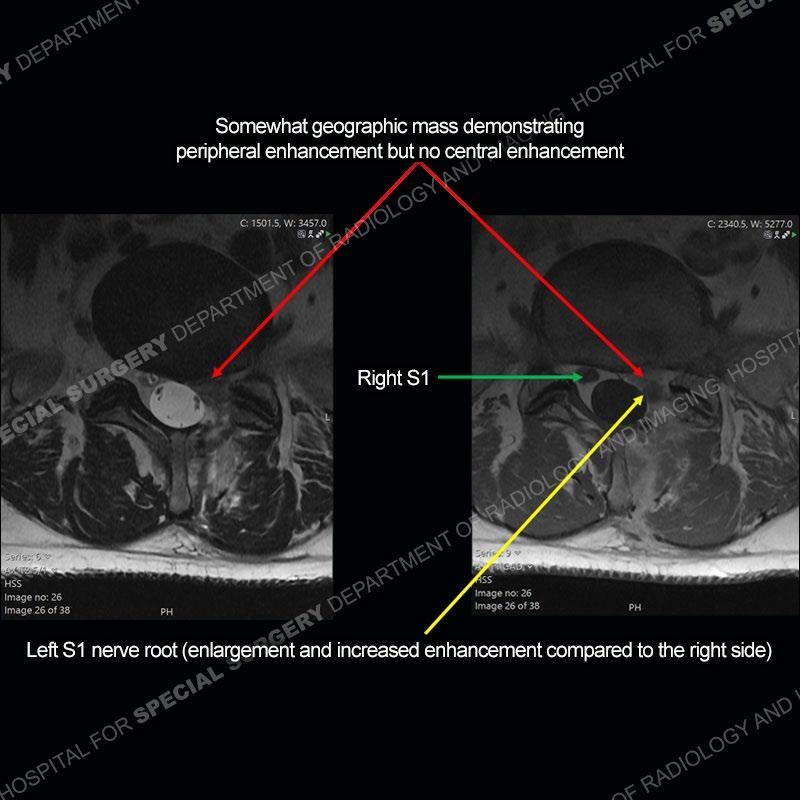
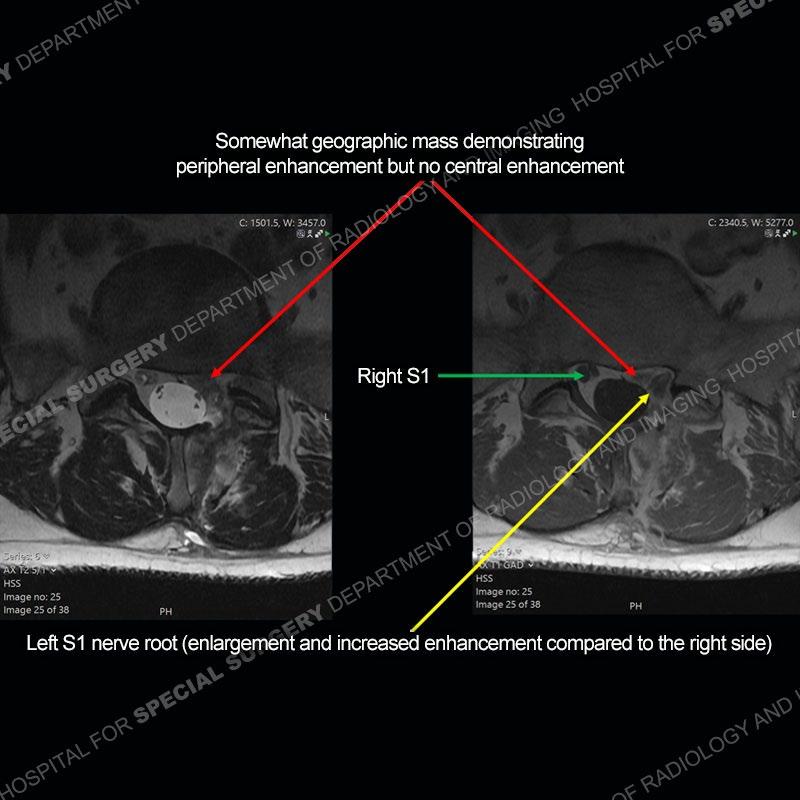
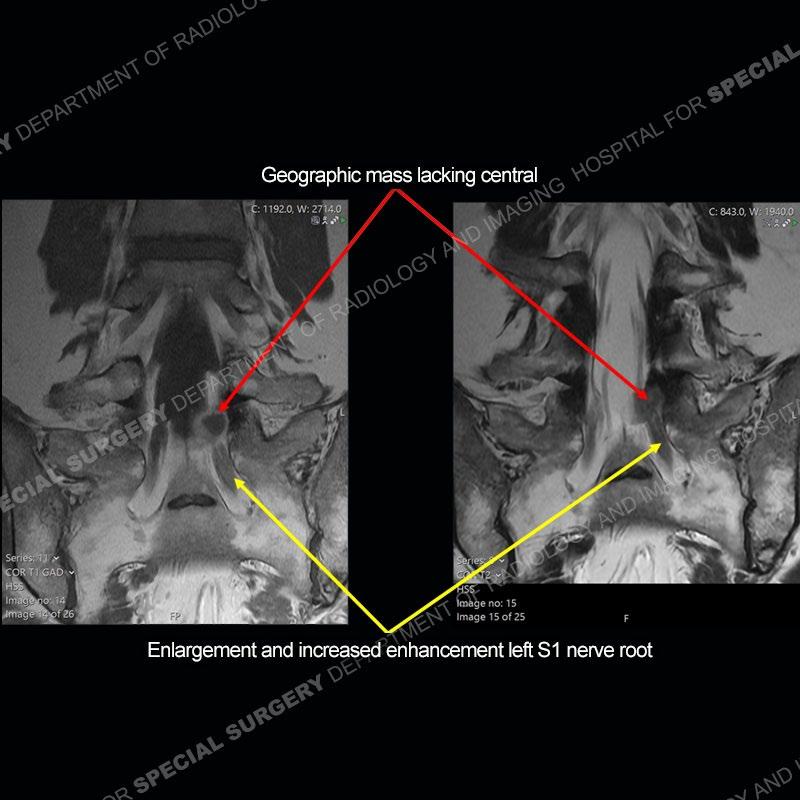
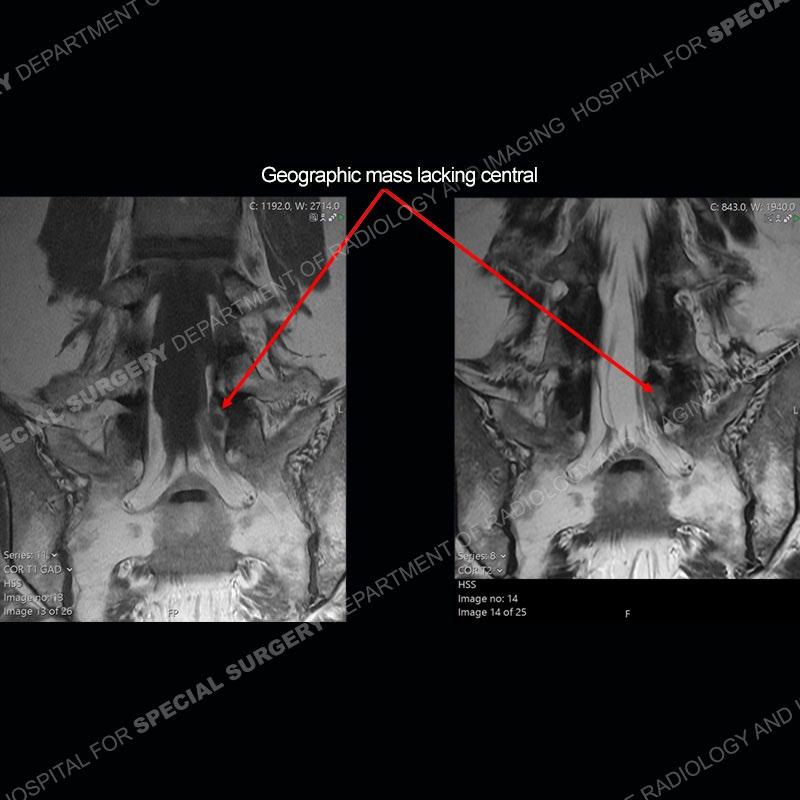
Post operative changes are seen on the left side at L5-S1 where there is near complete removal of the left sided L5 lamina, partial resection of the left L5-S1 facet joint, and resection of the left sided ligamentum flavum. In the anterolateral epidural space about the subarticular recess is a mass that demonstrates similar T1 and T2 signal characteristics to the adjacent degenerated disc. There is enhancement about the periphery of the mass, but the majority of this somewhat geographic or polyploid mass demonstrates no enhancement. The mass exerts prominent mass effect on the left S1 axillary sleeve/proximal nerve root. The left S1 nerve root shows enlargement and increased enhancement as compared to the contralateral right side.








Diagnosis: Recurrent Disc Herniation
Not as much of a diagnostic dilemma as some other cases but more so just a very nice example of what can be a difficult assessment at times. The evaluation of granulation tissue/scar/epidural fibrosis vs. disc herniation particularly in the earlier post operative period can be very difficult. Clues that can assist in identifying a disc herniation are a more geographic or polypoid nature to the mass, signal characteristics similar to the adjacent degenerated disc, mass effect upon the thecal sac/adjacent neural structures, and a typical enhancement pattern. As the disc material is avascular, as long as imaging is performed in a relatively rapid fashion after contrast administration (within 20-30 minutes), the granulation tissue around the disc will enhance but the disc material itself will not. If there is a marked delay between contrast administration and imaging, there may be diffusion of contrast into the disc making the assessment very difficult. The marked utility of contrast to help delineate disc vs. scar has led to our institution employing contrast fairly uniformly within the first two years following surgery.
The scar tissue in the setting of prior disc removal will be present in the anterior and anteriorlateral aspect of the epidural space. The signal characteristics can be somewhat variable from slightly more T2 hyperintense earlier on to T2 hypointense as the scar matures. However, the signal does not tend to follow the adjacent degenerated disc. The scar can produce mass effect, but it does not have to do so. In addition, at times the scar may be associated with a retraction of the adjacent thecal sac. Given the vascular nature of the scar there is typically somewhat avid, uniform enhancement which occurs fairly rapidly after contrast administration and begins to diminish within 20 minutes or so. Trying to discern the difference between scar and disc is of paramount importance given the rather poor outcomes associated with resection of scar as compared to disc material.

References
Frederik Abel, MD, Ek T. Tan, PhD 8, J. Levi Chazen, MD, Darren R. Lebl, MD, MBA, and Darryl B. Sneag, MD. MRI after Lumbar Spine Decompression and Fusion Surgery: Technical Considerations, Expected Findings, and Complications. Radiology Volume 308, Number 1 July 2023 https://doi.org/10.1148/radiol.222732
Hemmo A. Bosscher MD, FIPP, James E. Heavner PhD, FIPP. Incidence and Severity of Epidural Fibrosis after Back Surgery: An Endoscopic Study. Pain Practice Volume 10, Issue 1 January/February 2010 Pages 18-24 https://doi.org/10.1111/j.1533-2500.2009.00311.x

Passavanti, Z., Leschka, S., Wildermuth, S. et al. Differentiating epidural fibrosis from disc herniation on contrast-enhanced and unenhanced MRI in the postoperative lumbar spine. Skeletal Radiol 49, 1819–1827 (2020). https://doi.org/10.1007/s00256-020-03488-8
