•
Clinical risk predictors of pneumonia among stroke patients admitted for inpatient care at a provincial hospital in Thailand Chanapong Rojanaworarit 1, Yu He 1, Supattra Nonkhlor 2, Nuttawoot Phothisan 2 1
MPH Program, School of Health Professions and Human Services, Hofstra University, 2 MSc Program, Department of Epidemiology, Faculty of Public Health, Mahidol University, Thailand Results
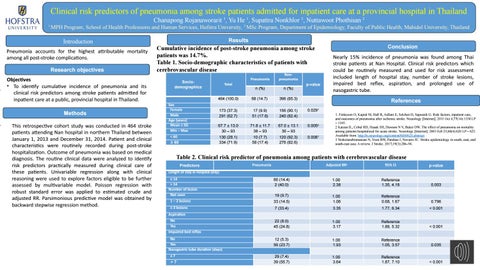
Introduction Pneumonia accounts for the highest attributable mortality among all post-stroke complications. Research objectives Objectives • To identify cumulative incidence of pneumonia and its clinical risk predictors among stroke patients admitted for inpatient care at a public, provincial hospital in Thailand. Methods This retrospective cohort study was conducted in 464 stroke patients attending Nan hospital in northern Thailand between January 1, 2013 and December 31, 2014. Patient and clinical characteristics were routinely recorded during post-stroke hospitalization. Outcome of pneumonia was based on medical diagnosis. The routine clinical data were analyzed to identify risk predictors practically measured during clinical care of these patients. Univariable regression along with clinical reasoning were used to explore factors eligible to be further assessed by multivariable model. Poisson regression with robust standard error was applied to estimated crude and adjusted RR. Parsimonious predictive model was obtained by backward stepwise regression method.
Cumulative incidence of post-stroke pneumonia among stroke patients was 14.7%. Table 1. Socio-demographic characteristics of patients with cerebrovascular disease Pneumonia
Nonpneumonia
n (%)
n (%)
464 (100.0)
68 (14.7)
396 (85.3)
173 (37.3) 291 (62.7)
17 (9.9) 51 (17.6)
156 (90.1) 240 (82.4)
0.0291
67.7 ± 13.0 30 ‒ 93
71.8 ± 11.7 38 ‒ 93
67.0 ± 13.1 30 ‒ 93
0.0052
130 (28.1) 334 (71.9)
10 (7.7) 58 (17.4)
120 (92.3) 276 (82.6)
0.0081
Sociodemographics
Sex Female Male Age (years) Mean ± SD Min ‒ Max < 60 ≥ 60
Total
p-value
Conclusion Nearly 15% incidence of pneumonia was found among Thai stroke patients at Nan Hospital. Clinical risk predictors which could be routinely measured and used for risk assessment included length of hospital stay, number of stroke lesions, impaired bed reflex, aspiration, and prolonged use of nasogastric tube. References 1. Finlayson O, Kapral M, Hall R, Asllani E, Selchen D, Saposnik G. Risk factors, inpatient care, and outcomes of pneumonia after ischemic stroke. Neurology [Internet]. 2011 Oct 4;77(14):1338 LP – 1345. 2 Katzan IL, Cebul RD, Husak SH, Dawson N V, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology [Internet]. 2003 Feb 25;60(4):620 LP – 625. Available from: http://n.neurology.org/content/60/4/620.abstract 3 Venketasubramanian N, Yoon BW, Pandian J, Navarro JC. Stroke epidemiology in south, east, and south-east asia: A review. J Stroke. 2017;19(3):286–94.
Table 2. Clinical risk predictor of pneumonia among patients with cerebrovascular disease Predictors
Pneumonia
Adjusted RR1
95% CI
p-value
66 (14.4) 2 (40.0)
1.00 2.38
Reference 1.35, 4.18
0.003
19 (9.7)
Length of stay in hospital (day) ≤ 14 > 14 Number of lesion Not seen 1 ‒ 2 lesions
33 (14.5)
1.00 1.06
Reference 0.68, 1.67
0.796
≥ 3 lesions
7 (33.4)
3.35
1.77, 6.34
< 0.001
No Yes Impaired bed reflex
22 (8.0) 45 (24.8)
1.00 3.17
Reference 1.88, 5.32
< 0.001
No Yes Nasogastric tube duration (days)
12 (5.3) 56 (23.7)
1.00 1.93
Reference 1.05, 3.57
0.035
29 (7.4) 39 (55.7)
1.00 3.64
Reference 1.87, 7.10
< 0.001
Aspiration
≤7 >7