About this Report
Our Annual Report follows best practice in corporate governance by reporting our performance against strategic objectives and national targets and presenting information about our services and financial performance transparently and honestly.
The structure of the Report and Accounts also follows the requirements of the Companies Act 2006, as amended, and consists of a Performance Report, an Accountability Report, Remuneration and Staff Report and the Financial Statements.
If you would like a copy of this document in large print, Braille or audio tape, or if English is not your first language and you would like this information explained in your own language, please contact 01707 388000.
Se desideri una copia di questo documento in caratteri grandi, Braille o nastro audio, o se l'inglese non è la tua lingua madre e desideri che queste informazioni siano spiegate nella tua lingua, contatta lo 01707 388000.
Jeśli chcesz otrzymać kopię tego dokumentu dużą czcionką, pismem Braille'a lub taśmą audio lub jeśli angielski nie jest Twoim pierwszym językiem i chciałbyś, aby te informacje zostały wyjaśnione w Twoim języku, skontaktuj się z 01707 388000.
Bu belgenin BÜYÜK YAZDIR, Braille veya ses kasetinde bir kopyasını almak istiyorsanız veya İngilizce ilk diliniz değilse ve bu bilgilerin kendi dilinizde açıklanmasını istiyorsanız, lütfen 01707 388000.
Glossary of Abbreviations
ACOM Adult Community Operating Model
ADHD Attention Deficit Hyperactivity Disorder
AHP Allied Health Professional
ASD Autistic Spectrum Disorder
BAF Board Assurance Framework
BAME Black, Asian and Minority Ethnic
BI Business Intelligence
BMS Building Management System
BPPC Better Practice Payment Code
BREEAM Building Research Establishment Environmental Assessment Method
CATS Clinical Assessment and Treatment Service (MSK)
CEO Chief Executive Officer
CETV Cash Equivalent Transfer Values
CHIS Child Health Information Service
CHSWG Children’s Hearing Services Working Group
CLCH Central London Community Healthcare NHS Trust
CQC Care Quality Commission
CQUIN Commissioning for Quality and Innovation
CRE&D Celebrating Racial Equality and Diversity
CYP Children and Young People
CYPT Children and Young People’s Integrated Therapies
DHSC Department of Health and Social Care
ED&I Equity, Diversity and Inclusion
EDS Equality Delivery System
EFL External Financing Limit
EHCP Education, Health and Care Plan
ENHT East and North Hertfordshire NHS Trust
ENT Ear, Nose and Throat
EoE East of England
EPR Executive Performance Review
EPRR Emergency Preparedness, Resilience and Response
EPUT Essex Partnership University NHS Foundation Trust
FFT Friends and Family Test
FReM Financial Reporting Manual
FSS Family Support Service
G2O Good to Outstanding
GAM Group Accounting Manual
GDPR General Data Protection Regulation
GP General Practitioner
HAH Hospital at Home
HCP Health and Care Partnership
HCT Hertfordshire Community NHS Trust
HCT HIVIS HCT’s Health Immunisation Vision Insight System
HEH Herts & Essex Hospital
HILS Health & Independent Living Support
HLRR High Level Risk Register
HSJ Health Service Journal
HWE Hertfordshire and West Essex
HWE ICS
Hertfordshire and West Essex Integrated Care System
IBD Inflammatory Bowel Disease
ICB Integrated Care Board
ICS Integrated Care System
ICTs Integrated Care Teams
IMD Indices of Multiple Deprivation
IQIPS Improving Quality in Physiological Services
IRM Integrated Referral Management
IUATC Integrated Urgent Assessment and Treatment Centre
JTAI Joint Targeted Area Inspection
LEAP Lived Experience Advisory Panel
LED Light Emitting Diode
LFPSE Learning from Patient Safety Events
LGBTQI+ Lesbian, Gay, Bisexual, Transgender, Queer, Intersex +
MDT Multidisciplinary Teams
MHLDA Mental Health Learning Disability and Autism
MSK Musculoskeletal
NBI Not Brough In
NED Non-Executive Director
NHSE NHS England
NICE National Institute for Health and Care Excellence
NZCR Net Zero Carbon Roadmap
ONS Office for National Statistics
OPR Operational Performance Review
PAH The Princess Alexandra Hospital NHS Trust
PALMS Positive Behaviour, Autism, Learning Disability and Mental Health Service
PASQAT Paediatric Audiology Quality Standards
PCN Primary Care Network
PHN Public Health Nursing
PIFU Patient Initiated Follow Up
PPFC People Performance and Finance Committee
PSED Public Sector Equality Duty
PSIRF Patient Safety Incident Response Framework
RSV Respiratory Syncytial Virus
SaLT Speech and Language Therapy
SEND Special Educational Needs and Disabilities
SIPC Strategy Involvement and Planning Committee
SLCN Speech, Language and Communications Needs
SLT Speech and Language Therapist
ToD Teachers of the Deaf
UCCH Unscheduled Care Coordination Hub
UKAS United Kingdom Accreditation Service
VCSFE Voluntary, Community, Faith and Social Enterprise
VSM Very Senior Manager
WDES NHS Workforce Disability Equality Standard
WNBI Was Not Brought In
WRES NHS Workforce Race Equality Standard
1 Foreword by the Chair and Chief Executive
We are pleased to present the 2024/25 Annual Report for Hertfordshire Community NHS Trust (HCT). Over the past year, our staff have continued to show strong commitment and professionalism as we work to deliver high-quality, patient-focused care across our communities. The progress made across our services reflects our focus on innovation, partnership working, and improving health outcomes.
A key priority for us remains delivering care closer to home. Services like Hospital at Home, Urgent Community Response, and our virtual ward capacity have enabled thousands of patients to be treated safely in their own homes. New clinical pathways, better use of digital tools, and a focus on early intervention have made our services more effective, more accessible, and better aligned to people’s needs.
We have continued to strengthen collaboration across the health and care system Through our role in the Hertfordshire and West Essex Integrated Care System, and partnerships with primary care, local authorities, hospices, and the voluntary sector, we are working together to address key challenges such as access, inequality, and service integration. Projects like diabetic eye screening in the community, joint clinics for children, and targeted outreach in underserved areas are helping to close gaps and improve care.
Our staff are central to everything we do. We remain committed to supporting their wellbeing, development and inclusion. This year’s staff survey results show HCT is one of the top-performing NHS community trusts in the country, with particularly strong feedback on compassionate leadership, inclusivity, and psychological safety.
Our Equity, Diversity and Inclusion Strategy continues to guide us as we embed a culture where every member of staff feels valued, heard and supported to thrive. Initiatives like the development of our ‘Just Culture’ approach, staff networks, Shadow Board, and leadership development programmes reflect our commitment to making HCT a supportive place to work, which we know helps improve patient care.
Looking ahead, we recognise the ongoing pressures facing the health and care system. However, with a clear strategy, strong partnerships and a skilled workforce, HCT is well placed to respond to these challenges and make the most of new opportunities. We thank our staff, partners, local communities, and the people who use our services for their continued support.
We remain focused on delivering better care, closer to home.


Dr Nicolas Small, Chair
Date 16 June 2025
Elliot Howard-Jones, Chief Executive
Date 16 June 2025
2 Performance Report
2.1 Performance Overview
As Chief Executive Officer, I am delighted to present our 2024/25 Performance Report. Our Performance Report summarises our strategy, including our vision, values and strategic objectives. It includes our key achievements during the year, a summary of our operational and financial performance, plus the key risks and issues impacting on the achievement of our strategic objectives.
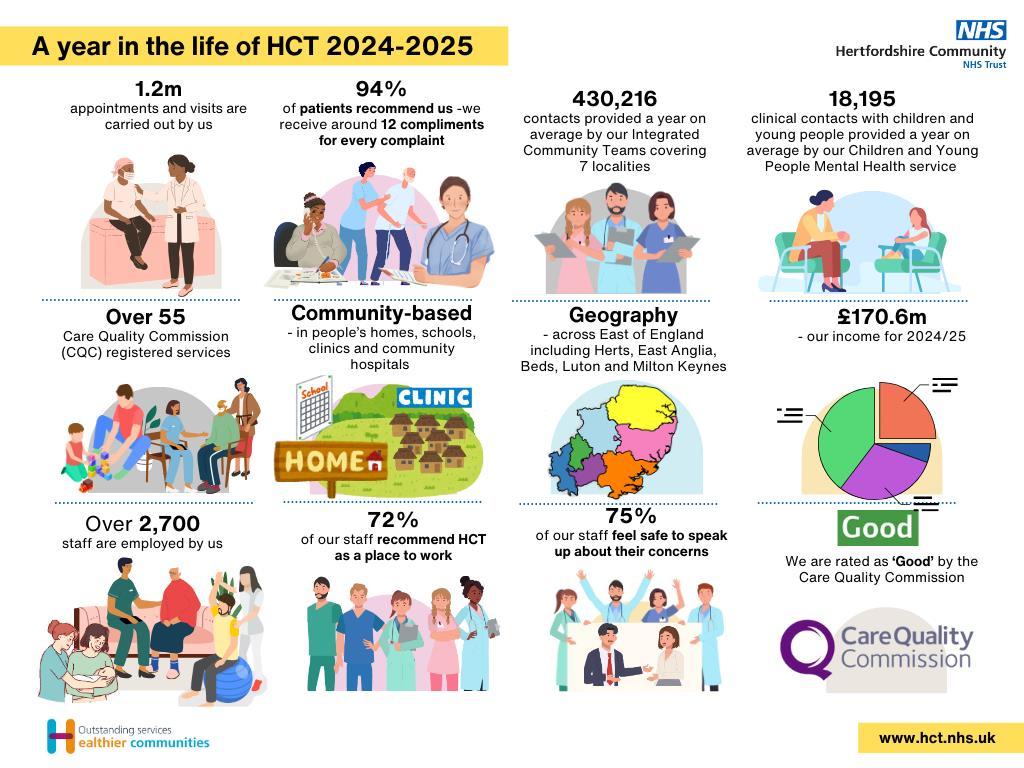
We are continuing our work to recover service performance and respond to increasing demand, working alongside system partners to keep people out of hospital. Our Urgent Community Response service is performing strongly against a national target of 70%, with 78% of people seen within two hours. Bed occupancy rates were 138% in January against our planned target within the Hospital at Home service.
The Unscheduled Care Coordination Hub (UCCH) is seeing on average 15 patients a day, with 84% of patients accepted onto our case load avoiding a hospital admission. I am delighted to report that UCCH has been shortlisted for the HSJ digital awards which is testament to the commitment, hard work and tenacity of the teams working to deliver this innovative service.
Referrals have increased across all services, leading to longer waiting times and a rise in waiting list numbers compared to last year. Despite this, progress continues in reducing long waits. The greatest pressure remains within Children and Young People’s (CYP) services.
Our Community and School Aged Immunisation Service (CSAIS) teams this year have produced some astounding results, and we are very proud to be leaders in this programme nationally.
A key focus this year has been to improve population health outcomes and there has been a particular focus on addressing health inequalities through a targeted programme of work. The Trust has significantly increased its focus on ‘did not attend’ and health inequalities generally, incorporating these into its quality priorities, with effective measures already in place.
Our Business Intelligence (BI) developments have enabled increased automation of our Operational Performance Review and development of an integrated Assurance and Support Framework, which will allow us to support our operational services in a more effective way.
Many of our achievements reflect the efforts we have made to improve the experience of those who use our services, whilst making HCT a great place to work for our staff. Our staff have provided excellent support to patients and system partners during periods of significant operational pressure are to be commended for their professionalism and commitment to our patients.
We continue to support our new staff with an improved onboarding and induction package to ensure that they feel welcomed and valued by the Trust. The latest NHS Staff Survey results were highly positive, with the Trust scoring above average in all nine People Promise themes. We were the top-performing community trust in seven areas including access to learning and development opportunities and having good working relationships.
We are dedicated to being a sustainable healthcare provider that acts responsibly to achieve greater energy efficiency and minimise our impact on the environment. Work continues on the implementation of our Green Plan and this year we have approved capital business cases for works to enhance our environmental sustainability and reduce our carbon footprint.
To conclude, I want to express my sincere gratitude to our staff for their dedication in overcoming the unprecedented challenges we face daily. Their commitment to the Trust’s values of Innovative, Caring and Agile, continues to shine through in everything they do.
2.2 Looking ahead
As we shape our plans for the coming year, the Trust remains committed to making a meaningful impact on our patients and the communities we serve. While financial considerations guide our decisions, our focus remains firmly on transforming services and fostering the growth of our people and working towards providing sustainable services for the future.
There will be a necessary focus on reducing running costs where we can, working with our people to improve productivity and reduce waste so that available resources are targeted at improving frontline care.
Key to this is our commitment to collaborative working and strengthening the voice of community services within the local system and exploring ways in which we can improve the experience of our patients. We will continue to work collectively with the ICB and our system partners to improve access to services and reduce waiting times, continue our
focus on prevention and provide alternative models of care that will allow patients to be cared for at home, rather than in a hospital setting.
Our plans align well with the three main shifts set out by the Government’s 10 Year Health Plan, recent planning guidance and joint ICB plans. The Trust is taking steps to make sure that the decisions we take are informed by data and we are investing in technology as a means of improving our productivity and performance where it makes sense to do so. Our work to improve recruitment and retention of frontline staff will also be key to ensuring safe delivery of services.
Our plans encompass initiatives designed to address the challenges of an ageing and frail population. We are committed to proactive care, empowering individuals to maintain their health and well-being while preventing the worsening of symptoms. Additionally, we are dedicated to reducing health inequalities, using data to address any gaps in provision and eliminate any unwarranted variation in the services we provide to our communities.
Overall HCT has performed well against the national priorities as described in this Annual Report. This coming year, we will continue to build on our successes, taking account of ongoing financial constraints, to drive improvements where needed to ensure services are provided in the best interests of our patients.
2.3 About the Trust
2.3.1 The Trust’s principal activities
Hertfordshire Community NHS Trust is the principal provider of community-based healthcare services to the 1.2 million population of Hertfordshire, we also provide services in west Essex and beyond. The Trust is rated as 'Good' by the Care Quality Commission It had an income of £170.6m during 2024/25 (£157 4m in 2023/24) and employed around 2,770 staff (2,590 in 2023/24).
Community health services continue to be at the forefront of NHS care and support. Every day we deliver a wide range of high-quality health services to people in their homes, in local clinics, in schools and in our community hospitals. We support people at every stage of their lives, from antenatal, health visiting and school nursing services for children and young people, to community nursing and therapy, specialist dentistry, rehabilitation and palliative care. In 2024/25 we delivered over 1.2 million patient contacts excluding our immunisations services.
We work in partnership with colleagues across the NHS, social care, education, charities and local government, helping people to maintain their health and wellbeing, be as independent as possible through self-care, and ensuring that we deliver joined up local care and support A full list of our services and where they are provided is set out below:
Adult Services
• Acute Falls Clinic (community element)
• Acute Therapies Service (Outpatients –Lister Hospital)
• Adult Bladder & Bowel Care Service
• Adult Speech & Language Service
• Cardiac Rehabilitation Service
• Integrated Heart Failure Service
• Hertfordshire Integrated Diabetes Service (South & West Herts)
• Hospital at Home
• In-reach Team/Transfer of Care Hub
• Clinical Navigators (Lister Hospital) (Lister Hospital)
• Integrated Care Teams
• Community Frailty Assessment Service
• Integrated Community Respiratory
• Community Inpatient Beds (Queen Victoria Service Memorial, Danesbury and Herts and Essex)
• Community Neurological Rehabilitation (including Early Supported Discharge)
• Diabetic Retinal Screening Service (Herts and West Essex)
• Discharge Home to Assess Teams
• East & North Herts Diabetes Service
• East & North Integrated Care Coordination Centre
• End of Life and Specialist Palliative Care
• Enhanced Health in Care Homes Service
• Foot Health Service (Podiatry)
• Lymphoedema Service
• Minor Injuries Unit, Cheshunt Community
• Hospital (in partnership with Herts Urgent Care)
• Minor Injuries Unit, Herts & Essex Hospital
• Musculoskeletal Services
• North Herts Anticoagulation Service
• Nutrition & Dietetics Service
• Phlebotomy Service
• Pulmonary Rehabilitation Service
• Skin Health Service
• Tissue Viability & Leg Ulcer Service
Children & Young People’s (CYP) Services
• Child Health Information Service (East of England) (BLMK from Sept 2024, now Herts, Norfolk, Suffolk, C&P and BLMK)
• Children’s Asthma and Wheeze Service
• Children’s Wellbeing Practitioner team
• Community School Aged Immunisations Service
• CYP Phlebotomy Service
• CYP Referral Hub
• Positive Behaviour, Autism, Learning
• CYP Community Nursing Disability and Mental Health Service (PALMS)
• CYP Community Paediatrics
• CYP Continence Service
• CYP Continuing Care Service
• CYP Eye Services
• Public Health Nursing Services
• Special Educational Needs and Mental Health Support team
• Special School Nursing Service
• Special Community Dental Service
• CYP Hearing Service (Audiology) (adults and children)
• CYP Nurse Training Team
• CYP Integrated Therapy Services
• Specialist Nurse Co-ordinators (Transition and Sickle Cell)
• Step2 Service
Nursing Services
• Infection Prevention & Control Team
• Looked After Children/Care Leavers Team
• Rapid Response to Unexpected Child Death Team
• Safeguarding Adults Team
• Safeguarding Children Team
2.3.2 Our Trust strategy

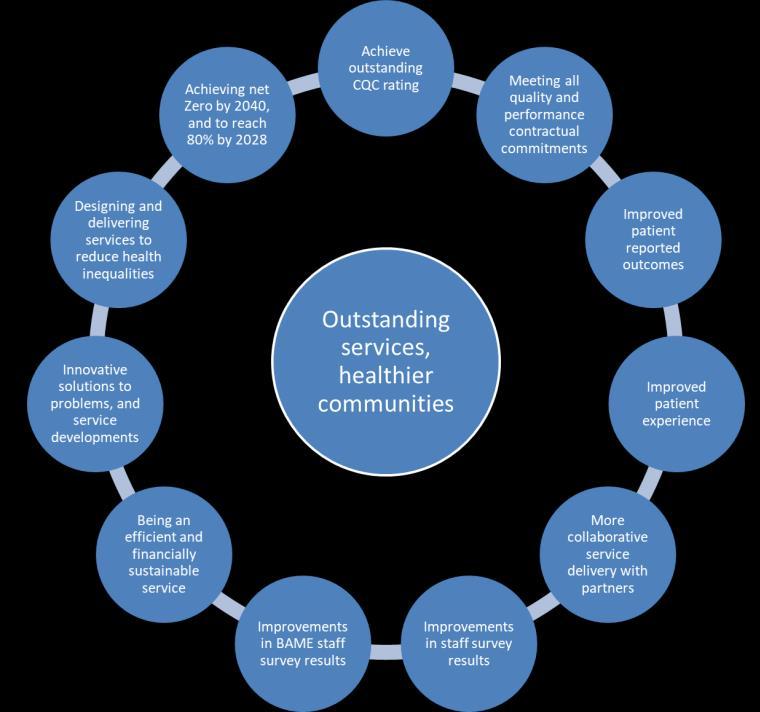
Our patients, families, carers and communities are at the very heart of our vision of Outstanding Services, Healthier Communities. Our aspiration is to ensure our communities are as healthy as possible, and our services are outstanding and high quality. Our vision is underpinned by our values which were developed following consultation and engagement with our staff and wider stakeholders. Our three Trust values reflect how our people need to operate in our health and social care system to ensure we succeed:
• Innovative - we seek new ideas and adopt best practice to improve our services
• Caring - we act with kindness and consideration for others
• Agile - we deal with new situations quickly and successfully Our four objectives set out how we want to deliver outstanding quality and performance for our patients, service users and their families through working with our system partners, innovating and continuously improving and having well trained, developed, supported and happy staff:
• Outstanding quality and performance - through our approach to Continuous Quality Improvement (CQI) and through involving patients, families, carers and our staff to provide the best possible care to patients within available resources
• Joined up local care - by working in partnership with others, we will improve the quality of what we do, provide a better experience for patients and better value for money. We will develop integrated clinical pathways to improve the care people receive in the community to support their health and wellbeing and reduce health inequalities
• Great place to work - we will make the Trust a great place to work by living our values and creating an inclusive, open and compassionate culture. We will motivate and retain our people through excellent leadership at all levels of the
organisation, continuous professional development and support for health and wellbeing
• Best value through innovation - known for our innovations as an outstanding provider of clinical services; we will harness modern processes, systems, and technology to support continuous quality improvement, efficiency, and ensure the best possible value for the public purse
Our Trust strategy and enabling strategies reinforce our commitment to working together with our partners to provide joined up local care and our strategies are the result of engagement with our system partners and reflect both system and ICB priorities as well as those of our partners
Our priorities are reflected in our Trust Delivery Plan which is designed to achieve the strategic objectives and outcomes set out in our organisational strategy and priorities set out within operational planning guidance:
2.3.3 Strategic partnerships
HCT continues to develop and extend our partnership approach across the numerous systems that we work within at all levels, allowing us to work with others to design, grow, innovate and deliver outstanding care closer to home.
Our organisational goal of ‘Joined Up Local Care’ has been the foundation for the work we have undertaken with system partners over the last year, including other NHS providers, Primary Care Networks, local government, charity, faith and voluntary sector organisations, educational settings and community and patient representative groups. Our Board has challenged us to leverage HCT’s capabilities and use the opportunities offered by partnerships to address more specifically the need of underserved populations, with a focus on doing all we can to improve access to services and help reduce health inequalities.
Key areas of partnership work this year have included:
We are proud to be a key partner in the Hertfordshire and West Essex Integrated Care System (HWE ICS), continuing to engage and actively contribute to ICS programmes including:
• We have expanded our Hospital at Home capacity and capability, challenging ourselves to do more to support more people to safely undergo treatment and care at home – this has supported the ICS’s ambition of achieving a 25% reduction in unplanned admissions for older, frail people
• Establishing the Unscheduled Care Co-ordination Hub (UCCH) with EEAST and the ICB This is one hub serving the whole of the ICS, with GPs, medics and paramedics who will help to decide on the best local care for patients. Performance of the HWE UCCH shows circa 50% of C3-C5 incidents are passed to Community Care, the highest in the East of England region
• Driving the further deepening and broadening of care closer to home through representing HWE community providers at ICB level, including on the Integrated Care Board (ICB), ensuring that community solutions are a key consideration in developing services, allowing better access for patients, service users, and their families.
Hertfordshire & West Essex Integrated Care System
East & North Hertfordshire Health & Care Partnership
• As part of the ENH HCP we have progressed the Care Closer to Home Programme (which our Associate Medical Director co-chairs) with focussed multi-organisation work to identify those at risk of admission to enable a more considered proactive approach to their healthcare
• As part of this we are supporting a number of pilots in Primary Care Networks to trial a case management and multi-disciplinary approach to better anticipate acute deteriorations. These pilots will help to test and refine the model
• We have continued to extend the Hospital at Home service in east and north Hertfordshire in partnership with colleagues across the system, informed by feedback and involvement from our patients, their families and carers. We have extended the number of different pathways available through our service, ensuring more people are able to safely avoid a hospital attendance and admission
• The introduction of an Integrated Heart Failure Service in the east of Hertfordshire has supported Princess Alexandra Hospital NHS Trust (PAH) to free up capacity to focus on severely unwell patients The service provides patients with advice, guidance and support for their condition, enabling them to receive care and treatment closer to home
South & West Hertfordshire Health & Care Partnership
• We have worked with partners to make treatment much more accessible, with an initial focus on expansion of CYP intravenous antibiotic virtual ward capacity at Peace Children’s Centre. This means that CYP are treated closer to home
• We have supported work on town redevelopment schemes to include health hubs, with an ambition to co-locate services wherever possible, making services easier to access
West Essex Health & Care Partnership
• Our partnership approach with Primary Care on the Integrated Urgent Assessment and Treatment Centre (IUATC) at Princess Alexandra Hospital (PAH), has laid the foundation for further partnership working. The Centre has helped to reduce the number of attendances at PAH emergency department, with continued development of community and out of hospital pathways
• Over winter we expanded our inpatient bed capacity at Herts and Essex Hospital (HEH) to support shared management of winter pressures at PAH. These were fully utilised, with our in-reach team working with PAH to quickly identify suitable patients to move into a community bed, improving hospital flow and supporting patient’s recovery and rehabilitation
• A new HCT-led Hertfordshire & West Essex Diabetic Eye Screening Programme commenced in April 2024. Through this we have begun to further extend and build relationships with GPs, hospital eye services and optometrists across the ICS, including in west Essex
Mental Health, Learning Disability & Autism Health & Care Partnership
• We have continued to champion the focus on neurodiversity services, which now has much clearer visibility and co-ordination of aims through the collective work of the Mental Health, Learning Disability and Autism (MHLDA) HCP
• HCT has developed an electronic referral pilot to enable an integrated front door to neurodiversity services. The operational / workforce approach to pathway management across system partners supports a shared ambition to reduce wait times for our CYP
HWE Community Provider Collaborative
• HCT has continued to develop informal collaborative ICS-wide working with Central London Community Healthcare NHS Trust (CLCH) and Essex Partnership University Trust (EPUT) and delivered a programme of operational improvement
• In response to the further development of the HWE ICS operating model, HCT’s CEO was asked to lead the formation of a formal Community Collaborative across HWE ICS with Essex Partnership University Trust (EPUT) and Central London Community Healthcare (CLCH). This is building on the strong foundations from informal working and is further strengthening the voice of community providers as the Government and NHSE seek to move towards more proactive care and work into the community
• The Collaborative has developed a shared workplan, which includes continued input to, and driving of, the Care Closer to Home Programme, consistent panICB implementation of the national core offer for adult community services and identifying opportunities to improve sharing and use of joint resources where it is strategically and operationally appropriate to do so
• The Collaborative has also provided the modelling of the community capacity required to support the ICS’s ambition for a 25% reduction in non-elective admissions
Primary Care
• We have continued to work closely with our GP colleagues through Primary Care Networks and Integrated Neighbourhood Care Boards
• We have further strengthened our working relationships with the establishment of an ENH Community and Primary Care interface meeting, designed to facilitate mutual sharing of issues and learning, and co-design of solutions
• Our Digital team have continued to develop thinking on our referral processes following engagement with Primary Care, which highlighted a long and overly complicated process
• Our Integrated Care Teams work across seven localities, providing around 33,000 contacts with patients a month, linking into both GP and secondary care to ensure the patients’ needs are promptly met. We have incorporated feedback from Primary Care into the new Adult Community Operating Model (ACOM)
Others, including other ICSs, County Councils, Schools, Hospices and the voluntary sector
• Because of the work we do, our partners extend beyond traditional healthcare settings. We have strong relationships with local government, educational settings, charity and voluntary sector organisations, and patient representative groups
• A key piece of partnership working this year has been the joint response to the Hertfordshire SEND inspection and subsequent report, with all involved organisations coming together to agree a focused action plan. The action plan was co-produced with professionals from across health, education and social care in Hertfordshire; parents and carers; and children and young people with SEND
• We have extended out partnership working with Garden House and Isabel Hospices, developing a more integrated model, with specialist palliative care nurses part of the UCCH workforce This supports the ICS’s 25% reduction in non-elective admissions ambition and provides invaluable support to patients and families for loved ones to be cared for either at home or in a hospice setting
We continue to seek our patients’ input and views into the way we deliver our services, with family and patient engagement especially key in the development of our CYP services. Our Health Inequalities Steering Group oversees our approach, recognising that we want to do more to target, listen, hear and respond to the health needs of those who experience greater inequity. We have continued to develop our Lived Experience Advisory Panels (LEAP), which help us to review recent patient experiences focusing on what matters most to patients, their families and carers, with particular focus on ethnic minority groups and vulnerable populations across HWE.
We have also continued to raise awareness of our social value approach, recognising the importance of understanding, and enhancing the social value impact we have as an organisation to improve the wellbeing of the communities we serve. Social value impact has become a lens that we apply to our delivery plan and ongoing work, with identification of a number of specific initiatives we can focus on to leverage our social impact goals. For example, we analyse our cancelled and missed appointments by indices of multiple deprivation (IMD) and this has helped us focus on how we design our services to make it easier for people to attend appointments, including where we locate service provision.
2.3.4 Strategic developments
Our organisational strategy includes eleven strategic outcomes. These outcomes are the main way that we monitor delivery of our organisational strategy The main way we do this is through our ‘strategy assurance and progress report’ which is put together every six months. This report is discussed at Quality Committee, People, Performance & Finance Committee (PPFC) and Strategy, Involvement & Planning Committee (SIPC), before ultimately being presented to Trust Board. This process means that each committee has oversight of the strategic outcomes that they have lead responsibility for and can assure themselves that we are progressing on our journey to achieve that outcome.
The strategy assurance and progress report details many of our achievements over the last year. The table below provides a few examples of some of the key developments that have directly contributed to our strategic outcomes over 2024/2025.
Strategic Outcome
Achieve Outstanding CQC rating
Improve clinical and patient reported outcomes
Examples of what we have done to support delivery
• We have continued to develop a new ‘organisational excellence’ framework which ensures a much stronger link between our organisational strategy, our vision and values, and our annual delivery plan. This year, using a robust analysis model, we identified a series of ‘breakthrough objectives’ which teams have been able to focus on, with a clear ‘golden thread’ back to the organisational strategy
• As part of this organisational excellence programme, we have been working on a ‘quality management system’ to ensure that the processes, systems and organisational rhythms are aligned to support high performing teams and encourage and support quality improvement across the organisation
• Following focussed work across the organisation, 94% of teams are now using Patient Reported Outcome Measures, and 90% are using Clinical Outcome Measures.
• 4 services have been identified in phase 1 of this programme and are becoming ‘outcome measures champions’
• We are building a specific outcome measures dashboard, which will enable us to maintain oversight of how we are impacting on patient outcomes at a service and Trust level
Improved Patient Experience
• One of our Trust’s key objectives for the year is to improve the response rate we achieve for the ‘Friends and Family Test,’ so we can better understand how our patients are experiencing the care we are providing. Whilst our overall response rate is still low, it has increased by 10% over 2024/25
• Of the responses we receive, we are proud that we consistently score above 95% of people saying their experience of HCT services were good or very good
• We have also implemented a number of specific initiatives this year to support how we improve and understand patient experience including:
o Our Diabetic Eye Screening Service have launched a series of community engagement events
o We have launched an engagement and involvement toolkit available to all staff
o Our CYP engagement group has been established and is working on setting up an HCT Youth Council
We have a large number of examples of where we have worked in collaboration with our system partners to develop services, reduce inequalities and deliver patient-centred care. Some examples over the past year include:
• We have launched the Urgent Care Coordination Hub (UCCH) in collaboration with East of England Ambulance Service, coordinating community response to 999 callers for the ICB. This has already proved successful in reducing ambulance callouts, conveyances and hospital admissions – enabling more patients to receive the care they need in their own home
More collaborative service delivery with partners
• Pilot of Joint Paediatric Audiology and Ear Nose and Throat clinic with West Herts Hospital Trust to support CYP who need hearing assessment and ENT consultation so as single co-ordinated appointment can take place resulting in agreed care plan for CYP at end of one appointment rather than two or more appointments being required.
• Working closely with new Family Support Service (FSS) provider, One YMCA, in Hertfordshire, to provide a seamless Public Health service for families in Hertfordshire
• Working with East & North Herts Trust on MSK in-reach to acute rheumatology clinics, to reduce the number of patients needing a consultant by using our skilled community MSK Physiotherapists –reducing waiting lists and improving patient care
• Young Carers Oral Health Project – working with Primary Care and Garden House Hospice, supporting young carers to understand how to support their family members with good oral hygiene, preventing the need for acute or emergency treatment
Improvement in staff survey results
• Mobilisation of new Diabetic Eye Screening Service, in collaboration with East & North Herts Trust, working together to support a successful mobilisation, transfer of some staff to HCT and joint service development work to ensure the service meets the needs of the population
Our 2023 staff survey results were published early in 2024/25. We were really proud of the improvements that we saw, indicating that HCT is a great place to work Some key highlights include:
• In 86% of staff survey questions, HCT scored higher than the average for other NHS Community Trusts
• 68% of questions showed an improvement from the 2022 staff survey (which had already shown an improvement in 53% of questions from the 2021 survey)
• Of the seven questions we have identified as ‘strategic staff survey questions’ six showed improvements from the previous year’s survey, and six were higher than the community services average
• There were also some key questions on which we were pleased to see that we scored particularly highly when compared to the national results (out of 270 organisations) Many of these align strongly with our vision and values:
o 8th nationally in ‘I look forward to going to work’
o 10th nationally in ‘I am trusted to do my job’
o 3rd nationally in ‘people I work with are understanding and kind to one another’
o 4th nationally in ‘I would feel secure raising concerns about unsafe clinical practice’
o 5th nationally overall in the ‘Inclusion’ People Promise theme
o We were in the top 10% of 9 out of the 22 People Promise Elements including ‘we are compassionate & inclusive’, ‘diversity & equality’ and ‘we each have a voice that counts’
Whilst we are extremely proud of these results, we also know that this is not a consistent picture for every team or every member of staff We have done a detailed analysis of our staff survey results to identify specific subjects and teams and have put an action plan in place This includes each team developing a staff survey action plan to address local themes
Improvements in BAME staff survey results
• Our 2023 staff survey results showed that across eight out of the nine staff survey themes, the scores for BAME staff were equal to, or higher than, the results for white members of staff. We are pleased that our continued and proactive work in this area continues to ensure that at a Trust level, we can be confident that our BAME staff are not experiencing an inequality in their experiences of working for HCT
Innovative solutions to problems and service developments
• While the overall scores for BAME staff are positive, as with last year they conceal differences among smaller staff groups, highlighting the need for a deeper understanding of different smaller staff cohorts. As with the broader staff survey results, we have done a detailed analysis to identify the groups who do have a less positive experience of HCT and have put actions in place to support them
Examples of innovative service developments over the past year include:
• CYP Speech & Language Therapy - The service over December 2023 and January 2024 tackled a large backlog of EHCP assessments. To achieve this, the team moved away from a longstanding model of assessment in school, specifically linked to undertake an EHCP assessment. Instead, the team profiled the waiting list, identified CYP already known to the service, engaged with school on different models of getting information from the setting; meaning only CYP who required school based assessment were seen in school and others had reports provided from existing information or were invited to clinic for a shorter assessment. This resulted in large numbers of assessments and reports being completed over a 4-8 week period – clearing the backlog
• Integrated Heart Failure Service - Working with palliative care, PCNs and secondary care in the Lower Lea Valley area, this service has supported patients to prevent admission to secondary care and enabled patients to be cared for in their preferred place
• MSK services – Osteotomy - All atraumatic and non-acute knee pain will be received into the HCT MSK CATS Service, assessed and if appropriate referred for specialist radiological imaging from community services If, following imaging, patients are suitable for the new integrated osteotomy pathway, HCT will refer directly to the knee unit at ENHT. It is anticipated that the new pathway will streamline the patient journey and experience, improve waiting times and save on secondary care appointment time by preparing necessary pre-operative imaging in community services and directly referring to a specialist knee clinic
• Nutrition and Dietetic – We are using our nutrition & dietetics expertise to support East & North Herts Hospital Trust, supporting their catering provision, making sure that the food that they serve can play a key role in improving the health and recovery of their patients
• We have developed a digital front door to allow a single point of access for healthcare professionals, and other referrers to access our health referral forms via the Trust internet. This makes referral to our services easier, and improves efficiency or receiving them within HCT
Designing and delivering services to Reduce inequalities
• Hospital at Home – we have implemented ECG real time data capture directly into SystmOne This allows clinical staff to be able to monitor and record ECG data to enhance delivery of care and improve timely clinical decision making
Our Health Inequalities Steering Group leads our work to ensure that we are proactively seeking to address inequalities of access and outcomes for our population Some examples of what we have done includes:
• Development of new Health Inequalities dashboard, to be used to identify and analyse ‘do not attend’ rates which can often be greater for areas of higher deprivation
• Introduction of ‘Ask Listen Do’ resources to enable patients with learning disabilities, autism or both to give feedback including complaints
• Implementation of McGowan Training for Autism and Learning Disabilities
• Partnership working with health visitors, vaccination teams and dental team to support access through pop up clinics in areas of high deprivation
• Our net-zero roadmap is in place, and has supported a significant allocation of capital funds over the next five years for environmental sustainability initiatives
Achieving net-zero by 2040, and to reach 80% by 2028
• We have installed a range of energy saving measures across our sites including LED lighting, solar panels and building management systems
• We have reduced our electricity consumption by 16%, and gas consumption by 20% between 2023/24 and 2024/25
• During 2024/25 100% of the Trust’s non-clinical waste was diverted from landfill resulting in 7,824 kg of CO2 being saved
2.3.5 Focus on health inequalities
HCT has continued this year to work collaboratively with patients, families and carers, as well as engaging with regional partners and the ICB. There has been a strong focus on digital inclusion; we are aware that it is essential to consider the impact digital solutions have on inequalities as we work to deliver outstanding patient-centred care closer to home. Our plans for digital inclusion have been guided by NHSE digital inclusion framework and a further focus on this important area is planned for the coming year.
The Health Inequalities plan, which received final approval in April 2023, outlines HCT’s objectives and plans to reduce health inequalities across Hertfordshire. NHSE’s statement on health inequalities has influenced the plan which has been extended to cover 2025/26 and focuses on five pillars to reduce health inequity: Identification, Access, Experience, Outcomes and What can you do?
Key developments in relation to the five pillars include:
• HCT are focusing on ensuring Was Not Brought In (WNBI) is recorded accurately within patient records. This is a quality priority for the Trust. This will help us to identify vulnerable children and adults who may be at risk of health inequalities if they miss their appointments
Identification
Access
Experience
Outcomes Drivers
• The SystmOne reasonable adjustment flag is now embedded across HCT services, is used for all patients and service users who need reasonable adjustments and is reported within the BI portal. Since its launch in April 2022, over 3000 reasonable adjustment flags have been recorded including vital information to help support a reduction in health inequalities. HCT are following all national guidance on plans for linking the reasonable adjustment flag to the National Spine
• The dental team are continuing their primary prevention initiative of ‘pop up’ dental clinics in children’s centres located in IMD 1 and 2. Pre-school children and their families have been offered oral health advice as well as dental screening and fluoride varnish application by the Special Care Dental Service. This primary prevention initiative supports the CORE20PLUS5 aim of reducing the number of children admitted to hospital for dental general anaesthetic. The Dental team are expanding the work to include gypsy traveller and Roma sites across the county
• HCT continues to work with Communities First and Healthwatch supporting teams to use volunteers for engagement and co-production work
• The digital team have been focused on digital inclusion ensuring that: created forms can be opened on any device (laptop, tablet, phone) in the preferred language option used by the referrer Fonts can be enlarged on users’ devices, simple language is used and forms can be co-designed with relevant stakeholders. This work will actively improve patient experience
• The Inpatient teams have been auditing their use of an “Up and Dressed” process “PJ paralysis” refers to the lack of movement that occurs when people remain in their pyjamas or gowns for longer than necessary. This can lead to a higher risk of infection and loss of mobility and strength The team are carrying out audit cycles to review their process. To reduce the risk of health inequalities and improve inpatient outcomes, provisions have been made for spare clothes and laundry facilities to support individuals without family support
What will you do?
• The Oliver McGowan training has proved very popular with staff reporting that they have found both the eLearning and in person sessions to be very impactful
• Staff have also reported very positively to in-person Shared Decision Making training
2.3.6 Operational developments
HCT continues to prioritise the services which support urgent and emergency care for adults and children, whilst also maintaining delivery and reducing waiting lists. We continue to see increased referrals within our core services with a higher acuity of patients into many of our teams. Services and the Trust leadership maintain a high level of scrutiny of our waiting lists and continue to support the ongoing initiative to improve these.
We have been prioritising care to those with the greatest need, when required, and have been working with system partners to tackle pressures due additional demand.
We continue to work collaboratively with colleagues within Primary Care, Essex Partnership University NHS Foundation Trust (EPUT) and at Princess Alexandra Hospital NHS Trust (PAH) to deliver the Integrated Urgent Assessment and Treatment Centre (IUATC). We are working towards Phase 2 of the development, which includes greater utilisation of community services, both from within the IUATC but also supporting primary care, to make referrals before presentation at the IUATC
We are also working closely with system partners including EEAST, primary care, local acute trusts and care providers to maximise the opportunity to support patients to remain in their home and receive care closer to home through a range of services including Urgent Community Response, Hospital at Home and ICTs.
Thanks must go to our staff who continue to work hard to deliver high quality care and have maintained patient safety across our services during times of continued high demand.
Patient Initiated Follow Up (PIFU)
Patient Initiated Follow Up (PIFU) puts patients in control of their follow up appointments. PIFU is used in acute settings and national data reporting is mandatory.
Hertfordshire Community NHS Trust has collaborated with NHS England to be the first community trust nationally to pilot PIFU for community services (Adults and Children’s). PIFU has been implemented in 5 services, and a trajectory for further roll out across the trust has been agreed.
Patients on PIFU have access to the service should they need to discuss their condition or require an appointment within a defined period (6-12 months). This ensures patients only attend follow up appointments when and if they are clinically needed and frees up clinical time to see other patients.
A bespoke BI dashboard has been developed by HCT so that services can track their use of PIFU, and monthly data will be shared with NHS England.
Ongoing engagement with clinicians, parents and administrators will provide the necessary feedback to evaluate PIFU across HCT and make changes where appropriate.
Growth within the Hospital at Home (HAH) service
Throughout 2024/25 we have continued to grow and develop our HAH service. The service consistently demonstrates its agile and innovative approach to delivering patient centred care closer to home by flexing its baseline capacity to ensure patients can safely receive the treatment they require within their own homes.
The utilisation of the 204 commissioned beds has remained above 100% with December reported at 112% and January 138%. This flexible approach to the delivery of care allows patients with a higher level of acuity within their own home environment leading to improved patient and clinical outcomes. Where appropriate patients are supported with remote monitoring technology. The service is based on a clinical capability model which also includes shared decision making between the patient and the clinical team. Throughout 2024/25 the service has continued to develop new clinical pathways in conjunction with system partners further expanding the breadth and depth of its offer.
Children’s Hearing (Paediatric Audiology)
This small team provides a comprehensive audiology diagnostic and management service to children and young people aged 0-18 within West Hertfordshire. The team has worked tirelessly over the past year to reduce waiting lists and improve the quality within the service. Audiologists in the service have all contributed hugely by offering additional weekend appointments to tackle the waiting list over the year with the service waits falling to under one year having been over 65 weeks at the start of 2024-25.

Multidisciplinary working has increased this year to plug identified gaps in care for our population and to reduce long waits between services Joint clinics with Ear, Nose and Throat consultants (ENT – run by West Hertfordshire Hospitals Trust) have commenced at HCT sites to ensure patients undergo testing and receive management plans from ENT the same day. MDT clinics for CYP with a unilateral and mild hearing loss have commenced These CYP would otherwise not receive the same specialist support all in one appointment. This clinic aims to deliver equitable care for those patients who otherwise would not meet the threshold of need for intervention from the different services. Patient feedback so far has been overwhelmingly positive.
The service is undergoing the national NHS England PASQAT Paediatric Audiology Hearing Improvement Programme with a robust action plan and many improvements already made based on recommendations given by both NHS England and IQIPS (UKAS accreditation). The team had an IQIPS benchmarking assessment in Autumn 2024 and hope to apply for accreditation in Summer 2025.
The service has also continued providing mutual aid support to the paediatric audiology department in East and North Hertfordshire (ENHT) for babies referred from the newborn hearing screening programme.
Family engagement is improving through recruitment of new parent representatives to attend the Children’s Hearing Services Working Group (CHSWG). In addition, the service is undertaking targeted work around children not brought in (NBI) to appointments, particularly those from areas of highest deprivation to understand how the service can increase access and address any health inequalities. Implementation of a patient self-booking system for one of the service pathways has shown positive outcomes in reducing rates of NBI. This was implemented in November 2024, with reduction in NBI for this pathway from 17% to 9%.
CYP Therapies
Within CYP therapies waiting times for initial assessment have improved over the last 12 months. For Occupational Therapy 77% of children are seen for a health assessment within 14 weeks and 87% of children are seen for a speech and language therapy initial assessment within 10 weeks.
Following a targeted piece of work in SaLT, 49% of Education Health and Care Plan (EHCP) needs assessment reports are submitted within statutory timescales. An audit of EHCP reports showed that whilst the quality of CYP reports was good, the health advice was not always clearly translated into final plans. As a result we have changed our report format to be clearer for EHC coordinators to understand and accurately transfer content into plans.
Following a pilot project children’s physiotherapy has gone live with patient self-booking for initial assessments allowing parents/carers the flexibility to book appointments at times convenient to them. The CYP Physiotherapy service have joined a research project run by Oxford University to look at evidence-based interventions for children with cerebral palsy. Following successful completion of the training, we are now offering all eligible families a chance to participate.
The Occupational Therapy team have 2 quality improvement projects underway to improve practice. Development of home programmes to support attainment of client centred goals and embedding Occupational Performance Coaching in our care plan pathways to support self-management and reduce ref-referrals. The initial assessment report has been reviewed to populate from the assessment templates to reduce the time spent on report writing.
The Speech and Language Therapy (SaLT) has expanded their targeted language groups, introducing a group to support Key Stage 3 secondary school students. This group aims to help students explore supportive language strategies to increase selfmanagement of their language difficulties in the classroom. Speech and Language Therapy Education Leads have developed ‘The Herts Shining Communication Award.’ This is a tool for schools to use to support and improve the outcomes for children presenting with speech, language, and communication needs (SLCN). The aim of the tool is school settings to identify their strengths and areas of development in terms of the support provided for children with SLCN across 8 different ‘rays’ (families, quality, leadership, intervention, identification, environment, training, knowledge). The SaLT service has also updated the speech sound care pathway introducing an early year’s speech clinic. These changes were based on service users and staff feedback along with evidence-based research.
HCT’s East of England (EoE) Child Health Information Service (CHIS)
The EoE Child Health Information Service has now formally launched, expanding its existing comprehensive failsafe functions and GP practice engagements to now cover the entire region. This ensures that every corner of the region benefits from the meticulous and robust HCT systems in place. In addition, the EoE CHIS Service has begun to pilot digital immunisation scheduling engagement. This pioneering tool aims to increase vaccination uptake among an increasingly digitally dependent population. By leveraging modern technology, the platform ensures more efficient and widespread communication, as well as directly supporting accessibility standards.
Health Immunisation Vision Insight System (HIVIS)
HIVIS is an innovative tool designed and built by HCT to aid commissioners, local authorities, and other stakeholders in visualising the uptake of vaccines and immunisations within their communities. This interactive heat map provides a detailed overview of vaccination patterns, highlighting areas with low uptake. By utilising HIVIS, stakeholders can effectively identify cohorts that require targeted interventions, thereby enhancing the response to immunisation gaps. This targeted approach helps to ensure better health outcomes by focusing resources and efforts where they are most needed. By addressing these disparities, the system supports improved overall community public health and aids in achieving comprehensive immunisation coverage and prevent disease outbreak and spread.
Call and Recall
The Call-Recall Service for Immunisations in the East of England is a CHIS hosted project funded by NHS England. The service aims to increase vaccination uptake among children and pregnant women by proactively contacting unvaccinated individuals and their parents/carers. The service is delivered by the Child Health Information Service (CHIS) and our Community and School-Aged Immunisation Service (CSAIS), who are collaborating to identify and contact unvaccinated individuals. The service will focus on increasing uptake of routine childhood vaccinations, particularly MMR, RSV, Flu and COVID-19 vaccines, to reverse recent declines in immunisation rates.
The service employs a diverse team with appropriate training and language skills to conduct sensitive and culturally appropriate vaccine conversations. Key performance indicators include contacting 100% of unvaccinated individuals, achieving over 50% positive outcomes from calls, and reaching ≥95% MMR uptake for specific age groups by the end of Q2 2025. The service aims to reduce health inequities, mortality, and morbidity from vaccine-preventable diseases, and decrease hospital admissions and absenteeism.
Dental services
Our Special Care Dental service was awarded a new contract by the ICB in October 2023 and has been expanding over the last 6 months, with plans for further expansion in 2025/26. A new dental surgery has been installed in Nevells Road Clinic, Letchworth and a further surgery will be completed within the Dental Department at Cheshunt Community Hospital. This will enable staff to offer enhanced quality pathways for special care patients and anxious children.
The dental team have been funded by Hertfordshire County Council to extend their special school screening approach into schools within areas of deprivation. Many schools have agreed to a toothbrushing initiative for reception age children. The team
continue to operate pop-up clinics working in children’s centres located in high deprivation areas. Additionally, they are planning visits to Gypsy, Traveller and Roma sites to engage communities on oral health, conduct screenings and apply fluoride treatments

To assist children who suffer from severe dental anxiety, the Dental service has introduced a nurse-led pathway scheme. Videos were created to reassure anxious children by demonstrating what will happen at an appointment. This involved children of our staff playing the role of patients, being greeted by one of our dental team, being talked through what to expect, having an oral examination, learning to brush correctly, and having an x-ray. The team have also worked with experts by experience within Hertfordshire County Council Purple All Stars and have created similar videos for adults with special needs.
Pharmacy services
Pharmacy have led on a number of exciting projects on our wards this year:
• The Hospital at Home Pharmacy team have led on the development of a number of new pathways and clinical guidelines for HAH, allowing us to safely and effectively widen the scope of patients we can support. In particular, they have taken lead roles in the Intravenous Antibiotics Multidisciplinary meeting
• The anti-coagulation pharmacist continues to actively switch suitable patients from warfarin to safer and easier to manage Direct-Acting Oral Anticoagulants and initiation of Vit K antagonists
• Education and training to develop the next wave of Pharmacy talent is crucial for succession planning, especially in the fast developing Community Trust sector. The Pharmacy Department is very proud to host our first ever Pre-registration trainee pharmacy technician (jointly with East and North Herts Trust) as well as employ our first junior pharmacist in Hospital at Home
• Supporting our prescribers with their continuing professional development and providing a safe space to share experiences and learning is key to ensuring that they stay up to date and competent. To this end, the Pharmacy Department launched our inaugural Prescribing Forum to great success and feedback. These are hosted on a quarterly basis and prescribers have found them most useful
• The team has worked alongside the Clinical Systems team this year to launch Script Switch to all prescribers in the Trust. Script Switch is a system that provides actionable information, advice and guidance to reduce risks, improve outcomes and reduce prescribing costs. Whilst more work needs to take place for all prescribing services in HCT to use this software, savings this year have reached almost £10k and are in line with expectation
• The Pharmacy safety team have developed our process and involvement in medication safety incidents, embedding PSIRF into our practice. The overall aim is to support the medication safety culture within HCT, engage with patient facing
staff and managers and have oversight of learning from incidents across HCT. By ensuing we focus on low/no level harm in addition to serious incidents, we have been able to better understand the learning and actions, and support patient facing staff better by linking different parts of the organisation together to develop improvements
• Due to the increasing antibiotic usage within our Hospital at Home teams, the Pharmacy team have introduced two new audits to support good antimicrobial stewardship and compliance with formulary. We have also introduced a range of audits to support services with better medicines management
• We have developed a high-level Medicines Optimisation Plan in response to the ICS Medicines Optimisation Transformation Board provider request. This twoyear programme aims to reduce polypharmacy, reduce anti-cholinergic burden, support deprescribing and improve discharge and transfer of care with regards to medicines. The work covers all applicable services across HCT including wards, Hospital at Home, Integrated Care Teams and community clinics. We will need to work in partnership with other stakeholders such as the Primary Care Networks to deliver the benefits and work on this will begin in earnest in 2025/26
2.3.7 Corporate developments
Patient Safety Incident Response Framework (PSIRF) and Plan
HCT has continued to roll out and embed the Trust’s PSIRF and Plan across the Trust. The Patient Safety team have been visiting teams to raise awareness and After-Action Review training has been rolled out which supports learning on the front line and promotes a just and restorative culture. We are responding to incidents in a variety of ways to ensure that learning turns into sustainable improvement. The Trust has transitioned to reporting incidents to the NHS England Learning from Patient Safety Events (LFPSE) service through our incident reporting system, Radar, which is an improved national service for the recording and analysis of patient safety events that occur in healthcare in England.
Integrated Referral Management (IRM)
The IRM Programme brings together a number of digital projects designed to improve the referral processes. This year the programme has been revised and expanded to cover five workstreams to capture and improve the complete patient referral journey using digital forms and automation. Replacing manual paper referral forms with bespoke user-friendly digital forms allows external parties to submit referrals online at any time Mandated fields and validation rules mean that referrals are submitted with accurate and relevant information for clinical triage. This allows for a more streamlined and improved referral in processes for Primary Care and all other referrers, with significant potential for cost and efficiency savings, an improved experience for those using the service and an opportunity to significantly reduce the administration time required to process referrals
We are continuously striving to improve and are investigating accessibility features with a focus on contrast for dyslexia, animation to appeal to a younger generation and new colour design palate for more attractive visuals. The new digital forms are available for 11 of our services via a Digital Front Door hosted on the HCT website.
As part of the high-profile Mental Health, Learning Disabilities and Autism (MHLDA) Neurodiversity Programme HCT are leading on the establishment of a single point of
referral (ASD and ADHD) covering both ENHT and HCT, a first step towards mobilising a countywide neurodiversity pathway. The Trust is also working on a complex pathway redesign within our MSK service allowing clinicians to complete referral triage whilst ensuring accurate and robust reporting for the future.
Bighand Corti Artificial Intelligence (AI) Proof of Concept
BigHand approached HCT to be part of a proof of concept utilising new and exciting AI functionality and software to revolutionise clinical note taking. The aim is to help reduce manual processes by using the AI software to summarise and instantaneously transcribe conversations between clinicians and patients. A six-week trial has been confirmed with the Dental Service to test the software during face-to-face clinic appointment for nurse led assessments.
2.3.8 Key strategic risks and uncertainties
In March 2024, the Audit Committee reviewed HCT’s Risk Management Framework, Risk Appetite Statement and Board Assurance Framework (BAF), which was approved without material change. Taken together these documents set out how risks are managed within the Trust The Risk Appetite statement and Risk Management Framework were reviewed by the Board in June 2023 and will be presented again in June 2025.
Risks to the achievement of the Trust's strategic objectives are identified by the Executive Team and added to the BAF. The BAF is submitted for review and discussion by the Audit Committee and the Board of Directors. Strategic and high-level risks and their implications are considered by each Board Committee, and each BAF and highlevel risk has a lead Committee identified which monitors and seeks assurance with regards to the management and mitigation of the risk.
The Trust’s main strategic risks are linked to the delivery of the Trust’s strategic priorities and include both threat and opportunity risks These are listed below:
STRATEGIC RISKS
• The ability of the Trust to meet patient demand as a result of a growing patient base, increasing reliance on community services providers and insufficient capacity
• The ability of the Trust to provide appropriate care as a result of inadequate or failing standards and ineffective governance
• Cyber threats and potential compromises in information security that can arise as a result of vulnerabilities in cyber security protection
• The implementation and embedding of digital and technological solutions to support transformation, service improvement and efficiency
• Financial management and expenditure control affecting underlying financial position which could affect service delivery and ability to operate
• The ability of the Trust to address health inequalities as a result of inadequate information, which could impact on vulnerable groups and those with protected characteristics being underserved
• Compliance with regulatory standards and responding to legislative changes
• The ability of the Trust to deliver its strategy and provide outstanding joined up care through partnership working and collaboration, which could lead to poor patient outcomes and experience and poor value for money for the system
• Major disruptive external events which may occur as a result of environmental hazards, accident or system failure including impact on availability of estates
• Ability of the Trust to recruit and retain the skilled workforce it requires to meet service needs
• The wellbeing, general resilience and morale of staff arising from sustained high levels of demand, workforce pressures and exposure to stressful situations
2.3.9 Going concern
The Trust is required under International Accounting Standard 1: Presentation of Financial Statements to assess the Trust financial and operational activities and whether any of these raise concerns for the Trust to be considered a going concern, and to agree the basis that its financial statements are prepared on with external audit. The Trust’s management is satisfied that there is no financial risk or operational risks or other risks that might cast significant doubt upon the ability of the Trust to continue to operate as a going concern The Board of Directors has therefore assessed the Trust as a going concern in accordance with Department of Health and Social Care Group Accounting Manual (GAM) 2024/25
The organisation continues to work as part of the HWE ICS and continues to remain a statutory organisation, with a long-term strategy and plan to ensure its future sustainability and positive service delivery model.
Given the above and an overall review of the Trust's future cashflows, its current liabilities and assets and, as a non-trading entity in the public sector, there is full expectation that the services provided by the Trust will continue in the future. On that basis, the Board of Directors considers it is appropriate to prepare the 2024/25 Accounts on a going concern basis. The financial statements do not include the adjustments to the valuation of its assets and liabilities that would result if the Trust were unable to continue as a going concern.
2.4 Performance Analysis
The purpose of this section of the report is to provide an analysis of the Trust performance across areas including Quality, Operational and Financial Performance plus an assessment of progress made in relation to Sustainability and our work on Equity, Diversity and Human Rights. There are separate reports below covering each of these areas.
2.4.1 Performance summary
The NHS national priorities and operational planning guidance for 2024/25 were published in March 2024 and set out national priorities and key areas of focus where systems needed to develop longer-term plans to meet the demands for the future Service recovery remained a priority for 2024/25 and improving productivity following the COVID pandemic. Longer term priorities included a focus on improving population health more broadly, modernising infrastructure and improving digital maturity.
This aligns well with HCT’s priorities set out within the Trust Strategy and our enabling strategies and HCT has a key role to play working with partners to deliver system priorities. Our organisational strategy is underpinned by our True North domains and associated breakthrough objectives. The Trust has chosen five breakthrough objectives for the year which we have been targeting, adopting a continuous quality improvement approach:
There has been a sustained focus on improving our performance management throughout the year with the development of an integrated Assurance and Support Framework Services, business units and the Executive team undertake a monthly review of performance within Executive Performance Review (EPR) and Operational Performance Review (OPR) meetings and going forward there will be a more in-depth focus on individual services areas via new Executive and Operational level Integrated Assurance and Support meetings The Board of Directors monitors and reviews performance at each bi-monthly board meeting via the Service Recovery and Performance Report which provides performance information including operational, quality and workforce performance.
HCT has continued its work on productivity improvements within key services and has continued to transform all its services, through better use of technology and estates, pathway redesign, and a focus on self-care and prevention. Social value has been a key area of focus throughout, with work ongoing to address health inequalities including work on reasonable adjustments and work on digital inclusion.
Oversight of programme and project delivery and operational performance is achieved through internal trust governance structures which are summarised below:

Monitoring and Assurance Through Trust Governance Structures
Overall HCT has performed well against the national priorities and expectations as described in this Performance Report and elsewhere in the Annual Report.
2.4.2 NHS System Oversight Framework
The NHS continues to use the NHS Oversight Framework. The framework is designed to support the ambition for system led delivery of integrated care in line with the direction of travel set out in the NHS Long-Term Plan.
A set of oversight metrics is used to test alignment with the framework’s five national themes. Where an organisation is triggering a concern and a potential support need is identified, NHSE will consider why the trigger has arisen and whether a support need exists. For HCT during 2024/25 the Trust remained in Segment 2, meaning that no concerns were raised by NHSE and no support needs have been identified.
The Trust participates actively in the Hertfordshire and West Essex Integrated Care System (ICS) and is a key contributor as a member of the Integrated Care Board, supporting partners and the ICB in delivery of the Integrated Care Strategy.
2.4.3 True North Domains and Breakthrough Objectives
The themes within the Oversight Framework are reflected in our True North Domains and breakthrough objectives for the year:
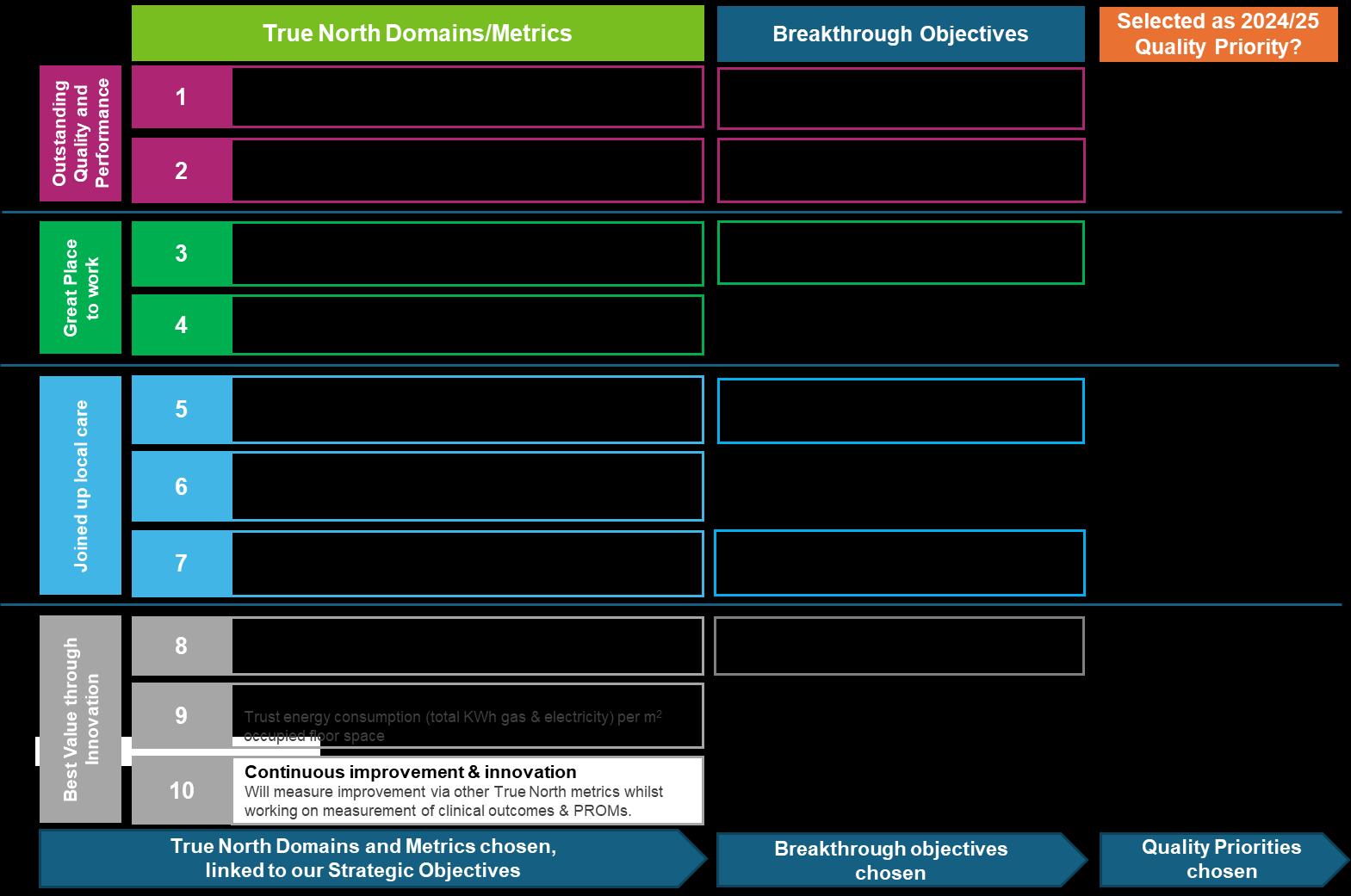
Transformation and quality improvement techniques have been used to drive improvement in key areas of performance including our breakthrough objectives. The Trust set itself challenging targets for its breakthrough objectives for the 2024/25 reporting year and whilst the Trust has seen improvement in its breakthrough objectives, further focussed work will be required to fully achieve our breakthrough KPIs against a backdrop of continuing high levels of demand and complexity of need.
The figure below provides an overview of our performance across the five breakthrough objectives for 2024/25:
True North metrics, Breakthrough Objectives and Quality Priorities
D1 - Reduce pressure ulcer incidents: Reduce the rate of low, moderate, and severe pressure ulcer incidents by 20% compared to the average monthly rate over the past 12 months
D2 - Improve waiting within target: Improve the percentage of patients waiting within target to 75% across HCT by the end of 2024/25.
D3 - Reduce staff turnover in the first two years of service: Continue to maintain overall Trust turnover in first two years of service at below 13% by the end of 2024/25.
Note: the KPI calculation is a rolling measure
D5 – Equality of access: No difference in DNA (did not attend) or NBI (not brought in) rate between a defined group of the population known to experience inequalities compared to the wider population
D7 – Improve FFT response rate: For each service to achieve a response rate of at least 2% of total contacts by the end of 2024/25 – if a service is currently above 2% then target is to maintain or improve the current rate.
D8 - Improve productivity: Improve productivity (cost/time per contact) and to continue to develop our productivity analysis to cover the full scope of services and better understand productivity at service level.






During the year we saw a significant improvement in our staff turnover rate, bettering our target of 13%. We also achieved modest improvements against a number of other
indicators including FFT response rates and our DNA/NBI figures. In terms of waiting lists our performance dipped by around 2% overall, reflecting the challenging environment and increasing demand for our services, particularly within CYP services.
2.4.4 Quality performance
Detailed information and analysis on the Trust’s performance and objectives in relation to the quality and safety of our services is contained within our Quality Account for 2024/25 which is due to be published in June 2025 This will be available on the Trust website at https://www.hct.nhs.uk/our-publications
The Trust continues to operate within a strong framework to ensure that we continue to deliver high quality services. We define quality as delivering:
• Excellent clinical effectiveness and outcomes: consistent and improving care
• An outstanding patient and carer experience: responsive and inclusive care
• Improving patient safety through learning: safe and compassionate care
Quality performance and quality improvement initiatives are driven, assessed and measured by several sources - internally through our Quality Committee and externally through our commissioners, the Care Quality Commission, other statutory and regulatory bodies, national initiatives, reports and guidance.
Examples include the following:
Responses to internally identified areas for improvement
Some of our improvement measures, controls and assurances include:
• Quality Assurance Framework including accreditation
• Continuing implementation of the Patient Safety Incident Response Framework
• Project to support development and implementation of Clinical and PatientReported Outcome Measures
• Reports on all aspects of quality improvement and performance are submitted to the Trust’s Quality Committee and Trust Board (including patient safety incidents, learning from deaths, complaints, compliance with National Institute for Health and Care Excellence (NICE) guidelines and participation in clinical audit)
• Identification and sharing learning and improvements from patient care incidents, complaints, and clinical audit with staff through editions of ‘Sharing Lessons in Practice’ and ‘Making Things Better’ newsletter
• Identification and management of quality-related risks, with escalation to the HighLevel Risk Register for additional oversight and monitoring
• Record keeping dip tests, self-assessments (Quality Wheels), and internal peer reviews as part of the Quality Assurance Framework, leading to improvement actions monitored through locally held Continuous Quality Improvement Plans
• Accreditation Programme to enable operational services to attain an accreditation rating based on the outcome of Quality Assurance Framework self-assessments and internal peer reviews, demonstrating delivery of consistent and improving high quality care
• The performance monitoring of service quality delivered as part of the monthly Operational Performance Review and Executive Performance Review
• Clinical audits informed by national and locally agreed professional standards, with review of outcomes and identification of learning through the Clinical Audit Working Group
• Responses to staff concerns raised with the Freedom to Speak Up Guardian
• Responses to patient surveys and questionnaires, including the national ‘Friends and Family Test’ (FFT)
• National NHS survey outcomes, reviewed by HCT’s Staff Council and Joint Negotiating Committee to develop an action plan to address outcomes
• Patient Led Assessment of the Care Environment (PLACE)
• Learning from the review of deaths – all deaths occurring in our community hospitals and some deaths of patients in the community are subject to case record review with oversight by the Learning from Deaths Panel
• Development of quality priorities to support delivery of HCT’s strategic objectives and outcomes
• Development of Operational Excellence through our new Integrated Assurance and Support Framework and Quality Improvement (QI) offer.
Responses to areas for improvement identified by commissioners and other statutory/regulatory bodies
• Quality key performance indicators are agreed in our contracts with commissioners (plus monitoring through regular meetings and quality assurance visits by the commissioners)
• Findings from Care Quality Commission inspections, reviews and through regular engagement meetings
• Benchmarking of key national targets by NHS England (NHSE)
• Two commissioner-led quality assurance visits to services providing support and healthcare to children and young People with Special Educational Needs and Disabilities (SEND)
• Review of complaints and concerns raised through the CQC
• Risk management through the Learning from Patient Safety Events (LFPSE)
• Section 11 audit of Safeguarding Children services and a review to provide assurance of compliance with safeguarding adults best practice carried out by commissioners (completion of two-year improvement plan approved by commissioners in November 2024)
• Joint Targeted Area Inspection (JTAI) multi-agency response to children who are victims of domestic abuse
• Table-top Paediatric Audiology Service Quality Assurance Toolkit (PASQAT) review of Children’s Hearing Service and subsequent visit from NHS England
• Improving Quality in Physiological Services (IQIPS) accreditation pre-assessment visit to Children’s Hearing Service
• Royal College of Physicians (RCP) Pulmonary Rehabilitation Services Accreditation Scheme (PRSAS) pre-assessment visit to Pulmonary Rehabilitation service
• NHS Elect review of Community Paediatric waiting lists
• Commissioner-led partnership quality visit to Lower Lea Valley Integrated Community Team
• NHS England Screening Quality Assurance Service (SQAS) pre-visit evidence submission regarding Herts & West Essex Diabetic Eye Screening Programme (visit scheduled for June 2025)
National initiatives, reports, guidance and legality
• External, national initiatives such as supporting patient flow, developing sepsis management, and reducing health inequalities
• NHS England workforce implementation plan engagement, enabling support for Nursing Associates registration, the First Contact Practitioners (Allied Health Professionals (AHPs)) pilot and future planning for AHPs
• Care Quality Commission Fundamental Standards of Care
• NHS Elect initiatives including Never Events and collaboratives
• The NHS Outcomes Framework
• NICE guidance and quality standards
• Implementation and embedding of the NHS England Patient Safety Strategy, including the Patient Safety Incident Response Framework (PSIRF) for Involving Patients in Patient Safety and the Patient Safety Syllabus
• Participation in Professional Nurse Advocate Programme
• UK Accreditation Service (UKAS) Improving quality in physiological services (IQIPS) accreditation for Paediatric Hearing services (HCT service registered in March 2023)
• Royal College of Physicians Pulmonary Rehabilitation Services Accreditation Scheme (PRSAS)
• UNICEF Baby Friendly Initiative Gold Award
• Compliance with CQC Regulation 20: Duty of Candour, the National Quality Board’s National Guidance on Learning from Deaths
Care Quality Commission
HCT’s overall CQC rating was confirmed as ‘Good’ following a CQC core service and well-led inspection of the Trust carried out during February/March 2020.

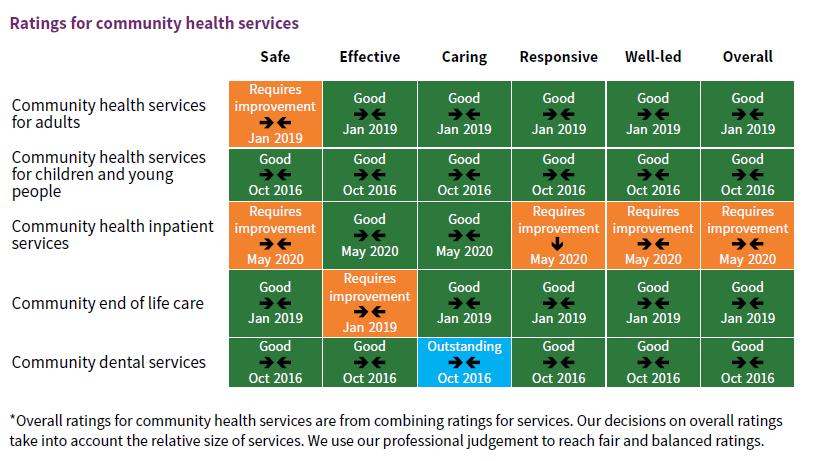
An internal audit was undertaken in June 2024 to provide assurance that HCT has a robust programme in place to implement previous regulatory compliance recommendations from the CQC and to increase the overall rating from "good" to "outstanding".
The audit found well-designed controls surrounding the retention of evidence on completed CQC and Good To Outstanding (G2O) programme actions, and an appropriate governance structure surrounding the G2O programme which showed regular scrutiny and reporting at an operational and strategic level.
An overall rating of ‘substantial assurance’ was awarded.
CQC liaison and inspection activity
There have been no CQC inspections or assessments of HCT services during 2024/25. During 2024/25 quarterly engagement meetings have been held between HCT Quality Team members, and CQC’s Herts & West Essex operational managers and regulatory coordinator, offering an opportunity for open discussion regarding areas of challenge and risk, identifying areas of good practice and any changes in Trust services or leadership. These meetings were extended from December 2024 to provide opportunity to showcase HCT services or highlight areas of good practice or innovation. The CQC’s Regulatory Coordinator for Herts & West Essex has also attended a number of Board and Board Committee meetings throughout the year.
We have continued to respond to any enquiries raised with the CQC in relation to our services and have been proactive in escalating any concerns we believe may be raised with the CQC.
2.4.5 Operational performance
HCT’s operational performance during 2024/25 is set out below. Where available trend data is provided below.
Performance is compared to two different periods: a pre-pandemic comparator (2019/20) and also to last year (2023/24). This is to ensure we have a meaningful
comparator and accurate representation of performance and recovery. In many respects performance is strong, including performance in our Urgent and Emergency Care services (Urgent Community Response and Hospital at Home), School-Aged Immunisations service and the Public Health Nursing service. Performance against access targets in Adults and CYP services however requires improvement, in particular, the deterioration in ‘waiting within target’ performance
Performance summary
At Trust level, compared to 2023/24, referrals were 4.1% higher at the end of March 2025; 5% higher in adult services and 0.7% higher for CYP specialist services1 . Compared to 2019/20, referrals were 24.1% higher in 2024/25; 21% higher for adult services and 40.5% for CYP specialist services.
Overall, Trust ‘waiting within target’ performance was 66.2% at the end of March 2025 which is less favourable than the March 2024 position of 70.7%. This measure encompasses all service specific waiting times (i.e., not just for those with an 18-week target). Performance was 77.7 % in adult services (vs 82.8% in March 2024) In CYP specialist services, current performance is 46.9% (vs 52.1% in March 2024). The pressure on waiting times primarily results from increased referrals translating into longer waiting lists.
The total Trust waiting list rose to 18,388 (i.e., waiters across all services) which is higher than March 2024 when the total list was 17,413. The total number of patients waiting is 46.6% higher than March 2019. The long-term trend can be seen below:

SPC: Total Trust waiting list
Performance in relation to long waits shows 290 patients waiting over 52-weeks, an improvement on March 2024 when there were 329.
For the year 2024/25, performance in the East and North Herts Urgent Community Response (UCR) service has consistently remained above the target for more than 70% of patients to be seen within two hours, with performance averaging 74% for the year. The Hospital at Home service has also delivered above targeted performance, with occupancy exceeding the target capacity of 204 available virtual ward beds per day. Since December 2024, the service has helped to address system winter pressures through operating at between 111% and 137% of the targeted 204 bed capacity each month. This is well above the national occupancy target of 80% and the local stretch target of 85%. Referrals accepted were also significantly above the planned monthly target of 522 over the year, with 761 referrals accepted in March.
1 The summary in terms of referrals and waiting times focuses on CYP specialist services, rather than HCT’s universal CYP services (Public Health Nursing and School-Aged Immunisations) as the latter have a different set of key performance indicators and are not services with waiting lists.

Equalities analysis using the indices of multiple deprivation (IMD) shows that waiting time performance for patients living in more deprived and less deprived neighbourhoods is very similar. We see a higher rate of patients not attending their appointments (DNAs) for those living in a relatively more deprived location, although parity was achieved in March 2025.
Waiting times
The improving trend of reducing long waits has continued over the past year.
Over 65-weeks and 78 week waits: In March, there were no over 78-week waiters. There were 11 over 65-week waits, showing the considerable progress made from the high point of 127 over 65-week waits in August 2023.
52-weeks: There were 290 patients waiting over 52-weeks (down from a high of 627 in August 2023), of which 226 waits are for Community Paediatrics (provided in south and west Herts) and 34 waits are for Pain Management and Chronic Fatigue. There has been a significant reduction of over 52-week waiters in Paediatric Audiology (provided in south and west Herts), with 17 in March 2025, a reduction from a high of 318 in October 2023.
Trust level 52 and 40-week waits performance is shown below.
Trust over 52-week waits:
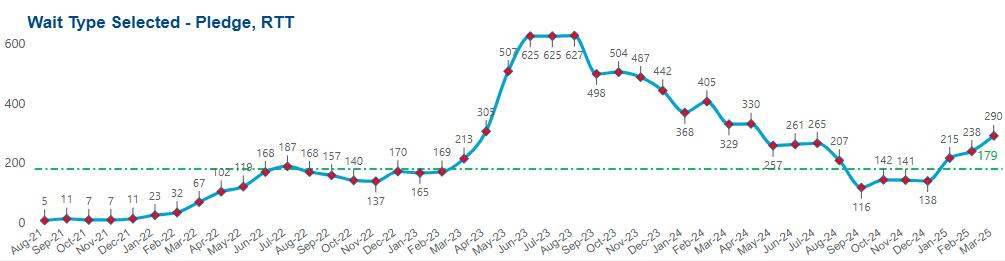
At the end of March 2025 18-week performance in the three consultant-led services (Community Paediatrics, Paediatric Audiology and Skin Health) continues an improving trend to stand at 62.1% but remains below the target of 92%.
In March 2025, across all services, 21.2% of patients were waiting over 18 weeks, an improvement of 2.9% compared to the end of 2023/24:

Community hospitals
Bed occupancy remains the highest at Danesbury with an average of 88% over the past 12 months. Herts & Essex and Queen Victoria Memorial Hospital (QVM) have an average occupancy of 84% and 79% respectively.
The average length of stay (ALOS) twelve-month average at both Herts & Essex and QVM remains above the contractual length of stay target of 19 days (for non-stroke beds) at 23 and 26 days respectively.
At Danesbury, the ALOS twelve-month average is 36 days. Danesbury is therefore achieving the contractual length of stay target for stroke beds which is below 42 days.
Admission rates into our community hospitals show no significant change over the year. Danesbury and QVM both have an average of 18 admissions a month, with Herts & Essex averaging 36.
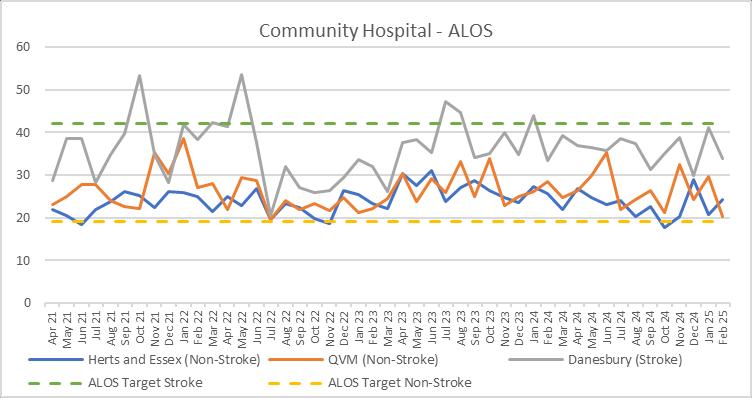
Community Hospitals – Average length of stay (ALOS in days) to February 2025 (most recent reported period)
Integrated Community Teams (ICTs)
Overall, in the east and north Herts ICT (including the small Royston team which is part of the Cambridgeshire & Peterborough Integrated Care System) the number of individuals being referred to the ICT is relatively stable with 15,851 patients referred in 2024/25 but contacts are 2.5% higher than in 2023/24. The remit of the ICT has extended considerably over recent years to now include Urgent Community Response and Hospital at Home services. The service identifies that patient complexity is increasing with more intensive treatments required e.g. numbers of intravenous antibiotics and end of life patients. This is reflected in the increased follow up ratio. A range of service design and technical transformation projects are currently underway to support the ICT.
Public Health Nursing
The service continues to perform well and meet its Key Performance Indicators (KPIs) as illustrated by the graphs for mandated contacts below.

School-Aged Immunisations
The HCT Community and School-Aged Immunisation Service (CSAIS) administered over 470,000 flu vaccinations to children and young people aged 4-16 across Hertfordshire, Bedfordshire, Luton, Milton Keynes, Norfolk, Suffolk, Cambridgeshire and Peterborough in the 2024/25 flu season. Uptake exceeded expectation with 78.8% of children aged 4-16 receiving a flu vaccine in Cambridgeshire (top of national rankings), 75.7% in Norfolk (second in national rankings), 70.1% in Suffolk and 68.4% in Hertfordshire. Peterborough and Bedford sit above the national average of 54.6% for primary aged children and 46.4% for secondary aged children and both have made improvements on last year’s uptake. The CSAIS teams work every year to improve vaccine coverage in the Special Educational Needs schools (SEND), pupil referral units and for the home schooled. We are very proud to be leaders in this programme nationally. The current contractual target is 65%.
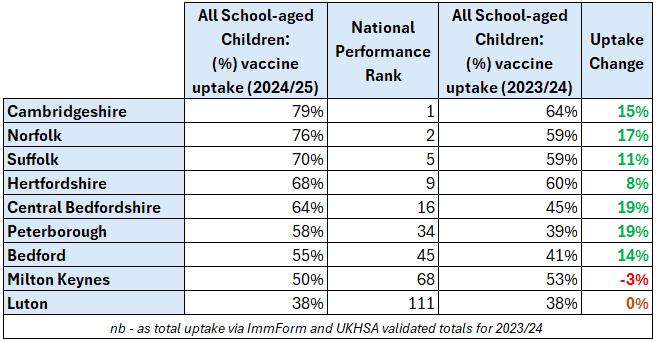
Table: School aged immunisation % vaccinated and national rank for the 2024/25 academic year compared to the 2023/24 academic year
Equalities analysis – Index of Multiple Deprivation (IMD) comparative analysis
The Trust routinely monitors performance of our services for those at risk of health inequalities (such as those living in more deprived neighbourhoods) as we continue to take forward work to analyse, develop and implement our action plan in relation to addressing health inequalities. In 2021, the Board agreed that those at risk of inequalities who have longer waiting times would be prioritised for appointments, in conjunction with prioritising by clinical need. The waiting time IMD analysis provides visibility on performance in this area.
The graphs below look at patients waiting over 12 weeks and compares those living in IMD deciles 1-3 (relatively more deprived neighbourhoods) versus those living in IMD deciles 4-10 (less deprived).
For CYP services we can see that patients living in IMD1-3 are not being disadvantaged against the 12-week measure. Overall, there is a strong correlation between the two IMD groupings. In recent months, performance is generally better for those living in more deprived areas (IMD1-3):

IMD waiting times analysis (over 12 weeks) – CYP Services
For Adult services, again there is a strong correlation between the two IMD groupings for waits over 12 weeks, with the percentage more favourable to those in more deprived neighbourhoods (IMD 1-3) in recent months:

IMD waiting times analysis (over 12 weeks) – Adult Services
Our IMD based analysis of ‘did not attend’ and ‘not brought in’ rates for appointments does show a disparity; with higher DNA percentages apparent for patients living in IMD 1-3. However, in March (see graph below) we see that there was parity between the two groups. There is also an improving trend since October 2024 in the monthly number of DNA/NBI instances – down from 3295 in October to 2676 in March 2025. The Trust now has a much greater focus on DNA and health inequalities generally, including this as a quality priority, with many excellent measures already in place. We also see increasing use of the reasonable adjustments flag in patient records.

Time sequence graph showing IMD grouping comparison of DNA percentages
Operational Assurance and Support Framework
We are currently holding portfolio level meetings (groups of services) as we pilot the introduction of an Assurance and Support Framework. Key features of the framework approach are:
• Focus on services and portfolios – one process for assurance and support across HCT, centred on services
• Consistent written approach to internal assurance and support - seeking to wrap corporate support around operational services in a more effective way
• Integrated oversight using five domains:
o Quality and safety
o Operational performance
o Workforce and culture
o Finance
o Strategy, quality improvement, transformation and external relations.
Business unit performance trends
The triangulated statistical process control (SPC) charts below highlight two predominant data features: a pattern of increased referrals and sustained pressure on CYP waits. The percentage waiting chart relates to ‘waiting within target’ performance.
For adult services, we can observe a) an increasing referral trend across the time series b) an increase in the number of contacts delivered over the last year c) a trend during 2023/24 where waiting times performance recovered strongly to pre-pandemic levels which has largely been maintained. The recent increase in contacts is likely to correlate to stabilisation in waiting times evident since May last year.
In the charts below, orange data points are used to highlight concerns and blue highlights data points of an improving nature. Grey presents data showing normal variation:

For CYP services the charts show, a) high number of referrals compared to prepandemic levels and now showing normal variation, b) normal variation in contacts c) sustained pressure on waiting time performance highlighted by the run of orange data points since July 2022:
Adult services SPCs

CYP services SPCs
Friends and Family test
In 2024/25, there were 9,504 patient responses counted with 94.5% providing either good or very good feedback. In terms of the response rate, 0.82% of contacts led to an FFT return against the Trust target of 2%, with a 1.16% response rate at the end of the year in March 2025.
Data quality
In the most recently published national update (December 2024), Trust data quality remains very strong in headline national metrics with an overall Data Quality Maturity Index (DQMI) compliance score of 91.6 which is significantly above the national average. The Community Services Data Set (CSDS) score is 93.1 and the Mental Health Services Data Set (MHSDS) scores 97.3 and both are above the national average. All scores are out of the maximum compliance ratings of 100. Reports are published by NHS Digital
End of year review of 2024/25 annual forecasts
All 2024/25 forecasts were set to have 75% confidence intervals. Overall, annual forecasting has been accurate other than for CYP total waiters where outturn is much more positive than expected with fewer waiters at the end of March 2025 than was anticipated. We have also seen slightly stronger growth in demand for adult services than was forecast and this is likely to have resulted in the number of total waiters being
at the upper end of the range.
2025/26 performance forecasting
The following domains have been forecast for 2025/26: total waiters, contacts, referrals, waiting within target, 52 week waits and 18 week waits. 2025/26 forecasts are set out below.
Our forecasts use algorithms to analyse data patterns and predict probably outcomes. They primarily employ an exponential smoothing approach, which is effective in capturing trends while addressing challenges related to data seasonality, noise, and irregular peaks. We have found that this ‘out of the box’ functionality is accurate in many scenarios and performs well on our data which tends to have good data quality, long and consistent time series, and be subject to seasonality.
Waiting within target for CYP specialist services is forecast to remain stable at between 40% and 50% in most months:

2025/26 CYP waiting within target forecast
Referrals to CYP specialist services are expected to follow a seasonal pattern and to remain largely stable:

2025/26 CYP referrals forecast
The total waiting list in CYP services is expected to remain stable:

2025/26 CYP total waiting list forecast
In adult services, waiting within target is expected to be consistent with a mid-point forecast between 75% and 80%:

2025/26 adult services waiting within target forecast
Referrals to adult specialist services are forecast to retain the level of growth seen in 2024/25:

2025/26 adult services referrals forecast
The total waiting list in adult services is expected to remain above the number preceding mid-2024 with a mid-point slightly above the current position:
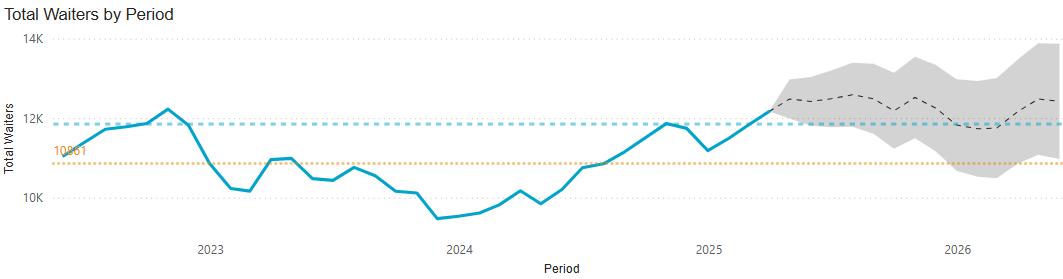
2025/26
At Trust level, the total waiting list is expected to remain at or above current levels and waiting within target performance is likely to remain under pressure between 65% and 70%: 2025/26

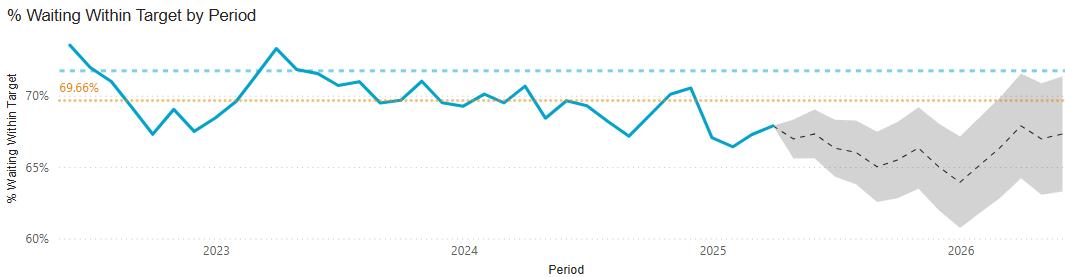
52-week waits are forecast to rise, to plateau and then to reduce (potentially close to the current level), however the forecasts provide a wide range within the confidence interval:

Risks to delivery of service performance and recovery
Whilst there are some services where performance and recovery is more challenging, there are also general risks to HCT service performance and recovery at an overall level. The identified overall risks are:
• Delivery is impacted by workforce availability due to recruitment and retention difficulties, competition for bank/agency staff and sickness.
• Delivery of is impacted by overall increase in demand across multiple services which exceeds activity plan expectations and planned workforce capacity hence leading to increases in waiting lists.
• Delivery is impacted by further COVID peaks/ winter demand pressures and the need to redeploy staff to surge enhanced services and hence reduced delivery capacity for planned care services.
• Delivery may be impacted by ongoing industrial action which would be likely to result in delayed care and longer waiting times in some services.
In addition to the general risks to service recovery and performance, we have reflected on the High-Level Risk Register (HLRR) the specific risks faced in some services around recovery and performance. Specific risks for Community Paediatrics, CYP therapies, ICT staffing, Public Health Nursing, PALMS, Paediatric Audiology and Adult SLT are recorded on the HLRR.
A further risk is that performance and recovery is unequal and health inequalities are further exacerbated if there is insufficient focus/differentiated approach for those at risk of inequalities. We continue to take forward work to analyse, develop and implement our action plan in relation to health inequalities and are mindful of this risk in our planning. At the November 2021 People, Performance and Finance Committee (PPFC) and at Board it was agreed that those at risk of inequalities (such as those in most
deprived IMDs) who have longer waiting times would be prioritised for appointments, in conjunction with prioritising by clinical need. The waiting time IMD analysis above provides visibility on performance in this area.
2.4.6
Financial Performance
This section is a summary and overview only. Further details of the Trust’s financial position for the financial year 2024/25 can be seen in the financial statements and notes to the accounts in the Annual Accounts section of this Report which begins on page 116
2.4.5.1
Financial Reporting
The Trust reports under the National Health Service Act 2006, chapter 41 schedule 15: Preparation of Annual Accounts.
2.4.5.2
Sources of Finance
The Trust’s funding sources would normally come from contracts with commissioners to provide health services. The Trust has previously operated with most of its funding being on a block basis for its services, i.e. the Trust is paid a fixed sum of money to deliver a range of services with an indicative level of activity.
Formal contracting arrangements between commissioners and providers for services with a value above £0.5m continue. Values less than £0.5m are transacted by a ‘Low Volume Activity’ annual payment amount, covering both contractual and non-contractual transactions. The contracts with the ICBs and NHS England, together with contracts with Local Authorities, have formed most of the Trust’s income during 2024/25. In addition to the Trust’s core services, the Trust has continued to operate as the lead provider for COVID-19 mass vaccinations across a number of geographic areas. For 2024/25, the funding for this has been based on direct reimbursement of actual costs incurred by the Department of Health and Social Care.
2.4.5.3
Summary of Financial Performance
The Trust is reporting a deficit year-end position of £228k for the 2024/25 financial year, representing £100k over performance against plan. Whilst the overall financial outcome is favourable relative to the revised plan, the overachievement against plan reflects significant work on performance improvement and efficiency schemes, however a gap remains between the level of recurrent savings achieved and the requirement identified through financial planning.

Non-recurrent mitigations contributing to the year-end position include one-off deficit funding, Elective Recovery Fund (ERF) income, and additional non-recurrent income from the ICB as a share of their year-end underspend. These mitigations have been used to offset year-to-date overspends across several services, including HCT inpatient wards, Hospital at Home, and Integrated Care Teams (ICTs). The overspends were primarily driven by operational pressures linked to expanded capacity within the ICTs and elevated occupancy levels in inpatient units, both of which were necessary to support system-wide Urgent and Emergency Care demands. The revenue position for 2024/25 reflects a £100k improvement against the original financial plan. This improvement is primarily driven by the receipt of additional system capital funding, which enables the reclassification of approximately £100k of revenue expenditure to capital programmes. As a result, the Trust’s net underlying run-rate at the year-end stands at a £3.0m deficit. The table below shows how HCT spent its funds in 2024/25. Threequarters of our expenditure is on staff costs, with a further 8% being spent on supplies, services and drugs.
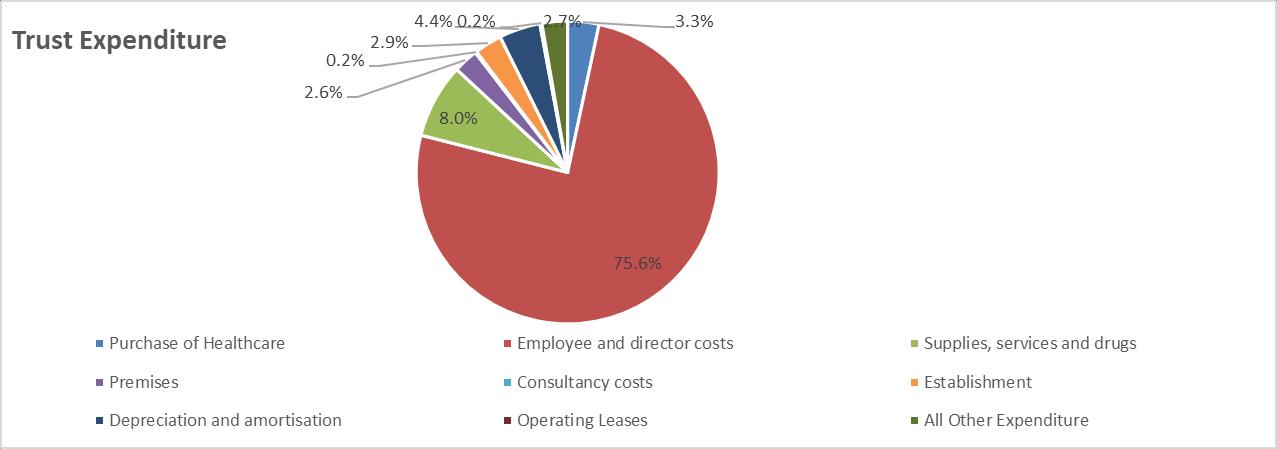
2.4.5.4 Capital Investment
Each year the Herts and West Essex system – via the ICB - is set a maximum capital spending limit. Within this, individual providers agree their own Capital Resource Limit (CRL). The Trust has met its CRL requirement for 2024/25 and has not overspent.
During the year, the Trust invested £4.95m in capital schemes (excluding the capitalised costs of new leases), compared with a planned spend of £4.86m – resulting in a minor overspend of £97k. This was offset by a £102k underspend on IFRS 16 lease capitalisations.
Key areas of capital investment included estates moves, ICT infrastructure replacement, green energy initiatives (e.g. air source heat pumps), and equipment for dental and audiology services
Capital expenditure is typically financed through internal sources, such as depreciation, amortisation, proceeds from asset disposals, and available cash reserves. In 2024/25 depreciation and amortisation totalled £7.6m, up from £6.9m in 2023/24.
The Trust’s cash reserves decreased in-year from £28.8m to £20.1m. This reduction reflects improvements in payment performance and a corresponding decrease in payables, alongside increased in receivables and capital spending, including IFRS 16 lease commitments
The monthly capital spend against plan can be seen in the chart below:

2024/25 Monthly capital spend
2.4.5.5
Cash
NHS Trusts are normally required to manage cash within their notified External Financing Limit (EFL). This limit is set by the Department of Health and Social Care and determines how much cash a Trust may spend beyond the income generated by its normal day-to-day operations. It is a breach of financial duty to overspend against the EFL. However, to enable NHS providers to utilise the resources available to them in the most effective way, the requirement to meet an EFL was removed as part of the COVIDrelated emergency funding arrangements and NHS England ensured that the NHS would have sufficient cash available to meet the demands caused by the pandemic; at the end of 2024/25, the requirement to operate within EFL has been removed following consultation.
At the end of the financial year the Trust had a cash balance of £13.4m, which is a reduction of £6.7m when compared with the prior year balance of £20.1m. This is in addition to the reduction of £8.7m reported at the end of 2023/24.
The Trust receives interest on these balances at 0.11% below the Bank of England base rate. This means that the Trust has generated £993k in interest received, slightly below the £1,008k planned.
2.4.5.6
Better Payments Practice Code
The Trust is required to comply with the Better Practice Payment Code (BPPC). The Code requires organisations to pay 95% of suppliers within 30 days of receiving a valid invoice. The cumulative position shows that we underachieved the target by volume by 2% in 2024/25 which is a slight deterioration on the previous year (2023/24underachieved by 0.2%) and underachieved the target by value by 2% (2023/24exceeded by 2.4%). Slow turnaround times in the coding and transfer of NHS invoices for approval was identified as the main driver of the deterioration, so targeted focus continues to be applied to improve this.
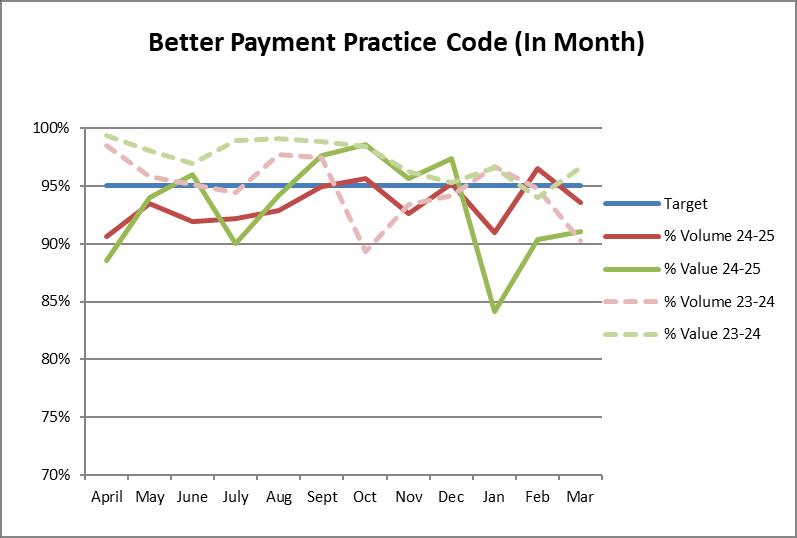
2.4.7 Sustainability
Background
We recognise that climate change poses a major threat to our planet and to the health and wellbeing of the population, and that HCT must play its part to support the NHS vision “to deliver the world’s first net zero health service and respond to climate change, improving health now and for future generations”.
‘Delivering a Net Zero National Health Service’ defines clear targets for the NHS to reach net zero carbon. These targets are:
• for the emissions we control directly (the NHS Carbon Footprint), net-zero by 2040, with an ambition to reach an 80% reduction by 2028 to 2032
• for the emissions we can influence (our NHS Carbon Footprint Plus), net-zero by 2045, with an ambition to reach an 80% reduction by 2036 to 2039
HCT is dedicated to being a sustainable healthcare provider that demonstrates social value and acts responsibly to minimise its impact on the environment and reduce its carbon footprint in line with national targets and the legislative framework.
Sustainability policies
HCT Green Plan (2022-2025)
In the HCT Green Plan we have set out the opportunities we identified to become more environmentally sustainable over the three years from 2022 to 2025.
HCT’s Green Vision is:
To become one of the most environmentally sustainable community providers in the NHS
As we pursue this, we commit to rapidly reducing our emissions, seeking the fastest trajectory to net zero:
• For emissions we directly control (NHS Carbon Footprint) we will achieve net zero by 2040, with an ambition to reach 80% reduction by 2028.
• For wider emissions we can influence (Carbon Footprint Plus), we will achieve net zero by 2045, with an ambition to reach 80% reduction by 2036.
The Trust has identified the following priorities for the Green Plan period:
• Target all forms of waste e.g. via LED lighting, heating control/insulation, waste and travel reduction
• Decarbonise heat – as natural gas for heat comprises 49% of our Carbon Footprint, we will aggressively target heat decarbonisation, planning for and commencing replacement of gas boilers with greener alternatives
• Greener supply chain – as our supply chain contributes over 75% of our Carbon Footprint Plus
• Data and decision making – we will implement carbon data analysis and reporting to measure progress, inform decision-making and target effective action
• Sustained engagement and simple communication with staff, patients and partners to support behaviour change
Net Zero Carbon Roadmap (2022-2040)
In addition to our Green Plan, we developed a Net Zero Carbon Roadmap (NZCR), which covers a longer period and incorporates the NHS’ wider ambitions for net zero. It provides more detail on the challenges faced and options available to reach net zero on the ‘Carbon Footprint’ emissions which result directly from Trust activity.
The Net Zero Roadmap supports our Trust capital planning as the roadmap identifies the scale of the capital investment required and provides a view of the profile of capital spend over time to achieve the required Net Zero.

NHS Estates Net Zero Carbon Delivery Plan
The national NHS Estates Net Zero Delivery Plan addresses the aspects of the net zero strategy pertinent to estates and facilities activities. The Trust’s Green Plan closely reflects this, and the national plan has supported us in developing our decarbonisation plan and estates strategy. It sets out a clear four step investment approach to
decarbonising NHS sites:


Sustainability performance
The Trust Board Lead for Net Zero reported to the Trust’s Strategy, Involvement and Planning Committee in November 2024 on the progress made in the third year of implementation of the HCT Green Plan. At that point, the status of the delivery of actions in our 3-year Green Plan 2022-25 was as follows:

An overview of progress and performance against the Green Plan is set out below.
Workforce and leadership
HCT has clear leadership and governance in place for environmental sustainability and net zero with Antonia Robson, Director of Business Services, providing overall leadership and chairing the Trust’s combined Green Steering and Green Champions Group which meets monthly and oversees implementation of the Green Plan.
The Board is well-sighted, engaged and supportive, with progress in implementing the
Green Plan last reviewed at Strategy, Involvement and Planning Committee (SIPC) in November 2024 and a discussion to inform the development of our next Green Plan at SIPC in March 2025.
We have continued to engage staff in the Trust’s green work this year. We have a Green Champions Network which meets virtually monthly and includes a champion for most Trust services. These champions promote green action and behaviours at a service-level and share successes and learning. We have been delighted to hear about the initiatives being undertaken by our services to reduce negative impacts on the environment.
We have engaged with all staff through:
• A programme of communications and engagement activity, which has included the Trust’s all-staff ‘Team Conversation’ meetings, regular articles in our staff bulletin, a workshop at Annual Leaders conference and a week of Green Learning Conversations and screensavers to coincide with COP29.
• A Green Award in our Leading Lights annual staff awards.
• Promotion of the ‘e-learning for healthcare’ Net Zero modules on our My Learning Zone staff training platform.
• Use of the ‘green spoke’ of the Quality Wheel to prompt services to review how they are doing on sustainability and plan continuous improvements.
The Trust is engaged with green work at a system, regional and national level and regularly attends the ICS Green Group and regional/national webinars and networks to enable partnership working and sharing of best practice.
Digital transformation
HCT recognises the importance of digital transformation to enable delivery of more sustainable models of care and reduce travel and use of consumables, such as paper. The Trust has a good starting point in terms of its digital maturity, for example all services use electronic patient records and we use digital systems for many aspects of administration and healthcare delivery, including use of video conferencing for consultations. However, there is considerable potential for further digital transformation and the approval by the Board in 2022/23 of our new Digital Strategy gives us an agreed way forward.
Notable digital transformation delivered during 2023/24 have already been mentioned In addition to these, we have started a project which aims to reduce the amount of correspondence and leaflets printed and posted by the Trust. The initial scoping work has identified considerable potential, and this will be taken forward as a priority initiative in 2024/25.
Estates and Facilities
The following has been delivered by HCT in relation to the 4-step approach to decarbonise estates:
• LED lighting implementation: this year completing rollout to four leasehold sites, building on our previous implementation in all freehold sites
• Building Management Systems (BMS) upgrades which allow for the remote control and monitoring of a building’s main mechanical plant e.g. boilers, ventilation and air conditioning. Building management systems should mitigate
issues with peaks in demand and reduce the overall energy demand. BMS have been implemented at a further four sites this year, meaning that we have upgraded a total of eight sites over the past two years
• Building fabric: we have commissioned surveys of building insulation across our estate to inform required investment for 25/26
• Air source heat pump: we have made an important first step in decarbonising heat and moving away from dependence on gas boilers with the installation of a heat pump at Park Drive Health Centre
• All utility invoices (electricity, gas & water) are checked and validated with monthly cost and consumption reports provided to estates. From these, and benchmarking data provided nationally, we can see (graphs below) the positive impact of the above measures, and the solar PV panels installed across nine sites in 2022/23 and 2023/24, on our energy consumption and associated carbon footprint. This has had the added benefit of protecting us from increased energy costs at a time of rising energy prices
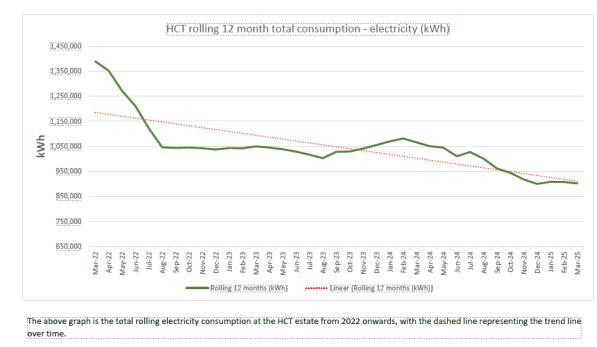

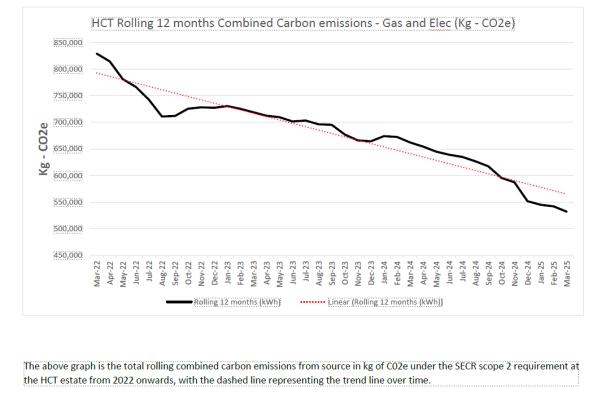
HCT electricity and gas consumption and associated carbon emissions charts


HCT energy consumption and emissions benchmarked against all community trusts nationally
Waste and recycling
The Trust continues to deliver and improve on waste hierarchy initiatives and the Trust’s Soft FM Manager has tendered and mobilised new waste disposal services to comply with national guidelines, to drive the net zero agenda and to reduce costs.
The Trust has upgraded its waste services to comply with the new government ‘Simpler Recycling’ initiative and included food waste collection services within its bed bases as a phase 1 approach.
Internal waste receptables are supplied and installed via Estates & Facilities to ensure correct segregation is conducted at point of disposal and posters/literature is being provided to support site-based knowledge.
The Trust has a walking aids reuse programme.
National – All Community Trusts
Non-clinical waste data
As an organisation we are committed to diverting waste from landfill and during 2024/25 the Trust produced 91.1 tonnes of waste of which 100% was diverted from landfill by utilising recycling and energy for waste (EfW) routes.
This form of disposal has resulted in 7,824 kilograms of CO2 being saved.

Clinical waste data


27 being planted, 3 off the road, 5 powered
All clinical waste produced within the organisation is processed at facilities that commit to zero to landfill. Non-infectious waste undertakes an alternative treatment process which shreds and disinfects the waste, compacts and bales it as solid recovered fuel (SRF). Infectious waste is sent for incineration and used as energy from waste (EfW). All residual ash and lime produced by this process is also recycled and used within 3rd party industries.
66.2 tonnes of clinical waste have been processed this year, of which:

38% used as EfW

Adaptation, green spaces and climate change risks
62% solid fuel recovered
We have Business Continuity Plans in place for extreme weather events and as we take forward our Estates Strategy, we will consider what adaptations to our estate are needed to mitigate the effects of climate change.


We were delighted to receive fruit trees from the NHS Forest this Spring to enable us to plant an orchard within our grounds at Danesbury Neurological Centre and Queen Victoria Memorial Community Hospital to provide benefits to patients, visitors and staff and support nature.
Climate related risks are identified and managed through our Trust-wide risk management processes. Our Board Assurance Framework includes a principal risk covering disruptive events including events arising from environmental hazards, operational risks are captured in the Trust service level risk register with higher-level risks escalated to the High-Level Risk Register. As stated elsewhere in this report the status of all risks is discussed routinely within Executive Committee, Board SubCommittee and Board meetings.
Supply
chain, procurement and social value
We recognise the contribution that commissioning, procurement and commercial services can have in delivering sustainability and social value, and our duty under the
Public Services Value Act. Our Hertfordshire and West Essex Procurement Service, which supports HCT and other providers in the system, has embedded a minimum 10% social value weighting into all tenders in line with requirements across the NHS. In many cases, this social value weighting includes sustainability benefit.
The Procurement Service also continues to implement the NHS’ net zero roadmap for procurement, including embedding of practice around Procurement Policy Notices to drive reduction of carbon in our supply chain.
Travel and transport
HCT has a cycle-to-work scheme and a compliant lease car scheme in place to support reduction in emissions associated with staff travel. Coming out of the COVID pandemic, we implemented a hybrid home/office-based working model for our non-clinical staff and our clinical staff continue to use a mix of video conferencing, telephone and in-person contacts for patient consultations and staff meetings to ensure that patient and staff needs are met whilst reducing travel where possible.
During 2024/25, we repeated our Staff Travel Survey which gives us a strong understanding of staff travel patterns, behaviours and plans to inform our work to support greener travel. The data shows us that many staff are adopting hybrid working, where this is compatible with their work duties, but tells us that most staff are highly dependent on cars for travel. This emphasizes the importance of the Trust supporting a switch from petrol/diesel cars to greener electric or hybrid vehicles.
Sustainable models of care
All the areas of focus described above will support us to deliver more sustainable services in the future. As a community provider, HCT is at the forefront of sustainable care delivery within the local healthcare system, with care delivered in patients’ homes, at educational settings or as close to patients’ home as possible thereby avoiding/reducing patient or service user travel.
This year HCT has further expanded its Hospital at Home service to more than 200 patients at any time, and this is making a valuable contribution to more sustainable care delivery, with acute-level care provided for patients in their own homes, avoiding the need for hospital admission and supporting earlier discharge.
The Trust also provides primary and secondary prevention through its services, promoting health and preventing exacerbations. Examples include:
• The National Child Measurement Programme and advice provided via Public Health Nursing e.g. to encourage breast feeding and prevent obesity by encouraging healthy eating, healthy weight and physical exercise
• Vaccination programmes delivered by our Community and School Aged Immunisation Service
• Many of our services have a focus on preventing deterioration and exacerbations and supporting rehabilitation; to take just a few examples our frailty, diabetes, dental and children’s asthma and wheeze services
Task force on climate related disclosures
The NHS Group Accounting Manual sets out recommendations for climate-related disclosures for inclusion in the annual report. The Trust has summarised in the table below how it meets each of these recommendations.
Pillars
Governance
Recommendations Comply or Explain
Describe the Board’s Oversight of Climate Related Issues
Governance
Describe Management's role in assessing and managing climate-related issues
See section 2.4.7 on Workforce and Leadership. Further information around Governance can be found in Section 6
‘Governance, Reporting & Monitoring’ of the HCT Green Plan 2022-25 which is available on the HCT website Green plan | Hertfordshire Community NHS Trust. NB. The Strategy Planning and Engagement Committee referenced in this has been renamed Strategy Involvement and Planning Committee (SIPC).
See section 2.4.7 on Workforce and Leadership. Further information around how HCT’s green plan was developed can be found in Section 6
‘Governance, Reporting & Monitoring’ of the HCT Green Plan 2022-25 which is available on the HCT website Green plan | Hertfordshire Community NHS Trust. The Green Plan describes the Trust’s assessment of climate-related issues for HCT.
Risk
Risk
Risk
Metrics and Target
Describe the organisation's processes for identifying and assessing climate-related risks
Describe the organisation's processes for managing climate-related risks
Describe how processes for identifying, assessing and managing climate-related risks are integrated into the organisation's overall risk management approach
Disclose the metrics used by the organisation to assess climate-related risks and opportunities in line with its strategy and risk management process
See section 2.4.7 on adaptation, green spaces and climate change risks.
See section 2.4.7 on adaptation, green spaces and climate change risks.
See section 2.4.7 on adaptation, green spaces and climate change risks.
Sustainability performance is tracked against the HCT Green Plan 2022-25. Utility invoices are used to track consumption and compared with benchmarking data provided nationally. Energy consumption and emissions are benchmarked against all community trusts nationally. Data is also collected on clinical and non-clinical waste and recycling. We also assess staff travel patterns via our annual Staff Travel Survey and monitoring of staff travel
Metrics and Target
Describe the targets used by the organisation to manage climate-related risks and opportunities and performance against targets
expenses claims. Data is included in section 2.4.7.
See section on HCT Green Plan on page 52-53, which sets out the carbon footprint reduction targets the Trust has set itself in line with the wider NHS’ targets The Trust also compares itself to national benchmarking data with the aim of improving the Trust’s position relative to other community trusts.
2.4.8 Equity, diversity and human rights

The Trust is committed to delivering services that are responsive to and fully meet the diverse needs of our communities, patients and service users in order to improve health outcomes.
In line with our ‘great place to work’ strategic objective, we aspire to be a Trust that celebrates difference and to create a culture of inclusion, valuing the unique contribution from all our staff and the work that continues in this area This year, in our staff survey, when compared with 16 other community trusts nationally, we scored higher than average for ‘being compassionate and inclusive’, and ‘everyone having a voice that counts’.
Our achievements in 2024/25
Our Equity, Diversity and Inclusion Strategy
We continue to implement the work programme set out in our Equity, Diversity and Inclusion Strategy (ED&I), which was ratified by the Trust Board in December 2022. Our strategy builds on our Clinical and People strategies, setting out our 5 ED&I strategic priorities, which are:
To strengthen our channels for listening to the diverse voices of our staff
To continually develop our understanding of our local communities
To improve identification of, access, experience and outcomes for under-served groups
To have a workforce that is representative at all levels
To be recognised externally as a Trust committed to promoting diversity.
A review of our strategy in January 2024 showed that progress has been made under all of these priority areas.
Evaluating and Reporting on our Equality Performance
Workforce Race Equality Standard (WRES)
The national NHS Workforce Race Equality Standard (WRES) is designed to improve the representation and experience of Black and Minority Ethnic staff at all levels of the organisation. There are nine indicators that make up the WRES, split across workforce data and national NHS Staff Survey results.
Although there is still much work to do to bring the experience of our Black and minority ethnic staff fully in line with our White staff, in the last report the Trust ranked in the top 20% nationally in four out of the nine indicators. Our workforce overall has broadly the same proportion of staff from non-white ethnicities as the overall non-white working age Hertfordshire population but lower than the overall non-white population. More work is required to ensure equal representation at higher levels of the organisation, particularly within the senior leadership team.
Workforce Disability Equality Standard (WDES)
The Workforce Disability Equality Standard (WDES) report is a set of ten metrics that enable NHS organisations to compare the experiences of disabled and non-disabled staff. 5.4% of our workforce is recorded as living with a disability or long-term condition, with these being well spread across levels in the organisation. There was one disabled member of staff involved in a formal capability case in the year out of a total of three, and we were pleased to have scored significantly better than the national average in five out of the ten indicators linked to the 2023 Annual Staff Survey results and have been working with our Together We Can (Disability and Long Term Conditions) Network on the areas requiring more work, including on the area of making reasonable adjustments which though improved requires continued focus.
Gender Pay Gap Report
As an employer with more than 250 staff we are required by law to carry out Gender Pay reporting under the Equality Act 2010 (Gender Pay Gap Information) Regulations 2017.
In our most recent report, our Trust mean gender pay gap (the difference between men’s and women’s average hourly pay) was 6.9%, an improvement compared to the previous year (10.1%), and substantially better than the national ONS average of 13.8%. Our median gender pay gap was 2.1% (the previous year was 4% in favour of women). Our Trust is around 93% female.
Equality Delivery System 3
The Equality Delivery System (EDS), which was relaunched in 2022, is an improvement tool for patients, staff and leaders, and is a requirement for both NHS commissioners and NHS providers. The EDS provides an opportunity to review and develop our approach in addressing health inequalities through three domains: Commissioned or Provided Services (selecting 3 different services annually), Workforce Health and Wellbeing and Inclusive Leadership. It is driven by data, evidence, engagement and insight.
Having gathered evidence, the EDS framework has entailed us working with stakeholders to assess ourselves against the three domains. The scoring criteria is prescriptive, with the Trust scoring ‘achieving’ across all three domains.
Rainbow Badges/LGBTQI+
In conjunction with the Proud to Be Network (LGBTQI+ Staff Network), we developed our Rainbow Ally badge training which was launched during LGBT+ History Month. This learning opportunity, which offers space for reflection launched in spring 2024 and so far, 260 people have accessed it. Team members are empowered to deliver the training to colleagues without the need of a formal ‘trainer.’
Meeting the Needs of our Patients and Service Users
Clinical and Quality Strategy
Our Clinical and Quality Strategy highlights ‘an absolute need to reduce the inequalities of access and outcomes within the populations we serve’ and sets out four strategic priorities and accompanying plans specifically relating to this, which are:
• To develop a better understanding of the inequalities experienced by different populations we serve, including identification of people at risk of experiencing health inequalities
• To improve access to care
• To improve equality and experience of care
• To put specific initiatives in place to reduce the inequality in outcomes between populations experiencing inequalities and the wider population
The detailed implementation of our work on health inequalities is set out in our Health Inequalities Plan which is monitored through the Trust Health Inequalities Steering Group.
Patient Engagement and Experience Strategy 2021-2024
Our Patient Engagement and Experience Strategy supports delivery of our commitment to working in partnership with patients, the public and local communities to help improve and develop our services. The strategy sets out the Trust’s plans on how we will use feedback from people who use our services. It also outlines how we intend to work with different equality groups to enable discussion about our patients’ diverse needs. Furthermore, it will demonstrate the improvements we have made as a result of patient feedback.
Care Plans
Our Care Plans recognise the diverse needs of patients/carers and include all aspects of an individual’s life where support might be required, for example, psychological, physical and spiritual or religious. Multidisciplinary team meetings are used to discuss a patient’s preferences and ensure that everyone likely to care for that person has knowledge of the spiritual and/or religious issues important to them.
Interpreting
support for patients
The Trust is committed to providing effective communication with non-English speakers, people for whom English is a second language and patients with a sensory impairment who require communication support. The Trust commissions a confidential translation and interpreting service to ensure that patients, their families and carers are provided with appropriate communication support when accessing our services. We aim to ensure that all patient information leaflets, booklets and posters state that patient information can be
made available in braille, large print or audio versions In 2024, a project was initiated to explore digital solutions for translating Trust communications.
Improving care of people with learning disabilities and autism
HCT continues to support people with a learning disability, autism or both Working under the guidance of the steering group they have been working on:
1. Creation of a Learning disability and autism webpage - a patient-friendly webpage with information and links to support people with learning disabilities, autism or both.
2. Using Ask Listen Do resources - Creation of a steering group to promote use and understanding of Ask Listen do resources which empower patients with learning disability and autism to give feedback and raise complaints. The Complaint policy has been adapted to include Ask Listen Do Radar as also been adapted to include prompting on ask listen do.
3. Engagement with Purple All Stars learning disability group - to create videos to support social stories within the dental team The photo below shows the group in the dental service’s sensory room at Cheshunt Community hospital.
Meeting the Needs of our Staff
Shadow Board

Our Trust Board’s commitment to inclusion is demonstrated by our highly innovative Shadow Board (SB), launched in October 2022 and chaired by the Trust Chair SB considers Trust strategies, policies, and planned activities with an EDI lens. In its first years, SB has amplified the voices of staff representing colleagues and patients who might otherwise be less heard Board reflect, that the insights and perspectives of SB, have supported personal and collective growth and enabled Board to take a more inclusive approach to Trust operation and governance.
Staff networks
We have a strong and effective Celebrating Racial Equity & Diversity (CRE&D) Network, with its own Chair, Deputy Chair and executive committee. In addition to supporting us to improve our WRES measures, the network has led on a wide range of developments over the last year as described in some of the sections below. In addition, supported by the Board, the network organised the Trusts’ first Community Engagement Event on the eve of Black History Month. The family friendly event in Watford showcased services provided by the Trust and partner statutory and VCFSE organisations to connect with potentially underserved communities and attracted social media and local radio coverage.
Our Together We Can (Disability and Long-Term Conditions - DLTC) staff network continues to grow in maturity; led by three co-chairs, this network helps drive our work on our WDES measures and the disability agenda more widely. Quarterly Neurodiversity “Listen & Learn” sessions are provided, the network continues to support the embedding
and widespread use of the Workplace Adjustment Passports and work adjustments relating to neurodiversity. The network also supports delivery of Trust events like the Annual Leaders conference.
Our Proud to Be (LGBT+) staff network is also maturing under the chairmanship of two co-chairs; and continues to be a reference group for the Trust. Proud To Be also supports Trust events like the Annual Leaders Conference.
The demographic makeup of the Trust in terms of ages and sex means the Menopause Network provides a valued resource for staff approaching and experiencing menopause It provides a forum for sharing support and ideas on how to cope with symptoms. It also provides opportunities to raise practical ideas about how the Trust can build on being a Menopause friendly employer.
We are proud to be an Armed Forces friendly organisation and recognise the value armed forces members bring to the Trust. The role of our Armed Forces Champion Network is to ensure that the armed forces community is supported, raising awareness of both the moral and contractual obligations under the Armed Forces Covenant, the NHS Constitution, the Health and Social Care Act and other Acts.
Launched during summer 2024, the Young Persons Network is the newest staff network. The Trust is committed to recruiting and retaining young people, supporting their personal and professional development. The network provides a setting where the opportunities and challenges experienced by people starting their NHS careers can be discussed and the Trust can explore how best to meet their needs and expectations.
Anti-racism
Working with our CRE&D Network, we are committed to taking an anti-racist stance and have signed up to the East of England Anti-Racism Strategy and achieved the RACE Equity Code kite mark.
Our ED&I Strategy sets out our Trust anti-racism statement, which is as follows:
We recognise that racism and racial inequality still exists in our everyday lives. It runs through our structures and systems, in our society, the health service and areas of our Trust, and we understand that we all have a role to play in this.
By embracing an anti-racism approach we commit to consciously looking at ways to change our activities and actions to break down the barriers to race equality. This requires solidarity, bravery and honesty in recognising that there remains much to do and we will work together to listen to experiences and take action to address inequity. We believe that by getting this right on racial equity, one of the most challenging areas, we can pave the way to improve all areas of equality.
Led by the Chief Executive, the Trust delivered a strong response to the social unrest of Summer 2024 Concurrent with the events, the CEO wrote a response outlining his condemnation of the violence and intimidation, staff were supported travelling to, from and during work, an all-team conversation was held, and CRE&D Network hosted dropins were provided.
The Head of EDI conducted research and developed recommendations for the Trust to further embed anti-racist practice. An action plan to deliver the recommendations, which include revising the learning and development offer, an anti-racist and antidiscriminatory review of HR policies and processes and the development of an EDI data dashboard has been agreed.
Talent management programmes
In 2021, we introduced our ‘Developing Our People’ programmes (formerly named Talent/Personal Effectiveness programmes) at all levels; under-represented groups are directly invited to apply to these programmes and are prioritised for places. In total over 400 staff have now been through the programmes. The programmes focus on personal and career development and seek to give staff the confidence to pursue their career aspirations. In 2024 we launched the Thrive programme. Thrive is the umbrella term for the career development offers to support colleagues from Black and Minority Ethnic backgrounds Thrive includes facilitated sessions on ‘Succeeding at application and interview,’ ‘Career confidence’ and ‘Taking the next steps in your career.’ The Inclusive Mentoring Plus programme is also open for applications.
Leadership development
In common with previous years, inclusion was a main theme of our leadership development this year, with inclusion and compassionate leadership continuing to be key themes at our leadership conferences and forums At our 2024 Leaders’ Conference, we continued the theme of kindness from last year with a topic on “EDI In Action: What you can do to help bring change” and keynote addresses on “Culture, Collaboration and Compassion” and “Being at your best.. More often” exploring “how the SUMO principles can help you feel inspired, equipped and empowered to deal with challenges and opportunities both in and outside of work ”.
Accreditation
The Trust has been re-assessed and maintained our Level 2 Disability Confident Employer status under the Disability Confident scheme. Under this scheme, applicants with a disability are guaranteed an interview subject to meeting the essential criteria for the job. We undertake to support our staff with a disability, including making reasonable adjustments for them in their jobs.
Our Carer’s Network continues to develop and grow We are delighted to have been awarded Level 1 under the Carer Confident Employer scheme in 2024.
In addition, we hold Silver accreditation as an employer who supports veterans, reservists and their families and in 2024 were awarded Veterans Aware accreditation.
Policy developments
We have a suite of policies to support the wellbeing of our staff, including a wellestablished Equality, Diversity and Inclusion Policy and policies relating to the Management of Sickness Absence, Stress Management, Flexible Working, Freedom to Speak Up, Alcohol and Substance Misuse, Mental Health Wellbeing, Transgender, Menopause, and Domestic Abuse.
As part of our commitment to ensure we have ‘just and restorative culture,’ in April 2024 we agreed a new 'Just Culture' pre-investigation checklist and published as part of our Disciplinary Policy. The aim of this checklist is to ensure that appropriate reflection takes
place prior to commencing an investigation, in terms of treating staff equitably, avoiding unconscious bias and identifying learning.
Our reports and plans to further promote diversity and inclusion can be found on our website at: Equality, diversity and inclusion | Hertfordshire Community NHS Trust
Performance report signed by the Chief Executive
Signed Elliot Howard-Jones Chief Executive
16 June 2025
3 Accountability Report
3.1 Corporate Governance Report
This section of the Annual Report explains the composition and organisation of the Trust’s governance structures and how they support the achievement of the Trust’s objectives.
3.1.1 Directors’ Report
The Board of Directors 2024/25
The Trust Board of Directors of 31 March 2025 consisted of the Chair (appointed in June 2024), four Non-Executive Directors (appointed through NHSE) and four voting Executive Directors including the Chief Executive. The Board of Directors is supported by a non-voting Non-Executive Director (associate) and two non-voting Executive Directors.
The Board of Directors is responsible for setting and developing the strategic direction of the Trust, sustaining business viability, and holding the Executive Directors to account for all aspects of the Trust's activities, including quality and safety of patient services, financial management and legal compliance. The role also includes seeking assurances from the Executive Directors that the risks to the Trust are being appropriately assessed and managed.
In 2024/25, the Trust Board of Directors met formally on six occasions between June 2024 and March 2025. The Board members meet face-to-face and virtually and the public are also invited to attend virtually. The Annual General Meeting to present the 2023/24 Annual Report and Accounts was held virtually on 25 July 2024 and was well attended.
The Board of Directors has a duty to operate in a way that is transparent and to comply with best practice in probity. To this end, the Board of Directors signs up annually to following the Nolan principles of good governance and the principles and values set out in the NHS Constitution. The Board also conducts an annual self-assessment to ensure compliance with the NHS Code of Governance for NHS Provider Trusts. The Board of Directors knows of no information which would be relevant to the auditors of which the auditors are not aware.
Throughout 2024/25, the Board of Directors has continued to undertake a programme of collective and individual development. The Board of Directors regularly hears specific stories from, or about, individual patients or services at the start of its meetings in public. There have been six Board development sessions between April 2024 and March 2025, this allowed dedicated time to increase strategic understanding, develop specific areas of knowledge related to the Trust’s services and the environment in which it operates, and facilitate strategic planning.
The voting members of the Board of Directors also act as the corporate trustees for HCT’s charitable funds, for which a separate report and accounts are published.
Changes to the Board of Directors in 2024/25
The following changes were made to the Board of Directors in 2024/25:
Dr Linda Sheridan, Chair, retired in April 2024 and was replaced in June 2024 by Dr
Nicolas Small.
Alison Ryder, Director of People, retired at the end of May 2024 and was replaced by Marcus Riddell, Chief People Officer, in July 2024
David Bacon, Director of Finance, Systems and Estates, retired in July 2024 and was replaced by Frances Khatcherian in October 2024. Simon Rudkins acted as Interim Director of Finance, system and Estates between July and October 2024.
Board of Directors and committee meeting attendance 2024/25
In 2024/25, the Trust Board of Directors was supported by the following committees, with membership and attendance records for meetings in 2024/25 as indicated (number attended/total meetings held in year eligible to attend as a committee member).
The majority of the committees and supporting meetings, with the exception of the Board meeting in public, were held virtually using video conferencing.
The Trust Board of Directors as of 31 March 2025

Committee Membership
• Chair – Trust Board
• Chair – Charitable Funds Trustees
• Member – Charitable Funds Committee
• Member – Strategy, Involvement and Planning Committee
• Member – People, Performance and Finance Committee
• Member – Remuneration Committee
Appointment history
• Appointed 3 June 2024 to 2 June 2027

Committee membership
• Chair - People Performance and Finance Committee
• Member - Audit Committee
• Chair - Remuneration Committee
Appointment History
• Appointed from 4 April 2022 to 3 April 2025
• Appointed from 4 April 2025 to 3 April 2028
Dr Nicolas Small, (Voting Member, Independent NonExecutive Director) Trust Chair
Nicolas was appointed as Trust Chair on 3 June 2024, joining the Trust from his role as a partner member (Primary Medical Services) of the Hertfordshire and West Essex Integrated Care Board (ICB).
Nicolas studied Medicine at St Mary’s Hospital London and was a GP in Hertsmere for 28 years. He became very involved in commissioning and championed patient involvement, working closely with the voluntary sector. As well as his clinical leadership he was training and education lead for Primary Care Education for HWE ICB. He is also the former chair of Herts Valleys Clinical Commissioning Group (CCG).
Nicolas brings a wealth of experience and skills to the role. His passion for community services and partnership working is helping us to continue delivering the best quality care for our patients and leading innovative service changes to help us meet the needs of our local communities.
Chris Ford (Voting Member) Independent Non-Executive Director
Chris was appointed to the Board in April 2022. He is a qualified accountant with a background in the NHS; he has worked for the NHS for 36 years in various financerelated roles.
Chris held the position of Director of Finance in a number of organisations and has experience of working within the NHS commissioning and regulatory sector, as well as most forms of NHS provider.
He has extensive experience in financial management and recovery, and has been involved in developing local, regional and national level transformation initiatives.

Committee membership
• Chair - Audit Committee
• Chair - Remuneration Committee
• Member - Quality Committee, NonExecutive Director for Freedom to Speak Up
• Member - People, Performance and Finance Committee
Appointment history
• Appointed from 1 April 2020 to 31 March 2023
• Appointed from 1 April 2023 to 31 March 2026

Committee membership
• Chair – Strategy, Involvement and Planning Committee
• Member – Quality Committee
• Chair – Charitable Funds Committee
Appointment history
• Appointed from 1 July 2021 to 30 June 2024
• Appointed from 1 July 2024 to 31 December 2024
• Appointed from 1 January 2025 to 30 June 2027
Richard Rolt (Voting Member)
Independent Non-Executive Director
Richard was appointed as a Non-Executive Director on 1 April 2020 and chairs the Audit Committee. He has a background in IT and commercial business management and worked previously for the NHS as ICT Services Director, supporting the Hertfordshire health system.
During recent years Richard held the positions of Chief Operating Officer and Chief information Officer at Viapath, a large pathology provider set up as a joint venture between Guy’s and St Thomas’ NHS Foundation Trust, King’s College Hospital NHS Foundation Trust and the private sector.
Richard joined the pioneering biotech start-up, Genomics Ltd as Vice President, Operations in 2021 and currently holds the post of Vice President, Technology.
Rukshana Kapasi (Voting Member)
Independent Non-Executive Director
Rukshana has been working in the NHS and charitable sector for the last thirty years as a commissioner, clinician, senior leader and Board member. She has stimulated some key directional changes in the public sector such as undertaking research and pilots which led to the introduction of Patient Advisory Liaison services into hospitals in England, Patient Choice in primary care and ethnicity monitoring to improve health inequalities.
Rukshana introduced the first digital Inflammatory Bowel Disease (IBD) standards to IBD centres across the UK in 2019 as Chair of IBDUK, a partnership of 17 Royal Colleges and patient organisations.
She is Barnardo’s first Director of Health, leading the transformation of the largest children’s charity in the UK to a health and social care provider.
As well as developing its health growth strategy, and value proposition, she is shaping wider system change for child health equity through a number of strategic partnerships including a partnership with Sir Michael Marmot’s Institute of Health Equity and 3 ICSs. Rukshana is an Advisory Commissioner for the Health Devolution Commission.

Committee membership
• Chair - Quality Committee
• Member - Audit Committee
• Member - Strategy, Involvement and Planning Committee
• Member - Charitable Funds Committee
Appointment history
• Appointed from 1 April 2020 to 31 March 2023
• Appointed from 1 April 2023 to 31 March 2026

Committee membership
• Member – Strategy, Involvement and Planning Committee
Appointment history
• Appointed 25 June 2019 (unremunerated)
• Extended in 2020 until 30 June 2021 (unremunerated)
• Extended in 2021 until 30 June 2022 (unremunerated)
• Extended in 2022 until 31 March 2023 (unremunerated)
• Extended in 2023 until 31 March 2024 (unremunerated)
• Extended in 2024 until 31 March 2025 (unremunerated)
Sarah Wren (Voting Member)
Independent Non-Executive Director
Sarah was appointed as a Non-Executive Director in April 2020. She is the Chief Executive of Health & Independent Living Support (HILS). HILS is one of HCT’s key partners and delivers services across the county to support many frail older people who also receive services from the Trust’s teams. Sarah has led HILS to become the largest social enterprise provider of meals and independent living support in the UK.
She is an associate member of the National Malnutrition Task Force which leads several initiatives to tackle malnutrition and dehydration. She was also the Chair of Healthwatch Hertfordshire from 2012 to 2014 and sits on several working groups and Integrated Care Board (ICB) Boards and Committees in relation to nutrition, frailty and prevention.
She was awarded an MBE in 2012 for services to the community sector and an OBE in 2022 in recognition of services to older and disabled people in Hertfordshire.
Luke Edwards (Non-Voting Member)
Associate Non-Executive Director (Independent)
Luke was appointed as an Associate Non-Executive Director in June 2019. He is currently on secondment to the College of Policing having undertaken a number of Director roles in the Home Office since 2019.
Immediately prior to that he worked for Lord Caster of Coles at NHS Improvement, delivering a series of reviews to improve the efficiency and effectiveness of health services.
He has more than 20 years’ experience in a range of public services, including in the Home Office, Ministry of Justice, Revenue and Customs and the NHS.
His previous roles include being Director of Fire Policy, leading on Covid enforcement policy for HMG, developing the payment by re-offending outcomes programme at the Ministry of Justice and managing the collection of student loans.


Elizabeth’s portfolio:
• Executive lead and advisor for psychologists, medical, dental and pharmacy professionals on the Trust Board
• Clinical leadership
• Caldicott guardian
• Responsible Officer for medical revalidation
• Guardian for safe working hours
• Executive lead for learning from deaths
• Executive lead for medicines management
• Executive lead for health inequalities
• Executive lead for mental health and learning disability (jointly with Director of Nursing and Quality)
• Executive lead for Research
Elliot Howard- Jones (Voting Member)
Chief Executive Officer
Elliot joined HCT in November 2020. He was previously Director of Performance and Improvement in the NHS England East of England regional team. As part of this, he was Strategic Incident Director for COVID-19 for the East of England and led the operational response and strategic planning for the COVID-19 pandemic across the region.
He has also held Director positions in acute and mental health trusts, in commissioning and at the Department of Health and Social Care.
Dr Elizabeth Kendrick (Voting Member)
Chief Medical Officer
Dr Elizabeth Kendrick was appointed as Medical Director in October 2019, having previously been Acting Medical Director and Deputy Medical Director.
Dr Kendrick has been a GP for 21 years, winning the Fraser Rose medal for highest mark in the MRCGP in 2003. She also works as a GP with Special Interest (GPwSI) for older people providing clinical input to our inpatient unit at Herts and Essex hospital. She has an MSc in leading service improvement.
She was previously National Professional Advisor for older people to the Care Quality Commission. Prior to this, she was End of Life Lead for the North-East and Commissioning Lead for the frail elderly for North Durham Clinical Commissioning Group.

Frances' portfolio:
• Financial management
• Performance management
• Contract management
• Business planning
• Digital and innovation
• Senior Information Risk Owner (SIRO)
• Estates
• Financial and corporate governance
• Internal and external audit
• Charitable Funds
• Business and commercial development

Sarah’s portfolio:
• Executive Lead and advisor for nurses and allied health professionals on the Trust Board
• Board Lead for safeguarding
• Director of Infection Prevention and Control
• Quality and governance
• Clinical leadership
• Patient safety
• Patient experience
• Medical Devices
• Executive Director for Freedom to Speak Up
• Executive Lead for mental health and learning disability (joint with Medical Director)
• Executive Lead for Vaccination Programme
Frances Khatcherian (Voting Member) Chief Finance Officer
Frances was appointed as Director of Finance, Systems and Estates on 7th October 2024. Prior to this she was Interim Director of Finance and Director of Financial Recovery, at The Queen Elizabeth Hospital King's Lynn NHS Foundation Trust.
Before joining The Queen Elizabeth Hospital, Frances was Director of Operational Finance – Intervention in the Midlands region, which followed a role at NHS England and NHS Improvement. Frances took the role into NHSE during the pandemic and supported the changes in framework and funding to support the reaction to COVID. The role evolved into looking at the financial sustainability of systems and providers post-pandemic, focusing on productivity and financial control and governance.
Prior to this, Frances worked in an acute provider for several years after joining the NHS in 2013 with a mental health provider.
Frances’ finance career began in 2003 at a manufacturing company before eventually moving into corporate banking financial institutions during the financial crisis and supporting on the HBOS integration in Lloyds banking group.
Sarah Browne (Voting Member)
Chief Nursing Officer
Sarah was appointed as Director of Nursing and Quality in February 2019 from Essex Partnership NHS Foundation Trust (EPUT), a combined mental health and community trust with services in Essex and Bedfordshire where she was Deputy Director of Nursing and Director of Infection Prevention and Control.
Sarah was previously Acting Executive Nurse at South Essex Partnership University NHS Foundation Trust, and she has worked at a senior level in the former Bedfordshire Community Health Services Trust. Sarah brings a breadth and depth of experience to the Trust role. She has extensive experience of integrated community and mental health services, nursing and clinical leadership and workforce transformation across complex systems. She has worked at local, regional and national levels and led the COVID vaccination programme across two systems, setting up mass vaccination sites.
In 2021, she was awarded the title of Queen’s Nurse by The Queen’s Nursing Institute.

Antonia’s portfolio:
• Executive lead for net zero
• Contracting
• Analysis and reporting
• Clinical systems
• Corporate governance
• Business support

Marcus’s portfolio:
• Operational Human Resources
• Workforce Planning and Information
• Learning and Development
• Organisational Development
• Staff wellbeing, reward and recognition
• Equity, Diversity and Inclusion
• Payroll and Occupational Health (outsourced contracts)
Antonia Robson
Director of Integrated Business Services (Non-voting member)
Antonia has worked as Associate Director, and latterly Director, of Integrated Business Services at HCT since December 2017, having previously been Assistant Director of Planning and Contracting for the Trust.
Antonia joined NHS in 2009, initially as Associate Director of Corporate Services at Luton Primary Care Trust (PCT) and then as Director of Business Services for both Luton and Bedfordshire Primary Care Trusts in 2011. She has also worked for NHS Central Eastern Commissioning Support Unit, supporting commissioners across Hertfordshire, Bedfordshire and Essex and leading on strategic development.
Prior to joining the NHS, Antonia worked for Barclays Corporate Banking for 12 years, predominantly in strategic marketing, planning and sales management, bringing commercial experience to the Trust from these roles. She has a post-graduate diploma in marketing as well as an MBA.
Marcus Riddell
Chief People Officer (Non-Voting Member)
Marcus was appointed as Chief People Officer on 1 July 2024. Prior to this he was Interim Chief People Officer, and Deputy Chief People Officer, at Essex Partnership University NHS Foundation Trust.
Before joining Essex Partnership, he was Director for Strategic Partnerships at NHS Professionals, a role that followed a series of roles at NHS England and NHS Improvement. In addition to being Head of Equality and Inclusion – Evidence and Policy, during the pandemic, Marcus led the Covid-19 Risk Assessment Delivery Unit and efforts to increase staff Covid-19 vaccination uptake. Marcus’s earlier work in healthcare focused on temporary staffing and supply at the Department of Health and Social Care, and subsequently NHS Improvement from 2017-2020.
Marcus’s career began in 2006 at the Department of Communities and Local Government as an administrative assistant, before eventually filling Private Office roles for both Labour and Conservative Ministers. Marcus later moved to the Ministry of Defence as the Policy Officer for the Pakistan Desk. He subsequently moved to the Home Office to focus on domestic counter terrorism.

Marion’s portfolio
• Operational management
• Emergency planning and resilience
• Communications with general practices and primary care networks
• Integrated care

Sarah’s portfolio
• Strategy development
• Communications and engagement
• Partnership and business development
Marion Dunstone (Non-voting member)
Chief Operating Officer
Marion was appointed as Director of Operations in January 2016, having acted into the role for the previous six months, and became Chief Operating Officer in October 2019. Prior to this, Marion was General Manager for Children’s and Young People’s Services. Marion has many years of experience in the NHS. She initially qualified and worked as a dietitian and has managed adult and children’s services in hospitals and within the community.
Marion leads the operational delivery of adult and children’s services across HCT and is the emergency planning lead for the organisation.
Sarah Brierley (Non-voting member)
Chief Strategy & Partnerships Officer
Before joining HCT Sarah worked in a range of corporate and operational roles across a range of NHS trusts including the Royal Free London NHS Foundation Trust, Barts and the London NHS Trust (St Bartholomew’s Hospital), North Middlesex University Hospital NHS Trust and East and North Hertfordshire NHS Trust where she held successive roles including Divisional Director, Director of Business Development and Partnerships and Executive Director of Strategy.
In October 2020, Sarah took on the role of Joint Director of Strategy for both East and North Hertfordshire NHS Trust and Hertfordshire Community NHS Trust before joining HCT full time in August 2021. Sarah’s portfolio spans strategy development, transformation, strategic partnerships, business development, communications and engagement.
The Board of Directors Register of Interests
The table shows the Board Members and their interests declared as of 31 March 2025 and interests declared by Board Members who were in post during 2024/25. The Trust has published on its website an up-to-date register of interests, including gifts and hospitality, for decision-making staff (as defined by the Trust with reference to the guidance) within the past twelve months, as required by the ‘Managing Conflicts of Interest in the NHS’ guidance
Name Position Interests Declared
Dr Nicolas Small (Voting Member)
Trust Chair
Sarah Brierley (Non-Voting Member)
Sarah Browne (Voting Member)
Marion Dunstone (Non-Voting Member)
Luke Edwards (Independent)
Chris Ford (Voting Member)
Chief Strategy & Partnerships Officer
Chief Nursing Officer
• From March 2024: Independent Member, Thames Regional Flood & Coastal Committee – Environment Agency
• From February 1992: brother and sister are dental surgeons working in NHS/private practice in North Central London
• From July 2022: sister is a GP and Primary Care Services Partner Member, NHS NW London ICB and Medical Director for Primary Care, North West London
• None
Elliot Howard-Jones (Voting Member)
Rukshana Kapasi (Voting Member)
Chief Operating Officer
Non-Executive Director (Associate)
Independent Non-Executive Director
Chief Executive
Independent Non-Executive Director
Dr Elizabeth Kendrick (Voting Member)
Chief Medical Officer
• From January 2021: daughter worked for HCT on the Reservist Bank within the People Team and during COVID vaccination programme
• None
• Director, Public Safety Group, Home Office. From January 2025 seconded to College of Policing (primary employment)
• From September 2024 Non-Executive Director role at Oaklands College, St Albans. Both Oakland College and HCT have RSM as their internal auditor
• None
• Director of Health, Barnardo’s
• Advisory Commissioner for the Health Devolution Commission
• Director of Antiba Ltd
• Husband works as a drug developer for GSK
• One off payment of £200 for work done for Alpha Sights in January 2024
Name Position
Frances Khatcherian (Voting Member)
Marcus Riddell (Non-Voting Member)
Antonia Robson (Non-Voting Member)
Richard Rolt (Voting Member)
Sarah Wren (Voting Member)
Audit
Chief Finance Officer • None
Chief People Officer • None
Director of Integrated Business Services
Independent Non-Executive Director
Independent Non-Executive Director
• None
• Vice President, Technology at Genomics Ltd
• Chief Executive of Health & Independent Living Support (HILS)
The Trust has an Audit Committee which is chaired by a Non-Executive Director and has two other Non-Executive Directors as members, one of whom is financially qualified. At 31 March 2025, membership was:
Chair: Richard Rolt (Non-Executive Director)
Members: Chris Ford (Non-Executive Director)
Sarah Wren (Non-Executive Director) (*)
(*) Also Chairs the Quality Committee The Chair of the Audit Committee also sits on the Trust’s Quality Committee.
The Audit Committee met five times in 2024/25 with four standing meetings and an extraordinary meeting to review the Trust’s Annual Accounts, Annual Report, Quality Account and other mandatory submissions.
In 2024/25, internal audit services were provided by RSM and the external auditors were Azets.
External Auditors were appointed on a two-year contract covering 2023/24 and 2024/25. External auditor independence and effectiveness was assessed by the Audit Committee against the specification as part of the procurement process The external audit plan for the year was presented to the Audit Committee for consideration with an interim report showing progress against plan. The cost of external audit, for work undertaken in 2024/25 was £116,841 plus VAT (£113,000 plus VAT in 2023/24).
The external auditors have not undertaken any non-audit work which may have given rise to a conflict of interest or compromised the audit function. As far as the Directors are aware, there is no relevant audit information of which the Trust’s auditors are unaware. The Directors have taken all the steps that they ought to have taken as directors to make themselves aware of any relevant audit information and to establish that the auditors are aware of that information.
Disclosure of corporate governance arrangements
The NHS Code of Governance sets out a common overarching framework for the corporate governance of NHS trusts, reflecting developments in UK governance requirements and the development of integrated care systems. Trusts must comply with each of the provisions within the code or be able to explain in each case why they have departed from the code. The Trust has completed a review of compliance for each of the provisions within the code and the Board has confirmed compliance with 102 of the relevant provisions within the code There are three provisions where the trust has departed from the code. For the provisions which require an explanation in the Annual Report a supporting explanation is provided in the table below:
Provisions which require a supporting explanation
A.2.1 The board of directors should assess the basis on which the trust ensures its effectiveness, efficiency and economy, as well as the quality of its healthcare delivery over the long term, and contribution to the objectives of the ICP and ICB, and place-based partnerships. The board of directors should ensure the trust actively addresses opportunities to work with other providers to tackle shared challenges through entering into partnership arrangements such as provider collaboratives. The trust should describe in its annual report how opportunities and risks to future sustainability have been considered and addressed, and how its governance is contributing to the delivery of its strategy.
A.2.3 The board of directors should assess and monitor culture. Where it is not satisfied that policy, practices or behaviour throughout the business are aligned with the trust’s vision, values and strategy, it should seek assurance that management has taken corrective action. The annual report should explain the board’s activities and any action taken, and the trust’s approach to investing in, rewarding and promoting the wellbeing of its workforce.
Compliant Annual Self-Assessment Template is completed each year for the Board and each of the Board committees.
Trust is a member of the Community Provider Collaborative with CLCH and EPUT Chairs, CEO and Director of Finance meetings also take place .
See Section 2.4.6 on Sustainability.
A.2.8 The board of directors should describe in the annual report how the interests of stakeholders, including system and place-based partners, have been considered in their discussions and decision-making, and set out the key partnerships for collaboration with
Compliant Culture is assessed and monitored through the People Strategy and the Patient Engagement & Experience Strategy.
We have several networks in place
• Proud to Be which supports our LGBTQI+ colleagues and allies
• Together we Can, which supports our staff with long term conditions and disabilities
• CRE&D which supports our ethnic minority colleagues
• Menopause Network
See Annual Report Section 3.2.2.11
Compliant See Section 2.3.4.1 on Strategic Partnerships. Oversight provided by bi-monthly SIPC meetings.
Provisions which require a supporting explanation
other providers into which the trust has entered. The board of directors should keep engagement mechanisms under review so that they remain effective. The board should set out how the organisation’s governance processes oversee its collaboration with other organisations and any associated risk management arrangements.
B.2.6 The board of directors should identify in the annual report each non-executive director it considers to be independent. Circumstances which are likely to impair, or could appear to impair, a non-executive director’s independence include, but are not limited to, whether a director:
• has been an employee of the trust within the last two years
• has, or has had within the last two years, a material business relationship with the trust either directly or as a partner, shareholder, director or senior employee of a body that has such a relationship with the trust
• has received or receives remuneration from the trust apart from a director’s fee, participates in the trust’s performance-related pay scheme or is a member of the trust’s pension scheme
• has close family ties with any of the trust’s advisers, directors or senior employees
• holds cross-directorships or has significant links with other directors through involvement with other companies or bodies
• has served on the trust board for more than six years from the date of their first appointment
Compliant Independent Non-Executive Directors are identified in Section 3.1.1.4
Provisions which require a supporting explanation
• is an appointed representative of the trust’s university medical or dental school
Where any of these or other relevant circumstances apply, and the board of directors nonetheless considers that the non-executive director is independent, it needs to be clearly explained why.
B.2.13 The annual report should give the number of times the board and its committees met, and individual director attendance.
C.4.2 The board of directors should include in the annual report a description of each director’s skills, expertise and experience.
C.4.7 All trusts are strongly encouraged to carry out externally facilitated developmental reviews of their leadership and governance using the Well-Led framework every three to five years, according to their circumstances. The external reviewer should be identified in the annual report and a statement made about any connection it has with the trust or individual directors.
C.4.13 The annual report should describe the work of the nominations committee(s), including:
• the process used in relation to appointments, its approach to succession planning and how both support the development of a diverse pipeline
• how the board has been evaluated, the nature and extent of an external evaluator’s contact with the board of directors and individual directors, the outcomes and actions taken, and how these have or will influence board composition
• the policy on diversity and inclusion including in relation to disability, its objectives and linkage to
Compliant See Section 3.1.1.3
Compliant See Section 3.1.1.4
Compliant See Section 2.4.3.1. CQC core service and well-led inspection of the Trust was carried out during February/March 2020.
Explain HCT does not have a Nominations Committee The following is in place to offset this:
• In relation to appointments, we have recruitment training for all managers, diversity champions sit on interviews and when staff are in post they have access to talent programmes, career coaching and mentoring.
• The policy on diversity and inclusion as well as the setting up of a Shadow Board shows the progress we are making.
• We upload the WRES and WDES data following approval at Board.
Provisions which require a supporting explanation trust vision, how it has been implemented and progress on achieving the objectives
• the ethnic diversity of the board and senior managers, with reference to indicator nine of the NHS Workforce Race Equality Standard and how far the board reflects the ethnic diversity of the trust’s workforce and communities served
• the gender balance of senior management and their direct reports
D.2.4 The annual report should include:
• the significant issues relating to the financial statements that the audit committee considered, and how these issues were addressed
• an explanation of how the audit committee (and/or auditor panel for an NHS trust) has assessed the independence and effectiveness of the external audit process and its approach to the appointment or reappointment of the external auditor; length of tenure of the current audit firm, when a tender was last conducted and advance notice of any retendering plans
• where there is no internal audit function, an explanation for the absence, how internal assurance is achieved and how this affects the external audit
• an explanation of how auditor independence and objectivity are safeguarded if the external auditor provides non-audit services
The Board has agreed that a joint Remuneration and Nominations Committee will be established for 2025/26.
Covered in Independent auditor’s report to the directors of Hertfordshire Community NHS Trust and reviewed by Audit Committee.
See section 3.1.1.6
Not applicable
See section 3.1.1.6
Compliant
Provisions which require a supporting explanation
D.2.6 The directors should explain in the annual report their responsibility for preparing the annual report and accounts, and state that they consider the annual report and accounts, taken as a whole, is fair, balanced and understandable, and provides the information necessary for stakeholders to assess the trust’s performance, business model and strategy.
D.2.7 The board of directors should carry out a robust assessment of the trust’s emerging and principal risks. The relevant reporting manuals will prescribe associated disclosure requirements for the annual report.
D.2.8 The board of directors should monitor the trust’s risk management and internal control systems and, at least annually, review their effectiveness and report on that review in the annual report. The monitoring and review should cover all material controls, including financial, operational and compliance controls. The board should report on internal control through the annual governance statement in the annual report.
D.2.9 In the annual accounts, the board of directors should state whether it considered it appropriate to adopt the going concern basis of accounting when preparing them and identify any material uncertainties regarding going concern. Trusts should refer to the DHSC group accounting manual and NHS foundation trust annual reporting manual which explain that this assessment should be based on whether a trust anticipates it will continue to provide its services in the public sector. As a result, material uncertainties over going concern are expected to be rare.
Compliant See section on Statement of directors’ responsibilities in respect of the accounts
Compliant See sections 3.1.3.4 and 3.1.3.5
Compliant See sections 3.1.3.2, 3.1.3.3 and 3.1.3.4
Compliant See section on Statement of directors’ responsibilities in respect of the accounts
Provisions which require a supporting explanation
E.2.3 Where a trust releases an executive director, e.g. to serve as a non-executive director elsewhere, the remuneration disclosures in the annual report should include a statement as to whether or not the director will retain such earnings.
‘Comply or explain’ requirement applies
C.4.12
C.4.13
The Remuneration Committee should not agree to an Executive member of the Board leaving the employment of the Trust except in accordance with the terms of their contract of employment, including but not limited to serving their full notice period and/or material reductions in their time commitment to the role, without the Board first completing and approving a full risk assessment.
The Annual Report should describe the work of the Nominations Committee(s), including:
• the process used in relation to appointments, its approach to succession planning and how both support the development of a diverse pipeline
• how the Board has been evaluated, the nature and extent of an external evaluator’s contact with the Board of Directors and individual Directors, the outcomes and actions taken, and how these have or will influence Board composition
• the policy on diversity and inclusion, including in relation to disability, its objectives and linkage to Trust strategy, how it has been implemented and progress on achieving the objectives
• the ethnic diversity of the Board and senior managers, with reference to indicator nine of the
Compliant This does not currently apply to any of the Trust Executive Directors.
Explain The following statement to be added to Remuneration Committee Terms of Reference:
‘except in accordance with the terms of their contract of employment, including but not limited to serving their full notice period and/or material reductions in their time commitment to the role, without the board first completing and approving a full risk assessment.’
Explain HCT does not have a Nominations Committee. The following is in place to offset this:
• In relation to appointments, we have recruitment training for all managers, diversity champions sit on interviews and when staff are in post they have access to talent programmes, career coaching and mentoring
• The policy on diversity and inclusion as well as the setting up of a Shadow Board shows the progress we are making
• We upload the WRES and WDES data following approval at Board
The Board has agreed that a joint Remuneration and Nominations Committee will be established for 2025/26.
NHS Workforce Race Equality Standard and how far the Board reflects the ethnic diversity of the Trust’s workforce and communities served
• the gender balance of senior management and their direct reports
3.1.2 Statement of the Chief Executive’s Responsibilities as the Accountable Officer of the Trust
The Chief Executive of NHS England has designated that the Chief Executive should be the Accountable Officer of the trust. The relevant responsibilities of Accountable Officers are set out in the NHS Trust Accountable Officer Memorandum. These include ensuring that:
• there are effective management systems in place to safeguard public funds and assets and assist in the implementation of corporate governance
• value for money is achieved from the resources available to the trust
• the expenditure and income of the trust has been applied to the purposes intended by Parliament and conform to the authorities which govern them
• effective and sound financial management systems are in place and
• annual statutory accounts are prepared in a format directed by the Secretary of State to give a true and fair view of the state of affairs as at the end of the financial year and the income and expenditure, other items of comprehensive income and cash flows for the year.
As far as I am aware, there is no relevant audit information of which the trust’s auditors are unaware, and I have taken all the steps that I ought to have taken to make myself aware of any relevant audit information and to establish that the entity’s auditors are aware of that information.
To the best of my knowledge and belief, I have properly discharged the responsibilities set out in my letter of appointment as an Accountable Officer.
Signed Elliot Howard-Jones Chief Executive
16 June 2025
3.1.3 Annual Governance Statement 2024/25
Scope of responsibility
As Accountable Officer, I have responsibility for maintaining a sound system of internal control that supports the achievement of the NHS trust’s policies, aims and objectives, whilst safeguarding the public funds and departmental assets for which I am personally responsible, in accordance with the responsibilities assigned to me. I am also responsible for ensuring that the NHS trust is administered prudently and economically and that resources are applied efficiently and effectively. I also acknowledge my responsibilities as set out in the NHS Trust Accountable Officer Memorandum
The purpose of the system of internal control
The system of internal control is designed to manage risk to a reasonable level rather than to eliminate all risk of failure to achieve policies, aims and objectives; it can therefore only provide reasonable and not absolute assurance of effectiveness. The system of internal control is based on an ongoing process designed to identify and prioritise the risks to the achievement of the policies, aims and objectives of Hertfordshire Community NHS Trust, to evaluate the likelihood of those risks being realised and the impact should they be realised, and to manage them efficiently, effectively and economically. The system of internal control has been in place in Hertfordshire Community NHS Trust for the year ended 31 March 2025 and up to the date of approval of the annual report and accounts.
Capacity to handle risk
The governance structure within the Trust enables an embedded risk management approach across all corporate and operational services, with discussions being reflected at the key governance committees reporting directly to the Board of Directors.
This ensures the identification, assessment, management and monitoring of strategic and operational risks at all levels. In addition, an annual audit cycle of governance due diligence is undertaken by the internal auditors who report to the Audit Committee and provide assurance on the efficacy of the Trust’s governance programme. The annual audit cycle includes an audit of the risk management process, including escalation / deescalation of risk to and from the HLRR and the impact of the approach on the BAF.
The risk architecture / risk management process is supported by clearly defined leadership roles in all levels of the Trust from staff to Board members. Every staff member is responsible for identifying, escalating and managing risks within their sphere of competency, responsibility and accountability, supported by their managers, as outlined in the Risk Management Framework.
Managers are required to demonstrate that appropriate control measures and assurances are in place, and actions are being undertaken to mitigate negative risk and enable positive risk achievement, reporting and escalating issues to their respective lead Executive Director responsible for the aligned portfolio of services.
The Trust uses an electronic risk management system, into which staff are required to record risks, along with relevant controls and actions to address any related issues. Training in relation to risk management and how to use the electronic risk management system is provided by the Trust’s risk management function. An ongoing programme of
risk management, incident and patient experience training is delivered annually with additional support provided directly to staff when requested. The training programme is supported with on-line guidance and videos, supplemented by guidance tools embedded into the electronic risk management system utilised by the Trust.
There are named key specialists and subject matter experts within the Trust who offer further specialist risk management training and guidance to all Trust employees, including for health and safety, back awareness, patient handling training, infection prevention and control, safeguarding adults and children and information governance. The Trust’s annual training programme reflects this provision. Key elements are recorded within staff mandatory training records, a summary of which is monitored at Executive Team and Board level.
The risk and control framework
In February 2024 the Trust reviewed its Risk Management Framework, Risk Appetite Statement and BAF, in line with agreed review cycles Feedback from this year’s Internal Audit review of the Trust’s risk management arrangements confirmed that overall, the Trust’s risk management process was well defined, with a clear risk management framework, and policies, roles and responsibilities of key staff and groups defined.
Policies and standard operating procedures to support effective risk management in practice are reviewed and refreshed in line with national guidance. They support the overall risk management approach and associated workforce and organisational development training programmes.
Risks to the achievement of the Trust's strategic objectives are reviewed by the Executive Team and are captured on the Trust's BAF. The BAF is regularly reviewed and discussed by the Audit Committee and the Board of Directors. Risks and their implications are considered by each Board Committee and each BAF risk has a lead Committee identified This Committee monitors and seeks assurance with regards to the management and mitigation of the risk. The BAF is assessed annually for ‘fitness for purpose’ by the Audit Committee.
Risks identified at Business Unit level are entered on Business Unit Risk Registers and risks scoring 15 or over are escalated to the HLRR The HLRR is considered monthly by the Executive Team and at each Board meeting. Each high-level risk has an identified lead Committee which is responsible for assurance in relation to the management of the risk. Risks on the HLRR that are considered by the Executive Team to have a strategic impact are captured on the BAF.
Local risk activity is reviewed at service and business unit level. High level risks are scrutinised further at Executive Team and Board committees with a remit to challenge where appropriate and receive assurance on the efficacy of controls and actions.
Business unit performance meetings and focused reviews enable lessons to be shared in the identification and management of risk while supporting the alignment of resources to optimise the Trust’s ability to achieve its objectives.
As of 31 March 2025, there were 63 risks being actively managed across all operational and business units within the Trust. The Trust’s risk management function works with risk owners to ensure they are being reviewed, managed, and updated appropriately.
The Board of Directors business cycle ensures there is oversight, review and challenge of both the HLRR and the BAF at both Board and Committee level.
Risk management is seen as an integral part of everyday clinical and non-clinical practice, supporting the delivery of the Trust's strategic objectives. Lessons learned from risks that materialise, plus sources such as complaints, claims, incidents and internal or external reports are shared throughout the organisation through a variety of communication channels including newsletters, bulletins, operational forums and video updates.
Strategic risks
The strategic risks on the BAF as at 31 March 2025 were: Ref
PR-01
PR-02
PR-03
There is a risk that the organisation is unable to meet patient demand as a result of a growing patient base, increasing reliance on community services providers and insufficient capacity. This may lead to extended waiting times for patients and harm to patients.
There is a risk that patients do not receive the appropriate care as a result of inadequate or failing standards and an ineffective governance structure failing to identify and respond to issues. This may result in harm to the patient and potential legal and regulatory action being taken.
There is a risk of a successful cyber-attack as a result of vulnerabilities in the existing cyber security protection This may lead to the data loss and/or corruption, systems being unavailable, financial loss and/or regulatory sanction.
PR-04
There is a risk that the organisation is unable to operate efficiently and meet expected performance as a result of an inability to effectively implement and embed digital and technological solutions to support effective transformation, improvement and efficiency This may lead to delays in patient waiting times, errors on patient management and loss of contracts.
PR-05
PR-06
There is a risk that the Trusts underlying financial position is not in balance as a result of a Trust wide failure to control expenditure or secure sufficient income to fund the services provided This may result in the inability to continue to provide services at the expected level and the potential loss of contracts and ultimately, ceasing to operate
There is a risk that a Trust-wide failure to control expenditure to within the budget levels set will result in the Trust being unable to achieve its financial plan in the current financial year.
Ref ID Risk Description
PR-07
PR-08
There is a risk that the organisation is unable to address health inequalities as a result of inadequate information to identify inequalities, improve access and/or improve experience of patients This could result in the continuation of impacted patients from vulnerable groups and those with protected characteristics, being underserved and not receiving the healthcare available to them.
There is a risk that the trust fails to maintain compliance with Statutory, Legal and Regulatory standards as a result inadequate understanding of legal and regulatory matters and as a result of inadequate internal practice in the review and delivery of required activities This may result in failing to meet expected standards of care and financial and/or regulatory sanction.
PR-09
PR-10
There is a risk to the Trust’s ability to deliver its strategy and provide outstanding joined up care as a result of sub-optimal partnership working and collaboration at provider, place and/or system level This may lead to gaps in or duplication of services, inability to shift resources to support greater provision of preventative care and care closer to home leading to poor patient outcomes and experience and poor value for money for the system.
There is a risk of a major disruptive external event occurring as a result of environmental hazards, accident or system failure that may lead to the Trust being unable to provide care to our patients and/or a negative impact to the health of patients, staff or others.
PR-11
There is a risk that our Estates locations are unsafe and/or are not available to us as a result of failing infrastructure and/or external events (climate or geographical) This could result in an inability to deliver services to our patients and/or a negative impact to their health.
PR-12
PR13
There is a risk that the Trust will be unable to recruit and retain the skilled workforce it requires to meet current and future service needs, as a result of tight labour markets, strong competition for roles and high staff turnover in the first two years of service. This may lead to a failure to deliver service/contract requirements, patient safety issues and staff burnout.
There is a risk that the physical and mental wellbeing, general resilience, and morale of staff is threatened as a result of sustained high levels of demand, workload pressure, staff isolation and exposure to stressful situations. This may lead to increased staff absence
and a deterioration in the quality of patient care staff are able to provide.
The overall risk score is calculated as the product of current likelihood and current impact. There is a maximum score of 25 for each rating. The following table shows the calculation formula used, where the total score is the consequence multiplied by the likelihood:
Quality governance
The Quality Committee monitors arrangements and seeks assurance on behalf of the Trust Board in respect of the quality and safety of services provided by the Trust, including follow-up actions as necessary. These include:
• Monitoring progress in delivery against the Clinical and Quality Strategy
• Monitoring progress in delivery against the Patient Engagement and Experience Strategy
• Making things better Quality Improvement approach
• Compliance with the Quality Assurance Framework
• Standing reports on patient incidents and complaints and patient experience, including follow-up actions
• Clinical audit (national and local) plan
• Good to Outstanding Programme plan
• Quality priorities for each year with action plans to achieve them
• Production and content of the Trust’s Quality Account
• Relevant subject specific annual reports (e.g. medicine management, safeguarding, infection control, research)
• Clinical policies
• CQC registration compliance
• Infection Prevention and Control
• Safeguarding
• Safe staffing levels
• Learning from Deaths
• Freedom to Speak Up
• Quality Impact Assessments
• Response to external reports and initiatives
• Monitoring progress against relevant action plans
• Assessment and challenge of quality information
• Board Assurance Framework and High-Level Risk Register risks reporting to quality committee as well as reviewing wider risks that may impact quality.
The Quality Committee also undertakes periodic operational reviews where specific services or specialties are reviewed in depth.
During 2024/25 the committees supporting the Quality Committee were:
Group
Clinical Governance Sub Committee
Associated Forums
Medicines Management
Safeguarding Adults
Safeguarding Children
Infection Prevention and Control
Medical Devices
Patient Safety Assurance Panel
Learning from Deaths Panel
Clinical Advisory Group
NICE Working Group
Pressure Ulcer Working Group
Clinical Audit Working Group
Inpatient Steering Group
Inpatient Falls Working Group
Good to Outstanding Steering Group
Clinical Transformation Programme Board
Health Inequalities Steering Group
Clinical Outcomes Steering Group
Learning from Deaths
In addition to the Quality Committee Chair’s Assurance Report, the Trust Board receives regular reports on complaints, incidents, safe staffing, infection prevention and control, Freedom to Speak Up and Learning from Deaths. Quality issues and risks also feature in the Chief Executive’s report and the Director of Nursing and Quality and Medical Director’s report which are submitted to each Board meeting.
Well-Led Framework
In April 2024, the CQC (working closely with NHS England) published updated guidance for NHS trusts structured around eight key lines of enquiry. This framework maintains focus on strong integrated governance and leadership across quality, finance and operations, in line with the changing operating environment and increases emphasis on organisational culture, improvement and system working. The guidance sets out criteria for how each of the eight well-led quality statements is assessed and what good leadership looks like for each statement.
A gap analysis between this guidance and HCT’s 2023 well-led self-assessment was completed in July 2024 demonstrating that the evidence submitted for the 2023 well-led self-assessment either fully or partially met all criteria for each of the 8 well-led quality statements.
A further well-led self-assessment, together with an independent well-led review, is planned for Q4 2024/25 and Q1 2025/26.
Registration with the Care Quality Commission
The CQC has not taken enforcement action against the Trust during 2024/25 and the Trust has not participated in any special review or investigations by the CQC during that time. The Care Quality Commission (CQC) confirmed HCT’s overall rating as ‘Good’ following a core service and well led inspection of the Trust during February/March 2020.
CQC Registration and Statutory Notification changes
• April 2024: Registration of the Integrated Community Heart Failure service and Herts & West Essex Diabetic Eye Screening Programme
• June 2024: Statutory notification regarding the appointment of Dr Nicolas Small (Trust Chair) and Marcus Riddell (Chief People Officer)
• June 2024: Notification regarding the departure of Dr Linda Sheridan (Trust Chair), Alison Ryder (Director of People) and Sam Tappenden (Director of Strategy)
• July 2024: Statutory notification regarding the appointment of Frances Khatcherian (Director of Finance, Systems and Estates)
• July 2024: Notification regarding the departure of David Bacon (Director of Finance)
• September 2024: Addition of headquarters address for the Beds, Luton & Milton Keynes Community School Aged Immunisation Service
• October 2024: De-registration of the Long Covid Rehabilitation service
Managing conflicts of interest in the NHS
The Trust has published on its website an up-to-date register of interests, including gifts and hospitality, for the Board of Directors within the past twelve months as required by the ‘Managing Conflicts of Interest in the NHS’ guidance.
The Trust publishes an up-to-date register of interests for Board members annually. The Audit Committee received the up-to-date Register of Interests for all decision making staff in September and March. The Board meeting in public received the up-to-date Register of Interests for Board members in March. This is recorded in the publicly posted Board minutes and in the end of year Annual Report
NHS pension scheme rules
As an employer with staff entitled to membership of the NHS Pension Scheme, control measures are in place to ensure all employer obligations contained within the scheme regulations are complied with. This includes ensuring that deductions from salary, employer’s contributions and payments into the scheme are in accordance with the scheme rules, and that member scheme records are accurately updated in accordance with the timescales detailed in the Regulations.
Payment of Trust staff
The Trust uses the national Electronic Staff Record (ESR) system to maintain staff records and to pay its staff. The annual Service Auditor Report identified two control weaknesses. However, other compensating controls demonstrate that the control deficiency had been sufficiently mitigated locally.
Modern Slavery Act 2015 - Transparency in supply chains
The Trust is aware that slavery and human trafficking can occur in many forms, such as forced labour, domestic servitude, sex trafficking and workplace abuse. The Trust is committed to maintaining and improving systems, processes and policies across the organisation to avoid complicity in human rights violation.
Our policies, governance and legal arrangements are robust, ensuring that proper checks and due diligence take place in our procurement and employment procedures to ensure compliance with this legislation.
Equity, diversity and human rights
Control measures are in place to ensure that all the organisation’s obligations under equality, diversity and human rights legislation are complied with.
Climate change
The trust has undertaken risk assessments on the effects of climate change and severe weather and has developed a Green Plan following the guidance of the Greener NHS programme. The Trust ensures that its obligations under the Climate Change Act and the Adaptation Reporting requirements are complied with.
Emergency preparedness, resilience and response (EPRR)
The NHS requires Trusts to maintain essential services during disruption, whatever the cause. The Trust works both internally, with partner agencies and external organisations to ensure resilience during times of disruption. Business Continuity and other Plans are in
place to maintain vital services when interruptions occur, for example severe weather, industrial action or disruption to transport. This approach proved its value across the organisation during the COVID-19 pandemic and other emergency situations.
Emergency Planning (known by the NHS as EPRR) exists to work alongside internal and external partners to achieve this in ways that provide safety and protection for patients and staff at all times. Emergency Planning activity is defined by and measured by the NHS EPRR Core Standards HCT was rated as Fully Compliant across the 58 Standards which made up the 2024 NHS England Core Standards Assurance process for EPRR.
In accordance with the NHS EPRR Core Standards requirements, HCT’s Emergency Planning arrangements are overseen by Marion Dunstone, Chief Operating Officer, who is the organisation’s EPRR Accountable Emergency Officer. Marion chairs the Quarterly EPRR meeting (an Executive team sub-group) which reviews Emergency Planning progress and developments.
Since the end of the COVID-19 Incident, Operational (Bronze) meetings have been retained, with the focus amended where required to the current operational situation of the Trust and the system Board of Directors’ arrangements are in place to enable ‘emergency’ decisions to be made outside of scheduled Board meetings where required.
Review of economy, efficiency and effectiveness of the use of resources
The Trust’s financial performance is monitored at the monthly People Performance and Finance Committee (PPFC) The committee monitors financial performance in its broadest sense and is concerned with the overall efficiency and effectiveness relating to the deployment of Trust resources. Further assurance is sought at the Trust Board of Directors
The Trust’s Audit Committee also performs a pivotal role in providing the Board of Directors with assurance on the use of resources. Each year the Audit Committee commissions the internal auditors to undertake reviews of key internal risks to gain assurance that there are sufficient and appropriate processes in place to demonstrate the economic, efficient and effective use of resources. If gaps are identified action plans are put in place and monitored to ensure these are addressed.
To ensure that the Trust can demonstrate the effectiveness of its services, it participates in local and national benchmarking exercises. The Trust is a member of the NHSE Model Health System cohort for community trusts. This group enables the Trust to compare itself with peer organisations and share best practice to promote improvement.
The Trust continues to participate in the national reference costs collection process and submitted its national cost collection return in July 2024 National guidance on contracting within the NHS requires organisations to consider the costs of its activities in the setting of financial envelopes. Where proposals for service transformations and improvements are being considered, the impact on the cost base is also taken into account.
Information governance
During 2024/25 no information governance incidents have occurred that required reporting to the Information Commissioner’s Office.
All information governance incidents are taken seriously and advice is taken as appropriate from the Medical Director, as Caldicott Guardian, and/or the Director of
Finance, as Senior Information Risk Owner (SIRO). Incidents are fully investigated, remedial action is taken and lessons learned are applied across the organisation.
The Trust’s Information Governance Group, which includes the SIRO and Caldicott Guardian, reviews all data security incidents Changes in practice have been made in some cases to minimise the risk of repetition, a standard operating procedure has been adopted across the Trust for the handling and processing of correspondence that includes Personal Confidential Data.
During 2023-24 The Trust has achieved ‘Standards Met’ compliance for the Data Security and Protection Toolkit (DSPT) which has been verified by independent auditors.
For 2024-25 there have been significant changes to the Data Security & Protection Toolkit which ensure it is aligned to the National Cyber Assurance Framework The Trust’s overall score is assessed based on five objectives which are then broken down into a series of principles and contributing outcomes. The five objectives are:
• Managing Risk
• Protecting Against Cyber Attack and Security Breaches
• Detecting Cyber Security Events
• Minimising the Impact of Incidents
• Using and Sharing Information Appropriately
The final published score for 2024-25 is not due for final submission until 30th June 2025 The Trust anticipates achieving ‘Standards met’ status subject to verification from internal auditors.
Data quality and governance
The Directors are required under the Health Act 2009 and the National Health Service (Quality Accounts) Regulations 2010 (as amended) to prepare Quality Accounts for each financial year.
The Trust has a formal reporting process to collate the quality data (both quantitative and qualitative including elective waiting time data) which forms the basis of information provided in the end-of-year Quality Account. Trust performance data is reviewed and validated internally through relevant performance and quality governance committees and groups, including the Executive Team, prior to sign-off. It is shared with our commissioners and is incorporated within our contract review meetings, thus ensuring external validation of all relevant data.
The Quality Account is developed through a robust process which commences early in Quarter 4 each year and involves input and oversight from the Executive Team and Trust Board of Directors. The draft Quality Account is shared with key stakeholders for comment, providing an external overview of its content and balance as well as agreement for the key quality priorities set out in the Account. The final version is signed off by the Executive Team and the Board of Directors.
Review of effectiveness
As Accountable Officer, I have responsibility for reviewing the effectiveness of the system of internal control. My review of the effectiveness of the system of internal control is informed by the work of the internal auditors, clinical audit and the executive managers and clinical leads within the NHS trust who have responsibility for the development and maintenance of the internal control framework. I have drawn on the
information provided in this annual report and other performance information available to me My review is also informed by comments made by the external auditors in their management letter and other reports. I have been advised on the implications of the result of my review of the effectiveness of the system of internal control by the Board, the Audit Committee and Quality Committee and a plan to address weaknesses and ensure continuous improvement of the system is in place.
The Head of Internal Audit opinion for 2024/25
The Head of Internal Audit opinion for 2024/25 is that:
"The organisation has an adequate and effective framework for risk management, governance and internal control. However, our work has identified further enhancements to the framework of risk management, governance and internal control to ensure that it remains adequate and effective."
One ‘substantial assurance’ opinion was issued on CQC Good to Outstanding Strategy Three ‘reasonable assurance’ opinions were issued on Data Quality; Key Financial Controls (Cash and Treasury); and Risk Management. Two ‘partial assurance’ opinions were issued on Medicines Management and Efficiency Audit
Trust management have agreed actions to address all of the findings reported by Internal Audit during 2024/25 and nine remained overdue at the time of drafting the 2024/25 Internal Audit Annual Report with 18 implemented and 15 not yet due. Actions are being monitored by management through the action tracking process in place. During the year progress has been reported to the Audit Committee, with the validation of the action status confirmed by Internal Audit on a monthly basis.
Assurances as to the effectiveness of internal controls
Executive managers within the Trust, who have responsibility for the development and maintenance of the system of internal control, also provide me with assurance. The Assurance Framework itself provides me with evidence that the effectiveness of controls that manage the risks to the organisation achieving its principal objectives have been reviewed. My review is also informed by:
• Internal audit reports and the Head of Internal Audit opinion
• External audit
• CQC registration requirements and outcomes
• CQC inspection reports
• The Trust’s monthly Service Recovery and Performance Reports
• Minutes and papers of the Trust Board of Directors Board committees and subcommittees, including reports from Executive Directors as standing items
• Reports from the local counter-fraud specialist
• Submissions to, and feedback from, NHS England
• Quality and service review meetings with commissioners
• Board of Directors and Executive site visits and ‘deep dives’ into services
• Assurance reports from the chairs of groups which report to the Executive Team
• Compliance with the NHS Data Security and Protection Toolkit (DSPT)
• Board self-certification of compliance with NHS Provider Licence conditions GC6 and FT4
I have been advised on the implications of the result of my review of the effectiveness of the system of internal control by the Audit Committee, Quality Committee, People Performance and Finance Committee and the Executive Team.
The following have a role in maintaining and reviewing the effectiveness of the system of internal control:
The Board of Directors has been actively involved in developing and reviewing the Trust’s risk management processes, including receiving and reviewing minutes and chair’s observations from all committees which report to the Board of Directors. The Board also reviews the BAF, HLRR, Service Recovery and Performance reports and Quality reports in line with the Trust business cycle.
The Audit Committee has been a directing force in relation to reviewing the framework of internal control particularly regarding corporate risk, the Board Assurance Framework, the HLRR and counter fraud
The Quality Committee is responsible for the governance and management of clinical risk, including ensuring compliance with regulatory standards and requirements, adoption of clinical policies and review of clinical aspects of performance, including incidents and complaints. The Committee also provided assurance to the Board of Directors in respect of patient safety, quality of services and patient experience
The People Performance and Finance Committee scrutinised current financial performance and future financial plans; reviewed financial, workforce and business risks; monitored those decisions involving finance, resources and assets were properly made to promote good financial practice throughout the Trust and received assurances that an integrated and holistic approach was taken to the use of all the Trust's resources for the delivery of the Trust strategy.
The Information Governance Steering Group – meets bi-monthly The Head of Information Governance is responsible for the day-to-day governance and management of information associated risk and compliance through the DSPT.
The Executive Team met weekly and operationally managed all areas of risk, including the risk and control framework. The Executive Team also populates and reviews the Board Assurance Framework and reviews the HLRR, as well as ensuring that key risks have been highlighted and monitored within their directorates and that necessary action has been taken to address them
Internal Audit has reviewed and reported upon control, governance and risk management processes, based on an audit plan approved by the Audit Committee and endorsed by the Board of Directors. Where scope for improvement was found, recommendations were made, and appropriate action plans agreed with management
Clinical audit is overseen by the Trust’s Clinical Governance Sub Committee, which reports to the Executive Team and gives assurance to the Quality Committee. The clinical audit programme is also reported to the Trust’s Audit Committee. Lessons learned from clinical audits are shared through the Clinical Audit Working Group, are detailed in the annual Quality Account, and are reported to Trust committees as part of the regular reporting cycle Plans are in place to share lessons learned more widely
through other staff communication channels such as All Staff Bulletin and Team Conversation.
My review confirms that the Trust has a generally sound system of internal control that supports the achievement of its policies, aims and objectives.
Conclusion
No significant control issues have been identified for 2024/25
Signed Elliot Howard-Jones Chief Executive
16 June 2025
3.2 Remuneration and staff reports
3.2.1
Remuneration report
Remuneration and the Remuneration Committee
The Trust’s Remuneration Committee, which met four times during 2024/25, makes decisions to recommend to the Trust Board on the remuneration and terms & conditions of the Chief Executive and Executive Directors on Very Senior Manager (VSM) contracts. The Committee also reviews all severance payments made during the year and considers implementation of any local expenses and benefits which are outside of national terms and conditions.
During 2024/25, membership of the Committee consisted of:
• Richard Rolt – Non-Executive Director (Chair of the Remuneration Committee)
• Chris Ford – Non-Executive Director
• Dr Nicolas Small – Trust Chair
The following were also in attendance:
• Chief Executive
• Chief People Officer
• Director of Finance, Systems and Estates
During 2024/25, the main agenda items addressed by the committee were:
• The VSM pay award
• Director of Finance appointment
• Redundancy payments
The Chair and Non-Executive Directors are remunerated at rates prescribed by the Secretary of State for Health and Social Care. Executive Directors are remunerated as set out in the NHS Very Senior Managers (VSM) Pay Framework and senior managers are paid in accordance with NHS Agenda for Change pay scales.
Executive Directors are appointed on substantive, permanent contracts with remuneration overseen by NHS England. In the event of termination by the Trust, any payment due is paid in accordance with the reason for termination and the contract of employment however there have been no contracts terminated during 2024/25 Changes to the Executive Team this year have been the substantive appointment to the Director of Finance, Systems & Estates and Directors of People posts following retirement of the previous postholders.
Fair pay disclosure
Reporting bodies are required to disclose the relationship between the remuneration of the highest-paid director / member in their organisation against the 25th percentile, median and 75th percentile of remuneration of the organisation’s workforce. Total remuneration is further broken down to show the relationship between the highest paid director's salary component of their total remuneration against the 25th percentile, median and 75th percentile of salary components of the organisation’s
workforce.
The banded remuneration of the highest paid director in Hertfordshire Community NHS Trust in the financial year 2024/25 was £175k - £180k (£165k – £170k in 2023/24). This is a change between years of 6% (6.3% in 2023/24). The relationship to the remuneration of the organisation's workforce is disclosed in the below table.

No performance or bonus related pay was received by the highest paid director in 2024/25 (nil in 2023/24) so the additional disclosures differentiating total remuneration and salary only components of pay are no different to those disclosed above.
The ratios of total remuneration of the highest paid director to the median and 75th percentile points have increased from 2023/24 to 2024/25.
In 2024/25, three (five in 2023/24) employees received remuneration in excess of the highest paid director. Remuneration ranged from £12,659* to £196,000 (£10,370*£217,350 in 2023/24). The percentage change in average employee remuneration between years was 0.2% (6.6% in 2023/24).
Total remuneration includes salary, non-consolidated performance-related pay, benefits-in-kind, but not severance payments. It does not include employer pension contributions and the cash equivalent transfer value of pensions.
*This is based on salary rates for apprentices. (This section was subject to audit and is referred to in the Auditor’s Opinion).
Compensation on early retirement or for loss of office and payments to past directors
The Trust made no payments in respect of exit packages or severance payments to Directors in 2024/25 and no payments were made to past Directors. (This paragraph was subject to audit and is referred to in the Auditor’s Opinion).
Exit packages
18 exit packages were agreed in 2024/25 in relation to a contractual redundancy payment
£100,001 - £150,000
£150,001 - £200,000
Non-contractual exit payments
The Trust made 0 non-contractual exit payments in 2024/25. Non-contractual payments are those made without contractual or legal obligation, including those from judicial mediation.
Board of Directors salaries and pensions
(This section was subject to audit and is referred to in the Auditor’s Opinion).
Board of Directors salaries and allowances 2024/25
1.Chairretiredfrompost20thApril2024.
2.ChairjoinedtheTrust3rdJune2024.
3.Directorwasinpost1stApril2024-31stJuly2024,andretired31stJuly2024.
4.InterimDirectorofFinancefromJuly2024toOctober2024.
5.DirectorjoinedtheTruston16thSeptember2024.
6.Whereaseniormanager’sremunerationincludeselementsfortheirmanagementroleandanotherrole,forexampleclinicalrolesofmedicaldirectorsandsimilarstaff,theremunerationreport mustreflectthetotalremunerationpaidbytheTrustfortheindividual’sservicestotheTrust,includingfordutiesthatare
7.DirectorjoinedtheTrust1stJuly2024.
8.Directorwasinpost1stApril2024-31stMay2024,andretired31stMay2024.
Board of Directors salaries and allowances 2023/24
1. Whereaseniormanager’s remunerationincludes elements fortheirmanagementroleandanotherrole,forexampleclinicalroles ofmedicaldirectors and
theremunerationreportmustreflectthetotalremunerationpaidbytheTrustfortheindividual’s services totheTrust,includingforduties thatarenotpartoftheir managementrole.
2.This directorwas inpost1April2023-31March2024.Threemonths ofthis was as asecondedemployeefrom EastandNorthHertfordshireNHSTrustandnine months was as asubstantiveemployeewithHertfordshireCommunityNHSTrust.
2023/24
Pension benefits 2024/25
PensionBenefitsofindividualsinpostatyearend
3. ARyderretiredfromtheTrustduring2024/25andisexcludedfromthedisclosure.
Pension benefits 2023/24
2.CashEquivalentTransferValuesarenotshownforbenefitsunderspecificsectionsoftheNHSPensionSchemeonceNormalPensionAgeforthatSectionhas beenreached. 2023/24
Cash Equivalent Transfer values (CETV) exclude the value of pensions and lump sums for NHS Pensions Schemes where members have reached Normal Pension Age under that aspect of the scheme.
CETV figures are calculated using the guidance on discount rates for calculating unfunded public service pension contribution rates that was extant at 31 March 2023. HM Treasury published updated guidance on 27 April 2023; this guidance will be used in the calculation of 2023 to 24 CETV figures
Accrued pensions and CETVs are based on current membership of one of the specific NHS Pension schemes If members opt to move entitlements between schemes under the ‘McCloud judgement,’ actual pensions and CETVs may change’
Cash Equivalent Transfer Values
A Cash Equivalent Transfer Value (CETV) is the actuarially assessed capital value of the pension scheme benefits accrued by a member at a particular point in time. The benefits valued are the member’s accrued benefits and any contingent spouse’s (or other allowable beneficiary’s) pension payable from the scheme. CETVs are calculated in accordance with the Occupational Pension Schemes (Transfer Values) Regulations 2008.
Real increase in CETV
This reflects the increase in CETV effectively funded by the employer. It does not include the increase in accrued pension due to inflation, contributions paid by the employee (including the value of any benefits transferred from another scheme or arrangement) and uses common market valuation factors for the start and end of the period. As stated above, the value of pensions and lump sums are excluded from the CETV once a member reaches Normal Pension Age under that aspect of the scheme. For this reason, there may be a reduction in CETV shown.
Pension liabilities
Pension liabilities are treated as payables in the accounts. The accounting policy refers to the treatment of pensions within the Trust’s accounts.
3.2.2 Staff Report
Staff groups
The breakdown of the Trust by staff group is shown below:
Trust Employees by Staff Group - 31 March 2025
Add Prof Scientific and Technical
Additional Clinical Services
Administrative and Clerical
Allied Health Professionals
Estates and Ancillary
Medical and Dental
Nursing and Midwifery Registered
Students
For the purposes of the graph below a senior manager has been classed as a nonclinical member of staff at Agenda for Change Band 8a or above.
Number of Senior Managers by Agenda For Change Band 31 March 2025
Staff by gender
The mix of staff by gender as at 31 March 2025 is shown below (table broken down by directors, senior managers (non-clinical), all other staff):
The Trust Board of Directors and Executive Directors by gender
The mix of gender on the Board of Directors as at 31 March 2025 was as follows (table broken down by chair and NEDs, Exec and combined, with percentages):
Note: Includes voting and non-voting members.
Staff by ethnic background
A breakdown of staff by ethnic background is provided below. This is according to data obtained from the Hertfordshire County Council Diversity and Inclusion Annual Report 2021-2022.
Ethnicity of Trust Staff versus the Local Population 31 March 2025
This is according to data obtained from the Hertfordshire County Council Diversity and Inclusion Annual Report 2021-2022.
Staff by age band
The age breakdown of staff at 31 March 2025 was as follows:
Age Range of Trust Employees 31 March 2025
Staff by pay band (full time equivalent)
The breakdown of staff by pay band in 2023-2024 and 2024-2025 was as follows:
BandingbyFTE 2023/24 2024/25
Staffing cost analysis
The tables below show the average number of staff throughout the year and the total cost of staff to the Trust as an employer:

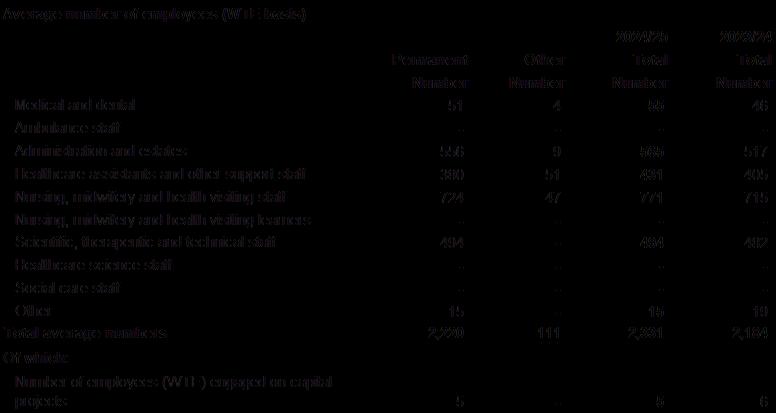
Trade Union Facility Time (April 2024 to March 2025)
The following information is published in accordance with the Trade Union (TU) (Facility Time Publication Requirement) Regulations 2017.
19 of the Trust’s employees (16.16 full-time equivalent) were union officials during this period. 15 of these employees spent a small proportion of their working hours on facility time. The total cost of this facility time to the Trust was £15,325 representing 0.01% of the total pay bill. The time spent on union activities as a proportion of total paid facility hours was 8.71%
The Trust believes that we get good value for money for the small amount spent on union representatives and functions better as a result of their input.
Workforce Vision
To underpin delivery of our Great Place to Work strategic objective, our People Strategy sets out our plans to ensure our people continue to be engaged, developed, well-led and supported. Our Strategy can be summarised as follows:

This is supported by our annual People Plan which describes the activities we will undertake to achieve this vision, some of which are set out in the sections below.
Staff engagement
We continue to use a wide range of online methods of communication with staff, such as our fortnightly Team Conversation Q&A and Listen and Learn sessions with our Chief Executive, which are open to all staff. Our weekly ‘All Staff Bulletins’ provide staff with regular updates and we also support our leaders with meetings, resources and bulletin updates on matters relating to managing staff. Our People Team run a bi-monthly People Manager meeting, which is well attended and is both informative and a learning/discussion opportunity regarding HR matters. During 2024, the team have also introduced a programme of regular online drop ins, available to everyone for recruitment, ESR and rostering queries.
Two interactive Staff Summits provided the opportunity to directly engage with staff at all levels about ‘hot topics’ within the organisation, such as Quality Improvement, EDI and staff retention.
Having conducted a light touch review of our Shadow Board with its members this year and developed and agreed recommendations to further embed it in the Trust, we continue to benefit from the broad range of insights and perspectives of this diverse group. We have increased our 2,7 networks to seven: our CRE&D network (Celebrating Racial Equity and Diversity); our Together We Can (Disability and
restrictive or long term health conditions) network; our Proud To Be (LGBTQI+) network; our Armed Forces network; our Carer network; our Menopause network and our newly formed Young Persons Staff Network and engage with them regularly.
Staff recognition
We were pleased to hold our annual ‘Leading Lights’ staff recognition event in June 2024 This enabled us to recognise our inspiring individuals and teams who have made exceptional contributions to the Trust, celebrating achievements across eight categories, with over 300 staff attending. Having re-launched our ‘HCT Superstars’ scheme in early 2024, we have since recognised over 130 'Superstars' This complements our annual event by providing a way of recognising exceptional individuals on a more frequent basis, with badges and certificates presented locally to staff throughout the year. We have also recognised many staff via our All Staff Bulletin, show casing positive patient feedback as Glimpses of Brilliance.
Staff Surveys
The Trust runs the national NHS Staff Survey as a full online census of all staff and 64% of staff completed the 2024 NHS Staff Survey. Despite this being slightly less than the 2023 survey (66%), it is still a good response rate and compares to 50% nationally.
Staff Benefits
We are pleased to have continued to offer free car parking on all sites this year. Along with offering free Blue Light cards (discount card for Healthcare Workers), we have also continued to support our staff to mitigate the high cost of living by providing our benefits portal, which promotes information on our staff benefits and initiatives and provides access to a wide range of discounts for external retailers and services.
Talent Management
We expanded our ‘Developing Our People’ programme offer (formerly called Personal Effectiveness Programmes) and offered an additional two programmes in order to meet demand and to ensure that a choice of delivery model was available. In total more than 400 staff have now accessed these programmes, which focus on personal and career development.
As part of our inclusive talent management approach, we launched ‘Thrive,’ a suite of career development offers specifically for staff from Black and Minority Ethnic backgrounds. These were guided by staff engagement, with offers including virtual and face-to-face training sessions, and an Inclusive Mentoring Programme.
Leadership development
The trust is committed to continual leadership development through a comprehensive development programme that includes opportunities for leadership and management training, action learning sets, coaching and access to system strategic leadership programmes A highlight of the leadership calendar was our Annual Leaders Conference, which built on our organisational development themes of compassion and inclusion This event was supplemented by two shorter Leaders Forums during the year, as well as our Essential Leaders Day, designed for our frontline leaders
Staff development
This year we have continued our support for career development as part of our offers to retain staff. Career conversations with appraisers has been part of our appraisal processes for many years and, in addition, our 100th request for a Conversation with one of our career coaches was submitted during the year. We have developed a ‘Career Safari,’ a comprehensive repository of staff career journeys designed to inspire staff which wish to progress.
We have particularly focussed on our administrative staff as part of the Excellence in Administration programme. We have created administrator career pathway information to give more visibility to available opportunities both within administration and, for those who might wish to progress, into clinical roles. We have introduced a specific session for administrators as part of our corporate welcome events and we used our Excellence in Administration conference to run a career café to enable staff to find out from corporate services about their work, roles available and routes into them. The conference, attended by 120 staff from operational and corporate services, also heard from Rob Hosking about Resilience for themselves and in their teams.
We have worked with NHS Hertfordshire and West Essex to deliver an improved work experience offer, whereby specific nursing and AHP services are able to provide work experience for young people considering clinical careers.
Approximately, 75% of our Apprenticeship Levy funds are being spent on enable our staff to progress into Nursing Associate, registered nurse or Allied Health professions. 8 staff members have qualified during 24-25 and 49 staff continue on health care professional programmes.
We have used also our CPD funds to enable individuals to attend specialist clinical training and update sessions, as well as broader personal development.
Staff recruitment and retention
Our staff turnover has reduced throughout the year from 11.1% in April 2024 to 9.1% in March 2025. Over the past year, we have undertaken a variety of measures including improvements to our onboarding and induction programmes, embedding of our buddy scheme, manager training on a variety of People Team processes, bespoke support for our international recruits and undertaking targeted exit interviews. We have set up a Young Person’s staff network to engage with our young people on issues related to recruitment, retention, policies and practices, and to provide information to help them to develop their careers within HCT.
A main area of focus in 2024 has been reviewing our Applicant Tracking System to ensure the best possible candidate experience. This meant that we decided to bring our recruitment administration support in-house which was previously undertaken by Trac, this transition happened on 4th November 2024 and since then our Time to Hire has seen an improvement in December 2024 of 61.05 days compared to 77.04 days in December 2023 Further transformational work is being undertaken in 2025 to streamline the entire recruitment process; this in turn should enable a further reduction in the time to hire KPI We have also introduced inclusive recruitment training for our managers.
Diversity and inclusion in employment
We review and report on the profile of our workforce through our Public Sector Equality Duty (PSED) report, NHS Workforce Race Equality Standard (WRES) report, Workforce Disability Equality Standard (WDES) and Gender Pay Gap Report, with the development of associated action plans.
Disability
The Trust has been reassessed and maintained Level 2 Disability Confident Employer status under the Disability Confident scheme. This supports employers to make the most of the talents disabled people can bring to the workplace, by helping them to successfully recruit and retain disabled people and those with health conditions.
186 Trust staff have declared they have a disability equating to 6.7% of the workforce (an increase compared to the 5.4% last year). Over the last year we recruited 41 new staff with a disability to work in our services.
Health and wellbeing
Recognising the demands that our teams continue to be under, supporting the health and wellbeing of our staff has continued to be a very high priority for the Trust. We have renewed the contract for our Employee Assistance Programme for a further 3 years, which offers confidential telephone support, including counselling, to staff. We continue to support staff with musculoskeletal issues with our fast-track physiotherapy service. We have also renewed our Schwartz Licence for a further two years; and have been undertaking planning for a 2025 ‘roadshow’ of Rounds. Funded by charitable funds, our Quality Team have introduced a pilot programme of wellbeing checks for staff; with nurses visiting operational Trust sites to offer cholesterol and blood pressure checks, as well as supportive wellbeing conversations. These checks have been very popular with staff (386 checks carried out in 2024) and funding has been identified to continue to provide this wellbeing support and evaluate its effectiveness in 2025. We have also expanded our team of Professional Advocates as an additional support to staff and provided refresher training to our Mental Health First Aiders.
The Trust’s Health at Work Service is provided by East and North Hertfordshire NHS Trust, which is accredited under the SEQOHS (Safe Effective Quality Occupational Health Service) scheme In 2024/25:
• 531 pre-placement assessments were undertaken
• 541 employees were referred to the Health at Work Service for advice
• 379 appointments were attended for occupational immunisations, including vaccines and blood tests for Hepatitis B, chickenpox, measles, mumps, rubella and tuberculosis (but excluding flu).
Staff sickness continues to be managed with the support of our Health at Work (Occupational Health) Service For the 12 months to March 2025, our cumulative absence rate (Full Time Equivalent) was 4.1%. This equates to 14.53 calendar days per employee, which is a decrease compared with the previous year’s rate of 3.5% (12.98 calendar days per employee).
Our uptake of vaccinations by staff was 50% for Flu and 26% for Covid
Declaration
I confirm adherence to the reporting framework in respect of the Accountability Report.
Signed Elliot Howard Jones Chief Executive
16 June 2025
Statement of directors’ responsibilities in respect of the accounts
The directors are required under the National Health Service Act 2006 to prepare accounts for each financial year. The Secretary of State, with the approval of HM Treasury, directs that these accounts give a true and fair view of the state of affairs of the trust and of the income and expenditure, other items of comprehensive income and cash flows for the year. In preparing those accounts, the directors are required to:
• apply on a consistent basis accounting policies laid down by the Secretary of State with the approval of the Treasury
• make judgements and estimates which are reasonable and prudent
• state whether applicable accounting standards have been followed, subject to any material departures disclosed and explained in the accounts and
• prepare the financial statements on a going concern basis and disclose any material uncertainties over going concern
The directors are responsible for keeping proper accounting records which disclose with reasonable accuracy at any time the financial position of the trust and to enable them to ensure that the accounts comply with requirements outlined in the above mentioned direction of the Secretary of State. They are also responsible for safeguarding the assets of the trust and hence for taking reasonable steps for the prevention and detection of fraud and other irregularities.
The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the accounts.
The directors confirm that the annual report and accounts, taken as a whole, is fair, balanced and understandable and provides the information necessary for patients, regulators and stakeholders to assess the NHS trust’s performance, business model and strategy
By order of the Board
16/06/2025 Chief Executive
16/06/2025 Chief Finance Officer
Independent Auditor’s Report to Directors of the Trust
Report on the audit of the financial statements
Opinion on the financial statements
We have audited the financial statements of Hertfordshire Community NHS Trust (the ‘Trust’) for the year ended 31 March 2025, which comprise the Statement of Comprehensive Income, the Statement of Financial Position, the Statement of Changes in Taxpayers Equity, the Statement of Cash Flows and notes to the financial statements, including accounting policies and other information. The financial reporting framework that has been applied in their preparation is applicable law and UK adopted international accounting standards, in conformity with the requirements of the Accounts Directions issued under Schedule 4 of the National Health Service Act 2006, as interpreted and adapted by the Department of Health and Social Care Group Accounting Manual 2024 to 2025.
In our opinion, the financial statements:
• give a true and fair view of the financial position of the Trust as at 31 March 2025 and of its expenditure and income for the year then ended; and
• have been properly prepared in accordance with UK adopted international accounting standards, as interpreted and adapted by the Department of Health and Social Care Group Accounting Manual 2024 to 2025; and
• have been prepared in accordance with the requirements of the National Health Service Act 2006.
Basis for opinion
We conducted our audit in accordance with International Standards on Auditing (UK) (ISAs (UK)), applicable law and Practice Note 10 ‘Audit of Financial Statements and Regularity of Public Sector Bodies in the United Kingdom’, as required by the Code of Audit Practice (“the Code of Audit Practice”) approved by the Comptroller and Auditor General. Our responsibilities under those standards are further described in the ‘Auditor’s responsibilities for the audit of the financial statements’ section of our report. We are independent of the Trust in accordance with the ethical requirements that are relevant to our audit of the financial statements in the UK, including the FRC’s Ethical Standard, and we have fulfilled our other ethical responsibilities in accordance with these requirements. We believe that the audit evidence we have obtained is sufficient and appropriate to provide a basis for our opinion.
Conclusions relating to going concern
In auditing the financial statements, we have concluded that the directors’ use of the going concern basis of accounting in the preparation of the financial statements is appropriate.
Based on the work we have performed, we have not identified any material uncertainties relating to events or conditions that, individually or collectively, may cast significant doubt on the Trust's ability to continue as a going concern for a period of at least twelve months from the date when the financial statements are authorised for issue.
Our responsibilities and the responsibilities of the directors with respect to going concern are described in the relevant sections of this report.
Other information
The other information comprises the information included in the Annual Report, other than the financial statements and our auditor’s report thereon. The directors are responsible for the other information contained within the Annual Report. Our opinion on the financial statements does not cover the other information and, except to the extent otherwise explicitly stated in our report, we do not express any form of assurance conclusion thereon.
Our responsibility is to read the other information and, in doing so, consider whether the other information is materially inconsistent with the financial statements or our knowledge obtained in the audit or otherwise appears to be materially misstated.
If we identify such material inconsistencies or apparent material misstatements, we are required to determine whether this gives rise to a material misstatement in the financial statements themselves. If, based on the work we have performed, we conclude that there is a material misstatement of this other information, we are required to report that fact.
We have nothing to report in this regard.
Opinion on other matters required by the Code of Audit Practice
In our opinion:
• The parts of the Remuneration and Staff Report to be audited have been properly prepared in accordance with the requirements set out in the Department of Health and Social Care Group Accounting Manual 2024 to 2025; and
• Based on the work undertaken in the course of the audit of the financial statements, the other information published together with the audited financial statements in the Annual Report for the financial year for which the financial statements are prepared is consistent with the financial statements.
Matters on which we are required to report by exception under the Code of Audit Practice
Under the Code of Audit Practice, we are required to consider whether the Annual Governance Statement does not comply with the guidance issued by NHS England or is misleading or inconsistent with information of which we are aware from our audit. We are not required to consider whether the Annual Governance Statement addresses all risks and controls or that risks are satisfactorily addressed by internal controls.
We have nothing to report in respect of the above matters.
Responsibilities of the directors
As explained more fully in the statement of directors’ responsibilities in respect of the accounts, the directors are responsible for the preparation of the financial statements in the form and on the basis set out in the Accounts Directions included in the Department of Health and Social Care Group Accounting Manual 2024 to 2025, for being satisfied that they give a true and fair view, and for such internal control as the directors determine is necessary to enable the preparation of financial statements that are free from material misstatement, whether due to fraud or error.
In preparing the financial statements, the directors are responsible for assessing the Trust’s ability to continue as a going concern, disclosing, as applicable, matters related to going concern and using the going concern basis of accounting unless the directors have been informed by the relevant national body of the intention to dissolve the Trust without the transfer of its services and functions to another public sector entity. The directors are required to comply with the requirements set out in the Department of Health and Social Care Group Accounting Manual 2024 to 2025.
Auditor’s responsibilities for the audit of the financial statements
Our objectives are to obtain reasonable assurance about whether the financial statements as a whole are free from material misstatement, whether due to fraud or error, and to issue an auditor’s report that includes our opinion. Reasonable assurance is a high level of assurance, but is not a guarantee that an audit conducted in accordance with ISAs (UK) will always detect a material misstatement when it exists. Misstatements can arise from fraud or error and are considered material if, individually or in the aggregate, they could reasonably be expected to influence the economic decisions of users taken on the basis of these financial statements.
A further description of our responsibilities for the audit of the financial statements is located on the Financial Reporting Council’s website at: www.frc.org.uk/auditorsresponsibilities. This description forms part of our auditor’s report.
Extent to which the audit was considered capable of detecting irregularities, including fraud
Irregularities, including fraud, are instances of non-compliance with laws and regulations. We design procedures in line with our responsibilities, outlined above, to detect material misstatements in respect of irregularities, including fraud. Owing to the inherent limitations of an audit, there is an unavoidable risk that material misstatements in the financial statements may not be detected, even though the audit is properly planned and performed in accordance with the ISA’s (UK).
The extent to which our procedures are capable of detecting irregularities, including fraud is detailed below:
We obtain and update our understanding of the Trust, its activities, control environment, and likely future developments, including in relation to the legal and regulatory framework applicable and how the Trust is complying with that framework. We determined that the most significant legal and regulatory frameworks that are applicable to the Trust, which are directly linked to specific assertions in the financial statements, are those related to the financial reporting frameworks. These include the National Health Service Act 2006 and international accounting standards, as interpreted and adapted by the Department of Health and Social Care Group Accounting Manual 2024 to 2025.
Based on this understanding, we identify and assess the risks of material misstatement of the financial statements, whether due to fraud or error, design and perform audit procedures responsive to those risks, and obtain audit evidence that is sufficient and appropriate to provide a basis for our opinion. This includes consideration of the risk of acts by the Trust that were contrary to applicable laws and regulations, including fraud.
In response to the risk of irregularities and non-compliance with laws and regulations, including fraud, we designed procedures which included:
• Enquiry of management, internal audit, and those charged with governance concerning the Trust’s operations, the key policies and procedures, and the establishment of internal controls to mitigate risks related to fraud and noncompliance with laws and regulations, together with their knowledge of any actual or potential litigation and claims and actual, suspected and alleged fraud;
• Reviewing minutes of meetings of those charged with governance;
• Assessing the extent of compliance with the laws and regulations considered to have a direct material effect on the Trust’s financial statements and the operations of the Trust through enquiry and inspection;
• Reviewing financial statement disclosures and testing to supporting documentation to assess compliance with applicable laws and regulations;
• Performing audit work over the risk of management bias and override of controls, including testing of high-risk journal entries and other adjustments for appropriateness, evaluating the rationale of any significant transactions outside the normal course of business and reviewing key accounting estimates including land and building valuation, for indicators of potential bias;
• Other audit procedures responsive to the risk of fraud, non-compliance with laws and regulation or irregularity including testing the accuracy and occurrence of variable income and assessing the completeness of non-pay expenditure; and
• Assessing whether the engagement team collectively had the appropriate competence and capabilities to identify or recognise non-compliance with laws and regulations. We concluded that more experienced audit team members needed to be allocated to perform work on the significant risks identified.
We also communicated potential non-compliance with laws and regulations, including potential fraud risks to all engagement team members, and remained alert to any indications of fraud or non-compliance with laws and regulations throughout the audit.
Because of the inherent limitations of an audit, there is a risk that we will not detect all irregularities, including those leading to a material misstatement in the financial statements or non-compliance with regulations. This risk increases the more that compliance with a law or regulation is removed from the events and transactions reflected in the financial statements, as we will be less likely to become aware of instances of non-compliance. The risk of not detecting a material misstatement resulting from fraud is higher than for one resulting from error, as fraud may involve collusion, forgery, intentional omissions, misrepresentations, or the override of internal control.
Report on other legal and regulatory matters
Reports
in the public interest or to the regulator
Under the Code of Audit Practice, we are required to report to you if:
• we issue a report in the public interest under Section 24, Schedule 7(1)(1) of the Local Audit and Accountability Act 2014;
• we make a written recommendation to the Trust under Section 24, Schedule 7(2) of the Local Audit and Accountability Act 2014; or
• we refer a matter to the Secretary of State and NHS England under Section 30, Schedule 13(13) of the Local Audit and Accountability Act 2014, because we have reason to believe that the Trust, or an officer of the Trust, is about to make, or has made, a decision which involves or would involve the incurring of unlawful expenditure, or is about to take, or has begun to take a course of action which, if followed to its conclusion, would be unlawful and likely to cause a loss or deficiency.
We have nothing to report in respect of the above matters.
Report on the Trust’s arrangements for securing economy, efficiency and effectiveness in its use of resources
Under the Code of Audit Practice, we are required to report to you if, in our opinion, we have not been able to satisfy ourselves that the Trust has made proper arrangements for securing economy, efficiency and effectiveness in its use of resources for the year ended 31 March 2025.
We have nothing to report in this respect.
Responsibilities of the Accountable Officer
As explained in the Statement of the chief executive’s responsibilities as the accountable officer of the Trust, The Chief Executive, is responsible for putting in place proper arrangements for securing economy, efficiency and effectiveness in the use of the Trust’s resources.
Auditor’s responsibilities for the review of the Trust’s arrangements for securing economy, efficiency and effectiveness in its use of resources
We are required under Section 21(2A)(c) of the Local Audit and Accountability Act 2014 to be satisfied that the Trust has made proper arrangements for securing economy, efficiency and effectiveness in its use of resources. We are not required to consider, nor have we considered, whether all aspects of the Trust’s arrangements for securing economy, efficiency and effectiveness in its use of resources are operating effectively.
We have undertaken our review in accordance with the Code of Audit Practice, having regard to the guidance issued by the Comptroller and Auditor General in November 2024. This guidance sets out the arrangements that fall within the scope of ‘proper arrangements.’ When reporting on these arrangements, the Code of Audit Practice requires auditors to structure their commentary on arrangements under three specified reporting criteria:
• Financial sustainability: how the Trust plans and manages its resources to ensure it can continue to deliver its services;
• Governance: how the Trust ensures that it makes informed decisions and properly manages its risks; and
• Improving economy, efficiency and effectiveness: how the Trust uses information about its costs and performance to improve the way it manages and delivers its services.
We have documented our understanding of the arrangements the Trust has in place for each of these three specified reporting criteria, gathering sufficient evidence to support our risk assessment and commentary which will be included in our Auditor’s Annual Report. In undertaking our work, we have considered whether there is evidence to suggest that there are significant weaknesses in arrangements.
Delayed certificate
We cannot formally conclude the audit and issue an audit certificate for Hertfordshire Community NHS Trust for the year ended 31 March 2025 in accordance with the requirements of the Local Audit and Accountability Act 2014 and the Code of Audit Practice (the “Code”) until we have completed all our responsibilities mandated by the Code.
Our Consolidated NHS Provider Accounts (CPA) group audit work for the period ended 31 December 2024, as mandated under Part 1 of the National Audit Office’s group instructions, is currently outstanding and the National Audit Office has yet to confirm whether this audit will be selected as an additional sample for their group audit testing.
We are satisfied that this work does not have a material effect on the financial statements, or on our conclusion on the Trust’s arrangements for securing economy, efficiency, and effectiveness in its use of resources for the year ended 31 March 2025.
Use of our report
This report is made solely to the directors of the Trust, as a body, in accordance with Section 21 of the Local Audit and Accountability Act 2014. Our audit work has been undertaken so that we might state to the Trust’s directors those matters we are required to state to them in an auditor’s report and for no other purpose. To the fullest extent permitted by law, we do not accept or assume responsibility to anyone other than the Trust and the directors of the Trust, as a body, for our audit work, for this report, or for the opinions we have formed.
Paul Grady
Paul Grady, Key Audit Partner for
and on behalf of
London
17 June 2025
Azets Audit Services, Local Auditor
Hertfordshire Community NHS Trust
Annual accounts for the year ended 31 March 2025
Statement of Comprehensive Income
/ (deficit) on
/ (loss)
In assessing and reporting its financial performance against its control total, the Trust makes adjustments to its reported surplus or deficit, above, to take into account the impact of certain technical accounting entries. This adjusted figure is shown below.
Statement of Financial Position
The notes on pages 137 to 176 form part of these accounts.
Elliot Howard-Jones Chief Executive
16 June 2025
Statement of Changes in Taxpayers Equity for the year ended 31 March 2025
Taxpayers' and others' equity at 1 April 2024 - brought forward
Surplus/(deficit) for the year
Transfer from revaluation reserve to income and expenditure reserve for impairments arising from consumption of economic benefits Impairments Revaluations
Public dividend capital received Other reserve movements
Taxpayers' and others' equity at 31 March 2025
Statement of Changes in Taxpayers Equity for the year ended 31 March 2024
at 1 April 2023 -
and others' equity at 31 March 2024
Information on reserves
Public dividend capital
Public dividend capital (PDC) is a type of public sector equity finance based on the excess of assets over liabilities at the time of establishment of the predecessor NHS organisation. Additional PDC may also be issued to trusts by the Department of Health and Social Care. A charge, reflecting the cost of capital utilised by the trust, is payable to the Department of Health as the public dividend capital dividend.
Revaluation reserve
Increases in asset values arising from revaluations are recognised in the revaluation reserve, except where, and to the extent that, they reverse impairments previously recognised in operating expenses, in which case they are recognised in operating income. Subsequent downward movements in asset valuations are charged to the revaluation reserve to the extent that a previous gain was recognised unless the downward movement represents a clear consumption of economic benefit or a reduction in service potential.
Other reserves
The balance of this reserve represents the opening balance for the Hertfordshire Community NHS Trust at its establishment in November 2010; the balances were transferred from Hertfordshire PCT.
Income and expenditure reserve
The balance of this reserve is the accumulated surpluses and deficits of the trust.
Statement of Cash Flows
Note 1 Accounting policies and other information
Note 1.1 Basis of preparation
The Department of Health and Social Care has directed that the financial statements of the Trust shall meet the accounting requirements of the Department of Health and Social Care Group Accounting Manual (GAM), which shall be agreed with HM Treasury. Consequently, the following financial statements have been prepared in accordance with the GAM 2024/25 issued by the Department of Health and Social Care. The accounting policies contained in the GAM follow International Financial Reporting Standards to the extent that they are meaningful and appropriate to the NHS, as determined by HM Treasury, which is advised by the Financial Reporting Advisory Board. Where the GAM permits a choice of accounting policy, the accounting policy that is judged to be most appropriate to the particular circumstances of the Trust for the purpose of giving a true and fair view has been selected. The particular policies adopted are described below. These have been applied consistently in dealing with items considered material in relation to the accounts
Accounting convention
These accounts have been prepared under the historical cost convention modified to account for the revaluation of property, plant and equipment, intangible assets, inventories and certain financial assets and financial liabilities.
Note 1.2 Going concern
These accounts have been prepared on a going concern basis. The financial reporting framework applicable to NHS bodies, derived from the HM Treasury Financial Reporting Manual, defines that the anticipated continued provision of the entity’s services in the public sector is normally sufficient evidence of going concern. The directors have a reasonable expectation that this will continue to be the case.
Financial risk, including the consideration of future risks and the Trust's historical ability to meet these challenges. The emergency financial arrangements implemented within the NHS in response to the pandemic were replaced by the return to more normal contract arrangements in the 2023/24 and 2024/25 financial years. This means that the Trust and its commissioners have agreed contract values for the 2025/26 financial year.
Operational risk, this included assessment of risks arising from loss of key management and key staff without replacement, governance risk ratings, Care Quality standards and adaptation to fundamental changes in technology.
Other risks considered included assessment of serious non-compliance with regulatory or statutory requirements and any pending legal or regulatory proceedings against the trust.
Given the above, the Trust Management have assumed that sufficient income will be received during the 2025/26 financial year to continue its operations. Management have also continued to review the Trust's future cash flows, its current liabilities and assets and as a non-trading entity in the public sector to assure itself that there is full expectation that the services provided by the Trust will continue in the future.
The Trust management is satisfied that there are no operational risks or other risks that might cast significant doubt on going concern.
The Trust's management has assessed that the Trust is a going concern in accordance with the GAM 2024/25 issued by DHSC.
Note 1.3 Revenue from contracts with customers
Where income is derived from contracts with customers, it is accounted for under IFRS 15. The GAM expands the definition of a contract to include legislation and regulations which enables an entity to receive cash or another financial asset that is not classified as a tax by the Office of National Statistics (ONS).
Revenue in respect of goods/services provided is recognised when (or as) performance obligations are satisfied by transferring promised goods/services to the customer and is measured at the amount of the transaction price allocated to those performance obligations. At the year end, the Trust accrues income relating to performance obligations satisfied in that year. Where the Trust’s entitlement to consideration for those goods or services is unconditional a contract receivable will be recognised. Where entitlement to consideration is conditional on a further factor other than the passage of time, a contract asset will be recognised. Where consideration received or receivable relates to a performance obligation that is to be satisfied in a future period, the income is deferred and recognised as a contract liability.
Revenue from NHS contracts
The main source of income for the Trust is contracts with commissioners for health care services. Funding envelopes are set at an Integrated Care System (ICS) level. The majority of the Trust’s NHS income is earned from NHS commissioners under the NHS Payment Scheme (NHSPS). The NHSPS sets out rules to establish the amount payable to trusts for NHS-funded secondary healthcare.
Aligned payment and incentive contracts form the main payment mechanism under the NHSPS. API contracts contain both a fixed and variable element. Under the variable element, providers earn income for elective activity (both ordinary and day case), out-patient procedures, out-patient first attendances, diagnostic imaging and nuclear medicine, and chemotherapy delivery activity. The precise definition of these activities is given in the NHSPS. Income is earned at NHSPS prices based on actual activity. The fixed element includes income for all other services covered by the NHSPS assuming an agreed level of activity with ‘fixed’ in this context meaning not varying based on units of activity. Elements within this are accounted for as variable consideration under IFRS 15 as explained below.
Where the relationship with a particular integrated care board is expected to be a low volume of activity (annual value below £0.5m), an annual fixed payment is received by the provider as determined in the NHSPS documentation. Such income is classified as ‘other clinical income’ in these accounts.
Elective recovery funding provides additional funding to integrated care boards to fund the commissioning of elective services within their systems. Trusts do not directly earn elective recovery funding, instead earning income for actual activity performed under API contract arrangements as explained above. The level of activity delivered by the trust contributes to system performance and therefore the availability of funding to the trust’s commissioners.
NHS injury cost recovery scheme
The Trust receives income under the NHS injury cost recovery scheme, designed to reclaim the cost of treating injured individuals to whom personal injury compensation has subsequently been paid, for instance by an insurer. The Trust recognises the income when performance obligations are satisfied. In practical terms this means that treatment has been given, it receives notification from the Department of Work and Pension's Compensation Recovery Unit, has completed the NHS2 form and confirmed there are no discrepancies with the treatment. The income is measured at the agreed tariff for the treatments provided to the injured individual, less an allowance for unsuccessful compensation claims and doubtful debts in line with IFRS 9 requirements of measuring expected credit losses over the lifetime of the asset.
Note 1.4
Other forms of income
Grants and donations
Government grants are grants from government bodies other than income from commissioners or trusts for the provision of services. Where a grant is used to fund revenue expenditure it is taken to the Statement of Comprehensive Income to match that expenditure. Where the grants is used to fund capital expenditure, it is credited to the Statement of Comprehensive Income once conditions attached to the grant have been met. Donations are treated in the same way as government grants.
Apprenticeship service income
The value of the benefit received when accessing funds from the Government's apprenticeship service is recognised as income at the point of receipt of the training service. Where these funds are paid directly to an accredited training provider from the Trust's apprenticeship service account held by the Department for Education, the corresponding notional expense is also recognised at the point of recognition for the benefit.
Note 1.5
Expenditure on employee benefits
Short-term employee benefits
Salaries, wages and employment-related payments such as social security costs and the apprenticeship levy are recognised in the period in which the service is received from employees. The cost of annual leave entitlement earned but not taken by employees at the end of the period is recognised in the financial statements to the extent that employees are permitted to carry-forward leave into the following period.
Pension costs
NHS Pension Scheme
Past and present employees are covered by the provisions of the two NHS Pension Schemes. Both schemes are unfunded, defined benefit schemes that cover NHS employers, general practices and other bodies, allowed under the direction of Secretary of State for Health and Social Care in England and Wales. The scheme is not designed in a way that would enable employers to identify their share of the underlying scheme assets and liabilities. Therefore, the scheme is accounted for as though it is a defined contribution scheme: the cost to the trust is taken as equal to the employer's pension contributions payable to the scheme for the accounting period. The contributions are charged to operating expenses as and when they become due.
Additional pension liabilities arising from early retirements are not funded by the scheme except where the retirement is due to ill-health. The full amount of the liability for the additional costs is charged to the operating expenses at the time the trust commits itself to the retirement, regardless of the method of payment.
Note
1.6 Expenditure on other goods and services
Expenditure on goods and services is recognised when, and to the extent that they have been received, and is measured at the fair value of those goods and services. Expenditure is recognised in operating expenses except where it results in the creation of a non-current asset such as property, plant and equipment.
Note
1.7 Discontinued operations
Discontinued operations occur where activities either cease without transfer to another entity, or transfer to an entity outside of the boundary of the Whole of Government Accounts, such as private or voluntary sectors. Such activities are accounted for in accordance with IFRS 5. Activities that are transferred to other bodies within the boundary of the Whole of Government Accounts are ‘machinery of government changes’ and treated as continuing operations.
Note 1.8 Property, plant and equipment
Recognition
Property, plant and equipment is capitalised where:
• it is held for use in delivering services or for administrative purposes
• it is probable that future economic benefits will flow to, or service potential be provided to, the Trust
• it is expected to be used for more than one financial year
• the cost of the item can be measured reliably
• the item has cost of at least £5,000, or
• collectively, a number of items have a cost of at least £5,000 and individually have cost of more than £250, where the assets are functionally interdependent, had broadly simultaneous purchase dates, are anticipated to have similar disposal dates and are under single managerial control.
Where a large asset, for example a building, includes a number of components with significantly different asset lives, eg, plant and equipment, then these components are treated as separate assets and depreciated over their own useful lives.
Subsequent expenditure
Subsequent expenditure relating to an item of property, plant and equipment is recognised as an increase in the carrying amount of the asset when it is probable that additional future economic benefits or service potential deriving from the cost incurred to replace a component of such item will flow to the enterprise and the cost of the item can be determined reliably. Where a component of an asset is replaced, the cost of the replacement is capitalised if it meets the criteria for recognition above. The carrying amount of the part replaced is de-recognised. Other expenditure that does not generate additional future economic benefits or service potential, such as repairs and maintenance, is charged to the Statement of Comprehensive Income in the period in which it is incurred.
Measurement
Valuation
All property, plant and equipment assets are measured initially at cost, representing the costs directly attributable to acquiring or constructing the asset and bringing it to the location and condition necessary for it to be capable of operating in the manner intended by management.
Assets are measured subsequently at valuation. Assets which are held for their service potential and are in use (ie operational assets used to deliver either front line services or back office functions) are measured at their current value in existing use. Assets that were most recently held for their service potential but are surplus with no plan to bring them back into use are measured at fair value where there are no restrictions on sale at the reporting date and where they do not meet the definitions of investment properties or assets held for sale.
Revaluations of property, plant and equipment are performed with sufficient regularity to ensure that carrying values are not materially different from those that would be determined at the end of the reporting period. Current values in existing use are determined as follows:
• Land and non-specialised buildings – market value for existing use
• Specialised buildings – depreciated replacement cost on a modern equivalent asset basis.
For specialised assets, current value in existing use is interpreted as the present value of the asset's remaining service potential, which is assumed to be at least equal to the cost of replacing that service potential. Specialised assets are therefore valued at their depreciated replacement cost (DRC) on a modern equivalent asset (MEA) basis. An MEA basis assumes that the asset will be replaced with a modern asset of equivalent capacity and meeting the location requirements of the services being provided. Assets held at depreciated replacement cost have been valued on an alternative site basis where this would meet the location requirements.
Properties in the course of construction for service or administration purposes are carried at cost, less any impairment loss. Cost includes professional fees Assets are revalued and depreciation commences when the assets are brought into use. IT equipment, transport equipment, furniture and fittings, and plant and machinery that are held for operational use are valued at depreciated historic cost where these assets have short useful lives or low values or both, as this is not considered to be materially different from current value in existing use.
Note 1.8 Property, plant and equipment (cont'd)
Depreciation
Items of property, plant and equipment are depreciated over their remaining useful lives in a manner consistent with the consumption of economic or service delivery benefits. Freehold land is considered to have an infinite life and is not depreciated. Lease holder works are recorded as furniture and fittings and depreciated over the life of the lease.
Otherwise, depreciation or amortisation is charged to write off the costs or valuation of property, plant and equipment and tangible non-current assets, less any residual value, on a straight line basis over their estimated useful lives. The estimated useful life of an asset is the period over which the NHS trust expects to obtain economic benefits or service potential from the asset. This is specific to the NHS trust and may be shorter than the physical life of the asset itself. Estimated useful lives and residual values are reviewed each year end, with the effect of any changes recognised on a prospective basis. Assets held under finance leases are depreciated over the shorter of the lease term and the estimated useful lives. Property, plant and equipment which has been reclassified as ‘held for sale’ cease to be depreciated upon the reclassification. Assets in the course of construction and residual interests in off-Statement of Financial Position PFI contract assets are not depreciated until the asset is brought into use or reverts to the trust, respectively.
Revaluation gains and losses
Revaluation gains are recognised in the revaluation reserve, except where, and to the extent that, they reverse a revaluation decrease that has previously been recognised in operating expenses, in which case they are recognised in operating expenditure.
Revaluation losses are charged to the revaluation reserve to the extent that there is an available balance for the asset concerned and thereafter are charged to operating expenses.
Gains and losses recognised in the revaluation reserve are reported in the Statement of Comprehensive Income as an item of ‘other comprehensive income’.
Impairments
In accordance with the GAM, impairments that arise from a clear consumption of economic benefits or of service potential in the asset are charged to operating expenses. A compensating transfer is made from the revaluation reserve to the income and expenditure reserve of an amount equal to the lower of (i) the impairment charged to operating expenses; and (ii) the balance in the revaluation reserve attributable to that asset before the impairment.
An impairment that arises from a clear consumption of economic benefit or of service potential is reversed when, and to the extent that, the circumstances that gave rise to the loss is reversed. Reversals are recognised in operating expenditure to the extent that the asset is restored to the carrying amount it would have had if the impairment had never been recognised. Any remaining reversal is recognised in the revaluation reserve. Where, at the time of the original impairment, a transfer was made from the revaluation reserve to the income and expenditure reserve, an amount is transferred back to the revaluation reserve when the impairment reversal is recognised.
Other impairments are treated as revaluation losses. Reversals of ‘other impairments’ are treated as revaluation gains.
De-recognition
Assets intended for disposal are reclassified as ‘held for sale’ once the criteria in IFRS 5 are met. The sale must be highly probable and the asset available for immediate sale in its present condition.
Following reclassification, the assets are measured at the lower of their existing carrying amount and their ‘fair value less costs to sell’. Depreciation ceases to be charged and the assets are not revalued, except where the 'fair value less costs to sell' falls below the carrying amount. Assets are de-recognised when all material sale contract conditions have been met.
Property, plant and equipment which is to be scrapped or demolished does not qualify for recognition as ‘held for sale’ and instead is retained as an operational asset and the asset’s useful life is adjusted. The asset is de-recognised when scrapping or demolition occurs.
Note 1.8 Property, plant and equipment
(cont'd)
Donated and grant funded assets
Donated and grant funded property, plant and equipment assets are capitalised at their fair value on receipt. The donation/grant is credited to income at the same time, unless the donor has imposed a condition that the future economic benefits embodied in the grant are to be consumed in a manner specified by the donor, in which case, the donation/grant is deferred within liabilities and is carried forward to future financial years to the extent that the condition has not yet been met.
The donated and grant funded assets are subsequently accounted for in the same manner as other items of property, plant and equipment.
Useful lives of property, plant and equipment
Useful lives reflect the total life of an asset and not the remaining life of an asset. The range of useful lives are shown in the table below:
Note 1.9 Intangible assets
Recognition
Intangible assets are non-monetary assets without physical substance controlled by the Trust. They are capable of being sold separately from the rest of the trust’s business or arise from contractual or other legal rights. Intangible assets are recognised only where it is probable that future economic benefits will flow to, or service potential be provided to, the trust and where the cost of the asset can be measured reliably.
Internally generated intangible assets
Internally generated goodwill, brands, mastheads, publishing titles, customer lists and similar items are not capitalised as intangible assets.
Expenditure on research is not capitalised. Expenditure on development is capitalised where it meets the requirements set out in IAS 38.
Software
Software which is integral to the operation of hardware, eg an operating system, is capitalised as part of the relevant item of property, plant and equipment. Software which is not integral to the operation of hardware, e.g. application software, is capitalised as an intangible asset where it meets recognition criteria.
Measurement
Intangible assets are recognised initially at cost, comprising all directly attributable costs needed to create, produce and prepare the asset to the point that it is capable of operating in the manner intended by management.
Subsequently intangible assets are measured at current value in existing use. Where no active market exists, intangible assets are valued at the lower of depreciated replacement cost and the value in use where the asset is income generating. Revaluations gains and losses and impairments are treated in the same manner as for property, plant and equipment. An intangible asset which is surplus with no plan to bring it back into use is valued at fair value where there are no restrictions on sale at the reporting date and where they do not meet the definitions of investment properties or assets held for sale.
Intangible assets held for sale are measured at the lower of their carrying amount or fair value less costs to sell.
Note
1.9 Intangible assets
Amortisation
Intangible assets are amortised over their expected useful lives in a manner consistent with the consumption of economic or service delivery benefits.
Useful lives of intangible assets
Useful lives reflect the total life of an asset and not the remaining life of an asset. The range of useful lives are shown in the table below:
Note 1.10 Inventories
Between 2020/21 and 2023/24 the Trust received inventories including personal protective equipment from the Department of Health and Social Care at nil cost. In line with the GAM and applying the principles of the IFRS Conceptual Framework, the Trust has accounted for the receipt of these inventories at a deemed cost, reflecting the best available approximation of an imputed market value for the transaction based on the cost of acquisition by the Department. Distribution of inventories by the Department ceased in March 2024.
Note 1.11 Cash and cash equivalents
Cash is cash in hand and deposits with any financial institution repayable without penalty on notice of not more than 24 hours. Cash equivalents are investments that mature in 3 months or less from the date of acquisition and that are readily convertible to known amounts of cash with insignificant risk of change in value.
In the Statement of Cash Flows, cash and cash equivalents are shown net of bank overdrafts that are repayable on demand and that form an integral part of the Trust’s cash management. Cash, bank and overdraft balances are recorded at current values.
Note 1.12
Recognition
assets and financial liabilities
Financial assets and financial liabilities arise where the Trust is party to the contractual provisions of a financial instrument, and as a result has a legal right to receive or a legal obligation to pay cash or another financial instrument. The GAM expands the definition of a contract to include legislation and regulations which give rise to arrangements that in all other respects would be a financial instrument and do not give rise to transactions classified as a tax by ONS.
This includes the purchase or sale of non-financial items (such as goods or services), which are entered into in accordance with the Trust’s normal purchase, sale or usage requirements and are recognised when, and to the extent which, performance occurs, ie, when receipt or delivery of the goods or services is made.
Classification and measurement
Financial assets and financial liabilities are initially measured at fair value plus or minus directly attributable transaction costs except where the asset or liability is not measured at fair value through income and expenditure. Fair value is taken as the transaction price or otherwise determined by reference to quoted market prices or valuation techniques.
Financial assets or financial liabilities in respect of assets acquired or disposed of through leasing arrangements are recognised and measured in accordance with the accounting policy for leases described below.
Financial assets are classified as subsequently measured at amortised cost Financial liabilities classified as subsequently measured at amortised cost
Financial assets and financial liabilities at amortised cost
Financial assets and financial liabilities at amortised cost are those held with the objective of collecting contractual cash flows and where cash flows are solely payments of principal and interest. This includes cash equivalents, contract and other receivables, trade and other payables, rights and obligations under lease arrangements and loans receivable and payable.
After initial recognition, these financial assets and financial liabilities are measured at amortised cost using the effective interest method less any impairment (for financial assets). The effective interest rate is the rate that exactly discounts estimated future cash payments or receipts through the expected life of the financial asset or financial liability to the gross carrying amount of a financial asset or to the amortised cost of a financial liability.
Interest revenue or expense is calculated by applying the effective interest rate to the gross carrying amount of a financial asset or amortised cost of a financial liability and recognised in the Statement of Comprehensive Income and a financing income or expense.
Impairment of financial assets
For all financial assets measured at amortised cost including lease receivables, contract receivables and contract assets, the Trust recognises an allowance for expected credit losses.
The Trust adopts the simplified approach to impairment for contract and other receivables, contract assets and lease receivables, measuring expected losses as at an amount equal to lifetime expected losses. For other financial assets, the loss allowance is initially measured at an amount equal to 12-month expected credit losses (stage 1) and subsequently at an amount equal to lifetime expected credit losses if the credit risk assessed for the financial asset significantly increases (stage 2).
For financial assets that have become credit impaired since initial recognition (stage 3), expected credit losses at the reporting date are measured as the difference between the asset’s gross carrying amount and the present value of estimated future cash flows discounted at the financial asset’s original effective interest rate.
Expected losses are charged to operating expenditure within the Statement of Comprehensive Income and reduce the net carrying value of the financial asset in the Statement of Financial Position.
Derecognition
Financial assets are de-recognised when the contractual rights to receive cash flows from the assets have expired or the Trust has transferred substantially all the risks and rewards of ownership.
Financial liabilities are de-recognised when the obligation is discharged, cancelled or expires.
Note 1.13 Leases
A lease is a contract or part of a contract that conveys the right to use an asset for a period of time in exchange for consideration. An adaptation of the relevant accounting standard by HM Treasury for the public sector means that for NHS bodies, this includes lease-like arrangements with other public sector entities that do not take the legal form of a contract. It also includes peppercorn leases where consideration paid is nil or nominal (significantly below market value) but in all other respects meet the definition of a lease. The trust does not apply lease accounting to new contracts for the use of intangible assets.
The Trust determines the term of the lease term with reference to the non-cancellable period and any options to extend or terminate the lease which the Trust is reasonably certain to exercise.
The Trust as a lessee
Initial recognition and measurement
At the commencement date of the lease, being when the asset is made available for use, the Trust recognises a right of use asset and a lease liability.
The right of use asset is recognised at cost comprising the lease liability, any lease payments made before or at commencement, any direct costs incurred by the lessee, less any cash lease incentives received. It also includes any estimate of costs to be incurred restoring the site or underlying asset on completion of the lease term.
The lease liability is initially measured at the present value of future lease payments discounted at the interest rate implicit in the lease. Lease payments includes fixed lease payments, variable lease payments dependent on an index or rate and amounts payable under residual value guarantees. It also includes amounts payable for purchase options and termination penalties where these options are reasonably certain to be exercised.
Where an implicit rate cannot be readily determined, the Trust’s incremental borrowing rate is applied. This rate is determined by HM Treasury annually for each calendar year. A nominal rate of 4.72% applied to new leases commencing in 2024 and 4.81% to new leases commencing in 2025.
The Trust does not apply the above recognition requirements to leases with a term of 12 months or less or to leases where the value of the underlying asset is below £5,000, excluding any irrecoverable VAT. Lease payments associated with these leases are expensed on a straight-line basis over the lease term. Irrecoverable VAT on lease payments is expensed as it falls due.
Subsequent measurement
As required by a HM Treasury interpretation of the accounting standard for the public sector, the Trust employs a revaluation model for subsequent measurement of right of use assets, unless the cost model is considered to be an appropriate proxy for current value in existing use or fair value, in line with the accounting policy for owned assets. Where consideration exchanged is identified as significantly below market value, the cost model is not considered to be an appropriate proxy for the value of the right of use asset.
The Trust subsequently measures the lease liability by increasing the carrying amount for interest arising which is also charged to expenditure as a finance cost and reducing the carrying amount for lease payments made. The liability is also remeasured for changes in assessments impacting the lease term, lease modifications or to reflect actual changes in lease payments. Such remeasurements are also reflected in the cost of the right of use asset. Where there is a change in the lease term or option to purchase the underlying asset, an updated discount rate is applied to the remaining lease payments.
The Trust as a lessor
The Trust assesses each of its leases and classifies them as either a finance lease or an operating lease. Leases are classified as finance leases when substantially all the risks and rewards of ownership are transferred to the lessee. All other leases are classified as operating leases.
Where the Trust is an intermediate lessor, classification of the sublease is determined with reference to the right of use asset arising from the headlease.
Finance leases
Amounts due from lessees under finance leases are recorded as receivables at the amount of the Trust’s net investment in the leases. Finance lease income is allocated to accounting periods to reflect a constant periodic rate of return on the Trust’s net investment outstanding in respect of the leases.
Operating leases
Income from operating leases is recognised on a straight-line basis or another systematic basis over the term of the lease. Initial direct costs incurred in negotiating and arranging an operating lease are added to the carrying amount of the leased asset and recognised as an expense on a straight-line basis over the lease term.
Note
1.14 Provisions
The Trust recognises a provision where it has a present legal or constructive obligation of uncertain timing or amount; for which it is probable that there will be a future outflow of cash or other resources; and a reliable estimate can be made of the amount. The amount recognised in the Statement of Financial Position is the best estimate of the resources required to settle the obligation. Where the effect of the time value of money is significant, the estimated risk adjusted cash flows are discounted using HM Treasury's discount rates effective from 31 March 2025:
HM Treasury provides discount rates for general provisions on a nominal rate basis. Expected future cash flows are therefore adjusted for the impact of inflation before discounting using nominal rates. The following inflation rates are set by HM Treasury, effective from 31 March 2025:
Early retirement provisions and injury benefit provisions both use the HM Treasury's post-employment benefits discount rate of 2.40% in real terms (prior year: 2.45%).
Clinical negligence costs
NHS Resolution operates a risk pooling scheme under which the trust pays an annual contribution to NHS Resolution, which, in return, settles all clinical negligence claims. Although NHS Resolution is administratively responsible for all clinical negligence cases, the legal liability remains with the Trust. The total value of clinical negligence provisions carried by NHS Resolution on behalf of the trust is disclosed at Note 21.2 but is not recognised in the Trust’s accounts.
Non-clinical risk pooling
The trust participates in the Property Expenses Scheme and the Liabilities to Third Parties Scheme. Both are risk pooling schemes under which the trust pays an annual contribution to NHS Resolution and in return receives assistance with the costs of claims arising. The annual membership contributions, and any excesses payable in respect of particular claims are charged to operating expenses when the liability arises.
Note 1.15 Contingencies
Contingent assets (that is, assets arising from past events whose existence will only be confirmed by one or more future events not wholly within the entity’s control) are not recognised as assets but are disclosed in Note 22 where an inflow of economic benefits is probable.
Contingent liabilities are not recognised, but are disclosed in Note 22, unless the probability of a transfer of economic benefits is remote.
Contingent liabilities are defined as:
• possible obligations arising from past events whose existence will be confirmed only by the occurrence of one or more uncertain future events not wholly within the entity’s control; or
• present obligations arising from past events but for which it is not probable that a transfer of economic benefits will arise or for which the amount of the obligation cannot be measured with sufficient reliability.
Note 1.16 Public dividend capital
Public dividend capital (PDC) is a type of public sector equity finance based on the excess of assets over liabilities at the time of establishment of the predecessor NHS organisation. HM Treasury has determined that PDC is not a financial instrument within the meaning of IAS 32.
The Secretary of State can issue new PDC to, and require repayments of PDC from, the Trust. PDC is recorded at the value received.
A charge, reflecting the cost of capital utilised by the Trust, is payable as public dividend capital dividend. The charge is calculated at the rate set by HM Treasury (currently 3.5%) on the average relevant net assets of the trust during the financial year. Relevant net assets are calculated as the value of all assets less the value of all liabilities, with certain additions and deductions as defined by the Department of Health and Social Care. This policy is available at https://www.gov.uk/government/publications/guidance-on-financing-available-to-nhs-trustsand-foundation-trusts.
In accordance with the requirements laid down by the Department of Health and Social Care (as the issuer of PDC), the dividend for the year is calculated on the actual average relevant net assets as set out in the “pre-audit” version of the annual accounts. The dividend calculated is not revised should any adjustment to net assets occur as a result the audit of the annual accounts.
Note 1.17 Value added tax
Most of the activities of the trust are outside the scope of VAT and, in general, output tax does not apply and input tax on purchases is not recoverable. Irrecoverable VAT is charged to the relevant expenditure category or included in the capitalised purchase cost of fixed assets. Where output tax is charged or input VAT is recoverable, the amounts are stated net of VAT.
Note 1.18 Climate change levy
Expenditure on the climate change levy is recognised in the Statement of Comprehensive Income as incurred, based on the prevailing chargeable rates for energy consumption.
Note 1.19
Third party assets
Assets belonging to third parties in which the Trust has no beneficial interest (such as money held on behalf of patients) are not recognised in the accounts. However, they are disclosed in a separate note to the accounts in accordance with the requirements of HM Treasury’s FReM
Note 1.20
Losses and special payments
Losses and special payments are items that Parliament would not have contemplated when it agreed funds for the health service or passed legislation. By their nature they are items that ideally should not arise. They are therefore subject to special control procedures compared with the generality of payments. They are divided into different categories, which govern the way that individual cases are handled. Losses and special payments are charged to the relevant functional headings in expenditure on an accruals basis.
The losses and special payments note is compiled directly from the losses and compensations register which reports on an accrual basis with the exception of provisions for future losses.
Note 1.21
Gifts
Gifts are items that are voluntarily donated, with no preconditions and without the expectation of any return. Gifts include all transactions economically equivalent to free and unremunerated transfers, such as the loan of an asset for its expected useful life, and the sale or lease of assets at below market value.
Note 1.22 Early adoption of standards, amendments and interpretations
No new accounting standards or revisions to existing standards have been early adopted in 2024/25.
Note 1.23 Standards, amendments and interpretations in issue but not yet effective or adopted
The DHSC GAM does not require the following IFRS Standards to be applied in 2024/25:
IFRS 17 Insurance Contracts – The Standard is effective for accounting periods beginning on or after 1 January 2023. IFRS 17 has been adopted by the FReM from 1 April 2025. Adoption of the Standard for NHS bodies will therefore be in 2025/26. The Standard revises the accounting for insurance contracts for the issuers of insurance.
IFRS 18 Presentation and Disclosure in Financial Statements - The Standard is effective for accounting periods beginning on or after 1 January 2027. The Standard is not yet UK endorsed and not yet adopted by the FReM. Early adoption is not permitted. The expected impact of applying the standard in future periods has not yet been assessed.
IFRS 19 Subsidiaries without Public Accountability: Disclosures - The Standard is effective for accounting periods beginning on or after 1 January 2027. The Standard is not yet UK endorsed and not yet adopted by the FReM. Early adoption is not permitted. The expected impact of applying the standard in future periods has not yet been assessed.
Changes to non-investment asset valuation – Following a thematic review of non-current asset valuations for financial reporting in the public sector, HM Treasury has made a number of changes to valuation frequency, valuation methodology and classification which are effective in the public sector from 1 April 2025 with a 5 year transition period. NHS bodies are adopting these changes to an alternative timeline.
Changes to subsequent measurement of intangible assets and PPE classification / terminology to be implemented for NHS bodies from 1 April 2025:
•Withdrawal of the revaluation model for intangible assets. Carrying values of existing intangible assets measured under a previous revaluation will be taken forward as deemed historic cost.
•Removal of the distinction between specialised and non-specialised assets held for their service potential. Assets will be classified according to whether they are held for their operational capacity.
Changes to valuation cycles and methodology to be implemented for NHS bodies in later periods:
•A mandated quinquennial revaluation frequency (or rolling programme) supplemented by annual indexation in the intervening years.
•Removal of the alternative site assumption for buildings valued at depreciated replacement cost on a modern equivalent asset basis. The approach for land has not yet been finalised by HM Treasury.
Note 1.24 Critical judgements in applying accounting policies
The following are the judgements, apart from those involving estimations (see below) that management has made in the process of applying the trust accounting policies and that have the most significant effect on the amounts recognised in the financial statements:
Items of property, plant and equipment are depreciated over their remaining useful lives in a manner consistent with the consumption of economic or service delivery benefits. Freehold land is considered to have an infinite life and is not depreciated. Lease holder works are recorded as Furniture and Fittings and depreciated over the life of the lease.
Property, plant and equipment which has been reclassified as ‘held for sale’ cease to be depreciated upon the reclassification. Assets in the course of construction are not depreciated until the asset is brought into use or reverts to the trust, respectively.
The cost measurement model outlined in IFRS16 - Leases will be an approximate proxy for value in existing use or fair value for the Trust's leased properties.
Note 1.25 Sources of estimation uncertainty
The following are assumptions about the future and other major sources of estimation uncertainty that have a significant risk of resulting in a material adjustment to the carrying amounts of assets and liabilities within the next financial year:
Asset valuation
The total balance of Property, Plant and Equipment as at 31 March 2025 is £51m. Where non-estate assets are of low value and/or have short useful economic lives, such as operational equipment, they are carried at depreciated historical cost (cost less any accumulated depreciation) as this is not considered to be materially different from fair value. The lives of equipment assets are estimated using historical experience of similar equipment lives with reference to national guidance and consideration of the pace of technological change. The value and remaining useful lives of estate assets are estimated by the Trust’s valuer, Cushman & Wakefield. Valuations are carried out five-yearly, or more often if market conditions are subject to significant fluctuations, with interim desktop valuations and the use of indices. Valuations are performed in accordance with the Royal Institute of Chartered Surveyors’ RICS Valuation – Global Standards ('Red Book Global Standards') and other relevant RICS guidance notes, primarily on the basis of depreciated replacement cost for specialised operational property and existing use value for non-specialised operational property. In particular, land and building assets are valued as a single combined hospital facility (‘single alternative site model’), as described in the previous section. The composition of this alternative replacement model requires the operation of significant levels of professional estimation by the valuer.
The valuer has highlighted a number of assumptions that have been made in carrying out the valuations. These include environmental matters, physical state of the properties and statutory and planning assumption. It was confirmed that, at the date of the valuation, 31 March 2025, enough evidence from property markets existed to ensure that the valuation was not reported as being subject to ‘material valuation uncertainty’ as defined by VPS 3 and VPGA 10 of the RICS Valuation – Global Standards. The valuation was based on a RICS Building Cost Information Service All-in Tender Price Index (BCIS TPI) published on 31 March 2025 and no significant correction to this is anticipated. The Trust’s valuation also depends on the BCIS Location Factor applied, and an estimation of external / economic obsolescence levels.
Because the Trust undertakes annual revaluations of estate assets, estimation uncertainty relating to asset lives and depreciation does not present significant risk of causing material adjustments. In addition, any impact on PDC dividend will not be material, so there are no cash implications to valuation. However, as in previous years, the Trust’s reliance on valuation methods does present a risk of causing a material adjustment to the carrying amount of non-current assets’.
Note 2 Operating Segments
The Trust engages in its activities as a single operating segment i.e. the provision of healthcare. The main source of revenue for the Trust is from commissioners of healthcare services which are principally ICBs and NHS England. The Department of Health has deemed that as ICBs and NHS England are under common control they are classed as a single customer for the purposes of segmental analysis.
Note 3 Operating income from patient care activities
All income from patient care activities relates to contract income recognised in line with accounting policy 1.3
Note 3.1
*Aligned payment and incentive contracts are the main form of contracting between NHS providers and their commissioners. More information can be found in the 2023/25 NHS Payment Scheme documentation. https://www.england.nhs.uk/pay-syst/nhs-payment-scheme/
**Increases to the employer contribution rate for NHS pensions since 1 April 2019 have been funded by NHS England. NHS providers continue to pay at the former rate of 14.3% with the additional amount being paid over by NHS England on providers' behalf. The full cost of employer contributions (23.7%, 2023/24: 20.6%) and related NHS England funding (9.4%, 2023/24: 6.3%) have been recognised in these accounts.
***Additional funding was made available directly to providers by NHS England in 2024/25 and 2023/24 for implementing the backdated element of pay awards where government offers were finalised after the end of the financial year. NHS Payment Scheme prices and API contracts are updated for the weighted uplift in in-year pay costs when awards are finalised.
Note 3.2 Income from patient care activities (by source)
Note 4 Other operating income
Note 4.1 Additional information on contract revenue (IFRS 15) recognised in the period
Revenue recognised in the reporting period that was included in within contract liabilities at the previous period end
Note 5 Operating leases - Hertfordshire Community NHS Trust as lessor
This note discloses income generated in operating lease agreements where Hertfordshire Community NHS Trust is the lessor. The Trust has applied IFRS 16 to account for lease arrangements from 1 April 2022
Note 5.1 Operating lease income
Note 5.2 Future lease receipts
Note 6.1 Operating expenses
Note 6.2 Limitation on auditor's liability
The limitation on auditor's liability for external audit work is £1,000k (2023/24: £1,000k).
Note 7 Impairment of assets
/
Impairments relating to Changes in Market Price and those Charged to the Revaluation Reserve relate to the valuation carried out on the Trust's Property, Plant and Equipment. This reflects the movements in the 'Fair Value' due to changes in property prices. Further information is contained within Note 14.1
Note 8 Employee benefits
Note 8.1 Retirements due to ill-health
During 2024/25 there were 2 early retirements from the trust agreed on the grounds of ill-health (1 in the year ended 31 March 2024). The estimated additional pension liabilities of these ill-health retirements is £229k (£222k in 2023/24).
These estimated costs are calculated on an average basis and will be borne by the NHS Pension Scheme.
Note 9 Pension costs
Past and present employees are covered by the provisions of the NHS Pension Schemes. Details of the benefits payable and rules of the schemes can be found on the NHS Pensions website at www.nhsbsa.nhs.uk/pensions. Both the 1995/2008 and 2015 schemes are accounted for, and the scheme liability valued, as a single combined scheme. Both are unfunded defined benefit schemes that cover NHS employers, GP practices and other bodies, allowed under the direction of the Secretary of State for Health and Social Care in England and Wales. They are not designed to be run in a way that would enable NHS bodies to identify their share of the underlying scheme assets and liabilities. Therefore, each scheme is accounted for as if it were a defined contribution scheme: the cost to the NHS body of participating in each scheme is taken as equal to the contributions payable to that scheme for the accounting period.
In order that the defined benefit obligations recognised in the financial statements do not differ materially from those that would be determined at the reporting date by a formal actuarial valuation, the FReM requires that “the period between formal valuations shall be four years, with approximate assessments in intervening years”. An outline of these follows:
a) Accounting valuation
A valuation of scheme liability is carried out annually by the scheme actuary (currently the Government Actuary’s Department) as at the end of the reporting period. This utilises an actuarial assessment for the previous accounting period in conjunction with updated membership and financial data for the current reporting period and is accepted as providing suitably robust figures for financial reporting purposes. The valuation of the scheme liability as at 31 March 2025, is based on valuation data as at 31 March 2023, updated to 31 March 2025 with summary global member and accounting data. In undertaking this actuarial assessment, the methodology prescribed in IAS 19, relevant FReM interpretations, and the discount rate prescribed by HM Treasury have also been used.
The latest assessment of the liabilities of the scheme is contained in the Statement by the Actuary, which forms part of the annual NHS Pension Scheme Annual Report and Accounts. These accounts can be viewed on the NHS Pensions website and are published annually. Copies can also be obtained from The Stationery Office.
b)
Full actuarial (funding) valuation
The purpose of this valuation is to assess the level of liability in respect of the benefits due under the schemes (considering recent demographic experience), and to recommend the contribution rate payable by employers.
The latest actuarial valuation undertaken for the NHS Pension Scheme was completed as at 31 March 2020. The results of this valuation set the employer contribution rate payable from 1 April 2024 to 23.7% of pensionable pay. The core cost cap cost of the scheme was calculated to be outside of the 3% cost cap corridor as at 31 March 2020. However, when the wider economic situation was taken into account through the economic cost cap cost of the scheme, the cost cap corridor was not similarly breached. As a result, there was no impact on the member benefit structure or contribution rates.
The 2024 actuarial valuation is currently being prepared and will be published before new contribution rates are implemented from April 2027
NEST Pension Scheme
Where staff are not eligible for, or choose to opt out of, the NHS Pensions Scheme, they are entitled to join the National Employment Savings Trust (NEST) scheme. NEST is a government backed defines contribution scheme set up to make sure that every employee can easily access a workplace pension scheme. The employer's contribution rate in 2024/25 was 3% (2023/24 3%)
Note 10 Finance income Finance
Note 11.1 Finance expenditure
Finance
Note 12.1 Intangible assets - 2024/25
Note 12.2 Intangible assets - 2023/24
Note 13.1 Property, plant and equipment - 2024/25
at 1 April 2024 - brought
Note 13.2 Property, plant and equipment - 2023/24
/ gross cost at 1 April 2023 - as previously
at 1 April 2023 - as
13.3
- 31 March 2025
Note 13.5 Property plant and equipment assets subject to an operating lease (Trust as a lessor) - 31 March 2025
Note 13.6 Property plant and equipment assets subject to an operating lease (Trust as a lessor) - 31 March 2024
Note 14 Revaluations of property, plant and equipment
A full recalculation of the Trust's land and buildings was carried out at 31 March 2025 by an independent, qualified valuer, using the Modern Equivalent Asset (MEA) methodology, in accordance with DH guidance and the NHS Group Accounting Manual.
The valuation was carried out by Cushman & Wakefield, 60 Grey Street, Newcastle upon Tyne, NE1 6FA. This was carried out in accordance with the Royal Institute of Chartered Surveyors (RICS) Valuation - Global Standards, which incorporate the International Valuation Standards (IVS) and the RICS UK National Supplement (the "RICS Red Book"), insofar as these terms are consistent with the agreed requirements of the Department of Health and Social Care, and HM Treasury.
The Existing Use Value (EUV) of the properties has predominantly been determined using the Depreciated Replacement Cost (DRC) approach. This methodology is appropriate due to the specialised nature of the assets, for which there is no active market and comparable transactions typically occur only as part of a broader entity sale. Where appropriate, for non-specialised properties, the EUV has been assessed based on market evidence from comparable transactions conducted on arm's length terms
The Existing Use Value is assessed in accordance with UK VPGA 6. Under these provisions "Existing Use Value" is defined as follows:
"The estimated amount for which a property should exchange on the valuation date between a willing buyer and a willing seller in an arm's length transaction after proper marketing and where the parties have acted knowledgeably, prudently and without compulsion, assuming that the buyer is granted vacant possession of all parts of the asset required by the business, and disregarding potential alternative uses and any other characteristics of the property that would cause its market value to differ from that needed to replace the remaining service potential at least cost".
The definition of MEA Modern Equivalent Assets - a structure similar to an existing structure with an equivalent, productive capacity, which could be built using modern materials, techniques and designs. Replacement cost is the basis used to estimate the cost of constructing a modern equivalent asset.
The value of land has been assessed on the basis of the construction of a modern equivalent asset, over a number of storeys, with the associated footprint that such a construction would require. Non specialised property is held at existing use value and is not materially different from its open market value.
Note 15 Leases - Hertfordshire Community NHS Trust as a lessee
This note details information about leases for which the Trust is a lessee.
The Trust leases a number of properties from NHS Trusts, NHS Property Services, Local Authorities and commercial companies, from which it provides patient care.
The Trust has applied IFRS 16 to account for lease arrangements from 1 April 2022 without restatement of comparatives. Comparative disclosures in this note are presented on an IAS 17 basis.
Note 15.1 Right of use assets - 2024/25
Note 15.2 Right of use assets - 2023/24
Note 15.3 Reconciliation of the carrying value of lease liabilities
Lease liabilities are included within borrowings in the statement of financial position. A breakdown of borrowings is disclosed in note 20.1.
Lease payments for short term leases, leases of low value underlying assets and variable lease payments not dependent on an index or rate are recognised in operating expenditure. These payments are disclosed in Note 6.1. Cash outflows in respect of leases recognised on-SoFP are disclosed in the reconciliation above.
* The Trust has one peppercorn lease which has been valued on a MEA revaluation basis, so not included in this figure. The movements for this lease can be found in note 14.2 through impairments.
Note 15.4 Maturity analysis of future lease payments
which leased from leased from DHSC group Total DHSC group bodies
bodies: (Restated) (Restated):
The 2023/24 comparators have been restated to reflect the finance charge attributable to that year
Note 16.1 Receivables
Of which receivable from NHS and DHSC group bodies:
Note 16.2 Allowances for credit losses
There were no allowances for credit losses in relation to contract receivables and contract assets in 2024/25 (nil 2023/24)
Note 16.3 Exposure to credit risk
Given that the Trust's significant receivables would normally sit with other NHS bodies, the Trust does not consider that it is exposed to significant credit risk.
Note 17.1 Cash and cash equivalents movements
Cash and cash equivalents comprise cash at bank, in hand and cash equivalents. Cash equivalents are readily convertible investments of known value which are subject to an insignificant risk of change in value.
Note 17.2 Third party assets held by the trust
Hertfordshire Community NHS Trust does not hold cash and cash equivalents which relate to monies held by the Trust on behalf of patients or other parties and in which the trust has no beneficial interest.
Note 20.1 Borrowings
Note 20.2 Reconciliation of liabilities arising from financing activities
Note 21.1 Provisions for liabilities and charges analysis
Pensions: early departure costs
Early Departure costs relate to a constructive obligation with the NHS Pensions Agency to refund it the costs of pensions paid to staff who have retired due to ill-health in earlier years. The value of the obligation has been assessed using past claims and numbers expected to take this option and the uncertainty relates to the length of time these pensions will be payable.
Legal claims:
These are provisions for Employer Liability and NHS Resolution member provision.
Redundancy:
These are provisions for the potential costs of staff redundancies resulting from service re-configuration.
Other:
Other includes provisions for dilapidations in respect of leased buildings, the non-achievement of improvement targets which have been invoiced on an estimated basis but may have to be part credited when actual activity becomes available, and the review of floor space utilisation with respect to specific rental income.
Note 21.2 Clinical negligence liabilities
At 31 March 2025, £1,035k was included in provisions of NHS Resolution in respect of clinical negligence liabilities of Hertfordshire Community NHS Trust (31 March 2024: £997k).
Contingent Liabilities relate to the member proportion of Public Liability and Employer Liability Claims with NHS Resolution
Note 24.1 Financial risk management
Financial reporting standard IFRS 7 requires disclosure of the role that financial instruments have had during the period in creating or changing the risks a body faces in undertaking its activities. Because of the continuing service provider relationship that the Trust has with its commissioners and the way those commissioners are financed, the Trust is not exposed to the degree of financial risk faced by business entities. Also financial instruments play a much more limited role in creating or changing risk than would be typical of listed companies, to which the financial reporting standards mainly apply. The Trust has limited powers to borrow or invest surplus funds and financial assets and liabilities are generated by day-to-day operational activities rather than being held to change the risks facing the Trust in undertaking its activities. The Trust’s treasury management operations are carried out by the finance department, within parameters defined formally within the Trust's standing financial instructions and policies agreed by the board of directors. The Trust's treasury activity is subject to review by the Trust's internal auditors.
Currency risk
The Trust is principally a domestic organisation with the great majority of transactions, assets and liabilities being in the UK and sterling based. The Trust has no overseas operations. The Trust therefore has low exposure to currency rate fluctuations.
Interest rate risk
The Trust borrows from government for capital expenditure, subject to affordability as confirmed by NHS England. The borrowings are for 1 – 25 years, in line with the life of the associated assets, and interest is charged at the National Loans Fund rate, fixed for the life of the loan.
The Trust may also borrow from government for revenue financing subject to approval by NHS Improvement. Interest rates are confirmed by the Department of Health and Social Care (the lender) at the point borrowing is undertaken.
The Trust therefore has low exposure to interest rate fluctuations.
Credit risk
Because the majority of the Trust's revenue comes from contracts with other public sector bodies, the Trust has low exposure to credit risk. The maximum exposures as at 31 March 2022 are in receivables from customers, as disclosed in the trade and other receivables note.
Liquidity risk
The Trust's operating costs are incurred under contracts with commissioning organisations, which are financed from resources voted annually by Parliament . The Trust funds its capital expenditure from funds obtained within its prudential borrowing limit. The Trust is not, therefore, exposed to significant liquidity risks.
Note 24.2 Carrying values of financial assets
Note 24.3 Carrying values of financial liabilities
Note 24.4 Maturity of financial liabilities
The following maturity profile of financial liabilities is based on the contractual undiscounted cash flows. This differs to the amounts recognised in the statement of financial position which are discounted to present value.
The 2023/24 comparators have been restated to reflect the finance charge attributable to that year
Note 25 Losses and special payments 2024/25
Where nil values are returned, this reflects occurrences of losses or special payments where the total value is under £1,000
Note 26 Related parties
There have not been any related party transactions with individuals during 2024-25.
The Department of Health and Social Care is regarded as a related party. During the year Hertfordshire Community NHS Trust has had a significant number of material transactions with the Department, and with other entities for which the Department is regarded as the parent Department.
In addition, the Trust has had a number of material transactions with other government departments and other central and local government bodies. The most significant of these include NHS England; Essex Partnership University NHS Foundation Trust; East and North Hertfordshire NHS Trust; West Hertfordshire Teaching Hospitals NHS Trust; NHS Cambridgeshire and Peterborough ICB; NHS Hertfordshire and West Essex ICB; NHS Property Services; HMRC; NHS Pension Scheme; NHS Professionals and Hertfordshire County Council
The Trust is linked to Hertfordshire Community NHS Trust Charitable Funds but this is not consolidated as they are not material. In 2024-25 the Trust made payments of £22k on behalf of the charity for which re-imbursement is expected (2023-24 £74k)
Note 27 Events after the reporting date
There have been no non-adjusting events after the reporting period.
Note 28 Better Payment Practice code
NHS Payables
The Better Payment Practice code requires the NHS body to aim to pay all valid invoices by the due date or within 30 days of receipt of valid invoice, whichever is later.
Note 29 Capital Resource Limit
Note 30 Breakeven duty financial performance
Note 31 Breakeven duty rolling assessment