Dr. Stacy Fisher
American Heart Association
Chesapeake Medical Imaging

Bailey Bullock’s Heart & Soul Foundation
Alcohol and Cancer
Dr. John Martin Butterfly Network
New Year’s Health Resolution

Dr. Stacy Fisher
American Heart Association
Chesapeake Medical Imaging

Bailey Bullock’s Heart & Soul Foundation
Alcohol and Cancer
Dr. John Martin Butterfly Network
New Year’s Health Resolution

Dr. Larry Bryant – Your Local Certified TeethXpress Provider
Are missing teeth affecting your confidence and quality of life? TeethXpress offers a revolutionary solution for securing a brand-new smile in as little as ONE DAY!
With this advanced dental implant technology, you can enjoy a strong, natural-looking set of teeth without the hassle of traditional dentures.


• Walk Out with a New Smile the Same Day No need to wait months for a full set of teeth! TeethXpress provides a permanent solution in just one visit. Your new teeth are custom-crafted for a natural, comfortable fit.
• Short Healing Time
Unlike traditional implants that may require lengthy recovery, TeethXpress minimizes downtime, allowing you to enjoy the benefits of a fully restored smile quickly.
• A Superior Alternative to Traditional Dentures
Say goodbye to slipping dentures! TeethXpress implants provide stability and comfort, allowing you to eat, speak, and smile with confidence.
• A Worthwhile Investment in Your Health
A beautiful, functional smile enhances both your appearance and overall well-being. TeethXpress is designed to improve not only your confidence but also your ability to enjoy everyday activities without worry.

As a certified TeethXpress provider, Dr. Bryant and his team at Bryant OMS Associates specialize in helping patients achieve a lasting, healthy smile. With expertise in full-mouth implant procedures, Dr. Bryant ensures every patient receives a personalized treatment plan tailored to their unique dental needs.
Take the First Step Toward a Confident Smile! Schedule a consultation today to find out if TeethXpress is the right solution for you.

Welcome to Transformations Center for Weight Loss (TCWL). Our professional and dedicated doctor-led team is here to help you refresh your lifestyle and learn how to love your body! At TCWL, we are passionate about helping each person that walks through our door achieve lasting results that they can feel proud of. With the right tools, education, motivation, and inspiration, our enthusiastic and knowledgeable staff will provide everything you need to achieve and maintain a healthy weight for the rest of your life!





Undeniable Results
Uncompromising Standards
We offer a wide range of treatments and surgeries, including facial rejuvenation, body contouring, breast augmentation, and more. Whether you are looking to enhance your appearance or restore your original look, we are here to help. Contact us today to learn more about what we can do for you






Dr. Nadya Clarke is a Board-Certified plastic surgeon who is experienced in aesthetic surgical procedures of the face, body, and breasts. She also performs an array of aesthetic non-surgical procedures.









CHESAPEAKE MEDICAL IMAGING
Doctors can now detect subtle shifts in heart function
MARYLAND HOSPITAL ASSOCIATION
HEALTHY HOSPITALS. HEALTHY COMMUNITIES.
BRYANT ORAL & FACIAL SURGERY
Maryland’s Premier Oral Surgeon Transforming Smiles and Lives
BE SPOKE AESTHETIC
As a Board-Certified Plastic Surgeon, I’ve seen aesthetic trends
FROM PAIN TO PROGRESS, JANET MERICA’S STORY
It was a great day when Maryland native Janet Merica spoke





As we step into February, American Heart Month serves as a powerful reminder to prioritize one of the most crucial aspects of our well-being: our heart health. Cardiovascular disease remains the leading cause of death in the United States, yet much of it is preventable. Through awareness, proactive healthcare, and simple lifestyle changes, we can truly make a difference.
Here at Maryland Health Magazine, I’m proud to say we’re dedicated to providing you with the latest tools and information to take control of your health. In this issue, we’ve curated expert advice and resources that matter most to our Maryland community. You’ll find tips on heart-healthy eating, the importance of testing, preventative care, advanced medical technology, and CPR—all practical advice that can lead to significant changes.
Having recently undergone two heart procedures myself, I now approach this topic not only as the Publisher but also as a patient. The shock of receiving a diagnosis, the anxiety that accompanies waiting and preparing for a procedure, and the same lingering cloud that hangs over you—even after receiving the all-clear—has given me a new perspective. I understand firsthand the importance of knowing your health status and taking proactive steps to safeguard your heart.
I’m especially inspired by the stories of Marylanders we feature this month and every month-individuals and families who’ve faced heart health challenges head-on and emerged stronger. Their journeys serve as a reminder that it’s never too late to make positive changes and that a supportive community can make all the difference.
For me, American Heart Month isn’t just about raising awareness; it’s a call to action. Whether you’re starting fresh or fine-tuning your habits, small, consistent steps—like walking more, choosing healthier meals, and staying connected with your doctor—can lead to lasting improvements.
At Maryland Health Magazine, we’re here to be your partner in health, wellness, and fitness. With our focus on local expertise and practical advice, we’re making it easier for you to stay informed and inspired. Let’s commit to putting heart health first—not just in February, but all year round.
Sincerely,
R odney
Folma
R , S R ., G R oup p ubli S he R h WF m a G azine G R oup

Publisher Rodney Folmar, Sr.
Editor in Chief
Melissa Shelby
Content Creator Daine Taylor
Writers
Wendy Begay, Julia Fischer, Barbara Forman, Darla Frisk, Daine Taylor, Carolyn Tolbert, Rodney Folmar, Sr., Jasmine Wheeler
Advertising & Digital Sales
Will Summer Greg Baily
Graphic Design
William Hodges
Susan Holgram
Distribution Kathy Wilson
Photography Ron White
Anthony G. Gallegos Gill Associates Photography
Contact us contact@gmfmediagroup.com 301-889-9580
hwfmg
healthwellnessfitnessmag healthwellnessfitness
HEALTH WELLNESS & FITNESS MAGAZINES ARE PUBLISHED BY GMF MEDIA GROUP, LLC. A NEW JERSEY BASED PUBLISHING, ADVERTISING AND MARKETING COMPANY.

The information printed in this magazine has been provided as a public service. Every effort has been made to ensure accuracy; however, the authenticity cannot be guaranteed. All advertisements in this magazine have been furnished by advertisers. Typographic, photographic, and printing errors are unintentional and subject to correction.
The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Never disregard professional medical advice, or delay in seeking it, because of something you have read or seen on our web site. Never rely on information on our web site and/or in the magazine in place of professional medical advice.




Join a SPIRIT Club fitness class for a fun, social, and interactive way to stay active! Designed to support all fitness levels and abilities, certified trainers will lead accessible exercises with seated versions always available.

Date and Time
CRAB Annapolis Adaptive Boating Center
7040 Bembe Beach Road, Annapolis, Maryland
March 5 @ 1 pm - 2 pm

| The Baltimore Breathwork Sound Bath February
For Ages 13+ this transformative experience utilizes breathwork, sound healing, and guided imagery to leave you feeling lighter!
Date and Time
Roland Park Community Center
5802 Roland Avenue Baltimore, MD 21210
Sunday, February 2, 2025
Doors at 2 pm

| Health & Fitness ExpoWashington DC 2025
The Health & Fitness Expo in Washington DC is open to everyone, featuring new running technologies, fitness apparel, and health information through interactive displays. Runners need to attend to gather race essentials.
Date and Time
Walter E. Washington Convention Center, Washington DC, USA 20 Mar, 2025 Thu, 10 am – 2 pm

Nature doesn’t stop during the cold months! Animals and plants have adapted to a different routine to get through the winter and we are going to learn how they do it. Come explore the park in this child-friendly event, and remember to dress for the weather we are going outside!

Date and Time
FRP Kaufman House at Fountain Rock Park
From: Jan 27 2025 to Mar 3 2025
Every Tuesday: 10:00am to 12:00pm
Looking for free dental care for your kids? Give Kids a Smile Day is here to provide families with accessible and quality oral health services! Join us for Give Kids a Smile Day, hosted by the Maryland State Dental Association, this event offers free oral health exams, fluoride

Every February, thousands of undie runners in cities across the U.S. come together, whether it be in-person or virtually, to support those affected by NF, a group of genetic conditions that cause tumors to grow on nerves throughout the body. Cupid’s Undie Run kicks off with drinking and dancing, then we jog it out with a mile(ish) run and end it all with an epic dance party!
Date and time
The Admiral’s Cup 1647 Thames St, Baltimore, MD 21231 February 8, 2025 12 pm –4 pm
This is a free educational support forum for men and their spouses , which is professionally facilitated and meets monthly to share resources, and discuss medical information, experiences, and coping strategies. Meets the first Wednesday of every month at 4 p.m.
Date and time
Kaufman Cancer Center
54 E. Lee Street, Bel Air, MD 21014 March 5, 2025, 4 pm to 5 pm
Contact Name: Carole Powell
Contact Phone: 443-643-3350

treatments, healthy snacks, and giveaways for children ages 1-17. No insurance is required to attend. Additional health screenings and resources will be available to support your family’s well-being. Reserve your spot today –spaces are limited! Contact 800-621-8099 or email gkas@ada.org
Date and Time
3201 Tioga Parkway Suite W Baltimore, MD February 8, 2025 from 11 am to 3 pm Every Tuesday: 10:00am to 12:00pm
Who: Anyone with prediabetes. Family & Friends Welcome.
What : Each month this group presents a new topic centered around managing pre-diabetes. Conversations with the group to learn and support one another forward on the journey of improved health.

When: The 2nd Thursday of every month from 5:30p.m. – 6:30pm
Where: Havre de Grace Activity Center 351 Lewis Lane, Havre de Grace, MD 21078 March 6, 2025, 10 am to 11 am
Contact Phone: 1-800-515-0044
Come out for a fun morning of yoga with these baby goats. This is a beginner’s class for all ages and experience levels. You goat this. Cost is $33 (+tax/fees) and includes approximately 1 hour of goat yoga and
Treat yourself to a rejuvenating getaway at the Women’s Wellness Weekend on Virginia’s beautiful Eastern Shore! This special weekend retreat offers a wide variety of activities designed to nourish your mind, body, and spirit. Enjoy yoga, meditation, workshops, and outdoor adventures in a serene, coastal setting. Perfect for women seeking relaxation, connection, and self-care, this event promises to leave you refreshed and inspired.
Date and Time
Friday, April 4 – Sunday, April 6, 2025 Location Mack, 16 Strawberry St, Cape Charles, VA 23310


Empower your mind, body, and soul at the DC Women’s Wellness Expo! Join us for an inspiring day at Howard University’s Burr Gymnasium, featuring the latest in fitness, nutrition, mental health, and self-care. Enjoy interactive workshops, expert sessions, and a chance to connect with a vibrant community of like-minded women. Invest in yourself, celebrate your well-being, and leave inspired to live your best life.
Date and Time
Sunday, March 23, 2025
10:00 AM – 5:00 PM
Location
Howard University – Burr Gymnasium 635 Gresham Place NW, Washington, DC 20001

1 beverage. Please arrive 15 minutes prior and bring an old towel or mat for the class.
Date and time
Ministry of Brewing 1900 E Lombard St, Baltimore, Maryland March 15, 2025 at 10 am to 11 am
| MEDICAL & MENTAL HEALTH WELLNESS FAIR
The Hampton Alumnae Chapter of Delta Sigma Theta Sorority, Inc., invites you to the Medical & Mental Health Wellness Fair. This enriching event will provide resources, screenings, and expert guidance on physical and mental well-being. Don’t miss this opportunity to prioritize your health and connect with a supportive community.
Date and time
Saturday, March 22, 2025 10:00 AM – 4:00 PM
Location West Hampton Community Center 1638 Briarfield Rd, Hampton, VA
MIDDLEBURG WELLNESS DAY 5K & KIDS FUN RUN 2025
Join the Middleburg community for Wellness Day 2025! Start the day with a 5K and Kids Fun Run, then explore the many health and wellness businesses showcased in the Ballroom and Terrace Room of the Middleburg Community Center. Enjoy live demos, presentations, and giveaways that will inspire your next wellness step. Bring the whole family for a day dedicated to health and connection!
Date and time
Saturday, April 12, 2025 8:00 AM – 2:00 PM
Location
Middleburg Community Center
300 W Washington St, Middleburg, VA


ON FEBRUARY 7, 2025, MILLIONS ACROSS THE COUNTRY WILL UNITE FOR WEAR RED DAY, A NATIONAL MOVEMENT DEDICATED TO RAISING AWARENESS ABOUT HEART DISEASE—THE LEADING CAUSE OF DEATH AMONG WOMEN. BY WEARING RED, INDIVIDUALS AND COMMUNITIES CAN MAKE A BOLD STATEMENT: WOMEN’S HEART HEALTH CANNOT BE IGNORED.
WHILE THIS DAY SERVES AS A VITAL REMINDER OF THE RISKS AND PREVENTION STRATEGIES, THIS MOVEMENT GOES BEYOND A SINGLE DAY, AND YOU CAN CONTRIBUTE TO THIS WORTHY CAUSE YEAR-ROUND.
Wear Red Day was established in 2004 by the American Heart Association (AHA) as part of its Go Red for Women® campaign, a nationwide initiative to raise awareness about heart disease in women.
Cardiovascular disease is one of the leading causes of death for women in the US, and for decades, women faced underdiagnosis, misdiagnosis, and a lack of research focused on their unique symptoms and risk factors. Wear Red Day was created to change that narrative—to educate women, encourage prevention, and spark advocacy for better heart health. Wearing red can be a powerful symbol of visibility, unity, and empowerment. It sends a message that women’s heart health matters and that no one should fight this battle alone. By coming together in solidarity, we can break the silence around heart disease and help save countless lives.

More than just a symbolic event, Wear Red Day is a call to action. The campaign encourages women to learn their personal risk factors, embrace heart-healthy habits, and advocate for better healthcare policies. It also funds research to close the gender gap in heart disease diagnosis and treatment. Through community events, health screenings, and policy initiatives, Wear Red Day empowers women to take control of their heart health.
On February 7, the M&T Bank Stadium and the Warehouse at Camden Yards will be illuminated red for National Wear Red Day, and you can show your support for women’s heart health by donning red attire. Whether it’s a red dress, tie, or pin, this small but powerful gesture helps raise awareness and demonstrates solidarity in the fight against heart disease.
You can also amplify the message by sharing on social media. Post a photo of yourself in red, share important heart health facts, or use hashtags like #WearRedDay and
#GoRedForWomen to spread the word.
Be sure to make time for regular check-ups, monitor your blood pressure and cholesterol levels, and have an open conversation with your doctor about your heart health. Another way to get involved is by encouraging or organizing community events that promote heart health awareness. Whether it’s a wellness challenge at work, a heart health seminar at your local school, or a charity walk in your neighborhood, the more people who participate, the greater the movement’s impact.
Also consider supporting organizations like the American Heart Association, which fund essential research and advocacy to combat heart disease. This year the organization is offering a 5x match for every dollar donated. Volunteering your time or donating to these groups can help fund life-saving initiatives that change the course of many lives.
Together, we can turn awareness into action, save lives, and build a future where heart disease is no longer the leading cause of death among women. Every voice, every effort, and every red outfit counts.

aryland Health Magazine is dedicated to helping connect you with top healthcare providers, organizations, and resources to support a healthy lifestyle and heart-friendly living.
This page is your comprehensive guide to the healthcare providers, advocacy groups, and heart health organizations working in your area to support your cardiovascular well-being. From top cardiologists and medical centers to community programs offering screenings and heart-healthy initiatives, this list connects you to the resources you need to live a healthier life. Stay informed with resources tailored for Maryland residents, and take your first steps toward a stronger, more heart-healthy life.
CARDIOLOGISTS
Interventional Cardiologists
Dr. Terence Bertele, MD George Washington University Hospital 12070 Old Line Ctr, Waldorf, MD 1-720-903-3007
Dr. Martin A. Albornoz, MD Ascension St. Agnes Hospital 3407 Wilkens Ave, Baltimore, MD (410) 644-5111
Electrophysiologists
Dr. Stephen R. Shorofsky, MD University of Maryland Medical Center 22 S Greene St, Baltimore, MD 1-443-348-9838
Dr. Sunjeet S. Sidhu, MD MedStar Washington Hospital Center 3333 N Calvert St, Johnston Professional Bldg. Ste 650, Baltimore, MD, 21218 1-570-659-6406
Pediatric Cardiologists
Dr. Nicholas P. Pietris, MD University of Maryland Children’s Hospital 22 S Greene St, N5w72c, Baltimore, MD, 21201 1-443-348-9173
Dr. Alicia H. Chaves, MD University of Maryland Children’s Hospital 22 S Greene St, # N5W40, Baltimore, MD, 21201 1-443-348-0093
PRIMARY CARE PHYSICIANS
Family Medicine Doctors
Dr. Haroon Akhtar, MD Frederick Health Hospital 13671 Georgia Ave, Aspen Hill, MD, 20906 (240) 514-0000
Oluwatoyin A. Adekeye, NP LifeStance Health 810 Bestgate Road, Suite 325, Annapolis, MD, 21401 1-833-789-5210
Internal Medicine Specialists
Dr. Ali J. AfrooktehMD Frederick Health Hospital 187 Thomas Johnson Dr, Suite 4, Frederick, MD, 21702 (240) 651-0420
Dr. Azeez A. Abiodun, MD Luminis Health Doctors Community Medical Center 8118 Good Luck Rd, Glenarden, MD, 20706 (301) 474-4443
CARDIAC SURGEONS Thoracic Surgeons
Dr. Rachel E. Harrison, MD MedStar Washington Hospital Center
3333 N. Calvert Street, Baltimore, MD, 21218 1-650-397-9311
Dr. Richard J. Battafarano, MD Johns Hopkins Bayview Medical Center 10751 Falls Road, Lutherville, MD, 21093 (410) 583-2900
Dr. Brian T. Bethea, MD MedStar Washington Hospital Center
3333 N. Calvert Street, Baltimore, MD, 21218 1-775-383-6692
Vascular Surgeons
Dr. John A. Bartkovich, MD TidalHealth Peninsula Regional 145 E Carroll St, Salisbury, MD, 21801 (410) 548-2600
Dr. Khanjan H. Nagarsheth, MD University of Maryland Medical Center 419 W Redwood St, Baltimore, MD, 21201 1-443-940-6524
NURSES AND NURSE PRACTITIONERS
Cardiac Care Nurses
Rachel McCumbers, MS, CRNP, FNP- BC University of Maryland
Medical Center
22 S. Greene Street, Baltimore, MD 21201
800-492-5538
Carol R. Wade RN, DNP, CRNP University of Maryland Medical Center
22 S. Greene Street, Baltimore, MD 21201
800-492-5538
TESTING AND DIAGNOSTIC CENTERS
Echocardiography Labs
The Johns Hopkins Echocardiography Laboratory - Bayview Medical Center
4940 Eastern Ave, Baltimore, MD 21224
443-997-0270
CardioCare LLC
5530 Wisconsin Avenue, Suite 700, Chevy Chase, MD 20815
Phone: (301) 656-5050
University of Maryland Medical Center Midtown Campus
827 Linden Ave, Baltimore, MD 21201
Phone: (410) 225-8000
Stress Testing Facilities
Maryland Cardiology Associates
7474 Greenway Center Drive, Suite #1100, Greenbelt, MD 20770
Phone: (301) 441-3050
University of Maryland Medical Center Midtown Campus
827 Linden Ave, Baltimore, MD 21201
Phone: (410) 225-8301
Holter Monitor Services
CardioCare LLC
5530 Wisconsin Avenue, Suite 700, Chevy Chase, MD 20815
Phone: (301) 656-5050
Heart Center at Mercy
301 St. Paul Place, Baltimore, MD 21202
Phone: (410) 332-9752
NON-PROFIT ORGANIZATIONS
American Heart Association (AHA)
AHA Mid-Atlantic Affiliate
217 E Redwood St, Suite 1100, Baltimore, MD 21202
Phone: (410) 246-6700
Maryland Heart Rescue Grasonville, MD, United States, Maryland
Phone: 1 443-521-0527
SUPPORT GROUPS
Heart Disease Support Groups
Mended Hearts of Central Maryland International Headquarters and Resource Center 1579 US Highway 19 S Leesburg, GA 31763 USA
Phone: (888) 432-7899
Community Wellness Workshops
Living Well Chronic Disease Self-Management Program
Prince George’s County Health Department, 1701 McCormick Dr, Largo, MD 20774
Phone: (301) 883-7879
Tevis Center for Wellness 291 Stoner Ave, Westminster, MD 21157
Phone: (410) 871-7000
LOCAL GOVERNMENT HEALTH AGENCIES
Maryland Department of Health
201 W Preston St, Baltimore, MD 21201 (410) 767-6500
Baltimore City Health Department 1001 E Fayette St, Baltimore, MD 21202
Phone: (410) 396-4398
REHABILITATION CENTERS
Cardiac Rehabilitation Facilities
University of Maryland
Medical Center Cardiac Rehabilitation Program 22 S Greene St, Baltimore, MD 21201 Phone: (410) 328-8910
Adventist HealthCare Shady Grove Medical Center 9901 Medical Center Dr, Rockville, MD 20850
Phone: (240) 826-6000
Wellness and Fitness Programs Focusing on Heart Health
Columbia Association 6310 Hillside Ct #100, Columbia, MD 21046
Phone: (410) 715-3000
NUTRITIONISTS AND DIETITIANS
Certified Heart Health Nutritionists
University of Maryland Medical Center Nutrition Services 22 S Greene St, Baltimore, MD 21201
Phone: (410) 328-8910
Website: UMMC Nutrition Services
MENTAL HEALTH SERVICES
Psychologists Specializing in Chronic Illness
• Sankofa Health Center Address: 8501 LaSalle Rd, Towson, MD 21286
Phone: (410) 296-5462
Support for Stress
Management and Coping Strategies
MedStar Health Address: 10980 Grantchester Way, Columbia, MD 21044 Phone: (877) 772-6505

Much like the shift towards “quiet lMaryland is addressing a long-standing gap in healthcare coverage: the affordability of hearing aids for adults. While insurance coverage for children’s hearing aids has been required by law, adults have been left without similar support, forcing many to delay or forego treatment due to high out-of-pocket costs.
Hearing loss isn’t just an inconvenience; it can lead to social isolation, cognitive decline, and reduced quality of life. However, the financial burden of hearing aids—ranging from $1,000 to $6,000 per device—has often been a major financial hurdle.
Insurance providers must now cover medically necessary hearing aids for adults. The new law sets a minimum benefit of $1,400 per hearing aid per ear, with coverage available every 36 months. Patients can choose higher-priced devices and pay the difference, ensuring greater flexibility and access to advanced technology.
By addressing this gap in coverage, the law not only reduces the financial burden but also encourages individuals to take charge of their hearing health. It’s a significant step toward reducing the stigma around hearing loss and increasing access to necessary care.
Residents are urged to review their insurance policies and consult with providers to understand changes to their coverage.

Maryland continues to confront the devastating opioid crisis, which has led to numerous overdoses and strained emergency healthcare services. One critical issue has been the lack of standardized protocols in hospitals for treating patients experiencing opioid-related emergencies. This gap has often resulted in inconsistent care and missed opportunities to initiate long-term treatment.
To address these challenges, Senate Bill 1071 mandates that hospitals implement specific protocols and capacities for treating patients with opioid-related overdoses or emergencies.
Key provisions include:
Standardized Treatment Protocols: Hospitals must adopt consistent procedures to ensure timely and appropriate care for opioid-related emergencies.
Referral Systems: Patients diagnosed with opioid use disorder or treated with medication for their condition must be referred to community providers for voluntary continuation of treatment.
Peer Support Integration: Hospitals are required to collaborate with peer support professionals to assist patients, increasing the likelihood of successful recovery.
By enforcing these measures, the law aims to improve immediate care for overdose patients, establish a seamless transition to ongoing support, and reduce the burden on emergency services. This comprehensive approach is designed to address both the acute and chronic aspects of opioid use disorder, promoting sustained recovery within the community.

Access to essential mobility devices has long been a challenge for individuals who rely on orthoses and prostheses. Many Marylanders, particularly those on Medicaid, have faced significant financial barriers, often preventing them from obtaining or replacing these critical devices. High costs, combined with restrictive insurance policies, have left many struggling to maintain their mobility and independence.
To address these inequities, the state has enacted the “So Every Body Can Move Act,” also known as House Bill 865. This law mandates that Medicaid provide comprehensive coverage for orthoses and prostheses, including replacements. It ensures that individuals requiring these devices can access medically necessary care without financial constraints.
Additionally, the law prohibits insurers from charging higher copayments for orthoses and prostheses than for other medical benefits. This eliminates discriminatory cost structures, making these life-enhancing devices more accessible to all.
For many, having access to proper mobility aids means fewer hospital visits, reduced pain, and a higher quality of life, which ultimately alleviates the burden on the healthcare system. Without proper access to these devices, individuals often face increased reliance on caregivers, greater healthcare needs, and a reduced ability to participate in daily activities.
By reducing financial burdens and expanding coverage, this legislation empowers individuals with mobility challenges to lead more active, independent lives.
On January 7, 2025, State Senator Katherine Klausmeier was appointed as Baltimore County Executive, marking a historic milestone as the first woman to hold this position. She succeeds Johnny Olszewski, who resigned to serve in the U.S. House of Representatives.
Klausmeier, 74, brings extensive experience from her tenure in the Maryland General Assembly, where she has been a steadfast advocate for Baltimore County since 1994. Her legislative focus has encompassed healthcare, education, and economic development, reflecting her commitment to the well-being of her constituents.
In her new role, Klausmeier has identified public safety and addressing aggressive driving as top priorities, aiming to enhance the quality of life for county residents. She has also indicated that she will not seek re-election in 2026, emphasizing her dedication to serving the remainder of this term with a focus on continuity and stability.
Klausmeier’s appointment is a significant achievement for gender representation in Baltimore County’s governance, inspiring women across Maryland to pursue leadership roles. Her leadership is anticipated to bring a renewed focus on health and wellness initiatives, aligning with her legislative history of supporting healthcare access and public health programs.

Maryland’s healthcare landscape is poised for exciting advancements with the appointment of Michael Greenebaum as the new chair of the University of Maryland School of Medicine’s (UMSOM) Board of Visitors. A respected business leader and philanthropist, Greenebaum succeeds Cynthia Egan, who served as chair since 2013 and now holds the title of chair emerita. Greenebaum brings decades of expertise and a deep-rooted commitment to health and community service. As president of Greenebaum Enterprises, a prominent real estate development firm, he has not only contributed to Maryland’s economic growth but also championed numerous philanthropic initiatives. His family’s legacy includes the founding gift for the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center, which has since become a beacon of hope and innovation in cancer treatment.
A member of UMSOM’s Board of Visitors since 2012, Greenebaum has played a key role in shaping its direction. As the inaugural vice chair and leader of the board’s campaign committee, he spearheaded efforts that raised $6.4 million in just two years. His work in aligning the School of Medicine and Medical Center’s development strategies has set the stage for greater collaboration and impact.
Dean Mark T. Gladwin, M.D., praised Greenebaum’s leadership, calling it transformational for UMSOM’s future. For his part, Greenebaum expressed a heartfelt dedication to advancing the school’s mission of improving health outcomes through innovation, education, and patient care.
For Maryland residents, this appointment underscores UMSOM’s commitment to excellence in medical science and healthcare. With Greenebaum at the helm, the Board of Visitors is set to continue driving advancements that will benefit communities across the state and beyond.


The American Heart Association is proud to announce a historic milestone in its mission to double survival rates from cardiac arrest by 2030 and create a world of longer, healthier lives: the signing of the HEARTS Act.
This landmark legislation establishes a federal grant program that, once funded, will help support schools so they have the lifesaving tools, training, and education to ensure that everyone has the knowledge and resources to act in a cardiac emergency.
The HEARTS Act, also known as the Cardiomyopathy Health Education, Awareness, Research, and Training in Schools Act, was signed into law in late December 2024 by President Biden.
It represents a significant step forward in ensuring schools across the U.S. are equipped with automated external defibrillators (AEDs), cardiac emergency response plans, and lifesaving CPR training programs.
Dr. Stacy Fisher, Associate Professor of Medicine and Associate Director of the Adult Congenital Heart Program at Johns Hopkins University, as well as a member and former President of the American Heart Association’s, Baltimore & Greater Maryland Board of Directors, celebrated the bill’s passage.
“ I am absolutely thrilled about the HEARTS Act bill that President Biden signed. It’s really important because it will help support communities’ access to trained individuals, training and resources with the possibility of saving more lives with better outcomes.”
This legislation was inspired in part by the real-life events surrounding Buffalo Bills defensive back Damar Hamlin, who experienced a cardiac arrest during a 2023 game in Cincinnati against the Bengals. He survived thanks to immediate CPR and the use of an AED, and was subsequently diagnosed with Commotio Cordis, a rare condition where a chest impact at a critical moment can disrupt the heart’s rhythm, causing cardiac arrest.

Dr. Stacy Fisher, Associate Professor of Medicine and Associate Director of the Adult Congenital Heart Program at Johns Hopkins University, as well as a member and former President of the American Heart Association’s, Baltimore & Greater Maryland Board of Directors.
Credit: Johns Hopkins University
Hamlin’s story helped galvanize national attention and secure bipartisan support for the HEARTS Act from leaders like Majority Leader Chuck Schumer, Sens. Cory Booker and Susan Collins, and Reps. Frank Pallone, Sheila Cherfilus-McCormick, and Bill Posey.
In March 2023, the NFL established the Smart Heart Sports Coalition with founding members including the American Heart Association, Damar Hamlin’s Chasing M’s Foundation and the MLB, MLS, NBA, NCAA, and NHL. The Smart Heart Sports Coalition is advocating for all 50 states, including Maryland, to adopt evidence-based policies that will prevent fatal outcomes from Sudden Cardiac Arrest among high school student athletes.
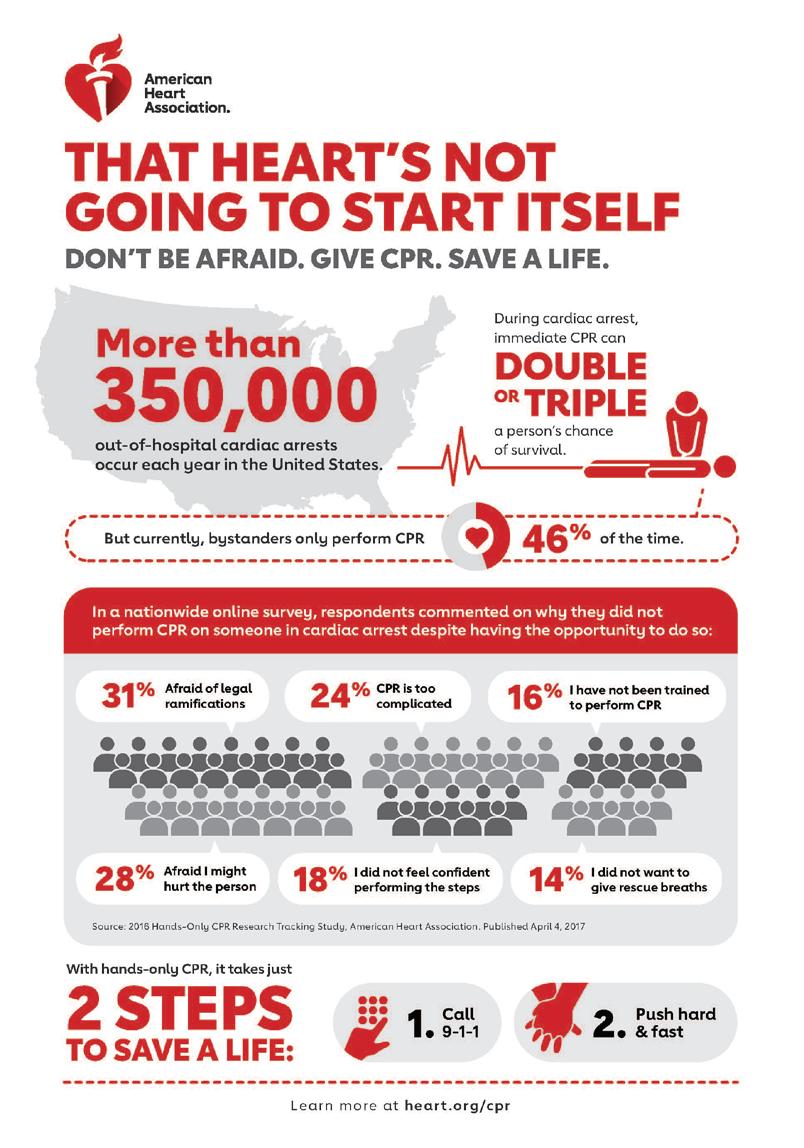
Every year, more than 350,000 cardiac arrests occur outside hospitals in the U.S., with nearly 90 percent proving fatal without CPR, according to the Sudden Cardiac Arrest Foundation. Immediate intervention, especially through CPR, can dramatically increase survival rates and improve quality of life after an emergency.
“Cardiac arrest survival without CPR is absolutely dismal, and with CPR, we meet people who are survivors on a regular basis,” said Dr. Fisher.
“ If everybody in high school has a requirement to know CPR, you have your entire population, over time, trained to be first responders. Whether you’re at a train station, a bus stop, on the athletic field, or in the grocery store, there should be somebody around you who has formal training and can recognize an emergency and start immediate treatment until formal EMS is available.”
The HEARTS Act will bolster state efforts through a new, competitive grant program to provide schools with additional resources for CPR and AED training, the purchase of AEDs and related equipment and the development of cardiac emergency response plans.
The HEARTS Act could also address disparities in access to lifesaving care. It includes provisions to adapt its implementation to the existing infrastructure of the individual communities. Training and resources may be distributed through centralized programs or local outreach efforts, with schools playing a key role in ensuring widespread CPR education and access to emergency care.
“One of the biggest priorities of the American Heart Association is ensuring access and trying to make care available to everyone.”
“One of the biggest priorities of the American Heart Association is ensuring access and trying to make care available to everyone. It’s very empowering to have the knowledge to recognize and initially treat an emergency well,» said Dr. Fisher. «To have it expected that people would have access to emergency care no matter what state they live in is absolutely wonderful.”
The HEARTS Act is an important step forward in creating a culture of preparedness during a cardiac emergency outside of a hospital. With more people trained to respond and better access to resources like AEDs, we can save countless lives.
The American Heart Association encourages everyone to take charge of their heart health and support initiatives like this. Together, we can create a healthier, more resilient future.
Visit www.heart.org to learn more and get involved.




s a child, she would visit the patients, liA recent warning from the U.S. Surgeon General Dr. Vivek Murthy has revealed a health risk that many Americans might not have seriously considered: the link between alcohol and cancer.
In an advisory issued in January, Dr. Murthy explained that alcohol is connected to at least seven types of cancer and urged Americans to rethink their drinking habits, while calling for updated warning labels on alcoholic beverages to highlight these dangers.
Arecent warning from the U.S. Surgeon General Dr. Vivek Murthy has revealed a health risk that many Americans might not have seriously considered: the link between alcohol and cancer.
In an advisory issued in January, Dr. Murthy explained that alcohol is connected to at least seven types of cancer and urged Americans to rethink their drinking habits, while calling for updated warning labels on alcoholic beverages to highlight these dangers.
For many, alcohol is a part of everyday life, whether it’s a glass of wine at dinner, a craft beer at a local brewery or a celebratory cocktail. But the new advisory highlights a sobering reality: alcohol is responsible for about 100,000 cancer cases and 20,000 cancer-related deaths each year in the United States.
“Alcohol is a well-established, preventable cause of cancer,” Murthy said. “Yet the majority of Americans are unaware of this risk.”
Alcohol is now recognized as the third-leading preventable cause of cancer, after tobacco use and obesity. It has been directly linked to cancers of the breast, liver, mouth, throat, esophagus, voice box and colorectum. While heavier drinking increases the risk, even moderate consumption, like one drink per day for women or two
for men, can raise the likelihood of certain cancers. This applies to all alcohol, including beer, wine, and liquor.
For many, alcohol is a part of everyday life, whether it’s a glass of wine at dinner, a craft beer at a local brewery or a celebratory cocktail. But the new advisory highlights a sobering reality: alcohol is responsible for about 100,000 cancer cases and 20,000 cancer-related deaths each year in the United States.
The advisory also seeks to debunk a long-standing misconception that moderate drinking, particularly of red wine, offers significant health benefits. While some studies suggest a small benefit for heart health, Dr. Murthy emphasizes that these potential gains are outweighed by the substantial risk of cancer.
“Alcohol is a well-established, preventable cause of cancer,” Murthy said. “Yet the majority of Americans are unaware of this risk.”
Doctors and nurses are being urged to integrate alcohol screenings into routine visits and help patients understand how their consumption affects their health. For individuals, especially those with a personal or family history of cancer, cutting back on alcohol could be a powerful step toward reducing their risk.
Alcohol is now recognized as the thirdleading preventable cause of cancer, after tobacco use and obesity. It has been directly linked to cancers of the breast, liver, mouth, throat, esophagus, voice box and colorectum. While heavier drinking increases the risk, even moderate consumption, like one drink per day for women or two for men, can raise the likelihood of certain cancers. This applies to all alcohol, including beer, wine, and liquor.
The good news is that small, intentional changes can make a big difference. Opting for alcohol-free alternatives, limiting consumption to special occasions and finding healthier ways to manage stress are just a few strategies that can improve overall well-being.
This update serves not only as a warning but a call to action to rethink acceptable drinking habits and focus on healthier lifestyle choices.
By staying informed and taking proactive steps, Marylanders can lead healthier, longer lives.
The advisory also seeks to debunk a long-standing misconception that moderate drinking, particularly of red wine, offers significant health benefits. While some studies suggest a small benefit for heart health, Dr. Murthy emphasizes that these potential gains are outweighed by the
The Maryland Hospital Association (MHA) has recently launched the «Healthy Hospitals. Healthy Communities» campaign, a statewide initiative aimed at addressing health disparities, improving access to care, and fostering stronger connections between hospitals and communities throughout Maryland.
The initiative builds on the MHA’s history of advocating for health equity and seeks to unite healthcare providers, policymakers, and community organizations in a shared mission.
“Hospitals are here to care for people, drive innovation, and uplift our communities,” said Tom Kleinhanzl, MHA Board Chair and President & CEO of Frederick Health. “This initiative is a chance to celebrate the committed partners who collaborate with us across the health care continuum to make a difference in every community throughout the state.”
The campaign addresses the social determinants of health, such as housing, education, and economic stability, which can be closely tied to health outcomes. By tackling these issues, Maryland hospitals are working to bridge gaps in care and support underserved populations.
As Melony G. Griffith, president and CEO of the MHA said, “being able to be here in the



community, talking with people that are serving and saving lives every day” highlights the essential need for ensuring access to high-quality healthcare for all.
The campaign emphasizes early intervention, preventive care, and partnerships to address these issues head-on. Maryland hospitals are also expanding outreach efforts to ensure residents in rural and urban areas alike have access to the resources they need.
By addressing chronic conditions, substance use, and mental
health challenges, the campaign seeks to lower emergency room visits and hospital readmissions, easing the strain on healthcare resources while improving lives.
A major focus of the Healthy Hospitals, Healthy Communities campaign is accessibility. Programs like the University of Maryland Medical System’s Center for Addiction Medicine
(CAM) offer comprehensive substance use care including counseling, medication management, and inpatient services for those in need.
“CAM provides comprehensive substance use services to patients in Baltimore City and the surrounding counties and states, and we provide counseling, medication management, and inpatient services,” said Carson Herbert, clinical social worker lead at the Midtown Campus. “CAM believes in affordability, accessibility, and
availability. Therefore, we are open 365 days a year.”
These services not only aid individuals in recovery but also strengthen families and reduce stigma in the community, ultimately contributing to better public health outcomes.
“I’m just thankful for the work that the University of Maryland is doing to help support folks that are in recovery and helping them with managing their substance use disorders,” said Melissa R. Wells, delegate for District 40 in Baltimore City. “And just really grateful that it’s helping not only support those individuals, but support their families and our community.”
Additionally, the campaign has expanded its focus to address food insecurity, a critical issue affecting health outcomes. Hospitals
“The Healthy Hospitals, Healthy Communities campaign is a testament to the critical role healthcare institutions play in addressing systemic health challenges and fostering equity”
are partnering with local food banks and community organizations to provide nutritious meals and education on healthy eating. For many residents, these efforts mean the difference between managing a chronic condition and facing severe health complications.
By tackling these issues, Maryland hospitals are working to bridge gaps in care and support underserved populations.
“What I saw today was close to amazing,” said Christina Fitts, MHA board member and CEO of AJ Fitts Unlimited, LLC, who praised the
campaign during an outreach visit to the University of Maryland. “I didn’t realize that these services were available to the citizens that not only reside in Baltimore City, but on the outskirts and other states.”
The Healthy Hospitals, Healthy Communities campaign is a testament to the critical role healthcare institutions play in addressing systemic health challenges and fostering equity. By
taking a holistic approach and building strong partnerships, Maryland hospitals are setting an example for the nation.
This initiative serves as a call to individuals, families, and communities to unite in building a healthier Maryland.
Residents can support the Healthy Hospitals, Healthy Communities campaign by using local hospital services, attending community health events, advocating for policies that address social determinants of health, and volunteering or donating to outreach programs. Check out the Maryland Hospital Association website for more information.



By Wendy Begay
With a new year comes renewed promises to ourselves, especially about healthy habits. For example, you might say, «This is the year I will lose weight or focus on exercise.» However, these New Year’s resolutions can quickly fall by the wayside. If this sounds like you, know you are not alone. Statistically speaking, 23% of people quit after one week. Only 57% stick to resolutions for one month, and just 9% go all the way. As depressing as that sounds, New Year’s Resolutions come from a good place. They are a desire to do or feel better. It’s the approach that tends to trip people up.
| Where Did the Idea of New Year’s Resolutions Come From?
According to History.com, the ancient Babylonians made the first New Year’s resolutions
more than 4,000 years ago. Today, the practice continues, especially with younger people. A Pew Research Survey found that 49% of people making resolutions are between 18 and 29. The numbers drop as ages increase.
The most common resolutions involve healthy habits. A new year means a fresh start, which is a motivating concept, especially when it comes to feeling and looking better. It is also a trendy thing to do. How many times does someone ask you about New Year’s resolutions each year?
| Why are New Year’s Resolutions Such a Challenge?
The answer to that question is almost as old as the practice itself. There are different reasons why people don’t keep their resolutions beyond “Quitters Day,” which is the second Friday in January.
The simple answer for many is their goals are not realistic. If you resolve to go to the gym every single day, chances are you will fail. Few people can keep up an exercise schedule like that, and the goal doesn’t allow for rest or days when you just can’t make it.
Another common issue is resolutions that are too vague. Goals need to be measurable for them to be achievable. If you promise to lose weight in the next year, you may be less motivated without an actual goal to achieve, like 20 pounds.
Or, you may choose an actionable, measurable resolution but fail to create a strategy to support it. How are you planning to lose that weight?
| Are New Year’s Resolutions Worth the Effort?
When approached with the right mindset, New Year’s health resolutions can be a powerful tool for personal growth. They provide a yearly opportunity to identify areas for improvement and set goals to work towards.
There is a downside to the practice, as well. Failing year after year to achieve a goal can be depressing. Still, never making goals will do more damage to your self-confidence than not seeing a resolution to fruition. The right New Year’s resolution might change your life.
New Year’s resolutions are also a practical way to
determine what you can and can’t do. I was one of those people who resolved to go to the gym daily, but I learned the hard way that it was an unattainable goal.
Even if I didn’t keep that promise, I could assess my abilities. When I realized that every day wasn’t going to happen, I reevaluated my schedule and determined that three days a week made more sense. Use these experiences as learning opportunities. Remember, progress is progress, no matter how small.
| How Can You Find Success With Your New Year’s Resolutions?
Take a more thoughtful approach to making New Year’s resolutions this year. Here are some tips:
• Don’t overwhelm yourself with goals. Choose one or two that you want to focus on.
• Select realistic goals.
• Create a strategy to meet your goal.
• Don’t be afraid to make adjustments if necessary. If you set the goal too high, lower it to a level you can manage.
Finally, be kind to yourself. If you fail occasionally, get back on that horse and keep at it.
Sticking to resolutions can be challenging, but it is possible if you approach it with the right attitude and plan. Don’t expect perfection; just focus on your goals and move forward, not backward.







The science of the American Heart Association sets the standards for high-quality care, and access to that care is something that all patients deserve. Each year, the American Heart Association recognizes hospitals across the country for consistently following up-to-date, research-based guidelines to ensure all patients have access to the best practices and lifesaving care.
Thirty-six (36) hospitals in Maryland are among the more than 3,000 nationwide that participate in the American Heart Association’s Get With The Guidelines® and other programs to improve outcomes for Americans who experience heart disease or stroke.
Heart disease and stroke are the No. 1 and No. 5 causes of death in the United States, respectively. These health crises require swift and proven treatment to ensure the best outcomes for patients.
Annapolis
Luminis Health Anne Arundel Medical Center
Baltimore
Ascension Saint Agnes Hospital
Greater Baltimore Medical Center
Johns Hopkins Bayview Medical Center
MedStar Franklin Square
Medical Center
MedStar Good Samaritan Hospital
MedStar Harbor Hospital
MedStar Union Memorial Hospital
Mercy Medical Center
Sinai Hospital of Baltimore
The Johns Hopkins Hospital
University of Maryland
Medical Center
University of Maryland
Every 40 seconds, someone in America has a stroke or heart attack. High-quality care should be accessible to all, and sites awarded through the Get With The Guidelines program help work toward the Association’s shared vision of health and hope for everyone, everywhere. These awards are issued for:
· Get With The Guidelines – Stroke
· Get With The Guidelines – Heart Failure
· Get With The Guidelines – Resuscitation
· Get With The Guidelines – AFib
· Get With The Guidelines – Coronary Artery Disease Hospitals can also receive simultaneous recognition through the Mission: Lifeline®, Target: Stroke ℠, Target: Heart Failure ℠ and Target: Type 2 Diabetes ℠ programs, as well as for being a Primary Stroke Center or Comprehensive Stroke Center.
Learn more at www.heart.org/getwiththeguidelines
Medical Center Midtown Campus
Bel Air
University of Maryland
Upper Chesapeake Medical Center
Bethesda
Suburban Hospital Johns Hopkins Medicine
Clinton
MedStar Southern Maryland Hospital Center
Columbia
Howard County General Hospital
Cumberland
UPMC Western Maryland
Easton
University of Maryland
Shore Medical Center at Easton
Elkton
ChristianaCare - Union Hospital
Frederick
Frederick Health Hospital
Germantown
Holy Cross Germantown Hospital
Glen Burnie
University of Maryland
Baltimore Washington Medical Center
Hagerstown
Meritus Medical Center
Lanham
Doctors Community Medical Center
La Plata
University of Maryland
Charles Regional Medical Center
Largo
University of Maryland
Capital Region Medical Center
Olney
MedStar Montgomery Medical Center
Prince Frederick
Calvert Health Medical Center
Randallstown
Northwest Hospital
Rockville
Adventist HealthCare
Shady Grove Medical Center
Salisbury
TidalHealth Peninsula Regional
Silver Spring
Adventist HealthCare
White Oak Medical Center
Holy Cross Hospital
Towson
University of Maryland
St. Joseph Medical Center
Westminster
Carroll Hospital Center

February is a month dedicated to the heart in many ways. It is a time to celebrate love and relationships. As American Heart Month, it is also about raising awareness and focusing on cardiovascular health.
In 1963, President Lyndon Johnson proclaimed February American Heart Month to encourage people to take action to prevent heart disease, which is now the leading cause of death in the U.S. According to the Centers for Disease Control and Prevention (CDC), one in five deaths is the direct result of heart disease. While heart health should be a priority all year round, take a few extra minutes to learn something new about heart disease prevention this February.
Heart disease is an umbrella term for certain heart conditions. Included on this list is the most common heart disease in this country–coronary artery disease (CAD). It is sometimes called ischemic heart disease.
CAD involves plaque buildup in the arteries that feed blood to the heart. This build-up reduces blood

flow to this critical organ, preventing proper oxygenation.
For individuals with CAD, the first significant sign of illness is often a heart attack. Angina or chest pains are potential heart attack symptoms, but not everyone experiences them.
Other conditions associated with heart disease include arrhythmias, congenital disabilities, and heart valve disease. CAD and other conditions that fall into the heart disease category can lead to myocardial infarction, heart death, stroke, and blood clots.
Heart disease is a condition that does not discriminate. It impacts men, women, and all ethnic and racial groups. It does tend to hit some demographics harder, though. For example, 47% of black men develop cardiovascular disease, while it impacts only about 36% of white men.
Health disparities such as this continue to challenge healthcare professionals in complex ways. Social constructs such as socioeconomic status, access to healthcare, and food deserts tend to have a more significant impact on minorities.
Certain groups are more likely to develop risk factors for heart disease, as well. Rates of hypertension or high blood pressure are highest in the black community. Hypertension is the most significant risk factor for cardiovascular disease.
Black women are particularly susceptible to hypertension. However, it is Asians that most often have untreated high blood pressure.

There is also a slight gender gap associated with heart disease. The prevalence of heart conditions is lower in women. However, there is some indication that women may be more likely to downplay the symptoms of cardiac disease, leaving it undiagnosed.
“Heart
disease
is an
umbrella term for certain heart conditions. Included on this list is the most common heart disease
in this country–coronary artery disease (CAD).”
Lifestyle changes can be significant in heart disease prevention strategies. With a new year comes renewal and new chances. Take advantage of that ambitious spirit to develop a heart healthy lifestyle. A 2023 narrative review published in Cureus recognized the impact lifestyle modifications can have on cardiovascular disease. The study authors emphasize diet, physical activity, sleep, stress, weight, and smoking all influence heart health.
Keep in mind a heart-healthy diet can make a significant difference. It’s all about lowering those low-density lipoprotein levels in the blood, which create plaque in arteries. Shift your focus to nutrient-dense foods and portion control for the new year. The Mediterranean and DASH diets top the list for recommended dietary patterns.
Create time for exercise to lower blood pressure. The recommended amount of physical activity is 150 minutes of moderate-intensity cardio exercise. The CDC also suggests at least two days of muscle-strengthening exercise each week.
The CDC estimates that one in three people does not get adequate sleep, and chronic sleep deprivation can seriously impact heart health.
Being overweight increases your risk of heart disease by 28%. People who are overweight tend to have many risk factors at once, including high blood pressure, high blood sugar, high blood triglycerides, and low HDL cholesterol levels.
Having high levels of cortisol for long periods of time can increase risk factors for heart disease, such as high blood pressure and cholesterol levels.
One in every four cardiovascular-related deaths involves a smoker. Secondhand smoke puts the people around you at risk of heart disease. As American Heart Month approaches this year, consider your risk factors for heart disease. At the same time, map out a plan to increase awareness of lifestyle changes that reduce the risks and create prevention strategies that will make your heart healthier.

In the spring of 2024, Maryland passed a groundbreaking law known as the Bailey Bullock Act.
This legislation, signed by Governor Wes Moore, mandates that all schools—public and private—implement cardiac emergency response programs. These programs include the presence of automated external defibrillators (AEDs), regular CPR training, and emergency response drills.
This represented a monumental public health improvement for Maryland students, but for Patrice Bullock, a board-certified Family Nurse Practitioner, this achievement was a deeply personal one.
Her son, Bailey, was a vibrant and ambitious young athlete at John Carroll School in Bel Air, Maryland. A natural talent, he excelled in basketball, football, and track, with dreams of going pro. Patrice recalls Bailey’s drive and determination with pride. “He wanted to play professional sports, and I have no doubt he would have achieved his dreams if his life hadn’t been cut short.”
Bailey tragically passed away after suffering a sudden cardiac arrest following a track and field event on May 2021. He was only 16. It was a moment that changed Patrice’s life forever.
Bailey was diagnosed early in life with Wolff-Parkinson-White (WPW) Syndrome, a condition where an extra electrical pathway in the heart triggers rapid heartbeats, which
By Daine Taylor
can cause symptoms like palpitations, dizziness, fatigue, chest pain, and fainting.
She recalls that due to a lack of care and necessary resources, her son “didn’t receive CPR for over eight minutes…That’s just unacceptable.”

In the aftermath of Bailey’s passing, Patrice channeled her pain into purpose. She founded Bailey’s Heart and Soul Foundation with a clear mission: to raise awareness about heart health and equip communities to respond effectively to sudden cardiac emergencies. “The foundation focuses on screening for cardiac risk factors that could potentially lead to sudden cardiac arrest, such as cardiomyopathy and hypertrophic conditions.”
She emphasizes the importance of immediate action during cardiac emergencies and being prepared for the worst in any foreseeable situation. “We provide training on CPR and how to use an AED, and we stress the importance of the response time factor when someone collapses. Treat every collapse as a cardiac emergency and start CPR right away. CPR can double and sometimes triple the chances of survival in sudden cardiac arrests.”
One of the foundation’s core missions is to educate parents about monitoring their children’s heart health, particularly those involved in sports. “Parents need to ensure their kids are getting comprehensive physicals, especially if there’s a family history of cardiac issues,” Patrice advises.
She also highlights the critical role of coaches in safeguarding young athletes. Parents should ask essential questions: “Are the coaches CPR-certified? Do they have an AED on hand? Do they know the steps in responding to a cardiac emergency?”
Patrice urges parents to teach their children to advocate for their own health, and for teachers and coaches to be more receptive as children may not know exactly how to articulate how they’re feeling. “If a child says, ‘I don’t want to participate in sports today,’ it might not be laziness—it could be a health concern. Coaches need to listen to these signs and communicate with parents to ensure timely follow-up.”
The American Heart Association’s 2022 report revealed that cardiac arrest is a major public health crisis, with over 356,000 out-of-hospital cases annually in the U.S., nearly 90 percent of which are fatal.
The passage of the Bailey Bullock Act marked a major milestone in Patrice’s advocacy journey. “As a community, how do we respond to emergencies? Are we prepared? This act helps ensure we are,” she explained. “The act requires
schools to have cardiac emergency response programs, conduct drills, and review their effectiveness afterward.” These measures ensure that schools are better prepared to handle emergencies, providing a layer of protection for Maryland students.
Sen. Ben Brooks of Baltimore County and Del. Jessica Feldmark of Howard County sponsored the legislation, which was approved unanimously by both chambers of the General Assembly.
Beyond legislative changes, Bailey’s Heart and Soul Foundation encourages community involvement. Patrice advocates for participation in cardiac screenings, CPR and AED marathons, and certification programs. “Knowing the survival chain can save a life,” she said.
The chain of survival outlines crucial steps to improve cardiac arrest outcomes: recognize the emergency, call for help, perform CPR, use an AED, and provide advanced and post-cardiac arrest care.
Prompt action can be vital, as survival chances drop with every minute of delay, and anyone can help, even without medical training. She also reminds the public of the Good Samaritan Act, which protects individuals who step in to help during emergencies. “It’s better to start CPR than not to start at all. The brain only has about four minutes before irreversible damage occurs, so responding timely can make all the difference.”
While her foundation focuses on young athletes, Patrice is quick to point out that heart health is a universal concern. “Heart issues not only impact adolescents and young athletes but also older adults and minority communities, who are at higher risk for heart attacks, high blood pressure, and other cardiac-related diseases.”
She urges people of all ages to be proactive about their heart health. “Stay active, follow the DASH diet, limit nicotine intake, and prioritize regular screenings,” she advises. The Dietary Approaches to Stop Hypertension (DASH) diet promotes heart health by emphasizing fruits, vegetables, whole grains, and low-fat dairy while limiting salt, sugar, and saturated fats.
Bailey Bullock would have been 20 years old today at time of writing, and his mother’s work ensures that his legacy lives on—not just in the hearts of those who knew him, but in the lives that her advocacy is saving.
Bailey’s Heart and Soul Foundation stands as a beacon of hope, reminding communities that preparation, education, and swift action can make all the difference. To learn more about Bailey’s Heart and Soul Foundation and how you can get involved, visit their website.
CARL BAYARD OF ROCKVILLE, MARYLAND, HAS ALWAYS BEEN PROACTIVE ABOUT HIS HEALTH. SO WHEN HE HEARD ABOUT A PROGRAM CALLED DARE TO C.A.R.E. (CAROTID ARTERY, ABDOMINAL AORTA, RENAL ARTERY, EXTREMITY ARTERY DISEASE), WITH THE HEART HEALTH FOUNDATION (HHF), HE DECIDED TO LEARN MORE. THIS INNOVATIVE INITIATIVE, SPEARHEADED BY VASCULAR SURGEON, JOHN MARTIN, MD, MBA, FACS, OFFERS FREE SCREENINGS, EDUCATION, AND OTHER PREVENTIVE STRATEGIES IN THE FIGHT AGAINST HEART DISEASE.
Carl considers himself incredibly lucky. This is because an ultrasound screening he received at HHF revealed a serious hidden health issue - an abdominal aortic aneurysm (AAA). An AAA occurs when the aorta, the body’s largest artery, develops a bulge that gets progressively larger and fills with blood. The American Heart Association aptly describes the aorta as “The Pulse of Life,” carrying oxygen-rich blood to all areas of the body.1
There are times when an AAA grows larger and starts to leak or rupture, starving blood vessels and causing life-threatening internal bleeding. The scary thing is that most AAAs are completely asymptomatic,2 meaning that patients aren’t even aware of the problem until they’re rushed to the hospital in a harrowing race against time for emergency medical care. This is why Carl was indeed very fortunate to learn about free cardiovascular screenings offered by HHF.
In Carl’s case, the screening revealed an AAA that was 3.2 centimeters in diameter and growing. Because it had not reached the high risk category of about 5 centimeters, Dr. Martin put him on a preventive strategy of getting ultrasound studies and exams every 6 months. Although his first screening was in 2003, he didn’t have surgery to correct the AAA until 2010, when it had grown to 5 centimeters. Was it hard for him to wait 7 years to have surgery? Not really, says Carl. He had full trust in his doctors and other healthcare professionals at HHF.
Carl is a Korean War veteran who subsequently became a diplomatic courier with the Foreign Service of the US State Department. During this illustrious 35-year career, he delivered top-secret information to American embassies all over the world. It was an often dangerous position in which he experienced a couple of plane crashes and (we’re guessing) other threats to life and limb. These experiences cemented his previous attitude of being very conscientious about his health.
So Carl doesn’t really ‘fit the mold’ of someone who might be at risk for heart disease. Actually, he’s one of those thrill-seekers who loves to hunt, fish, hike, and go camping. He and his wife, who he met in Germany, raised several English Springer Spaniels that joined in on their many outdoor adventures. Talking about exercise!
There are several risk factors for AAA, such as high blood pressure, family history of AAA, tobacco use, and atherosclerosis (hardening of the arteries),3,4 In Carl’s case, he feels that a family history of AAA might have been the culprit.
Worldwide, AAA rupture leads to about 170,000 deaths annually.5 It’s considered a common condition in the US, occurring in about 1.4% of the US population between the ages of 50 and 84, or approximately 1.1 million people.6 This is why Dr. Martin and his colleagues emphasize the extreme importance of early detection of AAA and other cardiovascular diseases.
Carl is a perfect example of the positive impact of early detection. In his case, he was closely monitored and provided with various patient education resources. When it was time for surgery, it involved only an overnight stay in the hospital, going in at 6:00am and leaving by noon the next day. If the AAA had remained undetected, he might have died or been subjected to a long hospitalization and slow recovery. Instead, he went back to his big game hunts and other escapades with his English Springer Spaniels. Go Carl!
Carl’s journey is a testament to the power of proactive health and a positive mindset. With Dare to C.A.R.E. by his side and his unwavering commitment to wellness, he’s proving that longevity is within reach. As he sets his sights on 100, he does so with determination, vitality, and a zest for life. And what about you?
Over 800,000 people die from cardiovascular disease each year, and we don’t want anything like this to happen to you. Take charge of your heart health by staying active, eating well, scheduling regular doctor’s visits, and prioritizing preventive care. Your future self will thank you.
1. American Heart Association. Your aorta: the pulse of life. Last reviewed January 30, 2024. https://www. heart.org/en/health-topics/aortic-aneurysm/your-aortathe-pulse-of-life. Accessed January 10, 2025.
2. Haque K, Bhargava P. Abdominal Aortic Aneurysm. Am Fam Physician. 2022;106(2):165172. https://pubmed.ncbi.nlm.nih.gov/35977132/
3. Cleveland Clinic. Abdominal aortic aneurysm. Cleveland Clinic Last reviewed August 15,

Carl’s journey is a testament to the power of proactive health and a positive mindset. Thanks to early detection, careful monitoring, and trust in his doctors, he turned a life-threatening condition into a story of resilience and longevity.
2023. Available at: https://my.clevelandclinic.org/ health/diseases/7153-abdominal-aortic-aneurysm. Accessed January 9, 2025.
4. Society for Vascular Surgery. Abdominal Aortic Aneurysm. Your Vascular Health. https://vascular. org/your-vascular-health/vascular-conditions/commonconditions/abdominal-aortic-aneurysm. Accessed January 10, 2025.
5. Golledge J, Thanigaimani S, Powell JT, Tsao PS. Pathogenesis and management of abdominal aortic
aneurysm. Eur Heart J. 2023;44(29):2682-2697. doi:10.1093/eurheartj/ehad386
6. Cleveland Clinic. Abdominal aortic aneurysm. Cleveland Clinic. Last reviewed August 15, 2023. Available at: https://my.clevelandclinic.org/ health/diseases/7153-abdominal-aortic-aneurysm. Accessed January 9, 2025.
7. Heart Health Foundation. Home Page. Available at: https://hearthealthfoundation.org/. Accessed January 10, 2025.
HOW A SIMPLE VISIT TO HER SPINE DOCTOR CHANGED EVERYTHING FOR A MARYLAND NATIVE
It was a great day when Maryland native Janet Merica spoke up at her doctor’s office. Initially, she went to her spine doctor because she was having low back pain. This led her to the Heart Health Foundation (HHF) of Maryland and their flagship program called, Dare to C.A.R.E.(Carotid Artery, Abdominal Aorta, Renal Artery, Extremity Artery Disease).
When the people at HHF first met Janet, she could barely walk around the block because of extreme leg pain due to peripheral artery disease (PAD). Today, her life is very different and much better. Let’s learn more about Janet and her successful journey to better health.
| Janet’s Health History

Janet has a family history of both high cholesterol and high blood pressure, and this likely influenced her own risk factors for developing these conditions.1 Sadly, she added to her risk factors by becoming a heavy smoker and having an unhealthy diet. She also developed Raynaud’s Syndrome, Sjogren’s Syndrome, and CREST Syndrome. Although these conditions are different from one another, they all have symptoms that affect mobility, pain, and fatigue levels.
Low back pain due to a bulging disc further affected her ability to get around and perform her daily activities. It became increasingly difficult for Janet to exercise, something she knew was critical in helping her manage her high blood pressure and cholesterol.
When she was 63, Janet went to her spine doctor because she was experiencing extreme low back and leg pain. She’s a school bus driver who works 40 hours per week, and her ability to do her job became increasingly difficult. Although Janet had been having this pain off and on for at least 10 years, somehow, she says, this pain felt different. “It felt like someone was stabbing me in the rear end.”
The initial recommendation from her doctor was to have spinal injections to help relieve the pain. It was a good thing that Janet listened to her body and requested an x-ray, because it indicated arterial blockages in both of her legs - a strong sign of PAD. Janet’s spine doctor was knowledgeable of the HHF and referred her for an immediate screening.
The no-cost sonogram at HHF on both of Janet’s legs indeed revealed PAD. In fact, she only had 30% of the normal blood flow into each of her legs.
It’s estimated that 6.5 million people in the US are living with PAD.5 Although patients with this disease might not have symptoms, they often experience leg pain when walking, cramping in the arms, legs, and calves, and coldness in the lower legs or feet. PAD is often caused by a build-up of fats and cholesterol in the artery walls that blocks blood flow. Complications of PAD if not caught soon enough can lead to stroke, heart attack, and amputation of affected limbs because of tissue ischemia (cell death).
Janet learned from her difficult experience and took the advice of the healthcare professionals at HHF to heart. She quit smoking completely on the day of her surgery! Her recovery has been excellent, and
she returns to HHF every year for checkups and patient education about managing her health. Do you remember how she couldn’t even walk around the block due to leg pain? Well, today she exercises regularly by traversing the many nature trails close to her home - without leg pain. She also still works full-time driving a school bus. Today, at 65, she’s a great example of someone who strives for better health.
According to the American Heart Association, a healthy lifestyle that reduces the risk of heart disease, stroke and other cardiovascular problems involves:
• Lowering cholesterol and blood pressure
• Having a healthy diet
• Staying away from tobacco products
• Improving well-being
• Getting enough sleep
We asked Janet if she had any advice for the rest of us about taking care of ourselves. Her first recommendation is to never start smoking. Second, it’s important to listen to our bodies. Being attentive to the type of pain we have and how we’re feeling helps us communicate better with our doctors.





Join us as we expand our reach across the DMV, to include Washington, DC, and Virginia! Maryland Health Magazine is not just a publication; it’s a powerful educational resource dedicated to fostering lasting health transformations.
Our readers seek insights on weight management, balanced nutrition, preventative care, chronic diseases, dental care, fitness and health screenings, making it the perfect platform for your brand.
We deeply appreciate the support and feedback from our readers and partners, and we’re committed to promoting health, wellness & fitness throughout the DMV.
Partner with us as an advertising or marketing partner to connect with an engaged audience eager for valuable health content. DEADLINE FOR APRIL/MAY EDITION IS FRIDAY MARCH 21, 2025 12:00 NOON.

It’s not just about what you eat; how much you eat also matters. For example, the proper serving size for a piece of meat is about two to three ounces. That’s about the size of a deck of cards. If you eat more than that, you are increasing your caloric intake and reducing the effectiveness of your diet.
An easy trick for managing portion sizes is to:
• Fill one-half of your plate with healthy vegetables.
• Fill one-fourth with a lean protein, plant, or animal
• Fill the final one-fourth with healthy carbohydrates such as whole grains or fruit.
If you eat just a single item, use a small plate or bowl.
Your heart has a thankless job. It tirelessly pumps blood, nutrients, and oxygen throughout your body. Certain factors put a strain on this critical organ, such as:
• High blood pressure
• High cholesterol
• Inflammation
• Poor circulation
• Obesity
Many of these risk factors are preventable with healthy lifestyle choices.
Key Contributors to a Heart-Healthy Diet
Harvard Health states that people who follow the proper diet consistently will lower their risk of heart disease by 31%.
A heart-healthy diet starts with plenty of fruits and vegetables, whether fresh, frozen, or canned. Fresh is always the best choice but check the ingredients if you choose frozen or canned. They should be low in sodium and have no added sugar.
Fat has a flawed reputation, but it’s not all bad. Healthy fats like omega-3 fatty acids lower bad cholesterol (LDL) levels, increase good cholesterol (HDL), and reduce your risk of cardiovascular diseases.
Healthy fats include:
• Vegetable or nut oils
• Olive oil
• Canola Oil
• Nuts
• Seeds
• Avocados
• Oily fish, such as salmon
Simply replacing saturated fats, like those in butter, with unsaturated fats like margarine helps lower blood cholesterol levels.
Along those same lines, you want to avoid fatty cuts of meat and opt for lean choices such as skinless chicken or fish.
A practical approach to a low-fat diet is to:
• Choose low or nonfat dairy products
• Eat fatty fish such as salmon or tuna twice a week
• Substitute plant proteins such as legumes or soy for a couple of meals a week
• Choose ground meat instead of steaks
• Avoid fried and breaded foods
Eating plant protein instead of animal, even for a few meals a week, will help keep you on track. More plant protein will also increase your fiber intake.
Fiber is a critical nutrient in preventing heart disease. It lowers the amount of bad cholesterol your body absorbs from food. Studies also show that it helps fight inflammation. Harvard Health suggests a fiber-rich diet may reduce your risk of heart attack or stroke by as much as 30%.
Whole grains, fruits, vegetables, legumes, nuts and seeds are good sources of fiber.
When it comes to heart health, what you don’t eat is as important as what you do. Brown Health states unprocessed foods like sausage, bacon, and hot dogs are among the top things to avoid. They tend to be high in sodium and unhealthy fats.
Fried foods also make the list. Those French fries you get at the drivethrough are likely full of saturated and trans fat.
Add sugary foods to that list, as well. That would include soda and breakfast cereals.
For many, baked goods are the most painful thing they must avoid. Cookies, cakes, and pastries contain high amounts of sugar and fat. Don’t be afraid of the rare treat, though. Eating right isn’t about restrictions—it’s about making mindful daily choices that protect your heart and overall health. By prioritizing whole, nutrient-dense foods, incorporating healthy fats and fiber, and managing portion sizes, you are being proactive about your heart health.

BY DARLA FRISK
When it comes to oral surgery, Dr. Larry Bryant is a name synonymous with precision and compassion. As the Chief of Facial Trauma at the new University of Maryland Capital Region Medical Center in Largo, Dr. Bryant is there for patients during one of the most devastating times of their lives. He and his skilled team are on call 24/7 to this Level II trauma center for facial reconstruction and treatment.
At his practice, Bryant Oral & Facial Surgery, the specialty is dentoalveolar surgery, or the surgical treatment of the teeth, jawbone, and surrounding soft and hard tissues. Dr. Bryant has become one of Maryland’s leading oral and maxillofacial surgeons by providing patients with the highest standard of care, state-of-the-art services, and innovative treatment options.
| Developing the Passion
As a predental student in 1975, Larry Bryant attended Harvard University’s summer program. He knew at this point that he wanted to go to dental school but didn’t understand the unique specialties available to him.
During a rotation at Massachusetts General Hospital, he developed his passion for surgery. He was able to interact with surgeons who specialized in the treatment of the jaw and face, and he understood his calling. He graduated with honors from Howard University College of Dentistry. Bryant then completed his oral and maxillofacial surgery training at Woodhull Medical and Mental Health Center in New York and a
fellowship program in orthognathic surgery and dental implantology at Montefiore Medical Center.
For the past two decades, Dr. Bryant has been at the helm of his highly respected oral surgery practice in the Bowie-Mitchellville area of Prince
George’s County, Maryland. His practice is known for its family-centered approach, combining state-of-the-art technology with compassionate, patient-focused care: Bryant and his staff service patients in Maryland, DC, and Virginia.


GLENN DALE. MD
301-249-0553
| TeethXpress: The Promise of Innovation
“Technology has revolutionized dental care,” according to Dr. Bryant. A good example is the TeethXpress Implant services offered in his practice. TeethXpress allows replacing an entire arch using four to six implants and a hybrid prosthesis. And it is done in one day.
TeethXpress is a revolutionary alternative to traditional dentures. It provides a permanent, stable, and natural-looking solution for full-arch tooth replacement—replacing all 12 teeth from the incisor region to the molars. Unlike conventional dentures, which can be uncomfortable, slip while eating or speaking, and require messy adhesives, TeethXpress secures a complete set of prosthetic teeth using strategically placed dental implants.
Additionally, TeethXpress preserves jawbone health by stimulating bone growth, preventing the bone loss that often occurs with removable dentures. The procedure is completed in just one day, allowing patients to leave the office with a fully functional, confident smile—no waiting, no multiple visits, and no dietary restrictions.
Dr. Bryant and his team at Bryant Oral & Facial Surgery harness cutting-edge technology to provide same-day dental implants for their patients. The process begins with Cone Beam Computed Tomography (CBCT) right in the office, a capability that sets Dr. Bryant apart from other oral surgeons.

Unlike traditional X-rays with a two-dimensional view, CBCT scans allow the oral surgeon to see detailed cross-sections of the mouth from multiple angles, ensuring more precise diagnostics and treatment planning. With this advanced imaging technology, the lab can craft a custom prosthetic tailored during the implant procedure, providing patients with a seamless experience and optimal results.
| Who Is a Good Candidate for TeethExpress?
“The ideal candidate for TeethXpress is someone who is just losing the teeth and has enough bone to place the implants,” explains Dr. Bryant. “It might not work as well for someone who lost their teeth some time ago.”
A patient’s overall health is another key in determining whether dental implants are the right option for them. Certain conditions, such as uncontrolled diabetes, can pose risks and may disqualify a candidate. However, those with stable blood sugar and well-managed diabetes can still be eligible for implants.
In addition, Dr. Larry Bryant visits Malawi, one of the poorest countries in the world, once a year. As part of the Smiling Surgeons’ Team, he and his colleagues treat patients with advanced oral diseases and tumors

of the jaw and face in this small country in Africa. Malawi currently has just one oral surgeon in the country to care for more than 22 million people.
Dr. Bryant loves playing with his grandchildren and when not providing oral care services. He is also an avid swimmer and a member of his church management team.
Dr. Larry Bryant’s commitment to dental health extends beyond the walls of his practice. Whether performing complex facial trauma surgeries, providing cutting-edge dental implant technology, or giving much-needed critical care to underserved communities abroad, Dr. Bryant sets the standard for oral and maxillofacial surgery.
BY BARBARA FORMAN
eart attack, stroke, and other forms of cardiovascular disease cause more deaths than any other type of illness. The crazy thing is that many of these deaths could be prevented with early detection and simple lifestyle changes.
Now doctors have more diagnostic tools than ever to help establish viable treatment plans. Radiology has come a long way in the last 30 years. Simple, non-invasive procedures are now available that allow doctors to accurately diagnose many types of heart disease in their earliest stages.
Doctors can now detect subtle shifts in heart function that can be addressed before serious health problems develop. This groundbreaking technology goes beyond being state-of-the-art, it enables physicians to observe life in real-time. Presenting opportunities that many thought were unattainable. It exemplifies the pinnacle of early detection. In the realm of cardiovascular health, it has truly transformed the landscape.

“Our mission is to provide the highest quality medical imaging available,
delivering unparalleled, uncompromising service to our patients, our referring doctors, and our community.”
Located in Maryland, Chesapeake Medical Imaging has set the standard for radiology in the Mid-Atlantic Region. With 13 locations, 15 doctors, and 175 support staff members, Chesapeake Medical Imaging is the leader in its field. Staff at Chesapeake Medical Imaging offer a level of patient care that is unmatched. Every patient has access to the highest quality care and the most advanced technology
available. They are able to play an active role in every aspect of their treatment giving them an added incentive to make positive lifestyle changes in every aspect of their treatment.
Chesapeake Medical Imaging offers all types of radiology services, including MRI, CT scans, mammography, ultrasounds, and stereotactic breast biopsies that are essential to women’s
health and wellness. Its shining star, however, is the cardiovascular imaging service. Cardiovascular imaging has advanced to the point where many exams are now mostly non-invasive and capable of providing high-quality images. It gives doctors an opportunity to see inside the heart and blood vessels in a way that was only dreamed of in the past. They are also able to watch the organs as they work.
In the past, doctors were forced to use heart catheters to get the most accurate look inside the heart and blood vessels. This was an invasive procedure that held many risks for the patient and a limited view for the doctor. With the cardiovascular CT scan, doctors can now get the most accurate non-invasive predictor of heart attack risk us the CT calcium score. For a
more detailed view of coronary arteries the coronary CT angiogram is now often used in place of heart catheterization. These non-invasive procedures offer minimal risk to the patients. Patients with a history of heart disease can be closely monitored for any potential signs of distress or concern. By watching the heart function and the blood
flow through the vascular system, the doctors can pinpoint problem areas with maximum accuracy and minimum risk. Finding these problems in their earliest stages opens the door to more treatment options and fewer long-term health issues. Simply stated, early detection saves lives and improves quality of life.
Dr. Mark Baganz, MD Founder and Medical Director, has over 20 years of experience working with radiology. He has witnessed firsthand the advancements of cutting-edge technology and how it has played an integral role in saving lives. While he started out in neuroradiology, he quickly discovered how radiology could be used to assist with finding an accurate diagnoses and creating a more effective treatment in the field of Cardiology.
During his time working with neuroradiology, he was introduced to the latest radiological tests for the cardiovascular system. He was fascinated by what he referred to as the “gee whiz” factor. By using these CT scans and other highly advanced procedures, he could literally see inside the heart and blood vessels. He could monitor blood flow and calculate the amount of calcium buildup in the blood vessels. Chesapeake Medical Imaging is using cardiovascular radiology to improve heart

DR. BAGANZ Founder and Medical Director, Chesapeake Medical
health and change the lives of its patients. Dr. Baganz and the dedicated staff at Chesapeake Medical Imaging are committed to excellence and providing the quality of care that exceeds the expectations of their patients.
Patient satisfaction is always the goal they strive for. This new technology is able to dramatically enhance the quality of care each patient receives and will improve the quality of life for those in Annapolis County, Prince George’s County and throughout Maryland. When patients arrive at the facility, the staff does everything in their power to ensure the patient’s diagnostic needs are met in every way. Whether they are being evaluated for possible heart disease or have already received a diagnosis and are working on a treatment plan, they always receive the highest quality of care. They leave the facility with the most accurate information possible when it comes to their cardiovascular health. Advancements in the field of radiology give the staff of Chesapeake Medical Imaging all the information they need to change lives one heartbeat at a time.
CHESAPEAKE MEDICAL IMAGING SCHEDULING: 855-455-8900
WWW.CMIRAD.NET

BY NADYA CLARKE, MD
AS A BOARD-CERTIFIED PLASTIC SURGEON, I’VE SEEN AESTHETIC TRENDS IN PLASTIC SURGERY EVOLVE EVERY FEW YEARS. ALTHOUGH THIS CAN BE REGION SPECIFIC, THERE HAS BEEN AN OVERALL DIVERGENCE FROM EXTREME MAKEOVERS AND A NEW EMPHASIS ON SUBTLE AND NATURAL APPEARING ENHANCEMENTS THAT REFINE AND REFRESH NATURAL BEAUTY. THIS SHIFT REFLECTS CHANGING BEAUTY IDEALS, ADVANCEMENTS IN SURGICAL APPROACHES, AND A GROWING DESIRE FOR GRACEFUL, UNDETECTABLE RESULTS.
SHIFT IN BEAUTY TRENDS
Much like the shift towards “quiet luxury” in the fashion world, there has been a rise in aesthetic procedures that whisper rather than yell. This shift is partly driven by once-secretive celebrities now openly sharing their experiences of scaling back exaggerated surgical results. Stories of famous figures dissolving aggressive facial filler, downsizing breast implants, or reversing overstated buttock augmentation have been common recently. Patients now seek refinement of their natural beauty rather than drastic overhauls.
THE RISE OF SUBTLE PLASTIC SURGERY ENHANCEMENTS
With patients now desiring to look like refreshed versions of themselves, advanced non-surgical, minimally invasive and sophisticated surgical techniques have emerged.
Botox , a neurotoxin widely used for its ability to temporarily relax muscles and smooth wrinkles and fine lines in the forehead, brow, and crows feet, has surged in popularity. The term "baby Botox" (small doses of Botox for subtle wrinkle reduction) has also gained popularity.
Dermal fillers address volume loss in the cheeks and lips, contour the jawline, and smooth fine lines. The application of these products has evolved to mimic the natural volume distribution of youth,
rather than indiscriminate filling of the face. My approach prioritizes minimal product for maximum impact, using precise placement and a layered technique over multiple sessions for better control and a more natural result.
Micro fat grafting of the face is similar to dermal fillers for facial rejuvenation; however, fat is harvested via liposuction from an area, and injected as a permanent solution to volume loss. Liposuction, a procedure that removes excess fat from specific areas, now prioritizes refining the treated area without over suctioning, preserving delicate contours — especially in areas like the abdomen.
Smaller Breast Implants that are more harmonious with a patient’s frame have taken the place of excessively large implants.
Body contouring procedures, such as tummy tucks and arm and thigh lifts, have become more common with the rise of weight loss medications, and demand for inconspicuous scars and naturally appearing belly buttons has reached an all-time high.
The new era of plastic surgery is highly personalized, and is all about refinement, balance, and subtlety. This shift signals a positive change, one that
celebrates individuality and beauty in its most authentic form. As a plastic surgeon, my focus is on customizing treatments to fit each patient’s individual needs, rather than following a one-size-fits-all standard of beauty. This patient-centric approach ensures results that blend seamlessly with an individual’s natural features. The focus remains on enhancing confidence rather than altering identity.

BOARD CERTIFIED PLASTIC AND RECONSTRUCTIVE SURGEON OWNER, BESPOKE AESTHETIC PLASTIC SURGERY
3202 Tower Oaks Blvd Suite 200 Rockville, MD 20852 (301) 500-00215
www.bespokebeautymd.com bespokebeautymd@gmail.com @nadyaclarkemd

SLEEP APNEA, A COMMON BUT FREQUENTLY UNDIAGNOSED CONDITION, IS MORE THAN JUST A SLEEP DISORDER. ITS FAR-REACHING EFFECTS TOUCH NEARLY EVERY ASPECT OF HEALTH AND WELL-BEING.
Beyond causing restless nights and chronic fatigue, sleep apnea is a significant contributor to systemic health issues such as cardiovascular disease, diabetes, and weight gain. These complications often develop silently, as the condition’s symptoms can be subtle or easily overlooked.
While much attention is given to the respiratory challenges associated with sleep apnea, its connection to dental health remains an underappreciated yet critical aspect of diagnosis and treatment.
By examining the oral health indicators and understanding the broader implications of sleep apnea, patients and healthcare providers alike can take a more comprehensive approach to managing this pervasive condition.
| How Common Is Sleep Apnea, & Why Is It Often Undiagnosed?
Sleep apnea is more prevalent than many realize. For Dr. Edward H. Chappelle, Jr., DDS, one of the most pervasive issues his patients face stem from sleep apnea.
“You’d be surprised at how many people are walking around that you know have issues because of diabetes and the undiagnosed sleep apnea,” Chappelle said.
In fact, according to the American Medical Association about 30 million people in the United States have sleep apnea, but only 6 million are diagnosed. The condition often goes unrecognized because the body adapts to its symptoms, allowing individuals to function despite underlying health challenges.
One of the lesser-known impacts of sleep apnea is its role in disrupting the body’s natural repair mechanisms. During sleep, the body produces hormones such as cortisol, which are crucial for regulating stress and metabolism. However, sleep apnea can lead to an overproduction of cortisol, contributing to weight gain, cardiovascular problems, and other health issues.
Without proper rest, the body’s ability to heal and function optimally is compromised.
| What’s the Link Between Sleep Apnea & Dental Health?
Sleep apnea can also significantly impact dental health. Mouth breathing during sleep often leads to dry mouth, which reduces saliva production and increases the risk of cavities, gum disease, and bad breath.
Teeth grinding, or bruxism, is another common issue associated with sleep apnea, potentially causing tooth wear,
fractures, and even tooth loss. This grinding can strain the jaw, resulting in temporomandibular joint (TMJ) disorders and associated pain. Jaw misalignment and cheek biting during sleep can exacerbate discomfort, while headaches often arise from both teeth grinding and TMJ disorders.
Dentists play a key role in identifying the signs of sleep apnea. One common indicator is teeth grinding, or bruxism. “People who have sleep apnea have a tendency to grind their teeth,” Chappelle explained. “You can see signs like wear facets on teeth, which show they’ve been rubbing together.”
Teeth grinding is one of the body’s reflexive responses to obstructed airways, as it helps stimulate the muscles needed to open the airway during sleep.
“It’s basically an airway issue,” Chappelle said. “The question is, what is the cause of that diminished airway? Is it that the tongue falls back? Is it that the tongue is large? Is it that you can’t breathe through your nose?”
These structural factors often start in childhood and, if untreated, persist into adulthood
The effects of untreated sleep apnea extend far beyond snoring and daytime fatigue. By disrupting normal sleep cycles, the condition prevents the body from achieving the deep, restorative sleep necessary for overall health.
Over time, this lack of quality sleep can lead to serious systemic issues. For instance, the overproduction of cortisol—a stress hormone linked to poor-quality sleep— hinders weight loss and promotes fat storage, often resulting in weight gain.
Cardiovascular disease is another major concern, as interrupted breathing during sleep places significant strain on the heart and blood vessels, increasing the risk of heart attack and stroke.
Additionally, poor sleep quality affects insulin sensitivity and glucose regulation, which can worsen or even contribute to the onset of diabetes.
Understanding the symptoms of sleep apnea early can empower individuals to seek timely diagnosis and treatment, improving overall well-being.
For more insights into health and wellness topics that can impact you and your community, subscribe to Maryland Health Magazine today. Stay informed and take charge of your health journey with expert advice and the latest updates delivered directly to you.

DR. EDWARD CHAPPELLE, JR., DDS
Bowie Dentist



For many individuals, losing weight can seem like a daunting, lifelong challenge. Maybe you’ve gone through numerous diets, injections, dedicated hours at the gym, yet the scale remains stubbornly unchanged. This journey can be incredibly frustrating, disheartening, and often feel isolating. However, it’s important to recognize that the weight loss process and results can vary greatly from person to person.
Success lies in finding what works for you, and that starts with understanding the challenges you’ll face and options available.
Losing weight is rarely a straight path—it’s filled with ups, downs, and unexpected obstacles. Many people start strong, only to hit frustrating roadblocks that make progress feel impossible.
One of the most frustrating aspects of weight loss is hitting a plateau. You’ve been diligent with your efforts, but suddenly, the progress stops. It’s easy to feel like giving up but making a few small adjustments can often help you break through. Reassess your habits—small changes in portion sizes or activity levels may be stalling progress. If needed,
safely reduce calories without dropping below 1,200 per day. Increase exercise, aiming for at least 150 minutes of aerobic activity weekly, and add strength training to boost calorie burn. These tweaks can help you push past the plateau and keep seeing progress.
Emotional eating is another common hurdle, as stress, boredom, or even celebrations can lead to mindless overindulgence. Breaking this cycle requires awareness—recognizing triggers, finding alternative coping strategies, and fostering a healthier relationship with food. Provide healthier alternatives for when you’re feeling snackish, and remove some of the more tempting treats that may lead you astray.
Support can also be key in overcoming emotional eating. Without a strong support system, it’s easier to turn to food for comfort. Lean on friends and family, or consider joining a support group where you can share struggles, gain motivation, and stay accountable on your journey.
Maintaining your weight loss goals can often be even more challenging than shedding pounds in the first place. Strict, short-term diets often lead to yo-yo dieting, making longterm success difficult. The most effective approach is one that prioritizes balance, consistency, and lifestyle changes you can maintain for life.
The path to weight loss looks different for everyone, and success often depends on finding the approach that fits your lifestyle, goals, and circumstances.
Take, for example, Jessica from Annapolis, a busy mom of two who realized that incorporating exercise into her life didn’t have to mean long hours at the gym. She started with daily walks at Quiet Waters Park, eventually adding strength training at home. For her, the key was finding something enjoyable and manageable exercise became less of a chore and more of a stress reliever.
Meanwhile, Mark of Baltimore struggled with his eating habits. Years of trying restrictive diets left him feeling frustrated and defeated. With the help of a dietitian, he learned to focus on small, sustainable changes, like portion control and incorporating more whole foods into his meals. Mark’s approach wasn’t about eliminating all his favorite foods but finding a balance that worked for him.
Then there’s Lena, who, after battling obesity for years, spoke with her doctor about FDA-approved weight loss medications. While skeptical at first, she discovered that the medication helped manage her appetite and gave her the boost she needed to stay consistent with her healthier habits. It wasn’t a cure-all, but it was an effective tool when paired
with her commitment to making long-term lifestyle changes. Lastly, we have Priya, who knew she needed to make broader lifestyle changes. She focused on mindful eating, ensuring she was fully present during meals to recognize hunger and fullness cues. She also prioritized getting more sleep and reducing stress through yoga and meditation. These foundational changes supported everything else she was doing to lose weight and maintain her results.
While their stories are different, they each shared one thing in common: they each found a method tailored to their needs and circumstances.
There’s no universal solution, and each step forward—no matter how small—counts as progress.
Factors like age, health conditions, genetics, and lifestyle all play a role in determining what approach will work best for you. That’s why working with professionals—whether it’s a dietitian, personal trainer, or doctor—is so valuable. They can help tailor a plan that aligns with your needs and goals. Remember, trial and error are part of the process. If something doesn’t work, it doesn’t mean you’ve failed; it means you’ve learned something about yourself.
Weight loss is as much a mental journey as a physical one. A positive, resilient mindset can make all the difference. Instead of focusing on setbacks, view them as opportunities
“Weight loss is as much a mental journey as a physical one. A positive, resilient mindset can make all the difference.”
to adjust and improve. Celebrate your progress, no matter how small, and remember that consistency matters more than perfection.
The path to weight loss isn’t linear, and it’s rarely easy. But it is possible, and it starts with finding the approach that works for you. Be patient, be kind to yourself, and don’t be afraid to ask for help. Your journey is unique, and every step forward, no matter how small, is a step toward a healthier, happier you.
Take the first step today—whether it’s taking a walk, meal prepping, or scheduling an appointment with a healthcare professional. You’re not alone in this journey, and you have the power to succeed.
BY DAINE TAYLOR

Whether it’s missing out on conveHearing loss is a significant issue affecting millions of Americans, and Maryland is no exception. According to data from Johns Hopkins University and the CDC, about 15 percent of adults in Maryland experience hearing loss, with prevalence increasing sharply with age. Nearly 60% of adults over 70 face hearing challenges, yet only 20 percent of those affected use hearing aids.
Whether it’s missing out on conversations, struggling to hear your favorite music, or feeling isolated in social settings, untreated hearing loss can take a toll on emotional and mental well-being. For adults, the financial burden of hearing aids has been one of the most significant barriers to treatment, with
the cost of these devices often ranging from $2,500 to $8,000 per pair.
But now, a new law is changing the game for state residents.
While previously, insurance coverage in the state was mandated only for children under 19, beginning January 2025, Maryland’s House Bill 1339 and Senate Bill 778 extend this benefit to adults.
“At the moment, the biggest challenge [to access] is cost…If this law does what we hope it will do, it will greatly increase accessibility to hearing healthcare for everyone,” said Pamela Dr. Rebecca Jahed, Clinical Audiologist, for Freedom Hearing Center, a medical-based hearing care practice with locations
across Maryland. “Hearing healthcare is an important part of overall health and wellbeing and we truly believe that everyone should have access to hearing devices when needed.”
The new mandate requires insurers, nonprofit health service plans, and HMOs to cover up to $1,400 per hearing aid every 36 months. Individuals can also choose higher-priced devices and pay the difference without penalties to providers.
This change also aligns with broader efforts to make hearing aids accessible to everyone. In 2022, the FDA introduced over-the-counter hearing aids for mild to moderate hearing loss, offering an affordable option for those who don’t require prescription devices. However, over-the-counter devices aren’t suitable
“Hearing healthcare is an important part of overall health and well-being, and we truly believe that everyone should have access to hearing devices when needed.”
Pamela McIntyre, Director of Operations for Freedom Hearing Center
for everyone, particularly those with more severe hearing loss.
This expansion addresses a critical gap for older adults, as hearing loss increases sharply with age. Approximately 6 in 10 adults over 70 experience hearing loss. With this change, many can now afford devices that can enhance their quality of life, improve communication and potentially reduce risks like social isolation and cognitive decline. By addressing financial and accessibility barriers, this legislation helps ensure that all residents can get the care they need. If hearing loss has been holding you back, now is the time to take the first step toward better hearing health.
Marylanders looking to benefit from the new law should start by reviewing their insurance plans.
“This is Maryland state legislation, which should not affect federal programs so Medicare and any government insurance would not be impacted by the new law,” said Dr. Jahed. “Since there are so many different insurances in Maryland and insurances renew on an annual basis, this will affect each person differently.”
This coverage applies only to hearing aids prescribed, fitted, and dispensed by licensed audiologists. Schedule a hearing test if you’re experiencing difficulties, and they can evaluate and determine whether hearing aids are appropriate for you.
Check your current benefits to understand how the new law applies and contact your insurance provider or consult your HR department if you’re covered under an employer-sponsored plan. Call the number on the back of
your insurance card to understand how the new law applies to your coverage. Key questions to ask include:
• Does my insurance plan provide the $1,400 benefit per ear?
• When will I be eligible for this benefit?
• Am I required to use a third-party provider associated with my insurance, or can I work with any audiologist of my choice to access this coverage?
Hearing aids are not just medical devices; they are vital tools for enhancing quality of life. By improving communication and reducing the risks associated with untreated hearing loss, Maryland’s expanded coverage empowers residents to stay engaged with their communities and lead healthier lives.
“People can be leery to have their hearing tested assuming that audiologists just want to sell hearing aids. The truth is we just want to help people. There are many things that can contribute to hearing loss including medication, certain medical conditions and genetics, and the longer one goes without treatment the harder it can be to adjust to hearing devices,” said Dr. Jahed.
“Our clinic works with multiple manufacturers that provide FDA approved prescription devices with a range of price points. We do our best to help our patients with financing options and even have a program where we donate devices twice a year to someone in our local community.”
With expanded coverage, there’s no better time to reconnect with the world around you. You can reach out to Freedom Hearing Center today for guidance and support through the entire process.

Prince Frederick Office 135 West Dares Beach Road, Suite 102 Prince Frederick, MD 20678 443-295-7555
Waldorf Office 3475 Leonardtown Road, Suite 102 Waldorf, MD 20601 443-374-8432
Solomons Medical Center
14090 H.G. Trueman Road, Suite 1400 Solomons, MD 20688 443-295-7100
Greenbelt Office
7247 Hanover Parkway, Suite A Greenbelt, MD 20770 443-295-7555
Leonardtown Office
41660 Courthouse Drive, Suite 301 Leonardtown, MD 20650 443-295-7100, Option 5
www.freedomhearing.com

DR. REBECCA JAHED, CLINICAL AUDIOLOGIST