April 16, 2025
Compliance4U newsletter provides you with insight into the day-to-day functions of the Health Plan’s Compliance Program.
Regulatory Affairs & Communication (RAC)
Welcome to the Compliance RAC SLA series, where we delve into Service Level Agreements (SLAs) frequently encountered in daily operations. In this first installment, we will focus on the Compliance Inquiry Log, an important tool for efficiently managing compliance and regulatory inquiries.
The Compliance Inquiry Log serves as a centralized platform for submitting compliance or regulatory questions, as well as documents required for regulatory submissions. This log ensures inquiries are handled efficiently and directed to the appropriate Subject Matter Expert (SME) for resolution.
Inquiries submitted to the Compliance Inquiry Log are categorized into three types: Standard, Urgent, and Expedited. With the process for each type as follows:
• Standard and Urgent Inquiries: The Inquiry Intake Lead will confirm receipt of the inquiry within one business day, as well as assign the inquiry to the appropriate SME, who will take on the role of the compliance lead.
• Expedited Inquiries: For inquiries marked as expedited, the Inquiry Intake Lead will prioritize the review and immediately assign the inquiry to the relevant SME. The compliance lead will then contact the submitter following their initial review.
Once assigned, the compliance lead will commence their research and aim to complete it within:
• 3-5 business days for standard inquiries
• 1-2 business days for urgent inquiries
• ASAP for expedited inquiries
However, in cases where the compliance lead is unable to complete the research, or if regulatory review is needed, the inquiry will be escalated to the appropriate regulator. It is important to note that our internal SLAs no longer apply once an inquiry is transferred to regulators, as they operate under their own timelines and processes. The compliance lead will continue to follow-up with the regulator until a response is received.

What’s going on at the State and Federal levels? To support you in your role and ensure timely awareness of changes to regulatory and contractual requirements, RAC attends regulatory calls (DHCS Managed Care Plan Call - MCPC) and other regulatory meetings/calls where key regulatory information is shared
DHCS hosted the Birthing Care Pathway Webinar
On Wednesday, March 5th, DHCS conducted the Birthing Care Pathway webinar. The session focused on the development of the Birthing Care Pathway, a program designed to support Medi-Cal members from conception through twelve months postpartum. The webinar highlighted key findings from member engagement efforts and outlined actions taken to address identified concerns, including the creation and implementation of 42 policies targeting provider access, behavioral health, risk assessment, payment models, and support for justice-involved individuals. Additionally, the webinar introduced strategic opportunities for further improvements, such as enhancing provider diversity, expanding behavioral health resources, and fostering collaboration between state agencies to strengthen maternal care services.
For more details, please refer to “CA Birthing Care Pathway Webinar.”
DHCS hosted the March CalAIM MCP TA Meeting
On Thursday, March 27th, DHCS hosted the CalAIM March meeting to provide updates on several key topics, including the Knowledge Gap of PCPs, ECM/CS/CCM JSON Exchange, new time limits for Community Supports services, and an update for the Asthma Remediation Community Support. Additionally, DHCS used this meeting as a forum for Kings/Tulare and RAMP to introduce valuable resources for MCPs and their providers. Kings/Tulare
presented their Knowledge Management Page, designed to build a connected community of care by centralizing and curating provider resources. RAMP shared their best practices and introduced their technical assistance services to further support MCPs in their efforts to improve their Asthma Preventative Services, and the updated Asthma Remediation Community Support. For more details, please refer to “March CalAIM MCP TA Meeting.”
RAC maintains materials from those weekly calls. Check out previous meetings HERE.
All Plan Letters (APLs)
DHCS and DMHC release APLs to communicate changes in federal or state policy or procedure and instruct managed care plans (MCPs) on implementing these changes. RAC analyzes the APLs to ensure compliance with the requirements and to meet timely filing. Draft APLs (denoted by “XXX” indicating that both regulators have not assigned a policy number) are issued by both DHCS and DMHC regularly to solicit feedback from MCPs before they are officially published and become effective. During this period, MCPs can provide feedback or concerns to DHCS and DMHC on upcoming APLs. Here are the APLs that were recently released:
A. DHCS Regulatory Notices
No new DHCS APLs or draft APLs have been issued since the last reporting period that are applicable to Health Plan.
B. DMHC Regulatory Notices
APL 25-007 (OFR) – Assembly Bill 3275 Guidance (Claim Reimbursement)
Issue Date: April 1st, 2025
Summary: Assembly Bill 3275 (Soria, 2024) amended Health and Safety Code sections 1371 and 1371.35 relating to reimbursement of claims for health care services, and enacted Health and Safety Code section 1371.34 enhancing consumer protections relating to grievances about claims for health care services. Beginning January 1, 2026, Health Plan must ensure the following requirements in regard to Claim Reimbursement are in place:
• Health Plan must acknowledge receipt of all claims per Rule 1300.71(c)
• Health Plan must reimburse complete claims within 30 calendar days of receipt
• If a claim is contested or denied, the plan must notify the claimant in writing within 30 days.
• Claims paid after 30 days will accrue 15% annual interest starting from the 31st day.
• Failure to pay the required interest will result in an additional penalty of $15 or 10% of accrued interest (whichever is greater).
• Written notices must specify which parts of a claim are contested or denied and the reason.
• If a claim is contested due to missing information, it must be resolved within 30 days of receiving additional details.
• Any complaint about claim payment delays or denials from an enrollee must be treated as a grievance under Health & Safety Code Section 1371.34.
• Review and update provider contracts, claims policies, service agreements, and disclosures to ensure compliance with AB 3275.
• Submit an amendment filing affirming compliance with AB 3275 and APL 25-007 by August 1, 2025.
• Ensure delegated entities (e.g., claims processors, risk-bearing organizations) comply with the new rules.
• Compliance will be reaching out soon to schedule a kick-off meeting on this new APL.
Reminder All Plan Letter (APL) Policy Filing Process
All policies must complete the policy workflow before submission to DHCS/DMHC. Policy owners must ensure their policies are approved by their department executive on the Policy Management Application (PMA). Upon receipt of the policies, the Compliance Policy team will review and then send the policies for CEO approval. Once all approvals have been obtained, Compliance will submit the policies to DHCS/DMHC.
RESPONSIBLE PERSON
Regulatory Reports
Under our contract with DHCS and in compliance with our Knox-Keene license (DMHC), we must routinely submit reports demonstrating compliance and performance. Below is a list of reports due for submission in the next few weeks. The table includes a hyperlink to the report and the accountable Director and
Executive for the report. Check out the list to find out which ones are in your department. Click on the report title for more information.
Report Title
Provider Directory File & Use 2025-04
Provider Directory Spring Summer 2025
ECM/JSON 2025-03
CBAS Waiver 2024-03
CBAS Quarterly 2025-Q1
274 File 2025-03
MCPDIP 2025-03
Data Certification 2025-03
Quarterly FWA 2025-Q1
Post Payment Recovery 2025-03
PIN 2025-03
Encounter Data 2025-03
Consolidated Billing 2025-03
NEMT/NMT 2025-01
DMHC Monthly Financials 2025-03
Pending Unresolved Grievance 2025-Q1
New Members Mailing Attestation 2025-04
Annual Marketing Plan 2025
CAC Demographic Report 2025
Member Death Notification 2025-Q1
CY 23 Phase 2 Contract Flagging
Provider Network Impact Report 2025-Q1
Quarterly Network Change Report 2025-Q1
LTC QAPI Program
Provider Complaints
Ana Aranda Liz Le
Ana Aranda Liz Le
Clarence Rao Victoria Worthy
Pamela Lee Tracy Hitzeman
Pamela Lee Tracy Hitzeman
Clarence Rao Victoria Worthy
Clarence Rao Victoria Worthy
Tamara Hayes Betty Clark
Cambria Day Betty Clark
Christopher Navarro Michelle Tetreault
Ana Aranda Liz Le
Clarence Rao Victoria Worthy
Clarence Rao Victoria Worthy
Dale Standfill Liz Le
Somatra Sourng Michelle Tetreault
Ramanpreet Kaur Lakshmi Dhanvanthari
Vena Ford Evert Hendrix
Vena Ford Evert Hendrix
Setar Testo Tracy Hitzeman
Somatra Sourng Michelle Tetreault
Clarence Rao Victoria Worthy
Ana Aranda Liz Le
Ana Aranda Liz Le
Kathleen Dalziel Robert Ruiz
Provider complaints come to the Health Plan in different forms (e.g., direct call to us or dispute submission to DMHC). While our Provider Services and Claims teams address those coming into us, Compliance is the point of contact for those coming through DMHC. In 2025, Health Plan received 9 requests (2 new Provider Complaints and 7 additional information requests), disputing 2 claims. In 2024, we received 67 requests (28 Provider Complaints and 39 additional information requests), disputing 56 claims. In addition, each complaint may
contain multiple issues that require a response. In 2023, Health Plan received 20 requests (13 Provider Complaints and 7 additional information requests), disputing 28 claims.
Compliance coordinates a cross-functional group to review each complaint we receive. This group investigates the cases (from the original request to claim processing and dispute resolution) and prepares a comprehensive response to the DMHC about the provider’s concerns and the actions taken by us These tables outline the status:

Table 2: Provider Complaint Closures by Decision

Word Scramble
Instructions: Rearrange the letters to form the correct word in each of the lines below.
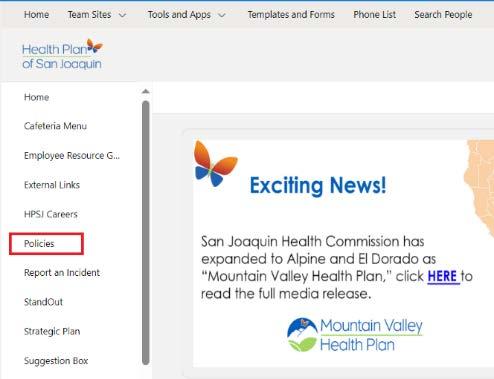
Do you have a question for Compliance? To submit an inquiry, go to Team Sites > Compliance > Requests > Submit an Inquiry on SharePoint or simply use this link: check it out here.