

HEALTHEQUITY4LGBTQ+
ABOUT
HEALTHEQUITY4LGBTQ+ aims to create cross-disciplinary conversations around LGBTQ+ health by leveraging expertise across many domains. Through bridging research and policy with lived experience, HEALTHEQUITY4LGBTQ+ hopes to raise awareness of the breadth of the health disparities facing the LGBTQ+ community and increase understanding of why these inequities are happening and how we can address them.
The mission of this organization and newsletter is to advance health equity for the LGBTQ+ community by increasing education, building policy awareness, and sharing resources.
Education is critical to understanding the extent of the health inequities facing the LGBTQ+ community. The goal of this newsletter is to raise awareness around the various health inequities facing this community and pose solutions for policymakers, organizations, and individuals to enact.
Everyday, policies affecting LGBTQ+ health are enacted, proposed, or struck down. We must advocate for beneficial and against harmful policies. Another goal of this newsletter is to spotlight policies and mobilize advocacy efforts.
This organization and newsletter are only a piece of the larger infrastructure that is tackling the issue of LGBTQ+ health inequities. Countless, hard-working organizations and individuals are at the front of the fight for equity. This newsletter hopes to highlight these resources, which are essential for moving the work forward.
Above all, we hope to center LGBTQ+ voices in this work and through each of these goals. If you have interest in sharing your experiences in the healthcare system, highlighting the work you do, or collaborating in any way, please contact us at healthequity4lgbtq@gmail.com.
HEALTHEQUITY4LGBTQ+

The NIH recognizes sexual and gender minorities as a health disparity population; improving the health and well-being of LGBTQ people is a key priority of the Healthy People 2030 initiative. Yet, inequities remain. In the United States today, LGBTQ+ individuals face significant health inequities in regard to disease prevalence, healthcare access, and exposure to social determinants of health. Understanding of these inequities by LGBTQ+ people, health care providers, policymakers, non-profit leaders, and the general public is crucial for addressing them.
The health inequities facing LGBTQ+ people are broad in scope. They encompass sexual and reproductive health, mental health, cancer screenings, health insurance access, substance use disorder, homelessness, and so much more. In this issue, we will focus on key disparities related to health care provision and culturally competent care for the LGBTQ community.
HEALTH EXPERIENCES
UNIQUE HEALTH NEEDS
CULTURALLY COMPETENT CARE
RESEARCH SPOTLIGHT: A CONVERSATION WITH DAVID YU
POLICY IMPLICATIONS

HEALTH EXPERIENCES
LGBTQ+ people often report adverse experiences within the healthcare system as a result of discrimination, bias, and/or lack of knowledge of the provider on sexual orientation and gender identity. Feeling un-welcomed in the healthcare environment can also result in avoidance or delays in seeking care, in turn, worsening the outcomes of LGBTQ+ individuals.
In a survey from the Kaiser Family Foundation (KFF) comparing experiences of LGBTQ+ vs. nonLGBTQ+ patients in the healthcare systems, it was found that although both populations are likely to have a care provider they see regularly, LGBTQ+ individuals were more likely to have challenges in accessing care, difficulty affording care, and considerable variation in the utilization of essential health services.
Source: LGBT+ People’s Health and Experiences Accessing Care, https://wwwkfforg/report-section/lgbt-peopleshealth-and-experiences-accessing-care-report/

ACCESSING QUALITY CARE:
Compared to their non-LGBTQ+ counterparts, LGBTQ individuals were more likely to report adverse experiences with healthcare providers including: feelings that their concerns were being dismissed, their provider was making assumptions around their needs, and/or they were being blamed for their health conditions.
Such experiences create challenging environments for LGBTQ+ individuals to receive high-quality healthcare.
AFFORDING CARE:
The KFF survey found that 30% of LGBTQ+ people had trouble affording their healthcare bills in the last month, compared to 19% of non-LGBTQ respondents. As a result, many LGBTQ+ people had to utilize all of their savings, had payments sent to collection, or struggled to afford food and other basic needs.
26%
of LGBTQ respondents’ health insurance was not accepted by their preferred primary provider.
Relatedly, LGBTQ+ individuals also face barriers related to health insurance, including having insurance that does not cover prescription medications or recommended tests and/or results in high out of pocket costs. 26% of LGBTQ+ respondents reported that their insurance was not accepted by their preferred physician, which can lead to a difficult choice between quality and affordable care.
Finally, LGBTQ+ respondents reported differential rates of utilization across essential healthcare services, such as mammograms and other cancer screenings, than their non-LGBTQ+ counterparts. Such differential rates of utliization contribute to disparate health outcomes for the LGBTQ+ community.
Mental Health & Suicide Education
LGBTQ Health Needs
The LGBTQ+ community experiences various health disparities across physical, mental, reproductive health, and access to healthcare. In this section, we will provide an introduction to understanding a number of these inequities. This list is not exhaustive and does not meet the full depth of experience, but provides an initial understanding of the unique needs of LGBTQ folks.

An estimated 39% of LGBTQ+ identifying people report experiencing mental illness. LGBTQ+ people experience minority stress, microaggressions, prejudice, rejection and isolation, and other unique circumstances that heighten their risk of mental illness.
For example, LGBTQ+ people are more likely to experience anxiety and depression than their heterosexual counterparts. They also experience higher rates of suicide/suicide attempts, are found to be more susceptible to eating disorders, and are at increased risk of PTSD.
Read more: Understanding LGBTQ+ Mental Health Or, read Issue 1 of our newsletter

HIV/Sexual Health
Gay and bisexual men experience the highest rates of HIV than any other population, with a disproportionate impact on Black and Latino men LGBTQ+ men are also at high risk for other sexually transmitted infections. Additionally, LGBTQ+ youth are more likely to engage in sexual activity at an earlier age, but have less comprehensive sexual education, have lower rates of STD testing, and use condoms ineffectively.

Stigma may also play a role in the disparate impact of STIs and HIV on the LGBTQ+ community. For example, one study found that stigma played a role in both whether to get tested and how often to get tested, due to fears of rejection, isolation, and the desire to reduce contact with healthcare professionals.
Read more: How HIV Impacts LGBTQ+ People
Debunking Common Myths about HIV
The impact of stigma on HIV testing decisions for gay, bisexual, queer and other men who have sex with men: a qualitative study

Gender-Affirming Care
Gender-affirming care can include hormone therapy, reconstruction surgeries, speech therapy, and mental health counseling, among other services. Accessing such care continues to present barriers for transgender and gender nonconforming youth and adults in the U.S., and beyond.
Currently, 23 states ban or restrict access to care for transgender youth, while only 11 states have enacted a “shield law” which protects individuals, families, and medical providers from civil and/or criminal charges if they seek genderaffirming care in a different state.
Read more: LGBTQ Policy Spotlight: Bans on Medical Care for Transgender People
Transgender Healthcare “Shield Laws” Bans on Best Practice Medical Care for Transgender Youth
Substance Use
LGBTQ+ people are found to have higher rates of substance use and substance use disorders than their heterosexual counterparts.
For example, an estimated 6.7% of LGBTQ adults in 2020 used opioids in the past year, compared to 3.6% of the overall adult population.
LGBTQ+ people are also found to have higher rates of smoking, vaping, and tobacco use. Given the compounding risk for other mental illness, targeted treatment methods should be considered when treating the LGBTQ+ community.
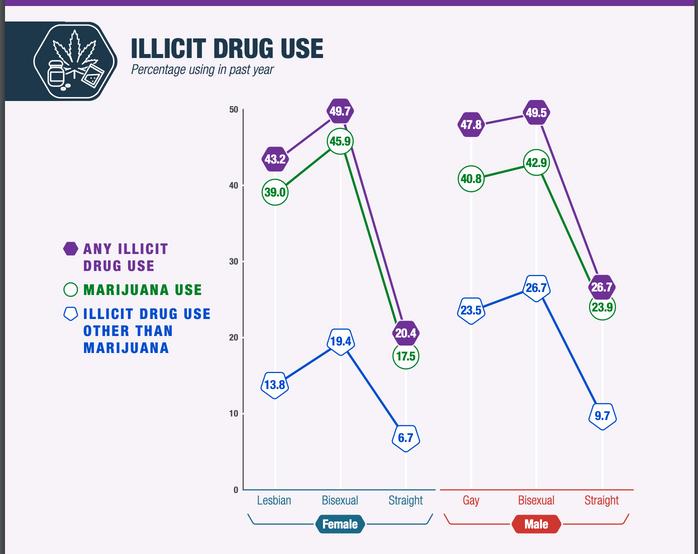
Read More: Substance Use and SUDs in LGBTQ* Populations
Lesbian, Gay, and Bisexual Behavioral Health: Results from the 2021 and 2022 National Surveys on Drug Use and Health

Cancer Screenings

Reproductive Health
Reproductive Justice encompasses the tenants of: the right to have a child; the right to not have a child; and the right to parent a child in a safe and healthy environment. The reproductive justice movement must also include LGBTQ+ individuals. Members of the LGBTQ+ community, including lesbian and bisexual women, transgender men/transmasculine people, and non-binary people all access abortion services, seek contraceptive options, utilize assisted-reproductive technologies, among other services. However, barriers to care present impediments to LGBTQ people accessing these services and a lack of integration of LGBTQ identities into services, such as sex education and family planning, result in inadequate provisions of necessary care
Read more: Not Up for Debate: LGBTQ People Need and Deserve Tailored Sexual and Reproductive Health Care
Queering Reproductive Justice
Cancer-related data for the LGBTQ+ community is overall limited due to a lack of data collection regarding gender identity and sexual orientation. However, disparities related to cancer prevalence exist, as do differences in cancer screenings. The latter can in part be attributed to the systemic barriers and discrimination LGBTQ+ people face in the healthcare system that can often result in avoiding or delaying care.
For example, lesbian women are less likely to be screened for cervical cancer. Additionally, transgender people are less likely to be screened for breast cancer and colorectal cancer. LGBTQ+ competency training among providers along with the specific inclusion of cancer-related modules provides an avenue for addressing these key disparities related to cancer screenings and diagnosis that affect the LGBTQ community.
Read more: AACR Conference Examines Cancer Disparities in the LGBTQ Population
Barriers and Facilitators to Cancer Screening Among LGBTQ Individuals
CULTURALLY COMPETENT CARE
Drivers of health inequities among the LGBTQ+ population that we see today include: discrimination and bias in the healthcare system, differential access to health insurance, and overall feelings of needs not being met, resulting in delays or avoidance of care.
Culturally competent care presents an opportunity to train healthcare professionals around the unique health needs of the LGBTQ+ community, foster respect for the identities and experiences faced by members of this community, and overall improve the healthcare provision for this population.
Much research has gone into identifying best practices around inclusive care for the LGBTQ+ community with some key tenants emerging. In the following sections, we will review various components of inclusive care that can improve the healthcare experiences for LGBTQ+ patients.
Creating an accepting and affirming environment
Creating a healthcare environment that makes LGBTQ+ people feel accepted, respected, and included can be a first line of passage into a positive healthcare experience. Behaviors may include:
Utilizing chosen names and respecting pronouns, as well as collecting this information on intake forms.
Collecting data on sexual orientation and gender identity for Electronic Health Records.
Holding yourself and colleagues accountable
Apologizing when a mistake is made

Increasing Healthcare Providers Knowledge of LGBTQ Health Needs
The first step in addressing any problem is recognizing that it exists. Understanding the various health inequities facing the LGBTQ+ community, the drivers of these inequities, and best practices to address them is critical for all health care providers. Accomplishing this may look like:
Ensuring staff are trained on LGBTQ+ terminology including terms related to gender identity and sexual orientation Training staff on the unique health and treatment needs as well as their relation to the social determinants of health
Educating practitioners on the history of LGBTQ+ discrimination and its impact on healthcare today

Continuing to Research and Understand the Evolving Health Needs of the LGBTQ+ Community
LGBTQ+ rights are up for debate every day and new policies have the potential to restrict their access to care and reinforce the histories of discrimination. Understanding how health needs are changing over time is imperative to ensuring care remains inclusive, and may involve:
Listening to LGBTQ+ individuals and understanding their unique health needs and experiences
Prioritizing funding for research that focuses on LGBTQ+ health disparities and in particular underrepresented populations including, transgender men and women, nonbinary people, and LGBTQ+ people of color. Increasing data collection related to LGBTQ health to better understand the gaps and disparities
Spotlight
A CONVERSATION WITH DAVID YU:
David (Hyunmin) Yu is a PhD student at the University of Pennsylvania dedicated to addressing and improving culturally competent care for the LGBTQ+ community. As a researcher, nurse practitioner, and member of the LGBTQ+ community, David brings both personal and practical experience to this topic.

David’s Background:
As a patient, David met with a healthcare provider in regard to HIV preventative measures, but the conversation did not go well. The provider was not well-informed on prevention options, and overall, David’s needs were not being met, nor respected. As a practitioner, David noticed that there was discrimination in the field against the LGBTQ+ community; whether that be through microaggressions, bias, or unfair experiences, he noticed that many clinicians were not well-informed about the overall unique needs of the LGBTQ+ community. These compounding experiences led to his interest in LGBTQ health.
He first was interested in general training programs for LGBTQ+ health and began looking at training programs within nursing curricula. How are nursing programs educating their students on LGBTQ health? Then he broadened his scope and began to look at all healthcare professionals in diverse disciplines and across various healthcare settings. He also looked at different state policies and how this impacted LGBTQ+ health training programs.
From this research, David realized that there were effective training programs and there were parts that worked, so his response was: what drives the implementation of these programs? LGBTQ+ health related programs are not offered in all curricula or at all healthcare institutions, so what leads some facilities to implement and others to not? This is what much of David’s current research seeks to answer. His goals are to get nuanced, detailed factors as to what facilitates and/or presents a barrier to implementing inclusive practices for LGBTQ+ patients at healthcare facilities across the nation.
In the future, David would like to also expand his work to test implementation strategies aimed at enhancing LGBTQ+ inclusion in healthcare settings and promote healthcare surveys to understand the effectiveness of the strategies and the degree to which patients and/or employees feel included in the system.
Defining Inclusive Care for the LGBTQ+ Community:
David recognized three components of inclusive care, as it pertains to the LGBTQ+ community:
Recognize and affirm diverse sexual orientations and gender identities by systematically collecting them in health records
Acknowledge that there are unique specific health needs affecting the LGBTQ+ community.
Provide culturally responsive care to this population in order to address disparities and outcomes.
Recognition and affirmation are significant starting points. However, addressing all three components is essential to achieve LGBTQ+ inclusion.


Balancing the DualImpact of Structural and Cultural Barriers:
David noted that state level laws and policies can have a substantial impact on the type of care that can be provided, as well as hospital regulations, personal bias and beliefs, and financial constraints. However, even when state-level laws create restrictions to care, there is variation within these states. In more restrictive states, David says that some hospitals and staff are “doing their best in a confined environment”.
Combatting the Fear of Messing Up:
In one review that David conducted, it stood out to me that LGBTQ+ competency training helped nurses feel more comfortable and decreased their anxiety around providing care to LGBTQ+ patients. David added that discomfort and bias often arises from our fear of the unknown. Often, bias can come not from explicit prejudice, but from a lack of awareness. But, the fear of doing the wrong thing often leads us to not do anything, which is also harmful.
Understanding LGBTQ+ identities and needs exposes the issue and the patient population, so although they may not solve everything, cultural competency training is a good start.
RESOURCES
Human Rights Campaign: Health Equality Index
The Health Equality Index was developed by the Human Rights Campaign to respond to the need for LGBTQ+ people to have equitable, inclusive, and high-quality healthcare.
Participating healthcare facilities are scored across five criteria: Non-discrimination and staff training
1. Patient services and support
2. Employee benefits and policies
3. Patient and community engagement
5.
4. Responsible citizenship
Read the full HEI 2022 Report and explore the HEI map to understand how healthcare facilities near you rank
Movement Advancement Project Equality Maps
Movement Advancement Project utilizes mapping technologies to illustrate the impact and state of LGBTQ+ policies across the U.S. From LGBTQ anti-bullying policies, bans on drag performances, to employee non-discrimination policies, MAP allows you to understand the protections and restrictions in place affecting the LGBTQ+ community.
Explore the maps related to healthcare and many of the other social issues or continue reading for further discussion on some of these policies.
Policy Implications
From the federal to organizational level, policy has the potential to improve or diminish the experience within the healthcare system and the overall health outcomes of LGBTQ+ people.
Understanding policy barriers and facilitators to providing culturally competent care is critical for moving forward and improving the inclusivity of care for the LGBTQ+ community.


Health Insurance
Access to health insurance is a critical point of entry into the healthcare system for all individuals. For LGBTQ+ people, health insurance presents unique barriers to care.
Health insurance non-discrimination policies include protections from denying LGBTQ+ people access to health insurance and/or being denied coverage for certain procedures on the basis of gender identity or sexual orientation.
Currently, 26 states and U.S. territories do not have any explicit laws that provide insurance protections on the basis of sexual orientation or gender identity. Additionally, 2 states explicitly permit insurers to refuse coverage for gender-affirming care.
Within State insurance benefits, coverage also varies across the country. 25 states currently include gender affirming care in their state employee health benefits, 13 states explicitly exclude it, and 12 make no mention. The map below from the Movement Advancement Project displays this distribution across the 50 U.S. states, D.C., and 5 territories.
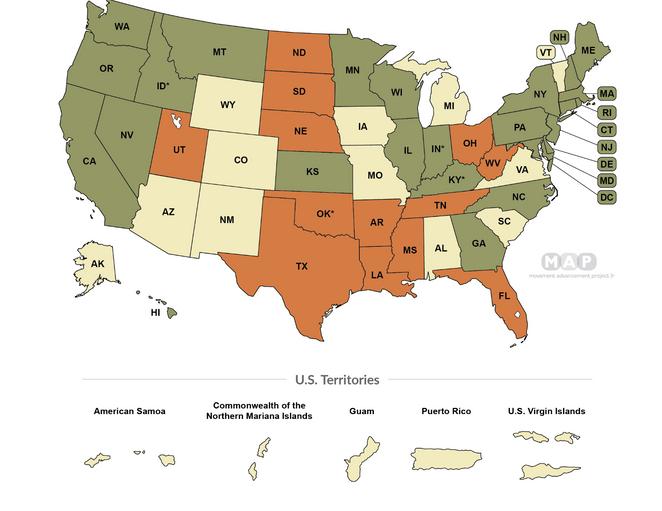
Source: Movement Advancement Project, https://www lgbtmap org/equality-maps/healthcare laws and policies
Data Collection
Data collection is a significant contributor to our understanding of LGBTQ+ health. Without data, we cannot fully understand the breadth of the issues at hand.
The Behavioral Risk Factor Surveillance Survey (BRFSS) is a largescale health survey conducted around the world, in which all 50 states participate. Currently 33 states include questions about gender identity and sexual orientation, while 17 do not.
The results of the BRFSS inform efforts at the Centers for Disease Control, Department of Health and Human Services, and many other federal agencies to target and create health promotion services. Without robust data collection, including around LGBTQ+ identities, this data and its subsequent health promotion activities are severely limited and further reproduce a cycle of exclusion and inequity for under-recognized and under-resourced communities.
Additional Barriers
Beyond policies that explicitly target healthcare services, many of the laws that regulate the lives of LGBTQ+ people more broadly also impact their overall health.
For example, laws around parental recognition in same-sex relationships or adoption and assisted reproductive technologies all impact the social well-being of LGBTQ+ individuals and their families.
Other discrimination laws including, protections against discrimination in housing and ability to access credit, as well as protections in spaces of public accommodation all impact how LGBTQ+ people navigate the world and have access to essential needs. However, not all states have explicit protections against di i i i i h i

To advance the overall health and well-being of LGBTQ+ individuals we must advocate for their full inclusion and protection in both healthcare settings and the social world at large.
Sources
American Association for Cancer Research. (2021). AACR Conference Examines Cancer Disparities in the LGBTQ Population. https://www.aacr.org/blog/2021/01/26/aacr-conference-examinescancer-disparities-in-the-lgbtq-population/
American Medical Association EdHub. (2023). 3 Ways to Provide Culturally Affirming Care to LGBTQ Patients https://edhub ama-assn org/pages/3-ways-provide-culturally-affirming-lgbtq-care
Bass, B & Nagy, H (2023) Cultural Competence in the Care of LGBTQ Patients In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563176/
Centers for Disease Control and Prevention, Behavioral Risk Factor Surveillance System. https://www.cdc.gov/brfss/about/index.htm
Dawson, L., Fredericksen, B., Long, M., Ranji, U. & Kates, J. (2021). LGBT+ People’s Health and Experiences Accessing Care. KFF, Women’s Health Policy. https://www.kff.org/reportsection/lgbt-peoples-health-and-experiences-accessing-care-report/
Dawson, R. & Leong, T. (2020). Not Up for Debate: LGBTQ People Need and Deserve Tailored Sexual and Reproductive Health Care. Guttmacher Institute.
https://www.guttmacher.org/article/2020/11/not-debate-lgbtq-people-need-and-deservetailored-sexual-and-reproductive-health
Haviland, K , Swette, S , Kelechi, T , & Mueller, M (2020) Barriers and Facilitators to Cancer Screening Among LGBTQ Individuals with Cancer Oncology Nursing Forum, 47(1), 44-55 DOI 10.1188/20.ONF.44-55
Human Rights Campaign. (2022). Healthcare Equality Index 2022. https://reports.hrc.org/hei-2022? ga=2.176030946.1182749902.1711115113-2091995173.1709174531
Human Rights Campaign Foundation. (2023). Debunking Common Myths About HIV.
https://www.hrc.org/resources/debunking-common-myths-about-hiv
Iott, B.E., Loveluck, J., Benton, A. et al. The impact of stigma on HIV testing decisions for gay, bisexual, queer and other men who have sex with men: a qualitative study. BMC Public Health 22, 471 (2022). https://doi.org/10.1186/s12889-022-12761-5
Mass General Brigham, McLean. (n.d.) Understanding LGBTQ+ Mental Health.
https://www mcleanhospital org/essential/lgbtq-mh
Movement Advancement Project “Equality Maps: Bans on Best Practice Medical Care for Transgender Youth”. https://www.lgbtmap.org/equalitymaps/healthcare/youth medical care bans
Sources
Movement Advancement Project. “Equality Maps: Data Collection”
https://www.lgbtmap.org/equality-maps/data collection
Movement Advancement Project. "Equality Maps: Healthcare Laws and Policies.”
https://www.lgbtmap.org/equality-maps/healthcare laws and policies
Movement Advancement Project “Equality Maps: Nondiscrimination Laws”
https://www lgbtmap org/equality-maps/non discrimination laws/housing
Movement Advancement Project. “Equality Maps: Parental Recognition Laws.”
https://www.lgbtmap.org/equality-maps/recognition/parenting/assisted reproduction
Movement Advancement Project. “Equality Maps: Transgender Healthcare "Shield" Laws.
https://www.lgbtmap.org/equality-maps/healthcare/trans shield laws
Movement Advancement Project. (2023). LGBTQ Policy Spotlight: Bans on Medical Care for Transgender People.
https://www.mapresearch.org/file/MAP-2023-Spotlight-Medical-Bansreport.pdf
National Coalition for LGBTQ Health. (2022) Inaugural State of LGBTQ Health National Survey.
https://healthlgbtq.org/wp-content/uploads/2022/06/State-of-LGBTQ-Health-NationalSurvey-2022 pdf
National Institute on Drug Abuse (n d ) Substance Use and SUDs in LGBTQ Populations
https://nida nih gov/research-topics/substance-use-suds-in-lgbtq-populations
National LGBT Health Education Center (2017). Focus on Forms and Policy: Creating an Inclusive Environment for LGBT Patients.
https://www.lgbtqiahealtheducation.org/publication/focus-forms-policy-creating-inclusiveenvironment-lgbt-patients/
National LGBT Health Education Center. (2016). Understanding the Health Needs of LGBT People.
https://www.lgbtqiahealtheducation.org/publication/understanding-health-needs-lgbt-people/
National LGBTQ Task Force. (n.d.). Queering Reproductive Justice.
https://www.thetaskforce.org/programs/queering-equity/queering-reproductive-justice/
Substance Abuse and Mental Health Services Administration. (2023). Lesbian, Gay, and Bisexual Behavioral Health: Results from the 2021 and 2022 National Surveys on Drug Use and Health
https://www samhsa gov/data/sites/default/files/reports/rpt41899/2022 LGB Brief Final 06 07 23 pdf

