INDEPENDENT PRACTITIONER TODAY
The business journal for doctors in private practice



By Robin Stride
This month’s Independent Practitioner Today is packed with a wide range of information, useful tips, and observations from a variety of expert writers – all aimed at helping your private practice move forward again.
Our exclusive website story last week reported that private healthcare and consultants’ earnings are at last seeing a ‘modest revival’. So we hope this issue’s practical advice will be a big help as you move towards some sort of recovery.
According to data from leading digital services provider Healthcode, a slight improvement in insured patients’ activity was registered in the first half of June.
Billing volumes in the third week of May were 67% down on the same period in 2019 but had revived slightly last month when they were 56% below the previous year’s figure.
Of course, there is much to be done now and some, such as the London Consultants’ Association, are voicing less than optimistic views about the future.
It is calling for concerted action from everyone: ‘Apart from the consultants, who recognise the reality of the destruction of their business, there seems to be a mistaken acceptance that there will be natural restoration of private practice postCovid.
‘This is unlikely to occur without an underlying support strategy and there is a need for all these components – private medical insurers,

providers and the consultants – to work together to develop a strategy for the future survival of the sector.’
See page 10.
We hope to see some strong leadership to bring this about, but meanwhile the private doctors finding their feet again on the ground in the ‘new norm’ can find a wealth of immediate support for their own business published here:
Page 4: Private doctors’ experience in the pandemic is likely to make them reassess their business model and clinical priorities, says the Independent Doctors Federation’s Dr Neil Haughton.
Page 12: Following the LCA urging private doctors to think twice about accepting 50% fee cuts from insurers for virtual consultations (see our website story, 17 June), surgeon Mr Ian McDermott spells out just why this work is worth every penny.
Page 16: Our AZ of top tips from the accountant’s desk continues with a very topical ‘L’…Leaving lockdown: lessons in IT security.
Page 18: Private doctors’ organisations – as we reported on our website last month – have welcomed an NHS England pledge paving the way for a resumption of consultants’ work in the independent sector. We share contents of the letter that has raised private doctors’ hopes of getting back to work.
Page 20: David Hare, boss of the Independent Healthcare Providers Network, tells us: ‘I firstly want to assure Independent Practitioner Today readers that independent healthcare providers absolutely under

stand the impact this has had on consultants’ working life and the frustrations they feel and, as a sector, we are doing everything we can to release private practice and get more private consultants back to work.’
Page 22: Positive patient experience is the most powerful way to influence the reputation of your service, requiring discipline across all aspects of your practice.
As a result, it is imperative to have a clear strategy that is understood by everybody involved. Our Guide To Delivering Superior Patient Experience In Private Practice continues as Jane Braithwaite shows how to get started or review and evolve your current offering.
Page 25: Tips for staying secure while working from home. Remote working opens great possibilities for flexible working practices, but it also significantly raises the risk from cyber threats and data breaches, warns IT director Murray Hart.
Page 30: Now reorganise your private practice to best advantage, post

Covid 19. Stephanie Carmichael show how.
Page 32: As growing numbers of independent practitioners move closer to resuming private practice, Prof David Gartry shares his story. Page 34: Ten billing rules to ensure your practice recovers. Words of wisdom from Medical Billing and Collection’s Simon Brignall. Page 38: Change is inevitable. Cavendish Medical’s Dr Benjamin Holdsworth shows why diversification in your investments will mean not missing the next Amazon.
Page 40: The CQC regulates you, but who regulates the regulator? Hempsons solicitor Philippa Doyle says if you get a bad report – and they are still coming through –then make sure you challenge it. Page 46: Covid19’s impact will be felt for some time to come, so for those starting out in private practice – or needing a review – it will be a tougher environment. Accountant Ian Tongue prescribes some financial considerations for success.



TELL US YOUR NEWS. Contact editorial director Robin Stride

5 new diagnostic centres bankrolled
A network of up to five new diagnostic facilities are being set up in the UK by Rutherford Health for private and NHS patients P6

Email: robin@ip-today.co.uk Phone: 07909 997340 @robinstride
ADVERTISE WITH US. To advertise in the journal or our website business and lifestyle directories, contact advertising manager
Margaret Floate at margifloate@btinternet.com.
Phone: 01483 824094
GET A SUBSCRIPTION DISCOUNT
£90 independent practitioners. £210 organisations. £90 GPs and practice managers (private & NHS). Save £15 paying by direct debit: individuals £75 (organisations £180).
TO SUBSCRIBE
Email karen@marketingcentre.co.uk Or phone 01752 312140 Or go to the ‘Subscribe’ page of our website www.independent-practitioner-today.co.uk
Chief sub-editor: Vincent Dawe
Head of design: Jonathan Anstee
Publisher: Gillian Nineham at gill@ip-today.co.uk Phone: 07767 353897
The possibility of consultants’ income from self-pay bouncing back and increasing, when the public health conditions allow, is one bright ray of light to look forward to.
Potentially, tens of thousands of patients who might not have considered private healthcare in the past would do so in the future when there is room for them.
Consultants will be ready, but are your hospitals harnessing this sort of income as well as they might?
The topic came under the spotlight at market analysts LaingBuisson’s Private Healthcare Summit 2020, held as a webinar and attended by around 200 people.
And a sorry picture it painted of missed opportunity to make the most of the market. Ancient phone systems that keep self-pay inquirers waiting and then don’t ‘know’ how long for means business is missed.
And how about a self-pay adviser walking around the hospital corridors with a patient in tow as she tried for find a spare room to discuss the individual’s details.
‘Excruciating’, observed Richard Gregory, the self-pay business adviser who was on site witnessing it. What’s more, he warned that consumers still did not fully understand the self-pay option even existed – maybe they thought private care was all insurance.
He said some revolutionary things about price too – see page 5 – and while agreeing that the terms and conditions are more accessible now, he complained ‘they are still convoluted; they are still double Dutch to a certain extent and in some cases there’s five or six pages. It doesn’t need to be that complex; they can be simplified and written in language that we can all understand’.
Much work to be done, then, before the rush…

Statistics show private care’s pain Official figures confirm the extent of the financial battering suffered so far by independent practitioners during the Covid-19 pandemic P9
A trawl through the archives
A look back through our journal’s archives of ten years ago reveals that although times change, some issues are not so new P14

When called to a Coroner’s court Dr Gabrielle Pendlebury follows last month’s advice on how to prepare for an inquest by looking at what to expect on the day P27


No patient privacy if you’re cuffed Surgeon Mr David Sellu, convicted for the manslaughter of a patient – later overturned – recounts his experience of being a hospital patient in prison P36
PPUs pushing up in Northern Ireland NHS private patient services in the ‘six counties’ come under the spotlight in our monthly round-up of PPU progress around the country P42
Business Dilemmas: Consent lost in translation?
Our medico-legal slot answers a doctor’s fears about obtaining informed consent using a translator P45
Doctor on the Road: Mean, green and nice to be seen
BMW has turned its large X5 SUV into a plug-in hybrid, which will appeal to the eco-conscious doctor P48
Profits Focus: Tapping into self-pay
Our unique benchmarking series looks at the financial fortunes of general surgeons P50
By Edie Bourne
Some doctors may mistakenly believe they will not face large tax bills because of the recent easing of the pensions savings tax rules in April.
In the Budget, the Chancellor Rishi Sunak raised the threshold at which tax-free allowances begin to reduce and the strict ‘annual allowance’ begins to be tapered.
Under the new rules, anyone with a ‘threshold’ income of £200,000 or more, plus an ‘adjusted’ income of £240,000 or more, is subject to a reduced annual allowance.
The threshold income includes earnings from all sources, so this might include NHS salary, private practice or academic work, investment returns and buy-to-let incomes.
The adjusted income also adds in
pensions growth for the year. This growth can be substantial for many private doctors who have NHS work.
The standard annual allowance figure is £40,000, but this then tapers on a sliding scale to as low as £10,000 depending on earnings.
But there is a further rule which can apply. Doctors earning over £312,000 a year from all sources will face a tapered annual allowance of just £4,000.
worse position than before the changes.
‘We’ve seen a few cases where doctors believe they are now in the clear because the rules have recently changed, but the reality is rather different.

Patrick Convey
Patrick Convey, technical director at specialist financial planners Cavendish Medical, explained: ‘After years of causing misery and impacting the NHS workforce, the tapered annual allowance improvements were welcomed by many senior doctors.
‘However, there is a catch for the highest earners, who are now in a
‘The calculations are particularly complex, so it is difficult to get right, particularly given the challenges most of the NHS workforce have faced recently.
‘Add in the surprise move by the Treasury to pay the tax charges of clinicians – if they qualify – for the 2019-20 tax year and it is easy to see why mistakes can occur.
‘It is imperative doctors get their own tax position checked carefully. The highest earners will also need to establish whether pension
savings are still valuable given the tax issue. Every situation is different so they will need careful consideration to ascertain the best move forward.’
The annual allowance figures for 2019-20 are issued by the NHS Pensions Agency in October and HM Revenue and Customs has proposed to pay tax charges for qualifying medics. Doctors must still declare their position on their annual tax submission.
Doctors can ask the NHS Pension Scheme to pay their annual allowance tax bill on their behalf, with the member’s benefits in retirement being reduced accordingly.
The ‘scheme pays’ application deadline has been extended from 31 July to 31 October 2020 for tax bills arising in 2018-19. The extra three months is to assist healthcare workers impacted by the Covid-19 response.
A private baby scan clinic’s successful appeal against the taxman’s demands to charge VAT has brought some advice to doctor entrepreneurs from a specialist medical accountant.
Vanessa Sanders, a partner with Stanbridge Associates, said: ‘It would appear that it is imperative that any services being claimed as exempt from VAT should adhere to the strict rules surrounding medical care, including using medically licensed and registered professionals with appropriate professional indemnity in place.
‘It would also be pertinent to consider the marketing of any business model to ensure the raison d’être is aligned with the actual practice.’
In a recent case in the tax tribunals, a decision was reached which gives hope to those who wonder
about whether or not their services can remain exempt from VAT.
The case concerned ‘Window to the Womb’ franchisees who conduct more than 120,000 ultrasound scans annually and are registered by the Care Quality Commission (CQC) because they perform a ‘regulated activity’ at specified premises, defined as ‘diagnostic and screening procedures’.
The business’s marketing materials mention a ‘well-being report’ based on information gathered from the scan, as well as including a ‘baby bonding’ experience, because of the 4-D images of the unborn baby.
The company argued that the service offered was medical care in the form of diagnostic scanning rather than merely ‘bonding’ imagery, so was VAT-exempt.
Window to the Womb said all franchisees were required to use qualified sonographers, who had to be registered with the Health and Care Professions Council, be full members of the Society of Radiographers and hold adequate professional indemnity cover.
These sonographers were professionally distinguishable from ‘ultrasound technicians’, who merely produced images using ultrasound equipment. The sonographers attracted higher fees because of their professional qualifications, all of whom added an annual £100,000 to clinic costs.
HM Revenue and Customs claimed the primary purpose of the supplies was not demonstrated to be to protect health. The company intentionally marketed the business as high-quality 4-D images of the unborn child for the
‘bonding’ purpose, with no followup treatment offered if issues were detected – despite the clinic’s referral back to the NHS if considered necessary.
The tribunal noted 79% of clients bought scans to obtain the well-being report or information about the foetus’s growth and presentation as described in the marketing literature, although it was difficult to assess if they would have paid the same for a mere 4-D image without the service provider’s medical qualifications.
The tax tribunal judge stated: ‘In my view, it is likely that those remaining 21% are not purchasing scans principally for the 4-D imagery… Some may well do so, but most will be principally concerned to satisfy themselves that the foetus is healthy.
➱ continued on page 7
By Robin Stride
Private doctors’ experience in the pandemic is likely to make them reassess their business model and clinical priorities, according to the president of the Independent Doctors Federation.
Talking at LaingBuisson’s Private Healthcare Summit webinar, private GP Dr Neil Haughton said it would make them look closely at their services, what works, what patients want and what generates income most efficiently.
They needed to be prepared for future developments, as well as continuing to provide excellent safe healthcare, but be flexible and responsive both clinically and financially.
Referring to his own practice’s experience at the Portobello Clinic in London, he said income plummeted to less than 10% of normal almost overnight.
It made contingency plans for the next few months, reviewed finances, took a Covid Business Interruption Loan, furloughed staff, including two part-time doctors, the physiotherapist – who was no longer in demand – plus two receptionists; and all took temporary salary cuts.
‘What we thought was going to last a few weeks was clearly going to take months,’ he told the conference. ‘At least we could generate some income, unlike our dental colleagues or those working in non-essential medicine, or private consultants whose hospitals were now almost wholly NHS.
‘A couple of months later and business is slowly picking up, patients are returning to London and the problems delayed by three months now are presenting themselves, including two bowel cancers that have sadly spread much

further than they should have done.
‘We will be fine, I hope, as we have loyal patients who have relied on our service for more than 20 years and it has given us the opportunity to review our business offering, consolidate and prioritise more efficient sources of income, as we have no idea how long this will last or if the peak will return.’
In the post-Covid world, if there ever was one, the practice would have to work in a very different way affecting its building, basic clinical care, staffing, the business and regulation, he said.
‘The building seems to change daily, with ever more social distancing signs, Perspex screens, warning tape across floors, more rooms used as waiting rooms so
patients can stay apart, staff stationed in separate areas for their own safety and, of course, hand sanitiser everywhere. Our opening hours are also shorter for now due to fewer staff.
‘Employees are kept to a minimum and there has been hardly any holiday taken, as there’s nowhere to go, they wear masks and gloves all day and keep two metres from each other and patients where possible.
‘We carried out thorough risk assessments to protect our staff, especially those from BAME backgrounds.
‘Unfortunately, some have now been made redundant and others have had their hours reduced, but morale is high and all staff members have been incredibly flexible. I have been really impressed by their positive attitude and resilience’.
Clinical care was quite different, with many more virtual consultations. He occasionally worked from home, but in the surgery wore a mask, gloves and apron when seeing a patient, who had to sit two metres away and wear a mask too.
‘I cannot carry out high-risk procedures, not even a throat swab and cannot really examine the throat in case an aerosol is created, and I rarely listen to anyone’s chest now due to the deep breathing required.
‘All surfaces are wiped down after each patient and the whole practice is constantly being cleaned.’
His referrals had plummeted from over 20 a week to about two, partly because the patients were
not in London or were reluctant to go near hospitals for investigation, but there was also nowhere to refer.
‘We also didn’t know which consultants were working or where, and maybe this should be considered for the future, although this situation is improving.’
He usually carried out annual screening for patients, but these had been on hold since early March, so he worried about what had been missed or delayed.
There would also now be a new chronic illness to manage: the post-Covid patient with lung scarring, renal impairment, possibly diabetes and who knew what else would transpire, requiring lifelong management.
Dr Haughton said he also worried about the mental health impact this period would have on
recovered patients, their families, healthcare staff and a public living with a fear of contagion.
Watchdog streamlined
He predicted the Care Quality Commission (CQC) could be streamlined and made more costeffective and efficient.
‘My NHS GP colleagues have said their job has become “do-able” for the first time in years without the CQC looking over their shoulders.’
Patients paid to see private GPs in person and for continuity of care and while NHS general practice might become more remote and formulaic, independent GPs had the flexibility to fill the gap which that leaves and become more responsive to patients’ needs, which could in the long-run be to their advantage.
Dr Haughton observed: ‘You cannot replace looking a patient in the eye in person to understand why they are in your room and, fortunately, we can still see their eyes over the mask.’
He felt remote diagnostics could become more routine. ‘Patients could own their own stethoscopes, blood pressure and ECG monitors, oximeters – already becoming important with Covid – otoscopes and even capsule endoscopes and ultrasound, giving the physician a virtual examination kit from wherever the patient might be.’
Blood testing was more challenging, but could be carried out on small samples couriered to the lab. Results and recordings could then be part of an online referral to the consultant who could be anywhere in the country or beyond.
Prices need to be fixed and transparent when private hospitals start catering again for self-pay patients, according to a leading independent healthcare adviser.
Richard Gregory recommended the price needed to be fully inclusive of all elements, with a generous aftercare commitment. Providers might experience ‘a couple of hits’, but the impact on goodwill to the business and the compelling nature of their proposition would far outweigh the risk.
This meant operators or providers would have to tackle difficult conversations up front with consultants around fees and their proportion of the package.
Customers should potentially be risk-assessed and have this built into the price, so it took away the complexity and was much clearer, he said.
He urged providers not to baulk at providing payment options – ‘it works in dental practices and cosmetic surgery’.
Mr Gregory said there was no doubt that waiting lists would ‘burgeon beyond belief’ with serious and unsatisfied healthcare needs, and an unknown proportion

would undoubtedly seek to pay for their own treatment.
The two questions they would ask were ‘If I do go private, is it going to be safe?’ and ‘Will I be able to get treatment more quickly than if I wait on the NHS?’
He said: ‘The next preoccupation in my view is going to be encapsulated in two questions: “Can I afford it, given the uncertainty with the economy and my own personal uncertainties?” and secondly “How much is it actually going to cost me?”
Next, on contacting the provider to understand the options, ‘they are going to expect you to get
Before Covid-19, market analysts
LaingBuisson predicted a 4.5% growth in self-pay this year and 5% next, but its consultant Liz Heath told the webinar she remained cautiously optimistic about the future.
With 725,000 fewer NHS elective admissions during lockdown, she saw a big opportunity for the private sector to meet customers’ demands.
Affordability was an issue, but with more finance plans available for customers, these could be used even by those who could afford to pay up front, because they could spread the cost at 0% interest.
Some good news for self-pay consumers was a drop in diagnostics pricing due to competition.
Patients are going to expect you to get down and personal with them and to make them feel welcome and recognised RICHARD GREGORY
Providers’ guide pricing and transparency had improved, Ms Heath reported, but the wide range in prices and an absence of explanation for this was an issue. Average price points had changed very little in the last few years, suggesting sensitivity over pricing or providers looking at efficiencies.
NHS PPU websites were still ‘very variable’ and often a missed opportunity to bring in business.
down and personal with them and to make them feel welcome and recognised’.
Price and a personalised service – the ‘me’ factor – would be the order-winners ‘and the sooner you start satisfying those order-winners, you are definitely going to start seeing a lot more self-pay demand materialising into business.’
Mr Gregory urged providers not to slip into any old habits once people returned. They needed to ‘beef up’ their game and realise that what the consumer expects is what should be driving the changes in their processes.
She believed there was a big role for consultants to lead in clinical and non-clinical technology and innovation. This would be vital to engage with potential and existing customers – and some doctors had stepped up to the challenge.

By Edie Bourne
Large numbers of doctors who worked through the pandemic fear they will face a regulatory or even criminal investigation if patients are harmed due to delayed referrals or non-Covid-19 services being unavailable or limited.
These concerns are held by more than two in five (43%) of doctors, according to a survey for the defence body the Medical Protection Society (MPS).
The defence body has now called on the Government to commit adequate resources and support to clear the backlog of referrals and delayed follow-ups in secondary care ‘to avoid a potential patient safety crisis and a tsunami of future claims and investigations’.
MPS medical director Dr Rob Hendry said: ‘It will take some time for all services to be up and running normally. Covid-19 will continue to bring pressures and complications, compounded by the upcoming winter, and this is on top of the referral backlog.
‘Buried within these many delayed referrals will be patients with serious conditions, not yet identified. For some, if diagnoses
are missed or significantly delayed, this could seriously impact those patients’ prognoses and outcomes. It’s not difficult to see how we could be facing another different kind of patient safety crisis.
‘The prospect of an adverse outcome under these circumstances would be devastating for any patient, and the psychological impact on the already emotionally and physically exhausted doctors involved would be significant.’
He said the MPS was continuing to press the Government for emergency laws to protect doctors from investigations arising from impossible situations like this.
But it hoped that through Government-led planning, support, resource and sharing of best practice and learnings, the referral backlog will be dealt with quickly and any looming crisis averted.
The BMA has urged the Government to be honest with the public about the scale of the task ahead and outline a credible plan prioritising the sickest patients left without treatment.
According to a NHS Confederation report, ten million people will be on the waiting list for NHS treatment by Christmas.
‘DOCTORS MUST BE IMMUNE FROM CORONAVIRUS NEGLIGENCE CLAIMS’
Doctors and others involved in treating patients during the Covid-19 pandemic should be able to do so without the risk of being sued for negligence.
That is the overwhelming verdict of the public in a survey commissioned by the Medical Defence Union (MDU). Seventy per cent of 2,108 UK adults expressed this view, and only 7% of respondents disagreed.

The MDU is calling for the Government to act to stop the NHS being overwhelmed by an avalanche of negligence claims over the next few years. It fears the health service could be overwhelmed in just a few years by the cost of negligence claims that it expects without Government intervention.
Chief executive Dr Christine Tomkins said doctors and staff working under the NHS banner needed exemption from ‘an avalanche of negligence claims that may otherwise follow the pandemic’.
She added: ‘Staff responding to Covid-19 are likely to be judged long after the public memory has faded, and by standards unreflective of current conditions. Anyone who says otherwise, to try to reassure doctors involved in dealing with the pandemic, hasn’t experienced the harsh reality of clinical negligence claims. It is unlikely the courts will relax long-established legal principles in judging the standard of care provided.
‘Several US states have introduced legal protections for healthcare workers. If there is political will to make this happen, as we have seen in other areas of policy, there is no reason why an exemption shouldn’t be granted.’
A network of up to five new diagnostic facilities are being set up in the UK by Rutherford Health for private and NHS patients.
It has struck a £55m development framework agreement with investors Equitix Ltd, a developer and long-term fund manager of core infrastructure assets in the UK and Europe.
Centres will provide a variety of diagnostics services including positron emission tomography, computed tomography, magnetic resonance imaging, ultrasound, endoscopy, and X-ray.
Equitix will have a right of first refusal in respect of the development and funding of a further five centres beyond the initial five.
Rutherford said it had agreed with The Somerset NHS Foundation Trust to create the first facility and it is expected to be operational in the second half of 2021.
Its chief executive Mike Moran said: ‘The demand for diagnostic capability in the NHS, and private sector, has increased significantly over the last five years with demand outstripping supply year on year.
The agreement with Equitix will

enable Rutherford Diagnostics to meet the rising demand for diagnostic clinical services.’
Equitix has over £6bn of assets under management. It has invested
in healthcare assets since its inception in 2007 and healthcare is now its largest sector for investment, representing over 39% of its total portfolio.
Compiled by Philip Housden
London leads the way NHS trusts are beginning to reopen private patient capacity following the peak of the Covid-19 crisis.
But outside London the picture is patchy, with most trusts struggling to adapt to the reduced capacity available for NHS services and working through how best to utilise the extension to the national agreement with the independent sector.
Shams Maladwala, managing director at The Royal Marsden Priv ate Care, told Independent Pract itioner Today : ‘Throughout the Covid-19 pandemic, The Royal Marsden has played a crucial role as London’s leading specialist cancer centre and continues to offer patients the highest standards of care.
‘To coincide with NHS efforts to recover cancer activity, we are increasing activity across all our services to continue to offer patients world-leading treatment and care in a safe environment.
Thanks to our unique and integrated private care-NHS model, we
continue to adapt quickly to Government guidance, putting measures in place to ensure the safety of our patients and staff at all times.
‘We have strict infection control policies, pre-assessment for each patient and regular staff-testing.
‘To minimise the number of visits a patient needs to make to the hospital, we have launched virtual consultations and a courier pharmacy service.
‘Where patients need to come into the hospital, we have a number of new safety measures in place, including more spacing to allow for social distancing in our communal waiting areas, floor markings, clear infection control signs and social distancing for staff and patients.
‘Cancer services across London are being co-ordinated by specialist “Cancer Surgery Hubs” led by The Royal Marsden and partners, ensuring patients get the life-saving surgery they require. In doing so, we have also been able to collect and analyse data, enabling an evidence-based approach to patient safety and infection control.
‘This is also supported by several research studies that our teams have launched in response to the pandemic, intending to understand and mitigate for the impact of the virus.’
He said the unit was excited to continue its expansion in the Harley Street area and work had now restarted at its new diagnostic and treatment facility at Cavendish Square.
Due to launch in early 2021, it will be open six days a week and will treat a range of tumours.
The Royal Free opened up Hadley Wood Hospital in Barnet, north London, from 15 June to both private and NHS patients.
The trust has implemented vigorous infection control protocols to ensure the facility is in line with NHS guidance. The PPU at the Royal Free Hospital remains closed, with some outpatient/ diagnostics being available for clinically urgent patients.
Medical director Prof George Hamilton said : ‘We are looking
forward to re-establishing our PPU services at Hadley Wood Hospital to deliver private elective care and NHS services.
‘We are also developing plans to open up our PPU facilities at the Royal Free Hospital site. There will be more news about this very soon.’
London North West Univer sity Healthcare NHS Trust (LNWH), experienced a peak of Covid-19 cases early on in the pandemic. Now David Osborne, head of business development at TrustPlus Private Healthcare at Northwick Park, confirmed that the PPU was being used as a ‘query Covid ward’ for the care of NHS patients. He said LNWH was working to ensure that it could provide a safe and sustainable hospital environment for all patients and staff and looking to restart private patient activity as soon as practicable.
Philip Housden is a director of Housden Group. See his feature article on PPUs in Northern Ireland on page 42
Doctors’ revalidation submission dates have been put back by up to 12 months due to the coronavirus pandemic.
It means doctors with a revalidation date between 17 March 2020 and 16 March 2021 can have their revalidation delayed for up to a year. In response to feedback from Responsible Officers (ROs), the GMC has increased flexibility during the pandemic so ROs can make a revalidation recommendation at any point from now up to a doctor’s new revalidation date.
GMC chief executive Charlie
Massey said: ‘The coronavirus pandemic is an unprecedented challenge and we are doing all we can to support doctors and employers. Deferring revalidation dates will help free up more time, allowing them to provide the best possible care to patients.
‘We’ve also listened to Responsible Officers, who told us they would welcome flexibility in making recommendations to revalidate doctors whose dates have changed. So, we have agreed that those recommendations can be made at any time up to a doctor’s revised date.’
The GMC has also confirmed that a missed appraisal as a result of the pandemic should not prevent a recommendation being made about a doctor’s revalidation.
This means ROs can make a revalidation recommendation for a doctor with less than five annual appraisals, providing there is a legitimate reason for the missed appraisal and that other necessary supporting information has been collated.
The GMC is writing to all doctors affected by the date changes with more information.
➱ continued from page 3
‘Their principal purpose is to monitor the pregnancy and, if necessary, receive a diagnosis of any abnormality.’
It was ruled that these could be considered examples of medical care, making the scanning services VAT-exempt.
Considering this judgement, it would appear there is scope to consider some other services which are primarily for the health of the consumer such as cosmetic procedures. It seems it is all in the evidence of the processes involved, the records kept and the mind-set and intention of the consumer.
By Charles King
Bupa UK Insurance has enhanced its remote services package Bupa From Home so people can access round-the-clock advice and care from the safety of home.
The move was announced after concern from doctors about people being reluctant to access healthcare during Covid-19, reflected in the sharp drop in GP referrals for cancer and mental health conditions.
New services include remote consultant appointments from thousands of Bupa-recognised consultants and a dedicated Bupa Covid-19 online hub to help people manage their physical and emotional wellbeing.
Expanded services include a Digital GP service for all UK insurance customers, available since the pandemic, and prescriptions 24 hours a day, seven days a week in partnership with the online healthcare provider Babylon.
Customers with mental health cover in their policies now have the option of consultations with

Bupa-recognised therapists over the phone or video, plus online cognitive behavioural therapy.
Bupa has expanded a rapid cardiac assessment service to all health insurance customers. This enables them to have assessments with in-depth triage by video consultation and diagnostic testing from home, speeding up access and reducing the need for face-toface visits.
Physiotherapists are on hand for phone or video consultations to assess conditions and design personalised exercise programmes
and cancer patients can have their treatment through a home chemotherapy service.
The insurer reported an upsurge in demand for remote care. The number of appointments through its Digital GP service has increased threefold since March and calls to its Anytime Healthline have more than doubled compared to the previous year.
Bupa UK Insurance chief executive Alex Perry said: ‘This pandemic has seen a huge increase in the use of healthcare delivered by phone, video or in the home. Now more than ever, customers are looking for safe and convenient ways to access advice and care to support their physical and mental health.
‘Bupa has been at the forefront of innovative new services over the past few years and expanded them in response to this crisis.
‘Bupa from Home provides reassurance for customers knowing they can speak to a full range of experts easily and often on the same day, to get the help, support and advice they want and need.’
Product and service developments for remote health diagnosis, treatment support, advice and therapy are likely to surge due to the pandemic, according to market analysts LaingBuisson.
Its Health Cover UK Market Report, edition 16 reports the number of lives covered by private medical insurance rose to 6.84m at the start of 2019 (6.83m in 2016) driven by more demand from small and medium-sized enterprises and individual policies covering more family members.
Well-being is an emerging standalone product in the market and demand is tipped to grow well in a post-coronavirus world as employ-
ers consider wider workforce coverage for employees to meet their duty of care.
Tele-health and self-management of healthcare and well-being are also expected to drive forward developments as working practices change.
But the company said Covid-19 had dealt the health cover sector a huge challenge as independent hospital capacity had been signed over to support the NHS pandemic response ‘and demand for elective acute treatment remains temporarily unmet’.
Philip Blackburn, report author, said health cover faced uncertain pandemic-related challenges due

Al Russell, CEO of the London Clinic
The London Clinic is offering video consultations to UK and international patients via a new partnership with Trustedoctor’s Connect online service.
Hospital chief executive Al Russell said: ‘We are thrilled to be introducing this new service, which will bring some of the services of our hospital, along with the unparalleled expertise of our consultants and healthcare professionals, right into people’s homes.’
The hospital said it was excited at Connect’s ability to allow multiple people to join consultations simultaneously, such as specialists, patients, family members and interpreters. Patients would have the confidence of a completely secure platform to share medical records and a clear pathway of referrals.

to coronavirus. Many businesses were unsure about their futures and unemployment had risen sharply.
Trustedoctor co-founder Lukasz Rzeczkowski said the partnership would put it firmly on the map within the private healthcare market in the UK. ‘So far, we have been working across the UK with the individual doctors, private clinics and private patient units of the NHS hospitals.’
Orthopaedic surgeon Mr Taff Edwards used the virtual platform to advise a patient in Russia ahead of treatment at the hospital. He said: ‘This will definitely become a standard for patient-todoctor interactions in the future. London is a highly respected medical hub and international patients need to establish trust with their designated physicians before they make their decisions about treatment options. The Trustedoctor platform is a game-changer in this sector.’
By Leslie Berry
Official figures confirm the extent of the financial battering suffered so far by independent practitioners during the Covid-19 pandemic. It is estimated there has been an 84% drop in privately funded care.
After a slight rise in the estimated number of overall privately funded episodes of care – 3% in January 2020 and 4% in February 2020 – in March, the data shows an estimated drop of 30% compared with 2019.
To follow was an estimated 84% drop between April 2019 and April 2020.
According to the Private Healthcare Information Network (PHIN), the type of private treatments delivered during the pandemic has also changed significantly, with medical oncology becoming the largest single specialty performed, making up an estimated 63% of all privately funded admissions in May 2020.
PHIN said these insights were based on its private healthcare dataset and look at how the nature of privately funded care changed as the UK went into lockdown and independent hospitals and NHS private patient units diverted resources to support the NHS.
PHIN’s chief medical officer Dr Jon Fistein ( pictured right ) said: ‘While the impact on privately
funded care is still emerging, with some of the underlying data still incomplete, we can start to picture the impact Covid-19 has had on the private healthcare market in the UK.
‘As hospitals have diverted their resources to support the NHS effort, private care took a back seat. It is reassuring to see that urgent care – such as medical
Footnote:
Year-on-year change is calculated using sites with confirmed volumes for 2020 and 2019 for each month, removing influence of delay in private data submissions due to Coronavirus. 2020 volumes are estimated based on sites with confirmed activity. Estimates assume these sites are representative of the entire market, with confidence varying depending on number of submitting sites.
oncology – has continued to be provided during the difficult time.

‘We will be keeping an eye on the situation and what happens over the coming weeks and months.’
Specialty
Trauma &
The analysis was launched in PHIN’s new Quarterly Digest – a new newsletter with insights from PHIN’s data, updated from PHIN’s work, and expert opinions.
General surgery
Other Medical oncology
Ophthalmology
Gastroenterology
Specialty
Trauma & orthopaedics
General surgery
Other
Medical oncology
Ophthalmology
Gastroenterology
Urology
Footnote:
Plastic surgery
Gynaecology
ENT
Anaesthetics
Urology
Plastic surgery
Gynaecology
ENT Anaesthetics
Recent share is based upon only sites that have submitted data more recently. However, the make-up of these providers is generally representative of the entire market. While medical oncology represents a greater proportion of activity than seen historically, this may be influenced by larger variations caused by smaller number of discharges.
Medical oncology May 1st 63% of private discharges
Medical oncology
May 1st
63% of private discharges
THE LONDON Consultants’ Assoc iation (LCA) survey results ( Independent Practitioner Today , June 2020) demonstrated that the consultant body – the doctors who provide the services the private sector has flourished on – have a less than optimistic view of the future
They feel they have had little involvement in any proposals to restart private practice.
With our sister organisation, the Federation of Independent Practitioner Organisations (FIPO), we are in close touch with their memberships and the frustrations and the inconsistencies they are experiencing are informing our views.
The extraordinary cooperation between the private hospital providers and the NHS during the emergency was to provide bed capacity should the NHS become overwhelmed.
But the private healthcare market is not only restricted to the hospital providers; it also comprises the private consultants, the insurers and, of course the patients who choose to use its services.
There is a need for all these components to work together to develop a strategy for the future survival of the sector. Apart from the consultants, who recognise the reality of the destruction of their business, there seems to be a mistaken acceptance that there will be natural restoration of private practice after the Covid pandemic.

DR MARK VANDERPUMP, Chairman, LCA
This is unlikely to occur without an underlying support strategy and there is a need for all these components – insurers, providers and the consultants – to work together to develop a strategy for the sector’s future survival.
Major issues identified include:
Loss of public confidence in accessing healthcare;
Difficulties for insurers in delivering the services their subscribers pay for;
Finding sufficient fee capped consultants who will wish to continue to work privately;
Providers who are reintroducing access to their hospitals with inconsistent protocols for both inpatients and outpatient clinics. These vary significantly even between sites within the same provider.
All these difficulties, coupled with the continuing increase in
There seems to be a mistaken acceptance that there will be natural restoration of private practice after the pandemic

HITTINGER, Company Secretary, LCA
indemnification costs and the other overheads of private practice, mean many consultants who would be considered at the peak of their career have stated that they will give up private practice entirely, as evidenced in the LCA survey.
The private sector provides a safety valve for the NHS and contributes an estimated 10% of healthcare in the UK.
With waiting lists predicted to reach up to 10m and strict rationing in the public sector inevitable, it is in all interests that the market survives.
We believe there are a number of actions that those who comprise the private healthcare market and who are to some extent codependant could consider to support private doctors and help reestablish private healthcare:
Many consultants who would be considered at the peak of their career have stated that they will give up private practice
Low insurer reimbursement levels for ‘feeassured’ consultants, applying to all younger consultants given recognition in recent years, is making private practice increasingly financially nonviable.
There has been minimal reimbursement rises since the early 1990s, with many of the reimbursements for the most common surgical procedures reduced significantly.
As older, non ‘feeassured’ consultants retire, this will leave behind a generation of ‘pricefixed’ consultants, many of whom indicated their intention to retire from private practice in our survey.
During the crisis, re imbursement must be considered within the context of reduced patient flows and increasing overheads. Insurers must withdraw threats to deflate re imbursement for ‘virtual’ consultations (see overleaf).
To encourage private patients to remain with an insurer, we suggest they reinstate access, even temporarily for one year, to those insured
patients with exclusions to policies such as chronic disease management and pre existing conditions.
Ensure consistency with Covid protocols for admissions and clinics, waive room rental charges for a defined period – for example, three months, dependant on an approach to the Competition and Markets Auth ority (CMA), see below.
The LCA has advised each consultant to send a communication to all those patients on their individual practice list to inform them that they are open for business.
The private hospitals should undertake to do the same by going direct to the community and informing them that private practice facilities are now open and available by advertising in The Evening Standard , Metro , The Times and Telegraph, as these papers are read by the majority of private patients.
It would also be beneficial for the hospitals to inform the GPs that business is returning to normal.
Having good, well communicated infection control and safety policies and procedures would also help reestablish patient confidence.
We believe that the IHPN, as the representative organisation of the private hospital providers, is well placed to approach the CMA on behalf of the entirety of the sector. The remedies demanded from the private healthcare market investigation of 2014 are no longer proportionate or appropriate. The market is now entirely different and will remain unrecognisable for some time to come.
Hospital episode statistics and data flows should be streamlined and directed to a single body so that the financial overheads for the sector for these data flows are reduced.

Following the London Consultants Association urging doctors to think twice before accepting 50% fee cuts from insurers for virtual consultations – see our website story, 17 June – surgeon Mr Ian McDermott spells out why this work is worth every penny



ONLY SOMEONE who has not been forced into doing tele-consults with their patients would ever try and tell you that they are easy . . . because they are absolutely not.
So-called ‘telemedicine’ via platforms such as Zoom or Microsoft Teams has been a life-saver over the Covid lockdown period, and it has allowed doctors to still be able to have consults with those patients who need to be ‘seen’.
We have read a lot about the positives of telemedicine and how this could ‘transform’ the way that we work. The reality, however, really is not quite that simple.
Scheduling video consults oneself is somewhat tedious and timeconsuming.
Some platforms such as Doctify or Meddbase are now offering video consult facilities, which might make scheduling and setting things up easier – but only ever always at a price, adding even further to consultants’ costs.
However, the real problem with telemedicine is the significant disruption that occurs to the normal human-to-human interaction. With telemedicine, one loses a large proportion of the usual nonverbal communication cues that can be so vital when trying to form a rapport with a patient or when trying to work out a complex problem or discuss difficult or bad news.
Far from ideal
It is also far harder to guide or direct a conversation when speaking to someone remotely, which makes it more difficult to target key areas and focus the discussions on key issues.
In some instances, it is possible to do a very basic elementary visual clinical examination; for example, asking someone to move their knee within the field of the camera. However, this is far from complete or ideal and of no use whatsoever for many specialties.
In my practice, Zoom and Teams have been an absolute blessing, but to think that they have made clinical appointments easier would be completely wrong.
A proper tele-consult is more difficult, more tiring and slower than an equivalent face-to-face appointment, with a higher propensity for miscommunication and for errors.
It defies belief that any insurer should kick us even harder when we are already down by imposing a 50% cut in re-imbursement rates

Mr Ian McDermott: Says a fee cut will be another nail in the coffin of private practice for doctors already struggling due to the pandemic
Indeed, prior to the lockdown, some medical negligence insurance companies did not actually cover video-consults, although thankfully they did issue special cover notes once it became apparent that tele-consults were becoming a necessity.
Personally, I am very thorough in what I do and my tele-consults tend to take up the full half hour or even one-hour slots that I allocate each patient – depending on what prior warning I receive as to how complex their case might potentially be.
However, after the consultation, one then has to dictate the patient’s clinic letter, and this can take several minutes.
At a later stage, one also then has to check and edit one’s clinic letters too. This normally adds on at least an extra 15 minutes in total to each patient slot.
Added to this, however, is the enormous amount of additional time that it now takes to actually get anything done, in terms of trying to book patients in for investigations or actual treatments. There is now a myriad of additional forms and new processes, which seem to change on a weekly basis.
There are also constant obstructions imposed on us due to the stifling bureaucracy of the NHS. So, everything is now more than twice as difficult and is taking more than twice as long as normal.
So, what is the reaction to all this hardship by some of the private medical insurers? To cut reimbursements for tele-consults by 50%.
It has been quite evident for a long time now that certain of the insurers have opted to pursue a strategy of ‘cheap’, with a blatant ‘race to the bottom’.
However, this approach is deeply cynical and really quite blinkered, and will only serve to damage the entire sector.
At a time when:
The number of private patients seeking treatment has plummeted;
Access to clinic space for most people was removed for all except just a tiny number of emergency cases;
Private consultants’ and private patients’ access to theatre slots has been decimated and relegated in most private hospitals to just limited evening and weekend slots only;
It is taking more than twice as long to get anything done;
Theatre productivity rates and throughput have dropped to well below 50%;
The very future of private practice itself is under significant threat. It defies belief that any insurer should kick us even harder when we are already down by imposing a 50% cut in reimbursement rates.
And all this at a time when most of us are still carrying enormous inevitable ongoing costs.
The recent London Consultants Association (LCA) survey (Independent Practitioner Today, June 2020) has highlighted that many consultants no longer view private practice as worthwhile or financially viable. This act by some private medical insurers will be just another nail in the coffin of private practice for some.
For others, like water inevitably
finding its way to the sea, they may simply choose to find a way round this latest hit – with the only feasible option being to reduce teleconsult slots to 15 minutes or even less.
Lowering quality lowers safety and takes away one of the unique selling points and the raison d’être of the whole private sector, which is its differentiator from cheap lowquality conveyor belt-style medicine.
Perhaps some cynical insurers believe that some consultants might be using tele-consults as an excuse to rack up reams of fees for a host of quick five-minute ‘how are you doing’ check-ups?
If some consultants are actually doing this, then they need to be identified and routed out. However, for the vast majority of consultants, we are in medicine specifically to deliver the very best care we can for each and every patient and, in current times, teleconsults have been somewhat of an evil necessity and a burden, as well as a positive blessing.
Increasingly, as the financial consequences of the Covid crisis hit, individual policy-holders and corporates will question the value and necessity of private health insurance.
To those insurers who seem determined to rush ever faster in their race to the bottom – good luck with what you might well eventually end up finding down there.
Mr Ian McDermott is consultant orthopaedic surgeon at HCA’s London Bridge Hospital and managing partner of the London Sports Orthopaedics practice

A look back through our journal’s archives of ten years ago reveals that although times change, some issues are not so new


Consultants working in the Harley Street medical enclave were losing potential overseas patients to other specialists abroad who were promoting themselves more aggressively. Has anything changed?
Independent practitioners in London and elsewhere were being advised to take serious marketing action to tackle the trend and protect their profits.
One practice that did so revealed to Independent Practitioner Today that is had reversed a £100k income drop by sending its manager to Middle East medical functions.
She said: ‘The doctors recognised we needed to engage with potential patients and their referrers because London is not now their only medical destination.
‘We re-engaged with referrers and patients and reversed a trend
in lower patient numbers. It has been a worthwhile investment of time and resources. Other practices need to consider doing this according to their patient mix and specialty.’
But Keith Pollard (right), the then boss of a treatment abroad website, said he was the ‘only Brit’ at medical travel events in Dubai, India, Singapore, Korea, Hungary, Malta, Cyprus and Italy the previous year.
He warned that Harley Street’s reputation as a centre of medical excellence was not getting across to doctors’ would-be customers abroad.
Harley Street was ‘missing a trick’ and losing out in a big way while other international medical centres promoted themselves, he claimed.
Doctors completing fee-paying reports were being advised of the importance of completing them quickly.
The Medical Defence Union’s (MDU’s) warning followed the case of a GP criticised by a coroner for failing to provide a report into a patient, despite apparently being contacted five times over the previous seven months.
The MDU said it was clear that if doctors had agreed to prepare a report or provide evidence, they must do so without unreasonable delay.

The BMA’s private practice committee welcomed Bupa’s resumed recognition of new consultants for re-imbursement purposes.
Its chairman, Mr Derek Machin, said he was ‘delighted’ there would be no time restrictions from the insurer.
He told the BMA’s Annual Representative Meeting in Brighton that the union had remonstrated with Bupa over the suspension of new recognition, which began the previous 23 December.
‘They told us that they wanted to review the recognition process because they were concerned that newly appointed consultants were not sufficiently experienced to undertake independent practice outside the more supportive NHS,’ Mr Machin said.
‘They had discussed this with the top-earning consultants and produced a survey of existing, recognised consultants, which asked whether newly appointed consultants should be excluded for one, two or three years. In other words, would you like to stymie your keen young competitors for one, two or three years? We rigorously opposed this and other suggestions in their survey.’
Bupa said it had listened to feedback from consultants, medical bodies and customers and had made no decision at that time to change its Bupa Partnership.
Chancellor George Osborne’s first Budget brought a welcome triple boost surprise to private doctors. Accountants said the Budget gave independent practitioners even more benefits from incorporation.
It also provided increased incentives to build up their practice and keep more money when they sold it.
And it encouraged more young doctors to start up independently.
Share your experience of what has and has not worked in your private practice. Even if it’s bad news, let us know and we can spread the word to prevent other independent practitioners falling into the same pitfalls. Contact editorial director Robin Stride at robin@ip-today.co.uk





Julia Burn continues with her A-Z of top tips from the accountant’s desk. This month she turns to a –very topical ‘L’
AS I WRITE this, it is still not clear to many independent practitioners when they will be approaching some sort of normality
Recent polls in the media show that many members of the public fear that releasing the lockdown is too early, so will they visit practitioners anyway? This is reflected in the low numbers contacting GP surgeries and, indeed, turning up at A&E.
With the return to normality likely to be a gradual one as various lockdown restrictions ease, it is important to revisit financial forecasts and amend them as you get greater clarity on levels of trading.
This may mean you need to revisit your cash flow requirements and apply for either a bounce-back loan or make an application for a Coronavirus Business Interrup tion Loan. Both schemes remain open.
Also, part-time work may be more appropriate for your staff and their taking advantage of the flexible job retention scheme should also be explored.
One of the major issues that practitioners need to think about when they do return is their IT security and that of their colleagues and patients.
Practitioners need to be as savvy
as they can as they go back to work and get their systems up and running.
There have been numerous phishing emails ranging from those telling taxpayers they can claim tax refunds to help protect themselves from the Coronavirus outbreak, to ones stating that someone is eligible for a tax refund. These ask you to click on a link or visit a particular website in order to make your claim.
There will be additional security risks as practitioners go back to their consulting rooms, hospitals, clinics and surgeries.
Cyber criminals will be looking to attack businesses from every angle and will be looking for weaknesses in not only the technology that they use but also the way in which they operate, especially those that suspended operations for a period.
Practitioners will be under pressure when they get back to work to get going and to start generating revenue, but they need to make sure that they do not compromise their situation by rushing and not taking the necessary steps.
It is not just phishing attacks. Systems could have been hacked while staff were furloughed, ready
to be exploited when individuals return to work and it is important that software security is up to date and that subscriptions for those have been paid on time.
Practitioners also need to make sure their normal control procedures are adhered to and not compromised due to individuals not attending their normal place of work. Criminals will be looking hard to see how they can take advantage of the current situation.
Practices should always be alert to possible attacks. Phishing is an ongoing issue, but there is still the threat of ransomware which targets organisations through loopholes outside of the email vector. For example, servers and ports can be left unintentionally open to the internet and therefore are open to attack. Cyber criminals often rely on businesses not knowing their systems and these access points. Now is a good time to get to know the entire IT infrastructure to find any holes.
Malware disguised as a popular app or software will continue to be an issue. It is imperative that staff are allowed to download and install only those from legitimate sources, like Google Play, App Store or directly from vendor website.

It is better if these approved software and apps are distributed through a centralised system managed by IT. Physical security devices like CCTV and biometric scanners that are used to protect the office should be monitored and checked more closely than before for anomalies and tampering.
What is normal network activity for a remote workforce may not be when they are ensconced back in the office. Whether a business has in-house or outsourced security operations, there is now a need to retrain the team to spot ‘new’ suspicious behaviours and how to take necessary action.
While the digital era has already witnessed a wide variety of scams, the outbreak of Coronavirus has led to a sharp increase in the number of ways individuals are being contacted by fraudsters who represent themselves as HM Revenue and Customs (HMRC) officials. Here are a range of examples of the types of scam in circulation, with advice on how to recognise them and avoid being taken in.
Coronavirus-specific scams
Emails telling taxpayers they can claim tax refunds to help protect themselves from the Coronavirus outbreak;
Text messages telling taxpayers
they can claim a goodwill payment from HMRC;
Text messages threatening to impose a fine for leaving the house more than once.
Neither the HMRC specifically nor Government more widely communicates with individuals either by email or by SMS text, unless you have signed up to the relevant protocol with them.
Certainly, payments that can be claimed by taxpayers or fines that can be imposed are not dealt with in this way. However, fraudsters may change the ‘display name’ on their email address to make it appear genuine.
Although these scams have been around much longer, it is worth a reminder to be wary and to reiterate that HMRC does not use these forms of communication to notify taxpayers of refunds. These scams could be in the form of:
Emails which state that you are eligible for a refund and ask you to click on a link or visit a website to make your claim;
Text messages claiming to be from HMRC offering you a tax refund if you provide personal or financial details;
WhatsApp messages or social media messages.
How to handle these scam messages
If you receive one of these messages :
➠ Do not reply to these emails, texts, WhatsApp or social media messages.
➠ Do not call the phone number listed in an email or text.
➠ Do not click on any links or open any attachments in emails.
➠ Do not provide any personal or financial details.
➠ If in doubt about whether an email or text is genuine, click on/ hover your cursor over the ‘display name’ email address from which you have received the email. This will show you the full details of the sender and will make it clear whether the email is from a genuine Government or HMRC source.
➠ If you are still unsure, forward it to HMRC and then delete it. If you are in doubt about the source of one of these messages, forward it to HMRC.
You can do this via email at phishing@hmrc.gov.uk or via text at 60599 (network charges apply) and then delete it.
Phone calls threatening legal action
Taxpayers have also received calls stating that they owe significant amounts of tax and that unless
The outbreak of Coronavirus has led to a sharp increase in the number of ways individuals are being contacted by fraudsters who represent themselves as HM Revenue and Customs officials
they press 1 to speak to a caseworker and make a payment immediately, legal action will be taken against them. HMRC do not make such calls.
If you receive such a call, disconnect immediately and report it to HMRC at phishing@hmrc.gov.uk including details of the date of the call, the phone number used and the call content.
Finally, be aware that if you receive an offer from a company to apply to HMRC for a tax rebate on your behalf, they are not connected with HMRC in any way. They will normally charge a fee, which could be sizeable.
Always read the disclaimers and small print before using this kind of service.
Businesses and individuals now have to be on their guard as we come out of lockdown and gradually get back to work. The Government’s ‘Stay Alert’ statement is just as relevant to keeping us safe from an IT perspective as it is to one of public health.
Attacks can come from any quarter to our PCs, laptops, smartphones and via emails and texts. We must be vigilant to protect both ourselves and our business.
Julia Burn is a senior manager at Blick Rothenberg
Private doctors’ organisations – as we reported on our website news section last month – have welcomed an NHS England (NHSE) pledge paving the way for a resumption of consultants’ work in the independent sector. Independent Practitioner Today here shares contents of the letter that raised private doctors’ hopes of getting back to independent practice.
Sent to regional bosses last month, it is from Neil Permain, director of NHS operations and delivery, NHS England and Improvement. We hope you find it useful. Do let us know how the return to private practice is being facilitated in your area. Email robin@ip-today.co.uk
I’M WRITING to clarify some issues about the current ‘de-escalation’ phase of the national independent sector contract following a number of questions from both NHS colleagues and from the independent sector.
On 15 May 2020, in acknowledgement of the improving national picture for the NHS with regard to the operational pressure from Covid-19, we entered the next phase of our arrangements with independent sector providers.
The de-escalation notice issued on that day enabled independent providers within our arrangements to restart routine elective activity, for both NHS and private pay patients.
This followed the national letter to the NHS of 29 April 2020 and reflected the subsequent plans within some NHS regions to resume elective work, and the need to enable independent providers to deliver it.
The national picture has continued to improve, with NHS hospitals and wider health systems recovering more capacity following the initial Covid-19 surge...
As the 15 May notification set out, the resumption of routine
elective activity for both the NHS and for private patients was subject to NHSE’s approval locally.
We authorised each Local NHS Lead, or a nominated system or local deputy, to discuss and agree resumption with local independent providers as appropriate.
However, the way that this deescalation phase in the contract has been interpreted by the Local NHS Leads has been highly variable and in a number of cases not consistent with the spirit or terms of the contracts we have with the IS providers.
I’m writing, therefore, to try and clarify the position and explain what should and should not be happening at this stage. The clarification is set out in the explanation and examples below, and any further questions can be escalated via the IS Coordination Team at england.ISCoordination@nhs.net.
De-escalation is a stage when it is allowable to resume routine elective work for both NHS and private work. If one applies – i.e. its allowable to do NHS routine work in general – then the same applies to private work in general.
The de-escalation stage was designed simply to acknowledge the point at which the NHS was no longer restricting all routine elective work, with ‘Surge’ having been defined as the point where elective work was restricted and so shouldn’t be carried out for either NHS or private work. So the contract de-escalation phase was very much an on/off decision point where we came out of surge and away from that position of totally restricted routine work.
There was no intention, and there is no contract mechanism, to allow for the following:
For the decision to be reversed –there is no mechanism under the contracts to retract the permission to resume routine NHS and private electives once it has been given – so we have either left the stage where routine elective is totally restricted or not. We can’t keep re-applying and removing the restrictions.
For operating restrictions on private work at a specialty or subspecialty level – so we can’t pick and choose what types of private elective care can be done in any particular locality or at any particular time.
For approval forms and separate approval processes with additional criteria setting out terms for resumption.
For mandated common PTL [patient tracking list] management with NHS input to decisions about individual private patient admission decisions.
What does remain in place – and this is the key principle and contract mechanism that continues to apply that the permission to resume electives is in the context of there being excess capacity – is the overriding obligation of the independent sector provider (ISP) to:
‘Make available to the Commissioner all facilities, diagnostics, staffing, management and full organisation capability (the latter to include but not limited to central management and administrative support services), necessary for the provision of the Services to Service Users [i.e. the defined services for NHS patients] and for the support of the response by the NHS to the Covid-19 pandemic in accordance with this Service Specification.’ So this key clause makes available to the NHS all of the capacity of the ISP should you need to use that capacity.
This clause also effectively deals with the situation in which there is another Covid-19 surge during the period covered by these arrangements, because if the NHS needed all capacity in the ISP to cope with the surge, then private work would have to cease to ensure NHS total access.
So, if we found that staff and resources were being diverted to private work at the expense of NHS work, we would draw providers’ attention to that obligation. This is, in practical terms, going to apply if we are directing NHS work to the IS, or asking to locate NHS teams in the ISP to do NHS work, and finding they have no capacity, or are refusing that work, during the remaining term of the current arrangements.
If there is no capacity conflict, then we can cannot (sic) restrict
private routine work for any other reason; for example, trying to restrict the times for NHS work and then not using those times.
We don’t want to undermine locally agreed approaches on prioritisation with the ISPs and these should continue if mutually agreed.
Exceptions to the national resumption policy may also be needed; for example, where the local system is unable to start any routine NHS electives due to severely restricted capacity or exceptional Covid-19 pressure, but these are only exceptions where there is a complete continued restriction on any elective work.
In all other cases, I am confirming here that the default position is that ISPs have permission to resume routine electives – both NHS-funded and private – nationally anywhere in the country, subject to all other provisions in the contract and particularly the prin-
ciple of making full capacity available to the NHS if needed, as set out above.
Decisions about the referral and prioritisation of NHS patients will be for local NHS organisations to make. They will continue to make judgements about when and how different types of routine NHS elective work is resumed, and how capacity across providers is utilised for NHS work.
This includes, for example, total discretion over whether Choose and Book/ERS referral is switched on locally.
For privately funded patients, however, scheduling, prioritisation and resumption of types of work is entirely a matter for independent providers, rather than for the NHS, to determine.
The wider context, of course, is that under the current arrangements, any private patient admitted to an ISP during the current
contract term results in a financial offset to the cost to the NHS – so any capacity that you are not using in your ISPs and that is used for private patients reduces the cost to the taxpayer.
Where there are concerns within NHS or independent sector organisations about the application of the policy, the relevant parties should escalate this to the IS co-ordination team, who will provide assistance in resolving the matter.
Whilst maintaining the resilience of the NHS to cope with the ongoing Covid-19 pressures, our common aim is to ensure that as many patients as possible receive the care they have been waiting for, both across the NHS and the independent sector. We greatly appreciate your co-operation in making this happen.
See ‘It’s time to give doctors their lives back’, p20












David Hare, boss of the independent hospitals’ national body, gives this message to Independent Practitioner Today readers:
‘We are doing everything we can to release
private practice
and get more
private consultants back to work’
ONE OF the paradoxes of the coronavirus pandemic has been that healthcare has been blowing hot and cold.
While in some ways the health service has never been busier –dealing with thousands of hospital admissions for Covid-19 in what undoubtedly represents the biggest healthcare challenge in a century – in many ways, it has been a time of mass underutilisation of health services.
Indeed, the most recent NHS performance figures – the first to show the impact of lockdown on the health service – have demonstrated astonishing falls in the number of GP appointments.
There has been a 70% drop in the number of people referred for routine elective care compared to the same period last year, a plummeting in the number of diagnostic tests being carried out and rapid falls in A&E attendances.
To coin the phrase of the pandemic – these are unprecedented times. And no more so than for many independent doctors.
Livelihoods affected
Their livelihoods have been drastically altered by the private healthcare sector’s deal with the NHS whereby virtually all independent inpatient capacity has been blockbooked, coupled with the suspension of all routine elective care for both NHS and private patients.
And for a sector that delivers almost a quarter of a million acute private patient journeys each year, this is a significant change to their way of life.
I firstly want to assure Independent Practitioner Today readers that
We acknowledge that now is the time to ramp up non-urgent work done across the NHS and the private pay market
independent healthcare providers absolutely understand the impact this has had on consultants’ working life and the frustrations they feel and, as a sector, we are doing everything we can to release private practice and get more private consultants back to work.
Unprecedented times call for unprecedented actions. And as we look back just a few short months ago to March, when this contract was first agreed, it was based on an urgent and pressing need from Government to block-book all of the private hospital capacity in the face of an unknown pandemic, which had overwhelmed many countries’ health services across Europe and effectively rendered most of the population housebound.
Equally, while tackling coronavirus and ensuring that the acute and critical care facilities were in place was a priority, it was also acknowledged that urgent cancer and cardiac care must be enabled to continue during this time and hence the need to secure as much inpatient capacity as possible.
It was therefore right that the
providers responded to this unprecedented call for national help – a contribution which has been recognised and welcomed by the public.
Recent polling by the Independent Healthcare Providers Network (IHPN) found that three-quarters of the public were aware of the deal, with two-thirds believing it was right that the independent sector has supported the NHS during this time.
Much excellent partnership working has taken place during this time, with NHS oncology departments moving wholesale into private hospitals, benefitting tens of thousands of patients up and down the country, from Norwich to Nottingham, Southampton to Salford.
But with new Covid-19 cases thankfully having come down in recent weeks and hospitalisations also falling, we acknowledge that now is the time to ramp up nonurgent work done across the NHS and the private pay market, not least given that recent analysis has shown that NHS waiting lists for elective care could hit ten million by the end of the year.
In recognition that we are now ‘post-surge’ in terms of the virus, since 15 May the NHS has activated the de-escalation period under the contract that enables non-urgent work to be conducted, providing local NHS sign-off has been given.
That process has been bureaucratic and while progress has been made in all areas of the country with private work starting to flow,
further communication has recently gone out from the NHS leadership to local teams making clear that private elective work should only be prohibited where local areas are undertaking no elective work, whether NHS or private, or where independent sector is being utilised by the NHS.
We believe this will give the green light to independent providers to kick-start their private work once again, and where there remain blockages in this happening, the sector – including IHPN –will continue to do what they can to resolve such issues.
Looking forward, while it looks like we are through the worst of the virus for the moment, with a huge backlog of operations to contend with and the real prospect of a second wave of the virus this winter, independent healthcare providers are committed to continuing to support the NHS through this very difficult time.
But, equally, a dynamic private patient market is key to their business – and, of course, the wider British economy – and as the end nears for the current NHS contract, providers are committed to supporting independent practitioners and establishing new arrangements to ensuring that their livelihoods not only survive But thrive.
See ‘Get ready to re-open’, p30
David Hare (right) is chief executive of the Independent Healthcare Providers Network (IHPN)

Last month, Jane Braithwaite (right) described why patient experience is so important. This month, she gets practical and discusses how to get started or review and evolve your current strategy


YOUR PATIENTS must be at the centre of every aspect of your thinking. To improve patient experience, then, patients must be put first.
When producing any strategy, and particularly when considering patient experience, the key components to consider are your vision statement and your goals and objectives.
Your vision statement focuses on tomorrow and describes what you want to become. Many companies create both a mission and vision statement, with their mission statement describing what they are today.
If we take HCA Healthcare for example, its mission and vision statements are as follows:
Mission – Our mission is to provide compassionate care and exceptional service to every patient, every day.
Vision – Our vision is to be a worldclass hospital.
It also has a clear set of values, which you can see listed on its website and you may find these interesting and potentially helpful.
In developing your patient experience strategy, you may wish to develop your mission and vision statement and your values, and I would highly encourage this.
As a minimum, I suggest you need clarity on what you aspire to be and therefore your vision statement is essential.
Your patient experience vision must be entirely patient-focused and should describe what you aspire to be in the experience of your patients.
Your vision will become your roadmap. Writing a single statement that encapsulates this is difficult and you may prefer to write a small number of statements that
give you clarity and communicate these to your team.
Armed with your vision statement, the next step is to clarify the goals and objectives that need to be achieved to deliver this ambition and make it reality.
It is often easier to set quantitative goals that are tangible and we often see these described as service levels.
But we also need to address qualitative objectives, which are softer and more emotional and therefore harder to define and even harder to measure. Measurement is crucial and we will dedicate a full article to measurement later in this series.
A good starting point is always to reflect on our patient expectations and ask the question: ‘What do patients want?’
Taking first our quantitative, tangible goals; we know that funda -
mentally our patients want a good outcome from their treatment and we can set very precise objectives and measurements related to this. We know that patients will be able to access an increasing amount of information regarding surgical outcomes via the Private Healthcare Information Network (PHIN), although currently it is fairly limited – for example, the number of cases you perform for each type of surgery – but this will be enhanced in time.
Your specialty or NHS hospital may have certain goals for surgical outcomes, but you may want to set you own objectives that differentiate you, say, from other surgeons. If we pose a slightly different question such as ‘What do patients want before, during and after treatment?’, we start to consider a broader set of goals.

When a patient is researching their symptoms and the treatments available, they want access to high-quality information from a highly regarded source that is accessible to them in terms of language and the way it is presented.
Website is key
There is an opportunity to ensure that your website and any other collateral that you provide to patients is written accordingly and enhances your patients’ experience of your practice.
We know that patients want to be able to contact you easily, the phone needs to be answered reliably and needs to be answered in a manner that enhances your patients’ experience.
New patients want quick access to their first appointment, as they are anxious and highly motivated to explore treatment options. How quickly do you want to ensure you see new patients? Is one week acceptable for your patients? How quickly do you need to be able to offer surgery?
The answers to these questions
will become your goals and will dictate how you set up your clinic and theatre lists and give your team complete clarity on how to organise your practice.
This same approach should be taken when thinking about followup activities, such as communicating results.
Every interaction your patient has with your practice should be considered.
Now let us turn our attention to the less tangible, qualitative and emotional aspects of patient experience and set goals for our patient experience strategy that ensure we deliver against these important but often overlooked aspects.
Again, we think about this from the patient’s perspective by asking ourselves questions like ‘How do you want your patients to feel about your service?’
We are trying to understand what patients want in a wider sense than merely the treatment they receive. Another approach is to consider ‘How do you want
patients to describe your service to their friends and family?’
Some common phrases that we may want our patients to use include: ‘I trust my doctor’, ‘I feel safe’, ‘I feel well informed’ and ‘They are easy to contact’.
When a patient is researching your service, ideally, we want them to feel an emotional connection: ‘This doctor understands me’.
You may find useful insights in how your patients feel now by looking at ‘thank you’ cards and emails that you received recently.
What words do they use to describe you? Are these in line with your vision?
In fact, any patient feedback provides a good insight into how your patients feel about your service now and offer you a baseline to measure yourself against. More on this when we talk about measurement in a future issue.
You may need to review the patient information you offer, including your website to ensure it reflects how you want your patients to feel. Are you providing enough information regarding preventative care and aftercare ?
One aspect of private healthcare that we shy away from considering is price, but this is an important part of your patient experience strategy.
You may want to ensure that you are highly competitive from a price perspective or you may be more aligned to a certain brand of lager with a view to being ‘reassuringly expensive’.
Either approach is good, but your patient experience strategy must support this.
As you confirm your goals and objectives, you will be thinking about who is involved in delivering your patient experience. It is important to identify everybody in your team who interacts with your patients and to ensure that this group of individuals feels and acts as a team. Later in our series, we will discuss in detail some ideas on how to achieve this.
The physical environment in which you see your patient is clearly very important and often limited in how much change you can make. Ask yourself: Is your clinic/consulting room easy to find?
How inviting is the reception area and your receptionist?
How good are the facilities including the waiting room, toilets and, most importantly, your consulting room?
How can we ensure that these physical characteristics enhance your patient experience?
A final point is that patient expectations are always evolving and your patient experience strategy will need to be reviewed regularly to ensure it addresses these changes in expectations.
The Covid-19 crisis has changed our patient expectations and we need to ensure we are mindful of this.
Six months ago, our patients would have expected their first appointment to be a face-to-face consultation with you but now many patients would prefer to have an initial consultation by phone or video prior to committing to travelling to see you face to face.
This may also be true for followup appointments. In time, this may revert, but for the foreseeable future this type of expectation needs to be addressed.
In summary, patient experience is about always putting the patient first. In creating your strategy, you will need to define your vision statement, describing where you want to be and then define clear goals and objectives to allow you to deliver that vision and make it reality.
Your goals will be quantitative and qualitative and will need to be defined clearly so that they can be communicated, understood by everyone on your team and measurable. And you need to build in a review process to adapt your strategy to embrace changes in patient expectations over time.
Next month, we will be focusing our attentions on how we put patients first and how we deliver excellent customer service before, during and after their treatment. As part of this, we will explore how we support patients with helpful and accurate information throughout their treatment journey.
Jane Braithwaite is managing director of Designated Medical, which offers business services for private consultants, including medical secretary support, book-keeping and digital marketing

Home and remote working for independent practitioners and their staff opens great possibilities for flexible working practices, but it also significantly increases the risk from cyber threats and data breaches, warns Murray Hart
1Firewall and antivirus protection
There is no way around it, you just need to have these to be safe.
Antivirus software is important to have on your personal computer, but its importance is even bigger if you are using your own computer for working. Prevent malware from compromising your work and your systems.
It is highly likely that your own device does not have security measures as secure as your workplace one.
Firewalls acts as a barrier, preventing unauthorised access to your device or network. Your place
of work may have a network firewall on the company router and a personal one on your individual computer making it harder for hackers to get through.
Antivirus software protects your device from malware, such as viruses, worms and Trojans. Ensure both securities are kept up to date.
This may well have been done automatically in the workplace, but a personal home-based computer is unlikely to have both precautions in place, meaning the data stored is less secure.
It is therefore important to con➱ p26

sider tightening up other areas of security to lessen the risk.
If you are using a computer provided by your employer, this should be checked for you. If you are using your own computer, you can look at getting a virtual private network (VPN) to secure your connection and encrypt your data further. With VPN, your important data cannot be accessed by anyone you do not want to.
2 Designated drive or system – or Cloud-based workspaces
If you have network access, you should save files to the designated drive or system and ensure no files are left on your own hard drive.
An alternative is for your practice to provide Cloud-based workspaces. This may need discussion, but is relatively inexpensive and particularly relevant to sensitive medical information.
As an added security feature, I recommend always encrypting the hard drive of your computer or laptop if using it from home.
It does not prevent a potential hacker gaining access; rather it means that if unauthorised access to the data is gained, all they can see is ciphertext.
The sensitive information is scrambled into random code, so is of no use to a hacker. You can only turn the ciphertext into plaintext if you hold the encryption key. Your IT department may have already suggested this, but a simple programme download, such as BitLocker Drive Encryption, provides an additional layer of security.
Also consider encrypting sensitive individual documents as well as your email. There are many on the market and you may have already been using this, but if not, again, it is worth considering.
Also ensure mobile phones encrypt data while at rest. This will protect data on the device, but if you are using practice mobile phones at home, this will add to security.
Most modern devices have encryption built in, but encryption may still need to be turned on and configured. There is a lot of mobile device management software on the market that will set up devices with a standard configuration.

4 Keeping sensitive information safe/ Cloud storage
You may still be handling letters or other hard copies, such as information you printed out or took home to use while working from home. You should store documents in a place where there is a low possibility of other people accessing them. For example, a locked drawer or safe.
Make sure that important files are backed up in case something happens to your device. If your practice already provides access to Cloud storage, this is perfect; otherwise you should consider it. It is easy to implement.
You should never back up your organisation’s data to your personal storage spaces. This could easily happen without you realising though, so it is a topic for you to discuss with your IT department.
Everyone is familiar with the need to ensure passwords are ‘strong’ and not linked to personal data. Hackers have dictionaries and use sophisticated methods of detection that can be surprisingly successful.
It is recommended that passwords are changed every 90 days or even earlier and companies need to put into place facilities whereby homeworkers that do not comply cannot access sensitive data.
6
Protect your wi-fi
The router is perhaps the most important gadget in your home. It checks all incoming and outgoing traffic, acting as a sentry to make sure that nothing dangerous comes in and nothing sensitive goes out.
It controls access to your home wi-fi network and, through that, all your phones, tablets, laptops, and more. If someone else gains access to that network – whether a remote hacker or your next-door neighbour – it can be quick work to compromise those devices.
Enable password protection on your home wi-fi, if it is not set up already. Your IT department should be able to advise you on when and how to use VPNs to connect to secure workspaces.
7 Avoid oversharing your screen
During online meetings and calls, be extra cautious when sharing your screen with others. If possible, do not leave any windows open that you do not want to share, as these may have details that are sensitive to you or another person whose data you have access to.
Accidents do happen and sometimes you might share something that you did not mean to. While it can be awkward, it is also a privacy issue. You might be oversharing content that is not meant to be viewed by others.
The router is perhaps the most important gadget in your home. It checks all incoming and outgoing traffic, acting as a sentry to make sure that nothing dangerous comes in and nothing sensitive goes out
8
Avoid social media when working
Limit your private social media to personal devices and do not share any personal information on messages or emails.
It could open you up to become a victim of ‘phishing’. Just check with the person who asks for information before sending important personal information. Although this seems obvious, it is easy to get tricked. Also, never open an attachment that comes from an email you do not know.
It is also a risk to share pictures of your remote working station in social media. You might accidentally share important information while you do it. The same goes with using your webcam. With webcams, you might also accidentally share too much about your home or your family members. Lastly, as no one knows how long the pandemic is going to last, it is a good idea to create a comfortable working environment for yourself. Getting every inch of your body aching with unergonomic working methods will do no good for you or your private practice business.
Murray Hart (right) is senior IT director at transcription company OutSec Services Ltd


Dr Gabrielle
Pendlebury follows last month’s advice on how to prepare for an inquest by looking at the different ways you could be involved in an inquest hearing and what to expect on the day
Pre-Inquest Review Hearings: How they differ to an inquest In complex cases, the Coroner may hold a Pre-Inquest Review Hearing (PIRH) with interested persons to decide on the scope of the investigation, identify witnesses and to plan the inquest date and duration.
Pre-inquest review hearings were formally legislated for in the Coroners and Justice Act 2009 (Rule 6) and came into force in 2013.
The purpose is to assist in the management of the inquest itself; this is particularly useful in com-
plex cases. The Coroner would normally alert you to a PIRH. This can sometimes be at very short notice, so it is good to alert your defence body as early as possible if you have been notified of an inquest, as they can then liaise directly with the Coroner and try to reduce the risk of a ‘surprise’ PIRH at short notice.
At the PIRH, the Coroner will want to determine:
Identity of interested persons;
Scope of the inquest;
Issues to consider;
Length of hearing and set hearing dates;
Whether the Right to Life, Article 2 of the European Convention of Human Rights (ECHR) is engaged;
Whether a jury is required;
Witnesses (Rule 23 or live);
Disclosure.
Failure by the Coroner to hold a PIRH can lead to the ordering of a fresh inquest. The Coroner will provide an agenda in advance and this can be requested if not offered.
Rule 23 (R23)
Something that is determined before the inquest or at the PIRH is whether the witnesses will give
their evidence live or whether their statements will be merely read, pursuant to Rule 23.
This is something that is worth trying to lock down in advance, and your medical defence organisation (MDO) can address this with the Coroner. If you are being called to give live evidence, but your MDO feels that the statement could be read, an application in writing can be made to have the statement read under R23.
Attending an inquest as a witness
You can be called to attend an inquest hearing as a witness in two ways:
1
As a ‘Witness of Fact’: If you are called as a witness of fact, it would usually indicate that the Coroner believes your involvement in the case to be peripheral. Your statement will form the basis of your oral evidence and you may be asked questions in order to clarify certain aspects.
2
As an ‘Interested Person’ (IP): If you are called as an IP, it would indicate that the Coroner believes you to be more centrally involved in the circumstances leading to death.
If you are granted IP status, you are entitled to have legal representation, receive disclosure of the documents that the Coroner intends to rely upon at the inquest and ask questions of other witnesses.
For these reasons, and because there is a higher risk of criticism, it is important to know whether you have been granted IP status at the inquest. There are a number of statutory grounds under which a person can be given IP status. They are set out at section 47(2) a-m of the Coroners and Justice Act 2009. Doctors and medical professionals are usually recognised under section 47(2)(f): ‘A person who may by any act or omission have caused or contributed to the death of the deceased, or whose employee or agent may have done so.’
Also, the Coroner has a ‘catch all’ discretion under section 47(2) (m) to grant IP status to anyone who is deemed to have ‘sufficient interest’.
Witness evidence is given under oath, which means that you are under a legal obligation to tell the truth at an inquest.
On occasion, a doctor may be criticised in the Coroner’s report or during an inquest. If this occurs, they are required to inform the GMC without delay
In most courts, the Coroner sits at the head of the chamber, with the witness box to one side. The advocates’ bench is in front of the Coroner, and behind that is general seating.
Inquests are held in an open (public) forum and some will generate media attention, so reporters may be present. Additionally, all inquests are now audio-recorded.
When the Coroner has heard all the evidence, they will sum up and deliver their conclusion.
This can be in ‘short form’ or a narrative verdict. It is important for you to obtain the outcome of the inquest and, if you are legally represented, the lawyer will make sure that this is received.
However, in some instances, a doctor can give evidence without receiving the final outcome, thus never knowing about potential criticism or if a ‘Regulation 28’ report (see below) will be issued. If you are without legal representation, it is important to find out the outcome by contacting the Coroner directly.
Following the inquest, the Coroner has a duty to make recommendations in cases where the evidence suggests that further avoidable deaths could occur and that, in the Coroner’s opinion, preventative action should be taken.
The Coroner will prepare a report, which will be sent to the person or authority that may have the power to take the appropriate steps to reduce the risk. They have a duty to provide a response within 56 days of the date the report is sent.
If a doctor is concerned that
they may be – or have been – criticised in the context of a Coroner’s inquest, including in a Regulation 28 Report, then they should contact their MDO at the earliest opportunity to seek advice about the appropriate steps to take.
The Regulation 28 report may also be made available to the media, and your MDO can assist with preparing for any media reports and monitoring for coverage.
by the Coroner
On occasion, a doctor may be criticised in the Coroner’s report or during an inquest. If this occurs, they are required to inform the GMC without delay.
This may result in an investigation by the GMC. This is a rare occurrence, but if it does happen, your MDO can guide you through the process and direct targeted continuing professional development around the issues raised to demonstrate evidence of remediation to the GMC.
Where to turn for help and support during an inquest
Any involvement in an inquest can be incredibly stressful, prompting mixed feelings and potentially concerns about your own professional welfare.
These feelings can be managed with careful preparation and support. Seek support from colleagues who have experienced inquests in the past, as they will be in a good position to empathise with any concerns you may have but also give relevant information, regarding the process.
If you experience feelings of being overwhelmed, such as anxiety, alert your GP and do not be afraid of seeking psychological support, which may aid your ability to negotiate the inquest without too many sleepless nights.
Finally, remember to seek support from your defence organisation. Make contact as soon as you are aware of an inquest.
Dr Gabrielle Pendlebury (right) is a medico-legal consultant at Medical Protection

Be prepared – reading statements that you have submitted and any other relevant documents will refresh your memory of events. You may take case documents into the courtroom and refer to these while in the witness box. Consider marking or highlighting important sections in advance for ease of reference on the day.
Dress smartly. This is a formal occasion and a suit or other business attire is considered appropriate.
Arrive on time. Register your arrival with the Coroner’s officer or clerk. You will be shown into the courtroom and be seated ready to be called to take the witness box.
Switch your mobile phone off.
Be polite and remember it is fine to give your condolence to the family if you see them at court.
When called, you will be asked to ‘swear in’ by reading an oath on a holy book, or a non-denominational statement of truth. After this point, any failure to tell the truth would amount to perjury.
Each witness will be questioned by the Coroner and then by interested persons, including the family.
Direct your answers to the Coroner, whom you should address as ‘Sir’ or ‘Madam’.
Answer the question you have been asked, not the one you wanted to be asked. If you are unsure of the question, seek clarification.
Keep your answers brief and factual.
Use non-technical language whenever possible. Ideally you should answer in lay terms.
Keep calm. The tendency is to speed up when nervous, but make sure you speak clearly and slowly.
Remember that media may be in attendance, dependent on the level of press interest in the case. Statements made during an inquest may be covered by media outlets if the case is open for press to attend. If asked for additional statements by media before, during or after the inquest, contact your MDO before making any comment to get media advice and support.
Discussing the facts of the case outside the courtroom, as this could be seen as interfering with the inquest process.
The temptation to fill gaps in proceedings by speaking. The Coroner may be making notes from the evidence or preparing their next question.
Straying into the remit of an expert, unless you are qualified to give such an opinion. Remember that a witness of fact should confine evidence to facts within their direct experience.
Leaving court before the Coroner releases you.

Identify how to maintain or increase practice turnover after the pandemic and in keeping with the new norm, says Stephanie Carmichael (right)
RECEPTION/WAITING ROOMS
Strategy – Reduce the number of patients allowed in the waiting room at one time as well as reducing contact between these people: Limit the number of seats in the waiting area and organise the seats to ensure they are two metres apart. Although this may appear challenging, there are a variety of ways around this.
Most private practice waiting rooms have always had a lot of room. As much as it was kudos, it also provided the patient with reassurance that paying privately also provided a better service.
So patients grew to expect complimentary coffee machines, tea or snacks, often with a large table comprising magazines and books and large comfy chairs.
However, by simply removing the coffee machines and large table and organising the chairs in rows obeying social distancing, it will be easy to comply with the new Government legislation.
This does not mean that the patient misses their cup of coffee, as it can be organised that the coffee machine is placed at the reception area and the receptionist offers it to the patient as they signin – to avoid fingering the machine. But magazines, books and toys should be removed totally, as wiping down between patients would be impractical.
A fish tank on the wall could be considered, as an aquarium is therapeutic. Place a tray by the door to enable patients to leave their cups and saucers for collection.
Limit the appointment to the patient alone and only allow them to be accompanied if necessary and by prior arrangement.

Keynote: This is the easy part. Far more difficult is the re-organisation of the back offices.
Strategy – Communication with the patient in advance of their visit will ensure the appointment runs smoothly and without event: Ensure visitors before their visit are emailed the policies that have been put in place for their safety prior to the appointment.
Post signage at the entrance to your practice so everyone coming in understands the changes and understands their personal responsibilities.
Clearly mark where the toilets are to avoid patients wandering down passages and/or knocking on other doors.
Link up a TV screen that displays non-audio but visual messages of how patients should behave in the waiting/reception area. Additionally, use this screen to announce who the next patient is, what room they should go to, if a multiple practice, and any other useful information.
Keynote: Clear communication from the onset, both on the website and email content, will result in less verbal explanation by your reception staff. This will, in turn, improve the patient experience.
Strategy – By encouraging telemedicine appointments, the number of waiting room patients should diminish naturally.
Telemedicine is easily achievable with today’s technology, although we know virtual consultations for

insured patients especially have caused controversy (see page 12).
Even elderly patients normally have children who understand how this works and, in the main over time, fewer people will find this a hindrance and more will embrace it as the new norm.
The most important thing here is to choose the best video conferencing software that meets your needs.
Before choosing software, ask yourself what you will need this software to accomplish. It may be that you will just have a face-toface appointment in the first instance.
But you may wish, further down the line, to share your screen to show your patient an X-ray or MRI scan. Thought needs to go into this aspect as, realistically, this decision will be key to how versatile you can be in providing virtual appointments and follow-ups.
In effect, this method could increase patient visits. Patients who come a long distance may well be more encouraged to ask for an appointment more often when they do not need to organise their lives to take possibly a whole-day return trip to visit you in person.
Keynote: When booking a virtual appointment or visit, patients will assume that this meeting will take less time compared to attend-
ing in person. You want to make sure that by using technology you are speeding up the process and not slowing it down, so you need to work smarter not harder. No need to offer your patient a glass of water; a lot of time can indeed be saved by getting straight to the point with no discussion about how long it took to get there.
With fewer staff available at reception, it may be appropriate to reevaluate the practice receptionist’s duties.
Pre Covid-19, two to three receptionists were normally on hand in an average private practice waiting room. They received the patient, pressed the automatic entry bell, registered the patient, answered the phone, ensured tea/coffee, magazines were on hand for the patient’s comfort, answered questions as to where the bathroom was and directed them verbally towards the appropriate clinician’s rooms as and when they were called.
In between these duties, they will have been diarising appointments, phoning patients to re-arrange appointments, if appropriate and typing up urgent referral notes as well as organising their own breaks.
Looking after the tea and coffee facilities, the non-functioning of the TV screen and wiping down surfaces every hour will also be part of their new responsibilities.
For one person to do all of this is impossible. A shift will need to be put in place with back-up for illness and holiday as appropriate. Keynote: Staff will need to be rotated more frequently and it will be pertinent for the receptionist duties to be minimised to enable her/him to focus on patient needs in the waiting room alone.
However, the receptionist is a vital component of a successful practice. Their communication skills and time spent attending to patient needs is invaluable in making the patient experience as positive as possible.
This will be one of the most challenging aspects of the new norm. Due to social distancing, back-
office practice staff will need to alter how they work. Physical limitations may mean job shares or redundancies. Even with technology, doctors’ assistants are vital, so support staff may be an area to reconsider.
Consider what areas of support work could be appropriate for outsourcing. As an example, internal staff who spend 30% of their time typing amount to an expensive form of typing. Instead, have them work on your social media profile. Blogs are highly effective marketing tools and will give an added element to your practice.
Consider using internal staff more effectively by retraining them. Flexi-working could be considered.
Keynote: Prior to Covid-19, receptionists answered calls often in the middle of registering a new patient. If rushed, the attention needed to turn the call into a prospective patient often got side-
lined. Stats have shown that 66% of phone calls got unanswered. Retrain staff on the importance of the phone call, provide them with sales training and give them the time to devote to the call – and practices will see an increase in business.
Use your internal staff as effectively as possible and use outsourcing to complement your staff. The combination is both more efficient and cost-effective.
COULD TASKS BE AUTOMATED OR OUTSOURCED?
Strategy – Improving processes for tasks that take too much of your time or your administrative staff.
It is only through innovation and adapting to this changing world that a private practice will survive. A good management system can save time and therefore money, so:
Take a thorough look at the technology and systems that you
are using. Evaluate what works for you and what could work better in the new norm.
Consider what elements of the practice could be outsourced. You probably already outsource your IT and website requirements, but what about billing, typing and human resources?
Keynote: Technology, while getting more sophisticated, is providing better value for less cost. Any practice that bought into a system when it first came out will have paid a premium – just like a shiny new car.
If your system is five years old or more, new brands will have come out offering improved systems at a lower price. While it is a big exercise to spend time evaluating, this may be the most worthwhile time spent in reducing costs.
Stephanie Carmichael is senior manager, medical division, OutSec Services Ltd
Unprecedented times call for unprecedented action. It’s time to get private practice back on its feet and, as independent practitioners re-open their businesses, we know they need all the help and support they can get.
In normal times, many consultants and GPs would be relaxing on holiday – and so would we. But not this year. With so much happening and new developments affecting the private healthcare sector daily, we will bring you an August issue for the first time; otherwise, there will be too big a gap until September and you could miss some crucial developments. It will be packed with more informative articles and the news we think you and your business needs to know.

In the meantime, keep in touch with the latest news which thousands of independent practitioners are now accessing – as well as our monthly digital isssue – on our website:
As growing numbers of private doctors move closer to resuming private practice, Prof David Gartry shares his story of The Wimpole Eye Clinic and its phased re-opening

AFTER APPOINTMENT as consultant surgeon to Moorfields Eye Hospital some 25 years ago, and having built up a private practice both there and at The London Clinic, it was my long-term ambition to enjoy the independence –not to mention the legacy and the hoped for investment value – of owning my own clinic.
The plan had been to invite my closest subspecialist colleagues to work with me; colleagues to whom I have referred numerous patients
over the years and to whom I would happily send all my friends and family, not just my mother-in-law.
I had been looking for premises around Harley Street over the years when one happy patient asked if I had ever thought of owning my own clinic? Had I!
Unworkable constraints
I explained that, notwithstanding the expense, it seemed all the decent properties were taken –mostly by Howard de Walden.
Those still on the market, often after months or years, either needed major re-constructive surgery or had unworkable legal constraints.
My patient had been ‘in property’ all her career and reassured me she was confident of finding something suitable. I reassured her I would not hold my breath.
Then, a few months later, she called with the news that a doctor who owned a clinic at 46 Wimpole Street with the freehold was thinking of selling.
The main aim is to avoid patients sitting with others in the waiting room – even if there is adequate distancing
Prof David Gartry (centre) opened The Wimpole Eye Clinic in London on 29 October 2015 – and closed it again on 23 March this year, the day of the lockdown
It was perfect for developing into an eye clinic with plenty of space and a layout that permitted good patient flow – which was to come in particularly useful as lockdown began to be relaxed.
So after a six-month period of refurbishment, I opened The Wimpole Eye Clinic on 29 October 2015 – and closed it again on 23 March this year, the day of the lockdown.
And to think that I had assumed that 2020, regarded as a decent
standard on the eye chart, was certain to be a good year for ophthalmologists.
And so to lockdown. My colleagues and I had much NHS admin to do at Moorfields in firstly cancelling patients who could be safely removed from clinic and theatre lists and then stratifying them for re-booking at a later date according to their level of risk.
A small help
We all took part in an ‘emergency or semi-emergency’ rota, which made us feel that at least we were helping in some small way – that is to say, less guilty – while others were at risk on the front line.
I convinced myself that, as it had
been 35 years since I was a casualty officer at University College Hospital, I would most certainly have been more of a hindrance than a help to those who actually knew what they were doing.
As I readily admit to friends and family: ‘I used to be a real doctor!’ I therefore kept my head below the Moorfields parapet and stuck to the rota.
But it must be said that, at best, our work at Moorfields Eye Hospital has been part-time due to the lockdown – I have done only one emergency corneal transplant, for trauma, in almost three months.
We are all aware, of course, that it will be ‘payback time’ soon.
On the private side, and as the lockdown has eased, a number of clinics have opened in a limited way, respecting the Government guidelines on distancing and precautions regarding personal protective equipment (PPE) and seeing strictly limited numbers of patients as clinical need versus risk, specialty and premises allowed.
I asked the adviser who had helped with my original Care Quality Commission application to provide an on-site risk assessment.
This was an essential step, which I would strongly recommend to those who are planning to open up their practices.
Although we had been observing strict guidelines at Moorfields, and I was familiar with the numerous precautions, there were other very constructive suggestions made at the inspection specific to my clinic.
The adviser also provided a comprehensive 30-page Covid-19 protocol. The key points are set out in the box below.
Prof David Gartry is founder of the Wimpole Eye Clinic, senior consultant surgeon to Moorfields Eye Hospital, London – specialising in corneal, cataract and laser refractive surgery – and visiting professor to The School of Health Sciences, City, University of London
1 Patient criteria/selection. Those over 70, especially those with significant co-morbidity, should not attend unless essential; for example, in our case, those with potentially sight-threatening conditions or those patients requiring careful monitoring, important post-operative reviews and those on steroid medication or immunosuppression. This is certainly not an exhaustive list, of course, and is dependent on specialty and circumstances. Routine new and follow-up appointments should be delayed until there is a further relaxation of the lockdown.
2
At the time of arranging the appointment, a standard Covid-19 patient questionnaire should be sent to the patient by email along with any registration documents. Ideally, these should be completed and returned in advance to minimise paperwork in the clinic. Inevitably some patients will forget to do this and are asked to complete the forms on arrival.
3
Patients should be asked to arrive on time, not before. If arriving early then they should wait outside – for example, in their car, if possible.
4 Patients should, ideally, attend the clinic on their own. Some may require help from a partner or perhaps an interpreter, but the number of persons inside the clinic should always be kept to a minimum. If they were driven to the clinic, then their driver/ partner should wait in the car.
5 On arrival, the patient’s temperature should be checked. We use a digital noncontact thermometer.
6 Ideally, if the appointments are correctly scheduled, the doctor/ assistant should be ready to take the patient directly into their consulting room. The main aim is to avoid patients sitting with others in the waiting room – even if there is adequate distancing.
We have made 10am the first appointment of the day – instead of 8.30am – to help patients and staff avoid the rush hour. My first clinic as lockdown was eased (4 June) comprised only six patients booked between 10am and 2pm. I normally work with three optometrists, but until the situation eases further, only one.
7
Wall-mounted sanitising gel dispensers should be available throughout the clinic – including one just inside the main entrance and another close to the reception desk, which should have a solid transparent plastic screen to separate the receptionist from the patient.
Clinical-grade soap dispensers and automatic air hand-dryers help to maintain good hygiene, if not sterility.
8
The waiting room should be arranged so that no patient is within two metres of another. The social distancing floor stickers should be strategically positioned throughout the clinic and in the consulting rooms and the few seats available should be wipeable –that is to say, not cloth upholstery.
9 No fans are allowed, as these simply recirculate air, and air-conditioning units should be of the type that bring fresh air into the building – ‘fresh air’ being a relative term in central London, of course.
10 If possible, restrict tests and examinations to those that will make a difference to the patient’s management.
11 PPE – the advice that we were given was as follows: All patients should wear masks inside the clinic. Staff are advised to wear hats, standard surgical masks (unless there is aerosol generation), scrubs, single-use plastic aprons, single-use nitrile gloves and protective wrap-around goggles or similar.
In ophthalmic practices, we can also fit large solid transparent plastic screens to the slit-lamps and similar items of equipment to act as an additional barrier.
All staff should ensure they follow the usual ‘bare below the elbow’ policy and carefully wash hands before and after each patient contact.
12
All equipment should be wiped down between patients with 70% alcohol wipes as well as the arms of chairs, door handles, bannisters and any item the patient is likely to have touched. The PPE is disposed of in clinical waste bags and the scrubs are bagged and laundered in the usual way.
Extra out-of-hours cleaning rotas should be put in place to cover all clinic days and a careful log maintained.
13 Ideally, patients should make payment by phone, but where a credit card payment is made, either the secretary or the patient can enter the details and the PDQ terminal wiped down with Azowipes or similar.
Implementing these ten simple billing rules will mean your practice is best positioned to recover from the impact of the Coronavirus. Simon Brignall (right) has suggestions for independent practitioners to put in place

TO SAY that Covid-19 has had a detrimental impact to the independent healthcare sector is an understatement. Private consultants, GPs and clinics have seen a loss in income that varies depending on their specialty and patients treated.
To ensure this impact is minimised over the medium to long term, it is important that practices are best positioned to take advantage of any recovery. Here are ten simple rules to put in place to achieve this goal:
1
Make sure you spend as much time as possible focusing on your core skill set: treating and looking after patients
It seems obvious, but it is important to prioritise seeing and treating as many patients as possible, as the shutdown means there will be a pent-up demand for your services.
If you and your secretary can focus on the medical side of the practice, this will increase the revenues for the practice, because you are focused on what you do best rather than spending time on tasks that can be delegated.
Running a private practice is not easy and many tasks do not fall naturally into a consultant’s skill set. Take stock and consider what elements of your practice could be outsourced – enabling you to generate that all-important cash flow.
2
Make sure your work is invoiced as soon as possible
As things open up, most consultants will naturally try to see as many patients as they can to make up for lost income and deliver urgent care to patients who need their services.
It is important that this work is invoiced as soon as possible to derive the benefit of this activity and to make sure you are not just storing up problems for the future. Remember, some major insurers now enforce time limits for submitting invoices and if you miss the deadline, they will not pay. Late invoices indicate poor service to patients and are a major contributor to their dissatisfaction and lead to bad debts.
Delaying the patient’s aware -
ness of a shortfall means that the patient assumes the invoice has been settled, which can lead to disputes over the bill.
Late invoices sent direct to patients can be ignored if they think you are not serious about wanting payment.
3 Take this opportunity to review your fees
It is important to regularly review your fee structure and thus, if it has been a while since you have done so, use this time to review your rates for consultations and procedures.
I still come across practices that have not reviewed their prices for years and sometime decades.
If you bill your procedures to insurance guidelines, make sure your price list is still current, because these constantly change and are not often communicated clearly. You could be charging less than you could or more than you should. Practices still make wrong assumptions, leading to issues with insurance companies, delays in payments and losses in revenue.
4 Review the way your work is being billed to ensure you are compliant with the regulations communicated monthly from the Clinical Coding and Schedule Development Group (CCSD)
If you are taking the time to review your fees, this would also be a good time check that you are abreast of the CCSD’s monthly changes and establish if/how they affect your specialty and possibly your income.
Practices commonly make billing errors through being unaware of the changes and so it is important to establish what rules each insurer adopts, as each insurance company can choose their own variants.
5 Make sure that your price policy is clear and that your patients are notified of it before commencing treatment This should be second nature, as a clearly defined, well documented, and communicated price structure and a patient registration form is vital in a modern practice. It will ensure no room for ambi-
guity by laying out responsibilities for payment of your medical invoice, leading to fewer delays in getting your money.
Remember, fee and payment terms transparency is a key requirement of the Competition and Markets Authority.
6
Ensure that your practice has a robust chasing process in place for outstanding invoices
The current crisis has highlighted the need to have strong procedures in place to resolve aged debt.
These procedures need to be applied on a consistent and continual basis to result in benefits to the practice. This will ensure these invoices are fully paid and improve your cash flow.
The vast majority of calls we have received during the crisis have been from practices with issues in this vital area, meaning they continued to run high levels of bad debt. Almost every practice that joins Medical Billing and Collec tion (MBC) has an outstanding backlog of invoicing going back years.
Debt levels can typically be over 20% of turnover and sometimes have reached 50% of annual turnover and I have seen this increase over recent months. On average, we achieve bad debts of less than 0.5%. This is a huge difference.
7
Make sure you are aware of any bad payers so you can better police them more effectively Visibility around problem payers means you can request the patient settles any outstanding invoices before you allow them to make their next appointment.
If you do not do this, you will end up regularly throwing money away by adding to the problem.
When we take on a practice’s backlog of outstanding invoices, there are often patients who have built up debt over years, yet the practice has continued to see them despite never being paid.
8 Ensure you have key management information on your practice to allow for informed decision-making
It is quite common for me to speak to a consultant who has no or minimum access to up-to-date
accurate data on their practice. All practices should know where patients are coming from and how their patients break down in terms of volume of insured, self-pay, medico-legal and international patients.
It is also good to have information about patient activity. Consultants should have access to reports that show their monthly revenue, payments received and the breakdown of any outstanding invoices.
Without this information, it is difficult to understand which direction your practice is going and it is quite easy to come to the wrong conclusions. This is more important than ever as practices recover from the current crisis.
At MBC, we provide all the above data online 24/7 to assist you in the running of your practice.
9
Put in place a robust secure IT infrastructure to deal with the practice’s administration
This often is a common weakness in many practices and is generally only highlighted when it is too late.
Enjoy the peace of mind that your business is on a secure platform that meets General Data Protection Regulations and that your data is secure. A wide range of options can facilitate this, so it should not be difficult to implement.
10 Consider whether now is the time to join thousands of other doctors who have outsourced this crucial element to a professional billing company
Most consultants find the billing and collection side of the practice a challenge to manage and that weakness can result in unnecessary and often consistent financial losses.
Outsourcing could be the best decision you make this year to guarantee your practice is ready to face what lies ahead with a cost structure correlated to received income.
See ‘Make the leap away from Covid captivity’, page 46
Simon Brignall is director of business development at Medical Billing and Collection

Surgeon Mr David Sellu, convicted for gross negligence manslaughter of a patient at a private hospital – later overturned – continues describing how he was treated as a ‘very non-private’ patient while he was a prison inmate

Adapted from Did He Save Lives? A Surgeon’s Story, £9.99, Sweetcroft Publishing ISBN 9781912892327 from Amazon. His story continues in Independent Pract itioner Today next month

THE YOUNG man behind the reception window in the hospital looked up from the computer.
‘We are from HMP Highpoint South,’ the male officer said, as he handed over a letter in a brown envelope. ‘You are expecting this prisoner.’
We were told the triage nurses would see me soon. The male officer went to make a phone call and this was the first time I had been left alone with the female.
After a long period of silence, I turned to her and asked: ‘Do you like your job?’ She looked at me, looked towards the reception desk and replied: ‘Would you like doing a job like this?’
This was not what I expected, but I was determined to find out more.
‘Why do you say that?’
‘It is a lousy job. Would you enjoy being verbally and sometimes physically abused almost every day? She pondered for a moment and continued: ‘This prison is so overcrowded and we are so short-staffed it is a surprise no one has been killed.’
‘Why do you do it? It was your choice.’
‘I need the money,’ she said. ‘It pays the bills.’
Twenty minutes later the male officer returned and announced: ‘We are going to be here till late tonight. Three-hour wait.’
‘Mr Salou,’ called a tall nurse after 40 minutes as she looked around the main waiting groom.
I tried to lift my right index finger in the air but, with the handcuffs still in place, I resorted to a nod and a ‘Yes.’
We followed the nurse to a room off the larger waiting room full of pieces of medical equipment and boxes of medical stock and I wondered whether it also doubled as a
store. I sat on the chair the nurse showed me, but the officer I was handcuffed to was left standing. The furniture was rearranged to enable the nurse and the female officer also to sit down.
‘Am I not entitled to have this consultation in private?’ I inquired, looking first at the nurse and then at each of the officers in turn. The nurse looked at the officers and the best response was a shrug from the male officer. No one moved. After a brief pause the nurse asked me to recount my history.
‘I will need to see your legs, so I can see the difference between the two sides,’ the nurse suggested. The prison jeans I was wearing were too tight around the legs for me to roll them up, so the only choice was to take them down.
The presence of the two officers and the fact that I was handcuffed to one of them made this an awkward instruction to follow. I stood up, managed to undo my belt and the zipper on my jeans and to pull them down, all with my left hand.
‘Yes, I can see both legs are swollen, the left more so than the right,’ the nurse observed.
‘Pitting oedema, no previous history of DVT, no pain but a little tender below the popliteal fossa,’ I offered. ‘I am on Amlodipine 10mg and Bisoprolol 5mg each daily for hypertension and Simvastatin 20mg at night to lower my cholesterol.’
I had checked the doses prior to leaving the prison, knowing I would be asked this information. The nurse looked at the referral from the prison GP I had barely seen, presumably to determine whether I had a medical background.
She went on to measure my
The presence of the two officers and the fact that I was handcuffed to one of them made this an awkward instruction to follow blood pressure. It was high, at 170/ 98 . I had not taken Amlodipine for four days, as it is known to cause swelling of the ankles, but this had made no difference. Moreover, I was stressed by everything that had happened so far and by the possibility I had a DVT. Pulse 62 per minute. This should have been higher, given how I felt, but Bisoprolol works by lowering heart rate. Oxygen saturation 98 % – normal.
The nurse made no comment. ‘I shall arrange for you to have blood tests and the doctor will see you when the results are available.’
I put my trousers back on and was ushered back to the waiting area. Everyone stopped what they were doing to take a look at me.
‘David Sellu,’ called out the nurse. We followed her into a room where I was instructed to lie on a couch. ‘I am going to take some blood.’
‘What tests am I having?’ I asked.
‘The doctor will discuss that with you later. Three tubes.’
I was not going to refuse the tests, but it would have been very nice to know what they were for. It is not easy taking blood from me – dark skin, not very prominent veins around the front of the elbow.
After prodding there for a while, her eyes lit up as she noticed some prominent blood vessels on the outer side of my wrist area with my palm facing upwards. She patted the area a few times but I interrupted and said:
‘That is my radial artery. In some people like me, it does not run its normal course and it is displaced
outwards. Aberrant radial artery, have a feel.’
‘Oh yes, you are right. That’s a bit dangerous where it is. Could easily be injured.’
‘I have managed so far to avoid any mishaps,’ I assured her.
‘I will get a doctor to do your bloods. Too difficult for me.’
Twenty minutes later a doctor arrived and managed to locate a vein deep in front of my left elbow and she was getting ready to take the samples.
‘What blood tests am I having?’ I asked.
‘Full blood count, urea and electrolytes, liver function tests, D-dimer.’
She spoke slowly, looking all the time at the request form. I was not sure the lack of explanation as to what these tests meant was because she had discovered I was a doctor.
If not, I wonder what other prisoners would have made of this
under similar circumstances. She was efficient at taking blood. First stab and three vacuum bottles were filled and within a minute or two the process was complete.
Back again in the large waiting room and this time a group of young children turned their attention to me. I felt uncomfortable and humiliated.
The male officer asked: ‘Do you have a technical background?’
‘I was a consultant surgeon.’
His ignorance explained a lot about the officers’ attitude to me. All prisoners were criminals.
‘There is a campaign to have my case reviewed. It’s on the internet.’
‘Oh, I see.’
Then more silence. My wife and children did not know I was in this department being investigated for a potentially serious condition. It would have been comforting to have my family with me, but instead I was handcuffed to a prison officer, sat in silence, far from home.


WHEN ONE looks into the future, it soon becomes apparent that a crystal ball would be useful. Unfortunately, they are in short supply.
At times of economic uncertainty such as this, it can be tempting to run ‘what if’ scenarios in our heads, such as ‘perhaps I should move into tech stocks and pharmaceutical companies, as surely these sectors will do well’ or to pick out specific companies that appear likely to thrive in the future.
Two challenges exist. The first is that you will not be the first person to have thought this and these views in aggregate are already reflected in market prices.
The second is that, in making such concentrated bets, you have a high chance of being wrong and missing out on the companies that end up driving future returns. Remember, 30 years ago Amazon did not exist.
To get a feel for what these concentration risks look like, academics are fortunate to be able to dig

around in a vast bank of historic stock market data in the US, known as the CRSP database (the Center for Research in Security Prices).
One such study reveals some surprising and useful findings using data from 1926 to 2015. While investment wisdom and empirical evidence support the notion that stocks – in aggregate – outperform

cash over longer periods of time, a forensic look at individual stock returns tells a vastly different story.
Here are some of the insights that the paper provides:
➲ The median time that a stock is listed on the CRSP database is only seven years, during the period 1926 to 2015. That is not long.
➲
Just over 40% of all stocks have a holding period return – simply, the return of an asset or portfolio over the whole period during which it was held – that exceeds the return of cash over the period that the stock was in the database.
More than half deliver returns that are negative. The average life-
time return on any single stock was -3.7% a year. That is not good.
➲ 26,000 stocks have appeared in the CRSP database since 1926, yet only 36 stocks survived the entire 90-year period. That is not many. ➲
US $32 trillion of wealth has been created since 1926 (to 2015), which has been generated entirely by the top 1,000 companies, representing less than 4% of the total number of companies listed over time. The top 30 firms – 0.1% of all stocks – accounted for around 30% of the total stock market’s wealth creation. That is rather concentrated.
As the author of this particular study states: ‘Non-diversified portfolios are subject to the risk that they will fail to include the relatively few stocks that generate large cumulative returns.
‘Indeed, the results help to understand why active [investment] strategies, which tend to be
Non-diversified portfolios are subject to the risk that they will fail to include the relatively few stocks that generate large cumulative returns
poorly diversified, most often lead to underperformance.’
At times like this – and, in fact, across all time periods – it makes enormous sense to remain highly diversified, at the risk of missing out on the next Exxon – the firm that has added most value to the US market ever – Apple or Amazon. Simply looking at the changing guard of the top ten US firms by revenues in 2000, 2010 and 2020 is revealing.
Correctly picking which few companies are going to be driving stock market returns over the next decade or two will not be easy nor likely.
Making sure that you own them can be achieved by owning a broadly diversified portfolio with many hundreds, if not thousands of companies in them.
Missing out on these companies – and perhaps other companies which do not even exist yet – could make all the difference between a
In making concentrated bets, you have a high chance of being wrong and missing out on the companies that end up driving future returns
good outcome and an extremely poor one. As Tennyson said, the old order changeth!
Dr Benjamin Holdsworth (right) is director of Cavendish Medical, specialist financial planners helping consultants in private practice and the NHS

The content of this article is for information only and must not be considered as financial advice. Cavendish Medical always recommends that you seek independent financial advice before making any financial decisions.
Levels, bases of and reliefs from taxation may be subject to change and their value depends on the individual circumstances of the investor. The value of investments and the income from them can fluctuate and investors may get back less than the amount invested.
Independent Practitioner Today has joined forces with leading healthcare lawyers Hempsons to offer readers a free legal advice service.
We aim to help you navigate the ever more complex legal and regulatory issues involved in running and developing your private practice – and your lives.
Hempsons’ specialist lawyers have a long track-record of advising doctors – and an unrivalled understanding of the healthcare system as a whole.
Call Hempsons on 020 7839 0278 between 9am and 5pm Monday to Friday for your ten minutes’ of free legal advice.

Advice is available on: Business structures (including partnerships)
Commercial contracts Disputes and litigation
HR/employment Premises
Regulatory requirements and investigations


The Care Quality Commission regulates you – but who regulates the regulator? Lawyer Philippa Doyle (right) says if you get a bad report – and they are still coming through during the lockdown –then make sure you challenge it

IT WAS disappointing to read in the press that the Care Quality Commission (CQC) has found that dozens of its reports are flawed.
In January 2020, it was reported that the watchdog had been compelled to retract almost 40 inspection reports into care and nursing homes after finding that there was ‘duplicate material’ in 78 reports, where identical quotes from patients, service users or families or sections of evidence had been pasted into reports into different institutions.
In 38 out of the 78 reports, the CQC had found that the homes in question would need to be reinspected for it to be ‘confident in the ratings and findings’. All the homes were in the north of England except for one in London. This is devastating news for the sector. But it does underline the importance of challenging a CQC inspection if you are a provider
from any sector and feel that the due process has not been followed. Ultimately, it is the providers who regulate the CQC. Only if providers complain, challenge or report back to the CQC can poor inspection practices be identified and addressed.
Inspection report suspended
We recently complained regarding the conduct of an inspector during and immediately following the inspection of a private hospital. The CQC immediately suspended the production of the draft inspection report pending the outcome of the investigation into the inspector’s conduct.
CQC encourages providers to speak up and will take proportionate action where justified.
We have supported several GP practices to challenge their inspection reports, including where they have been placed in special measures.
Inspectors do sometimes get it wrong. They miss things. They misinterpret information
In the current Covid-19 crisis, there will be a small number of draft reports still coming through the system from inspections carried out before the shutdown. These will still need to be challenged in the usual way if you are not content.
We supported the collection of feedback from staff and commenced the complaints process to scrutinise the sometimes overbearing approach of inspectors.
We have supported dentists and achieved a turnaround on ratings and sought to limit co-ordinated reviews of practices in the same group on the same day.
We recommend bringing a complaint to the CQC as soon as an issue arises.
If you feel that your CQC inspection has been conducted by someone who was unprofessional, was not listening to what you had to say or came with a very fixed agenda, you should raise this through the CQC complaints process straightaway. Do not wait for your inspection report, as a complaint at that point can seem a little like ‘sour grapes’.
An early complaint can result in the production of a draft report being placed on hold pending the outcome of the investigation and it is far easier to prevent the publication of a report in the first place, than it is to get one removed once it is online.
The CQC must investigate concerns when they are presented to it and must treat every concern as a legitimate verifiable concern even if providers have a suspicion that vexatious or vindictive complaints have been made. A fair and balanced process must be followed. If it is not – speak up.
Alongside this, the Factual Accuracy Challenge (FAC) process is a key and important process to utilise to its fullest. The CQC would have you believe that the process is limited to you saying ‘we have five staff members, not four’, but the FAC is the only real opportunity you have, post inspection, to address any anomalies.
While routine inspections are now not taking place, the CQC can and will still take enforcement action where serious cases of risk and safety arise and once lockdown is lifted, the inspection process will, in time, recommence.
So go to town and throw the kitchen sink at your FAC – but do it fast; you only have ten working days to respond, and rarely will you get an extension on that. Every single point you take issue with needs to be addressed. If you don’t challenge it, then it will stand as drafted.
Your main route then is a rating review. We recently launched a rating review for a private cosmetic clinician. A rating review can only be a challenge against failure to follow due process.
The review resulted in changes to the provider’s report, as the CQC had failed to follow its own internal processes in ensuring all sections of the report were peerreviewed prior to publication.
A rating review is a little like a judicial review. If a public body has failed to take relevant evidence into consideration or has taken into consideration irrelevant evidence or has failed to follow due process, then a challenge is worth taking. Particularly given the potential impact on reputation.
Inspectors do sometimes get it wrong. They miss things. They misinterpret information.
Make sure you have your say and make sure your report is the most accurate representation of your service that it can be.
Philippa Doyle is a solicitor at Hempsons
Northern Ireland’s NHS private patient services come under the spotlight in our monthly round-up of PPU progress. Philip Housden (left) reports

THE NHS in Northern Ireland is organised into six health and social care trusts (HSCs), which manage all healthcare services in a single management structure.
The most recently published annual accounts of the five HSCs that provide hospital care – the sixth HSC is the NI Ambulance Service – have been used in this article.
In 2018-19, Northern Ireland total private patient revenues totalled an estimated £5.1m, up 6% and £0.3m from £4.8m the year before. The total spend of £5.1m represents a steady 0.11% of total HSCs expenditure in NHS Northern Ireland.
Belfast HSC Trust, accounts for nearly 75% of this total, with revenues in 2018-19 of £3,768,000. This is growth of 4.1% on 2017-18.
These results suggest that the trust has weathered the loss of Bupa recognition for services in late 2017. Significant revenues are earned from self-funded fertility services provided from the Regional Fertility Centre.
Total private patient revenues are 0.24% of total expenditure, which in equivalent terms would place the HSC 68th in the list of NHS trusts in England outside London.

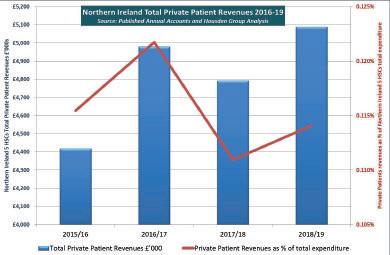
Western HSC Trust has the highest volume of private activity after Belfast. Revenues were £638,000 and 25% up in 2018-19.
Maternity rooms
Income at Altnagelvin Hospital, Londonderry, appears to be linked to amenity payments for single rooms, particularly maternity,
where the mother pays for private room but remains an NHS patient. Earnings elsewhere in the three other remaining HSC trusts amounted to £683,000 in 2018-19. Overall, there are few if any signs of HSCs supporting growth in private patient services currently. Therefore, the present overall earnings pattern can be expected
to be maintained in 2019-20 accounts.
However, moving into 2020-21, private patient income may be substantially reduced.
When the independent sector restarts services for private patients, it will be the three main private hospitals in Northern Ireland that benefit, together with some provid-
ers in the Republic - particularly in Dublin – due to the geography and improved journey times.
How does Northern Ireland compare? Exact comparisons are difficult due to the differing income and expenditure patterns of NHS bodies across the UK, as both Northern Ireland and Scotland accounts include a wider range of services than just acute hospital care.
However, as can be seen from the comparison chart below, this total for Northern Ireland of 0.11% is well below that of Wales (0.17%) but significantly higher than in Scotland (0.03%). See our May and June issues, respectively, for the details on these countries.
All are below the 0.46% average for NHS trusts in England outside of London, although Wales is comparable to the lowest regional figure in England which is the North-east at 0.18%.
Philip Housden is a director of Housden Group
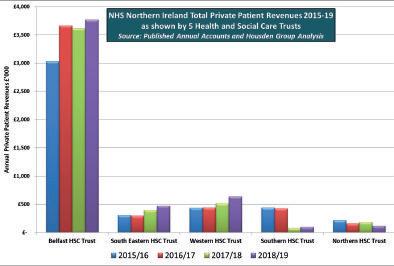
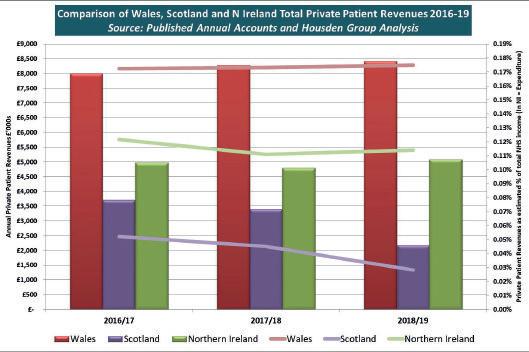


A self-pay patient’s demand for a refund for the treatment, and consultation, raises the question of a gesture of goodwill? Dr Sissy Frank (left) addresses the problem
QI saw a self-funded patient at my dermatology clinic who was seeking treatment for his acne scarring. After discussing all the options, the patient later called the clinic to arrange laser treatment.
The procedure went smoothly but he failed to attend a followup appointment and has now called the clinic to complain of redness and itchiness around the treatment site.
But he refuses to attend the practice so we can assess him and is demanding a refund for the treatment and the original consultation.
He claims that he has thousands of followers on social media and we will regret it if we refuse. How should we respond?
AEven though the patient’s behaviour may seem unreasonable, his expression of dissatisfaction with your treatment means the matter should be treated as a complaint.

In the response, the clinic complaints manager should reassure the patient that his concerns are being taken seriously, explain that the practice is going to investigate in line with its complaints procedure and include a copy of that procedure so he understands what to expect.
It will obviously be difficult for the complaints manager to carry out a detailed investigation if the patient refuses to engage, but he or she can still review the records and describe the treatment and the advice given, including the aftercare instructions at the time of the procedure.
They would normally take statements from you as the treating consultant and may also liaise
with any nursing staff who came into contact with the patient.
When a patient makes a complaint, the GMC expects you to ‘respond promptly, fully and honestly to complaints and apologise when appropriate’.
In practice, the complaints manager should usually obtain the clinician’s input in order to provide a factual account of the care relating to the complaint, a clear explanation of the treatment and a response to the concerns raised.
The response may include options to try to resolve the concerns such as the opportunity to see another specialist not involved in the patient’s clinical care to consider whether additional treatment may be appropriate.
If deemed appropriate, the complaints manager could also consider apologising for the fact that the patient is dissatisfied with the results.
Ultimately, it is for you as the treating physician or the clinic to decide whether to accede to the request for a refund.
Such ex gratia payments can be made as a goodwill gesture. Unfortunately, even if you do decide to re-imburse the patient, there is no guarantee that the patient won’t escalate his concerns, but be reassured that such a gesture cannot be held against you.
The Compensation Act 2006 makes it clear that an apology, offer of treatment or other redress does not, in and of itself, amount to an admission of negligence or breach of duty.
The response letter should explain what the patient can do next if still unhappy. The Independent Healthcare Sector Complaints Adjudication Service provides a complaints review service to subscribing independent providers.
Patients will occasionally behave inappropriately when they are unhappy with treatment, but you should not let this influence your own approach. Bear in mind that a professional and courteous response may well be disarming and help to restore his trust, so it is worth seeking specific advice from your medical defence body.
Even if the patient escalates his complaint, the fact that the clinic can show it has responded appropriately can help to avoid criticism of the complaints handling process.
A doctor expresses concerns about consent issues when a son wants to act as an interpreter in the consultation for his mother. Dr Sissy Frank gives her advice
QA man has contacted me asking if I will treat his elderly mother privately because he is worried about the length of the NHS waiting list for cataract surgery.
He explained that he would need to accompany her to the consultation and interpret because she speaks very little English. However, I am worried that it will still be difficult for her to understand all the risks and give her consent.
AIt is not uncommon for a family member to translate for someone who can’t speak English during appointments and a familiar face can also provide additional reassurance for the patient, who may be anxious or confused. However, involving a relative does raise medico-legal issues.
Assuming that you have no concerns regarding the patient’s comprehension, you should seek her consent before allowing her son to sit in on the consultation. Do not rely on his assurance that she has no objection.
Next, you are right to be concerned that the patient should have a complete understanding of her condition, the proposed treatment and the risks and benefits of that treatment as well as possible alternatives so that she can give her informed consent.
The law now considers the validity of consent from the patient’s perspective – rather than what would be deemed acceptable to a responsible body of medical opinion – and obliges doctors to take reasonable care to ensure the
patient is aware of any material risks involved in proposed treatment and of reasonable alternatives, including the option of no treatment.
This necessarily means the discussion may be quite detailed, as you need to determine the patient’s priorities and ensure they are properly informed about risks they would consider significant.
For understandable reasons, a family member might be reluctant to worry their relative by passing on disturbing aspects of treatment or an uncertain prognosis or may potentially lack neutrality and, advertently or not, misrepresent what you are saying.
You need to be sure that her son is able to convey his mother’s wishes to you and translate everything you say clearly and accurately without bias, particularly information about risks.
You may also need to ensure that the son understands sufficient medical terminology that he can appropriately convey the information you are seeking to provide.
Speak to the patient’s son and explain that the information that you are seeking to convey is complex. Reassure him he can be there to support his mother, but you would prefer to use a professional independent translator, ideally one with experience in medical translation.
Alternatively, depending on the language, you may be able to seek help from a colleague in your practice or at the hospital where the procedure will be carried out. Again, you will require the patient’s consent to have a third party present during the consultation. You should keep a record of this consent and the details of the other person present, including their name and role.
Given the potential communi-

cation challenges in this case, you should also consider what additional support you can offer the patient, such as an information leaflet in her own language to take away and read in her own time. Finally, bear in mind that consent is increasingly seen as a process, rather than a one-off
discussion. You will need to work in partnership with your translator to ensure the patient has every opportunity to ask questions and express her concerns throughout her time under your care.
Dr Sissy Frank is a medico-legal adviser with the MDU
• Completely open scanner that is well tolerated by claustrophobic patients
• Weight-bearing scans for spine and joints enable a more precise diagnosis
• Patients who are large or cannot lie down can be accommodated

more information go online at: www.trulyopenmri.com or call: 020 7370 6003 0161 434 8039

The impact of Covid-19 will be felt for some time to come, so for those starting out in private practice – or needing a review – it will be a tougher environment in these changed times. Ian Tongue prescribes ten financial considerations for success
AT THE same time as trying to establish your business, there will be more competition than usual due to established consultants rebuilding their practices.
In no particular order, here are the ‘must haves’ your business needs to succeed:
A key factor for success is engaging the services of a highquality secretary. Often a consultant will gravitate towards their NHS secretary, but the role is different, as you need someone who can help run the finances by ensuring all work is billed and chased for payment in addition to their secretarial duties.
If that is your NHS secretary, then great. The relationship will already be established and you should be able to hit the ground running.
You will need to decide whether they become an employee of your business or whether they are selfemployed for these services. It is common for the secretary to be self-employed, but some prefer the security and lower hassle of being employed.
This is not a choice between status; the agreement between you will determine the secretary’s employment status. It is always a good idea to discuss this with your accountant before committing.
Employing the services of an accountant who understands the medical profession should prove invaluable.
A general accountant is unlikely to understand the nuances of the medical profession and how the
Covid-19 situation will affect the market.
Working with your accountant before you commence is ideal and you should look to build a longterm relationship with them, receiving advice at the different stages of your career right through to retirement.
Depending on your specialty, you may have to incur significant amounts of costs in marketing yourself and your business.
Almost all consultants engaging in private practice must have a quality website. And do not underestimate the power of social media when it comes to the private medical sector.
If you get admitting rights at a private hospital, it will often have a team looking after consultants who will help you with marketing. After all, they have a vested interest in your success.
Clearly, the insurance market forms a substantial part of the private medical sector and you will need to register with the various insurers.
They have tariff rates for procedures and, as a new consultant, it is unlikely that you can negotiate something different.
However, with the impact of Covid-19, it is anticipated that fewer procedures can be carried out in any given time and therefore it is anticipated that pricing will need to change, otherwise many will have to focus on the selfpay market.
The self-pay market is usually
more profitable and pricing more flexible. Always consider how you take payment in this market, as you do not want to end up doing work for free by incurring bad debts. Do not assume that everyone seeing you will pay you after the work is carried out. It is always best to take payment up front for those self-paying.
It may be tempting to discuss pricing with colleagues, but be very careful, as the Competition and Markets Authority has been circling over the medical sector for some time and has punished businesses where its believes uncompetitive practices have been taking place.
Engaging a specialist accountant should give you access to advice you need on the most taxefficient trading structure. You may start out as one structure and then change to another later; for example, starting out as selfemployed and then changing to a limited company.
There can be significant savings for one structure over another and considerations such as pensions and your spouse’s tax position play a significant part in this decision-making. Also, your longerterm financial goals and requirements for income are considered as part of this decision.
We have seen from the impact of Covid-19 that work such as compiling medico-legal reports has been less affected by the virus. Specialties with clinical and non-clinical work help provide a more consistent income source in times of uncertainty as well as when you are building your private practice.
Having a clear plan from the outset can be especially important for ensuring that you take the right path for your career and maximise the return from your efforts.
Some consultants draft a business plan when they start out, but in most cases, something less formal is fine. Establish the direction of travel for your private work from the outset and structure your business needs around this.
When running a business, you are required by HM Revenue and Customs to keep adequate accounting records. From an accountancy perspective, this can
be a simple spreadsheet, but it is common to invest in electronic practice management packages which can also help manage the day-to-day finances.
There are several packages on the market to consider. All provide demonstrations for you to look at. Your secretary may have experience of one package over another, which can provide an advantage when choosing.
Speaking to helpful colleagues can provide invaluable information when establishing your private practice, as they will have a current insight into the private practice landscape you are operating in.
They will have their own experiences to draw on and, no doubt, can provide some helpful dos and don’ts.
The adage of ‘ability, availability and affability’ is extremely important to any private medical practice.
The private medical sector requires you to run a business and you cannot always rely on your medical reputation to draw work in.
While not exhaustive, the above points cover several key areas to consider for the establishment and development of a successful private practice.
The current landscape will provide additional challenges and therefore you will need to adapt. Speak to your accountant regularly to keep things on the right track financially.
Ian Tongue (right) is a partner with of Sandison Easson chartered accountants

Do not assume that everyone seeing you will pay you after the work is carried out. It is always best to take payment up front for those self-paying
DOCTOR ON THE ROAD: BMW X5

Eco-conscious independent practitioners will want to give this impressive hybrid car some serious consideration, says our motoring correspondent Dr Tony Rimmer (right)

WE ALL know that, in the medical world, regulation changes are happening constantly. To respond to them and stay competitive, all private doctors have learnt to change the way things are done – sometimes very quickly – and accept that this will happen repeatedly
It has been no secret to all car manufacturers that there is a general trend to electrify all vehicles to cut emissions and reduce road transport’s contribution to global warming.
Most governments have supported this move with regulations to reward the car-makers who move quickly to adopt the new technology.
New EU rules came into force on 1 January 2020 that will heavily penalise car makers if average CO2 emissions from the cars they sell rise above 95g per kilometre. If carmakers exceed that limit, they will have to pay a fine of €95 (£79) for every gram over the target, multiplied by the total number of cars they sell.
To comply, this means that they have to sell an increased number of hybrid and preferably fully electric cars from now on.
This is why we have seen the launch of so many high-profile new electric cars such as the electric Mini, the Fiat 500 and the Vauxhall Corsa.
Regarding petrol hybrid electric vehicles (PHEVs) bought as company cars, from April 2020 they are taxed not only on their CO 2 emissions but on their electriconly range as well.
And this is why premium car maker BMW, a favourite of many independent practitioners, has released the X5 xDrive45e. This plug-in hybrid replaces the previous 40e model and is based on the latest fourth-generation X5.
To get the extra electric-only range needed, the battery is now much larger: 24kWh instead of 9.4kWh. The four-cylinder petrol engine has also been replaced with a 282bhp turbocharged six-cylinder 3.0litre unit. The electric motor is good for an additional 111bhp. This means that the 45e is a fast SUV.
The updated interior includes a digital dash and better tech, including all the controls to


choose between the major driving modes: sport, electric, hybrid and adaptive.
To make the best use of the available battery power, the adaptive mode will work out, from your satnav destination, where best to use the electric drive and minimise the use of petrol. It calculates that you will arrive with a fully depleted battery ready for a recharge; clever stuff.
The X5 remains a large, roomy and luxurious SUV not dissimilar to a Range Rover. Passenger space and luggage space has hardly been compromised by the bigger underfloor battery although there is no seven-seat option on this model.
Smooth and quiet
On the road, the new powertrain is impressive. In hybrid mode, you move off under silent electric power and the engine only kicks in with a decent prod of the throttle.
When it does, the transition is smooth and quiet.
Pushed hard, this X5 feels as fast as the figures suggest despite the

To get the extra electric-only range, the battery is now much larger: 24kWh instead of 9.4kWh
significant kerb weight of nearly two-and-a-half tonnes.
Unfortunately, the handling suffers from the extra weight, although excellent chassis tuning negates this effect to a great degree. The ride is excellent on the standard air suspension and you can waft along in great comfort, particularly on the motorway.
So, should the eco-conscious independent practitioner consider this new hybrid X5?
Well, it depends the type of driving you do. If you mainly do urban runs and have access to overnight home re-charging, you can save a lot in running costs and do your bit to save the planet.
Although BMW quote an electriconly range of 54 miles, in the real world it will be 30-40 miles. But this is much better than rivals such as the Volvo XC80 T8, so the newX5 goes to the top of the class.
Dr Tony Rimmer is a former NHS GP practising in Guildford, Surrey
Body: Five-seat SUV. Four-wheel drive
It calculates that you will arrive with a fully depleted battery ready for a re-charge; clever stuff
Engine: 3.0litre six-cylinder petrol. Single electric motor
Power: 282bhp (petrol) and 111bhp (electric)
Torque: 600Nm (combined)
Top speed: 146mph
Acceleration: 0-62mph in 5.6 seconds
WLTP economy: Up to 201mpg
CO2 emissions: 31g/km
On-the-road price: £63,165


Bouncing back! General surgeons’ latest accounts examined in our benchmarking survey, by Ray Stanbridge, have eased well into the recovery position
OUR REPORT in Independent Practitioner Today a year ago stated that 2017 was not a great year for general surgeons. We were also less than optimistic about the future. However, we are pleased to say that events have proved us to be wrong and general surgeons look to have had a reasonable year in 2018.
Our survey shows that gross income from private practice for general surgeons increased by 10.5% between 2017 and 2018, rising from £133,000 to £147,000.
Costs increased by a relatively
small amount – 3.3%, going up from £61,000 to £63,000.
As a result, pre-tax profits rose by a most encouraging 16% on average, increasing from £72,000 to £84,000.
What then are the reasons for these changes?
We have noticed that, for many general surgeons, self-pay income is increasing.
Patients are paying for minor and intermediate procedures through, for example, encashment of tax-efficient ISAs. In addition, several general surgeons did
well in the 2017-18 financial year from Choose and Book work.
While this is often localised, it can be very profitable in individual cases. Most of these payments in 2018 were made to surgeons as selfemployed, rather than as employed or quasi-employed consultants.
But the situation may well change in future if the IR35 tax rules proposed become fully operational, meaning that we will see Choose and Book work treated as salaried income.
We have noticed quite a large increase in costs of staff between 2017 and 2018. Family staff salary rises are frequently correlated with the increase in tax-free personal allowances. Also, some private hospitals have sought to increase secretarial charges under the provisions of the Competition and Markets Authority (CMA) rules, effective from 2015.
Surprisingly, consulting room hire costs seem to have fallen a little, for reasons that are not immediately obvious. It may be that increases in secretarial costs include an element of room hire costs. More analysis is required here.
Professional indemnity/insurance costs showed a small increase
General surgeons are typically not as aggressive as some of their colleagues in seeking cheaper sources of indemnity cover and continue to support the main medical defence organisations
between 2017 and 2018. General surgeons are typically not as aggressive as some of their colleagues in seeking cheaper sources of cover and continue to support the main medical defence organisations.
Other costs have remained broadly like those in 2017. There has been a small increase in conference costs, generally reflecting a professional body’s choice of an exotic location. On the other hand, there was a small decline in ‘other costs’, primarily marketing.
As we have previously reported, it is increasingly difficult to define a ‘general surgeon’ because specialisation has completely changed what a traditional general surgeon does.
Year ending 5 April. Figures rounded to nearest £1,000 (percentage is also rounded up)
Source: Stanbridge Associates Ltd.


However, breast work continues to dominate. But we were surprised to find how well general surgeons performed in 2018. A preliminary look at 2019 results suggest that this performance has been maintained. We shall monitor with interest.
Note that the basic requirements
for those eligible to be a member of our survey are that the surgeons:
Are not in full time private practice;
Hold either an old-style or a new-style NHS contract;
May or may not have incorporated their business;
May or may not work in a group;
Have a keen interest in private practice;
Have been engaged in private practice for at least five years;

Earn at least £5,000 a year from private practice.
Readers should also bear in mind that there are increasing difficulties of making year to year comparisons when we compile this survey. General surgeons, as do other consultants, now trade in a variety of ways; for example, though limited liability compa nies and limited liability partner ships.
Other general surgeons have specialised completely in one area, particularly breast surgery, rather than undertake a variety of proce dures. This trend, in turn, has been encouraged by the process of revalidation.
For these and other reasons, our survey should not be regarded as statistically significant, but we hope it is a reasonable representation of what an average general surgeon earns and spends.

Next month: Cardiologists
Ray Stanbridge is a partner with accountancy, finance and tax advisory medical specialists, Stanbridge Associates Ltd
Years ending 5 April
Source: Stanbridge Associates Ltd

By industry for industry, Healthcode are the experts in information technology focussing solely on solutions for the healthcare sector. Trusted by leading hospitals, independent practitioners and insurers to deliver high quality, secure, cost effective IT systems that connect key stakeholders to seamlessly enable transparency within the sector and enhance patient safety.
• Circa 20k clinician accounts
22k practitioner accounts
• Over 300 private hospitals
• All major private medical insurers
• Process and clear an average of 28k bills daily worth £3bn
£3.3bn






Coming in our August issue, on our website from 14 August: Catch up with all the news and information affecting you and your practice as – hopefully – private practice picks up
Now make sure your private practice is best positioned to benefit from the recovery. Simon Brignall, of Medical Billing and Collection, has some excellent advice at a time when many consultants are reviewing their arrangements after Covid-19 provided the breathing space to discover they have real problems with their invoicing
Our guide to delivering superior patient experience in private practice continues: in part 3, Jane Braithwaite (right) looks at putting patients first and ensuring excellent customer service before, during and after appointments. And see how you can support patients with engaging, helpful and accurate content. She says: ‘Your patient should be at the centre of your patient experience strategyand every interaction your patient has with your practice is important.’

As some private hospitals and clinics move more towards greater availability for consultants and their patients, what’s the latest from your private hospital’s trade body? David Hare, boss of The Independent Healthcare Providers Network, gives you an update
We report on how some ophthalmologists have been coping during lockdown
Published by The Independent Practitioner Ltd. Independent Practitioner
Today is editorially independent and thanks Bupa for its assistance with distribution.
Printed by Pepper Communications Ltd Material is governed by copyright. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form without permission, unless for the purposes of reference and comment. Editorial layout is the copyright of the publishers. If you wish to use it for promotional purposes on websites or for reprints, we would be happy to discuss licensing the copyright to you.
© The Independent Practitioner Ltd 2020
Registered office: 7 Lindum Terrace, Lincoln LN2 5RP
Write to
Independent Practitioner Today 7 Lindum Terrace, Lincoln LN2 5RP
TELL US YOUR NEWS
Robin Stride, editorial director
Email: robin@ip-today.co.uk
Phone: 07909 997340

@robinstride
ADVERTISE WITH US
Independent Practitioner Today’s Accountant’s Clinic A to Z series lands on the letter ‘M’ and something most doctors do not find is easy
– Managing your practice
Cavendish Medical brings you another topical article to help you make the most of your personal finances
Planning new or replacement staff? In our ‘Keep it Legal’ column, Hempsons’ solicitor Julia Gray writes that it is important to make probationary periods work for you. Are you getting maximum benefit from probationary periods for new staff? She examines the purpose and operation of probation and suggests how it can work most effectively in independent practice
Our Business Dilemmas series continues as MDU medico-legal adviser Dr Kathryn Leask answers some difficult questions from a private psychiatrist who is being chased by the police to provide information about a patient, particularly in relation to his mental health and what medication he takes. Can he provide any information about the patient to the police? And she answers a private paediatrician who is caught in the middle between a child’s warring father and mother
Surgeon Mr David Sellu, convicted for gross negligence manslaughter of a patient – overturned on appeal after a 30-month prison sentence – continues his story and wonders how inmates with no medical background would fare if they needed treatment while ‘inside’
ADVERTISERS: The deadline for booking adverts in our August issue is 24 July

To advertise in the journal or our website business and lifestyle directories, contact Margaret Floate, advertising manager
Email: margifloate@btinternet.com Phone: 01483 824094
GET A SUBSCRIPTION DISCOUNT!
£90 independent practitioners. £90 GPs and practice managers (private & NHS). £210 organisations. Save £15 paying by direct debit: individuals £75 (organisations £180).
TO SUBSCRIBE
Email karen@marketingcentre.co.uk or phone 01752 312140 or go to the ‘Subscribe’ page of our website www. independent-practitioner-today.co.uk
Publisher Gillian Nineham
Phone: 07767 353897.
Email: gill@ip-today.co.uk

SAVE £15 WITH DIRECT DEBIT!
Guarantee delivery of your next copy of Independent Practitioner Today. Take out a subscription and you will get full access to our news, features and previous issues on our website. See details on the left.
BACK ISSUES: £12.50 including post & packaging CHANGING ADDRESS,
Phone 01752 312140 or Email karen@marketingcentre.co.uk