INDEPENDENT PRACTITIONER TODAY
The business journal for doctors in private practice
Getting uninsured patients to pay their bills
How to tackle the billing issues posed by self-pay patients P44


How to tackle the billing issues posed by self-pay patients P44

By Robin Stride
Private practice incomes remain healthy and major business opportunities beckon for doctors who understand the changing market and take advantage.
That was the overwhelming message in this year’s keynote speech given to more than 100 private consultants and GPs at the Independent Doctors Federation’s (IDF) annual general meeting.
Many members were encouraged by the upbeat stateofthemarket analysis presented to the meeting by a leading adviser to specialists.
Based on latest tax return figures and discussions with independent practitioners, he revealed:
n A further rise in selfpay – something he said most consultants have been ‘pretty slow’ to take advantage of;
n Higher price potential in the self pay market, if providing a quality service;
n Predictions of higher fee levels following a drop in senior consultant numbers in private practice;
n More beneficial closer working relationships with private medical insurers;
n Increasing NHS spend in the private sector.
gloom and doom merchants are wrong – unless people are overdeclaring their income to the taxman, which I doubt.’
He observed that with the NHS in continuing ‘turmoil’ and the private sector undergoing great change, real opportunities were developing for excellent independent medicine, although ‘the problem is that all doctors state they provide an excellent quality of service and, by definition, this cannot be true’.
Mr Stanbridge, of Stanbridge Associates, believed basic market economics meant the NHS could not exist longterm in its current form. It would always be in crisis, innovation would be stifled and it would try to reduce cost of supply.
The long term solution was to reduce the supply of specific services and look at charges and copay. But services in the short term would be rationed and transferred to the private sector to try to cut costs.
He said although conflicts continued with some insurers, they now accounted for less than 50% of the market.
Mr Stanbridge forecasted that closer working relationships with insurers would increase quality and efficiency. He said senior insurer officials now recognised that one size did not fit all and they had to change the way they worked with providers.
This could potentially mean additional financial rewards for provider quality and clinical efficiency and for new products and services.
Giving what he called ‘a talk of hope’, he said growth in the number of consultant groups would be another bonus. Groups were achieving a ‘staggering’ 15%+ compound growth in income.
They could increase quality and business efficiency, subspecialise and provide cross cover, reduce ‘cock ups’ and cut costs – for example, by negotiating lower medical indemnity.
And they could also innovate, invest, develop and market selfpay services and improve practice management. He predicted a growth in professional managers running the practice as a business and also a decline in traditional secretaries.
Despite Competition and Markets Authority rules, he reported consultants were investing in new technologies and methods of delivery. There was also a large increase in the number of private investors interested in ‘smallscale’ investment.
Mr Stanbridge said insurers were recognising new facilities that provided good and costefficient services.
n IDF reports, page 4
n Getting self-payers to pay, p44


There was an impending shortage of supply of consultants, only those really interested in private practice would remain and insurers were reconsidering their strategies.
Independent Practitioner Today columnist and medical accountant Ray Stanbridge told doctors: ‘The Xxxxx
Mr Stanbridge told the meeting at the King’s Fund, London: ‘I think we are going to see a lot more innovation in the next few years – there is money to be made.’






I want to wind down
Accountant Susan Hutter advises a doctor who wants to wind down his practice P12
A knock-out idea
How an anaesthetist’s app for calming anxious children won him a top award P26
How to build a brand
The third part of our ‘Practice Builder’ series shows the importance of brands P29
Breathe life into your PPU
The ‘year in the life of an NHS PPU’ shows how to spring-clean your contracts P34
Keep tabs on staff sickness
Legal advice on how doctor employers can alter staff sickness absence procedures P41
Getting uninsured patients to pay up
Self-pay patients are on the rise and so are the problems of gathering their fees P44

By Robin Stride
An insurance industry leader has voiced fears of a doubling of the tax on private medical insurance unless the Government can be persuaded to call off its attack on premiums.
Stuart Scullion, chairman of the Association of Medical Insurers and Intermediaries (AMII), warned that the Treasury might be tempted to increase the insurance premium tax rate to bring it in line with VAT – at a whopping 20%.
centage point, bringing the tax to 10%, was declared in George Osborne’s March Budget.
Insurers and cash plan providers have strongly criticised the move, with Bupa UK’s managing director Richard Bowden saying the latest rise makes no sense when the independent sector is reducing the burden on an increasingly strained NHS.

‘I love reading Independent Practitioner Today, but can’t you print something happy for once? It can be quite depressing.’
That was a comment to us from one of the consultants at last month’s Independent Doctors Federation AGM.
The frontpage news that our readers need to know has not always been welcome during this period of great change in private practice, we admit.
But we always try to balance it with useful advice from experts about what you should think about or do as a result.
Some recent headlines have been nothing to cheer about:
‘Doctors facing a £1m+ claim surge’, ‘Bonuses trigger tax hit’, and ‘Are you fixing prices?’are just some of the stories that have grabbed attention.
So it is a pleasure to run the splash headline in this issue: ‘Healthy returns’. Things are looking up in the world at last – at least according to one leading specialist adviser.
His was welcome news to all those present and we hope it is to you. Be sure to tell us your good news too. We know many of you are, like some doctors in this issue, incredible entrepreneurs who deserve to have their uplifting business stories told.
TELL US YOUR NEWS Editorial director Robin Stride at robin@ip-today.co.uk Phone: 07909 997340 @robinstride
TO ADVERTISE Contact advertising manager Margaret Floate at margifloate@btinternet.com Phone: 01483 824094
TO SUBSCRIBE lisa@marketingcentre.co.uk Phone 01752 312140
Publisher: Gillian Nineham at gill@ip-today.co.uk Phone: 07767 353897
Head of design: Jonathan Anstee Chief sub-editor: Vincent Dawe 11,648 circulation figures verified by the Audit Bureau of Circulations EDITORIAL
Now the trade body has pledged to step up its campaign to get the Government to make medical insurance cheaper by exempting it from the new 10% insurance premium tax.
It will lobby the Government as a single voice, representing insurers and companies who sell private medical insurance.
Mr Scullion said: ‘We believe the success of this lobbying will be determined by consolidated and continued pressure on Government to reconsider their position on insurance premium taxation attracted to health insurance products.
‘The Chancellor’s decision to include health insurance under a general insurance umbrella is illogical. Health insurance is an elective insurance: people choose to protect their health.
‘Increasing insurance premium tax will only discourage people from health insurance options, and deter businesses from providing health benefits for their staff.’
Following the Chancellor’s postelection Budget last July, the first insurance premium tax rise came into force last November with an increase of 58%: from 6% to 9.5%.
But a second hike of a 0.5 per
Mr Scullion told AMII’s AGM: ‘As people are deterred from health insurance options, they are driven to an overburdened and over stretched National Health Service. This does not make sense for the longterm wellbeing of the nation.’
He paid tribute to healthcare cash plan provider Medicash, and its chief executive Sue Weir, who has led the campaign calling for health insurance to be exempt from the tax.
Mrs Weir told the meeting she would lobby the Government to make all healthcare insurance products exempt in line with life insurance, permanent health insurance and other ‘longterm’ insurance products.
She said: ‘This is a stealth tax that affects millions of people. It will place a further burden on an already hugely strained NHS and it directly contradicts all the Government’s stated commitments around the health and wellbeing of the nation.
‘It’s a fact that healthcare cash plans have a positive impact on business productivity and absenteeism as well as the physical and mental health of workers across the country.’
The UK now differs from its EU counterparts, with 12 member states exempting health insurance from the premium tax and only Greece applying a similar rate.
By Edie Bourne
Senior doctors are being urged to take advantage of valuable protection schemes to help them safeguard their pension from harsh tax charges.
These schemes are now open for applications and some practitioners will need to make an urgent review of their benefit accruals.
As a result of the recent cut to the lifetime allowance limit – the total amount you can contribute to your pension free of tax – the Government has introduced new pension protections which could potentially restore many doctors with a higher overall allowance. The lifetime allowance was cut
further last month to just £1m following a series of reductions over the last four years.
Fixed Protection 2016 (FP2016) is now available to those who do not already hold a previous version of fixed, enhanced or primary protection.
Specialist financial planners
Cavendish Medical told Independent Practitioner Today this would allow doctors to retain a £1.25m lifetime allowance limit as long as all benefit accrual had been suspended from April.
Doctors are advised to check immediately whether they are in a position to apply.
Individual Protection 2016 (IP2016) is available for those that

Patrick Convey ‘The tax charge if you breach the lifetime allowance can be a staggering 55%’
have pension savings in excess of £1m as at 5 April. Pension savers with this protection are able to carry on contributing to their pension.
Cavendish Medical’s technical director Patrick Convey said: ‘Every senior doctor is likely to breach the new allowance due to the very nature of making pension
HM Revenue and Customs has warned highnetworth investors that offshore schemes will bring them no riches.
Its message came after it protected £365m in tax by defeating a tax avoidance scheme involving dividends paid on shares to a company based in the Cayman Islands. A tax court ruled that the Clavis Liberty Fund 1 LP scheme created an artificial tax loss; the judgment covering 99 partners and protecting tax at stake in other cases.
The judgment is significant for HMRC, as it is the first time this particular antiavoidance legislation has been tested in court.
Jennie Granger, HMRC director general of enforcement and compliance, said: ‘This is an impor
tant success for HMRC both in terms of the money that it will bring in and the powerful signal it sends to anyone who might be tempted to use any form of offshore arrangement to avoid paying the tax that is due.
‘In the space of a week, HMRC has secured three court victories, protecting more than £1bn in tax and proving that tax avoidance doesn’t pay. It’s time for people to get out of these schemes – they don’t work and we will defeat them.’
The scheme involved a limited partnership, registered in Jersey and claiming to carry out UK trade. Each of the scheme’s 99 users contributed a sum which was used, together with a large bank loan, to acquire rights to dividends declared by a Caymanregistered company.
The partnership claimed a deduction for the cost of the dividend rights, but sought to exclude the dividend payments paid from its trading profits, giving rise to a loss.
A wide range of clinicians – not just plastic surgeons – will be affected by new GMC standards from next month for doctors carrying out cosmetic procedures.
Doctors carrying out any procedure or treatment with the primary objective of changing an aspect of a patient’s physical appearance need to be aware of and follow the new guidance.
Medical Defence Union (MDU) medico legal adviser Dr Nicola Lennard said: ‘As explained in the guidance, getting the patients’ fully informed consent is key to avoiding misunderstandings.
contributions into the NHS scheme over a number of decades.
‘Unfortunately, the pension protections available are nearly as complicated as the pension schemes themselves, so it is a very difficult area for the busy professional to get right. If you are unsure how to proceed, you should seek help without delay –the tax charge if you breach the lifetime allowance can be a staggering 55%.
‘To make matters more complex, although applications are now open, the online service will not be launched until July. If planning to retire before July, you will need to make a temporary application to HMRC.’
patient’s consent themselves, rather than delegate it to another colleague.
It recognises that patients can be misled by cosmetic services marketing and warns doctors not to use promotional tactics in ways that could encourage people to make an illconsidered decision or provide their services as a prize to lure them in.
Dr Lennard added: ‘Before starting to offer cosmetic treatments, doctors should also check with their medical defence organisation to ensure they have appropriate indemnity in place for the work they are doing.’
Growing popularity of nonsurgical cosmetic treatments, such as botulinum toxin and dermal fillers, means more private doctors now offer cosmetic procedures to patients.
King Edward VII’s Hospital in London has appointed Tim Brawn as its new fundraising director. He will work with the hospital’s friends and supporters to further redevelopment and expansion plans.
‘A robust consent process which ensures patients are given all the information they need about a procedure, including the risks, along with time to consider and change their mind, is important with any treatment, but particularly so with cosmetic treatments, where patients may have high, or even unrealistic expectations.’
Previously, he was with Combat Stress, the veteran’s mental health charity.
Detailed GMC guidance on this issue states doctors carrying out an intervention must seek the
But nearly a fifth of cosmetic intervention cases notified to the union in the last decade involved nonsurgical procedures.
See ‘GMC grips beauty ops’, page 7
By Robin Stride
Young doctors in private practice are wanted by the Independent Doctors Federation (IDF) as it seeks to enhance its role as the ‘voice of independent practice’.
IDF president and council chairman Dr Peter King-Lewis said the IDF was thriving but needed more young members if it was to be taken seriously ‘by those seeking to carve out the future of private practice: the hospital groups and the private medical insurers’.
He added: ‘We must as independent doctors be truly representative.’
Latest figures show IDF membership grew from 1,146 to 1,187 in the last year. 64% are inside London and 36% outside.
But there are concerns that the proportion of those aged under 50 has reduced. It fell from 28% to 26% last year.
Private GP Dr King-Lewis told over 100 doctors at the organisation’s annual general meeting: ‘Currently, those who are fighting for a fair future for independent practice are those who can safely say the bulk of their career is behind them. We are working for the future careers of others – the
Private practice has much to offer the growing numbers of NHS GPs who are considering walking out early, according to an independent doctors’ leader.
And he said the Independent Doctors Federation (IDF) would help those who wanted to take up this ‘rewarding and viable career option’.
IDF GP committee chairman Dr Neil Haughton told the group’s annual general meeting that a BMA poll last year of more than 15,000 GPs found that 34% of those aged 50-54 wanted to retire early.
‘I can’t remember ever hearing about a private GP retiring early –usually quite the opposite. But what a waste of expertise and experience – hounded out by QOF points, targets and regulation.’
But he said private general practice was thriving and the IDF could provide support to disaffected NHS colleagues if they wished to join the independent sector.
Dr Haughton said: ‘We are so lucky that we can practise the way
we do, prescribe without interference, refer to the colleagues we know, trust and suit our patients, and provide the level of service and continuity that has been all but lost in the NHS.’
Giving his annual verbal report, he said private GPs did face challenges, but they were ‘in a far better place than the alternative and we should be proud of the standards achieved by our members’.
In the last year, progress had been made by persistently engaging with the Care Quality Commission (CQC), the private insurers, vaccine suppliers and others.
He had opened his doors to senior CQC GP advisers to give them direct experience of how a private practice ran and the differences between independent and NHS GPs. The exercise was extremely useful and rewarding on both sides.
Dr Haughton said he was impressed by the progress the CQC had made and things had mostly come a long way in the last 12 months, although the message
newly-appointed consultants and GPs coming to private practice.
‘These are the people who need to be welcomed and brought into the IDF. They are needed working in the committees now, to sit on the executive and take over running the federation in the future.’
But he said newly-qualified postgraduates were not all leaving the NHS for private practice – many were leaving to go abroad. ‘With the prospect of loss of independence to the hospitals, heavily reduced fees and open- and selfreferral excluding GPs, why wouldn’t they?’

did not always quite get down to the inspectors on the ground.
He told doctors: ‘I know there is still far to go, but be assured that we have influence and contacts at the highest levels of CQC to address policy concerns.’
Private GPs had experienced more problems with vaccine supply, most recently the meningitis B vaccine, but manufacturers were addressing this. Problems were usually due to trying to keep up with demand.
He told the meeting, which included doctor guests from Bupa, that the IDF remained strongly opposed to private insurers trying to bypass GPs by allowing direct patient referral for some conditions or by open referral to their choice of consultant. He said this fundamentally undermined the role of primary care and potentially patient safety.
Dr Haughton added that the IDF was changing and expanding and needed to maintain its position as ‘the most respected voice of independent practice’.
Dr King-Lewis also appealed to IDF members to help bring younger doctors on board.
‘If the hospitals, the insurers and the independent doctors work together, independent practice can and will thrive. Succumb to infighting and it will wither on the vine and we will be partly to blame.’
He said among his priorities for the next year were raising the IDF’s profile, increasing membership, better understanding the various needs of members, and building on discussions with private medical insurers.
Closer links made with the insurers
The head of the IDF’s specialists’ committee has pledged continued engagement with private medical insurers in the year ahead.
Dr Brian O’Connor said that although problems with insurers remained, he had some good meetings with them in the last year and the federation liked to think it was ‘the voice of reason in the independent sector’.
He added: ‘There seems to be a change in attitude as private medical insurers realise that, without doctors on board, they cannot grow the market.’
The IDF also aimed to influence the Private Healthcare Information Network (PHIN), which is publishing performance information in the independent sector. Dr O’Connor said the federation wanted to ensure appropriate data was collected.
Talking of the Competition and Markets Authority and its change of heart about requiring HCA to divest some hospitals in London ( Independent Practitioner Today , April 2016), he said the specialists committee had always felt the hospital group provided ‘a terrific service’ in London.
By a staff reporter
A second healthcare centre has been opened by a company formed thanks to the vision and drive of an entrepreneurial consultant radiologist.
Consultants are now seeing patients at LycaHealth’s new multispecialty clinic in Orpington, Kent – six months after the brand was launched last November in Canary Wharf by the Mayor of London Boris Johnson.
The company said it now has a combined strength of more than 100 consultants using both facilities, but would always welcome more specialists on board who could bring special skills and strengths to its offering.
As before, the centre offers comprehensive, multispecialty consultation, diagnostics and wellness services.
LycaHealth celebrated the opening by hosting its first continuing professional development event and welcomed over 100 GPs to listen to three consultant speakers –orthopaedic surgeons Mr Suhaib Sait and Mr Ajeet Kumar and neurosurgeon Mr Richard Gullan. Chief executive and radiologist
Dr Manpreet Gulati said: ‘We are delighted to open our second centre in less than six months after our flagship centre opened in Canary Wharf and are overwhelmed by the response we have had from our GP colleagues.
‘We aim to bring a high-quality client experience to the healthcare sector, with patients seen in modern, stylish and welcoming surroundings.
‘We have plans for further centres to open around the UK and South Asia and eventually Africa over the next few years.’
The company said it was committed to make ‘significant capital investment’ to develop its plans.
LycaHealth is backed by entrepreneur Subaskaran Allirajah, chairman of Lyca Group, the world’s largest international mobile virtual network operator.
He told Independent Practitioner Today: ‘Manpreet has a powerful vision for the future of healthcare which is much more patient-centric than the current provision and is driven by his personal experience.
‘It was this vision that attracted me to launch LycaHealth in the first place. The second centre is an

equally stunning facility and I have great hopes for the future of LycaHealth.’
Dr Gulati said the Canary Wharf centre had a very corporate feel to its ambience and catered to highprofile clients such as bankers, lawyers and IT professionals, who, in their mind, came to attend a business appointment with the doctor.
In Orpington, the clinic aimed to offer the same high-quality experience in a ‘very hospitalitylike setting’ and commensurate
The Independent Doctors Federation (IDF) is to have a new management structure.
Until now, there has been a council consisting of elected and co-opted members as well as senior employees. But president and council chairman Dr Peter King-Lewis said that as the IDF had grown in numbers and complexity so had the council.

Now a board of governors will oversee all IDF

Co-founders
Dr Manpreet Gulati (right) and director
Sen Kandiah, outside the new LycaHealth centre
with the surrounding demographic.
The new centre has the same range and quality of diagnostics and Philips imaging equipment – a 3 Tesla MRI and ultra-low radiation dose 128-slice CT scanners as well as X-ray and fully loaded high-resolution ultrasound facilities.
Also available is a spacious physiotherapy and sports-injury and rehabilitation gym housing advanced equipment through a strategic relationship with physiotherapy partners Healthshare.
activities, be chaired by a lay member and meet three times a year. The board will delegate the day-to-day running of the IDF to the executive committee, and committees will report into the executive committee.
The IDF will be working in the next few months on a position statement about doctors’ medical indemnity.
Future presidents and chairmen of the IDF
will serve a two-year term, not three, and there will be a president-elect for the preceding two years. Specialists’ committee chairman Dr Brian O’Connor is now president-elect and will take over at the AGM next year.
Tributes were paid to IDF managing director Fiona Merrick who is retiring after 16 years. She is handing over to independent medical business expert Sue Smith, who has been appointed interim chief executive.
A cosmetic surgeon has launched a ‘one stop shop’ consultancy offering private doctors business backup services.
Mr Paul Baguley, who has a private practice in Yarm, North Yorkshire, said his company aimed to provide new and established consultants with a package of expert help and support in starting out, maintaining and growing their independent venture.
Step into Practice allows member clinicians to tap into a network of associated partners and suppliers who, it says, will save them time and money through preferential rates.
Members can be provided with ‘everything they need to succeed in their own practice’. This includes a full office management system with IT hardware, PPM software, staffing, virtual or physical office management, templates,
insurance – including medical indemnity – accounting, banking, financial advice and investment help.
Mr Baguley said this would allow doctors get the business side of the practice completely managed so they could focus on the clinical side.
Members pay £250 monthly (£2,500 for a year) and can gain access to a secure website which offers them online templates, protocols, system manuals and check lists ‘so they can hit the ground running’.
He added: ‘We believe that membership will realise at least a 20% monetary saving in any practice, savings which allow members to take a greater salary or reinvest in the business. But the real savings are in time and energy setting up and maintaining the practice.’
A new app service dubbed the ‘Uber for private healthcare’ aims to deliver a doctor to the patient’s door in 60 minutes.
Patients using GPDQ (GP Delivered Quick) can track their GP and receive live updates about appointments seven days a week from 8am to 11pm at a location of their choice.
App co founder NHS and private GP Dr Anshumen Bhagat told Independent Practitioner Today: ‘GPDQ provides another option for patients who want to see a doctor when it suits them – it really is that simple.
‘It also enables all GPs in the UK to see patients on a private basis, work flexibly and earn extra income in the process.
‘They’re essentially running a
The GPDQ service allows patients to order and track a private GP on a mobile

virtual clinic through our stateoftheart mobile platform.’
The company said doctors’ earnings started at £90 for a 25 minute visit, increasing at weekends and bank holidays. All its registered doctors are required to work in the NHS for at least two sessions a week.
Via the app, patients pay £120 during weekdays, £150 at the weekend and £200 on bank holidays.
By Charles King
An entrepreneurial consultant has announced he resigned his practising privileges after nearly 20 years in response to the Competition and Markets Auth ority (CMA) private healthcare investigation.
Dr Tony Lopez, who created The Imaging Clinic Limited (ICL) in 2003, set up his largest joint venture (JV) with BMI Healthcare at Mount Alvernia Hospital, Guildford, Surrey.
There, ICL jointly owns and operates with equal equity, four complex imaging fixed facility scanners, including a 128 slice CT, 1.5T MRI, full field digital mammography and a dualheaded gamma camera with SPECT, and it has invested over £2m.
The JV company BMI Imaging Clinic Ltd has also operated both mobile 3T MRI and PET CT scan
ners at the same facility with plans to install a fixed facility later this year.
But the consultant radiologist told Independent Practitioner Today that arrangements needed unwinding, as his personal share exceeded the maximum 5% consultant equity stake allowable under the CMA’s final order.
He said he had to decide between:
Selling his 50% equity stake to BMI Healthcare or another independent party that has no practising privileges in the hospital;
Purchasing BMI Healthcare’s entire equity stake and resigning his practising privileges at the hospital;
Maintaining his existing equity stake in parity with BMI Healthcare and again resigning his practice privileges at the hospital.
Although he received significant offers from other parties and also made ‘a considerable offer’ to
acquire the whole business from BMI, ultimately he decided to retain his stake and resign his practising privileges at Mount Alvernia.
Dr Lopez said: ‘I was left with no choice and was not prepared to leave my valuable investment and years of hard work behind.’
Consequently, and with great disappointment, he migrated his practice to his NHS hospital and other local private facilities.
He said one of the CMA’s conclusions was that equity ownership by consultants in private health facilities might give rise to an ‘adverse effect on competition’. This reflected possible distortion of referral decisions to particular hospitals and distortion of patient choice of diagnosis and treatment options.
But it was also acknowledged that equity ownership schemes might be beneficial where these
‘result in a reduction to barriers to entry that is likely to be as least as beneficial to competition as any distortion is harmful’.
Dr Lopez said the BMA suggested to the CMA that the initial proposed limit of 3% on equity stakes in a hospital or equipment at which a consultant had practising privileges, or the ability to commission tests, was too low to encourage consultants to become engaged in the running of a hospital.
The association unsuccessfully argued that a minimum stake of 10% was more likely to encourage innovation while still ensuring that the equity stake did not influence referral or commissioning behaviour.
One outcome, though, is that Dr Lopez finds he now has far more time available and plans a number of new business ventures, particularly with other consultants nationally.
By Leslie Berry
New GMC guidance for doctors carrying out cosmetic procedures anywhere in the UK coming into force in June (see page 3) covers both surgical and non surgical procedures.
The 21 page document says doctors must:
☛ Advertise and market services responsibly: Any advertising must be clear, factual and not use promotional tactics, such as ‘twoforone’ offers to encourage patients to make ill considered decisions. It also includes a ban on offering procedures as prizes. Doctors must not allow others to misrepresent their services.
☛ Give patients time for reflection: Make sure they have the time and information about risks, to decide whether to go ahead with a procedure. Patients should not feel rushed or pressured.
☛ Seek a patient’s consent themselves: The doctor carrying out a cosmetic procedure is responsible for discussing it with the patient, providing them with the information and support they need, and for obtaining their consent. This responsibility must not be delegated.
☛ Provide continuity of care: The doctor must make sure patients know whom to contact and how their care will be managed if they experience any complications and that they have full details of any medicines or implants.
☛ Support patient safety: Doctors must make full and accurate records of consultations, using systems to identify and act on any patient safety concerns, and contribute to programmes to monitor quality and outcomes, including registers for devices such as breast implants.
GMC chairman Prof Terence Stephenson said: ‘Cosmetic interventions should not be entered into lightly or without serious considerations. Above all, patients considering whether to have such a procedure need hon

We do sometimes come across poor practice and it is important that patients are protected from this GMC chairman Prof Terence Stephenson (above)
est and straightforward advice which allows them to understand the risks as well as the possible benefits.
‘It is a challenging area of medicine which deals with patients who can be extremely vulnerable. Most doctors who practise in this area do so to a high standard, but we do sometimes come across poor practice and it is important that patients are protected from this and that doctors understand what is expected from them.’
Prof Sir Bruce Keogh, national medical director at NHS England, said: ‘The independent review I chaired, following the PIP breast implant scandal, highlighted major problems with unsafe practices in the cosmetic sector, including poor followup care and record keeping, and misleading and inappropriate advertising and marketing techniques.
‘This addresses these issues and will drive safer care, more ethical practice and, overall, a better
experience for people undergoing cosmetic procedures. It will also help ensure doctors are seen to be open and honest, that they work within their competence and seek appropriate training and advice where necessary.
‘This marks an important step forward for patient protection across a wide range of cosmetic and lifestyle procedures, including areas such as laser eye surgery.’
The GMC said it was working closely with the Royal College of Surgeons (RCS), which has published its own set of professional standards, specifically for cosmetic surgery.
College vice president Mr Stephen Cannon said: ‘Our professional standards for cosmetic surgery, coupled with the GMC’s new guidance, will raise the bar and make absolutely clear what we expect of all surgeons working in the private sector.’
The message to surgeons and doctors working in the cosmetic surgery industry was simple – if they were not working to the new surgical standards, they should not be treating patients at all.
A new RCS certification scheme later this year aims to allow patients to more easily search for a surgeon who has the necessary skills and experience to perform the procedure they are considering.
Consultant plastic surgeon Mr Douglas McGeorge said the British Association of Aesthetic Plastic Surgeons (BAAPS) welcomed both sets of guidelines as a step forward to establishing basic care standards for aesthetic procedures.
He added: ‘We look forward to advancing the process of enforcement of these guidelines, so that all patients will be properly counselled and treated: able to make informed decisions about their healthcare – without being pressurised by unscrupulous practitioners and financial inducements.’
Sally Taber, director of the quality assurance mark Treatments You Can Trust, said she hoped the
Make sure you are appropriately trained and experienced to practise safely
Ensure the patient receives information about the risks and benefits of each procedure
Consider what risks this particular patient might need or want to know and ensure the patient has understood these
Document very thoroughly the consent process
Ensure patients have adequate time to reach an informed decision and seek expert psychological input where appropriate
Keep records of your outcomes for appraisal purposes
For surgeons implanting prostheses, develop a records system that enables the identification of affected patients, should a patient safety issue arise
Ensure advertising literature does not create unrealistic expectations
Keep your defence body informed about the type of work you are carrying out so that it can ensure you are appropriately indemnified
Source: MDU
‘excellent’ GMC document would be translated, where appropriate, by the Nursing and Midwifery Council and the General Dental Council for their registrants.
The GMC is currently developing a guide for patients considering cosmetic procedures, which will advise them on things to consider and the questions they should ask their doctor.
Detailed guidance for doctors carrying out cosmetic procedures is available at www.gmcuk.org/ cosmetic.
By a staff reporter
The NHS is putting the final touches to a new private patient outpatient and diagnostic facility in the Harley Street enclave.
Heart and lung specialists the Royal Brompton and Harefield Hospitals hope to open the centre in the next few weeks.
A spokesman said the development, at 77-78 Wimpole Street ( pictured right ), had been a challenging project, which has seen the refurbishment of a part newbuild and part-existing listed building from office use to an innovative medical facility.
The conversion has expanded and strengthened the building’s infrastructure while having to stick
to its listed building restrictions.
A key milestone was reached with the successful delivery of 5 tone MRI and PET CT scanners, which were craned in via the building’s atrium.
Once complete, 77-78 Wimpole Street will feature a suite of diagnostics including the trust’s first Rubidium PET-CT/CT scanner.
Diagnostics will include:
MRI – cardiac and general;
ET-CT – cardiac, oncological and neurological;
CT – cardiac, lung and general;
Echocardiography, including stress and contrast;
Non-invasive cardiology: ECG, exercise tolerance tests and cardiac monitoring;
Lung function and chest X-ray;
Consultants from the trust will extend their practice to the facility, along with a range of other specialists, to offer a complete multi-disciplinary approach.
When the facility opens, it will offer same-day and short-notice appointments from Monday to Saturday with rapid diagnostics and consultations all available at the one location.
General manager at Wimpole Street, Zohreh Palmer, said: ‘Royal Brompton and Harefield Hospital’s leading cardiac and respiratory specialists will be working with us and we are committed to delivering the world-class centre of excellence that our hospitals are known for.
‘We look forward to working closely with the medical profes -
sionals in the area and will offer a flexible, friendly and professional approach to provide the services and care they require.’
Independent Practitioner Today revealed the NHS’s move into the private care sector’s ‘homeland’ 13 months ago. A spokesman said then: ‘There are collaborations in the works with other local healthcare providers, as well as plans to build upon existing relationships with the local GPs, embassies and businesses in the area. More information will be available on these closer to launch.’
Royal Brompton and Harefield Hospitals’ Specialist Private Care provides private care at what is the largest specialist heart and lung centre in the UK.
Independent practitioners and hospitals are promised a quicker and easier process for submitting e-bills for patients with a VitalityHealth policy following the insurer’s investment in Healthcode’s membership inquiry and enhanced bill validation services.
The UK’s official clearing company for electronic bills said providers can now use the secure online service to instantly confirm that a patient is a member of a valid scheme and request their policy details – a check that previously took up to 24 hours.
This is complemented by Healthcode’s enhanced clearing service which adds a layer of intelligence to the validation process, ensuring that only bills for positively identified VitalityHealth members are submitted to the insurer.
Any typographical anomalies between the details recorded by the provider and those stored by VitalityHealth will be automatically amended.
Healthcode said the new services will increase the first-time pass rate for invoices and ensure submitted bills are accurate, eliminating the queries which can delay payment.
Ryan Murray, head of hospital services at VitalityHealth called the Healthcode services ‘a great investment’.
He added: ‘By improving the billing submission process, our providers will reduce administration time and expedite payment processing. At the same time, the membership inquiry service means patients, consultants or the hospital provider can be instantly reassured the patient has an active VitalityHealth policy in force.’ Healthcode managing director Peter Connor said: ‘When invoices are submitted with the incorrect membership number or patient address details, it is frustrating for all concerned and can also be upsetting for patients who need clarity about their treatment funding.’


Independent research for the GMC has found that four out of ten doctors are changing their practice as a result of their last appraisal.
The findings are from an interim report from a UK-wide collaboration of researchers, known as UMbRELLA, led by Plymouth University.
It is based on a survey completed by more than 26,000 doctors (16% response rate) along with hundreds of Responsible Officers and feedback from patient and public representatives.
A further revalidation report has been published by a collaboration of the Universities of Manchester, Plymouth and York on behalf of the Department of Health in England. The report sets out the findings of an online survey of Responsible Officers.
It concludes that revalidation has had important impacts on medical performance and identifies areas where the process could be made more effective.
GMC chief executive Niall Dickson said the findings from both reports showed revalidation
was starting to have an impact, but they highlighted issues which showed the system could be improved.
He added: ‘We want revalidation to be a positive experience and we want to maximise how it can contribute to high-quality and safer care.
‘At the same time, we fully understand the pressures that doctors are under and the different context they are working in. We will be taking all this into account as we work with others to shape the future of revalidation.’

Findings from report include:
Around a third of doctors said revalidation has improved the appraisal process.
More than 40% of doctors believe appraisals are effective in helping them to improve their clinical practice. Less than a third disagreed.
Doctors in some specialties –such as anaesthetics, psychiatry and emergency medicine – struggle to collect patient feedback.
Doctors who obtained patient feedback found it is the most helpful infor mation to support reflection on their practice.
‘We fully understand the pressures that doctors are under’ Niall Dickson, GMC chief executive Independent Practitioner Today is your vital resource! To see previous editions, as well as the articles featured in this month’s journal, sign up today to become a subscriber
Subscriptions cost only £75 if you use direct debit for our annual ten issues a year – and you will then have access to a library of useful articles to help you. You will find many of the answers to the questions you are asking are just waiting to be read!
To subscribe, use the form on page 28, phone 01752 312140, email lisa@marketingcentre.co.uk or go to our website at www.independent-practitioner-today.co.uk



Are you really doing the job you do best? That you enjoy most?
For 18 years we’ve helped large and small healthcare organisations across the world transform, grow, and improve the way they manage their businesses. Making your life better. And your patients.



While you concentrate on caring for your patients, our role is to help remove the yoke of management.
Not just the day-to-day logistics, but strategically, short and long term. Over the years we’ve transformed and grown countless practices and business. Planning and developing medical facilities. Marketing your healthcare services professionally, by knowing and employing the technology and media that deliver results.


Our teams are tailored to your needs. And if those needs change, so does our team. We have crisis management experts available 24 x 7. We combine clinical expertise with commercial sense and experience. We see the full picture, providing support when and where you need it most.
We work with both public and private sector healthcare providers. Our case histories in operations management, clinical advice, consultancy and development are outstanding.
To give it a thorough examination, call Peter Goddard on +44 (0)203 356 9699 or mobile +44 (0)780 314 4954
www.worldwidehealthcare.co.uk
Q I am looking to wind down my private practice. What would you advise?
Accountant Susan Hutter (pictured right) says:
MANY OF you will know that Independent Practitioner Today often looks at the issue of how to expand your practice and what trading vehicle should be used.
But it is useful to also know about the opposite end of the spectrum – where a consultant is still working but wishes to start winding down.
Many consultants come to a point in their careers where they either wind down their NHS commitments, or retire from them, but are not yet ready to retire from private practice.
Often they may wish to continue performing operations or taking clinics, but do wish to continue with the wider, commercial side of their practice.
In these circumstances, as their income is reducing, the consultant will normally need access to their profits in their entirety and therefore sheltering them within a limited company structure is no longer useful.
The tax advantages of a limited company are effectively erased when all the profit earned needs to be drawn out for living expenses. At that stage, the expense of having a limited company and all the compliance that it entails is no longer worth it. There are two main ways of closing a company down.
As long as all debts have been settled, the company can prepare final accounts and apply for an informal striking off at Companies House and also with HM Revenue and Customs.
What normally happens is that, after all debts are settled, there is a sum of money left in the firm’s

bank account. This can be drawn out by the consultant as an income distribution – i.e. a dividend.
The dividend will then be subject to income tax and taxed depending on the consultant’s marginal tax rate. If the consultant is a basicrate taxpayer, then no extra tax will be due.
If they are a 40% taxpayer, the effective rate of tax on the dividend is 25% and 30.56% for a 45% taxpayer.
However, there may be a tax advantage of having a formal liquidation whereby a licensed insolvency practitioner will be required to carry out a member’s voluntary liquidation in order to close the company down.
The advantage of doing this is that monies left in the company’s bank account, post liquidation, to be drawn by the consultant will be regarded as a capital distribution as opposed to an income distribution.
In these circumstances, providing that the company is a qualifying trading company, the rate of capital gains tax will only be at 10%.
If it is not a qualifying trading company, the rate of tax is 28%.
The company accountant will be able to advise here.
One would therefore have to carry out a fairly simple calculation to decide whether or not the cost of the liquidation is outweighed by the tax saving. Depending on the complexity of

the liquidation, one would be looking at fees of between £4,000 and £6,000 including VAT. There is no detrimental effect to the consultant in either of these methods, because one is not looking at an insolvency situation, merely a voluntary liquidation. Therefore, for example, the consultant would not be precluded from being a company director in the future or having another company. The closure is merely an administrative task.
Whichever way the company is closed down, immediately after closure, the consultant will become a sole trader and all income, less expenses, of the private practice will need to be entered on the personal tax return and income tax will have to be paid.
One would lose the potential tax advantages of research and development tax credits and also raising money from third parties in a tax efficient manner under the Enterprise Investment Scheme (EIS). Therefore, this course of action should only be taken towards the end of the consultant’s career or if they have taken a decision that they do not wish to develop their private practice.
Post liquidation, accountancy fees would be reduced, as a limited company’s accounts would not have to be prepared together with all the paperwork that goes with it. Generally, life becomes simpler from a financial point of view. As always with these situations, professional advice should be taken.
Susan Hutter is a specialist accountant for the medical profession and a partner at Shelley Stock Hutter

ESMYA® is the first medical treatment for the long-term management of moderate to severe symptoms of uterine fibroids.1

O Licensed for intermittent use1
O Fast, reliable and sustained control of bleeding2
O Significant and sustained reductions in fibroid volume from baseline2
PRESCRIBING INFORMATION
Esmya (ulipristal acetate) Please refer to the SmPC before prescribing. Presentation: 5mg tablet. Indication: Pre-operative or intermittent treatment of moderate to severe symptoms of uterine fibroids in adult women of reproductive age. Dose and administration: One tablet of 5mg to be taken orally once a day for a maximum of 3 months, starting during first week of menstrual cycle. This 3 month treatment course can be repeated. Re-treatment courses should start at the earliest during the first week of the second menstruation following the previous treatment course completion. Each treatment course should not exceed 3 months. Treatment free intervals are required between courses. Repeated intermittent treatment has been studied for up to 4 intermittent treatment courses. Please refer to SmPC for missed dose information. Patients with renal or hepatic impairment: No dose adjustment in mild to moderate renal impairment or mild hepatic impairment. Not recommended for patients with severe renal impairment and moderate or severe hepatic impairment unless patient is closely monitored. Children and adolescent under 18 years: No relevant use. Contraindications: Pregnancy, Breastfeeding, Genital bleeding of unknown aetiology. Uterine, Cervical, Ovarian or Breast cancer. Hypersensitivity to active substance or any excipients. Pregnancy and lactation: Contraindicated during pregnancy and lactation. Warnings and Precautions: Should only be prescribed after careful diagnosis and pregnancy should be precluded prior to treatment. Use in women with severe asthma insufficiently controlled by oral glucocorticoids is not recommended. Concomitant use of hormonal contraceptives are not recommended hence a non-hormonal contraceptive method should be used. Reversible histological changes of the endometrium: ‘Progesterone Receptor Modulator Associated Endometrial Changes’ (PAEC) may be observed in patients. Also, reversible thickening of the
endometrium may occur during treatment. If it persists beyond 3 months following the end of treatment and return of menstruations, and/or an altered bleeding pattern is noted, this may need to be investigated as per usual clinical practice. Please refer to SmPC for further details on endometrial changes and management of the same. In case of repeated intermittent treatment, periodic monitoring of the endometrium is recommended. This includes an annual ultrasound to be performed after resumption of menstruation during off-treatment period. Treatment leads to significant reduction in menstrual blood loss within 10 days and patients should notify their physician if heavy bleeding persists. Drug interactions: Hormonal contraceptives and progestogens are likely to reduce the efficacy of ulipristal acetate by competitive action on progesterone receptors, hence co-administration is not recommended. Not recommended for patients receiving moderate or potent CYP3A4 inhibitors or potent CYP3A4 inducers (e.g. rifampicin, carbamazepine, phenytoin, St John’s wort). Co-administration of P-gp substrates (e.g. dabigatran etexilate, digoxin) should be separated in time by at least 1.5 hours. Undesirable effects: The following adverse reactions have been reported during first treatment courses: Very Common (>1/10) Amenorrhea, Endometrial thickening; Common (>1/100 to <1/10) Headache, Vertigo, Abdominal pain, Nausea, Acne, Musculoskeletal pain, Hot flush, Pelvic pain, Ovarian cyst, Breast tenderness/pain, Fatigue, Weight gain.; Uncommon (>1/1000 to <1/100) Anxiety, Emotional disorder, Dizziness, Dry mouth, Constipation, Alopecia, Dry skin, Hyperhidrosis, Back pain, Urinary incontinence, Uterine haemorrhage, Metrorrhagia, Genital discharge, Breast discomfort, Oedema, Asthenia, Increase in cholesterol level Increased triglycerides, Rare (≥1/10,000 to <1/1,000) Epistaxis, Dyspepsia, Flatulence, Rupture of ovarian cyst, Breast swelling. When comparing repeated treatment courses, overall adverse reaction rates were less frequent in subsequent
O Improved quality of life compared to baseline2
O Well-tolerated2
treatment courses than during the first one and each adverse reaction was less frequent or remained in the same frequency category (except dyspepsia which was classified as uncommon). Overdose: Limited experience. Single doses of up to 200mg and daily doses of 50mg for 10 consecutive days administered to a limited number of subjects, and no severe or serious adverse reactions were reported. Special precautions for storage: Keep the blisters in the outer carton to protect from light. Legal Category: POM Basic UK NHS cost: £114.13 per pack of 28 tabs. Marketing Authorisation Numbers: EU/1/12/750/001, EU/1/12/750/002, EU/1/12/750/003, EU/1/12/750/004, EU/1/12/750/005. Marketing Authorisation Holder: Gedeon Richter Plc., Gyömrői út 19-21., 1103 Budapest, Hungary. Further information is available from: Gedeon Richter UK Ltd, 127 Shirland Road, London W9 2EP. Tel: 0207 604 8800. Email: info.uk@gedeonrichter.eu Date of Authorisation: 27th of May 2015. Date of Preparation: 16th of June 2015.
Adverse events should be reported. Reporting forms and information can be found at www.mhra.gov.uk/yellowcard. Adverse events should also be reported to Women’s Health Division of Gedeon Richter (UK) Ltd on 0207 604 8806 or drugsafety.uk@gedeonrichter.eu
References 1. ESMYA® SmPC. May 2015. 2. Donnez, J; Hudecek, R; Donnez, 0, et al. Efficacy and safety of repeated use of ulipristal acetate in uterine fibroids. Fertil Steril 2015; 103(2):519-27.

The right staff are critical to your success. Pam Underdown explains why the team you surround yourself with can make or break your business, how to find the right teamplayers and ensure they produce a consistent experience for patients every time they visit
SETTING UP the right team to represent your medical aesthetic practice is imperative to the success of your business.
The team you surround yourself with can make or break your practice. Getting the right team players on board is difficult and ever-changing, but vital to your success.
Many aesthetic practitioners have challenges with their staff, who:
Do not care about the practice as much as they do – for many, it’s just a job;
Are not converting prospective patients into paying patients – in fact, some even chase patients away;
Do not know how to promote the practitioner or the practice as the best choice to the patients. So, do you have the right team in place? And, do they know their main job is to promote you and your aesthetic services and that starts with impeccable patient service?
If a member of your team always goes the extra mile, they need to know that they are supported, listened to, respected and valued
It’s imperative every team member who works for you knows exactly what is expected of them. What if they aren’t pulling their weight? Are they going off sick all the time?
Perhaps targets aren’t being met or some team members aren’t upselling like they should be?
Maybe you have even heard the odd story from one or two patients who said that staff are sending them elsewhere when they know there is a better deal on?
Always complaining
Some team members always seem to have something to complain about: not being paid enough, targets too high, prices too high, not being valued enough – aka ‘the grass is always greener on the other side’ syndrome.
On the flip side, you know the team members you do wish to have on board. They are the first to arrive – except for you – the last to leave and the last to take a
lunch if someone else is not running on time.
They are responsible for their own schedule, the first to work hard to fill in gaps, the first to hear the stress when a practitioner is too busy, they are responsible for all paperwork, they can operate all of the systems easily and they always have a smile on them, no matter how busy they are.
If a member of your team always goes the extra mile, they need to know that they are supported, listened to, respected and valued. Let them know you appreciate them and make sure that you thank them for doing their job well.
All of this acknowledgement and praise is essential for a happy, productive environment both for your team and your patients. Remember, your patients deserve a calm, friendly and stress-free environment and are the first to pick up on the atmosphere if it doesn’t feel right.


The whole team should acknowledge just how important the front desk position is. They are usually receiving the lowest pay but the highest amount of pressure
Where can you find the right team players? Good candidates are everywhere that good service is provided. Look for new receptionists or patient co-ordinators at a high-end restaurant you dine at, at your exclusive hair salon, retail boutiques, the department store cosmetic counter or anywhere else where quality services and products are sold.
Talk with the well-groomed, well-trained staff that understand the importance of awesome patient service and find out if they are interested in making a change. They have already demonstrated they know how to treat customers, so they are most likely going to treat your aesthetic patients with the same quality service.
It can take a lot of time and money to train the right person to fit into a front-desk position. Train them correctly and encourage their growth. It is hard work at the front desk – hearing other staff laughing and talking to each other and feeling like they are too busy to take part.
The whole team should acknowledge and understand just how important the front desk position is. They are usually receiving the lowest pay but the highest amount of pressure.
The Disney factor
So how can you keep loyal staff members? Let us refer to an example of an organisation that I have spoken about before in a previous article. This is one that not only looks after its ‘guests’ but also its employees so well that they are some of the most loyal in the world: The Walt Disney Company.
Disney executives believe in MBWA or ‘Management by Walking Around’ and are commonly seen walking around the rides and exhibits, talking to the guests and the employees. They ask questions and they find solutions to make everyone’s experience, including that of the employees, a positive one.
Everyone at Disney is on a firstname basis and they wear only their first names on their uniforms. It is in the training manual that all employees are to wear their name tags at all times.
When Michael Eisner was in charge of Disney, if he was noted
not to have his name tag on while walking in the park or ‘on stage’, he was reminded by one of the employees that he was ‘out of uniform’. At Disney there is no double standard. Everyone, even Michael Eisner, had to follow the rules.
Disney believes that extensive training of the cast members is a key to the employee commitment to quality and pride. Every new employee including the street sweepers have intensive training before he or she is considered ready to ‘go on stage’ in front of the guests.
All cast members know where every attraction is, when it starts, and how long the waiting time is. It all gets back to the Disney philosophy of friendly, smiling cast members who are always ready to help you and make your Disney experience a memorable one.
Disney managers and executives have recognised the necessity of knowing what their guests are experiencing, thinking, seeing, touching and smelling.
Which is why every executive and middle manager will spend several days each year as a cast member to understand the feelings of both the front-line cast members and the guests.
What lessons can your practice borrow from Disney? First, Disney leads by example. Most Disney executives come from within or from the bottom up. Disney has a rigorous selection process for all its employees. No one is selected after a single interview.
Employees that don’t work out in the job they were given are seldom dismissed. Disney assumes the person was right but the job was wrong and they are retrained for another position.
Those employees that do a good job are promoted within the organisation. Consequently, Disney reports one of the lowest employee turnover rates in the entertainment industry.
Make sure your employment process is also very selective. Ensure that every applicant watches a video on the philosophy of your business and the expectations for all the employees. When some candidates learn about the dress code and the team
Disney believes that extensive training of the cast members is a key to the employee commitment to quality and pride










HMRC tax investigations and disputes create difficult and stressful times.
As an award winning firm of tax experts, our highly experienced partners specialise in resolving problems relating to tax investigations and disputes with HMRC.
To find out, in confidence, how we can help call 0800 734 3333.
‘Here to help. Not to judge.’

Here are the most common reasons why your staff may move on:
Lack of recognition and appreciation (huge one)
Lack of communication (another huge one)
Lack of leadership and vision from the management
They don’t feel part of the team and feel isolated
They are not getting along with other staff
They lack clear job descriptions and expectations
Their work doesn’t feel meaningful
They feel as though they are not contributing and don’t feel valued
Feeling stressed and overworked
Higher salaries and benefits elsewhere
There’s no career path/training: they feel they’re not going anywhere

Newly renovated, furnished, two-bedroom flat with two bathrooms available to rent.
The artist-designed flat (visible in picture above) with spectacular views overlooking the old port, five minutes’ walk from centre of town offers:
l Spacious living room l Wifi internet
l Dining room l TV
l Modern kitchen l Balcony
l Lift l Beaches
l Easy public transport to l Flower, vegetable and fruit Antibes, Nice, MonteCarlo markets nearby
Contact: Ninafromkaur@hotmail.com
member philosophy, they may not pursue their application any further, as it may not be right for them.
One of the most important things that contributes to the success of any top-performing practice is the ability to transform all of the right staff into a dream team of ‘A’ players.
Strong leadership
It all starts with a strong vision of leadership. However, there is an important difference between ‘leadership’ and ‘management’. Management is a bottom-line focus: How can I best accomplish certain things? Leadership deals with the top line: What is the outcome? What are the things I want to accomplish?
In the words of business expert Peter Drucker: ‘Management is doing things right; leadership is doing the right things.’ If you are ‘managing’ the people who work for you, then you only have ‘staff’.
But if you provide leadership and vision, then your team gets aligned with your purpose. They will love working for you and making your business a success, because they know it will affect their lives as well.
There are times when your staff may burn out from overbooked scheduling and demanding patients, so it’s easy for them to feel overworked and under-appreciated when working at a fastpaced, busy practice.
Rather than deal with their leaving and you scrambling to replace them, which is costly and time-consuming, you need to do everything you can to keep hold of the best team members by preventing problems before they get to that level.
Here are a few strategies that work:
1
Hold staff lunch meetings. Once a month (weekly is better), have lunch catered in and get
your staff together for a fun meeting. Talk about what’s going well, what could be better and open it up for suggestions on how to turn your practice into the best of its kind. Staff will perform better when they are part of the team and you listen and hear them and their suggestions.
2
Work as a team – celebrate as a team. You want staff to share fun memories with each other and not just see each other as colleagues in a busy, stressful environment where there is no time to chat and relax.
At least once a year, hold your annual staff party where they can let down their hair.
3
Finding good people is only half the battle. The other half is retaining them. Building a high-performing team starts with goals, roles and reviews. However, they are looking for leadership and encouragement from you. Keep it simple. Tell them what you expect from them, give them the training they need, listen to their input, give them goals to strive for, make them feel part of the team and, by all means, show your appreciation.
4 Say ‘thank you’. A simple thing to do that carries a lot of weight is to say ‘thank you’ every night to every team member as they walk out the door. If you do this, you’ll have a better chance of them walking through the door again in the morning.
5
Conduct an anonymous staff survey to really find out what your team enjoy or don’t enjoy about working at your practice. Ask for ideas and input about improvements and then get everyone involved to ensure buy-in and engagement.
Pamela Underdown (right) is chief executive at Aesthetic Business Transformations



In a crowded market, it’s often the little things that have the biggest impact.
So if you want to stand out from your competitors, a focus on client service could be the key. Stephanie Vaughan-Jones (right) looks at what constitutes gold-standard service and why it has never been more important to provide it
COMPETITION AMONG practices is on the rise. In the UK, there is an increasing demand for cosmetic procedures alone.
One recent report suggested surgical aesthetic enhancement has increased by 13% since 2014. And it seems the UK’s affiliation with cosmetic surgery has not yet reached its peak, with the number of men seeking procedures increasing too.
This growth in client demand is not only driving competition in cosmetic clinics, but also throwing a spotlight on private practices.
The result? Clinics across the industry are recognising the need to stand out from the crowd. The need to go that extra mile in order to truly ‘wow’ their clients.
So if you haven’t already done so, now is the perfect opportunity to take stock of your own customer service. Look at everything objectively as if you were a client seeing your practice for the first time.
While there is no definite right or wrong, there are without doubt a number of key factors that form the basis for any first-class customer experience.
So, here are key elements that help create this ‘gold standard’ service:
1Above and beyond the industry standard
Some may ask: ‘Isn’t “standard” good enough?’
Well, think of it from a patientperspective and the answer is simple – no. Imagine you were buying a new car and had a choice of two dealerships: one of which was friendly, efficient and helpful, and one of which didn’t even pick up the phone.

Whom would you choose? I certainly know where I’d take my custom.
From the second a client makes an initial inquiry, they will already be expecting a certain level of service. It is up to you to meet and exceed this.
In a consumers’ market, the onus is on the business to win the client over – not the other way around.
The rewards of great service, however, are there to be reaped. Word quickly spreads about
➱ p22
remarkable service – and this is worth its weight in gold.
Clinics that raise the bar are inevitably the ones that rise to the top. Not only do they exceed their own expectations of what constitutes good service – but also the industry’s standard. This can be hugely powerful.
So take time to think about those extra things you could do. for instance:
Remembering patients’ names when they call;
Using their preferred method of communication;
Addressing with time and care any reservations they may have.
Aim to surprise and delight clients at every opportunity; make them feel nurtured and special.
It is more often than not the little touches that inspire customers to share their experience with others. By going above and beyond, you aren’t just impressing one client, but an infinite
By going above and beyond, you aren’t just impressing one client, but an infinite number of potential clients in the future
number of potential clients in the future.
Provide consistency at every touchpoint
Like many things in life, good things come to those who wait. That includes winning the trust of your customers. It can take four, five, maybe even ten or 20 positive encounters with a company before a consumer begins to trust them.
The smartest business-people understand this. They know that customer service is a long game; that the benefits are not apparent overnight, but that building loyalty and strong client relations is the key to success.
They also know that relationships like these are crafted through steady and unwavering service at every touchpoint. Be it the way a client is greeted at the front desk, how quickly emails are answered or the way the phone is answered.
Think of your own practice and how it is run day to day – and then ask yourself the following questions:
Is the level of service you offer the same at every point of contact?
How does this represent your practice as a brand?
Is every patient greeted at the front desk like they are your most important client?
Is there someone available to always answer the telephone, with a bright and helpful manner?
Do you answer your patients’ queries within a working day or suggest a time when you will get back to them?
If the answer is not yes, then it may be time to consider ways you can improve each element. It is this consistency and reliability that fosters trust and helps form long-lasting bonds between a client and business.

The benefits of excellent customer service won’t become apparent overnight, but building loyalty and strong client relations are worth their weight in gold.
This trust is equally important when it comes to current or existing customers as well.
At no point should a client ever walk away thinking ‘that wasn’t my usual standard of service’. It takes time to earn a person’s hardwon loyalty, so treasure it and do everything you can not to lose it.
Carefully cultivating a culture which puts people’s happiness above all is an essential part of any successful business.
For it to really be effective, though, this ‘people first’ focus has to be at the heart of everything you do; not simply an addon or afterthought.
When Ed Reeves and Rachel
Clacher founded Moneypenny 16 years ago, there were two things they were absolutely sure of. The first was creating a company they would like to work for themselves, and the second was creating a company they would like to do business with.
These two simple sentiments have since shaped everything they’ve done; and little did they realise it at the time, but this was the most powerful decision they could have made.
Why? Study after study shows happy staff are more likely to deliver good customer service and create happy customers. Happy customers are more likely to be loyal customers; and loyal customers are extremely valuable.
Happy staff are also more likely to stay in their jobs for longer, honing their role and making clients even happier. It’s a virtuous circle.
Thinking in this way also
Study after study shows happy staff are more likely to deliver good customer service and create happy customers
encourages you as a business owner to consider whether you are putting your clients first.
Ask yourself whether you would want to be a patient at your clinic? Is it easy to arrange a consultation? Can patients speak to someone if they need advice or reassurance?
Or are they greeted by an engaged tone and voicemail and left feeling disappointed?
What is their experience like when they arrive for an appointment? Is your post-treatment care the best it can be?
Seeing the clinic from a patient’s point of view will sharpen your focus and shed light on any areas that may need improvement.
Put people first and success will follow. It is the absolute golden rule of customer service.
Stephanie Vaughan-Jones is channel manager at telephone answering specialist Moneypenny

BY ROBOT
Prof Keyoumars Ashkan of the London Neurosurgery Partnership talks to Leslie Berry about the developments in neurosurgery, including The Harley Street Clinic’s latest acquisition – the ROSA Robot

BY ITS nature, dealing with the most delicate structures – namely the brain and spine – neurosurgery is heavily reliant on technology to achieve the best outcomes with the least risks to the patients.
Modern tools allow neurosurgeons to perform operations unthinkable even 50 years ago, and the field continues to advance.
Neurosurgeons of the London Neurosurgery Partnership, a group of 11 subspecialist neurosurgeons at The Harley Street Clinic, have been proactive to provide access to the state-of-the art technology at the clinic.
One of them, Prof Keyoumars Ashkan, is particularly excited by the range of tools now available to treat patients with brain tumours.
He says: ‘Removing brain tumours remains one of the biggest challenges in neurosurgery to maximise the extent of resection while protecting patients against any deficits.
‘We now have access to a spe-
The ability to perform intraoperative navigation has been one of the most important recent advances in brain tumour surgery

cialist microscope at The Harley Street Clinic, which allows resection of tumours labelled with a fluorescent dye, helping to distinguish normal brain tissue from the tumour; something that is often otherwise hard to do.
‘For those tumours in close proximity to the motor and speech areas, we are now equipped to offer awake surgery with intraoperative neurophysiological monitoring, again increasing the surgeon’s confidence to remove tumours as safely as possible.’
In his view, the ability to perform intra-operative navigation has been one of the most important recent advances in brain tumour surgery, essentially allowing fusion of a patient’s MRI images with their anatomy on the operative table to guide surgery.
The technique allows for more accurate surgery, smaller openings and therefore faster healing.
He says surgeons at the clinic have had access to modern navi-
We were among the first to offer a truly multidisciplinary team approach to the management of patients with brain tumours in the private sector
ROSA’s arm is designed to reproduce the movements of a human arm
gation machines, such as the Stealth system, but what is really exciting is the recent acquisition of a ROSA Robot.
This combines ultra-modern navigation technology with a robotic arm. The navigation component acts as a ‘GPS’ of the brain, utilising a unique laser-based registration system to allow highly accurate surgical planning based on a patient’s images. Its arm, designed to reproduce the movements of a human arm, gives surgeons great dexterity of movement and complete freedom in the choice of trajectory when navigating in the brain.
Prof Ashkan explains: ‘The ROSA Robot allows for precise and safe navigation of the patient’s brain anatomy. It also speeds up the whole surgical process and the reduced operative time is likely to translate into safer surgery, less time under anaesthetic and lower infection risk.’
ROSA Robot can also be used for
any neurosurgical procedure requiring safe access, particularly to deep brain structures.
In deep brain stimulation surgery, electrodes are placed accurately in structures deep in the brain to treat a range of conditions. These include Parkinson’s disease, tremor, dystonia or intractable pain and surgery for epileptic patients whose seizures are difficult to treat with medications.
Prof Ashkan adds: ‘Although referral to a neurosurgeon immediately triggers one to think about surgery, at London Neurosurgery
Partnership we are committed to a holistic approach to patient care, always considering alternative therapies to surgery when appropriate.
‘For example, by virtue of being Cyberknife-trained, I offer this form of focused radiation therapy to many of my patients at the clinic when deemed a better option than surgery.’
He believes the biggest strength at the clinic is its multidisciplinary team philosophy of care.
‘We were among the first to offer a truly multidisciplinary team approach to the manage -
ment of patients with brain tumours in the private sector, with regular meetings to discuss our patients and decide on the optimum management plan. Indeed, teamwork is an essence of London Neurosurgery Partnership, underpinning its very formation over five years ago.’
Prof Ashkan is professor of Neurosurgery at the London Neurosurgery Partnership and King’s Health Partners. He specialises in the treatment of brain tumours, movement disorders, intractable pain and spine disease
“Kay and her team provide a seamless outsourced switchboard service. The result? More enquiries, outstanding service levels.”
Moneypenny will support your existing team by looking after overflow calls, or by providing a fully outsourced switchboard facility. moneypenny.co.uk 0333 202 1005
London Neurosurgery Partnership is the conglomeration of 11 subspecialist neurosurgeons in London, who offer the full spectrum of cutting-edge neurosurgical expertise to treat patients with brain and spine disease.
For referrals, contact Dianne Johnston on 020 7034 8707 or email her at dianne.johnston@ hcahealthcare.co.uk.
For more information about Neuroscience at The Harley Street Clinic and The London Neurosurgery Partnership, visit http://theharleystreetclinic. com/neurosciences.

Doctor entrepreneurs can act on their inspirations – or put them to sleep. Julia Laflin tells the story of an award-winning invention from an anaesthetist

IT’S ONE thing to have a great idea but quite another to turn your notion into meaningful reality.
Dr Peter Brooks, consultant anaesthetist at the Bupa Cromwell Hospital and also Chelsea and Westminster NHS Foundation Trust, together with colleague Dr Corina Lee, knew they wanted a tool to calm and distract children before anaesthesia.
Their persistence, together with right delivery partnership, resulted in the creation of the double award-winning RELAX Anaesthetics tablet.
Explains Dr Brooks: ‘We wanted to improve the experience of young patients and their parents in the anaesthetic room for everyone’s benefit.
‘The thought of needle procedures can be terrifying for children and dealing with their anxiety levels can considerably prolong the time it takes to insert a cannula. In many cases, attempts at intravenous access has to be abandoned and inhalational induction used instead.’
The doctors knew that tabletbased games, to a certain extent, diverted children’s attention away from needle procedures.
But using their own devices or those belonging to the child or their parents had significant limitations.
It took too long to select games that were appropriate or appealing to the child’s age or gender. And often the games were too long and involved.
But, most importantly, when the patient’s or parent’s own tablets or mobiles were used, this detracted from the interaction
between the anaesthetist and the child, which was key to the clinician reaching the desired procedural outcome.
Recognising that there was no easy way to organise a limited number of gaming and other apps and segment them into age and gender selections, they put in an application for funding, support and development for their idea to hospital charity CW+’s Enterprising Health innovation initiative.
Dr Brooks says: ‘CW+ is in a creative and co-funding partnership with Imagineear, a company with a successful three-year trackrecord in digital healthcare provision. With funding and development provided from the charity and Imagineear, RELAX Anaesthetics was soon ready for trials in paediatric theatres at Chelsea and Westminster.
Charity support
‘It was helpful to work with the charity, whose focus is on patient care, and with Imagineear, who have already developed a number of well-received digital reference and training tools for clinicians and condition self-management tools for patients.
‘The time-frame and successful creation of RELAX Anaesthetics could have been compromised if we’d had to apply for full funding or worked with a digital start-up company.
‘I know that digital healthcare can be a graveyard for good concepts that have been poorly executed or hit unsurmountable stumbling blocks in their development if the roadmap was flawed in the first place. But I was able to be confident about the whole process from an early stage.’

We wanted to improve the experience of young patients and their parents in the anaesthetic room for everyone’s benefit
The technical build, from idea initiation to prototype, took two months. RELAX Anaesthetics is provided on an Android tablet and includes art and music distractions as well as third-party games that are quick to access and engage with.
Its design includes the ability to capture anonymised data on usage, including the length of each interaction and the type of application used for distraction.
Dr Brooks continues: ‘The time spent in the anaesthetic room and the method of induction used will impact on theatre efficiency and drug costs. But of greater importance, we want to improve the child and parent’s experience and offer patient-centred care.
‘Controlled trials at Chelsea and Westminster by Dr Lee and my colleagues have proved this. For example, six-year-old Rosa needs multiple operations. The previous time she was in the anaesthetics
room, she was petrified and it took an hour and a half to get her to sleep. For her latest procedure, we used the RELAX tablet and it took just four minutes.’
RELAX Anaesthetics beat 340 contenders to be an NHS England Innovation Acorn Challenge Award winner in 2015 for small ideas that make a big difference.
Last January, it won the Association of Anaesthetists of Great Britain and Ireland’s award for Innovation in Anaesthesia, Critical Care and Pain 2016.
Dr Brooks says the tablet is attracting interest from hospitals in the private sector around the country, as well as the NHS. And new versions are currently in development.
RELAX Hospital is now being launched for needle procedures on paediatric wards and this is being followed by RELAX GP, which he anticipates will be popular in private practice.
An independent firm offering one to one meetings anywhere in the UK giving advice and help with:

• how to start in private practice
• how to maximise private practice income
• computer software
An independent firm offering one to one meetings anywhere in the UK giving advice and help with:
• tax and financial advice re: car purchases
• how to start in private practice
• ways to reduce tax payments
• computer software
• how to maximise private practice income
• setting up in Chambers/Groups
• ways to reduce tax payments
• limited companies and LLP’s
• setting up in Chambers/Groups
• financial planning
• record keeping
• limited companies and LLP’s


• tax and financial advice re: car purchases
• pensions: NHS, personal and employee schemes
• pensions: NHS, personal and employee schemes
• purchase of consulting rooms and surgeries
• inheritance tax and capital gains tax planning
• purchase of consulting rooms and surgeries
• VAT
• inheritance tax and capital gains tax planning
For more information please contact us by:
• VAT
Wilmslow
Harley Street
For more information please contact us by:
Phone: 01625 527351
Wilmslow
Fax: 01625 539315
Phone: 01625 527351
Phone: 020 7307 8759
Harley Street
Fax: 01625 539315
Phone: 020 7307 8759
Email: info@sandisoneasson.co.uk
Fax: 01625 539315
Fax: 01625 539315
Website: www.sandisoneasson.co.uk
Email: info@sandisoneasson.co.uk
Website: www.sandisoneasson.co.uk
Dear Reader,
Subscribing to Independent Practitioner Today is the only way you can be sure you will see every issue. Don’t risk missing out. Our personal subscription for doctors and managers is only £90 a year and £210 for organisations. But you can cut this to just £75 and £180 respectively if you pay by direct debit.
So take advantage of this offer now for our unique business journal dedicated to supporting you in your private practice. We’re confident your subscription will repay itself many times over!
Editorial director

listed
encose a cheque made payable to The Independent Practitioner Ltd Please debit my Mastercard/Visa/ Amex/Diners
Instructions to your Bank or Building Society to pay Direct Debits

Name and full address of your bank/Building Society Banks and Building Societies may not accept Direct Debit instructions for some types of account
of account holders
Post your application (No postage required – UK only) to: Independent Practitioner Today Subscriptions Department, FREEPOST, PO Box 36, Plymouth, PL1 1BR
at www.independent-practitioner-today.co.uk
If an error is made by The Independent Practitioner Limited or your Bank or Building Society, you are guaranteed a full and immediate refund from your branch of the amount paid.
You can cancel a Direct Debit at any time, by writing to your



He is looking at four different topics aiming to help consultants as they look to build their practice. In March and April, he covered teamwork and choosing a private hospital. In this, his third article, he looks at branding and why this is an important subject in today’s private healthcare marketplace.
Each article is aimed at consultants who may be at different stages of their career.
Whether taking your first steps in private practice or wishing to take the business a stage further, either by yourself or as part of a group, your next step should be to take your branding seriously.

SO MANY people see a brand as a logo and perhaps a website or a leaflet. There are many definitions of what defines a brand, but a simple one to remember is that ‘it is what people say about your company/service when you are not there’. Your brand is who you are, what you stand for and how that information is communicated to others as a total identity.
According to leading agency Brand Finance, powerful brands are those that create a strong, permanent and positive association in people’s minds. Everyone reading this will have inbuilt thoughts – both good and bad – about major UK and international brands that they regularly come into contact with. Brandwatch, another branding agency, says that customer opinion is more influential than ever in determining brand perception. It is because of this that successful
branding is important. OK, I am sure that a group of doctors who team up and decide to brand themselves may not overtake the world’s biggest brands: Apple, Google and Coca-Cola.
But within the niche area of private healthcare, and especially looking at doctors themselves, true branding is in its relative infancy, with only self-pay specialties such as cosmetic surgery having taken the subject seriously.
If branding is understood and enacted more universally in private healthcare, I am sure that real benefits are to be had.
The major private hospitals have all – Nuffield and HCA most recently – been active in their branding and positioning. Drilling down, as a team working in one or more hospitals or even if you are looking to just promote yourself, then I am sure that you would wish your ‘brand’ to be strong.
So what should you do first?
There is one big decision that you have to take at the outset, whether – if your chosen hospital appreciates you enough – to take the easy decision and work entirely under the hospital’s umbrella branding.
Obviously, by following the hospital’s own branding, this is going to be cheaper for you. But you will be tied in and if the hospital’s internal politics change or a new chief executive arrives who is not as positive about your brand as the previous incumbent, then this cheaper choice may, in the medium or longer term, be a mistake.
Also, if you have decided to work in two or more hospitals, you will probably want to look at your own or your team’s individual branding options.
To get your brand off to the right start, you should consider hiring a professional brand/ design/marketing agency. Choose
more than one to consider and listen to what they have to offer.
How many doctors ‘talk the talk’ on brand and marketing and then when it comes to putting out a website, they call in favours from an old friend or family member who ‘does marketing’ and comes up with a design that is off the shelf and does not match the team’s brand attributes?
There is an old saying: ‘You pays your money and you takes your choice’. If you want to create a brand that will help you achieve your goals, you will need to invest.
I said earlier that many people think of branding as just a logo or a website. These marketing essentials should, of course, reflect your image of how you wish to be perceived and are the initial steps in your branding journey.
A good agency will talk through your ideals, your strengths, your plans and your vision.
Your brand also needs to occupy
a position of strength and distinction among your competitors, and together you should agree imagery and a style that will suit you – and your team, if you are part of one.
Use it consistently
It is one thing to develop a strong brand; you then have to ensure that it is used in a consistent manner with everything that you produce. The brand identity should incorporate not just the logo but colours, fonts and the style of bespoke photography that matches the image you are wishing to portray.
To emphasise the point, I was in a Co-operative Bank a couple of days before writing this article. While waiting – and I was only sitting down for ten minutes – two people entered the banking hall separately thinking it was Barclays Bank, which happens to be two doors away.
Was there any coincidence that the Co-operative’s brand colours


























are a very similar blue to that of its competitor? I realise that I have used an example from financial services, but the underlying principles remain the same.
Branding should also – funding permitting – eventually encompass the building you use, the furniture, wallpaper and carpets and even the location of the practice.
From these initial meetings –and there should be at least two or three – the agency can develop a brand that is relevant to you as a team or company and relates in a powerful way to your customers and patients.
One thing to point out early is that branding is not a quick win. A new healthcare brand will take time as well as the investment.
If the brand is not a well-established hospital, it will take longer and cost more money. But if the seeds are sown correctly, then the future should reap rewards for you or your team.

There are four elements of what constitutes a good brand:
The way you talk about your service;
The way you visually represent yourself;
Your environment;
Your behaviour.
These need to be accepted and driven by everyone associated with you and your team. There is another old saying: ‘do as you say and say as you do’, but to be successful at branding, this is what you all have to do.
Just think of the service that you receive at point of sale from your preferred brands and what annoys you about the less favoured ones.
The management of each will say that customer service is ‘top priority’ and yet the good brands get it right from top to bottom.
Whatever a brand thinks about the promises it makes, it is the customer and, in our case, the patient who experiences the reality – and



a conflict between the two can end the association.
The consultant can have an excellent bedside manner, but if the practice manager is unnecessarily rude, then the brand is compromised.
Having taken the team’s brand ethos on board, this would need to be communicated with anyone with whom you are associated professionally.
The development of the brand will be covered in my next and final article in the Practice Builder series: ‘The Marketing Mix’.
But for the brand to succeed, you will need to communicate with your referring GPs (and nonreferrers by means of a mailing and a separate email).
You will also need to communicate with your patients, both one to one and by follow-up and increasingly via social media


updates using Twitter, LinkedIn and possibly Facebook if you are looking at the Middle East market.
Loyal customers are more valuable than ever, but they are more fickle too.
Good branding offers an emotional connection between the practice and patients. From the visit to the website/app or brochure to the first phone call, to the initial visit, to the consultation, each link in the team’s chain needs to buy into your values and without this commitment, your branding will not succeed.
The final instalment next month will look at the marketing mix and how it may benefit your practice
Malcolm McCoskery is a consultant in marketing, whose 20-year private hospital career included senior management posts at four different private hospitals/groups. Email him at: m.mccoskery@yahoo.co.uk

The seca 287 ultrasonic measuring station –defining the essence of technical practicality.
From the fully automated ultrasonic height measurement to the voice guidance system for self-sufficient measurement – the intelligent measurement technology of the seca 287 measuring station makes your everyday work more efficient. All measured data can be comfortably transmitted into an EMR system or printed out using seca 360° wireless technology.
www.seca.com















Abuse of prescribing is being taken very seriously by the GMC and is in the top three areas where doctors are asking for more information. Dr Gail Gilmartin (right) gives some topical advice

Abuse of prescribing is taken very seriously by the GMC because of the adverse consequences for both the doctor and patients

PRESCRIBING IS a complex area and can be the source of a wide range of problems, from simple harmless errors to significant fatal mistakes and serious ethical dilemmas about patient safety. It will hardly come as a surprise to hear that practitioners who abuse prescribing can face erasure from the medical register. Practices must ensure that they have robust systems in place for the issuing and reviewing of prescriptions – particularly for controlled drugs. These should cover all prescriptions, no matter the format or how they are generated. Private practitioners should seek prompt advice from their medical defence organisation if they have concerns about health issues or professional issues relating to mis-prescribing, be it on their own behalf or relating to a colleague.
In the GMC’s latest State of medical education and practice in the UK report (SOMEP), prescribing has been identified as one of the top three areas where doctors seek further information or advice.
While this report focuses on the many and varied questions related to prescribing in general, there is also a clear message about the risks of abusing a prescribing system.
Reference is made to a particular case study involving a hospital doctor fraudulently obtaining prescription-only medicines. He was referred to the GMC after a conviction for stealing prescriptions over eight months, some of which were forged under the
names of non-existent doctors and using the names of non-existent patients.
The doctor explained that this was to treat his own medical condition and acknowledged that his actions were a ‘stupid mistake’ and a ‘one-off’.
But a GMC fitness-to-practise panel concluded that, despite some evidence of insight, his actions were premeditated and prolonged, which indicated an underlying attitude problem that was fundamentally incompatible with being a doctor. He was subsequently erased from the medical register.
Abuse of prescribing is taken very seriously by the GMC because of the adverse consequences for both the doctor and patients involved. For patients, this may include falsified notes and the effects this can have on their future healthcare and medical records.
Doctors are in a position of great trust and have easy access to both prescriptions and medicinal products. It is easy to abuse the system by issuing prescriptions –for example, as described above or by taking drugs directly if available in a hospital setting or if handed in by patients.
Self-prescribing doctors
Of course, doctors recognise that self-prescribing drugs of dependence such as opiates or powerful painkillers is entirely unacceptable.
But the reality is that they should also avoid diagnosing and treating themselves with other medications. If not, they may be called upon to justify why it was necessary to prescribe in these circumstances.
The GMC has raised fitness-topractise proceedings against doctors for prescribing themselves with drugs such as benzodiazepines and opiates and non-benzodiazepine hypnotics.
However, we have also dealt with cases where doctors have been referred to the GMC for selfprescribing antibiotics.
A common feature of many such cases dealt with at MDDUS is an underlying health problem. The SOMEP report confirms that ‘doctors may be more vulnerable to mental health problems than
the general population. A higher proportion of doctors experience social dysfunction, fatigue, depression and substance abuse than the general population’.
Although the case summarised above lead to the doctor being erased, this is not typical of health cases. Indeed, a doctor cannot be erased for ill health.
We assist many doctors with health problems who are either reported or self-report to the GMC. Often they have significant underlying health issues which they have not adequately acknowledged or sought assistance for.
Sadly, many speak of early embarrassment and a consequent reluctance to seek help. An initial lapse and self-medication can then lead to an escalating picture where, ultimately, the health issue comes to light – but possibly only after very significant abuse of prescriptions and medication.
We always advise that members seek appropriate healthcare and, if in difficulty, they should discuss their professional concerns in confidence with one of our advisers.
In our experience, the complexity of prescribing systems allows many routes for abuse.
These include:
Staff adding medication to records/computer scrips and overriding the system to print off a new scrip;
Doctors changing medication recommended on hospital letters to access medication themselves;
Ad hoc prescriptions generated by any member of staff where there is no system regarding such scrips and no system to identify those requesting or picking up a prescription/medication;
Doctors using medication they issue in patients’ names.
In order to try to minimise the risks, it is essential to have in place robust systems which are clearly understood by all staff involved. In addition, regular audit of prescribing patterns can help to identify anomalies – and perhaps deter staff from trying to misuse the system. This is particularly so where controlled drugs are involved.
Careful checks should be in
Each doctor is personally accountable for the prescriptions they sign. This applies even when a prescription is issued on the advice of a colleague
Ensure robust systems are in place for issuing and reviewing prescriptions
Be aware of prescribing risks
Avoid selfprescribing unless in an emergency
Conduct regular tailored audits of prescribing patterns
Seek prompt advice if concerned about health issues relating to prescribing
Practitioners can face erasure from medical register for prescribing abuse
place to ensure that those patients receiving repeat or continuing prescriptions for controlled drugs have an ongoing need.
Each doctor is personally accountable for the prescriptions they sign. This applies even when a prescription is issued on the advice of a colleague; for example, when GPs prescribe in line with specialist advice.
You must therefore make sure you can justify your actions when doing this and be able to explain why a prescription was appropriate.
When abuse of prescribing systems comes to light, this is invariably very distressing for all concerned. It is important that practitioners seek advice from their medical defence organisation.
With appropriate guidance, both the practice and the doctor concerned can be helped through the processes that follow.
Dr Gail Gilmartin is a medical and risk adviser at Medical and Dental Defence Union of Scotland (MDDUS)


Philip Housden continues his journey following a year in the life of a NHS Private Patient Unit. This month: the spring-clean



SPRING IS here and this is an important time for private practice: for both consultants and for providers.
Demand is seasonal and from now until the summer holidays is a crucial time for elective surgery in particular.
In a trust, the new financial year has rebased financial and other targets and, as we know, these are not getting any less challenging. For an increasing number of NHS trusts, their private patient unit (PPU) services will be part of the solution to help meet those financial challenges.
I think it will help consultant users of PPUs to know what your private patient unit will be concentrating on right now. This might stimulate ideas and opportunities right on your doorstep.
First, we can look to internal management matters. If not done already, I suggest the private patient manager carries out a financial and contracting springclean.
Contracts with insurers may have differing renewal dates, but it makes sense to compare and contrast tariffs, review issues raised by consultants or others about areas of concern on costs inputs that may be hitting margins.
An external benchmarking review may be in order to also provide evidence of the need for a local price rate ‘catch-up’. The evidence gleaned from this review is vital to put against the insurers’ arguments that inflation has been low
for so long and also insurer’s desire to see long-term decline in tariffs in real terms in order to protect/stimulate the sector.
Any consultant with a concern over insurer coding and re-imbursement rates may wish to talk things through with their private patient office, as insurer contract renewals is the time to sort these.
An example might be where a change in practice or technique might be impacting on the present insurance complexity code. This same dialogue is also useful for reviewing fixed-price/self-pay surgery prices.
Looking more widely at the impact of other NHS initiatives on private patient development, I have been dismayed by the lack of any clear reference by Lord Carter in his recent report1 and his 15 recommendations to the potential for income generation and commercial activities.
Financial balance is exactly that: a balance between income and expenditure. But it seems that income generation has been ignored. The evidence from many trusts is that private patients –and other commercial activities –are clearly an opportunity to make better use of expensive NHS assets.
The closest I think we get in the report is in Recommendation 6 that ‘estates and facilities are used in a cost-effective manner’. Surely a trick has been missed here?
This missed opportunity is even more galling because it is so highprofile. To achieve real change, we need to start at the top. The single most important ingredient for future growth in private patient activity within a NHS trust is to ensure leadership support. This means finding opportuni-
ties for the trust senior executive team to be seen and heard to be overtly supporting the PPU.
Yes, overtly: prepared to declare that private patient services are a normal part of the work of the trust.
There is a direct correlation here: the stronger such support, the higher the confidence of consultant users, the faster the growth.
In trusts that are under-achieving on private practice incomes, there is often reticence to provide that vocal support. Consultants usually have a pretty good feel for where their trust chief executive and senior colleagues on the board stand on private patients.
Overall, though, disappointment is only a minor setback, as in a growing number of trusts there is a renaissance of private patient activity taking place.
This momentum is being driven forward by convenience for the consultant as the key customer as much as it is by the financial challenges of the day.
In next month’s article, I will be considering the importance of the local PPU management team and the impact the right appointment has to creating consultant user confidence.
Philip Housden (right) is a director of Housden Group, a management consultancy specialising in commercial support in the healthcare sector
Reference

1. Lord Carter’s report on: ‘Operational productivity and performance in English NHS acute hospitals: Unwarranted variations’ (February 2016)
Following my 2014 Independent Practitioner Today series on PPUs, I have continued to work with many NHS trusts to help develop and grow profitable private patient services.
This has enabled a real insight into the day-to-day challenges of delivering a private service within a public sector environment.
I am passionate about how PPUs can be part of the answer to the strategic and financial challenges that the NHS faces and so, in these articles, I plan to share learned, practical insights and also comment on how PPUs can best respond to changing policy issues and healthcare current affairs.




Should I stay or should I
go?
Patrick Convey considers why opting out of your NHS pension is not a quick decision
YOU WOULD be forgiven for losing track of all of the pension changes that have occurred in the past ten years.

It seems we cannot go one Budget without HM Revenue and Customs and the Treasury adding yet further complication and additional taxation. The latest attack on pensions has been twofold.
Firstly, the lifetime allowance has now been reduced from £1.25m to £1m.
Any excess over the lifetime allowance is taxed at up to 55%. While there are some transitional protections available to protect a higher amount, there are various rules to follow.
In all likelihood, unless you are coming towards the end of your career, these protections may not be suitable and you may not even qualify for them.
The second assault has been on those who earn over £150,000 a year, as this group will gradually see their annual allowance reduced from the current £40,000 down to as low as £10,000 for those who earn more than £210,000 gross from all sources.
Any excess contributions are added to your income for the tax year and taxed at your marginal rate of income tax.
Those in the NHS and who also run their own private practice may be caught by both of the changes mentioned above.
You will undoubtedly have colleagues who are leaving the scheme and telling you that you are mad for not doing so.
But it is not that simple
The NHS Pension Scheme is a defined-benefit scheme, which
We have carried out some research to see what the impact would be of staying in the scheme versus opting out
provides benefits based upon your length of service and your pensionable salary. The pension is Government-backed and indexlinked in retirement and also provides benefits for a surviving spouse.
Due to the rising costs, in recent years the private sector has been closing down such schemes almost as rapidly as the Government has been changing the rules.
The term gold-plated is banded around in the press and, in reality, it probably is not that far from the truth.
We have carried out some research to see what the impact would be of staying in the scheme versus opting out.
For an average doctor with 25 years’ service in the NHS and a pensionable salary of £100,000, by staying in the scheme and continuing to contribute for ten more years, he or she would be better off within 13 years of retirement versus a colleague who leaves the scheme.
The situation changes the closer you get to retirement and will be dependent upon possible pay rises, your position in relation to the lifetime allowance and whether there have been any annual allowance charges.
It should also be remembered that if you opt out, you will lose other benefits such as death-inservice life assurance and may also face reduced ill-health retirement options.
Each individual will require specific advice.
However, the message to take away is that the decision to opt out is not one that should be taken lightly, as it may cost in the long run.
See accountant Ian Tongue’s analysis of pension changes, p50
Patrick Convey (right) is technical director of Cavendish Medical, specialist financial planners helping senior consultants in private practice and the NHS

The content of this article is for information only and must not be considered as financial advice. Cavendish Medical always recommends that you seek independent financial advice before making any financial decisions. Levels, bases of and reliefs from taxation may be subject to change and their value depends on the individual circumstances of the investor. The value of investments and the income from them can fluctuate and investors may get back less than the amount invested.



UK Top 20 accountants specialising in the healthcare sector
National firm of the Year 2013
• AISMA member (Maidstone and Leicester offices)
12 offices including London City
Tax Structures for Hospital Consultants - dispelling myths
Surgeon groups and consortia
GP Practices including mergers and federations
Solvent liquidations (for companies at the end of their lives)
For more information please contact: South East
James Gransby FCA
E: james.gransby@mhllp.co.uk
T: +44 (0)1622 754033
M: +44 (0)7712321899
East Midlands


Robert Nelson DChA FCA
E: robert.nelson@mhllp.co.uk
T: +44 (0)1162 894289
M: +44 (0)7814009160
General email: healthcare@mhllp.co.uk www.macintyrehudson.co.uk



Independent practitioners acting as expert witnesses are probably most frequently asked to write a liability and causation report. Michael R. Young has some excellent tips

WHEN YOU first start out as an expert witness, you will probably have no idea what a liability and causation report should look like or how many pages it should contain or what it should include – or omit.
Let’s not forget what a liability and causation report is about:
☞ Was Dr X in breach of his or her duty of care, such that the care and treatment Dr X gave fell below an acceptable standard (i.e. liability)?
☞ Did the substandard care cause physical injury and financial loss and expense (i.e. causation)?
The first page is the introduction and should include the following information:
Why the report has been written – i.e. its purpose;
Your name and qualifications, as the report author;
The name of the firm of instr
ucting solicitors, not the individual solicitor’s name;
The name of the solicitor’s client;
Whether the client is the claimant or the defendant;
A summary of your instructions, including the date of the letter of instructions. This is the terms of reference. It is best not trying to paraphrase the instructions because, in doing so, you may unknowingly alter their meaning. So it is advisable to copy the instructions word for word from the solicitor’s letter.
The sources of the evidence. This should be comprehensive and must include where the evidence has come from, the dates the evidence relates to and – perhaps equally as important – what is missing.
A list of the contents and page numbers. This helps the reader find information quickly.
I also include a paragraph to demonstrate I understand the Bolam and Bolitho tests, which reads:
‘During the process of evaluating all the evidence and information made available to me, and throughout the preparation of my report, I will remain mindful of the direction of McNair J. to the jury in Bolam v Friern Hospital Management Committee when reaching my conclusions regarding the issue of liability (the Bolam test) and of Lord BrowneWilkinson in Bolitho v City and Hackney Health Authority.
‘The questions I will therefore ask are:
1How might a reasonable, responsible and respectable body of medical/dental practitioners have conducted themselves?
2Can I provide a logical explanation for what was actually done or omitted, knowing all of the facts of the case?’
The report must contain a statement that you understand your duty to the court and have complied with that duty. The declaration (see page 36) can be set out on the second page.
A summary of your conclusions comes on the next page of the report. These could, of course, just be copied and pasted from the conclusions section, but it is a summary, so it should summarise. It may help if the summary is thought of in terms of the following questions:
Was there a breach of duty of care? If so, in what context did it occur?
Two further questions then follow – was anything done that should not have been done and
Ask yourself if you are sticking to your instructions and answering the question. It is easy to lose sight of this
was anything not done that should have been done?
Did the breach of duty result in substandard care and/or treatment?
Did any substandard care and/ or treatment cause physical injury and financial loss and expense?
I developed section headings, based on how I approached the evidence and on my method of answering the solicitor’s questions.
Section 1: A synopsis of the evidence
This is a pure statement of fact. It helps to refer to your original notes and arrange the evidence thematically.
By doing this, you reduce the risk of missing anything out when tackling this section.
Ask yourself if you are sticking to your instructions and answering the question. It is easy to lose sight of this.

Section 2: Interpretation and analysis of evidence
Do not be tempted to discuss or give opinions. Interpretation is defined as ‘explaining the meaning of’. Analysis has two definitions: the first is ‘a detailed examination of the elements or structure of something’. The second is ‘the separation of something into its component parts’.
Section 3: The argument or discussion
Here you can expound the various arguments, interpretations and approaches to the topic; define and evaluate the significant strengths and weaknesses of each, possibly reaching new and overarching conclusions.
It is important that all treatment under scrutiny is put into context, which means judging it against concurrent accepted practice.
Whenever you make a point or


statement in any report, ask: ‘Can I prove it or is this just supposition?’ Support your arguments with evidence drawn from reputable sources. Develop a method of setting out the discussion in a logical and coherent order.
I developed the ‘PEACH’ method:
First, look for a particular point (P) you want to make, for example ‘X should not have done Y’; Then look for the evidence (E) to either support or refute the point – or do both;
Next, analyse (A) the evidence; Finally, come to your conclusion (C);
Later in your report, you will highlight (H) your conclusion about each point in your summary.
A major problem with some reports is that the author’s conclusions do not logically follow Do









from what has been previously stated. Faulty expression is usually to blame, especially if the writer has two unconnected statements to make, but instead of using two separate sentences, connects them with an ‘and’ or ‘while’. So avoid long, overcomplicated sentences.
The conclusions are based on a balance of probabilities – more likely than not – and are not always based on certainties.
Conclusions must also include a summary of the strengths and weaknesses of the case. Be careful about unwittingly giving guarantees one way or the other about the claimant or defendant’s case. Be honest in your appraisal and try to signpost any lines of argument that the other side may use.
The solicitor will appreciate this.
Remember, the report is aimed not only at helping the solicitor decide if the case is worth pursuing but also at helping the lawyers decide how to proceed. So if a current condition and prognosis report would be useful or if further investigation by a certain specialist would help, now is the time to say so.
The report must contain a statement of truth that says: ‘I confirm that I have made clear which facts and matters referred to in this report are within my own knowledge and which are not. Those that are within my own knowledge I confirm to be true. The opinions I have expressed represent my true and complete professional opinions on the matters to which they refer.’
The report must be signed and dated.
Adapted from The Effective and Efficient Clinical Negligence Expert Witness , by Michael R. Young, price £60 from Otmoor Publishing
I, declare THAT:
1. I understand that my duty in providing written reports and giving evidence is to help the court, and that this duty overrides any obligation to the party by whom I am engaged or the person who has paid or is liable to pay me. I confirm that I have complied and will continue to comply with my duty.
2. I confirm that I have not entered into any arrangement where the amount or payment of my fees is in any way dependent on the outcome of the case.
3. I know of no conflict of interest of any kind, other than any which I have disclosed in my report.
4. I do not consider that any interest which I have disclosed affects my suitability as an expert witness on any issues on which I have given evidence.
5. I will advise the party by whom I am instructed if, between the date of my report and the trial, there is any change in circumstances which affect my answers to points 3 and 4 above.
6. I have shown the sources of all information I have used.
7. I have exercised reasonable care and skill in order to be accurate and complete in preparing this report.
8. I have endeavoured to include in my report those matters, of which I have knowledge or of which I have been made aware, that might adversely affect the validity of my opinion. I have clearly stated any qualifications to my opinion.
9. I have not, without forming an independent view, included or excluded anything which has been suggested to me by others, including my instructing lawyers.
10. I will notify those instructing me immediately and confirm in writing if, for any reason, my existing report requires correction or qualification.
11. I understand that:
My report will form the evidence to be given under oath or affirmation
Next month: The clinical negligence clinical examination
The book costs £60, but Independent Practitioner Today has secured discount of a third off for readers, so you pay only £40.
Listen to the audio content which accompanies the book at this website: www. otmoorpublishing.com/audio.

For more information and to order, email stephen. bonner@otmoorpublishing.com, quoting reference ‘Young/IPT’.
Questions may be put to me in writing for the purposes of clarifying my report and that my answers shall be treated as part of my report and covered by my statement of truth
The court may, at any stage, direct a discussion to take place between experts for the purpose of identifying and discussing the expert issues in the proceedings, where possible, reaching an agreed opinion on those issues and identifying what action, if any, may be taken to resolve any of the outstanding issues between the parties
The court may direct that, following a discussion between the experts, a statement should be prepared showing those issues which are agreed and those issues which are not agreed, together with a summary of the reasons for disagreeing
I may be required to attend court to be cross-examined on my report by a crossexaminer assisted by an expert
I am likely to be the subject of public adverse criticism by the judge if the court concluded that I have not taken reasonable care in trying to meet the standards set out above.
12. I have read Part 35 of the Civil Procedure Rules and the accompanying practice direction and I have complied with their requirements.
13. I have read the ‘Protocol for Instruction of Experts to give Evidence in Civil Claims’ and confirm that my report has been prepared in accordance with its requirements. I have acted in accordance with the Code of Practice for Experts
Making reasonable adjustments to staff sickness absence procedures is a potential headache for private doctors who employ staff, warns Fiona McLellan. Here she talks through what you can do
THE RECENT Court of Appeal decision in Griffiths v Secretary of State for Work and Pensions provides important guidance for employers on whether reasonable adjustments need to be made to sickness absence management procedures.
Managing attendance is a perennial headache for employers who have to deal with the practical problems it presents to the effective running of their business. At the same time, they have to carry out the difficult balancing exercise of supporting staff in
what can be sensitive/difficult circumstances, while managing their absence fairly to minimise the risk of complaints or claims.
A key issue for employers, particularly when managing longterm absence, is the need to consider the question of whether or not the employee in question is ‘disabled’ – as defined at s6 of the Equality Act 2010 (EqA). This places the employer under a ‘duty to make reasonable adjustments’ – as defined at s20 – to enable the employee to overcome substantial disadvantage caused by their disability.
➱ p42

• Tax consultancy
• Self-employed and company accounts
• Property investment structuring
• Payroll and VAT services
Contact: Nick Brecker. Tel: 020 7253 0030
Email: nbrecker@caldwellandbraham.co.uk
Web: www.caldwellandbraham.co.uk

What is a disability?
An employee is disabled if s/he suffers from a physical or mental impairment that has a substantial and long term adverse effect of their ability to carry out normal daytoday activities.
Certain medical conditions will be deemed under the EqA to constitute a disability, specifically: blindness, severe sight impairment, severe disfigurements, cancer; HIV infection and multiple sclerosis.
When does the duty to make reasonable adjustments arise?
If a staff member is disabled, s/he will be afforded protection against disability discrimination by the EqA and, in turn, the employer may be under a duty to make reasonable adjustments for that staff member.
The duty to make reasonable adjustments arises when an employer knows or ought reasonably to know that a member of staff is disabled and is placed at a substantial disadvantage by one or more of the following:
A provision, criterion or practice (PCP) – most likely to be relevant to managing attendance situations;
A physical feature of the employer’s premises;
An employer’s failure to provide an auxiliary aid.
In such circumstances, the employer will need to take appropriate steps to address the disadvantage being suffered. What is reasonable will be determined by the particular circumstances.
In the context of managing sickness absence, it is likely that an employer will be aware of a staff member’s medical condition and prognosis through the individual’s attendance record and their provision of information to the employer or, especially in longterm absence situations, through Fit Notes or reports from a GP or occupational health provider.
This information means it is probable that an employer will either know, or ought reasonably to know, that the staff member is disabled.
If that is the case, the Griffiths decision means that employers must turn their attention to whether or not the process, whether formal or informal, for managing the employee’s absence
places the employee at a substantial disadvantage in comparison to nondisabled employees.
If so, the statutory duty to make reasonable adjustments will be triggered and steps will need to be taken to reduce the risk of grievances or litigation.
This case related to a longserving employee of the Department for Work and Pensions (DWP) who suffered from a number of medical conditions, specifically postviral fatigue and fibromyalgia, which was diagnosed following an occupational health referral on the employee’s return to work. The DWP ultimately accepted that the employee was disabled.
The DWP operated a formal attendance management policy under which a series of warnings could be issued to staff absent on account of sickness.
These warnings culminated in the sanction of dismissal. A DWP employee would receive a warning if their absence reached a certain level triggering the application of the policy.
The trigger point was eight days’ of absence in any rolling 12month period. However, the policy provided that, as a reasonable adjustment, the trigger point could be increased for disabled staff.
Ms Griffiths was issued with a written warning following a 66 day period of absence – 62 days of which were on account of her disabilities – and cautioned that further periods of absence could result in the issue of further warnings under the policy.
In response, Ms Griffiths raised a grievance and requested that two reasonable adjustments be made to counteract the substantial disadvantage she asserted she suffered under the policy. Specifically, she asked that:
Her disability related absence (62 days) be discounted and consequently the written warning withdrawn;
The policy be adapted and her trigger point increased by an additional 12 days, thereby providing her with a trigger point of 20 days’ absence before the policy would be applied.
The grievance was not upheld and the DWP declined to implement the adjustments requested by Ms Griffiths. She therefore brought proceedings in the Employment Tribunal (ET), under s20 of the EqA, asserting a failure by the DWP to make reasonable adjustments for her.
Both the ET and the Employment Appeal Tribunal (EAT) determined that there was no breach of the EqA, because the DWP’s duty to make reasonable adjustments was not engaged.
The courts’ decisions were predicated upon the fact that the DWP applied the policy to all staff, both disabled and nondisabled, equally. These decisions were not surprising, as this had been the consistent prevailing view of the courts to such claims for many years.
Both courts determined in any event that the adjustments being requested by Ms Griffiths were not reasonable.
However, the Court of Appeal found that Ms Griffiths had been subjected to substantial disadvantage by the application of the policy because, on account of her disability, she was more likely to be absent than an employee without her disability and consequently suffer a disadvantage by the application of the policy. This thereby triggered the duty to make reasonable adjustments.
Importantly, the Court of Appeal determined that the relevant PCP placing Ms Griffiths at a substantial disadvantage was the need for
This case clarifies that employers will need to make reasonable adjustments to absence management processes, such as the trigger point for taking formal action
DWP employees’ to maintain a certain level of attendance at work so as not to be subject to the risk of disciplinary sanctions. Such a provision will ordinarily lie at the heart of any attendance management process, meaning that the decision has farreaching implications for all employers, given that managing sickness absence is, unfortunately, a regular occurrence.
What is reasonable?
The Court of Appeal did not, however, accept that the adjustments suggested by Ms Griffiths were reasonable, determining that:
It was not reasonable to expect an employer to discount lengthy periods of absence – in this case, 62 days where the trigger point was eight days – particularly in circumstances where the illness did not arise from a oneoff medical condition and there could be further periods of lengthy absence in the future;
The request to extend the trigger point by 12 days and thereby to 20 days was completely arbitrary and there was no obvious period by which the trigger point should be increased. The Court of Appeal also noted that if periods of future absence were lengthy, this adjustment would be futile.
Unhelpfully for employers, the Court of Appeal indicated in its judgment that, in many cases, employees will be better served by raising a claim for disabilityrelated discrimination (under s15 of the EqA) than a reasonable adjustments claim.
Disabilityrelated discrimination claims are notoriously difficult for employers to defend, notwithstanding that such discrimination can be objectively justified.
To invoke this defence, an employer would require contemporaneous documentation or evidence to show that its actions were a proportionate means of achieving a legitimate aim – i.e. there were no viable alternative options with a less discriminatory impact. Managing absence and seeking to improve attendance rates will be a legitimate aim for employers, but the manner in which they go about achieving it will be key and will inevitably include implementing reasonable adjustments for disabled employees.
This case clarifies that employers will need to make reasonable adjustments to absence management processes, such as the trig
ger point for taking formal action. This will be the case – even if the policy applies equally to all staff – where an employee can demonstrate that their disability predisposes them to higher rates of absence and consequently a greater risk of sanction in comparison to colleagues.
This is plainly not going to prove difficult for many employees to show.
While this decision may create obligations for employers, and the need therefore to consider the steps taken in managing absence carefully, it does not mean that any adjustments proposed by staff will necessarily be reasonable and so have to be implemented.
The Court of Appeal decision makes it clear that only steps that directly relate to the ability to integrate the employee into employment – that is to say, steps that enable an employee to remain at work or to return to
work – are likely to be reasonable in the context of attendance management.
Steps that relate to an employee’s personal circumstances, such as removing a warning, are unlikely to be reasonable adjustments.
In private practices, where there may not be formal attendance procedures, following this decision it will be even more important to ensure that all staff are at least initially treated equally. Where there is information pointing to a need for adjustments, time and care should be taken, perhaps with focused input from the employee’s GP or an occupational health provider, on possible adjustments that allow the employee to reduce their levels of absence and/or return to work.
All attendance management discussions/decisions should be recorded in writing so there is a contemporaneous record that can
be referred to if there are future complaints or disputes.
Conclusion
This is a difficult area both practically and legally, given that claims for discrimination can be raised under various different heads of claim by any employee/worker –there is no qualifying service level – and the level of compensation that could be awarded is uncapped. It would therefore be prudent to review your attendance management procedures/practices to ensure these are clear, consistently followed and take proper account of potential disability discrimination issues, including the need for reasonable adjustments. If in doubt, take legal advice earlier rather than later to avoid a large legal headache.
Fiona McLellan is a partner in Hempsons employment/discrimination team
Independent Practitioner Today has joined forces with leading niche healthcare lawyers Hempsons to offer readers a free legal advice service.
We aim to help you navigate the ever more complex legal and regulatory issues involved in running and developing your private practice – and your lives.
Hempsons’ specialist lawyers have a long track-record of advising doctors – and an unrivalled understanding of the healthcare system as a whole.
Call Hempsons on 020 7839 0278 between 9am and 5pm Monday to Friday for your ten minutes’ of free legal advice.







Self-paying patients are on the increase – and more and more consultants are needing help to gather their fees as a result. Gary Nials analyses the problems and shows what can be done
There has always been a percentage of people who have sought private healthcare treatment without having an insurance policy and this market still appears to be very buoyant
MANY PRACTICES still seem to think of private practice as the insurance market – but, in reality, it is not that simple.
An analysis on the invoices we raised in 2015 for people who owed doctors money shows that the private medical insurance (PMI) market only accounted for 55% of the total.
The remaining 45% was split between self-payers and other organisations such as embassies, hospitals, solicitors – for medicolegal work – and other commercial organisations.
Amazingly, the lion’s share of this non-PMI invoicing was selfpay, which accounted for an astonishing 29% of the total
amount invoiced; an increase of nearly 20% in the last three years.
This figure of 29% is an average across all our consultants and can be significantly more, depending upon the specialty, type of practice/clinic and taking into account the location of the practice.
Indeed, for some of our consultant clients, self-pay turned out to be the largest part of the practice.
The reason the average of 29% is so high is down to many factors, but here are the major ones: ☞ NHS. Ninety per cent of the population does not have private medical insurance. With the NHS suffering longer waiting times in many areas, coupled with the bad press on the quality of care on the
wards, this is leading to an increasing number of people seeking an alternative and willing to pay, even if just for the initial consultation.
☞ Insurance policies. In order to control the costs of the annual premiums, insurance policies will have elements which are not covered by the policy. This will be due to benefit limits, patient excess on the policy, co-share policies, where the patient agrees to pay a percentage of each invoice, and for many other reasons.
☞ Overseas patients. If your practice is based in central London, this has always been a part of practice life with patients coming from outside of the UK seeking private healthcare.
☞ Self-pay. There has always been a percentage of people who have sought private healthcare treatment without having an insurance policy and this market still appears to be very buoyant.
The reason that this information is so important for consultants to know is that if you do not know what the statistics are in your own practice, you cannot make sure it gets dealt with correctly from both a billing and collection process.
In our experience, this is rarely dealt with correctly. And there is quite often a lack of clarity regarding billing self-pay patients and also collecting the money. This results in the practice hav-
ing a huge amount of outstanding debt, which is either chased on a sporadic basis or not chased at all. And that means debts then amount to a significant sum of money.
The reasons for this debt can be down to many factors, but, typically, what we see is a lack of a robust system in place to deal with this element of the practice.
What the practice needs to do is to set up a system to deal with each element of the self-pay income stream. I highlight the main ones below.
When your practice decides to see a patient who is not a UK resident, you need to decide in advance what your charges are going to be so that it is clear to them exactly what the total cost of the treatment will be. Then have a discussion about the method of payment.
When we deal with these patients on behalf of our clients, we quite often collect the money in advance because once the patient has left the UK, then the chances of collecting payment dramatically reduce.
A common way of encountering an overseas patient is through the hospital. Here the hospital may well agree to collect all money due from the patient, but unless you get your invoice to the correct department/contact in the hospital in a timely manner, it is likely that your fee will not get collected.
That then leaves you with the problems of chasing the patient for payment after he has left the UK.
The majority of practices are likely to have an element of patients who are self-pay. Therefore, they should have a price list and agreed methods of payment
made clear in advance, so that the patient is expecting an invoice and is prepared to pay either on the day or shortly afterwards.
When doing this for our clients, we have a variety of methods available to us including taking payment on the day by debit or credit card or, depending upon the requirements of the practice, we can even take money in advance and also install our client self-pay module, where appropriate.
When you cannot collect payment on the day, you will need to put in place a system where the patient is chased for payment after an agreed period of time and then chased on a regular basis until payment is collected.
Depending upon the specialty and type of practice, this is typically the largest volume of the self-pay invoices – and it is also the hardest to collect.
This is because most patients do not understand their insurance policy and they believe that all costs are going to be met by their insurer. So when they receive an invoice for their element of the treatment, it is an invoice they are not expecting.
From our experience, a lot of them ignore the invoice, as they are under the misapprehension it is a copy of what has been sent to the insurer. So unless you follow this up with a phone call, it will just be ignored.
Once they are aware that the invoice is correct, then they may contest this with their insurer, as they erroneously believe all costs should be met under the terms of their policy.
A large part of what we do on behalf of our clients is liaise between the insurer and the patient to ensure that it is clear who owes the money.
Once the patient accepts that
Amazingly, the lion’s share of this non-PMI invoicing was self-pay, which accounted for an astonishing 29% of the total amount invoiced; an increase of nearly 20% in the last three years
the money is owed by them, and depending upon the amount that they owe, then you need to be in a position to either take payment immediately or agree payment terms.
The practice should put a robust system in place in order to maximise the opportunity of the selfpay market as well as collect all the money earned. The alternative would be to use a professional medical billing and collection company.
Next month: Increasing your self-pay market share
Gary Nials (right) is the managing director of Medical Billing and Collection


A two-day fully inclusive residential medical management course for senior SPRs and new consultants covering leadership and negotiation, private practice, business planning and appraisal. Only £250.
To be held in Balliol College, Oxford, on 13th and 14th September 2016. For more details, see: www.oxbridgecourses.com
Staff issues can get independent practitioners into deep water – and not just due to employment legislation. Dr Beverley Ward (right) answers two private doctors’ concerns that could go all the way to the GMC

QI have recently discovered that my practice secretary has been saving work to a memory stick and taking it home to get through the backlog.
ticularly vulnerable to loss or theft, it’s unwise to turn a blind eye to your employee storing identifiable patient information on a memory stick.
If you do, you risk an inadvertent breach of patient confidentiality which could result in patient complaints, action by the Information Commissioner’s Office (ICO) and even a GMC investigation.
The press may also get hold of the story. The consequences could be financial as well as reputational: the ICO has powers to fine organisations up to £500,000 for reckless breaches of the Data Protection Act.
Explain to your secretary the risks of carrying information to and from work on a memory stick and tell her to desist. It could also be an opportunity to discuss her workload and consider whether she needs additional support.
This incident is also a timely reminder of the need for an information security policy within your practice, which all staff should follow.
•
•
•

I don’t want to discourage her and there have been no mishaps, but I am concerned that the memory stick might go astray and I doubt it’s encrypted.
How should I address this?
AStories of lost or stolen memory sticks containing patient data appear in the press with alarming regularity. The data often involves sensitive information that no patient would want to be disclosed.
As a doctor, you have an ethical contractual duty to protect patient confidentiality and ensure that identifiable patient data is not improperly disclosed in any circumstances.
In addition, the Data Protection Act 1998 (DPA) imposes a legal duty on those responsible for personal data to ensure it is held securely and protected from unauthorised or unlawful processing.
Since mobile devices are par
Such policies usually include rules relating to the use of home computers or mobile devices. The ICO has said that risks associated with the use of mobile and home working need careful consideration, but it is possible to use these tools securely with appropriate scanning, security software and encryption.
Seek advice from an IT specialist, but bear in mind the need for a signed written contract with all thirdparty suppliers, including IT contractors, which sets out your confidentiality requirements.
QAs a favour, I agreed to examine one of my staff, who was worried about a mole on her back.
Stories of lost or stolen memory sticks containing patient data appear in the press with alarming regularity
investigation should make a decision regarding whether the complaint is upheld or not.
Contemporaneous notes made at the time of the consultation would be helpful to support the evidence you give.
The complainant should be advised of how to escalate matters should she be unhappy with the outcome of the local investigation.
Many private healthcare facilities have now signed up to become members of the Independent Sector Complaints Adjudication Service (ISCAS). ISCAS has produced a code of practice which it expects its members to adhere to when handling complaints.
This is a threestage process, with attempts at local resolution, followed by a review of the complaint by senior management within the organisation and finally an independent review of the incident.
The independent review is undertaken by an ISCAS adjudica
tor who can make recommendation not only for an apology to be given, but also for a goodwill payment to be made, up to a limit of £5,000.
Unfortunately, there are occasions when the complainant remains unsatisfied and chooses to refer the matter to the GMC.
Any complaints that you receive during your clinical practice should be discussed as part of your annual appraisal and the learning points identified should be acted up.
Keeping evidence of these discussions and the continuing professional development undertaken as a result, can be helpful in demonstrating that you have responded appropriately should the worse happen and the GMC decide to investigate the matter.
Dr Beverley Ward is a medico-legal adviser at the MDU
As far as I am concerned, the consultation was uneventful, but it has come back to haunt me when I gave the staff member a verbal warning about her persistent lateness.
She has now told the practice manager that she was unhappy with my examination because I stood too close and touched her ‘more than necessary’.
And she has threatened to complain about me to the GMC and is clearly trying to cause trouble. But what should I do?
AThe GMC guidance in Good Medical Practice states doctors should, wherever possible, ‘avoid treating themselves or anyone with whom they have a close personal relationship’ and many practices operate a policy that members of staff cannot also be patients.
This enables the practice to keep the doctorpatient relationship demonstrably separate from the employeremployee relationship and also helps to avoid a potential area of dispute.
Although you may be upset by the actions of your staff member, she is entitled to have her complaint investigated in the same way as any other patient.
It is also in your interest that her claims are shown to be without foundation.
As the patient has made a serious allegation against you, it’s important that you do not try to respond to her directly. Not only would this be a conflict of interest, but you could inadvertently inflame the situation. Instead, ask two senior members of your team to deal separately with the complaint and the employment matter.
Depending on their experience, the manager dealing with the lateness issue may want to seek employment law advice. However, the practice should be careful not to inadvertently reveal any health details known to them only in the context of the doctorpatient relationship.
The manager dealing with the complaint about your conduct should follow practice policy when investigating this.
You will need to provide a statement detailing what happened, describing the clinical aspects of your consultation, as well as making it clear that you deny the allegation.
Details of the investigation should be kept in a complaints file and a senior person independent from the complaint and

If you
like
the idea of a full-size Land Rover Discovery but are attracted to the benefits of a more affordable, compact and fuel-efficient sports utility vehicle (SUV), then our tester Dr Tony Rimmer (right) believes you should look hard at this new car. The compromise is minimal and you will save significantly on costs
AS ANY independent practitioner knows, the key to any successful enterprise is a good business plan and decent investment.
The subsequent hard work will then pay dividends in both satisfaction and financial terms. As I mentioned in my review of the new Jaguar XE last month, the giant Tata group bought Jaguar Land Rover eight years ago and has certainly reaped dividends from its hard work.
It has invested in new factories,
expanded the workforce and replaced all the ageing products with up-to-date vehicles.
Lagging behind
The latest model in its line-up to be superseded by a brand-new replacement is the Land Rover Freelander. This small SUV had been around since 1997 and, despite some significant updates, was really showing its age.
Competition such as the BMW X3 and Audi Q5 were streets
ahead in terms of quality and refinement. The Freelander name has been dropped and we now have the Discovery Sport.
Based on the modern platform of the hugely successful Range Rover Evoque, it sacrifices some of that car’s style for greater practicality.
A longer wheelbase means a lot more available space for passengers and luggage. In fact, the Sport can be a full seven-seater, which is quite remarkable for such a compact SUV.

The rearmost seats fold neatly into the boot floor when not needed and take up minimal space with hardly any compromise. The higher roof-line also means better headroom for rear passengers.
Certainly, from the front, it has the same good looks as its small Range Rover cousin and, with more upright rear quarters, still looks smart and classy.




‘There is no doubt that the general quality levels have been raised significantly compared to the old Freelander. This is a car that can hold its head high’
The interior design and trim will be very familiar to Evoque owners and the trademark rotary gear selector that rises serenely and dramatically when starting the engine is a feature also shared with modern Jaguars.
There is no doubt that the general quality levels have been raised significantly compared to the old Freelander. This is a car that can hold its head high in the company of its premium-brand competitors.
Interior space is excellent, the boot is capacious and the occasional rearmost seats are really easy to erect and fold away when needed. I love the fact that this is all on offer in a car with much less bulk that full-sized SUVs like the Audi Q7 or Volvo XC90.
The Discovery Sport is going to have great appeal for those of you with more than two children and who need all the space and convenient features to cart them and their friends around but want a neat city-friendly SUV.
Land Rover took a bit of a risk when it first released the Discovery Sport in 2014. It was only available with a 2.2 litre diesel engine that was from an original Ford design and had been around for several years. It was noisy and not as clean nor efficient as the latest diesels.
The company had set up a brand-new £500m factory in
Body: Seven-seat SUV. Permanent four-wheel drive
Engine: 2.0 litre four-cylinder
twin turbo-diesel
Power: 178bhp
Torque: 430Nm
Top speed: 117mph
Acceleration: 0-60mph in 8.4 secs
Claimed economy: Combined 53.3mpg
CO2 emissions: 139g/km
On-the-road price: £34,200
Wolverhampton to build a new state-of-the art 2.0 litre turbo-diesel known as the Ingenium engine. Unfortunately, it needed supplies for the new Jaguar XE and XF models, too, and the leaping-cat brand took precedence until production increased significantly.
Fortunately, the car is so good overall that the old engine was only a minor Achilles heel and first adopters have not lost out too much.
But now all Discovery Sports come with the new engine and my test car had the more powerful 180bhp version with the super smooth nine-speed automatic transmission.
Overall economy is an impressive 53.3mpg and CO2 output is only 139g/km. It feels smooth, too, and like most of the best diesel engines, there is no excessive noise nor vibration compared to petrol units.
The compact exterior dimensions, together with sharp steering and a firm but comfortable
ride give the driver some surprising tactile satisfaction.
I found it easy and enjoyable to punt this Land Rover along some of my favourite twisty roads.
Motorway comfort is also assured, so your passengers will appreciate the ride, too. I did not have the chance to take my test car off road, but am secure with the knowledge that, being a Land Rover, the Discovery Sport will do amazing things if asked.
The Discovery Sport will be a great success for Land Rover and it deserves to be so.
Those of you who like the idea of a full-size Land Rover Discovery but are attracted to the benefits of a more affordable, compact and fuel-efficient SUV should look hard at this new car.
The compromise is minimal and you will save significantly on costs. This could leave you with more to invest in a business plan to move your professional and commercial interests forward.
Dr Tony Rimmer is a former NHS GP practising in Guildford, Surrey
It’s all been happening on the pensions’ front. Ian Tongue (left) continues his series for new doctors in private practice with a recap of the pension annual allowance and new tapering rules

THERE HAS been much talk lately of the pension annual allowance due to the significant changes which applied from 6 April 2016.
One thing for certain is that there is a lot of confusion over these changes, which is not surprising given the constant attack on pensions for higher earners. This article recaps on the changes and how they may affect you.
The pension annual allowance is an overall amount that can be paid into a pension each year and receive tax relief on the pension contributions. The annual allowance has varied considerably over recent years, peaking at over £200,000 and falling to the current level of £40,000 a year.
As with the income tax personal allowance – which is removed for those earning more than £100,000 – the Government has decided to reduce the £40,000 allowance

further for those earning more than £150,000.
A band has been created between £150,000 and £210,000 whereby the £40,000 is reduced gradually down to a minimum of £10,000 at the £210,000 – and higher – earnings level.
This is where it starts to get complicated.
For an NHS consultant with superannuable earnings of £85,000, you would see superannuation contributions deducted from your taxable pay at 13.5% –which amounts to £11,475 – and you would receive full tax relief on those contributions under PAYE.
However, the £11,475 contributions are disregarded for the purposes of the annual allowance calculations and a separate calculation of ‘deemed contribution’ is made which is based on the capital growth of your pension rather than actual contributions.
This is because the NHS Pension Scheme is known as a ‘defined benefit’ pension scheme. This means that what you put in is not proportional to what you get out. Your pension under the NHS scheme is a product of earnings and length of service rather than how much you put in.
The other main type of pension scheme is known as a ‘defined contribution’ and the majority of those not working on the public sector have these types of schemes.
If you have taken out further pensions (not added years), then they will almost certainly be of this type. The actual contributions paid are the relevant amount against the annual allowance for these types of savings. Contributions from all sources are added together when testing against the £40,000 (or less) limit.
If you have added years, you will effectively get more than one year of pension growth within the calculations each year, thereby increas
ing your deemed contribution under the NHS Pension Scheme.
Let’s look at a member in the 2015 pension scheme with 20 years’ service with a superannuable pay level of £85,000 at the start of the year (6 April 2016) and £88,000 at the end of the year (5 April 2017) with 0% inflation, which is the HM Revenue and Custom’s rate for 201617 calculations:
Capital value at the start of year: 20/54 x £85,000 x 16 = £503,704
Capital value at the end of year: 21/54 x £88,000 x 16 = £547,556
Therefore, pension growth in the above calculation is £43,852.
As mentioned above, the annual allowance level is reduced from £40,000 to as low as £10,000 for those earning £210,000 – but what is included as ‘earnings’?
Unfortunately, the answer is pretty much everything recorded as income on your tax return.
To make matters worse, your NHS employment earnings are net of employee pension contributions so these are added back on together with the employer’s superannuation contributions as well.
A useful tool to assess your earnings is the ‘total reward statement’ available from the NHS Pensions portal. The statement indicates your pay before employee superannuation deductions and also provides the detail of how much employer superannuation contributions have been made.
Your private practice earnings are added onto the amount calculated above, which will inevitably result in a significant proportion of consultants being affected by the pension annual allowance tapering measures.
Tax planning opportunities may exist, depending on your cir
cumstances and future events, such as forthcoming pay increments or clinical excellence awards – where still available.
Discuss your circumstances with your accountant well in advance, as the reinstatement of the full £40,000 could save you up to £13,500 in tax charges.
If you have exceeded the annual allowance level for your own circumstances, the first thing that can come to your aid is to look back at the last three years to see if there are any unused amounts –years where the limit was not exceeded – which can be deducted from the excess for the year. If there are unused amounts, this may significantly reduce or extinguish any excess, resulting in no tax being due this time.
If, after the above, an excess still arises, tax is payable on the excess
at your marginal rate of tax. In the example on the opposite page, should the consultant have no unused relief and earnings did not exceed £150,000, a tax charge of £1,541 would arise.
Should the consultant in question have this growth from 6 April 2016 and total earnings exceeded £210,000, they would have an eyewatering tax charge of £15,233 –again assuming that there is no unused relief available from looking back three years.
The tax itself can either be paid through self assessment or, for amounts exceeding £2,000, the pension scheme can pay the amount due. This is known as a ‘Scheme Pays Election’ and there are strict timescales to apply for this.
For example, for the 2015 16 year (year ended 31 March 2016 for NHS Pensions), a ‘scheme pays election’ would need to be made by 31 July 2017.
Who will tell me I have gone over the annual allowance?
The above is clearly complex and, realistically, the majority of consultants will not be aware of their actual position.
NHS Pensions prepares annual allowance statements, but these are often slow to be prepared or, in some cases, inaccurate and so it is vital that your accountant is reviewing matters annually.
Clearly, the changes to the annual allowance are complex and can justifiably be see seen as very unfair. Ensure that your accountant is au fait with the changes and is able to advise you of your position, otherwise you could get caught out with an unexpected tax charge.
Next month: Working in a group: recent changes – a tax and competition perspective
Ian Tongue is a partner with accountants Sandison Easson & Co


For anaesthetists to maintain latest encouraging income levels, they will probably have to work harder, warns Ray Stanbridge
GROSS PRIVATE practice incomes for private anaesthetists have increased by £7,000 (or 9.5%), going up from £74,000 to £81,000 between 2013 and 2014. Costs on average have risen by 8.3%, from £24,000 to £26,000. As a result, taxable profits have risen by 10% from £50,000 to £55,000. At first sight, this looks like a healthy increase.
However, our data does not cover, in full, the effects of insurance company fee reductions and increases in growth of Choose and Book business. We would not expect to see such a strong increase for 2015.
There has been little change in costs between 2013 and 2014. Some anaesthetists have increased the salary costs, particularly when employing spouses, to take advantage of the rise in the tax free personal allowances.
Accounting/legal costs seem to have edged up slightly, for no particular reason. Other costs have broadly remained the same.
We are still seeing a continuation in the growth in number of anaesthetic groups. Our view is that being a group member, on the balance of probability, does lead to enhanced incomes.
The growth in provision of pain
We are still seeing a continuation in the growth in number of anaesthetic groups. Our view is that being a group member . . . does lead to enhanced incomes
management services is also an interesting development. Consultants who have chosen to enter this market can, in individual circumstances, earn significant sums. We would expect this trend to continue.
The downside
On the downward side, there was a time when anaesthetists seem to have been ‘picked off’ by insurers. Such activity seems to have reduced in recent months, as insurers turn their attention to other consultant sectors.
The growth in Choose and Book work has also stimulated income, but at generally lower margins.
There does seem to be no stopping the growth of the NHS spend in the private sector. But, sooner or later, we would expect to see the NHS use its buying power to reduce fees. After all, the NHS is now probably in a stronger economic position in the market than many insurers.
We do not believe that costs will change significantly, apart from inflationary increases.
As a result of all these factors, our current view is that anaesthetists’ net taxable incomes in the foreseeable future would probably expect to rise at the level of medical inflation.
There will be a reduction in fees,
Effectively, anaesthetists will have to work harder to generate the same rewards
Year ending 5 April. Figures rounded to nearest
Source: Stanbridge Associates Ltd.






Uniting both the Surgical and Non-Surgical Communities
SURGEONS / COSMETIC DOCTORS / GPs / COSMETIC NURSES / DERMATOLOGISTS / PRIVATE CLINICS / HOSPITALS / DENTISTS

5000+ Visitors
200+ Exhibitors
Non-Surgical Conference
Live Demonstrations
Surgical & Non Surgical Workshops

Aesthetic Nursing Conference
Merz Aesthetic Theatre
Getting Started in Aesthetics Theatre
NEW FOR 2016 Co-located with





@ccr_expo www.facebook.com/ccrexpo1


British Cosmetic Dermatology Group Meeting




















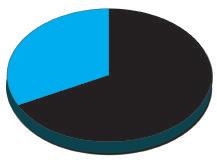
in real terms, although more activity. Effectively, anaesthetists will have to work harder to generate the same rewards.
As we have reported previously, Independent Practitioner Today is ceasing to produce this extremely popular Profits Focus in the current format.
The primary reason is that, with all the changes that have occurred in the market, it is very difficult to provide a realistic year to year comparison.
Our benchmark spotlight on the specialties we have been looking at has never been statistically sig
nificant, but the practical problems of data recording and analysis have become ever more complex.
Changes in the market place have included:
➲ The growth of incorporation as a means of conducting private practice;
➲ The growth of groups – both formal and informal;
➲ The changing gender nature of the private provision of anaesthetic services. There are, for example, an increasing number of
female consultants who are perhaps looking for a better worklife balance than some of their older colleagues;
➲ The significant increase in Choose and Book work. Some consultants who historically would have conducted this work through their private practices are now choosing to work under PAYE – or in some cases as an employee of private hospitals. Given such scenarios, the need to pay professional indemnity premiums, for example, falls;
➲ The growth in pain management services, particularly over the past few years.
Our survey qualifications remain as they have always done.
In this survey, our anaesthetists:
Continue to work in the NHS and are not in full time private practice;
Hold either an old style or a newstyle contract with the NHS;
Have been in private practice for at least five years;
Are seriously interested in pursuing private practice in a business;
Have generated gross income of at least £5,000 for the year end to 5 April 2014;
May or may not have incorporated their business and/or be a member of a formal or informal group.
Years ending 5 April Source:
Make sure you don’t miss our next issue, published on 23 June. You may not receive every issue if you have not yet subscribed to the journal. Don’t risk missing out on vital topics we tackle next month, including:
If you are not taking as much advantage of the growing self-pay market as you should, then it is time to increase your market share.
Gary Nials of Medical Billing and Collection shows how
Specialist medical accountant Vanessa Sanders gives her verdict on whether a company is still a good choice for your private practice
Have you checked your pension and your pay slips? Cavendish Medical has some profitable advice
As HCA’s The Princess Grace Hospital becomes the first private hospital in the UK to use the STRYKER MAKO robot
– the latest innovation in hip and knee surgery – consultant orthopaedic surgeon Prof Fares S. Haddad (right) writes on the role of robotic technology in surgery

Our Practice Builder series ends with a look at the ‘marketing mix’: the team is in place, the hospital(s) chosen, the branding has been established. So what next?
Ten legal pitfalls to beware of when designing your brand
EDITORIAL INQUIRIES
With clinical negligence claims on the rise, to what extent should your decision-making be influenced by the medico-legal climate? The MDU’s Dr Nicola Lennard considers two contrasting scenarios
Judith Hulf, senior medical adviser at the GMC, chaired the group behind the guidance for doctors carrying out cosmetic procedures. She talks about why it was necessary and the impact it will have
Property matters: it is the perfect time to look for a pied à terre on the French Riviera
The private hospitals body hits back at BMA criticism of the independent sector
Thinking of selling your practice? Susan Hutter outlines what you need to know first
In the last of her series, Pam Underdown looks at why 79% of business owners will not survive next year. ‘Playing it safe is a dying strategy. Nothing is safe anymore. Change really is the new normal’
June – time to make changes in your PPU
So what is the keen petrol-head medic to do when funds won’t stretch to a best-in-class open-topped sports car like the Porsche Boxster? Motoring columnist Dr Tony Rimmer finds one that fits the bill
ADVERTISERS: The deadline for booking advertising for our June issue falls on 27 May
Robin Stride, editorial director
Email: robin@ip-today.co.uk Tel: 07909 997340
ADVERTISING INQUIRIES
Margaret Floate, advertising manager
Published by The Independent Practitioner Ltd. Independent Practitioner
Today is editorially independent and thanks Bupa for its assistance with distribution.
Printed by Pepper Communications Ltd
Material is governed by copyright. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form without permission, unless for the purposes of reference and comment. Editorial layout is the copyright of the publishers. If you wish to use it for promotional purposes on websites or for reprints, we would be happy to discuss licensing the copyright to you.
© The Independent Practitioner Ltd 2016
Registered office: 7 Lindum Terrace, Lincoln LN2 5RP
Email: margifloate@btinternet.com Tel: 01483 824094
Publisher Gillian Nineham Tel: 07767 353897.
Email: gill@ip-today.co.uk
SUBSCRIPTIONS
£90 independent practitioners.
£90 GPs and practice managers (private & NHS). £210 organisations.
But if you pay by direct debit, individuals pay only £75, and organisations £180. Call Proact Ltd on 01752 312140
Email: lisa@marketingcentre.co.uk


SAVE ON SUBSCRIPTIONS!
To guarantee your copy of Independent Practitioner Today by taking out a subscription (at the rates shown on the left), phone 01752 312140 or send off a subscription form on page 28 or email lisa@marketingcentre.co.uk or go to the ‘About’ page of our website www.independent-practitioner-today.co.uk
If you pay by direct debit, individuals pay only £75 for a subscription. Just fill in the form on page 28 and send it to the Freepost address shown at the bottom of the form.
BACK ISSUES: £12.50 including post & packaging
Phone 01752 312140 or Email lisa@marketingcentre.co.uk
I’d be in serious trouble without the diary management feature on ePractice manager! It means I can focus on treating patients while my PA is able to coordinate my appointments remotely across the three practice locations.
Ernest Barlow-Kearsley, Total Footcare Solutions


Securely manage your
patient appointments
Healthcode’s ePractice solution provides independent practitioners the ability to manage their clinics online from multiple locations. The appointments solution is designed for both individuals and group practices to ensure efficient organisation for appointments within your practice.
Using ePractice to manage your patient appointments, you can:
• Easily manage and track your appointments
• Access patient appointments from multiple treatment sites
• Generate appointment reports for clinic and theatre lists
• Set up recurring clinic sessions
• Auto-prompt to raise invoice on completion of appointment
Healthcode’s ePractice solution offers:
Patient Billing
Patient Management
Payment Tracking & Financial Reporting
Appointments
Membership Enquiry
Complimentary ePractice App
Experts in Online Solutions for Smarter Healthcare... ‘code for success.