INDEPENDENT PRACTITIONER TODAY
In this issue
Good logo design
Aspects to consider before creating a new logo for your practice P18



Good logo design
Aspects to consider before creating a new logo for your practice P18


Cheap and cheesy social media can ruin your brand
Nikki Milovanovic warns that ‘being on social’ is not the same as being great on it P22

In this issue
Why are we so bad at calling for help?

The first instalment of our serialisation of ‘Beneath The White
by Dr Clare Gerada n See page 48
A non-binary approach is required
Does the Equality Act protect non-binary individuals working in your practice? P32

By Robin Stride
Doctors who were forced to move to the 2015 NHS Pension Scheme have been told they will not need to decide which set of compensation benefits they wish to receive until their time of retirement.
Previously, they were told that they had to choose now.
Results of the so-called ‘McCloud’ consultation released last month, hailed as ‘good news’ by leading specialist medical accountants, concluded that doctors have the right to make a ‘deferred choice’ about which remedy benefits to take.
It can be the pension benefits from their previous 1995/2008 pension scheme or those from the 2015 scheme.
The consultation also explored the option to make an ‘immediate choice’ now of which pension benefits to take for the remedy period, to run from 1 April 2015 to 31 March 2022.
When the 2015 scheme was introduced, older members – those within ten years of retiring – were allowed to continue with their final salary schemes in the 1995 or 2008 sections.
But the Court of Appeal in 2018 found this discriminated against younger members in a case brought by judges (named McCloud) and firefighters.
The Government has now agreed

to redress this discrimination across all public sector pension schemes at an expected cost of around £17bn.
Specialist financial planners Cavendish Medical called it ‘an extremely complicated situation’, but said the consultation outcome was generally accepted to be the better of the two options presented.
Technical director Patrick Convey said: ‘In essence, it means that doctors will be able to choose the most lucrative scheme benefits by way of compensation when they come to retire.
‘This, of course, does not make the calculations of the already fiendishly complex NHS pension any easier. The Government even recognised in the consultation that this outcome will still place an ‘administrative burden’ on the doctors – many of whom have already had the most challenging of years.
‘They could be concerned that the last five years of tax calculations
and annual allowance payments will need to be recalculated. It is also likely that the pension figure they have been working towards is now wrong’.
He told Independent Practitioner Today: ‘In the next few months, we will be working through the finer details of this compensation scheme to ensure the doctors in our care have the best outcome.’
Less welcome is the Government’s conclusion to a related consultation that no further flexibility will be introduced to NHS pension schemes.
Mr Convey said: ‘It is disappointing that the Government received overwhelming feedback from medical and financial professionals in the consultation that confirmed the annual allowance was causing doctors to reduce shifts or retire early, and yet still ruled against introducing some flexibility.
‘For example, this could have

been an opportunity to allow doc tors to change the rate at which their pensions grow in order to mitigate against annual allowance breaches.
‘Instead, the Government stated that the tapered annual allowance rule changes introduced last year were enough to help the workforce crisis. We are not sure that is the case.
‘The rules surrounding pensions and tax charges are still too complicated and excessively punitive for those working hard to help patients.’
n Cavendish Medical is staging a free pensions and tax webinar to help doctors understand the McCloud remedy. See page 4
The BMA, with the backing of thousands of its members, fiercely opposed the pensions changes forcing doctors to move to a new pension scheme in 2015.
Its pensions committee chairman Dr Vishal Sharma said the Government had listened and it was ‘common sense’ for it to opt

for deferred choice, with this crucial decision being made at the time of retirement.
Doctors should not be forced to make an immediate decision on which scheme to be a part of, especially in the middle of a pandemic when they were facing intense career pressure.
He added: ‘It is only at the point of retirement that doctors will have in their possession all of the relevant information from which they can make an informed decision as to what is the best decision for them.’
➱ continued on page 3




TELL US YOUR NEWS. Contact editorial director Robin Stride

Dr Claire Wratten of the MDU analyses clinical negligence claims in private practice and offers advice on managing risk. The first in a new series P14

Email: robin@ip-today.co.uk Phone: 07909 997340 @robinstride
ADVERTISE WITH US. To advertise in the journal or our website business and lifestyle directories, contact advertising manager Andrew Schofield at Spot On Media. Phone: 0161 408 3912
Email: andrew@spotonmedia.co.uk
GET A SUBSCRIPTION DISCOUNT
£90 independent practitioners. £210 organisations. £90 GPs and practice managers (private & NHS).
Save £15 paying by direct debit: individuals £75 (organisations £180).
TO SUBSCRIBE
Email karen@marketingcentre.co.uk
Or phone 01752 312140.
Chief sub-editor: Vincent Dawe
Head of design: Jonathan Anstee
Publisher: Gillian Nineham
Email: gillian.nineham@gmail.com Phone: 07767 353897
Follow Independent Practitioner Today on

With so many doctors increasingly seeing patients via remote and virtual consultations, it is good to see the GMC offering guidance to help the profession deal with some new challenges.
Good practice in prescribing and managing medicines and devices (see page 4) is a 12-page document covering 74 key points.
It has been issued some weeks ahead of 5 April, when it takes effect, to give doctors time to familiarise themselves with the regulator’s standards for good practice when prescribing remotely and face-to-face.
Seeing patients virtually can be efficient and convenient for doctors and patients. It is clear that it will carry on for certain consultations in many private doctors’ practices long after lockdown has ended.
But as the pandemic continues, telemedicine is also bringing mounting concerns to some practitioners who are worried about the long-lasting effects of
telemedicine on their professional practice (see page 8).
With the escalating use of remote consultations, it is distressing to hear that most doctors fear they run a greater risk of future claims if things go wrong.
Three-quarters are now more worried about missing a condition they would have spotted in a face-to-face encounter.
As many as 70% of doctors working both health sectors told a defence body’s survey that they had concerns about the increased use of telemedicine.
Twenty per cent believe all consultations should be done remotely in the future unless there is a compelling reason not to.
But others fear virtual consultations present greater medico-legal risks than talking to patients face-to-face. They are rightly worried about telemedicine’s limitations and potential security issues.
Let us know your views by emailing robin@ip-today.co.uk

Safety knows no boundaries
Prepare for a busy year ahead on safety and regulation in the private sector, says the boss of the Independent Healthcare Providers Network P21

Qualities you need to take the lead
Jane Braithwaite looks at the attributes required to be a good leader in private practice in her series on managing people and teams P24


IT takes the pain out of invoicing
Experienced practice manager Desné Marston explains how Healthcode’s Clearing Service effortlessly achieves accurate and prompt billing P28
Billing matters whatever your size
Doctors, groups, clinics and hospitals all experience difficulties with their billing and collection. Simon Brignall looks at the scale of the problem P35

Long-term drugs need monitoring Diane Baylis of the MPS advises on how to manage caring for patients with long-term conditions, citing the pitfalls from the society’s case files P40
OUR REGULAR COLUMNS
Doctor on the Road: The new Golf has driving down to a tee
It’s back! Dr Tony Rimmer tests the latest version of an old favourite that has wooed doctors for decades P44
Starting a private practice: Ten reasons to fail in private practice
Ian Tongue highlights the key areas that can be a sure-fire way to hit snags in running a practice P46
Profits Focus: Cinderella to princess?
Profits for radiologists have shown a welcome rise –despite heavier costs in this specialty P51
By Edie Bourne
Specialist medical accountants have welcomed the Government’s pensions announcement of a deferred choice option as ‘good news’ for those doctors affected.
The thumbs-up came from Stanbridge Associates whose partner Vanessa Sanders recommends doctors avoid any knee-jerk reactions and wait for further information on this complex area ‘to which no one yet has all the answers’.
Rulings mean:
1. Eligible members who were moved to the reformed pension scheme in 2015 – or later if they had tapered protection – will be moved back into their legacy pension scheme for the period when discrimination occurred, between 1 April 2015 and 31 March 2022.
2. When benefits are paid at retirement, they will get information to enable them to choose to receive legacy pension scheme benefits or benefits equivalent to those available under the reformed pension scheme for service between 2015 and 2022, when all members will be transferred.
3. Deferring the choice until the point benefits are paid allows individuals to decide which pension scheme is more beneficial, based on facts rather than assumptions. The level of both pension scheme benefits will be known at retirement.
4. From 1 April 2022, all who continue in service as active members of the pension scheme will become members of the reformed scheme, regardless of age, so there will be no discrimination on those grounds.
Mrs Sanders said meaningful interaction with the tax system had to wait until the law was changed and it was clearer how the deferred choice underpin would affect aspects like pension savings’ growth and excess tax charges.
Many would be concerned about possible changes to their annual allowance tapering, tax charges arising due to having excess growth in excess of the allowance, and of being a member of more than one pension scheme.
But at this point there was little to be gained from performing iterative calculations about estimated pension growth in the legacy scheme compared to what had happened. Doctors were not yet in a position to make any changes to their choices, as the legislation had not yet come into effect.

Accountant Vanessa Sanders of Stanbridge Associates
She said there were tax consequences resulting from the proposed changes, such as different levels of pension contributions being deducted by a change in scheme.
Complexities meant tax paid might be more or less than had been notified to HM Revenue and Customs and could need rebalancing.
Some who had voluntarily elected for private pension schemes to pay their excess tax charges might need compensation to be placed in a similar position to before the discrimination caused a reduction to their pension pot.
continued from front page
The BMA says the Government’s pension remedy fails to compensate doctors who have suffered.
Dr Vishal Sharma, BMA pension committe chairman, said he was worried at a failure to ensure that those who made decisions based on the age discrimination could rectify this.
‘Doctors may have opted out of the scheme, taken early retirement, cancelled added years contracts or decided to work part-time, with knock-on effects to their pension entitlement.
‘The Government has said that these decisions will be assessed on a case-by-case basis, requiring doctors to prove that these decisions were made as a result of the discrimination.
‘This puts all of the onus on individual members and is a huge
administrative burden for doctors when they should be focusing on patients. The approach should be far more streamlined, giving automatic eligibility to members in certain circumstances to purchase any pension entitlement lost as a result of these decisions.’
A new partnership will see King Edward VII’s Hospital provide advanced breast care services to patients for the yet-to-be opened 184-bed Cleveland Clinic London.
The deal, bringing together two not-for-profit healthcare providers, means that women having consultations at the US complex will have access to the independent charitable hospital’s facilities for diagnostics, screening and treatment.
Cleveland Clinic London opens its first outpatient centre at 24
Portland Place, in the Harley Street Medical Area, this September and its hospital is due to open early next year in Grosvenor Place.
The comprehensive service at King Edward VII’s Hospital includes a Breast Health Centre , offering triple assessment breast screening, reconstructive and oncoplastic breast surgery.
Cleveland Clinic London’s boss Dr Brian Donley said: ‘Cleveland Clinic celebrates its 100th anniversary this year and as we prepare to
welcome our first patients in London, we are proud to partner with other high-quality providers to deliver the best possible care.
‘King Edward VII’s world-leading expertise in breast care will ensure that our patients receive the best preventative care and treatment.’
Lindsey Condron, chief executive at King Edward VII’s, said it was committed to providing the highest quality in women’s health services, ensuring women can access healthcare as a preventative
measure as well as when intervention is needed.
He said: ‘There is clear synergy in the values of the two organisations and we’re proud to be partnering with Cleveland Clinic London in creating a seamless patient pathway that gives women greater access to the highest standards of care.’
Services offered by Cleveland Clinic London’s Outpatient Centre will include in-house GPs, bespoke health assessments and specialist consultations.
By Douglas Shepherd
Updated GMC prescribing guidance, effective from 5 April, aims to support doctors who are increasingly seeing patients via remote and virtual consultations.
Good practice in prescribing and managing medicines and devices sets out the regulator’s standards for good practice when prescribing remotely and face to face.
It also covers when prescribing unlicensed medicines and for when patient care is shared with another doctor.
The guidance makes clear that the same standards remain when prescribing remotely as they do when seeing a patient face to face, such as being satisfied that an adequate assessment has been made, establishing a dialogue and obtaining the patient’s consent.

Key updates include:
New advice for doctors not to prescribe controlled drugs unless they have access to patient records, except in emergencies;
Stronger advice on information sharing, making it clear that if a patient refuses consent to share
information with other relevant health professionals; it may be unsafe to prescribe;
Alignment with the GMC’s updated Decisionmaking and consent guidance, highlighting the importance of good two-way dialogue between patients and doctors in all settings.
Specific advice is also given for doctors prescribing remotely for patients overseas and those in nursing homes or hospices.
GMC medical director Prof Colin Melville called remote medicine ‘a new reality’, adding: ‘It’s vital that the principles of good practice apply, whether a consultation is face to face or remote.’
Good practice in prescribing and managing medicines and devices is available online.
See ‘Doctors fear perils of remote consultations’, page 8
The new prescribing guidance from the GMC makes no distinction between private and NHS prescriptions, but in several areas it advises doctors on how they can work safely when not the patient’s regular prescriber – which might be the case for independent practitioners.
Although the council has advised previously on remote prescribing, this was only in a small section of its previous guidance.
According to Dr Caroline Fryar, advisory services head at the Medical Defence Union (MDU), remote prescribing is now referred throughout, as it is such a prominent modality.
She highlights these key passages for independent practitioners:
The importance of a dialogue with the patient;
The considerations required if the prescriber has no access to the medical records;
Do not prescribe controlled drugs or medicines liable to abuse, overuse, misuse or addiction without access to patient records other than in rare, specified circumstances (para 60-61 of the guidance);
The importance of sharing information with other health care professionals, with consent.
Dr Fryar said: ‘With many consultations moving online during the pandemic, doctors have become even more adept at assessing patients virtually.
‘Prescribing as part of a remote consultation is often entirely safe and reasonable as long as the prescribing doctor has enough information about the patient, can make an adequate assessment and have a proper dialogue with the patient.

‘However, as ever, doctors need to apply their judgement and remain alert to situations in which a face-to-face consultation may be needed.’
She added that prescribing to patients overseas presented ethical and legal difficulties and doctors needed to consider if they had appropriate registration and indemnity.
‘NHS Pensions and Tax – What you need to know’ is a free webinar for Independent Practitioner Today readers on Wednesday 10 March, 6.30pm.
Advisers from specialist financial planners Cavendish Medical will discuss:
Current NHS pension benefits and recent changes;
2015 pension scheme age discrimination ‘remedy’ choice;
The impact of NHS annual and lifetime allowances, and changes to the tapered annual allowance;
Pension tax payment options;
Recent changes to Clinical Excellence Awards;
Other income sources – tax planning and pension savings.
Cavendish Medical director Dr Benjamin Holdsworth said: ‘It is difficult to imagine the NHS pension and its impact on tax positions becoming more complex, but last month we saw the conclusion of two key consultations which will directly affect pension scheme members.
‘For many, these new issues to consider will prove burdensome, particularly as they come at a time when the profession is still being truly tested after the most challenging of years. Doctors simply do not have the time to study the rules and nuances of every regulatory change.
‘In addition, there are also deadlines to remember. Those wishing to claim the tax rebate offered by the Government for annual allowance charges in 2019-20 must ensure they have applied for Scheme Pays to settle the tax charge initially, as well as completing the correct application form.
‘We are hosting the webinar to explain these issues in more detail as well as other key financial points you should be considering as part of your overall financial plan.’
The main presentation will last around 45 minutes plus 15 minutes for questions at the end. To register your attendance, go to https://cavendishmedical.com/ webinar-nhs-pensions-and-tax10th-march/
By a staff reporter
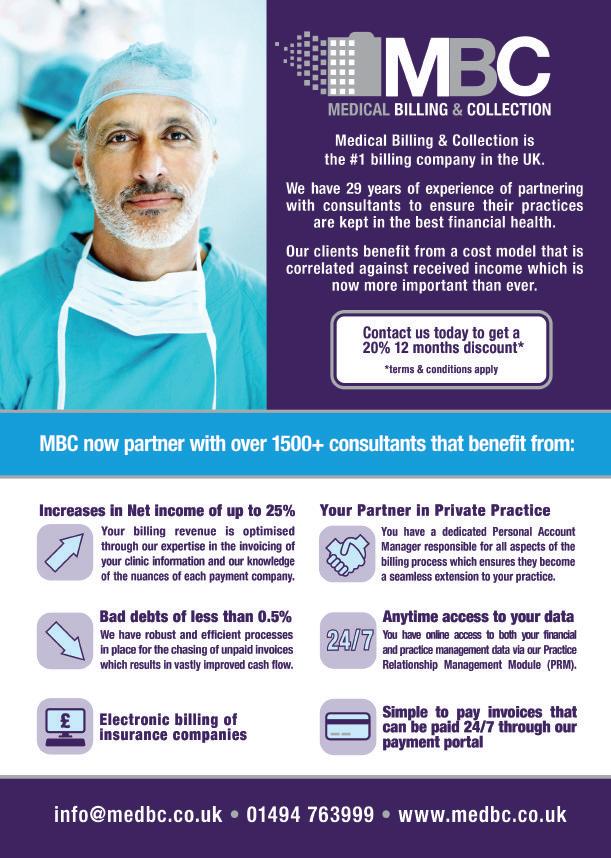
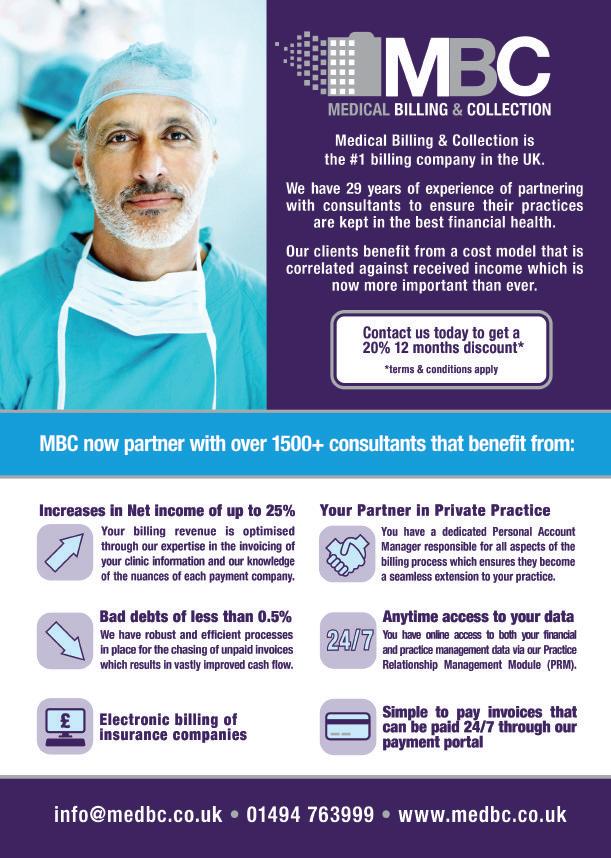
Civica, a global leader in software for public services, has completed the acquisition of Medical Billing and Collection (MBC) from ICS Global.
The acquisition is predicted to help MBC drive improved operational efficiencies for its independent practitioner clients through innovation around data, automation and new technologies.
Civica said its strategy and focus provided a foundation for growth and innovation, as well as supporting the billing arm to respond quickly to evolving customer needs and market developments.
The acquisition will strengthen its position in the UK health and care market, adding new medical billing and collection capability to help customers manage efficient billing and recovery of debt.
MBC’s experience complements
Civica’s existing health and care solutions and provides an opportunity for growth. The combined business supports annual care billing across the group of over £3bn.
MBC executive chairman Garry Chapman told Independent Practitioner Today : ‘We are delighted that the legal process has completed, and we are now part of the Civica family. We had been approached by several companies over the years and we rejected those approaches, as we felt that they could not add value to our business.
‘With Civica, it was obvious from the start that not only could they add value but also the way that they worked and treated their employees was an excellent match.
‘Their experience in the healthcare market combined with their skill set in software development and automation will further enhance our ability to adapt to the
ever-changing healthcare market and provide an even better service to our existing and future clients.
‘Their expertise in assisting companies to grow will help take MBC to the next level, which will benefit our clients, our staff and the existing management team.’
Civica chief executive Wayne Story commented: ‘The acquisition will mean we can offer even broader solutions to our combined care customers.
‘At a critical time for care services around the UK, we look forward to supporting the sector with improved efficiencies and ultimately better patient care.’
Civica said it saw MBC as the UK’s number-one medical billing service provider to the independent healthcare sector.
Founded in 1992, the Buckingham shire-based company currently works with around 1,500 consultants spread across many

specialties including groups, clinics and hospitals.
Its tailored medical billing and collection services cut bad debts to an average of 0.5%, improve operational efficiency leading to an increase of net income by up to 25% and free up more time for care professionals to focus on patients.
Civica, one of the UK’s largest software companies, has over 30 years of expertise in delivering improved outcomes for public services worldwide.
It delivers software solutions to over 500 customers across the NHS and private care sector globally, from electronic prescribing and patient records to enhanced workforce efficiency. The company provides cloud delivery to over 20,000 clinicians.
www.civica.com
Employees are keeping silent about their mental health conditions at work during the pandemic – even though their job has been a contributing factor for many.
A study of 3,614 employees by Bupa in partnership with Business in the Community found that only 14% of workers disclosed to their manager that they were suffering from a mental health issue.
And a third of people who have experienced work-related mental ill-health have told no one, with men significantly more likely to keep their condition a secret (35%) compared with women (26%). Work-related pressure in the pandemic was identified as the most common cause of mental health issues (51%), while another 35% put symptoms down to workload, long hours and not taking leave.
A third of participants said their mental ill-health was caused by not being supported in their role, potentially an indication of their reluctance to share their circumstances.
Bupa is now expanding access to mental and behavioural health platform SilverCloud for its corporate customers at no extra charge via Bupa Touch, its online customer portal.
SilverCloud supports employees in developing resilience and wellbeing strategies, helping prevent everyday mental stresses and strains from developing into more serious issues.
Bupa and SilverCloud has previously partnered to offer selected mental health services, but this is the first time the healthcare company is offering SilverCloud to its

entire base of corporate health insurance customers at no extra charge.
Mark Allan, commercial director at Bupa UK Insurance, said: ‘Although mental health has come to the fore during the global pandemic, and addressing these issues is a priority for many businesses, the research shows that a good number of employees feel uncom-
fortable turning to their manager for help.
‘While businesses around the country are focused on creating cultures that are open about mental health, it can be difficult for workers, especially when working remotely, to have these kinds of complex conversations.
‘SilverCloud offers a digital route for these employees to seek mental health support and take further action, if needed.’
➲ Don’t miss our new book serialisation starting in this issue: Beneath
The White Coat –doctors, their minds and mental health, edited by Dr Clare Gerada. See page 48

Private healthcare providers have welcomed a recognition in last month’s NHS White Paper that patients will be able to choose from a wide range of healthcare providers so long as they meet health service standards.
David Hare, chief executive of the Independent Healthcare Providers Network (IHPN), said: ‘It is clear that independent healthcare providers will continue to be vital in supporting the NHS over the coming years by improving access and efficiency in NHS care.
‘We want to see this sit alongside models of integrated care which bring the best of public, voluntary
and independent sector providers together to deliver great care to NHS patients and to avoid what the former Health Secretary Jeremy Hunt described as ‘cosy local monopolies’.
NHS performance figures last month showed record long waits with almost 225,000 people waiting more than one year for vital NHS treatment.
Mr Hare said the Government’s proposals for NHS reform must be judged not only on whether they ensured patients receive integrated, joined-up care, but also that they gave patients quick access to diagnosis and treatment.
In the first 11 months of the pan-
demic, independent sector providers treated millions of NHS patients, including 2.5m under the unprecedented contract putting all independent hospital capacity at the disposal of the health service.
Mr Hare added: ‘We will look closely at proposals for a new provider selection regime where patients and taxpayers alike will want assurances that the NHS will have access to the best and most innovative services regardless of who provides them, and that poorly performing services will be challenged to improve, including through the option of alternative provision.’
Independent healthcare providers have delivered over 100,000 cancer treatments for NHS and 35,000 for private patients during the pandemic, according to the Independent Healthcare Providers Network (IHPN).
The NHS patients’ data covers the end of March 2020 to the beginning of January 2021, while the private patient figures cover from April to October 2020.
For NHS patients, this included around 50,000 chemotherapy sessions, 15,000 cancer surgeries, 20,000 cancer diagnostics tests, 5,000 cancer endoscopies and 10,000 cancer imaging procedures
IHPN said independent providers continue to support the NHS including delivery of urgent cancer surgery and chemotherapy, while also treating growing numbers of private cancer and other patients.
Its chief executive, David Hare, added: ‘As part of the historic agreement with the NHS, I’m proud of the role that independent providers have played in ensuring cancer treatment could still continue during Covid-19 with the delivery of almost 100,000 cancer surgeries, chemotherapy sessions and cancerrelated diagnostic tests and endoscopies delivered to NHS patients.’
See David Hare’s article on p21
Ophthalmic Consultants of London (OCL) has been joined by a leading practitioner of adult vitreoretinal surgery, Mr Chien Wong. He is also a consultant ophthalmologist at three major NHS hospitals in London: Moorfields Eye Hospital, The Royal Free Hospital and Great Ormond Street Hospital for Children (GOSH).
Mr Wong has been credited with transforming the surgical treatment of complex retinal detachment in premature babies
and, in recognition of this achievement, was appointed head of the UK national centre for retinal detachment in premature babies at GOSH.
He is the seventh consultant and first vitreoretinal surgeon to join the OCL partnership in the Harley Street enclave.
The private clinic reports ‘a significant increase in demand’ since the start of the pandemic, as Covid-19 forced the NHS to cancel thousands of ‘non-essential’ eye operations.


Surgeons have warned that private healthcare has no hope of dealing with mounting NHS waiting lists.
Responding to a report from the think tank Reform called ‘What’s next for the NHS?’, Royal College of Surgeons of England (RCSE) president Prof Neil Mortensen said: ‘So long as we are still caring for thousands of Covid patients in NHS hospitals, then yes, we will need continued access to the independent sector’s separate sites.
‘But there isn’t enough private sector capacity to deal with the huge surgical backlog, which could be as high as 10m patients, as this report suggests.
‘We need a “new deal” for surgery with investment in NHS capacity, to get back to meeting legal waiting times standards.’
The RCSE agreed with the spirit of a report recommendation that ‘NHS England and Improvement should mandate the publication of wait list recovery plans by integrated care systems and trusts’.
But Prof Mortensen said this lacked ambition in only referencing use of independent sector capacity.
Health service commentator Roy Lilley wrote on his nhsManagers.net blog: ‘Some say there could be as many as 10m people waiting. The fact is, we don’t know.
‘Whatever the number, we know it’s a lot, so treat it like the national emergency it undoubtably is.
‘Forget the private sector; it’s boutique and we need industrial. Anyway, it sucks NHS staff out of the system. They have 8,000 beds and little emergency back-up if something goes wrong.’
By Vanessa Sanders
Independent practitioners whose businesses deferred VAT payments last year can now join a new online VAT Deferral New Payment Scheme to pay it in smaller monthly instalments.
Private doctors do not generally need to pay this tax, but some are registered for VAT if, for example, they provide medico-legal services.
These specialists may now be struggling with cash flow, particularly if they are not using a cash accounting scheme for making returns and are paying VAT on invoices sent to their clients for which they have yet to receive payment.
With effect from March 2020 when the pandemic hit with the first big lockdown, VAT-registered businesses were allowed to defer their VAT payments to help with this lack of cash flow.
The Montefiore Hospital in Hove, Sussex, has unveiled the newest member of its surgical team – a fivefoot robot which will assist in knee and hip replacement operations.
Called Mako and made by Stryker, it is the first robot to be used by the hospital and the first of its kind in the Sussex area.
The hospital said it was the only robot which can be used in all three joint replacement procedures – partial knee, total knee and total hip replacement.
Now the Government has decided to open a new deferral opportunity provided businesses have met their obligations under the first scheme by the time they decide to enrol.
This means the business must have paid the deferred VAT from the first scheme in full, on or before 31 March 2021, before joining the new scheme.
If you decide to enrol your business in the new deferral scheme, you may do so using HM Revenue and Customs’ (HMRCs’) online facility available between 23 February 2021 and 21 June 2021.
Joining allows you to:
Pay the deferred VAT in equal instalments, without the attachment of interest, and;
Choose the number of instalments, depending on when you join the scheme.
The table above from HMRC sets out the monthly joining deadlines
Date to join by: Number of instalments: 19 March 2021 11
and the corresponding number of maximum instalments, including the first payment, which must be made upon joining.
How to join
You must:
➤ Join the scheme yourself by creating a Government Gateway account (www.gov.uk/log-in-register-hmrc-online-services) and although you may ask for assistance to complete the VAT returns and subsequent submission, your accountant cannot join the scheme on your behalf;
Consultant knee surgeon Mr Sandeep Chauhan said: ‘It allows for incredible precision, as the 3D plan means you cannot deviate from that path which avoids the removal of healthy bone tissue.

‘This is extremely exciting for me and my fellow orthopaedic surgeons and very good news for patients, as this precision means less trauma during surgery, reduced pain after surgery and improved recovery.
‘This robot will revolutionise hip and knee replacement surgery at The Montefiore.’
Vanessa Sanders is a partner with accountancy, finance and tax advisory medical specialists Stanbridge Associates Ltd
➤ Be up to date with your VAT returns, including correcting any errors from previous periods to enable you to quantify the VAT you wish to defer;
➤ Pay the first instalment when you join;
➤ Pay the instalments by direct debit.
If you will be unable to meet your obligations for payment under the first scheme or you are unable to set up a direct debit, you may contact HMRC to discuss.
The VAT helpline is 0800 024 1222.

By Leslie Berry
Doctors have expressed fears about the long-lasting effects of telemedicine on their professional practice.
Three-quarters are now more worried about missing a condition they would have spotted in a faceto-face encounter.
With Covid-19 escalating the use of remote consultations, most fear they are at greater risk of future claims if things go wrong.
Seven in ten doctors in NHS and private practice told a defence body’s survey they had concerns about the increased use of telemedicine. They agreed the associated medico-legal risks are greater than with face-to-face consultations.
Only one in five doctors agreed that all consultations should be done remotely in the future unless there was a compelling reason not to.
The profession was completely split down the middle over security issues arising from remote consultations. 45% said they were worried about privacy and confidentiality while 45% were not.
One in five doctors in the MPS
survey of 1,250 NHS and private doctors admitted they struggled with telemedicine due to their own digital literacy or ability to use technology.
The defence society said the Government and healthcare system should take a long-term strategic approach when it comes to the role of virtual care beyond the pandemic, taking account of doctors’ concerns, patients’ experiences, and research on digital inequality.
Medico-legal lead Dr Pallavi Bradshaw said there were concerns around telemedicine’s limitations, the need for support and training due to the different skills required and the desired role of virtual care beyond the pandemic.
Many doctors were concerned about the potential for medicolegal disputes and investigations, she said. ‘A key concern for doctors is the potential for vulnerable patient groups to be left behind and for health inequalities to grow, if there is desire for more patient consultations to be delivered online after Covid-19.’
Tell us your views on the use of telemedicine in your private practice. Email robin@ip-today.co.uk
The following statements were provided. Optional answers were: ‘strongly disagree’, ‘tend to disagree’, ‘strongly agree’, ‘tend to agree’ or ‘don’t know’. The agree and disagree answers have been combined:
The benefits of telemedicine have been unquestionable and it will remain a fundamental tool in practice. Agree: 70%, disagree: 19%
I am more worried about a claim or investigation arising from a remote consultation with a patient,than a face-to-face encounter.
Agree: 60%, disagree: 30%
I am more worried about missing something in a remote consultation. Agree: 76%, disagree 13%
I struggle with telemedicine due to my own digital literacy/ability to use technology. Agree: 20%, disagree: 69%
I believe the medico-legal risks associated with telemedicine are greater compared to face-to-face consultations. Agree: 70%, disagree: 19%
I am worried about privacy/confidentiality and security issues with telemedicine. Agree: 45%, disagree: 45%
I have no concerns around the increased use of telemedicine, and all consultations should be done remotely in the future unless there is a compelling reason not to. Agree: 19%, disagree: 70%
We should stop thinking of telemedicine as a different kind of medicine; it is just medicine delivered in a different way. Agree: 61%, disagree: 28%
If consultations are to become predominantly online, I am worried that some patient groups may be left behind – for example, due to age, disability, low income, digital literacy, language, internet access, location. Agree: 83%, disagree: 6%
If some patients feel excluded from telemedicine, I am worried about a potential breakdown in the doctor-patient relationship or conditions being left untreated. Agree: 80%, disagree 9%
Over half of independent practitioners (56%) told a survey they are concerned about facing investigation if delayed referrals harm patients or non-Covid-19 services are unavailable or limited.
The MPS questionnaire of 530 private doctors follows a Macmillan report estimating around 50,000 ‘missing’ cancer diagnoses in the UK.
A ‘significant’ number of claims, complaints and investigations are expected by the defence body where delayed referrals have seriously impacted on patients’ prognoses and outcomes due to circumstances beyond their doctors’ control.
The MPS wants emergency laws to protect healthcare workers from unfair investigation.
Medical director Dr Rob Hendry said: ‘We are also concerned about how clinical negligence claims – directly and indirectly related to Covid19 – will be handled. The current legal tests for breach of duty and causation will need to be applied fairly and robustly given the rare and extreme circumstances of the pandemic.
‘There is no precedence for what is acceptable or reasonable in such circumstances, including the direct impact of Government policy on patient care both in the public and private sector.
‘Similarly, expert witnesses will be challenged in offering opinions given that healthcare systems and usual practices have been so dramatically disrupted.

‘The court and judges will ultimately be tasked with dealing with these claims fairly, but it is important that these issues are recognised and debated so the process is fit for purpose.’
A membership scheme from Rutherford Health, offering access to advanced cancer treatment and care, is the first healthcare plan in the UK to focus exclusively on comprehensive cancer cover.
Rutherford Direct offers customised membership plans to cover people diagnosed with cancer for the cost of treatment across a wide range of conditions at various independent healthcare providers.
Plans start at £29 monthly.
Chief executive Mike Moran said: ‘It’s vital we continue to develop greater options for patients who often have to wait too long for treatment and to offer a healthcare plan that gives them reassurance and certainty that they will be taken care of as they deal with their illness.’
Rutherford Cancer Centre North West, in Liverpool, has installed a Magnetic Resonance Linear Accelerator (MR Linac) system for delivering precise radiotherapy and treating hard-to-reach tumours.
By Olive Carterton
Independent practitioners who have staff working from home have been served a reminder of the importance of investing effort into ensuring it is successful for all.
Seven out of ten employers and six in ten employees agree the pandemic has changed their relationship.
But as many as one in three employees warn Covid-19 has weakened their relationship and their all-important sense of belonging – and that is significantly impacting productivity, according to a report.
MetLife UK research found that with two in five (41%) office workers primarily working from home, there had been a fall in collaboration and social interaction among colleagues, representing a decline in that all-important sense of community.
Two-thirds (67%) of employers confirmed their current employee benefits packages are being changed to support employees’ needs.

The Institute of Sport, Exercise and Health (ISEH) has announced the launch of an Elite Sports Concierge Service through a partnership with HCA Healthcare UK.
Under the leadership of Prof Fares Haddad, Mr Sam Oussedik and Prof Mathew Wilson, the service provides rapid-access medical services to high-acuity patients in the acute care setting.It also offers a single point of contact for priority entry, supporting elite athletes and Premier League football clubs. The institute said HCA was
uniquely placed to offer a broad spectrum of experts and specialties in the event of a medical emergency.
Access to the service is contingent upon membership, which offers sports clubs and institutions:
Multidisciplinary care from HCA UK’s leading consultants;
Rapid access to diagnostics and treatment;
Intensive care facilities to support complex care;
Seamless VIP pathway into The Princess Grace or the Wellington hospitals and specialist clinics;
Company director Adrian Matthews said: ‘The pandemic has undoubtedly shifted the dynamic between employers and their employees. It has not only revolutionised how and where we work, but it has also left many people missing the less tangible aspects of office.
‘Homeworking has removed many of the cultural, emotional and communications bonds employers have spent decades establishing.
‘And our research shows how this has resulted in significant erosion of how cared for employees’ feel by their employer and their sense of “belonging” – a reality experienced across companies of all sizes.’

How to be a flexible working winner! Turn to page 20 of our February issue to read our feature article on home working


Cover for all athletes and staff aged 18+ officially registered with the club and players’ immediate families;
Dedicated support from an Elite Sports concierge manager.
ISEH clinical director Prof Haddad said: ‘We have designed the service to facilitate the immediate and early management of athletes who require urgent medical attention in order to ensure a smooth path to recovery so that they can return to competing as quickly as possible.’
Market analyst LaingBuisson has launched the second edition of its Digital Health UK Market Report.
Report author Martin Bell said: ‘Covid-19 has undoubtedly accelerated digital transformation in healthcare and technology is being used more than ever.
‘This offers the opportunity for healthcare providers to transform their services, not only in terms of efficiency but also offering patients choice. This, in turn, creates opportunities for investors and suppliers.’
Take-up of new technology during the pandemic was beyond expectations at this time last year, but he said there remained the challenge of using and scaling existing technologies and ensuring their penetration across all areas of the market.
The report contains the latest data on a range of existing and legacy technologies in UK healthcare, including patient admission systems (PAS), electronic patient records/electronic medical records (EPR/EMR), specialist clinical systems, digital apps, wearables, artificial intelligence, interoperability across systems and sectors, pathology and radiology.

Dr
Harriet Leyland
Independent GP booking and healthcare management app ‘myGP’ has appointed Dr Harriet Leyland as clinical adviser. She also runs her own healthcare consultancy and advisory business, HML Health.

A look back through our journal’s archives of a decade ago reveals that although times change, some issues are not so new


London was making it very difficult for potential private patients to access health, according to cancer specialist Prof Karol Sikora.
He reached the conclusion after ringing hospital switchboards one evening saying he was a 60-yearold man from Dubai and where could he get a prostatectomy.
Only one of the four hospitals he contacted helpfully offered to ring back.
But, he added, ‘they didn’t, of course.’
Prof Sikora told a conference that to ‘sell’ London to potential patients was ‘dead easy.’
The difficulty was that the right administrative structure was not there, he concluded.
Independent practitioners’ longrunning battle with the taxman over recognition of mileage claims between places of work received a huge lift following a new tax ruling.
Accountants said the case implied independent practitioners could argue they had a home base if they:
Had no permanent office space at their private hospitals;
Organised their work from home;
Maintained an office there;
Received business correspondence at that address.
If the home was the office, travel to a private work appointment would be allowable against tax along with travel from NHS places of work to a private hospital.
We wrote that this could potentially improve the profits of an estimated 13,000-15,000 doctors, including around 70 consultants known to be locked in arguments with the taxman about mileage claims.
Private patient power was putting practitioners under pressure to improve non-clinical aspects of their performance or risk losing business to other consultants.
Only 55% of patients would definitely recommend their specialist to others – compared to 85% four years previously, according to a new survey by an independent marketing agency commissioned by private practice management specialists PHF Services.
Its director Richard Gregory said: ‘Industry players always refer to increasing patient choice, but our research warns that they are also expecting better service. Consultants and hospitals should be concerned.’

The survey showed patients were harder to please, expected more value for their money, and were less tolerant of shoddy service, especially appointments punctuality.
Conference quote from consultant spinal surgeon Mr Khai S. Lam –who was treating embassy patients in the UK, among others, and ran three clinics a year in Kuwait – ‘Learn a bit of their language and book your holidays for when they are celebrating their religious festivals.’
Don’t
Cosmetic surgery patients were being urged to research costs. Plastic surgeon Mr David Crawford said: ‘If a price sounds too good to be true, it generally is.’ He warned patients not to be pressurised into committing to surgery because of a special offer. Hospitals should offer a fixedprice package to include their fees, surgeons’ and anaesthetists’ fees, implant costs and all aftercare, including dressings, he said.
Independent practitioners were being warned to be vigilant following a surge of fake phishing emails sent out by fraudsters. The email informed the recipient they were due a tax rebate and provided a click-through link to a replica of the HM Revenue and Customs (HMRC) website.
Share your experience of what has and has not worked in your private practice. Even if it’s bad news, let us know and we can spread the word to stop others falling into the same pitfalls.. Contact editorial director Robin Stride at robin@ip-today.co.uk




Our A-Z of top tips from accountants to doctors continues as Julia Burn (left) turns to the letter S
SPRING IS in the air and, thankfully, there seems to be light at the end of the tunnel.
As lockdowns begin to be relaxed and a bit of our old life resumes, businesses can hopefully get back to some form of normality, albeit in potentially a completely different format to previously.
During the pandemic, the Government has offered various measures to support businesses, including the furlough scheme, which, during the Budget on 3 March 2021, has been extended to September 2021. Other support measures include the Coronavirus Business Interruption Loan Scheme
(CBILS) and bounce-back loans, which are coming to an end at the end of March to be replaced by the Recovery Loan Scheme, which currently runs to 31 December. Details of this loan scheme are pending clarification.
HM Revenue and Customs (HMRC) has also offered deferral of payments of certain taxes, which, although helping with immediate cash flow issues, can just push the problem further down the line and create worse headaches when the original liability becomes due at the same time as the next liability.

So it is necessary to consider what other support is available for businesses to ensure they can recover from what has been a very difficult period for many.
Alternative areas of support Keeping on top of accounting and finance records will be an even more important task than usual to ensure that any issues arising are dealt with quickly and to ensure that they do not affect the smooth running of the practice.
Many accountants offer outsourcing solutions. These provide a back-office function, keeping your financial records up to date and leaving you the time and resources to concentrate on the day-to-day running of the practice and what you do best.
The future of businesses are uncertain and the ongoing effect of the pandemic cannot be accurately anticipated. It is important to maintain up-to-date information to allow quick decisions to be made to keep expenditure controlled and cut costs when necessary.
Maintaining cash flow forecasts will give a reliable way to make sure that any pinch points are identified quickly so they can be dealt with appropriately. Your accountant will be able to assist with cash flow forecasting for the business.
Where a private practice has had to fully or partially close, getting back up and running again could be costly in terms of keeping both
In a new series for Independent Practitioner Today, Dr Claire Wratten (below) analyses clinical negligence claims in private practice and offers advice on managing risk. This month: anaesthetists


MEDICAL NEGLIGENCE claims in anaesthetics are relatively uncommon, but, of course, if you are facing a claim, it can be very distressing.
At the MDU, our expert claims handlers and medico-legal advisers understand how stressful this can be and the importance of mounting a robust defence of your position.
In our experience, common causes of claims against anaesthetist members working in inde -
pendent practice include dental damage, which accounted for a third of all notifications, drug errors or adverse reactions, and needle misplacement.
While few cases result in compensation being paid, it is nonetheless better to avoid a claim altogether.
This article looks at the main themes cited in 170 clinical negligence claims notified to us by members and suggests way to manage medico-legal risk factors.
Compensation costs millions In almost three-quarters of cases reviewed (73%), the claim was successfully defended without any payment of damages or claimant legal costs.
Of cases settled, compensation payments ranged from under £1,000 to over £2.6m. The average cost of each settled claim was well over £100,000, with some claims resulting in compensation payments of over £1.5m each.
The size of the compensation
While the number of claims brought against anaesthetists while working in private practice has not increased significantly in the past few years, the cost of claims has spiralled
Ensure the patient has given fully informed consent before being anesthetised. For example, patients should understand why a treatment is necessary, the risks involved and any alternatives. This discussion should be documented in the notes.
Record any warnings given pre-operatively, such as of a sore throat post-operatively or of some awareness during sedation.
If there are additional risk factors for a particular patient, such as the risk of dental damage, you should discuss them and document them in the records.
Try to avoid giving the impression that the cost of repairing dental damage will automatically be met.
Develop a regular routine for pre- and postoperative assessments. Make a note of your assessments in the records.
Check the past medical history, known allergies and concurrent medication before prescribing any drug.
Document that you have checked pressure points and ensure those assisting you are aware of the risks to pressure points.
Make sure procedures are in place to eliminate the risk of ‘wrong side’ errors, such as checking the patient’s clinical record and consent form and confirming details with the patient.
Consider your professional duty of candour. If something goes wrong, apologise and notify the patient and any necessary parties as soon as possible.
does not reflect the magnitude of the clinical error, but rather the injury to the patient.
If the person can no longer work and requires a significant level of care, then considerable sums may be paid. For example, neurological injury or spinal cord damage leading to significant disabilities.
The risk of damage to teeth and dental work when using a metal laryngoscope is well known and was the primary reason for the claim in a third of cases analysed.
Risk may be greater where the intubation is particularly difficult, either for anatomical reasons or because of circumstances.
Difficult intubations cannot always be anticipated and, in an emergency setting, securing the airway as quickly as possible may sometimes be necessary even at the expense of damage to teeth. Dental damage in such situations is not necessarily negligent. In cases where compensation was paid, the average amount was around £5,000. However, some claims totalled over £20,000 due to the need for extensive dental restoration work or dental implants.
Drugs routinely used by anaesthetists have many potential dangers, so it is notable that few claims –just 17% – arose from drug errors or adverse drug reactions.
Many claims involved the prescription of a drug to a patient with a known allergy. For example, over £350,000 in compensation and legal costs was paid to a patient with a penicillin allergy who was given amoxicillin during a hysterectomy and had a severe allergic reaction.
While such incidents are uncommon, the majority of incidents could be avoided had standard checks been undertaken.
Claims due to needle misplacement accounted for 12% of cases. Allegations included compartment syndrome following an injection, nerve damage caused during nerve block procedures and injuries to the spinal cord during epidurals.
Because of the potential for patients to have life-changing injuries as a result of these incidents, compensation payments can be high with some claims resulting in compensation well in excess of £1m being paid.
In one such case, a claim was settled after it was alleged the patient should have been informed of the possibility of severe paralysis. The consent form signed by the patient made no reference to this known but rare risk.
Awareness, which covers a whole range of experience, only factored in a small number of notified claims in our analysis (6%), and the majority of cases were successfully defended. Where cases settled, the damages resulting were relatively low – generally under £30,000.
Awareness claims can arise regardless of the technique used, whether balanced anaesthesia with relaxant and inhalation agent or total intravenous anaesthesia.
Brain damage or death is thankfully a very rare outcome in the claims we analysed, occurring in 6% of notified cases. However, it is worth noting that serious adverse outcomes do occasionally occur and patients need to be offered relevant information in order to provide informed consent.
Examples included airway obstruction leading to hypoxia, coagulopathy resulting in haemorrhage then hypovolaemia leading to cardiac arrest and anaphylaxis leading to cardiac arrest. One case settled for more than £2.6m in compensation and legal costs.
The soft tissue structures of the oropharynx, nasopharynx and trachea may sustain instrumental injury, which occurred in 3% of cases. These cases rarely resulted in settlement and where they did, the amount paid was usually very modest.
One claim involved the perforation of a patient’s oesophagus due to an orogastric calibration tube being inflated after having been
placed incorrectly by the anaesthetist in the oesophagus during a gastric band procedure.
The patient alleged that he was not adequately informed of the risk of this injury and would not have consented to the procedure had this been brought to his attention.
The risks to anaesthetised patients of sustaining pressure damage or nerve palsies as a result of positioning on the operating table are well known, although there were only 3% of notifications in this category and few resulted in compensation being paid.
Allegations that the consent procedure was inadequate feature in many of the claims being made against anaesthetists, but in 2% of cases this was the prime focus for the claim.
Commonly, it was alleged the risks of a procedure were not adequately explained. However, none of the claims which centred solely on this issue were settled.
Recently updated GMC guidance on Decision-making and consent places greater emphasis on doctors and patients taking decisions together based on exchange of relevant information specific to the individual patient.
Claims involving anaesthetists can arise for a wide range of reasons and very few cases result in compensation being paid.
Nonetheless, there are steps you can take to manage common risk factors and reduce the risk of misunderstandings which can lead to a claim, as explained in the box on the left.
While the number of claims brought against anaesthetists while working in private practice has not increased significantly in the past few years, the cost of claims has spiralled.
This is not due to worsening clinical standards but to a deteriorating legal environment which the MDU is campaigning to reform. You can see more at www. themdu.com/faircomp.
Dr Claire Wratten is senior claims handler at the Medical Defence Union
Private doctors are looking forward to a more efficient and technologically advanced future after switching to remote working amid the Covid-19 pandemic

WITH MANDATORY social distancing, self-isolation and travel restrictions, private clinicians have embraced telemedicine as never before to keep their patients safe and supported.
And with a faster service, less paperwork and more convenience, doctors say digital prescribing in the private medical setting is the final piece of the puzzle when it comes to providing a fivestar service to patients.
Dr Charlotte Norton, medical director of The Slimming Clinic, the UK’s largest provider of private doctor-led weight loss pro -

Being able to send the medication to our patient’s home at the touch of a button is far more convenient for us and for them and is definitely something we will continue to do into the future
DR CHARLOTTE NORTON
grammes, said: ‘Many of our patients are prescribed medication which needs to be kept cold. Previously, we would have prescribed and dispensed the medication at the same time, so the patient could take it home with them. During lockdown, we can no longer do this.
Touch of a button
‘Being able to send the medication to our patient’s home at the touch of a button is far more convenient for us and for them and is definitely something we will continue to do into the future. Remote


working has become the norm as a result of the pandemic and will continue to be.’
She added: ‘It’s of significant benefit to both patients and our doctors.
‘It gives the patient more control; they can see when their delivery is coming and manage it themselves and doctors can be confident patients’ needs are being met while operating remotely.’
Dr Norton added that technological advances such as remote prescribing has allowed The Slimming Clinic to grow its business and reduce overheads. The entire team works remotely and the company has closed 24 shopfront clinics.
She said: ‘Electronic prescribing is a huge asset to independent practitioners because it gives you the ability to write a prescription anywhere and at any time, whether that’s in a consultation room or home.
With the ongoing restrictions, it has come into its own, providing much more convenience and keeping patients safe in their homes
CAROLINE CORRIGAN, MidexPRO

ing it through as quickly as possible.
‘With the ongoing restrictions, it has come into its own, providing much more convenience and keeping patients safe in their homes.
It is clear digital prescribing has been extremely valuable to doctors and patients throughout the pandemic
DANIEL LEE, director, CloudRX
‘Turning to electronic prescribing allowed us to provide a national service almost overnight. It has facilitated a geographical reach with no limits as to where you can send the medication, which is especially important in expanding your business.
‘You can support a customer on the other side of the country over the phone or webcam and have the medication sent to their door.’
Benefiting thousands
MidexPRO, which provides practice management software to private clinicians, say its partnership with digital prescription service CloudRx has benefited thousands of patients across the UK.
Caroline Corrigan, operations director, said: ‘We’ve always been keen on remote prescribing and had already begun conversations with our customers when Covid19 hit, so it was just a case of push-
‘There’s certainly no room for going back now. We recognise the huge benefits for patients and consultants. It means we can offer a five-star service to our valued clients, who can, in turn, offer a fivestar service to their patients.
No queuing
‘There is no queuing at chemists or waiting for a consultant to write out a paper prescription; you can literally get it delivered to your door. At one click of a button, you can have your medication less than 24 hours later all over the UK – which is really the key.’
She added: ‘People expect to be able to order things at the touch of a button through online shopping. Next-day delivery is the norm. Electronic prescriptions are really no different to that.’
Although it is well established in the NHS, private clinicians do not have access to the Electronic Prescription Service (EPS), used by 96% of NHS GPs and more than 99% of NHS pharmacists1 – which saw a surge in use during the pandemic.2
Daniel Lee is director and superintendent pharmacist at CloudRx, which enables private clinicians to digitally sign prescriptions and send medication directly to the patient within 24 hours.
He said: ‘There is a clear technology gap between the electronic prescribing capabilities of the NHS and the digital infrastructure available to independent private clinicians. We developed CloudRx specifically for private GPs and consultants to help reduce their reliance on paper prescriptions and provide a convenient digital option for patients.
‘We accelerated the roll-out of CloudRx in response to Covid-19 – helping patients attending virtual consultations and those needing repeat prescriptions to access their medication safely and easily.
‘It is clear digital prescribing has been extremely valuable to doctors and patients throughout the pandemic, and will prove to be an essential service in the future.’
www.cloudrx.co.uk
References
1. NHS Digital: Electronic Prescription Service. https://tinyurl.com/y66kpgfc
2. ‘Items dispensed from electronic prescriptions increase by 22% in March 2020’, Pharmaceutical Journal https://tinyurl.com/hfbnps7b

In the first article of a new series on design, branding and marketing, Simon Marett and Michael Sullivan look at the world of logo design. They highlight the pitfalls to avoid and the aspects you should be thinking of before you go ahead and design a new logo for your healthcare practice


AT THE outset, it might look like a cost-effective option to ‘do it yourself’ when designing a logo for your practice. It may seem easy with online software or an app you have downloaded, but there is more to good logo and brand design than you think. Here are a few aspects for you to consider.
Know your audience
This might sound obvious, but it is amazing how many healthcare websites we come across that have not taken a step back and thought carefully about who their patients and clients are
and what they are looking for with a private healthcare practice.
This is a starting point for any design, logo and branding project. Most private healthcare clinics would be considered premium brands and the fees charged are often a reflection of that.
Designing a logo in Word software with a childish font and garish colours is not going to appeal to affluent professionals who are looking for a high-end, marketleading healthcare clinic.
Take 30 minutes out with your team to discuss what your patients are looking for and document this in a simple creative brief for a designer to respond to.
Start black and white
Think about some of the most iconic logos you see in your everyday life. Some immediately that spring to mind include Nike, Apple, Amazon and John Lewis.
What they all have in common is they are simple, uncomplicated and memorable. The argument here is that if a logo works in black and white then it will work when you start adding colour.
We recommend this to all our clients when they come to us looking for a new or redesigned logo or brand.
Even if you have a strong inkling that purple is going to be the colour for your clinic, get a designer to sketch it out in black and white first. If it does not look quite right in black and white, it is unlikely to look good in full colour.
p20

Designing a logo in Word software with a childish font and garish colours (left) is not going to appeal to affluent professionals


3 Think mobile
We all now live in a world where people are glued to their mobile devices and that is not likely to change any time soon. So stop a moment and have a think about what that means for your logo for your new clinic or practice.
There is no point spending hours and hours looking at how your logo is going to appear on letterheads, business cards and brochures when the vast majority of your patients and future patients will experience your logo via their mobile phone and a small screen.
Concentrate on keeping your logo simple and test it out on a mobile phone early on in the process or you will soon be going back to square one.
4 Less is more
Successful branding is more than just a logo; it is about the whole package: logo, avatar, strapline, colour palette, typography and imagery.
One of the most common mistakes we come across in logo design is placing all the emphasis on the logo and packing too many words and elements into it.
Going back to some of the biggest and most successful healthcare and medical brands, such as GSK, Novartis, Bupa and Boots, they are all short and simple with eight characters or less.
The more characters you add to your logo, the more complicated and difficult to read it becomes.
So, if you have a killer strapline that is going to sell your clinic, do not pack it into the logo. Position it on the website homepage instead or put it on the back of your business card.
5 A flexible toolkit
In today’s digital world, it is vital that you build flexibility into

One of the most common mistakes we come across in logo design is placing all the emphasis on the logo and packing too many words and elements into it
(Above:) The vast majority of your patients will experience your logo via their mobile
your logo design, because it is guaranteed to appear in a number of places and several different formats.
Having one version of your logo that only works on a white background is going to cause problems when a business partner with a dark background website wants to put your logo on their homepage.
You are also going to need to think about how your logo is going to work on mobile – see point 3 above – as well as the social media channels like Facebook, Instagram or LinkedIn.
You may also want to introduce an avatar or icon as part of your brand toolkit.
Ask your designer or agency to create a set of brand guidelines or a brand book to follow as part of your logo or brand work. Adaptability within a simple brand framework is the name of the game.
Less is more when it comes to designing a logo (left)
Building a strong logo and brand is important for any successful healthcare practice.
You will never have a second chance to make a first impression, so why take a risk and cut corners on an aspect of your clinic that carries such importance.
Working with a good designer or marketing agency about your logo plans need not cost the earth and is guaranteed to be a sound investment.

There is no substitute for experience and they will help you through the process, provide options and help save you time, money and effort by putting your clinic on the right path for future success.
Simon Marett (left) and Michael Sullivan (right) are managing director and creative director of Ellerton Marketing Ltd, a specialist strategic marketing consultancy for independent healthcare practitioners

for a busy
MUCH WORK around further improving patient safety and reforming healthcare regulation was understandably put on hold last year while the health system responded to the Covid emergency.
But 2021 looks set to see several key changes which will have significant impacts for independent healthcare and those who work in the sector.
Firstly, at the beginning of this year, the Government published its response to the Independent Medicines and Medical Devices Safety Review (IMMDS), led by Baroness Cumberlege.
This was set up to examine the use of three medical interventions – the hormone pregnancy test Primodos, the anti-epileptic drug sodium valproate, and surgical mesh – and, more broadly, how the healthcare system can improve its response to concerns raised about medicines and medical devices in the future.
With increasing numbers of implantable devices being used in modern medicine and growing numbers of patients using a mix of NHS and private healthcare, it is vital that the independent sector is fully integrated into any measures to improve safety in this area.
We therefore welcome the Government’s response to the IMMDS review, which included a commitment to amending the Medicines and Medical Devices Bill currently going through Parliament to include the creation of an independent patient safety commissioner role.



sations across the UK, ensuring that no patient – regardless of where they access their care – falls through the gaps.

Of course, 2021 will also see the long-awaited Government response to the Paterson inquiry.
The former Bishop of Norwich’s report in February last year made over 15 recommendations directed at all parts of the healthcare system. These included healthcare professionals, the NHS and independent sector, professional and systems regulators, a wide range of issues looking at safety and quality of care, responding when things go wrong, working with others to keep patients safe, and governance, accountability and culture.
The commissioner will act as an independent advocate for patients and help promote the importance of the views of patients in relation to medicines and medical devices.
Critically, the commissioner’s remit will cover both NHS and independent providers, and the post holder will have the ability to make reports and recommendations to both sectors.
The Government has also taken onboard Baroness Cumberlege’s recommendation to create a central patient-identifiable database to collect key details of the implantation of all medical devices. This will support research and auditing of the device safety and patientreported outcomes measures.
Demonstrating the Government’s commitment to a ‘whole systems’ approach to patient safety, work is now in progress to establish a UK-wide medical device information system. This will facilitate the routine collection of medical devices, procedure and outcome data from all NHS and private provider organi-
As outlined in my previous columns, this year will also see a step change in healthcare regulation with the Care Quality Commission (CQC) developing its new five-year strategy to enable it to better regulate individual providers as well as assess local healthcare systems.
At the start of this year, the CQC also launched an additional consultation looking at specific changes to help enable it to be a more ‘dynamic, proportionate and flexible regulator’. This will have key implications for independent sector providers and practitioners in the sector.
Proposed changes include moving away from a fixed inspection schedule and inspection visits to a greater use of wider sources of evidence, tools and techniques.
Other proposals include changing the frequency of ratings reviews with the move away from site inspection as the mechanism through which a rating can be changed.
The move to a more flexible system is welcome, but the devil is in the detail and it is as yet unclear what data and information the regulator will use to base its judgements.
Reading the testimonies of the individuals affected by Paterson’s appalling crimes, one cannot fail to be moved by their suffering. The Independent Healthcare Providers Network (IHPN) is committed to supporting the Government’s implementation of the Paterson inquiry’s recommendations.
This will including working with those in the sector to further embed the principles from our Medical Practitioners Assurance Framework – which stakeholders tell us is having added real value to governance.
2021 will clearly be a busy year for safety and regulation, not least as we continue to adapt to the ‘new normal’ post-Covid world with an ongoing focus on stringent infection control and prevention.
The IHPN has long advocated a ‘whole-systems’ approach to patient safety and healthcare regulation issues and 2021 looks like the year this will bear fruit.
We are committed to working with and supporting all clinicians in the sector so that we can continue delivering the safe, effective and joined-up care our patients expect and deserve.
David Hare is chief executive of the Independent Healthcare Providers Network



Having spent significant resources and countless hours training, doctors must convey their expertise to the public – especially vital in an overcrowded market. Nikki Milovanovic warns that ‘being on social’ is not the same as being great on it
DR CASESTUDY has a good idea of the image he wants to portray and, as an astute entrepreneur, values getting the message out ASAP so he can focus on his busy clinic –which is ideally getting busier, due to his investment in social media.
Now, if he is inclined to throw that investment right out the window, he might consider these surefire strategies that promise little to no success:
Option a) Instant clinic, just add water; or
Option b) You get what you pay for.
The prognosis? Unfollowable.
Option a) is unfortunately alltoo common and sees clinics ‘playing it safe’ by replicating the status quo.
This tack frequently employs a wealth of stock imagery, #IrrelevantHashtagging and the occasional
foray into badly-lit ‘before and afters’.
Sometimes, clinics even go the extra mile to incorporate a signature colour palette – a robust way to demonstrate one’s overcommitment to teal.
While a certificate of achievement from FaceTweet Academy and a ‘don’t make waves’ strategy might seem desirable, on closer inspection, this approach translates into mediocrity with a capital ‘meh’.
Playing it safe isn’t just about individual content or design preferences, although they definitely matter. This type of strategy actually diverts traffic and can drain resources to yield few results.
Now, I anticipate your healthy scepticism, which presumably sounds something like: ‘Well, hot-
shot, if so many clinics are doing it, how can it be wrong?’
Since it’s an essential component of any successful social media strategy, let’s consider content.
We’ve all seen countless websites, digital ads and printed promotional materials emblazoned with the same uninspired stock images – and I guarantee you know them as well as I do.
Picture it: a plump-cheeked brunette smiles serenely while gloved hands wield a syringe or cup her face from angles that defy anatomical possibility. A popular variation is ‘stares into your soul, poreless cheek grazed by orchid, stock image beauty’.
While such images are updated biennially – or thereabouts – to maintain a contemporary aesthetic, the series will inevitably also include ‘mud masque over full
foundation,’ ‘malaise while attractive’ and my personal favourite, ‘gasp in mirror’ – thus ensuring their suitability for the global promotion of all things beauty/wellness.
The fact that we’re sufficiently familiar with this niche subgenre to warrant the UK’s first sectorwide eyeroll – and yet they are still being used almost across the board – should sound some alarm bells. If aesthetic experts can recognise overused images, surely the digitally-savvy patients on social media will too.
Let’s rejoin our colleague, the illustrious Dr Casestudy, as we delve into the second strategy for terrible socials. Cue the Game of Thrones memes: winter is coming, and cold calls are here.
Promising to increase patient acquisition astronomically at half the cost, or less, of a traditional agency, they sound too good to be true.
But, sadly, even seasoned practitioners like Dr Casestudy will fall foul of the seductive siren call stemming from ‘cheap and cheerful’ services.
It’s worth noting that 2020’s disruptions in employment due to Covid-19 have spawned a tremendous increase in digital marketing start-ups – with many claiming to be specialised in UK aesthetic treatment.
Spamming clinics
Not only are they spamming clinics’ inboxes, but my own business gets five or more cold calls a week from the very same ‘experts’ who can’t distinguish a medical clinic from an agency. It’s hard to take them seriously.
These ‘specialists’ promise to
We’ve all seen countless websites, digital ads and printed promotional materials emblazoned with the same uninspired stock images
optimise social by blasting out content tailored to clinics’ desired patient base, and seem cost-effective enough to be worth the punt. And while clinicians know they could definitely do better – if they only had the time – since ‘it’s just about output’, what’s the harm in outsourcing . . . right?
I’m going to answer that ques -
tion by translating their pitch for you.
‘Hi <your username>, the algorithm said you ‘do beauty’.
‘We’re playing the odds by pasting this exact message to everyone, so do you fancy paying a low monthly fee for low-value content?
‘To make it worth our while, our content is 98% recycled and from 2014, but you can rest assured it’s industry-specific. In fact, it’s the exact same content scheduled for your competitors. (Since it’s so cheap, they bought it too – don’t miss out!)
‘If paying to damage your brand sounds ideal, let’s organise a call in which we’ll use many incomprehensible buzzwords while telling you whatever you want to hear. Want proof of efficacy? Enjoy these charts and a word cloud –now with 50% more jargon!
‘Don’t worry about replying; we’ll revert every few weeks imply-
Get ready in advance of April 2022 when the proposed changes to the NHS Pensions will allow you to reclaim some or all of any Annual Allowance tax you may have suffered in the past.
With our knowledge and in-house calculators, we will be able to predict in advance and check statements produced by NHS Pensions and Scottish Public Pensions Agency for accuracy for any refunds due.
For further information contact us at aa@semail.co.uk or telephone 01625 527351.
ing your interest, based on the assumption that if you knew what a scam this was, you’d have already blocked us.’
You know the song, so sing it with me: you can’t cut prices without cutting corners, even in social media.
Nikki Milovanovic (below) is the founder and managing director of Sophisticated Comms, an agency specialising in creative strategy, social media and public relations for the lifestyle, beauty, health and wellness sectors

In our series on ‘The power of people’, Jane Braithwaite explores the broad subject of managing people and teams, covering topics including responsibility as employers, leadership styles, different employment models and well-being. In her third article, she focuses on leadership and management in private practice





















































































































WHEN IT comes to the subject of people management, every organisation aims to create high-performing teams and one of the key contributing factors to success is leadership and management.
We know that good leadership and management is vital to gain the greatest contribution from our people, but how do we define a good leader and how does a great leader differ from a great manager?
We all have vivid personal experiences of leaders and managers and can recount stories of great bosses and those who were not so great, but articulating exactly what characteristics make a great leader or manager is hard.
Who is the best manager you have ever worked for? Try articulating concisely what made them great?
I bet most people find it much easier to describe the characteristics of their worst manager rather than their best and can offer countless examples of their failures and how truly awful they were to work for.
It is much harder to state clearly what makes a great manager so great. They just are!
But to be a good manager or leader and to improve, we need to understand what skills are most important, what we want from our leaders and what our teams need from us.
The difference between leadership and management
Leadership and management are different in nature.
A leader sets a vision and the direction for the team and motivates each individual team member to join together with others as one team to achieve the set vision. People follow leaders.
A manager manages the process of the work, working with the individuals in the team to ensure they are able to make their contri-
bution in an efficient and effective manner. A manager drives for order and accountability, creating improving systems and processes.
Individuals within the team will be motivated to follow a good leader and to work with a good manager.
A great leader inspires people and motivates them to act, setting the direction and the vision of where they are heading, even if they are not certain how they will get there.
Good leaders are often charismatic, engaging and outgoing, but there is, of course, an exception to every rule.
They tend to cope well with chaos or a crisis situation and are able to determine a way forward and articulate that to others.
Leaders are good at handling change and developing confidence in others to initiate the changes.
They create ideas and engender enthusiasm to explore new opportunities and, in doing so, may be perceived as rule-breakers. You could argue that great leaders are of a more creative nature.
In a crisis situation such as the all too familiar Covid pandemic, a leader will motivate the team to commit to working hard even when exhausted and build confidence that the goal will be reached despite the way forward lacking clarity.
A manager manages the work of whatever nature and, by definition, requires a deep understanding of the operations of the business or team.
A good manager will be analytical, assessing how things are done and looking at ways to change and
The skills of leaders and managers are different, but to manage a business, clinic or team, the person in charge needs to have both leadership and management skills to some degree
During the Covid crisis, we have experienced first-hand some very high-profile leaders and managers in action. I will avoid naming any individuals to avoid tipping into a political debate, but I am sure it has become obvious to us that some individuals are better at leadership than management and vice versa.
improve either to create greater efficiency or to achieve certain goals.
In almost any work situation, a good manager will also need to a be a good people person, able to relate to individuals on a one-toone basis and as a team.
Managers are good at creating and improving systems and process. They aim to create order and to simplify. They are problem solvers who desire stability and control.
The skills of leaders and managers are different, but to manage a business, clinic or team, the person in charge needs to have both leadership and management skills to some degree.
Much has been written about great leaders over the years and, in time, I am sure we will read about the great leaders during the Covid pandemic.
Any historical list of the greatest leaders is likely to include Nelson Mandela, Martin Luther King, Winston Churchill and Mahatma Gandhi and I am sure we can all name a few others.
Each of the individuals I have included had a cause they were so passionate about, that their name became synonymous with that cause. Take, for example, Martin Luther King’s cause which is well known as his ‘dream’.
If we review the leadership characteristics of these individuals to look for consistencies that help us understand what makes them great leaders, in each case we see a

relentless determination, incredible will power, courage and unfailing motivation even when tested to breaking point.
As leaders, they each won the hearts and minds of their people, with Gandhi being remembered as ‘the father of his country’. In summary, we can deduce that key traits of a great leader are a clear cause, the ability to communicate that cause well, to create an enthusiastic following and an unfailing determination to achieve it.
It may feel more relevant to us to consider leaders within the business community, and any current list of the ‘greatest business leaders’ is likely to include the following people.
Tim Cook
Chief executive of Apple; Sheryl Sandberg
Chief operating officer of Facebook; Mary Barra
Chairman and chief executive of GM Company; Elon Musk
Founder of PayPal and Tesla; Warren Buffett
Chief executive of Berkshire Hathaway; Bob Igor
Executive chairman of Disney; Reed Hastings Chief executive of Netflix.
There are some big names here, some of whom have become almost celebrity figures, but that does not detract from their capabilities as great leaders.
Again, we can review their leadership styles to understand what makes them the great leaders they are recognised to be and look for consistencies that allow us to learn from them.
Interestingly, the themes here differ from our earlier examples of great leaders where their commitment to their cause seemed to be the greatest factor.
While I am certain that each of these business leaders has a cause or a vision as we tend to refer to it in a business setting, but most of what is written about their leadership style is their approach to creating and managing their teams.
They surround themselves with exceptional people and they empower these people to be innovative and take ownership.
They work hard to understand the strengths of the individuals within their teams and allow them to apply those strengths.
They support and encourage, acting as an enabler and they praise their team members for their great work, making a point of not taking credit themselves.
‘It doesn’t make sense to hire smart people and tell them what to do; we hire smart people so they can tell us what to do’ – Steve Jobs.
What also seems to distinguish them most is their decision-making process. They claim to make very few decisions themselves but encourage their teams to make the decisions, trusting their ability to do so, which has the added impact of ensuring their teams take ownership. They are clearly defining themselves as leaders and enabling their teams to do the managing.
Leadership and management are different and require different skillsets. We may feel that some people were born great leaders, but, in reality, their skills have been developed by life experience and formal training.
It is possible for anyone to improve their leadership and management skills and the best starting point is improving selfawareness.
In next month’s article, we will be exploring some of the best tools and methods available to leaders and managers to improve their own personal development, shaping them to enhance their leadership and management skills.
In the coming months, leaders will need to demonstrate a strong determination and perseverance, and we will include the development of resilient leadership skills in our discussion.
If you would like to share your comments regarding leadership and management or discuss support for your team, please do get in touch.
Jane Braithwaite (right) is managing director of Designated Medical, which offers business services for private consultants, including medical secretary support, book-keeping and digital marketing
They surround themselves with exceptional people and they empower these people to be innovative and take ownership
Vision – A great leader has a vision (cause or dream), that they can communicate clearly to people and inspire them to have confidence in their vision, even if they cannot articulate exactly how it will be achieved.
Perseverance – Master a determination to succeed and continued confidence in the vision. A great leader has absolute faith in achieving their vision which builds faith in their team.
Create the best team – Learn the ability to recruit the best individuals and allow them to participate fully by empowering them to make decisions and take ownership.
Decision-making – Foster a willingness to delegate decision-making as much as possible to team members. A leader trusts the team to make the right decision.
Role model – Set a good example that your team can respect and trust.
Know your team – Develop a clear understanding of the individuals on your team. Fully understand their strengths and weaknesses. Create opportunities for an individual’s strengths to be used to gain maximum impact.
Make hard choices – Being the leader means making the hard choices. Be prepared to make the tough decision and communicate clearly to the team your reasons for doing so.
Support the team – Provide your team with the support and resources they need to succeed.


Billing accurately and promptly is one of the vital signs of a healthy practice. Desné Marston (below), with nearly 30 years of practice management experience, explains how Healthcode’s Clearing Service powers this critical business process


YOU COULD be one of the most skilled and respected doctors in your specialty, but if your bills are error-strewn, do not meet the private medical insurer’s rules or are submitted long after the patient has been discharged, you risk cash flow problems that could jeopardise the long-term survival of your practice.
If your independent practice is to prosper, billing is one area that you need to get right, so it is reassuring to know that Healthcode’s clearing technology enables you to send bills quickly, easily and securely to their intended recipient.
Billing insurance firms was once a purely paper exercise. Practices drew up an invoice that needed to include all the information required by that insurer in the correct format, such as the patient address, policy number, date of treatment and procedure code. These rules varied.
The invoice was usually printed and posted, which was costly and time-consuming. Plus, it was impossible to be sure that it had been received and when it might be paid.
Practices were no wiser about
problems, until they were notified of a query or asked to resubmit the invoice, causing unwelcome delays.
The whole process was inefficient, unsecure and burdensome for billing staff, while from a financial perspective, it was virtually impossible to make accurate cash forecasts.
Nor was paper invoicing popular with the insurers themselves. After all, each practice might only send a few invoices per week but insurers would be faced with thousands every day.
Even if only a fraction contained
Electronic clearing houses are essentially online hubs which pre-screen claims for medical practices and transmit them securely to private medical insurers

errors, it would be many hours administrative time before issues could be resolved and the payment finally made.
Insurers turned to Healthcode to develop a Clearing Service for medical bills that would provide an accurate, efficient, secure and cost-effective alternative to traditional paper invoicing.
We launched the Clearing Service in 2002 and before the pandemic struck, we were processing more than 7m invoices each year for practitioners and hospitals, equating to more than £3.3bn of activity.
Electronic clearing houses are common in countries like the US, where insured healthcare is the norm. They are essentially online hubs which pre-screen claims for medical practices and transmit them securely to private medical insurers. They also enable practices to submit all their invoices from a single platform.
As you can see from the diagram at the top of the page, Healthcode’s Clearing Service works along exactly the same lines:
➲ A practice generates an invoice or batch of invoices using Healthcode or third-party billing software.
➲ It uploads the invoice – or the batch – for clearing and validation by our Clearing Service.
➲ The Clearing Service automatically checks that each invoice complies with the relevant insurer’s own validation rules, including:
❍ The invoice number and date;
❍ Provider details, name, pro -
vider number or professional number, specialty and billing address;
❍ Patient’s full name, birth date, address, insurance company/ paying organisation, policy number, diagnosis and description where applicable, lead practitioner;
❍ Treatment type, date, service delivered, procedure code, description and, where applicable, fee.
➲ The Clearing Service sends validated invoices to the relevant insurer for processing and payment. It flags invoices with errors and anomalies to the practice so they can be corrected and resubmitted.
➲ The practice can see the status of each invoice.
➲ The insurer pays the practice and sends remittance advice. Practices can also use the Clearing Service to view and print remittances where the insurer has made this information available.
From paper bills and payments by cash or cheque to e-commerce and contactless payments, financial transactions have been part of a digital revolution and the pandemic has accelerated that process. However, it simply would not be possible without technology which enables transactions to be processed seamlessly, efficiently and in a fraction of the time of oldschool paper-driven systems. We are proud to have made this a reality for independent practitioners since 2002.
Desné Marston is product marketing manager at Healthcode
While paper billing of private medical insurers has largely been consigned to the past, you may be tempted to email your bills directly. However, using a clearing service to submit bills brings a host of business benefits that do not generally apply when you do it yourself. We think these are five of the most compelling:
You can submit invoices to all the major insurers from one platform, rather than spend precious time finding contact details and sending them out to each one separately. Uploading an invoice or batch of invoices takes seconds and invoices are instantly validated in line with the relevant insurers’ rules so they are ready for payment on receipt.
2 Minimise human errors, invoice queries and rejections
Healthcode’s Clearing Service automatically sends validated invoices to the correct recipient, so there is no chance of mis-keying an address or an invoice being lost.
Errors that would cause an invoice to be rejected or queried by the insurer are flagged immediately, so you can fix them there and then, rather than discover the problem several weeks later.
3 Better cash flow and forecasting
When invoices are validated by the Clearing Service, they can enter the insurer payment cycle quicker. Plus, you have reassuring confirmation that your invoice has been received, which helps with cash flow forecasting.
4 Protect-sensitive data
The Clearing Service is a secure, encrypted system which complies with data protection law, so your invoices are safe from prying eyes. Sensitive patient and financial information should never be sent by unsecure email. In the event of a data protection breach, you risk a fine and damage to your reputation.
5 Expert technical support
Knowledgeable customer services team is available to answer queries and help resolve problems straight away, which simply is not an option if you go it alone. We have also produced video guides on how to create and submit an invoice.


IN THE past few months, it might appear – at least to some – that making money in markets is easy. Just buy Tesla or Bitcoin and you are sure to double your money. That is to confuse gambling with investing, and these are certainly not recommendations.
Bitcoin– boom, bubble or bust?
In October 2008, a mysterious white paper was published by an unknown author titled ‘Bitcoin: A Peer-to-Peer Electronic Cash System’ and the world had been introduced to its first ‘cryptocurrency’.
Bitcoin is driven by ‘blockchain’ technology, which is a digital record of transactions. The main attraction compared to traditional
currency was clear – Bitcoin provides a decentralised way for two parties to exchange value.
In other words, Bitcoin has no need for a governing body, no central bank and is merely a digital ledger that facilitates and records transactions.
Without getting too granular about how exactly this works, the complicated mathematical procedures in place make falsifying Bitcoin transactions unlikely with today’s technology – although never say never.
Twelve years down the line, the cryptocurrency space has seen thousands of alternatives, or ‘altcoins’, come to market, all of which attempt to improve upon the blueprint pioneered by Bitcoin.
One challenge is scalability –Bitcoin can handle a paltry 350,000 daily transactions compared with VISA who executed around 500m per day in 2019.
Furthermore, in a society that is ever more focused on sustainability, a currency that requires enormous warehouses full of energy-hungry computer equipment to keep it going feels like a square peg in a round hole.
A useful tool built by the University of Cambridge estimates that the Bitcoin network currently consumes around 110TWh of energy per year, roughly the same as the Netherlands.
Despite the implementation issues, the value of Bitcoin – and
many of the ‘altcoins’ mentioned previously – have skyrocketed of late, leading to a lot of excitement for investors – or rather gamblers.
The only thing we know for certain about investing in cryptocurrency is that it is highly speculative. The extraordinary volatility of most ‘coins’ makes them an unreliable store of value.
Going to sleep and waking up 10% richer – or poorer – is commonplace. Furthermore, Bitcoin is not a capital asset, meaning it does not pay dividends, nor does it have a positive expected return.
Positive outcomes are simply the result of demand outstripping supply, although investors are quick to forget that the future expectation of demand is already factored into the current price.
There are 18.6m Bitcoins in existence, yet recently the sale of 150 Bitcoins resulted in a price drop of 10%, demonstrating no depth or liquidity to the Bitcoin market.
It is possible that we may one day transition to a world where cryptocurrency is adopted by the masses. Who knows if that is even remotely likely and, better yet, who knows which cryptocurrency will be the one that ticks all the boxes?
However, as an investment today, cryptocurrency plays no role in portfolios and any investor (gambler) should be willing to accept a maximum loss of 100%.
GameStop – the reddit vs Wall Street saga
Here is another example of gambling masquerading as investing. At the time of writing this – in what is a fast-moving situation – a group of amateur investors using discussion website reddit as a platform banded together to take on the professional hedge fund space in the US.
The group focused their conversation on a few stocks, the most recent of which is an American consumer electronics firm, GameStop. On the one side we have the hedge fund managers, who are engaged in a process known as ‘shorting’, essentially betting that the share price of GameStop will go down over time.
A successful short involves borrowing stock from a third party, selling it on the marketplace and then buying it back later when the price has fallen.
This allows the short seller to return the stock to the third party and cash in the difference in price. The danger of this is that if prices were to rise, purchasing the stock back becomes more and more expensive for the short seller and they cannot afford to return their borrowed stock. Professional investors are aware of these risks more than anyone.
The companies featured recently on the forum are heavily shorted and include GameStop, AMC Entertainment, Koss Corp and Blackberry (a throwback). By purchasing shares in these firms, investors are bidding up prices, creating huge losses for some of the hedge fund managers.
The only thing we know for certain about investing in cryptocurrency is that it is highly speculative
These are not small market movements either. As of 27 January, the share price of GameStop closed nearly 2,000% up since the start of the year. Yet, on 28 January, the price fell by almost a half.
A quick glance at the forum shows that the motivation for some is to ‘stick it to the man’, whereas others are perhaps looking to make a quick buck.

As the situation progressed, it certainly caught the eye of the regulator on suspicion of market manipulation, as well as the eye of newly appointed US Treasury Secretary Janet Yellen, whose team announced they were ‘monitoring the situation’.
Either way, it is difficult to see how this will have any sort of happy ending. Other than the handful of investors (gamblers) who might sell at the right time, the only guaranteed beneficiaries to all this are the market makers and middlemen.
If you want excitement, just follow the stories and enjoy the schadenfreude that follows. This is gambling and best avoided.
Dr Benjamin Holdsworth is director of Cavendish Medical, specialist financial planners helping consult ants in private practice and the NHS
The content of this article is for information only and must not be considered as financial advice.
Cavendish Medical always recommends that you seek independent financial advice before making any financial decisions.
Levels, bases of and reliefs from taxation may be subject to change and their value depends on the individual circumstances of the investor. The value of investments and the income from them can fluctuate and investors may get back less than the amount invested.
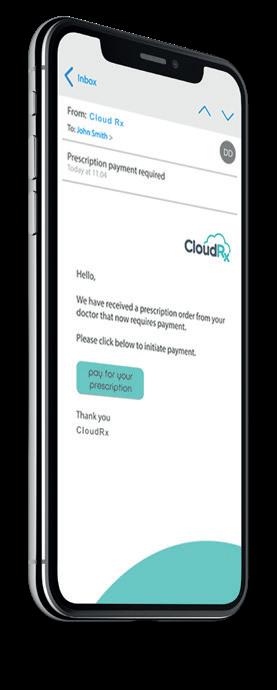
A digital prescription platform to allow convenient prescribing from home
CloudRx is a digital prescription system that allows prescribers to create and send an electronic prescription to our fully licensed pharmacy for fast delivery direct to your patient. It can be used from home by doctors working away from their practices.
No cost to prescribers
Simple and quick prescription creation.
Legal paperless prescriptions, including repeat prescriptions and controlled drugs.
Patients receive text and email requesting secure payment. Alternatively, we can invoice the prescriber or clinic each month.
Prescriber Fees can be added if requested
Medicines are dispensed and dispatched by a variety of delivery options
Fully integrated into MidexPRO
Register for free by visiting cloudrx.co.uk

“We have worked with CloudRX to maintain a cold chain for the medication and direct delivery to patients at home.”

KEEP IT LEGAL: THE EQUALITY ACT
To what extent does the Equality Act protect non-binary individuals working in your practice? Bronya Greatrex gives her legal view

A RECENT EMPLOYMENT tribunal claim has shed light on the extent of the protection offered by the gender re-assignment provisions in the Equality Act.
This article looks at some of the failings of the employer in that case and highlights some of the things that your practice may need to be thinking about when it comes to diversity and inclusion.
Who is protected from discrimination?
Section 7 of the Equality Act 2010 protects individuals against discrimination on the basis of gender re-assignment but, until recently, the definition of gender reassignment had gone unchallenged.
S7(1) Equality Act 2010 states: ‘A person has the protected characteristic of gender re-assignment if the person is proposing to undergo, is undergoing or has undergone a process (or part of a process) for the purpose of reassigning the person’s sex by changing physiological or other attributes of sex.’
The definition was previously thought to protect individuals who had made, were making or were proposing to make a change from their natal sex to that of the opposite sex – that is to say, a change from male to female or female to male.
This widely held interpretation of the Equality Act was therefore a strict binary interpretation protecting individuals who either identified as exclusively male or exclusively female.
As awareness of gender identity has developed, it has become clear that a strictly binary approach is not inclusive of the full range of potential gender identifies.
The LGBT Foundation describes non-binary as a term ‘used to describe people who feel their gender cannot be defined within the margins of gender binary. Instead, they understand their gender in a way that goes beyond simply identifying as either a man or woman.’
Some non-binary individuals also identify with the umbrella term ‘transgender’, meaning identifying with a gender other than the one you were assigned at birth, but not all non-binary people feel that this definition applies to them.
Under the heading of nonbinary, there are many nuanced
Gender-fluid people may present in a mixed mode where they may adopt what is traditionally considered to be a more male or a more female presentation from day to day
Ms Taylor brought a claim against her former-employer JLR for, among other things, gender reassignment discrimination in an employment tribunal.
She had notified JLR that while she had no intention of undergoing a surgical transition, she was transgender and identified as gender fluid, presenting in a mixed mode and sometimes dressing as male and sometimes as female.
gender identities including gender fluidity. For individuals who are gender fluid, their gender identity or gender expression is not fixed and may change over time.
This means that gender-fluid people may present in a mixed mode where they may adopt what is traditionally considered to be a more male or a more female presentation from day to day.
In recent years, there has been mounting criticism for the terminology used in the Equality Act from organisations that support and campaign for LGBT+ rights such as Stonewall.
This criticism centred around the use of the words ‘gender reassignment’, which is usually used to describe someone’s transition from one binary gender to another and in circumstances where an individual is undergoing some form of medical intervention.
This meant that many transgender and/or non-binary individuals believed they had been left unprotected by the Equality Act.
This position was supported by the recommendations made in the Women and Equalities Select Committee report on transgender equality. This report called upon the Government to amend the Equality Act to protect gender identity rather than just gender reassignment requiring medical intervention.
JLR sought to rely on the widely held view set out earlier, that the law did not protect non-binary or gender fluid individuals, as this was not encompassed in the definition of gender reassignment.
The tribunal was therefore tasked with determining what Parliament had intended in relation to the gender re-assignment provisions when it enacted the Equality Act.
Despite the widely held view that non-binary individuals were not protected by the Act, the tribunal found in favour of Ms Taylor, that gender is a spectrum and that the Equality Act protects anyone moving along that spectrum from discrimination without the need for medical intervention.
It found that this includes nonbinary, including gender fluid, employees.
On finding that Ms Taylor had been subject to gender re-assignment discrimination, the tribunal

also awarded aggravated damages against JLR. Aggravated damages are rarely awarded and only in cases where the losing party is found to have acted aggressively, maliciously or oppressively.
As JLR have decided not to appeal this decision, and unless or until this position is challenged in a higher court, this finding will remain the current law in this area.
This significantly widens the pool of individuals protected by the Act and it is important that all employers are aware how easy it is for this protection to be engaged.

ALL PRACTICES should be aware that, under the current law, as soon as any employee makes it known that their gender identity is anything other than their natal sex, they are likely to be protected from any discrimination under the Equality Act.
This could include an employee approaching any member of the practice to state an intention to pursue gender reassignment or it could be as simple as an employee starting to dress or otherwise change personal attributes that indicate that their gender may be changing, fluid or non-binary.
The employee’s ultimate ‘end destination’ is irrelevant. In order to protect the practice against risk, it is therefore prudent to presume that the Equality Act will apply in circumstances where there is any uncertainty about an individual’s gender identity and any policies dealing with gender reassignment discrimination should be amended accordingly to cover more complex gender identities.
Where an employee approaches a member of the practice about their gender identity, it is important to listen and take the time to understand their position and any concerns they may have.
A lot of damage can be caused by management and colleagues misusing terminology and/or downplaying genuine concerns.
Where a practice has an HR function, it is important that HR is properly trained and prepared to deal with gender identity matters. It is not the responsibility of a non-binary employee to educate their HR representatives.
However, not all practices will have a designated HR function. In these circumstances and/or in addition to HR, it is advisable to have a nominated equality and diversity representative and to seek advice from LGBT+ organisations, trade unions and legal advisers as appropriate.
One of the main criticisms of JLR was its failure to protect Ms Taylor from harassment from other employees and third parties. Ms Taylor had been unwilling to
provide names of the offending parties, meaning that JLR had felt unable to investigate the harassment or to sanction anyone for it.
It is always difficult for an employer to properly investigate allegations of misconduct where an employee is unwilling to provide names.
If your practice is faced with this, the employee should be encouraged to provide full details of the misconduct including naming the offending parties.
The practice should consider how it can support an employee in doing this and protect them against any potential detriment for providing this information.
However, where an employee is simply unwilling to provide names, the tribunal’s finding in Taylor v JLR shows that consideration may be given to what other steps an employer has taken to address the misconduct.
In these circumstances, the practice should consider the wider culture of their practice and what can be done to address any ongoing harassment.
The practice could, for example, issue a statement to all staff reminding them of the practice’s expectations in relation to diversity and equality and warning them that any form of discrimination is unacceptable, that it will be taken extremely seriously and may result in disciplinary action up to dismissal.
It may also consider what support it can provide to the employee in relation to the harassment and whether further training or guidance is necessary for all staff.
Another area that is not straightforward when dealing with employees who are undergoing gender re-assignment or who identify as transgender or nonbinary is in relation to the appropriate toilets for them to use.
JLR is a very large organisation with a number of large sites and it was therefore open to greater criticism about the provision of toilets than a smaller employer is likely to be.
The potential facilities and
A lot of damage can be caused by management and colleagues misusing terminology and/or downplaying genuine concerns

options available to transgender or non-binary employees will therefore vary depending on the size of your practice, but it is important to show that proper consideration has been given to the practical and logistical barriers an employee may face and the feasible options for dealing with these.
What is clear from the case law in this area is that it is not appropriate to instruct a transgender or non-binary employee to use the disabled toilet. Disabled toilets should rightly be reserved for disabled staff and/or patients.
The key for any practice facing
this is to include the employee in the decision-making process so that any approach can be agreed with them and signposted to other staff and/or patients as is necessary and in a sensitive and supportive way. It should not be left for a transgender or non-binary employee to worry about this decision alone.
JLR was heavily criticised by the Tribunal for a number of things that serve as best practice reminders to employers.
These are useful learning points for all employers, including doctors as employers. As minimum best practice, employers should have regular training and policies in place that deal with diversity and equality issues.
Equality and diversity and bullying and harassment policies should be reviewed to ensure that they are fit for purpose and are up to date with current understanding in relation to gender identity. However, it is not sufficient for there to be policies in place, unless all staff including partners, practice managers and HR are aware of these policies and apply them. This applies to all policies and not just diversity and equality related policies. Practices should not fall into the trap of thinking that simply having a policy in place will absolve them of liability for their employees’ misconduct.
It is important that your practice is seen to take diversity and equality issues as seriously as other policy issues. Where there is concern that members of the practice are not promoting and supporting diversity and equality in the way they should be, this should be dealt with as seriously as any other breach of policy would be.
If you would like any further advice or support for your practice on any of the issues raised in this article, Hempsons employment team would be more than happy to assist.
Bronya
Greatrex (right) is a solicitor at Hempsons



Consultants, groups, clinics and hospitals all experience difficulties with their medical billing and collection. Simon Brignall (right) examines the scale of the problem and shows that it is often a challenge for everyone in private healthcare

THE NATURE of my work means I often speak to consultants about the issues they are facing around their medical billing.
It is common for them to be worried about a wide range of issues including:
The size of their aged debt and problems with cash flow;
Lack of transparency and access to accurate up-to-date data;
Billing errors resulting in lost income.
My first response is always to
reassure them that they are not alone. We see these issues across our entire client base.
Our clients can range from consultants new to private practice through to well established consultants, groups, clinics and hospitals. The problems are the same. Just the amounts concerned vary.
I thought it might be beneficial to look at each of these problems in turn from the perspective of the range of clients mentioned.
One of the benefits of being new to private practice is that you start off debt-free. However, you will soon realise that despite the excellent care your patients have received, not all the invoices you raise are settled promptly. This can be for a variety of reasons such as:
Issues with insurance companies;
Shortfalls, excesses and co-payments;
Delays in invoicing leading to delays in payments;
Lack of a robust chase procedure;
Limited payment pathways.
Quite soon, the debt starts to pile up and this is often around the same time that patient footfall starts to increase.
When you start out in private practice, there can be a lot of upfront costs such as medical indemnity/insurance and staffing.
You may also choose to invest in software or even a website and so it is important to ensure you get paid for the work you do, as you create a tax liability when you raise an invoice whether it is paid or not.
Some consultants choose to do the billing themselves, but, in my experience, a specialist’s time is valuable and better employed in growing the practice, looking after patients, and leaving this key area to experts such as a medical billing company.
Established consultants often find that if they have not resolved the problem, then their aged debt pile just keeps getting larger each year, leading to unnecessary write-offs and cash flow difficulties.
Practices can become victims of their own success where, although the consultant is very active, the money coming does not reflect the work being done. As you can imagine, this can be very frustrating.
We have partnered with consultants who have had 50-100% of their annual turnover outstanding when they initially came to us. We average bad debts of less than 0.5%.
To help achieve this, check out what we always do – see box on the opposite page.
In my experience, it is common for these tasks to get set aside in a busy practice, leading to increased

aged debt. Not all medical secretaries enjoy chasing outstanding debt – and even for those that do, there can be an opportunity cost.
Managing patient inquiries is a more efficient use of their time instead of being on hold with an insurance company. Practices’ revenue often rises when they can focus more on the clinical side of the practice.
Groups have the added complexity of not only additional consultants but also various models. These models range from virtual groups where they function as individual practices behind the scenes, to more formal structures such as limited liability partnerships with shared administration and a common bank account.
Consultants who make up the group can be working at different locations and have their own patient demographic each with its own challenges.
Some clinics invoice facility fees for treatments and diagnostic testing and this can be on top of consultant billing. We partner with a range of clinics, each with their own specific nuances and payment pathways.
Private medical insurance contracts are unique to each clinic and
Some clinics we have worked for had over £1m in outstanding debt at the start. Your size does not mean you are free from billing and collection problems
the billing and collection process being routinely actioned. From what I see, this rarely happens.
Consultants who are managing this task can get behind on their billing or have difficulties managing the various platforms.
Medical secretaries, even if they are up to date with their billing, can still have issues with allocating received payments and chasing outstanding debt. This can reflect poorly on the practice and result in dissatisfied patients and losses in income.
Established practices can suffer from the same problem due to poor infrastructure, higher patient volume or staff absence.
Groups and clinics are organic in nature and often are required to make binary decisions about staffing, which makes managing this difficult.
An outsourced billing option can be the best solution, as you have the capacity of the billing company on tap to manage increased activity effectively.
the invoicing needs to be raised in accordance with the rules specified in each agreement.
This can prove challenging and, if not managed effectively, can result in considerable aged debt or lost income.
Some clinics we have worked for had over £1m in outstanding debt at the start. Your size does not mean you are free from billing and collection problems.
Most billing companies’ fees are calculated against the practice’s received income. So charges are always correlated against a provider’s cash flow.
A common complaint I hear from consultants is that they have limited or no visibility of their practice finances. But if you have no access to up-to-date accurate financial information on your practice, how can you manage it effectively or make strategic decisions about its direction and growth?
New consultants generally rely on their PA to provide them with information on their practice and some even carry out the billing role themselves. Both options rely on
Groups will also want to monitor their performance. Depending on their structure and ethos, they give access to this data to either the group lead or let each consultant access their own data. Accurate data is important, as this is often used when calculating the allocation of funds to each consultant.
Clinics can have multiple locations and departments, which require regular detailed financial reporting to the management team.
With 24/7 access to our reporting tool, consultants can run a range of reports to review their practice at both the summary and granular level. This means they can review our performance as well as their own.
We provide groups with access to their data at either the group or consultant level and, for clinics, we replicate the organisational structure in our software, which enables us to tailor specific reporting as required.
Medical billing problems can impact all levels of private healthcare regardless of size and type. If any of these issues sound familiar, then I recommend you do a review and then implement processes to rectify any problems you identify.
A good option may be to engage the service of a medical billing and collection company who are experts in this field.
Clinics and hospitals who outsource can also free up valuable space for revenue-generating activities.
Mistakes in the billing process can be costly and result in thousands of pounds in lost income. I see this problem across the board.
Each insurance company has its own rules about the billing of multiple Clinical Coding and Schedule Development (CCSD) codes. It can be confusing and I still come across practices where they are billing at the wrong rates.
This can soon add up, as each insurer has its own CCSD fee schedule for billing and rates can vary by as much as 100%.
Groups, by their very nature, are more complex, as each consultant
Clinics and hospitals who outsource their billing can also free up valuable space for revenuegenerating activities
Ensure all invoicing is raised immediately
Where possible, use electronic billing to ensure that you have confirmation of the receipt of the invoice by the payee
Seek to obtain any missing data quickly that may delay invoices from being dispatched, such as missing insurance details, medical reports or patient contact information
may have their own fee schedule due to their individual experience or different contractual relationship with the medical insurers.
One of the first things we do when we take a new clinic on board is to confirm that it is invoicing in line with the terms of its contract.
You would be surprised how often we discover that the prices in a clinic’s software either differ from their contractual rates or an agreed annual uplift has not been applied. Simon Brignall is director of business development at Medical Billing & Collection
Identify and resolve any Electronic Data Interchange (EDI) errors that have occurred with invoices raised to the medical insurance companies
Offer a range of payment pathways, including the ability to take payment 24/7
Collect money up front when appropriate
Ensure all money received is reconciled and that invoices raised to patients for any outstanding balances – that result from excesses, shortfalls and co-payments – are sent out promptly
Adhere to a robust chase procedure that identifies outstanding invoices and ensure they are routinely chased and this activity logged
Keep a record of any issues that are causing payment to be delayed and resolve these as soon as possible
Independent Practitioner Today has joined forces with leading healthcare lawyers Hempsons to offer readers a free legal advice service.
We aim to help you navigate the ever more complex legal and regulatory issues involved in running and developing your private practice – and your lives.
Hempsons’ specialist lawyers have a long track-record of advising doctors – and an unrivalled understanding of the healthcare system as a whole.
Call Hempsons on 020 7839 0278 between 9am and 5pm Monday to Friday for your ten minutes’ of free legal advice.

Advice is available on: Business structures (including partnerships) Commercial contracts
Disputes and litigation
HR/employment
Premises
Regulatory requirements and investigations


A private GP asks for advice about signing a DNACPR form. Dr Kathryn Leask gives her response

QI am a private GP. A 40year-old female patient has asked me to sign a DNACPR form for her, as she does not want to be resuscitated in the event of a cardiac arrest. She has no health problems and has capacity to make her own decisions about her care. She is adamant she would not want to be resuscitated due to the risk of permanent disability.
New sessions are available for independent private practice on Saturdays.
Fully CQC-registered clinic Nursing support
Appontment-making Secretarial support
Billing service In-house pharmacy
We are a leading private outpatient clinic and we are inviting new applications for practising privileges for our extended opening hours on Saturdays.


Her reason for making this request now is that she has witnessed a friend of a similar age, who was also previously fit and well, having a cardiac arrest associated with having Covid19, who now has severe physical and intellectual disabilities.
I have discussed with her that there are many reasons why a person may suffer a cardiac arrest, some of which are treatable with a potentially good outcome.
I have also advised the patient that any such event is likely to occur in an emergency setting where those present may not know what her wishes are, meaning that attempts at resuscitation are likely to be made until more information became available.
Please could you advise on the best course of action?
AA Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) decision is not legally binding, but is intended to be a guide for the decisions and actions of those who may be present when a person suffers a cardiac arrest or sudden death.
The GMC states that making and recording a DNACPR decision in a patient where a cardiac or res
piratory arrest is expected and resuscitation is unlikely to be successful ensures that the patient dies in a dignified and peaceful manner.
DNACPR decisions may also be appropriate where CPR might be successful in returning spontaneous circulation and breathing, but where the benefits may not outweigh the risks and burdens.
Where a clinical decision is being made about the appropriateness of a DNACPR, this should be discussed with the patient, if possible, so that their preferences and wishes can be taken into account.
When a patient’s wishes to make provisions for their future care should they lose capacity to make decisions for themselves, a Lasting Power of Attorney (LPA) for health and welfare is more appropriate. The patient can complete the forms themselves using the Office of the Public Guardian website or obtain professional advice from a solicitor. Completion of this allows the patient to appoint a deputy to make decisions for them if they are no longer able to make decisions for themselves.
In addition to the LPA, a patient can also arrange an Advance Decision which can include information about what treatment they would or would not want in the event of a cardiac arrest.
Unlike a DNACPR, a valid LPA and Advance Decision would be legally binding. While a patient may ask their GP to act as a certificate provider for their LPA, confirming the patient understands the content and implications of it, they would be advised to seek appropriate legal advice when drafting an advance decision to ensure its validity.
Dr Kathryn Leask is a medico-legal adviser at the MDU
www.gmc-uk.org/ethical-guidance/ ethical-guidance-for-doctors/treatmentand-care-towards-the-end-of-life/ cardiopulmonary-resuscitation-cpr
Domestic abuse has sadly been on the rise in lockdown. Dr Sissy Frank (right) discusses what to do if you suspect domestic abuse
QI have just had a remote consultation with a patient who described feeling low, tearful and anxious all the time as well having general aches and pains.
At first, I thought she may be feeling low due to the ongoing pandemic, so I asked her about her home life and support network.
She explained that she no longer speaks to most of her friends and family members. as her husband does not like them.
As her private GP. I am concerned that having no contact with her family and friends is resulting in her being extremely isolated at an incredibly challenging time.
Additionally, when I asked her to book a follow-up appointment, she explained that she had to check with her husband before doing so.
I am concerned that she may be subject to domestic abuse within the home.
What should I do?
AIt is estimated that in the UK, 1.6 million women and 757,000 men were subjected to domestic violence and abuse in the year ending March 2020.
According to the Office for National Statistics, there has been an increase in demand for support services for those affected by domestic abuse during the pandemic.
This could be due to people in


lockdown spending more time in their homes and it is becoming more difficult for individuals to leave the home or to access available support services such as attending counselling.
However, doctors are often able to identify people who may be affected by domestic abuse, so it is important that you are able to spot possible signs and be aware of your duty to safeguard patients and to maintain confidentiality.
Understandably, patients may be unwilling to disclose that they are suffering abuse or are at risk of harm. Clinicians should bear in mind that domestic violence and abuse includes controlling or coercive behaviour in an intimate or family relationship.
It is beneficial for staff and clinicians to be trained to explore these issues sensitively with the patient if possible.
Your practice should also have a policy for managing cases of suspected domestic abuse, and this should include a named senior person to liaise with local services for victims of domestic abuse and the creation of a care pathway that facilitates access to such services.
Dr Sissy Frank is a medico-legal adviser at the MDU
Be alert to the possibility of domestic abuse in any patient and make careful records of any concerns
Be aware of and follow local and national guidance – for example, from the RCGP, on the identification and management of patients presenting with signs of possible domestic abuse
Ensure your practice has a clear procedure in place for dealing with suspected domestic abuse
Liaise with local services who offer support for victims of domestic abuse
Consider the family as a whole and whether abuse is, or may be, present in the household. For instance, consider whether there may be children or others who potentially may be at risk
Be mindful of your duty of confidentiality and seek consent for disclosure unless there is a compelling reason not to do so
Seek advice if you are considering disclosure without consent or if consent is refused
Record your reasons for disclosing information and whether you have consent for disclosure and document your reasons if you decide not to share information
• Completely open scanner that is well tolerated by claustrophobic patients
• Weight-bearing scans for spine and joints enable a more precise diagnosis
• Patients who are large or cannot lie down can be accommodated

more information go online at: www.trulyopenmri.com or call: 020 7370 6003 0161 434 8039
Caring for patients with long-term conditions can be challenging, as they are often on longterm medications and have complex needs. Diane Baylis advises on how to manage these challenges and ensure patient safety
THERE ARE 15.4m patients living with a long-term condition (LTC), in England. The conditions are defined as one ‘that cannot, at present, be cured but can be controlled by medication and other therapies’.1
The number of people with LTCs is set to rise due to an aging population and unhealthy lifestyles.
With healthcare litigation increasing across all providers, and patients rightly expecting safe care, it is paramount that private doctors are aware of the risks and take steps to mitigate them – especially those related to managing the medication of those with LTCs.
Clinical negligence claims linked to long-term conditions
A review of Medical Protection’s high-value (£1m+) clinical negligence claims revealed that a poor standard of chronic disease management is a frequent factor.2
Deficiencies in chronic disease management made up 11% of these high-value claims, identifying that, over time, suboptimal
management of LTCs can cause more insidious development of complications.
Systems failures were found to be a main contributory factor, particularly:
Inadequate monitoring of the disease progression;
Inadequate assessment of the patient’s condition;
Failure to adjust treatment where necessary;
Failure to monitor and act on tests results.
Examples included:
☛ Inadequate monitoring of renal function in a patient with hypertension, leading to the development of chronic renal failure requiring dialysis.
☛ Inadvertent continuous longterm use of oral steroids in the treatment of severe asthma, leading to osteoporosis, back pain and disability.
☛ Failure to monitor a patient’s full blood count during carbimazole treatment, leading to the development of neutropenia.
Doctors must ensure they have a robust system for appropriate monitoring of LTCs, including:
1 The management of LTCs should be evidence/researchbased in line with national guidance; for example: NICE,3 National Guideline Centre,4 British Thoracic Society guidelines,5 GMC prescribing guidance.6
2 Systems for follow-up and review. Patients taking potentially nephrotoxic medication long-term should be regularly reviewed and consideration should be given to the need to monitor renal function.
3
Systems to ensure patients attend for blood monitoring and reviews. A patient known or suspected to have chronic kidney disease should be monitored and managed according to guidelines.

4 Systems to ensure abnormal blood results are appropriately followed up and advice communicated to the patient, including the stopping or adjustment of medication/treatment.
When undertaking an LTC review, you may also find it beneficial to consider the following:
The disease/condition:
Check the patient’s understanding;
Monitor disease progress.
Monitor and review:
Adherence to treatment (compliance, concordance);
Effectiveness of treatment;
Side-effects (symptoms);
Adverse effects.
Secondary prevention:
Check the patient’s understanding;
Assess and monitor the risk factors.
Effect on the patient:
How is the illness/condition effecting the patient’s life/work?
How is the illness/condition effecting family/carers?
Consent
When prescribing a new medication or re-issuing a prescription, issues relating to the consent process – for example, risk/benefits of the medication – should be highlighted to the patient as well as documented in the patient’s record.
Discussion of all the issues surrounding the treatment is an integral part of the patient’s clinical care.
These discussions may take place over several consultations, all forming part of the consent process. Provision of information is key to obtaining valid consent and the use of patient information
Provision of information is key to obtaining valid consent and the use of patient information leaflets can be used as a part of this process
References
1. DoH, Improving the health and wellbeing of people with long-term conditions (2010). http://webarchive.nationalarchives.gov. uk/20130107105354/http://www.dh. gov.uk/prod_consum_dh/groups/dh_ digitalassets/@dh/@en/@ps/documents/ digitalasset/dh_111187.pdf
3. National Institute for Health and Care Excellence (NICE): www.nice.org.uk/
4. National Guideline Centre. www.rcplondon.ac.uk/about-us/whatwe-do/national-guideline-centre-ngc
5. British Thoracic Society (BTS) guidelines:www.brit-thoracic.org.uk/ standards-of-care/guidelines/
leaflets can be used as a part of this process.
Globally, the population is living longer and presenting with multiple comorbidities that demand increasingly complex interventions, therefore the prevalence of LTCs will continue to grow. Patient expectations are changing, and this means that patients may be more likely to be dissatisfied and complain about their care.
It is likely that private doctors will increasingly be the focus of the care of these patients and it is imperative that they adopt a culture of safety and ensure safe systems for monitoring and managing patients taking longterm medications.
Diane
Baylis (below) is clinical risk educator at Medical Protection


2. Medical Protection Casebook, High value claims (May 2016) www.medicalprotection.org/docs/ default-source/pdfs/casebook-pdfs/ uk-casebook/uk-casebook_may_2016. pdf?sfvrsn=12
6. GMC: Good practice in prescribing and managing medicines and devices, www.gmc-uk.org/ethical-guidance/ ethical-guidance-for-doctors/ prescribing-and-managing-medicinesand-devices
Mrs D was a 70-year-old retired teacher who had struggled with recurrent UTIs. She was seen privately by Dr W, a urologist, who prescribed her antibiotics in the long term as a prophylactic measure and advised alternating between trimethoprim and nitrofurantoin. Sixteen months after commencing nitrofurantoin, she began to feel short of breath and also felt tired and generally unwell at a follow-up appointment.
Dr W documented that her urinary symptoms had improved. He conducted an examination including satisfactory BP and pulse. There was no ankle swelling or palpitations and he commented in the notes that Mrs D’s chest had no crackles or wheeze and no dullness on percussion. No blood tests were done at this stage.
Gradually, her breathlessness got worse and she noticed it even when sitting reading. Four months later, Mrs D was admitted to hospital via A&E in respiratory failure. A high-resolution CT scan showed pulmonary fibrosis, with the likely diagnosis being subacute pneumonitis secondary to treatment with nitrofurantoin.
Within a month of withdrawal of nitrofurantoin, she improved clinically, becoming less breathless and her respiratory failure resolved. Mrs D made a claim against Dr W, alleging he failed to consider that the long-term use of nitrofurantoin may have caused her symptoms.
We sought expert opinion from a clinical pharmacologist who referred to the relevant edition of the BNF, which stated on nitrofurantoin: ‘Cautions: on long-term therapy, monitor liver function and monitor for pulmonary symptoms especially in the elderly (discontinue if deterioration in lung function).’
She commented that although the BNF records the need to monitor periodically, the exact definition of ‘periodically’ is not given. In her view, it should have been every six months.
Medical Protection sees a number of claims regarding inadequate monitoring of long-term nitrofurantoin with patients developing hepatic or pulmonary complications. Many claims relate to inadequate systems for monitoring.
Expert opinion sought on these claims advises that BNF guidance for monitoring should be followed. To screen for hepatic complications, repeat prescribing of nitrofurantoin should generate liver function tests (LFTs) at least six-monthly.
To screen for pulmonary complications such as pulmonary fibrosis, doctors should advise patients starting on nitrofurantoin to attend urgently if they develop breathing problems. They could be reviewed for respiratory symptoms at the point of taking LFTs at least six monthly, with consideration of more frequent monitoring.
Our ongoing series by Philip Housden (below) reviews the 17 NHS trusts delivering private patient unit acute care services to the southern home counties of Kent, Sussex, Surrey, Hampshire and the Isle of Wight

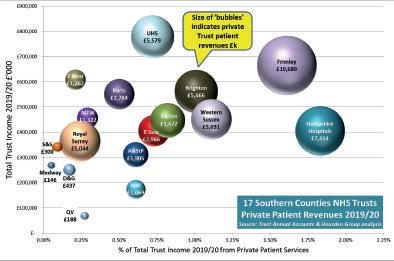
THE PANDEMIC has, of course, significantly changed the NHS PPU landscape in 2020, but the results this article and analysis is based on are those reported in trusts’ 201920 Annual Accounts, published last autumn.
Analysis shows that total private patient incomes declined by 0.5% from £55.8m to £55.5m, representing 0.78% of these trusts’ total revenues, down from 1.01% in 2016-17.
Results are ahead of the combined national average, excluding London, of 0.43% – including the capital, it is 1.04%.
The Southern Home Counties region remains the highest grossing area outside London. However, performance in 2019-20 was patchy, even before Covid, with some trusts routinely choosing to move bed capacity away from PPUs to core NHS supply during the winter.
Top trust by both overall earnings and percentage of turnover remains Frimley Health, which is based on its Parkside Suite brand.
Services are provided at Frimley Hospital, Surrey, with 26 en suite inpatient overnight rooms plus further day case capacity and beds and other services at Wexham Park, Slough, Berkshire.
The trust is planning further expansion on opening the new Heatherwood Hospital, Ascot, in the winter of 2021-22, providing care to both NHS and private patients from six operating theatres, 48 inpatient beds and 22 daycase cubicles.
Frimley Health delivered private patient incomes of £10.7m in 2019-20, up 13.4% and £1.2m from £9.4m the previous year. This is 1.61% of total trust incomes, up from 1.56%. The trust ranks 11th by total revenues in England and first outside London.
Neighbouring Hampshire Hospitals’ Candover Suite grew £0.6m in 2019-20 to £7.4m (9%). The 22 inpatient beds and a range of supporting outpatient and diag-
nostic services has supported sustained growth for several years and the trust has further room to grow in the Winchester market.
The trust still leads the region by percentage of total incomes, with private patients now accounting for 1.83% of trust revenues.
Brighton and Sussex grew by 12.6% and £635,000 to £5.7m without having designated PPU beds although offering services from the Royal Sussex County Hospital, the Royal Alexandra Children’s Hospital and the Princess Royal Hospital through the Select Healthcare brand.
The trust has significant potential for further growth if designating capacity within the hospital rebuild, now underway, and future trust mergers.
Southampton is fourth highest grossing by revenue in the region despite having no private inpatient inpatient beds. It relies instead on a range of day case and diagnostic capability, including a small number of chemotherapy day case beds.
Its private patient revenues declined by 0.7% in 2019-20 to £5m. Royal Surrey’s revenues fell by 10% to £5m in 2019-20. The trust’s private patient service is concentrated on delivering complex surgery and niche services including radiotherapy, nuclear medicine, brachytherapy and robotic surgery. These are delivered without having designated private inpatient beds. The trust has, however, opened the Shere Suite to provide private maternity care through reserving superior en suite rooms for new mothers, offered to those with a planned date for delivery.
Merger planned
At Western Sussex Hospitals, the trust delivers inpatient services from both the 16-bed Chichester Suite at St Richard’s Hospital, Chichester, which supports a wide range of surgical activity including bariatrics, and also the five-bed Downlands Suite at Worthing Hospital.
The trust is planning to merge with Brighton from April 2021 and
combined private patient earnings will then be on par with Frimley Health’s.
Epsom and St Helier’s private patient revenues fell by £1.1m from £4.8m to £3.7m in 2019-20. The trust has potential for further growth out of the 20-bed Northey Suite at Epsom and further untapped opportunities out of the St Helier site.
East Sussex Hospitals had a good year, increasing income from £2.1m to deliver £3.0m for the first time, a growth of 39%. This was achieved following a strategic review by concentrating on tariff strengthening, income capture and building consultant relationships.
The 19-bed Michelham Suite at Eastbourne General Hospital has been partially refurbished in order to take advantage of BMI’s closure of 52 bed Esperance Hospital, in the town in July 2019.
Along the coast, Portsmouth Hospitals’ Harbour Suite has 13 protected private beds and supported the trust returning to growth in 2019-20, with an increase of £440k to £2.8m – up 19%. The unit offers a step down from critical care and has been redirected to Covid support for some time.
Ashford and St Peter’s fell back by £200,000 to £1.9m. The trust has from time to time reviewed its relationship with BMI Healthcare regarding the onsite Runnymede Hospital and the opportunities this could present for increasing private patient revenue.

Maidstone and Tunbridge Wells experienced a further fall of 9% and £137,000 in 2019-20 to £1.3m. This is the sixth year that income has fallen from the high of £8.1m in 2013-14.
The drop can be explained due to the loss of inpatient capacity to NHS demands and also competition from GenesisCare for private cancer services.
But actions taken following a review of the future opportunity undertaken in 2018-19 has in part arrested the decline. This review led to the reinstatement of private patient beds within a smaller Wells Suite of eight beds re-opened just prior to the onset of the pandemic.
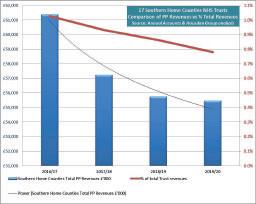
East Kent owns Spencer Hospitals, a subsidiary company managing PPU services of varying size out of Margate, Ashford and Canterbury. The trust has opportunities to grow through future trust site and service reconfiguration.
Spencer provides NHS Choose and Book and was one of the first multi-site PPU ‘chain’ brand. It has total income from all sources of over £10m. However, the trust reported a decline of 55% and £1.5m last year to £1.25m private patient income.
It is not known if this decline is due to the accounting treatment of Spencer as a trading subsidiary or the result of actual trading performance.
Five remaining trusts were at or under £1m a year revenues. Isle of Wight has reduced private patient bed capacity and declined by £155,000 and 13% to £1.1m. Dartford and Gravesham was down £208,000 and 32% to £437,000; Surrey and Sussex held steady at around £300,000.
Queen Victoria Hospital in East Grinstead, £40,000 down (18%) to £188,000, is also reviewing the opportunity to merge with Brighton and Sussex ,which would then bring the regional burns and plastics centre within scope of private patient services development.
Medway was up £15,000 to £146,000 and is not known to be considering developing a private patient service.
Looking beyond the present extreme impact of Covid on resources, capacity and forecast earnings for 2020-21 and 2021-22, the region can be expected to return to delivering significant revenues for trusts from private patients.
However, given that medical insurance and self-pay demand rates are strongest in the Southeast, it is considered that at least half of the region’s trusts are underperforming their local catchment market for private patients and are therefore missing out on several millions of pounds worth of revenues a year.
Into 2021-22, this will be a market ready for re-investment in capacity. Perhaps recent and potential trust mergers, and the experience of working with the independent sector during the pandemic, might open up options for trusts to consider new partnerships and joined-up working to take advantage.
Next month: the Northern Home Counties
Philip Housden is managing director at Housden Group commercial healthcare consultancy

It’s back! Dr Tony Rimmer (right) tests the latest version of an old favourite that has wooed doctors for decades



WE ALL feel comfortable with a bit of familiarity.
Our patients feel more comfortable with us and trust us more if we have met them more than once. We both know pretty much what to expect of each other. The relationship has great value.
If car manufacturers can do the same and build a product that inspires confidence in potential buyers, then they achieve more sales and, over the years, repeat business.
There is one car maker that has done just that with its medical clientele. The Volkswagen Golf has been the doctors’ favourite for the last three decades.
The Golf’s blend of style, practicality, quality and affordability has ticked all the boxes for many of us medics. The range is broad enough to accommodate all individual needs, from the functional base models up to the sporty range-topping GTI and R models. As has been quoted many times, it is ‘all the car you’ll ever need’.
Since the launch of the Mark 1 in 1974, the Golf has kept up with all the automotive advances the industry has developed through successive revised models while keeping all the features that loyal buyers value.
The compact hatchback shape has evolved slowly with no major styling departures to frighten off new or repeat customers. Under the skin, there have been some significant changes over the years with different chassis, engines and drivetrains.
However, perhaps the biggest and most challenging technical
change sweeping the motor industry is electrification. Although VW has produced an all-electric e-Golf Mk 7 since 2015, it has been compromised by using the same chassis as its combustion engined siblings.
A whole new approach was needed and Volkswagen has built a dedicated electric platform for its new iD3 which will be the ‘Golf for the future’.
So, does that mean the end for the regular Golf? No, it doesn’t. There is plenty of life left in the petrol- and diesel-powered hatchback, and to show its confidence in the product, VW has released the new Mark 8 Golf.
Again, the range is extensive with a GTI and R models, but there will not be an e-Golf variant – the iD3 fills that role.
At entry level is the 1.0litre three-cylinder 108bhp petrol engine. Then we have the 1.5 litre four-cylinder 128bhp or 148bhp petrol engines. Two versions of the 2.0 litre diesel powerplant (113bhp and 148bhp) are still offered.
There is a brand new 48v mildhybrid system available on the bigger petrol engines. This is essentially a 48v starter motor/ generator that can recover energy on braking and redeploy up to 16bhp and 25Nm to boost and smooth out acceleration. It is only available with the automatic direct-shift gearbox (DSG).
I have been driving this latest version of the Golf to see what changes have been made to keep it fresh and appealing for us loyal followers.
My test car was a 1.5litre petrol

Externally, VW has not messed with the styling too much
VW GOLF 1.5 etsi 150ps style dsg
Body: Five-seat hatchback, front-wheel drive
Engine: 1.5litre four-cylinder turbo petrol
Power: 150bhp
Torque: 250Nm
Top speed: 127mph
Acceleration: 0-62mph in 8.4 secs
Claimed economy: Combined 49.55mpg
CO2 emissions: 130g/km
On-the-road price: £28,035
eTSi mild hybrid 150bhp model with DSG. First impressions are that, externally, Volkswagen has not messed with the styling too much.
Although the frontal aspect is lower and the rear LED lights have been redesigned, this is instantly recognisable as a Golf.
It is only when you step inside do you see the true extent of the thorough modernisation that has been applied.
Digital dials sit in front of the driver and a large central touchscreen now takes over from the physical knobs and switches of previous models. It is fresh and modern but takes a little getting used to.
The DSG gear selector is now a small central lever and the dashboard is much less cluttered. Technologically, Apple CarPlay and Android Auto are standard and the infotainment has been updated accordingly.
The five-door hatchback body is basically the same as the Mark 7, so the typical Golf roominess and versatility remain unchanged. The
chassis is pretty much the same too so the handling, ride and roadholding is as it was before.
As for the 48v mild-hybrid system, it works smoothly and effectively to give the impression that, around town, the engine is bigger and torquier than the 1.5litre engine on board.
The only downside to all these changes is that there is less obvious higher quality trim around and the Golf now feels little different from its SEAT or Skoda siblings. I would suggest that this is deliberate, as Volkwagen will increasingly be focused on its all-electric iD range. The latest Golf Mark 8 remains an excellent all-rounder. The option of a variant to satisfy all tastes is impressive.
I reckon that the new GTI will be a great driver’s car and I think that the latest plug-in hybrid GTE with an increased electric-only range of up to 43 miles will appeal to many of us who want to step towards electrification without making a complete commitment.
Dr Tony Rimmer is a former NHS GP practising in Guildford, Surrey


A successful private practice is key to ensuring that your hard efforts and precious time are rewarded. But there are a number of key aspects that can make or break the success of your business.
In no particular order, Ian Tongue highlights the following key areas that can be a sure-fire way to experience difficulties and possible failure of your practice – such as putting all your eggs in one basket

Having spoken at many events about private practice best practice, a common theme emerges from consultants who have a successful independent practice: their choice of secretary.
A secretary needs to be efficient throughout the process, which starts with initial patient contact, but, for many, involves taking things right through to receiving payment.
With patients’ first contact being with the secretary, ensure that the secretary has the right manner with patients – and being available is extremely important, otherwise work can be lost.
With such control over the billing process, if this is not working efficiently, you could end up not getting paid, which is akin to working for free. In extreme circumstances, a lack of financial ability can cause significant financial loss for the practice.
2 Not having a medical accountant
Having the right team is not limited to your secretary. A specialist medical accountant cannot only advise you on tax and accountancy matters but can provide prac-
tical guidance in running a private practice.
They should also have excellent knowledge of the NHS Pension Scheme and how annual allowances charges arise and can be managed. Bad advice can lead to significant financial loss.
A good example of this are the forthcoming pension changes known as the McCloud remedy (see page 1 and 3), which few nonspecialist accountants will understand and be able to advise on – possibly resulting in unnecessary tax being paid.
3 Not seeing private practice as a business
Medics do not usually have any financial training, and embarking on running a private practice can be daunting. It often can be a challenge to overcome the barriers for charging patients for your time, which is an alien concept.
It is essential that you treat your private practice as a business from day one and a medical accountant is best placed to offer practical guidance on how to do this.
Without doing this, it is likely that you will end up with problems such as fees written off due to money not being collected or not understanding how the insurers
pay you and how patients can often have an excess payment which can be deducted from your fees.
4 Operating your private practice with a taxinefficient trading structure
Choosing a trading structure that is most appropriate to your circumstances is really important. While it will not necessarily cause the failure of your private practice, it can often be an indirect factor when deciding whether it is worthwhile financially to carrying out private work.
In certain earnings zones, you can be paying extremely high tax rates, which can make you decide to cease private work when some tax planning could have mitigated this and allow you to have a financially viable private practice.
5 Investing in the wrong equipment
In certain specialties, particularly cosmetic, the pace of technological change can be fast and the next ‘wonder’ treatment is always round the corner. Some of these may well be viable, but the equipment itself to carry out such work can often be very expensive.
As doctors, you are almost
Choosing a trading structure that is most appropriate to your circumstances is really important
always a good credit risk, so there will be no shortage of available finance to obtain equipment. But that does not mean that the longevity of the treatment is sound and, in some cases, the treatments do not turn out to be the next wonder treatment – leaving you with equipment that cannot be used but you are still paying for. This can be a very expensive mistake.
6 Not saving enough for tax
Not saving for tax can be a sure-fire way to feel that it’s not worth carrying out private practice and it can lead to significant distress. The tax system can be complex, but there are some basic things which can alleviate most surprises when it comes to your tax liability. It would surprise many that if you commenced your private practice in, say, May of 2021 you
would pay no income tax on the earnings as a sole trader or divi dends from a company until January 2023.
As you would expect, the first tax bill can be a bit of a shocker, so it is best to get into the habit of saving monthly and providing your tax and accounting records to your accountant soon after the financial or tax year-end.
7
Having all eggs in one basket
One thing that Covid has laid bare is the fragile capacity of the NHS and how the Government used powers to take over many of the key private hospitals.
No one would have anticipated that before Covid, but it highlights how having admitting rights in more than one private hospital can spread risk, as certain hospi tals had significantly more capac ity to offer private work than others.
This situation is a driver for many looking for their own facili ties that can help manage the impact on the private medical sec tor for any future pandemics.
8 Lack of marketing and having a poor website
In the digital age that we live in, one of the first things that a patient is likely to do when look ing for private medical treatment is to search for you on the internet. Ask yourself whether a patient would have a positive result from doing this or would they see an outdated website that could give the impression of disinterest.
For certain specialties, having an excellent website and marketing strategy is essential and not embracing this can lead to the pri vate practice not being viable, irrespective of how good a surgeon or physician you are.
Private hospitals usually have liaison teams for their consultants to help you promote yourself, so take on board their assistance. At the end of the day, you have a com mon objective and they will have a team dedicated to your success.
9 Medico-legal exposure
Medico-legal work has, for many, been a lifeline through the Covid crisis, but it does come with its own set of pitfalls that need to be understood.
You must choose wisely when it comes to deciding who you are going into business with, as a group that is not successful can result in significant financial loss



With 58% of doctors now suffering from some form of anxiety or depression – and 46% saying their condition had worsened since last March – we begin serialising sections of a new book edited by Dr Clare Gerada (right). This month: Doctors and mental illness


A MEDICAL DEGREE gives no protection from the normal vicissitudes or hardships of life. Doctors have the same mental illnesses as the general population.
Where doctors do differ is not in the illnesses they get, but rather in how they present, their prevalence, potential impact and outcome.
Perhaps the most significant difference is how hard it is to cross that invisible boundary from professional to patient, even when that boundary is for a physical, rather than a psychological disorder.
I am guilty of this myself. When knocked off my bike en route to my evening surgery, instead of abandoning ship and going to the accident and emergency department, I hailed a taxi and completed the clinic – with blood oozing from my foot and in great pain.
It did not cross my mind that I could have cancelled and sought help. This was a physical illness. It is even harder for doctors to seek help for mental illness. For doctors, mental illness is their shameful secret, hidden from sight.
This means large numbers of depressed and anxious doctors are denied help – usually through their own reluctance to seek it. It is vital that this ‘secret’ comes into the open and that they are able to receive appropriate treatment.
This is not just for the doctor’s sake, but also for their patients, since untreated mental illness is linked to more medical errors.
High rates of mental illness in doctors are a global phenomenon. In every system – privately, insurance or nationally funded – and across all specialties, ages, gender, and levels of seniority, doctors are at risk of mental illness.
A review in 2010 identified 19 papers on depression and anxiety in doctors. The reported rate varied from 14% to 60%.
Current levels of depression, as determined by an Australian survey, showed similar rates to the general population, but higher than for other Australian professionals. Approximately 21% of doctors reported having ever been diagnosed with or treated for depression and 6% had a current diagnosis.
Another review published in 2014 found 112 articles on depression in American doctors. Rates of depression ranged from 1% to 56%, an enormous variance, reflecting sample size, methodology used and cut-off limits for ‘caseness’.
The larger and more robust studies included in this review found between 22% and 35% of doctors reported between four and five symptoms of depression.
A similar figure was found in another systematic review, which included 54 cross-sectional and longitudinal studies involving 17,560 hospital trainees from 18 countries.
Similar levels of depression were found regardless of the country in which the study was done, and gave a pooled prevalence of around 30%. There is a trend for newer studies to find higher rates, which, while modest, is notable given the reduction in duty hours and improved working conditions over the last decade.
A study of American interns found the percentage of doctors meeting the diagnosis of severe depression increased from 4% before starting work to 27% one year later. Overall, over the 12 months, 42% of the doctors met the criteria for depression at one or more of the quarterly assessments, though only 23% sought help.
The pressure to address overwhelming medical needs, intensity of workload, difficult clinical encounters and being sued or facing complaints are all contributors to high rates of mental distress.

Everyone is familiar with the term ‘anxiety’ and no part of our daily lives can be free from it. Where anxiety becomes a problem is when it becomes pervasive and the symptoms begin to interfere with work, life and relationships. Three of the most common anxiety disorders doctors suffer from are generalised anxiety disorder (GAD), panic disorder and posttraumatic stress disorder (PTSD), with GAD being the most common.

GAD is characterised by out-ofcontrol, intrusive anxiety present for most days, about several subjects for more than six months.
Anxiety is less well studied among doctors than depression has been, and studies are of lower quality, as they do not tend to use formal diagnostic instruments, and therefore ‘anxiety’ tends to encompass a range of different diagnoses, from ‘stress’, ‘psychological distress’, generalised anxiety or phobic anxiety states.
Evidence-wise, it is not possible to say whether rates of anxiety are more, less or the same as in the general population. Experiencewise, generalised anxiety is a common finding in the doctors we see in our service, either presenting alone or alongside a depressive disorder.
I would suggest that anxiety is almost pathognomonic of being a doctor in today’s healthcare system. There are so many anxietyprovoking events in clinical practice that it has become normal for doctors to ignore their racing heart, fearful thoughts or the vague feeling of constant nausea in their everyday lives.
Exposure to traumatic events is generally unavoidable in medicine, but more so for those who work at the front line of acute care such as A&E, intensive care, anaesthetists, surgeons and obstetricians.
For all doctors, though, contact with dying patients, serious injury, patients with intense pain and distress is commonplace in their everyday clinical lives.
Outside their consulting rooms, doctors also experience further traumatic events from being subjected to bullying, complaints, assault or racism.
Most people who are exposed to a traumatic event have no adverse long-term problems and resume their normal functioning. Some may even have an increase in wellbeing, confident that they handled the event or themselves well.
A small number, however, will experience a range of adverse psychological effects, including PTSD.
Symptoms include persistent thoughts, images, flashbacks or

Adapted from Beneath The White Coat: Doctors, their minds and mental health (chapter 9), edited by Dr Clare Gerada, ©2021 Taylor & Francis, ISBN: 9781138499737
Price: £22.99
Independent Practitioner Today readers can save 20% on Routledge.com with discount code BWC21. Offer ends 31 August 2021. Order now: www.bit.ly/ Routledge_IPT
dreams in response to reminders of the event, the desire to avoid discussion or reminders of the trauma and a host of other symptoms such as loss of interest, withdrawal and anger.
Symptoms need to be present for more than one month and not caused by medication, substance use or other illness.
Awareness is increasing that those working in the front line of healthcare also suffer from this disorder.
A past chairman of the GMC once remarked that doctors should take a leaf out of army personnel and learn to be resilient. He was referring to dealing with complaints and referrals to the regulator, but his comments were taken as a general view that doctors were not resilient enough to survive the rough and tumble of a career in medicine.
I imagine he now regrets this comment, but the sentiment behind it, that working in the NHS is akin to serving in the armed forces, seems a good analogy given the prevalence of PTSD in healthcare staff.
Over the decade, my service has cared for hundreds of doctors with various forms of addiction, mainly alcohol and drug, but also others too, including gambling, sex and porn addiction.
I am often struck how far doctors need to fall before they reach out for care. Often, they continue drinking and using drugs despite serious relationship difficulties, problems at work, loss of livelihood, housing and physical illness.
This is the nature of addiction, compulsion to use, despite harm done to self and others. Untreated, the doctor is likely to present in a crisis, potentially following a drink-drive offence, being caught stealing drugs from work or having an accident.
Some die before they get the chance to present at all, whether through accident or suicide.
Overall, drug and alcohol use are probably lower in doctors than in the general population, though in the absence of large studies, it is not possible to be certain.
➤
An individual with a personality disorder thinks, feels, behaves or relates to others differently. There is scant research into doctors with this disorder, possibly due to it being uncommon, but also because of the difficulty of diagnosing it.
It is likely to be even less common in medicine, as medicine selects against some traits common in people with personality disorders – such as poor impulse control, lack of empathy – and for ones such as resilience and obsessiveness.
In my experience, where personality disorder does present, it is accompanied by performance issues at work or professional misconduct, such as boundary violations.
When you look back into these doctors’ histories, often there are repeated complaints the doctor was ‘not a team player’, they become angry when stressed and elicited fear, shame and rage in others, and consequently distress in their teams. Not all disruptive behaviour is due to an underlying personality disorder, some might be just bad behaviour.
Whether doctors have the same, lower or higher rates of mental illness than the general population is not the main issue.
What is important is ensuring that this group, who, after all, have a critical role to play in the care of millions of people, receive timely help such that they do not pose a risk, not just to themselves but also to the patients they manage.
Doctors with mental illness are more likely to stay at work than not – a term called presenteeism –and working at suboptimal levels due to their symptoms.
There is evidence that medical errors are more common in depressed doctors, both an increase in self-reported errors and also when objectively measured. Depression is closely correlated with fatigue, which might explain the higher levels of medical errors found in doctors with this condition.
Mental illness matters, as it has a significant macroeconomic impact too. In the UK, the total cost to employers of mental health problems among their staff is estimated at nearly £26bn each year: £8.4bn from sickness absences and £15.1bn from reduced productivity at work.
While these figures are for all staff, doctors are an expensive resource and their absenteeism will place a large hole in services finances.
A mentally unwell doctor is likely to enter a downward spiral as feelings of hopelessness and worthlessness lead to declining performance and a greater risk of errors, causing further despair. Patient care and professional standing can then be placed at risk, possibly leading to more complaints and concerns. This is why it is so important to minimise the barriers to accessing care.
It appears that doctors do have higher rates of mental illness, certainly in the more common conditions, such as depression and anxiety. It is perhaps not surprising given the nature of their work. Next month: Burnout in doctors
Dr Clare Gerada is medical director of the Practitioner Health Programme, London, and a former RCGP chairman


Profits
for radiologists have shown a welcome rise – despite heavier costs in this specialty. Ray Stanbridge reports on our latest benchmark survey
SOME RADIOLOGISTS believe they are the Cinderella of the medical profession – pushed around by hospitals and some of their surgical and medical contemporaries and badly treated by insurance firms. Our figures, however, tend to contradict this not uncommon view.
Figures for our latest benchmark survey find that average incomes for this specialty from private practice rose by about 9% from £154,000 in 2018 to £168,000 in 2019.
Costs rose by a surprising 21% from £37,000 to £45,000.
As a result, taxable profits rose by 5% from £117,000 to £123,000. However, it should be noted that margins appear to have fallen from 76.1% to 73.2%.
What are the reasons for these figures?
We have seen continuing growth in the market for diagnostic services in excess of growth rates in the market itself.
A growing number of patients continue to pay for diagnostic services themselves and this continues to offset pressures on fees from
AVERAGE INCOME AND EXPENDITURE OF A CONSULTANT RADIOLOGIST WITH AN ESTABLISHED PRIVATE
and, in some cases, hospital groups.
We also continue to hear of a shortage in supply of newly qualified radiologists and this, in micro-economic terms, suggests a long-term upward pressure on fees and incomes.
Why have costs risen fairly significantly over the year?
We have noted, as with other disciplines, that staff costs continue to rise broadly in line with the growth in personal tax allowances.
Use of home costs have risen sharply as an increasing number of radiologists now do much of their reading work from home. Indeed, some now have quite sophisticated home offices to enable them to perform their duties.
Directly correlated with this trend has been the growth of ‘other expenditure’ for many radiologists; this has involved investment in IT equipment at their home offices.
Home office costs have also risen again, reflecting the trend for increasing use of home. Other costs have remained broadly the same between 2018 and 2019.
In our 2020 report, we felt that

radiologists continued to have a bright future. We see no reason to change this view.
I have commented regularly in the past about the difficulty of effecting year-on-year comparisons of incomes and expenditures of the various specialtiess.
Some radiologists have incorporated their businesses. Others have become members of both formal and informal groups. Yet others have invested in equipment in partnership with hospital groups or others.
As I stated in 2020: ‘The market
structure is in a constant state of change and while our survey should not be taken as significant, it does provide a reasonable snapshot of what is happening to the average private radiologist practice over the years.’
Finally, I list the requirements for radiologists to qualify for our survey. Consultant radiologists must:
Have at least five years’ experience in the private sector;
Earn at least £10,000 gross from private practice;
Hold either a new-style or oldstyle NHS contract;
Be seriously interested in private practice as a business. This condition effectively excludes most small earners who look to their practice as primarily to meet school fees and holiday costs;
Work as a sole trader, through a formal or informal partnership, limited liability partnership, group or a limited liability company.
Next month: Urologists
Ray Stanbridge is a partner with accountancy, finance and tax advisory medical specialists, Stanbridge Associates Limited
Years ending 5 April
Source: Stanbridge Associates Ltd







Coming in our April issue, published on 6 April.
Burnout in doctors is the big topic tackled in our serial adaption from the new book, Beneath The White Coat –doctors, their minds and mental health. We all have ebbs and flows in job satisfaction, and years of being in the psychological trenches with our patients will have its effects.

Emotional depletion, negative attitudes towards patients and the feeling we cannot achieve more are not uncommon, and hopefully fleeting symptoms. Dr Clare Gerada explains what can be done about it
When things go wrong – the MDU presents a round-up of learning points arising from orthopaedic surgeons in private practice
Medical Billing and Collection looks to the future
Over 20,000 independent practitioners already have a profile on The Private Practice Register (The PPR) which enables them to keep their essential information and documents in one place and connect seamlessly with insurers and hospitals. Healthcode’s Fiona Booth looks at what they can expect from the next phase of this innovative project
For independent practitioners who employ staff, Hempsons’ solicitors provide an employment law round-up and look at what to expect in 2021
Branding your practice. Simon Marett has more advice to help you close the gap between good and bad
The
Published by The Independent Practitioner Ltd. Independent Practitioner Today is editorially independent and thanks Bupa for its assistance with distribution. Material is governed by copyright. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form without permission, unless for the purposes of reference and comment. Editorial layout is the copyright of the publishers. If you wish to use it for promotional purposes on websites or for reprints, we would be happy to discuss licensing the copyright to you.
© The Independent Practitioner Ltd 2021 Registered office: 7 Lindum Terrace, Lincoln LN2 5RP

The madness of markets. Markets can often feel like they have gone a bit mad. It is easy for doctor investors to fall into the trap of FOMO (fear of missing out) and wish they had more of a certain stock, group of stocks or sector in their portfolio. But Cavendish Medical warns the overwhelming evidence says this is a bad idea
If you work in a private patient unit in the northern home counties or hope to do so again soon, check out Philip Housden’s analysis of their earnings. He foresees opportunities to develop new NHS private patient services in this region
Personal development for leaders. It is possible for anyone to improve their leadership and management skills and the best starting point is improving self-awareness, says Jane Braithwaite. She explores some of the best tools and methods available to leaders and managers
Urologists’ private earnings come under the spotlight in our benchmarking series Profits Focus
Business Dilemmas hears from a doctor who was redeployed to support colleagues in the NHS at the start of the pandemic. He will continue to do so, but has decided to retire from private practice. MDU medico-legal adviser Dr Sissy Frank explores the issues around patient records to consider so that he can retire in an ethical, yet timely manner
Our motoring correspondent Dr Tony Rimmer reports on the Polestar 2, Volvo’s all electric sub-brand
Plus all the latest news, views and regular features. Don’t forget to see our weekly news updates on our website!
ADVERTISERS: The deadline for booking adverts in our April issue is 19 March
Write to Independent Practitioner Today 7 Lindum Terrace, Lincoln LN2 5RP
CHANGING ADDRESS, EMAIL ADDRESS OR SUBSCRIPTION DETAILS?
Phone 01752 312140 or email karen@marketingcentre.co.uk
TELL US YOUR NEWS
Robin Stride, editorial director
GET A SUBSCRIPTION DISCOUNT!
£90 independent practitioners.
£90 GPs and practice managers (private & NHS).
£210 organisations.
Save £15 paying by direct debit: individuals £75 (organisations £180). TO SUBSCRIBE
Email karen@marketingcentre.co.uk or phone 01752 312140

Email: robin@ip-today.co.uk Phone: 07909 997340 @robinstride
ADVERTISE WITH US

To advertise in the journal or our website business and lifestyle directories, contact advertising manager Andrew Schofield at Spot On Media. Phone: 0161 408 3912 Email: andrew@spotonmedia.co.uk
Publisher Gillian Nineham Phone: 07767 353897.
Email: gillian.nineham@gmail.com
Guarantee delivery of your next copy of Independent Practitioner Today. Take out a subscription and you will get full access to our news, features and previous issues on our website. See details on the left.
BACK ISSUES: £12.50 including post & packaging Follow Independent Practitioner Today on




