
2 minute read
Welcome to My Blood, My Health Digital Magazine
from MBMH Issue 4 English
by healcanada
Welcome to the fourth issue of "My Blood, My Health" magazine. This December edition is dedicated to innovative treatment approaches. CAR-T cell, Gene therapy, and new targeted treatments have been made accessible recently to patients afflicted with blood disorders. These innovations are crucial to improving patientlifeexpectancyandqualityof life(QoL).
With this magazine, we aim to pursue Heal Canada's mission to empower patients to access better andequitableservices.We'redeeply grateful to our readers for their continued interest and support. Yourengagementdrivesustobring insightful and valuable content to encourage patient-centricity in healthcare.
Thank you for participating in our journey, and welcome to this enlighteningissue!
Fromyourdedicatedteam

Cheryl Petruk, MBA B.Mgt. CEO & Founder of Heal Canada
Brigitte Leonard, Ph.D Chief Scientific Officer
My Blood, My Health Director
Heal Canada is a registered Not For Profit Organization in Canada healcanadaorg
Disclaimer: The Patient Advocacy Digital Magazine provides general information and resources to promote patient empowerment and awareness. The content is not a substitute for professional medical advice or treatment. Always consult with qualified healthcare professionals for personalized guidance regarding your specific medical condition or situation
What is CAR T-cell Therapy, and Why is it Important?
Cheryl Petruk, MBA
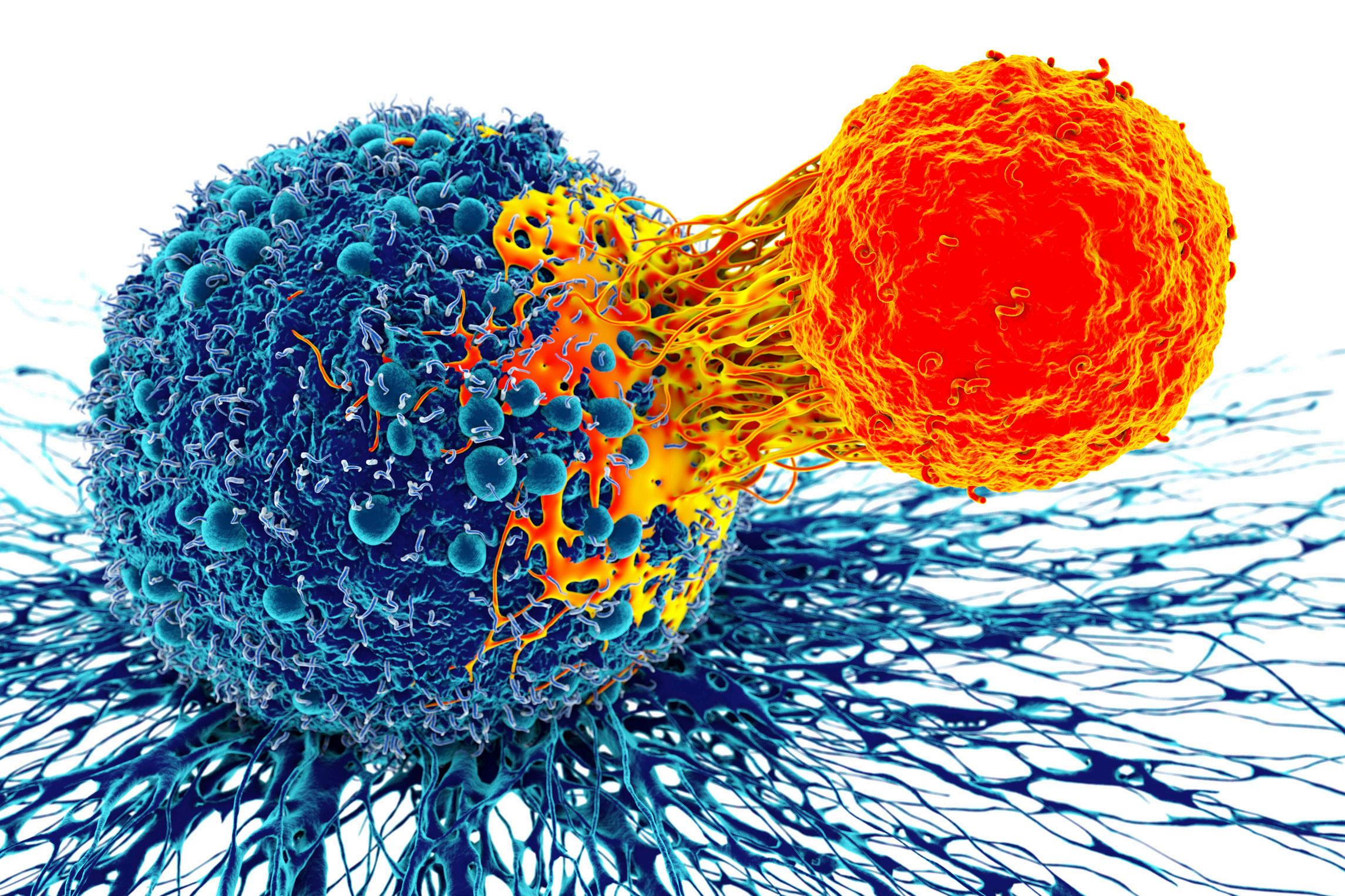
Chimeric Antigen Receptor (CAR) T-cell therapy represents a breakthrough in the field of immunotherapy, offering hope to patients with certain types of cancer that have resisted traditional treatments like chemotherapy and radiation. This innovative approach involves genetically engineering a patient's own immune cells to fight cancer more effectively. By harnessing the body's natural defence mechanisms, CAR Tcell therapy has opened new avenues for treating blood cancers and is expanding into the treatment of solid tumours.
In this article, we explore the fundamentals of CAR T-cell therapy, its importance in the fight against cancer, how it works, the types of diseases it treats, and the future of this groundbreaking treatment. We also discuss the challenges and potential risks associated with CAR T-cell therapy and highlight why patient advocacy is crucial for expanding access and improving outcomes.
How Does CAR T-cell Therapy Work?
At its core, CAR T-cell therapy is a type of adoptive cell transfer. It is a form of immunotherapy in which a patient’s immune cells are collected, modified, and then infused back into the body to target cancer cells. CAR T-cell therapy specifically focuses on T-cells, a type of white blood cell that plays a crucial role in the immune response.
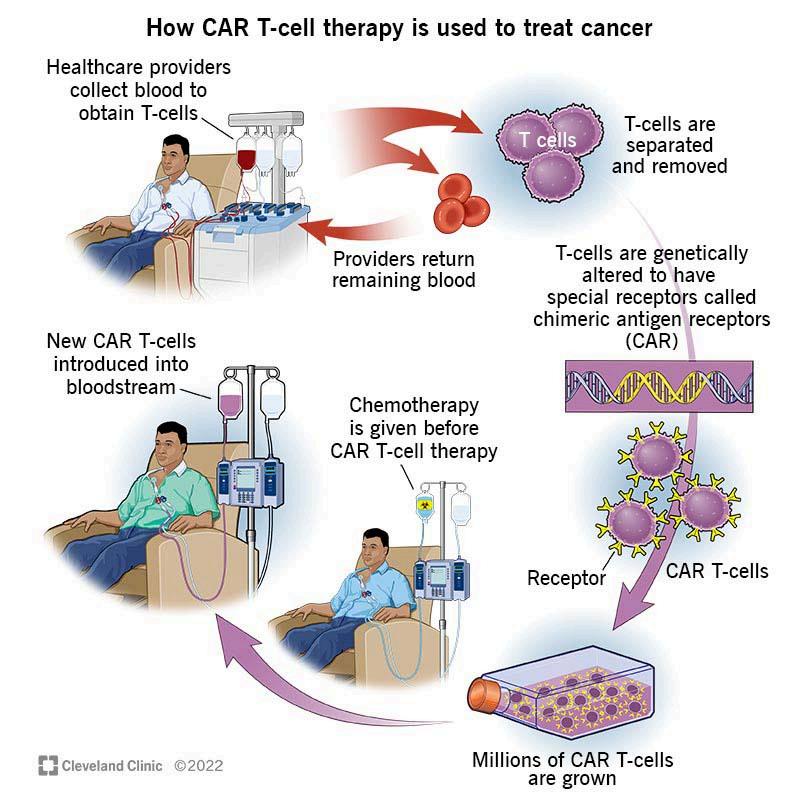
The process of CAR T-cell therapy involves several key steps: Collection of T-cells: First, blood is drawn from the patient, and T-cells are isolated through a process called leukapheresis These cells are then sent to a laboratory for genetic modification.
1. Genetic Modification: In the lab, the T-cells are genetically engineered to express a chimeric antigen receptor (CAR) on their surface. This receptor enables the T-cells to recognize and bind to a specific antigen found on the surface of cancer cells.
2. Expansion of Modified T-cells: Once modified, the CAR T-cells are expanded in large numbers This process ensures there are enough engineered cells to target and destroy the cancer effectively.
3. Infusion: The modified CAR T-cells are infused back into the patient, where they begin hunting down and destroying cancer cells. These engineered cells continue proliferating in the patient’s body, providing ongoing surveillance against cancer.
5.
4. Targeting Cancer Cells: The CAR T-cells are designed to recognize specific proteins on the surface of cancer cells, such as CD19, which is commonly found in certain blood cancers When the CAR T-cells bind to these proteins, they trigger a potent immune response, destroying the cancer cells.





