SPONSORSHIP GUIDE FALL 2023
Welcome to HCAA’s Annual Digital Sponsorship Guide. We at HCAA have had an amazing trajectory of successful conference events. We know this success could not have happened without the partnership of our sponsors. Since its inception in 2020, our Digital Guide has focused on providing another opportunity for our amazing Sponsor Partners to let you know about their very valuable products and services.
We invite you to please take time to use it to find out more about what they offer! Remember, here at HCAA, it is always about “the value of connection”!
Carol Berry, HCAA CEO
Susan Crolla, Executive Director
Contents 6 Degrees ........................................ 6 AccuRisk Solutions .............................. 150 Advanced Medical Pricing Solutions (AMPS)........... 8 aequum, LLC ................................... 150 Alaffia Health .................................... 10 Amino Health 12 AMWINS 14 Availity ........................................ 150 CareGuide Advocates ............................. 16 Carelon RX ...................................... 18 Cedar Gate Technologies ......................... 20 Cervey 22 ClaimDOC 24 ClaimReturn, LLC 26 Claros Analytics .................................. 28 Community Health ............................... 30 Comprehensive Healthcare Systems ................ 32 Coral .......................................... 150 CVS Health 34 DataPath, Inc. 36 Deerhold ....................................... 38 Denniston Data, Inc. ............................. 151 ECHO Health, Inc ................................ 40 Excess Reinsurance .............................. 42 EZaccessMD..................................... 44 First Dollar 46 Frazier Healthcare Partners 48 Goodroot, Inc. ................................... 50 Gradient AI...................................... 52 Healthcare Bluebook ............................. 54 Healthee........................................ 56 Health in Tech 58 Health Payer Consortium 60 Hercules Health ................................. 62 Hines & Associates .............................. 151 Hi-Tech Health .................................. 64 Homestead Smart Health Plans .................... 66 Ikigai Growth Partners ............................ 68 Imagine360 70 Integrated Payor Solutions 72 Javelina from Mphasis ............................ 74 Liberty Mutual Insurance Company ................ 76 Liviniti .......................................... 78 MDI NetworX .................................... 80 MedWatch ...................................... 82 Medxoom. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 84 MPowered Health 86 Nokomis 88 Ocozzio ......................................... 90 OptumRx ....................................... 92 Payer Matrix .................................... 94 Phoenix Benefits Management .................... 96 Planwatch 151 Prescryptive Health 98 Prime/MRx 100 Renalogic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 102 Rocky Mountain Review .......................... 104 RxBenefits ..................................... 106 Scripius PBM ................................... 108 ServeYou RX 110 Sharecare 112 Smart Data Solutions ............................ 114 Swiss Re Corporate Solutions ..................... 116 TALON ........................................ 118 The Phia Group ................................ 120 TrueRx ........................................ 122 US Benefits Insurance Services 124 Vālenz® Health 126 Varis LLC ...................................... 128 VBA ........................................... 130 Vida Health .................................... 132 Viveka Health .................................. 151 Walmart Health Virtual Care 134 WellRithms 136 Welvie ......................................... 138 WEX .......................................... 140 WithMe Health ................................. 151 WLT Software .................................. 142 Xevant. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 144 zakipoint Health 146 Zelis 148
Sponsorship Guide Table of
– A –
Audit/Actuarial/Financial Services
Nokomis 88
Varis 128
Varis LLC 128
– B –
Broker/Consultant
Frazier Healthcare Partners 48
Hercules Health 62
Ikigai Growth Partners 68
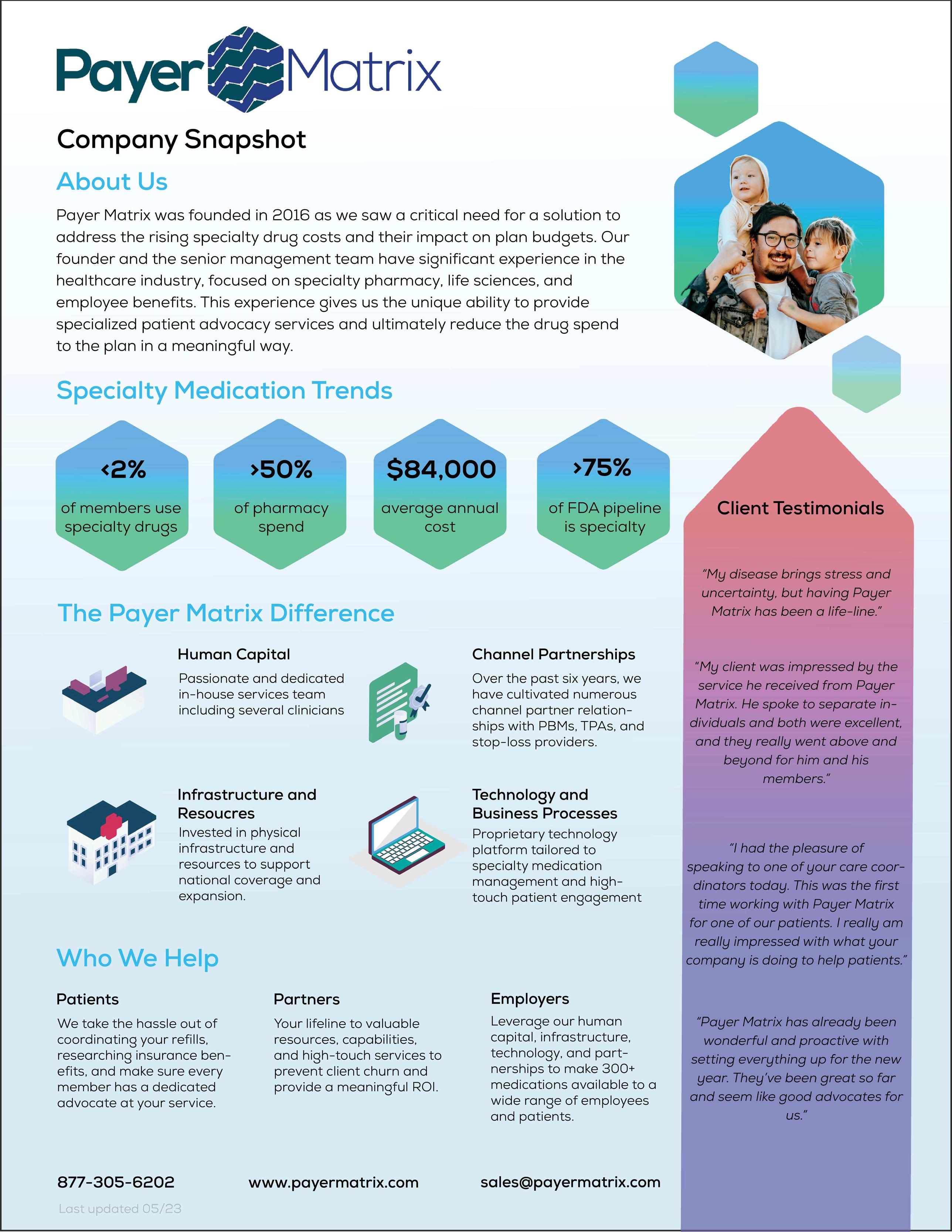
Payer Matrix 94
The Phia Group 120
– C –
Claim System Development/Management/Support
Availity 150
ClaimReturn, LLC 26
Coral 150
Javelina from Mphasis 74
Vālenz® Health 126
VBA 130
Viveka Health 151
Cost Containment/Large Claims/ Catastrophic Claims Management
6 Degrees 6
Advanced Medical Pricing Solutions (AMPS) 8
aequum, LLC 150
CareGuide Advocates 16
ClaimDOC 24
Deerhold 38
EZaccessMD 44
Goodroot, Inc. 50
Health Payer Consortium 60
Homestead Smart Health Plans 66
Imagine360 70
MedWatch 82
Renalogic 102
Rocky Mountain Review 104
The Phia Group 120
Vālenz® Health 126
WellRithms 136
Zelis 148
– D –
Data Analytics
Cedar Gate Technologies 20
Claros Analytics 28
Gradient AI 52
Healthcare Bluebook 54
Planwatch 151
Vālenz® Health 126
VBA 130
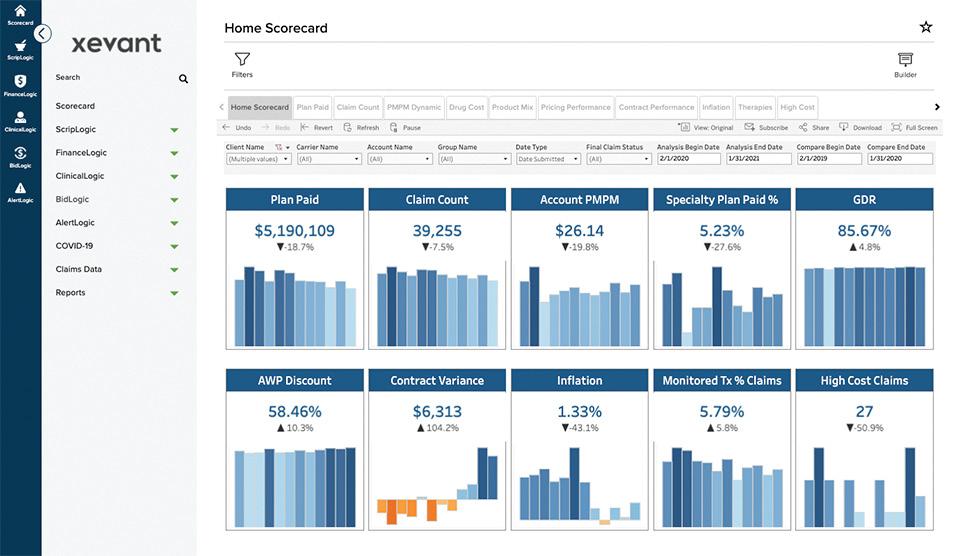
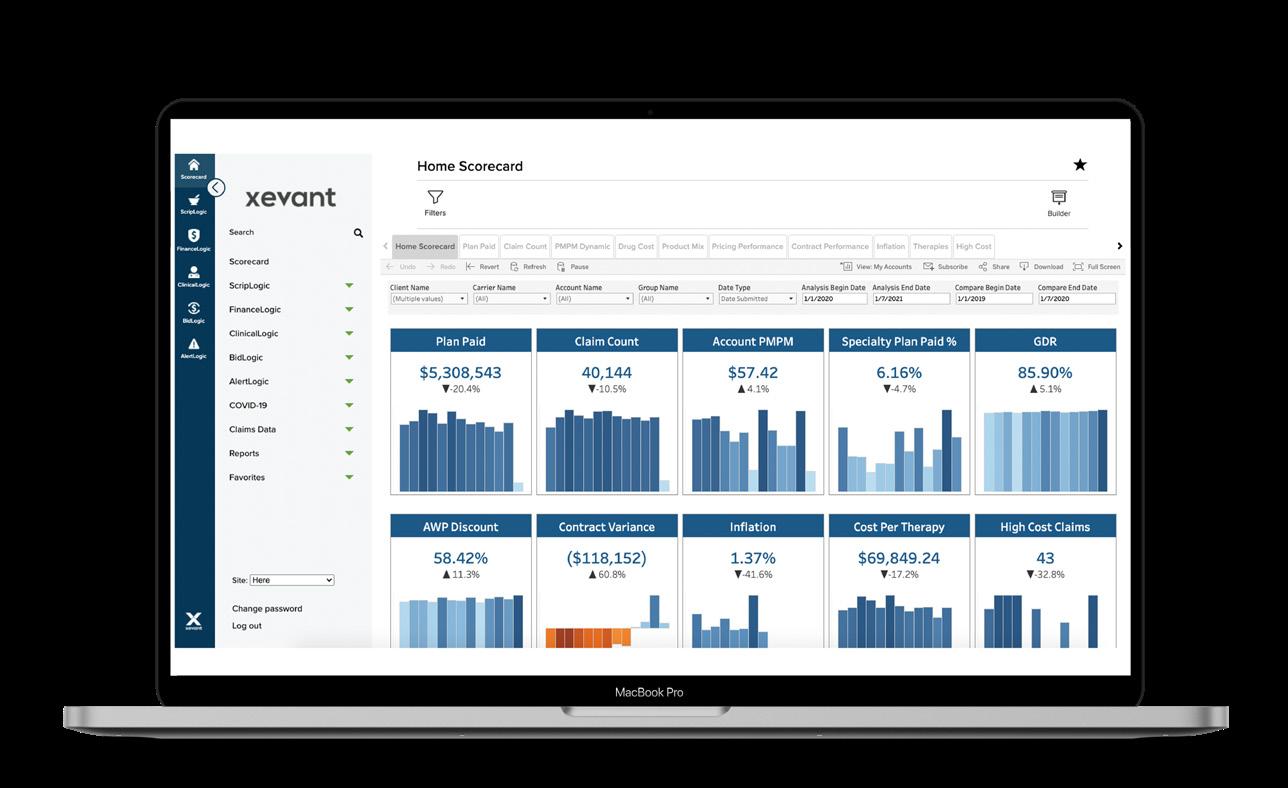
Xevant 144
zakipoint Health 146
– L –
Legal Counsel
aequum, LLC 150
– M –
Marketing Community Health 30
Ocozzio 90
Medical Management/UR/IRO/ Disease Management
Hines & Associates 151
MedWatch 82
Vālenz® Health 126
Welvie 138
– P –
Pharmacy (PBM/Consulting/Audit/Services)
AMWINS 14
Carelon RX 18
Comprehensive Healthcare Systems 32
CVS Health 34
Liviniti 78
OptumRx 92
Phoenix Benefits Management 96
Prescryptive Health 98
Prime/MRx 100
RxBenefits 106
Scripius PBM 108
ServeYou RX 110
TrueRx 122
WithMe Health 151
4 | HCAA Sponsorship Guide Fall 2023 Company Sponsorship Guide
Index
HCAA Sponsorship Guide Fall 2023 | 5 Company Sponsorship Guide Index Provider (Physician/Hospital/PHO) EZaccessMD 44 Imagine360 70 Walmart Health Virtual Care 134 – S –Software Development/Support Alaffia Health 10 Amino Health 12 Availity 150 Cervey 22 DataPath, Inc. 36 Deerhold 38 Denniston Data, Inc. 151 ECHO Health, Inc 40 First Dollar 46 Hi-Tech Health 64 Integrated Payor Solutions 72 Javelina from Mphasis 74 MDI NetworX 80 Medxoom 84 MPowered Health 86 Smart Data Solutions 114 TALON 118 VBA 130 WEX 140 WLT Software 142 zakipoint Health 146 Stop Loss Carriers/MGUs AccuRisk Solutions 150 Excess Reinsurance 42 Health in Tech 58 Homestead Smart Health Plans 66 Imagine360 70 Liberty Mutual Insurance Company 76 Swiss Re Corporate Solutions 116 US Benefits Insurance Services 124 Vālenz® Health 126 – T –Third Party Administrator Imagine360 70 Transparency Healthcare Bluebook 54 – W –Wellness/EAP/On-site Clinics/Telemedicine CVS Health 34 EZaccessMD 44 Healthee 56 MedWatch 82 Sharecare 112 Vālenz® Health 126 Vida Health 132


Ensure Fairness and Transparency in Healthcare We set healthcare free from constraints of traditional models and out-of-date billing practices. With our clinical expertise, industry experience, and proprietary evidencebased technology, we help solve some of the most complex issues in healthcare. Our solutions include everything from: Reference-based pricing Clean Claim Reviews/Payment Integrity Out-Of-Network Transplant & Specialty 503.640.9933 info@6DegreesHealth.com www.6DegreesHealth.com Contact:
HCAA Sponsorship Guide Fall 2023 | 7
Powering Healthcare
Cost Management Solutions

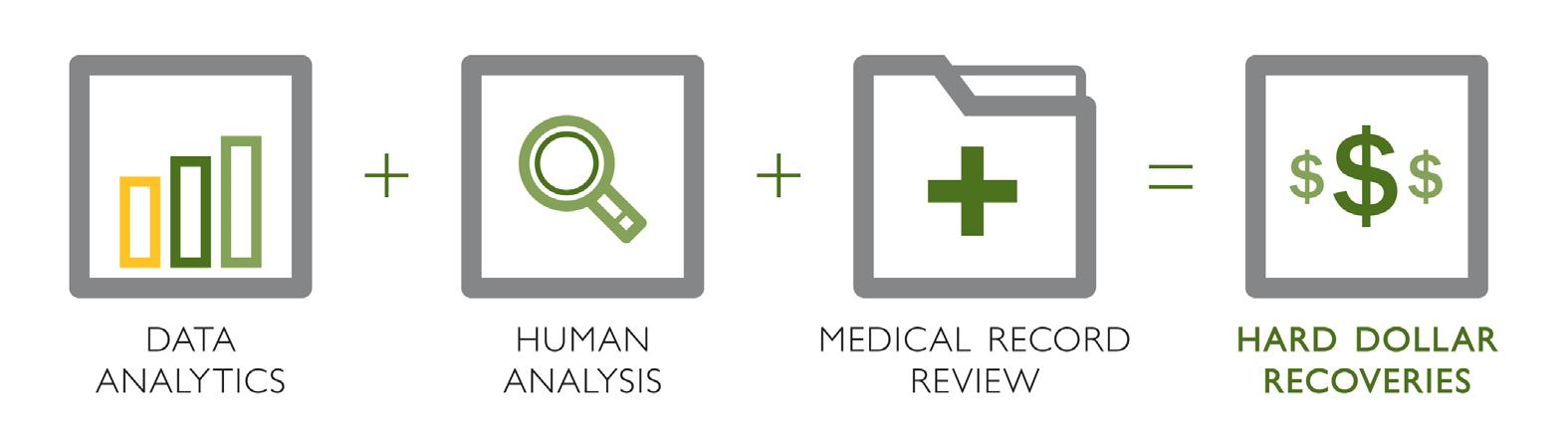
Cost Containment Experience Impacting Savings
16+ years of experience and historical reimbursement data resulting in transparent pricing that’s fair for all.
Physician-led Medical Bill Review Confirming Accurate and Reasonable Pricing
30-member physician panel reviews claims at the line item level, resulting in an average of 10% savings on hospital and facility claims.
On-demand Insight Delivering True Transparency
Next-generation portal and analytics platform providing visibility into claims flow, performance metrics, real-time trends, claim-level data, and more.
Care Navigation Team Connecting Members with Healthcare Options
Healthcare resources offering a variety of care options to optimize savings, schedule procedures, and check eligibility.
Enriched Member Experience
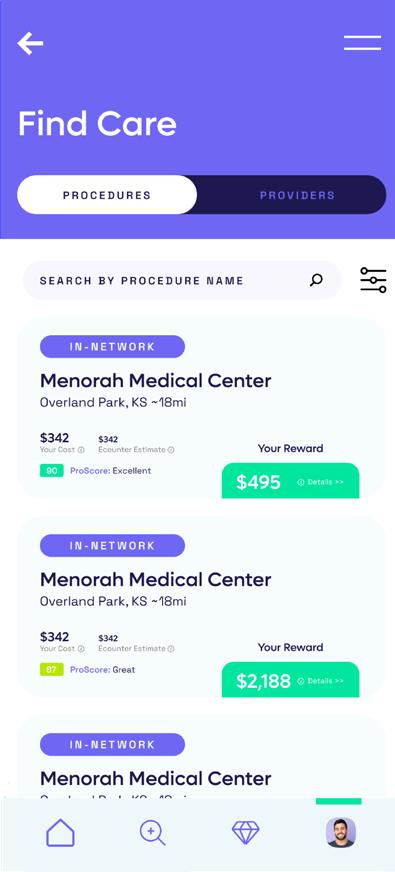
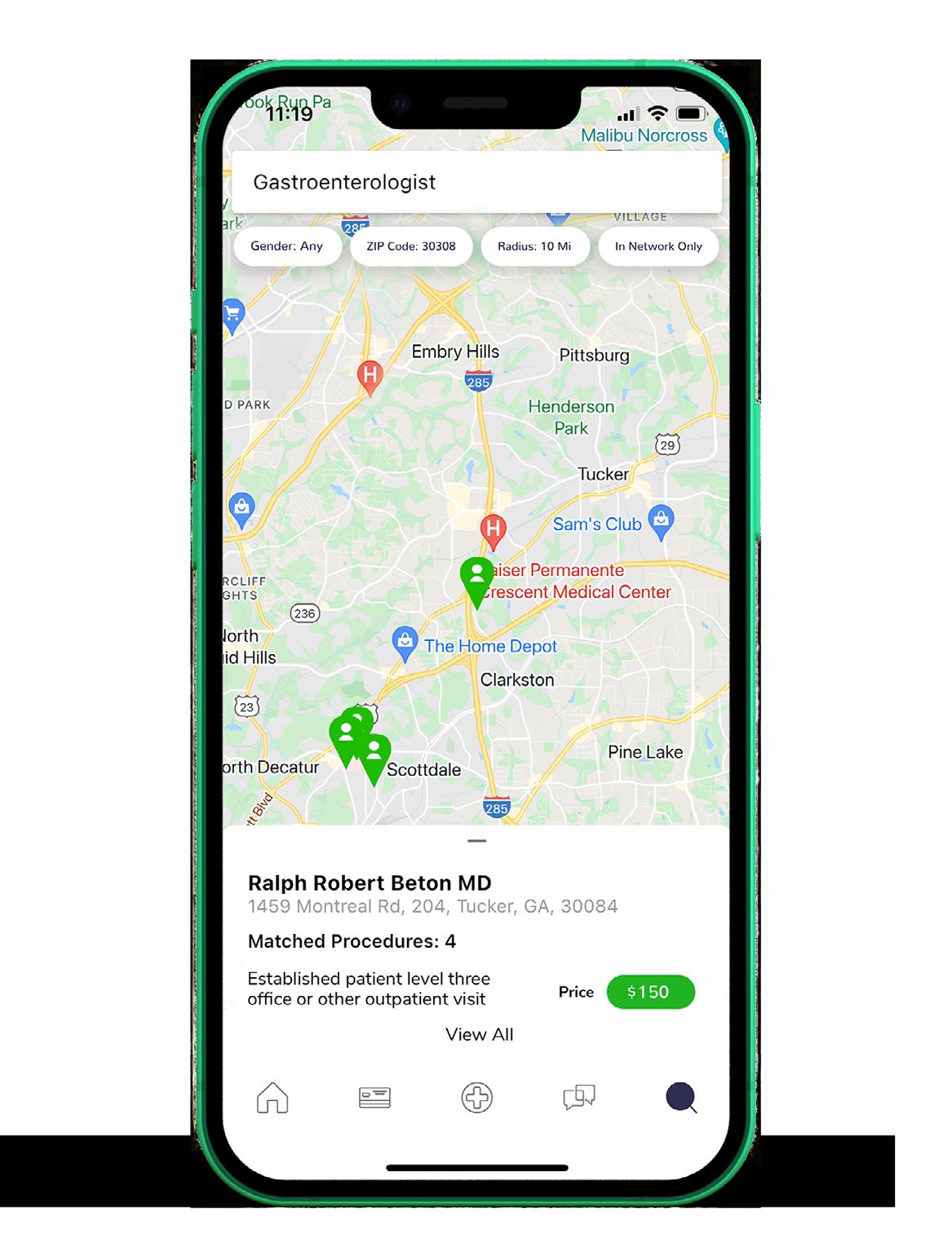
AMPS Connect Enabling Smarter Healthcare Decisions
Mobile application allowing members to compare providers, schedule procedures, submit balance bills, and communicate with the AMPS’ Member Advocacy team.
Rapid Response Reducing Member Abrasion Settlement early in the process once a balance bill is received, reducing member abrasion.
Enhanced Member Advocacy Providing Faster, More Frequent Communication
Accelerated contact with members by returning calls within 24 hours and more frequent communication throughout the process.
Additional Savings Opportunities
Pharmacy Solution Providing Honest Pricing and Better Benefits
A non-traditional PBM (Drexi) enabling savings with transparent pricing and pass-thru on prescription medications at more than 65,000 pharmacies.
Stop Loss Coverage Optimized for RBP Performance
Programs with some of the largest stop loss carriers in the industry, creating competitive pricing and tailored to AMPS’ RBP performance, historical data and enhanced analytics.
Centers of Excellence Improving Patient Care
Second opinion review allowing access to a high-quality network to address misdiagnosis, over utilization, sub-optimal treatment and overpricing.
2005
Year Founded
1+ BILLION Claims Managed Annually
600+
Number of Clients
Average Facility Savings 73%
Average Plan Savings Over PPO
146%
26% Average Medicare Reimbursement Rate
Make your healthcare dollars go further.
sales@amps.com www.amps.com
Advanced Medical Pricing Solutions (AMPS)
HCAA Sponsorship Guide Fall 2023 | 9
WHAT MAKES US DIFFERENT
WHO WE ARE
Alaffia Health is a healthtech company that uses machine learning and AI to eliminate fraud, waste, and abuse in medical claims We review claims on a pre-payment basis to proactively prevent overpayments We’re on a mission to eradicate improper payments so that providers and payers can focus on what matters most – providing the highest quality of care to patients at the best prices.



r e i m b u r s e d f a s t e r
O U R C L A I M
R E V I E W
P L A T F O R M
O u r c l a i m r e v i e w p l a t f o r m p r o v i d e s t r a n s p a r e n c y a n d r e a l - t i m e i n s i g h t s o n y o u r c l a i m s w e a r e r e v i e w i n g . S t a y i n f o r m e d t h r o u g h o u t t h e e n t i r e r e v i e w p r o c e s s b y v i e w i n g l i n e - b y - l i n e r e v i e w s i n f u l l d e t a i l a l o n g w i t h d e n i a l r a t i o n a l e V i e w a l l s u p p o r t i n g d o c s a n d c l a i m r e p o r t s d i g i t a l l y o n o u r p l a t f o r m .
A U T O M A T E D
B I L L R E V I E W S
T h e A l a f f i a p r o p r i e t a r y O C R s y s t e m c o n v e r t s m e s s y i t e m i z e d c h a r g e s a n d m e d i c a l r e c o r d s i n t o d i g i t i z e d f o r m a t s u s e d t o a u t o m a t i c a l l y r e v i e w i n d i v i d u a l l i n e c h a r g e s a n d c l i n i c a l d e t a i l s
C O N S U L T A T I V E
P R O V I D E R
C O M M U N I C A T I O N
A l a f f i a e d u c a t e s p r o v i d e r s o n b e s t b i l l i n g p r a c t i c e s t o r e d u c e f u t u r e m i s b i l l i n g .
A l a f f i a u t i l i z e s P r o v i d e r S i g n - O f f
A g r e e m e n t s t o c o n f i r m t h e f i d e l i t y o f e a c h r e v i e w f i n d i n g
I N D U S T R Y L E A D I N G
S A V I N G S
A l a f f i a d e l i v e r s a n a v e r a g e s a v i n g s o f 2 2 % a b o v e i n d u s t r y d i s c o u n t
Alaffia Health
A R T I F I C I A L I N T E L L I G E N C E T E C H N O L O G Y T h e A l a f f i a s y s t e m t r a c k s f r a u d , w a s t e , a n d a b u s e t r e n d s o v e r t i m e , g i v i n g y o u d e e p e r i n s i g h t s i n t o y o u r p r o v i d e r s ’ f u t u r e b i l l i n g b e h a v i o r A l a f f i a p r o c e s s e s c l a i m s a n d r e c o r d s 5 x f a s t e r t h a n p e e r s , a l l o w i n g p r o v i d e r s t o g e t
TO LEARN MORE CONTACT US AT SALES@ALAFFIAHEALTH.COM WWW.ALAFFIAHEALTH.COM

HCAA Sponsorship Guide Fall 2023 | 11
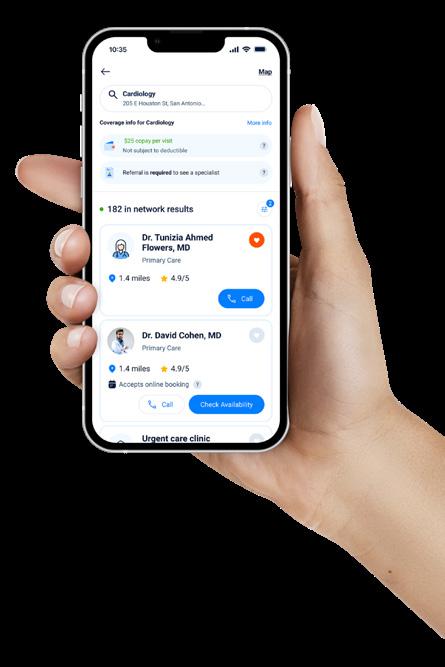
All-in-one digital healthcare navigation platform
Amino Health empowers plan members and care coordinators to make informed healthcare decisions through an intuitive, integrated platform experience.
Leverage innovation to win and retain customers
Delight members with a digital navigation solution that supports nearly any network, plan design, or point-solution you or your customer can imagine
Engage members for better outcomes
Plan sponsors with Amino guide members to top providers at 3x the rate of populations who rely on traditional provider directories, while also maintaining a 35% engagement rate across members.
Make compliance a strategic advantage
Amino is on the forefront of supporting plan sponsors in meeting Transparency in Coverage requirements - all within a consumer-friendly navigation experience.
Add functionality without sacrificing margin
Upselling premium features offsets the investment in new or improved core functionality.
Amino Health
www amino com
"Amino has been a great partner every step of the way and our customers love them!" Amino Partner

HCAA Sponsorship Guide Fall 2023 | 13
Pharmacy Benefit Manager
Individual attention and solutions for every group.
The Pain Points...
We understand the pain points for both you and your employees.
Employer
Our healthcare expenses are going up, how do we control costs?
How do I stay profitable and offer comprehensive healthcare coverage?
How do I decrease our administrative burden, while still assisting employees with navigating the complexities of their benefits?

Employees
I can’t afford my deductible; what are my options?
My drug is no longer covered; what am I supposed to do?
I am retiring and am bombarded with commercials, literature, and opinions who do I trust?
The Solution.
PBM
Independent PBM that makes clinically based decisions delivering lowest net costs for the members and groups

Guiding members in making informed decisions about their prescriptions
Retiree RxCare
Medicare education and support for members and groups
Patient Assistance
Proactive, member level advocacy, seeking lower drug costs for the member and group


Medical Drug Strategy
An innovative approach to saving members and groups money through managing medical drug spend
AMWINS
Amwins Group Benefits, LLC. 50 Whitecap Dr. | North Kingstown, RI 02852 amwins.com
A consultative PBM
We provide customized services that maximize clinical outcomes, member satisfaction, and cost effectiveness. 01.23
HCAA Sponsorship Guide Fall 2023 | 15

HCAA Sponsorship Guide Fall 2023 | 17

Carelon RX A way that combines new perspectives and deep expertise — creating value through cost savings and better health outcomes. When we put people first, everyone benefits. Services provided by CarelonRx, Inc. CarelonRx is redefining the right way to deliver pharmacy benefits carelonrx.com

HCAA Sponsorship Guide Fall 2023 | 19
Visual, Sharable Benefits Analytics
Cedar Gate Healthcare Benefits Analytics is an employee benefits analytics and reporting application for self-funded employers, their payers, and their broker/consultant advisory partners seeking to meet the plan sponsor’s clinical and financial performance goals. It enables benefits managers to tailor plan parameters and model performance based on the characteristics of the member population. Visual dashboards distill the data into prescribed actions, preventing clients from getting lost in the analysis. Focused reports track the efficacy and impact of care management activities and point solutions by monitoring performance indicators in member cohorts. Unlike the competition, the Healthcare Benefits Analytics tool is built for self-service plan design and reporting, reducing or eliminating the need for additional consultants or vendors. It pulls data from a common data lake that is shared by Cedar Gate’s Care Management application, ensuring the accurate translation of data to insights, and insights to action. The application is cloud-based and built on a next-generation NoSQL database for rapid interpretation of unstructured data. It enriches member data to identify savings recommendations and generates visual dashboards that communicate insights and key points to all stakeholders.
COST, QUALITY, TRENDS, & COMPARISONS
Monitor performance indicators and correct undesirable trends.
COHORT IDENTIFICATION

Conduct population risk stratification to identify specific cohorts that need to be monitored and reported on.
PRE - CONFIGURED DASHBOARDS & REPORTS
Render stunning visuals with over 100 out-of-the-box clinical and financial reports and dashboards that communicate key facts to an array of stakeholders.
MEMBER, PLAN & BENEFITS BENCHMARKING
MEMBER DATA ENRICHMENT
Augment member data with over 5,000 types of data enrichment.
DIY DASHBOARD & REPORT CREATION
Create custom reports and visualizations on the fly with an easy-to-use tool designed for the non-technical user.
PLAN & BENEFITS MODELING
Test changes to plan elements based on the member population profile to generate recommendations that will have the greatest clinical and financial impact.
Compare real-time performance against Cedar Gate’s proprietary commercial benchmark dataset of over 11 million members — by region, state, MSA and industry type.
Cedar Gate Technologies HEALTHCARE
CEDARGATE.COM | ©202 3 CEDAR GATE TECHNOLOGIES ® PROPRIETARY AND CONFIDE NTIAL INFORMATION. ALL RIGHTS RESERVED.
BENEFITS ANALYTICS
HCAA Sponsorship Guide Fall 2023 | 21
CLAIMS ADJUDICATION
What makes us different? Well...you do.
Cervey’s Adjudicator is a next-gen plan management and claims adjudication platform designed for you, with you. We offer a solution as unique as the needs of your clients, empowering you to provide nimble support in an ever-changing industry.
We listen. You leverage.
From customized pricing based on NADAC, AWP, WAC, MAC, ACQ to rulesdriven engines, Cervey’s Adjudicator provides the innovative flexibility you’ve been waiting for. We’re not just software. We are your partner in building a solution to help you maximize your strategy.
Claims adjudication doesn’t come in one size fits all... and neither should your software.
• Infinite Flexibility: Never out of the box. Our team of in-house developers offer endless benefit configurations designed to meet your unique needs.
• Comprehensive Expertise: With two decades of experience in claims adjudication, 340B, specialty and patient assistance, let Cervey’s seasoned team tailor your total solution.
• Unmatched Service: When you need support, you need an expert. You call we answer. No outsourcing. No robots. It’s as simple as that.

• No Competing Interests: Cervey is a privately held company, independent from any PBM ownership. Your success is our success. No question.
• Industry Readiness: Cervey’s flexible model allows us to quickly adapt to any future industry changes and requirements, including NCPDP F6 and beyond.
• Interoperability: Our extensive API framework simplifies the data integration with your internal processes and external business partners.
Cervey
HCAA Sponsorship Guide Fall 2023 | 23
Key Differentiators
Pave the Way®
Pave the Way® is ClaimDOC’s trademarked proactive healthcare provider outreach program, which begins up to 60 days prior to the effective date. Our Member Advocates create a one-on-one relationship with each member to help them navigate their new plan. As part of the onboarding process, our implementation team explains the reimbursement method and claims submission process to each provider to ensure a smooth transition between plans. On average, 90% of providers contacted through Pave the Way® accept our fair payment solution.
Pave the Way® is the most differentiating aspect of ClaimDOC’s reference based pricing plan (RBP). There’s nothing like it on the market today.
True, Fiduciary Protection
90% average provider participation
ClaimDOC bears costs for risk management for the plan as well as for member legal disputes related to RBP services.
FREE Physician Claims Processing
Unique to ClaimDOC, all provider/HCFA claims under $2,000 are repriced and defended at no cost to encourage and support complete network replacement.
Detailed, Line-by-Line Audits
Our proprietary claims management and audit system is custom engineered to allow for detailed line-by-line audits. Our in-house audit team is comprised of healthcare experts who conduct “eyes on” reviews of all UB-04 facility claims, ensuring maximum savings. Many RBP programs only review balance bills and appealed claims.
No Outsourcing
At ClaimDOC, we do everything in-house, including implementation, provider relations, balance bill support, clinical auditing, legal management, and member advocacy. Our highly responsive Member Advocates guide clients through our program to ensure a smooth experience for all.

ClaimDOC
ClaimDOC, LLC | 3200 Westown Pkwy, West Des Moines, IA 50266 | 888-330-7295 | claim-doc.com
1
2 3 4 5
Pave the Way® with ClaimDOC
HCAA Sponsorship Guide Fall 2023 | 25
If you are a healthcare claims payer…
You are almost certainly a healthcare claims over-payer.
ClaimReturn can help fix that…at no cost to you.

The ClaimReturn Solution
ClaimReturn’s proprietary artificial intelligence platform reviews and analyzes your claims in a matter of minutes, sending up flags that our team inspects individually. Then we get fast to work on recovery. Our exclusive reporting system lets you follow our progress every step of the way. And ClaimReturn’s exhaustive analytics makes it easier to recognize future overpayments, making our recovery process both retroactive and proactive.
ClaimReturn Offerings
Post-Pay: After the claim is paid, we identify billing anomalies on a technical component and coding basis review across hundreds of logic statements within our rulesbased engine. We then recover those overpayments and return them to you.

Our Promises
COB: We identify claims whereby the plan paid, but Medicare should have in fact been the primary payer. We correct the payment ledger with Medicare as the payer and return the amounts you paid back to you.
To-Pay: After claim adjudication but before the bill has been paid, ClaimReturn provides a “final check” and makes payment recommendations preventing overpayment before any funds are sent to providers.
ClaimReturn’s collaborative approach to recovery is professional and respectful. We will never damage your provider relationships, your contracts or your own brand in the name of recovery.
We are not a collection service; we are a correction service.
We also promise full transparency in our process and analytics. We believe that the more you know, the more confident you’ll be in our work and proprietary systems.

Inaccurate claim payments are flying everywhere. We catch them.
Michael Loprieno Director of Analytics
claimreturn.com
858-324-5345 630-947-5346 michael@claimreturn.com
HCAA Sponsorship Guide Fall 2023 | 27
Our next generation rating manual, Actuarial Advisor, allows you to swiftly price plans for groups of any size with or without historical claims experience while accounting for customizations such as reference-based pricing. Trained on billions of dollars in claims data, Actuarial Advisor is the most accurate rating manual on the market.

Claros Analytics Tired of pricing plans inefficiently? Scan to learn more about our premier software solutions Now with web-based functionality. Schedule a demo today! sales@clarosanalytics.com 609.275.6550 clarosanalytics.com Your Enhanced Capabilities ( Quickly determine how changes to a plan design will impact the final cost ( Quantify risk for prospects considering self-funding ( Forecast plan enrollment and budget rates ( Calculate claims reserves in seconds
Instantly incorporate changes and
highly
using our suite of
software. Trusted
the richest national
products
to
and beat
in
RIGHT
Claros.
produce
accurate projections
predictive analytics
by actuaries and trained on
claims data set, our
allow you
save time, cut costs
competing firms. STEER your clients
the
DIRECTION with
HCAA Sponsorship Guide Fall 2023 | 29
PUBLISH YOUR OWN HEALTH AND WELLNESS MAGAZINE!
PUBLISH YOUR OWN
HEALTH AND WELLNESS MAGAZINE!
Want healthier employees?
Want healthier employees?
Need to lower the cost of benefits?
Need to lower the cost of benefits?
Community Health offers a full suite of customized services, magazines, websites, apps, and more. Improving engagement, controlling cost, and reducing administrative burden.
get real results!
Community Magazine Group creates custom health and wellness magazines for some of the largest employers in Western New York and Western Pennsylvania. We offer a full suite of print and digital publications, along with wellness survey and engagement tools.
GET REAL RESULTS!
In Western New York and Southwestern Pennsylvania, Community Health wellness engagement has led to:
In Western New York and Southwestern Pennsylvania, Community Magazine Group wellness engagement has led to


• Quadrupling of participation in employee wellness programs
• Quadrupling of participation in employee wellness programs

• Reduction in annualized cost increases from 13% to 3%
• Reduction in annualized cost increases from 13% to 3%
Learn how your organization can take control of employee wellness. Contact publisher MARK HORNUNG at (773) 573-9794 and mhornung@cmgms.com.
Learn how your organization can take control of employee wellness. Contact publisher MARK HORNUNG at (773) 573-9794 and mhornung@cmgms.com.
Community Health
HCAA Sponsorship Guide Fall 2023 | 31
[ 01 ] User-Friendly System

We make managing benefits a breeze with customizable dashboards and reporting so that you can see what you need to see in the way you want to see it.

[ 02 ] Secure & Compliant
Multi-factor authentication, full HIPAA compliance, SOC 2, and HITRUST certification provide the highest levels of security to provide you and your organization with peace of mind.

Leveraging our Novus 360 solutions platform, we’ve developed the only fully integrated benefits admin solution that digitizes how you administer your benefits. As a result, your organization can control costs while making it easier for your members to access and understand their healthcare.
[ 03 ] Quick Implementation
Time is money. Go live with Novus 360 solutions in as quick as 3 weeks to 6 months.
[ 04 ] Dedicated Support
We believe that client implementation is a collaborative effort. Your dedicated account manager will be there for you every step of the way.
Comprehensive Healthcare Systems
need
All in one
Say hello to Comprehensive. Comprehensive Healthcare Systems is
All the bene fits management solutions you
.
place.
modernizing benefit program management. Our innovative software and services platform lets your organization streamline your program’s needs easily and efficiently.
The Difference
Looking for a better way to benefit? See all the ways Comprehensive can benefit your organization at comphealthcare.com
“It’s a great pleasure working with Comprehensive to enhance our business growth, reduce administrative expenses, and ensure HIPAA compliance. We interacted with your team, who worked beyond our expectations. We look forward to working with Comprehensive on future projects”
The better way to benefit
Fund Manager Teamsters

HCAA Sponsorship Guide Fall 2023 | 33

CVS Health Choose CVS Health® to help you successfully control costs and connect your members with convenient, quality care. ©2023 CVS Health and/or one of its a�liates. 011223 Contact CVS Health today to learn more about how we can help. cvshealth.com Lowering your costs with effective management strategies that are based on your goals. Engaging your members with personalized, omnichannel outreach that helps support healthier outcomes. Investing in innovative new technologies to deliver intelligence-driven insights that put you in the driver’s seat.
your needs with recommendations, solutions and support from seasoned account teams.
Meeting
HCAA Sponsorship Guide Fall 2023 | 35
Get where you want to grow with DataPath solutions as your travel partner.
Technology? DataPath has the proven all-in-one cloud platform for comprehensive administration of CDH Accounts, HSAs and Investments, COBRA, Billing, and Well-Being benefits.
Productivity? Our extensive business process outsourcing (BPO) services provide the service expansion, staff supplementation, and cost savings you’re looking for.
Education and Marketing? DataPath offers the industry-experienced, award-winning marketing services that you won’t find anywhere else.
Where do you want to grow? Let’s start the journey. Contact DataPath today.
dpath.com/tpa-grow

DataPath, Inc.
HCAA Sponsorship Guide Fall 2023 | 37



Deerhold Deerhold MRF Insights Deerhold Ltd., Boston www.deerhold.com smacewen@deerhold.com WE’D LOVE TO HEAR FROM YOU!

HCAA Sponsorship Guide Fall 2023 | 39
The ECHO Advantage
Enjoy the simplicity of a single payment solution:
Convert costly check payments to a fully digital platform
Eliminate the pain, risk and time involved in the 1099 process
Offer customized, consolidated family EOBs

Avoid fees for setup and implementation
Save time and money with a fl exible digital payments solution.
Health plans leverage our 25 years of experience to solve complex payment requirements.
Expect more. More efficiency. More choice. More savings.
Flexible solution
ECHO is a comprehensive solution, not a one-size-fits-all approach. Our end-to-end solution is tailored to fit your needs for vendors, commissions, and member payments.


Network scale
With 1.6M + unique provider and vendor connections, we have the largest payment network, allowing increased digital adoption rates and fast, painless payment processing.
Seamless integration
Implementation and workflow designs are built around unique needs for seamless integration, with minimal time commitment for IT teams.
Compliance expertise
We’re compliance experts, processing HIPAA, HITRUST, OFAC, and IRS 1099 compliant transactions, for your peace of mind.
Tested credibility
We are trusted to process $110B+ in payments every year, we can help with your payment challenges, too.
echohealthinc.com

Electronic payment modalities:
Included services:
• Print and postage
• Bank fees
• Admin console
• Digital check
• Digital wallet
• Virtual card
• All payer ACH
• EFT fraud protection
• 1099 processing for all payments
• Provider portal
• Member ID cards
• Member EOBs
ECHO Health, Inc
©2023 ECHO Health Inc. All rights reserved. The ECHO logo is a registered mark of ECHO Health Inc., and may be registered in the United States or other countries. Form No: SB20005042023
HCAA Sponsorship Guide Fall 2023 | 41
Reimagine the Stop Loss Experience With Excess Reinsurance
The cost of providing healthcare benefits to employees presents challenges for many organizations. Excess Reinsurance is here to help clients navigate this complex and ever-changing landscape. The exceptional attention and care we provide clients include an unwavering commitment to understanding the changes related to regulations, best practices, and industry trends.
At Excess Reinsurance we pride ourselves on creating lasting relationships with our clients while delivering custom and flexible solutions based on their needs. Whether you’re looking for a traditional product, a shared risk arrangement, or a unique solution, our team has the skills and knowledge to develop a curated solution to help you accomplish your goals.
We pride ourselves on developing unique solutions while remaining true to our core principles:
• Integrity
• Stability
• Innovation
• Quality Service
Provides a simplified, level-funded solution with integrated aggregate accommodation

Ensures employers are satisfying the ACA’s employer mandate by providing affordable solutions
Provides integrated stop-loss coverage and legal defense protection for self-funded RBP plans
Transparent Risk Strategies
Delivers the advantages of being in a captive without the complexity, collateralization, downside risk, and excessive fees typically present in traditional captives
Provides alternative funding solutions for self-funded plans and members by sourcing specialty medications at no cost
Manages your risk with maximum protection against high-value claims by providing custom specific and aggregate stop loss solutions
Excess Reinsurance
excessre.com
Powered by Excess Reinsurance
XS RE EXCESS REINSURANCE
XS
RE EXCESS REINSURANCE
HCAA Sponsorship Guide Fall 2023 | 43




















EZaccessMD www.EZaccessMD.com | 855-313-8145 | © 2023 EZaccessMD. All Rights Reserved. EZaccessMD completes telemedicine with a house call. When the doctor needs diagnostics, we arrive at your door in a few hours. From X-rays to lab tests, our services are immediate and free to the employee. House Calls are Back! Mobile Testing 24/7/365 On-Demand EZaccessMD: We Come to You Diagnostics EZaccessMD Traditional Telemedicine X-ray, Ultrasound, EKG Strep, Flu, UTI Echocardiogram Ear and Throat Exams Range of Motion Prescriptions Phone/Video Consult

HCAA Sponsorship Guide Fall 2023 | 45
The health wallet for modern benefit providers

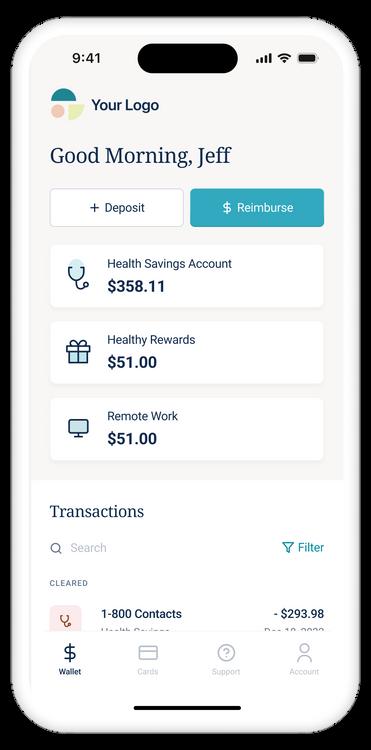

Our Health Wallet platform gives you the infrastructure to launch taxadvantaged accounts, supplemental benefits, or whatever you dream up.
Individual Benefits
HSAs, Health Rewards
Employer Benefits
FSAs, HRAs, LSAs, Commuter
Build a better member experience
Made for your platform
Get to market in record time with our turn-key solution, own your data, and fully embed the experience into your member portal over time with APIs and Widgets (SDKs)

Built for your administrators
We help your team do what they do best. Our admin tools give you control over the customer experience and the power to resolve issues fast and independently
Designed for humans
Members love to use our health wallet our utilization rates are double the industry average And with intuitive design and an accessibility score of 97, it’s easy to see why
+36% Utilization
Supplemental Benefits
OTC, Dental/Vision, Diet
First Dollar
Increase 72 Member NPS 92
CSAT
Member
HCAA Sponsorship Guide Fall 2023 | 47
31 years of dedicated healthcare investing in the middle market
Deep healthcare domain expertise with extensive industry network developed over decades of experience

• 42 platform investments made
• Over 130 add-on acquisitions completed
Successful track record of building category-defining and rapidly growing healthcare companies
Thesis-driven investing with an Executive-inResidence model
Control transactions in profitable and growth-oriented healthcare services companies
Dedicated Center of Excellence team with functional experts driving value-creation initiatives
Current Investment Portfolio
Tech-enabled Revenue Integrity and CDI services for hospitals and health systems
Global pharma CDMO specialized in OSD and manufacturing technology


Real-time data and insights provider to healthcare & life sciences




ABA autism therapy provider
Orthopedic physician practice management
Enterprise pharmacy solutions to hospitals / systems


Cold chain shipping solutions for pharmaceutical & life sciences companies
Mental health solutions provider for K-12 students

Tech-enabled revenue cycle management solutions
Multi-capability med device contract manufacturer
Generic pharmaceutical repackaging and distribution services
FDA 503B-registered compounding pharmacy

In-home and mobile clinic health assessments provider
Manufacturer of anesthesia and respiratory medical products



Dermatology practice management

Frazier Healthcare Partners Two Union Square, 601 Union Street, Suite 3200, Seattle, WA 98101 | (206) 621-7200 www.frazierhealthcare.com
$10 - 75M Entry EBITDA $7.0B Fund Capital Raised $1.5B Frazier Growth Buyout Fund X

HCAA Sponsorship Guide Fall 2023 | 49
The healthcare solutions you and your clients have been waiting for
Supercharge your offerings—and growth— with benefit savings employers will love
As fiduciary advisors, trusted guides and strategic thinkers, you play a key role in helping employers design and administer high-impact benefit plans that their employees, and bottom line, will appreciate. But pharmacy costs are often overlooked, meanwhile, 72% of employers rank them as a top concern.
TPA Solutions
Prenegotiated Pharmacy Benefits
Our network of highly discounted PBM contracts, enhanced with specialty solutions, clinical outreach, international filling and integrated cash solutions, unlocks more choice, leverage and on average 30% savings for groups of all sizes.

Pharmacy Benefit Consulting
Bring your clients best-in-class pharmacy benefit resources, clinical insights and savings through specialized Rx services, including trend management and market support, that deliver the lowest possible pharmacy costs year after year.
CareCost Navigation
Differentiate your business by offering benefit navigation services that focus on cost reduction for the employee and employer without compromising quality.
Member Engagement App Suite
Ditch those disconnected systems. Our streamlined benefits app and cloud-based admin console empower plan administrators to lower costs through AI driven pharmacy and medical savings suggestions, integrated virtual care, care navigation and a multi-service messaging console. Connect members with the right benefits at the right time – all through one app!
helping TPAs grow their business and expand their
portfolio.


TPA
Let’s Reinvent Healthcare, Together
help employers save significantly on
Learn more at goodrootinc.com
We
healthcare, while
product
HCAA Sponsorship Guide Fall 2023 | 51


HCAA Sponsorship Guide Fall 2023 | 53
When Congress needed to understand healthcare transparency to create the landmark No Surprises Act legislation, there’s a reason Bluebook was the only transparency company asked to testify before the Senate. We were one of the first to introduce “transparency” to the healthcare market nearly 20 years ago.
Founded on the belief that everyone should have access to the true quality and cost of healthcare, Healthcare Bluebook is the most experienced and trusted expert in healthcare pricing, quality, and consumer behavior today.

Out of the gate, our core cost navigation solution met many of the initial transparency requirements.
Bluebook’s compliance solution is 100% Compliant with TiC and NSA rules and includes:

24,000
Allowing us to serve:
Bluebook Comply Base navigation supports all current requirements, including the expanded list of surgical procedures required as of 1/1/24. Additionally, we will support all future legislative requirements if/when they become officially mandated, such as Rx and Advanced EOB functionality.
• MRF Data + Historical Claims Data
• Consumer-Friendly Terms (CFTs) for all 500 currently mandated services
• Total cost illustrations based on entire episode of care
Comply Base Standard Features
• Industry’s Most Intuitive UI/UX
• Dual-Level Reporting (TPA vs. Employer)
• Qualified Payment Amounts (QPA)
• White-Labeling / Co-Branding Capabilities
Comply Premium Upgrades
• Quality Metrics
• Member Engagement and Incentives
• Plan Design Integration
• Bluebook CareConnect™ Concierge Support



• Bluebook Rx™ Pharmacy Cost Navigation



Learn how our Medical + Rx cost and quality navigation solutions can use compliance to create meaningful, hard-dollar savings for your employers and their employees. Contact TPASupport@healthcarebluebook.com to schedule a demo.

Healthcare Bluebook
586 18,000 Hosted Machine Readable Files Available Unique Provider Networks Total Searchable Medical Procedures
50+ TPA & Health Plan Partners 25k+ Affiliated Employer Groups 4M+ Supported Members
Base Navigation Premium Navigation
© 2023 Healthcare Bluebook All Rights Reserved LIT 10338
HCAA Sponsorship Guide Fall 2023 | 55
Cut healthcare costs instantly with one seamless, unified benefits platform
Make health benefits more effortless and less costly for everyone involved with Healthee’s industry-leading AI-powered technology.
Reduce Care Costs
Steer employees towards cost-saving, informed decisions with a simplified benefits experience. Employees can save money on procedures with cost transparency tools, find top-quality in-network providers, and access free telehealth care.
Increase Benefits Engagement
Revamp how your company and your employees engage with benefits. Employees can discover all their available benefits and better understand their coverage, while your company can leverage engagement data to make strategic cost-saving decisions.
Results That Speak for Themselves
2X Benefits Engagement | National funds management company
-4% Claims Costs | Ecommerce marketing platform
-5% Health Insurance Costs | Food and beverage distributor
-14% Health Insurance Costs | Medical equipment company
Guy Benjamin Co-Founder and Co-CEO guy@healthee.co
Healthee
“Our employees are finally empowered to use their health benefits and price out healthcare spending. Healthee adds an important tool to our benefits arsenal.”
Gillian Maccarone, HR Administrative Manager, Nassau Financial Group
HCAA Sponsorship Guide Fall 2023 | 57
GET YOUR TIME BACK WITH THE FUTURE OF SELF-FUNDING.
Waiting to quote and underwrite a group often takes days, sometimes weeks. The process of traditional self-funding is complex and overly complicated for everyone involved, costing both time and money.
What if you could underwrite hundreds of groups a day?
It’s simple—just Power On with Health in Tech.
OUR SOLUTIONS—YOUR PROGRAM
At Health in Tech, our end-to-end solutions are designed to give you full autonomy, so you have the power to create whatever you want. We help you build your system, designed specifically for your needs and your market, so you can run with it.
BEST OF ALL!
You can go from WEEKS to MINUTES to quote and bind small to medium-sized groups. Produce a firm proposal that has 12 plans with 4 tier rates in only 2 minutes!
The industrys most advanced underwriting and quoting platform.
Creative risk-mitigating and stop-loss solutions.
Member benefit utilization and accessible, transparent data.
Accessible reference-based pricing networks.


POWER ON THE FUTURE OF SELF-FUNDING
Get started today and learn more about what Health in Tech can do for you.
QR CODE HERE HEALTHINTECH.COM

HCAA Sponsorship Guide Fall 2023 | 59





















































































































































































































































































































































































Health Payer Consortium EXPERT MEDICAL BILL REVIEW We find savings others miss. SPECIALTY NETWORK CONTRACTS RBP SOLUTIONS OUT OF NETWORK SERVICES We save you time & effort, improve patient outcomes & generate defensible savings. healthpayerconsortium.com 844-888-1HPC Client First, Always. +
HCAA Sponsorship Guide Fall 2023 | 61
Bringing the Power of Consumerism to Healthcare
A first-of-its-kind healthcare SuperApp for self-funded plan sponsors that helps members make better decisions around quality medical care delivery, so everyone wins.
The only self-funded healthcare engagement platform of its kind.
Hercules Health rewards habitual app utilization by giving cash incentives earned through intelligent healthcare shopping tied to quality and cost. More app use equals more savings for members and plan sponsors alike.


Comprehensive Compliance
Hercules Health delivers best-in-class price transparency that is fully compliant with the Transparency in Coverage (TiC) and the No Surprises Act (NSA) rules and regulations.
Hercules Health
Contact us today. info@herculeshealth.com herculeshealth.com

HCAA Sponsorship Guide Fall 2023 | 63


We’ll tailor your claims administration platform to meet your needs – no matter what they are. What else can our highly flexible, cloud-based software do for you? TPAs, Let’s Ease Your Workload Cut Costs Save Time Grow Your Business sales@hi-techhealth.com 908.813.3440 hi-techhealth.com
HCAA Sponsorship Guide Fall 2023 | 65
It’s about time you found out about

As the workloads of TPAs continue to grow and evolve, it’s about time you had some help.
Presenting Claim Watcher – a powerful and efficient costcontainment tool that addresses the growing challenges and expectations faced by TPAs and their clients.
Our solution works on a few different levels:
For our TPA partners, we seamlessly integrate into your workflows as we take a closer look at claims to correct any billing or coding issues.
For the clients you serve, we provide significant savings – typically 20-30% on their health benefits spend.
And for members, our premier concierge service is on hand to assist with provider appointments and any general questions. And, if a member receives a surprise balance bill, we’re there too – with full and free legal defense, and timely, proactive outreach to update the member so they feel supported while also being protected.
Reach out today to learn more about how Claim Watcher can benefit you, your clients, and their members.

Homestead Smart Health Plans
Seamless integration.
Client retention. Superior member experience.
claimwatcher.com | info@claimwatcher.com | 844.307.3788
HCAA Sponsorship Guide Fall 2023 | 67
Too many TPAs limit their own revenue, their value to their customers, and their ability to di erentiate their services by not taking advantage of innovation opportunities. Every employer client represents an opportunity to establish a special relationship between you and each employer by presenting opportunities for additional value, quality improvements, and cost savings that your competitors can not or are not doing.
Ikigai Growth Partners evaluates hundreds of early-stage firms, looking for the few hidden gems that add value to your relationships. Current hot deliverables include:
• Digital direct contracting, DPC networks, vendor management, and bundled services
• Surgical optimization; faster recovery with almost no opioid utilization
• Caregiver support services for employees supporting aging loved ones
• Musculoskeletal (MSK) true digital front door, allowing immediate access to care triage and virtual expert support
• Virtual group mental health therapy
Don’t limit your organization to only those standard services and o erings that mimic your competitors. Add value to your relationships through innovation.
Come explore with us.
Michael Brouthers Founder/Principal Ikigai Growth Partners mbrouthers@ikigaigrowthpartners.com
ikigaigrowthpartners.com
Ikigai Growth Partners
HCAA Sponsorship Guide Fall 2023 | 69

Help clients cut healthcare costs, weather inflation and improve hiring. Trust the difference an experienced RBP solution makes. 78 World Class NPS Score • 98% Member Satisfaction Guaranteed Cost Savings 15-30% SAVINGS Concierge member support SUPPORT Access to quality care QUALITY imagine360.com Your health plan can do better. We promise.
HCAA Sponsorship Guide Fall 2023 | 71
Cloud-Based Solutions That Are a TPA's Dream

Integrated Payor Solutions
Power your business and sort through adminstrative hassle easily with Encompass+. Sort through the chaos of the No Surprises Act with Transparency+, the most efficient and inexpensive solution to meet compliance. Go from Chaos to Clarity and Achieve Your Business Dreams Learn More and Request a Demo Today IntegratedPayorSolutions.com Compliant and Secure Scalable to Grow as You Grow Easy to Use Low Barrier to Entry Built for Growth No Strings Attached Ultra-Quick Compliance Inexpensive and Efficient Shawn Evans CEO Integrated Payor Solutions sevans@integratedpayorsolutions.com
Access the industry’s most powerful, flexible, secure platform and stand-alone transparency solution with Integrated Payor Solutions. Our cloud-based platforms are built on Salesforce making them simple to use and scalable to grow with you.
HCAA Sponsorship Guide Fall 2023 | 73






ENGINEERING CONNECTED EXPERIENCES FOR SMARTER, EFFICIENT PAYER ENGAGEMENT Provider Credentialing Automate & Reduce the enrollment and credentialing process by 40% EnrollEnrich.io Enrich member experiences while reducing enrollment efforts and errors by 30% Member/provider “super App” Redesign provider engagement with AI-enabled smart integrations AuthEnrich.io Transform experience across stakeholder spectrum with Pre authorization For more details, contact T J Ruesch Vice President, Healthcare Sales, Mphasis Javelina tj.ruesch@eldocomp.com 602.604.3100 javelina.mphasis.com



HCAA Sponsorship Guide Fall 2023 | 75
Liberty Mutual | Employer Stop Loss
Our mission is to be a leader in the excess loss industry through outstanding services, relationship building and innovative products.
We understand that relationships are one of the driving forces in our industry today. We are committed to meeting the special needs of our broker partners and, most importantly, our self-funded employers. Through every step of the way, we pay great attention to details and respond promptly to all different aspects of the industry.
Partner with Liberty Mutual, and you benefit from the financial strength, security, and capacity of a Fortune 100 carrier. Go beyond business as usual.
To learn more, please contact:
Karthik Mohan
Vice President, Sales & Distribution
Liberty Mutual Medical Stop Loss 860-408-7896
Karthik.Mohan@ironshore.com
Services offered:
Specific excess loss coverage
•Incurred and paid, run-in and run-out contracts
•Specific attachment points available from $20,000 (per state regulations) to $1,000,000
•Eligible groups down to 50 covered lives (Per state regulations)
•Aggregating specific deductibles available

• Coverage available in all states except WA
Aggregating excess loss coverage
•Incurred and paid, run-in and run-out contracts
•Monthly aggregate accommodation available
• Terminal liability option available
•Non-experience aggregates are available on existing full insured employers
In-house clinical team and ProAct Care Solutions
• The Liberty Mutual ProAct program engages select vendors that provide the leading expertise in catastrophic claim management and clinical consulting services. In many cases, fees for services are considered eligible expenses under the Stop Loss Policy for members that exceed the specific deductible.
• Provide access to our robust in-house clinical review team offering expert guidance to producer partners and informed risk assessments.
Liberty Mutual Insurance Company For mid / large markets This document provides a general description of this program and/or service. See your policy, service contract, or program documentation for actual terms and conditions. Insurance is underwritten by Liberty Mutual Insurance Company or its affiliates or subsidiaries. Some policies may be placed with a surplus lines insurer. Surplus lines insurers generally do not participate in state guaranty funds and coverage may only be obtained through duly licensed surplus lines brokers. © 2019 Liberty Mutual Insurance, 175 Berkeley Street, Boston, MA 02116. NI5067 06/20
HCAA Sponsorship Guide Fall 2023 | 77
Company Overview
The Liviniti Difference
Built on a foundation of full disclosure to our clients, we are a PBM that operates under a philosophy of complete transparency, trust and alignment. Working with Liviniti, clients can expect:
• Pass-through pricing that returns network discounts and rebates to clients
• Reduced drug spend with clinical programs that focus on lowest net cost
• Deeper savings through innovative drug procurement options
Overview of Services
• Exclusive focus on self-funded employer plans
• All-inclusive administrative fee for standard PBM services
• Deep clinical expertise – founded and led by pharmacists
• A live, US-based service team to handle member calls
• Flexibility and choice in plan design, pharmacy networks and formulary options
• Smart technology for a better service experience
• Rich history of innovation and PBM “firsts”
RxCompass
Our latest innovation, RxCompass, evaluates a range of drug procurement options to identify the lowest-cost source for high-cost brand and specialty medications. Owned by Liviniti, RxCompass is offered exclusively to Liviniti clients.
Our transparent model saves more than $23 per script.
Cut Costs. Keep...
Visibility
Know exactly what you’re paying for PBM services.
Value Flexibility
We always focus on selecting the most cost-effective drug.
Tailor your pharmacy benefits exactly how you want them.
We make it easy for your members to get answers and support.
Liviniti
Service
Contact Us: solutions@liviniti.com www.liviniti.com | www.myrxcompass.com Liviniti and RxCompass are service marks of Southern Scripts Holdings, LLC.

HCAA Sponsorship Guide Fall 2023 | 79
MDI NetworX
HCAA Sponsorship Guide Fall 2023 | 81
30+ Programs & Services > One Partner Solution


At MedWatch, our focus is to provide clients with solutions that effectively control medical costs and enhance the outcomes of care.
Our program options allow the plan to build a tailored and effective benefit offering that not only saves the plan and plan member money, but provides enhanced care options. By promoting the utilization of quality services that result in better outcomes, members are more likely to engage and use their benefits wisely.
Compassionately Built – Seamlessly Integrated
We’ve carefully constructed 30+ programs and services that fit together seamlessly to meet members where they are in their health journeys.
With 35+ years in the industry, MedWatch’s continued innovation and growth, proprietary technology, depth of staffing, experience, and expertise provides clients with the best solutions and partner available.

( Utilization Management
( Case Management & Specialty Case Management
( Chronic Condition Case Management
( Disease ManagementLiving Well with Chronic Conditions
( High-Cost Infusion/ Oncology Treatment Program
( Dialysis Claim Review & Pricing
( Telemedicine
( Employee Assistance Program


( And More

MedWatch
Urmedwatch.com | sales@urmedwatch.com | 321.249.9179 Full Spectrum Care Management
( Pathways Concierge Member & Provider Support
Uniquely customized to the need of each
“Because no one should have to walk their healthcare journey alone.”
ANNIVERSARY 35th
Sally-Ann Polson | President & CEO
ANNIVERSARY 35th
HCAA Sponsorship Guide Fall 2023 | 83
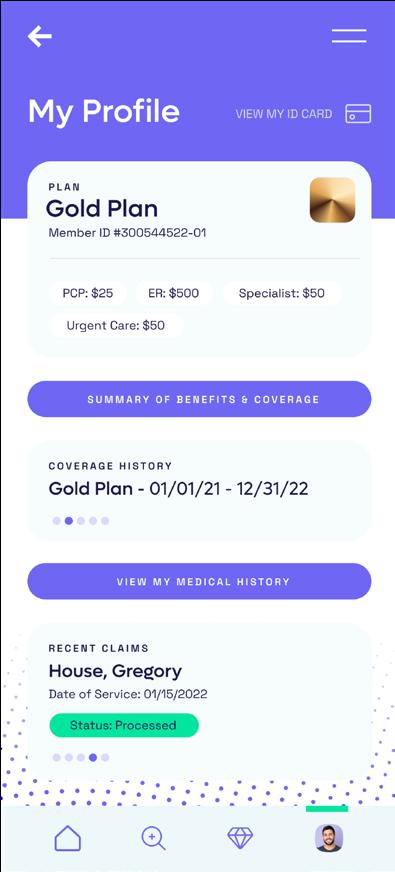
Optimize your healthcare benefits experience now
Are you a self-funded employer, TPA or broker looking for a better solution for today’s workforce?
Medxoom dramatically improves the healthcare benefits experience for your members By unifying all key components of your health benefits Medxoom helps match members with the best price vs quality provid driving greater member satisfaction and cost savings. Medxoom does th hard work of integrating all the disparate pieces of the benefits ecosyste into one member-optimized experience
The Problem
Healthcare coverage is too expensive. Employers are finding it
• 8% Y0Y increases in premiums
• 250% increase in deductibles
Medxoom
1 2 3 4 Medxoom Solution Pricing
Call or Click for Provider Cost & Quality • Procedure, Test & Bundle Price Comparisons • Clear Picture of Member Responsibility Communications
Group & Personalized Messaging
Concierge Savings & Appointment Alerts
Unified In-App, SMS & Email Messaging Identity • Digital ID Cards • Member Claim History • Coverage Details & Plan Docs Payments • Integrated Member Net Due • All-Digital Plan to Provider Payments • Payment Card & Financing Options Modern Member Experience Increased Engagement Cost Savings Tools Comparison Shopping Measurable Savings Save 10-30% + =
•
•
•
•
HCAA Sponsorship Guide Fall 2023 | 85

-
HCAA Sponsorship Guide Fall 2023 | 87
CLAIMWISE™ & CLAIM ACCOUNTABILITY
What is ClaimWise™?
Nokomis developed its own proprietary claim review technology, ClaimWise™, because we recognized the need to customize technology for health plans’ specific needs and relationships Powered by Oracle and SOC 2®-certified, we built ClaimWise™ from the ground up, which allows us to develop unique customizations
The power of ClaimWise™
Nokomis provides an independent review of all claims, regardless of dollar amount or provider type –– we’re experts at finding inaccuracies in claims that look “okay” at face value. When a claim is submitted to ClaimWise™, it’s passed through hundreds of custombuilt rules, millions of code edit combinations, and scores of reference tables –– which can all be customized by client. This process uses intelligent claim selection to identify claims that likely contain inaccuracies, which our team of expert coders, reviewers, and analysts will then further investigate and request records as needed
Capture an average of 9% in incremental savings with claim review that uses technology AND human experts
Our unique combination of ClaimWise™ technology and experienced certified coders find claim inaccuracies that others miss, regardless of dollar amount. We review all claims in one business day, before payment. We call this approach Claim Accountability
Low friction and low risk with less than 1% in appeals
We always do the heavy lifting wherever we can, customizing our rules and edits to adapt to our clients' specific needs and integrating with any existing systems already in place.
9%
1%
Nokomis
info@nokomishealth.com | nokomishealth.com | (612) 825-2342
100% of claims
record reviews Clinical & payment policies
edits, fraud, waste, and abuse
Accountability
Claim Accountability goes beyond Payment Integrity
Integrity
Review
Comprehensive
Code
Claim
Nokomis
Payment
HCAA Sponsorship Guide Fall 2023 | 89
Ocozzio
team of self-funded experts use industry knowledge and experience to identify opportunities, solve
and generate business. From marketing intelligence and strategy to messaging, execution and reporting,
is the marketing department you’ve always dreamed of but never thought you could afford.
A complete marketing team working for you. Ready to meet your marketing team? Connect with Ocozzio today. Zach Swenson | 706.922.1912 | zswenson@ocozzio.com
Ocozzio’s
problems
Ocozzio
WHAT YOU GET?
HCAA Sponsorship Guide Fall 2023 | 91

OptumRx Flexible solutions Dedicated support team TPA expertise With the right strategic partner, you can deliver care without compromise. optum.com/rx/tpas © 2022 Optum, Inc. ORX8978362_221216
HCAA Sponsorship Guide Fall 2023 | 93
HCAA Sponsorship Guide Fall 2023 | 95
A Collaborative Model
That Rises To Meet Your Needs
Phoenix is a modern pharmacy benefits management (PBM) company that provides brokers, TPAs, and self-funded organizations with scalable, individualized pharmacy plans that save money on prescription medications for both the plan and its members.

What Sets Us above the rest?
Open-Architecture Approach
Phoenix uses an “open-architecture” approach to plan design and management. This means you can choose the elements that work best for your needs, and nothing that you don’t. Plus, we’ll implement it in a seamless way that allows for limited member disruption.
Exclusive Pharmacy Network Contracts
We are completely independent and own 100% of our contracts, which means more flexible plan design options and better overall plan management whether you choose an Open, Preferred, or Limited Network.
Honest Rebate Opportunities
Our goal is to eliminate the questions—what drugs are included, when, and how much? With Phoenix, it’s simple: every rebatable drug, every time. Whatever arrangement best suits your needs, we’ll do rebates your way. And we pay out faster than the competition.
Customized, Comprehensive Pricing
Whether it’s a passthrough or a traditional model, Phoenix finds a way to meet your needs and save you money while offering strong plan benefits to members. We take a comprehensive approach to pricing, completely customizing a model that works for you.
Above & Beyond Customer Service
From Implementation to Account Management and Member Services, customer service excellence is integral to our culture. When you partner with Phoenix, you benefit from a relationship that grows your business.
Phoenix Benefits Management
Phoenix Makes Pharmacy Benefits Simple With: PBM Services for Self-Funded Plans 340B Services RxAdvantage Savings Card MyRxAdvocate Specialty Savings Program Magnolia Mail-Order Pharmacy
Informed Decisions. Better Outcomes. Reach out to us for your complimentary Plan Cost Analysis and discover opportunities to save on pharmacy costs. <sales@phoenixpbm.com> <888.532.3299> phoenixpbm.com Phoenix Pharmacy Benefits Management 410 Peachtree Parkway, Suite 4225 Cumming, GA 30041

HCAA Sponsorship Guide Fall 2023 | 97
Reinventing pharmacy benefits management
A better way to empower your employees & reduce costs
Many employers believe they need a traditional PBM to manage their pharmacy benefits. We exist to offer a choice, so you can manage your plan, your way.
Our new model delivers the clinical, operational and customer service you value from a PBM, plus we offer transparent pricing and a health intelligence platform that puts the focus back on what matters most: you and your members. We believe:
The system is fundamentally broken and the solution must empower patients with transparency, choice and control.
A better pharmacy experience begins in the prescriber’s office – and a prescription is the natural gateway to the care cycle.
The pharmacy ecosystem needs to be rewritten so that incentives are aligned with better financial outcomes for pharmacies and better health outcomes for patients.
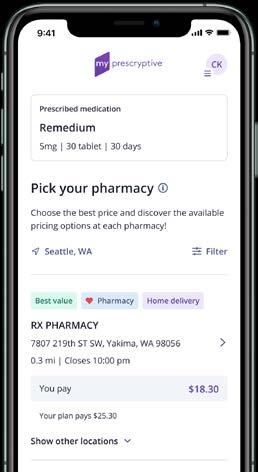
What’s different about Prescryptive Benefits?
TRANSFORMATIVE PRICING MODEL
The best partnerships are built on trust. We offer fully transparent pricing, 100% pass-through of rebates, and no hidden fees.
HEALTH INTELLIGENCE PLATFORM
Our secure, HIPAA-compliant platform connects benefit plan information, the patient, and the provider, all at the point of care, enabling better, more informed health decisions.

GUARANTEES AND ACCOUNTABILITY
We act in the best interest of our clients and their members by serving as a named fiduciary for the client’s benefit plan in the areas of formulary management, pharmacy network contracting and management, rebate contracting and payment administration, and adjudicating charges to the benefit plan. We put our fees at risk to hit aggressive financial guarantees for our clients.
76%
of unidentified or unfamiliar calls go unanswered.1 Meanwhile, 90% of text messages are read within three minutes.2
81%
of consumers want shopping for healthcare to be as easy as shopping for other services.3
As consumers shoulder more and more of the healthcare costs, the ability to shop will become imperative.
Prescryptive Benefits lowers the cost of drugs by eliminating the middlemen from the drug market and enabling consumers to take charge of their health.
Prescryptive Health
prescryptive.com
Unstoppable trends and behaviors that demand a better experience
1 BGR | 2 Tatango | 3 Harris Poll Consumer Experience Index, 13 July 2020 1 2 3 © 2023 PRESCRYPTIVE. ALL RIGHTS RESERVED.
HCAA Sponsorship Guide Fall 2023 | 99
the Possibilities
Magellan Rx Management, a Prime Therapeutics LLC company, is a next-generation pharmacy benefit manager on a quest to evolve and inspire the pharmacy industry and lead our customers and members toward a brighter, healthier future.
Connect with us at the HCAA TPA Summit and see how we can help you solve complex pharmacy challenges.
JERRY HOMSTAD
Vice President, Sales
homstadj@magellanhealth.com
Jerry Homstad

NICK STANBURY

Vice President, Sales
stanburyn@magellanhealth.com
Nick Stanbury, Esq
Prime/MRx
Illuminating
HCAA Sponsorship Guide Fall 2023 | 101
Protect Plan Assets and Reverse the Progression of Chronic Kidney Disease
The costs of chronic kidney disease (CKD) and dialysis are catastrophic for health plans and their members, but proactive and preventative action pays off Renalogic enables health plans to identify and get ahead of hidden CKD risk.
Identify hidden CKD risk
ImpactIQ enables third-party administrators to identify, stratify, and quantify the hidden risks posed by CKD. By analyzing biomarkers, claims data, and member and provider-reported information, ImpactIQ identifies health plan members with diagnosed CKD, undiagnosed CKD, and those with an increased risk of developing CKD due to comorbidities and health trends.

Early, specialized clinical intervention
Prevent, delay, stop, or reverse kidney disease with ImpactCare. The only program of its kind, ImpactCare combines early identification with specialized clinical intervention and management. Registered Nurses work with members to slow the progression of kidney disease, preserve or improve kidney function, improve overall health, and reduce the cost of care for members who might otherwise progress to end-stage renal disease.
99.7 percent of participating members have avoided dialysis.
Navigate members to lower cost, highquality treatments
Managing chronic disease conditions can be overwhelming and confusing for plan members. ImpactAdvocate is a comprehensive advocacy program that helps members traverse the challenging healthcare landscape.

Supporting members with Stage 4 or higher kidney disease, ImpactAdvocate helps members understand their clinical and coverage options, as well as which treatment options might yield the highest quality results at the lowest costs.
Reduce catastrophic claim costs
Renalogic’s flexible repricing solution, ImpactProtect, protects self-funded plans from devastating, high-cost dialysis claims. Over the past 20 years, Renalogic has saved clients more than $760 million on billed charges. Today, Renalogic works with over 400 self-funded plans across the country.
ImpactProtect typically saves clients between $100,000 and $200,000 per member and keeps claims’ costs below the stop-loss specific deductible.


Clients save 82 percent on net claims.

Renalogic SCAN TO LEARN MORE Renalogic • Phone: 888.808.9380 • Renalogic.com • Sales@renalogic.com
Advocate Care Protect IQ
HCAA Sponsorship Guide Fall 2023 | 103
Great teams build great products for those in need. We combine team member expertise and experience to secure advantages for our Clients. RMR provides access to credentialed and certified professionals. - CPC,CIC, RN, MD, & Ph.D, AHIMA, HIT, Nurse Auditors, and Veteran Contracting Officers.
Receiving Healthcare should not bankrupt an individual nor plan. Even more so if the cost of that healthcare is consistently inaccurate and left unchecked. Cost Containment should help, but it needs to become more comprehensive and impactful. We work tirelessly, from all corners of our industry, to increase your CLEAN CLAIM CONFIDENCE to the highest risk areas of your plans. LARGE DOLLAR CLAIMS.
At RMR we understand that our Clients have specific needs. Let’s talk. Now more than ever, it is necessary to stay on top of the changes weaving their way into our industry. In turn, it is our belief that Cost Containment efforts must also evolve to maintain relevance and effectiveness. RMR’s products strive to be dynamic. This ensures both product compliance and relevant results are delivered.
Rocky Mountain Review RMR Rocky Mountain Review Jason Nau VP | Director of Business Development -(307) 431-5612jason.nau@rm-review.com -Code Compliance Reviews -Single Case Agreements -Group Wide Contracting -Clinical Standards of Care Eval -Specialty Drug Therapy Contracts -Medical Record Retreival Products We Defend Rocky Mountain Review promotes Payer Strength, Increased Transparency, and Billing/Coding Integrity. Let’s work together. Have a LARGE DOLLAR CLAIM? Call us. Let us show you what we can do. Moving Mountains one claim at a time...
-Third Party Administrators -Stoploss Carriers/MGUs -Self-Insured Companies -Large Dollar Claims -In Network/Out of Network -Inpatient/Outpatient -CAR- T Therapy -NICU/ICU -Trauma Centers -Burn Unit -Oncology and Radiation -Durable Medical Equipment -Rehabilitation -Air Flight/Ambulance -DRG and fee-schedule Validation -QPA Data Analytics With Focuses On
Who We Serve
We are stronger together... Something is wrong.... Call: (307) 431-5612 Solution...
R OCK Y M OUN TA IN R EVIEW
HCAA Sponsorship Guide Fall 2023 | 105

RxBenefits 800.377.1614 RxBenefits.com
HCAA Sponsorship Guide Fall 2023 | 107
Welcome to Prescription Savings
When you switch to Scripius, you get a full-service Pharmacy Benefits Manager (PBM) that provides cost savings, superior service, and complete access to claim-level data. Plus, we’re so confident your switch will be easy, we give you a first-year savings guarantee and a money-back satisfaction guarantee.
You get the least expensive price tag.
Our five-year average Per Member Per Month (PMPM) cost from 2016-2020 was $66.65, and we haven’t found a lower PMPM in the market.1 PMPM is the most accurate price tag because it includes all your costs: administrative fees, clinical programs, network discounts, rebates, maximum allowable cost lists, and ingredient costs. It’s the real price tag you’re paying.
You get clinical programs that work.
Beyond achieving a high generic utilization rate, our pharmacist team works to save you money in all aspects of your drug spend. Our team secures enhanced rebates and renegotiates network contracts, and they implement clinical programs like our medication management, biosimilars, and opioid management programs. All in all, our programs equated to MORE THAN $54 MILLION IN SAVINGS.
You get agile customizations with speedy market adjustments.
It’s a volatile marketplace and you need a PBM that can make dynamic reactions to surprise price increases and new pipeline medications. While some take 45 days to react to marketplace changes (the time lost can cost clients thousands of dollars), we can often make changes on day one.
You get guaranteed savings in year one.
Million
Million
$54.7 MILLION
We are so confident we can save you money that we guarantee it. If you share your data and let us reprice your claims, we will give you a first-year savings amount that we will guarantee. Email GetSavingsNow@Scripius.org to start the conversation.
Scripius PBM
$0 $20 $40 $60 $80 $100 National Paid PMPM Scripius Paid PMPM 2020 2019 2018 2017 2016 57.86 86.20 61.93 87.24 65.19 89.27 70.66 93.11 77.64 97.39
1 Source: The 2021 Economic Report on U.S. Pharmacies and Pharmacy Benefit Managers, Adam J. Fein, Ph.D., Drug Channels Institute (March 2021) and Scripius internal data.
PROGRAM 2021 SAVINGS Medication Management $20.9
Biosimilars $2.9
Enhanced Rebates $11 Million Opioid Management $2
Network Negotiations $18
TOTAL
© 2023 Scripius. All rights reserved. 2403350 01/23
Million
Million
Scripius.org
HCAA Sponsorship Guide Fall 2023 | 109
888-243-6890
Collaborating with benefits brokers, third-party administrators, and consultants to design and deliver strategies that reduce clients’ prescription drug costs and improve member satisfaction.
FULL-SERVICE national PBM with our own mail order, specialty pharmacy, call center, network, & clinical programs.

PRIVATELY-HELD since our inception in 1987, we don’t have pressure from investors.
36 YEARS of proven success servicing self-insured mid-market employers.
Exceptional service, end-to-end flexibility, and solutions that meet our clients’ goals.
THE SERVE YOU RX DIFFERENCE
Our 2022 overall trend of 5.07% and specialty trend of 2.67% far surpass the industry of average of 9.5% and 11.7%, respectively.1
Our clinical programs drove a 15% increase in targeted adherence rates, resulting in fewer hospitalizations and better overall outcomes for members.
100% of our clients were prepared to meet Section 204 transparency reporting requirements by the December 27, 2022 reporting deadline
Each account has a dedicated Clinical Account Executive (a PharmD), Account Executive, and account management team.
Our call center has a 99% first-call resolution rate.
Our clients own their data. We help them use it to make informed decisions.
We have a 99.9% implementation accuracy rate and can implement some groups in 30 days or less.
There’s no guess work. We provide straightforward pricing and contracting practices.
sales@serveyourx.com New
Send
If you have groups seeking service improvements, we can help!
ServeYou RX
©2023 Serve You Rx 230006SA(0523)
ServeYouRx.com
groups
save an average of 32% on their total drug spend by switching to Serve You Rx.
& savings
us a claims file for a rapid repricing
analysis
1. IQVIA 20222023 Health Care and Pharmaceutical Marketplace Trends. US Pharmaceutical Trends, Issues, & Outlook for AMCP. March 23, 2023, presentation (Doug Long). Trend numbers are based on drug spend and do not account for any rebates.
HCAA Sponsorship Guide Fall 2023 | 111
Sharecare

All together better
At Sharecare, our mission is to collectively empower the health and well-being of every human.
Sharecare is a health & well-being hub that unifies all the elements of individual and collective health to work together so everyone can live better, longer - regardless of whether they are an employee, health plan member, patient or community member.
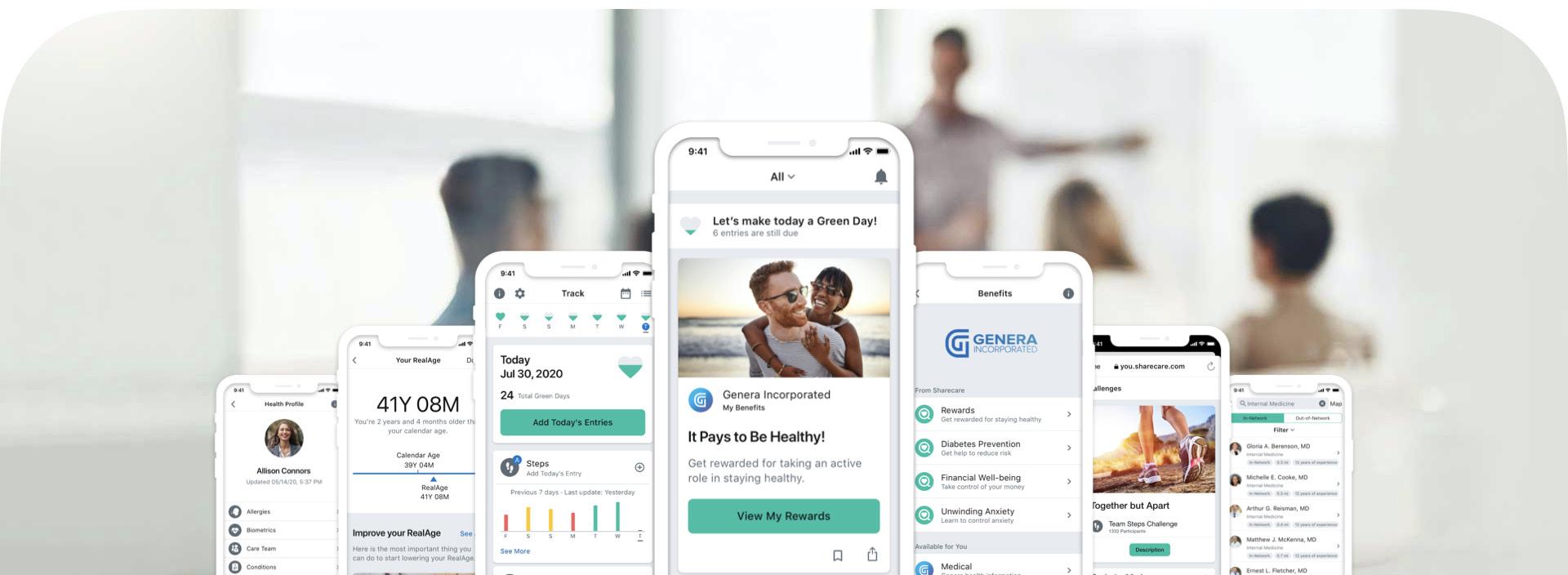
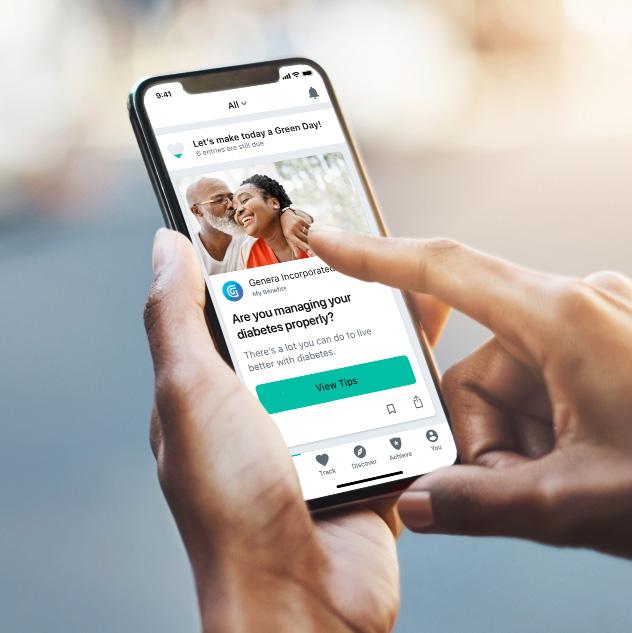

Designed to help people, workforces and communities optimize their well-being, our interoperable platform integrates fragmented point solutions to foster a frictionless user-friendly experience that engages people in all aspects of their health. From medication adherence and managing a chronic condition such as diabetes or heart disease to developing better eating habits, improving sleep and reducing stress, Sharecare dynamically supports each individual through the lens of their personal health journey and connects them to the right stakeholders at the right time.
We believe everyone’s health & well-being is inherently interconnected – a person’s physical health is connected to their mental and emotional health. But, also an individual’s health is connected to a greater collective –their friends, colleagues, employers, doctors, insurers, and local community. Yet, the category remains incredibly disconnected with hundreds of fragmented point solutions.
At Sharecare, we see our role as the great unifier. We unify the elements of an individual’s health –physical, mental, emotional, etc. – with the greater collective – users, employers, doctors, insurers, governments, etc. – to create one health & wellbeing hub where every piece works together so everyone can live better, longer.
We sum it up as ‘All Together Better’ – all the pieces of an individual’s health, unified with the greater health collective, in one connected system that’s working together, for better, for all.

HCAA Executive Forum Sponsorship Guide Fall 2023 | 113
Empowering Healthcare Companies
Smart Data Solutions is a strategic partner in healthcare process automation and interoperability that utilizes data and intelligent automation to digitally transform operations and deliver outcomes for our clients which reduce costs, streamline workflows, and improve overall customer experience.

Our Capabilities
INTELLIGENT DOCUMENT MANAGEMENT
3 BENEFITS FOR TPAS WHEN PARTNERING WITH SMART DATA SOLUTIONS
A strategic partner to help you better utilize your resources

WORKFLOW MANAGEMENT
Utilize our OneStream Managed Gateway for easier processing of all document types
MEDICAL RECORDS
APPEALS
An industry expert in process automation to help reduce common errors for TPAs
CLEARINGHOUSE
Smart Data Solutions 960 Blue Gentian Road | Eagan, MN 55121 | www.sdata.us | 651.894.6400
MANAGEMENT
PRIOR AUTHORIZATION
MAILROOM & DOCUMENT CAPTURE AUTOMATION CLAIMS PROVIDER DATA
PLAN MANAGEMENT
INTEROPERABILITY
ENROLLMENT
US
CONTACT
HCAA Sponsorship Guide Fall 2023 | 115 TODAY’S INNOVATIONS | TOMORROW’S SOLUTIONS
Corporate Solutions
You want unparalleled customer service. Employers need the right stop loss coverage. At Swiss Re Corporate Solutions, we deliver both. We combine cutting-edge risk knowledge with tech-driven solutions and a commitment to put our customers first. We make it easy to do business with us and relentlessly go above and beyond to make stop loss simpler, smarter, faster and better. We’re addressing industry inefficiencies and customer pain points, moving the industry forward – rethinking employer stop loss coverage with you in mind.
corporatesolutions.swissre.com/esl
Employer Stop Loss: Limit Health Care Exposure. Advancing Self-funding

Insurance products underwritten by Westport Insurance Corporations and North American Specialty Insurance Company. © Swiss Re 2021. All rights reserved.
Together.
HCAA Sponsorship Guide Fall 2023 | 117
SOLUTIONS for Third-Party Administrators
The Transparency in Coverage Rule and No Surprises Act didn’t just create a need for a scalable technology solution that ensures compliance with the mandates, it has manifested a new participant-driven healthcare ecosystem through which your clients and their covered members can greatly benefit.
Are your groups protected today AND equipped for long-term success? TALON’s suite of software services is designed to fulfill ALL transparency requirements, while also capitalizing on the opportunities presented by a rapidly evolving industry.
ASK YOURSELF the Following Questions:
1 Are we providing the appropriate protections and guidance to our clients?
2 Can our system deliver the required shopping experience, including accurate estimates of encounter costs both at plan-level and subscriber level?
3 Are eligibility updates, plan design feeds, consumption accumulators, QPA and Advanced EOBs fully automated?
4 Have we protected ourselves and our clients from costs for accessing and downloading publicly accessible files?
5 Have we architected a compliance solution that scales and will work long-term?
WHY TALON?
Our dynamic platform goes far beyond JUST compliance—providing a streamlined, end-to-end solution for lowering healthcare spend and fostering a happier, healthier, more productive workforce.

Our system creates free-market dynamics, starting with subscriber engagement through alignment of incentives, providing true ROI.
The unmatched digital experience provided by our innovative MyMedicalShopper™ platform EMPOWERS employees to be informed and make smart, economical decisions about their own care.
As an added incentive for choosing low cost, high-quality care, TALON’s patented and intuitive MyMedicalRewards™ program rewards employees through HSA/HRA contributions or gift cards.
TALON seamlessly integrates with any existing system with no distraction or disruption.
TALON protects your clients from overpaying for care, lowering healthcare spend by 20-40%!
TALON
The Time to Act is NOW. Are You Equipped to Meet the Challenges ahead? Let’s talk TODAY about what TALON can do for you and your clients. moc.hcethtlaehNOLAT@selas | 0203.292.306
HCAA Sponsorship Guide Fall 2023 | 119
THE PHIA GROUP’S SERVICES
Learn Plan Save Protect
The Phia Group Is Empowering Plans To Contain Costs Through Comprehensive Consulting, Legal Expertise, Innovative Plan Design, Superior Claim Negotiation & Unrivaled Recovery Services

Learn: Plan:
Independent Consultation & Evaluation (ICE)
General Consulting & Third-Party Agreement Review
Family and Medical Leave Act – Policy Review & Drafting
Phia Document Management® (PDM) & the Flagship Template
Plan Drafting Services – Including Wraps & SBCs
Gap Free Review® – Including Stop-Loss & Employee Handbooks
Save:
Subrogation & Reimbursement
Overpayment Recovery
Claim Negotiation & Sign-Off (CNS)
Phia Unwrapped – Out-of-Network Solution
Protect:
Plan Appointed Claim Evaluator® (PACE)

Balance Bill Resolution & Reference-Based Pricing Support
No Surprises Act
Balance Bill SafeGuard
Phone: 781-535-5600
Email: info@phiagroup.com
Website: phiagroup.com
The Phia Group
HCAA Sponsorship Guide Fall 2023 | 121
Customized Pharmacy Benefit Plans
We create and manage customized pharmacy benefit plans that fit the unique needs of each client. Tell us about your employers’ greatest benefit challenges, and our strategists will design solutions that optimize medications, lower costs, enhance employee health, and minimize disruption.
Exceptional Service Creates Satisfied Clients
Our focus on client communication and patient care helps you retain and gain more clients by delivering an exceptional pharmacy benefits management experience.
ROI Visibility with Quarterly Plan Reviews
Each client has quarterly reviews that show how we fulfilled our savings promise, how many members we assisted, and patient satisfaction scores.
One Team of Experts for All Needs
Every client and TPA has one team for implementation, reporting, monitoring, and ongoing consulting. You’ll have access to the same team for every call and question.
OUR ACCOUNT MANAGERS RETURN CALLS PROMPTLY
97% FIRST CALL RESOLUTION
4.7/5 PATIENT CARE SATISFACTION
Transparent Pricing and Rebates
Our model is designed around integrity. That means no spread in medication pricing and clients receive 100% of manufacturer rebates.
Working With Us is Simple
You’ll have clear contracts, a clinical pharmacist on your team, no-hassle integration, and innovative, proven solutions.
SCHEDULE A MEETING WITH SARAH HOWLETT, MBA, BUSINESS DEVELOPMENT DIRECTOR SARAHH@TRUERX.COM
TrueRx
PBM
THE UNIQUE VALUE WE PROVIDE OUR TPA PARTNERS 866-921-4047 hello@truerx.com truerx.com ©2023 True Rx Health Strategists
A Trusted
Partner with Proven Solutions
WITH 70+ TPAS
INTEGRATED
NATIONWIDE
HCAA Sponsorship Guide Fall 2023 | 123
Turn to a Stop-Loss Provider You Can Trust
Established nearly 15 years ago, USBenefits Insurance Services, LLC is a full service Managing General Underwriter, providing Medical Stop-Loss insurance coverage for employer groups through qualified Third Party Administrators (TPAs), consultants and brokers.

“In an ever-changing, oversaturated environment, it’s important to partner with a stop-loss company that will bring both stability and trust. Our customers have confidence in USBenefits, knowing that we’ll always provide actionable answers to their questions.”
 — Joseph Dore, President of USBenefits Insurance Services
— Joseph Dore, President of USBenefits Insurance Services
Unlike many other companies, we still answer our phone.
Contact us today to learn more or to request a stop-loss quote:
USBenefits Insurance Services, LLC
Send
Fax:
US Benefits Insurance Services
RFPs to: quotes@usbstoploss.com Phone: 877.877.4USB
866.504.4USB
Irvine,
dba Employer Stop Loss Insurance Services, LLC (CA only) usbstoploss.com Connect with us on LinkedIn |
43 Corporate Park, Suite 101
CA 92606
HCAA Sponsorship Guide Fall 2023 | 125
Drive better decisions with deep transparency
Reimagine what a health plan should be. It starts with the Vālenz® Health fully integrated Healthcare Ecosystem Optimization Platform and its single point of entry for deep data transparency – driving cost control, improved plan design, higher care quality, and a better member experience.

Under the Claim Cost Arc SM , we engage early and often with data, empowering you to make better decisions across the member journey and life of a claim. That level of data transparency is key to balancing cost, quality and utilization, and keeping administrators, payers, providers and members aligned along the way.
If you want a strong, vigorous and healthy medical cost containment partner committed to deep transparency, choose Valenz. Choose smarter, better, faster healthcare – visit valenzhealth.com or call us at (866) 762-4455 today.
HCAA Sponsorship Guide Fall 2023 | 127
For more information, please contact VARIS: (916)294-0860 or info@varis1.com
ABOUT VARIS
SERVICE OVERVIEW
Founded in 2004 as a private, national, woman-owned company, VARIS specializes in providing overpayment identification services exclusively to health care payers to identify and recover improper payments due to coding, billing and/or processing errors for inpatient and outpatient paid claims. VARIS serves clients that represent more than 35 million covered lives throughout the United States and Puerto Rico.
Plans range in size from 2,000 members to 15+ million, including some of the nation’s largest payers. The size and scope of our clients demonstrate our scalability and understanding of each individual’s unique needs and requirements. We are currently contracted to perform overpayment identification services for clients who are Medicare Advantage Contractors, Medicaid Managed Care contractors, Commercial payers, State Medicaid, Administrative Service Organization (ASO), and Medical Service Organizations (MSO).
VARIS’ expertise is in pre-payment, post-payment, and onsite auditing.
SERVICE OFFERINGS
VARIS proudly offers the following services:



• Inpatient DRG Review (MS-DRG, APR-DRG, CMS-DRG, AP-DRG, TRICARE-DRG)
• Outpatient/APC Review
• Clinical Validation
• Readmissions
• ER/ED Leveling
• Consulting Services
TAPRx REVIEW PROCESS
VARIS’ proprietary tri-level, risk analysis and stratification process (TAPRx Review) provides the most thorough recovery audit reviews in the industry. 100% of the health plan’s inpatient/outpatient claims data is reviewed at some level during our process, resulting in up to 3% hard dollar recoveries back to the bottom line.
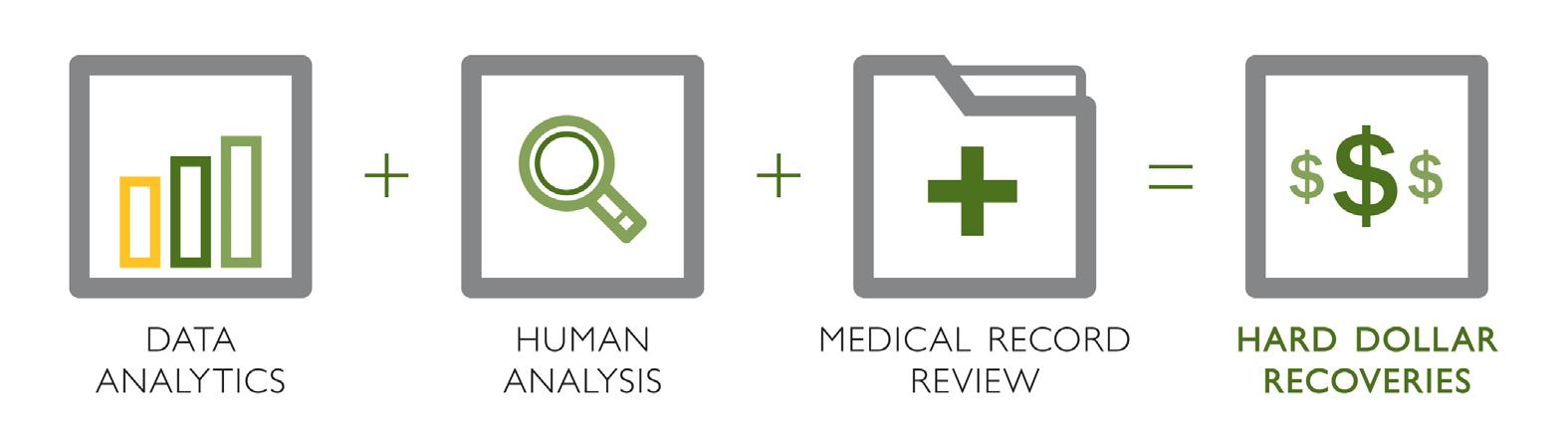
EXPERTS IN OUR FIELD
VARIS’ success is based on our uniquely qualified and experienced team of coders, who are certified by the American Health Information Management Association (AHIMA) and/or the American Academy of Professional Coders (AAPC). All of our certified coding professionals, Clinical Validation Registered Nurses and operational team are employees of VARIS. We do not conduct nearshore or offshore business practices.
VARIS’ Coding Validation Specialists (CVS) remain objective when performing reviews for our clients. Audits are conducted in accordance with health plan policies and payment methodology application, including provider contract provisions.
HCAA Sponsorship Guide Fall 2023 | 129
INDUSTRY-LEADING HEALTHCARE TECHNOLOGY

Rising costs and evolving regulations cause chaos, consistently throwing a wrench into payers’ plans. Having the technology to successfully adapt and grow, despite these changes, is vital. VBA’s suite of flexible, scalable and interoperable solutions are designed to help payer deliver high-quality care to their members.
Why Choose VBA?
Thousands of APIs Enable interoperability for more efficient functionality
Flexible Choose fully integrated or standalone solutions


Configurable Serving payers of all types







Evolving 10+ Software releases per year
Reliable 99.999% uptime
U.S. Based 100% Staff, development, and support

VBA Learn how VBA can move your healthcare technology forward from chaos to clarity
PROVIDING ULTIMATE CLARITY FOR YOUR BUSINESS
vbasales@vbasoftware.com | 1.866.731.1571 | vbasoftware.com
HCAA Sponsorship Guide Fall 2023 | 131
Like many Americans, Joaquín had multiple co-occurring chronic conditions:
• Diabetes
• High blood pressure
• High cholesterol
In 6 months with Vida Joaquín achieved:
Weight loss
22 lbs
The 5 keys to Joaquín’s success:
• Chronic pain
• Obesity
Hypertension
1. Strong relationship with his registered dietitian
• Twenty video chats with his RD over 6 months and 135 asynchronous messages
• Provider trained to recognize warning signs for physical and mental issues
2. Mental health support to address anxiety and depression
• All members screened for anxiety and depression in onboarding
• All Vida providers use cognitive behavioral techniques

3. Flexible care adapted to his current needs
• Medical Nutrition Therapy for a personalized eating plan
• Educated on exercise techniques adapted for his chronic joint pain
4. Engaging content and prompts
• Personalized content educates on the “why ” and “how” to help change habits
• Machine-learning delivers content at the right time for a great member experience
5. Lifelong skills to sustain health
• Ongoing support to maintain new skills, while stepping down to less intense care

• Adaptable pathways to pursue a new health goal
Good health can be gained through practice. With Vida, members build the foundational skills to get and stay healthier.
Vida Health Contact Us vida.com
Five reasons why Vida’s human-led solution leads to better cardiometabolic outcomes
6% from baseline Systolic, 8 mmHg diastolic, from baseline avg of 151/91 to an average of 130/83 A1C 8.5 to 6.6
21 mmHg 1.9 pts
HCAA Sponsorship Guide Fall 2023 | 133


HCAA Sponsorship Guide Fall 2023 | 135
Out-of-Network Claims

Shielded claims resolve provider reimbursement disputes, ensuring plans and members pay a reasonable price for healthcare. Shield renders balance billing ineffective and unenforceable.
Transfer the risk of disputed NSA claims, including Air Ambulance claims, to WellRithms. Shielded claims result in immediate bill closure and plan asset protection.

WellRithms
No Surprise Act Claims
info@wellrithms.com 80 % GUARANTEED SAVINGS EXPERIENCE UP TO O V E R P A Y I N G F O R H E A L T H C A R E STOP and Eliminate Risk With WellRithms Shield Indemnification™
WellRithms.com
HCAA Sponsorship Guide Fall 2023 | 137
Empowered Members, Lower Plan Costs, Satisfied Clients
At No Cost to TPAs
Approximately 15 million Americans have surgery every year,1 and as many as 50% of those surgical procedures are medically inappropriate.2
Advantages for TPAs
( No cost (billed to group as a claim)
( Value add
The truth is, when patients hear the word surgery, most never take the time to consider all their options, often leading to avoidable medical expenses. Welvie is changing that.
Welvie My Surgery® is a proprietary six-step online program designed to educate and empower plan members who are considering surgery, arming them with the information needed to make the best decision for their health and well-being. When surgery is necessary, they are guided though the process every step of the way to drive better outcomes and ensure that the benefits outweigh the risks.
Step 1: Get the Right Diagnosis
Step 2: Find the Right Doctor
Step 3: Make a Decision
Step 4: Learn About Hospitals
Step 5: Prepare for Surgery
Step 6: Recover at Home
( Engaged population
( Reduced claims
( Informed decisions
( Happy clients
Proven Results
Savings of $15.00 PEPM on surgery spend.
93% of participants said they were better prepared for their surgery.
95% of participants said they were better informed when speaking to their doctor.

Welvie
Call (312) 579-3023 or visit welvie.com. Get Started with Welvie today! 1 “Strong for Surgery,” American College of Surgeons. 2 Washington Post website: Spinal fusions serve as case study for debate over when certain surgeries are necessary. Peter Whoriskey and Dan Keating (October 27, 2013): washingtonpost.com
HCAA Sponsorship Guide Fall 2023 | 139
Who is SimplifyWEX the business of running your business
WEX frees you from the administrative burdens slowing you down by streamlining:
How you manage your employee benefits
How you modernize and manage your fleet and save on fuel costs
WEX is the global commerce platform that simplifies the business of running a business by:

• Automating highly manual processes and reconciliations
• Connecting disjointed payments and data exchange through personalized technology solutions and resources
WEX’s wide range of solutions can be seamlessly embedded into your existing business systems and delivers security and scale through integrated data and analytics, and reliable performance at scale.
The continual investment in customer-focused innovations and experiences, in concert with our rich transactional data and behavioral insights, allows us to innovate more quickly to deliver new, more personalized solutions to the market.
WEX
How you pay and get paid by suppliers
Simplify Employee Benefits Streamline Making & Receiving Payments Manage Fleets & Mobility
HCAA Sponsorship Guide Fall 2023 | 141
Web Portal 2.0
MediConnX360, Powered by TALON, is an identically operating native app for iOS and Android, and a web portal unlike any other, providing patients, payers, employers, providers, and brokers with ondemand, all-inclusive access to the data and services they need. That means members are instantly connected – and stay connected – to the industry’s most comprehensive, compliant, and automated benefits administration solutions.
o With MediConnX360 you can:
• Grant on-demand access of machine-readable files and reports to administrative and employer users.
• Distribute information to a large audience, using the integrated announcement feature

Provide directed selling methodologies
o And your members will be able to:
• Utilize price comparison shopping, including quality metrics and innetwork guidance.
• Verify claim payments.
• Access ID cards, Explanation of Benefits (EOBs), and Advanced Explanation of Benefits (AEOBs).
Search physicians linking members with providers.
Securely send messages and attachments.
Manage enrollment, family status changes, and ID card requests.
…and much, much more!
WLTSOFTWARE.COM
Compatible with Mobile and Desktop

HCAA Sponsorship Guide Fall 2023 | 143
Automate Your Analytics: Complete Pharmacy Benefits Optimization
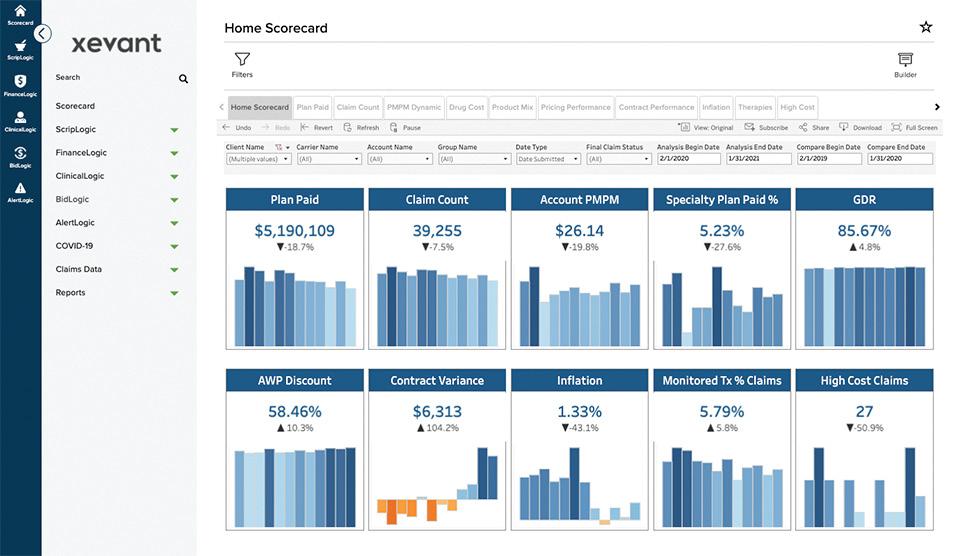
Imagine a virtual pharmacy benefits expert analyzing your data every single day, looking for opportunities to reduce cost and improve outcomes, and instantly alerting you to take action immediately.
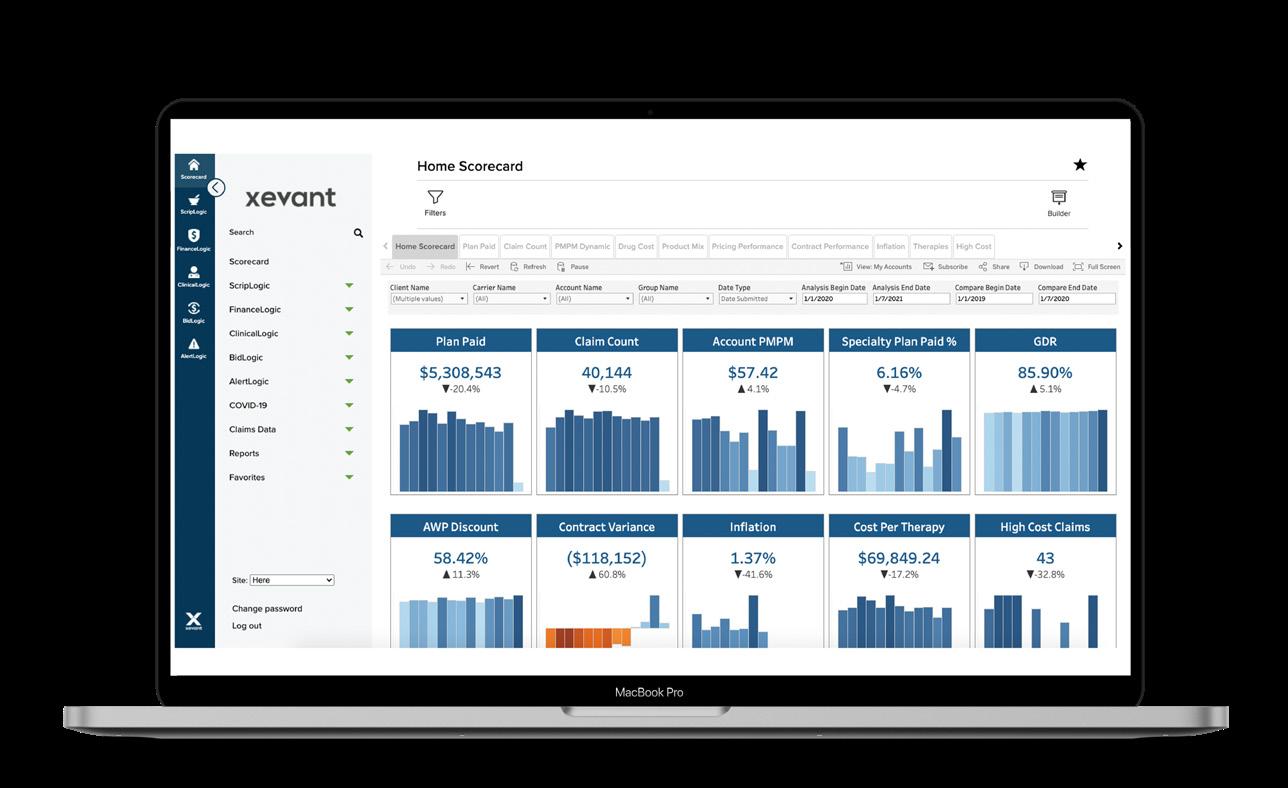
Xevant Unlocks The Full Value of Your Solutions
Xevant enables you to fully maximize the value of your proven solutions by instantly and autonomously identifying issues that are uniquely solved by the solutions only you can provide.
Save
Replace
Elevate Accuracy and Quality
In today’s commodity-based view of pharmacy benefits, a premium is placed on the ability to deliver better quality. Xevant infuses proven, expert pharmacy analysis in every daily review of claims.
Accelerate
Your clients depend on you to achieve the lowest costs and highest outcomes. Streamline, accelerate, and maximize client performance by identifying and solving issues immediately.
Achieve Client Satisfaction and Retention
Xevant creates an environment where clients would never dream of leaving for fear of losing savings and outcomes that only you can provide.
Xevant WWW.XEVANT.COM (888)774-5551 ® ANALYTICS MEETS AUTOMATION
decades-old, manual, and costly processes of
and analysis by
expert
reporting
deploying Xevant’s full suite of automated
analytics.
Time and Money: Automate
Performance
Results
and
SCHEDULE A DEMO OR TALK TO AN EXPERT TODAY (888) 774-5551 sales@xevant.com www.xevant.com © 2021 Xevant, Inc. All Rights Reserved.
HCAA Sponsorship Guide Fall 2023 | 145
Lowering Employers’ Healthcare Costs
zAnalytics
zakipoint Health uses predictive analytics and integrated solution pathways to clarify employers’ healthcare spend and drive actions to reduce it.
Help employers understand their healthcare spend and recognize opportunities for cost savings
• Prioritized opportunities for saving based on current spend and population health
Provide population-specific action plans and solution tools to improve benefit utilization and drive action
• Library of actionable solutions in step-bystep pathways to guide implementation
Enhanced member experience to access personalized information
• Personalized recommendations to improve member engagement based on predictive analysis
Enable employers to visualize the impact of actions on spend and member health
• Set goals and track progress with a dashboard of engagement and quality metrics
Solutions to enable patient centric care
Unified Data Platform
Predictive analytics and algorithms to identify gaps in care, cost drivers, risk drivers, etc.
Personalization
Use data driven technology & CRM to personalize member experience and interactions
Asynchronous multi-touch communication
Digital assistant available 24/7 to support members in their day to day queries, issues & easily connect to human touch
Artificial Intelligence
Pro-actively promote appropriate behaviour e.g. close gaps in care, make PCP appointments, use alternative places of care
Nudges
Predictive analytics and algorithms to identify gaps in care, cost drivers, risk drivers, etc.
zConnect Cost Estimator Tool Solution
• zConnect is a dynamic, embedded multi-touch mobile provider search tool configurable to any plan design and network design
• zConnect allows members to search and compare the prices for healthcare services at different places of care based on contracted network negotiated rates
zakipoint
Health
IDENTIFY
CONNECT
ACT
TRACK
E: marketing@zakipointhealth.com P: 617 657 9254

HCAA Sponsorship Guide Fall 2023 | 147
About Us
We believe in a better way to price, explain, and pay for healthcare on behalf of insurers and their members.
As the leading payments company in healthcare, we price, pay and explain healthcare for payers, providers, and healthcare consumers. Zelis was founded on a belief there is a better way to determine the cost of a healthcare claim, manage payment-related data, and make the payment because more affordable and transparent care is good for all of us.
Why Zelis?
We partner with more than 700 payers, including the top-5 national health plans, Blues plans, regional health plans, TPAs and self-insured employers, 1.5 million providers and millions of members, enabling the healthcare industry to pay for care, with care. Zelis brings adaptive technology, a deeply ingrained service culture, and an integrated pre-payment through payments platform to manage the complete payment process.
Zelis brings efficient, purpose-built solutions backed by a passionate team and agile technology to harmonize the complete payment process in healthcare.
Zelis has been recognized as an INC 5000 Fastest Growing Company annually for the past 11 years, and is a certified Great Place to Work.
Zelis Pay for care, with care. zelis.com © 2022 Zelis Executive Summary ENTERPRISE
Faster, more accurate healthcare payments. Only with Zelis. B $27+ Network & Claims Cost Savings Since Inception SERVICE SEGMENTS TPAs, Regional and National Health, Dental and Taft Hartley Plans 5 OFFICES 1,300+ ASSOCIATES Atlanta, GA | Bedminster, NJ Overland Park, KS | St. Louis, MO St. Petersburg, Fl. 700+ Payer Clients 13YRS Average Client Tenure 99% Clients Retention Rate 1.5+ Enrolled Providers M Payment Communications Annually 500 + M $100+ Payments Delivered to 700k+ Providers on Behalf of 335+ Payer Clients Annually B
HCAA Sponsorship Guide Fall 2023 | 149

aequum, LLC AccuRisk Solutions Availity Coral 150 | HCAA Sponsorship Guide Fall 2023 Company Additional 2023 Sponsors






Denniston Data, Inc. Planwatch Hines & Associates Viveka Health WithMe Health HCAA Sponsorship Guide Fall 2023 | 151 Company
















































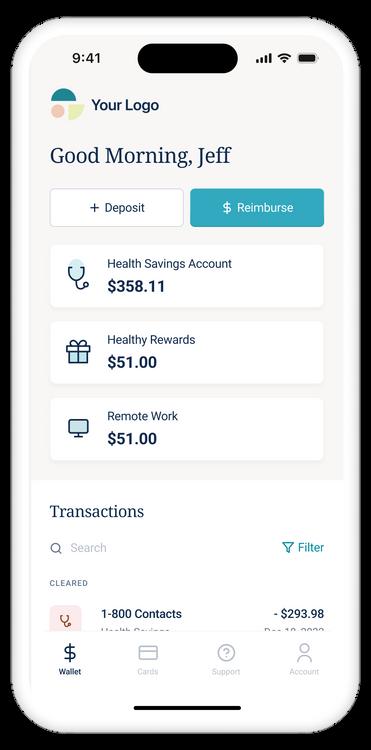





















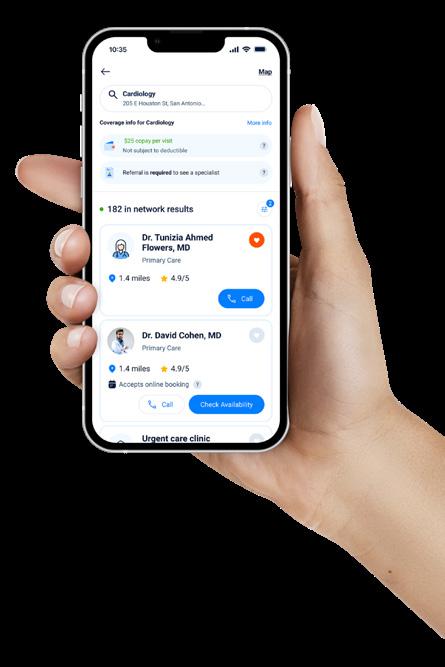



































































































































































































































































































































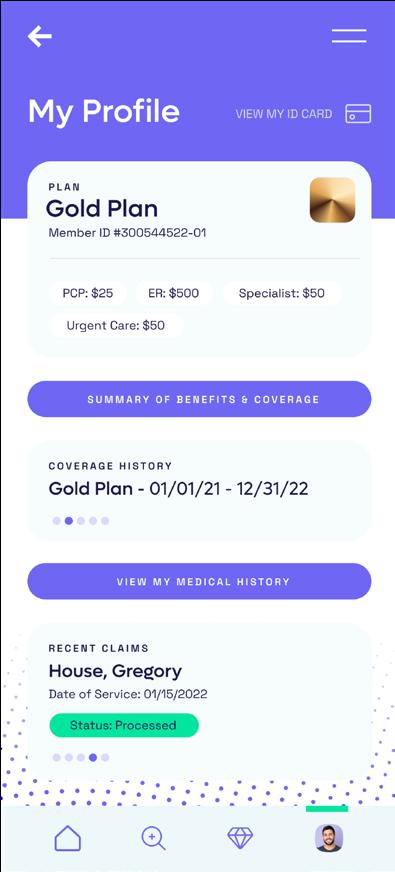
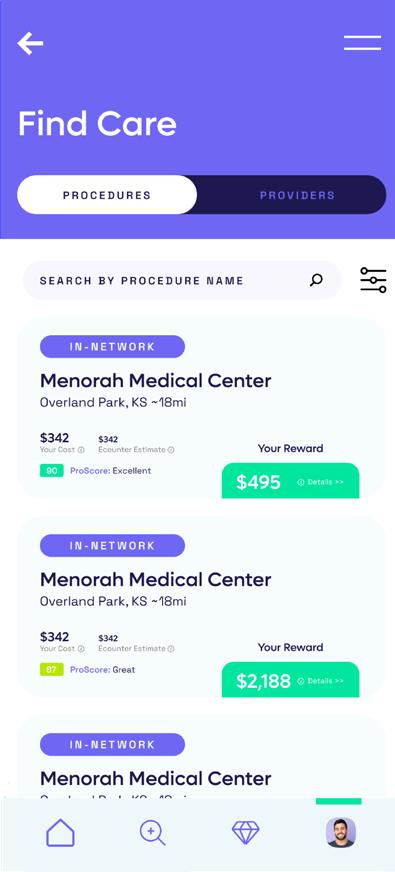

























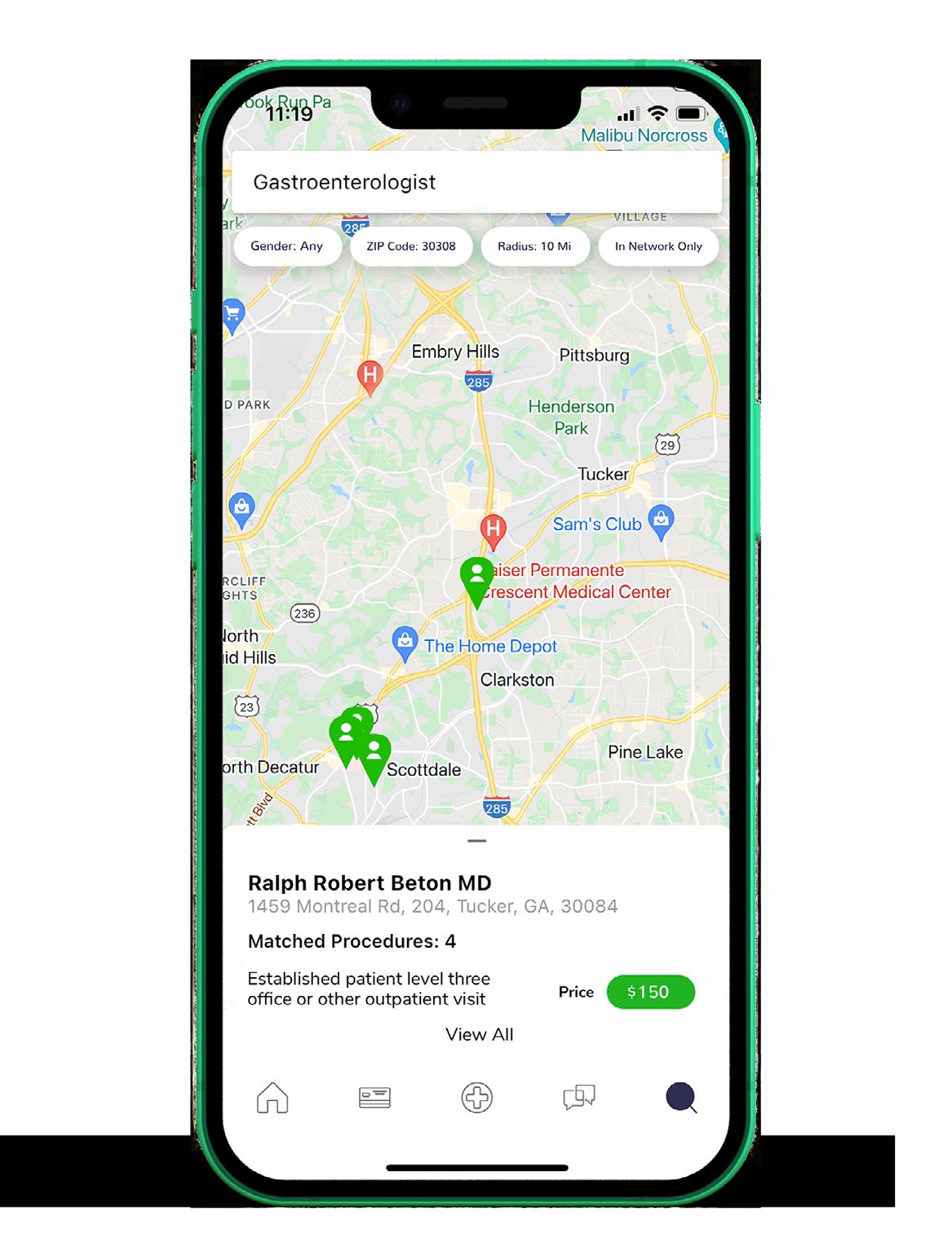


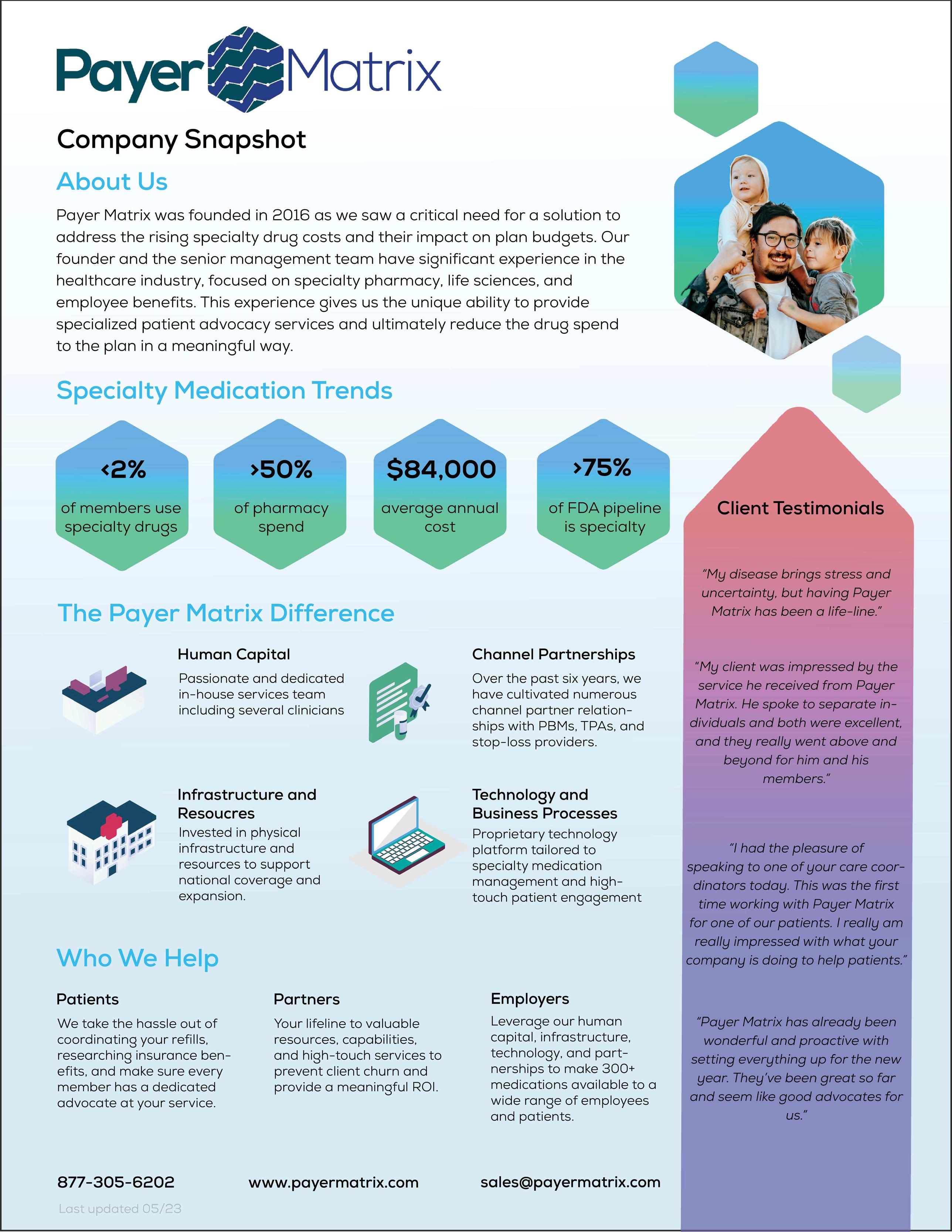

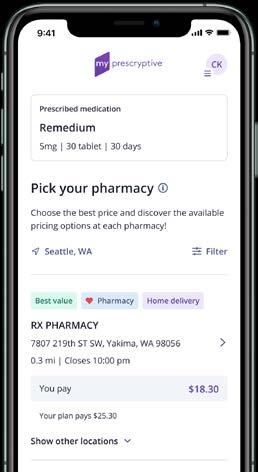











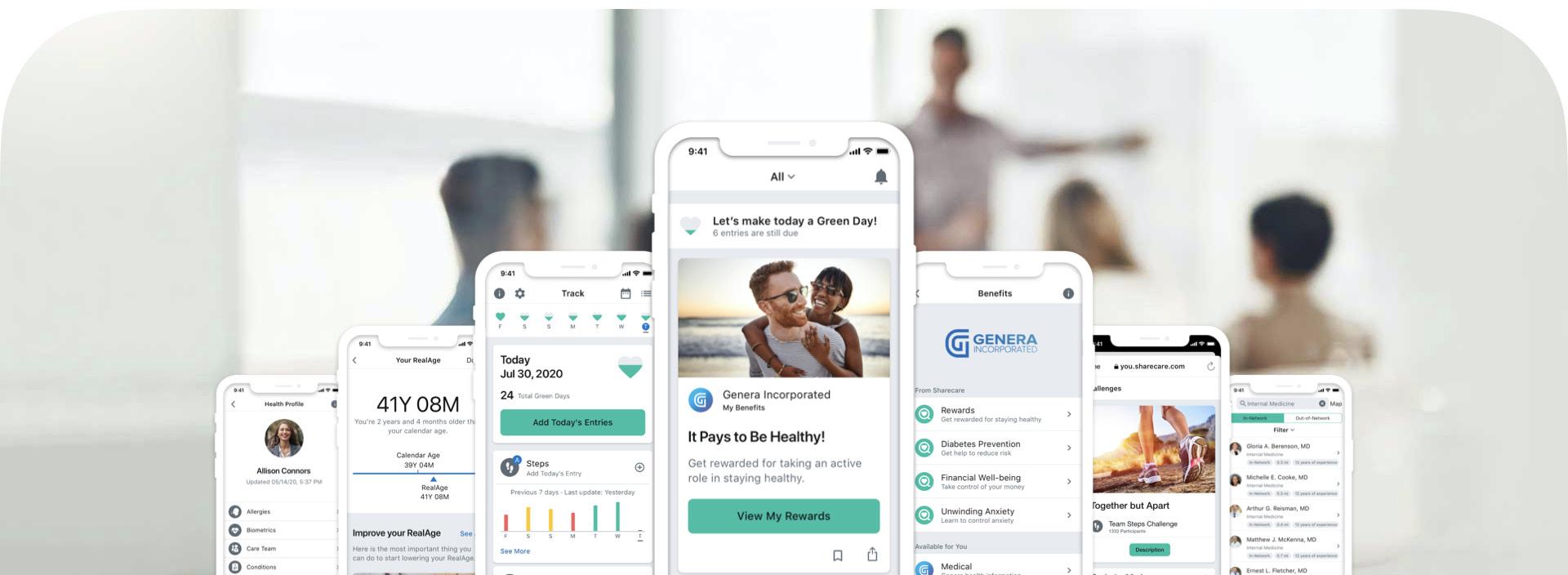









 — Joseph Dore, President of USBenefits Insurance Services
— Joseph Dore, President of USBenefits Insurance Services