How six tech-savvy leaders use data to track patient journeys, set successful recovery paths, and support healthier communities P8





How six tech-savvy leaders use data to track patient journeys, set successful recovery paths, and support healthier communities P8












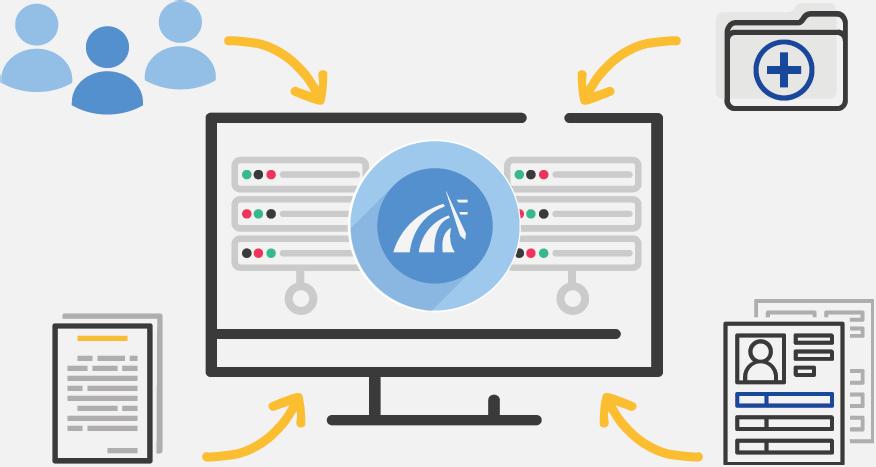
Exclusion monitoring and license verification are critical tools for ensuring compliance, program integrity, and patient safety. It’s vital to continuously monitor all primary sources at both the federal and state levels to guarantee the most qualified providers are caring for your patients.

Why should you choose ProviderTrust’s platform for exclusion monitoring and license verification?
ProviderTrust’s enhanced, proprietary data engine is what sets our holistic compliance monitoring apart. Our smarter monitoring science enables us to catch more employee eligibility issues than any other solution, from finding an OIG exclusion to verifying a license expiration or sanction.
Want to learn more about what makes ProviderTrust’s compliance monitoring smarter?

Explore our website:
www.providertrust.com/our-company
“We
“When you lead information systems for a healthcare provider, you are more than an IT professional. . . . We’re ultimately responsible to the patients.”
—Kory Hudson, Singing River Health System
really want to be thinking ahead. We want to be experimenting with very new technologies and bringing some modernday solutions to our healthcare systems.”
—Martin Hadida, Memorial Healthcare System
“When you have any kind of dispute or investigative concern, you’re going to want to go back and look at the electronic record to figure out what really happened.”
—Amy Sellars, Cardinal Health





VP, Creative Production
Kevin Warwick
Editorial Manager
Frannie Sprouls
Managing Editor
KC Esper
Editors
Melaina K. de la Cruz
Sara Deeter
Julia Thiel
Hana Yoo
Staff Writers
Zach Baliva
Billy Yost
Contributing Writers
Will Grant
Frederick Jerant
Russ Klettke
Natalie Kochanov
Donald Liebenson
Keith Loria
Maggie Lynch
Lewis Mergler
Katie Oltmanns
Senior Designer
Vince Cerasani
Senior Photo Editor & Staff Photographer
Sheila B. Sarmiento
Photo Editor & Staff Photographer
Cass Davis
Social Media Manager
Ashley Rupprecht
CORPORATE
CEO & Publisher
Pedro A. Guerrero
Chief of Staff
Jaclyn Gaughan
President, Group Publisher
Kyle Evangelista
VP, Hispanic Division
Head of Audience & Engagement
Vianni Lubus
VP, Finance
David Martinez
VP, Sales
Ben Julia
Senior Director, Client Services
Cheyenne Eiswald
Senior Client Services Manager
Rebekah Pappas
Client Services Manager
Brooke Sackett
Director, Client Services–Corporate Partnerships
Taylor Frank
Director, Talent Acquisition & Engagement
Haylee Himel
Director, Talent Acquisition
Heather Steger
Senior Director, Corporate Partnerships & DEI Partnerships
Krista Horbenko
Director, Events
Jill Ortiz
Communications Manager
Cristina Merrill
Director, Sales
Kelly Stapleton
Director, Sales Training & Development
Alexa Johnson
Director, Sales Onboarding
Justin Davidson
Content & Advertising Managers
Ashley Alcock
Megan Apfelbach
Brandon Havrilka
Leon Hu
Annie Peterson
Kayla Plastiak
Ashika Sachdev
Aliana Souder
Drew Thomas
AHL Magazine® is a registered trademark of Guerrero, LLC.
Facebook: @ahlmagazine
LinkedIn: @american-healthcare-leader
Twitter: @AHL_Magazine
©2022 Guerrero, LLC guerreromedia.com
1500 W. Carroll Ave., Suite 200 Chicago, IL 60607
Reprints
Reprinting of articles is prohibited without permission of Guerrero, LLC. Printed in China. For reprint information, contact Reprints & Circulation Director Stacy Kraft at stacy@guerreromedia.com.
not great at math, I’ve worked in Excel only enough times to count on one hand, and anything involving the back end of a computer doesn’t come easily to me. I was born to be a “words person.”
I think my hesitance to working with numbers was partially because they felt so abstract—I couldn’t see a connection to them like I could with words. That is, bear with me, until I learned how philosopher Immanuel Kant views math and numbers.
Very simply, Kant theorized that everything can be broken down numerically and math is understood and accepted by humans because we can compare those abstract theories to concrete examples in life. We can walk through our neighborhoods and see four cars parked on the street, one man walking one dog, and fourteen trees planted along the sidewalk. When we are born, we can differentiate clearly between one parent over another. Everything is one thing, and together, they are more than one.
I like thinking of the world this way. I like thinking that there are 7.8 billion people on Earth, and billions of those people can each have 4 limbs, 20 fingers and toes, 32 teeth, 78 organs, 206 bones, and 37.2 trillion cells. Yet that person can still be considered 1 individual. And within that individual is an entirely separate, unique set of data.
The healthcare leaders highlighted in this issue have learned to use that data to not only become better informed about the individuals under their care but also pioneer methods of recovery, privacy, and discovery. Each personalized data set offers a story within it, showing strengths, weaknesses, hindrances, and the potential to overcome them. The ability to leverage that information opens windows to infinite opportunity—and, ultimately, better healing.
With data as the driver of every new innovation, these “numbers people” are building connections never thought possible and paving the path to the future of healthcare.
KC Esper Managing Editor

I’m not much of a “numbers person.” I’m


Six executives share how they humanize data to calculate the best patient experience
Supplemental photos
by Sheila B. Sarmiento






Lisa Abbott empowers her team to be progressive drivers of Lifespan through mentorship, respect, and compassion for the community
of human resources and community affairs at Lifespan, Rhode Island’s largest health system and employer, Lisa Abbott feels an incredible obligation to keep the people in the state employed and make world-class healthcare accessible to the community. She achieves this by assembling missiondriven teams and creating an inclusive culture based on Lifespan’s core values.
Lifespan serves Rhode Island and New England through its offerings as a comprehensive, integrated, academic health system with five hospitals and affiliation with the Warren Alpert Medical School of Brown University. Lifespan’s over seventeen thousand employees represent a broad spectrum

of experience, occupations, and cultural backgrounds. With the acquisition of Coastal Medical Group in April 2020 and the potential merger with Care New England, Rhode Island’s biggest employer is getting bigger—and Abbott is making it more inclusive.

When managing a merger from an HR perspective, Abbott is fully aware of the importance of making sure no parties feel like they are losing their identity. “It’s all in that cultural assimilation,” she says. “How do we preserve the best of who they are and what they bring and at the same time welcome them into the Lifespan family?” It’s a delicate balance, but regular communication and inclusivity in the business culture help lead the way for combined growth.
Coastal Medical Group officially becoming a part of the Lifespan health network arms the company with a high-performing primary care practice. Coastal not only aligns with Lifespan’s
As the senior vice president
 Lisa Abbott SVP of HR & Community Affairs Lifespan
Lisa Abbott SVP of HR & Community Affairs Lifespan
business strategy, but significantly simplifies the process of connecting patients to the specialists they need, allowing the company to better serve the community.


The potential merger with Care New England would provide Lifespan with service lines in obstetrics and gynecology and childbirth, while Lifespan’s domain is more related to pediatrics. This merger would deliver the ability to be synergistic with healthcare offerings from cradle to grave. “There’s not a lot of redundancy in the system; there’s a lot of opportunity for more continuity of care,” Abbott explains. “And there’s a lot more opportunity to deliver a better patient care experience.”
Abbott believes the Care New England merger would provide incredible community benefit as well. As head of community affairs at Lifespan, Abbott oversees a community health institute that strives to alleviate social determinants that keep people from receiving care such as food scarcity, access to quality care, or transportation to a job. “We see our ability through this merger to expand exponentially the services that we can provide around social determinants and people’s needs,” Abbott says.
Abbott is in her sixth year leading the HR department at Lifespan. She’s
had the opportunity to build teams in executive leadership, HR, and community affairs among other areas. When it comes to her approach for encouraging her teams to be progressive drivers of Lifespan, Abbott states, “My job is to coalesce around [Lifespan’s] mission, and make sure everybody sees why their job is related to our mission and why that makes them essential.”
She places an emphasis on hiring people who want to serve a purpose greater than self—an invaluable quality that cascades into the organization. “I’ve been very fortunate in my career to have good mentors and to have been given real breakthrough opportunities,” she says. Abbott pays it forward with her involvement in mentoring her teams in HR and community affairs with the same encouragement and guidance she received early in her career.
“My job is to coalesce around [Lifespan’s] mission, and make sure everybody sees why their job is related to our mission and why that makes them essential.”
“I want [employees] to come in engaged and motivated, and I want them to go home feeling like they matter today,” Abbott notes. “I want them to bring a good version of themselves home. So I try to instill that passion in the team. I want people to feel passionate about the mission.”

This level of respect doesn’t stop at her direct reports and department members. Lifespan values the voices of every employee and conducts engagement surveys to hear their concerns and opinions about the company. Abbott is a proponent of this open dialogue and wants to make sure everyone feels heard. She explains, “We try to communicate what we’ve acted on as a result of what people shared was important. Because that’s what they need to see—they need results.”
Abbott explains that Lifespan’s “CARE” values—Compassion, Accountability, Respect, and Excellence—are also a




driving force in how she approaches her team. “We’re going to treat each other with respect,” she notes, “and we will continue to have that as a theme of our action plan going forward.”
Lifespan was also recently awarded a $10 million grant to build pipeline programs for Black and Indigenous populations. “As the state’s largest employer, I feel an incredible obligation to keep the people employed that work at Lifespan and create employment opportunities for those looking for them,” Abbott says.

She wants her team to feel passionate about the mission and their purpose at Lifespan, while opening avenues for new members to find a place where they belong in the organization. “We’re here because we deliver health with care. It’s all about the patient experience,” she says. “We touch, in some way, everyone in our community, and that matters.” AHL








Kory Hudson brought Singing River Health System’s technology to a new level. Now, he’s using those capabilities to enhance patient care even further.
to correct misconceptions about his work, his role, and his region. He is the director of information systems and health information management at Singing River Health System, which spans the Mississippi Gulf Coast. Hudson is out to prove that the rural, southern system can provide the kind of high-quality care and experiences patients expect from a major metro market.
While most people think of in-house IT leaders as simply the hospital’s “tech guys,” he insists that his team’s role is one of service that makes a direct impact on clinicians, patients, and the communities it serves.
Singing River is a system comprised of three hospitals with various primary and specialty care clinics where patients— or “guests”—seek emergency services, cancer and cardiovascular treatments, surgical procedures, inpatient and outpatient rehab, and more. With more than 3,500 employees, 450 physicians, and 700 licensed beds, Singing River Health System is the secondlargest employer in its region and contributes approximately $270 million to the local economy.
These facts and figures provide context to Hudson’s work and motivate him to
approach all he does with the patients and community in mind. “When you lead information systems for a healthcare provider, you are more than an IT professional,” he says. “We take this job seriously because Singing River’s employees are our customers, which means we’re ultimately responsible to the patients.”
Those patients are coming to Singing River Health System for routine and life-saving care; Hudson’s team works both behind the scenes and with those on the front line to make sure each patient receives the very best care possible.
That makes Hudson, and the 120 individuals who report to him, the guardians of data and security. “Everyone who works here needs to be able to trust that they can perform their work effectively. It’s our responsibility to provide the best technology and the best service with no interruptions,” he explains.
Hudson is a veteran leader who takes a hands-on approach, with an MBA and certifications in health information administration to back him up. He applies his training to optimize systems and implement advanced software and technical services that save organizations millions. Singing River is on par with its major market counterparts, but like most effective leaders, Hudson has to overcome considerable challenges to keep pace with the ever-evolving industry.
With career opportunities limited and industries concentrated in small pockets throughout the Mississippi Gulf Coast, many individuals in Singing River’s sixcounty market are industrial or part-time workers. Many insured patients have high
Kory Hudson is on a mission
copayments, and a large percentage are uninsured. That reality means Hudson must maximize each dollar in his budget and prioritize every project to bring the highest return to the patient.
It takes careful communication with dedicated system leaders to navigate these concerns and ensure patients living in the area have access to the modern comprehensive care they would find in big cities. When it comes to competing with places like New Orleans, Houston, Dallas, and Atlanta for IT talent, Hudson takes a creative approach. He looks to recruit top professionals but also grooms capable people with nontraditional backgrounds who are willing to develop IT skills on the job.
These strategies are helping Singing River Health System thrive. Hudson was an integral leader in the installation of Epic, an enterprise electronic health record, which reduced paper records by 90 percent and brought more than $2 million in savings. Large software implementations in healthcare require key partnerships, and Hudson turned to Harmony Healthcare IT to archive the legacy data from the outdated systems Epic replaced.



allows Singing River to consolidate and store protected health information and previous business records. The partnership, Hudson says, saved his organization considerable time and money associated

“Everyone who works here needs to be able to trust that they can perform their work effectively. It’s our responsibility to provide the best technology and the best service with no interruptions.”
with maintaining dozens of various smaller systems, and it now benefits from having access to one archive that approved users can access any time.

With Epic implemented and electronic health records in place, Singing River can easily execute its mission to improve health and save lives while providing a seamless patient record independent of location. Hudson says his team has extended Epic to other local providers and even explored projects to link with outside clinics that use other systems. For instance, when a prominent community health provider passed away unexpectedly, Singing River volunteered to honor his legacy by taking authorized ownership of his patient records and fulfilling information requests.
These are just some of the key ways Hudson is working to make an impact through data, analytics, and technology. He also started an initiative to implement an enterprise-wide imaging platform that unites siloed systems and gives providers access to all of a patient’s medical images from every service line. Moving to an enterprise-wide solution drives better patient outcomes, as AI tools can scan multiple images and data sets to predict diseases and assist in diagnoses.
In October 2020, Singing River Health System acquired Garden Park Medical Center from HCA Healthcare. The 130-bed facility, now known as Singing River Gulfport, expands access to patients and features robotic surgery technology, a Level III trauma center, and a cardiac catheterization lab. As leaders increase volumes at the new facility, Hudson is deploying his IT professionals to bring its systems and technologies up to the Singing River high standards.
One of the things Hudson enjoys most about his work is the chance to see the impact it makes in the community. When COVID hit the Gulf Coast, Singing River’s first drive-through vaccination event
“We take this job seriously because Singing River’s employees are our customers, which means we’re ultimately responsible to the patients.”Kory Hudson Director of Information Systems & Health Information Management Singing River Health System
served seven hundred people, but that wasn’t enough. Hudson’s team worked overtime to automate the process, equip clinicians with handheld devices, and introduce wireless capabilities. These measures dramatically reduced wait times and doubled the number of vaccinations administered at a second event and led to Singing River vaccinating more than sixty-five thousand people against the deadly virus to date.
In fact, after arriving onsite to drop off equipment, many people from the IT department stayed behind to help their colleagues at Singing River greet patients and get them checked in to receive a dose of the COVID-19 vaccine.
The patients who came that day may never realize the impact Hudson and his team had on their ability to access care. But to Hudson, serving his community in this way just affirms he’s doing his job right. AHL

Harmony Healthcare IT is proud to serve Singing River Health System in its mission to provide a seamless patient record. As a data management firm, we partner with organizations across the healthcare continuum to consolidate and manage legacy data through extraction, migration, and archiving. To learn more about our comprehensive solutions, visit harmonyhealthcareit.com.




At the nation’s oldest cancer center, audit and advisory expert Eugene Cullen works behind the scenes to mitigate risk, leverage opportunities, and help clinicians provide life-saving care

to remember why his work matters; all he has to do is look around. As he walks Roswell Park Comprehensive Cancer Center’s twenty-eightacre campus on any given day, he’ll pass full operating rooms, encounter 150 chemotherapy patients, and interact with top researchers and physicians actively pursuing the latest breakthroughs.
Founded in 1898, Roswell Park is the nation’s oldest cancer center. As vice president of internal audit and advisory services, Cullen’s job is to manage risk through the performance of internal audits and risk assessments and providing advisory services to facilitate positive change. This helps clinical and nonclinical teams and operations improve efficiency and effectiveness to the benefit of Roswell Park and its patients.
Cullen is a realist. He knows administrators, clinicians, and other care providers are busy working as hard as they can to save lives. That’s why he does all he can to identify realistic improvements that can be made within the parameters of the organization and the constraints of the burdensome and highly regulated healthcare industry.
“Auditing and advising a medical facility is not an exercise in idealism; it’s an exercise in practicality,” he says. “We can’t produce lofty goals and fancy reports that sit on a shelf. We have to suggest changes that people are willing to make so we can improve patient care.”
At Roswell Park, Cullen’s internal audit and advisory services team gives input to leaders and board members regarding risk mitigation and performance improvement opportunities. He’s been in the role for ten years and is applying the full knowledge from a long career in the healthcare industry.
Cullen earned a master’s degree in healthcare from New School University and worked for Big 8, Big 6, and Big 4 advisory firms where he represented major clients like Northwell Health, Lenox Hill Hospital, NYU Downtown Hospital, RWJ Barnabas Health, Stony Brook University Hospital, Greenwich Hospital, St. John’s University, and Empire Blue Cross.
Cullen started when computer systems were just beginning to change the way providers and patients interact. Compared to today’s tech-filled and regulated world, it was a simpler time. Physicians had more freedom to dictate treatments. Payments and reimbursements were relatively straightforward. Administrators knew what to expect.
But now, times have changed. “The fast-paced nature of healthcare has totally changed the auditing and advisory landscape,” Cullen says. “It is night and day.” Regulations and restrictions have increased. Costs have climbed higher.




 Eugene Cullen
VP of Internal Audit & Advisory Services
Roswell Park Comprehensive Cancer Center
Eugene Cullen
VP of Internal Audit & Advisory Services
Roswell Park Comprehensive Cancer Center
Technology has brought new threats. The ability to identify clinical, regulatory, process, privacy, and IT risk matters that should be mitigated is perhaps more critical than ever before.
It takes a diverse team to do this work well, and Cullen has purposely assembled a group of people from different vocational backgrounds. He has an IT professional, a regulatory expert, and a generalist. “I ask each person on my team to be a go-to person for one area and then provide support in other matters,” he says. “We have to be ready to address any issue that comes our way.”
The small but mighty team is agnostic by design and supported, when needed, by outside advisory expertise. Instead of focusing on any specific area, they work with finance, information technology, accounts receivable, clinical services, research, and all other departments to leverage opportunities and identify risks. They also perform an annual assessment that outlines the highest risks to the entire organization. Once either process pinpoints a risk to mitigate or an opportunity to leverage, Cullen’s team develops an action plan and initiatives to help facilitate the change.
As hospitals, clinics, and health systems implement new technologies to drive innovation, IT security is always on Cullen’s mind. Since financial margins are tight, the industry was notoriously slow to adopt some of the same security

measures that are common in banking and other sectors that gather sensitive personally identifiable information.
Medical records contain names, insurance information, diagnoses, social security numbers, addresses, phone numbers, and all the information bad actors need to commit identity theft or medical fraud. “Hospitals are more vulnerable than other institutions to cyberattacks because we’ve put a target on our backs. Hacking a hospital is simply easier than hacking a bank,” Cullen says.
The stark reality forces him to respond accordingly. His team at Roswell Park has performed reviews to ensure each user who needs to access data has the appropriate level of access. They assess the design and effectiveness of information technology security controls including employee access controls, training and education, preparedness for ransomware attacks, effectiveness of computer backups, and data recovery systems to keep important patient records secure from threats and natural disasters.
Leaders at Roswell Park Comprehensive Cancer Center are vocal about the organization’s purpose. They want all employees to understand why the organization exists. Its stated mission is “to eliminate cancer’s grip on humanity by unlocking its secrets through personalized approaches and unleashing the healing power of hope.”
Cullen says his team does what it does so its colleagues can focus on fulfilling that mission. “An IT security event or a regulatory blow would distract people here from doing important, life-saving work,” he explains. “I prevent those distractions so our doctors can do
“The fastpaced nature of healthcare has totally changed the auditing and advisory landscape. It is night and day.”
research, perform surgeries, and treat cancer patients.”

Cullen has both hard data and anecdotal evidence that demonstrate the impact of his work. His team has contributed to improved patient throughput, increased physician satisfaction, lowered wait times, prevented online threats, identified opportunities to reduce expenses and improve revenue, and improved electronic medical record documentation.
At a place like Roswell Park, those results matter. The organization has roughly 3,700 employees, 350 faculty members, 800 nurses, and hundreds of funded research projects. Each year, it treats nearly 5,000 admitted patients and 270,000 outpatient visitors. At any one time, the group has about 43,000 active patients. Because of Cullen’s work, organizational risk is mitigated, and patients can access the best possible care from first diagnosis to the end of their cancer treatment. AHL

Congratulations Eugene Cullen for the well-deserved recognition you are receiving as a leader and innovator in health care. Phillips Lytle is proud of its longstanding relationship with Roswell Park Comprehensive Cancer Center. Our attorneys are privileged to support an organization that has had such a profound impact on the lives of so many patients and families.
Phillips Lytle congratulates Eugene Cullen on his recognition by American Healthcare Leader. Our firm has firsthand experience with Mr. Cullen’s passion for innovation and his goal of always putting patient safety first. We’re proud to have him and Roswell Park Comprehensive Cancer Center as leaders in our community.
We salute your Healthcare Heroes who are curing cancer and providing the highest standard of care for patients from WNY and beyond.
CTG : “Innovative leaders like Eugene Cullen are key to transforming healthcare. His commitment to improving the lives of patients, as well as the physicians and nurses who care for them, is a driving force behind Roswell Park’s success as both a leading, compassionate care provider as well as a thriving business.” –Christine Blanchard, Managing Director, Client Partnerships
CTG is proud to partner with Buffalo’s Roswell Park and share their commitment to:
• Transform patient and provider experience

• Improve operational security, efficiency and agility
• Maximize organizational performance

 By Keith Loria
By Keith Loria

never backs down from a challenge or an opportunity to find unique solutions
he was happy with when he was contacted six years ago by Memorial Healthcare System (MHS) in Hollywood, Florida, with an offer he couldn’t refuse. The position of director and enterprise data architect involved leading four different teams: database, business intelligence (BI), interfaces, and software development.
In that arrangement, he saw tremendous possibilities to create exponential returns that would benefit both the organization and patients.
“Traditionally, what I find is that these teams do not usually report to the same leader,” Hadida explains.
“The database team may work closely with the BI team, but they’re usually separate from software development and interfaces.
“I think it’s that combination of having them all report under me—all of these teams meeting together on a regular basis, all of the managers for these teams and I strategically thinking ahead about how we can help each other out—those are the unique opportunities that I saw that led me to Memorial, and I feel like we’ve been accomplishing that,” he adds.
Hadida was born in Argentina. When he was three, his family moved to Venezuela and then made their home in Miami Beach when he was eight. He headed west to California to
attend college, first at the University of California, Santa Cruz, for his undergraduate degree and then to the University of California, San Diego for his master’s.
“I would say that my career kind of started there, in San Diego,” Hadida reflects. “One of the things I learned in the interim between my bachelor’s degree and my master’s degree is that employers were looking for job experience. So I decided that I would pursue a master’s degree and also look for some part-time work so that I could have some job experience.”
He found that experience at the San Diego Supercomputer Center.
“I did some really exciting work,” he recalls. “I learned how to be innovative at the Supercomputer Center. I learned that you can really accomplish anything by working together.”

Hadida spent thirteen years in California, but Miami Beach was his true home. So he moved back and got a job at the University of Miami’s Health System (UM), where he worked on a key project: the implementation of the Epic system.
“That was one of the most exciting projects I had been a part of,” he says.
“There was a lot of great energy—it was a really big project with a lot of people, and a lot of teams were involved. At the time, I was transitioning from being more of a software developer to being the manager of the interface team. That was a critical transition for me in my professional career.
“I was very much hands-on,” he adds. “I liked doing the work. I wasn’t necessarily thinking about going down the management track, but my boss at the




time, who I respected a lot, mentioned this possibility, the opportunity to be the manager for that team.”
His next stop was at Jackson Health System, where he lent his expertise managing the interface team.
“I brought with me a lot of my best practices, a lot of the experience I developed during those last three years at UM,” he notes. “I feel like I turned that team around from one of those low-performing teams to one of the higherperforming teams in that department. I’m very proud of that.”
As much as Hadida enjoyed that work, he saw his position at Memorial as an opportunity to innovate. One key project he’s led involved the interface team and implementing a new module for the Cloverfield interface engine, one that allows for storage of real-time messages in the Microsoft SQL server database.
“This is something that wasn’t possible before with Cloverleaf here at Memorial,” Hadida says. “When I read that this [module] is something that was available, I immediately saw some opportunities for my business intelligence team and my software development team. We pitched the idea, we got the support that we needed, and we introduced this feature. It’s called the message archive, or the message warehouse. And once we had these messages
stored in the SQL service database, all of a sudden my BI team and software development team were able to easily make use of it.”
Another project the business admission team is working on is a readmissions alert.

“We’re able to detect when a patient has just entered our emergency department and if they’ve been here during the last thirty or sixty days,” Hadida says. “So we can send an alert right away to let people know, ‘Hey, there’s a potential readmission here,’ and we can get involved and interact and intervene, and maybe learn some lessons about why they came back and what we could have done better during the previous admission, which also affects how we treat that patient now that they’re back.”
Since joining Memorial Healthcare System, Hadida has not been afraid to take on some tough tasks, including leading a strategy for data structure and centralization.
“That admittedly has been a challenge for us in our organization,” he notes. “We’ve become very decentralized when it comes to data, and this is something that I see often our industry. In the information age, everybody needs access to data; everybody has a lot of reports and analytics that they need to do.”
For example, Memorial Healthcare System has three business intelligence teams—one in IT, one on the business side, and a population health BI team. Hadida explains that the three directors have been working closely to centralize

“We’re developing this innovation center in our office base because of the new normal now. A lot of people are working from home these days, so we’re repurposing our physical space, whether it’s a patient room or a doctor’s office, that were mocking up with new technologies and devices.”
data and standards, with the goal of everyone reporting out of the same place and working with the same numbers.
Recently, MHS made a strategic decision to leverage the Epic Caboodle Data Warehouse as its single enterprise data warehouse (EDW). For Hadida’s BI team, this meant migrating away from its homegrown EDW and onto Caboodle. They started this migration by focusing Epic data sources first. All three BI teams are now heading in this direction, and Hadida notes that these efforts have been going well thus far.
In looking to the future, Hadida is excited about Memorial Healthcare’s plans to create an innovation center, which reminds of him of a time much earlier in his career at the San Diego Supercomputer Center.
“I feel the same creative juices flowing with our innovation center,” he says. “We really want to be thinking ahead. We want to be experimenting
with very new technologies and bringing some modern-day solutions to our healthcare systems.

“We’re developing this innovation center in our office base because of the new normal now,” he continues. “A lot of people are working from home these days, so we’re repurposing our physical space, whether it’s a patient room or a doctor’s office, that we’re mocking up with new technologies and devices. I’m very excited about that and I feel my teams are going to be a big part of that.” AHL
Applied Reliability Lab (ARL) is a data analytics firm supporting organizations’ transformation into a data-driven culture. This transformation takes more than technology; transformation requires changing mindsets, attitudes, and habits by embedding data into the fabric of the organization. People want to use data and encourage others to do the same. We support this effort with custom training and consulting efforts.
We love solving problems that lie on the boundary of theory and the unknown.
Custom Visual Analytics training


Consulting and Coaching
Identification and elimination of repeat unintended eventsRoot Cause Analysis (RCA) Logic Trees to identify Physical, Human, and Latent Roots.
info@arl.us
Building trusted data cultures enables humans to solve their most challenging problems.


Amy Sellars brings her background in education to her legal work at Cardinal Health, solving cases by using data to tell a more complete story


 By Maggie Lynch
By Maggie Lynch
between teaching and litigation. Amy Sellars, assistant general counsel and director of the Discovery Center of Excellence at Cardinal Health, found that harmony and calls it “the search for the truth.”


Sellars began her career in the classroom, teaching English and theater to high school students. She initially pursued a career as a teacher of these subjects because she loves narratives. After a bit of “disenchantment” with the United States education system, Sellars began working for an education tech start-up, where she first felt the spark to pursue law.
The nonprofit was a company dedicated to improving teaching in Title I schools. Schools classify as Title I if 40 percent of the students they serve are below the poverty line, and these institutions are part of a federal program that provides funding. The company
Sellars worked for was also federally funded, and with that came a lot of reporting requirements.
“I spent a lot of time trying to figure out how all of our project managers and education subject matter experts were going to gather data, and how we were going to track that data and report on that data,” Sellars says about her time spent at the nonprofit. While this was not the role she intended to have when beginning her work there, she realized she had a talent for it.
“I also realized that data was telling stories,” Sellars adds, “that data made us rethink the things we thought we knew. When I went to law school, I really thought I was going to go into education law—I thought I was just extending the place that I started.”
Instead, Sellars found that there were many narratives to tell and problems that data could solve as the driver of these stories. After taking her first course in electronic discovery, or e-discovery, she says, “I realized this was an incredible combination of my love of stories and my interest and capability with data and databases. And that was it. I didn’t look back at education law again.”
There is a strong chord

 Amy Sellars Assistant General Counsel and Director of the Discovery Center of Excellence Cardinal Health
Amy Sellars Assistant General Counsel and Director of the Discovery Center of Excellence Cardinal Health
Yet what Sellars learned during her time spent in education was not for naught. “Being a teacher means that you’re sort of unflappable. When you’re staring down thirty-five high schoolers who don’t really want to talk about Romeo and Juliet , you become able to survive almost anything, I’d say,” she says, laughing. “So [teaching] has taught me that you have to rely on your passion, especially when you are talking about something that someone may not understand.”
Being unflappable is an imperative skill for a litigator, but as an attorney in the healthcare industry, where things are constantly changing, the flexibility learned at the helm of a high school class has also given her a leg up. “When you talk about flexible— when you talk about how we bounce back


when things don’t work out—there is no better training for dusting yourself off and starting over again than being a teacher,” Sellars says.
In healthcare, this knack for trial and error enables evidence-based learning and processes. So Sellars’s entrance to the industry was an easy transition. Cardinal Health is a multinational healthcare services company, and according to Sellars, “a healthcare enablement company.”
As the director of e-discovery, she states that her team’s focus is often on litigation over product liability or litigation between companies that Cardinal works with regarding potential or possible contract disputes. Her work allows Cardinal to use data to make more strategic, better-informed decisions regarding ongoing litigation, as well as recognize opportunities for system enhancements.
With e-discovery, Sellars and her team are able to find any electronic data that may be used as evidence in a case. “If there’s no evidence, the court will say,
“When you talk about flexible— when you talk about how we bounce back when things don’t work out— there is no better training for dusting yourself off and starting over again than being a teacher. ”
‘We have to throw this case out.’ It would be the same with any electronic information. In our case, the smoking gun might be in an email and not fingerprints on a weapon,” Sellars explains.
She states that her team’s goal is to forensically reconstruct a narrative from the past through records of communication, as well as documents and purchase histories. “When you have any kind of dispute or investigative concern, you’re going to want to go back and look at the electronic record to figure out what really happened,” Sellars notes.
This is done by sorting broad swaths of text data into buckets using algorithms that enable concept clustering. With this tool, Sellars says, “We can very quickly pull these groups of documents that are similar together in a way that we’ve never been able to do internally before.”

With the ability to search through documents and reconstruct a story of what may have occurred, Sellars and Cardinal are able to more easily resolve cases and better support Cardinal employees and patients.
Yet Sellars says e-discovery is not the most imperative skill to have in healthcare law. Collaboration is. She says, “I think much collaboration is required in law and in healthcare to maintain balance and make sure you’re getting the right mix of expertise in any given dispute or question.”



With innovations happening rapidly in both healthcare and law, experts like Sellars need to ensure their teams are always on the same page—a skill that is especially important during the most tumultuous times, as 2020 evidenced. She says, “At the same time that we’re growing apart, the need for us to collaborate is growing.” AHL
Consilio : “Amy Sellars is known as a stalwart leader in e-discovery, technology, and legal operations, complemented by her genuine character and sincere passion for strong ethics, fairness, and humanity. We at Consilio are honored to be a longtime partner to her and her team.“ –Nancy Daniel, Senior Director




at Kentucky-headquartered medical provider Kindred Healthcare, Meredith Booth has realized that not everyone derives the same joy from compliance that she does. However, as the organization’s chief privacy officer and division vice president of compliance, Booth has made it her mission to change her colleagues’ perception.
“I’m not trying to make their lives harder,” Booth says with a laugh. “My goal is to make privacy— and compliance overall—a little bit more human and to let everybody else in the organization know that we’re here as a resource. We want to help answer questions and be that sounding board if they have any uncertainty about something.”
For Booth, employee education goes hand in hand with the effective protection of private information—whether that of Kindred’s patients or its employees. By instilling the importance of

privacy and compliance in individuals across the organization, Booth has facilitated the adoption of a more proactive attitude toward both issues. Furthermore, she has built a foundation ready to withstand the challenges of the digital era, all while propelling Kindred and its patients toward a brighter future.

When she first arrived at Kindred in 2016, Booth oversaw a hotline set up within the compliance department to receive tips about potential areas to investigate. “While it was an important part of the compliance program, it was only one part of it,” she says. “I’ve been fortunate enough to have taken on more responsibilities over time. Now, I really get to look at the big picture of our compliance program and see what we’re doing and whether we’re being effective.”
As the scope of her role broadened, Booth brought herself up to speed on previously unfamiliar topics. She delved into federal and state privacy regulations and gained a stronger appreciation for the auditing process. She then began applying her increased knowledge base to enhance Kindred’s compliance program and overall operations.
“My thought has always been to look at what we have to see what’s working and where we can improve,” Booth says. “We do strive for best practice, and we do want to be as secure of an organization as we can be. We want to make sure that our patients feel like their information is going to be secure when they come to us and that our employees understand their information is afforded the same protection.”
Booth closely monitors trends within Kindred and in the industry at large so that she can keep employees up-to-date. She puts together training units and educational pieces around emerging issues throughout the year as a supplement to the annual compliance training that all Kindred employees receive. “Privacy is one of those fields that until someone gets a feel for it, they might not understand why it’s so vital. We want our employees to understand the ‘why’ behind everything—why it is so important that we protect private information,” she explains.
Beyond teaching employees about privacy and compliance, Booth emphasizes clear and efficient communication.
“As soon as a patient says that they would
like a copy of their medical record, we need to know,” she says. “The goal is always to provide exemplary patient care and an exemplary patient experience. If a patient has had great bedside care but they never hear anything about this request, it will impact their overall opinion of Kindred.”
With electronic medical records and digital healthcare services becoming more common, Booth believes that timely responses to patient requests are more critical than ever. At the same time, increased digitization at Kindred has presented new challenges for her department, as have new government regulations pertaining to digital privacy.

“We’re always trying to figure out how we can respond to changes and how we
Meredith Booth Chief Privacy Officer and Division VP of Compliance Kindred Healthcare
can anticipate the requests that are going to come as a result,” she elaborates. “We partner a lot with our security department to find out what they’re seeing as far as cyberthreats. Then we look at how we can protect everyone without locking the system so much that employees can’t use it.”
Booth has encouraged implementing multifactor and single sign-on authentication and similar strategies to bolster various system/ application security without overburdening Kindred employees. She also turns to trusted external parties, such as healthcare data and technology company ProviderTrust, to help navigate the ever-shifting industry and regulatory landscape.
“ProviderTrust has been a great partner from the beginning,” she confirms, highlighting the company’s assistance with licensure and credentialing matters during the COVID-19 pandemic. “If they heard about a different waiver or a state coming out with a change in their requirements, they were really helpful in passing on the information. And if we saw something come up on our end, we could fact-check with them to see if we had missed anything.”
“Meredith has an unwavering commitment to ensuring only the most qualified employees are caring for Kindred’s patients, which includes partnering with ProviderTrust,” says Donna Thiel, chief
compliance officer at ProviderTrust. “Immediate notification of any employee who has a licensure issue or is excluded by a state or federal governing body allows Meredith to take immediate action to protect Kindred’s patients.”

With organizational partners and employees alike doing their part to aid in Kindred’s compliance efforts, Booth hopes to grow even more adept at preempting issues before they arise. Likewise, she seeks to continue creating a seamless patient experience by matching the caliber of Kindred’s medical care with a prompt and respectful completion of record requests.
“If we are the last impression that someone has of Kindred, we want it to be a good one,” Booth emphasizes. “We want patients to understand that compliance/privacy is here to protect their information, but we are also here to provide it to them as soon as they request it.” AHL

“My goal is to make privacy—and compliance overall—a little bit more human and to let everybody else in the organization know that we’re here as a resource.”
Every step executives take on their career journeys is pivotal to achieving their current successes. Along the way, individuals accumulate technical skills, foster relationships, and develop the leadership acumen that has turned them into pioneers of the industry.
46. Greg Duckett Baptist Memorial Health Care Corporation 52. Bernie Rice Nemours Children’s HealthIn thirty years at Baptist Memorial Health Care Corporation, Greg Duckett has helped rebuild relationships, adapt to change, and strive for excellence
By Billy YostGreg Duckett still remembers the faculty advisor at Oberlin College who recommended he drop out and attend trade school instead. He was attending the university on an academic scholarship, choosing that route over other schools that had recruited him for his football prowess. (He would still go on to play football at Oberlin—so well, in fact, that he was recruited to play at the semipro level.)
“I wanted to put my academic career first and try to avoid getting that ‘dumb jock’ label attached to me,” Duckett remembers. Yet he was still looked down on by his advisor. “The upside of that conversation was that it made me more committed than ever to proving him wrong.”
And Duckett did. He graduated from Oberlin, attended law school at the University of Memphis, and served there as student bar governor before ultimately being elected the university’s only African American student body president. He worked on behalf of Senator Al Gore and served an integral role in Mayor Richard Hackett’s administration as the city’s youngest and first ever African American chief administration officer. In 1992, he came to Baptist Memorial Health Care Corporation, where he is now senior vice president and chief legal officer.
“Baptist was the only major hospital in the community that did not have in-house legal
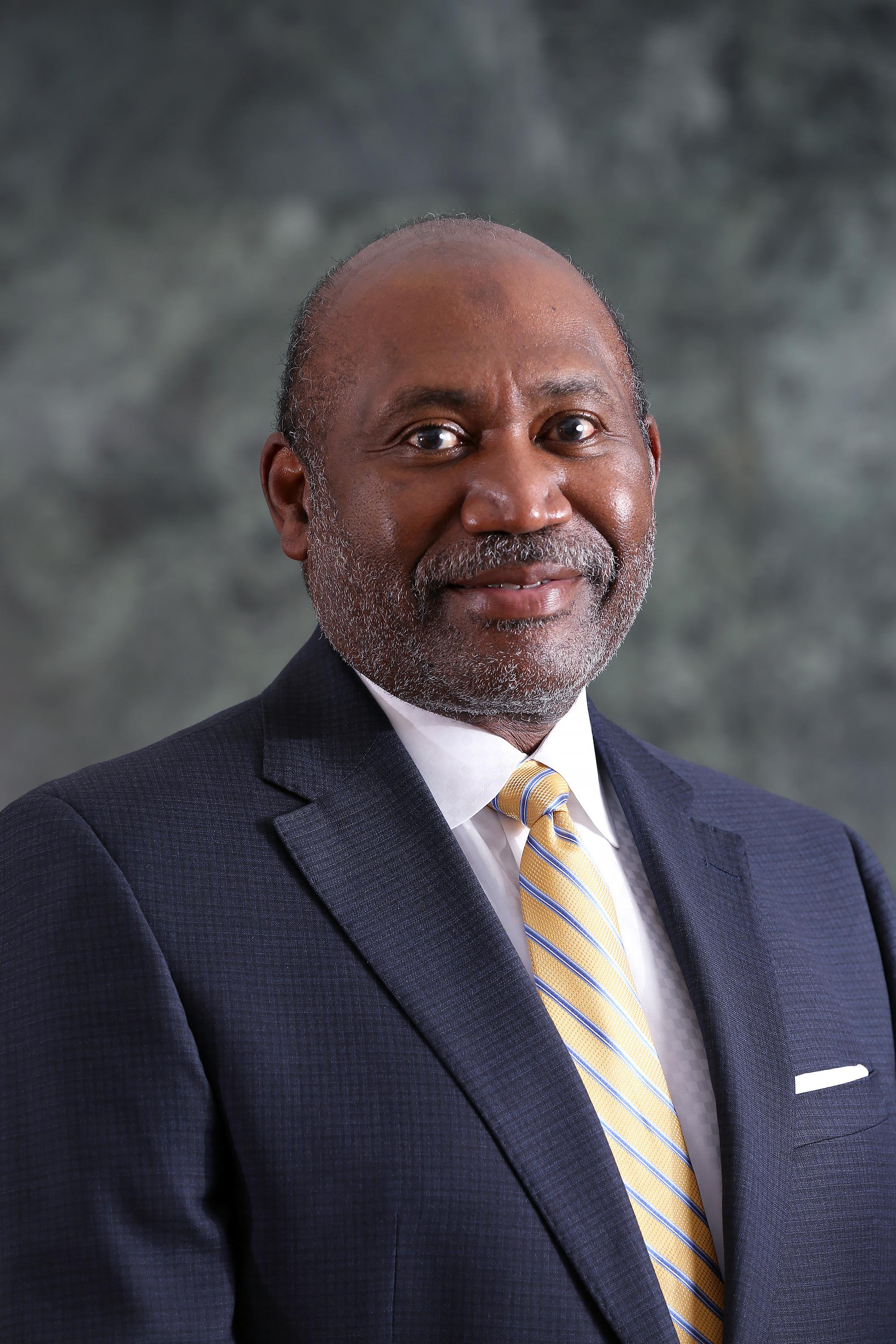 Greg Duckett
SVP and Chief Legal Officer Baptist Memorial Health Care Corporation
Greg Duckett
SVP and Chief Legal Officer Baptist Memorial Health Care Corporation
counsel at the time,” Duckett remembers. “I started as a vice president of government and community relations, but in speaking with the president and vice president, I shared that it was my goal to move into the legal role.”
In just six months, risk management, corporate communications, and internal audit were moved to report up to Duckett. He was promoted to corporate counsel shortly thereafter. “For the first four years, the legal function was me, myself, and I,” Duckett says. And while it would be easy to call the rest history, that history is storied.
Welcome to the Industry
Duckett’s first serious challenge was the creation of Tennessee’s TennCare program, the state’s Medicaid “expansion” project. With just six months on the job and an orientation schedule requiring him to visit all of Baptist’s seventeen hospitals, Governor Ned McWherter announced his administration’s plan to convert the traditional Medicaid program to a TennCare waiver, pulling the government out of negotiating and, instead, handing that to third-party managed care organizations that would handle agreements between hospitals and physicians.
“Candidly, it was removing a slice of the pie that otherwise could have gone to providers, giving it to a third party, and I found myself new in an industry trying to negotiate multimillion-dollar arrangements,” Duckett recalls. “Even our CFO didn’t know the drop-dead price we could afford to take, so it was a scary time.”
The CLO says it was the baptism by fire that he needed to acclimate to the Tennessee Hospital Association and that would aid efforts to negotiate changes to TennCare several times over.
“As the chief legal officer at a major hospital system, Greg always has a lot of balls in the air when it comes to juggling important issues,” says David King, shareholder at Polsinelli. “But he always demonstrates a lot of skill and insight when digging into the details, asking the right questions, and determining the best course of action.”
Tennessee is one of sixteen states that have not expanded their Medicaid programs over the years, so Duckett’s early tribulations would help establish the conditions under which he’d be working for the coming decades.
Duckett has also been on the front lines of helping reestablish connections with the University of Tennessee (UT) medical system. A once vital partnership was strained during a large portion of the 2000s, when the university moved a significant portion of its transplant operations to Baptist’s area competitor.
“The university was able to get enhanced graduate medical education funding, and it created a twofold dilemma for us,” Duckett explains. “Having an academic appointment is a major accomplishment for any physician, and suddenly, we no longer could offer that opportunity. Secondly, we found ourselves unable to expand different departments in our own health system.”
But over the last year and a half, Baptist has developed a joint venture with UT as well as its competitor. It allows the entire emergency medicine program to move back to Baptist and bring about new developments in anesthesiology, neurology, internal medicine, radiation, and oncology. “We’re also looking to enhance our cardiology department, although it
“The upside of that conversation [with a faculty advisor who doubted my abilities] was that it made me more committed than ever to proving him wrong.”
Harris Shelton commends
Greg Duckett for his innovative leadership and dedication to Baptist Memorial Health Care Corporation. We are honored to work with Greg and the rest of the Baptist team and congratulate them on this well-deserved recognition.
Harris Shelton is a full-service, regional law firm with a focus on health care law including regulatory compliance, litigation, licensure, privileging, credentialing, contracting, patient safety, risk management, insurance, finance, and mergers and acquisitions.



is already the largest group in the city of Memphis,” Duckett says.
Baptist Memorial Health Care Corporation is the largest provider of physicians and practitioners in Memphis, and Duckett says that’s due in part to the ways in which the organization incorporates what he calls “comanagement agreements” into established metrics.







“We do not work on a standard work relative value unit [wRVU] model,” he says, “and so by establishing metrics typically around quality of care and other factors, both the physician and the facility have incentives aligned to those metrics.”
Pride Points and Chance


Duckett considers the renewed partnership with the University of Tennessee one of the proudest moments in his career, but given his thirty years at Baptist, there are many. After city politics intervened in the creation of a joint venture, the one thousand employees that Baptist thought it would be allocating to the health center were suddenly out of a job.
“We had to stand in an auditorium and let these people know things had changed,” Duckett says. “It was one of the hardest days of my life. But our former president Steve Reynolds made a commitment that we would find positions for every one of them. Thank God we were able to do so. Steve is an amazing leader.”
Unaware of what his next career move might be now that his time in politics had come to an end, Duckett saw the opportunity as a potential job interview. “After we met, Steve wound up calling me a week later,” he says. “I’ve done a lot of things out of happenstance in my life; it’s just worked out that way.”
harrisshelton.com



Reynolds comes up a lot in Duckett’s interview. It was only by happenstance that the two ever met. After Mayor Richard Hackett bowed out of a speaking engagement after losing a narrow reelection campaign, Duckett stepped in to fill the spot, which was celebrating the tenth anniversary of the creation of the Baptist Memorial Healthcare System.
Call it happenstance or call it fate. Duckett’s path has been guided by his unwavering belief that he can—and will—do great things. AHL
Harris Shelton has had the good fortune to work with Greg Duckett and the Baptist team for many years. We have tremendous respect for the experience, skill, and leadership he brings to the table in helping Baptist find solutions to its legal matters and achieve its healthcare objectives.
| NASHVILLE OXFORD | COVINGTON
“I’ve done a lot of things out of happenstance in my life; it’s just worked out that way.”
Polsinelli congratulates Greg Duckett, Senior Vice President and Chief Legal Officer at Baptist Memorial Health Care, for his outstanding leadership at Baptist Memorial and in the greater Memphis community.
As the Chief Legal Officer at Baptist, Greg has helped to foster the company’s reputation as one of the premier health care systems in the nation. He has worked during these unprecedented times to provide executive leadership with dedicated support on legal and strategic matters that relate to many aspects of the company’s mission to build stronger and healthier communities, while focusing on providing high quality health care to under-served, uninsured and vulnerable members of the Baptist community.
As one of the largest health care law firms in the country, Polsinelli is proud to partner with Greg and his legal team in support of Baptist’s mission. Our multidisciplinary team of health care attorneys provides a broad variety of services to our health care clients including mergers and acquisitions; clinical alignment strategies; regulatory compliance; and government and commercial reimbursement and disputes.
Am Law 100 firm with 900 attorneys nationwide 21 offices from LA to NY 170+ services/industries polsinelli.com
 The choice of a lawyer is an important decision that should not be based solely upon advertisements. Polsinelli PC, Polsinelli LLP in California.
The choice of a lawyer is an important decision that should not be based solely upon advertisements. Polsinelli PC, Polsinelli LLP in California.
CIO Bernie Rice considers technology’s role in impacting—and saving—lives at Nemours
By Donald LiebensonWhen you think of IT, you generally think of big-picture issues, such as compliance, data backup, and cybersecurity. But ask Bernie Rice, senior vice president and chief information officer at Nemours Children’s Health, what he finds the most meaningful about his job, and he will tell you it’s the little things.
For example, most adults might take a hospital room TV for granted. But to a child, Rice says, a working TV can be very important. “For children in pain or who are nervous about being in the hospital, it’s a distraction technique,” he says. “In addition, thanks to a TV interface we created, a child can change the color of the lights in their room. That may seem like a simple thing, but it helps the child feel they are in control.”
Even more gratifying, Rice adds, is that through his department, older children who are long-stay patients have participated in virtual graduations.
Nemours, a nonprofit organization, is one of the largest integrated pediatric health systems in the country, with two freestanding children’s hospitals. It cares for more than 480,000 children annually at more than ninety-five locations in four states.
Rice has been at Nemours for twenty-two years. In his current role, he manages all of the organization’s IT systems as well as information security and physical security for the company’s corporate enterprise. He and his team are responsible for the IT needs of its eight thousand employees.
“We’re unique in the pediatric world,” Rice says of Nemours. “A lot of people are familiar with different things about the company depending on where they are, whether it’s a small clinic in a Gulf Coast fishing village or the Nemours
Children’s Hospital in Delaware, our largest location.”
Rice joined the company in 1999 and worked his way up to CIO, the role that he assumed in 2008.
He came to Nemours from AnheuserBusch, where he started as an intern and became IT manager for one of the compa-
ny’s eleven breweries in his hometown of Jacksonville, Florida. “It was a nice seven years I spent there,” he reflects. “We spent hundreds of millions of dollars in modernization in the plant. But I was in
“In the military, you think about leadership having to deal with difficult situations. People tell me all the time how cool I am under pressure. It’s just part of that training.”
 Bernie Rice SVP and CIO Nemours Children’s Health
Bernie Rice SVP and CIO Nemours Children’s Health
my thirties with two kids—one eight and the other four—and I wanted to spend more time with my family. I saw this job for an EMR administrator for a local kids’ organization and I thought, ‘I can do that.’ It blossomed from there.”

Rice grew up in a blue-collar family and became the first of his four siblings to finish college and get a degree. He joined the Air Force out of high school, and he credits the military for helping him realize his determination to attend college.
The military, he believes, breeds better employees and employers. “The military really is a melting pot,” he says. “People come from different backgrounds and ethnicities, but you do learn to function as one unit. You develop a great camaraderie. The military also instills a sense of structure and process.”
Now, Rice leads a team of roughly four hundred people. At the risk of cliché, he says with a laugh, working with his team is what he likes most about his job. “Over the years, we’ve grown into a phenomenal IT team that really delivers,” he says. “A lot of people, like me, were hired at the start of the EMR project, and a lot of them are still here.”
The military also prepared him to become a leader. “In the military, you think about leadership having to deal with difficult situations,” Rice says. “People tell me all the time how cool I am under pressure. It’s just part of that training.”
To complement that leadership style, Rice trusts and relies on his team. “I manage according to competencies,” he says. “Some need a little less guidance, while others need some more. I’m a believer in ‘There’s a reason I hired you; now go do it.’ I depend on their expertise and give them the freedom to manage their areas. I tell people all the time, ‘Your career is in your hands. I give you opportunity; you’re the one who takes advantage or not. It’s up to them to make a difference. It’s the same thing I tell my kids.”
IT has evolved exponentially since Rice became the CIO in 2008. Currently, he and his team are working on moving Nemours’ systems to the cloud. “When I first came here, healthcare was well behind the times when it came to technology. In my early days here, someone would deliver printed reports to the different departments on a cart. Now, we’re a very advanced hospital system. We are closer to the patients than we have ever been. Our technology is right at their bedside.”
After more than two decades, observing the impact of his department’s work gives him the greatest satisfaction of all. “It’s not about helping a company make money or getting a product out the door,” Rice says. “It’s really helping shape people’s lives. In pediatrics, there’s a saying: ‘We’re not saving lives; we’re saving lifetimes.’” AHL
are proud to be part of the team that supports Nemours and all the children that they serve.
Denise Chamberlain is passionate about bridging the gap between finance and operations. As CFO, she empowers Edward-Elmhurst Health employees to work as a united front.
By Katie OltmannsPortraits by Gillian Fry

When it comes to landing her current role at Edward-Elmhurst Health (EEH), Denise Chamberlain describes herself as Goldilocks. “I’ve been in bigger places, I’ve been in smaller places—but this, this is home,” she says.
Edward-Elmhurst, ranked as one of the top healthcare organizations in the country by Watson, is where Chamberlain is now the chief financial officer. Her journey there, however, was not always a smooth one. Chamberlain describes her career path to her current state of success as bumpy, beginning with the pursuit of her undergraduate degree. “I was just clueless,” she says.
She dropped out of college after her sophomore year and found herself working as a secretary for a family-owned company, where she grew curious about their financial situation. “I got curious about whether or not my division was making money because nobody told me that. As secretary, I did all the billing and knew what we spent,” she says, “so I literally started tracking it and putting it together.” The owner, after discovering this, took a great interest in Chamberlain and her overall drive and encouraged her to go back to school.
Seven years removed from any formal education and with a family of her own, Chamberlain not only went back to school but graduated with honors and obtained her first job in healthcare at Arthur Andersen in Dallas. She worked her way up the ladder with CFO jobs at small to midsize businesses in the southwest, then moved to Vanguard Health Systems in Phoenix to fulfill a role that she considers to be the true catapult for the rest of her career.
It was there that Chamberlain quickly discovered not just her passion, but the
eureka moment behind so much of what she has built and is currently building at Edward-Elmhurst Health. Vanguard was a for-profit healthcare chain (subsequently sold to Tenet), which was an entirely new sector of healthcare for Chamberlain. “At a for-profit chain, the CFO’s job really is financial operations,” she says. “Most things I do now [at EEH] were done for me there. I really had one job: put together a budget and deliver it.”
But Chamberlain soon discovered that to properly construct the budget, she needed to go directly into the hospital and understand what drove the results she reported on. She quickly understood there was a disconnect. “The level zero I knew about operations matched the level zero of what they knew about finance,” Chamberlain says, laughing.
“As with many health systems, we are close to the largest employer in town. We felt it was important to keep people working.”
“Neither one of us knew anything about each other.”
The hospital was losing money, and Chamberlain was brought in to turn things around. So she promptly began focusing on fostering the relationship between finance and operations, encouraging them to teach one another and work together—and to be a united front. The hospital went from losing money to having a 10 percent margin in her first three years there, which inspired the idea for her book, Money to Care: Hospital Finance for Nonfinancial Hospital Leaders.
It was in recognizing the need for nonfinancial people to understand finance that she found her second calling: teaching. Chamberlain now has her master’s degree in adult education and training and teaches classes to healthcare professionals as much as she can.
After Vanguard, her path led her to Illinois in a sort of happy accident. At the time, she was working for an interim company with CFO placement and was temporarily assigned to Edward-Elmhurst Health. Originally, she was solely interested in the role because she had family nearby, and this role gave her the chance to be close to them. After being there for just one month, she fell in love. She was ultimately asked to transition to the permanent role of CFO.
At EEH, Chamberlain has implemented staunchly successful operating improvement initiatives—especially when it came to bridging the gap between finance and operations. When she arrived, there was essentially no infrastructure for this connection, so she emphasized the importance of baking initiatives into the budget.

So far, she has assisted in developing teams, sending monthly reports to leadership, and being the voice for finance at enterprise-wide town halls. She is also part of monthly operation reviews in which all departments meet to discuss their finances, and all department heads are very integrated in their budget, she says.
“It’s not just that the finance department does it all and pushes it out,” Chamberlain notes. “We have really upped the game here of connecting finance and operations. It’s very transparent.” According to Chamberlain, the
whole enterprise now helps with what she calls “the hill, the hole, and the dirt.”
“The hill is that you always want to get better. The hole is inflation, new spend, all the things that will take away from our performance compared to last year. I have to somehow get from the bottom of the hole up to the top of the hill—and that’s with dirt. The whole enterprise is involved in identifying how big the hole is and where we are going to get the dirt,” Chamberlain explains.
“Denise’s vision and leadership has made working with Edward-Elmhurst over the past year a truly unforgettable experience,” says John Talaga, executive vice president of healthcare at Flywire and a close partner of Chamberlain’s. “Her laser focus on creating a better financial experience for her patients has led to a dramatic transformation in the types of consumer-friendly solutions they offer and the ways that they engage patients across their healthcare journey.”
Chamberlain is also responsible for moving forward with Edward-Elmurst’s Enterprise Resource Planning (ERP) software as it transitions to the cloud, which began before the COVID-19 pandemic. The health system was about to finish on-site demos with vendors when the pandemic shut processes down.

“All nonurgent capital was put on pause,” says Chamberlain, “but I made the decision that we needed to keep moving forward with this ERP selection. Everyone else in the country was basically in the same place we were, to move to the cloud . . . and so I thought that we would get a bit of an edge by continuing this process while many others went on pause.”
After ultimately deciding on using Workday to help with the process, EEH is now in its eighteen-month journey of fully implementing this new system. As for the rest of its experience with COVID19, Edward-Elmhurst was fortunate, says Chamberlain, due to meticulous and thoughtful finance management.
“We were blessed to have a year’s cash on hand,” she says. “There wasn’t a panic from a financial standpoint as our volumes plummeted and elective services stopped. From a cash flow perspective, we were still fine.”
Chamberlain emphasizes that the organization’s strong commitment to
“For me, it’s not about focusing on the money. It’s about doing the right thing, and the money will come. And I get the opportunity to live that personal mission in terms of how I view healthcare and how we work together.”
Impact Advisors looks forward to continuing to partner with you to innovate and drive meaningful change with measurable impact.

Impact Advisors’ experienced team of professionals is committed to helping our clients solve their toughest challenges with patientcentered, value driven outcomes that consistently exceed expectations.

UCB is a long standing strategic partner prepared to assist healthcare providers with the demands of revenue cycle management. Over our 60 year history of patient engagement, UCB has perfected our process to ensure both our clients and their patients receive best in class care. Our solutions include:







· Self-Pay Outsourcing
· Presumption Charity Analytics




· Medicaid Eligibility/Advocacy

· Insurance Resolution
· Bad Debt Recovery


Connect, download, join the conversation at Impact-Advisors.com









UCB: Serving the healthcare industry on a national level, one client at a time. KELLY





Kefielder@ucbinc.com







its community was a crucial aspect to maintaining as much normalcy as possible. EEH met with employees weekly to reassure them that their jobs were not in jeopardy. In fact, the company didn’t lay off any employees during even the most tumultuous times.
“As with many health systems, we are close to the largest employer in town. We felt it was important to keep people working,” she says. While a lot of calculated moves were behind their steadiness during the pandemic, every move they made in terms of financial stability was made with the priority being that EEH protects its people first—a commitment that’s also shown in its mantra: safe, seamless, and personal.
“Everything we do comes back to, ‘Is it contributing to being safe, seamless, and personal for our patients?’” Chamberlain says. “One of the things that makes us unusual is that our system CEO and our CEO/president of one hospital are both nurses. And consequently, everything starts with the patient and the nursing teams and support teams that are taking care of those patients.
“That’s part of the reason I love being a CFO here,” she adds. “For me, it’s not about focusing on the money. It’s about doing the right thing, and the money will come. And I get the opportunity to live that personal mission in terms of how I view healthcare and how we work together.”
National, and even global, forces have an unmistakable impact on an executive’s work. Whether it’s a legislative change or an industry-disrupting technological breakthrough, executives must constantly adapt their business strategies to keep their companies thriving.
64. Steven Begley YPrime 68. Richard Rew Luminex 72. Suresh Namala SeagenYPrime’s clinical trial data is safe
By Billy YostWhen Steven Begley was recruited to join YPrime in 2013 as the director of quality assurance, he was informed that four external audits of the quality assurance (QA) program had been previously unsuccessful. Begley, three promotions later and currently serving as chief privacy officer and senior vice president of quality and compliance, has since conducted twenty-five-plus audits a year of YPrime’s division—and not a single one has missed the mark.
It’s a valuable snapshot into what Begley has been able to bring to YPrime over the past eight years: extensive quality and compliance experience in the clinical trial and data field for organizations ranging from startups to huge companies working on the cutting edge of medical innovation.
Since coming to YPrime, Begley has built the company’s QA group from the ground up, and as the role of cybersecurity and data privacy grew exponentially through the 2010s, he’s helped spearhead security efforts that are second to none.
“I think I imagined there being more here when I first arrived,” Begley says, laughing, of his first days at YPrime. “But I sort of had to redo the things that had already been done and really work to develop a baseline quality system. Flow charts were the standard operating procedure here, and that needed to change quickly.”
Begley spent the first four to six months of his new role designing and building out YPrime’s quality
 Steven Begley Chief Privacy Officer and SVP of Quality & Compliance YPrime
Steven Begley Chief Privacy Officer and SVP of Quality & Compliance YPrime
“The more relationships you’ve built, the more you can go through direct channels to have conversations. The more connections you make, the more people understand that we’re all in this together .”
system—one he now continues to incorporate new pieces into, including a document management system. Currently, the SVP’s team is in the process of developing and implementing an automation test suite for YPrime’s testing group.
Over the years, Begley has helped move the organization away from an almost exclusively paper-driven company to a fully electronic one. Outside partnerships have also helped YPrime continue to do what they do best while letting those with specialized niches handle the rest.
“We were controlling everything because we had servers in our data centers,” Begley notes. “When those would go down, we had to have physical IT staff on-premise. We have been able to eliminate some of those necessities and let our partners, Microsoft in particular, manage it because they have the expertise. We’ve just seen our whole quality system greatly improve.”
The SVP says that moving away from basic data centers and into the cloud environment has helped make him more of an evangelist for the clinical trial world.
“As we transitioned to the cloud, I was able to go to industry conferences and talk about utilizing all the benefits that cloud infrastructure offers,” Begley explains. “On-premise was such a big issue for the pharma world, but we’ve been able to convince our customers that having a third party manage that hardware for you is the optimal solution.” YPrime developed an enterprise agreement with Microsoft that has continued to pay dividends and drive business forward.
When Begley joined YPrime in 2013, cybersecurity was not the hot topic it would soon become. “But toward 2017, I really began to do a lot more homework on the cybersecurity front,” the SVP says. Since that moment, the drive to build a world-class cybersecurity system hasn’t stopped.
Because one of YPrime’s primary products is eCOA, they are required to have security infrastructure not only in terms of website management but also for handheld devices. “We have custom-made tablets that allow us to control security not just when they’re in our
possession but when they’re in transit anywhere around the world,” Begley explains.
YPrime is active in supporting clinical trials across the globe, and along with the GDPR (General Data Protection Regulation) protocols, they also have had to comply with China’s Human Genetic Resources Administration (HGRAC) requirements since they came into effect on July 1, 2019.
“We needed to be able to encrypt data in transit as well as at rest,” Begley explains. “We’ve implemented some automated features that allow us to automatically remove access so the devices weren’t exposed beyond their need for an access point.”
Yet again, Begley says third-party audits have been crucial to building out YPrime’s security protocols. “I think third-party audits are something every company should do,” the SVP says. “You are always going to have blind spots and because you’re so close to it, you’re going to miss them.” YPrime even employs “white hat” hackers to probe the company’s security for breach potential.
YPrime also secured cybersecurity insurance in 2020 to account for the continually escalating cyber and ransomware attacks. “It’s really not a matter of if, but when you’re going to be hacked,” Begley says. YPrime also has backup offsite storage that is not connected to its network, which gives it the ability to quickly restore its system in the event of an outside attack.
While a pandemic may have slowed down large portions of the world, it’s only escalated activity on the cybersecurity front. “We’ve seen the number of malactors and ransomware attacks continuing to creep up,” Begley says. “We continue to secure our infrastructure, and we’ve created more segregation in our digital environments to prevent malactors from moving laterally through our networks.”
In building out a best-in-class security environment, Begley says he’s learned it’s imperative to develop partners across the company, and those partners shouldn’t always be department leaders—though that certainly doesn’t hurt. “The more relationships you’ve built, the more you can go through direct channels to have conversations,” Begley says. “The more connections you make, the more people understand that we’re all in this together.” AHL
While healthcare workers heroically labored on the front lines of COVID-19, an attorney like Richard Rew at Luminex worked behind the scenes to bring the first testing products to market
By Russ KlettkeBefore COVID-19 vaccines were made and distributed, medical device companies that could make testing kits were among the first segments of the healthcare supply industry of critical importance during the pandemic. As hospitals began to fill up in hotspot areas, the worried well—frontline healthcare workers among them— wanted to know if they or the people closest to them were infected.
Richard Rew, former senior vice president, general counsel, and chief compliance officer at Luminex Corporation, was right there in the thick of it. The company had the capabilities for making and distributing some of the PCR (polymerase chain reaction) tests, releasing its first shipment in early March 2020 and a few variations thereof in the months that followed.
“The federal government’s emergency use authorization made it easier,” says Rew. The type of test they initially released was the PCR type, detecting the presence
of the viral RNA that appear before antibodies form and patients’ symptoms present—which was highly sought after, particularly early in the pandemic. “We had the expertise and respiratory panels, which tests for other respiratory diseases to rule out other causes.”
To be clear, there were bureaucratic issues with the government’s response at that point. Private sector companies such as Luminex, ready and quite willing to go into production ASAP, were stymied then by a lack of coordination between different agencies that are charged with epidemic surveillance and solutions.
So once that was overcome, the company had to ramp up production quickly, facing other sets of regulatory and legal hurdles. Pandemic notwithstanding, it was all in a day’s work for the Luminex legal team.
It helped Rew that this wasn’t his first medical devices company, and it probably won’t be his last. In the summer of 2021, the company was acquired by DiaSorin,
an Italy-based, global diagnostics life sciences company, leading to the elimination of his position due to redundancy.
He was intimately involved with the merger—providing counsel to the board of directors, shareholder votes, and the like—and in this international transaction, he also dealt with issues around CFIUS, the Committee on Foreign Investment in the United States. The Committee is how the federal government reviews mergers of this nature as they might affect national security.
Given that Rew lives in Austin, Texas, he’s confident he’ll find his next engagement without having to move. The city has no fewer than sixty-two biotech, pharmaceutical, and life sciences companies based there, all of which exist in the high-stakes—and highly regulated— healthcare industry.
The coronavirus wasn’t even the first novel infectious disease he has worked with. The Zika fever epidemic, which first surfaced in 2015, was on Luminex’s radar such that the company performed preliminary research and regulatory work.
As a leader, Rew has a strategy that includes choosing people who “have more talent than me,” as he puts it. “I’ve hired a lot of future general counsel. Not many people will turn down a medical device company job in Austin. The city is booming with lots of sophisticated work. I just try to give them the opportunity to do sophisticated things, to grow their skills.”
Reflecting on the size and diversity of the health sciences sector in the Texas
capital (also home to the University of Texas), he also notes that the vibrancy of the city is attractive to young professionals, providing a healthy talent pool from which to draw ambitious attorneys.
As for the kinds of things he is able to teach them, he advises, “You have to be a meaningful member of the business.” He’s also served, as do many in the general counsel position, as the corporate secretary—by definition, the person interpreting and recording
“I’ve hired a lot of future general counsel. . . .[Austin] is booming with lots of sophisticated work. I just try to give them the opportunity to do sophisticated things, to grow their skills.”
the decisions in board meetings. “You have to know what legal guidance they [board members and C-level executives] need, and understand the relationships between them.”
But it’s also important in healthcare for the legal team, from top to bottom, to keep an eye on the regulatory environment as they advise senior management. “Keep in mind the Department of Justice prosecutes executives,” he says. Things to watch for include antikickback statutes, anything from the Food and Drug Administration, misbranding of
products, and violations relating to the Foreign Corrupt Practices Act.
While many attorneys in healthcare begin their careers in the health sciences, Rew says it’s not entirely necessary, citing himself as an example. His best advice is to, like him, find an industry that is interesting. “It helps to like what you’re doing and to like the people you work with,” he says. “Hard work and the issues you deal with are not so bad if you like the industry.”
Living in Austin, however, might also help. AHL
DLA Piper is proud to recognize the accomplishments of Richard Rew and Luminex.
For over a decade, we’ve partnered with Luminex to help empower labs and deliver transformative solutions. We salute Richard’s steadfast commitment to advancing healthcare by accelerating reliable, timely, and confident answers.

Suresh Namala uses his tech skills to help scientists in their quest to develop transformative, life-saving cancer medicines
By Zach BalivaOne big misdiagnosis changed Suresh Namala’s life and set him on a whole new career path. Namala was thriving as a technology director for Expedia when ongoing pain sent him to the dentist. That’s where he heard that dreaded word: cancer. The talented professional and father of a young infant examined his priorities, organized his finances, and started to get his affairs in order. One month later, Namala received some surprising but welcome news. What the dentist had found was not cancer, but another easily treatable condition related to stress.
Namala had always been purposeful with his career choices. In fact, it was a passion for exploration and travel that motivated him to apply at Expedia. As he
pondered his own cancer scare, his mind returned to his native India, where he had visited his dying grandfather in the intensive care unit. Namala recalled how the clinicians, equipment, medicines, and devices gave his family hope. As that memory lingered in his brain, the University of Nebraska–Lincoln MS and MBA graduate had an epiphany.
“I knew I could use my technology skills and work experience to make a difference in healthcare,” he says. “And I decided to find a job supporting a company that was developing medicines to help take care of patients.”
In the following days and weeks, Namala scoured the internet and mined his personal contacts for professional networking and career opportunities. But he
 Suresh Namala Executive Director of IT Security, Governance, Risk & Compliance Seagen
Suresh Namala Executive Director of IT Security, Governance, Risk & Compliance Seagen
“I knew I could use my technology skills and work experience to make a difference in healthcare . And I decided to find a job supporting a company that was developing medicines to help take care of patients.”
wasn’t looking for any job—he was specifically looking to step into a leadership-level technology role at an impactful healthcare or life sciences company.
Before long, Namala found an opening at Seagen. The biotech company, with headquarters in the Seattle area, exists to “discover, develop, and commercialize transformative cancer medicines,” and is known for the antibody-drug conjugate (ADC) technology that powers most of its approved medicines. As Namala researched the company, he knew he had found a match.
“Seagen makes life-saving cancer medicines, and they needed someone to lead the team that helps keep the company’s IT systems safe, secure, and compliant. I knew it was the golden opportunity for me to combine my skills and passions,” he says. Namala applied, and in 2020, he stepped in as the organization’s executive director of IT security, governance, risk, and IT compliance.
It’s an important role for a company at the frontlines of the fight against cancer. Namala leads a team of programmers and engineers. Together, they are responsible for IT security, IT compliance, governance, and risk. “Strong IT teams are critical for biotech and pharmaceutical companies because we want our researchers and scientists pursuing the innovations our patients rely on for care. We do our work so they can focus on their work,” Namala says.
Seagen’s ADC technology targets and attacks cancer cells. Unlike traditional chemotherapy, these antibodies specifically target certain proteins that are found on the surface of tumor cells.
That makes the intellectual property behind ADC a valuable trade secret that Namala must protect. He and his team have performed advanced threat modeling and implemented industry-leading cybersecurity measures to prevent attacks from hostile intruders looking to penetrate Seagen’s firewall and steal proprietary information.
Despite these steps, his team often detects attacks and other hacking attempts designed to breach the network. Because many incidents originate through phishing emails, the department has launched an internal awareness campaign so Seagen employees know how to respond to suspicious emails.
Namala’s team is also building important compliance and risk management functions. For compliance, it’s using Good Practice Guidelines & Regulations, a risk-based program that provides evidence for relevant audits and contributes to the department’s overall mission of patient safety, product quality, and data integrity.
Although Namala has logged twenty years in advisory, security, privacy, IT compliance, and IT operations, he had never before worked in the complicated healthcare space. Previously, he held positions at the University of Nebraska, the Nebraska Supreme Court, Deloitte, Microsoft, and Expedia. Namala says that mentors in his early career at Microsoft and Expedia and supportive colleagues at Seagen prepared him for and helped him navigate the transition.
“Companies may shape you, but people make up those companies. Relationships matter,” he says. At Seagen, Namala found willing guides and took professor-led courses to learn more about biotechnology. The new knowledge helps him better understand the company as he and his team ensure it remains a safe and compliant enterprise as it expands globally.
Seagen is growing. At the start of 2020, the company had three approved medicines; now, it has four. Namala is maturing IT security and IT compliance measures and getting the right tools in place to help Seagen scale. In doing so, he has a new lease on life and the chance to make an impact in a new industry.
“I don’t even feel like I’m at work anymore,” he says.
“I don’t have a job . . . I’m on a mission.” AHL
Awake Security is proud to partner with Suresh Namala and Seattle Genetics on their cybersecurity objectives. In Suresh’s words, “Awake Security and their managed services have significantly enhanced our detection capabilities, enabling my team to focus on additional areas of the business that previously could not be attended to. Awake’s artificial intelligence is key to the security of our environment because it highlights malicious traffic patterns and speeds up response times.” Read more at awakesecurity.com.
Dr. JoAnn Wood reflects on the importance of being present and supportive as CMO of Deaconess Health System
By Billy Yost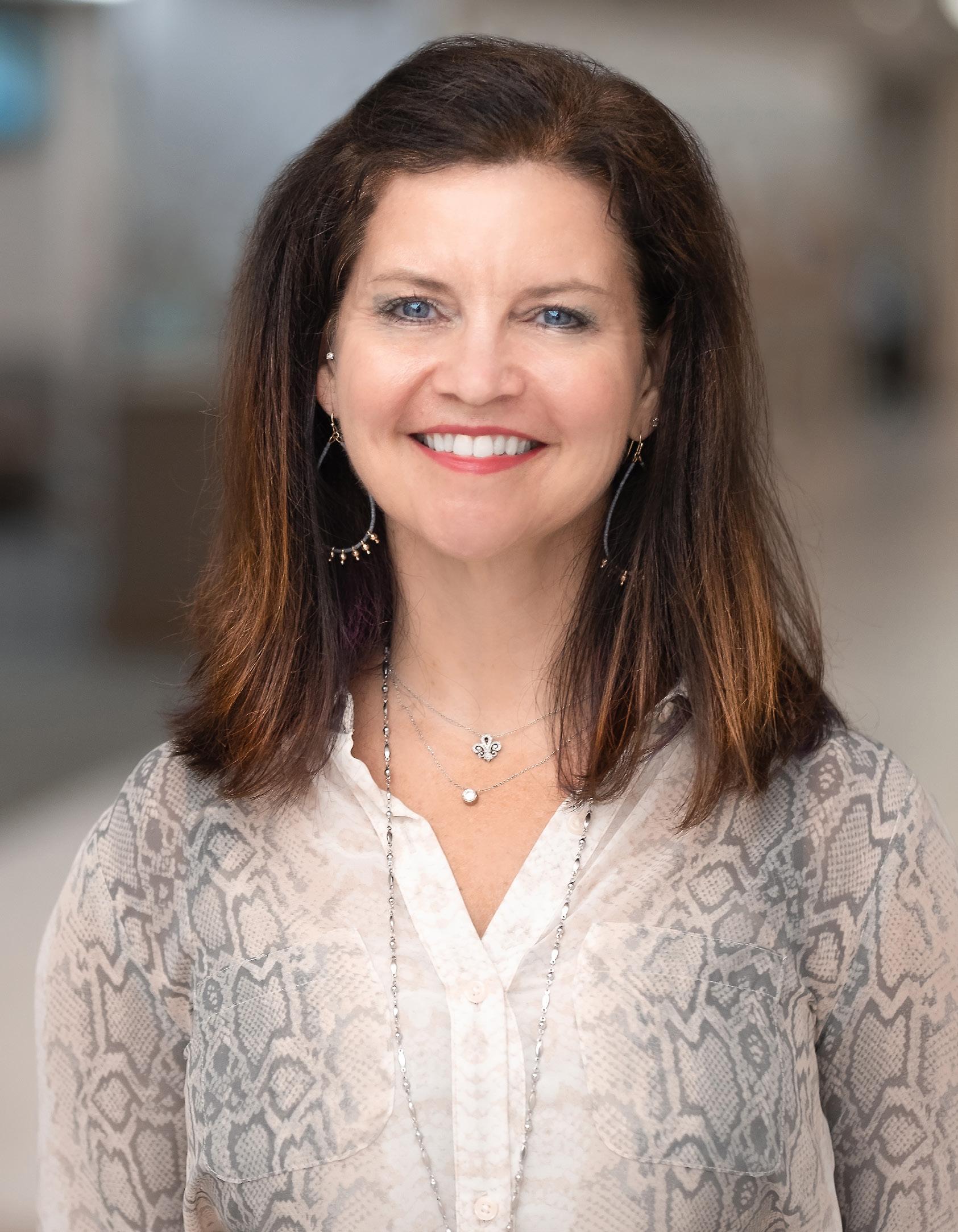 Dr. JoAnn Wood VP and Chief Medical Officer Deaconess Health System
Dr. JoAnn Wood VP and Chief Medical Officer Deaconess Health System
When chief medical officer at Deaconess Health System Dr. JoAnn Wood reflects on the well-being of the physicians and caretakers whom she’s tasked with overseeing, it’s not hard to pick up on an understandable sense of frustration. The health system continues to push back surgeries and elective procedures due to the ongoing COVID-19 pandemic. The frustration comes with the fact that this wave is different—it was preventable.
“We’re dealing with a pretty high volume at present,” Wood says. “It’s been harder for our employees this time around because we see people who didn’t get vaccinated and they’re the ones dying—it’s preventable.”
The CMO, who came to Deaconess in the middle of the first COVID-19 surge,
sees her tired team. She sees frontline workers who’ve practically lived at the hospital for the last year and a half. And she knows that no matter what efforts the leadership team executes on their behalf, unless the numbers go down, physicians and healthcare workers will continue to be working hours exponentially past their norms.
Wood says that the best lesson she’s learned about leading, one particularly important during the last year and a half, is one she learned from her father, a power plant superintendent.
“My dad always told me that he might not have an MBA, but he had an MBWA: management by walking around,” Wood recalls about her late father. “He warned me that if I chose a leadership position where I was responsible for a large number of people and I just stayed in my office, I would ultimately fail, because walking around with intent is just a critical aspect of leadership.”
The Deaconess leadership team takes that walk every Thursday with the goal of bridging gaps, expressing gratitude, and doing everything it can to support its healthcare teams. Wood considers it a standard of leadership, asking intentional questions to those she interacts with and holding herself accountable on following through.
Accountability is an absolute must for Wood, and it’s part of the reason she came to Deaconess. “You learn a lot about an organization when you see it handling crises, and I’ll tell you, Deaconess
is an extremely agile organization, and the leadership team I saw here takes accountability seriously and is quick to modify an approach in order to affect a goal,” Wood explains. “I’ve been so impressed with what I’ve seen so far.”
Upon arriving, Wood said that meeting physicians was her number one priority. It makes sense for a CMO who says that serving physicians is the most joyful part of her job. And while introducing herself to Deaconess’s physicians may sound easy in theory, Wood says that the quickly growing institution’s multiple cities made it challenging, especially since she was determined to make meaningful connections with her team.
“I think of my role as a partner, even if I may be their boss,” Wood explains. “I don’t think doctors go to medical school to follow. They’re all leaders, and so I see it as my responsibility to determine strategy and help develop our physicians.”
Wood joined Deaconess after spending eight years as CMO for Baptist Memorial Care, an organization well known for developing all of its talent, not just physicians. It’s where Wood perfected her ability to use the fewest possible resources to attain a goal, all while being thoughtful about how to achieve it.
One skill Wood says that she says she’s had help in sharpening over the years is patience. That help, too, came from her family. Wood’s younger brother Alan was born with Down syndrome, and Wood says her brother, who now lives with her and her husband, has been the best
“I don’t think doctors go to medical school to follow. They’re all leaders, and so I see it as my responsibility to determine strategy and help develop our physicians.”
Sound Physicians is a leading physician partner to hospitals, health plans, physician groups, and post-acute providers seeking to transform outcomes for acute episodes of care. For 20 years, our high-performing and a ordable care models have combined physician leadership, clinical process, technology, and analytics to consistently improve clinical and financial performance.
We are pioneers in value, working together with our partners and community providers to bridge gaps in patient care, from hospital to home.
soundphysicians.com
teacher of patience and love that anyone could ever ask for.
A byproduct of Alan’s diagnoses includes severe hearing loss, but Wood says her brother’s artistic talents continually impress her. “He’s been a blessing for me,” Wood says. “I’ve framed his art, and it’s something he loves doing. I’m afraid he’s stuck with me forever,” she adds, laughing.
Wood had a great deal of interaction with doctors growing up, both through Alan and because of her own type 1 diabetes diagnosis. “I think that had a big influence on my decision to go into medicine,” Wood explains. “You go to the hospital and you watch your brother get better. And for me, as a kid, I didn’t even understand I was sick until I started feeling better. I just remember thinking that doctors were so incredible, and that I wanted to do that for someone else.”
Right now, however, those doctors, nurses, and other staff that Wood leads are also in need of care and attention, as are
other healthcare workers across the US. “In fact, I want to take this opportunity to plead for people to go get vaccinated against COVID-19,” Wood states.

“We have to continue to focus on the fact that we remain in the middle of a pandemic right now,” Wood says. “The first time around, you hated it so much for people, but it wasn’t preventable at the time. This time is something else completely, and while I don’t know if we’ve been successful, the leadership team continues to try and be physically present on the wards alongside our team members to thank them, to support them, and to serve them.” AHL
Sound Physicians wishes to congratulate JoAnn Wood for her exemplary healthcare contributions. We are proud to collaborate with JoAnn as we serve the Deaconess Health System.
“It’s been harder for our employees this time around because we see people who didn’t get vaccinated, and they’re the ones dying—it’s preventable.”
Healthcare is a constantly evolving industry that demands executives to plan ahead. Often, this means business leaders need to address department- or companywide issues to remain focused on driving innovation and devising strategies to maintain a high level of care.
88. Eric Peburn Halifax Health
92. Jon Wright Atrium Health Wake Forest Baptist
82. Jared Swiecicki UChicago MedicineJared Swiecicki leverages his nontraditional path to revenue cycle to approach his role at UChicago Medicine with creativity and innovation
By Zach Balivaared Swiecicki (swi-sick-ee) once visited dozens of hospitals in forty-four states in a single year. He wasn’t an administrator, a sales rep, or a physician. In fact, Swiecicki was just twenty years old. He had taken a year off from studying public relations at Central Michigan University to intern as an actor and performer with a nonprofit that did therapeutic entertainment for patients in the Veterans Health Administration system.
Swiecicki performed in 320 shows that year and interacting with military veterans receiving care in VA medical facilities sparked in him a new passion. When Swiecicki’s internship ended, he returned to college determined to shift away from public relations to pursue a career in healthcare.
Swiecicki made the change after noticing how he could make an impact. “I saw exceptional facilities, and I saw facilities that were lagging behind. As I developed relationships with patients, I knew there must be something I could do to help them,” he explains. Swiecicki also thought
of his own grandfather, a military veteran who struggled to receive quality care at the end of his life.
That patient-centered focus and desire to make an impact led Swiecicki to earn a master’s degree in healthcare administration from Ohio University and has stayed with him throughout a career that has been defined by leveraging diverse backgrounds, collaborating on high-performing teams, and taking calculated risks to make an organizational difference.
He spent a decade building relationships and navigating fast-paced organizations like the American Hospital Association, University Healthsystem Consortium (now Vizient), and Northwestern Memorial Healthcare. Along the way, Swiecicki developed revenue cycle expertise and moved into accounting roles where he developed and implemented workflows, tools, and strategies to help facilitate positive change within healthcare organizations.
In 2017, Swiecicki joined his current organization, University of Chicago
Medicine, where as director of accounts receivable, he manages a forty-member team that processes cash and credit payments while handling insurance claims, follow-ups, denials, and disputes. For
we’re bringing in resources that allow departments to offer the highest level of patient care, expand to new locations, and continue to push the boundaries of medical services and technology,” he explains.
That reality motivates Swiecicki to push for fresh ideas, something he says he learned from Brad Cox during his time at Northwestern, where he was given the freedom to “fail well” in the pursuit of innovation. That freedom and sentiment continues at UChicago Medicine as Swiecicki works alongside Physician Group Executive Director Mamoon Nawabi and countless other leaders across the organization.
Some of Swiecicki’s risks have yielded big results for UChicago Medicine. Upon his arrival, he worked with his managers, Meaghan Kleinfeldt and Maryann Greene, to add notes, activities, and new data fields to the organization’s internal Epic billing system. At first, some users were hesitant to click through and enter more information, but when they got more complete patient data back to work with, they became enthusiastic adopters. Those employees understood they were armed with better data they could then use to drive conversations with payers.
Swiecicki, the job is a fulfilling one because he sees a direct connection between his work in revenue cycle and the medical center’s position in the market.
“Whenever my teams make strong agreements with a payer, capture revenues, or make a process more efficient,
“Jared’s strong collaboration with Availity and his ability to actively engage team members has yielded great results for his organization,” contends Swiecicki’s partners on the account management team at Availity. “He continues to drive down denials with his proactive, data-driven approach to revenue cycle management.”
“We’re bringing in resources that allow departments to offer the highest level of patient care, expand to new locations, and continue to push the boundaries of medical services and technology.”

“Improv, performance, and leadership are all about listening and responding, and those who want to succeed in revenue cycle need to bring innovation and creativity to the table.”
Buoyed by the early success, Swiecicki is looking for other ways to leverage automation and other tech tools. The first step is meeting with employees to uncover pain points. Swiecicki watched in horror as a business analyst showed him just how manual her reconciliation process was. He asked IT to find a way to automate the painstaking and repetitive task, and Director Drake Shrode built an Excel macro that saves hundreds of hours of work each month. That business analyst, Jessica Adamski, went on to use her saved time to find improvements of her own and is now the manager of cash and credits.
As a leader, Swiecicki does all he can to help employees continue their education and advance to the next steps in their careers. During his career, he’s seen one team member become a director, four become managers, and several others take on leadership or supervisor roles. Those are the moments Swiecicki points to as some of his proudest accomplishments. Although Swiecicki took a nonlinear and nontraditional path to his role and industry, he is thriving in revenue cycle at UChicago Medicine. He hopes others
will join him. “There are people in our department who come from healthcare backgrounds, people from other industries, and people who lack formal training,” he says. “I want everyone to know that they can follow any path to revenue cycle and add value by using their diverse knowledge and skill sets to help us find new solutions to old problems.”
Now that Swiecicki is firmly entrenched in healthcare and parenting two young children with his partner Katy, he doesn’t have much time to pursue acting or his other hobbies. However, he still relies heavily on the skills he gained performing for veterans and at Chicago’s Improv Olympics in his professional life.
“Improv, performance, and leadership are all about listening and responding, and those who want to succeed in revenue cycle need to bring innovation and creativity to the table,” he says. Theater, improv, and other nontraditional backgrounds can help anyone in healthcare observe, listen, and contribute to the organization's important mission. And for Swiecicki, that creativity has allowed him to not only fail well but succeed better. AHL
Halifax Health leaders reflect on wins and losses during the pandemic and how to come out stronger in the following years
By Will GrantIt wasn’t the way Halifax Health wanted to celebrate its enduring partnership with the University of Florida, but the first anniversary of the Halifax Health UF Health Medical Center of Deltona came and went with far more patients in its 2020 opening than it ever expected.
When its opening was being previewed by the Hometown News in January 2020, the pandemic hadn’t yet reshaped the entire trajectory of the world. The announcement of the Deltona medical center was yet another feather in the cap of a valued partnership between Halifax Health and the University of Florida.
The partnership began in 2015, when Halifax Health established a relationship with UF Health for heart and vascular surgery services. In 2017, the two organizations worked together to build out Halifax Health Medical Center’s kidney transplant program. The next year, the two announced a neurosurgery partnership.
The $153 million, 6-story, 202,242 square-foot building houses 4 operating rooms, 3 multipurpose procedure rooms, 30 medical and surgical rooms, and 13 intensive care rooms. Each room is fully integrated with systems and tools necessary for procedures and was designed with both physician and nurse access as well as patient comfort.
In a more conservative time, the medical center was planning to employ 211 full-time employees with an
estimated economic impact of $133 million—but that was prepandemic.
“2020 was definitely different than what we planned for as we built Deltona’s hospital in west Volusia County,’’ explains Halifax Health President and CEO Jeff Feasel in a press release. “If given the choice, we would have liked to have avoided opening this state-ofthe-art medical facility during the twenty-first century pandemic, but I am pleased to say our staff has met the challenge and performed admirably. The amount of care our team members have provided is truly impressive.’’
Since opening in February 2020, the medical center has cared for over twelve thousand patients, performed nearly four hundred surgeries, and admitted over one thousand patients, according to UF Health’s chief of staff.
Executive Vice President and Chief Financial Officer Eric Peburn is a longtime contributor not just to Halfiax’s evolving partnerships but also to the larger health system. Peburn came to Halifax Health in 1996 as corporate controller, working his way up through several promotions including director of finance and assistant administrator. He's been in his current role since 2007.
The former Ernst and Young senior auditor holds a bachelor’s and master’s degrees in accounting from the University of Florida. On top of being a former CPA and a member of the American Institute of Certified Public Accountants and Florida Institute of Certified Public Accountants, Peburn also served on executive committees and the board of directors for Daytona Regional Chamber of Commerce. He's currently a board member of Volusia Health Network, Halifax Insurance Plan, and Healthcare Purchasing Alliance. Peburn also
serves on the executive committee of the Civic League of the Halifax Area.
“Eric led a fantastic vision to expand Halifax Health,” says Bob Elliott, president at Noon Development. “We were honored to partner with him in adding 55,000 square feet of medical office space to the Halifax Health footprint, plus developing 4 express care locations broadening access to Halifax Health in this region.”
In addition to Peburn’s duty as CFO to keep the health system in good financial standing post-pandemic and throughout its growth stage, Halifax understands this as a crucial moment to do right by its patients. At the time of writing in fall 2021, it was the first time in more than five weeks that less than one hundred patients admitted to their hospitals were diagnosed with COVID-19.
“The decline in hospitalizations is an encouraging sign,” Chief Medical Officer Dr. Margaret Crossman says in a statement. “I’m confident there would have been far more hospitalizations and deaths had we not had such excellent vaccination uptake among our older and more vulnerable populations. We are now experiencing a relatively rapid downtick in new cases and COVIDrelated hospitalizations.”
Given Florida’s high elderly population and its noted refutation of vaccine mandates, health systems are not only battling a pandemic but also the politicization of the pandemic that has led to far higher COVID-19 numbers in geographic areas that aren’t as willing to mandate masks and other preventative measures.
But given Halifax Health’s continued demonstration of flexibility, adaptation, and patient-centered care, the latest numbers are a sign that the health system’s public outreach efforts are proving successful. But there’s still a long way to go. AHL


Jon Wright credits his talented, driven rev cycle team and patientoriented mission with helping Atrium Health Wake Forest Baptist come out strong amid a crisis
By Billy YostF or those on the finance side of healthcare, it can be difficult to feel the impact of their work as it directly relates to bettering patients’ health outcomes. It’s just the way it is—finance, supply chain, and revenue cycle teams don’t sit wall-to-wall with patients. For these departments, connecting their missions to a successful medical operation is hard if they haven’t built a strategy that puts patients at the heart.
That is, unless you’re on Jon Wright’s team. The associate vice president of
revenue cycle improvement at Atrium
Health Wake Forest Baptist constantly reminds his teams “that while we don’t attend to patients’ health directly, our efforts are critical to the health system’s core mission. We improve patients’ financial health. The revenue we collect covers the costs of life-saving treatments. Most importantly, the health system imports optimized revenue back into our academic and research programs.”
Wright has spent six and a half years advancing through three different
positions, standing up teams and tightening efficiencies. The health system’s cash yield has improved 155 basis points since 2018. “One basis point means another million dollars in revenue,” he explains. “I’m proud of my team for contributing to such significant change.” In the last three years, there’s been a 16 percent decrease in denial write-offs as a percentage of net patient service revenue and a 20 percent decrease in uncompensated care as a percentage of gross charges.

“Embedding unique performance improvement skills within the revenue cycle enables us to consistently identify and realize improvement opportunities,” Wright explains. For the 2019-2020 financial year—a year defined by the COVID-19 pandemic—Wright’s team hit 108 percent of its performance improvement initiatives’ targets. More impressively, in the 2020-2021 financial year, they hit 159 percent of those targets.
In February 2021, the American Hospital Association (AHA) published a report forecasting hospital revenues would be down between $53B and $122B due to the “lingering effects of COVID19.” At the time of writing, “lingering” is a hopeful word.
“AHA anticipates hospitals not going negative will still see an average of 10 to 80 percent margin reduction,” Wright says. “Having this revenue improvement program in place created natural forward momentum for our organization, which was especially helpful with unexpected strong headwinds from COVID.”
There are so many moving parts to the innovation occurring during these revenue cycle improvements that each probably merits its own investigation. But for Wright, it all comes down to a team that he is not shy to be bragging about. “There has been a big increase in revenue cycle consulting in the last decade, and so often that means bringing in consultants to find opportunities for improvements,” Wright says. “A firm will come in from twelve to eighteen months, and then they’ll move on to the next thing.”
Wright’s model is different. They’ve embedded driven professionals with improvement-oriented skills into the revenue cycle who might otherwise be working as consultants but who crave more of a connection to the patients they’re serving. “I would stack my team against the best consultants in the country,” Wright says. “These people work to understand our staff and our patients, and they’re right here alongside them every single day.”
That team was able to stand up a vendor management office (VMO) in the middle of the pandemic. “The reality is that health systems across the country have expanded their vendor partners in response to growing complexities of revenue cycle. Multiple vendors can be difficult to manage,” says Wright.
Upon establishing the VMO, the team found 57 percent of the vendors in its portfolio weren’t hitting performance targets. One fiscal year later, that number has been cut to 25 percent. “We’re holding our vendors accountable just as we do ourselves internally,” Wright says. Wright noted the vendor portfolio’s cost to collect also improved in the same period.
As Wright continues to embrace, stand up, and mature nontraditional revenue cycle practices, he’s invested in other ancillary support services, like the VMO, to further the mission. He spent his first couple of years in leadership maturing Wake Forest Baptist’s analytics abilities.
“Analytics is a means to an end, so I don’t want anyone to think we’re doing
“ Having this revenue improvement program in place created natural forward momentum for our organization , which was especially helpful with unexpected strong headwinds from COVID.”
We appreciate the oppor tunity to collaborate with to increase patient satisfaction and net recoveries

analytics just for the fun of it,” Wright says, laughing. “As we continue to mature our analytics, we lay the foundation for advancements in other areas. For example, as we are beginning to explore predictive analytics, we’re able to put the right account at the right time in staff’s hands.” In a time when more is expected for less, Wright says it’s more important than ever to prioritize work for staff in an order that will benefit the most people while creating less work.
Visibility into payer patterns is also paramount, Wright notes. The newly expanded analytical abilities of Wright’s team provide insight into individual payers, comparing each peer group on specific performance indicators.
“Understanding individual payer performance is invaluable,” he says. “Modeling parameters such as payer adjudication patterns, payment velocity, and denial appeals highlights where cash velocity and yield improvement opportunities exist.”
Wright and the revenue cycle team are also incorporating recent advancements in data analytics to stand up new quality performance tools, incorporating a new quality program with existing education program to make education continual.
“For the first time, we can share with a registrar the front-end denials their actions resulted in,” Wright says. “Who doesn’t like feedback on how they are performing well and where they can improve? We’re able to look at new quality issues as they arise and address them with quarterly education to frontline staff.”
With the recent roll out of the quality program to hundreds of registration team members, the team is already
seeing a decrease in registration-related denials and an increase in point-ofservice collections.
But Wright has only gotten started. For a man who graduated from Wake Forest and claims that he “bleeds black and gold,” he’s done his alma mater proud. But he’s insistent that his team, leaders, and the mission of the healthcare system are the ones responsible for his success.
In fact, he says he’ll stack his teams up against yours any day. Any takers? AHL

“Analytics is a means to an end . . . As we continue to mature our analytics, we lay the foundation for advancements in other areas.”
Executives know there is an increasing need to help individuals manage their own health anywhere and anytime.
To do that, healthcare leaders are developing products and services and offering resources catered to different communities’ needs—all aimed at motivating them to stay engaged with their health and empowering them to be their best, at home or at work.
98. LeAnn Harris Mercy 104. Ken Leidner Satellite HealthcareLeAnn Harris helps carry out Mercy’s extensive coworker benefit efforts, keeping all facets of well-being in mind
By Billy Yost
LeAnn Harris came to Mercy in 2010 to aid the organization in its investment in and creation of its coworker health and wellness initiatives. The goal was to standardize the whole system— more than nine hundred physician practices and outpatient facilities as well as more than forty hospitals—and create a shared service model that would enable Mercy to offer its coworkers benefits more as a collective, rather than as separate entities.
For Harris, who serves as vice president of health, benefits, and wellness, the goal has been to continue the mission of the Sisters of Mercy, a ministry whose two-hundred-year legacy of care is forwarded by more than forty thousand coworkers today. The VP sees her own role as an extension of the Sisters and is moved to provide the same degree of care and urgency for everyone supporting the Mercy mission as the physicians and frontline workers provide for their patients.
Prior to the COVID-19 pandemic, Harris had already positively impacted the workplace and wellness journeys of the broader Mercy network. “Over the years, we’ve been able to develop a very robust, outcomes-based wellness program to support our coworkers,” Harris explains. That includes a biometric screening with a premium differential when meeting individual health goals and a healthy activities rewards incentive, where coworkers and their covered spouses can each earn up to $400 by engaging in healthy lifestyle activities.
“We’re self-insured, so it’s important for us to help our coworkers understand that habits drive costs,” Harris says. “We want to educate them to be good consumers of healthcare and their benefits so they can have more money in their pocket.”
Mercy’s health plan offers an exclusive provider organization (EPO), which allows the health system to provide a high-quality, integrated continuum of care for its coworkers while managing costs for the wider health system. Over 80 percent of benefit-eligible coworkers are enrolled in this plan.
In terms of financial wellness, Mercy works with PayActiv to allow coworkers to get early access to their paychecks prior to payday. “It’s money they’ve earned, and we’re only paid every two weeks, so if there is an expense that needs to be paid tomorrow, this allows them access when they need it,” Harris says.
To help support coworker financial education and wellness, Mercy works with Fidelity to find and create tools that will help them learn about budgeting,
expense tracking, and other financial literacy instruments.
With the onset of the COVID-19 pandemic, Mercy recognized that it needed to provide more for its people in times of crisis. At the height of COVID cases, the organization offered emergency paid time off as well as major disaster PTO. “This was a time that you simply could not plan for, but I’m just so proud of what this team has been able to roll out to support our coworkers,” Harris says.
“There’s a saying that adversity doesn’t build character; it reveals it. That is certainly true of LeAnn,” says Rae Shanahan, chief strategy officer at Businessolver. “We’ve worked side by side with LeAnn and her team for years, providing technology and services to help power her benefits vision for Mercy’s workforce.
“Many things have shifted dramatically over the past eighteen months,” she continues, “but LeAnn’s visionary leadership has not been one. We’re proud that Businessolver continues to help support her in bringing Mercy’s benefits to employees so they can care for themselves and families as fully as they do for their patients.”
Along with an extensive mental health first aid kit, Harris said the organization placed a premium on listening to each other and recognizing when people need help through its Listen 1st campaign.
“Through our Mercy EAP [employee assistance program] and behavioral health services, we can provide so many tools and resources for people that need them,” the VP explains. “We’ve put together campaigns to simply let our coworkers know that this is a very hard time and that we are here to help.”
“We’re called to serve and just because we’re not at the bedside doesn’t mean that our role isn’t important. We’re here to support those who are caring for our patients , so they don’t have to worry about their pay or benefits.”
Harris says one of the silver linings of her team being sent home during the pandemic was the leg up it will offer Mercy in terms of talent attraction and retention.
“I’m fortunate to have a talented and diverse team, and had the pandemic not happened, I’m not sure the organization would have been ready to move to a workfrom-home model,” Harris says. “But to be honest, I have seen some of my teams become even more productive working from home—they’ve just flourished.
“We have also been able to retain talent in this new model,” she adds. “For example, we have had a couple highly talented coworkers whose spouses have been relocated to a new state and we have been able to retain them, whereas in our old model, they would have had to resign.”



Harris says the need to check in on her team, however, shouldn’t ever be overlooked. “There are a lot of people who get most of their social interaction from their job,” Harris says. “It’s imperative to check in on my team, to see how they’re doing, and to continue to form that Mercy mission for our new coworkers, who maybe haven’t stepped foot in one of our facilities.”


Given Harris’s pride in her diverse team, it’s no shock that she’s on Mercy’s Diversity, Equity, Inclusion Advisory Council and serves as the chair of the Social Determinants of Coworker Health Council. One of the council’s biggest victories was the creation of the Medical Premium Assistance Program, which allows coworkers who qualify to pay healthcare premiums that are reduced by up to 50 percent.
“If we have coworkers who are deciding whether or not to get coverage, we want to be able to help make that choice much easier for them,” Harris says. The VP says that in working with Experian to determine eligibility, the program allows individuals to retain anonymity and not place an undue burden on their own dignity.

After nearly eleven years at Mercy, Harris says her knowledge that the Sisters of Mercy laid the foundation for the role she’s in today is never far from her mind.
“I always think that one of the Sisters was in one of our positions years ago,” Harris says. “We’re called to serve, and just because we’re not at the bedside doesn’t mean that our role isn’t important. We’re here to support those who are caring for our patients so they don’t have to worry about their pay or benefits.” AHL
Aon congratulates LeAnn Harris for this well-deserved recognition; we are honored to call you a partner and friend. Aon is a leading global professional services firm providing a broad range of risk, retirement, and health solutions. We empower results for clients by using proprietary data and analytics to deliver insights that reduce volatility and improve performance. To learn more, visit aon.com.
Anthem Blue Cross and Blue Shield in Missouri is proud of our partnership with LeAnn Harris and the Mercy team. We join them in their mission to deliver a transformative health experience to the communities we serve. Thank you, LeAnn, for your continued innovation and partnership.




Empathetically designed benefits technology that empowers HR to deliver outcomes that put people first.

The heart is one of the first things you check to make sure all is well. We take the same approach.
The kidney care industry is complex. Satellite’s Ken Leidner uses his broad experience to forge meaningful partnerships with healthcare systems, nephrologists, and payer companies.
By Frederick Jerant Ken Leidner Chief Growth Officer Satellite Healthcare
Ken Leidner Chief Growth Officer Satellite Healthcare
T he kidney dialysis industry has many moving parts—the providers of the service itself, related hospital systems, and nephrologists. Each player is significant, and each player has its own set of concerns and aspirations.
Ken Leidner, chief growth officer at Satellite Healthcare, understands all of them, and uses his many-angled perspective to drive Satellite’s business forward.
After originally working in the investment banking/corporate development space, Leidner joined DaVita Healthcare Partners in 2004. He led a national sales team focused on inpatient/outpatient kidney care services and partnership opportunities with hospitals, physicians, and integrated health networks, as well as growing the business through mergers, acquisitions, and joint ventures.
“In my first six years there, I was a transaction director and coordinated over fifty successful transactions,” Leidner explains. “When I was promoted to VP, I began running two hospital-facing development teams—one that addressed hospital patients, the other geared toward their eventual discharge.”
A key accomplishment was merging and cross-training those teams, and then expanding their knowledge base to better partner with hospitals.
About four years later, a former DaVita colleague recruited him to DSI
Renal (later acquired by US Renal) as senior vice president of physician services. He consulted with affiliated nephrologists to help them expand their practices through strategic planning and cofounded the Nephrology Business Leadership University (NBLU), a five-day “boot camp” for second-year nephrology fellows, with the Dallas Renal Group and the University of California at San Diego.
“NBLU teaches fellows the business and economics of nephrology so they’ll be better prepared to embark on their own private practice paths,” Leidner notes. “They also learn the importance of marketing their business so they can build up their own patient bases.”
In March 2019, Leidner joined Satellite Healthcare, a not-for-profit organization founded by noted nephrologist Dr. Norman S. Coplon. “Although its key business segment is its eighty-five dialysis clinics, Satellite also operates the largest independent dialysis lab and does extensive applied pragmatic research,” Leidner explains. “It’s aimed at finding innovations that can have immediate impact on problems in the industry, and also performs contracted research for the FDA and others.”
Satellite has also recently launched an management services organization providing back-office functions to nephrology practices, as well as a new
“We can analyze the entire country in terms of population growth, the occurrence of chronic kidney disease and end-stage renal disease, and then determine locations where we’ll have the best chance of reaching patients that will benefit
care management program for chronic kidney disease and end-stage renal disease (ESRD) patients under a payment-for-performance model rather than the typical fee-for-service model, with the goal of delaying disease progression.
Leidner’s varied background with dialysis centers, hospitals, and nephrologists has given him a unique perspective. “It’s a complex system, and I think I navigate it better than many,” he says. “When I’m engaging different constituents, I see the perspective from the view of providers, hospitals, and doctors. That makes me a better partner for them, and I can also share my knowledge with my team, so they’ll become stronger and better at what they do.”
That’s important because Satellite’s model for kidney care, with emphasis on home therapies, is expanding from simply providing dialysis to providing
other interventional measures, such as ensuring patients see their expanded care teams, like nutritionists and behavioral health specialists who can help to coordinate their care.
“Education is important too,” Leidner remarks. “Right now, almost half of dialysis patients didn’t realize their kidneys were failing until they crashed and went to the ER. And although certain types of dialysis can be performed at home instead of a clinic, only 20 to 30 percent of patients know that home treatment was even an option.”
A key aspect of Leidner’s responsibilities at Satellite encompasses overseeing the company’s various partnerships with hospitals, health systems, and nephrologists. “The typical development approach is to simply sell an offering by creating a need. We prefer a consultative approach— that is, ‘I have solutions to solve various
“We prefer a consultative approach—that is, ‘I have solutions to solve various problems, so let’s focus on your situation and goals, and then we’ll present solutions to get there.’”
problems, so let’s focus on your situation and goals, and then we’ll present solutions to get there,’” Leidner says.


Leidner attributes meeting the company’s goals in part to his player/coach leadership style. For example, he’ll often run drills as a team and conduct role-playing exercises, and he’ll sit in on initial meetings, tacitly demonstrating his “other-centered” approach to the process and guiding the team toward consultative interactions. “Eventually, I move into the background and let the team take over completely,” he says.
The typical result? Within a year, engagements are up, partners are pleased, and long-term relationships begin to evolve.


He also has a unique outlook on strategic planning for growth. “We can analyze the entire country in terms of population growth, the occurrence of chronic kidney disease and end-stage renal disease, and then determine locations where we’ll have the best chance of reaching patients that will benefit,” Leidner explains. “Because Satellite is not-forprofit, we can concentrate on doing the right thing clinically instead of just satisfying shareholders. We may operate at reduced margins while innovating new models of care that align with mission and help underserved populations.”
Leidner cites a rural market in which Satellite partnered with a local nephrologist to set up a new model to support home-based dialysis. “It enabled patients
to skip the three-times weekly visits to the clinic. We were financially challenged there for five straight years, but we provided a service that the community needed and honed our model along the way,” he says.
Leidner is further bringing his problem-solving approach to insurance companies and other payers. “Medicare reimbursements barely cover the cost of delivery,” he says. “When Medicaid is involved, we may actually lose money.”
The company’s new care management program addresses the situation by delaying the onset of ESRD, lowering hospitalizations and increasing transplant rates.

“We explain to hospital CEOs and payers that up to 50 percent of kidney patients start their treatment journey by crashing in the ER—and that’s a highcost way to begin. And the total cost of care, which includes physicians, drugs, hospitalizations, and dialysis sessions, will be even more expensive,” he says.
“But they’re often receptive when we explain that our program of intervention and education can actually hold their costs down, because of fewer hospitalizations, more involved patients, and the potential to ethically postpone dialysis treatment,” Leidner adds.
In the end, Satellite’s penchant for education and long-term care keeps patients well and out of hospital systems. It’s a classic win-win situation. AHL
Ben Ochs, James Schmid, and Katie Jacoby explain how Anchor Health Properties sets itself apart as a community staple
By Billy YostWhen speaking with three executives on Anchor Health Properties’ leadership team, there is a synergy that just can’t be faked. It’s emblematic of the small-business and employee-owned mindset that has helped propel the success of the nationally active firm that, after thirty-five years, is still operating with the agility and patient-centric mindset that puts no project in a predetermined box.


CEO and Managing Partner Ben Ochs, Chief Investment Officer and Managing Partner James Schmid, and Executive Vice President of Strategy and Development and Partner Katie Jacoby shared how Anchor’s intensive investment in its operating platform; its core values, vision statement, and purpose statement; and its continued commitment to relationship-building both inside and outside the organization have helped spur Anchor’s growth into new regions, while still finding a way to stay deeply connected to the communities in which Anchor is active.
The Anchor Difference Anchor’s CEO (and former president of Brinkman Management & Development, which merged with Anchor Health Properties in 2015) is quick to point out what he sees as DNA-level reasons for Anchor’s continued evolution and success. “I think you have to start with the fact that we’re employee owned and operated,” Ochs explains.

“We’re a full-service, private healthcare real estate firm, so we don’t need to meet quarterly earnings targets,” he continues. “That allows us to be fully flexible, creative, and entrepreneurial in delivering the right capital solutions for our clients. I think that’s what helps set us apart from a lot of our peers in the industry and can allow us to bring solutions that other organizations might not be able to provide.”
Schmid approaches from another angle: Anchor’s fully integrated operating platform. In a highly niche real estate sector like Anchor’s, it takes a lot of operating
Katie Jacoby EVP of Strategy & Development and Partner Anchor Health Properties James Schmid Chief Investment Officer and Managing Partner Anchor Health Properties Ben Ochs CEO and Managing Partner Anchor Health Properties“We’re focused on being the best healthcare real estate firm in the United States. We understand that it’s aspirational, but I think that’s true of any good goal .”
—Ben Ochs
knowledge and relationships to succeed. The firm’s collaborative approach—both internally and externally— puts it in a good position to raise institutional capital.
“Ben and I invested heavily in the platform over the last few years to continue to exhibit institutional standards,” Schmid says. “Our ideal goal is to take on that responsibility under one roof and own it. I think that makes us truly unique.”
Jacoby ties these two sentiments together, noting that putting clients’ interests at the forefront serves as a central theme. “We try our best to understand the challenges faced by our healthcare partners and structure our organization, financial solutions, and relationships to support their real estate objectives,” the EVP explains. “Our goal is to empower our teams with the resources they need to make decisions on a daily basis that allow us to put our clients first.”
After the 2015 merger and significant growth of the firm, Ochs says it was imperative to bring the entire company together to help redefine itself going forward. What initially started out as a core value-defining expedition turned into something much more intensive.
With defined core values of accountability, innovation, collaboration, honesty and humility, ownership mentality, and relationship focus, the company continued to examine its mission and value proposition.
“We had defined what was important to us, but why is it that we do what we do?” Ochs asks. “What motivates us to get out of bed every day?” While multiple service lines lead in different directions at Anchor, they all lead back to one common motivator: pursuing better healthcare through real estate solutions.
That statement is matched with a lofty goal. “We’re focused on being the best healthcare real estate firm in the United States,” the CEO explains. “We understand that it’s aspirational, but I think that’s true of any good goal. You want to constantly be in pursuit of achieving it and hitting those cascading subgoals that help get you there.”
Schmid says that defining these ideals and goals has helped partner all three key platforms at Anchor under a common banner, and they’re seeing the benefit.
“We’re seeing it now everywhere from Philadelphia to Atlanta, from Seattle to San Diego,” the CIO explains. “We’re beginning to push into the top two or three ownership groups, if not higher, in terms of square footage, and we’ve really done that by building great relationships in those markets that encourages all three of our verticals to collaborate across the company and work together.”
Jacoby is able to personalize Anchor’s efforts in a way that underscores the company’s pursuit of better healthcare. “I had the unique opportunity to build a large, integrated healthcare project in my own community,” the EVP explains. “Before the project was built, my neighbors and I had to travel forty minutes to access the closest specialty care services. It’s tremendously rewarding to have played a role in bringing necessary healthcare services closer to home for my friends and family.”
The Long Haul
Anchor’s ability to be everywhere nationally can, at least in part, be attributed to the fact that between 35 to 40 percent of its workforce was remote even before the pandemic.
“With real estate, the adage is ‘location, location, location,’ but for us it comes down to ‘communication, communication, communication,’” Jacoby says. “Whether it’s connecting internally or listening to the needs of our tenants, quality communication is absolutely essential.”
Anchor has offices spread all over the country, which Ochs says underlines the organization’s commitment to making sure its people are part of their communities. It may mean that Anchor has had to invest more in making sure that the decentralized organization still feels connected, but it’s ultimately worth it.
“Our employees and our partners are incredibly diverse,” Ochs explains. “We want to make sure our employees are living, working, and playing in the communities where we’re active. We want our employees acting as representatives for the brand, not just checking in on an asset.”
It’s a long-term mindset based in building trust, relationships, and community. It’s not the quickest way to make a dollar, but it’s proven to be the strongest anchor for Ochs, Schmid, Jacoby, and their team. AHL
Our responsive billing and payments platform leverages deep analytics and machine learning to understand your patients capacity to pay, their preferred method of engagement, and where on their healthcare journey we need to meet them. We're delivering on your patients most important payments and maximizing collections for you and financial peace for your patients.

Availity RCM is powered by one of the nation’s largest network of payers and healthcare providers. Make Availity RCM your end-to-end clearinghouse and total revenue cycle solution.
Learn how Availity RCM helps you get paid more and get paid faster with:

• Denial management and prevention
• All-payer electronic claim attachments
• PM/EHR system integration features
• and much more!
Learn more at www.availity.com/RCM
• Automated claims editing
• Enhanced EDI enrollments
• Authorization services