Unbroken An Connection
During a time when in-person interaction is more complicated than ever, Head of Supply Chain Wendy Xia ensures that Agios Pharmaceuticals seamlessly connects with its patient population P44


As the only truly integrated premium courier and clinical packager, our custom-built kits streamline your production. Yourway considers every angle with our deep experience in material sourcing, to make sure your kit is designed efficiently, with useability, shipping, and even end use in mind. With primary and secondary packaging from a single source, why work with multiple partners when Yourway can do it all? Visit yourway.com to learn more. The Only Truly Integrated Premium Courier & Clinical Packager. Don’t Let Clinical Packaging Slow You Down. Customized Lab Kits and Material Sourcing from a Single Source. +
Stories of leaders who reinforce a connection with their communities during the most arduous times P8
Bridge the Gap

Contents 3
in this issue
The Path


With decades of HR experience under his belt, David Jones helps Stanford Health Care attract and retain the very best ▶P 64

At University of Chicago Medical Center, Catherine Garvey Goldthorpe combines an attorney’s acumen with a caregiver’s compassion P 70
Andrew Parker started Papa to make the quest for help seamless and easily accessible for seniors and families P 74

The Issues
Bill Pufko helps keep BMS’ workforce safe while making its ambitious 2030 sustainability goals a reality ◀P 80
Thomas White saw that health systems’ provider directories were disorganized and confusing. So, he made Phynd, a symplr company to fix that. P 84
At Cedars-Sinai, Patricia Campbell supports her talented pool of employees through any circumstance P 90
how the
a
4 AHL
Saira Hopper (Pufko), Gillian Fry (Jones and Love Fridge Chicago) See
Love Fridge Chicago,
mutual aid group, combats food disparities P10
The Farm on Odgen produces more than fresh food—it enhances civic engagement and prosperity P52

The Business
As CFO, Steve Aleman ensures Prime Healthcare’s finances are solid enough to outlast anything—even a pandemic P 98
Lars Taavola encourages Mallinckrodt’s highly scientific workforce to think creatively to expand the company’s IP portfolio P 106
Inside and outside Atara Biotherapeutics, Maribel Hines creates a space of inclusion and belonging ◀P 112


On the Cover
Wendy Xia’s portraits are by Tony Luong, a photographer based in Boston. To view more of his work, visit tonyluong.com.
The Impact
Carolyn Wood considers all points of the wellness spectrum as UPMC’s vice president of employee benefits P 118
To prevent burnout and support healthcare workers’ mental health, Dr. Saloumeh Bozorgzadeh created Caring for Our Caregivers P 124
Janel Lancaster helps keep North Carolinians healthy by overhauling HR operations inside UNC Health and supporting community initiatives outside of it ◀P 128

 Chris Schmitt (Hines), David Williams (Lancaster), Gillian Fry (Farm on Ogden)
Chris Schmitt (Hines), David Williams (Lancaster), Gillian Fry (Farm on Ogden)
Contents 5
Masthead
CREATIVE
VP, Creative Production
Kevin Warwick
Editorial Manager
Frannie Sprouls
Managing Editor
KC Esper
Editors
Melaina K. de la Cruz
Sara Deeter
Julia Thiel
Hana Yoo
Staff Writer
Billy Yost
Contributing Writers
Zach Baliva
Charles S. Donnavan
Charlotte Foer
Taylor Karg
Natalie Kochanov
Donald Liebenson
Keith Loria
Maggie Lynch
Javanna Plummer
Sara Verdi
Shira Vickar-Fox
Senior Designer
Vince Cerasani
Photo Editors & Staff Photographers
Cass Davis
Gillian Fry
CORPORATE
CEO & Publisher
Pedro A. Guerrero
Chief of Staff
Jaclyn Gaughan
President, Group Publisher
Kyle Evangelista
VP, Hispanic Division Head of Audience & Engagement
Vianni Lubus
VP, Finance
David Martinez
VP, Sales
Ben Julia
Senior Director, Client Operations
Cheyenne Eiswald
Senior Client Services Manager
Rebekah Pappas
Client Services Manager
Brooke Rigert
Director, Client Services—Corporate Partnerships
Taylor Frank
Director, Talent Acquisition & Engagement
Haylee Himel
Director, Talent Acquisition
Heather Steger
Senior Director, Corporate Partnerships & DEI Solutions
Krista Horbenko
Events Director
Jill Ortiz
Digital Events & Marketing Coordinator
Ashley Parish
Communications Manager
Cristina Merrill
Director, Sales
Kelly Stapleton
Director, Sales Training & Development
Alexa Johnson
Director, Sales Onboarding
Justin Davidson
Content & Advertising Managers
Megan Apfelbach
Leon Hu
Annie Peterson
Kelly Stapleton
Drew Thomas
AHL Magazine® is a registered trademark of Guerrero, LLC.
Facebook: @ahlmagazine
LinkedIn: @american-healthcare-leader
Twitter: @AHL_Magazine
©2022 Guerrero, LLC guerreromedia.com
1500 W. Carroll Ave., Second Floor Chicago, IL 60607
Reprints
Reprinting of articles is prohibited without permission of Guerrero, LLC. Printed in China. For reprint information, contact
Reprints & Circulation Director Stacy Kraft at stacy@guerreromedia.com.
6 AHL
From the Editor
Typically, the theme of AHL’s first issue of each year is “Community Impact.” These past few years, however, have been anything but typical.
At this point, there is a full year between where we are now and 2020 (praise be), yet the effects of COVID-19 and its variants are still quite present. Last year gave us some respite thanks to vaccines, and we’ve been able to taste normalcy in ways we craved deeply in 2020. But we’re still learning how to navigate the complex new world that the pandemic has mapped for us—namely, relearning how to interact with the people around us, in our own social circles, in our jobs, and in the world in general.
So, with all of this in mind, we rethought this issue. How can we impact communities if we have never felt more distant from the people around us? This year’s theme is instead about that effort to connect: how leaders reach for their community members to uplift and protect them, despite (and sometimes because of) the circumstances we’ve all been facing. Our special section highlights healthcare leaders who work in HR, IT, and other behind-the-scenes positions to build a link between their health systems and the patients they serve.
In addition, you’ll also see two unique photo essays that shine a spotlight on nonprofit organizations that go an extra mile to help their neighbors. AHL Photographer and Photo Editor Gillian Fry and I got an inside look at the Love Fridge (p.10) and the Farm on Ogden (p.52) to see how they impact neighborhoods across Chicago by combating food insecurities, establishing healthy habits, and building hope for the future.
These organizations are paving the way to sounder, closer communities. Though the road to “normal” may be long, the ideas and efforts that have arisen make the journey toward our next destination much more inspiring and promising. With leaders like these taking the wheel, I can’t wait to see where we go next.
KC Esper Managing Editor


Gillian Fry
Editor’s Letter 7
Change Within Reach

8 AHL

we navigate a divided and confusing moment in history, these organizations and leaders do everything they can to reach through the fog, extend a helping hand, and unite communities in ways never thought possible 10 The Love Fridge Chicago 22 Dr. Jimmy McElligott, Medical University of South Carolina 28 Dr. Eve Glazier, UCLA Health 34 Adrin Mammen & Jeffrey B. Short, Montefiore Health System 40 Mohamed Humaidi, Franciscan Alliance 44 Wendy Xia, Agios Pharmaceuticals 52 The Farm on Ogden The Feature 9
As
Mutual Aid
The

Love Fridge combats food insecurity by placing communitymanaged, easily accessible fridges and pantries across Chicago
 By KC Esper
By KC Esper
Photos by Gillian
Fry
10 AHL
◀ Lisa Glenn Armstrong, a multidisciplinary artist based in Chicago, designed the look of the Love Fridge website and brand. Vibrant palates and cheerful illustrations can be seen on every fridge in the city, though each is uniquely designed to reflect the neighborhood in which its placed.

in Motion

The Feature 11
When looking at everything the Love Fridge Chicago has built and accomplished so far, it’s easy to assume the organization has been around much longer than a year and a half. The summer of 2020 brought to light circumstances of inequity, frustration, and underrepresentation for communities across the world, but it also brought about a resurgence of public support for people in need—and with that came the Love Fridge.
Cofounder Ramon “Radius” Norwood, an artist and musician, saw a community fridge in Brooklyn and was inspired to replicate the idea in Chicago’s neighborhoods, particularly those south and west of the Loop that are devoid of fresh food sources and grocery
stores. He put out a call for volunteers, and hundreds of people responded, bringing with them an enormous amount of energy and urgency to help combat food insecurity during a time when so many people were unemployed and desperate for relief.
Now, the Love Fridge has thirty fridges and counting, many of them open 24/7 and all of them monitored, cleaned, and stocked entirely by the public. Organizations, kitchens, and farms can donate extra product to the fridges, and Chicago residents are encouraged to donate their time to maintain them. The amount that the Love Fridge has accomplished in such a short amount of time is astonishing, but the distance they can—and will—go is even greater. AHL

12 AHL
▲ There are no restrictions on the number of times someone can frequent the fridges, nor is there a cap on the amount of goods that can be taken from a fridge at a given time. People who use Love Fridges are empowered to take as much or as little as they need, as often as they need.
▲
are placed on city corners, inside the lobbies of restaurants and stores, or in alleys. Community members can elect to start their own fridge—which, if successful, will then be adopted as an official Love Fridge by the organization—or they can help manage one that has already been established.


 Fridges
Fridges
The Feature 13
◀ Most Love Fridges have a pantry for shelf stable items and dried goods.
The Love Fridge offers design templates and maintenance guidelines for people interested in starting a fridge. The criteria to become a new host includes having positive connections to the neighborhood, an assurance of viable foot traffic, the ability to build the fridge’s shelter, access to a power supply, and the capacity to cover the fridge’s electricity cost for the year. In some cases, the Love Fridge supplies building materials and financial assistance.



14 AHL
▼ This fridge sits outside of Stone Temple Church in North Lawndale. While many fridges are maintained by volunteers and members of the organizations they sit outside of, some fridges are almost entirely maintained by one family, like the Kindness Korner fridge in Southeast Chicago.

The Feature 15

16 AHL
Risa Haynes is the lead food distribution organizer for the Love Fridge. In addition to gathering donations from various partners across the city, she also helps clean, date-check, and stock each fridge.
▶ Haynes says that, in addition to the hundreds of people who help keep the Love Fridge operation going, there are eleven decision-makers at the core—but that number isn’t fixed. Passionate people are always encouraged to join the team.


◀ More than half of the stocked food comes from community member donations. Haynes encourages people to put out calls for food on social media—which, she says, works tremendously well. The rest is donated by local food pantries, nonprofits, and restaurants.


▲ The Love Fridge is not only interested in combatting food insecurity but also providing access to basic hygiene items. The organization partners with nonprofits like the Chicago Period Project to provide essential one-use products like tampons, diapers, and toilet paper.
 ▶ Pilsen Food Pantry is one of the main suppliers and distribution centers of nonperishable food and dry goods donations for the Love Fridge. They also share bottled water and canned coffee, which are popular staples among fridge users.
▶ Pilsen Food Pantry is one of the main suppliers and distribution centers of nonperishable food and dry goods donations for the Love Fridge. They also share bottled water and canned coffee, which are popular staples among fridge users.
The Feature 17
▲ As a mutual aid, the Love Fridge encourages community members to take ownership of each station and provides them with the resources they need to help with upkeep. This QR code refers volunteers to everything from cleaning checklists to the dos and don’ts of donating.



18 AHL
▲ In addition to stocking the fridges with fresh produce and prepackaged meals, Risa Haynes and her team also stock the freezers full of frozen meat and vegetables. During the pandemic, meat that would typically go to institutions to be sold was being redirected to food pantries. The Love Fridges were getting a surplus that they packed into their freezers. Now that restaurants and other organizations are back open, Haynes says that frozen goods, eggs, and milk are at a deficit but still in high demand.
◀ While summertime promises fresh fruit and vegetables, in the winter Love Fridge organizers encouraged volunteers to fill fridges with premade meals to provide a comfort to people in need. They also partnered with the Logan Foundation to supply thousands of hand and foot warmers.


The Feature 19
▶ Throughout the pandemic, restaurants like Kimski, located in Chicago’s Bridgeport neighborhood, obtained grants to keep people employed, keep the supply chain operating, and feed people for free. So, every night Love Fridge volunteers would gather excess meals to distribute to each fridge. Though many grants ran out, the Love Fridge still tries to supply delicious, ready-toeat food options as much as possible.
▼ Staple pantry items and ingredients like spices, salt, pepper, flour, garlic, and cooking oil are usually some of the most sought-after goods from fridge users


20 AHL
▼ Fruits and vegetables come from partners like the Edible Gardens at Lincoln Park Zoo, Imperfect Foods, the Urban Growers Collective, and Truong Enterprises Inc. According to Haynes, fruit is one of the most coveted and rare treats that the fridges get, as a typically expensive yet nutritious grocery item.
▲ Haynes stresses to vendors and community members that despite the pandemic clearing up, food insecurity is still at an all-time high and emphasizes the fact that neighborhoods on the south and west sides of Chicago are food deserts through and through. As such, making vitamin-rich items available is incredibly impactful, and with all hands on deck, the Love Fridge will continue making that access possible and improve the well-being of the city at large.




The Feature 21
The Value of

22 AHL
At the Medical University of South Carolina, Dr. Jimmy McElligott expands telehealth capabilities to reach every corner of his community
By Keith Loria
Virtual Care

The Feature 23
As one of seven kids and the son of two physicians, Dr. Jimmy McElligott often took care of his younger siblings, and it surprised no one when he decided to become a pediatrician.
He graduated from University of North Carolina Chapel Hill and the Wake Forest School of Medicine and came to the Medical University of South Carolina for his residency for pediatrics. After completing a fellowship at the Charleston University, he stayed on in an academic position and became focused on helping underserved children access care. There, McElligott saw the need to draw attention to the increasing gap in care in poor communities. That led him to telehealth.
“I got involved with some of the grassroots efforts to use virtual care to reach out to patients, and at my own institution, got involved in some health disparity-focused areas to improve health in South Carolina,” McElligott recalls. “People pushed me to the forefront, sort of leading the effort, and rapidly my predominantly academic position transitioned to more of a leadership executive position.”
Today, McElligott serves as the executive medical director for the Center of Telehealth at the Medical University of South Carolina (MUSC). Back in 2011, MUSC began thinking about the expanding telemedicine capabilities and McElligott started to put together a plan. He applied for some grants, gathered coordinators, and compiled a workbook
on telehealth that would become the guide for MUSC to follow.
“The effort to use virtual care to solve some of South Carolina’s health problems became a big deal and a big priority for MUSC,” McElligott shares. “I had to quickly learn how to do a lot of strategic planning, learn the different modalities, and learn how to work as a leader with other stakeholders throughout the state.”
Thanks to a $100 million-plus investment by the state, McElligott and his team of fifty have been able to advance telehealth, enhance the patient experience, and strategically integrate the technology throughout the system to support patients throughout their whole journey.
“When I first started down the path, the idea was for school-based telehealth: to find some of the underserved and rural schools and connect with telehealth,” he explains. “It wasn’t known if it was allowable in that way or billable, but we decided to get a grant and see if it could work.”
That led to a better understanding of the problems there were and what needed to happen to make things better.
“I spent a lot of time on the road, driving through rural South Carolina, meeting school nurses and talking with people about their concerns,” McElligott recalls. “I ended up going to the Board of Medical Examiners probably four or five times over a series of two years and talking with them about concerns and coming back with reassurances.”
24 AHL


Tabitha Safdi The Feature 25
Dr. Jimmy McElligott Executive Medical Director for the Center of Telehealth Medical University of South Carolina
It wasn’t long before his time dedicated to practicing pediatrics was reduced, and instead he was leading the charge for telehealth at MUSC’s Center of Telehealth. That meant telehealth programs for pregnant women, patients with diabetes, patients addicted to opioids, and more specialized care for those who needed it, like stroke survivors.
“Since then, it’s really been more about clinical care transformation than it is about using video or any other

technology,” McElligott explains. “It’s about how you change the way you do practice, why you change, and how to make things more efficient.”
Of course, when the pandemic hit, McElligott had to rethink everything. The telehealth goals changed, the bar changed, and it was time for telehealth to reach the potential he knew it could.
“I was fortunate that the state and MUSC had really, truly invested in telehealth and it was a core strategy,”
26 AHL
“I was fortunate that the state and MUSC had really, truly invested in telehealth and it was a core strategy. The pandemic validated a lot of our philosophies about why telehealth should be used—it should be used to make things efficient and should be for everyone.”
McElligott notes. “The pandemic validated a lot of our philosophies about why telehealth should be used—it should be used to make things efficient and should be for everyone.”

At the start of the pandemic, a lot of physicians were worried about the prospect of telehealth and seeing patients over video, but thanks to enough leadership direction, good planning, and data, telehealth has thrived throughout the pandemic. But some things needed to be simplified.
“We realized we needed to make things simpler for the patient, user experience had to get better, and digital literacy had to get way better,” McElligott says. “The eighty-year-old living alone in rural South Carolina needed to know how to use this, so we had to figure out how to walk everyone through it.”
For the most part, telehealth has been recognized as an effective solution and is now being used by patients and providers in record numbers—even Medicare and insurance companies are on-board with payments. That’s been a big part of acceptance and adoption as well.
“At one point, over half of care was virtual at the beginning of the
pandemic,” McElligott explains. “What my job turned into is trying to help a whole enterprise figure out the strategy of what is the right amount. People are trying to figure out what telehealth can be used for and balance their spreadsheets to plan for the future.”
Looking ahead, McElligott expects to concentrate on some new technology shifts that are changing virtual health and working to make things more cost efficient and streamline the processes the best way possible.
“My job has gotten bigger, because everyone is using telehealth now,” he says. “I’ve been part of an amazing ride over the last decade or so, and for me, it’s really all about the mission.” AHL
Our mission is to support the recovery of people with mental illnesses. Our statewide network of centers, clinics, and hospitals are home to a talented team of psychiatrists, mental health counselors, nurses, case managers, administrative and support sta , who are passionate about helping people through recovery. We believe that with the right treatment and support, recovery is possible.

The South Carolina Department of Mental Health’s mission is to support the recovery of people with mental illnesses. The state’s public mental health system serves approximately 100,000 people each year, including children, adolescents, adults, and families, statewide. Founded in 1821, it is one of the largest hospital and community-based systems of care in South Carolina.
We want you to be a part of our team! It’s not just a job... it’s a CAREER with Purpose! Administration Building 2414 Bull St. Columbia, SC 29201
(803) 898-8581 | www.scdmh.net


Tabitha Safdi
The Feature 27
Dr. Jimmy McElligott (second from the left) speaks to other healthcare leaders during the Telehealth Summit of South Carolina.
As president of the UCLA Health Faculty Practice Group, Dr. Eve Glazier strives to accomplish one of the organization’s biggest goals to date: vaccinating its entire patient population
By Sara Verdi
Portraits by Tommy Garcia

28 AHL
The Equity in Immunity

The Feature 29
ot many people can say that they have the unique coincidence of working at their very own birthplace, but Dr. Eve Glazier’s career path has come, quite literally, full circle. “Apparently, I don’t believe in straight lines,” she says, laughing, “but I was born at a UCLA Health hospital.” Glazier now serves as president of the UCLA Health Faculty Practice Group. But before she completed medical school and landed her current role, Glazier took a few other turns on her career journey.
Glazier grew up in Los Angeles and attended UC Berkeley for her undergraduate degree. “I studied comparative literature, drama, and dance. Even though my father was a physician, studying medicine wasn’t particularly on my mind,” she notes. During her senior year, though, Glazier fell with a severe illness which required her to take a step back from her studies.
“When I returned to school and eventually graduated, I decided that I wanted to pursue medicine,” she explains. “I came at it from an emotional and attached place after thinking about all of the amazing medical care that I had received—I wanted to be able to give that back somehow. Because my personal attachment to medicine was based on the everyday care of patients and building those special relationships, I knew right away that I wanted to pursue a career in internal medicine.”
Glazier attended medical school at Columbia and went on to complete her residency in internal medicine back in LA. “After that, I found myself kind of where I started!” she jokes. Glazier began a primary care practice at UCLA Health, where she still works under limited practice, and little by little, she began to take on more leadership-focused positions within UCLA Health. In 2017, Glazier stepped into her current role as president of the UCLA Health Faculty Practice Group.
The Faculty Practice Group, at a high level, fosters the infrastructure that benefits all clinical providers that support the clinical enterprise for UCLA Health. As president, Glazier leads and oversees the multispecialty physician group and leads the UCLA Health organizational priority of directing the strategy for population health, accountable care, and value-based models.
“Over the past few years, in support of this priority, I have had the pleasure of establishing authoritative bodies of governance to ensure that UCLA Health can meet and sustain our population health management goals, which include improving access, cost, and quality across the enterprise all while meeting regulatory obligations,” Glazier explains.
While Glazier is involved with helping build strategy in several different areas of the organization, population health strategies have come to the forefront with the onset of the COVID-19 pandemic—especially surrounding vaccine distribution strategy. While this is new territory for Glazier and the teams at UCLA Health, previously implemented programs and initiatives have paved the way for a particularly successful distribution strategy.
Before the discussion of the overarching strategy and approach that UCLA Health has taken with the vaccine rollout can be had, it’s important to understand just how large UCLA Health’s integrated health system is and what sort of impact they have on the communities they operate in.
“In a very short time, we have grown from being an academic tertiary and quaternary medical center to being a primary care-based integrated health system. We now have more than two hundred outpatient clinical practices in addition to four high-performing hospitals. We also have six ambulatory surgery centers in the community, several outpatient imaging facilities, and
N
30 AHL

The Feature 31
Dr. Eve Glazier President of the UCLA Health Faculty Practice Group UCLA Health
provide hospitalist care at twenty-two community hospitals. All of these contribute to the population health and organizational strategies,” Glazier explains.
According to a program implemented by the Faculty Practice Group’s Office of Population Health, the patient attribution model, the team was able to identify more than 630,000 individuals that consider UCLA Health to be their primary care facility of choice. “This expansive footprint allows us to engage with our communities, secure an integrated approach, and advance our mission in health equity and provision of care to under-resourced communities as well,” Glazier says.
According to Glazier, the vaccine distribution program was driven by three guiding principles. The first was to distribute the vaccine in an equitable and orderly manner in accordance with the CDC and the public health agencies of California, the second was to leverage up-to-date clinical and social risk data, and the third was to frequently communicate with patients in complete transparency.
“This was really difficult at first, with all of the anxiety, confusion, grief, and loss that has accompanied the virus,” Glazier admits. “By the time we got to the vaccine rollout, it was so important that we stick to

these principles for an equitable and highly informative distribution plan.”
Due to limited inventory of the vaccine itself, it was crucial that Glazier and the teams at UCLA Health applied the aforementioned clinical and social risk model to stratify distribution until inventory was no longer an issue. Thanks to the patient attribution model, UCLA Health was able to focus on leveraging the information collected in that initiative to identify the most vulnerable populations to prioritize vaccination.
“We had an amazing multidisciplinary team that developed a risk model incorporating clinical and social risk data from patient data to assign individuals a risk score. It sounds complex, but it’s incredibly nimble—we update the data every day and align it as information from the CDC is released,” Glazier says.
When scoring patients, UCLA Health factored in everything from health records to home address, access to transportation, ability to self-isolate, socioeconomic status, education, minority status, and language. Each of these factors would give patients points to add to their overall risk score, and that risk score then informs UCLA Health of how invitations to vaccinate are then sent out to patients.
32 AHL
Once the eligibility of patients for vaccination was identified, UCLA Health had to determine best practices for communicating with them. “We tried to connect with our patients through multiple channels,” Glazier explains. “We used a general population approach via emails and texts to distribute information about the vaccines and invitations to vaccinate, but we had to recognize that not everyone had access to the internet or text messaging.
“For many of our populations we took a more targeted outreach, for example employing teams of people who could call patients to help them make appointments,” she continues. “We even had homebound outreach to administer vaccines in the homecare setting.”
At the time of speaking, providers in the US were administering more than 3 million doses of the COVID19 vaccine per day on average. So much of that work is because of people like Glazier, who think not only innovatively but inclusively to ensure that patients know how to get vaccinated and do.

“It has taken mammoths of activity to communicate and distribute this vaccine,” Glazier notes, “but I feel so grateful to have been part of such a dedicated team that has made these efforts to be completely transparent and successful.” AHL

“[Communication] was really difficult at first, with all of the anxiety, confusion, grief, and loss that has accompanied the virus. By the time we got to the vaccine rollout, it was so important that we stick to these principles for an equitable and highly informative distribution plan.”
The Feature 33
Where the Patients Are
Adrin Mammen and Jeffrey B. Short usher
Montefiore Health System into the golden era of healthcare’s digital transformation
 By Billy Yost
By Billy Yost
34 AHL
Every initiative, every measure, and every proactive move Adrin Mammen and Jeffrey B. Short have enacted is summed up by Mammen in one perfect quote: “Our stance has always been to meet people where they are.”
Mammen, who serves as Montefiore Health System’s associate vice president and patient access transformation officer, and Short, who serves as its vice president, transformation officer, chief of staff, and leader of the faculty practice physician group, have cultivated an enduring partnership that has created staggering results in just a short timeline.
Prior to the COVID-19 pandemic, Mammen and Short embarked on an extensive digital transformation journey on behalf of the health organization. “We had started putting a road map together to expand patient access, improve productivity, and drive patient satisfaction,” Mammen explains. “Once we established our priorities, we started mapping out sequentially what, why, and how it was that we wanted to accomplish. Then the pandemic happened.”
The Silver Lining of Pandemic Transformation

For most healthcare organizations, the pandemic meant the grinding halt of any projects or initiatives not explicitly related to fighting COVID-19. It might be because of Mammen’s Baldrige National Examiner training, her Lean Six Sigma Black Belt, or her Six Sigma Master Black Belt, but she and Short saw the situation differently.
“The pandemic accelerated innovation in many different sectors by as much as ten years. Healthcare was no different,” Short says. “Regulators quickly removed reimbursement and regulatory barriers, and our clinicians and patients were willing to try telemedicine out of necessity. Suddenly thousands of patients and clinicians were using telemedicine. This rapid adoption transformed healthcare from a face-to-face business to one that was now a mixed model that includes a large virtual or online segment.”
“The pandemic allowed us to leverage a lot of the great work that we had done, and to do it quickly,”
The Feature 35
Mammen says. Working nimbly, they were able to transform their already existing plan and, essentially, put it into overdrive.
A telehealth program often requires one to two years to properly stand up in most healthcare settings. At Montefiore, the organization went from five telehealth visits in 2019 to 637,000 from March to December of 2020 alone.
“Key to the progress that was made is the leadership structure employed during the pandemic,” Short notes. “A central command structure was set up that simplified decision making and allowed us to quickly make decisions and allocate resources to key initiatives.”
The transformation begs an in-depth study of its own, but Mammen pauses. “That was just telehealth.”
The success and blowup of the telehealth program got the transformation team thinking about the health system’s scheduling process. “We were trying to get more and more appointments scheduled online because we were setting up COVID-19 vaccinations and our phone lines were being flooded,” Mammen explains.
Defied Expectations
Mammen says embracing online scheduling meant deconstructing some long-held beliefs about Montefiore’s patient population. “Our patients are located in the Bronx in New York; they’re a very socioeconomically diverse population, and a lot of our patients don’t speak English as their primary language,” Mammen says. Right or wrong, the AVP says expectations suggested that Montefiore’s patients may not have internet access in their homes due to economic instability, and that a lack of digital literacy may keep its patients from engaging online.
“We needed to take the chance and try to meet people wherever they are,” Mammen says. “If they want to engage with us digitally, we’ll be there for them. If they want to engage with us over the phone, we can meet them there as well.”
Mammen, Short, and the transformation team quickly found that questioning long-held beliefs was the right move. Montefiore discovered not only were its patients engaging digitally, but it had patients engaging via mobile devices in huge swaths of the area. “We’re able to engage with our patients via SMS and mobile apps,” Mammen explains. “The first month we rolled out our telehealth mobile app, it was in the Top 100 of the Apple App Store’s healthcare section.”
“The acceleration of online visits allowed us to engage patients and clinicians and create rapid learning cycles. We quickly gained insights on how to improve the experience and the process,” Short adds. “We learned about the importance of the ability to launch a visit without the need to download an app first. We also learned how vital in-visit translation was for our diverse patient base. The learnings came quickly, and we were able to react quickly.”
So, the transformation team went further. A chatbot was installed on the Montefiore website that uses artificial intelligence to help patients find the information they need quicker. Specifically, conversational AI enables the chatbot to update in real time with new information about the pandemic, vaccinations, or more common queries.
“We didn’t have to go in and change code every time we needed to update information, because the AI was doing it for us,” Mammen explains.
With that, the transformation team returned to its goal to help patients not only find information about their doctors or treatment on its website but also schedule appointments without picking up the phone. In August of 2021, Montefiore rolled out an interactive online directory that will allow patients to identify the appropriate physician based on their condition or specialty.
“We will use clinical focus terms to match patients with providers based upon their clinical need, using layman’s language,” Mammen says. “You can search
36 AHL


 Jeffrey B. Short VP, Transformation Officer, Chief of Staff, and Leader of the Faculty Practice Physician Group Montefiore Health System
Adrin Mammen AVP and Patient Access Transformation Officer Montefiore Health System
Jeffrey B. Short VP, Transformation Officer, Chief of Staff, and Leader of the Faculty Practice Physician Group Montefiore Health System
Adrin Mammen AVP and Patient Access Transformation Officer Montefiore Health System
The Feature 37
Karla Esqueche Altamirano (Mammen), Courtesy of Montifiore Health System (Short)
for ‘diabetes’ or ‘back pain’ and will find who you’re looking for.”
“We are thrilled that Montefiore Health is advancing their digital front door using symplr Directory,” says Tom White, CEO and founder of Phynd and now general manager of symplr, which acquired Phynd in February 2021. “Adrin is a visionary patient access and transformation leader and is driving Montefiore to deploy a modern digital patient experience using the symplr provider data platform. Our partnership will help Montefiore Health fulfill their mission and bring operational efficiencies to their entire enterprise, strengthening Montefiore’s position as a healthcare leader in the New York City area.”
That’s only phase one. Phase two will include the ability to self-schedule an appointment online. By the end of the year, Mammen hopes 5 to 10 percent of Montefiore’s appointments will be scheduled online.
Proactive Care
“I believe we are currently in the ‘golden age’ of healthcare,” Short says. “The present healthcare marketplace, due to the COVID-19 pandemic and other contemporary factors, is hungry for change in terms of digital transformation.

“Patients simply demand what the banking and travel industries have given them: self-service, on-demand access,” he continues. “Now we must deliver the ability to schedule medical appointments just as easily as people can check their bank balance or book a flight. These are things we at Montefiore are already actively working on.”
Mammen says Montefiore’s goal is to reduce the demands on patients while simultaneously improving their health outcomes. If an economically struggling patient can receive the care they need via a telehealth visit—one that will not require them to take a half or whole day off work—Mammen and Short want to make it happen. If the health system can find ways to engage with patients proactively to receive automatic communications to schedule their next appointments or refill a prescription, Mammen and Short want to make that happen, too.
And for the transformation team at Montefiore, it’s about far more than wanting. The team is already down the path.
“There are so many ways that I think we can be more proactive about managing our patients’ care,” Mammen says. “It’s something I’m thinking about all the time. And I really think we’re going to do it.” AHL
38 AHL
“We needed to take the chance and try to meet people wherever they are. If they want to engage with us digitally, we’ll be there for them. If they want to engage with us over the phone, we can meet them there as well.” —Adrin Mammen

The Intersection of Data

Mohamed Humaidi relies on his industry experience and data analytics expertise to optimize business practices and upgrade patient care at Franciscan Alliance
By Natalie Kochanov
40 AHL
and Point of Care

Mohamed Humaidi dreamed of becoming a doctor for years before he immigrated to the United States after high school. However, with no knowledge of English or a familial support system in the country, he soon recalibrated. He put medical school off the table, enrolling instead in an undergraduate program in computer information systems on the recommendation of a friend that he met in an English as a Second Language course.
A chance offer to join health insurance provider MetroPlus Health Plan as a part-time customer service representative while he was in school connected Humaidi with the healthcare industry, albeit in a different capacity than he had once hoped. “That was my first opportunity to work as a data analyst,” he says. “It showed me that I could help patients in many different ways.”
The intersection of information systems and healthcare proved to be a perfect place for Humaidi to build his career. As the culmination of his upward trajectory since that initial customer service role, he currently serves as vice president of healthcare data and analytics at Franciscan Alliance. At Franciscan, a healthcare system operating out of Illinois and Indiana, Humaidi leverages his two decades of industry experience to enhance business practices and patient care alike through data and technology.
From the start, Humaidi demonstrated an aptitude for data analytics. He climbed the ranks within MetroPlus before doing the same at fellow insurance organizations EmblemHealth and Affinity Health Plan, where he held his first director-level position.
The Feature 41
In 2015, Northwell Health—New York’s largest healthcare provider— recruited Humaidi as assistant vice president of accountable care analytics. “They needed someone to develop their operation health capabilities,” he explains. “I grew the team from the ground up and built a state-of-the-art data structure foundation for claims data warehousing and care management.”
Humaidi remained at Northwell for over four years, during which time he received a promotion to VP status. He stepped into a vice president of analytics role at Franciscan in late 2019 and gained his current title shortly thereafter.

“My role is to build our analytics enablement capabilities,” Humaidi says of his
current duties. “I’m working with payers to enable more frequent data processing so that we can develop a 360-degree view of patients for our physicians to access at the point of care.”
The 360-degree view encompasses not only Franciscan’s patient data but also claims data and social determinants of health data—information that Humaidi believes will assist doctors in caring for patients before they even fall ill. With more data at their fingertips, doctors can take a wider range of factors into account when providing medical advice.
Humaidi further advanced Franciscan’s ability to conduct population health analyses by establishing a claims data warehouse similar to the one that
he set up at Northwell. He has also introduced new querying and visualization tools, retired outdated legacy systems, and engaged enterprise cloud data management company Informatica to help streamline organizational processes and promote data quality and integrity.
But before he could begin achieving his objectives at Franciscan, Humaidi first needed to assess and restructure the team that he inherited upon his arrival at the organization. In addition to bringing in new leaders and talent as necessary, he broke down the team into three groups: data management, strategic advanced analytics, and clinical. “The three teams work very closely together to support the business needs,” he notes.
Humaidi personally stays abreast of business needs through regular meetings with Franciscan’s senior leadership regarding their strategic goals. He recently implemented a dashboard of quality measures to assist organization leaders in gauging progress toward those goals as well as overall performance across various categories, further enabling Franciscan to become a leader in healthcare outcomes.
Beyond long-term planning, Humaidi collaborates with operational leaders to prioritize immediate work efforts based on available resources—contributions that have mattered all the more since the onset of the COVID-19 pandemic. COVID amplified the demand for data as well, leading Humaidi to focus on patient tracking with the aim of improving treatment and support. He brought together members of the coding and documentation teams along with healthcare providers, technicians, and nurses to ensure the standardization of information system-wide.
Mohamed Humaidi VP of Healthcare Data & Analytics Franciscan Alliance
Rajaa
42 AHL
M. Humaidi
In general, Humaidi views data and technology as key facilitators of collaboration. At the same time, he understands the role that people play in unlocking the full potential of such resources. “Data without tools, technologies, and people is not an asset. But data with tools, technology, and people can become an asset for any organization,” he says.
As he pushes for Franciscan to invest in the human side of the equation moving forward, Humaidi plans to continue growing the organization’s technological footprint. In particular, he has secured approval to build a data lake and a data hub to consolidate data from scattered sources. The project will underpin Franciscan’s upcoming artificial intelligence initiatives and solidify the organization’s predictive analytics capabilities. Moreover, Humaidi will be able to resolve issues and address business needs more efficiently, to the benefit of patients who depend on Franciscan for care.
“It’s critical for healthcare providers to get the data that they need to act with appropriate insight at the point of care,” Humaidi emphasizes. “We want to be more proactive in taking care of the population that we serve so that we can provide the best possible care in real time.”
He may not have become a doctor himself, but Humaidi demonstrates every day the possibility of improving patient care from behind the scenes— one piece of data at a time. AHL

KPMG LLP helps organizations work together in new ways to transform and innovate the business of healthcare. We offer a portfolio of services focused on helping our clients comply with regulatory change, improve healthcare outcomes, embrace IA and AI, adapt to healthcare consumerism, and transact to gain market entry.

“We want to be more proactive in taking care of the population that we serve so that we can provide the best possible care in real time.”
The Feature 43
Where Science


44 AHL
Wendy Xia brings her emphasis on building and maintaining relationships to Agios Pharmaceuticals, where she helps strengthen connection between the company and the patients it serves
 By Billy Yost
Portraits by Tony Luong
By Billy Yost
Portraits by Tony Luong
Meets Heart

The Feature 45
The idea of work/life balance, no matter how popular the topic may be today, is still a relatively new concept. The “rise and grind” culture has been at the center of industries worldwide for as long as they’ve existed. It’s led to countless innovations, breakthroughs that have helped make the world much smaller, and everyday occurrences that, just decades ago, would have seemed like Herculean undertakings.
But devout dedication to the job, and nothing but the job, took its toll. The idea of a family life was often just a vague concept, a limited understanding of the few hours not spent on the clock. The eighties and nineties saw women granted at least a small share of that same lifestyle, but Wendy Xia quickly found that it wasn’t the kind of pace that would fulfill her.
The now vice president and head of supply chain at Agios Pharmaceuticals would transition from process and analytical chemistry positions because she couldn’t bear the thought of her daughter consistently being the last one picked up from daycare. With a husband working eighty hours a week to finish his postdoctoral studies, Xia knew that her family deserved more, and she knew in her heart that it was what she wanted as well.
Xia has accomplished a great deal in her career in roles at the Schering-Plough Institute, Merck, and Novartis, and has done so on her terms. “I think moms
tend to be overachievers,” Xia says. “I don’t think we should feel so guilty that we can’t always be perfect in everything that we do.”
Through extensive growth as a leader, the Shanghaiborn Xia has managed to make it look fairly seamless. And after a blitz of promotions at Agios, the VP is able to connect to patients, colleagues, and her family with a masterful balance.
Direct Connections
Coming to Agios was initially a shock for Xia. Recruited for an interview after just a year at Novartis, she couldn’t believe what she saw at the organization. “I arrived for my interview, and people were wearing shorts,” Xia says, laughing. “I swear that I saw people walking around wearing flip flops. At Merck, you could wear jeans, but typically on Fridays.”
During that same interview, Xia saw a different aspect of the culture at Agios that would help her make up her mind to transition there. “We went to the cafeteria and there was a ‘lunch and learn’ with a professor from Harvard,” the VP remembers. “It was an informal brainstorming session, and I just remember thinking that this was a place where I could have a blank canvas. I could bypass so much of the red tape that occurs in Big Pharma and have a more direct connection with our patients and our people.”
46 AHL

The Feature 47
Wendy Xia VP and Head of Supply Chain Agios Pharmaceuticals
After accepting the job, Xia got to work. As Agios’ first supply chain professional, she built the clinical supply chain from scratch to support the company’s clinical trials. When that was finished, she built a commercial supply chain to help the organization market and sell drugs, and in 2017 she led Agios’ first commercial supply launch (Tibsovo) in record time.
When it came to the pandemic, Xia notes that while tending to supply chain challenges was her initial concern, leadership became much more focused on employee experiences as the lockdown months continued. The Agios team had already successfully piloted hybrid work environments, but it was concerned about the potential burnout of employees working too many hours at home on top of tending to duties like childcare and homeschooling for parents.
“We wanted to make sure that we were still connecting and relating,” Xia says. “We wanted to make sure our people were balanced physically and mentally and still finding ways to interact about more than just work.”
Xia says Agios’ focus on creating virtual events and welcoming new hires with as much of a human touch as remote interaction allowed helped keep the organization feeling like a family.

People Come First
Though she has built so much in her time at Agios, the enduring value Xia gets from her role derives from the company’s patient-centric mindset. The pandemic offered an especially powerful example of this mission.
A patient in one of Agios’ global trials was making consistent trips from his home in Cairo, Egypt, to
48 AHL
“You cannot feel guilty about making sure you take the time you need to attend to your life. . . . you have to let go of the guilt that you’re not measuring up to that high bar we all burden ourselves with.”
MD Anderson Cancer Center in Texas for treatments.
With plane and international travel in various stages of intermittent shutdown, Agios wanted to make sure the patient’s lifesaving treatment was still delivered.
“It was a huge challenge for us to deliver medication to him from the United States,” Xia explains. “We had to have a special agent personally carry the medication, board an aircraft, and meet his family members at the airport in Cairo before it was shut down. We were able to eventually ship his treatment, resupply medication, and conduct his office visits virtually, but I think those efforts just underline what makes Agios so special.
“While the pandemic did present many unprecedented challenges to supply chain, some of the mitigation methods, such as direct-to-patients, are gaining more ground to offer more flexibility to patients and clinical sites,” she continues. “We are actively working with our clinical operation colleagues and engaging in conversation with regulators and industry-leading groups to hopefully make these changes in a permanent fashion.”
Agios further proves its patient-centric mindset through its continued support of individual patients far after their clinical trials have ended. If patients take particularly well to clinical trials that later go into production in differing doses and delivery, Agios will continue to provide that same medication for patients because they don’t want to disrupt the positive outcomes from what may be an evolved process or dosage after the trials process has been completed.
“Wendy’s knowledge, professionalism, and focus on patient centricity are visible in all the interactions we have with her,” says Fiona Geiger, vice president of client services at Yourway. “She thrives to find perfect solutions. As a service provider, knowing how Wendy expects nothing but the best, we feel honored to work with her to create effective solutions to ensure the studies under her command are flawlessly supported.”
This catered care is a costly and individualized effort, but Xia says it’s one of the many reasons she calls Agios home. And with a wall in Agios’ office adorned with the
A CULTURE THAT CARES
As a Chinese immigrant, Wendy Xia says she is continually optimistic about the growing representation of background and experience in her industry. While she routinely found herself both the only woman and the only person of Asian descent in meetings earlier in her career, she believes the social awakening of the past few years has helped move along issues of diversity and inclusion. That goes double for Agios.
The company has bolstered its community outreach and diversity awareness initiatives to show its allyship and support toward the people it serves. It hosts panels on the Black Lives Matter (BLM) movement and Asian American Pacific Islander (AAPI) hate crimes, and also collects and delivers donations to the local Boston Children’s Hospital.
“It’s not just BLM, or AAPI, or LGBTQ+ groups we’ve established,” Xia explains. “While our diversity council is doing great things, it’s the culture here that enables these things to grow and flourish.”

The Feature 49

50 AHL
portraits of hundreds of the patients they’ve protected (p.109), Xia is reminded of and motivated by that lifesaving mission every day.
Room for More

Xia says that despite opting for more regimented hours in her career early on, she hasn’t felt punished in her career for making more time for her family— and she hopes it’s a path more working parents are willing to follow.
“I think the standards moms hold themselves to couldn’t be done any better by any man,” the VP says, laughing. “You cannot feel guilty about making sure you take the time you need to attend to your life. There are times that you need to prioritize. Sometimes it will be work, sometimes it will be your family, but you have to let go of the guilt that you’re not measuring up to that high bar we all burden ourselves with.”
Xia says her own growth has been the result of many things, including amazing mentorship (like guidance from former CEO and current Chairman David Schenkein), HR-supported personality analysis, and the Women’s Leadership Circle group she has been part of over the years. “There are so many working moms out there, and it’s important that we connect,” Xia says. “Join a local group, join a Facebook group, get the support that you need and deserve to be happy and fulfilled.”
Just a year ago, Agios renovated its cafeteria. It’s a place that serves as much as a meeting room as it does an eating room. A bright blue sign was hung at the head of the room, saying simply, “Gather.” It’s in this last piece of Xia’s advice that we can see the commonality between her approach to life and Agios’ mission: fostering community and building relationships. Which, for Xia, makes sense. As the head of supply chain, connection is exactly her forte. AHL
“We wanted to make sure that we were still connecting and relating. We wanted to make sure our people were balanced physically and mentally and still finding ways to interact about more than just work.”
The Feature 51
Roots


Keeping in the Community 52 AHL
What happens when doctors prescribe fresh fruits and vegetables instead of medicine? The Farm on Ogden tests that out, while providing Chicago’s North Lawndale community so much more.
By KC Esper
 Photos by Gillian Fry
Photos by Gillian Fry
All the plants grown at the Farm on Odgen—and the fish that work to fertilize those plants—are visible through glass walls. The goal is to enable the community to see how lettuce like this is produced and make a connection to where their food comes from.

The Feature 53
▼ Dr. Wayne Detmer and Angela Mason were adamant about fixing this old Sherwin-Williams building rather than starting from scratch. “Part of our reasoning for not tearing down the building is because it sends a message to folks who spent their whole lives here that the way to fix the neighborhood is to destroy it, as opposed to saying, ‘Let’s restore this and maybe make it better than what it was before,’” Detmer says.
▼ As the crow flies, the closest commodity grocery store in this community is a mile and a half away—usually requiring two bus transfers to get there. Corner stores are closer, but their produce offerings are sparse and expensive. The Farm greatly increases access to fresh food.
When Angela Mason and Dr. Wayne Detmer met, it was an instant partnership. Both were hyperinterested in urban farming, combating food insecurity, and improving health outcomes. They combined their passions and their resources at the Chicago Botanic Garden and Lawndale Christian Health Center respectively to start the Farm on Ogden, an aquaponics farming operation in the heart of North Lawndale, a neighborhood that sits on Chicago’s West Side.
The Farm on Ogden’s mission is to not only provide a community center—full of health and educational resources, fresh foods, and job opportunities—in a historically under resourced neighborhood, but to also reframe the narrative about North Lawndale, as an area teeming with motivated, close-knit individuals. AHL


▲ Mason says the goal is to not only offer healthy, fresh food but to encourage people to think differently about vegetables. Many community members have never been introduced to such an abundance of edible plants, so having a variety helps expand their palate, nutrients, and diet.

54 AHL
▲ The Farm on Ogden produces more than 100,000 pounds of produce every year that is either distributed elsewhere or sold in its retail setting.



The Feature 55
▶ Anyone can purchase goods from the Farm’s retail store. The team tries to keep the rotation fresh and relevant to the community, bringing in items that they can’t grow themselves like avocados and dried beans. During the pandemic, it even started offering toilet paper and other hygiene products that were scarce.

 Angela Mason AVP of Community Engagement and Senior Director Windy City Harvest
Dr. Wayne Detmer Chief Clinical Officer of Operations Lawndale Christian Health Center
Angela Mason AVP of Community Engagement and Senior Director Windy City Harvest
Dr. Wayne Detmer Chief Clinical Officer of Operations Lawndale Christian Health Center
56 AHL
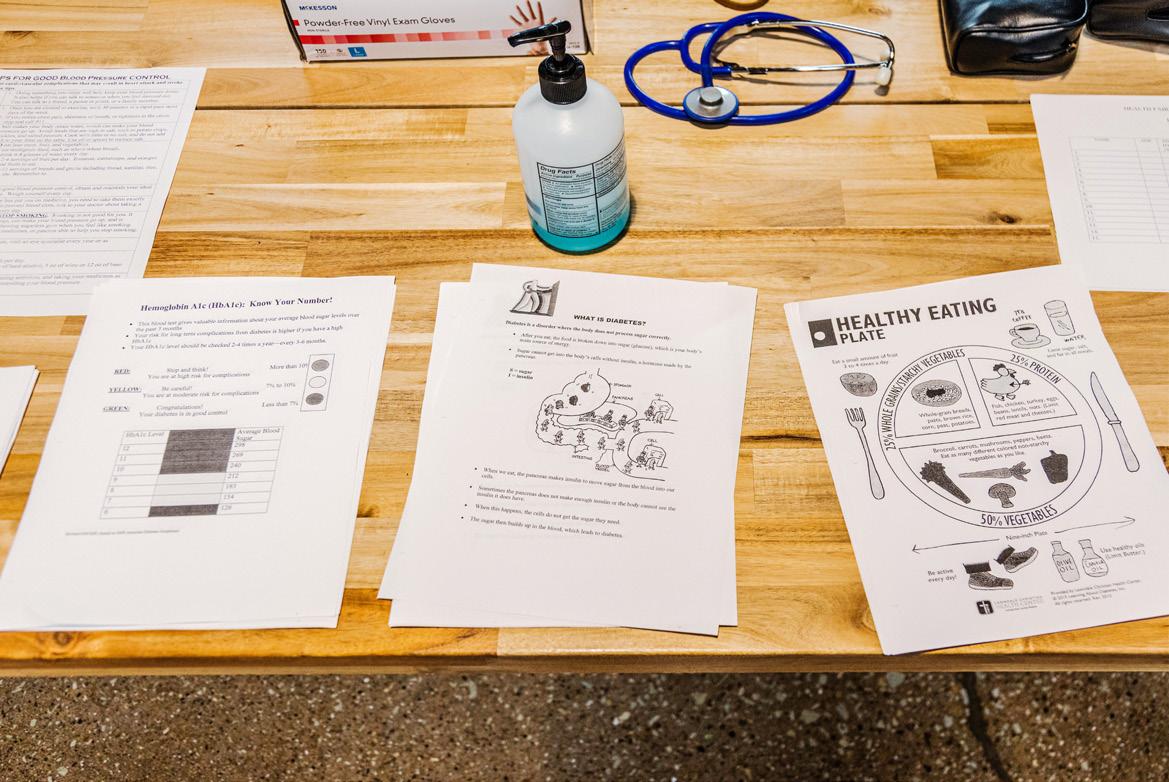
▲ Community members can use these tables to check their blood pressure and get information on how to manage their health at home.

▼ First-year medical students volunteer at the Farm through a six-week program. Detmer says that having students closely interact with North Lawndale community members gives them a better perspective early on of how to approach healthcare more holistically rather than turning to pharmaceutical remedies.

▲ Free health fairs like this one pop up frequently throughout the year. Prior to the pandemic, the Farm space also hosted cooking demos and informational classes—offerings that Mason and Detmer hope to resume in the next year.

The Feature 57
▼ These UV lights enable the Farm to grow more produce, quicker and year-round. They also use a lot less energy than traditional bulbs, which coincides with the Farm’s sustainability mission.

▶ Detmer and Mason also fought for these lights so that the Farm would glow a mellow purple color at night, serving as a beacon any time of day and giving the neighborhood a distinctive landmark.

58 AHL
All the produce grown at the Farm on Ogden is through a highly sustainable aquaponics system. Fish—in this case, tilapia—produce waste, which is then sent through a series of filters until the nutrients are stripped from it and returned into the water. This allows lettuces to grow without soil and without discarding any water or using any chemical fertilizers.




◀ Some of the water filters through this rock bed before heading into the lettuce baths. The high surface area of these rocks—coupled with the work of some worms who live beneath them—allows the water to oxygenate, creating a chemical reaction that transforms nitrogen into a more easily absorbable nutrient for the plants.

The Feature 59
▲ The Farm on Ogden is affiliated with the Chicago Botanic Garden and is part of the network that makes up Windy City Harvest. Every year, the Farm produces more than 70,000 starter plants for other plots to use across the Chicago.

▶ There are currently seventeen farm sites in the Chicagoland area that source their starter plants from the Farm on Ogden. Affiliated farms are as far north as Waukegan, as far south as Washington Park, and as far west as Austin.

60 AHL
▼ Andy McGhee is the mastermind behind the aquaponics system. Right now, the Farm’s greenhouse is growing at halfcapacity. In the future, the team hopes to have a multilevel growing system operating to produce more goods.


▲ Local high school students can come work at the garden from May until mid-October. The goal is to positively engage them civically, give them job experience, and help them learn about healthy eating.

▼ These walk-in coolers store leftover produce that kitchen staff at the Farm turn into high-value items, like salsa and jam, which customers can buy in the retail store.

The Feature 61
▲ Through VeggieRx, patients with high blood pressure and diabetes get ten boxes of vegetables, coinciding recipes, and coupons to the Farm’s retail shop, all paid for by their health insurance. After the tenth box, they’re encouraged to go back to their doctor to monitor their progress.


▶ The Farm on Ogden is concerned about all aspects of health, providing the community with not only fresh food but also second chances, job training programs, and a safe gathering space for anyone in the neighborhood. Detmer and Mason believe that achieving this mission will enhance the livelihood of North Lawndale’s population and serve as inspiration for future projects.
◀ The Farm’s partnership with Lawndale Christian Health Center enables it to reach the community by way of their doctors in a program called VeggieRx, which prescribes fruits and vegetables instead of medicine. Prescriptions for VeggieRx tripled during the pandemic, giving a lot more people easy access to fresh foods.

62 AHL
The Path
Every step executives take on their career journeys is pivotal to achieving their current successes. Along the way, individuals accumulate technical skills, foster relationships, and develop the leadership acumen that have turned them into pioneers of the industry.
64. David Jones Stanford Health Care
70. Catherine Garvey Goldthorpe University of Chicago Medical Center
63
74. Andrew Parker Papa
HR of a High Caliber

64 AHL
David Jones built his whole career on transforming complex organizations. Now, the respected CHRO is helping Stanford Health Care attract and retain the very best.
 By Zach Baliva
By Zach Baliva
Portraits by Gillian Fry
David Jones CHRO Stanford Health Care
The Path 65
On November 17, 2019, Stanford Health Care was ready to open its new 824,000-square-foot facility. It was a special day ten years in the making. For David Jones, the celebration was better than a trip to Disney World. The chief human resources officer rushed from floor to floor, helping other administrators cut ceremonial red ribbons and give tours. Public officials, donors, and other VIPs gathered in the atrium, where Jones’s colleagues high-fived as they celebrated the long-awaited opening of the facility. Three hundred patients came into the new hospital, but none of them came alone. They each had a dedicated nurse right by their side.
Stanford Health Care first announced the project in 2006. Jones says the opening was so special because of what it represented. “It took so many people working together to get to that point, and a world-class hospital and top-level employees together help Stanford continue to lead and change healthcare globally.”
Jones came to the organization in 2017 to help build a more engaged and effective workforce, and he has a long track record of driving big results. Jones took his first CHRO-level position at the age of twenty-six, when another departing leader recommended him to lead the medical center HR function and provide strategic oversight at a small community hospital. There, Jones got a front-row view as a new CEO pushed his leadership team to implement robust continuous quality improvement methodologies.
“It set me on a course I never imagined because I saw at the very onset of my career how HR was a strategic business function,” Jones explains, adding that he was tapped to promote high employee involvement as part of an organizational transformation.
Suddenly, Jones found himself working with an outside firm to complete a multiyear change process.
66 AHL
The Path 67
“We got tangible results to help improve the performance of the organization, and I saw that it was done through people and HR systems. The formative experience became the launching pad of my career .”
TALK ABOUT IT
After three decades in healthcare HR, David Jones is becoming a sought-after conference speaker. He’s lectured in Los Angeles, Rome, and everywhere in between on topics ranging from HR strategy and transformation to change management and crisis fatigue. In sharing his experience, perspective, and expertise, Jones says he hopes to inform and inspire audiences and help HR leaders discover how they can build world-class HR functions and strategies that will help their organizations not only advance but thrive. Jones has also published several academic articles and contributed to two books.
Together, they identified the top twenty business and quality issues the hospital needed to improve. Next, they assigned each issue to teams with dedicated leaders trained in a new quality process. While other hospitals were certifying a few people to lead everything related to quality, Jones and his team took a different approach and trained all leaders to use quality tools and track results.
It worked. The organization reduced the length of stays and improved customer satisfaction, productivity, cost savings, and other key metrics. “We got tangible results to help improve the performance of the organization, and I saw that it was done through people and HR systems. The formative experience became the launching pad of my career,” Jones says.
When a new chancellor recruited Jones to help drive change across the academic and clinical enterprise at the University of Nebraska Medical Center, the rising leader was put on the national stage alongside top faculty leaders and hospital executives. Jones continued to develop his skills, but after four years, he had a revelation. “I had only worked in healthcare, and I wanted to see how my skills would play in a different industry,” he explains.
Jones went to Ameritrade to lead a hypergrowth process at what was then one of the world’s fastest-growing internet companies. At the height of the dot-com boom, Jones filled Ameritrade’s C-suite with high-caliber tech and financial services leaders, tripled the company’s workforce, and staffed important new offices, including a 1,500-seat call center.
Although he enjoyed the experience, Jones returned to healthcare, where he continued to provide the transformational leadership that built his reputation. Stanford’s quest to build and open the most tech-advanced hospital in the world is part of what drew him to the organization in 2017.
“I like coming in when there is a lot of change and organizations are about to do something really
68 AHL
special,” Jones says. Additionally, he saw the chance to make an impact. When Jones stepped in as CHRO, Stanford was receiving high marks on customer satisfaction and quality.
“Stanford Health Care takes on some of the world’s most challenging medical conditions,” says Susan Guerra, chief customer officer at Collaborative Solutions and partner of Stanford Health Care. “Its focus on delivering excellent patient care while using innovative technology sets them above all.”
Jones knew, however, that the organization needed to elevate the people experience to match the patient experience. So he leveraged his extensive HR expertise to help Stanford Health Care attract and retain the best talent in the nation.
Jones gathered performance data to establish his road map to transform and rebuild Stanford Health Care’s HR function and simultaneously focused on staffing the organization’s new hospital. Some new tools have helped during the heavy lift. A new employee engagement process helps managers identify employees’ strengths, while a specialized app helps workers check in with their leaders.
Stanford’s HR teams were just starting to see results when the coronavirus pandemic threatened to derail their progress. “COVID-19 brings so much uncertainty to the function and the health system, and we decided to meet the challenge head-on,” Jones says. He reorganized the HR function around six new workstreams to align with the business response to COVID and a suite of services to help employees navigate concerns related to personal safety, childcare, new training, and other areas.
Since the onset of the pandemic, about two thousand team members, including physicians and staff members, have been infected by the virus. Many have opted into Stanford’s new program, which provides meal delivery, hotels for family members, emotional support, spiritual counseling, and other services coordinated by a personal case manager. These and other efforts distinguish Stanford in the marketplace and help with satisfaction and retention. During Jones’s tenure, the organization has seen turnover drop from 11 to 7 percent.
Today’s leaders in business and healthcare often talk about the VUCA world we live in—a world full of volatility, uncertainty, complexity, and ambiguity. Constant change seems to be the new norm. And in the medical world, a strong HR function and an engaged workforce are the only antidote. AHL
“COVID-19 brings so much uncertainty to the function and the health system, and we decided to meet the challenge head-on.”
The Path 69
A Nurse at Heart
Catherine Garvey Goldthorpe combines an attorney’s acumen and a caregiver’s compassion to defend healthcare providers at the University of Chicago Medical Center
By Natalie Kochanov
I
n 2016, Catherine Garvey Goldthorpe accepted her current role as associate general counsel and executive director of the professional liability plan at the University of Chicago Medical Center, which is part of the UChicago Medicine health system. However, she had first worked for the academic medical center decades earlier—as a registered nurse.
“Nursing is my love,” Garvey admits. “I have always kept my license active and will always be a nurse.”
Beyond maintaining an active nursing license, Garvey applies a caregiver’s perspective to her current work as an attorney. She empathizes deeply with the
healthcare providers at UChicago Medicine to whom she provides legal counsel. As a result, she seeks to make them more comfortable when defending a lawsuit. She shares wisdom learned from past experiences with colleagues across the health system with the end goal of improving patient care.
Garvey initially joined UChicago in 1984 after completing an undergraduate degree in nursing at the University of Illinois at Chicago. She enjoyed her duties as a staff nurse and considered pursuing a graduate degree in the field but settled on law instead to increase her opportunities for career advancement.
70 AHL
 Catherine Garvey Goldthorpe Associate General Counsel and Executive Director of Professional Liability University of Chicago Medical Center
Catherine Garvey Goldthorpe Associate General Counsel and Executive Director of Professional Liability University of Chicago Medical Center
The Path 71
Matt Schademann
72 AHL
“To me, the most rewarding part of this job is when I can alleviate a provider’s anxiety about being involved in the legal process . . . so that they can focus on our patients.”
For the next four years, Garvey attended night school at DePaul University while continuing to serve as a nurse at UChicago’s Wyler Children’s Hospital (now Comer Children’s Hospital). While there, she instituted a day treatment room, which allowed pediatric cancer patients to begin receiving treatment upon arrival while waiting for bed availability. “We were just starting all of the transplant programs at the University of Chicago,” she explains. “It was a very exciting time to be working at the hospital.”
Once she completed her JD, Garvey left UChicago Medicine to practice law. She spent twenty-five years defending medical malpractice lawsuits at a Chicagobased litigation law firm before starting her own firm, Brennan Garvey (now Brennan Burtker), in 2015. When she returned to UChicago Medicine the following year in her current capacity, she brought with her a wealth of malpractice defense expertise that she now exercises for the benefit of providers and patients alike.
Five years into the position, Garvey has found that no two days at UChicago Medicine are the same. “You think that you’re going to do one thing when you get to work in the morning, but then the phone rings and you get steered in a different direction,” she confirms. “But that is
what I love about
this job!”
Fortunately, Garvey thrives on the varied nature of her role. She oversees all claims and litigation and provides advice on a varied and unique array of legal matters to providers throughout the system. In addition, she collaborates with the medical staff office on privileging issues and works closely with the risk and patient safety team. “We work hand in hand investigating adverse events that happen at the hospital, both to make changes to improve patient care and identify events that could result in litigation,” she elaborates.
With years of trial experience, Garvey remains actively involved in lawsuits filed against the hospital. She coordinates with outside counsel on defense strategy and attends pretrials and mediations to settle certain cases outside of court.
Just as importantly, Garvey strives to reassure providers facing legal action. “Because of my nursing
background, I know firsthand what it would feel like if someone were to suggest that maybe I hadn’t provided the best possible care to a patient,” she says. “It’s stressful to be named as a defendant in a lawsuit or to be asked to give a deposition. I want to be as supportive as I can to our providers, making sure that I provide them the best possible representation. I want to help them navigate the legal process so that they can remain focused on patient care.”
Garvey understands that the trial process can be incredibly stressful and time-consuming to a healthcare provider. “Over the years, I’ve known excellent physicians that have left the practice of medicine after living through a negative trial experience,” she says. As a result, she regularly conducts “trial postmortems” as a way to share the trial experience and educate and support other providers at UChicago Medicine who may find themselves in similar circumstances.
Furthermore, Garvey delivers lectures across the health system to educate doctors on the law and how it pertains to particular subspecialties. Although she looks at each case with fresh eyes, she also tracks recurring issues in the interest of avoiding similar problems. By keeping providers informed of possible pitfalls and providing legal guidance, she facilitates their efforts to provide excellent patient care—an aim that will always resonate with her, as a nurse at heart.
“I understand what it feels like from their end,” she says. “To me, the most rewarding part of this job is when I can alleviate a provider’s anxiety about being involved in the legal process—something that’s very foreign to them—so that they can focus on our patients. I help them navigate this unknown legal world.” AHL
Aon congratulates Catherine Garvey Goldthorpe for this welldeserved recognition; we are honored to call you a partner and friend. Aon is a leading global professional services firm providing a broad range of risk, retirement, and health solutions. We empower results for clients by using proprietary data and analytics to deliver insights that reduce volatility and improve performance. To learn more, visit aon.com.
The Path 73
A Helping Hand on Demand
Andrew Parker started Papa, a digital assistance matchmaking platform, to make the quest for help seamless and easily accessible
By Charlotte Foer
74 AHL
 Andrew Parker CEO and Founder Papa
Andrew Parker CEO and Founder Papa
The Path 75
Courtesy of Papa
Andrew Parker was working at a telehealth company for seven years before he launched Papa, a digital assistance matchmaking platform. His father and grandfather were both entrepreneurs, and he dreamed of someday owning his own business. He just needed to find a niche that hadn’t been tapped into yet. That niche turned out to be closer to him than he thought.
Over a Zoom call, Parker holds up a framed photograph of three generations of men in his family. “I originally started this company as a way to help my grandpa, who we call Papa,” he says, pointing to the man in the middle of the picture. “He needed support and assistance driving, cleaning the house, and just someone to hang out with.”
Parker’s grandfather was elderly but still independent. He could take care of himself and live on his own but could use some help doing chores and picking up groceries. More importantly, he could use a friend—someone he could rely on while his family was busy at work or with their own kids. Recognizing that his grandfather needed more time than he could provide, Parker created a post on Facebook asking if any of his friends were available to hang out with Papa for $20 an hour.
“He loved his pal,” Parker says. “She was a girl named Andrea. She had come from Venezuela, and Papa came from Argentina, except sixty years before her. But they could relate that way. She didn’t come in a nursing outfit—she was wearing a T-shirt and jeans—and they became like best buddies.”
That trial run served as a foundation for Parker to build a larger company that matched older adults with buddies—or “Papa Pals,” as they’re lovingly referred to in the business. With Parker’s background in telehealth,
he knew how to leverage technology to deliver a good healthcare experience in a new way. So, he created a prototype and strung together a small sample of people who were willing to use it.
“Everyone had the same reaction—they really loved it,” he says. “I remember reading an article that said its more important to have, say, a hundred people who really love what you’re building than to have millions of people who download your product and never use it. I didn’t have one hundred, but I had ten, and that was good enough for me.”
Parker quit his full-time job and plunged all his efforts into creating the Papa platform. Now, Papa has four hundred full-time employees, twenty thousand Papa Pals, and about a million members who have access to Papa’s services through their health plans for no additional cost. The company has even expanded to include families on Medicaid to help with things like childcare and housecleaning.
Pals go through a series of personality tests, background checks, phone screenings, and training sessions before they’re ready to be linked with a member. During these early sessions, they’re trained on everything from how to use the app to how to respond when a member discusses serious topics like depression—and even how to get a member glasses if they mention needing new ones. Once the member is matched with a Pal, they can request specific services that meet their needs, such as scheduling doctor’s appointments, picking up medication at the pharmacy, setting up reminders to take those medications, and simply socializing.
“We’re not just providing partnership; we’re improving health outcomes,” Parker says. “We’ve helped reduce
76 AHL
relationships with their family members as not caregivers but as granddaughters and sons, is really inspiring.”
The Path 77
“The stories of older adults are so amazing, and for them to be able to tell their story to someone who cares , while building better
loneliness among our members by 80 percent, and we’ve helped cut healthcare costs by taking our members out of unnecessary hospital settings. We also had 97 percent of our members complete their annual wellness exams through our platform and got people to use health risk assessments and improve medication adherence.
“Ultimately, we improve their satisfaction with health plans and reduce what the market calls ‘unhealthy days’—days people feel physically and mentally unwell over thirty days,” he adds. “On the other side, the Pals are earning a living. We have people who wouldn’t necessarily want to be nurses or caregivers, but they want to hang out with older people and help.”
During the COVID-19 pandemic, Parker tapped into his telehealth knowledge to implement virtual visit technology, which enabled members to use in-person and digital options. Parker notes that the pandemic opened other doors for Papa that will help members immensely in the future.
It encouraged seniors who were embarrassed to talk about being isolated or lonely to be less apprehensive about admitting their feelings and motivated them to learn how to use the technology better. Moreover, parents who were moved into a home office were able to use Papa to help tend to their children while they worked. Lastly, health plans that hadn’t totally bought
in to the idea that loneliness was an issue were brought on board.
“Loneliness is something that everyone experiences, and it was only exacerbated during the pandemic,” Parker says. “We were literally sending younger people into older people’s homes, so a lot of people thought Papa would fail. But we doubled our headcount during the pandemic because more health plans wanted to develop a relationship with us, and we expect similar growth for 2022.”
In the coming year, Parker expects Papa to be available in the contiguous states and hopes to explore putting the company’s services in other channels, like hospital systems and senior living centers. For now, Parker remains motivated by the success stories he hears from Pals every day—of the woman who had been a surfer for thirty years getting to go to the beach again with her Pal, or of the man who showed his Pal photos of the animatronics he built for Disney in the ‘30s.
“The stories of older adults are so amazing, and for them to be able to tell their story to someone who cares, while building better relationships with their family members as not caregivers but as granddaughters and sons, is really inspiring,” Parker says. “I feel so proud of what we’ve built, and I’m excited to continue to grow.” AHL
78 AHL
“I remember reading an article that said it’s more important to have, say, a hundred people who really love what you’re building than to have millions of people who download your product and never use it. I didn’t have one hundred, but I had ten, and that was good enough for me.”
The Issues
National, and even global, forces have an unmistakable impact on an executive’s work. Whether it’s a legislative change or an industry-disrupting technological breakthrough, executives must constantly adapt their business strategies to keep their company thriving.
80. Bill Pufko Bristol Myers Squibb
84. Thomas White Phynd, a symplr company
79
90. Patricia Campbell Cedars-Sinai Health System
Keep Your Eye on the Patients
Bill Pufko helps Bristol Myers Squibb keep its workforce safe, get vital medicines on the market, and make its ambitious 2030 sustainability goals a reality
By Donald Liebenson
80 AHL
 Bill Pufko Chief Counsel for Environment, Occupational Health, Safety & Sustainability
Bristol Myers Squibb
Bill Pufko Chief Counsel for Environment, Occupational Health, Safety & Sustainability
Bristol Myers Squibb
The Issues 81
Saira Hopper
In December 2020, Bristol Myers Squibb (BMS) announced its ambitious corporate sustainability goals. These went beyond mere New Year’s resolutions. These were big-picture, decades-on goals.
Among them are a commitment for the company to purchase all of its electricity from renewable sources by 2030, and by 2040, be carbon neutral in its direct and indirect emissions, as well as reach its targets of equitable water use, zero landfill waste, and an entire fleet of electric vehicles.
This leading-edge agenda is one of the factors that brought Bill Pufko to BMS in October 2018. Pufko is BMS’ chief counsel for environment, occupational health, safety, and sustainability (EOHSS). “The company’s mission to deliver transformational medicine to patients around the globe really resonated with me,” he says. “The company is very passionate about well-being and improving and saving lives. We’re making important medicines that have very positive impacts on patients’ lives. I am just excited to be part of that mission.”
Pufko credits his mom, a dietitian, and his father, who worked in the aerospace industry, with instilling in him a strong work ethic and prioritizing a work/life balance. “They both worked,” he says. “I saw how hard they worked and how committed they were to their jobs, but even more so to our family. They had my schedule and my brother’s schedule, and somehow, they were always there for us. That is seared into my memory, watching them juggle work and family life.”
Pufko also cites sports coaches who challenged and pushed him. “Figuratively,” he jokes. “But they were all really good people from working-class backgrounds. They instilled in me the
notion of grit and determination. I remember them vividly: they left such an impression on me, and that carried over through college and here today.”
Today, Pufko uses that work ethic and determination to ensure that medicine development and delivery is done in compliance with EOHSS standards. Being responsible for all of BMS’ EOHSS legal matters in relation to manufacturing, research and development, and commercial operations, he is also charged with advancing a proactive approach to these issues, especially if it is related to safety.
“The company is very passionate about well-being and improving and saving lives. We’re making important medicines that have very positive impacts on patients’ lives. I am just excited to be part of that mission.”
82 AHL
“The safety of our workforce is our paramount concern,” he says. “We deal with the nuts and bolts of compliance, and safety is a major part of that. I also work on the EOHSS implications in our mergers and acquisitions because our deals often involve physical assets. There is diversity in my workload: compliance work, deal work, litigation. It makes my job a lot of fun. I never know what’s going to happen day to day.”
A recent reason for the variety in Pufko’s workload is BMS’ acquisitions of Celgene in 2019 and MyoKardia in 2020. The new, integrated company reported a revenue of $42.5 billion in its first full year, 2020. “EOHSS integration is a significant process,” Pufko says. “This has been a good opportunity to define our own culture as we bring these two companies together.”
That culture, he says, “is very much focused on our patients. With that patient-centric culture, compliance with environmental issues and the safety of our workforce, our contractors, and visitors to our site are important. We do the right thing. I know that sounds simplistic, but that is how we operate.”
As if working on integrating two large companies wasn’t challenging enough, COVID-19 threw a wrench in the plans that no one saw coming. But Pufko also takes pride in how BMS was able to keep its manufacturing plants running during the pandemic while meeting “a number of challenges, including, first and foremost, manufacturing BMS’ medicines while keeping the workforce safe with the guidance and processes we have in place,” he says.
BMS’ top medicines include Revlimid, a treatment option for multiple myeloma; Opdivo, a medicine that treats certain types of cancers; Eliquis, an anticoagulant
medication used to treat and prevent blood clots; and Orencia, a medication used to treat autoimmune diseases. Getting these and the company’s other medicines to patients is what drives Pufko, he says.
“Our facilities are subject to many compliance requirements regarding air, water, waste, and various other EHS regulations. To the extent there are OSHA issues, those would be under my purview,” he says. “I know that everything I do has an impact on our company’s ability to deliver critical medicines.”
In regard to sustainability, Pufko examines the company’s goals and processes on a micro and long-term level, he says. “Sustainability is at the forefront of a lot of people’s minds, not just because it’s right to operate according to sustainability principles but because it’s a critical issue in the ESG investor world as well. Sustainability issues are present in our day-to-day operations and long-term operational goals, and they also play a role in other aspects of our business, such as sourcing and procurement, because we want our partners to be aligned with our approach.”
Though the past year has been difficult, Pufko says that watching his team and the company at large work together to get things done has been especially satisfying. “I’m lucky to get to work with many talented EOHSS professionals and subject matter experts here and around the globe,” he says. “It’s been a great privilege working with former Celgene and MyoKardia colleagues—there’s a good cultural cohesion forming. On the COVID front, it has been great to watch these dedicated people keeping operations going so that we can continue to deliver for our patients.” AHL
 BILL PUFKO
CHIEF COUNSEL FOR ENVIRONMENT, OCCUPATIONAL HEALTH, SAFETY & SUSTAINABILITY AT BRISTOL MYERS SQUIBB
BILL PUFKO
CHIEF COUNSEL FOR ENVIRONMENT, OCCUPATIONAL HEALTH, SAFETY & SUSTAINABILITY AT BRISTOL MYERS SQUIBB
NEW YORK PALO ALTO NEW JERSEY UTAH WASHINGTON, D.C. © 2021 Lowenstein Sandler LLP lowenstein.com |
Lowenstein Sandler applauds
We salute this well-deserved recognition of Bill’s experience, knowledge, and leadership. Our firm is honored to represent Bristol Myers Squibb as one of its trusted counsel.
The Issues 83
Healthcare
Arrives at the Digital Front Door
Thomas White, CEO for Phynd, a symplr company, helps transform
hospital directory systems with a data management tool that organizes everything
By Keith Loria
84 AHL
 Thomas White CEO Phynd, a symplr company
Thomas White CEO Phynd, a symplr company
The Issues 85
Courtesy of symplr
homas White’s journey to launching Phynd (now symplr) took many interesting turns. After receiving his master’s in international business and Arabic and Middle Eastern studies, White proposed to his now-wife and went to Kuwait for work. But after experiencing the first Gulf War in 1993, he quickly realized the move wasn’t a good fit for the new couple.
So, he turned his focus to starting a real-time news service when the worldwide web was gaining prominence. He sold the company not long after and began looking for his next career direction.
At the advice of his father, White realized there were great challenges in healthcare that could only be solved by information technology. That counsel led White to partner with his brother Peter to launch Vocada in 2001. The company solved communication breakdowns between hospitals’ imaging departments and referring physicians with the goal of delivering critical test results in real time. Six years later, the White brothers sold Vocada to Nuance, which Microsoft purchased at the end of 2021.
“In the process, we learned that hospitals don’t have good directories of their providers,” White explains. “They know their credentialed population, but about 90 percent of referring physicians are not credentialed. Nearly all mission-critical processes in
healthcare require accurate credentialed and referring provider information.”
With this in mind, in 2013 White created Phynd, a company whose software platform serves as a single, central, and accurate hub of all credentialed and referring provider data in a hospital. It keeps track of who the providers are, what they do, where they work, what their specialties are, and which health plans they accept, and it serves that data hospital-wide and in real time.
Some of the largest and most forward-thinking health systems in the US rely on Phynd, including New YorkPresbyterian Health, Michigan Medicine, Yale-New Haven Health System, Cedars-Sinai Health, USC Keck Medicine, Duke Health, and SSM Health.
symplr acquired Phynd in February 2021, and White’s solution has been rebranded as symplr Directory. Today, symplr Directory is still solving health systems’ important provider data management challenges. Once he joined symplr, White took on the title of general manager of symplr Directory.
Providers as Part of the Product Offering
“If you look back about thirty or forty years ago, hospitals would build paper-based directories of all the doctors who worked in the facility, and that didn’t really change when they went online,” White notes.
T
86 AHL
“Providers, in essence, are part of the product of a hospital, and what was missing in the directory world was that they needed to be able to provide a search tool for patients that allows them to type in any terms . . . and find an urgent care center that took their insurance.”
The Issues 87
“Providers, in essence, are part of the product of a hospital, and what was missing in the directory world was that they needed to be able to provide a search tool for patients that allows them to type in any terms— like sore throat, tummy ache, etc.—or even just put a zip code and find an urgent care center that took their insurance,” he explains.
White’s solution eliminated the struggles consumers experienced in navigating these sorts of systems and allowed hospitals to index all of their providers in an easily searchable way.
Another new product recently launched with Phynd’s EMR partners is Schedule Advisor. This module allows hospitals to leverage the scheduling tools built into electronic medical records (EMR) and extend them directly to consumers to self-schedule appointments with providers. The open scheduling slots are then integrated into the best-in-class search so consumers can find the right provider and make an appointment in a single, easy-to-use workflow. This “digital front door” capability is a game changer, White says.
Solving a Forty-Year-Old Challenge
From a data management perspective, real-time enrollment of providers missing in the EMR and other systems has always been an unsolved issue, and hospitals historically have not adequately coped with older tools that document new providers.
“About 20 percent of the provider engagements every year are new, so it’s a significant amount of change,”
88 AHL
“If you look back about thirty or forty years ago, hospitals would build paper-based directories of all the doctors who worked in the facility, and that didn’t really change when they went online.”
White says. “Those changes create financial issues for hospitals because, if the profile is built incorrectly, the bills are delayed, and it can quickly become a multimillion-dollar issue.
“We plugged the directory data into all aspects of hospitals’ operations,” he continues. “We integrate directly into the EMR, and we are the enrollment tool for those systems.”
What’s unique about symplr Directory is that it’s both a data model that supports broad-scale integrations and also a human management system.
“I call it ‘feeds and fingers,’” White explains. “The feeds are the real-time bidirectional feeds coming from different clinical and operational systems. The fingers are the human element that are dealing with providers every day.”
For example, one of the biggest health systems in Michigan is a client, and it has twelve thousand users working in symplr Directory every day, making nearly two thousand daily provider data updates. The system is being used to inform on health plan and network participation, to verify HIPAA compliant information, and to manage credentialing and privileging data for any mission-critical, patient-facing applications.
“symplr Directory consolidates everything into one system,” White says. “Hospitals can implement updated provider data back into the EMR, manage the marketing information—such as the glossy bios and photos—and use our application programming interface to push it out to the website in real time.”
Solving Clients’ Needs in a Pandemic
The software also served as a vital resource for health organizations during the COVID-19 pandemic, during which White kept the business focused on its mission. “We were really nervous about the pandemic, like any small business,” White shares. “Our clients were and are at the front lines of managing patient care. We reached out to all of them to ask how we could help.”
One major health system in New York City asked Phynd to build a COVID-19 test location-search website, so consumers could find the most convenient of its eighteen mobile testing sites. Phynd tightened its own belts and focused on its core customers, yet still captured a number of new clients who were delving deeper into telemedicine and needed to better manage providers who were participating in telemedicine-based care delivery.
“We manage locations, so if hospitals have fifty urgent care centers or hospital centers, we treat them as providers, so you can search for them, look at them, and book them as a consumer, just as you would any product on Amazon,” White explains. “We can help manage who is in and who is out of telemedicine, for example, or where the testing sites are.”
Looking ahead, symplr is working on creating tighter integrations with other technology vendors and credentialing systems, as well. “We’re really a data management business, and we’re focusing in on that,” White says. “Our core thesis is that we have to be integrated into the backbone of a hospital system.” AHL
The Issues 89
The Best and Brightest
At Cedars-Sinai, Patricia Campbell works on all sides of HR to support her talented pool of employees through anything—even a pandemic
By Shira Vickar-Fox
Once a quarter, Patricia “Pat” Campbell pours herself a glass of dry wine and meets with her team for a virtual happy hour. They bring their pets and children to the screen, play trivia games (Campbell says she usually finishes last), and don’t talk about work. “It’s important to try to stay connected,” says Campbell about her staff, which has been working remotely for more than one year. Hosting virtual get-togethers is one of many adaptations made for Campbell’s team to keep up spirits and maintain camaraderie during this challenging
time. “I try to treat my team like an extended family,” she says. Campbell is executive director of employee benefits, HRIS, wellness, work/life EAP, and recognition at Cedars-Sinai Health System in Los Angeles. Cedars-Sinai is one of the largest nonprofit academic medical centers in the US and is consistently ranked as one of America’s Best Hospitals by US News & World Report Needless to say, leading several teams of the human resources department at a large, extremely busy medical center during a pandemic isn’t easy, nor will the
added workload from the pandemic ease up any time soon. A new COVID-related hurdle is managing remote staff who moved out of state and figuring out how to comply with labor regulations, tax issues, and other employment issues in more than a dozen states. Campbell sits on an out-of-state-workers task force in addition to her tremendous workload. And yet, through the stress of it all, Campbell manages to remain keenly attuned to the needs of hospital employees.
“Every day when I wake up, I want to make a difference for our employees by
90 AHL

B.E.D. Productions The Issues 91
Patricia Campbell Executive Director of Employee HRIS, Benefits, Wellness, Work/ Life EAP & Recognition Cedars-Sinai Health System
providing what they need for themselves and their family,” Campbell notes.
She adhered to that philosophy even before COVID-19 wreaked havoc on the industry and the world at large by upturning workplaces. Years ago, she redesigned the company’s wellness program to make it more inclusive. “We actually expanded it so that people could earn incentives if they simply went to the doctor and got a check-up, or did their dental preventive screening, or volunteered,” she explains. Her goal was to encourage people to think more broadly about wellness, especially those who are unable to participate in conventional wellness activities such as joining a weight loss program or participating in fitness challenges.
The result? “People feel like they have more choices on how they can help themselves,” Campbell notes. Additionally, employees followed through on their wellness commitments and earned money
toward their Health Reimbursement Arrangement (HRA). “They feel as though they can reduce their stress, we can reduce some of our workers’ comp claims, and it didn’t cost us anything to add those additional pieces in there.”
During the pandemic, Campbell oversaw the implementation of other programs to benefit employees. “We put in some additional pay practice guidelines,” she explains. “If anyone got COVID or a member of their household got COVID, we kept them home. They didn’t have to use sick time; they got paid no matter what.”
Campbell and her team also designed a “crisis care” program to reimburse expenses for short-term childcare or caregiving assistance. It allows employees to pay a friend, family member, or someone else to tend to an ailing relative or watch children to alleviate some of the burden of juggling work and managing family responsibilities.
In the early months of the pandemic, she helped create the Employee Resource Pool (a redeployment of staff members) and volunteered, ahead of her team, to become a frontline worker. It was important to her, especially during a time of heightened anxiety, to experience the work and allay any fears of volunteering during COVID-19. “I wouldn’t ask anyone on my team to do something that I wasn’t willing to do myself,” she says.
For a month she worked from 5 a.m. until 1:30 p.m. every Saturday and Sunday wherever she was most needed. She did temperature checks and handed out masks and hand sanitizers to people entering the medical facility. “It felt good to interact with those who had to come in to do patient care,” Campbell says.
Friendliness comes naturally to Campbell—she’s the kind of person who greets people every morning and chats up strangers in the elevator. Her rapport with people was even the key that opened the door to a career in human resources. She started her path at an insurance company and was hired by an HR firm because “I came across as so customer focused,” she says.
OUTSIDE OF HR
When Patricia Campbell isn’t flexing her HR muscle inside CedarsSinai, she’s expanding a different kind of skill set at home. Campbell grew up on a farm, and to relax, she loves cooking new cuisines and adjusting recipes to include fresh produce and good spices. She also enjoys time with her family and bringing them with her on tours of comedy clubs. She says, “Laughter, to me, is great medicine.”
That might be a credit to her upbringing in Mississippi, where hospitality is embedded in the culture, but it’s also a natural extension of a leader who values coworkers and is a fierce advocate for her team members. “I’m a firm believer in paying people what they are worth and what the market calls for,” she says, “and I fight for them with regard to that.”
In her more than five years at Cedars-Sinai, she’s cultivated a diverse department of more than twenty HR professionals and values the life experiences
92 AHL
The Issues 93
“If anyone got COVID or a member of their household got COVID, we kept them home. They didn’t have to use sick time; they got paid no matter what .”
and different perspectives they bring to the job. “I do believe in hiring the brightest and smartest people I can find, even if they’re smarter than me,” she says. “Many of them have strengths that I don’t have, but it makes for a wellrounded team.”
Campbell’s outside partners can attest to her ability to step into any HR environment and combine the best and brightest to build the perfect team. “When the longtime HR team turned over, Pat stepped into a very complex benefit environment,” explains Drew Erra, senior vice president at Aon. “She quickly assessed the most critical issues, built strong internal relationships, and partnered with our team to ensure the benefit programs were being appropriately administered.”
Campbell has now spent more than three decades in healthcare, and her off-hours are also spent in the same field. She’s on the board of directors of the Osborne Head & Neck Institute—a
nonprofit that seeks to improve lives around the world through ear, nose, and throat surgical care, including complex oncology conditions.
That mission sits close to home for Campbell: she’s paying her time forward as a former patient treated by the founder, Dr. Ryan F. Osborne, for salivary stones, a procedure that was made easier because of Osborne’s kindness and compassionate care. Currently, the organization is busy fundraising for a capital campaign to build a new state-of-the-art facility in Los Angeles.
Pulling from her personal experiences as a patient and her philosophy as an HR leader, Campbell has been able to make a difference inside and outside CedarsSinai. Between encouraging better health practices and navigating a pandemic, she’s found something that can keep people together amidst any challenge: resiliency. “This time has shown strength and outside-of-the-box thinking that none of us could have seen coming.” AHL
Experience Empathy at Work Employee Assistance Programs Student Support Programs Crisis Management Services
empathia.com 866.332.9595 Care at the intersection of competence and compassion. empathia.com 866.332.9595
to families and small groups of people, to entire workplaces, to community-wide impact.
94 AHL
“Every day when I wake up, I want to make a difference for our employees by providing what they need for themselves and their family.”
Aon’s Executive Benefits Practice has spent forty years developing expertise in the design, funding, and administration of benefits for physicians and executives to best meet the unique needs of tax-exempt hospitals and health systems. The tailored enrollment, communication, and administrative services we offer optimize the benefits our clients provide to their key employees, and this is how we set ourselves apart. At Aon, we take pride in our staff, which includes specialists in compliance and human resources, insurance product development and underwriting, healthcare operations, and benefits administration. We work together to deliver the highest quality products and services in the benefits consulting marketplace.
Setting New Standards
Milliman is proud to have a client like Cedars-Sinai whose work and vision we believe in.
Whether it’s delivering a high-value employee assistance program or responding to a workplace or community crisis, Empathia brings competence, compassion, and commitment to those we serve. We do important work driven by a more important mission: improving lives and helping people. We are proud to support exceptional partners like Patricia Campbell.
Since 1947, Milliman’s expert guidance and technology solutions have empowered clients to protect the health and financial well-being of people everywhere. We engage with clients to enhance healthcare systems, manage emerging risks, and advance financial security, so millions of people can live for today and plan for tomorrow with confidence.

TRI-AD delivers a total benefits administration solution. Our hallmark has been the development of long-term relationships with clients and a superior service experience for plan participants. We enjoy collaborating with Pat to help generate better outcomes for Cedar’s employees. TRI-AD congratulates Pat for her accomplishments and wishes her continued success!
Congratulations to Patricia Campbell and Cedars-Sinai for their extraordinary leadership and innovation within the healthcare sector. With a mission to be America’s retirement company, Voya Financial is grateful and proud to be your partner in providing retirement plan solutions that help create a better financial future for all employees.
We applaud Patricia Campbell for her role in bringing that vision to life. Thanks to her leadership, Cedars-Sinai has pioneered innovative employee benefits and wellness programs for employees. Together, we are helping to improve the health and financial well-being of people everywhere and setting new standards in employee benefits. milliman.com
Voya keeps you moving forward to and through retirement with confidence.

Voya helps Americans plan, invest and protect their savings — to get ready to retire better. We serve the financial needs of more than 14 million individual and institutional customers in the United States.
Our vision is to be America’s Retirement Company® while being equally committed to conducting business in a way that is socially, environmentally, economically and ethically responsible.
voya.com

The Issues 95
Willis Towers Watson is
Willis Towers Watson is a leading global advisory, broking and solutions company that helps clients around the world turn risk into a path for growth. Our unique perspective allows us to see the critical intersections between talent, assets and ideas —the dynamic formula that drives business performance. Together, we unlock potential.

CONGRATULATIONS, PAT! TRI-AD partners with Pat to enrich the health and

well-being of employees and their families with great initiatives like the Cedars-Sinai Crisis Care Program.

We congratulate Pat Campbell for her achievements and exemplary leadership. We are proud to support Cedars-Sinai as they continue to lead and innovate for the future and wellbeing of employees and our communities.
Anthem is dedicated to delivering better care to our members, providing greater value to our customers, and helping improve the health of our communities. Visit us at anthem.com/ca.

Benefits Administration Integrated Health and Wealth
Total
financial
WTW_8801_AHL Cedars Sinai_May21_v2.indd 1 5/24/2021 2:12:06 PM 96 AHL
proud to sponsor Cedars-Sinai
The Business
Healthcare is a constantly evolving industry that demands executives to plan ahead. Often, this means business leaders need to address department- or companywide issues to remain focused on driving innovation and devising strategies to maintain a high level of care.
98. Steve Aleman Prime Healthcare
106. Lars Taavola Mallinckrodt Pharmaceuticals
97
112. Maribel Hines Atara Biotherapeutics
Built on Solid Ground
As CFO for Prime Healthcare, Steve Aleman ensures that the organization’s financial footing is well-positioned to outlast the most strenuous circumstances
By Charles S. Donnavan
98 AHL
 Steve Aleman CFO
Prime Healthcare
Steve Aleman CFO
Prime Healthcare
The Business 99
Karen Vaisman
or more than three decades, Steve Aleman’s career has been motivated by wanting to know more. “I like challenges and I like hard work, and I’ve always liked the ability to take on new challenges,” he notes. “I think that’s how you gain an understanding of all facets of an organization, be in a position to understand all drivers of growth, how your decisions impact those drivers, and ultimately make better decisions to create value for the organization.”
Now more than ever before, leaders all over the world are facing change and complexity—the coronavirus pandemic has presented new challenges, new circumstances, and new uncertainties. Aleman emphasizes that to not only grow but to survive, adaptability is a requirement. Because change is constant and inevitable, leaders must be flexible to succeed.
As chief financial officer of Prime Healthcare, one of the nation’s leading health systems with forty-six hospitals in fourteen states serving over six hundred communities. The organization has 35,000 employed staff and provides 2.6 million patient visits annually. Aleman has leveraged his twenty-three years of diverse healthcare experience to help the company navigate the ever-changing US healthcare market.
Prior to joining Prime Healthcare, Aleman started his career in public accounting where he became a certified public accountant. While he enjoyed supporting his various clients who were generally owner/operator entrepreneurs, he sought to plant his career roots with growing companies in dynamic business environments.
He selected healthcare and started on the payor-side at WellPoint/Anthem, the largest for-profit managed healthcare company in the Blue Cross Blue Shield Association and in the Top 30 on the Fortune 500 list. After eleven years and contributing to the successful WellPoint/ Anthem merger, Aleman moved to the provider side where he has succeeded in various leadership roles such as internal audit, business development, compliance, and served as CFO of several national hospital companies.
“Throughout my career, I have worn many hats,” Aleman says. “It has helped me understand and enhance company growth drivers in an effort to create value. As a leader in healthcare, it is critical to maintain a focus on continuous improvement and evolution. Transformative change in healthcare is the norm, and to succeed and survive, leaders and companies must constantly evolve.”
F
100 AHL
The Business 101
“Just as you begin to develop business relationships with your corporate teams and define your strategic plan, the world is turned upside down and remote work environments become the norm.”
Aleman joined Prime in January 2020 prior to the COVID-19 outbreak in the US that changed every aspect of life.
“It was a challenging time in healthcare, and especially professionally challenging while stepping into a leadership role at a new company,” Aleman says. “Just as you begin to develop business relationships with your corporate teams and define your strategic plan, the world is turned upside down and remote work environments become the norm.
“However, it was also a very inspiring time to be in healthcare,” he continues. “Our frontline healthcare providers began to receive the recognition as the heroes they truly are—and the executive team supported them by being in the office every day to address their needs and rise up to meet the enormous challenges at hand.”
Aleman highlights that while the news focuses on “The Healthcare Divide” in reference to the disparity of care received in various population segments, he references that Prime has been at the forefront of bridging that divide.
“There are countless stories from the various communities we serve, where Prime was able to help patients and their loved ones deal with unforeseen
102 AHL
“It’s never a dull day and nothing is static. I never had to worry in my career about becoming complacent. I focus my day on how I can contribute to the company and grow my career along with that.”
challenges that haven’t been experienced in generations,” Aleman says. “It shows the bravery of those who provided care across our system, battling wave after wave of COVID surges from the early spike that hit our northeast facilities to the winter surge that ravaged California.”

Aleman notes that while Prime stepped up to help bridge that divide and ensure the underserved continued to have access to quality healthcare, it was still important as an organization to focus on growth drivers that could best position the company in a post COVID-19 world.
To see to that, Aleman and the finance side of Prime took on three key challenges. First, reengage an acquisition growth engine that had been on hold for the past few years. Second, reposition the company with leading banks and investment firms. And third, recapitalize the company to bring down the cost of capital, provide a long runway, and grow and strengthen the balance sheet.
Normally, these goals are challenging to execute in a short timeframe, but potentially even more challenging during a pandemic.
“Once again, you must leverage your assets and skill set to adapt to the challenges of the day and evolve
SUCCESS RISES IN THE WEST
MOSSADAMS.COM
When you go above and beyond, the sun rises on limitless potential. We believe in the value of applauding your achievements— and the possibilities they inspire.
Congratulations to Steve Aleman.
RISE WITH THE WEST.
The Business 103
Assurance, tax, and consulting offered through Moss Adams LLP. Investment advisory services offered through Moss Adams Wealth Advisors LLC.
your thinking and approach—focus on the solution for the problem, not all the reasons why a problem cannot be solved,” Aleman advises.
In early 2020, an attractive healthcare asset came to market just as COVID-19 was starting to tighten its grip on the nation: St. Francis Medical Center, the jewel of the former Daughters of Charity and Verity Health System. Certain interested parties turned their focus away from expansion, others fell victim to a tightening credit market.
“It was purchased out of bankruptcy, but the belief was this hospital could return to once again become community asset it once was,” he says. Aleman and the Prime executive team focused on the possible as opposed to the impossible and raised funding for the acquisition where others couldn’t. Then, the challenge turned to integrating a large safety net hospital during a pandemic—challenges that were faced head-on with hard work and creativity.
“Roughly eight months later, so far, the acquisition, integration, and community outreach efforts have been a resounding success,” he notes. “The pandemic actually brought about a unique opportunity whereby this community was in a period of great need and had no choice but to turn to the hospital for care and compassion. Prime and its heroic frontline caregivers answered the call to establish bonds that otherwise would have taken years to establish.”
Shortly thereafter, in late 2020 and early 2021, Aleman and Prime closed
multiple bond offerings that ultimately recapitalized the company, solidifying the company’s balance position for further growth for years to come.
“These financings affirmed the strength of Prime’s platform, strategic vision, and quality model. The model endured even through the pandemic with the historic acquisition of St. Francis Medical Center in Lynwood, California,” Aleman says.
Looking ahead, he expects to have an even more transformative impact in the years ahead from a quality and cost efficiency perspective. Aleman notes his success has always come by taking a solution-oriented approach to achieve both organic and strategic growth.
By following this work philosophy, Aleman has been able to enjoy a successful, dynamic career.
“It’s never a dull day and nothing is static. I never had to worry in my career about becoming complacent,” he notes. “I focus my day on how I can contribute to the company and grow my career along with that.” AHL
Moss Adams LLP provides assurance, tax, and consulting insight and expertise to public, private, and not-for-profit healthcare enterprises. We serve more than 3,700 clients across the healthcare continuum, from large health systems, hospitals, and long-term care organizations to clinics, medical groups, and physician practices. Visit mossadams.com/healthcare.
104 AHL


Healthcare’s
hospitals,
and
CainBrothers.com 333908 City National Bank Member FDIC. City National Bank is a subsidiary of Royal Bank of Canada. ©2021 City National Bank. All Rights Reserved. Discover The way up® at CNB.com. City National® proudly supports Steve Aleman and Prime Healthcare. WE MAKE IT OUR BUSINESS TO BE PERSONAL. The Business 105
We congratulate STEVE ALEMAN in over two decades as a financial and strategic leader guiding hospitals across the country. His knowledge has accelerated Prime
growth strategy and furthered their mission of saving
saving jobs
saving lives.
IP at Top of Mind
Lars Taavola helps Mallinckrodt Pharmaceuticals’ highly scientific workforce think creatively to expand the company’s IP portfolio
By Keith Loria
106 AHL
M allinckrodt Pharmaceuticals is a 150-plus-year-old company that needed help transitioning to a twenty-first century world both from a legal and a leadership perspective. Enter Lars Taavola, who joined the company during August of 2020 as vice president and chief intellectual property counsel, focused on refining Mallinckrodt’s IP strategy.
The fact that the company was also managing bankruptcy at the time due to various litigations just added to the challenge that awaited him. But less than a year later, Taavola has already made significant headway into restructuring the IP department and helping to reenergize the patient population.
“We needed to become a more entrepreneurial-minded company,” he explains. “I went to the business groups and others within the organization to explain how we needed to start thinking about our IP and how we needed to be a bigger part of the organization, rather than just simply a service provider. I think sometimes we took a very academic view of, ‘Should we get a patent, or should we not get a patent?’ Instead of saying, ‘How is our role going to contribute to our ability to improve patients’ health and the health of the business?’”
Taavola knew he wanted to be a patent lawyer in high school, though it wasn’t
the direction he followed right out of college. He worked as a chemical engineer for a while, but quickly realized that they only put chemical plants in remote locations, so while sitting by himself in Lake Jackson, Texas, he made the decision to answer the calling to law that had been in the back of his head.
After graduating from Boston University School of Law in 2002, he took a job at Kenyon & Kenyon, and because he had a chemical engineering degree, he was put on a pharmaceuticals project and started learning a great deal about that industry. His career progressed to the point where he started running IP departments, specializing in pharmaceuticals.
Joining Mallinckrodt during the pandemic may seem like an odd choice, but there were several reasons he wanted the job.
“One, my prior company was going through a lot of changes,” he explains. “Then I met the people at Mallinckrodt and there was no way I could turn it down. The people are of high quality and it’s very much a patient- and employee-centered company.”
One of the keys to his early success at the company was getting everyone on board about the importance of IP, especially the scientists, who needed to
The Business 107
Lars Taavola
and Chief Intellectual Property Counsel
inform the IP team about any clinical trials or other things in the works so it could get patents ready.
Taavola’s team consists of two patent attorneys and a paralegal in-house along with an outside counsel team. Being relatively new to the company, the biggest challenge is still just having everyone know who he and his team are and what they do.

“I’m in charge of all of our intellectual property, primarily for the brands business,” he explains. “For the generics business, we do make some finish dosages—some tablets and other things. But primarily, I investigate our patent portfolio. I’ve identified some gaps, and the team is working on changing the mentality moving forward. A commercial colleague might not think anyone is going to care about something simple—I need to show them why something is more than a simple idea.”
One of Taavola’s favorite examples to illustrate his point is Keurig Coffee, which made money because they patented the little container that the coffee came in.
“It’s kind of reminding people that we do have an impact on the business, and we need to remember who the overall audience is,” he says. “The biggest initiative I’ve done is getting IP involved throughout the process, which is an ongoing thing I am still working on.”
That means in product development, talking with the clinical regulatory team regularly and being a “fly on the wall” that sees everything and will buzz when it’s necessary to plan out the patent strategy. In other words, he aims to help the scientists think creatively to see what a savvy invention could be, even if they
VP
Mallinckrodt Pharmaceuticals
108 AHL
Victoria Yang
The Business 109
“A commercial colleague might not think anyone is going to care about something simple— I need to show them why something is more than a simple idea .”
We are proud to partner with you.






 E. Melnick, Ph.D.
E. Melnick, Ph.D.
might not think it is something worthy of a patent.
“Mallinckrodt is a very old company and also a very scientific company, so when they look at a patent, they always go to the most scientific aspect,” Taavola says. “What’s interesting about patent law is sometimes the most scientific aspect is not even patentable. We need to get people comfortable with the ideas part and what we can do there.”
Kate Doty and Morgan Kirley, partners at Polsinelli, appreciate Taavola’s fresh perspective to help expand his company’s patent portfolio protection. “You can tell that Lars values IP protection and that expanded patent filings and building value are a real priority for him,” says Kirley. “We have a lot of great brainstorming sessions, and Lars really looks at the patent issues from all angles.”
Currently, Mallinckrodt is developing two new products they are hoping will be approved. One is for deep partial






thickness burns, and the other is for people with severe liver disease.
This year, the company is anticipating emerging from bankruptcy, partly on the strength of its new patents, and Taavola hopes IP is viewed as both a legal and commercial function throughout the organization.
“I want people thinking about looping IP in, and I know we’re not there yet, but it’s becoming less of an afterthought,” he says. “[As] 2022 starts and I’m getting too many emails from people across the organization, that’s how I know we’ve succeeded.” AHL




Knobbe Martens and attorneys Ryan Melnick and Jane Dai are proud to help Mallinckrodt protect its worldwide intellectual property around innovative therapies for patients with severe and rare diseases. We congratulate Lars Taavola on this well-deserved recognition of his expertise and leadership.

Ryan
Partner 858-707-4000
Jane Dai, Ph.D. Partner 858-707-4000
ryan.melnick@knobbe.com
jane.dai@knobbe.com
110 AHL
“Sometimes we took a very academic view of, ‘Should we get a patent, or should we not get a patent?’ Instead of saying, ‘How is our role going to contribute to our ability to improve patients’ health and the health of the business?’”

Polsinelli is proud to support Lars Taavola, VP, Chief Intellectual Property Counsel for his work at Mallinckrodt Pharmaceuticals. Leaders stand out. advancing the innovative spirit The choice of a lawyer is an important decision that should not be based solely upon advertisements. Polsinelli PC, Polsinelli LLP in California. real challenges. real answers.SM Am Law 100 firm with 900 attorneys nationwide 21 offices from LA to NY 170+ services/industries polsinelli.com
A Penchant for Empowerment
Maribel Hines works to provide a space of inclusion and a sense of belonging for any person, in any circumstance, both inside and outside Atara Biotherapeutics
By Javanna Plummer
As the senior director of global talent development, diversity, and inclusion at Atara Biotherapeutics, Maribel Hines has made it her mission to not just create a diverse workforce but to foster a more diverse and inclusive work environment.
Atara Biotherapeutics is a leading resource in developing treatments for people with cancer, autoimmune, and viral diseases. Though its website states that it seeks “to transform the lives of patients with serious diseases through pioneering science, teamwork, and a commitment to excellence,” Atara is
focused on transforming employee’s lives, too—with some help from Hines and her people team.
For Hines, diversity goes beyond the categories of race, gender, and ethnicity. She acknowledges that these are important as a basis, but they are not an endpoint for D&I.
Looking beyond these dimensions and also focusing on neurodiversity, sexual orientation, physical ability, and socioeconomic backgrounds helps organizations like Atara build a diverse workforce and foster a more inclusive culture. Appreciating and drawing on each unique
experience helps the organization not only hire great talent but also create an environment where everyone thrives.
“We’re in a space where we need to innovate in service of our mission,” Hines says. “Diversity and inclusion are foundational steps in our journey, and they can’t be rushed just to check a box.”
To meet changing metrics of diversity, Atara has implemented robust programming aimed at bolstering a more varied and inclusive workforce and environment through educational, developmental, and conversational mediums. According to Hines, Atarians
112 AHL
 Maribel Hines
Senior Director of Global Talent Development, Diversity & Inclusion Atara Biotherapeutics
Maribel Hines
Senior Director of Global Talent Development, Diversity & Inclusion Atara Biotherapeutics
The Business 113
Chris Schmitt
(as employees are affectionately dubbed) have several choices when it comes to being part of the company’s diversity and inclusion framework.
For one, they can participate in an educational series aimed at “fostering inclusion, awakening unconscious bias, leveraging cognitive diversity, and scaling belonging” across all levels of the organization, from staff to senior leadership. Employees can also attend fireside chats that center on a specific theme. In honor of Pride month, for example, the theme of the chat in June was “Pride in the LGBTQIA+ Experience.”
For the talk, Hines enlisted a transgender moderator in addition to four panelists who identified as allies, advocates, and members of the LGBTQIA+ community. The goal of the event was to support a welcoming atmosphere, build connection, and open the door for employees to be able to share their own stories and experiences of understanding of acceptance.
This chat was the second of four that Atara planned to have in 2021. For the final two, the people team collaborated with Atarians to choose topics of interest, which ranged from gender to allyship and beyond.
In addition to placing an emphasis on more diverse hiring and inclusive internal resources by organizing programs like these fireside chats and the educational series, Atara has committed to remaining an all-inclusive company for years to come.
Hines states that Atara is being “thoughtful and planful” when it comes to its D&I strategy and acknowledges that doing so can translate to a highperforming team that is in service of Atara’s mission of transforming patients’ lives through pioneering science, teamwork, and a commitment to excellence.
The company’s initiatives are centered on building trust and enabling collaboration, which is one of the organization’s TRAIT values: transparency, respect, accountability, integrity, and trust.
To Hines, an effective workforce at Atara would embody these core values by modeling them in words and action.
“A high-performing team knows how to enable the people around them to cultivate the culture and drive the change,” she says. “I want to look back and see that the initiatives, programs, and tools I provided help to attract, develop, and retain great talent.”
According to Hines, Atara welcomes employee feedback and engagement. It surveys employees and actively draws on “culture champions” to provide progress updates and help the organization drive the culture forward. In other words, the company implements suggestions from employees who are passionate about contributing to a diverse, inclusive, and engaging work environment.
“Atara is focused on making sure people understand that inclusion is intentional,” Hines says, adding that bolstering team dynamics and psychological safety contributes to how people feel about going to work.
During the COVID-19 pandemic, psychological and physical safety were at the forefront of the company’s strategy. Hines, having joined Atara the week of lockdown in March 2020, was thrown into the thick of this fast-acting strategy as both a leader and an employee. Luckily, the company took great strides to make sure employees felt safe and cared for, especially essential workers.
Hines notes that Atara took a “people-first approach that was focused on safety through risk reduction.” This risk reduction included creating remote work practices for employees who could stay home and implementing safety precautions for those who could not, based on role responsibilities.
Additionally, the organization took measures to ensure employee wellness, with more than 110 virtual engagement opportunities, including guided mediation, chair yoga, webinars, happy hours, virtual cooking lessons, and an online art-focused workshop called “ARTara.” They also hosted lunches for essential staff and implemented recharge and meeting-free days to enable personnel recharge and renewal and allow focused time to get meaningful work done.
All of these efforts went toward making staff feel safe when the world endured such uncertainty. More so, to Hines, these efforts emphasized Atara’s culture, which she describes as “learning agile, diverse, and inclusive.”
Supporting a culture like this is also what Hines tries to accomplish through
114 AHL
The Business 115
“We’re in a space where we need to innovate in service of our mission. Diversity and inclusion are foundational steps in our journey, and they can’t be rushed just to check a box.”
EXECUTIVE LEADERSHIP PEOPLE MANAGEMENT CAREER PLANNING


her volunteer work outside Atara. “I am very purposeful about how I volunteer,” she says. And it’s no understatement: Hines splits her free time three ways to serve as a mentor for several other organizations.
First, she is on the advisory board of the University of Southern California—her alma mater—where, as a member, she provides advice, support, and feedback to university students about their careers and other topics. She is also a member of the Latino Alumni Association, where she mentors college freshmen.
Additionally, Hines works with Chrysalis, a nonprofit organization that focuses on creating a pathway to selfsufficiency for people in the homeless community and low-income individuals through resources and support. With this organization, Hines provides


feedback and grants mock interviews to help people who may have barriers in their job search.

“These are people who are serious about finding full-time employment but have experienced a significant setback either through incarceration, substance abuse, or sheer bad luck,” she says. “[Finding a job] can be challenging for these populations, and I want to help them.”
Inside and outside Atara, Hines strives to set everyone up for success and help ensure that they feel valued. Her volunteering and professional duties work hand in hand to ensure that others are given a fair shake. More so, her work emphasizes that a person’s success is not determined by their circumstances and instead proves that someone’s uniqueness can be used to their advantage. AHL
line,
(o) 818.907.1178 l (f) 818.907.1187 theexecutiveadvisory.com
TARGETED DEVELOPMENT CONFLICT MEDIATION
We build healthier companies, stronger teams, and e ective leaders.
Bottom
we help people be their best and companies thrive.
116 AHL
“A high-performing team knows how to enable the people around them to cultivate the culture and drive the change.”
The Impact
Executives know there is an increasing need to help individuals manage their own health anywhere and anytime.
To do that, healthcare leaders are developing products and services and offering resources catered to different communities’ needs—all aimed at motivating them to stay engaged with their health and empowering them to be their best, at home or at work.
118. Carolyn Wood UPMC
124. Dr. Saloumeh Bozorgzadeh Caring for Our Caregivers
117
128. Janel Lancaster UNC Health
Well-Being from All Angles
As vice president of employee benefits, Carolyn Wood considers all points of the wellness spectrum to keep UPMC employees safe and healthy
By Billy Yost
118 AHL
 Carolyn Wood VP of Employee Benefits UPMC
Carolyn Wood VP of Employee Benefits UPMC
The Impact 119
Kristin Miller
arolyn Wood came to the University of Pittsburgh Medical Center (UPMC) at the tail end of 2020. The COVID-19 pandemic has meant that despite being months on the job, she still has yet to meet many of her colleagues face-to-face.
Coming to a healthcare organization during one of the most severe health crises of modern history might seem a strange choice for the financial analyst turned retirement and benefits professional, who has an amazing résumé that includes manufacturing, defense, aviation, and even baking.
But Wood took the challenge on later in her career precisely because of the resilience she has demonstrated in all of her previous roles. After all, who better to help frontline employees navigate a challenge than someone who has managed to overcome hundreds of obstacles in her own career?
Wood has spent six months as vice president of employee benefits at UPMC, and while she may not have met all of her team in person yet, she’s helped make an immediate impact at a time when the healthcare organization needed all hands on deck to support its employees and deliver a strong total rewards program.
The Three-Legged Stool
Wood was excited to come to UPMC for several reasons. At the top of the list is knowing that the people she sees on the news as frontline and essential workers are the same people she’s helping support and lead more fulfilling and healthy lives. The opportunity to come to UPMC has also provided Wood a chance to pursue what she considers the future of benefits, which—as she puts it—looks like a three-legged stool.
“When we talk about the future of benefits, it’s this interconnected approach to physical, emotional, and financial well-being,” Wood explains. “All three of these affect each other, and I think it’s very important for an organization like us to demonstrate caring in each of these areas.”
While the physical and financial aspects of benefits have made significant headway over the years, Wood says only recently has the behavioral health and emotional well-being component been embraced more widely in the US workplace. The stress of the day-to-day experience of healthcare workers means that the organization has a tremendous opportunity to provide tools and
C
120 AHL
The Impact 121
“When we talk about the future of benefits, it’s this interconnected approach to physical, emotional, and financial well-being . All three of these affect each other.”
EVERYTHING FOR A REASON
Carolyn Wood speaks often of her belief in things happening for a reason. Most of her career jumps have come not from active solicitation but from phone calls from acquaintances wondering if she was up for a new challenge. She’s taken on new responsibilities in one major city after another, adding to a colorful skill set that’s made her an asset to any company she’s been part of.
“I’ve found that the diversity of experience in my career and the willingness to be resilient and move forward have served me well so far,” Wood says.
She got the call about UPMC the day she dropped off her youngest child at college for the first time. Coming to Pittsburgh allowed her to relocate to the city where her middle son resides. A solid trade.
resources for employees to deal with unprecedented challenges.
Telehealth is one area where UPMC has continued to expand its offerings to employees during and post COVID19. “One of the great things that has accompanied our telehealth program is the ability to help remove barriers to access and acknowledge that there was a behavioral health crisis in this country before COVID began,” Wood explains. “It’s allowed us to expand the ways in which we continue to support our people, finding innovative and creative ways to address these problems.”
UPMC’s health plan has offered behavioral or mental health first aid training for leaders, to help recognize employees who may need a hand but struggle to express it openly.
The Holistic Employee Experience
Wood says that evolving the holistic employee experience comes down to delivering the right benefits at the right time to ensure that they resonate with as many employees as possible. “That sounds like it might be easy, but it’s very, very hard,” Wood explains. “There’s a lot of data that needs to be collected and analyzed behindthe-scenes in order to do that.”
That process includes identifying at-risk populations, looking at turnover for key positions, and breaking down employee populations so as to figure out which benefits will provide the
122 AHL
maximum impact for the most people. One of Wood’s biggest achievements thus far is helping evolve that holistic experience conversation.
Part of the reason Wood has been able to make an immediate impact is because of her sheer breadth of experience. There are very few benefits professionals who are able to draw a parallel between a hospital system and a bread company, but that’s what makes Wood great. She sees a through line in the way organizations look after their people.
“Our mission and values were the same at a baking company as they are here, in many ways,” Wood explains. “This organization is deeply humane and very value-driven, and it reminds me of my
previous experience. It sticks with me because when an organization is truly about serving its people, you feel it.”
It’s perhaps that outlook that has earned Wood’s designation as a welcome addition to UPMC. “Getting a team excited about what they’re doing and the opportunities and shared commitment in this organization is really important for them to own their own pieces of the work,” Wood says. “We have the opportunity to work for an organization that is truly making a difference and moving the needle in such an unprecedented time.”
Wood’s excitement, her outlook, and her mission-driven work ethic are an ideal fit for an organization whose employee proposition is simply “Cares.” AHL
J. Heller Executive Chairman & CEO (215) 665-4141 mheller@cozen.com
Vincent R. McGuinness President & Managing Partner (215) 665-2097 vmcguinness@cozen.com
Lynn Krisay Brehm Member (704) 348-3460 lbrehm@cozen.com
John H. Wilson Co-Chair, Employee Benefits & Executive Compensation (412) 620-6511 jhwilson@cozen.com 775 attorneys 30 offices cozen.com
“This organization is deeply humane and very value-driven . . . It sticks with me because when an organization is truly about serving its people, you feel it.”
Michael
© 2021 Cozen O’Connor
Cozen O’Connor is proud to team with and support the work of Carolyn Wood and UPMC.
The Impact 123
For the Front Line
Dr. Saloumeh Bozorgzadeh taps into the psychology of healthcare workforces to create Caring for Our Caregivers, an initiative that provides mental health support and prevents burnout
By Maggie Lynch
“W
e find that in the middle of difficult situations, you don’t have the resources to tell yourself what you need—you’re kind of on autopilot,” says Dr. Saloumeh Bozorgzadeh, president of the Sufi Psychology Association and founder of Caring for Our Caregivers.
The crisis Bozorgzadeh is describing is the mental and emotional toll put on healthcare workers during the COVID-19 pandemic. As a clinical psychologist, she heard firsthand about the pain, fear, and depression that her clients working in the healthcare field were facing. One client, a nurse working with COVID patients, told Bozorgzadeh that the anxiety she was facing about catching the disease and passing it to her family was
so extreme that she would go so far as to isolate herself from other people completely. “This was a display of an incredible level of stress for someone to be under,” Bozorgzadeh says. “This is burnout.”
Burnout. It’s the culmination of all these feelings of stress and anxiety healthcare workers faced even before they were required to dress in protective equipment and see patients suffering from incredible levels of sickness day after day.
“My clients were telling me that if they had breaks, they were sitting in the break room and everyone was like a zombie, just staring off in shock,” Bozorgzadeh says. This comment sparked an idea, which would later turn into a nationwide initiative.
124 AHL
As a psychologist working with many clients in healthcare, Bozorgzadeh says, “Healthcare workers are really used to being the heroes and putting other’s needs before their own. A lot of times, they don’t take a lot of time for themselves, and they’re so used to that, that they don’t even really know how to.”
Knowing that self-care is not often second nature to healthcare workers, Bozorgzadeh launched Caring for Caregivers in April 2020, which would help give this population respite and emotional healing by meeting individuals like nurses, doctors, techs, and hospital staff where they already were: in the hospital break room.
“Prior to the pandemic, when we were doing wellness programs for hospitals, one of the challenges that has always been present with this population is that their schedule is focused on their patients,” Bozorgzadeh says. “The people that do come to workshops might get paged, and part of them is distracted.”
The Sufi Psychology Organization found that, while organizations were providing support through apps and online support groups, individuals working in healthcare often asserted that they didn’t want to attend or open an app once they’ve left the hospital.
“It’s not like other jobs where you can have a big meeting that everyone attends, and you can do a whole workshop for them,” Bozorgzadeh explains. “We knew we needed something they can use on their own time.”
The resource provided through the Caring for Our Caregivers initiative were electronic devices preloaded with videos from its sister organization, an app called Tamarkoz, which provides users with guided meditations using the Tamarkoz practice—a form of Sufi meditation
that enables individuals with the ability to connect with themselves through meditation and concentration.
“I use it both with healthcare workers and oncology patients,” Bozorgzadeh says. “The research that had been done on this form of meditation showed that people who were regularly practicing would see an increase in positive emotions, even in stressful times.”
Videos from the Tamarkoz app, ranging three to thirty minutes, were donated to the Caring for Our Caregivers cause and encompassed different components of meditation, including mindfulness, breathing exercises, movement practices, visualizations, and guided imagery. And to avoid potentially dangerous Wi-Fi interference at the hospital, each tablet is Wi-Fi disabled.
The Impact 125
“We find that in the middle of difficult situations, you don’t have the resources to tell yourself what you need— you’re kind of on autopilot.”
“It’s not like other jobs where you can have a big meeting that everyone attends, and you can do a whole workshop for them. We knew we needed something they can use on their own time .”
126 AHL
“With this practice, we were able to have multiple forms of stress relief in these tablets. So, no matter who the person is they can pick something that fits them,” Bozorgzadeh says.
According to Bozorgzadeh, the devices are meant to work in tandem with the culture of healthcare workers, who naturally look out for each other. Fellow nurses and clinicians are often able to notice when coworkers are at the point of burnout. Because of this, being able to direct stressed employees straight to a resource in the hospital makes it more likely that staff members will use it.
Dr. Saloumeh Bozorgzadeh President Sufi Psychology Association Founder Caring for Our Caregivers

“Our hope is that people in the hospital will tell each other to take breaks,” she says. “We wanted something there in the hospitals in the midst of crisis, so if they need an emotional break from what they’re going through, they have something there that can guide them.”
So far, these tablets, along with individually wrapped disposable headsets, have been donated to more than 340 hospitals in all 50 US states, as well as in 4 other countries. Yet, Bozorgzadeh wants to see more mental health-focused work in hospitals even after the pandemic comes to an end. She says, “I think this issue [burnout] needs to be escalated and elevated to the forefront of administrators’ minds.”
Bozorgzadeh states that money needs to be carved out for programs to support the emotional, mental, and physical health of healthcare staff. Beyond the money, though, the programs provided need to consider the psychology of the healthcare worker. “It’s not a onesize-fits-all approach,” she says. “You have to cater for how they think.”
For a staff so focused on the well-being of others, the opportunity to take time out of the day to simply slow down and breathe promotes happier employees and better patient care. But more than anything else, a program like Caring for Our Caregivers gives healthcare workers something they deserve day to day: a taste of their own nurturing medicine. AHL
The Impact 127
Maia Rosenfeld
With a Mission in Mind
Whether she’s supporting UNC Health through community initiatives or overhauling HR operations as a result of the coronavirus pandemic, Janel Lancaster works to keep North Carolinians healthy
By Taylor Karg
Since joining UNC Health as a senior compensation analyst in 2012, Janel Lancaster’s roles and responsibilities have evolved quite a bit. Now, as the system executive director of total rewards, human resources data, and customer experience, she’s responsible for compensation, employee benefits, HR data governance, ergonomics, and workers’ compensation.
UNC Health is an inclusive organization with nearly forty thousand diverse employees whose mission is to improve
the health and well-being of the unique communities it serves.
While Lancaster earned a bachelor’s degree in finance and a master’s in business analytics, most of her professional experience lies in HR. She was initially exposed to the industry while working in the finance department at Hall County Government, a local government agency in Gainesville, Georgia.
“I started as the payroll manager, which at the time, was in the finance department,” Lancaster says. “After a
128 AHL
 Janel Lancaster System Executive Director of Total Rewards, HR Data & Customer Experience UNC Health
Janel Lancaster System Executive Director of Total Rewards, HR Data & Customer Experience UNC Health
The Impact 129
David Williams
while, payroll transitioned into the HR department and I was asked to take on additional HR-related duties. I worked there for over six years and my role continuously evolved to include HRIS (human resource information systems), recruitment, and a generalist role.”
Lancaster and her now husband relocated from the Atlanta metro area to Raleigh, North Carolina, in 2011, and she began working at phonebook and digital advertising company DexOne. After about a year, the company announced it was being acquired and would be relocating HR to Dallas, forcing Lancaster to find another position.
This time around, Lancaster says, she was looking for a company whose values and beliefs matched her own. She came across the position at UNC Health, and as Lancaster puts it, “the rest is history.”
“I truly enjoy working for UNC Health. The company has a great mission—to support the health of North Carolinians— which aligns with my personal values. I’ve also been presented many opportunities to advance my career while working here,” says Lancaster, who will be celebrating her ninth anniversary with the Chapel Hill, North Carolina-based organization in October 2021.
Over the years, Lancaster has even helped UNC Health launch several community initiatives that align with its mission, including the notable Living Wage Project. The project, which rolled out in July 2019, raised the minimum pay rate to $15 per hour in the Triangle area—Raleigh, Durham, and Chapel Hill. “Being a leader in the state’s health system and raising the living wage opened the door for other businesses to follow suit,” Lancaster says.
Today, as the system executive director of total rewards, HR data, and customer experience, Lancaster’s day is filled with many competing priorities, and she tries to balance it all. “We’re now in the stabilization phase of the HR ERP (enterprise resource planning) software we implemented in December 2020, so my days are filled with navigating any system issues that may arise,” Lancaster says. “We’re also constantly navigating creative HR solutions for the rapidly changing healthcare market due to the ongoing challenges of the COVID19 pandemic.”
Like much of the world experienced, Lancaster and her team came into work one day and their environment, as they once knew it, completely shifted. “We had to put our normal practices on hold: we had to be adaptable and creative to address the new daily challenges that were affecting our staff,” she says.
In addition to collaborating with her colleagues in daily HR leadership meetings, Lancaster coordinated with both her team and the IT team to overhaul operations—essentially overnight. Together, they implemented a teleworking portal that allowed managers the ability to identify which members of their staff needed to transition to working remotely. The portal was also used to determine staff equipment needs such as laptops, monitors, and keyboards, and allowed leadership to provide each other with data to help make timely decisions around next steps. According to Lancaster, the portal was a huge success.
Among the other operational changes Lancaster and her team implemented as a result of the pandemic were a new subsidy program, childcare resources, paid time
130 AHL
The Impact 131
“We had to put our normal practices on hold: we had to be adaptable and creative to address the new daily challenges that were affecting our staff.”
CompLogix is a Human Capital Management software company based in Omaha, Nebraska, that provides a suite of cloud-based systems to support critical phases of the employee life-cycle.




Our user-friendly and intuitive compensation management tool paved the way for a complete suite of robust solutions to support talent management and HR processes. Our innovative compensation management system has been our main focus for over a decade.
We opened our doors in 1998 and have been working with national and global clients ever since — helping them create a web-based solution that is easy-to-use, robust and streamlined to make their compensation planning easier.




COMPENSATION MANAGEMENT





PERFORMANCE
MANAGEMENT
TOTAL REWARDS STATEMENTS

SHARE OWNERSHIP COMPLIANCE



www.complogix.io
Gene Moore gene.moore@complogix.io 402.597.3722, Ext 103
off flexibility, additional compensation for clinical staff, and policy revisions.


Lancaster and her team also had to adjust the total rewards strategy to accommodate the rapidly changing healthcare market. “Now, we’re reviewing benchmark data on a more regular basis. We’re using nontraditional market data and reaching out to associations regarding the pulse of the market so we can be a leader in the industry. We’ve implemented additional benefits to ensure the well-being of our teammates, and we’re constantly evaluating our benefits program and enhancing as needed,” Lancaster says.
Now, Lancaster says, the organization is in a phase of what they call “Working Forward,” meaning they’re determining which teammates will go back to the office and which will remain remote. However, Lancaster notes that because their transition to remote work was so successful, a large portion of teammates will remain at home going forward.
Lancaster points to her team, the other HR teams, and the entire organization for how well UNC Health handled—and
overcame—the challenges inflicted by the pandemic. “We’ve always been an adaptable, flexible, and creative organization, but the pandemic reinforced that fact,” Lancaster says.

Additionally, Lancaster attributes UNC’s success to its compensation management system, CompLogix. “Our partnership with CompLogix has provided better communication to our leaders and impacted teammates regarding pay increases, incentive plans, and total reward statements,” she explains.
“It also allowed the compensation and benefits teams to focus on other aspects of not only handling the pandemic but their everyday duties as well, such as enhancing our programs and brainstorming creative strategies,” she adds. “They weren’t bogged down with the technical work [of] manually administering those programs, which is what we were doing in the past.”
Looking to the future, Lancaster remains focused on the job, and more specifically, on supporting UNC Health’s teammates with new and creative HR solutions. AHL
132 AHL
“We’ve always been an adaptable, flexible, and creative organization, but the pandemic reinforced that fact.”
Wendy Xia (p.44) stands in front of Agios’ Patient Wall, which is adorned with the faces of people that the organization has helped throughout the years. It’s meant to enable a connection to Agios’ global community and serve as a reminder to everyone at the company that their work affects—and saves—real lives.

Contents 133
Tony Luong
People & Companies
A Agios Pharmaceuticals 44 Aleman, Steve 98 Atara Biotherapeutics 112 B Bozorgzadeh, Dr. Saloumeh 124 Bristol Myers Squibb 80 C Campbell, Patricia 90 Caring for Our Caregivers 124 Cedars-Sinai 90 D Detmer, Dr. Wayne 52 F Farm on Ogden, The 52 Franciscan Alliance 40 G Garvey Goldthorpe, Catherine 70 Glazier, Dr. Eve 28 H Haynes, Risa 10 Hines, Maribel 112 Humaidi, Mohamed 40 J Jones, David 64 L Lancaster, Janel 128 Love Fridge Chicago, The 10 M Mallinckrodt Pharmaceuticals 106 Mammen, Adrin 34 Mason, Angela 52 McElligott, Dr. Jimmy 22 Medical University of South Carolina 22 Montefiore Health System 34 P Papa 74 Parker, Andrew 74 Phynd, a symplr company 84 Prime Healthcare 98 Pufko, Bill 80 S Short, Jeffrey B. 34 Stanford Health Care 64 T Taavola, Lars 106 U UCLA Health 28 UNC Health 128 University of Chicago Medical Center 70 UPMC 118 W White, Thomas 84 Wood, Carolyn 118 X Xia, Wendy 44 134 AHL



Empowering Benefits Programs with Unmatched Data

Aon’s Executive Benefits Practice has spent 40 years developing expertise in the design, funding, and administration of benefits for physicians and executives — to best meet the unique needs of tax-exempt hospitals and health systems. The tailored enrollment, communication, and administrative services we offer optimize the benefits our clients provide to their key employees, and this is how we set ourselves apart. At Aon, we take pride in our staff, which includes specialists in compliance and human resources, insurance product development and underwriting, healthcare operations, and benefits administration. We work together to deliver the highest quality products and services in the benefits consulting marketplace.
aon.com/executivebenefits












 Chris Schmitt (Hines), David Williams (Lancaster), Gillian Fry (Farm on Ogden)
Chris Schmitt (Hines), David Williams (Lancaster), Gillian Fry (Farm on Ogden)





 By KC Esper
By KC Esper





 Fridges
Fridges









 ▶ Pilsen Food Pantry is one of the main suppliers and distribution centers of nonperishable food and dry goods donations for the Love Fridge. They also share bottled water and canned coffee, which are popular staples among fridge users.
▶ Pilsen Food Pantry is one of the main suppliers and distribution centers of nonperishable food and dry goods donations for the Love Fridge. They also share bottled water and canned coffee, which are popular staples among fridge users.




























 Jeffrey B. Short VP, Transformation Officer, Chief of Staff, and Leader of the Faculty Practice Physician Group Montefiore Health System
Adrin Mammen AVP and Patient Access Transformation Officer Montefiore Health System
Jeffrey B. Short VP, Transformation Officer, Chief of Staff, and Leader of the Faculty Practice Physician Group Montefiore Health System
Adrin Mammen AVP and Patient Access Transformation Officer Montefiore Health System









 By Billy Yost
Portraits by Tony Luong
By Billy Yost
Portraits by Tony Luong








 Photos by Gillian Fry
Photos by Gillian Fry








 Angela Mason AVP of Community Engagement and Senior Director Windy City Harvest
Dr. Wayne Detmer Chief Clinical Officer of Operations Lawndale Christian Health Center
Angela Mason AVP of Community Engagement and Senior Director Windy City Harvest
Dr. Wayne Detmer Chief Clinical Officer of Operations Lawndale Christian Health Center

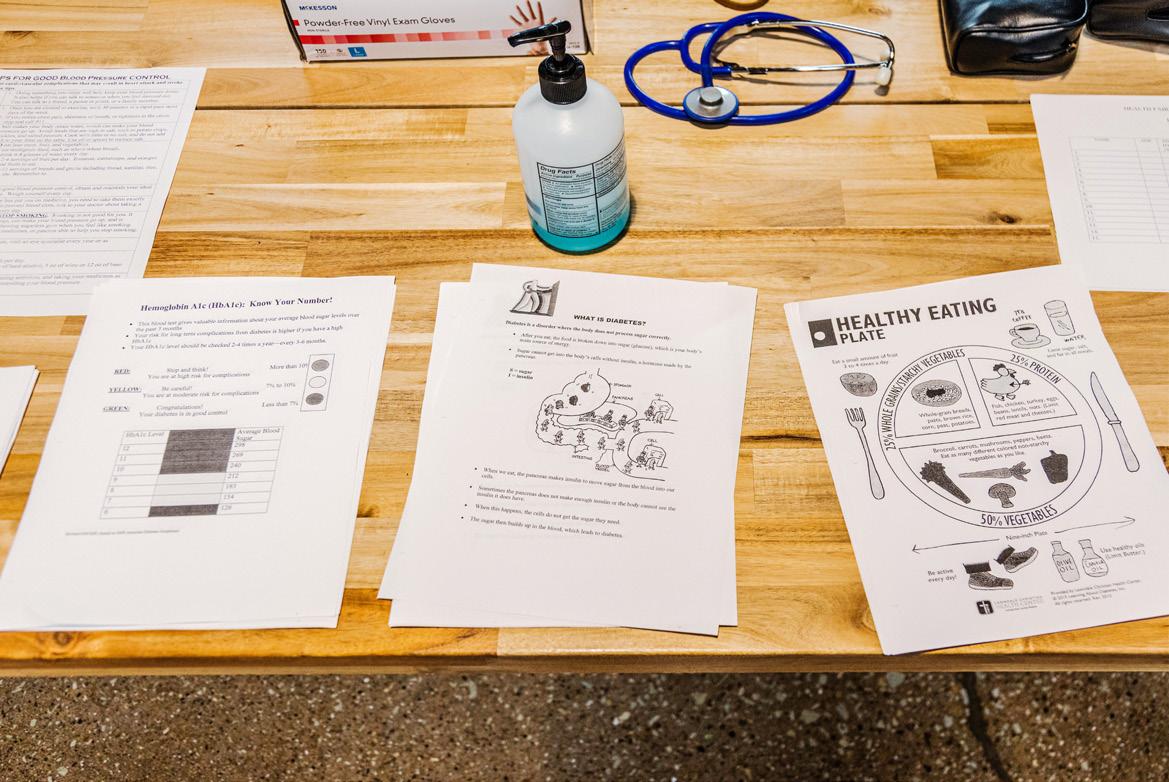



















 By Zach Baliva
By Zach Baliva
 Catherine Garvey Goldthorpe Associate General Counsel and Executive Director of Professional Liability University of Chicago Medical Center
Catherine Garvey Goldthorpe Associate General Counsel and Executive Director of Professional Liability University of Chicago Medical Center
 Andrew Parker CEO and Founder Papa
Andrew Parker CEO and Founder Papa
 Bill Pufko Chief Counsel for Environment, Occupational Health, Safety & Sustainability
Bristol Myers Squibb
Bill Pufko Chief Counsel for Environment, Occupational Health, Safety & Sustainability
Bristol Myers Squibb
 BILL PUFKO
CHIEF COUNSEL FOR ENVIRONMENT, OCCUPATIONAL HEALTH, SAFETY & SUSTAINABILITY AT BRISTOL MYERS SQUIBB
BILL PUFKO
CHIEF COUNSEL FOR ENVIRONMENT, OCCUPATIONAL HEALTH, SAFETY & SUSTAINABILITY AT BRISTOL MYERS SQUIBB
 Thomas White CEO Phynd, a symplr company
Thomas White CEO Phynd, a symplr company








 Steve Aleman CFO
Prime Healthcare
Steve Aleman CFO
Prime Healthcare










 E. Melnick, Ph.D.
E. Melnick, Ph.D.







 Maribel Hines
Senior Director of Global Talent Development, Diversity & Inclusion Atara Biotherapeutics
Maribel Hines
Senior Director of Global Talent Development, Diversity & Inclusion Atara Biotherapeutics





 Carolyn Wood VP of Employee Benefits UPMC
Carolyn Wood VP of Employee Benefits UPMC

 Janel Lancaster System Executive Director of Total Rewards, HR Data & Customer Experience UNC Health
Janel Lancaster System Executive Director of Total Rewards, HR Data & Customer Experience UNC Health






















