The Blueprint for a Longer Life

Dan Buettner embarked on a mission in 1999 to learn how communities foster generations of centenarians. Today, his Blue Zones Project brings those lessons to other regions around the world. P34






Dan Buettner embarked on a mission in 1999 to learn how communities foster generations of centenarians. Today, his Blue Zones Project brings those lessons to other regions around the world. P34








Keeping
P8
people well means more than medicine. See how leaders are changing their approach to care by considering patients’ wellness inside and out.
Lauren Misztal uses her diverse experience to guarantee efficient, cost-effective work for Mallinckrodt

▶ P50
At Gilead, Dr. Tashica Williams Amirgholizadeh keeps her love of science and learning at the heart of her profession
P59
From bandmate to head counsel, Andy Cohen brings a unique set of skills and a unified culture to Takeda
P64

Colin McDonald helps bring Cross Country Healthcare updated HR systems and a greater edge for diversity
P72
DentaQuest’s Nicholas J. Messuri nips healthcare fraud in the bud to ensure access to care for millions of customers
P75
Galia Porat helps craft a products-based settlement that positions Teva to address the American opioid epidemic

◀ P80

At Sutter Health, David Prahl uses an all-inclusive approach to shape the company’s complex litigation strategy

P86
Mary Klassen Szyndrowski adapts to improve support for the American Medical Association’s employees
P90
CHRO Susi Takeuchi allows UCLA Health’s HR department to float above its competition


◀ P96
Dan Buettner was photographed
an
based in Miami. To view more of her work, visit mbkoeth.com.
At Parkland Health, Gerry Baker looks to improve revenue cycle functions to impact today and the future
P104
CHOC’s Lynn Grieves keeps an open mind and a steadfast attitude to help anyone—or any place—persevere through tough times
▶ P114
by Mary Beth Koeth, artistCREATIVE
Director, Creative Production
Kevin Warwick
Managing Editor
KC Esper
Senior Editor
Frannie Sprouls
Editors
Melaina K. de la Cruz
Sara Deeter
Hana Yoo
Staff Writer
Billy Yost
Journalism Resident
Lindsey Lubowitz
Contributing Writers
Zach Baliva
Lucy Cavanagh
Peter Fabris
Donald Fricke
Natalie Kochanov
Keith Loria
Zack Price
Clint Worthington
Senior Designer
Vince Cerasani
Photo Editors & Staff Photographers
Cass Davis
Gillian Fry
CORPORATE
CEO & Publisher
Pedro A. Guerrero
Chief of Staff
Jaclyn Gaughan
President, Group Publisher
Kyle Evangelista
VP, Hispanic Division
Head of Audience & Engagement
Vianni Lubus
VP, Finance
David Martinez
Director, Client Services
Cheyenne Eiswald
Senior Client Services Manager
Rebekah Pappas
Client Services Manager
Brooke Rigert
Director, Talent Acquisition
Elyse Schultz
Senior Talent Acquisition Manager
Jacqui Bergman
Haylee Himel
Director, Strategic Partnerships
Krista Horbenko
Director, Events
Jill Ortiz
Digital Events & Marketing Coordinator
Ashley Parish
Senior Director, Sales
Ben Julia
Director, Sales Training & Development
Alexa Johnson
Content & Advertising Managers
James Ainscough
Megan Apfelbach
Ahmad Douzali
Kelsey Price
Kelly Stapleton
Drew Thomas
AHL Magazine® is a registered trademark of Guerrero, LLC.
Facebook: @ahlmagazine
LinkedIn: @american-healthcare-leader
Twitter: @AHL_Magazine
©2021 Guerrero, LLC guerreromedia.com
770 N. Halsted, Unit 307 Chicago, IL 60642
Reprints
Reprinting of articles is prohibited without permission of Guerrero, LLC. Printed in China. For reprint information, contact Reprints & Circulation Director Stacy Kraft at stacy@guerreromedia.com.
The week before I moved to Chicago, my grandma gifted me a copy of her favorite book of poetry: Poems from the Pond by Peggy Freydberg.
I loved it (and still do). The book itself is beautiful. The cover is wrapped in soft, sand-colored canvas and each poem is accompanied by bright photographs of Martha’s Vineyard, where Freydberg lived. The poems inside are sincere, observant, funny, painful, and everything in between. The most amazing aspect of the book, however, was neither the cover nor the poetry—it was the author.
Freydberg started writing poetry when she was ninety. Her work was chosen to be published after she gave a reading at the age of 106, and when the book was printed, she was 107 years old.
Throughout her life, and even at 107, Freydberg woke up every day ready to fulfill her purpose. She was closely connected to her kids, their kids, and their kids’ kids. She spent much of her time outdoors observing Stone Wall Pond, the pond referenced in the title of her book. She had two beloved cats who inspired her to write her most joyful poem: “A Letter to My Family, Explaining How I Feel About My Cats.” By all accounts, Freydberg was following the recipe for a long life, though perhaps unintentionally.
This issue of American Healthcare Leader is all about living longer, better. It details the lengths we go to find the solution to longevity and introduces the people who are working to help bring others the means to live healthier lives. As you read the stories in this magazine it’s clear that a single long life cannot be achieved by one person alone. Meaningful years are supported by community, nourishment, accessibility, and, in many cases, luck.
Freydberg’s poetry can teach us a lot about the ingredients that make a life well lived, but her work is also proof that one’s purpose has no expiration date and it’s never too late to chase a dream. To close, I’d like to offer a short excerpt from Freydberg’s poem, “Wait A Minute.” It’s in this stanza where perhaps the most important lesson about living can be found: to just keep going.
I will get up and start to seek and continue starting, so that every minute of this day will begin with an anticipation of the promise of the next one.
KC Esper Managing Editor

Five leaders on what it takes to enable healthier communities with a focus on mind, body, spirit, and environment


Mike Berger taps into the power of data on social determinants of health to enhance value-based care
By Keith Loria
Mike Berger describes himself as “always being an efficiency guy.” He’s always trying to build great process into everything he does. He studied industrial engineering in college and after graduating, went into consulting, where he was hired to improve processes in companies. Fast forward to today, he’s doing the same thing with data and analytics—the ultimate tools to improve the speed and accuracy of decision-making.
“I was in that mode for a good ten years and was good at putting in systems and applications that would help companies become more efficient,” Berger notes. “At the time, there wasn’t much thought about improved decision-making from analytics.”

By 2009, Berger made a switch to the healthcare space, running a reporting team for North Shore-LIJ Health System. He started building dashboards and showed them to leadership at the hospital. The feedback the leadership team provided, however, would change his trajectory.
After showing off the dashboards, the hospital leaders practically laughed him out of the conference room, saying Berger and his team had “no idea what actually happens in the hospital.” Fortunately, one motivating leader invited Berger to join her on rounds to get him out of “finance thinking.” More importantly, it allowed him to see exactly what healthcare workers face on a given day, which in addition to working with patients, includes working with hacked together Excel spreadsheets and an almost complete lack of information to make decisions.
“This is where they are delivering patient care and it seemed totally broken,” Berger recalls. “I had my ‘a-ha’ moment and thought that’s where I need to get involved. I want to help those people.”
He left finance and moved into a more centralized IT role around 2011, building North Shore’s data strategy and learning everything he could about modern data platforms. Berger ended up taking a position with Geisinger Health System, running their enterprise data warehousing and analytics competency center, which he notes was far ahead of its time, having been on Epic for over eighteen years at that point.
“They had some good reporting and analytics, but they didn’t know how to modernize,” he recalls. “This was a great opportunity for me to see what high-performing analytics looks like and it convinced me that I needed to get deeper into data science if I was going to help my organization truly unlock the value of analytics.”
So, Berger headed back to school, earning a master’s in data science from NYU’s Stern Business School. At the same time, he joined Mount Sinai Health System when they were looking for someone to deliver analytics for their newly formed population health division, which would manage risk on hundreds of thousands of lives.
“Over the past five years now, I’ve been heads-down in the data science and engineering space,” he explains. “I now understand the technology and the methodologies; but most importantly, I’m focused on how to improve decision-making on the front lines of healthcare, whether it’s decisions about a patient, a bill, a business investment, or even something larger.”
That’s the key focus of his role as chief data and analytics officer and vice president of enterprise data and data science.
“If everyone is making great decisions, you’re going to make money and achieve your mission,” Berger says. “The question we ask all the time is ‘How do we help decision making?’ and, more so, ‘How do we do it at a really high level?’”
A major focus of Berger’s teams is to use data to better improve the health and wellness of his patients by understanding how to incorporate an understanding of the social determinants of health into people’s care. He explains that a person’s health comes from genetics, from how well they are managing their chronic conditions by seeing their physicians regularly and PCP annually and adhering to their medication, as well as their engagement to take care of themselves through diet and exercise.
Research now shows, however, that if people are experiencing social determinants like housing insecurities or food disparity, then their ability to manage clinical conditions like diabetes or mental health are almost always far down on their priorities.

“Health systems now want even more data—they want to know about the patient when they’re not at the hospital or not in the doctor’s office.”

“These social detriments are extremely important. If you’re going to have a mission of really helping people be well instead of just fixing them when they are sick, you better understand their social situations,” Berger explains. “Do they have literacy issues? Do they have a way to get to a doctor or clinic if they need help? If you don’t come up with a plan to collect this information, understand it, and fix it, you will have a hard time effecting the right patients.”
Thanks to Berger’s data, Mount Sinai is able to better track the marriage of clinical information like procedures and diagnoses with their specific social determinants of health to build an effective and holistic method of prioritizing who needs help.
Connecting clinical intelligence with diagnoses also helps Mount Sinai understand and quantify reimbursement and care gaps, where a natural language processing-driven risk adjustment solution from Health Fidelity supports their efforts. Adam Gronsky, chief innovation officer at Health Fidelity, notes, “Mike recognized the power of NLP to improve coding accuracy at scale, but also saw its potential for unlocking previously untenable insights. He’s always looking to expand and develop new ways to apply our solutions to support the population health mission at Mount Sinai.”
Data is helping enhance population health outcomes, though Berger still calls it a “number’s game,” and his team continues to work with Health Fidelity to improve its prioritization and outreach approach to help understand who might have acute issues, and the factors driving those.
“We work with a team of nurses and social workers to outreach the patient, even when they don’t know who we are, but we know who they are and we care,” he explains. “We are going to share the data and try to get them motivated and engaged in managing their health and wellness and hopefully fix some of their issues.”
Part of being in a risk-bearing relationship like this, Berger adds, is to serve as “the angel on their shoulders” and make sure the data is being used for the betterment
of whoever needs help. If a patient has a clear opioid addiction, for example, by looking at their longitudinal information, you could see they’ve gone to numerous emergency rooms in the past twelve months. That clinical history is telling of their situations and the dates of these visits are used to create a real-time picture of the doctor at the point of care.
“If it was just about saving money, that would be easy; you just close the network and make it really hard for them to access care. That’s a lot of what happened in the ’80s when HMOs first came out,” he says. “When CMS and some of these other advocacy groups started rethinking what risk-bearing value care looks like in the last decade, they set expectations around quality and patient satisfaction and incentivized doctors to properly care for patients.”
Looking forward, Berger expects to get even more precise with data to better predict which populations will have acute issues, as well as the types of interventions most likely to change the outcomes for the better.
“We are seeing a virtuous cycle of data as people see that clinical decisions can be better with more data,” he notes. “Health systems now want even more data—they want to know about the patient when they’re not at the hospital or not in the doctor’s office. We’re seeing a lot of advancements in remote patient monitoring or the Internet of Medical Things, and the fact that we are a risk-bearing entity incentivizes us to keep the patient well. Data is making this all possible.” AHL
Accenture is a global professional services company with leading capabilities in data, analytics, and cloud. Combining unmatched experience and specialized skills across more than forty industries, we offer strategy and consulting, interactive, technology, and operations services—all powered by the world’s largest network of advanced technology and intelligent operations centers.




hones technology that reads clinical notes to improve value-based reimbursement performance
By Peter FabrisRoughly 110 million Americans are covered under value-based care (VBC). Risk adjustment is a significant component to VBC success; all covered lives have an estimated cost of care, and each patient has a unique “risk adjustment factor” based on various conditions, which acts as a multiplier of that estimate. The sicker the patient, the greater their maximum reimbursement.
If the cost of care comes in under that maximum, the difference is shared as revenue between the federal government and the health plan or provider organization (health systems and physician practices), whichever has assumed risk for that patient. This financially incentivizes organizations to provide thorough care at a lower cost. And it’s working—value-based care has grown exponentially in recent years.
Risk adjustment is complex for the CMS (Centers for Medicare & Medicaid Services) to administer, though. In order for organizations bearing risk to receive an accurate reimbursement, they must report the precise code or codes that match the full breadth of conditions documented for each patient visit, each year.
To do so, professional coders must interpret each visit’s data to submit the correct codes for each encounter. The clinical evidence for accurate codes is often in unstructured, difficult-to-access data. That’s where Health Fidelity’s software platform Lumanent comes in.
Lumanent simplifies risk adjustment for providers and payers by parsing unstructured clinical data (including physicians’ notes), highlighting areas where over- or under-coding has occurred (with the associated
clinical evidence), and sending to a coder for review. The technological key to the company’s product is a natural language processing (NLP) engine, a form of artificial intelligence, says Adam Gronsky, chief innovation officer for Health Fidelity.
“Our NLP is one of the few purpose-built to process clinical data. Since its inception, it’s ingested 107.7 million separate clinical records, each contributing to its maturation,” Gronsky says. “Years ago, only payers paid attention to risk adjustment via a retrospective model. As more organizations [like providers] adopt risk, we keep finding new applications for the engine and developing solutions to deploy it.”

Gronsky’s career path includes a master’s degree in healthcare administration and management, and a stint as senior product manager for the University of Pittsburgh Medical Center’s Technology Development Center from 2011 to 2015. His experience spans both sectors of healthcare—payer and provider—and he interacts with Health Fidelity clients directly.
His enthusiasm and knowledge clearly show how Gronsky has become a trusted advisor to many of them. These interactions motivate him to think beyond current offerings and consider ways to reshape how clinical risk is understood and managed. The aforementioned artificial intelligence component reads and understands written providers’ narratives describing interactions with patients and resulting findings and diagnoses.
“NLP can read and understand both unstructured data, which makes up 80 percent of all clinical data, and written paragraphs—even slang—and present it to a coder as evidence,” Gronsky says. This information
“Years ago, only payers paid attention to risk adjustment via a retrospective model. As more organizations [like providers] adopt risk, we keep finding new applications for the engine and developing solutions to deploy it.”


“You want to manage and treat the whole patient, not just the condition the patient is presenting with.”
cannot be accurately conveyed as structured data, simple checklists, or pull-down menus that computers can easily read. Many medical conditions are too nuanced and complex for that. For organizations dependent on clinical evidence to substantiate diagnosis coding, it enables population-wide reimbursement accuracy to be easily attained.
The platform can also discover if a diagnosis is not supported by sufficient evidence, suggesting that it be deleted. This protects the organization from audits and saves taxpayer money. The platform does not automatically add or change coding, but rather empowers human coders to better use their own expertise.

Gronsky also oversees the application of machine learning to the tool, which allows the platform to improve over time. “The system learns based on enduser actions and data ingestion,” Gronsky says. “It identifies patterns indicating that certain codes are or are not accepted based on what is contained in case documentation, and it’s got a 95 percent acceptance rate for identifying the correct coding category.”
The platform’s Pre-Encounter Prep module goes beyond reimbursement. When a patient is scheduled for an appointment, the tool analyzes the patient’s documentation and notifies providers of any suspected but unconfirmed conditions.
“The system really shines in physician practice settings,” Gronsky says. For example, let’s say you are a physician that has been treating a patient for congestive heart failure and diabetes for three years. This patient then comes to your office with complaints suggestive of sinusitis. But, since the patient is suffering from those other serious chronic conditions, when the appointment is set, Health Fidelity’s Pre-Encounter Prep notifies the care team if those conditions require annual reconfirmation for complete and accurate risk capture. With
Adam Gronsky Chief Innovation Officer Health Fidelitythat, you not only treat the sinus issue but also evaluate the patient’s status pertaining to the heart problem and diabetes. This is well-rounded medical practice.
“You want to manage and treat the whole patient, not just the condition the patient is presenting with,” Gronsky says. This is the goal of value-based care— treating the patient holistically rather than addressing only the most current acute issue. It’s a practice that should result in better patient care and reduced costs over the long run.
Since 2015, when Gronsky joined Health Fidelity, he has been immersed in a leadership role, driving innovation toward enabling payers and providers to more efficiently perform and leverage risk adjustment. The work is paying off. One major national health system increased its overall risk capture by nearly 15 percent over three years after implementing the Health Fidelity platform. That has resulted in a gain of $12 million compensation annually for the client, and significant savings for Medicare.
These shared benefits are just what the risk adjustment model is supposed to deliver, providing proof that Gronsky’s efforts are bearing fruit—and that there will be more to come. AHL




 By Billy Yost
By Billy Yost
On January 1, 2020, Todd Archbold stepped into the CEO position for Minnesota-based PrairieCare. The CEO has been with the organization for nearly fifteen years, and his elevation to the highest position in the executive suite is inspirational for a litany of reasons. A youth sports coach, school counselor, school social worker, and eventual healthcare social worker, Archbold’s uncommon path is the result of a motivated individual continually seeking to find new ways of positively impacting people’s lives.
Archbold’s promotion to CEO would be the obvious moment to stop and celebrate, looking back on a career that is already flush with so many unique twists and turns. Archbold may have been able to take that brief pause were it almost any other year than 2020. “Those first ten weeks, things were fantastic,” Archbold says, laughing. But the COVID-19 pandemic would provide Archbold, PrairieCare, and the entire healthcare industry at large one of the most challenging periods in American history.
PrairieCare is in an especially unique position due to its full continuum of psychiatric services, the organization’s well-earned reputation for high-quality mental health care, and one of the largest psychiatric medical groups in the region (of the 750 staff, over 200 are licensed clinicians and 45 are psychiatrists). “Even with that [mental health] staff, we still can’t meet all of the demand here in Minnesota,” Archbold explains. “There’s simply a demand for these services that still outstrips all of our growth.”
The growth the CEO speaks of is formidable by any standard. “We had a 30 percent growth rate every year for ten years with patient encounters,” he says. “One of my first initiatives as CEO was to build a culture focusing on communication, accountability, and planning. With that kind of explosive growth, I think we needed

to backtrack a bit and figure out appropriate channels to ensure accountability and maintain high standards.”

The strategy plan that the executive suite began working on in January (and deployed in July) 2020, has wound up being a vital reconfiguration during one of the most stressful periods in healthcare. “The new strat egy plan converging with the pandemic was probably the best thing we had going for us,” Archbold explains. “Our plan is based on refinement and excellence and has allowed us to create alignment throughout the organization. The focus on communication has helped ensure that our people are aligned in the planning process and with our strategy. It became our north star.”
PrairieCare’s EHR/RCM partner is impressed with Archbold’s visionary leadership. “Todd has a solid grasp of how technology can be scaled to benefit both patient care and operational performance,” says Yuval Lirov, ClinicMind president and CEO. “Todd has empowered his people to deliver a superior patient experience and achieve fantastic growth.”
And while Archbold has been focused on finding ways to increase efficiencies, it must be said that PrairieCare is an organization used to performing at incredibly high standards. “Throughout the pandemic, there have been extraordinary concerns over surges threatening hospital thresholds, many running at very high occupancy rates,” the CEO says. “That’s something I’ve been experiencing my entire career in acute care psychiatry. We are essentially experts at running at max capacity. The difference between operating sixty-five and seventy beds in our hospital can quickly amount to an extra two hundred people receiving critical care each year. We take that very seriously.”
It’s not just the volume but the quality of care that has set PrairieCare apart. Its mental health organization just recently received two national awards from both
“Our plan is based on refinement and excellence and has allowed us to create alignment throughout the organization. The focus on communication has helped ensure that our people are aligned in the planning process and with our strategy.”


the American Psychiatric Association as well as the Association of Medicine and Psychiatry for its outstanding innovation in patient care.
The Psychiatric Assistance Line (PAL) allows any healthcare provider in Minnesota to be immediately connected to a clinical social worker to help with assessment or referral, or one of its psychiatrists to help pediatricians better understand the differences between anxiety and ADHD, or an OB/GYN looking for more information on helping a patient deal with postpartum depression.
“It’s not interacting with a healthbot or leaving a message that you hope to have returned at a convenient
time,” Archbold explains. “It’s instantaneous so they can get the help while they’re sitting in their office with the patient.” In a time when PrairieCare has seemingly taken a pause from massive expansion to get its house better in order, it’s still finding ways to earn national recognition for innovation.
But on this issue, the CEO is as humble as one might expect a former guidance counselor to be. “I don’t think of it as innovation, that’s the kind of word I think of when I think of a company like Tesla,” Archbold says. “This relates back to that refinement and excellence. I think we had the gumption to think that this was a very simple thing we could do that could make a profound difference. Maybe some of the most innovative things can be the simplest.”

The same thinking has been applied to colocating PrairieCare’s mental health professionals in primary care settings, hospitals, and even schools. At a local pediatric clinic, there are three therapists and a psychiatrist on staff. “We believe that if primary care asks the right questions, the need for mental health services will become apparent, so we’ve parked our clinicians in those office settings,” Archbold says. “We know if a primary care provider makes a referral to see a psychiatrist, there’s a 50 percent chance the patient will follow through. So why not have that primary care physician walk the patient down the hall, in an environment the patient already recognizes? This is integrated care done right.” AHL
 Todd Archbold CEO PrairieCare
Todd Archbold CEO PrairieCare


At Prisma Health, Michael Burke applies his expertise in disaster management to his role as EVP and CFO to promote safety and the greater good
 By Keith Loria
By Keith Loria

As COVID-19 began to make its tremendous impact on the US in March 2020, Prisma Health needed the expertise of someone who had experience guiding a healthcare facility through a crisis. And they found the right person: Michael Burke.

Burke’s career dates back to 1979. He started at small community hospitals and worked his way up to major hospitals at Duke, Tufts, and New York University before retiring early.
“I got bored,” Burke says, laughing, “and told someone that I would be willing to consider doing interim work to help turn places around. The opportunity came for me to come [to Prisma] right at the peak of the pandemic. They wanted somebody who had been through a disaster before, and since I helped managed finances at NYU when they were closed for three months after Hurricane Sandy, I had an idea of what we needed to do.”
Burke’s work at NYU post-Hurricane Sandy in October 2012 included setting up a disaster accounting group and implementing procedures to recover as much money as possible. He has led similar initiatives at Prisma Health.
“What you have to do in these types of situations is get everybody to start realizing that their focus has to be on getting through and over the hump of the disaster, so to speak,” Burke explains. “You have to have everybody focus, all-hands-on-deck, on dealing with the disaster. At the same time, you basically freeze anything that you were doing from a spending standpoint, if possible, so that you can save that money—you’re going to need that to keep the places you have going operational. And you have to start operating differently so that you can deal with the disaster and still have cash.”
As the largest not-for-profit health organization in South Carolina, Prisma Health serves more than 1.2

million patients each year. Among many initiatives it took during the pandemic was establishing a facility exclusively for COVID-19 patients.
“We did that in about a week,” Burke remembers. “Anytime we found patients in regions where there was a spread, we would set up free testing sites in that region, do drive-through testing, and find people who tested positive and get them on their treatment to try to slow down the spread.”
Prisma Health also assisted nursing homes by providing them with doctors, testing residents, and supplying staff with personal protective equipment, or PPE.
“We started acting selflessly and started dealing with the health of the state, not necessarily worrying about whether we were going to meet our volumes,” Burke notes. “The government was good enough to give us a decent advance, and we kept applying for all the COVID relief funds as they came in so we’d have sufficient funding to be able to do things like that.”
Burke also notes that medical professionals are dealing with a different challenge as a result of COVID-19— people are not seeking treatment for chronic conditions or symptoms out of fear of contracting the virus in the hospital, thus delaying treatments for cancer or a stroke that should have been received sooner.
“Mortality is up because people are coming in with full-blown heart attacks and strokes when they could have gone in when they had other symptoms, like chest pains, and been treated earlier,” Burke says.
Of course, these fears could be quelled by properly educating the public about their risk of contraction as well as by providing them with the resources they need to stay healthy, starting with healthcare coverage. Burke strongly believes everyone should have access to basic healthcare and that there should be a public option.


“We’re trying to become a health company that protects the public health needs of the people. It’s not about making tons of money for a set of a few fortunate people, like those on Wall Street; it’s for the greater good of the state.”
“So that when you have these pandemic responses, people who are residing in their neighborhood that have symptoms of this virus can get tested and treated and stabilized,” he suggests. “And it doesn’t matter if they have private insurance, Medicare, Medicaid, or nothing. Everyone has to get the same treatment.”
After being offered the full-time role, Burke decided to stay on as Prisma Health’s chief financial officer in July 2020. One of the skills he has developed is the ability to unite people during a difficult time to continue

the organization’s important work. And at Prisma, that means putting the interests of patients first. It fits with the mission of Prisma to inspire health, serve with compassion, and be the difference.
“The team concept is really important in this,” he says. “Everybody has to work together for the goals for the team. The old adage ‘There’s no I in team’ is really true. These old adages are still around because they really apply. You have to do what’s best for everyone else and not what’s best for your own self-interest.”

In fact, the challenge to think differently and do what’s best for the community is one reason he was motivated to come out of retirement.
“I like doing this,” he says. “We’re trying to become a health company that protects the public health needs of the people. It’s not about making tons of money for a set of a few fortunate people, like those on Wall Street; it’s for the greater good of the state. I find that invigorating and important.”
It’s Burke’s hope that the pandemic will raise awareness of the need for a change in our country’s healthcare system.

“We have to take a different look at how we treat people as a society and our moral responsibility to the residents of our society,” he says. “Everybody should use this as a wake-up call as to what the country really needs as opposed to what we’re doing.” AHL
Versalus is a data-driven services company that helps hospitals improve performance in the clinical revenue cycle, where clinical decisions impact financial performance and compliance. We use data analytics to identify areas of opportunities and risk, work with hospital leaders and teams to translate data into actionable plans, and continuously monitor results to realize revenue opportunities.
KPMG helps organizations across the healthcare ecosystem work in new ways to transform and innovate. We offer market-leading portfolio tools and services to help clients comply with regulatory change, improve healthcare outcomes through data analytics, adapt to the consumerism of healthcare, transact to gain sustainable competitive advantage, and optimize technology.
power
dedicated people with passion.
why
want to recognize Mike Burke for his outstanding contributions.
exceeded expectations. And made a positive impact in the lives of so many.
Dan Buettner dedicates himself to teaching the lifestyle lessons he’s learned from the world’s longest-lived populations—and he’s only just begun
 By KC Esper
By KC Esper
Portraits by Mary Beth Koeth

What’s the secret to a longer life? Is it a perfect diet? The most expensive exercise equipment? Botox? Anti-aging serums? That magic spring from Tuck Everlasting?

In a consumeristic world like ours, where doing this and buying that promises a longer, forever-young life, it’s hard to imagine that the true solution to increasing our longevity would be simple—or possible at all.
In 1999, Dan Buettner embarked on a mission to discover how certain cultures around the world enable people to live well past their one hundredth birthdays. What he found was an obvious answer: people don’t try to live to be one hundred . . . they just do. Still, unless you’re born somewhere that enables this sort of longevity, “just doing it” may be impossible. It is possible, however, to take the principles those locations offer and emulate them in other communities around the globe. That’s what Buettner was determined to do.
Buettner’s story starts in Saint Paul, Minnesota. Growing up in a lower middle-class home, as one inside a six-person family, Buettner didn’t spend his youth at amusement parks or taking luxe vacations. Instead, his father, Roger, would drive him and his four brothers to the border of Canada to set up camp in the woods for weeks at a time. “We would go off the grid and live entirely off the land,” Buettner describes. “I was lucky to have a father like that.”
That gritty, salt-of-the-earth lifestyle transferred into his first job, too. At fourteen, he took a position selling newspaper subscriptions, where he learned how to communicate effectively with an audience and employ tools of persuasion to sell customers on a
concept. Then, at twenty-two, he met Remar Sutton, a then-columnist for the Washington Post, who, according to Buettner, is a “genius at creating visions and organizing events.”
After helping Sutton organize unique events, like a celebrity croquet tournament for National Public Radio, Buettner learned how to become a producer, how to create an event that generates publicity and gets sponsors, and, above all, how to get the public behind a concept that might seem out-there.
Buettner kept these kinds of skills handy as he pursued his own outlandish dreams: riding his bicycle across nearly every continent. “My father instilled this great zest for adventure,” he says, “and Remar showed me this ability to think big and then realize that larger vision. I knew I wanted to bike through South America, but I figured that without too much more effort, I could set a world record doing it.”
And he did. Buettner nonchalantly mentions this accomplishment, but the expedition was, naturally, anything but easy. Starting at the top of Alaska and ending at the tip of Argentina, Buettner and his brother rode more than fifteen-thousand miles, completing the first of three transcontinental bike rides that would each earn them Guinness World Records.
By 1992, Buettner and his team cycled across the Soviet Union—beating their previous world record by more than one thousand miles. And in 1993, they earned their third world record by riding from Bizerte, Tunisia, to Cape Agulas, South Africa. The latter trip inspired Buettner to write Africatrek: A Journey by Bicycle through Africa and coproduce a documentary using footage he shot during the ride.
“We stumbled upon a report from the World Health Organization that showed that Okinawans have the longest disability-free life expectancy in the world, and I said, ‘Aha! That’s a good mystery.’ If I can find out what they’re doing, maybe I can find a good recipe for the rest of us to follow.”

“It’s not the same kind of endurance needed to complete the Tour de France,” Buettner reflects. “It requires physical output for ten months, so you’re not going fast every moment. You’re going at a speed where you’re making decent miles, but you’re also stopping strategically so you don’t become fatigued or end up in a dangerous area.”
That pace allowed Buettner and his team the opportunity to absorb the cultures of each country—and each community—they passed through, which, in turn, inspired Buettner to create Quest Network, a company that sought to explain mysteries of ancient civilizations. Composed of archaeologists, biologists, and technologists, Quest Network was a team of fourteen people that used an expansive online audience to collaborate in answering a question like, “Why did the Mayan civilization collapse?”
“I got very good at synthesizing information in a scientifically responsible way to solve a mystery,” Buettner notes. “We stumbled upon a report from the World Health Organization [WHO] that showed that Okinawans have the longest disability-free life expectancy in the world, and I said, ‘Aha! That’s a good mystery.’ If I can find out what they’re doing, maybe I can find a good recipe for the rest of us to follow.”
That idea not only sparked his 1999 expedition but also a project bigger than Buettner ever could have expected. Tapping into the skills he learned as a young newspaper salesman and as an event organizer, he painted a vision of his research’s potential to eventually gain sponsorship from respected institutions like the National Institute on Aging and National Geographic
“Everybody else was looking for the secret to longevity in a test tube or a petri dish or in some genetic code,” Buettner says. “And I said, ‘Why don’t we just go to the places where people have achieved the outcomes we want and find out what they do?’ Nobody had ever done it.”
National Geographic funded a year of research, which would go toward compiling the magazine’s cover
story, “The Secrets of Long Life,” for its 2005 fall issue. Needless to say, exposing the recipe for longevity was popular among readers.
“Who doesn’t want to live longer?” Buettner asks, playfully. “One day you wake up and you see there’s a wrinkle or a gray hair or you notice a muscle that kind of hurts. And you start thinking about your life as a whole—that you want to walk your daughter down the aisle, or you want to see who your grandchild would be. I’ve never met a ninety-nine-year-old who didn’t want to live another year.
“I think it’s important to have a quality life, too,” he adds. “It’s not just about being around. It’s about being around something bigger than you.” That detail is at the heart of Buettner’s Blue Zones Project, an organization that enables communities in the US to provide the education and resources necessary for their residents to live better lives. It’s been Buettner’s most revered venture to date.
But let’s back up a moment. What exactly are Blue Zones? And how did Buettner find them?

After Buettner was given the means to conduct his research, he hit the books, looking for areas around the world where centenarian studies were already being conducted. In other words, he sought destinations where scientists had done demographic work to identify naturally high life expectancies. He found the first three areas—Sardinia, Italy; Okinawa, Japan; and Loma Linda, California—through existing academic literature by the WHO and similar scholarly resources. The last two—Nicoya, Costa Rica, and Ikaria, Greece— took a bit more digging.
“I hired demographers to pass through census data worldwide to find places where people were statistically living longer,” Buettner explains. “Our team would actually make a trip there and check birth certificates, then we would follow those birth certificates to see where those people were today—it’s a mathematical exercise. Then, I identified these places and named them.”




“The organizing principle is we’re not going to try very hard to change people’s minds. We’re going to change their environment so we can set them up for success.”
The name? Blue Zones—a title inspired by the blueink circles Buettner and colleagues would draw around key areas on maps.

Once each zone was identified, Buettner and his team flew out for weeks at a time to get a sense of the people, their culture, their communities, and their lifestyles. They not only found that these cities are full of older people but also that those older people are living with incredible vigor and are celebrated.
“You get a similar feeling in all of these places,” Buettner says. “It’s very clear that these people have a nice life and they are not a bunch of technology millionaires trying to find the next genetic intervention or the next nutraceutical that’ll help them live longer. These are people who are naturally living a high-quality life—socially connected, imbued with purpose, moving all the time.”
Buettner discovered nine common denominators— dubbed the Power 9—that allowed people in each of these places the ability to live life to the fullest (and the longest). For starters, people in these communities are “nudged into unconscious movement” at least twenty minutes a day. That movement can take many shapes, whether you’re a farmer in Sardinia, moving to keep your sheep in line, or you’re dining on a floor pillow in Okinawa, which naturally encourages you to engage your core muscles and use your legs to get up and sit down.
Residents have a strong sense of purpose and a vocabulary of purpose, but they also have daily rituals that slow them down, such as praying, taking naps, or participating in ancestral veneration (paying respects through meditation or a common ritual). They eat an
overwhelmingly plant-based diet that’s very high in carbohydrates, whole grains, tubers, nuts, and beans. They never overindulge on foods: they drink alcohol in moderation and design their kitchens so that they are not grazing all day but rather have specific mealtimes.
Those living within Blue Zones also put their families before their careers and have hobbies or religions in which they are actively involved. And above all, they have an immediate social circle of people who reinforce these behaviors. So, the healthy habits these people take on aren’t one-offs; they appear in clusters.

“They’re not just one disciplined individual imbued with responsibility,” Buettner says. “It’s very clear that these groups support each other, engage in the community, and have a mutually supportive network of people. We miss that in America.”
Companionship is not the only thing Americans are missing. The convenience of transportation and the sprawling landscape of America doesn’t lend itself to walkable communities in many circumstances. Easy snack and meal options are oftentimes processed foods, high in fats and simple carbohydrates. And, spiritually, many Americans constantly seek validation and a sense of purpose in their jobs, relationships, and hobbies, only to find themselves unfulfilled in one area or another.
All of this is not to say that changing the overall way of American life is impossible. In fact, that possibility was Buettner’s next goal: take the nine commonalities of the Blue Zones and inject them into communities across the US. That way, people across the country could learn them, practice them, and build future generations using them. That’s an idea people can get behind.
Corry, Pennsylvania—a small city outside Erie—was approved to be part of the Blue Zones Project in 2019. Get an inside look at what it takes to transform a city to have an edge toward wellness and endurance.
 By KC Esper
By KC Esper

Erie County Executive Kathy Dahlkemper championed the start of the project, then gained support from key stakeholders from three funding partners: UPMC Hamot, Highmark Health, and Corry Memorial Hospital, a LECOM Health affiliate. Sharecare—a company focused on combatting the fragmentation between doctors, health plans, employers, and education—stepped up to manage the entire project from start to finish.
Using the Power 9 (p.47) as guiding principles, project leaders educate people about well-being and how to achieve it. Corry community members can attend workshops to meet people, learn about healthy habits, and find purpose through their passions. Leaders will also organize events like cooking classes, potlucks, and walking moais, an Okinawan word that refers to a social support group.
After obtaining funding, Corry’s project leaders started their discovery phase. Here, they networked with community members to gain the support of schools, restaurants, grocery stores, and gathering spaces like churches. The purpose of this phase is to bring awareness to the project, create a framework to put policy in place, and map the best course toward goals that need to be met to not only become a Blue Zone but to stay one.




This step incorporates Blue Zone principles into public spaces through policy and long-term partnerships. Blue Zone-specific signage is placed throughout grocery stores in Corry to nudge consumers toward healthier choices. Leaders also work with store managers to place healthy snacks at impulse-buy areas, organize aisles to contain only organic/non-GMO products, and host demos on how to make nutritious meals. Outside of stores, leaders collaborate closely with organizations like the Salvation Army and food pantries to provide low-income families with wellness options. The local government assists with big-picture changes, like smoking policies and efforts to make the city more walker/biker friendly.

With these programs and policies in place, the team steps back to let the Corry community put them to use, keeping a close eye on how the population’s habits change as a result. Statistics showcasing the population’s obesity levels, percentage of smokers, poverty rate, drug users, stress levels, and healthcare costs are compared with baseline data over time to see how well the project’s efforts are succeeding. If the data shows an increase in wellbeing and life expectancy, Corry becomes a certified Blue Zone.

The Corry Blue Zone team, managers, and sponsors hope that this project can serve as a blueprint for other cities nearby. The smaller, more contained nature of Corry makes it the perfect pilot community to determine which methods work best and can be replicated. The success the team has in Corry will enable it to potentially make a difference statewide.
Shannon Wohlford Engagement Lead for People Corry Blue Zones Project Jennifer Eberlein Organization Lead for Places and Community Program Manager Corry Blue Zones Project Ashley Lawson Policy Lead Corry Blue Zones Project
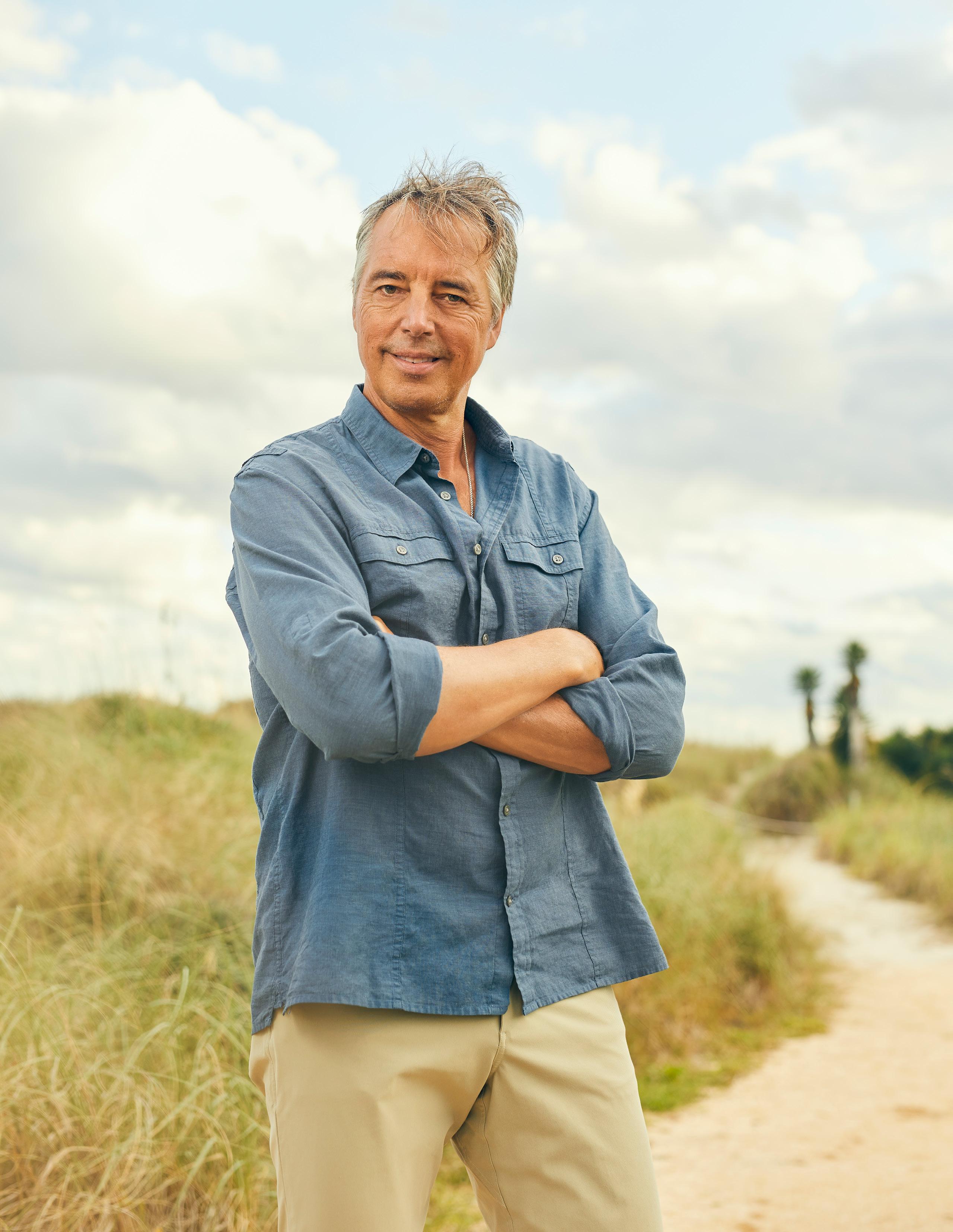
So far, more than four hundred cities have applied to become a Blue Zone. Each application is vetted to ensure that the city’s top players in government, healthcare, and education are on board to participate. Of course, not all of them can be changed at once. The two guiding factors that determine which cities are picked, Buettner explains, are, one, the entirety of the public sector being on board with the project and, two, that the public sector can pay for the necessary changes so that citizens aren’t saddled with higher taxes. Only then will Buettner’s team get to work.
“The organizing principle is we’re not going to try very hard to change people’s minds. We’re going to change their environment so we can set them up for success,” Buettner says. “The most effective and cost-effective way to change health behavior at the population level is through policy.”

Once a city is chosen to be “Blue-Zoned,” Buettner’s team of experts reviews policies to identify the best opportunities for change.
“They find the few policies that favor healthy food over junk food, limit junk food marketing, favor the pedestrian over the motorist, favor the nonsmoker over the smoker, and, for alcohol policies, make for maximum enjoyment with minimum damage,” Buettner explains. “Then our team comes in and spends weeks or months assessing the policies in place, assembles a customized menu of options for that city, and works with the city to pick out which of the policies are most effective and feasible in a five-year time horizon.”
The second step is administering the Blue Zone certification program for restaurants, grocery stores,
workplaces, schools, and churches. The team works to improve policies or layouts so that the public can use each place in a healthier way—encouraging people to use the stairs or to opt for plant-based foods, for example. Lastly, the Blue Zones team holds free purpose workshops and curated volunteer opportunities to connect like-minded people.

Over the span of the five years working with the community, the team receives an annual report card of its data and compares it to the baseline data it gathered to assess progress. “In almost every city, our work helps drops the average BMI [body mass index] of the population, the physical activity level goes up, the smoking level goes down, and citizens report greater levels of optimism,” Buettner notes.
“Politicians talk about creating healthier, better places to live in—the Blue Zones Project actually does it by making permanent change to the environment,” he continues. “And we hold ourselves accountable by these measurements.”
Buettner mentions that while many communities just aren’t naturally set up for this kind of success, there is one main player that can help change an environment from the get-go: the healthcare system.
“We created a company that keeps people healthy in the first place, which is antithetical to a healthcare system because their stock prices and profits are very much dependent on people getting sick,” Buettner explains. “But there are executives who want to make ethics as important as profit.”
One of those executives is Scott Reiner, CEO of Adventist Health, a nonprofit health system based

“Environmental change is slow. But to architect people’s choices to be better, you set up the whole population for long-term success by making permanent changes to the environment.”
in Roseville, California, with twenty-three additional hospitals in California, Oregon, and Hawaii. Adventist Health is sponsored by the Seventh Day Adventist Church, which also has a large following in Loma Linda, California—one of the first Blue Zones discovered.
Rooted by the same principles practiced in Loma Linda, Adventist Health was founded on the idea of helping a whole person: physically, mentally, spiritually, and socially. While the system has integrated its work into its processes and operations since day one, Reiner wants it to have a greater impact on the communities it serves outside of the hospital.
“Eighty percent of our patients come from either Medicare or Medicaid, so we serve older and poorer communities,” Reiner explains. “We look at how we can improve our hospital care, but we don’t think that’s all that we can do or should do. We think that the community needs an organization that cares deeply about their health, not just their healthcare.”
Reiner and his team created a 2030 strategy oriented around the mission to improve community wellbeing by actually improving the community. They looked “through the lens of the consumer” to think about how all aspects of the hospital system could improve to take more responsibility for their patients’ health—understanding who they are, where they came from, and what health disparities they might be facing.
“When we started looking into community well-being and individual well-being, we had to reach outside the idea of traditional hospital care,” Reiner says. “That’s where Blue Zones comes in.”
Reiner’s and Buettner’s values aligned perfectly and it was clear that both of their entities could work better
What the citizens of the Blue Zones have in common
1. Move naturally
2. Have a sense of purpose
3. Take time to downshift
4. Eat only until they’re 80 percent full
5. Have a plant-based diet
6. Drink alcohol in moderation, usually at dinner
7. Have a group of supportive peers and family members
8. Put their loved ones before their careers
9. Feel a sense of belonging in their communities
Source: bluezones.com
together. So, in April 2020, Adventist Health made a deal to acquire Blue Zones to make its 2030 goal a reality. With the partnership, the health system can extend its reach to work with, for example, policy makers and school systems, as well as engineers who build better streets and pathways and nonprofit groups that create affordable housing. Most importantly, the access points to these resources aren’t going to be in emergency rooms, Reiner confirms. They’re going to be stationed in centers and virtual platforms across these communities so that the public can proactively live healthier lives.
Luckily, the support from Californians so far has been incredible. “California has a natural inclination for people to think about wellness,” Reiner notes. “It’s a great platform for a more progressive model and idea about the evolving health system.”
Reiner says another main goal at the center of Adventist Health’s mission is to keep the cost of care down. “We have to make sure we care for the underserved populations and patients who have poor access to care,” he says. “Let’s face it, not all of them are thinking about Blue Zones if they can’t provide three meals a day for their kids. So, we’re working with Blue Zones leadership and our own internal team to make sure we can care for every individual in the community using this methodology. We want to help them work towards improving their health in ways that are reasonable and not overbearing or overwhelming.”
The hope, Reiner says, is to create a model for other health systems to enter into their community spaces to modernize care in the country. While Reiner and his team are still in the early stages of completing this goal, he hopes that the blueprint they develop will be capable of replication in any state, in any population, with any health system.
“Environmental change is slow,” Buettner says. “But to architect people’s choices to be better, you set up the

whole population for long-term success by making permanent changes to the environment.”
Now that Reiner and Adventist Health have taken over most of the Blue Zone Project’s operations, Buettner has moved from his executive position to one as founder. In many ways, this is another passing of the torch: just as the original Blue Zones inspired Buettner to carry forth their lessons into the community, Buettner inspired Reiner to carry forth the mission in ways never before considered.
“I was the innovator to start this, but Scott is the next chapter’s innovator,” Buettner says. “He has to take this thing and vector it into the American healthcare system—and that is a bigger job than what I created.”
That’s not to say Buettner’s chapter has ended. Projects up his sleeve include writing a book about plant-based food traditions, as well as planning his next transcontinental bicycle ride. Everything Buettner has done, from his years of research to his mission to transform communities, has not only provided him with his own sense of purpose but also equipped others with the tools they need to find their own missions.
“Any expedition I do in the future is going to enrich people’s lives, not just my own,” Buettner affirms.
With that goal resonates a mantra that Buettner has now dedicated himself to for decades. After completing world record-breaking, seemingly outlandish goal after goal, Buettner has come a long way from the woods of Minnesota. But he’s found a way to carry the lessons his father taught him as a boy—to connect with the earth and grab the reins of any great adventure—and inject them into his goal to help others live better lives.
With the road still ahead of him and so much more to accomplish, the possibilities of where Buettner can go next are endless. At this pace, one destination is certain—his one-hundredth birthday. AHL
Every step executives take on their career journeys is pivotal to achieving their current successes. Along the way, individuals accumulate technical skills, foster relationships, and develop the leadership acumen that have turned them into pioneers of the industry.
50. Lauren Misztal Mallinckrodt Pharmaceuticals 56. Darleen Souza Albany Medical Centers 59. Dr. Tashica Williams Amirgholizadeh Gilead SciencesLauren Misztal’s diverse experience and ability to take on new challenges guarantees efficient, cost-effective work for Mallinckrodt
By Lucy Cavanagh Lauren Misztal
Associate General Counsel for Litigation & Investigations and Data Privacy Officer
Mallinckrodt Pharmaceuticals
Lauren Misztal
Associate General Counsel for Litigation & Investigations and Data Privacy Officer
Mallinckrodt Pharmaceuticals
f all the skills that she has accumulated over her varied career, efficiency is what Lauren Misztal would highlight as the strength that makes her an asset to Mallinckrodt Pharmaceuticals. Misztal has worked in many different capacities, from the Department of Justice to private practice at Quinn Emanuel. She has built a wellrounded career that gives her a unique perspective and an edge in her current dual role as associate general counsel for litigation and investigations as well as data privacy officer.
When Misztal completed her undergrad at Georgetown University, she went to work in the compliance department at Goldman Sachs in New York, which gave her a taste of both the business world and the legal world. But she quickly discovered that her work with legal matters suited her personality better.
“I thought that it was a better fit for me than business school,” Misztal explains. “I was more drawn to law school given the fact that the subject matter is focused more on reading, writing, analysis, research, oral advocacy, and persuasiveness.”
Partially motivated by its proximity to the epicenter of federal law, Misztal decided to return to her alma mater for law school. “I wanted to be in DC because I knew going into law school that I wanted to be a litigator, not a corporate attorney,” Misztal shares. “I also knew that DC is the home of the federal government with a lot of different options for experience.”
An internship at the Department of Justice cemented her interest in litigation, and after graduation she took on an Article I clerkship on the United States Court of Federal Claims, which later led her to a long-term position at DOJ in the section of the civil division that litigates monetary claims against the federal government.
Of her time at DOJ, most of all, Misztal values the up-close experiences that she gained inside the courtroom during trials. “I did two trials when I was there, one of which I got to sit first chair,” Misztal explains. “When you’re a young lawyer, there’s no experience quite like that.”
After three years at the Department of Justice, Misztal interviewed at Quinn
“A good compliance program is all about making sure that we have spotted the gaps .”
Emanuel in DC and was hired on the spot as one of their first civil litigators at the same time that their DC office was about to undergo exponential growth.
Misztal’s work at Quinn Emanuel covered a wide range of matters such as mortgage-backed securities litigation, criminal investigations, civil internal investigations, and false claims act cases. She even had a few healthcare clients, which would foreshadow her next move.
“I ultimately decided that the best path for me would be to try to move in-house,” Misztal notes. In terms of her career trajectory, Misztal essentially hit the trifecta of legal experience through government work, private practice, and now as an in-house lawyer for Mallinckrodt Pharmaceuticals.
Mallinckrodt is a patient-centric specialty pharmaceutical company that develops and manufactures treatments for rare diseases and health conditions that are largely overlooked. Misztal joined the company in late 2019 while it was facing several significant legal issues, including a potential restructuring.
“I was really hungry for that,” Misztal says. “I wanted to come to an organization that had a lot of interesting legal circumstances and compliance challenges so that I could hopefully help the company navigate those things. I think that’s really where you’re learning the most—in an organization that is facing unique legal challenges. That’s where an attorney can grow.”
Shortly after joining the company, Misztal also took on the role of data
privacy officer, which gave her a new challenge of defining forward-looking compliance strategies instead of the backward-facing litigation that she was used to.
“A good compliance program is all about making sure that we have spotted the gaps,” Misztal says. “We’re making certain that people within the organization understand our regulatory obligations from a privacy perspective and that we have solid processes so that there are no issues in the future that will get us into legal or regulatory trouble.”
“I wanted to come to an organization that had a lot of interesting legal circumstances and compliance challenges so that I could hopefully help the company navigate those things.”
Given Misztal’s diverse experience, she was exceptionally poised to move in-house as she carried a prized quality for any company: efficiency. Contrary to many conceptions about the Department of Justice, federal lawyers do not have unlimited resources or budgets to accomplish their goals, so Misztal learned early on how to bill economically.
The same was true during her time at Quinn Emanuel, a firm that’s known for aggressive strategies that maximize client resources and that never lets a penny go to waste. “Since I have such a strong litigation and investigations background, I’m able to hire really good outside counsel, but I’m also able to collaborate with them and make suggestions to them,” Misztal explains. “I’d like to think I’m able to cut out some of the inefficiencies that can sometimes creep in.”





Misztal believes that her theme of effective and efficient work can also be attributed to another full-time role she assumes—a mother. She points out that, perhaps what the mainstream conversation doesn’t fully appreciate about the parenthood/work balance is how the two vocations are mutually beneficial.
“I don’t want people to think I can’t do things because I have kids. In fact, I want them to understand I love coming to work because I have kids,” she says. “I’m a much more dynamic and involved mom because of this outlet, my career. On the other hand, moms are usually better workers because we just need to be more efficient. I don’t waste time because of how valuable it is.” AHL

In the midst of a vaccination effort, Albany Medical Centers makes sure to reach underserved populations and protect overworked frontline workers
By Donald FrickeAs the primary medical hub for the Capitol Region of New York State, Albany Medical Center has been tasked with vaccinating one million people against COVID-19. When Governor Andrew Cuomo’s office divided the state into ten vaccination hubs, the healthcare system was tasked with overseeing eight counties in an effort to help the New York population reach the 70 percent threshold required for herd immunity.
“The hub has a few roles,” Dr. Dennis McKenna, president and CEO of Albany Medical Center, told New York’s Channel 6 News. “First and foremost, the creation and implementation of the regional vaccine administration plan. As well as the formation of a regional advisory task force [sic].”
That regional advisory task force is composed of sixty members, including county health department commissioners, healthcare entities, first responders, community organizations, and more.
Albany Medical Center is fighting a battle on several fronts. Even though they are tasked with the mass vaccinations, New York State is only able to distribute
its limited vaccines as it receives them from the federal government. Vaccination wait times were scheduled up to fourteen weeks out at the time of writing, when the state had entered its Phase 1B of the vaccination rollout. That phase includes firefighters, police, food and agricultural workers, postal workers, manufacturing workers, grocery store workers, educational workers, and people ages seventy-five and older.
A second task force has been created to oversee vaccination administration for people of color and other underserved minorities. The history of vaccines and their development means something very different to those communities, who were often experimented on or given experimental drugs as late as the twentieth century. The Tuskegee Experiment, forced sterilization, and a litany of other heartbreaking historical crimes against minorities are a far too recent reality for many.
Black residents of Albany County are more likely to be hospitalized for COVID-19 than their white counterparts and, earlier in the pandemic, they
At Littler, we are lawyers. We are also innovators and strategists, passionate problem solvers and creative disruptors. And we are committed to helping our clients navigate the complex world of labor and employment law by building better solutions for their toughest challenges.
Congratulations to Darleen Souza for her recognition in American Healthcare Leader!
We proudly support Darleen and her incredible work at Albany Medical Center. One
were shown to be dying at higher rates. That’s why Albany Health Centers has entrusted people from those communities, like Albany County Legislator Carolyn McLaughlin, to help build trust in the vaccination process.
“Think about if [the vaccine] wasn’t available to you,” McLaughlin told the Times Union . “I tell people, ‘Don’t self-select out of the opportunity to get the vaccine without the proper and adequate information.’ That’s why people like me, we’re trying to make ourselves available as an influencer in the community, a voice that people are going to listen to.”
At a time when the health organization is waging an all-out war against a pandemic, senior vice president and chief human resources officer Darleen Souza is making sure that the relentless efforts from Albany’s healthcare professionals and frontline workers aren’t going unrecognized. Souza spoke about recognizing employee efforts at length with Fond.
“Reinforcement is critical to our general well-being, whether it’s intrinsic or extrinsic,” the SVP said. “We have been
praised and recognized since infancy. It’s inherent. The need to know you are valued heightens at work. Age doesn’t matter, but understanding your role, fairness, and accolades does. The more personal your recognition, the better.”
Souza says it’s her goal to reward employees in as many ways as possible, but it’s a journey that she is continually working through. The team’s longterm goal is to create a system-wide incentive program that benefits everyone—in tandem with a personalized development plan.
“People don’t want to be recognized with a sundae party when their office printer is down,” Souza said. “Invest in making your employees’ day-to-day lives easier through addressing environmental issues, providing work-from-home opportunities, and cutting down on meetings. It is recognizing that there are obstacles to remove both personally and professionally in our lives.” AHL
Editor’s Note: At time of publishing, Darleen Souza was no longer with Albany Medical Centers.
Dr. Tashica Williams Amirgholizadeh keeps her love of science and learning at the heart of her profession at Gilead Sciences
By Lucy Cavanagh“D on’t limit yourself,” Dr. Tashica Williams Amirgholizadeh advises young people who are at the beginning of their careers—particularly in the sciences. “If you go down a straight-line path, you might come to a dead end, but it’s never too late to pivot and find something that feeds your passions.”
Amirgholizadeh certainly took heed of her own advice with an educational
path that started in chemistry at Baylor University and culminated at the University of California, Berkeley, where she attended law school.
At a young age, Amirgholizadeh discovered her deep fascination with science. Her parents and teachers nurtured her natural curiosity and scientific aptitude throughout her childhood. Growing up in a military family—and accustomed to
moving around more than the average child—Amirgholizadeh tapped into the natural world around her everywhere she went. Her family lived in a variety of places, including Texas, California, Hawaii, and even Germany, where she received the most encouragement to pursue science.
She followed that inherent love of learning to complete her undergraduate education at Baylor University, a southern Baptist university in Waco, Texas, that supported her faith as well as her scientific pursuits. Amirgholizadeh majored in chemistry and minored in mathematics, eventually matriculating into the chemistry graduate program at the California Institute of Technology, where she earned a PhD.
She praises both institutions for their dedication to creating safe environments where she felt free to ask questions and feed her curiosity. “[Attending these schools] kept with a theme for me,” Amirgholizadeh says, “which was to be part of small, intimate, and warm settings, but powerhouses when it came to science.” Her classmates became a family on whom she could depend, and she remains close to many classmates she has met during her journey.
By nearly the end of her graduate studies, Amirgholizadeh was faced with a dilemma: though her passion for science hadn’t waned, she could not see herself in a laboratory for the rest of her life.
“It [had become] tedious,” she explains. “That realization was dangerous because I knew my heart wasn’t in it.”
Dr. Tashica Williams Amirgholizadeh, PhD Associate General Counsel, Intellectual Property Gilead Sciences Inc.
The decision to abandon the track that she had been on her whole life was a daunting one, but Amirgholizadeh followed her gut and made the choice to pursue patent law, even though she knew it would mean more schooling. She was encouraged by friends and classmates, who also had pursued legal paths, to consider patent law. They noticed that, in addition to the scientific expertise that would make her an asset in patent law, she had other skills, such as creative thinking and attention to detail, that are essential for any good attorney.
After Amirgholizadeh was admitted to law school at the University of California, Berkeley, she explored other parts of her personality that made patent law such an ideal fit for her. “Patent law was a natural blend of the skills that I knew I had and others that I discovered,” she shares. “It put me on the right course that I am on today, and I have never looked back.”
After law school, Amirgholizadeh spent nearly six years as an associate with Sidley Austin LLP in Los Angeles. Her practice at the firm primarily
“If you go down a straight-line path, you might come to a dead end, but it’s never too late to pivot and find something that feeds your passions .”
focused on patent infringement litigation involving a wide variety of technologies, including biotechnology, medical devices, computer processor architecture, and plasma
what the playing field was [at the relevant time],” she explains. “What was out there historically and when was something truly invented.”
Amirgholizadeh believes that her experience at Sidley was important for the role she holds today because her insight allows her and her team to move nimbly in their hypercompetitive field. During those years at Sidley, she learned what it takes to invalidate a patent and saw how patents were attacked, which gave her the current insight to see problems upstream and know how to get ahead of them. “I have learned how to stress-test a portfolio,” she shares. “I have the freedom to investigate and I know how to make a quick risk assessment if issues do arise.”
display panels. Sidley afforded her the opportunity to train alongside talented patent litigators. She learned how to be a patent litigation detective to defend and challenge patents. “You had to figure out
Currently, Amirgholizadeh is associate general counsel in the intellectual property (IP) department at Gilead Sciences Inc., a leader in biopharmaceutical research based in Foster City, California. She is a valued member of the IP leadership team and manages a group she helped create that counsels on acquisitions, licensing, and other due diligence matters. With the help of her team and her litigation experience, Amirgholizadeh has advised Gilead on several multibillion-dollar acquisitions. With patent law, Amirgholizadeh struck an ideal balance between her curiosity and her love of science, and at Gilead, she gets to keep her finger on the pulse of cutting-edge research that makes her excited to go to work every day. “I still get really excited to read papers and journal articles about new discoveries,”
“I feel fortunate that I get to work at a place like Gilead. We create medicines that help patients and have the testimonials to prove that they’re helping them.”
she enthuses. “I get to learn continuously and indulge in my passion for science.”
At a company like Gilead, Amirgholizadeh enjoys working with exceptional scientists and other cross-functional colleagues with whom she can converse and learn, all while contributing to meaningful endeavors in the healthcare industry. “I feel fortunate that I get to work at a place like Gilead,” she remarks. “We create medicines that help patients and have the testimonials to prove that they’re helping them.”
Amirgholizadeh hopes to promote the pursuit of patent law among women, particularly women of color, who remain underrepresented in the sector. She emphasizes that it is never too late to change direction and that there is no single path to satisfying a passion in science.
“I hope that people see that they aren’t stuck in the path they choose at eighteen or nineteen years old—they don’t have to stay there,” she says. “If someone finds themselves in the same position I did, I hope that they would explore patent law and give it a chance. Then maybe they can continue to inspire the younger generations to do the same.” AHL
Gilead’s
We

Mayer Brown congratulates our friend Tashica Williams Amirgholizadeh on this welldeserved recognition of her accomplishments on behalf of Gilead Sciences.
We are honored to work with her and Gilead Sciences.
commitment to achieving the impossible is supported by talented professionals like Tashica. Venable has had the good fortune to work with her on many intellectual property matters, and we have tremendous respect for the technical skill and creativity she brings to solving complex legal issues.
 Andy Cohen VP and Head Counsel of R&D Legal Takeda Pharmaceuticals
Andy Cohen VP and Head Counsel of R&D Legal Takeda Pharmaceuticals
I t wasn’t until a recruiter called Andy Cohen that he realized he didn’t need to be embarrassed about putting his former job on his résumé. The recruiter knew Cohen from his first life and wanted to make sure he was talking to the same Andy Cohen—now vice president and head counsel of R&D Legal for Takeda Pharmaceuticals—whose career experience seemed to have one significant gap.
If you don’t know the name Andy Cohen, go ask your bespectacled friend with a wall of vinyl records and an encyclopedic recall of the Touch and Go Records roster—the same friend who keeps trying to get you to listen to bands whose names sound either oddly charming or vaguely threatening. They know Andy Cohen because he is one-third of the band Silkworm, a critically adored indie rock band from the epoch of ’90s indie rock. From 1987 to 2005, Cohen essentially lived in a tour van, playing shows all over the world, releasing records for high-prestige indie labels, and grinding out a music “career” (he jokingly asked that career be put in quotation marks).
The band’s trajectory has been memorialized in the documentary Couldn’t You Wait?, which features interviews with
Wilco’s Jeff Tweedy, Pavement’s Stephen Malkmus, and recording legend Steve Albini. Those names mean the world to a small sect of the music-listening population—and they’re names a few rungs higher in notability than was garnered by Silkworm over the course of their eclectic and brilliant run. At some juncture, the band members realized they would be happier making music if they weren’t relying on it to pay their bills. And Cohen, who had originally dropped out of college in order to pursue a life in music, decided to get serious about law school.
While Cohen continues to make music to this day, it took some time for him to feel comfortable about putting his past life on his résumé. “I didn’t want to look like some sort of nontraditional guy who seems like a flake because he just wasted these years of his life on music,” Cohen says.
The recruiter who had contacted Cohen thought just the opposite, and the lawyer slowly began to see his past life differently. “If you engage with your subject matter wholeheartedly, those interesting things in your background can supplement that,” Cohen says.
At Takeda Pharmaceuticals, Cohen would have no choice but to engage fully, as the company’s acquisition of Jersey-registered Shire Pharmaceuticals
“We are lawyers who are collaborative, pragmatic, and solution-oriented . Those all may sound like buzzwords, but if you really focus on those, it’s a much different message than working to be the most riskaverse team ever . . .”
created both a top-ten global pharmaceutical company and an integration effort that would require all hands on deck to see through to completion. When the deal first began, Cohen wasn’t yet in his present position, and as a Takeda deal lawyer he was assigned work streams that were ancillary to the core transaction deal.
“We took on a great deal of debt to complete this deal, so I did a lot of work to support the financing,” Cohen explains. “I also worked on various antitrust and other regulatory issues, really a grab bag of everything that wasn’t the core ‘scheme of arrangement’ in the argot of Jersey M&A.”
By the time Cohen assumed his head counsel position in October 2019, integration had already been initiated prepping the combination of the two massive companies. “When I first came to this role, we had a bit of disarray of teams that were spread all over,” the VP says. “From my perception, there were two big issues to address. One was everyone had just been through the same integration and that can be hard on morale. The second is that Takeda and Shire had somewhat different processes in everything from computer systems to work intake and tracking and even to the question of ‘What does it mean to be a lawyer here?’ that needed to be, and continue to be, addressed.”
“The benefits of this work are beyond what I’ve seen in fifteen years in this industry. It’s showing the possibility of what could happen if everybody puts their heads together.”
Cohen’s first goal—arguably one inspired by maintaining cohesion among bandmates in a van for all of those years—was to get everyone on the same page. “The biggest thing I’ve tried to do is to promulgate a unified culture,” Cohen says. “We are lawyers who are collaborative, pragmatic, and solution-oriented. Those all may sound like buzzwords, but if you really focus on those, it’s a much different message than working to be the most risk-averse team ever or that we’re going to fight every battle on every deal and make it really hard to make things happen. You can’t do as much as this company has been able to do with that kind of mentality.”
Baker McKenzie is proud to have worked with Cohen and his colleagues on many of Takeda’s most important collaborations, licensing deals, and other life sciences transactions. “Andy has an amazing ability to zero-in on the issues in a deal that are of greatest impact to Takeda and of greatest importance to his internal business colleagues,” says Randy Sunberg, chair for North America healthcare and life sciences at Baker McKenzie. “Andy always brings innovative and effective approaches to problem-solving in all aspects of negotiations and deal structuring.”
Cohen’s focus on collaboration came at an important time for the company. The unprecedented COVID-19 pandemic
has required collaboration and cooperation between entities usually battling it out for market dominance. A brief news rundown highlights Takeda’s partnering with Amazon Web Services and Accenture to move 80 percent of its applications to the public cloud over the next five years in an effort to boost its R&D pipeline for drug discovery.
Takeda also partnered with the Japanese government to distribute Moderna’s COVID-19 vaccine in Japan. “The benefits of this work are beyond what I’ve seen in fifteen years in this industry,” Cohen says. “It’s showing the possibility of what could happen if everybody puts their heads together.”
The relaxing of regulatory hurdles, antitrust and FDA interactions, due to the pressing nature of COVID-related work may help usher in further collaboration between competing entities.
While the pandemic has sent the bulk of Takeda employees home, Cohen admits he is antsy to get back into the office, when appropriate. “We’ve managed well through this, and I know a lot of work will be different going forward, but one of the things I love about Takeda is its focus on face-to-face interaction,” Cohen says. “I miss that a lot.”
While Cohen may have made his way in an entirely different field than music, some things never change—the man thrives off a crowd. AHL
As one of the first law firms to advise pharmaceutical companies on their global expansion 60 years ago, our healthcare and life sciences lawyers understand the challenges industry players face and what it takes to overcome them.
As trusted advisors to the world’s largest pharmaceutical, biotech, medical device and healthcare services companies, our team of more than 800 lawyers work with clients in complex and pivotal commercialization strategies, licensing and collaboration deals, complex and creative monetization and royalty structures, regulatory, M&A and other areas globally to assist them in pursuing their strategic objectives.
www.bakermckenzie.com
A true leader. We are honored to work with Andy Cohen and Takeda on many of their important transactions and value this relationship with Andy and his team.
National, and even global, forces have an unmistakable impact on an executive’s work. Whether it’s a legislative change or an industry-disrupting technological breakthrough, executives must constantly adapt their business strategies to keep their company thriving.
72. Colin McDonald Cross Country Healthcare 75. Nicholas J. Messuri DentaQuestColin McDonald leans on decades of HR experience and leadership to bring Cross Country Healthcare upgraded systems and greater diversity
By Clint WorthingtonBefore Colin McDonald was senior vice president of human resources at Florida-based Cross Country Healthcare, he worked as a recruiter for New YorkPresbyterian Hospital, one of the largest healthcare organizations in the world. One day, his supervisor offered him a promotion, replacing a white colleague who’d vacated the role, but without the same pay.
When he asked why he was going to be paid differently, his supervisor offered some much-needed perspective: “If you don’t take this job, you’ll just stay a Black recruiter. But if you do take the job, you’ll be a Black manager, one of only a few Black leaders in HR in New York City.” It was a powerful moment, not just for his career development but his work as a Black executive in healthcare. Now,
at Cross Country, McDonald leverages that experience and the leadership skills he’s cultivated over decades of HR work to keep the organization’s people power streamlined and advocate for greater diversity and inclusion.
The Jamaican-born McDonald emigrated to the United States in the ’70s. Early on, his mother hammered home the importance of a good education. “Everything [I’ve accomplished] is owed to her,” he says, proudly. He received his bachelor’s at the State University of New York at New Paltz, joining the historically Black fraternity Kappa Alpha Psi (a credit shared by US Vice President Kamala Harris). After that came a master’s in organizational leadership at Mercy College and a robust career in human resources, starting at New YorkPresbyterian and continuing to Cross Country, where he joined in 2014.
When he first arrived at Cross Country as an HR director, McDonald immediately recognized that the talent acquisition and human resources teams needed to be revamped from the ground up. “We were outsourcing a lot of our services, specifically from the recruiting function,” he explains. To address that problem, McDonald set about developing an in-house recruiting team, building every policy and system from scratch.
That’s not all: in addition to his everyday duties, which include touching upon virtually every aspect of Cross Country’s HR function across its several thousand employees, McDonald is hard at work employing technological solutions to help streamline systems. “In my first few years here, technology wasn’t at the forefront,” he says.
But that’s changed in the last two years with the arrival of new CEO Kevin Clark, whom McDonald describes as an “innovative, tech-savvy, positive” leader. Clark spearheaded a newfound investment in technology for the company. For HR, that
meant replacing the department’s archaic network of disparate record-keeping systems (one for employee records, one for recruiting, one for onboarding) with one comprehensive system.
After some research, McDonald and his team settled on Ceridian Dayforce, an upgraded HRIS platform that combines the recruiting and onboarding modules with succession planning, learning management, and performance management tools.
It’s a breath of fresh air from what they were doing before, McDonald notes. “We were creating metrics off Excel,” McDonald admits. But with Ceridian, employees can access payroll information, allow recruiters to onboard people more efficiently, and more.
That’s not the only way McDonald has used technology to streamline the HR function. Cross Country has recently implemented a benefits-focused
“You have to be that person who’s going to come in early, stay late, and take on those extra responsibilities. Because once the leaders know what you’re capable of achieving, then the color really doesn’t matter.”
platform that allows employees to access their info online through mobile apps and make changes to their benefits on-demand. “It’s a lot more seamless and intuitive,” he says.
Beyond technology, McDonald takes his status as a Black executive in healthcare seriously, investing deeply in diversity and inclusion initiatives to address systemic problems within the organization and healthcare in general. “A lot of this started coming to the forefront with the death of George Floyd,” he says. Organizations everywhere started to examine what they could do to address systemic inequality in their own houses—an effort long overdue. Fortunately, McDonald found himself in an organization far ahead of the curve.

“I have to tell you, this company has always believed in diversity, equality, and inclusion,” McDonald says. In particular, he credits Clark with immediately calling for organizational solidarity with Black Lives Matter and encouraging McDonald
to create an internal advocacy group, which would become “Cross Country Impact.” The group, centered on four major principles—educate, donate, advocate, and volunteer—gives Cross Country’s BIPOC employees a chance to talk openly about their status in the organization, issues with harassment, and more.
The results have been encouraging for McDonald. “Over 75 percent of our employees say this company excels as a diverse organization,” he notes. The organization now recognizes Juneteenth as an observable holiday and openly advocates for LGBTQ+ rights.
These matters carry a great deal of importance to McDonald, a Black executive who doesn’t often get to see others like him in high-profile positions. He sees plenty of Black executives who are good at what they do, but don’t get the opportunity to show it. The key, says McDonald, is finding a leader who is willing to take a chance on you.
“I was fortunate to have a CEO who knew my capabilities and allowed me to shine,” he observes. “It’s difficult to be a Black leader in any organization. You have to work a little bit harder than your white counterpart, you have to be as articulate, as present, as accountable.”
But despite these potential challenges, he urges aspiring Black executives to not let these obstacles be their downfall. “You have to be that person who’s going to come in early, stay late, and take on those extra responsibilities,” he says. “Because once the leaders know what you’re capable of achieving, then the color really doesn’t matter.” AHL
Independence changes everything. As a family-owned organization, Lockton is not driven by the quarterly pressure of financial markets. This independence frees us to always act in the best interest of our clients and creates an entirely different dynamic in the insurance industry—focused solely on clients’ success.
of Cross Country Healthcare
Colin McDonald SVP of HR Cross Country HealthcareNicholas J. Messuri has dedicated his career to nipping healthcare fraud in the bud. At DentaQuest, that mission helps ensure access to care for thirty million people. By
Billy YostThe sheer volume of names of national healthcare fraud committees Nicholas J. Messuri has chaired would occupy the bulk of the space in this article. The vice president and deputy general counsel for fraud prevention and recovery at DentaQuest has been called on by virtually every antifraud healthcare organization that exists, and his extensive pedigree in Medicare and Medicaid fraud investigation is in a league of its own.
Messuri was appointed to the board and then as board chair for the National Health Care Antifraud Association, head of the National False Claims Act Task Force, one of the first cochairs of the National Healthcare Fraud Prevention Partnership, and—back in his attorney general’s office days—was national president of the state attorney general’s Medicaid Fraud Control Units. That’s the beginning of the list.
The son of a blue-collar father who worked three jobs in order to ensure his kids would have a better life, he has spent the bulk of his career working to secure justice for those who need it most. He served first as a Middlesex County assistant district attorney, then in the Massachusetts attorney general’s office, and now on behalf of the over thirty million predominantly Medicaid/CHIP members whom DentaQuest represents.
His first twenty years were entirely in the public sphere, but Messuri would
eventually move into increasingly wider private roles, first at Tufts Health Plan in Massachusetts and, most recently, at DentaQuest, whose national presence has members in thirty states.
While Messuri has spent the better part of his career fighting bad actors, his
relationship to his work is not nearly as fire and brimstone as it may first appear. “People sometimes think of a prosecutor as someone who holds people accountable and sends them to jail,” Messuri says. “It was never like that for me. It was about helping the people that were on the receiving end of those that commit the bad acts, and making sure the ones who
“The vast majority of Medicaid benefits are going to children, and if they’re on Medicaid, there’s a good chance they need help.”

DentaQuest’s purpose is to not only ensure access to care for its millions of members, including roughly twenty-three million Medicaid/Medicare and seven million commercial members, but also to give them the tools to maintain optimal oral health. Its prevention-focused approach— Preventistry—does just that by promoting cost-effective, quality care through a network of more than eighty oral health centers in six states and nearly forty-thousand provider partners across all fifty states.
In addition to offering alternative financing and innovative care delivery options, DentaQuest has invested more than $230 million to help grow access to oral healthcare and create healthier communities.
committed those crimes get a fair shake and are treated fairly within the criminal justice system.”
That said, one doesn’t spend twenty years in the public sector fighting fraud without some skin in the game. “I’ve always wanted to be a champion for the underdog,” Messuri says. “I wanted to stand up for people with no voice. DentaQuest is in the business of protecting government taxpayer dollars
and making sure it is looking out for the people who are supposed to receive its services.”
DentaQuest’s mission is especially important to Messuri because its members require the loudest advocates available. “The vast majority of Medicaid benefits are going to children, and if they’re on Medicaid, there’s a good chance they need help,” the VP says. Messuri’s team of clinical investigators is
“I’ve always wanted to be a champion for the underdog. I wanted to stand up for people with no voice. DentaQuest is in the business of protecting government taxpayer dollars and making sure it is looking out for the people who are supposed to receive its services.”
trained to analyze data, look for outliers, and work to examine the root causes of what may be going wrong.
“Maybe our members weren’t billed correctly, maybe the services weren’t medically necessary, maybe the quality is subpar; we’re going to have our internal dentists and consultants look at those cases that need to be brought to the government’s attention,” Messuri explains.
Awareness and training are also a significant part of DentaQuest’s oversight. “We make sure our internal teams are training our providers’ staff, our customer service people, and our provider engagement professionals so if they’re in the field and they see something, it can be identified and brought back to my team for review,” the VP says.
Messuri says that DentaQuest’s investment in data analytics decades ago has continued to put their organization well ahead of the curve in identifying cases earlier in the process. “I believe we are a leader and one of the largest and successful Medicaid dental administrators in the country because we embraced the value of data analytics twenty years ago,” Messuri says. “Before the talk about big data or artificial intelligence, we were one of the first dental managed care plans
that was thinking about the value presented here by these technologies, and what it meant to providing quality health care at the lowest appropriate cost.”
That early investment hasn’t meant DentaQuest is resting on its laurels. “We’re on the cusp of hiring a company that is going to take our analytic efforts to a whole new level by using the best artificial intelligence out there to identify bad actors and bad outcomes even sooner,” Messuri says. “The company I work for has given me the tools that I need to do this job and has created this amazing culture of never being satisfied. It fits my personality and I’m fortunate to work for a company that embraces learning and growing and getting better.”
Messuri says the mission of DentaQuest is too important to take lightly. “There is so much written about the correlation between our gums, our teeth, and the health of our mouths, and how it’s all connected to other healthcare problems and the potential issues that can develop,” the VP explains. “We’ve got some of the best dentists in the world here working to make sure as many people as possible can obtain the dental benefit they need. We’re here to support them.” AHL
At Carter Arnett we offer the highest quality work product on par with the nation's largest law firms but with the specialized attention, fee flexibility and courtroom experience that only a boutique firm like ours can offer.

In the United States, recreational opioid use has increased in popularity over the past decade, causing cities to look critically at this trend. While there are many reasons people get hooked on these pain-relieving drugs, federal and state prosecutors say big drug manufacturers should pay for their alleged role in creating this national epidemic. Galia Porat, associate general counsel at Teva Pharmaceuticals, wants to reframe that narrative.
Porat knows that many view big pharma as a perpetual enemy, but she argues that Teva, the largest generic drug manufacturer in the world, didn’t perpetuate opioid abuse, as some believe. While trying to win hearts and change minds is a futile task, Porat is looking to back Teva as part of the solution—not the problem.
Porat started her legal career as an associate at Dechert, where she represented corporations and business executives in high-dollar civil and
criminal cases. During her time there, the firm represented Japanese manufacturer Takata in the largest automotive recall case in history.
Porat worked alongside renowned attorney Andrew Levander and learned all aspects related to defending companies against regulatory, international, and federal challenges. The Takata case and other experiences helped Porat realize she enjoyed taking a deep dive into the policies, practices, and strategies of a
 Galia Porat Associate General Counsel Teva Pharmaceuticals
Galia Porat Associate General Counsel Teva Pharmaceuticals
specific company. “I knew I wanted to install sprinklers instead of putting out fires,” she says. “It was the right move for me to go in-house at a public company.”
Teva has been a perfect fit. The parent company has headquarters and other facilities in Tel Aviv, while the US headquarters are in New Jersey. Porat speaks Hebrew and comes from an Israeli family. Although she hadn’t previously worked in pharma, her time at Dechert helped prepare her for her current role. “I know how government investigations work and I know how to defend a company,” she says. “A persistent lawyer with the right skills can learn any sector.”
Over the past decade, Teva has seen a “torrent” of lawsuits. Governments, plaintiffs, and plaintiffs’ lawyers are seeking large financial settlements, claiming Teva should provide compensation for failing to notice a spike in opioid prescriptions and then step in to slow drug manufacturing.
Teva, however, aims to address the wide-ranging litigation with a big-picture solution, using its manufacturing expertise and capacity. Treating opioid addicts with weaker medications to prevent devastating withdrawals is the gold standard for opioid abuse disorder and part of all medical addiction treatment programs.
Teva produces buprenorphine/naloxone (branded as Suboxone). Thus, the company has proposed a nationwide product-based resolution.
In 2019, Porat helped Teva craft and negotiate a creative arrangement that will settle thousands of lawsuits related
to the national opioid crisis. As outlined in the deal, Teva, without admitting fault for contributing to the epidemic, will donate $23 billion worth of Suboxone (at wholesale acquisition cost) and a cash sum over the next decade. The settlement’s framework, which allowed Teva to avoid a bellwether trial in Ohio, approached approval in mid-2020 but was delayed by the COVID-19 pandemic.
In the meantime, as the healthcare and pharmaceuticals industries move forward at a breakneck pace, Porat is looking for opportunities to reposition Teva. “People may view pharmaceutical companies as greedy or bad corporate actors, and it will take a lot to alter that strong perspective. Instead, I use my time to explain why we are necessary to the public and to educate regulators and lawmakers about how Teva can help,” she says.
Porat helps prep her executives, who are sometimes asked to justify their pricing structures before bodies like the United States House Committee on Oversight and Reform. She aids them with talking points and myriad briefing documents. In those moments, she focuses on Teva’s status as the leading manufacturer of generics, which help lower costs to patients and the healthcare industry as a whole.
This nuanced approach together with Teva’s pending settlement is helping the company make significant strides. After the deal made headlines, the company’s stock rose by 11 percent on the Tel Aviv Stock Exchange and 8.67 percent on the New York Stock Exchange. “We’re trying to be part of the solution and
“People may view pharmaceutical companies as greedy or bad corporate actors, and it will take a lot to alter that strong perspective . Instead, I use my time to explain why we are necessary to the public and to educate regulators and lawmakers about how Teva can help.”
Blank Rome’s Life Sciences attorneys provide sophisticated, cost-effective legal services to drug and medical device manufacturers.

Working closely with you, we offer strategic planning advice, regulatory assistance, and litigation services to meet your specific goals and ensure compliance in this highly regulated industry.
For more information, visit blankrome.com
help those who have been directly impacted,” Porat says.
With the deal expected to close in 2021, Porat has turned her attention to helping Teva fulfill its related obligations. She’s working with her counterparts in various business units as they prepare to manufacture and distribute millions of doses of Suboxone in the coming years.
“Galia is an outstanding lawyer and critical thinker,” says Sheron Korpus, a partner at Kasowitz Benson Torres, who represents Teva in complex litigation matters. “She is highly collaborative and takes an active role with outside counsel in guiding challenging matters to resolution.”
As Porat reflects on the many challenges related to opioid litigation and its intersection with the COVID-19
pandemic, she says the era has helped her redefine her leadership mentality and work ethic. “I’ve always dedicated myself to working hard and achieving the best results,” she explains. “But these times have forced me to focus on the most important things in both life and work. I trust my colleagues and outside firms to do their jobs without me micromanaging, and I make smarter choices about where I can add the most value.”
COVID-19 has brought one other unexpected benefit. As the world awaits a vaccine, individuals, corporations, communities, and governments suddenly have a newfound respect for pharmaceutical research and development. As the world looks on, Teva is ready to step into the spotlight. AHL
Galia leads the most complex litigation with innovative ideas, and we congratulate her on this well-deserved recognition.
“I knew I wanted to install sprinklers instead of putting out fires. It was the right move for me to go in-house at a public company.”
Healthcare is a constantly evolving industry that demands executives to plan ahead. Often, this means business leaders need to address department- or companywide issues to remain focused on driving innovation and devising strategies to maintain a high level of care.
86. David Prahl Sutter Health
90. Mary Klassen Szyndrowski American Medical Association
96. Susi Takeuchi UCLA Health
David Prahl uses an inclusive, hands-on approach to shape Sutter Health’s complex litigation strategy during challenging times
By Billy Yost
When David Prahl joined Sutter Health in 2013, he brought a wealth of employment law experience, but not the healthcare experience one might expect from someone who would later be tasked with overseeing Sutter’s complex litigation portfolio and building a more robust complex litigation program. “As an employment lawyer in private practice, I served clients across a wide range of industries, including healthcare,” Prahl explains. “But I focused my practice more on the financial services industry than any other.”
Eventually, Prahl had the opportunity to manage several high-profile litigation and regulatory matters that fell outside his regular employment law responsibilities at Sutter. These matters piqued his interest in healthcare law and motivated him to refocus his practice. “I really enjoyed that opportunity,” he notes, “and developed an interest in branching out to become as much a healthcare lawyer as I was an employment lawyer.
“It was especially rewarding to manage litigation involving legal issues that directly impacted Sutter’s core business and strategy,” he continues. “I felt like I could make more of a difference for Sutter and better enable the company to fulfill its not-for-profit mission.”
Prahl built a solid foundation in healthcare law while steadily learning the industry, eventually transitioning from employment counsel to his current role as deputy general counsel, which also includes leading Sutter’s vendor contracting team. The successful evolution is a testament to the DGC’s capacity for growth and willingness to look to mentors for advice and guidance. Now, Prahl is focused on enhancing Sutter’s complex litigation and vendor contracting
functions in the midst of a pandemic and one of the most challenging periods in the history of the healthcare industry.
The Value of Guidance
Prahl says he’s most grateful for his coworkers at Sutter, who helped him hone a new skill set in an unfamiliar industry. “I had to take the initiative to learn, including by asking some really basic questions of my colleagues at times. Their patience and generosity helped shape my approach,” Prahl explains. “They helped me understand that effective leaders have to convey to their teams
a willingness to engage, to be available to answer questions, and generally to be a resource for their team members.”
Experiences like these have influenced Prahl’s dynamic with his own team during
“I had to take the initiative to learn, including by asking some really basic questions of my colleagues at times. Their patience and generosity helped shape my approach.”
an uncertain time. “I try to make myself available as much as possible so there’s open dialogue, sufficient connectivity, and a sense that we’re working together. How you choose to respond to adversity is also important,” the DGC continues. “There’s plenty of it to go around right now, and it’s essential to know how to respond and model the right outlook, whether as a leader or a member of a team.”
In this regard, Prahl draws inspiration from an adverse summary judgment ruling in a major class action case while in private practice at Orrick, Herrington & Sutcliffe. “I still remember the date of the order and the awful feeling I had when I read it,” Prahl says. “But none of the leaders on our team panicked, which set the right tone going forward. Everybody rolled up their sleeves and immediately started working on a responsive appellate strategy, and the team ultimately reversed the decision in the Ninth Circuit Court of Appeals. I saw that leadership and valued it, and I try to emulate it today.”
If 2020 could be summed up in just one word, it might be “adversity.” Prahl says he’s proud that Sutter’s legal team has aggressively responded to the challenges posed by the pandemic. “Sutter’s Office of the General Counsel has very much taken an all-hands-on-deck approach,” the DGC says. “Initially, that meant just about every one of us was called away from our daily responsibilities to help the company adjust its healthcare delivery system to meet the challenges of the pandemic. The focus and scale of certain operations had to change pretty dramatically to help meet the anticipated surge of patients.”
For his part, Prahl coordinated an effort to obtain stays of Sutter’s litigation matters wherever possible, which helped free resources and enabled the legal team to better support Sutter’s response. He also led a cross-disciplinary project focused on anticipating and avoiding litigation trends emerging from the pandemic.
The challenges of responding to the pandemic have provided the DGC with new clarity moving forward. “The pandemic has been so disruptive that it’s important to take a fresh look at our program across the board, from how we try to anticipate and prevent litigation to how we manage our litigation to how we analyze its impact and learn from it,” Prahl says. “And as the pandemic shifts the healthcare landscape and new strategic priorities emerge, our litigation strategy must evolve to account for and reflect these new priorities. This is an opportunity to make our program even more efficient and impactful for Sutter.”
While Prahl is focused on enabling his team to meet the demands of a postpandemic world, he emphasizes that certain core objectives will remain consistent.

“In this role, I’ll always be responsible for anticipating litigation trends and finding ways to efficiently leverage our resources to reduce Sutter’s litigation risk profile,” Prahl says. “And when litigation can’t be avoided, we posture the company to advance an optimal position that is consistent with its priorities.
“These objectives can’t be met if I’m not sufficiently connected,” he continues, “both with the right company leaders, so I can know our strategic direction, and with my team, so I can know whether we’re helping advance it.” AHL




Why Jones Day? A true partnership based on communication, collaboration, conviction, and talent across specialties and jurisdictions.
Mary Klassen Szyndrowski continually adapts to improve support for both the AMA’s employees and the organization’s health-oriented mission
 By Natalie Kochanov
By Natalie Kochanov

n the surface, the American Medical Association (AMA) is a membership organization. But as Mary Klassen Szyndrowski explains, it’s much more than that. “The AMA is physicians’ powerful ally on patient care,” Klassen says. “We represent physicians and the patients they care for with a unified voice to all key players in healthcare.”
The AMA strives to remove obstacles that interfere with patient care and drives the future of medicine by reimagining medical education, training, and lifelong learning. It promotes innovation to tackle the biggest challenges in healthcare and improves the health of the nation by leading the charge to prevent chronic disease and health crises, all while eliminating health inequities. In other words, it’s much more than a membership organization.
Klassen’s role as the organization’s vice president of compensation and benefits revolves around the talented AMA employees working to achieve those goals. Bringing to bear her decades of experience within the human resources function, Klassen continues to enhance the employee experience by nimbly adapting to internal and external challenges alike. Her efforts and collaboration to reimagine policies and recommend new programs to aid employees in the face of everchanging circumstances not only benefit
individual workers but also allow the AMA to progress its critical agenda.
Klassen’s preparation for her current position began at railcar leasing company General American Transportation Corporation (GATX), where she transitioned from a role in accounting to one in payroll and external reporting soon after joining. It took moving into a compensation position at GATX, however, for Klassen fully to recognize that her career was on the right track.
“Compensation was where I felt at home,” Klassen says. “It was the best of both worlds: I was still doing analysis, but at the same time, I got to focus on people.”
Following a role managing GATX’s corporate HR, Klassen spent several years overseeing expatriate compensation and benefits at advertising agency Leo Burnett. She then gained further benefits experience at Sandoz Agro before leading compensation and benefits at data analytics company Information Resources Inc.
In each position, Klassen sought out opportunities to make improvements, whether for one individual or an entire class of employees. She discovered in the AMA a kindred mission: the organization’s goal to promote the art and science of medicine and the betterment of public health aligns with her own commitment to helping employees thrive.
As an AMA VP, Klassen applies her extensive HR knowledge to expand
benefits offerings and align compensation practices and programs across operating groups, all in collaboration with her team members. On top of her standard duties, the year 2020 saw her contending with the unique issues and questions that arose as the COVID-19 pandemic spread.
“What made 2020 challenging was both the phenomenal amount of change and the need for a rapid, yet thoughtful
response. At the AMA, we developed that response through a lot of collaboration and a lot of research. It truly took a village for us to work through how to support our employees during COVID,” Klassen reflects.
Klassen was a member of a crossfunctional team that researched and created a standard of conduct for COVID-19 policy to protect employees during the pandemic. “We were able to
 Mary Klassen Szyndrowski VP of Compensation & Benefits American Medical Association
Mary Klassen Szyndrowski VP of Compensation & Benefits American Medical Association
“ Compensation was where I felt at home . It was the best of both worlds: I was still doing analysis, but at the same time, I got to focus on people.”
develop an umbrella policy that sits on top of the regular policy manual,” she elaborates, adding that this policy was consistent with local requirements for a phased, volunteer-based re-opening of their office. In addition, guidelines were developed and communicated for most AMA employees to work from home while also ensuring the safety of essential employees.
For essential employees who needed to access the office, Klassen advocated for a temporary bonus as well as assistance with commuting costs, such as parking reimbursement for employees driving to the office and an Uber partnership to cover rideshare fees for employees who formerly relied on public transportation to get to and from work. Parking assistance continues to be provided to the essential workers, as well as the small number of employees who voluntarily returned to work inoffice later in the year.
Klassen and her team also investigated strategies for making remote work more comfortable and effective. To this end, the AMA modified its pay practices so that employees were able to take paid time off to care for loved ones diagnosed with COVID and continued its Caregiver Leave policy that provides paid leave to care for loved ones for other reasons.
Klassen’s team also increased the number of vacation days employees could sell to offset 2021 benefit premiums and increased the maximum rollover for unused vacation days into 2021. In addition, the organization pivoted to offering virtual wellness sessions and compiled a multitude of resources on its employee website, tackling topics from at-home childcare issues to mental well-being.
“We worked with some of our existing providers and explored new partnerships so that we could offer resources and outlets to help employees cope with their stress and anxiety and family needs,” Klassen says. She emphasizes that partnerships with caregiver platform Care.com and with NAMI Chicago, a local branch of the National Alliance on Mental Illness, created a wider range of options crucial to reaching and engaging with employees in need.
These resources became even more important as racial injustices across the United States compounded employees’ COVID-related stressors. AMA plans to continue partnering with NAMI Chicago in 2021 and researching additional resources to support employees.
“Employee welfare is our number one priority,” Klassen emphasizes. “We are very science-based at the AMA, so it’s all about when the science says that it’s safe to return to the office.”
In the meantime, Klassen will concentrate on rolling out a more robust employee assistance program to AMA workers. As she does so, she’ll keep an eye on both the research and its employee implications, looking as ever for ways to improve the lives of the employees endeavoring to make the country a healthier place. AHL
Alliant congratulates Mary Klassen Szyndrowski and the AMA team for the well-deserved recognition of making a difference across their organization.
Alliant’s experience, scale, and full range of services, including our proprietary Sagewell healthcare life and disability benefits trust, can help make a difference to your organization and its employees.

Alliant is dedicated to serving the business that matters most. Yours.
With a full range of property and casualty and employee benefits services, we will work tirelessly to design an insurance program that moves you forward, even in the most competitive of markets.
When Susi Takeuchi became CHRO of UCLA Health, she found HR in need of a lifeline. Three years later, the department floats above its competition.
 By Clint Worthington Portraits by Philip Cheung
By Clint Worthington Portraits by Philip Cheung

It took a few tries for University of California, Irvine’s (UCI) then Head of Human Resources Susi Takeuchi to accept an offer to become chief human resources officer at University of California, Los Angeles (UCLA) Health.
“At the time I was approached about the opportunity, I’d only been with UCI less than two years and felt like I was just not ready to leave yet,” she recalls. But, attracted to the size and reputation of UCLA Health, she eventually found its offer hard to pass up. A positive personal patient experience at UCLA Health further solidified her interest.
When Takeuchi first arrived on the job, she noticed how siloed the HR function seemed. As a competitive employer, UCLA saw candidates vying for positions inside the organization. Yet “some of our leaders at that time thought we didn’t need to do anything to attract candidates,” she recalls. “There was a general sense of complacency across the organization because we had such an outstanding reputation. People were stuck thinking they didn’t need to improve on anything because others were eager to work here.”
Takeuchi knew that the HR team still needed to work hard to make sure UCLA stayed the top academic medical center option for the nation’s best healthcare professionals. So, she created a teambased strategic plan to overhaul the
organization’s HR function to make it more functional, streamlined, and incentivized to draw in top talent.
Takeuchi’s first step was to assess where the organization was in terms of priorities and performance, in addition to where it wanted to be at the end of the process. She started by interviewing almost all 180 HR employees at UCLA Health as well as various other clients for feedback on where they stood.
The hands-on approach took HR employees aback at first: “They’d never done strategic planning before; they were very nervous about it,” Takeuchi remembers.
With that data, Takeuchi and her fellow leaders held strategic planning sessions with the HR employees, funneling and specifying the data even further until they had a full-fledged strategic plan. “It really paid off, involving all these people up front,” she says, noting that doing so allowed them to build a new overall HR mission, vision, and set of values from which they could work.
Takeuchi spends part of her time living on a boat parked in the marina close to UCLA Health. According to her, it helps her shave a five-hour commute by car down to forty-five minutes. But more

than a means of fast transport, the boat inspired a potent metaphor for the purpose and direction of the organization’s HR team.
Over three days of small group sessions involving every HR employee, Takeuchi tasked each employee group to draw a picture of any kind of water vessel they could imagine that described the current state of the HR function, including the people, the water, and the environment. Many groups drew sinking ships, sharks in the water, rain clouds, and people on decks shouting,
“Help!”—all-around indicators of a chaotic HR environment.
Then they were to draw the kind of functioning boat environment they wanted for the future. “What was amazing was that every single group drew almost identical pictures,” Takeuchi says, describing the sunny skies and one mighty vessel, “which meant we were all on the same page.”
There were still some sharks in the water (“HR will never get rid of all the sharks,” Takeuchi says, laughing), but they were more manageable. That

“What was amazing was that every single group drew almost identical pictures, which meant we were all on the same page .”
We are most grateful for her leadership and creating an environment at UCLA Health Human Resources that is the gold standard for other institutions to model. Her impactful mentoring has endeared herself to many across all UCLA campuses. JNI sincerely values our partnership.
exercise helped Takeuchi and her team learn where the HR department was hungry to be, which helped drive their vision for the end of the process.
Sail Toward New Goals



From there, Takeuchi set about asking HR employees, “What do you want people to say about you when you walk out of the room?” Together, they boiled down some key characteristics for which HR wanted to be known: they’re knowledgeable, resourceful, responsive, collaborative, and trusted.
To reinforce those values, Takeuchi set up initiatives like the Standing Ovation Awards, where twice a year, HR employees can nominate each other for demonstrating those traits.
Every year, Takeuchi and her team check in on their HR mission, vision, and guiding principles to see if there are ways that they want to modify them. Whether it’s growing the organization’s talent, facilitating an engaged workforce, integrating and synchronizing HR as a
department, or advancing HR talent, they strive to make sure the department is growing and learning along these lines. Since focusing on these initiatives, UCLA Health has won awards for its HR work, including Forbes’ Best in State and Large Employer Awards. In 2018, they ranked number eight on Indeed’s list of Top-Rated Workplaces (Best Hospitals). US News & World Report also ranks the hospital at number one in California and fourth in the nation, and ranks its medical school at number six in the nation for research. These are just some of the many accolades UCLA has received.
Takeuchi’s work, both at UCI and UCLA Health, has taught her that healthcare, specifically in the HR sphere, has a long way to go. As healthcare catches up to other industries’ approaches to HR, Takeuchi notes, “It’s reassuring to know that I’m in the same boat with everyone else.” But with her help, UCLA Health seems to be sailing for smoother waters. AHL

“HR will never get rid of all the sharks.”
Healthcare leaders know there is an increasing need to help individuals manage their own health, anywhere and anytime. To do that, they develop products and services and offer resources aimed at motivating members of every community to stay engaged with their health—empowering them to be their best, at home or at work.
104. Gerry Baker Parkland Health 110. Karen Hale AbbVieGerry Baker always had an interest in healthcare and during his early years in education thought he would be a pediatrician one day. As he moved through college, he embarked on a more business-oriented path, though he never lost his interest in the healthcare field.
“I took a health occupations class in high school and actually started my career right out of high school as a nurse’s aide,” he recounts. “While attending college, I realized that chemistry and microbiology were not my forte, so I majored in business. Despite this, I continued to work in healthcare as a unit tech while in college.”
Over time, Baker has become a trusted healthcare executive thanks to his revenue cycle management skills, which have proven to drive results in turning around operational challenges, decreasing investment in accounts receivable, and improving cash flow in profit and nonprofit entities.
Today, he works as senior vice president of revenue cycle for Dallas-based Parkland Health and Hospital System (PHHS), responsible for patient access, health information management (HIM), revenue integrity, billing, customer
service, and collections and managed care contracting functions.
“I was interested in joining PHHS because I believed in its mission, which is to ‘serve the underserved,’” Baker explains. “I thought that I could make a difference and improve the overall quality of care of the underserved in Dallas County.”
Baker has eight directors and one vice president reporting to him, and, together, his team manages more than seven hundred employees.
“My leadership philosophy is to hire competent professionals and allow them to do their jobs and manage them based on their strengths and abilities,” Baker shares. “I ensure that my team subscribes by holding everyone accountable and being transparent with expectations, while building trust directly with them and facilitating trust among their peers.”
While he’s been working for PHHS since November of 2017, Baker has more than twenty-five years of experience in revenue cycle management consulting to hospitals, physician practices, ambulatory care centers, and other healthcare clients.
“My experiences at all of my previous jobs—including while I was selfemployed for eleven years—prepared me for the role I have today,” he says. “At Ernst & Young, the experience of working with many types of hospital and physician practices and having exposure to various complex business problems was invaluable.”
Meanwhile, his work as a consultant allowed Baker to hone his skills at identifying and recommending solutions to solve problems that he would not have otherwise encountered by being with just one organization.
Prior to joining PHHS, Baker completed one last assignment, lasting eighteen months, as an independent consultant at a safety net public hospital in California. He believes that this experience fully prepared him for the role he has today, as the two institutions are very similar in size and scope and see some of the same challenges.
“Throughout my career, I’ve been focused on process improvement and gaining knowledge on best practices,” Baker notes. “I’ve had the opportunity to see what works for different types of organizations and what doesn’t work. But I’ve learned that one of the most critical aspects is people management and that if you get people to trust you, anything can be accomplished.”
That’s certainly been the case as Baker has had to lead Parkland Health’s revenue cycle function through this last complex year. On top of navigating a pandemic,
“As for my career, I hope to leave a legacy here at Parkland—that I, in fact, made a difference on the organization.”
 Gerry Baker SVP of Revenue Cycle Parkland Health
Gerry Baker SVP of Revenue Cycle Parkland Health
“I’ve learned that one of the most critical aspects [to improving processes] is people management and that if you get people to trust you, anything can be accomplished.”
he and his team launched an initiative to enhance billing software to improve patient care and overall quality.
He explains that Parkland, some years back, had combined its professional and hospital billing into one system, which was originally designed to handle hospital billing only.
“They had highly customized the application to handle the professional billing,” Baker says. “This created a major problem with being able to track RVUs and revenue at the provider level. When we realized that we were lacking this ability to truly track provider productivity at the granular level, out of this came the need to implement the enhancement: [Epic’s Professional Billing Module].”
This system was implemented over a year’s period with the help of the external Epic team and the internal IT resources. The implementation was completed in late 2020.
“This new program will give us insight into provider productivity and enhance our ability to capture revenue metrics by individual provider,” Baker explains. “In the future, this information may enable us to look at different ways to model how our employed providers are compensated.”
Obviously, 2020 presented many challenges. Baker says his key to leading through the complex year was staying focused on the end result, which, in addition to completing the Epic implementation, was improving PHHS’s denials management program. With
the goal of managing the claim denial process in the most efficient, holistic, and systemic way, Parkland turned to Change Healthcare’s revenue cycle technology and services to assist with both professional and hospital claim denials.
“Our RCM technology and exception-based workflows help Parkland accelerate clean claims and optimize reimbursement,” says Nicholas Raup, associate vice president of product management at Change Healthcare. “Working alongside Gerry and his team has been a true partnership. We are heavily focused on enhancing workflows, creating insights, and identifying best practice processes for denial prevention and resolution.”
“Through all of the challenges, we still were able to finish the year ahead of our cash goals, which is a big win,” Baker enthuses. “Other keys to leading through this complex year included taking advantage of government reimbursement programs that were born out of the PHE, monitoring productivity levels of remote staff—90 percent were working from home—and celebrating little wins along the way.”
In 2021, Baker hopes to continue to build the revenue cycle function at Parkland into a world-class operation, to enhance the healthcare system’s clinical documentation improvement program, and to improve revenue generation.
“As for my career, I hope to leave a legacy here at Parkland,” Baker shares, “that I, in fact, made a difference on the organization.” AHL
After a banner year in 2020, AbbVie is putting its money where its mouth is to help support underserved communities
 By Donald Fricke
By Donald Fricke
 Karen Hale VP and Deputy General Counsel AbbVie
Karen Hale VP and Deputy General Counsel AbbVie
Interestingly, 2020 was a banner year at pharmaceutical company AbbVie. The company’s stock rose 16.6 percent over an industry-wide growth of just 1 percent. The acquisition of Allergan, maker of Botox, helped expand and diversify the company’s revenue base along with helping grow its presence in new therapeutic areas. The acquisition also brought more leadership from the immunology and hematological oncology areas.
The addition of Botox to AbbVie’s portfolio was a shot of revenue-driving life, but it wasn’t the only deal that helped bolster the company’s future. Two immunology drugs were approved by the FDA in 2019: Skyrizi and Rinvoq have performed beyond company expectations, with revenues for the two drugs alone equaling about $2.2 billion.
AbbVie also saw new approvals in 2020. Oriahnn—developed to combat heavy menstrual bleeding in premenopausal women with uterine fibroids—gained FDA approval. Late-stage data from a migraine prevention candidate has also been promising.
It wouldn’t have been 2020 without a COVID-19-related transaction, and there, too, AbbVie has delivered. In late December, Harbour BioMed announced
that AbbVie had licensed their SARSCoV-2 neutralizing antibody and its program, and it initiated a Phase 1 clinical trial for the prevention and treatment of COVID-19.
“The rapid progress we have made to date is a credit to the outstanding research by our teams and university partners, the strength of HBM’s fully human antibody discovery platform, and AbbVie’s world-leading expertise in antibody and antiviral drug development,” principal founder, executive director, chairman, and CEO of Harbour BioMed Dr. Jingsong Wang said in a statement. “With the clinical program at AbbVie now underway, we are in a position to contribute a new therapeutic option to address this pandemic.”
The significant transactions of the past two years were aided by AbbVie’s internal legal team, including Vice President and Deputy General Counsel Karen Hale. Hale has been at AbbVie and its 2013 spin-off namesake Abbott Laboratories since 1997, where she served in patent litigation, commercial litigation, and ethics and compliance roles prior to assuming her current position in 2019.
Hale also leads AbbVie’s racial justice efforts, which aim to “establish a
long-term, multifaceted program focused on helping expand quality education, jobs, healthcare, and justice” on behalf of the pharma company.
That included a $50 million investment in a five-year program to support underserved Black communities across the United States. In collaboration with nonprofit partners, including Direct Relief, University of Chicago Medicine’s Urban Health Initiative, the National Urban League, Year Up, the United Negro College Fund (UNCF), and Providence St. Mel School, AbbVie is hoping to directly combat the issues of health and educational inequity that are common to so many parts of the US.
“We asked partners with deep community roots where they saw the greatest needs, and we heard that reducing health disparities and providing educational and workforce-related opportunities for underserved Black communities were urgent yet ongoing needs,” Hale said in a prepared statement. “While we know that change cannot happen overnight, we hope our commitments will help improve opportunity today while supporting important work to address long-term, systemic issues of racism.”
The DGC’s efforts haven’t gone unnoticed. She was celebrated as one of Black Enterprise’s Most Powerful Women in Corporate America. The 136 women who make up the list met the following criteria: “They have succeeded by leading with performance, deeply understanding their company culture, deftly navigating the corporate landscape, and—above all—wisely wielding their power to determine their own destiny.”
After a year of so many lows, Hale has been able to continue to invest her time and efforts in issues of the utmost importance, from her employer’s efforts to combat the COVID-19 pandemic to its outspoken mission to seek more equity for the most underserved in our communities. If this isn’t wielding power the right way, nothing is. AHL
in American Healthcare
With more than 200 lawyers based in New York City, Patterson Belknap Webb & Tyler LLP delivers a full range of services in litigation and commercial law. For more information, please visit www.pbwt.com
1133 Avenue of the Americas New York, NY 10036 www.pbwt.com
Patterson Belknap is proud to partner with AbbVie, and admire the company for its creative and cost-effective approach to legal matters. We congratulate our colleague, Karen L. Hale, on this well-deserved feature article and recognition of her leadership.We are thrilled to congratulate our colleague, Karen L. Hale, Vice President, Deputy General Counsel at AbbVie, on this welldeserved recognition of her leadership and accomplishments
Leader.
In Lynn Grieves’s life and career, he keeps an open mind and a steadfast attitude to help anyone or any place through triumphs and tribulations
By Billy YostThere’s a remarkable parallel that runs between the personal and professional life of the chief compliance officer at CHOC. Lynn Grieves didn’t set out to find a role in healthcare. He moved from public accounting and eventually found his way into the healthcare space both in compliance and internal audit, with a brief role on the operational side. It just sort of happened.
It’s the same exact phrase he uses when describing the adoption of his now eight-year-old son, Jaden. There may not have been any grand design in the CCO’s own planning, but both Grieves and his son are right where they belong.
Grieves’s tenure with CHOC was preceded by helming the CCO position and internal audit function at MemorialCare Health System for two decades. His transition from internal audit to the compliance side included one of the more difficult periods of Grieves’s career—an interim role where he was tasked with integrating a competing health system, a Catholic hospital that was a half-mile away.
“My job was essentially to lead the project team in closing down the Catholic hospital and integrate the workforce, medical staff, and operations into our health system,” Grieves says. “We did it on budget and on time, but my goodness,
it was a memorable year of my life.” The integration proved particularly challenging because Grieves was trying to merge church and state, so to speak. Bringing two long-term competing organizations together with dramatically different cultures and senior leadership management styles, one gets the feeling Grieves spent as much time playing referee as he did an operational officer. When it was over,
“It’s not cold, it’s not scary, it’s not isolated. It’s just an amazing place that is so warm and inviting.”
he was grateful to make the leap full-time back into compliance.
Since coming to CHOC in 2009, Grieves has had the opportunity to aid several modernization efforts, both to continue the cutting-edge efforts to find better ways to serve its patient population and to align with constantly changing privacy standards in the state of California.
The COVID-19 pandemic required Grieves and his team to aid the organization’s telehealth efforts at a rapid rate. “We’ve been doing telehealth for many years, but not in the traditional sense,” the CCO explains. CHOC has a presence in many hospitals in its four-county area and has one of the largest pediatric transport operations in the country, conducting approximately 4,500 transports per year. Many of these patient transports involve critically ill children who require a specialized transport team equipped with telehealth equipment, so specialists at CHOC can conduct telehealth encounters on the spot.
“COVID has ramped up our more traditional telehealth efforts considerably,” Grieves says. “There are so many legal
technical aspects that accompany this, from getting consent for the telehealth visits, to ensuring provider credentialing, to our international efforts so our specialists are able to relay their expertise all over the world.” CHOC is also working on expanding its relationships with nearby schools in an effort, Grieves says, to “go to where the kids are.”
Grieves also says that there are a number of legal obstacles to tackle when it comes to mental health treatment for its young patients. The 21st Century Cures Act was designed with the intention of getting patients information about their health as quickly and efficiently as possible, but when it comes to mental health and a pediatric population, that can be a difficult proposition. “Some of this information is not necessarily appropriate to share with the patient or legal guardian during treatment; these may be notes by our physicians where it would make the most sense to have available after their treatment,” Grieves says.
Patient consent laws for children ages twelve and younger differ wildly for patients seeking treatment from
 Lynn
Lynn
“We’re the only organization in our area with mental health inpatient treatment available for children younger than twelve. It’s been full since we opened it.”
twelve to eighteen years of age. Creating an accessible portal with the information of minors requires adherence to myriad privacy regulations, both state and federal.
CHOC’s Cherese Mari Laulhere Mental Health Inpatient Center is a point of pride for Grieves. “We’re the only organization in our area with mental health inpatient treatment available for children younger than twelve,” the CCO says. “It’s been full since we opened it.”
Grieves says the design of the facility promotes a healing, compassionate environment, while maintaining the highest safety standards. “It’s not cold, it’s not scary, it’s not isolated. It’s just an amazing place that is so warm and inviting,” Grieves says. CHOC is also planting mental health providers in its more localized clinical locations, so mental health can be treated at the same location as primary care.
Grieves may not have planned to come to work for a children’s hospital, but he and his wife have been on the front lines of making children and family’s lives better as part of Safe Families for Children. The social services organization was created in order to keep struggling families together by enlisting volunteers who are willing
to host children anywhere from hours to months while parents try to better their circumstances.
The Grieves family had temporarily hosted many children and seen them safely reenter their biological family homes prior to receiving a call that a baby born that day would be in need of temporary care. After several months, the child was given up by the mother and Grieves and his wife were asked by the mother to adopt him. “It just happened,” Grieves says. “We prayed about it. We had the means. And he’s been our son ever since.”
Jaden, now eight, knows he is adopted —knowledge that leading childcare experts highly recommended adopted children have. But even in the delivery of that news, it’s hard to imagine the youngest member of the Grieves family seeing anything different about his life. “We’re all adopted into God’s family,” Grieves says. “That’s exactly the way we tell him.” AHL
www.health-law.com































































Hooper, Lundy & Bookman is the largest law firm in the country dedicated exclusively to representing health care providers and suppliers.
Hooper, Lundy & Bookman proudly supports CHOC and congratulates Lynn Grieves on his recognition in American Healthcare Leader

One of Dan Buettner’s many passions is food. So far, he’s written two books of recipes based on the food traditions of citizens living in Blue Zones. This smoothie recipe offers a simple yet contemporary use for wholesome components. It combines bright, protein-packed ingredients to help you start your mornings right. It’s also completely customizable. Swap bananas for peaches in the summer or experiment with different berry combinations. Enjoy!


Ingredients

1 cup nondairy milk of choice
1/2 frozen banana
1/2 cup frozen strawberries
1/2 cup frozen blackberries or blueberries
1 tablespoon pea protein
Directions
Blend all ingredients in high-powered blender until smooth.
Source: bluezones.com


We’re passionate about innovations that have impact. Which is why we’re bringing consumer technologies into the digital patient experience. For example, by working with Change Healthcare, providers can improve efficiency and revenue capture while offering patients self-serve tools that match their familiar, everyday digital experience. It’s one more way we’re helping change healthcare for the better.
