
An Evolving Industry,
An Enduring Strategy
Duke University Health System’s Fabian Stone identifies four areas—talent management, efficiency, cash flow, and habits—where leaders can supercharge their revenue cycle operations p. 36


An Evolving Industry,
An Enduring Strategy
Duke University Health System’s Fabian Stone identifies four areas—talent management, efficiency, cash flow, and habits—where leaders can supercharge their revenue cycle operations p. 36
Nancy Sassower
Dive into the intricacies of Project One, Northwestern Medicine’s enormous initiative to unify its EMR system, from the perspectives of five of the project’s leaders, p. 101
12. Paul Tufano believes every patient, no matter their ability to pay, deserves access to healthcare.
24. Stephanie Schnittger’s approach to Inova Health System’s finances goes beyond dollars and cents.
18. Tommy Mitchell explains how procurement and innovation go hand in hand at GE Healthcare.
32. Piyush Sharma takes a patient-centric approach to compliance at Alexion Pharmaceuticals, Inc.

80. Dwight McBee instills in his team that even the smallest gestures can make a big impact for patients in their care.
94. Kimberly King Webb honors a spirit of collaboration in her legal work at CHRISTUS Health.
91. Natasha Milatovich is doing away with work/life balance and replacing it with life/ work integration at Adventist Health West.
98. Kevin Henley watched his father battle cancer, and now that experience motivates his legal work at Otsuka America Pharmaceutical, Inc.

36. Fabian Stone guides leaders into new territory for the healthcare revenue cycle.
60. Tommy Comer is expanding the definition of what it means to be a competent senior-care provider.
46. Kate Proctor deftly navigates the changing federal regulations surrounding hospice care.
68. Renee Ennis strives to earn clinical laboratories a more proactive role in patient care.


146. EnvisionRx provides healthcare organizations a solution to rising prescription drug costs.
174. Robert Brooks discusses how he helped add $600 million to Erlanger Health System’s bottom line.
149. Nancy Stockslager identified traits that top performers share at Gwinnett Medical Center to improve hiring.
178. Jessica Collins leads her legal team to be proactive partners in business decisions at athenahealth.

110. Cord Sturgeon details how he helped get Northwestern Medicine’s surgical staff on board with its EMR overhaul.
124. Lacy Knight oversaw the opening of a new Northwestern Medicine hospital during its EMR initiative.
116. Steve LoBue outlines how Northwestern Medicine’s EMR project changed the way he leads.
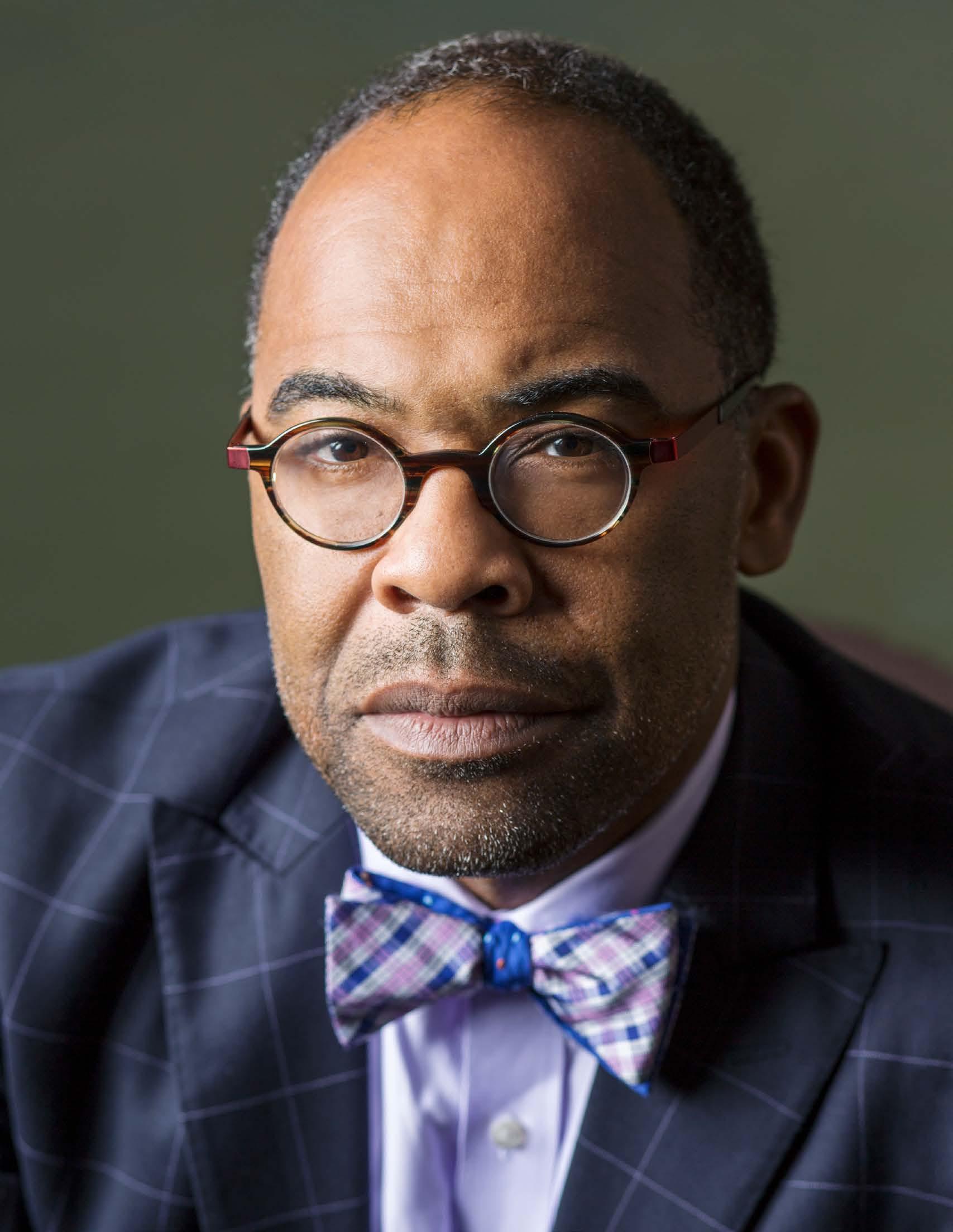
130. Nancy Sassower ensured Northwestern Medicine’s most important people had a voice during its EMR transformation: patients.

194. Priyanka Das Sarma develops programs for Hilton employees to replenish their minds, bodies, and spirits.
212. Eric Record increased engagement in Steel Dynamics’s wellness program by making it more responsive to employees’ needs.
208. Bernadette Melnyk wants The Ohio State University to be a beacon of wellness around the world.
216. John Bosco created a care system at Northwell Health where patients can see all their medical information from a smartphone.
VP, Creative
Kevin Beauseigneur
Director, Creative Operations & Editorial
Cyndi Fecher
Editor
Joe Dixon
Digital Content Manager
Frannie Sprouls
Contributors
Roland Archer
Abhinanda Datta
Jenny Draper
Lori Fredrickson
Will Grant
Leo Herrera
Joseph Kay
Russ Klettke
David Levine
Charlene Oldham
Anthony Ruth
Jeff Silver
Clint Worthington
Director, Design & Photo
Caleb Fox
Senior Designer
Anna Jo Beck
Designer Lauren Keeling
Photo Editors & Staff Photographers
Cass Davis
Gillian Fry
CEO
Pedro Guerrero
Managing VP
Marc Jerbi
VP, Hispanic Division
Vianni Busquets
Senior Director, Finance
David Martinez
Director, Client Services
Cheyenne Eiswald
Senior Client Services Managers
Rebekah Pappas
Katie Richards
Client Services Manager
Skylar Garfield
Director, Talent Acquisition
Elyse Schultz
Director, HR & Operations
Megan Thorp
Executive Assistant to the CEO
Jaclyn Gaughan
Senior Directors, Sales
Ben Julia
Sarah Jameson
Directors, Sales
Jane Haglund
Rachel Miller
Associate Director,
Strategic Development
Kara Thomas
Director, Strategic Partnerships
Krista Horbenko
Director, Business Development
Jenny Vetokhin
Business Development Managers
Erin Malone
Elif Negiz
Strategic Account Manager
Taylor Frank
Content & Advertising Managers
Megan Apfelbach
Lauren Cavers
Abbey Cunningham
Sarah Gaertner
Max Krevitz
Noah Miller
Brooke Rigert
Kelly Stapleton
Drew Thomas
AHL Magazine® is a registered trademark of Guerrero, LLC.
©2019 Guerrero, LLC
guerreromedia.com
825 W. Chicago Ave. Chicago, IL 60642
Reprints
Reprinting of articles is prohibited without permission of Guerrero, LLC. For reprint information, contact Reprints & Circulation Director Stacy Kraft at stacy@guerreromedia.com
One of the quickest ways to elicit groans from a staff is by telling them things are about to change. In fact, Mary Shelley, author of the classic novel, Frankenstein, wrote in her book, “Nothing is so painful to the human mind as a great and sudden change.”
Healthcare is by no means immune to these great changes. The industry-wide shift to value-based reimbursement from volume-based reimbursement has forced healthcare organizations to reevaluate how they deliver care to their patients. And that’s just one example of a change taking place in this rapidly evolving industry.
EMRs are also under the microscope, as large health systems in particular move to unify their systems to create one comprehensive record of care for all their patients. Northwestern Medicine, a health system with hospitals that serve patients over more than a 1,000 square mile area in northeastern Illinois, is on the forefront of this shift.
As part of our change management issue of American Healthcare Leader , five Northwestern executives explain the complexities of Project One, an initiative to unify the organization’s EMR across all of its care locations in an effort deliver even faster, more reliable patient care. (p. 101)
Each of these five leaders was tasked with helping oversee a different aspect of this enormous undertaking, from training clinicians on the new EMR to ensuring patient feedback was incorporated into the new system. Along with our guest editor, Northwestern Medicine’s Dr. Thomas Moran, who
helped hand-select the team that made this ambitious vision a reality, these individuals helped Northwestern enter a new era of patient care.
Hearing these executives’ stories, it became clear that there were two hallmarks of this successful transformation: communication and teamwork. Each of these leaders: Lea Ann Arnold, Cord Sturgeon, Steve LoBue, Lacy Knight, and Nancy Sassower, worked tirelessly to relay changes to staff, prepare them for updates to workflows, and solicit feedback from critical stakeholders throughout this three-year process.
Working on this issue made me reflect on how I could apply change management principles to my own life. Although I’m not overhauling a health system’s EMR, I realized there have been several opportunities for me to utilize communication and teamwork in my everyday life. From dealing with a move to preparing for how snow can impact a commute in the winter, or adjusting to a new job, change management can be beneficial to anyone if they practice applying its principles.
And with new changes coming to healthcare continually, it’s clear that leaders will have to embrace a positive approach to change management to stay ahead of their competitors and serve their customers.
Joe Dixon Editor


Every day physicians and nurses tell patients about something they need to change: stop smoking, take this medication, you will need surgery, and more. The changes never stop. Clinicians know it is hard for the patients, but they do it for their own good. But, try to ask a doctor or a nurse to change part of their workflow or daily routine and all hell breaks loose. Human beings naturally resist change. More specifically, humans resist change to their interpersonal relationships that are a byproduct of technical or workflow changes.
This resistance can be particularly fierce at a large health system such as Northwestern Medicine, where about one year ago, my team and I completed the transition to one unified EMR system—a major consolidation of our legacy systems. Health systems are complex, providing various combinations of care, activities, events, interactions, and outcomes that make an effort like ours quite the undertaking.
The EMR we use to care for patients and manage our health system can help or hinder us. But the EMR does one thing well—highlight our workflow problems. A key to successfully addressing workflow issues and to overhaul a health system’s EMR system is to fully understand the problem being solved for. To do this, it’s important to look at the processes, policies, and people involved in the workflows. By questioning each
step in the workflow we can remove unnecessary and inefficient steps, modify and align policies, and keep things simple. Keeping things simple sounds easy, but it is not always easy. Many solutions that come to the table seem obvious, but the obvious solution does not always produce the desired result. In medicine there are no certainties, and this axiom also applies to managing change in a system.
Another key to success to a project like this is to bring together the people who use the EMR, show them what tools are in the toolbox, and allow them to utilize the tools in the best way for the problem at hand. By listening to the people who use the EMR and freeing them to drive change, it allows you to nudge the system in the new direction.
Championing change is demanding and fatiguing; it requires you to challenge current workflows and processes and to stand up against the habits of established, well-worn behaviors.
Bringing people together and forming trusting relationships between the users of the EMR, the programmers of the EMR, and the leaders of the system leads to measurable change for the system by supporting the needs of the clinicians and, most of all, our patients.
Every step an executive takes on their career journey is pivotal to achieving their current successes. Along the way, individuals accumulate technical skills, foster relationships, and develop the leadership acumen that have turned them into pioneers of the industry.
18. Tommy Mitchell
21. Tom Vertich
24. Stephanie Schnittger
28. Craig Guinasso
32. Piyush Sharma

Paul Tufano is on a mission to provide access to care to underserved populations and to help provide a pathway to prosperity and independence
By Jeff Silver | Portraits by Cass Davis
Paul Tufano brings a unique perspective to the complexity of healthcare. It comes from his incredibly varied career, which has included leadership roles in law, government, and now healthcare.
Before taking on his current role as chairman and CEO at AmeriHealth Caritas—a national Medicaid managed care company with more than six thousand employees operating in fifteen states and the District of Columbia—Tufano served as general counsel for Independence Blue Cross; as general counsel for the Commonwealth of Pennsylvania under Republican Governor Tom Ridge; and as a partner in the Philadelphia law firm Blank, Rome, Comisky & McCauley. And despite his serving in the cabinet of Republican Governor Ridge, in 2002, then-Democratic Governor-elect Ed Rendell asked Tufano to serve as cochair of his transition team. Tufano believes the experience he gained from each opportunity prepared him for the next one and that they all now contribute to what he considers his most challenging—and rewarding— undertaking: leading a managed care organization.
“I’ve been able to gain an extraordinarily broad view of the issues that organizations face every day, as well as the stakeholders they serve and their relationships with them,” Tufano says. “The key to managing a diversity of needs and interests is to think broadly and strategically, and understand how all the individual pieces have to fit together seamlessly.”
That approach is important in the pursuit of AmeriHealth Caritas’s mission to help provide access to healthcare and build healthy communities among underserved populations. The strategy helps address obstacles that, even in this day and age, stem from uninformed opinions and bias, according to Tufano.
To combat misconceptions, such as Medicaid recipients don’t work (more than 70 percent do) or they receive cash payments (most don’t), Tufano takes advantage of every opportunity to disseminate the truth. “I often pull out my own insurance card to emphasize that we want our Medicaid members to have the same access to healthcare as those who are more fortunate,” he explains. “The least fortunate members of our society should be able to walk through a hospital’s front door to see a physician and be proactive about their health, rather than being forced to wait until they are so sick they have to go to the emergency room.”
“I often pull out my own insurance card to emphasize that we want our Medicaid members to have the same access to healthcare as those who are more fortunate.”
Whether he’s addressing members of Congress, state legislators, or the public, Tufano highlights that AmeriHealth Caritas is in the “dignity business.” To make that business successful, the company actively focuses on the social determinants of health and develops pragmatic programs to help members find pathways to prosperity and independence. This means caring for the whole person, not just a disease or condition. The company’s robust network of wellness centers go beyond medical care by providing, among other support resources, answers to insurance questions, information on how to earn a GED, classes in nutrition, financial literacy, job training, and referrals to programs offering heating assistance in the winter.
In the communities it serves, AmeriHealth Caritas partners with food pantries and grocers to address food insecurity, and works with ride-share services to help members without access to transportation get to their healthcare appointments.
“We become part of the communities we serve,” Tufano says. “We’re in a grassroots type of business, and we are committed to meeting our members where they are.”

“I actually look forward to a day when we don’t need Medicaid because it will mean we’ve eradicated poverty.”
Government service taught Tufano to listen as well—and to overlook labels that might obscure shared interests and objectives between what appear to be opposing parties. For example, after having worked on transition teams for both major political parties, he realized that each side was genuinely committed to giving their administrations the best possible start so they could effectively serve all citizens, whether or not they had voted for the incoming governor. Tufano’s experiences serve as an ongoing reminder to stay openminded, think creatively, and seek advice that others might not consider.
Tufano said his tenure in government helped him to appreciate the incredibly difficult work that faces state government officials who manage Medicaid programs. “They are the unsung heroes of government,” Tufano says. “They manage billions in taxpayer dollars, often the largest line item in a government’s budget. And no other program affects so many people.”
Tufano also learned the importance of compromise when developing effective solutions to complex challenges. “There are two sides to every story, and understanding
both is more important than winning every single time,” he says. “Healthcare is complicated, so we need to consider the best ideas from all sides in order to be as constructive, creative, and innovative as possible.”
It’s not uncommon for Tufano to take a historical perspective when describing AmeriHealth Caritas’s mission. He often refers to the first hospital in the US, the Pennsylvania Hospital—which was founded in Philadelphia, where the company is based—by Benjamin Franklin and physician Thomas Bond in 1751, with a mission to care for the poor. The implication is that even before the Declaration of Independence, the nation had a culture of equality, inclusion, and caring for the less fortunate.
“I actually look forward to a day when we don’t need Medicaid because it will mean we’ve eradicated poverty,” Tufano says. “But until then, it’s important to agree that providing efficient, affordable healthcare is as vital to society as are other demands on our resources. Once we have that agreement, we can start talking about how to work together and relegate poverty to a thing of the past.” AHL



We started over 35 years ago, serving a handful of members from a spare closet in a West Philadelphia hospital.
Today, we are a leader in Medicaid managed care, with 6,200 employees serving 5.3 million members nationwide.
Our mission to help people get care, stay well, and to build healthy communities is built on an integrated approach that brings together states, providers and caregivers to help members access the highest quality care and achieve their dreams.



By Leo Herrera
You may not think much about it, but almost everything made around you has been through a long journey.
The engines of the planes in the sky, the power plants that run the city’s electricity, and even the sensors doctors use for CT scans. All of these components have been thoroughly designed, tested, sourced for materials, tested again, and then delivered to the customer.
No one at GE Healthcare thinks about this more than Tommy Mitchell. As the organization’s vice president of procurement, Mitchell and his team perform a balancing act of delivering the best quality healthcare while reducing costs so patients and customers can afford their care. “But the two can be solved together. Every industry has something they’re working on, but in the healthcare industries, it’s more acute—we can’t provide healthcare if it’s too expensive.”
GE Healthcare has existed for nearly a century, the result of a merger between Victor Electric and General Electric, two of the biggest X-ray tube manufacturers at the time. Today, GE Healthcare also develops technology such as MRI machines, CT machines, and ultrasound, in addition to X-Ray tubes, to name a few. In recent years, GE believed its healthcare business wasn’t growing as much as it could, so Mitchell was brought in to help. “I came in with a bunch of people and tried to get healthcare moving again. Part of that was product cost and sourcing.”
Mitchell was already a twenty-three-year supply chain veteran at GE when he was offered the position. He had started working at the company while pursuing a manufacturing engineering degree at Boston University. GE had a training program for students that introduced them to supply chains in aviation, from production and quality control to process engineering. “Every six months you got a new role, so you get four to five years of experience in two years,” he says.
For the first decade at GE, Mitchell worked in the company’s aviation sector, first in Massachusetts, then in New Hampshire, then North Carolina. Around the same time, GE was pushing its Six Sigma philosophy to its leaders, leading Mitchell to work in finance, sales, and other areas of the business. During the process, he got insight into how important sourcing and procurement was to the supply chain.
Mitchell’s journey in developing supply chains through procurement brought him first to Shanghai, China for three years, Germany for four, and then India for three before returning to the US to work on supply chains for the power industry. “To go into a different country, with a different culture, and translate it into a local perspective, was invaluable. We really try to understand local requirements and operate locally,” Mitchell says. “Even though we’re a global player, we want to be a regional brand.”
GE Healthcare operates in more than 140 countries. Because of its global scale, one of Mitchell’s main concerns is maintaining the company’s reputation and adhering to quality across the globe. For example, while Germany has a more controlled and rigid approach to its processes, India has a more entrepreneurial and creative approach. On top of all this, each country has its own regulatory body that GE Healthcare has to


Congratulations to Tommy Mitchell
and his global supply chain team at GE Healthcare.
We’re proud to be a trusted supplier and partner for Tommy and others in the medical industry.
“We really try to understand local requirements and operate locally. Even though we’re a global player, we want to be a regional brand.”
accommodate. “We have about forty-five manufacturing sites within healthcare all over the world, in more than twenty countries,” he says. “That’s the biggest challenge—being global and yet maintaining the same standard in all those facilities.”
Another challenge is the conflicting pace of progress between the medical industry and the technology it uses. “We have a product that lasts more than twenty years, but the industry that makes those components changes every two to three years because it moves so much faster.” The key, Mitchell says, is product vitality, to drive product development cycles increasingly faster. Take an MR system for example. Instead of reinventing the entire system each time, GE Healthcare builds off a common operating platform and iterates improvements over the years. “With that iterative approach, we can incorporate technology faster and avoid obsolescence,” he says.
Perhaps the most exciting challenge is GE Healthcare’s commitment to developing technologies and solutions that enable precision health, the ability to diagnose exact issues and develop precision treatments. But before we can get to that point, Mitchell says, companies will have to find ways to reduce costs associated with machinery, such as precision imaging. “We’re fundamental in producing equipment that provides precision images,” he says. “We’re integral in designing and testing something. If you can’t produce it in volume at a reasonable cost, it doesn’t have the same impact. Precision health will be revolutionary, because it touches everyone.”




















































































































































wilbertplasticservices.com
866.273.1810
Mitchell’s responsibilities at GE Healthcare have only just begun, and in the following year, he will add material planning and logistics to his sourcing responsibilities. “We’re not just building widgets and trying to sell it with more features,” he says. “We’re trying to put a structure in place across the world that helps change lives.” AHL
By Roland Archer
With healthcare costs on the rise for another year, several major employers have been trying to find new ways to manage insurance and employee benefits— particularly for those that employ thousands of people growing increasingly frustrated with rising costs and a confusing marketplace.
To say this kind of directional change is necessary— not least of all from an HR standpoint—would almost be an understatement. A 2012 study by the Integrated Benefits Institute found that poor health costs employers $576 billion per year (compiling sick days, lost productivity, and medical expenditures), and as that cost continues to rise the average premium for employers has risen by nearly 20 percent in the past five years. What’s more, a recent report from the Kaiser Family Foundation notes that even when employers cover their insurance, employees are still picking up more of the cost.
There are opportunities for employees to save money, but it means a better understanding both of healthcare options and the marketplace. The healthcare market can be an overwhelming thing for even experts to try to understand, so American Airlines has decided it will take extra steps to make sure its workers understand what they need before forking over a chunk of their paycheck in the hope that if an accident or illness ever were to occur, the plan they chose would provide the appropriate coverage.
In 2019, American Airlines added a healthcare navigator to its employee benefit options, a lower core option deductible, domestic-partner coverage in the core option, and a new annual enrollment tool to help its employees choose the most appropriate medical plan for their needs.
The navigator, called Accolade, provides help to employees and their family members by helping them find in-network doctors and providers, identifying ways to help save money on healthcare expenses, and answering any questions and resolving issues related to healthcare bills.
On the prescription front, American Airlines is making use of Express Scripts to help employees fill short-term prescriptions at any pharmacy in the network and secure prescriptions for long-term or chronic conditions via mail-order service.
As consumers navigate an increasingly complex health insurance market, American Airlines simplified matters to provide savings for the nearly quarter of a million people it covers
Immediate savings are already available. American Airlines reduced its core option deductible by $500 for single employees and by $1,000 for families that it covers.
Besides that employee-friendly upgrade, the company is also pushing for change at local levels. American Airlines has joined Texas Instruments, Southwest
“Under Tom’s thoughtful direction, American Airlines is reimagining what healthcare looks like for today’s workforce and helping people live healthier lives, inside and outside the office.”
Airlines, and other employers in forming the Dallas-Fort Worth Business Group on Health, a coalition working on various healthcare issues. Together, the members provide coverage for more than seven hundred thousand employees and family members, and the group has to work hard and stay creative to ensure employees are satisfied with their options (and what they’re paying for them), Marianne Fazen, the group’s executive director, told The Dallas Morning News.
“The challenge is how to keep employees’ share of out-of-pocket costs low enough so they won’t stop using healthcare,” she said. “They resent all the cost-shifting, and the fear is they’ll get upset and go elsewhere to work.”
Tom Vertich, benefits strategy manager with American Airlines, has been an instrumental part of bringing plan changes to fruition for the company, which covers almost 250,000 members. His work in the field has given him insight to forward-thinking models. He’s worked as both a national accounts benefits consultant and as an HR benefits professional for three Fortune 500 firms, as well as being involved in various organizations dedicated to improving healthcare in the United States. He served on the National Association of Health Underwriters’ Health Care Reform Committee during the initial implementation of the Affordable Care Act, and was the president of one of its local Florida chapters. He also served as a local chapter president for the International Society of Certified Employee Benefit Specialists.
“American Airlines has been a long-standing partner committed to reducing healthcare costs and creating greater access to quality care for its employees,” says Hill Ferguson, CEO of Doctor On Demand. “Under Tom’s thoughtful direction, American Airlines is reimagining what healthcare looks like for today’s workforce and helping people live healthier lives, inside and outside the office.”
At American Airlines, Vertich is continually tracking data for employee health plans and managing the company’s pharmacy plan. He wants to ensure the data he collects is translated into something that is understandable to employees and that they take the opportunity to use the new navigation tools to make better decisions.
Whether American Airlines can poise itself to upset the healthcare model entirely and do away with middlemen like Amazon, Berkshire, and JP Morgan did in 2018 remains to be seen, but if the company’s new system improves user engagement, it’s a step in the right direction toward driving larger change in an industry that’s desperately in need of disruption.
Any positive change for employees should be recognized, but Fazen says the larger question remains unanswered.
“All of this is promising, and employers are glad to watch it happening,” Fazen told The Dallas Morning News of the coalition that includes American Airlines. “But we haven’t solved healthcare costs yet.” AHL

By Joe Dixon
Stephanie Schnittger’s comprehensive approach to helping manage Inova Health System’s finance department has made her a valuable team member for more than twenty years
As Stephanie Schnittger understands, it takes more than a command of numbers to help lead a major health system’s finance department.
The senior vice president of finance for Inova Health System began her career as an auditor for Ernst & Young LLP before joining Inova as its senior director of finance in 1997. Over the course of more than twenty years with the company, Schnittger worked her way through the ranks before assuming her current position in January 2018.
In that time, Schnittger has developed a holistic approach to managing her team that goes beyond simply looking at the company’s ledger.
“I think one of the things that make Stephanie stand out is that she has all of the accounting and financial chops, but she also really understands the operations of finance,” says Todd Stottlemyer, Inova’s former executive vice president and CEO of the Inova Center for
Personalized Health. “Also, importantly, she understands policy and healthcare’s regulatory framework. So, I think she brings a multifaceted perspective to anything she is involved in.”
Between 2015 and 2018, Schnittger and Stottlemyer worked closely together on the strategy surrounding the Inova Schar Cancer Institute. The Center is scheduled to open in the spring of 2019, and it will offer patients services such as imaging, proton therapy, oncology infusion, and more.
The project required Schnittger to leverage her financial, operational, and regulatory expertise as she helped develop a profitable, long-term business strategy for running the cancer center, while balancing that with tactical regulatory issues such as how changes in 340(b) pricing and reimbursement could impact the plan’s long-term viability.
In addition, throughout this process, Schnittger’s creative problem-solving tactics were essential to overcoming obstacles and delivering solutions that satisfied all stakeholders in the enormous project. This was particularly evident in developing the design for the future center’s cancer programs.
“A number of people wanted to go in a certain direction during this project, but they were not aware of some of the business and financial challenges associated with that approach,” says Richard Magenheimer, Inova’s CFO. “Stephanie felt that we should go in a different direction, and met with these folks numerous times and got them to come around to her solution. Not only that, they became active supporters of her approach.”

Stephanie Schnittger SVP of Finance Inova Health System
Stephanie Schnittger’s connection to major healthcare developments extends beyond her work at Inova. While her husband was working on Capitol Hill for then-minority leader—and future speaker of the house— John Boehner during the debate over the Affordable Care Act, Schnittger and her children were attending an event near Disney World. The debate in Washington DC prevented Boehner and Schnittger’s husband from attending the function as planned. Because she was pregnant with her fourth child at the time, Schnittger was unable to ride any of the rides, so her kids rode alongside Boehner’s wife, Debbie, and another colleague. “We have been living healthcare personally, politically, and professionally over the past many years,” Schnittger says.
Her collaborative style and willingness to challenge common wisdom have become hallmarks of Schnittger’s leadership approach to those who have worked with her.
“She brings a high level of courage to the table,” Magenheimer says. “Where other people might be hesitant to voice an opinion that differs from the boss, she’s very capable of holding her ground and articulating an alternative way of doing things. Good leaders admire that, and weak leaders are sometimes taken aback by that, but it’s something that I admire very much about her.”
Schnittger’s broad knowledge base, intense focus, and ability to multitask have allowed her to effortlessly handle a wide variety of responsibilities for Inova while also devoting time to her family.
“I think she’s incredibly productive with her time,” Magenheimer says. “Even while she’s commuting, she is actively involved in work-related matters. I see her accomplish things in a much shorter timeframe than what other people are able to do.”
Above all, Schnittger’s focus, collaboration, and expert decision-making are in the service of a greater mission, her colleagues say.
“I think she’s very committed to the mission of what we do in healthcare,” Stottlemyer says. “Oftentimes, it can be about balance sheets and income statements and cash flow statements, but I’ve also appreciated that she’s committed to Inova’s business of improving the human condition and to care for people.” AHL
BB&T is one of the largest financial holding companies in the US with assets of more than $222 billion, more than 37,000 associates, and more than 1,900 locations in 15 states and Washington, DC. Founded in 1872 and headquartered in Winston-Salem, BB&T offers a full range of consumer and commercial banking, securities brokerage, asset management, mortgage, and insurance products and services.
US Trust Institutional Investments & Philanthropic Solutions helps anticipate and address a nonprofit organization or institution’s needs and provides ongoing guidance on industry-wide best practices in governance, strategic resource development, and administration. Our dedicated team of specialists provides a mission-based approach to investment management, while adhering to the bank fiduciary standard.


WHEN YOU SUPPORT HEALTH, YOU PROVIDE HOPE We support your philanthropic passion

Stephanie Schnittger and her leadership at Inova Health System.
When you support health, you provide hope. At U.S. Trust, we’re committed to supporting people and organizations that play an important role in the communities where we live and work.

By Abhinanda Datta
Craig Guinasso is an integral cog in Genomic Health’s data security strategy
His innate desire to make a difference led him to the domain of information security. Now, as the chief security officer at Genomic Health, Craig Guinasso has found his calling.
His career began in law enforcement when he worked for ten years as a police officer for California State University Stanislaus. The university had just finished building new dorms and were advertising high-speed internet connections. Unfortunately, these high-speed connections were nothing more than unsegregated LAN connections. Soon, problems started to appear.
“The systems started going haywire. Students got into the academic systems and changed grades. I was asked to investigate these weird incidences. Back then, there wasn’t a lot of high-tech knowledge about institutional crimes or information security,” Guinasso says.
Fortunately for him, as a second generation security professional, Guinasso could seek guidance from his father, who worked for a variety of Silicon Valley companies, dealing with what we now know as information security.
“I had someone I could lean on and ask the right questions to, while being guided in the right direction,” Guinasso says. “I had the right tool set at the right time. I had been around law enforcement all my life and knew I wanted to be on the right side of the law. I was following my dad’s footsteps.”
As part of his ongoing career development, he started attending high-tech security and white collar crimes trainings and seminars (as they were called back then), while interacting with people in the private sector. These individuals were looking for people with a law enforcement background because of their forensic eye and reporting tactics. Soon, Guinasso found
his way into the private sector and eventually to Genomic Health.

“When the opportunity came along, it was very inspirational because aside from the work I had done in law enforcement, all of the information security work I had done so far was for companies where the data was just data,” Guinasso says. “If there was a compromise, there was a compromise. But here I am able to do things for people where it really matters.”
At Genomic, Guinasso provides a value proposition to the business that enables it to function in a secure way.
“My responsibilities are all things information security, and what that means is really doing vulnerability management,” he says. “I work very closely with the legal team negotiating master service agreements and reviewing the security aspect of contracts. I also work really closely with the other departments to help them evaluate new technologies and new systems so that those new ideas can be secured.”
Building relationships is important to Guinasso, and he likes to get involved in the earliest stages of an idea, whether it is changing a process, buying a product, or changing a vendor. He helps review every aspect of the new idea to provide the company with a quick security assessment. This ensures that they meet minimum security requirements and the employees get the user experience they expect.
Chief Security Officer
When he is not working to protect the illegal transfer of data, Craig Guinasso works with the Parent Teacher Community at the Redeemer Lutheran School as the president of the PTA.
“I spend a lot of time at my kids’ school,” he says. “I am involved in fundraising for the school and have raised $400,000 in the past 4–5 years through auctions.”
“Craig is one of those chief security officers that is truly blazing a trail, and this is especially true when it comes to cloud security,” says Sanjay Beri, CEO of Netskope. “We’re delighted to see this recognition of his leadership.”
Despite all of his accomplishments, a job as demanding as his is not without its challenges. For Guinasso, it is about keeping up with technology.
“Every day there is a new attack, and a new technology is created to defeat it,” Guinasso says. “It’s a cat-and-mouse game, and I would say that the number one challenge is to stay ahead of the game. Keep your technology up to date and patched and monitored.”
Guinasso’s leadership skills often harken back to his days in law enforcement.
“I had a sergeant who taught me everything I needed to know, and then just asked me to go out and do my job without getting him into trouble. I do the same,” he says. “I believe in hiring people that are better than I am, and once I hire them, I get out of their way.”
For the members of his team, Guinasso fosters an environment that is conducive to growing. With an understanding that the people on his team are critical to achieving the best security, Guinasso says he has a unique approach to training.
“There is a phenotype for security people. They can go out and get training and certifications, but that does not necessarily make them great security professionals. They have to follow their hunch. I have been good at enabling people’s abilities as opposed to simply training them,” Guinasso says.
He adds, “There are people who worked for me that have left for whatever reason. They call me and say they want to come back. It makes me feel good.” AHL
Druva’s industry-leading Data Management-as-a-Service platform unifies data protection, governance, and intelligence across enterprise data, delivering scalability and security, while reducing cost and complexity. Druva enables life science organizations, like Genomic Health, to establish central data compliance and governance practices, and helps prevent the mishandling of sensitive information like PII, PHI, and IP.
Defend against data breaches and cloud threats from hackers. Secure PHI, EHR, and other sensitive data in the cloud. Simplify compliance with HIPAA, HITECH, and more.
The Netskope Security Cloud helps organizations with safe cloud use by securing sensitive data like PHI across all your cloud services – from ones like Microsoft O ice 365, Box, Salesforce, and more, to shadow IT ones you may not know your employees are using.
Netskope is the leader in cloud security. We help the world’s largest organizations take advantage of cloud and web without sacrificing security. Our patented Cloud XD technology targets and controls activities across any cloud service or website and customers get 360-degree data and threat protection that works everywhere. We call this smart cloud security. To learn more, visit www.netskope.com
By Will Grant
Piyush Sharma shapes Alexion Pharmaceuticals, Inc.’s compliance program keeping patients’ best interests in mind
Piyush Sharma says going in-house was the turning point of his career. The current senior vice president and deputy chief compliance officer at biotech company Alexion Pharmaceuticals Inc. says that moving from a law firm where billing hours were the norm into a space where he genuinely felt he could help a company and its employees made all the difference in the world. Sharma has accumulated significant experience in the healthcare, oil and gas, and technology sectors, while becoming an expert in all things compliance, especially antibribery and anticorruption issues. Sharma’s talent for, and willingness, to build out extensive compliance projects has made him invaluable in multiple industries, but he’s happy to be back in healthcare. “For me, what I take pride in is helping the company and providing guidance and clarity to our employees,” Sharma says. “I want to make a difference by supporting the patients we serve and our employees.”
Sharma’s compliance work at Alexion is no small feat. The company does business in about fifty countries, and Sharma’s team is located all over the world. “It can be challenging to manage a remote international team,” Sharma says. “The way we succeed is ensuring that we are coordinated and connected at all times.” That means biweekly calls with his direct reports, a full compliance meeting once a month, and in-person quarterly compliance meetings. His next quarterly team meeting is in Zurich, Switzerland, and Sharma says it’s key to get everyone on the same page about new directives, goals, and initiatives. “We need to make sure we are speaking with one voice and have consistency in our approach, even when there are a lot of moving parts and the business is moving quickly,” he says.
Operating in a global capacity means it’s essential for Sharma to be in touch with regional and local compliance officers who are experts in their respective regions.
Piyush Sharma SVP & Deputy Chief Compliance Officer
Alexion Pharmaceuticals, Inc.

“I travel the world, but having a team in place where colleagues can be on the ground is very impactful,” Sharma says.
Although navigating Alexion’s roughly 2,500-person global organization may seem daunting, Sharma’s first in-house role at Pfizer included about eighty thousand employees when he left. “What we do here is very impactful and felt across the organization, much more directly than in a larger organization,” he says. “It’s part of what I like so much about working at Alexion.” This year, those key actions have included launching a new antibribery/anticorruption (ABAC) Program, which included new policies, procedures, systems, and trainings.
The new ABAC Program Sharma and his team deployed included building a transactional approval system from the ground up in partnership with New Yorkbased software company Lextegrity. The ABAC system implemented by Lextegrity has been user-friendly, engaging, accessible on multiple device platforms, and available in several languages. It has resulted in Sharma’s team looking for more opportunities to advance the global compliance program by incorporating reporting and predictive analytics.
Building out these programs is Sharma’s specialty, and it’s where he feels he’s able to be most effective. “For me, the biggest challenge is building a compliance program, but I think it’s also the most rewarding kind of experience as a compliance officer,” Sharma says. “Ultimately, you’re helping shape the culture of the company.”
Sharma says that in his past positions, as well as in his current role, he’s been fortunate to implement compliance programs in the best of circumstances: there’s the right tone from top leaders, management support, and appropriate oversight.
“I think the most successful compliance officers are the ones who are engaged and embedded within the business.”








































Lextegrity’s Integrity Gateway software mitigates fraud and corruption risks globally for leading life sciences companies.

www.lextegrity.com info@lextegrity.com
He says it’s that sort of forward-looking leadership that helps sustain and evolve the role of compliance as more than a department that the rest of the organization fears. “We’re working daily to shift the perception of compliance from the traditional policing role to a transformative one,” Sharma says. “We’re working with our business partners and stakeholders to support strategic imperatives, and we want to be seen as a business partner with a seat at the table.”
Once compliance is looked at not only as more than a function that puts on Band-Aids but also as a valuable contributing voice, that sort of paradigm shift has far-reaching and important reverberations, Sharma says. “Rolling out policies, procedures, and processes will always be part of the compliance function,” Sharma says. “But I think the most successful compliance officers are the ones who are engaged and embedded within the business, working seamlessly with stakeholders to support organizational objectives and strategy.”
Understanding the business and its people helps compliance officers transform a company’s culture into a competitive advantage for the business, Sharma says. This is especially true in the healthcare sector, where patients entrust their lives to companies such as Alexion. Because the stakes are so high, a healthcare company’s ability to deliver on its mission starts with its values and reputation. Sharma says that working in healthcare has given him a purpose, and he’s committed to helping his company make the largest impact it can, because lives literally depend on it. “Our drugs treat rare and fatal diseases,” Sharma says. “I am part of a mission to serve our patients, and I am on focused on what we can do, as a function and more broadly within the enterprise, to help the patient journey.” AHL
National, and even global, forces have an unmistakable impact on an executive’s work. Whether it’s a legislative change or an industry-disrupting technological breakthrough, executives must constantly adapt their business strategies to keep their company thriving.
36. Fabian Stone
43. Christopher Javillonar
46. Kate Proctor
52. Sylvia Tsengouras
56. Chris Bahrke
60. Tommy Comer
65. Angela Oakley
68. Renee Ennis
72. Michael Zaroukian
76. Robert Allen

Associate VP, Revenue Cycle and Health Information Management
Duke University Health System
Amid rapid changes in the healthcare industry, Fabian Stone says that revenue cycle leaders must face billing and payment challenges with a systematic approach to thrive
By David Levine | Portraits by Cass Davis
The long-standing practice of billing and collections is entering a new realm: revenue cycle management.
challenging. “Revenue cycle management is facing a set of challenges that require a thoughtful approach and leadership in response to consumer and market demands,” he says. “Leaders must understand how elements of clinical delivery impact financial performance.”
More than ever, this critical role in healthcare involves a delicate balancing act as revenue cycle leaders and their teams have to navigate a plethora of automated, regulated, and complex processes, while maintaining profitability for their organizations. And because more revenue is coming directly from patients, especially from those in high-copay or high-deductible insurance plans, revenue cycle leaders must seek new strategies for improving the financial health of their providers or hospital.
“At the end of the day, we get paid or we have to understand why we didn’t get paid,” says Fabian Stone, associate vice president of revenue cycle and health information management for Duke University Health System, a leading national academic health center in Durham, North Carolina. He oversees four departments—revenue, coding, documentation, and shares health information management—along with 420 direct reports. “Revenue integrity is the safeguard to protect our assets,” he says. Stone’s job is to protect and preserve that integrity. He says that revenue cycle teams spend money toward collecting payments from patients, educating providers on insurance policies, and appealing complex claims. But even with powerful management software and trained employees, maximizing profits can be
“For hospitals and health systems, the shift to value-based payment demands a relentless focus on improving patient outcomes and reducing total cost of care,” says Mark Colin, vice president and general manager of 3M Health Information Systems. “Under Fabian Stone’s leadership, Duke Health’s revenue cycle and health information management teams are meeting these challenges with innovative programs that safeguard revenue integrity and promote accurate outcomes data. We are proud to be Duke Health’s technology partner, and we look forward to our continued collaboration.”
One example of how changes in the healthcare industry have increased the importance of revenue cycle management comes from claims data, which Stone says is increasingly driving hospitals’ and physicians’ reputations. “The demand for quality measures, patient safety indicators, and patient satisfaction scores have made revenue collection about more than just collecting dollars,” he says. “Healthcare consumers rely on providers to improve their health, and healthcare providers do not turn away patients in need.”
Efficient processes for patients, providers, cash flow, and quality outcomes, he says, are contingent on incorporating a multilayered management approach, known by the acronym TECH—talent management, efficiency, cash flow, and habits.
“At the end of the day, we get paid or we have to understand why we didn’t get paid.”

The guiding principle of talent management is that people are an organization’s best resource. “Recruiting and keeping the right people for the right jobs is critical for success,” Stone says. “Revenue cycle needs people, such as medical coding analysts and clinical documentation nurses, who are active collaborators, quick learners, and sophisticated problem-solvers capable of adapting to change—these people are unicorns.” These employees also must be able to understand large data sets to educate physicians on insurance policies for improving reimbursement. For example, coders must be able to understand standard coding practices, quality measure guidelines, and payer-specific coding rules. But the right people are just one aspect of successful revenue cycle management, Stone says.
Revenue cycle leaders must also worry about efficiency. Organizations can enhance their efficiency by using technology as a tool for data governance to meet the goals and objectives of customers in quantifiable terms, Stone says. Technology can be useful in assessing data collection, claims submission, account processing, and automation. “A high level of efficiency begins and ends with accountable leaders who show the ability to change at a moment’s notice,” he says. “That flexibility will ensure adherence to regulations and mitigate risks that are associated with coding, billing, and records governance.” However, talent management and efficiency aren’t useful unless an organization can maintain its bottom line.
Tackling today’s challenges, while preparing for tomorrow’s.

Transforming health care from a system that treats disease to a system that improves health and wellness begins with accurate health information and payment. From improving efficiency of medical-records coding, to outlining success in value-based care, we help you tackle challenges in a fee-for-service world, while helping you thrive in value-based care.
It’s what we’ve been doing for more than 5,000 U.S. hospitals. It’s what we can do for you.
Get the details and read about results at 3m.com/his
Over 35 years of providing services to healthcare providers and payers
■ Provider Coding Support
■ Provider Document Integrity
■ Payer Coding and Consulting
■ Payer Nurse Reviews
■ Audit Services
■ HIM Management
■ Backlog Elimination/ Prevention
800.448.CODE (2633)
Stone says that declining revenue, tightening margins, and an increasing amount of bad debt are driving revenue cycle management teams to rethink how to stabilize cash flow and maintain profit. “Leaders must focus on understanding data from many sources, such as utilization trends, readmissions, and discharge dispositions,” he says. Also, leaders should provide stronger integration between clinical processes and denial processes—such as reviewing case types for prior authorization at scheduling, creating questionnaires at the operating room, and creating scheduling hubs, he says. This integration is essential to optimize payer relations, and it is at the core of developing policies that create a more cost-effective revenue cycle. Lastly, it’s important to step back from the nitty-gritty details and look at the bigger picture of the healthcare industry, Stone says.
Changing health policies require deeper understandings of the consumer experience to transform how a revenue cycle develops products, services, processes, and initiatives, Stone says. “This effort requires a human-centered approach for planning and implementation that guides staff toward becoming design thinkers who integrate the needs of people, the possibilities of technology, and the needs of the business together.”
Stone believes that an effective TECH leader must engage in performance monitoring and develop action plans to integrate people, processes, and
technology to come up with creative solutions to interdisciplinary challenges. Above all, Stone sees technology as a unifying solution to improve an organization’s talent management, efficiency, cash flow, and habits. “Leaders must guarantee the use of technology as the critical platform for tracking, automation, and interaction,” he says. “Technology is essential to improving both clinical quality and the revenue cycle performance and enhancing workflow.”
Stone’s faith in this approach stems from a long career in healthcare. He grew up in a small town outside Durham, North Carolina, and earned a bachelor’s of science degree in medical technology at Winston-Salem State University. He worked in a lab at the University of North Carolina (UNC) Hospital for a while, then took a sabbatical to study hospital management and obtain a master’s degree in hospital and business administration from Pfeiffer University. Back at UNC Hospital, he worked on practice management before moving into coding and compliance. Eventually, he “changed colors from Tar Heel blue to Duke blue,” and worked in several areas, including clinical documentation and health information management. He was named an associate vice president in 2012.
“Healthcare today is all about change, and organizations need leaders to manage that change,” he says. “This industry is highly regulated, and you have to mitigate all the risks that go with billing and records governance. A flexible and diverse workforce will allow you to manage change that is coming quicker and quicker.” AHL
By Will Grant
“I think acquisitions are fun.” Christopher Javillonar seems to have found the right gig, then. The general counsel for wheelchair and seating system design and manufacturer Permobil has overseen nearly two acquisitions a year since coming to the company in 2014. Permobil has continued to expand quickly, acquiring Ottobock’s OBSS and NUTEC custom seating business assets in the US and Canada as well as MAX Mobility in January 2018, Comfort Company in October 2017, and Prairie Seating in January 2017. Although the company recently celebrated its fiftieth anniversary, it shows no signs of aging as it continues to widen its geographic footprint and diversify its portfolio.
For Javillonar, approaching each acquisition with the right mentality is the first step in navigating what can often be a challenging process. “I don’t like to do things the same way just because that’s how they’ve always been done,” Javillonar says. “I like to look at a problem fresh.” That can mean a number of different things in the approach, but it almost always means a willingness to be flexible.
“Sometimes if we’re acquiring a company and it had a better template or contract, I don’t mind adapting and saying I’m going to take the best of any company that we come across,” Javillonar says. “If there's a better way, I’m about being adaptable and flexible as long as the overall impact is positive to the organization.”
Javillonar says that pride can often cloud decision-making during what can be a sensitive transition. Keeping both the acquirer and acquiree in mind as equal parts of the new organization is key, he says. “You have to be willing to set aside your own agenda,” he says. “What really needs to drive you are the questions, ‘Is this better for the company overall? Will this keep employees and the company safer?’”
Adaptability is also key for the legal team at Permobil, as Javillonar says the department is often required to wear more than just a legal hat. “We have to understand the business and that our role is not merely to find all the problems with what the business wants to do,” Javillonar says. “We need to find a way to help facilitate and make the business objectives a reality with the least risk possible.”
Permobil’s Christopher Javillonar challenges the status quo when helping the company acquire and integrate new businesses
In terms of minimizing risk, especially in such a heavily regulated industry, Javillonar says that Permobil makes his job fairly easy. “We’re fortunate to be working for this company that absolutely values quality in our products,” he says. “I tend to look at a lot of these risks like if this was your mother, father, or someone in your family that’s near and dear to you using one of our products, would you feel safe with them in that chair or using that medical device? For me, the answer is always yes.”
Christopher
General Counsel Permobil

Legal’s focus on adaptability is especially necessary when integrating a new company into the fold. Javillonar says that while acquisitions can often be long and taxing, it’s usually just the beginning of a successful integration.
The department’s role is not only to handle the nuts and bolts of the transition, but how to make the new extension of the company feel welcome. “We’re the legal department and we’re here to help,” Javillonar says. “People coming into the company during an acquisition need to cast aside previous thoughts of how the legal department worked and understand that we’re here to help facilitate and reach their objectives, not impede them. Now that we’re on the same team, let us know your objectives.”
Javillonar says that maintaining positive relationships with outside counsel is also a vitally important part of his role that he takes seriously. “I feel like that’s part of my job, to vet a lot of outside counsel so that we can immediately call upon them as needed,” Javillonar says. “Our outside firm becomes an extension of our team. They need to buy in to what we do and feel like they’re one of us.”
The fact that Javillonar has become an acquisitions expert is a testament to his own flexibility, having come from a litigation-heavy background. He says he still draws on that experience in his
“Sometimes if we’re acquiring a company and it had a better template or contract, I don’t mind adapting and saying I’m going to take the best of any company that we come across.”
in-house role. “In either role, you want to be indispensable to the organization,” Javillonar says. “You want the various business units to say, ‘We need legal’s input on this.’”
Transparency and communication are what keep his team running at peak performance, Javillonar says. And as Permobil continues to expand, he’s confident that legal’s role will be to continue partnering with the business. “The company has changed tremendously in my four years. I think that trajectory is going to continue in the next four years and beyond,” Javillonar says. “I look forward to helping it along.” AHL

By Jenny Draper
Legal leader Kate Proctor reveals how she navigates the regulatory matters of life and death

General Counsel
Hospice & Palliative Care
Hospice has been in the hot seat recently. Within the past few years, the US Department of Justice has amplified its review of claims for payment with an intense focus on hospice. In fact, the inspector general for the US Department of Health and Human Services, Daniel Levinson, addressed the issue directly in his keynote speech at the 2016 Health Care Compliance Association meeting. He announced his focus on three topics: physicians providing chemotherapy to patients who didn’t have cancer, the opioid crisis, and hospice.
“For a long time, hospice seemed like an island within the healthcare industry,” says Kate Proctor, general counsel at Seasons Hospice & Palliative Care. “Everybody would just understand why hospice was so important and why it should remain a Medicare benefit, but that has changed somewhat.” The massive increase in government scrutiny stems from hospice mirroring the uptick in healthcare spend. “Seasons Hospice has always been focused on patientcentered care,” Proctor adds. “Now we’re renewing our investment in that.”
Proctor joined the end-of-life care organization in 2014 as its first in-house counsel and took on the onslaught of new government regulations and payment reforms. Since then, her legal role expanded exponentially to handle employment risk management and more litigation in-house while growing the department as a business partner. The result: her legal team is helping Seasons lead the way for the highest standard of care across the healthcare spectrum.
“Our caregivers, nurses, social workers, chaplains, physicians, and aides are extraordinary,” Proctor says. “And people who work in hospice administration are a special type of person. They care passionately about what we do. It’s not just a business for them.” Proctor also

“Our company deals with life and death, and there are times where you are going to have to do the right thing for the patient regardless of whether you will be able to bill for those services under Medicare guidelines.”
acquired oversight of the quality department in January 2018, which she has married with risk management. For example, families complete a survey after a patient has died to monitor and ensure the highest standard of care beyond government-measured quality indicators.
Seasons supports about five thousand patients per day and about twenty-five thousand per year, with at-home care growing organically over two decades to house twenty-nine locations across nineteen states, thanks in part to a leadership team dedicated to innovation. Due to a high density of patients relying on Medicare and Medicaid—as high as 90 percent—Proctor credits the clinical team for developing a robust eligibility process to withstand increased government regulations. For example, three different sets of people, including multiple physicians, review each potential patient to reach a consensus before admission.
“Hospice patients need to have a prognosis of six months or less by the time they come to hospice, but physicians can’t tell the future,” Proctor explains. “If the hospice physician says a patient has six months to live,
but the government has a physician who disagrees, it’s essentially a battle of the experts. We developed multiple clinical resources and near constant training to help our physicians attempt to tell the future as closely as clinically possible.”
Risk management training is also a crucial tenet of Proctor’s compliance strategy. Since her arrival, training expanded from an annual compliance session to education across the workforce through a variety of mediums, from webinars and virtual classrooms to allstaff leadership training and in-person conferences. Discussion topics include government case studies to identify industry issues and in-house audit examples within its national network.
Today Proctor’s team is also envisioning a new care model based on hospice that’s interdisciplinary and treats the patient as a whole person while also reducing their reliance on high-cost emergency care. They often meet with hospitals, accountable care organizations, and insurance companies that are increasingly cost conscious and careful about preventing readmission.
In addition to her duties as general counsel for Seasons Hospice & Palliative Care, Kate Proctor also chairs the Seasons Hospice Foundation. The organization sponsors a children’s bereavement camp, called Camp Kangaroo, in about a dozen locations across eight states. Children who have been affected by a death in the family receive counselors, art therapy, and music therapy to help process grief.
The foundation also sponsors legacy projects, from a photograph to a video story, and its own version of the Make-A-Wish program. Proctor cites one last fishing trip, a family vacation to the Grand Canyon, and the visit of a Broadway star as examples of wishes the foundation has been able to fulfill.
“We’re devising new ways to provide palliative care to patients whether they are eligible for hospice or in a non-hospice context for chronic care management,” Proctor says. “We’re looking at how we can apply what we already know—how to manage pain and psychosocial issues—and create solutions for other healthcare providers.”
While she earned a juris doctor at Boston University after receiving a bachelor’s degree in history at the University of Wisconsin-Madison, Proctor launched her career at one of the only American firms with a dedicated hospice practice representing hospices all over the country. There at Reinhart Boerner Van Deuren, about 75 percent of her work was with hospice facilities, and she credits a firm partner for the advice she follows today at Seasons: “No is not the right answer,” she says. “We have to understand the goal and figure out how to get there together in a compliant way.”
Proctor’s dedication to find a solution to any problem stems from her steadfast commitment to patient care. “Our company deals with life and death, and there are times where you are going to have to do the right thing for the patient regardless of whether you will be able to bill for those services under Medicare guidelines,” Proctor says. “It is such a special time to be a part of somebody’s life and it’s important to make it as good as it can possibly be for both the patient and the family.” AHL
By Jeff Silver
Sylvia Tsengouras leverages her supply chain expertise and Fisher Clinical Services’ worldwide capabilities for the company’s clients
The complexity of clinical studies is mind-boggling. In addition to the scientific foundation of any particular hypothesis and the technical planning that underpins each inquiry, there are countless external factors that can impact their success.
Uncertainty surrounding geopolitical issues such as Brexit, for example, can impact factors like the accessibility and distribution methods of study medicines. Changes in associated import/export taxes can render established budgets obsolete. Expanding trials to multiple global study sites can introduce unanticipated rules and regulations that complicate supply chain and logistics strategies. Or simple delays in enrolling adequate numbers of eligible study subjects can create issues related to product expiration.
All of those complications occur in areas where Fisher Clinical Services excels. As a leader in clinical supply chain management, the company has the experience and expertise to handle nearly every conceivable inventory management, packaging, and distribution challenge associated with worldwide clinical trials that their clients might encounter.
Through its parent company, Thermo Fisher Scientific, Fisher Clinical Services has access to the resources and capabilities of Patheon, a contract development and manufacturing organization, which was acquired in 2017. In addition to more traditional supply chain management tasks, the company can address manufacturing needs, such as synthesizing
new drug formulations, creating stability studies, or developing new drug protocols.
According to Sylvia Tsengouras, Fisher Clinical Services’ senior clinical supply chain manager, effective supply chain management starts with five things:
• Preparing a strategic plan to develop and managing adequate inventory
• Implementing appropriate labeling and packaging designs
• Assuring flexible distribution
• Confirming an adequately programmed dispensing system
• Developing risk mitigation strategies for each component and stage of the study
However, companies often have multiple products in development at once, so they may not have the resources to support all these activities. Limited financial resources may make manufacturing on a large scale impossible; therefore, planning for limited quantities often becomes the first challenge.
“We have to forecast details down to the individual tablet to ensure adequate supply for all our clients’ study sites,” Tsengouras says.
For example, it may require one hundred sites to identify, screen, and enroll a total of fifty eligible subjects. Although not every site will enroll a subject, and others may enroll more than one, every site must have an adequate amount of supplies. Supply depots must have contingencies and additional supplies in place to distribute medications in a timely manner, Tsengouras says.

Sylvia Tsengouras Senior Clinical Supply Chain Manager
Clinical Services
“Regardless of their size, we help our clients get the best possible outcomes for their clinical trials—no matter what unexpected events might come up along the way.”
This is critical because delays in reaching enrollment targets can have ripple effects on a company’s supply chain. Extending a study by six months requires additional financial investment and can impact drug storage due to expiration deadlines and compliance with local regulations.
“We make every effort to anticipate any issue that might impact the clinical supply,” Tsengouras says. “It’s a matter of planning ahead, then thinking on your feet and acting efficiently to take quick action when necessary.”
To help ensure the accuracy of supply chain forecasting—everything from appropriate manufacturing volume to managing expiry dates—Tsengouras works with specialized internal teams that utilize simulation tools to develop various logistical scenarios along with the most effective solutions. That level of insight
is aligned throughout the company’s fully integrated global network, which includes Fisher Clinical Services experts who are familiar with regional regulations and compliance and have relationships with local customs officials. This provides capabilities to address nearly every possible contingency.
With all its experience and extended capabilities, she points out that Fisher Clinical Services can serve the needs of clients ranging from start-ups to pharmaceutical giants. For example, an emerging company consisting of a single team of scientists that has achieved positive laboratory and preclinical tests might need to convert a tablet formulation to liquid for trials with children, or to develop easy-open packaging for an elderly population.
On the other hand, a legacy company might want to redeploy internal resources away from compounds
that have already been in active development. Fisher Clinical Services’ offerings are able to handle manufacturing, supply management, packaging, labeling, and distribution to investigator sites. Tsengouras has collected years of experience dealing with challenges like these, but there are still some that stick out to her as particularly unexpected.
Years before she joined Fisher Clinical Services, Tsengouras faced one of the most challenging unanticipated issues of her career, she says. A massive flood destroyed the first floor of a packaging and storage facility, wiping out $1 million in supplies that impacted more than twenty ongoing clinical programs. She was able to save about $2 million to $3 million of her company’s product, which she had moved to a secure facility and tested for integrity and purity. The remaining supplies were available for use within a month.

Now, one of Tsengouras’ newest challenges is adhering to the stringent temperature requirements of new biologic compounds. This requires ensuring materials remain refrigerated or frozen within a narrow window of variation. “Through extensive planning, employing specific types of shipping containers, knowing the conditions we’ll encounter, and constant monitoring, we can maintain and protect the integrity of every shipment from endto-end,” Tsengouras says.
“Regardless of their size, we help our clients get the best possible outcomes for their clinical trials—no matter what unexpected events might come up along the way,” she says. AHL
At Fisher Clinical Services, we work as an extension of your team to ensure clinical trials and distribution plans can adapt quickly and are executed flawlessly. We strive to foster our trusted partnerships in order to give clients flexibility, dependable support, insight and expertise when they need it. We do all of this to eliminate complexities, ensure compliance and mitigate risk across the supply chain.
Contact us.
fcsinfo@thermofisher.com
By Lori Fredrickson
As increased demand creates new changes to the long-term care sector, Chris Bahrke is finding ways to scale for growth
Changes in the billing and reimbursement landscape amid an increased demand for long-term care have forced health service providers to navigate a host of new challenges across the managed care and commercial insurance space. And for providers in the postacute space, says Chris Bahrke, the key to managing those challenges is to look at where they’ve already occurred within the industry.
“We’re seeing a very unique progression from the acute space to the postacute space, where the same processes that have been occurring in that sector are now migrating to the postacute sector,” explains the vice president of revenue cycle at the Brentwood, Tennesseebased provider Diversicare Healthcare Services. “There is a need to now implement the revenue cycle from the acute space and apply it to the postacute care sector.”
When Bahrke first joined the organization in 2011, that was what he set out to do. Bahrke is no stranger to navigating periods of intense change—having worked for eight years as a manager at Arthur Andersen starting
in the mid-‘90s, where he implemented large-scale enterprise planning systems for various clients. He was forced to rethink his own career goals after the company was indicted amid the Enron collapse in 2002. This landed him in Nashville, Tennessee, where he worked for several years consulting with various healthcare organizations, which led him into designing and implementing payer compliance-based systems in the acute care space.
Working amid the changes taking place there is what led him to the postacute space, where he recognized there would be a need for his skill set. “I knew there would be a need at Diversicare to create new processes to drive scalability and create cost efficiencies because of reimbursement pressure; the introduction and growth of commercial insurance products; as well as the challenges that all healthcare providers face around payment reform,” Bahrke explains.
He adds that traditional postacute reimbursement methods had previously been very simple—they were per diem and all-inclusive, and most of the payers were government-based. But as commercial insurers have entered the postacute space, reimbursement and denial management have become more complex, with a shift away from per diem-based reimbursements. And amid that complexity, demand was rising, particularly at Diversicare, which was looking to double its size when Bahrke arrived at the company. To do that, Bahrke needed to find scalable ways to ensure that goal could be achieved.
His biggest initiative for the company was designing and developing a central billing office. “What that did was to enable us to acquire new centers without having to add resources on a one-to-one

Bahrke VP, Revenue Cycle Diversicare Healthcare Services




basis,” Bahrke says. The company would soon see the benefits of this project.
During an acquisition of a portfolio of twenty-two centers—nearly a 50 percent increase to its existing portfolio—Bahrke set out to find vet software vendors that would help them to streamline the process. After settling on PointClickCare, he worked to make sure that they were aligned on a methodology going forward. “I’m a big believer that we need to fit the process with the software,” Bahrke says.
Working under a tight timeline, with forty-five days to implement the first eleven new centers and then another thirty-day timeline to implement the remaining centers, Bahrke and his team worked with PointClickCare to implement a solution for a new billing platform. Once that was up and running, he worked closely with PointClickCare to adapt it further to their needs, particularly around the month-end close process, and he has moved on to transitioning their other centers on to that the PointClickCare platform.
“A renewed focus for PointClickCare is to ensure our customers’ business processes and systems are tuned to deliver the most value,” says Russ DePriest, PointClickCare’s senior vice president and general manager for skilled nursing. “We measure these efforts against days sales outstanding, and early returns are very encouraging.”
Throughout that process, Bahrke continued to work on enhancing the central billing office, making sure that the team members stationed there had the solutions they needed. And to do that, he focused on having collaborative discussions with his team, making sure that everyone felt involved in decisionmaking and was able to offer feedback. “I strive to not make decisions in a vacuum. I’m a big believer that if you make your team part of the solution, they will want to make a difference for that solution and the path to the solution will be accelerated,” Bahrke says. “That was a big part of our success.”
“I strive to not make decisions in a vacuum. I’m a big believer that if you make your team part of the solution, they will want to make a difference for that solution and the path to the solution will be accelerated.”
As other challenges require alternative new solutions, he continues to drive those collaborative discussions, both with his team members and with payers. “We’re learning to make sure that we’re clearly delineating with our commercial payers how we define a care level, and to clearly define exclusions and carve-outs to make sure that our contract rates are in line with market expectations,” Bahrke says.
He adds that insurers are learning more now about the postacute sector because they’re less familiar with it, leading to some confusion in contracts. He’s continued to implement changes using new technology, working with different vendors to develop payer compliance software that helps Diversicare identify services provided to patients, as well as designing and creating new reporting services. And as the company continues to expand and add other new centers, he’s comfortable that they now have the infrastructure to support that long-term growth.
“Just getting us to a point where we can utilize technology and change processes to drive efficiency has been one of the
biggest things we’ve done,” Bahrke says. And, knowing that he has team members who are part of that process and are comfortable coming to him with their opinions and feedback will be critical to that growth as well, he says. “If they want it to succeed, it’s going to succeed,” Bahrke says. “I have a great team who supports me, and I can’t do it without them.” AHL
PointClickCare Technologies Inc. is helping more than fifteen thousand long-term and postacute care (LTPAC) providers meet the challenges of senior care by enabling them to achieve the business results that matter— enriching the lives of their residents and patients, improving financial and operational health, and mitigating risk. PointClickCare’s cloud-based software platform is advancing senior care by enabling a person-centered approach to care, connecting healthcare providers across the care continuum with easy-to-use, regulatory-compliant solutions for improved resident outcomes, enhanced financial performance, and staff optimization. For more information on PointClickCare’s ONC certified software solutions, please visit pointclickcare.com.
Phone: 800-277-5889 Email: info@pointclickcare.com
Tommy Comer of Commonwealth Senior Living focuses on finding the best people for the company’s elder care communities, regardless of their professional experience
By Clint Worthington

Tommy Comer Chief Human Resource Officer

For years, the elder care industry has struggled with a difficult hiring landscape—by the year 2030, seniorliving communities are expected to experience a shortage of 2.5 million workers across the country. It’s a daunting human resources challenge, but Tommy Comer, chief human resource officer for Charlottesville, Virginia-based Commonwealth Senior Living, has found innovative ways to address those shortcomings. Born from his passion for supporting and developing frontline employees, Comer’s solution is simple, yet elegant—provide enticing incentives for interested job seekers, then give them training and experience once they’re on board.
His passion for professional development started long before Commonwealth, when he was a twenty-yearold worker at a big-box retailer. When his supervisor quit right before the holidays, Comer approached his manager and volunteered to take over those duties right away. After working in human resources for other industries for eleven years, he joined Commonwealth in 2014 to develop the company’s HR department.
When Comer first came on, the biggest challenge was creating an HR department for an organization that had existed for twelve years without one. His first move was to visit Commonwealth’s communities, ask the employees questions, and gather data. From there, Comer modernized handbooks, updated job descriptions, and removed unattractive perks from frontline positions, such as not being able to take a vacation in your first year of employment. Overall, though, Comer worked to disrupt the top-down, corporate-driven decision-making that typified Commonwealth’s culture, in favor of something that made the frontline employees feel more valued.
Even with all these changes, however, Comer recognized the inherent challenges of hiring for senior-care communities, even ones as attractive as Commonwealth. “It’s no secret that the hiring landscape is extremely challenging,” he admits, noting that workers need to have a certain level of rigidity in their schedules, and be willing to work the stressful hours required of senior care. Although the ideal candidates would be certified nursing assistants, there aren’t enough nurses to take all the positions available, Comer says.
“We want good, kind-hearted people who want to take care of residents. Other than that, we’re willing to look at anything.”
One of Commonwealth Senior Living’s more intriguing and fun initiatives, Comer says, is the Commonwealth Cares Golf Classic, a charity golf tournament designed to raise money for the company’s employee assistance fund. Now in its third year, the Commonwealth Cares Foundation has raised about $500,000 to help employees deal with unexpected financial emergencies. Aside from taking care of Commonwealth’s workers, Comer loves that the tournament forges connections between executives and frontline employees. “Hearing our employees’ stories is an eye-opening experience,” he says.
Given these challenges, Commonwealth takes the novel approach of opening their qualifications to people without senior-care experience. For Comer, the most important attribute of a senior-care worker is someone who has “the behavior and traits of a great caregiver,” as well as the interest. To that end, Commonwealth seeks out interested workers, regardless of experience level, and trains them as needed to perform the duties of senior caregivers.
In keeping with his “hire-for-heart” approach to professional development, Comer has several initiatives in place to bring passionate caregivers into the fold, even when they lack the necessary experience. For example, workers benefit from an active referral program that rewards them for bringing other caregivers to Commonwealth, which pays them persistent bonuses the longer their referral stays at the company. He has also instituted a program in which the company pays for worker training, including a forty-hour personal care aid course. That kind of training can often be a barrier for prospective employees, Comer says. “It usually means money spent and missed work for those people,” he says.
“There are simply not enough ten-year veteran certified nursing assistants walking around—we have to be patient.”
The company has also been experimenting with hiring nurses from other countries, including Jamaica, and bringing them to Charlottesville, offering them international work sponsorship opportunities. “We want good, kind-hearted people who want to take care of residents,” Comer says of his workers. “Other than that, we’re willing to look at anything.”
Comer’s work has yielded impressive results, leading to dramatically improved hiring speed and a modest decrease in turnover—doubly admirable given the industry typically sees a 50–60 percent turnover rate. However, these hiring measures have occasionally met some small moments of adversity. “There are some family members who get concerned about relatively inexperienced caregivers,” Comer says. However, he tries to educate stakeholders about the realities of the world we live in. “There are simply not enough ten-year veteran certified nursing assistants walking around— we have to be patient.”
At the end of the day, these novel hiring initiatives are part and parcel of Comer’s HR philosophy, which stresses the need to be “approachable, trusted, but full of brutal honesty.” To be a leader in human resources, Comer says, “you have to have some courage, and be willing to say what has to be said regardless of your audience.” It’s an intense but lonely job, one which requires individuals to understand the business and connect the big picture with a comprehensive HR strategy. And one Comer is up to challenge of doing. AHL
By Jeff Silver
Angela Oakley is confident that clear and understandable financial statements will help Mental Health Center of Denver develop solutions and partnerships that are just as innovative as its treatment programs
Mental Health Center of Denver (MHCD) is one of seventeen community mental health centers in Colorado, but it stands out as a leader in offering innovative, holistic programs for mental health and overall well-being.
Its Dahlia Campus for Health & Well-Being offers therapy and mental well-being programs, including a four-acre garden and farm space that’s open to the community. It offers an aquaponics greenhouse and 46,000 square feet of indoor therapeutic, classroom, play, and community gathering spaces. Skyline Academy is a day treatment and education program offered through the organization. In addition to individual and group therapy, Emerson St. for Teens & Young Adults offers free public workshops in creative writing, music, art, yoga, financial literacy, cooking, computer skills, as well as general education and employment support.
In spite of such progressive and groundbreaking approaches to mental health services, MHCD was less adept when it came to understanding its own finances. In fact, when Angela Oakley joined the organization as chief financial officer, she discovered that many leaders in the organization didn’t understand the financials.
“More than one person told me that our financials were a mystery,” Oakley says. “They didn’t have any understanding of what happened to money after they sent it to the office.” Another individual described getting a headache from looking at the highly detailed monthly statements—and Oakley herself was confused by many of the entries, some of which were accounts named for twenty-year-old grants that no one could remember.
These were important stumbling blocks. MHCD operates on a 2 percent margin and needs to be able to spot financial issues and respond to them quickly, appropriately, and effectively.
To make the numbers more accessible and more meaningful to daily operations, Oakley simplified their presentation to three pages each month—an income statement, a balance sheet, and a rolling forecast through the end of the year. Instead of hundreds of accounts, the each document covers just seven categories each of revenue and expenses.
She also worked with the IT team to create an online Team Profit and Loss tool, where program managers and higher level leaders can gain controlled access to more detailed statements arranged by service groups.
“Financial information needs to be clear and understandable so that readers can grasp the details—and their implications—immediately,” Oakley says. “Mystery isn’t a good thing when it comes to financials.”
Her simplified reports and efforts at basic financial education produced immediate results. Oakley
Angela Oakley CFO Mental Health Center of Denver

says that financial discussions are more interactive and productive, and that staff respond with more informed questions. In one instance it was discovered that a particularly important contract was not paying as much as expected. “I couldn’t believe how creative staff ideas were for addressing the shortfall,” she says. “We ended up identifying great opportunities, renegotiated the contract, and met budget for the year when we we’d been on track to miss it by a significant amount.”
One of Oakley’s other priorities is developing alternative funding sources. Currently, 75 percent of MHCD’s revenue relies on state and federal funds, 62 percent of which comes from Medicaid. Funding is further complicated by the fact that MHCD’s innovative programs frequently fall outside the requirements of traditional mental health reimbursement, which is typically bound by a limited number of in-office visits.
Due to the uncertain nature of some of its funding, MHCD nurtures its relationships with various foundations, grants, and relationships that provide alternative sources of revenue. Sanderson Apartments,
a permanent supportive sixty-unit tax credit housing project that was built with an equity partner that owns nearly all of the project, is one such partner.
Such progressive approaches often attract other interested parties. A local church contacted MHCD about the possibility of developing Glenarm Commons, another forty-eight unit tax credit project identified in downtown Denver. Based on MHCD’s efforts around faith and spirituality, The Rose Community Foundation also awarded a $30,000 grant to fund work on the Capacity Building to Assist Faith Communities Working with Refugees and Immigrants project.
Working with commercial insurance providers, which currently account for only 3–5 percent of revenue for community mental health organizations, is another funding source with tremendous potential. The challenge is convincing them that long-term programs that utilize intensive, high-level services that extend beyond a limited number of visits for therapy produce positive and cost-effective outcomes.
“On paper we look expensive,” Oakley acknowledges. “But we provide exceptional care that has tremendous
value to the community, reduces hospital visits, and lowers insurers’ cost of care over time.”
She leverages MHCD financials to help tell that story to prospective companies in black and red. The numbers help demonstrate how initiatives like the organization’s teen suicide prevention program saves lives and money, even though they don’t meet standard criteria for being billed to Medicaid.
“Commercial insurers are very interested in our approach, but it’s going to require more education efforts on our part to create a new type of contract that’s not based on the traditional rigid parameters for care and treatment,” Oakley says.
These are just some of the challenges she faces on a daily basis. In addition, the state’s Department of Health Care Policy and Financing, which is responsible for administering Colorado’s Medicaid and Child Health Plan Plus programs, has changed to value-based funding, as well as how it calculates payments.
But Oakley remains optimistic. “I’ve worked in finance for more than twenty-five years,” she says. “If we can maintain a clear understanding of the financials, I’m confident they’ll lead us to creative solutions and help us recruit like-minded partners along the way.” AHL
Citywide Banks is a Colorado-focused community bank committed to delivering responsive service, local expertise, and comprehensive financial tools for Colorado businesses, healthcare organizations, and families. Visit citywidebanks.com to learn more. Citywide Banks is a member FDIC and an Equal Housing Lender.

KeyBank is proud to support Mental Health Centers of Denver.
Combining a holistic approach with deep industry expertise, Key Healthcare helps nearly 10,000 organizations, practices, and facilities across the U.S. stay competitive while delivering the highest quality care.
See what a healthy dose of tailored, strategic solutions can do for your practice. Learn more at key.com/healthcare.

Since 1963, Citywide Banks has been committed to finding ways to positively impact our Colorado communities. For us, it’s about supporting powerful local causes like mental health wellness, and creating a dynamic banking experience that will continually evolve to meet the changing needs of our customers.
KeyBank ’s strong focus on healthcare allows our dedicated teams to provide comprehensive solutions, industry expertise, and unique insight to our clients on the issues and challenges faced by healthcare providers. Melissa Whitmer commends Angela Oakley for her leadership and vision and the difference that she has made in the healthcare community.
By David Levine
TriCore Reference Laboratories wants to boost the lab’s role in healthcare, and chief financial officer Renee Ennis is helping drive that transformation
TriCore Reference Laboratories is striving to become more than merely a lab. Instead, TriCore thinks of itself, as it says on its website, as a “clinical information company offering expertise in population health management and targeted intervention.” Based in Albuquerque, New Mexico, TriCore performs a full range of laboratory testing, under the direction of more than fifty pathologists and scientific directors, for healthcare providers throughout New Mexico. But, as Renee Ennis, TriCore’s chief financial officer, explains, it is repositioning itself to do so much more than that.
“The clinical lab has traditionally played a background or support role in the overall healthcare landscape. It is usually located in the basement of the hospital and is an afterthought, if you will, for most of
the care continuum,” Ennis says. “We are focusing on bringing the lab to the forefront. We want the lab to have a seat at the table to positively impact that overall care continuum.”
The force that is driving that transformation, she says, is lab data. “We have an immense amount of longitudinal patient lab data,” she says. “We service the three largest healthcare systems in New Mexico. If your insurance coverage changes, or if you go from one system or hospital to another, or your physician changes, we still have all your lab data.”
Any physician therefore can retrieve a patient’s entire lab record for any work done at TriCore. “This longitudinal patient view provides a stronger, more meaningful clinical insight to physicians, driving better
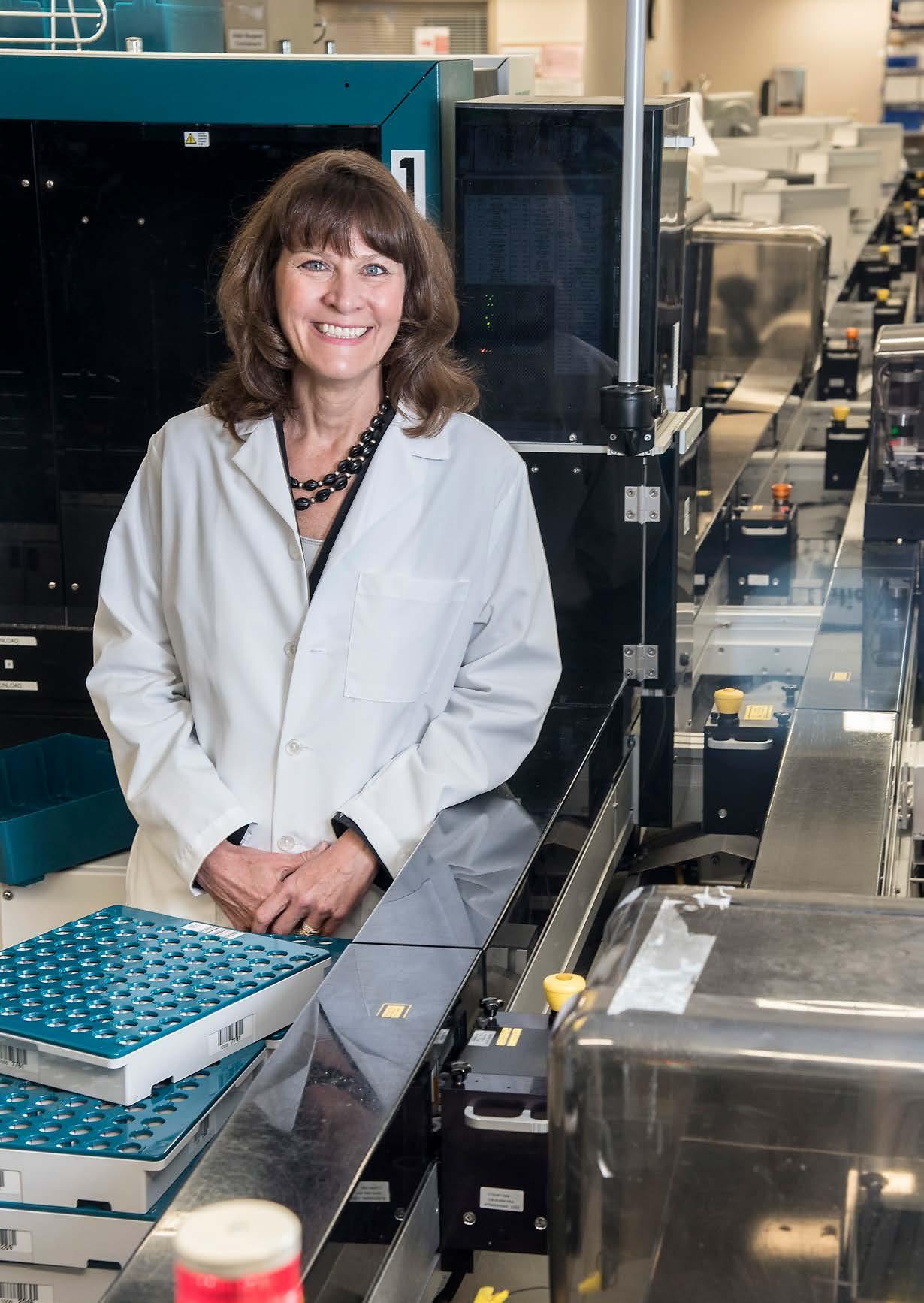
outcomes for patients, making life easier for providers, and hopefully reducing the cost of healthcare because physicians won’t be repeating previously performed lab work,” Ennis says. “In addition, clinicians can be alerted to gaps in care when patient labs are compared to standard guidelines of care.”
Ennis has a bachelor’s degree in finance. While working at a lab in Phoenix in the 1990s, she earned an MBA in healthcare management from the University of Phoenix. Then, she moved to a lab in Las Vegas to work as controller before she was recruited by TriCore to be their chief financial officer in 2004. In 2014, she moved to a large health system in New Mexico to be vice president of revenue cycle, then was promoted to CFO of the system, before rejoining TriCore in April 2018 to help lead the transformative changes it was looking to make.
The company’s transformational strategy, about five years in the making, was driven by changes in the healthcare payer landscape. “Lab work is transactional. The doctor orders the test, the patient has the test done, we provide the results. That works in a transactional or fee-for-service system,” she says. “As healthcare shifts to a value-based system, the focus is on population health and value-based reimbursement. We think the lab can help by providing actionable insight based on the vast amount of data produced by the lab work we perform.” Lab results account for about 70 percent of the data physicians use to make a diagnosis. “If we harness our data effectively, it has the potential to help providers make better decisions for individual patients and help health systems and payers make strategic decisions to serve a population’s healthcare needs.”
The rest of the lab industry is aware of this trend, she acknowledges. “There is definitely a movement within the industry in this direction, but others might not be moving as quickly as we are,” Ennis says. “As a leader in this transition, I think a lot of eyes are on what we are doing and how we are doing it.”
To understand how TriCore is accomplishing this, visualize a pyramid, Ennis says. “The base is what we call Lab 1.0, our foundational business, producing high-quality testing and results. That is our core business, what we do great.” One level up the pyramid and
“We are focusing on bringing the lab to the forefront. We want the lab to have a seat at the table to positively impact that overall care continuum.”
building on that foundation, the company is diversifying and generating other revenue streams by establishing and running labs in other facilities, effectively outsourcing TriCore’s management capabilities to hospitals, she says. For further diversification, they also created the TriCore Research Institute, leveraging TriCore’s expertise in new-test development and partnering with in vitro diagnostics companies to conduct device trials.
The third layer of the pyramid, Lab 2.0, is the transformation layer. “This is where the lab has a seat at the table with other disciplines,” she says. TriCore recently acquired the Rhodes Group, a laboratory IT company that has developed the technology infrastructure to harness the data TriCore generates and transform it into valuable information for TriCore’s healthcare partners.
One new value is “diagnostic optimization,” or turning that data into actionable insights for individual care and population health. For example, the company is working with a major payer in New Mexico to notify them about women in their plan who are pregnant.
“Our chief medical officer was reading a study that showed a significant number of women find out they are pregnant from lab testing done at an ER,” she says. “Women go in for some condition and the lab finds out they are pregnant before anyone else. If no one follows up, the only time the insurance company finds out is when she has the baby. At that point, it’s too late to intervene and ensure the mother gets proper and timely prenatal care.” TriCore now communicates with the insurer early. Then, the insurer can then connect the mother with care coordinators who will support her in her prenatal care.
Ennis says her role as CFO has changed as much as healthcare itself over the past 10–15 years. “Originally it was about producing and analyzing financial statements, sitting behind a desk and crunching numbers,” she says. “Today, you can’t succeed just by producing financial reports. I am out there peeking under the sheets, looking around the corners, using critical thinking skills, and becoming more of a strategic partner to the CEO and executive leadership team.”
It’s a change she relishes. “It’s more fun. I absolutely love it,” she says. “TriCore celebrated its twentieth anniversary in 2018. We are all excited about that, the growth we have experienced over the past twenty years, and we are really excited about seeing what the next twenty years look like.” AHL


By Russ Klettke
Dr. Michael Zaroukian and Sparrow Health System show how IT can make for healthier patients and balance sheets
The holy grail of US healthcare modernization is to improve patient outcomes while reducing costs by decreasing nonvalue-added care. On at least three fronts already, Dr. Michael Zaroukian has recently overseen and reported on three examples where Lansing, Michigan-based Sparrow Health System has achieved that difficult goal.
Zaroukian is a practicing general internist and board-certified clinical informaticist who collaborates with other healthcare and IT professionals to analyze, design, implement, and evaluate solutions that support transformational improvements in healthcare quality and value. As Sparrow’s vice president, chief medical information officer, and chief transformation officer, Zaroukian is well positioned to lead programs to improve the effective use of EMRs and other health information technology (HIT). In fact, Sparrow was recognized in October 2018 by the Health Information and Management Systems Society (HIMSS) with the 2018 HIMSS Davies Enterprise Award for three HIT use cases that dramatically improved patient outcomes.

Dr. Michael Zaroukian VP & Chief Medical Information Officer & Chief Transformation Officer Sparrow Health System
Zaroukian’s leadership in HIT helped Sparrow deliver key improvements in care and value with information and technology. But, Zaroukian is clear in his view that the successes in each case depended on having an organizational culture that embraces excellence and change—and leverages information technology as a valuable tool.
While street use of opioids is being treated as a national emergency, complications from overuse of physician-ordered opioids in hospitalized patients is also a problem, one that requires a different approach. Without ongoing awareness of other sedating medications a hospitalized patient may be taking, drug interactions or increasing an opioid dosage can cause some patients to experience respiratory arrest. If this occurs, it requires clinicians to rescue patients with Naloxone, an opioid antagonist.
“We want to do all we can to keep opioids from harming the patients we are trying to help,” Zaroukian says. “We do this by using information technology to promote respiratory depression risk assessment and intervention before Naloxone is required.”
Dr. Zaroukian says this is done by providing clinicians with EMR-integrated tools to automatically calculate a patient’s risk of respiratory depression based on EMR-recorded information, including their respiratory rate and oxygen levels. Sparrow clinicians employ the Michigan Opioid Safety Score (MOSS), which incorporates assessments of health risk, respiratory rate, and level of sedation to determine the risk of respiratory depression and to provide guidance regarding more intensive monitoring, modification of opioid dosage, using alternate pain management strategies, or getting direct physician input. “MOSS enables nurses to assess patient risk, providing a score and actionable decision support when certain risk thresholds are exceeded,” he says.
Sparrow reports that Naloxone rescue therapy is down by half, reducing patient length of stay, morbidity, and related costs. “This is a one example of why our caregivers are increasingly sold on the value

of our EMR and HIT. It’s a three-step process to transform a healthcare organization,” Zaroukian adds. “First, we provide them with HIT that works. Second, we help them use HIT pervasively and well. Third, we build on this to hardwire EMR-integrated best practices to truly transform care. We look at the data, find out where gaps exist, then use the data to identify and implement solutions that work.”
Blood and platelets are expensive and in short supply, yet about 35 percent of blood transfusions and 60 percent of platelet transfusions are deemed medically unnecessary. “Although reducing overall transfusions is an important goal, in emergency situations, such as at our Level I trauma center, seconds matter and rapid availability of multiple units of blood products is essential,” Zaroukian says.
Sparrow recognized that overuse of red blood cell (RBC) and platelet transfusions was a significant problem, working to address this through a
multidisciplinary project that replaced stand-alone blood product orders with evidence-based, guideline-compliant order sets, EMR-integrated clinical decision support, and compliance reports that encouraged transfusion ordering only when appropriate indications were documented. The organization also discouraged ordering more than one unit of RBCs in nonemergency situations. Provisions were also made for one-click ordering of emergent and massive transfusions when necessary.
Dr. Michael Zaroukian collaborated with Chris Nemets, Sparrow’s chief nursing informatics officer, on its CAUTI initiative.
Four-and-a-half years after implementation, RBC transfusions have decreased by 32 percent, while platelet transfusions have dropped by 25 percent. From a cost standpoint alone, that has amounted to $35.9 million in savings related to the purchase, administration, and costs of complications of blood product use.
“This initiative has also saved twenty-seven thousand hours of caregiver time that would otherwise have been spent in preparing and administering transfusions that were not medically necessary,” Zaroukian says. “Sometimes less is more when it comes to healthcare.”
“We look at the data, find out where gaps exist, then use the data to identify and implement solutions that work.”
Use of urinary catheters is necessary for millions of patients. But about five hundred thousand catheter patients suffer infections from their use each year, and of that group thirteen thousand die of related infections. Reducing catheter-associated urinary tract infections (CAUTI) draws from a strategy that relied on people and processes, informed by data. “Our goal was to remove catheters that are no longer medically necessary as soon as possible,” Zaroukian says. “With our CAUTI rates increasing for several years, we had to figure this out.”
Led by Chris Nemets, Sparrow’s chief nursing informatics officer, teams researched timely catheter removal protocols for patients slated for short-term catheter use (forty-eight hours or less) and for those needing longer-term catheters. When physician-facing protocols did not yield improvements, nurses volunteered to take the lead on catheter management and timely removal. To succeed, they needed what the EMR could provide: data on catheter use, tools for documenting catheter-related information, and clinical decision support to promote timely removal. They built new EMR protocols and used data reports to achieve an 81 percent decrease in CAUTI, from fifty-two patients in 2014 to ten in 2018.
“This was a matter of nurses and doctors working together, with nurses empowered by data and protocols to make decisions on catheter use and removal,” Zaroukian says. “It also helped us to avoid $1.1 million in CAUTI-related costs, with more than $300,000 per year in savings.” AHL
HIMSS is a global advisor and thought leader supporting the transformation of health through information and technology.
As a mission driven non-profit, HIMSS offers a unique depth and breadth of expertise in health innovation, public policy, workforce development, research and analytics to advise global leaders, stakeholders and influencers on best practices in health information and technology Through our innovation companies, HIMSS delivers key insights, education and engaging events to healthcare providers, governments and market suppliers, ensuring they have the right information at the point of decision
www.HIMSS.org
By Charlene Oldham
Robert Allen leads CHA Hollywood Presbyterian Medical Center’s leading-edge strategy to create a holistic approach to health and healthcare
Given its position near the nexus of Sunset and Vermont Boulevards in Los Angeles, CHA Hollywood Presbyterian Medical Center serves a highly ethnically and economically diverse population—providing care for the city’s homeless population, the Hollywood elite, and everyone in between. So it seems fitting the medical center is part of CHA Health Systems, an equally diverse parent company that has grown from a single obstetrics clinic in Seoul, South Korea, into an expanding network of hospitals, fertility clinics, wellness centers, and research facilities that employ about ten thousand people around the world.
“It’s a rather global organization,” says Robert Allen, president and CEO of CHA Hollywood Presbyterian Medical Center.
As CHA’s primary United States outpost, the medical center can contribute to research efforts that require a diverse pool of subjects. The staff can also collaborate with colleagues around the world to adapt and adopt best practices to fit their settings.
“So we sit in on phone calls with people from Korea, Australia, Singapore, and the United States, and we share ideas to see what’s happening throughout the world,” Allen says. “That’s very unique to this enterprise.”
Collaboration and creativity are necessities in today’s climate given the challenges of the American healthcare system, he says. Among other industry issues, he and his staff are constantly trying to navigate recruitment roadblocks while trying to serve patient populations that often approach illness and medical care in very different ways.
“Recruiting staff that is clinically competent and also able to take care of the emotional needs of a very diverse population is a significant challenge for us,” he says.
Large pockets of Hollywood Presbyterian’s service area are already designated as health professional shortage areas, as well as medically underserved areas by the US Health Resources & Services Administration. What’s more, Allen is competing with two other hospitals on the very same block in an environment where shortages,
especially for nurses, are expected to worsen. And costs are rising faster than Medicaid and Medicare reimbursements, which make up significant portion of Hollywood Presbyterian’s revenue. All of that means salaries alone won’t attract the clinical staff.

“It’s looking at everything nurses might face in a day and trying to make it as easy for them as possible to focus on what they went to school for, which is to provide nursing care,” Allen says.
For instance, contracting with additional doctors not only improves patient access to physicians, but gives nurses the support they need to provide comprehensive care. Executives are also considering childcare benefits and offering doctors a wide variety of financial partnership options when working with hospital and consulting clinical staffers, among other ideas that will help make their jobs easier.
“If you think about a hardworking executive who works eighty hours a week, that’s still less than 50 percent of the time healthcare is being delivered in a twenty-four hour organization,” Allen says. “The most important thing an executive can do is to make sure staff has what they need, help solve problems, and roll up their sleeves alongside them to help.”
Innovation needs to be an organizational objective, he says, especially considering the scope of the changes happening at Hollywood Presbyterian. For instance, the medical center launched an eye care initiative that Allen says will put the hospital on par with top academic medical centers. His team also plans on replicating aspects of CHA’s flagship Chaum wellness center in Seoul in an effort to address patients’ overall health rather than just their clinical needs.
Robert Allen President & CEO
Hollywood Presbyterian Medical Center


Nurses Internet Staffing Services, Inc. is a healthcare staffing company that has been serving the Greater Southern California for over 19 years. We employ Travel nurses, Registered Nurse, Licensed Vocational Nurse, and Certified Nurse Assistants.
With service contracts with over 50 hospitals in the area, we send qualified healthcare professionals to work at times and locations based on their convenience. We have been certified by the Joint Commission since 2007. Over the past 19 years, we have built a good reputation as a company with excellent resources and high integrity.
6055 E. Washington Blvd.
Suite 409
Commerce, CA 90040
323-720-9900
www.nursesinternet.com
“The most important thing an executive can do is to make sure staff has what they need, help solve problems, and roll up their sleeves alongside them to help.”
Hollywood Presbyterian is also in the midst of a $400 million expansion that will dramatically increase its capacity. The buildings are also being constructed to conform to new state regulations for facilities that are in seismically active zones.
The campus expansion, on pace to open in November 2020, will allow Hollywood Presbyterian to significantly expand its obstetrics and gynecology practice and its surgical capacity, among other offerings. The project has also allowed planners to build an emergency room specifically tailored to serve Hollywood Presbyterian’s patient population. As just one example, it will have facilities devoted to dealing with health issues that impact the homeless.
“Our emergency room is in a seismically active area,” Allen says. “So, that needs to be upgraded. We’re building a whole new emergency room. It will be state of the art and designed to take care of the needs of this community.”
And Hollywood Presbyterian isn’t just taking a holistic approach to health but also to healthcare. For instance, the medical center is part of the first cohort of the new Medicare initiative Bundled Payments for Care Improvement Advanced, which aims to link multiple providers’ payments for a single episode of patient care, such as surgery and pre- and postoperative services. It’s also working with insurers to explore innovative ways to control costs.
“Let’s face it; every healthcare executive knows what the problems are in this country related to cost and access,” he says. “But the book on how they’re going to get solved really hasn’t been written yet. And it’s always scary to head into uncharted waters, but it seems to be a requirement for the job.” AHL
Some executives feel the importance of their work because they have experienced its impact firsthand. Shaped by their mission to help others or by their personal experiences with healthcare, many executives are drawn to the industry from a sense of empathy and a desire to make a difference for others.
Dwight McBee is helping raise awareness at Temple University Health System about how the smallest details can make the biggest differences in the patient experience
By Jeff Silver

Chief Experience Officer
Dwight McBee began his career as an ICU nurse at Paul Kimball Medical Center (now Monmouth Medical Center South) before moving to AtlantiCare, where he worked his way up to leading the office of customer experience. Now, as chief experience officer at Temple University Health System, he has extensive expertise to draw from in his professional life. However, it is a deeply personal experience that has had the greatest impact on his approach to helping manage patients’ healthcare journeys.
As a toddler, his second daughter was diagnosed with Rett Syndrome, a rare spontaneous genetic condition that primarily affects girls. A pediatric neurologist told McBee and his wife, “Don’t bother saving for college for your daughter. You’ll spend all your money navigating the healthcare system.”
“That one comment was simultaneously rude, but also hopelessly honest—and it made a huge impact on me,” McBee says. “To this day I’ve never forgotten those words. They made me realize how immensely important
simple things—like the words we choose—are when we’re supposed to be helping patients.”
After this experience, McBee dedicated himself to his Christian faith and reconnected to his source of strength. He also reexamined other instances in the healthcare environment that had impacted his daughter’s experience with the healthcare system. He remembered physicians who sat on the edge of the bed and held her hand, or who shared something personal about themselves. Those simple gestures made the medical professionals more engaging and vulnerable, and they helped the McBee family trust the staff more. By creating a trusting relationship between the family and the clinical team, a partnership was formed that improved the quality of their clinical experiences.
While still at AtlantiCare, McBee helped put those realizations into practice by reconnecting the organization to a motivational story about a boy trying to save thousands of starfish that are stranded on the ocean shore by throwing them back into the sea one at a time.

Dwight McBee empowers his team to find their own way to connect with each of their patients.
“Creating sacred moments was the most important of the concepts because it empowered each individual to find their own unique way of connecting with patients.”
Even though his effort seems futile, the boy persists, knowing the he’s making a difference for each individual starfish. Based on the story, McBee and his team developed The Starfish Experience curriculum, which is built on three core concepts: narrating the story, creating trusting interactions, and creating sacred moments.
“Creating sacred moments was the most important of the concepts because it empowered each individual to find their own unique way of connecting with patients,” McBee points out. “We guided them with recommendations, like sitting down when they first meet patients, but we left it up to them to find the moments that were the most meaningful on an individual basis.”
In one instance, a nurse in the post-anesthesia care unit was approached by a woman in the grocery store who recognized her from her experience after surgery for breast cancer. She had saved a water cup on which the nurse had drawn a picture, something she did for each of her patients. The cup was the woman’s reminder of her successful treatment. That moment in the grocery store made the nurse realize that was her sacred moment.
During his time at AtlantiCare, McBee went on to develop an interactive training program to reinforce the training in The Starfish Experience. This included exercises to help increase staff vulnerability and sensitivities, such as blindfolding participants who aren’t told what comes next. The experience was intended to replicate the feelings patients have when they don’t fully understand their treatment or the various steps they are told to follow in a healthcare setting.
The programs all had a measurable impact on AtlantiCare staff. By the time McBee left the organization, it was rated one of the top three hospitals in New Jersey for nurses communication on the national HCAHPS survey.
“Binary Fountain believes in Dwight’s mission that the smallest details can make the biggest differences in the patient experience,” says Ramu Potarazu, president and CEO of Binary Fountain, Inc. “We have uncovered over ninety million patient insights from online reviews and patient surveys so systems like Temple can deliver a better patient experience.”

McBee’s leadership style is servant leadership, which focuses on effectively empowering others. He helps identify team strengths and provides the tools to leverage those attributes to create positive, productive results.
At AtlantiCare, for example, he was able to mentor one of his administrative secretaries. He helped her move from a role in which she simply generated reports to a leadership position that indulged her passion for working with other people to help them improve patient experiences. That transition helped patient satisfaction scores increase in several departments.
“Success is not measured in promotions or titles,” McBee says. “It’s about helping others to perform their best so that the entire team thrives.”
In his current role, McBee has developed similar programs to highlight the patient experience and raise awareness among the much larger staff. He and his team implemented the CICARE initiative—which stands for connect, introduce, communicate, ask and anticipate, respond, and end with excellence—to help guide patient interactions. Following lessons learned
from his AtlantiCare experience, CICARE is a simple set of guidelines for each interaction between staff members, patients, and organizational leaders that has begun to transform Temple’s culture. The development of the initiative was guided by the mantra: simplicity breeds compliance, and the simpler the expectations, and the easier they are to follow, the more likely staff members are to change their practice habits.
“We’re changing the culture by raising awareness; finding the smallest things that can make a huge difference in someone’s day,” McBee says. “I call it magnifying the mundane. We actively look for the subtlest elements of an excellent care experience and shine a light on them.” AHL
pCare provides patients and families access to personalized education, premium entertainment, and greater control over their environment via in-room televisions and tablets. We are proud to partner with Dwight McBee and his team to make staff lives easier and patients’ experiences better at Temple Health.
Visit pcareinteractive.com for more information.



By Jeff Silver
After years as a healthcare administrator, a personal experience changed how Lori Custer views her work and responsibilities
Lori Custer has years of experience supervising coding and billing, managing regulatory and compliance issues, and handling risk management for medical practices of all sizes. However, as chief compliance and privacy officer at Harbin Clinic, her dedication and loyalty go well beyond simple professionalism and commitment. That’s because two months after joining the Harbin team, she was diagnosed with breast cancer after undergoing a routine mammogram as part of the company’s wellness program.
The disease was spotted early, and after a lumpectomy, chemotherapy, and radiation, Custer is—as she describes it—cancer free and feeling great. But the experience had a huge impact on her, which includes how she views her job, as well as Harbin’s physicians, clinicians, and staff. “I’ll never forget how caring my team was,” Custer says. “My surgeon, Paul Brock, and
Lori Custer Chief Compliance and Privacy Officer
Clinic

oncologist, Melissa Dillmon, still check in with me outside of office visits to ask how I’m doing, but that’s how they are with all their patients.”
A devoted Christian, Custer was particularly moved by Dr. Brock’s offer to say a prayer for her just before her anesthesia was administered, while simultaneously assuring her that everything would turn out fine. “That meant everything to me,” Custer says. “Ever since, it’s made me feel that we have a responsibility to offer that same kind of hope, devotion, and love to every patient we care for.”
To this day, she continues to thank everyone from the receptionists to the clinical and medical teams. “Every hardworking employee who cares about our patients contributes to Harbin’s success as a business,” Custer says. “I feel privileged that they help make it possible for me to have a job here and to have gotten the treatment I received.” By thanking each person, she intends to help them understand how important their personal contributions are to the lifesaving work Harbin does.
“Harbin Clinic and its patients ultimately benefit because of Lori’s positive attitude and how it brings out the best in everyone else,” says Matt Sirmans, president of Garner and Glover Company. “Lori creates a culture where you want to exceed her expectations so everyone wins.”
Prior to coming to Harbin, Custer earned a law degree, specializing in healthcare and elder law. Her legal training enhanced her work as a health information auditor with Parkview Health in Lansing, Michigan, where she continued working while earning her degree.

Her role at Parkview required weeklong rotations of being on-call around-the-clock to address compliance issues for the organization’s eight hospitals. “Being on-call is the best training a compliance officer can have because it makes you think on your feet,” Custer says. “When you’re facing decisions about security or life-and-death issues, legal training helps you think a bit more objectively as you apply legal concepts to the matters that need immediate attention.”
With her dual roles in compliance and privacy, Custer handles a wide variety of responsibilities at Harbin. To help lead the ongoing transition to EMRs, she and her team work extensively with the organization’s approximately 250 providers to ensure appropriate use of the system and ongoing HIPAA compliance. This includes auditing for appropriate coding and billing to ensure timely and comprehensive recording of the entire course of a patient’s care.
The team works with physicians and other staff members individually to remedy such problems, always staying sensitive to the multiple demands on their time
and attention. For example, a physician who hasn’t kept track of each service they have provided may create issues from an audit perspective, but they may be more focused on making time to see an additional patient. “We work very hard to strike a balance between the demands of professional ethics and integrity and the business requirements of keeping the doors open,” Custer explains.
Lori Custer ensures that every Harbin Clinic employee knows their contribution makes an impact on patients.
To help raise awareness among Harbin physicians, clinicians, and other staff members, Custer’s department has always distributed HIPAA talking points to highlight a variety of compliance issues. That practice has recently been replaced by Risky Business, a monthly newsletter featuring real-world stories related not only to HIPAA, but also coding, general policies and procedures, and other clinical issues.
The new, more accessible format is expected to increase the already high level of engagement throughout Harbin. Even with the old talking points, Custer’s office frequently received calls with follow-up


“When you’re facing decisions about security or lifeand-death issues, legal training helps you think a bit more objectively as you apply legal concepts to the matters that need immediate attention.”
questions, or reports of situations that had been easily handled because of the information provided by the department.
Custer was recently part of the leadership team that created new statements of purpose and values for the organization. The objectives were to create statements that are simple, memorable, and less formal sounding than the previous ones.
The new statement of purpose is: “We are people caring completely for people.” The values are encapsulated by I CARE, which stands for: integrity, compassion, accountability, respect, and excellence. Custer believes that the two statements accurately reflect the ethics and integrity of the Harbin Clinic, which was established in 1871 and still has members of the Harbin family participating as practicing physicians.
“The new statements are easy to understand and to connect with,” she points out. “They apply to all of us, from patients to physicians, and provide tangible ideas that inform how we live our lives inside and outside of our jobs. They’re not just words. They truly are
values that we all should strive to live by.”
To be successful in her job, Custer works closely with Andy Goodwin, Harbin’s chief information officer. Like her, Goodwin has worked at much larger hospital systems. They share privacy and security as their top priorities and work cooperatively to continually introduce new best practices to support both endeavors.
Custer also gives tremendous credit to the rest of her team: director of risk management Theresa King, health information manager Tonya West, and compliance auditor Debbie Dawson. “No compliance department can be successful without a coordinated team effort,” she says. “I couldn’t do what I do without them.” AHL
and healthcare teams that make Harbin Clinic the gold standard of healthcare in North Georgia.
By Jeff Silver Faith,
focus, and fuel. These are the three elements that help make any plan come together, according to Natasha Milatovich. The regional vice president of human performance for the Southern California Region of Adventist Health West is quick to say that a commitment to performance excellence is also crucial for success. “Together, these are the elements that leaders of change initiatives thirst for and that are the most effective at achieving organizational renewal,” she says.
After witnessing the many transformational change efforts underway in the healthcare industry, Milatovich says, “We pay too little attention to change, and that slows our drive to achieve transformational change efficiently.” To avoid this oversight, she works tirelessly to ensure that Adventist Health better manages faith, focus, and fuel. “Investing a modest amount of time and effort on this up front avoids paying a lot more in time, effort, and expense in course corrections later.”
She adds, “At the core, when you look at the state of healthcare, associates seem to struggle with burnout because of the level of stress they deal with every day. On many occasions, we’re asking them to do more with less, to be a superman or superwoman; yet, as an industry, we’re not looking at what we can do to make people’s lives easier by helping them integrate work with their life and vice versa, making it difficult to find a balance.”
With master’s degrees in both human resources and business administration, senior HR certifications, and more than twenty years of healthcare HR experience under her belt, Milatovich is moving beyond work/life balance and striving to help the organization’s associates achieve life/work integration.
“Balance is something, to me, that evokes opposition; it’s almost a competition. Integration is about the way you design organizations to create synergies among all areas that define life,” Milatovich says. “So, it’s your personal well-being, your professional well-being, your family, the community you live in, and more.”
Natasha Milatovich leads Adventist Health West’s efforts to create life/work integration for associates in Southern California
Milatovich’s passion for people is strengthened by memories of her own upbringing. Her father was a pediatrician, her mother and sister both nurses. She remembers conversations around the dinner table about clinical issues and her family’s professional challenges. She also has memories of her mother being so tired at the end of the day she had to take a nap before cooking dinner. Those recollections—and other stories about clinicians who go into work wondering if the patient admitted twenty-four hours earlier lived through the night—all fuel Milatovich’s resolve.
To accomplish life/work integration at Adventist Health, Milatovich has been part of a team working

Regional Vice President of Human Performance, Southern California Region Adventist Health West
diligently to transform its HR department from a transactional resource into one that’s in proactive performance mode to provide better fuel, renewal, and growth opportunities for its associates.
“Our associates serve patients daily in an emotionally charged environment,” Milatovich says. “To provide better support, I work toward creating an HR practice that supports true life/work integration by deploying comprehensive plans that promote personal wellness and professional empowerment.”
Her efforts began about five years ago when Adventist Health started to align all of its corporate HR systems across its twenty-hospital enterprise. For Milatovich, that meant coordinating and unifying policies and procedures for about eight thousand associates across the Southern California region. Once that was completed, the organization implemented a new cloud-based IT system that has helped make HR more efficient by creating automated and self-service features.
Parallel with this process, Adventist Health introduced a new benefits plan in 2013 that incentivizes associates to live well. Those who voluntarily opt-in to this plan pay less per month for healthcare coverage but must earn a certain number of points per year to be eligible to enroll. Associates on this plan must complete an annual online wellness assessment, as well as an in-person biometric screening that measures weight, blood pressure, cholesterol, and other health measures. They also have to earn a certain number of additional points by participating in healthy activities such as annual doctor check-ups, exercise, and nutritious eating.
Shortly after implementing this new plan, Milatovich and her team realized
they needed to improve sources of fuel and renewal available to associates at work. This began with looking at the food and beverage options available at the company’s cafeteria.
She and her team took steps such as replacing fried foods with healthier, baked alternatives. They also began reducing the amount of sugar and salt in vending machines, and the on-site chefs began to offer healthy meals that associates could purchase to take home. For easier physical activity, walking paths were created and fitness centers were built, and leaders began encouraging their associates to take advantage of those during their breaks.
Milatovich and her team even created “Zen rooms” where associates can rest and listen to quiet music to recharge. Trained instructors are in place who can teach yoga, deep breathing, and other stress-relief techniques that associates can use to relax when they feel overwhelmed. On top of this, the company also provides offerings such as childcare services, an on-call counselor, and community outreach opportunities to help balance the pressures that come with working in healthcare.
“This is a strategic effort to help associates think less of what they have to do when they leave work so that they can focus on what’s most important while they are at work—taking care of our patients,” she says.
When associates have high-quality fuel sources and various ways to renew their minds, bodies, and spirits, Milatovich explains, it sets them up to pursue professional growth, improving themselves and the organization in the process.
In addition to fostering an environment that promotes health and
“To provide better support, I work toward creating an HR practice that supports true life/work integration by deploying comprehensive plans that promote personal wellness and professional empowerment.”

well-being, Adventist Health also advocates for continuous education, growth, and development.
“In traditional organizations, associates get their degrees, get into a job, and then try figure out the rest on their own,” she says. “In the model we are working on, our associates will have coaches that guide them to the next steps in their careers.”
These coaches, who will be available through the life/work centers that Milatovich and her team are helping to implement at Adventist Health, will be able to provide advice on an array of subjects, from earning professional certifications to how to expand one’s skills
within the company, or whether or not to pursue higher education.
Ultimately, Milatovich’s goal is that, by 2020, all these initiatives will position Adventist Health as an employer of choice for new recruits.
“We recruit people who have the energy and drive to experience the hazards and privilege of working in healthcare,” Milatovich says. “My job is to offer as much support as I can so they can be whole and fulfilled in the pursuit of achieving life/work integration, while finding greater purpose in their calling to serve and carry out Adventist Health’s mission to live God’s love by inspiring health, wholeness, and hope.” AHL
We are on this earth for a reason. Ours is to keep you healthy and surrounded by the people you love. That’s who we have been for as long as we’ve been in business, a healthcare partner with a sense of purpose, a commitment to our calling, and a tradition of excellence in care no matter where we meet you – in the safety of our hospital and physician offices or the comfort of your home. Together inspired®
By Jenny Draper
When Kimberly King Webb was two years old, her mother went back to school to become a nurse.
She worked night shifts, often bringing Webb along, where she would fall asleep watching her mother heal people. “I grew up in a hospital,” Webb says, jokingly. The legal leader recalls how her mother truly listened and cared for her patients—values that would take root not only in her own character but in the mission she champions at CHRISTUS Health.
“It’s really nice to work at a place where you’re able to live out organizational values that align with your personal values,” says Webb, deputy general counsel at CHRISTUS Health. “Rather than business as usual, our purpose really is about helping others. That’s something that really resonated with me. It feels like a higher calling.”
Championing excellence and compassion are core values inherent in the organization’s DNA. The Catholic, nonprofit health system spans more than six hundred centers comprising long-term care facilities, hospitals, walk-in clinics, and health ministries. With forty-five thousand employees, including fifteen thousand physicians, CHRISTUS Health has built a strong community dedicated to creating a personalized healing environment for each individual patient.
“From an employment perspective, we strive to ensure our associates are in an environment where they feel respected and treated with dignity,” Webb says.
To do so, the health system turned to Webb as the go-to expert on people and law. She launched her legal career in commercial litigation in 2007 at the firm Husch Blackwell after earning a juris doctor at Southern Methodist University’s Dedman School of Law and a bachelor’s degree in agricultural business from Florida Agricultural and Mechanical University.
“College was a transformative experience for me,” she says. “I was able to connect with so many people from so many different backgrounds. That same attitude of excellence and inclusion is

“It’s really nice to work at a place where you’re able to live out organizational values that align with your personal values.”
critical to my role as in-house counsel. We must build and nurture relationships to work together with our business clients. Servant leadership is key.”
In 2010, the attorney moved to Austin, Texas, where she joined the firm Norton Rose Fulbright. There, she refined her expertise in labor and employment litigation, from civil rights laws like Title VII to the Family and Medical Leave Act and the Fair Labor Standards Act. With a track record of favorable results and practical solutions, Webb found a new opportunity to deepen her commitment to creating positive work conditions by going in-house for one of her clients: CHRISTUS Health. She officially joined the organization on April Fool’s Day in 2013. Now based in Irving, Texas, the healthcare system used to comprise multiple regions with disparate HR policies and systems. Webb hit the ground running to help integrate HR processes into one, united identity. With employees spread throughout Texas, Louisiana, and New Mexico, she cultivated relationships among the various HR teams to understand each area’s unique needs and to collaborate on solutions.
When approaching such consolidation, Webb cites an African proverb: “If you want to go quickly, go alone. If you want to go far, go together.” Getting buy-in from diverse stakeholders across the organization was essential to the progress and implementation of a cohesive employment law strategy, she says.
First, she worked with an interdisciplinary committee to synergize employment policies under one organizational culture. The committee’s goals included ensuring legal compliance, eliminating duplication, and memorializing best practices. With so many policies to review, policy prioritization was a key tactic. High-priority policies, such as harassment, nondiscrimination, and fair pay, were tackled first, followed by others such as the dress code. The HR team also leveraged technology by developing a more user-friendly online platform to house documents, increasing transparency and engagement.
“Now we have a clear road map for managers and HR professionals, which really allows for more informed decisions and more consistency throughout the
organization,” Webb says. “I think that provides a higher level of equity and fairness for employees in each department and location.” The standing policy committee continues to meet for a monthly review. “Standardization does not mean one size fits all. We are constantly looking at the total circumstances to determine where policy consistency makes sense and when it does not.”
Webb also implemented a robust training program for managers, HR, and other associates. This includes quarterly HR trainings to ensure that the conversation between HR and legal is ongoing. Training topics include new developments in the law, compliance strategies, lessons learned, and evolving needs. “Ultimately, the right training means less time on risk management and more time on value-adding activities and doing good work,” she adds.
Both her knack for spotting paths toward greater efficiency and her commitment to the people at CHRISTUS Health has paid off. Since her arrival, the organization has experienced a significant decrease in litigation expense. Looking ahead, she’s turning her attention to empowering management to address routine labor and employment issues. Her team is now leveraging standardized policies to develop tool kits and templates to streamline processes.
Webb has helped human resources take a more proactive mind-set by working with HR leaders on the front end before employment law issues pop up—and that forward-thinking mind-set is enhancing CHRISTUS Health’s mission of care more than ever before. AHL
We warmly congratulate our alumnus, Kimberly King Webb Vice President and Deputy General Counsel CHRISTUS Health.
For her accomplishments and significant contributions as Interim General Counsel. We thank Kimberly for her vision and leadership.
Law around the world nortonrosefulbright.com
Carter Arnett is a business and intellectual property litigation firm based in Dallas, Texas. Respected, recognized, and results-oriented, our firm is the solution to your legal needs. Financial institutions | Energy | Infrastructure, mining and commodities | Transport | Technology and innovation | Life sciences and healthcare
More than 50 locations, including
After his father’s cancer diagnosis, Kevin Henley found his calling in healthcare compliance
By Anthony Ruth
Nervously waiting to learn the results of his California Bar exam, Kevin Henley had a phone call with his father that he still remembers, thirteen years later.
“I’ve always been able to protect you, and I can’t protect you here,” Henley recalls hearing, as his dad choked back tears. “We know the odds, and it bothers me so much that I’m not able to help you determine this outcome.”
That evening, Henley made the call to his parents—who grew up under Jim Crow laws and never had his educational opportunities—and proudly told them their son was now a lawyer.
But the following year, the tables took a devastating turn. Henley’s father was diagnosed with stage 4 kidney cancer, and Henley moved back to his family home in Maryland to help care for his dad. “This man I had always known as this protector and teacher just suddenly
looked vulnerable. I saw fear that I’d never seen before,” Henley says.
“I was so desperate for anything. I’m like, ‘I’m a lawyer, I’m supposed to have answers, I’m supposed to research,’” Henley recalls. He read everything about oncology he could get his hands on, but he was disappointed to learn that kidney cancer, being relatively uncommon, did not have a lot of treatment options. After initial treatments failed to produce results, Henley tried to get his father into a clinical trial in England, but the disease had already progressed too far.
His father’s death left a massive void for Henley. He remembers thinking, “I’m twenty-seven years old; I just lost my teacher, my best friend, my protector—what am I going to do?”
Meanwhile, a partner at Henley’s firm in the FDA healthcare practice, Vernessa Pollard, had become a friend and mentor
and started bringing him in on her matters. “All of her matters involved helping people who were trying to help other people,” he recalls. “I learned so much from that that I started to deliberately move my practice in a much more healthcare-related way.”
Henley also spent six months as a loaned associate to the Legal Aid Society in Washington DC, representing lowincome tenants at risk for eviction. He saw firsthand how mental illness— which affected a disproportionate number of his clients—permeates people’s lives and can inhibit their success. “I came away from that realizing, ‘Wow,
there’s a lot of good that can be done for people in this space,’” he says.
When Otsuka America Pharmaceutical, Inc., then a client of Henley’s firm, requested an on-site attorney for several months, Henley’s mentor offered him the role.
“Otsuka was doing a deep dive into the mental health space,” Henley says. The company was focusing on disorders as well as diseases, including cancers, that didn’t traditionally get a lot of attention from pharmaceutical companies. It was a perfect fit for Henley’s interests, and when a full-time role became available the following year, he jumped at it.
Henley came on as senior director, senior compliance counsel, with responsibility for four functions: Otsuka’s financial transparency program, and serving as compliance lead for the market access team, patient support program, and digital medicine business. At the time, Otsuka was in development with what is now Abilify MyCite, a version of the drug Abilify used to treat schizophrenia and other mental health disorders, but with an added sensor that connects to an app through a patch on the patient’s body. With the app, the patient and their physician can monitor that the patient is taking their

Kevin Henley Senior Director, Senior Compliance Counsel
Otsuka America Pharmaceutical, Inc.

medication correctly. The FDA approved Abilify MyCite in 2017, and the US had its first drug with a digital ingestion tracking system.
In helping to launch the first digital medicine, Henley collaborated with the product development team to work out the necessary patient privacy and compliance issues—work he found extremely rewarding.
Working in digital medicine also hits home for Henley, as he sees how data can be harnessed to provide information for family caregivers—a role he knows well. “The more your family is in the battle with you, the greater the likelihood you’re going to have a positive outcome,” he believes.
Henley never wants his compliance work to hinder his colleagues’ innovations. “My job is to do the blocking for them so they can get down the field,” and to help them bring their ideas to fruition
in the least risky way possible, he says. “It’s a failed model of compliance to have as your default answer, ‘No, we can’t do that.’”
Not all colleagues expected that from Henley’s department, and at times he’s had to be deliberate about communicating that he wasn’t there to get in their way. “Where I have guidance or perspective that might help inform the decision-making, so that we can get these products out to the patients who need them, I’m going to do that,” he says. He recognizes that sometimes tough conversations need to be had, but he believes that, ultimately, his colleagues know that he and his team have the company’s best interest in mind.
With this approach, Henley has become a trusted advisor to colleagues and seen his compliance portfolio grow to include the medical device division while helping his direct reports grow
into new areas of responsibility. He’s excited about Otsuka’s continued focus on mental health, which he sees as an ambiguous space where solutions are hard fought, but the payoffs for patients, and their families, can be huge.
“It’s not just that we’re manufacturing drugs. We are really doing everything possible, holistically, to improve outcomes and the lives of patients and caregivers,” Henley says.
He adds, “I think your parents are proud when they see that you’re doing right by other people.” AHL
McDermott ’s Life Sciences–Where Mission Meets Innovation. Whether you’re a global biopharma or medtech leader or a startup, we know it’s mission that drives you.
From FDA/regulatory, compliance and risk management, IP, litigation, corporate, and tax, our team delivers tailored life sciences legal solutions to keep your business moving forward.
In 2015, Northwestern Medicine embarked on a three-year initiative to unify its EMR system, a massive undertaking known as Project One. To achieve this momentous task, American Healthcare Leader guest editor, Dr. Thomas Moran, helped handselect a team of executives who lent their expertise to different aspects of this complex initiative.
American Healthcare Leader spoke to five of these executives about the strategies, struggles, and triumphs involved in making Project One a reality.

Cord Sturgeon Professor of Surgery & Physician
Informatics Director
Clinical
for Informatics & Internal Medicine Physician
LoBue Physician Director for Ambulatory Informatics

Lea Ann Arnold Director of Nursing Informatics, DNP, RN

With more than 2,200 patient beds across its system, every day at Northwestern Medicine is buzzing with activity. And when Northwestern’s clinical leaders began work on Project One in 2015, the day-to-day clinical activity didn’t stop. This meant physicians, nurses, and care team members were simultaneously caring for patients while working to implement the health system’s new EMR.
To help clinical staff manage this intense workload, executive leadership extended thoughtful consideration and engaged clinical and professional leaders to help guide decision-making related to content, workflows, and decision support for the duration of the project.
Lea Ann Arnold, DNP, RN, and Northwestern’s director of nursing informatics, led the effort for inpatient clinical work to ensure clinical leaders could provide input for the new EMR, as well as to help foster consensus across the entire system about the new design.
“The care team at our twenty-sixbed critical access hospital needed to have a voice in decision-making just as
much as the community hospitals and the academic medical center with 850 beds did,” Arnold says. “It was really about being intentional about decisionmaking and making sure that all voices were heard.” This approach allowed teams to learn from one another and explore best practices for the system, while keeping patient health and safety as their guiding principle.
To help achieve such a monumental task, chief nursing executives enlisted the help of operational project managers. These individuals stepped away from their clinical roles to serve as dedicated members of the project, which allowed them to stay completely
focused on the initiative without having to simultaneously manage daily bedside clinical responsibilities.
These operational project managers were involved in all phases of the project, from design and confirmation sessions to partnering with the training team, to helping predict the degree of change that the new EMR would bring to a team.
“These operational project managers and additional clinical experts became instrumental in helping us make sure we had tapped the right person on the shoulder to address issues as they came up,” Arnold says.
They also served as ambassadors between their departments, clinical team members, and executive leadership for the duration of the project, which helped Arnold foster enthusiasm and trust among clinicians for the initiative. For her, it was important that the entire care team saw this project as more than just an IT initiative.
The new EMR system serves three main purposes, Arnold says: to function as a communication tool to provide realtime care for patients’ immediate needs, to formulate a legal medical record and an accounting of care provided, and to help clinicians identify broader health trends in Northwestern’s patient population for research, prediction of health outcomes, and improved population health.
“The EMR is a tool for the healthcare team to enable excellent patient care delivery,” Arnold says. “It’s only going to be as good as the information that goes into the system, from design to data entry. That means our frontline staff has to design and develop how it’s going to work because they are the ones who will use this tool. The IT team is the enabler to make that happen.”
On a tactical level, Arnold and her team still had to confront how to most effectively get that message out. To begin,

“It was so rewarding to watch leaders from each site come together and really define a solution that we could use across the system.”
Arnold and her team orchestrated a grassroots effort to make sure everyone was attending and contributing to clinical content build-out sessions, which is where stakeholders reviewed all the information going into the system, and ensured that it was easily accessible for anyone who would need that information.
As content was finalized, communication experts assisted Arnold and her team in sending out newsletters to Northwestern’s various departments that highlighted how relevant information would be displayed in the new system. The goal was to familiarize physicians and nurses with the EMR and alleviate some of the stress of learning something new.
“For example, for the emergency department, we had a set of newsletters that went out specifically with content that was going to impact them,” Arnold says. “The same went for nursing, rehab services, wound care, nursing, dietary, and more.”
In addition, Arnold emailed the content of the newsletters directly to nurse leaders across departments, who then would go over EMR updates specific to their division with their staff in a daily huddle. Operational project managers also attended nursing leadership meetings to share the information on a routine schedule.
The impact of this collaboration has been clear, even shortly after Project One’s go-live date in March 2018, Arnold says. Reflecting on the three-year endeavor, Arnold says the work of Northwestern’s fall prevention team stands out as a prime example of the collaboration between clinical leaders throughout Project One.
“Everyone went in very passionate about the work they had already done to reduce patient falls. We had representatives from each of our hospital sites who helped design and develop a fall prevention program that IT then built into the new EMR,” Arnold says. “It was so rewarding to watch leaders from each site come together and really define a solution that we could use across the system.”
As a result of this team’s work, individuals using Northwestern’s new EMR will be able to see a history of a patient’s falls and their risk for future injury if they should fall again. This will help the care team collaborate and come up with a care plan to help mitigate that risk, Arnold says.
She is energized by the unity Project One catalyzed, and she is proud of the role she and the collective team served in fostering it.
“Having an EMR-focused project really helped build relationships across the system,” Arnold says. “I knew we had made progress when six different hospital team members came together and started pushing back on me as an advisory chair. They would say, ‘We need this to be better,’ and you heard this collective we not I. It was just one of those moments where I smiled and thought, ‘OK, we’re getting there.’”

Describe a key lever that helped move from a “we/they” mind-set to an “us” mind-set?
Arnold: There is a natural tendency to get defensive when protecting something that has proven effective in the face of change. In the beginning, statements such as, “We need this” or “Why do they need that?” hampered productive thinking.
Seeking to understand one another and building relationships across sites created a collaborative and engaging process to review content and workflows. Each hospital had worked hard to make improvements, and needed a voice to share their journey and be acknowledged for their efforts. Listening to one another and being allowed time to reflect, debate, and come to consensus led to more favorable outcomes. At times, people acknowledged that what was being described at one hospital was exactly what others had requested, and the transition to “us” evolved.

From his first day with Northwestern Medicine, Cord Sturgeon knew the EMR systems had to change.
“I remember the day I started at Northwestern in 2004,” Sturgeon says. “Someone showed me we had two different EMRs, and I said, ‘Who came up with this idea? Why are we doing this?’”
Eleven years later, Northwestern Memorial Hospital’s professor of surgery and physician informatics director would help lead the effort to guide and organize training for Northwestern staff across all surgical departments as it transitioned to Project One’s unified EMR system.
Before the project took off, Sturgeon knew it would be important to elicit feedback from surgical staff about what they disliked about the current system. Although the North, Central, and West regions of Northwestern Medicine had some overlapping concerns, the feedback Sturgeon and his team received also varied by location.
“In the Central region, for example, the biggest concern was that they had to use two different EMR systems,” Sturgeon says. “Those EMRs have different passwords, different order sets, and even different names for orders. It was a problem.”
Information sharing across regions was another pain point that Northwestern’s surgery staff wanted to improve upon with Project One.
“In the West region, physicians used Epic, but they send some patients downtown for complex procedures such as heart surgery or brain surgery,” he says. “However, physicians located downtown couldn’t easily view X-rays, blood work, or results of any other test physicians working out west had ordered.”
After gathering feedback, Sturgeon and his team were ready to start the transition to the new EMR. From the start, he knew it would be important to keep surgical staff apprised of any pertinent updates as Project One progressed. This meant attending meetings with the chairs and division chiefs, the surgical oversight committee, and every surgical division to ensure all necessary stakeholders were involved and kept in the loop on the transition to the new EMR system.
Sturgeon quickly discovered that the most daunting challenges of transitioning to the new EMR would be training thousands of staff members to use it and assuaging fears that physicians would lose data during the transition.


Describe a key takeaway, from a physician lens, that has changed the approach for future classes.
Sturgeon: We found that it was very helpful to have a brief monthly meeting with physician groups to engage and educate them about the coming changes, especially about new functionality. We highlighted how new features would improve their ability to care for patients and focus, and how we could either make data more visible, improve communication, or improve efficiency. Physicians quickly identified potential big wins, and started to anticipate these changes in a positive way. Later, when in training classes, they knew to ask about the new features highlighted in the monthly meetings, and were trained on how to navigate to them. Socializing these changes very early, and focusing on how they could improve the way that we care for patients, was a great way to build positive anticipation and acceptance among physician stakeholders.
“Every single provider, advanced practice practitioner, doctor, resident, nurse, medical assistant, back-line staff, biller, coder, and patient service representative had to be trained,” Sturgeon says. “We had to hire an army of people to assist with the training, and they offered classes Monday through Saturday. We had to offer classes at odd hours to accommodate different shifts at the hospital, so there was a complex matrix of class times available to get everybody trained.”
Northwestern employees were required to complete three training sessions: a class for inpatient services, another for outpatient procedures, and one more personalized to their medical specialty. After finishing the three classes, staff members earned certification to use the new EMR.
As for reassuring physicians that data wouldn’t be lost during migration to the new system, Sturgeon had a simple response: the data wasn’t going anywhere.
“When I went around talking to people about what’s going to happen to the old EMR, I would tell them it’s not going away,” he says. “You can log in to it even after the new system goes live and all the data will be there. I think that reassured a lot of people.”
Sturgeon also leveraged some of the new features that would be a part of the improved EMR as a selling point to his colleagues. Among the new features were Dragon Dictation and Haiku, the ability
to see diagnostic imaging from any of Northwestern’s facilities, and the implementation of smart phrases.
In particular, Sturgeon sees Dragon Dictation as a tool that will streamline physicians’ workflow throughout the organization. It allows physicians to create notes by speaking into their cell phones, and the app automatically will create a progress note within a patient’s chart. And these aren’t just Sturgeon’s predictions. Even only a few months after implementation, he is seeing the significant impact the new EMR system is having on surgeons and their ability to care for patients.
“I remember a patient who had come to Northwestern Memorial Hospital from one of our community hospitals for treatment of a complex cancer,” Sturgeon says. “When the patient arrived, even thought it was 5 p.m. on a Friday, the Cancer Center physicians downtown were blown away that they could see all of the images that had been taken at the other hospital, and they could see all of the patient’s lab and biopsy results. It allowed them to efficiently come up with a treatment plan for the patient’s cancer.”
He adds, “It’s immensely valuable for the doctor and patient that you don’t waste time digging through outside records or sifting through data that is not meaningful. This EMR allows you to sort and view the information that is pertinent to the diagnosis being treated.”


With visits to nonemergency care centers on the rise, it’s critical for ambulatory care physicians to have easy access to patient health information, regardless of where patients usually receive medical care. To ensure the success of Project One for Northwestern Medicine’s ambulatory care departments, the organization enlisted the help of Steve LoBue, Northwestern’s physician director for ambulatory informatics.
Throughout the project, LoBue served as the ambulatory physician leader for the team that oversaw the transition to one unified EMR across Northwestern’s three regions. To do this successfully, LoBue had to tailor his approach for each region because they used different systems and had different capabilities going into the project. This meant the transition to the new system would look different for each area.
“In the West region, they had a mature EMR on a single instance of Epic across the care continuum with minimal variation,” LoBue says. “In the North and Central regions, based on their size, the lack of a single EMR, unique clinical services, and noncentralized governance, there was less standardization and a lot more variability.”
LoBue sat down with American Healthcare Leader to discuss the challenges of migrating Northwestern’s ambulatory care services across regions, training care practitioners to use the new system, and how to lead with the entire health system in mind.
Why were you selected to oversee the transition to the new EMR for Northwestern’s ambulatory services?
Prior to the merger of Cadence Health and Northwestern Medicine, I had been the ambulatory physician EMR leader at Cadence for about ten years. Northwestern identified me for the postmerger Epic integration project because I had previously helped lead multiple Epic implementations and facility and physician practice integrations out in the West region.
For Project One, my role has really been to encourage the ambulatory team to think beyond the status quo, help consolidate workflow, and build decision-making. At the beginning, there was a lot of deviation across the system. You would go to one department for the same specialty, and you would see something completely different in another department. So, we knew there was a lot of standardization to solve for and lots of retraining and reworking to do.

“About
sharing before this was traditional faxing and copying.”
How was information shared between ambulatory care departments in different regions prior to Project One?
About the only choice for clinical sharing before this was traditional faxing and copying. The version of Epic we used did have Care Everywhere, which helped us break down some barriers by not having to ask patients’ permission to share their information between one Northwestern Medicine entity to another, but a lot of providers barely used that tool. Now, Care Everywhere is virtually unnecessary because we have one clinical record across the entire health system.
Describe some of the challenges you faced rolling out the new EMR for ambulatory care.
The challenges varied based on what your zip code was, but there were a few things that needed to be updated across the system. For example, we knew we were going to have to start using widescreen navigators to accommodate the new version of Epic, which were only used sporadically in the West region and minimally in the Central region prior to the project. That was a big change we identified early on, because the monitors basically have to be full HD to see the true Epic widescreen view. All ambulatory screens were switched out, even if they were relatively new.
We also had to completely revamp the order catalog because we were combining radiology and laboratory in multiple regions. Where we had been using multiple platforms to store patient information, we had to transfer all of that to Epic. That meant everybody’s order changed to make results in multiple systems match up to the new order catalog. This aided in the tracking and trending of patient care and quality. That kind of pushed some of the project’s build to the last minute because until orders are changed, you can’t finish building out your preference lists and order sets and smart sets.
How did you help Northwestern’s ambulatory care providers overcome these challenges?
We used cross-region collaboration to solve for deviation, which is a big part of how we managed to unify our clinical decision support tools within Epic. We leveraged our quality leaders in all three regions to help us develop rules going forward, as well to help create a basic design for the new system. By utilizing these leaders, who had really dug in and tried to understand this new system the best they could, we were able to go out into the practices across the health system and make sure all of the changes were understood by staff.
During stabilization after the go-live date in March 2018, there was some concern that content was missing from the build. We sent analysts and application coordinators out to the practices to poll physicians and operational leaders on what they felt they needed. By meeting, listening, and understanding needs, the perceived gap of content was reduced by about 80 percent, thereby avoiding an extensive rebuild.
What is your focus moving forward now that Project One has been rolled out?
It’s been a huge leadership challenge for me to shed my West region skin and to make sure that when I’m speaking, I’m speaking for the system as a whole. I’m also focused on managing physician burnout and how much a physician’s relationship to an EMR can have an effect on that. We’ve just thrown this huge project on top of doctors to adapt to; it’s a big change management effort for them. So now we’re trying to say, “OK, we get it; we’re on your side. Let’s talk together about how we can start to tackle some of these issues.”

How can other leaders move individuals to embrace the concept of “systemness?”
LoBue: Leaders need to listen, validate, and value. It is not enough to say we are better as a whole; there has to be a way in which the whole provides value to the individual. This means listening to what the concerns and pain points are. It means validating those concerns and addressing them. Truly value the input of everyone, and live out the value of the collective by including as many voices as possible. Invite those speaking about problems to help participate in the solutions, but do it in a welcoming way. Recognizing and including the negative voice during the planning is better than dealing with it afterward when the voice only gets louder.
Northwestern Medicine McHenry Hospital
Northwestern Medicine Lake Forest Hospita l
Northwestern Memorial Hospital
is
4 M Patient Records Converted
1,269 Physician Personalization Labs
725 Training Tracks
33,42O Learning Plans Assigned
4,754 Total Individual Classes
473
16,824 Total End Users Trained

Overhauling a major health system’s EMR system is daunting enough, but that wasn’t all Lacy Knight was tasked to do. In addition to his responsibilities for Project One, Knight, Northwestern’s North Region chief medical information executive, helped oversee the opening of the health system’s new Lake Forest Hospital, located in Lake Forest, Illinois, simultaneously.
More than seven hundred physicians and advance practice professionals work at the new community hospital, which opened in March 2018 coinciding with the rollout of Northwestern’s new EMR system.
Knight sat down with American Healthcare Leader to discuss the challenges of juggling two major projects at once, training staff to work at a new location, as well as what this project means for Northwestern’s future.
What considerations did you make for the opening of the Lake Forest hospital beyond Project One?
The new hospital incorporated additional technologies beyond the EMR change. For example, it added smartphone technology that was integrated into the nurse call system, and it connects staff members involved in caring for patients. It was the first in the system to have that degree of integration.
We also installed a tap-in/tap-out function for the EMR throughout Lake Forest hospital, which allowed individuals to quickly swipe into the EMR using their ID badges. There were concerns about how that would work prior to rollout, but extensive testing ensured we were prepared.
We also had to consider timing for some patients, because there were going to be patients that needed to be moved to the new hospital from the old hospital. There were also concerns about the operation of the new emergency departments while simultaneously managing the old emergency department.
The day before patients were moved, hospital staff met with every patient and wrote a summary of what was going on with them. They reviewed their medication lists and prepped them for transfer to the new hospital. The morning of, every patient was checked to make sure they were stable to be transferred. Some were transferred by ambulance; some were transferred
through a connecting tunnel that linked the old building to the new building. Finally, once they arrived in the new unit, patients were seen by hospital staff again to ensure everything was stable and that their information was in the new computer system. Volunteers from across the health system aided and assisted the Lake Forest staff during this critical time.
What did staff need to be trained on to operate at the new facility effectively?
We had to make sure that staff were trained on building safety and how to use everything in their environment, because many things were going to be different. For example, we were going to have computers installed in almost all the rooms, and the rooms were going from double occupancy to single occupancy.
We also installed new technology in the operating rooms. The emergency department layout was going to be different and have a different workflow. Staff also needed to be trained on the new nurse call system that is integrated into smartphones to streamline communication between staff and patients.
We spent a lot of hours programming that system so when a nurse comes on their shift, they sign in for the patients they’re going to be taking care of, and when the patient hits the call button, the alert goes to the patient care technician for certain things and to the nurse for other things.
What were the biggest challenges you encountered during this training?
Timing, training, and scope. With all the new technology being introduced into the hospital, plus the demands of training people on a new facility and an EMR, it was a lot of time. Some



of our nurses went through forty hours of training. Additionally, leadership wanted to perform simulations in the facility to make sure people were prepared to use the new equipment. It’s a small hospital, so there aren’t a lot of additional staff members to pick up the slack during this training. So, coordinating the training for everybody was a big challenge. We asked a lot of everyone, and they exceeded our expectations.
What was the key to overcoming these training challenges, as well as Project One’s broader implementation challenges?
I think the most important thing is that we always viewed Project One as a clinical initiative that was supported by information services, but we always intended for it to be clinician-driven. Our clinicians were looking forward to one shared medical record, improved access to information, and in the case of the new Lake Forest hospital, a new platform to enable improvements in care delivery. We had physician and nursing representatives as executive sponsors for the project. The steering committee included chief medical officers, chief nursing executives, in addition to other administrative roles. Then, the foundation of every level of our governance model and clinical content and discovery models relied on clinician involvement.
How do you see Project One impacting the future of care at Northwestern Medicine?
I think one thing that has been evident is that this is the first big project for Northwestern as a system. I feel like going through this, bringing people from every region and every hospital together to talk through what our future was going to look like, helped establish what and how Northwestern Medicine will work as a system. I think what has grown from this project is relationships and collaborations that resulted from people getting to know each other to work through problems together, which has been neat.

Describe a key advantage to going live with an EMR and a new hospital at the same time?
Knight: It gave us synergy. Preparing to open a new hospital required detailed planning of new workflows, comprehensive device and equipment testing, robust training, and simulation of patient transfer and all future patient care scenarios. Similar requirements hold true for a new EMR implementation.
Aligning the timing of both projects allowed for an integrated approach to training, including holding it in the hospital to help people acclimate to the new space. Separating implementation dates would have led to additional training and equipment testing time since it would have occurred in two different facilities over the course of a few months. Our success is a true testament to the care and commitment from each caregiver and all the support staff involved. I am grateful to have been a part of it.

It could have been easy for Nancy Sassower and the rest of her team at Northwestern Medicine to forget the big picture of Project One. But her team would never allow the sheer amount of day-to-day decision-making involved in implementing the new EMR system over nearly three years to overshadow one of the main priorities of this initiative: to improve the patient experience.
For the entirety of Project One’s implementation, Northwestern Medicine’s clinical coleader for informatics and internal medicine physician was instrumental in ensuring that patients’ interests were addressed and represented in the new system.
Sassower utilized a few different methods to fulfill that mission. First, she culled information from team members about their previous knowledge of the system and its pitfalls.
“We have all been patients too,”
Sassower says. “My team could put ourselves in the shoes of both being the clinician using the old EMR system, as well as know how it affected us as patients by using our own experiences.”
On the clinical side, historically, the disparate EMR systems made it difficult for physicians in different regions to efficiently share patient information, which opened the possibility for delays in the delivery of health information. With one record throughout all regions, the efficiency and quality of care delivery would dramatically improve, Sassower says.
Although drawing from firsthand experience was helpful, it wasn’t enough to give Sassower and her team a complete picture of how they could improve information sharing for Northwestern Medicine’s patients. So, she and her team went straight to the source.
Engaging with the Northwestern Medicine Patient Family Advisory Council, Sassower and her team gained critical information and feedback from patients about the current state of communication and health information sharing at the health system.


What key element kept physicians engaged for three years in the physician advisory group?
Sassower: In the quest for better care, our Northwestern Medicine physicians understand how critical the EMR is to achieving our goals and pursuing our mission. The ongoing engagement of our physician advisory group was driven by our motivation to be better. Although members of that group came from varying specialties and regions, we all knew that the only way to get better as a system was to stay connected throughout the project. Fragmentation meant potential failure, which was not an option. So, by staying united and engaged, we pushed the system as a whole for the first time in our history as system clinicians. The reward of working together toward a common goal pushed our culture to a new level. These intangible and unmeasurable benefits of this new physician community became the catalyst for the ongoing commitment to one another and the project.
They learned that patients who received care in multiple regions found it hard to maintain different sets of login credentials. As a result, Sassower’s team designed a more user-friendly patient portal with improved registration and login procedures, proxy access, better webpage design and language, easier access to patient information, appointment scheduling, and more, she says. The medical record belongs to the patient, Sassower says, and Northwestern’s goal is to be as transparent as the electronic system will allow.
Sassower and her team also led the Physician Advisory Group (PAG) for Project One. The group consisted of fifty physicians from the organization’s various regions. Members of this group worked together to share insights on creating an efficient and patients-first electronic record that provides consistency across the organization. With every decision made, patients remained a top priority, Sassower says.
“When I stop and think about one of our biggest successes, the value of the PAG is at the top,” she says. “The
unmeasurable benefit of sharing regional cultures will grow the roots to our success today and in the future.”
Sassower and the entire informatics team are helping to ensure the ongoing success of Project One by contributing to the newly formed Northwestern System Clinical Collaboratives. The collaboratives span all clinical departments and consist of both clinical and operational representatives from each region.
“We want to be as consistent as possible in our care delivery and quality,” Sassower says. “The informatics team is dedicated to being an integral part in supporting the collaboratives.” As Sassower and her team begin to see the fruits of the system clinical collaboratives’ labor, she emphasizes that she and the informatics team will continue to help these teams improve the patient experience throughout Northwestern Medicine.
“We’re honored to be a part of the system clinical collaboratives,” Sassower says. “It is definitely a high-power impact group. This is our future together, and we will work in tandem to accomplish our mission to serve patients first.”
Healthcare is a constantly evolving industry that demands executives to plan ahead. Often, this means business leaders need to address departmental- or company-wide issues to remain focused on driving innovation and devising strategies to maintain a high level of care.
136. Rhonda Collins & Ben Kanter
140. Lisa Odom
146. Matt Gibbs
149. Nancy Stockslager
152. Marnie Wilking
155. Scott Graham
158. Joe Saporito
162. Mark Mosby
166. Frank Venuto
170. Matt Morgan
174. Robert Brooks
178. Jessica Collins
183. Kate Willmunder
186. Marcus Johnson
190. Matthew Kirschner
Vocera communication technology isn’t just comprehensive and smart— it’s being created by the physicians and nurses who know why it matters
By Lori Fredrickson
Healthcare is an inherently chaotic environment. That’s why, as Drs. Rhonda Collins and Ben Kanter of Vocera explain, it’s so important for hospitals to implement a single communication system that makes clinical workflows and care team collaboration easier.
“In a hospital environment, clinicians are taking care of people who are likely experiencing one of the worst moments of their lives,” Collins explains. “Managing the human condition can be unpredictable and fatiguing at times. That is why we are working diligently to provide human-centered technology that supports the wellbeing of patients, families, and care teams, and creates an ideal healing and working environment.”
Since 2000, Vocera has been developing solutions that effectively solve healthcare communication and workflow challenges. Initially, the Silicon Valley company was known for its Vocera Badge, a wearable voice-controlled device. But as mobile healthcare evolved and the need for secure communication grew, Vocera expanded its technology to an all-inclusive digital platform that provides hands-free communication as well as secure text messaging, alert and alarm management, and interoperability with more than 140 clinical and operational systems.
Worldwide, more than 1,700 facilities, including nearly 1,500 hospitals and healthcare facilities, have selected Vocera solutions to improve team communication, speed response times, reduce
alarm fatigue, increase staff well-being, and improve patient care, safety, and experience.
The Vocera platform provides an intuitive system based on a deep well of research and awareness about why communication and workflow challenges occur and what is actually needed to address them. This is where Kanter, the company’s chief medical information officer, and Collins, its chief nursing officer, both come in. As a physician, Kanter was in private practice for twenty-five years, and he served as chief of staff and CMIO at Palomar Medical Center and Pomerado Hospital prior to working with healthcare IT companies. Collins, likewise, spent nearly twenty years in hospital leadership positions before transitioning to the healthcare technology industry.
At Vocera, one of Kanter’s roles is to represent the voice of physicians and gather data from clinical partners for next-generation technology, while Collins captures the voice of nurses and focuses on bridging gaps between patients, caregivers, and technology. Supporting them in this work at Vocera is a dedicated team of more than forty clinical executives who regularly meet with clinical and IT professionals to conduct clinical communication assessments and identify faster, better ways to connect people and information and simplify clinical workflows.
What makes the Vocera system so impactful, Collins and Kanter explain, is that it is designed to make communications more meaningful. “In the midst of sensory overload from alerts, alarms, texts, and calls, clinicians need to know what is the important information that requires action now,” Kanter explains. “We help turn data from multiple digital systems into actionable, timely information that improves clinical workflows and patient care.”


The Vocera platform is built to manage information from multiple systems and deliver it via voice, text, or alert, using real-time situational awareness about the patient and each member of the care team. The platform’s intelligence helps reduce interruption or alarm fatigue by understanding the relevance of data from each system, its potential impact on patient care, and the availability of each care team, sending only actionable messages with context to the right clinician on the right device.
For example, because all communication goes through an integrated platform, it knows the number of calls, texts, alerts, and notifications each team member has received within a certain time frame. This means it can redirect the next communication to a clinician who is available. If a nurse is responding to a code blue, for example, she should not receive calls, messages, alerts, or alarms until the code is completed. Triage and escalation rules in the platform accommodate provider-centric factors as well as operational context to make this type of determination.
Interoperability with hundreds of clinical and operational systems means that care team members using Vocera technology are empowered with contextual, patient-centric information anywhere and on any device. The system makes it easy to loop in any additional physician or caregiver without any chance of error being added to the message. “If a patient is having a heart rhythm disturbance, we’re able to add additional clinical context to the conversation by attaching information from other sources such as an electronic health record,” Kanter says.
The fact that the Vocera is intuitively comprehensive adds to its sophistication; it makes sense of where to send the right information from multiple systems about different patients to hundreds of care team members using various communication devices. The integrated platform enables a patient using a nurse call button to directly contact their specific caregiver through their mobile device, rather than sending that call to the nursing station, where it must be triaged or might not be responded to quickly. “For a patient that wait is
“Empowering patients to communicate directly with their care team has hugely improved the healthcare experience for them.”
like dog years,” Collins says. “Empowering patients to communicate directly with their care team has hugely improved the healthcare experience for them.” This human connection provides dual benefits: speeding up response times to patients’ needs and increasing the likelihood of high patient satisfaction scores, which impact reimbursement.
The Vocera technology is codesigned by a clinical leadership team that understands and cares about delivering a solution that addresses healthcare communication challenges today and in the future. “We focus on consulting with our customers, and we really do try to solve problems, rather than sell a product,” Collins says. “Decisions are being made about technology that will affect hospital staff for decades to come. It is so important to have early and consistent collaboration

between clinical and IT executives in healthcare organizations to make sure the right technology is used to its fullest extent by the right end users.”
For Kanter, who has focused for many years on solving issues that come with the rapid pace of change in the digital environment, it’s also about having a safe, secure and easy way to adapt to that change. “If there’s too much change over too short a period of time, chaos can ensue, and a chaotic care environment is bad for everyone involved, both clinicians and patients,” Kanter says.
A particularly pressing challenge for hospitals now, he adds, is that to be competitive, they need to be agile. “One of our major goals is to use our system’s integrations, rules engine, and communications technologies to turn data into information that’s actionable in real time,” Kanter says. AHL
The Vocera Badge, which nurses and physicians can wear around their necks, allows hands-free communication for clinicians on the go through the use of voice commands.
Missouri native Lisa Odom helps Cox HealthPlans maintain its focus on the community where CoxHealth was born more than 110 years ago
By Jeff Silver

Lisa Odom began working in the healthcare industry shortly after she graduated from college. Looking back, she says she had very little awareness of the complexities of healthcare or the requirements and challenges it presents. She learned quickly, though, as one of two accountants handling compensation of the clinical staff at the hospital where she was hired.
She is now chief financial officer at Springfield, Missouri-based Cox HealthPlans (CHP), the only locally based and provider-owned healthcare plan in the state, and has gained a wealth of experience and expertise during more than twenty years in the healthcare industry, as well as a deep bench of valued business partners, including EnvisionRx.
“EnvisionRx is a patient-focused, nimble, and flexible company,” says Matt Gibbs, EnvisionRx’s president, commercial and managed markets. “As the pharmacy benefit manager for Cox HealthPlans, we are able to react quickly to market demands, while ensuring members get the medicines they need at a cost they can afford.”
Cox spoke with American Healthcare Leader to discuss some of the challenges she faces, and how the company stays closely connected to the communities it serves in the face of ongoing consolidations in the healthcare industry.
How do you preserve your local focus in an industry that seems to be driven by mergers, centralization, and economies of scale?
Staying local has always been a priority for both CHP and CoxHealth, the parent of CHP. We’re both governed by a community board of directors, so we essentially always have a finger on the pulse of what the community needs. CoxHealth’s president and CEO, Steve Edwards, as well as the medical director of one of CoxHealth’s large physician groups, Mark Costley, MD, are both on CHP’s board of directors, so we’re able to keep the provider and insurance businesses closely aligned.
CoxHealth has also purchased two local hospitals in the past five years. To leverage economies of scale, we’re also part of the BJC Collaborative, whose founders include BJC HealthCare in St. Louis, St. Luke’s Health System in Kansas City, and Memorial Health System in Springfield, Illinois. The nonprofits work together to achieve higher quality of care, reduce costs, improve patient experiences, and implement population health best practices.
What kind of results has the close alignment of the community, CHP, and CoxHealth produced?
Internally, we’ve provided data analytics to the provider side on some of our population health initiatives. For example, we understand where members access care, so we’ve been one of the resources that helps guide the expansion of the healthcare system. By assisting in pinpointing opportunities for expanding access to care, in the past two years CoxHealth has set up new urgent care centers, retail clinics, and has expanded its telehealth services.
CoxHealth’s Center for Health Improvement, an outpatient department of the hospital, is another example. For members with diseases that are particularly costly—like multiple sclerosis and rheumatoid arthritis—the Center offers clinical care and more flexible schedules that can accommodate our members better. Since CoxHealth and its providers utilize the same EMR, we can maintain care coordination while
care quality is enhanced through access to the Center. It also provides educational sessions for patients who need information to help manage their illnesses.
Are there business advantages to having such deep local roots?
CoxHealth started out as a hospital in 1906, so we’re a well-known and well-respected name in the twenty-six counties we serve. CHP’s president, Matt Aug, is from Springfield, and Bart Stead, the director of marketing, is too. They know the communities we serve extremely well and have strong local relationships in addition to their healthcare expertise. I’m also a native of the area, but I’ve worked for larger companies, and I can tell you that the healthcare world is a lot smaller here. We’re all neighbors. I know people at the other local health system. I see people I know and work with at the grocery store, school, and at church. That’s a great incentive and responsibility to maintain the highest quality of care, great customer service, and competitive rates. And as long as we do that, our brokers and the rest of the community like having us as one of their options. They want to see us succeed. Our size and focus also means we’re more aware of exactly what the community needs and can be more agile and responsive to those needs than a larger company.
How are you addressing ongoing instability in the insurance markets?
We’re being very proactive and have formalized our approach to enterprise risk management. We created a cross-functional team to compile a complete picture of our concerns and are prioritizing them into categories of high, medium, and low concern. It’s a very holistic approach since each department and individual
The right solution now and into the future.

www.cognizant.com
brings unique expertise and perspectives. It’s also been great at educating everyone on how they contribute to our overall operations. Previously, many people didn’t understand the full scope, for example, of the director of medical services’ responsibilities, or how the IT department ensures that data is being aggregated and reported properly to the Centers for Medicare & Medicaid Services, or how I work with actuaries on pricing throughout the year. A good example of this is the Affordable Care Act’s risk adjustment program—its greatest impact is financial, but it requires everyone to contribute to make it successful.
How have your team members contributed to the financial department’s successes?
They have played a huge role in everything we’ve accomplished, in large part, because they’re all so willing to push themselves outside their comfort zones. Jennifer Keeling, director of accounting, for example, walked into the middle of a very complicated project for an accounts receivable module with our general ledger vendor and helped make it a great success. Tamara Thomas, manager of underwriting, has been an exceptional project manager on a new line of business we’re in the process of developing. And Sandy Hopkins, director of member and provider services, provided critical insights into what members and providers need as part of rolling out a new web portal. I couldn’t do what we do without them. AHL
About EnvisionRx
EnvisionRx is a division of EnvisionRxOptions, a pharmacy benefits and services company and a wholly owned subsidiary of Rite Aid. URAC-accredited for Pharmacy Benefit Management (PBM) and Drug Therapy Management (DTM), EnvisionRx provides affordable and effective prescription drug coverage for employers and health plans. With the options and flexibility needed to truly optimize all aspects of the pharmacy care experience—from full service to à la carte options—EnvisionRx uses its proprietary EnvisionCare model to ensure integration to achieve the very best outcomes for both plan sponsors and patients. For more information, visit envisionrx.com.

visibly differ en t
By Jeff Silver
As much as professionals and consumers alike complain about the state of modern health insurance, they probably don’t remember how it operated during the late 1970s and early 1980s. It was a time when most health plans offered minimal, if any, coverage for prescription medications.
Consumers and providers also take for granted that they can have prescriptions filled at a local pharmacy almost immediately.
Not so long ago, patients would have been required to pay out of pocket and submit receipts for reimbursement. Compared to current prescription management, in-office physician visits, in-patient hospital stays, and lab procedures all still take weeks—if not months—to process and reconcile.
According to Matt Gibbs, president of commercial and managed markets at EnvisionRx, the public can thank pharmacy benefit managers (PBMs) for such improvements. Yet, as drug prices continue to increase, many healthcare entities are seeking ways to better control costs. In pursuit of that goal, several PBMs and health plans have either merged, or are in the process of merging, as a new way to manage costs and to improve care with medical and pharmaceutical oversight.
“There has been a tremendous alignment of health plans and ownership relationships with PBMs,” Gibbs says. “As the plans attempt to leverage the economies of scale that come with having control over the entire patient care continuum, the results may not be optimal for all insurers or all patients.”
At its most basic level, the situation can result in a regional insurer, for example, paying a PBM that’s owned by a national competitor—a subtle but distinct conflict of interest. Furthermore, as part of their efforts to consolidate operations, larger PBMs may also only offer aggressive financial agreements with little room to customize services to a health plan’s own strategic plan.
EnvisionRx, on the other hand, is independent of any particular health plan, and therefore, an ideal partner for smaller, regional, or governmentsponsored health plans. The PBM’s nimble nature allows it to offer options to health plans that might want a fully outsourced PBM solution, full insourcing support, or pharmacy benefit services on an á la carte basis. This flexibility enables health plans to self-manage benefits as much as they want—from formulary

Matt Gibbs President, Commercial and Managed Markets
EnvisionRx
design or clinical reviews to pharmacy adjudication or medication therapy management, among others.
The PBM also offers flexible financial arrangements, such as a pass-through pricing model, that utilizes an administrative fee instead of the traditional spread model. With pass-through, all transactions, rebates, and savings benefit the payer because the company’s revenue stream is based exclusively on these administrative fees.
“We can provide our clients with solid financial deals, whether using our pass-through pricing model, traditional
pricing, or a combination of both,” Gibbs says. “We’re adaptable and creative enough that we’re able to see the upside beyond the spreadsheet.”
In addition to adapting to a health plan’s strategies, challenges, and existing strengths, EnvisionRx works as a consultant to address changing market conditions and business developments. The company’s expertise in nonessential drug management can also help create savings by avoiding newly labeled medications that are simply combinations of existing over-the-counter products in prescription strengths. Gibbs says their
“The work we do here can affect thousands, often in ways that get lost in the process of prescription adjudication or negotiating rebates.”
high costs and associated rebates make these products very lucrative for some PBMs—often at the expense of health plan members.
“We don’t wait for new regulations, compliance requirements, or any of the many other ongoing changes in the pharmacy environment,” Gibbs says. “We constantly anticipate evolving conditions with road maps to minimize risk and optimize clients’ operations.”
For example, Virginia Premier Health Plan (VPHP), a regional Medicaid plan, was able to save more than $40 million with EnvisionRx as its PBM. These savings came as a result of pricing transparency, regular improvements to retail rates and rebates, as well as efficiencies such as a compounding approach for a hyperinflated drug, reporting analytics to detect high-risk pregnancies, and other programs to help the insurer better care for VPHP’s many low-income Medicaid members.
Gibbs adds that the transparent nature of EnvisionRx’s relationships with clients helps streamline discussions about evolving challenges and the benefits they can expect from strategic changes.
A former pharmacist who has worked in the industry for more than twenty years, Gibbs remains passionate about the work that he does at the company. “I could still
be behind the counter dispensing medications, but at most I would be impacting a couple of hundred patients in a day,” he says. “The work we do here can affect thousands, often in ways that get lost in the process of prescription adjudication or negotiating rebates.”
Statistics support his assertion. Through its specialty pharmacy and medication management, EnvisionRx has posted impressive successes working with multiple sclerosis patients: adherence rates are at 92 percent, nearly twenty points above the industry average; the ninety-day discontinuation rate for those patients is 4 percent, about 50 percent better than industry benchmarks; Hepatitis C patients have shown a 98 percent treatment completion rate, compared to the industry standard of 88 percent.
Achieving those kinds of results and the ability to think like a health plan help set EnvisionRx apart from its competitors. “Health plans need to find PBM partners that can assume a ‘fully insured mentality’ so they can align strategies and solutions,” Gibbs says. “Then you can achieve outcomes that go beyond the bottom line. You are supporting a noble cause—transparency that supports access to the right medications and optimal patient outcomes. It’s what keeps me here.” AHL
By Jeff Silver
When it came time to complete the sunsetting of Gwinnett Medical Center’s (GMC) existing EMR systems and to prepare for implementing its replacement, the hospital’s information technology and services department had only weeks to put together a team of more than fifty experts. That meant identifying specialists that could act as liaisons between the technology and the clinical practices that would need to be translated into the new enterprise-wide system.
However, the transition also has implications across the entire health system, not just GMC’s two acute-care hospitals. Gwinnett Health System (GHS), GMC’s parent company, also includes Gwinnett Medical Group—which comprises hospital-owned physician practices, among other entities—so a broad-based approach was required.
Nancy Stockslager, GMC’s senior director of applications and clinical informatics officer, spearheaded the efforts. ”Not only did we have to fill a large number of positions, but we had to fill them with exactly the right people,” she says.
To address that, departmental leadership met to identify characteristics among top performers in a variety of disciplines. After lengthy discussions, they came to agree that higher-level critical thinking was a common thread between these individuals. Those characteristics include rational, logical thought, plus efficient and effective process recommendations that lead to the best solutions.
“Someone with higher critical thinking skills can assess a situation, analyze possible solutions, and evaluate the impact of each one on multiple workflows and other important factors,” Stockslager explains. “That leads to decisions that best meet the needs of the entire organization.”
She and her team decided to rely on objective supporting data to help pursue this line of thinking. GHS already used Healthcare Source as a tool to measure critical thinking in candidates for management positions, but the team needed additional perspectives that were specifically focused on technology employees. That led to the addition of a separate critical thinking test. The two assessments were combined to develop a pilot study that recruited the department’s associate leadership council to test the critical thinking hypothesis.
Stockslager says the results were eye-opening. All the top performers on the council—who were previously recognized through past successes—demonstrated high measures of critical thinking on both assessments. Additional metrics showed high scores for openness to change, innovative thinking, customer orientation, and multitasking abilities.

“We didn’t expect so many different categories to be aligned,” Stockslager says. “The pilot results got more and more exciting because we were testing a theory that was becoming increasingly viable as we went along.”
The pilot study demonstrated that top performers were also highly productive, and they were very wellrounded, including being good communicators. This was critically important because of the liaison responsibilities of the new team. “A highly analytical person with excellent problem-solving skills, but who doesn’t communicate well with users, wouldn’t be a good fit,” Stockslager adds.
With such positive results, critical thinking became an important screening tool in the hiring process. It was applied to both internal associates—who ultimately made up 30 percent of the new team—and external candidates, and was combined with personal interviews and
additional behavior-oriented questions. This created a streamlined screening process that led to more than half of the interviewed candidates being hired.
The assembled EMR project team has already demonstrated itself to be a highly effective, cohesive, and diverse group, she says. Some members have just graduated from college while others are close to retirement.
Many team members have clinical degrees and licenses, as well as technology experience or informatics degrees. This enables each individual to align with the clinical organizations with which they work. And because they have in-depth insights into the processes and challenges, they can recommend the most current and appropriate technologies. For example, the team’s women’s health analyst is an NICU nurse, has an informatics degree, and also has a doctorate in nursing practice; the laboratory analysts are medical technologists; the inpatient nursing and ancillary team primarily comprises nurses or other clinicians. Stockslager herself began her career in nursing clinical practice in pediatrics and the NICU.
“Each one of us has an understanding of the processes and what the outcomes should be for each specialty,” she says. “That helps us find the most appropriate solution for each of our customers’ unique needs.”
Incorporating critical thinking into the hiring process of the EMR team has been so successful that Stockslager is applying it to other areas. It’s being adapted to help fill other management positions within the department, and new questions have been developed to highlight candidates’ responses to difficult scenarios that commonly occur in the role.
Stockslager points to two partners that have provided critical assistance in making GHS’s EMR transition a success. ROI Healthcare Solutions, which has provided complete support for managing the legacy and sunsetting systems, and CSI Healthcare IT, which has provided exceptional short-term staff to help supplement the EMR project team. It has also provided leadership, support, and guidance on the project for testing, training, and at-the-elbow support programs for the project.
Once the EMR conversion is complete, the new Cerner system will offer a single source for comprehensive patient information. “The EMR is helping introduce new tools to provide more efficient and higher quality care that will be better for patients and for our caregivers,” Stockslager says. AHL

Since 1999, ROI has provided quality IT services to healthcare providers through industry-specific project leadership, planning, transformation, and ongoing support of EHR and ERP initiatives. Our differentiators include: our 10+year tenured team members, strong culture, proven methodologies, quality, and true partnership approach.
By Jeff Silver
Marnie Wilking develops rock-solid practices and protocols to protect the sensitive medical data of Orion Health’s customers
Industries evolve and mature in waves that are often driven by the threats they face. Soon after establishing an online presence, financial services companies were hit with security breaches and accompanying lawsuits, so the industry quickly learned how to protect clients’ money as well as their personal information.
Healthcare has begun to learn those same lessons only relatively recently. In fact, the industry now realizes that its information is even more valuable on the black market than financial records. Bank accounts and credit cards can be reimbursed and canceled, but personal medical information lasts a lifetime.
When Marnie Wilking assumed her role as global chief information security officer at Orion Health, she was coming from a twenty-year career in IT security in financial services. Her main responsibility was to establish a mature security program as quickly as possible for the company’s healthcare information technology solutions. This included setting up a security operations center (SOC), implementing automated delivery of Orion Health’s suite of SaaS applications, and qualifying for HITRUST certification.
“We needed automated, reliable delivery of security controls for every deployment,” Wilking says. “It protects our customers and goes a long way toward complying with the most stringent requirements.”
She developed key internal partnerships with the delivery engineering and operations teams. This enabled them to align their priorities, challenges, and solutions. She also identified outside vendors: Anitian for the SOC and Trend Micro Deep Security for a reliable, lightweight tool to perform multiple security functions. The teams moved forward with what Wilking calls security by design—an approach that became their North Star—and embedded security tools in the automated delivery of every solution. As a result, Orion Health achieved HITRUST certification for its Amadeus product in a little more than half the anticipated time.
One of the reasons Wilking and her team were able to make so much progress is that she made it clear from the beginning that she intended to be a facilitative business partner. Security is often seen as an obstacle to others within the business, but her goal was to enable the business to run better and as fast as her colleagues want it to go.
“I’m here to be an enabler, not to create unnecessary barriers,” Wilking says. “Removing myself from that process and empowering teams to make decisions demonstrated that I meant what I said.”
Once all the components of delivery automation and security were in place, she presented the results to Orion Health’s executive team, where she explained how online public-facing applications are typically attacked repeatedly on a daily basis. The goal is to create a
Wilking Global Chief Information Security Officer

There’s one priority as vital as your patient’s well-being… Their personal information.
“We are working with code developers to point out threats, how to avoid them, and give them tools to avoid having to go back to fix them later.”
More than 500,000 companies worldwide rely on Trend Micro™ XGen™ security, with a cross-generational blend of threat defense techniques, to stop patient information from falling into the wrong hands.
We protect your organization’s data across physical, virtual, cloud, and container environments and streamline compliance for HIPAA.
“funnel-shaped” process that limits the number of successful attacks. That is what Wilking’s system was doing: out of one thousand attacks per week, only two per week required active responses, and just one per month needed to be escalated to the security team.
“Many of the executives were initially shocked by the number of attacks,” Wilking reports. “But with a team and architecture in place to detect and respond in real time, they realized that the cost of their investment was well worth it.”
application security testing. She succeeded in shifting the focus on security earlier in the development process by enabling developers to embed security into code development. They are also being trained to identify and address security bugs and vulnerabilities at those early stages.
Smart, optimized, connected security solutions for your connected world.
trendmicro.com/healthcare
She also spends time educating customers on common misconceptions about the cloud. They range from believing it isn’t safe at all to assuming everything stored there is automatically secure. “Education is a big part of my responsibilities,” she says. “I discuss Amazon Web Services’ shared responsibility model, its infrastructure, capabilities, and how our team and products manage all of them. It helps them make more informed decisions.”
Wilking’s team is working with product development teams to automate
“We are working with code developers to point out threats, how to avoid them, and give them tools to avoid having to go back to fix them later,” Wilking explains. “This reduces costs, saves time that can be devoted to new features, and improves overall code quality.”
In addition to security, Wilking oversees privacy, quality and compliance, and patient safety. The structure has led to a consolidated approach to all information assurance issues that provides comprehensive and timely information and direction to Orion Health’s product development team.
“We’re executing a broader assurance by design approach,” she says. “We’re not where we want to be yet, but like everything, it’s always evolving.” AHL
By Charlene Oldham
Scott Graham leverages the Hedgehog Concept to improve pharmacy operations at Presbyterian Healthcare Services
Scott Graham is constantly working on going from “Good to Great.”
As a believer in the book of the same title by Jim Collins, Graham applied one of its key strategies, the Hedgehog Concept, to pharmacy operations at New Mexicobased Presbyterian Healthcare Services, where he took over as chief pharmacy officer in 2015. The Hedgehog Concept, part of Collins’s book, Good to Great: Why Some Companies Make the Leap…and Others Don’t, takes its name from the wily little animal whose top talent is evading foxes. The framework is designed to help organizations discover and develop their primary expertise by focusing on three questions:
• What can we be best in the world at?
• What drives our economic engine?
• What are we deeply passionate about?
“The intersection of these three circles is where the magic happens,” Graham says. “Understanding and answering these three questions honestly allows one to adopt a laser-focused approach to developing strategy.”
Presbyterian’s pharmacy team decided they should focus on delivering world-class pharmacy care to improve patient outcomes and reduce per-patient cost, while elevating the practice of pharmacy in its health system and beyond. It’s an ambitious aim, and one that can never truly be checked off as complete. But putting it on paper helped the department set goals and select strategies to accomplish them in a rolling four-year plan they update annually.
Some of those strategies have since spread to other parts of Presbyterian. For instance, the pharmacy team was the first to implement “just culture,” which centers on constant learning and improvement with a focus on patient safety in healthcare. Just culture training is now moving across the Presbyterian system, which includes nine hospitals, more than one hundred outpatient clinics, retail and specialty pharmacy services, and a reference laboratory that is a joint venture with the University of New Mexico.
Presbyterian’s first “model cell,” based on lean leadership principals of reducing waste, increasing efficiency, and improving quality through engagement with frontline staff, also started in one of the system’s pharmacy sites. It has since expanded to four additional pharmacy sites and other departments within Presbyterian.
“And, based on the success of the model cell, Presbyterian is going to be adopting learnings from the pharmacy department to aid in developing a management system for the organization,” Graham says.

Scott Graham Chief Pharmacy Officer Presbyterian Healthcare Services
What’s more, these systems have translated into savings. Within the pharmacy department, Graham says these and other strategies, including development of an Enterprise Pharmacy and Therapeutics Committee, have helped lower per-unit cost of medications on a year-over-year basis for the past three years, with the 2017 initiatives saving the company more than $4 million.
On the clinical side, the pharmacy team is focused on increasing its impact within the organization and the community as a whole, which is especially important in New Mexico, where nearly the entire state is a Designated Primary Care Healthcare Provider Shortage Area, according to the US Health Resources & Services Administration. Among other initiatives, Graham’s team has worked to get its pharmacist clinicians credentialed and privileged to help address community needs.
Through the credentialing process, pharmacist clinicians must undergo the same level of scrutiny as other medical providers. Privileging outlines the scope clinicians are permitted to practice under and puts periodic competence reviews in place. Pharmacist clinicians can perform physical assessments, order diagnostic tests, prescribe independently, and more. Presbyterian has about twenty-five clinicians practicing in its clinics—the largest number in the state—and in a number of settings including primary care, endocrinology, neurology, rheumatology, and more. Recently Presbyterian Pharmacy instituted its first inpatient pharmacist clinician service in a hospital setting.
“It really has created greater opportunities for pharmacists,” Graham says of the expansion of advanced practice credentialing. “And I would say Presbyterian has been at the forefront of recognizing the role pharmacists can play in the delivery of healthcare.”
Indeed, the dearth of doctors and other healthcare providers opens opportunities for pharmacists to get out from behind the pharmacy counter and into communities and clinics everywhere. With their skill set, pharmacists are also uniquely suited to treat today’s population, Graham says.
“Most of your chronic disease states today are driven by medication,” he says. “So, who better to be managing and tailoring your medication regimen than a pharmacist clinician who has spent six years in training for that?”
Graham says pharmacists are also in the perfect position to advance organizational initiatives such as Presbyterian’s antibiotic stewardship and opioid stewardship programs. During a recent accreditation visit, one surveyor declared Presbyterian’s antimicrobial stewardship program, led by credentialed and privileged pharmacists prescribing independently, could be a model for the nation, Graham says. Presbyterian’s opioid stewardship program helps to educate the community about the dangers of misusing prescription medications, oversees the appropriate prescribing of opioids across the organization, and offers services including drug take-back and disposal, buprenorphine induction, and Naloxone dispensing Moji Imaga
“Most of your chronic disease states today are driven by medication. So, who better to be managing and tailoring your medication regimen than a pharmacist who has spent six years in training for that?”
services. The pharmacy team is also active in implementing a new mobile immunization program, taking immunization services into rural communities where services are most needed.
“New Mexico is a very rural state in many regards and our immunization rate is a bit lower than the national average,” he says. “So we’re going to be taking immunizations into the community rather than expecting them to come to us.”

While such initiatives aren’t obvious or immediate money makers for the health system, they help improve the health of the overall community, which benefits Presbyterian and its providers in ways that can’t be measured by the bottom line. Their central goal is increasing their impact and moving patient outcomes from good to great, Graham says.
“I can honestly say, even with all of the challenges in healthcare, I don’t believe there has been a better time to be a pharmacist.” AHL
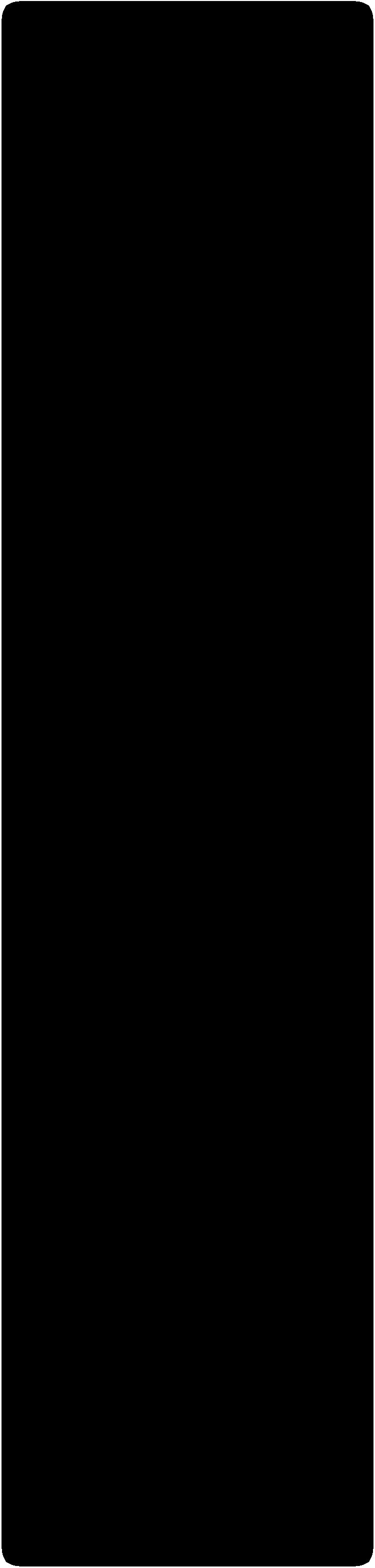
By Joseph Kay
Joe Saporito was restless.
He retired as a partner with the accounting and consulting firm KPMG in 2009. Then, he retired from NYU Langone Medical Center after completing five years as the vice president of finance and assisting the organization in improving its financial performance and credit rating from below investment grade to an A, all while withstanding the impact of Hurricane Sandy. Still, he needed a new challenge.
Saporito began teaching in the MBA program at Baruch College and fielded a handful of CFO offers, ultimately landing at Richmond University Medical Center (RUMC) after being recommended by the previous CFO. He interviewed with CEO Dan Messina and discovered that the professional chemistry was there, and the organization’s position was complex and demanding enough to pique his interest.
“RUMC was, and is, undergoing a major transformation. The facility had basically reached the point of breaking even after substantial losses in its past and a number of significant initiatives were underway,” he says. “Those are the things I’m helping the hospital achieve.”
Richmond University Medical Center operates one of two hospital systems on Staten Island. It is one of the only standalone community hospitals in the area, and it needs to compete against many larger systems, including the largest healthcare system in New York City. RUMC had emerged from bankruptcy in 2007, and by 2015, when Saporito started, had begun breaking even and producing small margins. The first thing Saporito had to do was to create a multiyear plan to invest in the development of an ambulatory care network, population health management, and build a new emergency department while maintaining profitability. Saporito worked with the senior management team to implement initiatives that helped reduce costs, improve care, and prepare the facility for the future.
The natural assumption might be that reducing costs would result in cutting services or negatively impacting the quality of services, but Saporito’s approach was much more nuanced. Through careful collection and use of
data, Richmond has been able to achieve better and more consistent outcomes at a lower cost. One example was in orthopedic surgery.
“We looked at a variety of orthopedic surgeons and specific cases. We looked at low-cost versus higher-cost providers of the same services and what drove the higher cost,” Saporito says. In some cases, the cost was driven by a less standardized approach—for instance, using multiple suppliers for certain types of orthopedic implants when one supplier produced outcomes that are just as good at half the cost. “The cost sometimes had an inverse relationship to outcomes, rather than a direct correlation,” Saporito explains. “By eliminating variation and reducing the number of suppliers of different types of equipment, we were able to reduce costs and improve care.”
One key element of the medical center’s success has been the strategic and engaged use of third-party outsourcing for critical support services. By effectively utilizing outsourcing, RUMC has been able to access the leverage, bandwidth, and expertise of a much larger system at a much lower cost.
On the expense management side, RUMC utilizes Nexera, Inc., a subsidiary of GNYHA, which provides purchasing and supply chain management services to help the medical center achieve supply cost metrics that rank in the first quartile when compared to industry benchmarks.
On the revenue cycle side, vendor nThrive Revenue Systems LLC provides revenue cycle outsourcing services. They handle billing on behalf of the medical center while financial leadership oversees the relationship and monitors performance. Because the revenue cycle of a hospital is so complex and vital,

INDEPENDENT CONSTRUCTION AND PROPERTY CONSULTANCY
Minimizing risk and creating opportunities to maximize the value of our clients’ developments and property assets. gardiner.com @gt_llp


“By eliminating variation and reducing the number of suppliers of different types of equipment, we were able to reduce costs and improve care.”
Richmond’s partnership with nThrive needs to be extremely sound. Saporito calls it Richmond’s largest and most successful outsourcing project so far.
“That organization basically does all of our inpatient and outpatient billing on behalf of the hospital. Our days in accounts-receivable are about forty-five; our cost-to-collect exceeds most benchmarks,” he says. “One of the things that makes it a success is that we really treat them as though they are employees of Richmond. They need to know that you’re watching them; you need to have performance metrics in place and you need to monitor on a daily basis.”
While those measures have had vital impacts across the hospital’s financial health, community support has also been indispensable. Part of Saporito’s role—and part of each RUMC leader’s role—has been to communicate the hospital’s financial needs and impacts to stakeholders. Strong messaging and healthy relationships have led to growing grant funding from the city, the state, and private institutions.
“Getting the word out and making sure officials understand how important the hospital is, how many lives we touch, and what our financial needs are, is an important element of getting that public support,” he says. “We all wear a lot of hats. Under the leadership of board chair Kate Rooney and CEO Dan Messina,
we’ve been very successful in growing community support.”
But more broadly, Saporito recognizes that this is a turning point for the way that Americans give, receive, and pay for healthcare. The transformation of payment models from paying for volume to paying for value is underway, part of a serious push for cost efficiency across the country.
“It’s important to control the growth in costs; it’s also important that we take advantage of the advances in healthcare delivery, like greater efficiency and the benefits of preventive care,” he says. “It really provides benefits to society as a whole if we can reduce per-capita costs in healthcare.”
“As a consultant I’ve been selling this change for many years. Fifteen or twenty years ago, we were projecting that the things happening today would happen,” Saporito adds. “One of the reasons I’m here is that I want to be on the front lines of that change. I wanted to experience it firsthand and have an impact.” AHL
“Joe Saporito is a board member of the Staten Island Performing Provider System. As a start-up, having a seasoned expert in finance with Joe’s expertise is invaluable. The SI PPS congratulates Joe Saporito on being recognized by American Healthcare Leader for his contributions to the field.”
-Joseph G. Conte, Ph.D, CPHQ, Executive Director, Staten Island PPS

SVP & CFO, Richmond University Medical Center

Since the inception of the Bank’s dedicated Healthcare Division in 2012, Investor’s has been providing tailored financial services and solutions to the Healthcare sector: from institutional entities to single practice clients. Our team prides itself on staying informed of the ever-changing regulatory environment impacting healthcare, and any changes new legislation may have on your business. It is this diligence that allows us to create solutions that suit your needs.
James Vincenti SVP/Healthcare Lending
jvincenti@investorsbank.com
Brian Gomez VP/District Manager
bgomez@investorsbank.com
By Jeff Silver
Fallon Health’s unique arrangement for outside legal allows Mark Mosby to deliver effective legal advice right from his client’s corporate headquarters

Fallon Health has a long history of distinguishing itself in the healthcare marketplace. The nonprofit was founded as a provider-payer partnership in 1977— decades before risk-sharing between providers and health plans became a mainstream practice. Fallon went on to become the first HMO in the country to offer a Medicare plan and the first in Massachusetts to offer a limited network. Fallon was the first—and still the only—health plan in the state that is both a healthcare insurer and provider that operates a Program for AllInclusive Care for the Elderly.
However, Fallon isn’t just committed to differentiating itself to health insurance consumers; the company has also extended that commitment to its corporate legal team. Mark Mosby, the organization’s chief legal counsel, is also a member of the law firm Epstein Becker & Green (EBG), a national firm specializing in healthcare, labor, and employment law. Despite working as outside counsel, Mosby is fully embedded into Fallon’s operations at its headquarters in Worcester, Massachusetts.
“Being at Fallon every day has enabled me to build relationships with colleagues and to learn the business so that my legal advice and counsel are based on a good understanding of the operational and financial challenges of implementation,” Mosby says.
In addition to avoiding the challenges and expenses of developing and maintaining an in-house legal department, Fallon, as a regional company, also benefits from EBG’s national perspectives, experiences, and resources in addition to Mosby’s own professional experience and insights, he says.
Mosby says that not being a Fallon employee has provided him with a greater degree of freedom while delivering legal advice in certain respects. “Compared to my former positions where I was an employee of an organization and served as in-house counsel, I have more independence now that allows me to be a bit more objective in rendering my opinions,” Mosby says.
Despite coming from an outside firm, Mosby says he immediately felt welcomed as part of the company’s executive leadership team. He has been in his role at
“Since coming here from the Midwest, I have had to quickly get up to speed on understanding the primary drivers of healthcare costs in Massachusetts.”
Fallon for more than three years, where he has been utilizing the more than twenty-five years of knowledge he has from working for for-profit and nonprofit health plans and health services organizations. During that time, Mosby interpreted federal and state healthcare and insurance regulations, oversight and reporting requirements, and—as part of a growing healthcare industry trend—evaluated which elements make some healthcare organization consolidations more successful than others.
At the same time, however, Mosby acknowledges that he has had to learn the nuances of Massachusetts’s regulatory and political environment. “The commonwealth is focused on reining in increasing healthcare costs in the state, and that focus impacts the regulatory and political environment,” he explains. “Since coming here from the Midwest, I have had to quickly get up to speed
on understanding the primary drivers of healthcare costs in Massachusetts and the measures being taken to help control those costs. Fortunately, I support a client that fully understands the cost drivers and participates in a number of efforts to address them.”
To help reduce these costs and stay ahead of industry trends, Fallon is working on several initiatives to support Massachusetts’s continued transition from volume- to value-based care. For example, the company collaborates with several major Massachusetts provider organizations and MassHealth, the state’s Medicaid program, to offer a managed care option to MassHealth members. The initiative is part of the state’s reform of MassHealth to include accountable care organizations (ACO), which enable physicians, insurers, and other healthcare providers to work together to provide integrated care with the goals of improving health outcomes and containing costs. Mosby provides legal support to the ACO program, which strongly incentivizes providers to deliver value-based care, he says.
Mosby points to several factors that need to be considered before organizations consider adopting Fallon’s approach to its legal department. First, being embedded with clients is key to gaining the requisite understanding of day-to-day operations and business priorities to succeed. Second, the attorney filling the role needs to bring a considerable depth of experience in advising corporations, and they must have the ability to manage and address a broad and complex range of legal issues. They should also be highly responsive and provide excellent judgment and strategic thinking, Mosby says.
“When one lawyer is functioning as the legal department, that lawyer has to find ways to manage the breadth, scope, and volume of legal issues on which an entire department would typically address and marshal all the necessary legal resources to support the client,” Mosby points out. “That single person also has to be able to anticipate and understand the client’s larger set of concerns and issues that extend beyond the narrow legal issue being presented.” AHL

ROBINSKAPLAN.COM
By Jeff Silver
Frank Venuto deftly navigates the challenges of recruitment and retention at Nebraska Medicine
A successful human resources practice in healthcare requires a delicate balance within several different areas of any organization’s operations. That has certainly been the case for Frank Venuto, chief human capital officer at Nebraska Medicine (NM).
The first is recruitment—a challenging priority for healthcare across the country. In addition to identifying qualified talent, Venuto also has to be careful to accommodate the priorities of other partners and constituencies.
He frequently recruits in rural areas of Nebraska, and many students in these areas go to NM’s academic partner, the University of Nebraska Medical Center (UNMC) and its outreach campuses for healthcare
education and training. “We have to respect the expectations of the regions that invest assets and resources in local educational programs where we recruit,” Venuto says. “They want their trained professionals to come back to their local communities where their hospitals need staffing support as much as we do.”
NM also works collaboratively with Metro Community College and other nursing schools to develop curriculum to address the needs of its clinical operations. For example—as part of another balancing act— Venuto pays close attention to the number of patient care attendants. If there are enough attendants to focus on patients’ basic care, patient care technicians
can devote their attention to assisting higher-skilled nurses. This makes patient care more effective and efficient and reduces the risk of professional burnout for everyone.
“Inadequate support makes it harder to achieve the highest levels of patient care,” Venuto says. “We try to avoid such barriers by developing more assistants and technicians through relationships with our partners’ academic institutions.”
To cast an even broader net, NM helps to develop students’ interests in healthcare careers as early as possible. It provides funding to some of Omaha’s high school healthcare academies, which offer in-school and after-school programming to become a certified nursing assistant.
For the past two years, NM also participated in CAREEROCKIT, an innovative program developed by the Omaha Chamber of Commerce that challenged local businesses to provide ten thousand work experiences to high school students in one week. In the first year, 125 students participated in a variety of activities at NM. In the emergency department, staff developed activities in which participants assumed the responsibilities of emergency technicians, nurses, and physicians and were able to experience what goes on in an operating room.
In the second year of CAREEROCKIT, NM hosted 325 students and added experiences for those who were interested in nonclinical careers. They were very surprised by how many nonclinical healthcare careers are available, Venuto says. Opportunities in accounting, HR, marketing, finance, and IT all piqued their interests, but the facility’s IExcel Lab—a virtual reality training

Officer
center—was one of the most popular attractions. Several students commented that they hadn’t fully understood the level of technology involved in healthcare.
As a result of its efforts, NM received the Nebraska Career Education Outstanding Business Partner award.
Like the CAREEROCKIT students, Venuto says that the more than thirty-seven thousand annual job applicants are typically surprised by the variety of services, experiences, and career paths NM can offer. Through its hospital locations, physician networks, and forty clinics and other branches throughout the state, options range from nursing, IT, support services, and advanced practice provider specialties in cardiology, obstetrics, and pediatrics, to transplantation, oncology, and multiple research opportunities.
“The variety of career options is available to every employee,” Venuto says. “We had a unit clerk who started working here when she was nineteen. Thirty years later, she’s our chief financial officer.”
NM is also successful in leveraging the recruiting power of digital technology. Once an applicant applies through one of NM’s social media job postings, a digital app automatically generates a text acknowledging the inquiry, and asks the candidate to respond to a few basic questions. After screening the answers, additional questions can be sent to the applicant with a video link and instructions to record their responses via video. This streamlines sharing applicant information between recruiters, department managers, and other stakeholders, Venuto says.
All of these efforts have resulted in a time-to-fill average of forty days for job vacancies, more than 16 percent shorter than the national average.
After new employees are in place, Venuto and his team implement several strategies to support retention and their professional development. They actively promote health and wellness with programming that focuses on physical, emotional, community, and financial wellbeing. This includes monthly challenges that ask them to reflect on aspects of their overall health and well-being. This helps to remind employees that balancing their lives and taking active steps to prevent burnout are important parts of a long-term career.
“We had a unit clerk who started working here when she was nineteen. Thirty years later, she’s our chief financial officer.”
NM has also developed a leadership training program for frontline managers. Beyond technical aspects, such as proper budget management, the program teaches how to lead and motivate employees by demonstrating care, concern, and compassion, and paying special attention to developing relationships with colleagues.
One last balancing act for Venuto is repositioning the HR department itself. He says that in the past, it took a very rigid stance on compliance with institutional policies and procedures. This created a disconnect with NM’s clinical operations and its workforce.
Venuto is building a new culture in which HR acts as a collaborative business partner with line operators to fully understand issues, develop practical solutions, and initiate proactive processes to avoid issues in the future.
“Our employees already have great pride in the organization and in what they do, and are fully committed to our motto: “Serious Medicine, Extraordinary Care,” Venuto says. “HR is doing everything it can to create a positive culture that employees can be just as proud of.” AHL
Jackson Lewis PC is a law firm with more than 850 attorneys in major cities nationwide. We represent more than 1,800 healthcare industry employers on the full range of labor and employment issues. To learn more, visit jacksonlewis.com/ industry/healthcare.







Matt Morgan on how he helped Montage Health install new enterprise software to increase the revenue cycle team’s efficiency and improve patient care
By David Levine
Efficient and effective healthcare in this day and age is not just about skilled physicians and state-of-the-art CT scans; it’s about software. To stay on the leading edge of this shift in the industry, the leadership at Montage Health, a regional health system located in Monterey, California, spent eighteen months implementing a new software suite across the organization. The company chose Epic as its provider, in part because it provides a “soup-to-nuts application,” says Matt Morgan, vice president, finance at Montage Health. “That has become the table stakes in our industry.”
Previously, whenever a new healthcare product or service—such as a surgical or imaging system—was added, it came with its own software. “We would always look for the best software for our various
different needs, cobble them together as best we could, and hope for interoperability,” Morgan says. But keeping these systems working together properly requires a lot of IT time and money. “In today’s environment, the ability to have a system that doesn’t require massive amounts of interface maintenance is the standard in healthcare,” he says. “We took dozens of software systems out of the company and replaced them with one.”
As head of finance, Morgan is not directly in charge of technology, but the new software system fully replaced all revenue cycle applications. So, as the executive lead for Montage’s revenue cycle, he oversaw how Epic processed transactions and worked to make them as clean as possible for proper charging,
Matt Morgan VP, Finance Montage Health

billing, coding, and payment. “The revenue cycle often represents the final touchpoint with the patient,” Morgan says. “After they are gone, our job is to appropriately charge, bill, and collect for the services they received,” he says.
A system-wide software installation is a monumental task. “Because it was so far-reaching, we had hundreds of people working on the build,” he says. Although the Epic platform is one integrated system, there are individual modules for finance, medical records, surgery, and nearly every other aspect of care delivered at Montage Health. “The challenge is to let each group build its module,” he says. “It’s impossible to have direct oversight on how everything relates to, for example, the revenue cycle. We all had to trust the other folks building their parts of this application.”
That work put a heavy drag on personnel resources, he adds. About one hundred people were dedicated to the project, along with 30–40 consultants to help with implementation. “We also depended on subject matter experts spread across the organization, because they have intimate knowledge of the daily work, and in many ways, they know how this place runs best,” he says. “But they also have jobs to do. Trying to help the directors and these subject matter experts balance their time between daily work and helping us get this up and running was a challenge.”
Getting everyone in the organization trained on the new system was another prominent hurdle. Epic presented a significant change in workflow for many people. “We trained more than two thousand people over the summer, including hospital staff and physicians. The intense training required to bring this live was a massive task, for sure,” Morgan says.
“We took dozens of software systems out of the company and replaced them with one.”
Although it was time consuming, it was a necessary task, he says. “A huge reason we took this on was to improve communication among the various parts of the organization.” The company settled on Epic software because it is used in many healthcare systems across the country—most importantly for Montage Health, at nearby University of California, San Francisco and Stanford Health Care. “If a patient comes through our emergency department who has been a patient at Stanford, which is a real possibility for us, Stanford is also on Epic. So the system reaches out and pulls that patient’s care information from Stanford,” Morgan says. “It’s an amazing opportunity to see holistically around the patient.”
Likewise, people who visit the area for business or pleasure are also often found on Epic systems. “We are a vacation destination, so we see people from all over the country. We have already received tens of thousands of records from other hospitals,” he says. “The opportunity to provide the best care possible to all who live and visit here is another reason for pursuing this.”
The installation has not been without hiccups, but overall the transition has been a success. “Within the first seven days, our revenue was back above target and remained there,” he says. “From a revenue cycle perspective, that is huge, so I can check that off.”
Exchanging patient records among other organizations is another accomplishment Morgan is proud of, along with the launch of MyChart, a patient portal, which had signed up about four thousand people as of August 2018.
“The job is not done,” Morgan says. “But I see certain teams around the hospital already becoming more efficient. That is exciting so soon after go-live.” AHL
With 2,900 professionals across more than twenty-five locations in the West and beyond, Moss Adams provides healthcare organizations with specialized accounting, consulting, and wealth-management services to help them embrace emerging opportunity. Discover how Moss Adams is bringing more West to business.
Willis Towers Watson is proud to congratulate Matt Morgan on his outstanding work to help Montage Health and its employees succeed.

Willis Towers Watson’s unique perspective allows us to see the critical intersections between talent, assets and ideas — the dynamic formula that drives business performance and success in hospitals and health care systems.
willistowerswatson.com

When you go above and beyond, the sun rises on boundless potential. We believe in the value of applauding your achievements—and the possibilities they inspire.
Congratulations to Matt Morgan of Montage Health on all of your accomplishments.
RISE WITH THE WEST.
By Jeff Silver
Erlanger Health System is the sole care provider for many patients across a four-state region— and therefore critical to their well-being. Robert Brooks plays an instrumental role in ensuring it can continue to provide life-altering care to those who need it most.
It would be difficult to overstate the importance of Erlanger Health System (EHS) to the communities it serves in Tennessee, North Carolina, Georgia, and Alabama. Serving about fifty counties across 50,000 square miles, it provides the only Level I Trauma Center, comprehensive stroke center, high-risk birthing unit, and Level IV neonatal intensive care unit in the region. It operates a fleet of six LIFE FORCE helicopters for patient transports, and is the only public safety-net hospital between Atlanta, Nashville, and Knoxville, Tennessee, and provided more than $120 million in uncompensated care in 2017.
EHS also supports thirteen smaller hospitals through affiliation agreements that provide care and specialists to keep patients close to home and help local hospitals stay in business. It operates three federally qualified community health centers and six hospitals that treat patients regardless of their ability to pay, offers on-site medical care for the area’s Volkswagen assembly plant, and recently opened a behavioral health facility as part of a joint venture with Acadia Healthcare.
“As an administrator, I don’t want to dictate how physicians should do their jobs. If I listen and provide support, we can develop much more meaningful outcomes.”
In spite of being such an active and indispensable resource for the region, about five years ago, EHS had accumulated more than $50 million in losses over the previous four years. When Robert Brooks, who has FACHE certification from the American College of Healthcare Executives, joined as executive vice president and chief operating officer, it was his responsibility to return the entire system to profitability.
“I’ve always had the philosophy that you can’t cut your way to profitability,” Brooks says. “You have to grow the business.”
To accomplish that, he identified areas where EHS was lagging behind industry benchmarks and examined service levels in the market. One concern he identified was an outdated process for transferring patients from other facilities. It created such long delays that patients were often admitted elsewhere before processing could be completed at EHS.
Brooks helped create the Erlanger Regional Operations Center—a high-tech communications hub that streamlined transfers from sixty-six other hospitals. Its success led to explosive growth in numerous specialty areas throughout EHS.
A $60 million expansion at Erlanger East Hospital added fifty-eight beds, four operating rooms, six intensive-care beds, and a hybrid lab for cardiac catheterization and interventional radiology. Erlanger Orthopaedic Institute was established at Erlanger
Baroness Hospital, adding six dedicated operating rooms for elective procedures that in the past were frequently delayed while trauma patients were prioritized.
EHS also developed a world-class neuroscience institute and grew to become the fourth-largest stroke center in the US, according to MedPAR data. Created shortly after the orthopedic initiative, the $20 million Heart and Lung Institute added four operating rooms and a hybrid facility for complex cardiac procedures. In addition to an on-site da Vinci robot, the Institute was one of the first facilities in the country to begin using a Siemens ARTIS pheno-drive minimally invasive robotic angiography system, which avoids the need for open chest procedures. A partnership with Columbia Heart Source is helping to improve recruitment and develop additional strategies to position EHS as an international destination for heart and lung care.
The hospital’s cancer program has also grown, particularly around urologic oncology. Capabilities for partial nephrectomy, which removes individual tumors, saves patients’ kidneys, and eliminates the need for dialysis, have successfully addressed multiple types of cancer.
The affiliated academic program is expanding EHS’s urology residency program to train physicians in these types of innovative procedures.
And as the only regional children’s hospital, EHS has just completed a new children’s outpatient treatment center. To make the environment warmer and more
welcoming to young patients, it provides patients with distractions including a full-size 1871 steam locomotive at the entrance, a fire truck that promotes fire safety, and a tow truck that highlights seat belt and bicycle helmet use.
The only resistance Brooks encountered to all of these undertakings—which have contributed $600 million to the bottom line—was concern from board members about managing so many large-scale projects simultaneously. However, they were all completed on time and on or under budget.
Brooks says his background helped contribute to these successes. He started his career as a fireman and paramedic, later becoming a critical care nurse. Then, he began his tenure as a flight nurse with STAT MedEvac for the University of Pittsburgh Medical Center, where he took on the role of base manager and then business development. That eventually led to a master’s degree in health administration.
“I’ve got a leg up because I understand what clinicians face on a daily basis,” he says. “I know how decisions we make around capital allocations will affect them on the front lines.”
That reasoning extends to how he communicates with medical professionals at all levels. For example, he understands that a physician who may appear upset or frustrated is usually trying to find solutions for patient care issues. “As an administrator, I don’t want to dictate how physicians should do their jobs,” Brooks says. “If I listen and provide support, we can develop much more meaningful outcomes.”
Even with the challenges of increasing operating costs and decreasing reimbursements and other income streams, Brooks is still driven by the individual patient successes he and his team help make possible.
“Not a day goes by that we don’t hear amazing stories about how our staff and facilities have saved lives,” he says. “That’s what we all work for every day.” AHL



By Charlene Oldham
At athenahealth, Jessica Collins makes sure the legal team is involved in business decisions from the start

Growing up, Jessica Collins remembers her physician father working long hours, sometimes hearing him take late-night calls. Although she never wanted to follow her father’s footsteps into the medical profession, she now finds herself in the position to help healthcare providers spend more of those long hours doing what they love best: caring for patients.
As senior vice president and general counsel for athenahealth Inc., Collins works to maximize the time and attention doctors and other healthcare providers can devote to patients rather than paperwork by providing cloud-based services including practice management and care coordination. Her legal team isn’t directly developing products or connecting with clients to streamline services in doctors’ offices and other medical settings, but she sees their work as a critical contribution toward achieving athenahealth’s mission to disrupt and transform healthcare by giving providers more freedom for face-to-face interaction with the patients they serve.
“One of the ways we do that is through relationships,” Collins says. “I take the viewpoint that to be a good lawyer, you have to listen more than you talk, which is funny because I think a lot of people think of lawyers as just talking all the time. But, if we are not in the position to listen and understand what the integral business functions are and what the various parts of the company are trying to do, then we can’t support them.”
To put herself and her staff in a better position to listen and learn, Collins and others in the legal department have been working more closely with other teams. Some legal team members even serve as designated legal representatives within other departments, sitting in on staff meetings and other important matters. Members of Collins’s staff become embedded in other departments so they can help address legal questions during the planning process and can also provide valuable background knowledge to the rest of the legal team if an issue requires more attention, she says.
“To be in a position where I’m able to help doctors do what they want to do versus filling out charts or spending more time on the phone when they could be face to face with a patient is really rewarding.”
“We spend time at the earliest formulation stages with our product development team and with our research development team to understand not only what they’re trying to accomplish, but how they are trying to do it so we can help them through regulations, compliance, contractual obligations, and internal policies at an earlier stage,” she says. “And it sounds like just a lot of talk, but it saves an enormous amount of time and makes the process more efficient.”
The legal team also devotes time to educating other staff members about industry issues including privacy and population health management. In addition to periodic teaching sessions, Collins’s department introduced an area on the company’s internal website they call “LegalEase,” which provides answers to a range of commonly asked questions.

“None of it is confidential information, and it’s not specific legal advice, but it’s a resource for people to get answers without having to ask six different lawyers the same question,” Collins says.
Too often, the legal team—especially in large companies—is seen as a barrier for developers or researchers, Collins says. But she’s finding that the more often she and the rest of her staff participate in conversations within other departments, the more often they’re invited to a seat at the table early on, the less often they have to introduce roadblocks near a project’s finish line.

Nixon Peabody proudly celebrates Jessica Collins and athenahealth.
We are focused on the future of health care. Our solution-oriented team tackles complex legal issues, identifies new market opportunities and drives strategic growth for clients in all corners of the health care industry.
100 Summer Street | Boston, MA nixonpeabody.com | @NixonPeabodyLLP
Stuart Henry Partner, Business Development
Stuart@VectorMediaGroup.com (212) 380-8227 x1003
“A lot of what we’re trying to do right now is be part of the thought process instead of the ‘say no’ process later on,” she says. “We actually get to be part of the team and, once you’re part of a team and you understand it better, I find you often feel more invested in the result.”
Collins attempts to create that engagement on her own team by soliciting ideas and input from every member of the legal staff. It’s an approach she learned from a mentor who treated her as a valuable team member even though she was fresh from law school. Her ideas weren’t always incorporated into projects, but, because she was an active participant throughout the planning process, she says she was able to learn why they didn’t make the cut. Engaging others in the decision-making process and fostering stronger connections between her team and the company helps Collins see her job as much more than reinforcing legal rules and regulations.
“To be in a position where I’m able to help doctors do what they want to do versus filling out charts or spending more time on the phone when they could be face to face with a patient is really rewarding,” she says.
Better yet, Collins managed to find a career just as fulfilling as her father’s, without quite as many late-night calls. AHL
Nixon Peabody ’s cross-disciplinary team brings our firm-wide collective knowledge to create success with clients who are shaping the future of healthcare. We use our working industry knowledge and insight to help clients manage and implement the changes to their businesses that help them thrive in this rapidly evolving industry.
By Jeff Silver Apria Healthcare’s
home delivery of medical and respiratory equipment fills an important role in enabling its patients to improve their quality of life. As with most areas of healthcare, however, ongoing industry changes were impacting company operations. Business volume increased at the same time that health insurance providers were demanding shorter time frames for deliveries. This was because the company had transitioned to centralized customer service and dispatching functions that ultimately resulted in an influx of same-day deliveries that local branches could no longer reschedule or reprioritize.
Issues began to accumulate as customers posted negative reviews online about deliveries arriving very late at night; delivery technicians expressed dissatisfaction with schedules and overtime; turnover rates increased; recruiting became more difficult; vehicle collisions were increasing; and overtime was at an all-time high—averaging 485 hours per driver annually in 2017—a total of about $5,000 per driver.
Kate Willmunder helped lead efforts at Apria Healthcare to improve the quality of life for its delivery technicians and patients
This perfect storm made Kate Willmunder, vice president of employee relations and HR compliance, and other executives acutely aware of how widespread these concerns had become.
“Our delivery technicians were struggling to make the time necessary to properly set up equipment and instruct patients on its use while still meeting their delivery windows,“Willmunder says. “Because local branches could no longer schedule or adjust deliveries, technicians were putting in more hours to complete the additional deliveries.”
In response, Willmunder helped launch DriveWise, a cross-functional corporate initiative to improve delivery technicians’ experience and patients’ quality of service. At a brainstorming session, participants from human resources, safety and risk management, logistics/operations, training and development, fleet, transportation safety management, and the Logistics Center of Excellence dispatching center (LCE), reviewed the available data and identified the major areas that needed improvement.
To verify its findings, the DriveWise team surveyed its 950 delivery technicians across 48 states. In addition to scheduling, compensation, and recognition, questions covered topics like road safety, personal protective and lifting equipment, and in-cab technology. Some of the findings were surprising—such as technicians feeling that in-cab technology was more distracting than helpful. Feedback from the survey was incorporated into plans for comprehensive upgrades and improvements.

Compensation reviews, which, according to Willmunder, were overdue, resulted in specific strategies for various markets, such as higher salaries where recruitment and retention were difficult. The company also hired recruiters to assist general managers with sourcing and hiring new technicians.
Capacity planning, driver schedules, and delivery management has also been improved. LCE software now provides local branches with real-time visibility into the time sensitivity of orders, order status, and technician routing. Options are available to adjust delivery times, send products by third-party couriers, or direct ship, when appropriate. Customer service and LCE staff also receive training to better determine which orders are truly time sensitive and to improve the predictability of route scheduling.
More efficient Department of Transportation compliance strategies have been implemented to reduce the time technicians spend on tracking and documentation. Company fleets have been reconfigured to include only noncommercial vehicles (which are not subject to Department of Transportation requirements) at certain locations. As a result, driver daily logs required to comply with DOT Hours of Service requirements are no longer needed at 92 of the company’s 350 branches. This has also eased recruiting efforts at those locations since a commercial driver license is no longer required.
Perhaps the most significant changes are safety-related. Distracted driving has been reduced by LCEs sending fewer and
shorter automated alerts to technicians. Drivers now receive detailed delivery instructions only after arriving at their destinations. The company has also modified its PACE collision prevention program to include proper use of in-cab technology and has created a new market operations support trainer position to help manage technician training.
“We’re working very hard to instill a culture of safety,” Willmunder says. “We care about our drivers and their well-being and want them to go home safely to their families every day.”
Drive, a new monthly newsletter, helps reinforce the company’s message. It highlights desired best practices—everything from the use of technology, safe driving, and vehicle inspections, to defensive walking, proper use of lifting equipment, and weather-related safety. The DriveWise team is also looking at vendors for high-top boots to provide technicians with additional ankle support.
Apria has even instituted reimbursement for parking tickets in some heavily congested cities so that technicians can avoid legal parking spots that may require them to carry heavy equipment for longer-than-reasonable distances.
These changes are starting to produce meaningful, positive results. Overall technician employment satisfaction ratings are improving and positive reviews are beginning to be posted online; overtime hours are steadily decreasing; costs associated with vehicle collisions have decreased; and the time to identify and onboard new recruits has been reduced.
“We’re working very hard to instill a culture of safety. We care about our drivers and their well-being and want them to go home safely to their families every day.”

Additional improvements are also underway. Willmunder is leading the DriveSafe initiative to discover what concepts have the most resonance with driving-related employees nationwide.
“A key part of making successful improvements was getting anyone associated with the logistics function deeply engaged in developing solutions,” Willmunder says. “By listening to their creative ideas, we expanded our concept of what was possible as part of a culture where safety is top of mind at all times.” AHL
By Joseph Kay
Marcus Johnson is leading the effort to automate processes and improve patient outcomes at Highmark Health
After nine years on the road as a business consultant, Marcus Johnson was ready for a new opportunity. He loved the work—the structured problem-solving, the teamwork, and the creative demands—but he missed his family, and he was over the lifestyle of constant travel.
That’s when Highmark Health called. They were looking to build an internal consulting group: a team that could assess processes across the enterprise and implement solutions without the expense and arduous onboarding of hiring outside consultants. Highmark Health, in the early stages of a bold strategic plan in concert with evolutions in American healthcare, needed nimble enterprise services. For Johnson, it meant a chance to continue doing the work he loved without the punishing lifestyle, as he joined the organization as its vice president of enterprise effectiveness.
“I looked at that and said, ‘This is perfect,’” he recalls. “I get to continue this work: the problem-solving, the use of analysis, the use of quantitative and qualitative data to help find insights, and I get to see my kids every night.”

A national health and wellness organization headquartered in Pittsburgh, Pennsylvania, Highmark Health is the second-largest integrated delivery and financing enterprise in the United States. Forty thousand employees support a diverse portfolio, with businesses in insurance, delivery, eye care, dental care, and more. The size of the system is daunting, but Johnson’s unit looks across its entirety.
Plus, its size and status as the only plan-led integrated delivery and financing system in the United States put Highmark in a unique position to drive a clinician-led transformation to quality in care, Johnson says—and
that’s the heart of the strategic plan. “We have strong incentives to do that. We’re bringing together the health plan and provider system to move care into the community and closer to the patient, delivering better health that is outcomes-oriented and a better experience for our members and patients.”
The first step was to gather data. The workforce knows their work best, and it is empowered to provide feedback and solutions to an attentive leadership. Johnson’s team went on to ask the workforce about the possibilities and perceived threats around automation, and received a surprisingly positive response.

“We do a lot of this through workshops,” Johnson explains. “We ask people for ideas around what can be automated, and we ask for their hopes and fears. We’ve been pretty surprised. Typically, the list of hopes has been a lot longer than the list of fears. People have been excited because they could stop doing work that they don’t really like to do.”
Overall, Johnson and his team recognized that many highly trained Highmark Health professionals were mired in simple, repetitive tasks—financial wizards writing manual journal entries, nurses replicating data entries, and so on. He adds, “A lot of the work we’ve been able to automate has been time-consuming, rote work that we have highly skilled people doing, which frees those hours for them to do the right work.”
“As an integrated partner woven into the fabric at Highmark, we support Marcus’s vision to optimize
processes and maximize Highmark’s professional talent,” says Scott Barnyak, founder and chief sales and marketing officer at SDLC Partners. “Our collaboration continues to focus on supporting their ongoing transformation with practical, yet innovative technologies such as robotic process automation.”
before making decisions.
The workforce was initially skeptical of the team’s follow-through. Certainly it’s simpler to gather ideas than to implement them, and few great ideas evolve into great solutions. But Johnson’s group had to build the trust with the workforce it needed for a strong, lasting partnership. By being realistic about its bandwidth, the team committed only to the efforts they knew they could follow through on, and the results have been promising.
“A lot of the work we’ve been able to automate has been time-consuming, rote work that we have highly skilled people doing, which frees those hours for them to do the right work.”

The other major fear was job loss. Successfully addressing this fear would protect the workforce and continue to build trust. Highmark Health is always hiring, notes Johnson, so they have been able to address concerns around job loss with a retraining program. The consulting team has partnered with human resources to create a comprehensive retraining platform so that Highmark Health employees are doing the right work for the company and themselves.
“We feel like that capability is very strong,” he says. “HR has the right training program in place, with people who are dedicated to internal mobility, working with people to get them into the right roles.”
Going forward, Johnson is already building a vision of what technologies can accelerate Highmark Health and support its strategic evolution. He points to natural language processing, machine learning, and AI as tools that will eventually transform the way Highmark Health works. While those technologies evolve, the consulting group can continue to optimize processes and support strong relationships between parts of the enterprise.
“It’s working in a more horizontal basis and having our work flow through the organization in a clean fashion, without divisions between functions, departments, and the business getting in the way of the right solution and experience for our patient,” he explains. “I’d love to see that we stop doing a lot of things we don’t need to be doing. We have an opportunity to ask, ‘Do we really need to be doing this at all?’”
With that, Highmark Health has proven the right home for Johnson—a perfect environment for his continuing growth as a leader.
“When you’re driving through a lot of change, that tests how you lead your team, your colleagues, and the people going through that change,” he says. “I’m continuing to hone my skills here.” AHL
DayBlink is excited to partner with Marcus Johnson and Highmark Health to transform the delivery of healthcare services nationwide. As a committed member of the thinkUP ecosystem, DayBlink will collaborate with the Highmark team to leverage our Agile methodologies, automate processes, create efficiencies, and accelerate the delivery of business value.

By Charlene Oldham
Matthew Kirschner spent the first eighteen years of his professional life as a management consultant and investment banker, working mostly with nonprofit hospitals. But he still considered himself a rookie after being recruited by one of his clients, UnityPoint Health, to an in-house position in 2013.
“I’d always worked with healthcare companies, but I felt like my knowledge of the healthcare industry was an inch deep and a mile wide,” Kirschner says. “I could talk a little bit about a lot of topics, but I couldn’t go in-depth.”
Kirschner feared he’d be behind in terms of industry knowledge, but decided to accept the offer, in part, because of all the changes happening in healthcare. With the uncertainties surrounding the Affordable Care Act and the shift toward more transparency in care costs, among other factors, Kirschner felt he could learn and grow alongside industry veterans. He also had a specific skill set to offer his new team.
“UnityPoint Health was in a big growth mode, and they were looking for someone who understood how mergers and acquisitions worked and who knew how growth transactions would impact our balance sheet, whether it was the debt portfolio or the investment portfolio,” says Kirschner, who serves as the nonprofit health system’s vice president, treasury.
Today, UnityPoint Health has expanded organically and through mergers and acquisitions to include nine geographic regions, more than twenty hospitals and hundreds of clinics, as well as home-care services throughout Iowa, Illinois, and Wisconsin. The rapidly growing company now boasts about thirty thousand employees.
Kirschner is in charge of UnityPoint Health’s debt and investment portfolios, its insurance renewal processes, and capital investment strategy, but he’s not just a money man. Among other duties, he helped roll out the health system’s new core values and standards of behavior framework in 2017.
“We have a philosophy at UnityPoint that we don’t try to hire the best position player, we try to hire the best athlete,” he said. “We put smart people in a role, but that doesn’t necessarily mean that’s all they do.”
Pinch hitting, so to speak, can be a challenge, but it keeps things interesting.
“There’s nothing mundane about what I do,” Kirschner says. “I get to reinvent myself with every new project that comes along.”
For instance, in his work to revamp UnityPoint’s capital allocation process into more of a competitive model, Kirschner takes on a role similar to the Shark Tank investors who vet entrepreneurs’ products on TV. Kirschner, along with the vice president of strategy and business development, developed a new process and a Business Opportunity Assessment Team (BOAT). He and other company leaders are evaluating in-house projects vying for funding, looking for ideas that will give UnityPoint new ways to generate revenue in an era when it’s increasingly difficult to make money through insurance reimbursements alone.
“But, more importantly than that, we’re a healthcare company. Our business is to ensure the wellness and health of the population we serve,” he says. “So, if we can find new, innovative ways to be more efficient and able to deliver better care, that’s important.”
Funding projects that address regulatory requirements and patient safety are a given, but the company’s process pits projects that involve new businesses or initiatives against each other to compete for capital. The BOAT considers factors such as return on investment and UnityPoint’s long-term strategic plan when evaluating proposals. Although the team feared some would question the approach, they were pleasantly surprised after implementing it for the first time in 2017.

Partner with the largest OCIO to healthcare organizations and the only asset management firm with HFMA peer reviewed designation1
Your investment decisions affect your organization’s overall finances. Learn how a holistic approach can help you effectively manage healthcare assets in a complex operating environment. Visit seic.com/HealthcareOCIO or call 610-676-7926.
“At the end of the day, all our constituents—even if their projects weren’t funded—felt like the process was fair, made a lot of sense, and that it allowed us to be the best stewards of our resources in a changing healthcare environment,” Kirschner says.
UnityPoint is also in the process of launching an Innovation arm that will include an accelerator and incubator that finds and supports start-ups that are working to develop products and ideas to improve operations at UnityPoint and the healthcare industry as a whole. Meanwhile, Kirschner and other company leaders are introducing comparably low-tech innovations that he thinks will make a big difference in patients’ care and experience. For instance, UnityPoint is moving toward scheduling systems that allow patients to book appointments online with either a specific care provider or the firstavailable doctor, depending on the patients’ preferences. The healthcare system is also working on making bills more patient friendly.
really pleasant and easy to come here,” he says. “We think innovation is critical to our organization and its ability to deliver great care. It’s also critical to our patients in their journey toward wellness.”
Company leaders also work to let their employees know how much they matter. For Kirschner, that translates into what he calls “leading from behind.” He trusts his staff to do their jobs while his role is to remove roadblocks and prevent pitfalls. He also gives staff members credit for the work they’ve done, inviting analysts to present their own data at important meetings, for example. The approach lets people know they are appreciated—and accountable—for their work.
“We feel like a family,” Kirschner says. “We have each other’s backs and, when someone tells us about something they’re working on, our first reaction is, ‘How can I help?’ That comes from the top and it’s one of the things that attracted me to this company.” AHL
1Distinction based on competitive research using publicly available information as of 12/31/2016. Largest based on number of healthcare clients, and/or on healthcare client assets under management in SEI’s OCIO program for which SEI has discretion for money manager hiring and replacement decisions on behalf of those clients.
Simple shifts like making bills easier to understand and expanding online scheduling options might not generate immediate returns, but they will encourage patients to take better care of themselves and, hopefully, recommend UnityPoint to friends and family, Kirschner says. It’s also a practical way of putting the company’s motto, “Know How Much You Matter To This World,” and helps to make healthcare easier and more personal, he says.
“We want to be the healthcare provider of choice for the regions we serve and the way we’re going to do that is to make it
As the largest OCIO to healthcare organization*, SEI is proud to work with Matthew in supporting UnityPoint’s overall goals. We’re HFMA Peer Reviewed with $15B in healthcare assets** and more than twentyfive years as an OCIO. Learn more about how SEI and UnityPoint create investment strategies for each asset pool at seic.com/ HealthcareOCIO.
*Distinction based on competitive research utilizing publicly available information as of 12/31/2016. Largest based on number of healthcare clients and/or based on healthcare client assets under management in SEI’s OCIO program, for which SEI has discretion for money manager hiring and replacement decisions on behalf of those clients. HFMA staff and volunteers determined that this product has met specific criteria developed under the HFMA Peer Review process. HFMA does not endorse or guarantee the use of this product.
**As of 12/31/17
Executives know there is an increasing need to help individuals manage their own health anywhere and anytime. To do that, healthcare leaders are developing products and services and offering resources that cater to different communities’ needs and motivate people to stay engaged with their own health.
194. Priyanka Das Sarma
199. Jim Feen
204. Ryan Murry
208. Bernadette Melnyk
212. Eric Record
216. John Bosco
By Charlene Oldham
Priyanka Das Sarma helps lead Hilton’s efforts to craft a benefits program that replenishes employees’ minds, bodies, and spirits

of Benefits
As a paralegal for Interstate Hotels, Priyanka Das Sarma worked closely with the human resources department to interpret the nuances of employment law. Still, she was surprised to get a call from the company’s head of HR encouraging her to apply for an opening as a benefits manager. Das Sarma held a law degree from her native Singapore and had no direct experience in the human resources field.
But she landed the job in time for the hospitality company’s first day of annual benefits enrollment. So, her orientation consisted of poring over plan documents and fielding phone calls from employees asking questions about health insurance, retirement plans, and more.
“All the other team members were off-site at different hotels. It was a baptism by fire,” she says. “I learned just by answering questions and asking them. That was my introduction to benefits.”
Das Sarma, who now serves as the director of benefits for Hilton, has seen a lot of changes in the nearly twenty years since her first frenetic day in the industry. The benefits business has expanded to encompass new offerings to meet the needs of a changing workforce and world. Das Sarma says she’s excited by the industry’s evolution and the opportunity it provides to design different plans.
“Historically, benefits’ bread and butter has been healthcare benefits. It was offering medical options at a reasonable rate,” she says.
But, as healthcare costs continued to rise, she and other benefits managers found it increasingly difficult to effectively control costs for companies or employees.
“If you’re looking for a silver bullet in benefits, healthcare is certainly not it anymore. So what else can we give our team members?” she asks.
Hilton has tried to answer that question in both big and small ways. For instance, it offers team members
financial assistance during an adoption, and all new moms get ten weeks paid time off after having a baby once they’ve worked at Hilton for at least a year. Dads and adoptive parents get two weeks of paid leave. When it rolled out its formal paid leave policy in 2016, the company wanted to extend it to both hourly and salaried employees—a fact that grabbed headlines at the time.
“We don’t tend to think differently in terms of salaried and hourly team members. I think at Hilton that’s what sets us apart from a lot of hotel companies,” Das Sarma says. “The team members in the field are really the ones serving our guests. We work to support them so they can do that.”
Less publicized benefits include Hilton’s recent extension of bereavement leave from three to five days, accident insurance as a voluntary benefit, and a ten-day advanced scheduling program aimed at helping hourly employees manage their other daily commitments and plan for upcoming special events. The company also recently introduced new financial wellness resources, a fitness discount program, and a back-up care program for employees who need childor eldercare on short notice.
“I think the spectrum has moved from the bread and butter medical and dental benefits to coming up with creative ways to help team members take care of themselves and their families,” she says.
The Go Hilton travel program, which offers discounted room rates and other benefits to team members and their friends and family members, is also an important recruitment and retention tool for the company, and it encourages all employees to take advantage of the rejuvenating power of travel, Das Sarma says. It also fits right under the company’s umbrella program called Thrive@Hilton, which aims to address employees’ well-being through three lenses—mind, body, and spirit.
“I think the spectrum has moved from the bread and butter medical and dental benefits to coming up with creative ways to help team members take care of themselves and their families.”
Hilton implemented the Thrive program in 2017, and Das Sarma says it really has changed the way many team members operate. For instance, the program prompted supervisors to talk with employees about how and when they work best and to make more accommodations when it was possible.
“So it’s not just the yoga classes and the workshops on eating healthier,” she says. “It goes beyond that into how we work. That flexibility we give team members is great, and I can say that’s definitely allowed me to thrive.”
Another part of the program, the Thrive Sabbatical, allows ten team members to either “give a dream or live a dream.” Winning program applicants are given four weeks off with full salary and benefits and a
$5,000 stipend to fund their dream. For twenty runners-up, Hilton donates $1,000 in their name to the charity of their choice. The inaugural class of sabbatical winners included a Hilton sales director who worked with the Lions Club to set up temporary eyeglass clinics that served as many as 1,500 people a day in remote villages in Mexico, and a Bogotá, Colombiabased hotel bartender who traveled to distilleries and vineyards around Europe to sharpen his skills while on sabbatical.
“I don’t know of any other company doing this. It’s really exciting and unconventional and new,” Das Sarma says of the company’s approach to benefits. “And I’m really happy to be in this space.” AHL


How Southcoast Health’s Jim Feen is creating innovative solutions to upgrade the billion-dollar regional health system
By Jenny Draper
Jim Feen has spent the past decade optimizing collaboration across Southcoast Health—a culture based on DevOps, a concept that combines software development (Dev) with information technology operations (Ops). The ideology has spread rapidly in the technical community since the early 2000s, and now the business world is realizing its bottom-line advantages as more companies seek to build and run resilient systems at scale.
Feen continues to champion IT governance and a strategic organizational structure to upgrade and optimize new IT platforms at Southcoast Health. The nonprofit, community-based health system comprises 4 hospitals and 450 providers that serve 33 communities in Massachusetts and Rhode Island.
“I’ve worked on the vendor side of healthcare IT,” says Feen, Southcoast’s senior vice president and CIO. “But as much as I enjoyed working with providers and health systems across North America, I felt compelled to give back more locally.”
Feen’s impact on and commitment to Southcoast has been felt beyond the organization, reaching all the way to the vendors he works with.
“It was a pleasure to work with Jim and his team at Southcoast Health throughout their implementation of Epic and beyond,” says Jason Mabry, CEO of Optimum Healthcare IT.
American Healthcare Leader spoke with Feen to discuss the role of DevOps in healthcare today, his new app development team, and how IT is impacting care delivery and costs at Southcoast.
Which experiences inspired you to pursue a career in healthcare?
Directly out of college, I worked as a unit coordinator in an emergency room. There I saw the impact of proper, streamlined processes in care delivery in the mid-nineties, well before the age of Meaningful Use measures. I recall working the third shift and having to run downstairs to the basement of the hospital to find a medical record for a patient in crisis in the ER, and later recognizing just how archaic it was. Having important information readily available can make a difference in helping a provider save a person’s life. It was eye-opening; knowing that there’s a huge opportunity in healthcare to create safer processes and systems through automation and technology.
How does DevOps address those needs in the healthcare industry today?
It underscores the gap that exists when vendors design technology for healthcare providers based on what they think they know about how healthcare operations function. We’ve chosen to strategically apply DevOps to solve really niche problems in areas where automation can get us a better result. We apply DevOps for things that may not be readily understood, defined, or available in the open market. We also use it to create intelligence on the programming side.
What changes did you make at Southcoast when stepping into the CIO role in 2017?
That transition happened right in the midst of completing a massive investment—a move to Epic on the clinical side and a move to PeopleSoft on the enterprise resource planning side of the business systems. I had just completed leading the implementation of those platform-change initiatives at Southcoast when my role changed. So it was a natural point for me to shift from an implementation focus to more of an operational and strategic focus to help our organization, group leaders, and providers leverage the investment our organization had made.

Jim Feen SVP & CIO Southcoast Health
What is the thinking behind the recent creation of the app development team?
As a lean organization with so much growth, we’re constantly challenged to try and do more with less. So, the focus on DevOps became pivotal for us as we tried to answer some complex challenges. When we were moving fifteen different EMRs into Epic, there was an opportunity to leverage the DevOps approach not only for how we get from old to new, but what technology and apps can we put around the process that make it easier. We’ve invested in staffing an app development team that creates workflow apps and programs—we currently have about forty different apps that solve different needs. As an example, very specific sequences need to happen when you move a patient from the emergency department to the operating room. We realized we could simplify the process by creating an app that outlines a location-based process. When the patient is here and needs to go there, it says exactly what needs to happen in our systems to do it successfully.
So, for what could have been a very complex and errorprone education process around patient movement became a DevOps initiative to simplify and standardize the conduit for managing a complex process.
“We’re constantly educating staff on how our technology can continue to challenge the status quo of traditional care delivery methods, and we’ll continue to use data in new ways to improve quality.”
Looking ahead, what are your goals for DevOps initiatives in the next few years?
There’s a lot of a transformational change that needs to occur across the system to leverage the tools and find new and innovative ways to better the business. Although we have many of the foundational blocks in place to advance the organization, we really see it as part of our stewardship to help the change management side. We’re constantly educating staff on how our technology can continue to challenge the status quo of traditional care delivery methods, and we’ll continue to use data in new ways to improve quality. Our focus has been on systems and workflow, so from an enterprise analytics strategy standpoint, it’s going to be a heavy focus in the next three years to try to eliminate data silos and improve self-service reporting across our organization.
How does that change management component shape your overall leadership style?
One of the key characteristics in my role is simply listening and trying to understand what the need is from the provider, the tech, or the therapist. If you’re not listening, you’re not engaging. What I try to instill across my team is that it starts and ends with a level of trust that the organization has in us to hear them. We’re not only on the edge of the latest and greatest technology, but also helping them do their jobs better. It doesn’t come from having all the answers; it comes from helping smart leaders and providers derive the answers.
I truly can’t imagine doing any other job. I’m deeply passionate about the honor of serving as a CIO. We have a tremendous obligation to help facilitate better and more efficient care now more than ever. AHL
ONGOING EHR SUPPORT IS MISSION CRITICAL. IT IS NOT FUNDED BY CAPEX. AND IT’S FOREVER.

Optimum Healthcare IT has a dedicated Managed Services practice designed by leaders with deep experience standing-up successful EHR support models in complex organizations.
Our Managed Services offers the following solutions for your organization:
• EHR APPLICATION END USER SUPPORT
• EHR APPLICATION MAINTENANCE
• EHR PRACTICE SUPPORT
• IT & EHR SUPPORT MODEL ADVISORY
• VIRTUAL STAFF AUGMENTATION
Our service process allows us to streamline your organization’s IT needs into our industry-proven solutions which will work best with the infrastructure of your project.
ADVISORY SERVICES
EHR IMPLEMENTATION
TRAINING & ACTIVATION
COMMUNITY CONNECT
MANAGED SERVICES
SECURITY SERVICES
ANALYTICS
ERP
LABORATORY SERVICES
Our partnership started with Optimum right at the beginning of our Epic implementation several years ago now, and they have not disappointed since. The Optimum team and attention to service have elevated what I now expect from an advisory, systems optimization, and managed service partner.
VP CIO, SOUTHCOAST HEALTH

Optimum Healthcare IT can help you get there. Your success is our success.
By Jenny Draper
Essilor’s Ryan Murry reveals how the company’s innovative wellness program is impacting lives
Although Essilor is a world leader in eye care, Ryan Murry and his benefits team are proving the multibillion-dollar company’s expertise spans across the health spectrum. This commitment to providing comprehensive wellness benefits is part of the company’s promise to its employees to help every person make a difference for themselves so they can contribute to Essilor’s mission of improving lives by improving sight.
Murry is specifically targeting Essilor’s top areas of medical spend—circulatory conditions, diabetes, neoplasms, musculoskeletal injuries, and digestive issues—with a comprehensive health improvement strategy that is transforming what well-being looks like across Essilor’s 8,500-person US workforce. “We found that obesity is an underlying condition shared by every one of the primary drivers of our medical spend,” Murry says. “So, we set out to find programs that can achieve and maintain health improvement results for those with one or more of these conditions.” In addition to requiring results, Murry’s team vets potential program partners to determine the best cultural fit for their organization. He points to the success of Naturally Slim, a behavior modification program that teaches people skills around eating and how to interact with food. In the two years since its launch, more than one thousand employees have lost an average of ten pounds during the ten-week program. “We’re seeing our people not only keep the weight off, but also improve their lab values such as blood glucose, triglycerides, HDL cholesterol, and blood pressure,” he says.
Murry arrived at Dallas-based Essilor in 2005 and served in various HR roles until he shifted his focus to benefits management. After leading Essilor’s benefits strategy for two years, he expanded his responsibilities to include compensation and mobility.
“We can design and select all the best programs in the world, but if we don’t communicate them effectively, the programs will fail.”
“I’ve spent a lot of time building relationships with business leaders, which is very helpful when we’re rolling out programs and communicating information to the organization.”
“I’m not a benefits expert, and I think that helps me in terms of being able to look at things from a different viewpoint,” Murry says. “What I have learned during my time in benefits is that the most important aspect of the role is effective communication at all levels of the organization. We can design and select all the best programs in the world, but if we don’t communicate them effectively, the programs will fail.”
As Essilor implements each health improvement program, Murry and his team focus on employee engagement before, during, and after the initial rollout. The results are impressive: In just two years, Essilor increased employee utilization of annual preventive visits from 50 percent to more than 70 percent, on the way to an 80 percent utilization rate, Murry says.
“When you get more engagement, you’re able to drive costs down,” Murry says. “I’ve spent a lot of time building relationships with business leaders, which is very helpful when we’re rolling out programs and communicating information to the organization.” The increase in engagement in health improvement programs has
contributed to significant savings for the company, from $1 million year-over-year claims savings in 2016 to more than $4 million in savings for the self-funded medical plan in 2017.
Another important element of Essilor’s success is to integrate health program vendors and encourage them to coordinate with one another to improve the experience for employees. For example, Murry spearheaded the Wellness Vendor Summit, an event that presented Essilor’s mission, vision, and culture objectives to its health and wellness providers. It created the collaboration Essilor needed to create a diverse and comprehensive range of resources in a new one-stop-shop online wellness platform for Essilor employees.
Partnering with Evive Health, the new resource presents a personalized platform for employees. It simplifies their user experience while also reinforcing the first steps of the Wellness Program: to encourage and motivate employees to complete annual preventive visits and cancer screenings based on age and gender.
A key personalization component of the platform is the My Personal Health Assistant (MyPHA). This service provides individualized coaching and a personal health summary to those with chronic health conditions. “We’re connecting them to the right care,” Murry says. “We’re making sure they adhere to their care plans and are fully aware of all the resources we have available to help.”
Murry also points to other wellness program components that improve personalization and employee engagement. Essilor employees can access Airrosti, a muscle manipulation treatment, as an alternative to physical therapy. “It can help people avoid surgery and get relief from chronic pain,” he says. Another form of individualized support is the RN Cancer Guides who cater to employees with a recent cancer diagnosis.
Murry is excited about another recently implemented program that targets digestive health. The Clarity program helps people recognize and understand the symptoms caused by different types of foods. Then it provides a customized program to modify their diet accordingly and better manage their symptoms and conditions.
Looking ahead, Murry is turning his attention to financial wellness. He’s already consolidated more than twenty stand-alone 401K plans into a single plan, which has saved Essilor more than $200,000 while reducing legal liability. “We continue to look at financial wellness programs and resources as ways to enhance our employees’ ability to save for retirement,” he says. He is looking forward to expanding Essilor’s support of employees’ financial well-being as they prepare for the future.
“Our company improves people’s lives by improving sight—it’s an easy mission to get excited about,” Murry says. “It’s a very nice match with what we’re trying to do in the benefits department. We’re willing to try any programs to address the needs of our population, because we really want to make sure we’re providing the right tools and resources to help our employees also improve their own lives.” AHL
Airrosti partners with employers like Essilor to significantly reduce musculoskeletal spend. Airrosti provides quality musculoskeletal care shown to be highly effective at rapidly resolving most soft tissue injuries and conditions. Airrosti provides complimentary member engagement, education, and injury prevention/surgical avoidance programs designed to reduce the need for care. Visit us at airrosti.com

By Jeff Silver
Bernadette Melnyk shares her modest goal for improving the well-being of The Ohio State University—and every other campus in the country
In 2017, the National Academy of Medicine launched the Action Collaborative on Clinician Well-Being—a national initiative to raise awareness about the importance of clinicians’ well-being and the prevalence of increasing depression, compassion fatigue, and suicide among healthcare providers. At that point, The Ohio State University (OSU) was already well ahead of the wellness curve.
This wellness effort is spearheaded by Bernadette Melnyk, vice president for health promotion, university chief wellness officer, and dean of the College of Nursing. In fact, in 2011, Melnyk became the first university official in the US with the title of chief wellness officer (CWO).
Melnyk had been studying corporate wellness in her previous position as dean of the College of Nursing and Health Innovation at Arizona State University. During that time, she had come to the conclusion that universities needed to place more emphasis on wellness by entrusting such responsibilities to a CWO. Through discussions with the university’s president and provost regarding the ROI associated with a CWO position, the new role was created to improve population health and well-being for faculty, staff, and students.
“When I arrived, there were already many good wellness-related projects and initiatives in place,” Melnyk says. “What we needed was a comprehensive team vision and alignment of all the health and wellness
efforts that were going on across the entire campus.”
She immediately created the One University Health and Wellness Council, which brings together leaders from every entity involved in well-being efforts. In addition to health groups and HR, the council includes representatives from vice presidents and deans, faculty, university staff, marketing and communications, facilities, and graduate and undergraduate students. It gained tremendous positive momentum quickly as the participants created a holistic and comprehensive view of all their activities, developed a vision, mission, and strategic plan, a scorecard to monitor key outcomes, and shared their enthusiasm for working toward common goals.
The overarching goal is to make OSU the healthiest university in the world and to create a culture that makes healthy behaviors the norm. Melnyk and the council intend to accomplish this by leveraging evidence-based interventions, developing and coordinating clear and supportive communication, and enhancing grassroots efforts. They also are committed to sharing best practices with other universities across the country.
“Reaching our goals requires a multicomponent strategy that stretches from top leadership to the grassroots level,” Melnyk says. “Perhaps the most important piece is creating a culture that supports healthy behaviors that people usually have trouble sustaining on their own.”
Wellness initiatives have successfully been implemented at nearly every level. Individuals can work with health coaches who offer advice on healthy eating, physical activity, and stress reduction. Staff and faculty social networks are targeted


with events like the annual Family Wellness Expo. In the workplace, Melnyk’s team coordinates the Buckeye Wellness Innovator program—faculty and staff volunteers who coordinate wellness activity programming campus-wide. At the administrative level, Melnyk and the council focus on implementing and evaluating the strategic plan, including initiatives such as tobacco-free and flexible work policies.
Specific physical activity programming is a key component of Melnyk’s strategy. There are many intramural and college-to-college competitions—everything from “Amazing Races” to dodgeball tournaments. Incentives for consistent engagement in wellness activities are offered, as well.
OSU was the first university-wide partner with the Center for Disease Control and Prevention’s and
Department of Health and Human Services’ Million Hearts initiative. The program’s goal is to prevent one million heart attacks and strokes by 2022. Through related screenings and education programming, Melnyk says OSU’s overall cardiovascular health improved nearly 7 percent in four years.
Bernadette Melnyk participates in the Nursing ROTC Bootcamp at Ohio Stadium.
However, physical wellness isn’t the only focus. Initiatives also address emotional, financial, intellectual, career, social, creative, environmental, and spiritual health and well-being. Advisors from the business school are available to faculty and staff for financial consulting. A new campaign, Just Breathe, has just been launched for emotional wellness, and provides a website with resources on mindfulness, imagery, and stress reduction.
“The healthcare system in this country remains a sick-care system that only treats people after problems—many of them preventable—can’t be ignored.”
“There have been upticks in stress levels on campuses across the country,” Melnyk points out. “Because we emphasize evidence-based quality improvement, when we see indicators like that, we intensify our efforts to address them.”
This comprehensive focus has produced positive results for OSU’s bottom line. The university has achieved a negative healthcare spend when most organizations are experiencing more than a 4 percent increase. That resulted in more than $15 million in savings on health and wellness spending on faculty and staff.
According to Melnyk, OSU’s average ROI on each dollar invested in wellness is $3.65, near the top of the average returns reported by several national studies.
Melnyk also established the National Consortium for Building Healthy Academic Communities (NCBHAC) with fifteen other universities. Its mission is to implement comprehensive approaches to well-being for faculty, staff, and students that will improve the population health of the thirty-three million people who live and work in US academic institutions. More than three hundred leaders and ninety-three universities attended NCBHAC’s first conference.
“The healthcare system in this country remains a sick-care system that only treats people after problems—many of them preventable—can’t be ignored,” Melnyk says. “At OSU, I want to create a culture and environment that changes that, where healthy lifestyles and behaviors are so supported that lack of physical activity, unhealthy eating, smoking, and stress aren’t the underlying causes of death and disease anymore.” AHL Join Us
Learn more. Join the e ort to make the US a healthier nation. Create a culture of wellness on your campus. Learn best practices. Promote and sustain wellness in academic settings of all sizes. healthyacademics.org

By Anthony Ruth
How Eric Record, Steel Dynamics’ wellbeing and benefits leader, got seven thousand employees to care about health
Long before Eric Record joined Steel Dynamics, he knew of the company’s legendary status. Right near Record’s hometown in northeast Indiana was a new steel company using a new technology, with a reputation as a good employer that paid good wages. All steel producers compete on cost; for Steel Dynamics to stand out, it became safer, more innovative, and built a culture of engagement.
“Engagement is the key that runs through everything,” Record says. “It brings open communication that supports innovation, supports continuous improvement, supports pointing out when things are going well and when things could be done better,” he says.
Among those things that could be done better was Steel Dynamics’ benefits plan, which included only one health plan. “Set it and forget it,” is how Record describes the old plan. “It didn’t require a lot of engagement or thought.” That model no longer worked for a company that had grown to more than seven thousand employees. “There needed to be more flexibility in what was offered,” Record says. “Not everybody has the same family or financial needs.”
When Record came on board as Steel Dynamics’ first wellbeing and benefits leader, one of his charges was to bring the company’s culture of engagement to its benefits plans. A key strategy in revamping the health plan offerings was to incentivize behaviors that improve health, prevent illness, and can reduce healthcare costs down the road. With the new plans, Steel Dynamics deposits “Dynamic Dollars” into its employees’ health savings accounts for wellness acts such as getting an annual physical or a biometric screening.
The transition took years, rolling out one new plan at a time. “We had the advantage of an engaged workforce to begin to cultivate a culture of health,” Record says.
“But the fact that it was rolled out over time, that it was communicated again and again, that we took the time to both educate and listen to employees as we implemented changes—that made the difference.”
A major component to the new healthcare offering is Castlight, an online tool that hosts all of an employee’s benefits in one place and makes it easier for them to review their claims, find providers, and research other cost and quality information. Nearly 90 percent of Steel Dynamics’ health plan participants have registered for the tool, which Record says is an industry-leading number.
Steel Dynamics also began offering employees virtual healthcare options, making it easier for employees who work long shifts to squeeze in a video visit with their doctor, or for employees with specific health conditions to interact with specialists.
Technology and data have helped Steel Dynamics make employee healthcare more individualized overall. “We’re not just getting a newsletter with general information,” Record says. “Participants get a unique experience, tailored to them, to help engage them in their health.” For example, Record gets an alert on his phone when it’s time for his preventive physical or a biometric screening.
To further connect Steel Dynamics’ culture with employees’ tangible benefits, Record created “Dynamic Rewards,” a total rewards program that encapsulates the entire value proposition for employees. “It’s one of the first things reviewed in new employee orientation,” Record explains. “Dynamic Rewards reminds people that work is not only about the paycheck or benefits. It’s also about giving folks the tools to create a safer, more productive working environment. It’s also about career opportunities.”

From your partners at Anthem.
As a result of these initiatives, Steel Dynamics has seen improvements in key health measures such as increased preventive health screenings, better prescription adherence, and a decrease in unnecessary ER visits. Even better, Record says, is that he’s seen an overall increased interest in well-being across the organization.
Record says other companies looking to innovate should think about building on existing cultural strengths and use them as springboards to the innovations they want to implement. “If you do that and you communicate, if you really listen and adjust as you go along, you will be in a good position to succeed and create something that’s meaningful and engaging,” he says. “How you engage with employees, that ends up being the secret to success.”AHL

It takes innovative spirit to drive continued success over ten years. At Steel Dynamics, Eric Record has spearheaded initiatives that have cultivated impressive engagement throughout many wellness and benefits programs. Anthem is honored to partner with Steel Dynamics and proud to say that Eric Record embodies innovation that endures.
BenefitWallet , A Conduent Company, is proud to partner with Steel Dynamics to deliver our health savings account (HSA) solution, helping employees prepare for retirement by saving and investing in their account. As one of the nation’s top providers of health accounts, we help millions of Americans lower their taxes today and save for healthcare expenses in the future.

Profi le shares the stories of the modern executive.





Share your story of exceptional leadership with our network of powerful business leaders.






By Clint Worthington
Northwell Health’s John Bosco uses new mobile technology to drive consumer engagement and build a comprehensive medical information exchange
Managing the largest integrated healthcare network in the state of New York—and one of the largest in the nation—takes a detailed understanding of patients and the ability to use information technology to address their needs. At Northwell Health, senior vice president and chief information officer John Bosco takes this responsibility extremely seriously. Throughout his nearly forty-year career in healthcare IT, he has worked to facilitate effective, high-quality service delivery at every organization he has worked, and Northwell is no exception. As the organization continues to refine its use of digital apps to drive consumer engagement, Bosco takes an active role in streamlining care for increasingly specific patient needs.
“Studies show that many people want their healthcare needs met digitally,” Bosco says. At Northwell, a significant part of that is the creation of comprehensive digital solutions, including a mobile app that offers patients easy access to everything they need to manage their care. Beginning its launch in 2018 and continuing
into 2019, the app’s goal is to allow each patient to create a detailed profile of themselves and their preferences, view their records, including previous visits, medical information, and educational materials on potential issues they might be having. In addition, the app allows patients to schedule appointments, check in and out of Northwell facilities, organize follow-up care, and pay bills online. In the future, the platform will also allow patients to connect to digital services for at-home care and have in-room features for patients during a hospital stay.
This project is a particular point of pride for Bosco, who strives to make the process as intuitive as possible for patients. “There’s no reason to go anywhere outside of Northwell if we do our jobs right,” he says, emphasizing the need for accessibility and easy navigation to build patient loyalty. For instance, Northwell delivered nearly thirty thousand babies in New York State alone this year. With the app, profiles will be built out for both mother and baby, providing a single, convenient place to manage care for the whole family. Bosco and other teams including marketing and the digital office will also use the app to make their patients feel they know them and their preferences intimately, which keeps them coming back.
“Few organizations are as strategic and forward-thinking as Northwell Health,” says Don Woodlock, head of the HealthShare business at InterSystems.
“Under the leadership of John and his colleagues, and powered by our HealthShare suite of connected health solutions, they have agility, innovation, and a passion for advancing patient care through IT.”

“There’s no reason to go anywhere outside of Northwell if we do our jobs right.”
In addition to the mobile app, another key mission has been to create a connected, integrated health network at Northwell. Using their internal health information exchange (HIE), healthcare professionals at Northwell can connect data from various EHRs and insurance claims, allowing clinicians and care managers to have a centralized hub for viewing patient information. The HIE “connects every corner of our health system,” says Bosco, linking everything from hospitals to imaging centers to the same data. This becomes especially helpful as Northwell continues acquiring new practices, surgery centers, and more, as well as its connection to the New York State health network. “It’s our most critical IT asset,” says Bosco. “We’re really proud.”
As new generations of patients grow up with technology as an important part of their lives, systems like these will become important to healthcare organizations. “Millennials expect a different experience; in the future they’re likely to only use a place that makes the experience convenient and mobile,” he says. Organizations across the industry are pouring many investment dollars into these processes, Bosco notes,
so it is critical that Northwell stays ahead of the curve to survive. In its quest to improve care delivery for patients, Bosco and Northwell look to some of its trusted vendors for support.
“Allscripts delivers healthcare organizations IT solutions for smarter care delivery—for healthier patients across their communities,” says Paul M. Black, CEO of Allscripts. “As a trusted partner to Northwell Health, we keep the focus on strengthening clients’ clinical and financial foundations for unparalleled patient outcomes.”
Consequently, Bosco is currently working on areas for future projects, in addition to refining Northwell’s mobile app and HIE. The organization is working on a number of other consumer engagement initiatives, including a partnership with healthcare company Conversa to allow Northwell to interact with patients after they have left. The goal is to provide further information about follow-up appointments, check in on their understanding of new prescriptions and medications, and more. Bosco believes these reminders are crucial for providing the best possible care for their patients.

Northwell Health, New York’s largest integrated health system, partnered with InterSystems to support seamless care and population health management.
Data from Northwell’s diverse clinical and administrative
systems is collected, aggregated, and delivered to clinicians in real time, facilitating the delivery of high-quality, coordinated patient care across the enterprise.
Learn more at InterSystems.com/Northwell
Before pursuing a career in healthcare, Bosco was almost a professional musician. “Growing up, I was only focused on being a classical pianist,” he says. Bosco took piano lessons and went to music schools throughout his youth. He auditioned at several music schools, such as Carnegie Mellon, and was even accepted into a few, before changing his mind at the last minute to pursue business school. “I kept playing after that, but I guess I never truly thought I could be one of the best,” Bosco says. He hasn’t played much in the ensuing decades—nowadays, he spends his free time in the outdoors as an avid downhill snow skier and hiker.
“Too many patients don’t make follow-up appointments or don’t take medications as directed,” he says. “Eventually, they end up back in the ER or the doctor’s office.” Furthermore, Northwell runs a clinical call center staffed with nurses, which patients can call to ask questions whenever they need.
These initiatives and more are designed to bring the healthcare expertise of Northwell’s staff outside the doctor’s office and into patients’ everyday lives. “We view the patient’s home and office as an extension of our health system,” Bosco says.
This passion to cultivate the best possible care for his patients extends to Bosco’s passionate, motivational leadership style. “I want employees to feel motivated and inspired every day they come to work,” he says. Foremost among his priorities is to help his staff understand their impact not only on Northwell, but directly with patients. “I don’t want them coming in every day as IT people, only caring about taking care of the network or some app,” Bosco says. “If just one of our 1,800 people indirectly makes a positive impact for our patients, whether by giving them a digital app or making sure clinicians have the tools they need, it’s worth it.”
To do this, Bosco cultivates a sense of familiarity and positivity within his department, hosting regular meetings to check in on staff and to make them feel valued. “I’m supposed to be the person with the vision; my teams make the vision happen,” he says. “It’s my job to motivate and inspire them every day when they come to work.”
Whether through strong, transformational leadership or the IT department’s work building consumer engagement, Bosco works hard to fulfill Northwell’s mission of providing the best possible care for its patients. Luckily, his passion is standard practice for the company at large. “I can’t emphasize enough how great a feeling it is to work at Northwell,” says Bosco. “At every departmental meeting, the discussion always goes back to what’s best for the patient.”AHL

Dr. Thomas Moran discusses how Northwestern Medicine’s Project One reflects broader industry trends surrounding EMRs and clinical data
By Joe Dixon | Portrait by Cass Davis

Dr. Thomas Moran, Northwestern Medicine’s vice president and chief medical information executive, and American Healthcare Leader ’s guest editor this issue, was a critical leader throughout the organization’s Project One, an initiative to unify all of its care locations across various regions on to one EMR.
Moran worked closely with the Northwestern’s physician and nurse leaders featured in this issue: Dr. Cord Sturgeon, Dr. Steve LoBue, Dr. Nancy Sassower, Lea Ann Arnold RN, and Dr. Lacy Knight, as well as Dr. Ranya Sweis, Dr. Phil Roemer, Dr. Tom Krejcie, and Dr. Andrew Naidech to devise the strategy to gather and disseminate information, train clinicians, and implement a new system-wide EMR. Read more about these leaders’ work beginning on p. 101
Moran spoke with American Healthcare Leader on how Project One came together, trends he is seeing with EMRs in healthcare organizations across the country, and how he thinks the next evolution of the EMR will manifest itself.
I was the system lead that coordinated a team that drove Project One from a clinical approach instead of an IT-led approach. We focused on what was needed to deliver a system that physicians and nurses and other caregivers would utilize to help care for patients safely and efficiently.
The clinical project leads organized an approach by partnering with nurses to come up with workflows that meet the needs of our patients, our physicians, our nurses, and the staff that work with them. We took a patients-first approach and focused on the patient experience as they move through our organization, as
well as understanding the specific experiences and nuances of each department across the organization.
How were system leaders selected for this initiative?
As a system that was growing by mergers throughout the project, we had a variety of different campuses throughout the system, from a 26-bed critical access hospital to a 850-bed academic medical campus. We needed to ensure each area or campus had a voice, so we looked to leaders from each area to provide the best individuals to best represent each campus.
These individuals had to have local knowledge, influence, and communication skills, as well be able to think about solutions at a system level. Responsibilities included messaging decisions to their local campus, gaining buy-in from the clinicians who work there, and providing feedback to the project team on issues or concerns.
What was the impetus behind Project One?
Providing a single, shared clinical record to help our clinicians facilitate and provide safe, world-class care to our patients where they live and work. Without a shared clinical record, clinicians have barriers in front of them that make it difficult to ensure they have the most relevant information available for each patient. Without having that information, care becomes inefficient for the patient, inefficient for the physicians and nurses caring for them, and it causes the patient to feel disconnected from their caregivers and the organization. The focus is on the patient and the patient’s needs; this means we have to provide the clinicians necessary information through a shared clinical record.
“Without a shared clinical record, clinicians have barriers in front of them that make it difficult to ensure they have the most relevant information available for each patient.”
What do other health systems debating an EMR overhaul like this need to consider?
I think the biggest, most important thing is to lay out and understand the scope and the impact that the project is going to have on the people who will use the tools. Be transparent and honest with them about the intent of the project so they work with you in developing the workflows that support safe, efficient care while capturing the revenue for the work they do.
No one likes things done to them, people like to be able to help contribute solutions to a problem. I think if you’re transparent enough and laying out what the goals are, you can get clinicians to come through and standardize more than you think. They just want to be part of the process.
What do you see for the future of the EMR?
I think the EMRs we use right now are a product of our past. They have been built for billing and coding, not for clearly conveying clinical information. I think we are going to need to make the shift to patient-bound care, which is care that gives the patient the ability to initiate data collection for the benefit
of their own health. From there, we can set up clinical care plans to guide them and begin to have them self-manage their health with our oversight, because the majority of a patient’s time isn’t spent in a hospital or a physician’s office.
Our goal is to keep patients out of the office, and to do that we need to give them tools to record their health information—such as wearables, scales, and blood pressure and glucose devices— to help them and us track how they’re doing more frequently against their baseline. Then, we can close the loop by providing patients with a guided care plan to help them understand when they are on track, doing well, and should stick to the care plan. At the same time, we can tell them when they are off track and it’s important to modify their care plan or necessitate a need to come in for a visit.
The industry has been too focused on when and where patient care is going to take place instead of turning the focus toward using a patient record that is updated by the patient and that acts a dashboard of the patient. The first page should be all a physician needs to manage a patient and understand what is going on with their health. That same dashboard should allow patients to participate and understand their health. AHL
About six months after Project One's successful rollout, the Northwestern Medicine team came to our photo studio to share some laughs and jokes with us.
Read more about Project One on p. 101
The Northwestern Medicine team takes a break from posing for photos to hydrate and tell some jokes

While waiting for his turn in front of the camera, Cord Sturgeon entertains his colleagues with Family Feud- style questions .


Caring for patients takes heart. It also takes a strong, modern network — one that is constantly learning, adapting, and protecting. With the right technology foundation, you can care for your patients one at a time, and all at once. At the heart of it, isn’t that what it’s all about?
Visit cisco.com/go/healthcare to learn more.