SOCIAL PRESCRIBING


ISSUE 4 VOLUME 14 | JULY-AUGUST 2021 O LANRUOJLAICIFF • OLANRUOJLAICIFF • O FFICIALJOURNAL • OFFICIALJOURNAL •
How social prescribing can help patients and busy healthcare practitioners An interview with Prof Fiona Lyons, HSE Sexual Health and Crisis Pregnancy Programme HIV AWARENESS
overview of the need for adequate folate intake FOLATE
An
APTAMIL TODDLER MILK


For more information, call our dedicated freephone on 1800 22 12 34 or visit nutricia.ie
This information is for healthcare professional use only. Aptamil Toddler Milk should be used as part of a varied and balanced diet from 1 year. Recommended serving per day is 300ml.
1. Irish Universities Alliance (IUNA), National Pre-school Nutritional Survey. Further analysis for Danone Nutricia (data available on request). Main survey available at: https://www.iuna.net/surveyreports 2. Food Safety Authority of Ireland (FSAI), Scientific Recommendations for Food-Based Dietary Guidelines for 1 to 5 Year-Olds in Ireland. Available at: https://www.fsai.ie/Dietary_Recommendations_1-5_Year_Olds/ 3. Food Safety Authority of Ireland (FSAI), Recommended Dietary Allowances for Ireland 1999. Available at: https://www.lenus.ie/handle/10147/44808
information is for healthcare professional use only.

June 2021
Aptamil
1 year.
serving per day
300ml. 1. Irish Universities Alliance (IUNA), National Pre-school Nutritional Survey. Further analysis for Danone Nutricia (data available on request). Main survey available at: https://www.iuna.net/surveyreports 2. Food Safety Authority of Ireland (FSAI), Scientific Recommendations for Food-Based Dietary Guidelines for 1 to 5 Year-Olds in Ireland. Available at: https://www.fsai.ie/Dietary_Recommendations_1-5_Year_Olds/ 3. Food Safety Authority of Ireland (FSAI), Recommended Dietary Allowances for Ireland 1999. Available at: https://www.lenus.ie/handle/10147/44808 For more information, call our dedicated freephone on 1800 22 12 34 or visit nutricia.ie MORE THAN 90% OF 1-3 YEAR OLDS IN IRELAND DO NOT GET ENOUGH VITAMIN D1 New FSAI Dietary Guidelines for Toddlers 2020 Fortified foods and drinks can contribute to the intakes of Vitamin D, Iron & Omega 3 in toddlers2 Just 2 beakers a day (300ml) of Aptamil Toddler milk provides toddlers with 93% of the RDA3 for Vitamin D and 45% of the RDA3 for Iron Available in 800g powder, 200ml & 1 litre liquid June 2021 Toddler Milk
This
Toddler Milk should be used as part of a varied and balanced diet from
Recommended
is
A SUMMER OF STAYCATIONS AND HOPE
Dear Readers,
Welcome to this issue of Nursing in General Practice. I hope you are all managing some time off during the summer months to recharge the batteries following an extremely busy and stressful number of months with a national mass vaccination programme and the cyber-attack.
In this issue, the featured articles include folate awareness, melanoma, social prescribing, allergic rhinitis, dry skin, and HIV.
In Ireland, the concept of social prescribing is a relatively new one. It has been widely used in the UK for a number of years with proven benefits. As general practice nurses, we have, unknown to ourselves, used the core principles of social prescribing in supporting people in obtaining and maintaining physical and mental wellbeing long before it became ‘fashionable’ by encouraging people to partake in various activities and support groups.
Also featured in this issue are the findings of a survey undertaken by the Asthma Society of Ireland as part of World Asthma Day in May of this year. The survey explored patient experiences during the pandemic, which revealed some interesting facts.

Some of findings include:
50 per cent of those surveyed had had an asthma attack in the past year.
14 per cent had experienced an attack in the past four weeks alone, 19 per cent in the past six months and a further 16 per cent in the past 12 months.
Worryingly, 26 per cent of respondents said that they had avoided attending an emergency department with their asthma despite experiencing an acute asthma flare-up.
71 per cent of those surveyed said that they were concerned about
contracting a more severe form of Covid-19 as a result of their asthma. This may account for the fact that 38 per cent also admitted that they have avoided support or healthcare services in the past year as they were concerned about the impact of Covid-19.
All those surveyed were taking asthma medication, but 80 per cent felt that their asthma was not considered to be a life-threatening condition by the general public. Only 20 per cent of people felt their condition was taken seriously as an illness by family and friends and just 13 per cent felt it was taken seriously as an illness at work.
These findings are of major concern. Frequently, I hear the comment that it is just “a touch of asthma” or “it’s very mild”. We really need to change these attitudes as Ireland has one of the highest prevalence rates of asthma in the world with one-in-10 children and
one-in-13 adults living with the condition. Experts would agree that there is no such thing as mild asthma and all patients with asthma should be managed and cared for as having a potentially life-threatening condition.

The key to this is ongoing regular reviews, self-management support and education. We know from the National Review of Asthma Deaths in the UK (2014) that it is people with “so-called” mild asthma that are dying from asthma as their condition isn’t taken seriously by family, friends or health professionals. In future guidelines, the Global Initiative for Asthma (GINA) will address the definition of mild asthma, which is to be welcomed (GINA, 2021).
I hope you all have a lovely summer and get a chance to enjoy our beautiful country with your family and friends during these uncertain times.
Welcome JULY-AUGUST 2021 1
A message from Ruth Morrow, Consulting Editor
Contents
EDITOR
Priscilla Lynch
CONSULTING EDITOR
Ruth Morrow
SUB-EDITOR
Emer Keogh emer@greenx.ie
ADVERTISEMENTS
Graham Cooke graham@greenx.ie
ADMINISTRATION
Daiva Maciunaite daiva@greenx.ie
04 NEWS
NEC and Irish healthcare news
12
Please email editorial enquiries to Priscilla Lynch priscilla@mindo.ie
Nursing in General Practice is produced by GreenCross Publishing Ltd (est. 2007).
© Copyright GreenCross Publishing Ltd. 2021
DRY SKIN AND DERMATITIS
Eamonn Brady, MPSI, discusses the most common dry skin conditions and the different treatment approaches
16
MELANOMA
Theresa Lowry-Lehnen gives an overview of melanoma incidence, diagnosis, treatment, and prevention
21
Please email publishing enquiries to Publisher and Director, Graham Cooke graham@greenx.ie
HIV
An interview with Prof Fiona Lyons , Clinical lead of the HSE’s Sexual Health and Crisis Pregnancy Programme, about challenges and developments in HIV detection and care
25
The contents of Nursing in General Practice are protected by copyright. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form by any means – electronic, mechanical or photocopy recording or otherwise –whole or in part, in any form whatsoever for advertising or promotional purposes without the prior written permission of the editor or publishers.
DISCLAIMER
The views expressed in Nursing in General Practice are not necessarily those of the publishers, editor or editorial advisory board. While the publishers, editor and editorial advisory board have taken every care with regard to accuracy of editorial and advertisement contributions, they cannot be held responsible for any errors or omissions contained.

ASTHMA SUPPORT

Sarah O’Connor, CEO of the Irish Asthma Society of Ireland, outlines how the society has been supporting asthma patients during the pandemic
27
27
29
FOLATE AWARENESS
Anna Wedderburn presents an overview of the need for adequate folate intake and its effects on overall health
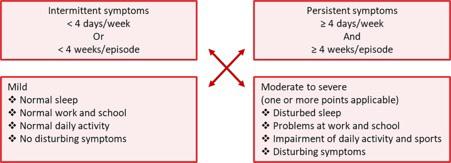
ALLERGIC RHINITIS IN FOCUS
Theresa Lowry-Lehnen looks at the different presentation and stepwise treatment approaches to this common condition
33
SOCIAL PRESCRIBING
Theresa Lowry-Lehnen explains the rationale behind social prescribing and the importance of high quality research and comparative evaluation
37 FOOD
Tom Doorley looks at the complexity of calories
38
33
39
40
FINANCE
Paul Redmond examines day-to-day banking options following the recent departure of some banks from Ireland
PRODUCT NEWS
A round-up of the latest product news
CROSSWORD
Test your word knowledge
2 JULY-AUGUST 2021
DRY & ROUGH SKIN UNDER CONTROL, FROM HEAD TO TOE















































Clinically proven for use all over the body with moisturising and keratolytic formulations even for plaques associated with psoriasis.





































Let your skin benefit from U-LifeTM, the one-stop solution with moisturising and keratolytic action for the management of dry, very dry, and chapped skin in specific areas of the body. U-LifeTM creams and anhydrous pastes are formulated with different urea percentages plus other specific ingredients to meet your skin’s needs and target specific areas (scalp, face, body, hands and feet).
















































RELIFE ™ MY SKIN SAYS HOW I FEEL.
Date of Item Dec 2020 IE20071 IR-REL-120-2020
WWW.RELIFE.IE
NEC NEWS
JOB OPPORTUNITY
Membership Officer: 7.5 hours per week. This will be a paid role with the candidate being employed directly by IGPNEA. This is an exciting opportunity for someone with the drive and eagerness to participate in and contribute to the growth of our organisation. Please spread the word, or if interested please send your CV to admin@ irishpracticenurses.ie You can find more details on our website.
WEBSITE AND SOCIAL MEDIA OFFICER
At the time of going to press we have offered a contract for the Website and Social Media Officer role. We will provide you with details and an update as soon as we have everything finalised.
MEMBERSHIP
A warm welcome to our new members, we now have over 950 members; our highest ever membership.
SIILO
Over 50 per cent of members are now using Siilo for secure messaging and news alerts. All members are asked to download the Siilo app today. Siilo works like WhatsApp, but specific for our needs. With security and privacy ensured, it a great way to communicate with your branches, find out what is happening within IGPNEA, and get news alerts such as Covid-19 vaccine bulletins.
To get Siilo on your phone
1. Go to the Play store or Apple store on your phone.
2. Download Siilo – Medical
3. Open the app and follow the steps on your phone once downloaded.
4. You can choose to import your phone’s contacts or not (your choice).
5. As an IGPNEA member, you are automatically verified for our network.
6. To access the full Siilo network (ie, people outside IGPNEA), you must verify your account with passport and ID. If you choose not to verify your account you can still access IGPNEA news, etc, and communicate with other members.
7. Enter your NMBI number (this may say IMC number).
8.You will then be added to your branch group on Siilo.
IGPNEA WEBINARS
We hope you are enjoying the IGPNEA webinars in partnership with www.medcafe. ie. The monthly webinars have been a great success and feedback from members has been very positive. Our most recent webinar on June 29 ‘Not my monkey – Transactional
analysis and knowing yourself’ with guest speaker Nurse Patricia McQuillan, Professional Development Co-ordinator for Practice
Nurses in the South East (CHO 5), provided great insight and understanding about the impact of people and events on our lives, an understanding of what triggers certain personal behaviours, and knowing how to respond rather than react to certain behaviours.
The webinar on ‘CDM – Heart failure', which was due to take place on July 13 with guest speaker Norma Caples, has been postponed until later in the year. However, we are pleased to be hosting a webinar on July 27 with guest speaker, GP and pharmacist Dr Paul Ryan, on the topic of polypharmacy. So save the date, for what promises to be another very interesting talk. That webinar will be our last for the summer season. We will take a break for August and be back with more webinars in the autumn. Recordings of our webinars are available for members on our website and at www.medcafe.ie

EDUCATIONAL HUB
More areas are now live on the Hub: Mental health, men’s health, respiratory, and cardiovascular are the most recent additions. The Hub is the quick find resource centre on the IGPNEA website for our educational materials. Sixteen out of the 20 areas are now active on the Hub and resources continue to grow as more content is added regularly. Each Hub has a variety of learning resources, e-learning courses, links to webinars and IGPNEAproduced educational material, including video presentations and articles.
VOLUNTEER PANEL
Many thanks to those of you who responded to our call for volunteers; we really appreciate your willingness to get involved and are delighted with the uptake. The role of volunteer liaison person is still open, the panel will remain open for this role and any future opportunities as they arise so please contact Mary via email (admin@irishpracticenurses.ie) at any stage if interested. We’d love to hear from you.
REMINDER TO SAVE THE DATE FOR AGM 2021 AND CONFERENCE 2022
The AGM this year will be held on Saturday, 16 October 2021 and it will be a virtual format similar to last year. We are delighted that the Waterford Branch will be hosting our next conference on Friday, 13 and Saturday, 14 May 2022 in the Tower Hotel in Waterford. Put the dates in your diary. We’re looking forward to an interesting programme and of
News 4 JULY-AUGUST 2021
Messenger
course the chance to meet up at the conference.
CHANGES TO ARTICLES OF ASSOCIATION
Thank you to all the Branch Representatives and our members who took time out of their busy schedules to attend our virtual EGM on June 10, where the following motions were passed: Motion 1: Articles 6.1 (+ 9.1, 9.2, 9.3) – New centralised bank account for branches. Motion 2: Article 14.4.1 – Adding in the option of a virtual AGM if circumstances don't allow a physical AGM. Motion 3: Article 17.2 –Inclusion of an EGM.
We are working on the
necessary processes to make the changes to the Articles of Association and have them approved by the Charities Regulator before they can be fully implemented within the IGPNEA procedures.
THE PEOPLE'S VACCINE ALLIANCE IRELAND
We are very pleased to be supporting Oxfam Ireland's new campaign: The People's Vaccine Alliance Ireland. The fairest and most effective way to end this pandemic is to ensure that everyone, everywhere has access to Covid-19 vaccines, tests and treatments. Oxfam's new campaign is aiming to achieve this.
SUMMER CLOSURE
IGPNEA will be closed for two weeks to allow for staff annual leave from July 12 to 27. During that time if there is anything very urgent
please email chair@ irishpracticenurses.ie
TWITTER
Don’t forget to follow us on Twitter @PracticeNurses . We now have over 1,650 followers.
CORRECTIONS FROM THE LAST ISSUE OF NIGP
1.There was a misprint in one line in last edition’s article: The Menopause: An overview. The line should read- “The average duration of hot flushes occurring in women is 5.2 [NOT 52] years, however, symptoms of lesser intensity may be present for longer.”
2. In the NEC news piece about the 2022 IPGNEA conference, it should have said Tower Hotel in Waterford as the venue for the conference in May 2022, not Talbot Hotel. Apologies.
SURVEY SHOWS THAT 30 PER CENT HAVE NEVER SPOKEN TO A HEALTHCARE PROFESSIONAL ABOUT THEIR ALLERGIES DESPITE EXPERIENCING FREQUENT SYMPTOMS
The Asthma Society of Ireland has shared the findings of a patient and carer survey, which highlighted that despite experiencing multiple hay fever symptoms, 30 per cent of respondents had not sought advice from their healthcare provider on managing their allergies.
Of those who have been diagnosed with allergies, the most common allergies were pollen (63 per cent) or house dust mites (56 per cent). Over 33 per cent of respondents reported a diagnosis of allergy to pet or animal hair whilst over a fifth had confirmed allergies to certain foods.
Some 304,000 people in Ireland have both asthma and hay fever, which can significantly affect quality-of-life.
Sneezing, stuffy nose, and runny nose were commonly experienced amongst the 655 patients surveyed. Of the symptoms most frequently experienced, 92 per cent cited urge to sneeze or sneezing fits, 91 per cent runny nose/rhinitis, 88 per cent stuffy or itchy nose, and 74 per cent of respondents reported itchy burning eyes.
Some 79 per cent of respondents also report experiencing fatigue associated with allergies; for some patients, tiredness can be caused by certain antihistamines and not the condition itself.
Dr Marcus Butler, Respiratory Consultant at St Vincent's University Hospital, Dublin, and Medical Director at the Asthma Society of Ireland, said: “The
findings are concerning for the asthma population in Ireland as while all of those surveyed reported experiencing asthma symptoms, 30 per cent had not sought advice from their healthcare practitioner in managing their symptoms.
“While the symptoms are frustrating for many, unmanaged hay fever or allergies can cause asthma symptoms to heighten and escalate into an asthma attack. An asthma attack is a respiratory emergency that should be taken seriously by patients and carers. Allergies and hay fever with asthma can be fatal. At least one person dies every week as a result of asthma.
News JULY-AUGUST 2021 5
NEWS
“Our research showed that 50 per cent of those surveyed had had an asthma attack in the past year – 14 per cent had experienced an attack in the past four weeks alone, 19 per cent in the past six months and a further 16 per cent in the past 12 months. So good hay fever management is crucial in preventing an asthma emergency.
“We really encourage patients to kickstart an improvement of their hay fever symptoms and better asthma control by flagging these symptoms with their
GP. The results of this survey indicate that there would be a real value to all GPs routinely asking the following question with an asthma patient – 'and, what about the nose'. If patients and GPs don’t discuss these symptoms, then they can’t create a plan for managing them."
Ruth Morrow, Respiratory Nurse Specialist at the Asthma Society of Ireland said: “Spring and Summer are the peak times for people with hay fever with 51 per cent reporting increased symptoms at this
high pollen time, that can really impact on quality-of-life and asthma management. Lying in bed at night and being close to meadows, fields or trees can further aggravate symptoms.
“The ALK supported pollen tracker on www.asthma.ie helps us to highlight when periods of high pollen or bad weather are coming up so people with hay fever can better manage their symptoms. We have also put together a number of practical tips for management of hay fever symptoms.”
IBS PATIENTS DO NOT HAVE INCREASED MORTALITY RISK
PRISCILLA LYNCH
Having irritable bowel syndrome (IBS) does not put one at increased risk of premature mortality, the recent Irish Society of Gastroenterology (ISG) 2021 Summer Meeting heard.
Dr Kyle Staller, Gastroenterologist/ Neurogastroenterologist Director, Gastrointestinal (GI) Motility Laboratory, Massachusetts General Hospital, Boston, US, gave an update on the latest approaches in IBS.

IBS affects an estimated 10-15 per cent of the population with substantial impacts on quality-of-life and work productivity and is one of the most common presentations to gastroenterologists, he noted.
Fear about the potential serious nature of bowel symptoms may underlie much of the explanation for seeking care for IBS, and the literature suggests that more than half of IBS patients fear that their illness will shorten their lifespan.
Despite clear diagnostic criteria, such as the Rome IV definition, which Dr Staller feels can be too strict, most clinicians consider IBS a diagnosis of exclusion, and over 50 per cent of patients with IBS will undergo colonoscopy at some point in their diagnostic workup given fears over missing something more serious like cancer.
To address this issue, Dr Staller and colleagues used a nationwide Swedish histopathology register to conduct a matched population-based cohort study to examine
the overall risk of death in individuals with IBS (over 45,000 people) undergoing colorectal biopsy compared to matched reference individuals. In a secondary cohort, they examined mortality in IBS patients without biopsy.
After adjustment for confounders, IBS was not linked to mortality (HR=0.96; 95% CI=0.92-1.00). Risk estimates were neutral when IBS patients were compared to their siblings. Underlying mucosal appearance on biopsy had only a marginal impact on mortality, and IBS patients without
colorectal biopsy were at no increased risk of death (HR=1.02; 95% CI=0.99-1.06). There was no link to increased cancerrelated death either.
“Now this is not scientifically groundbreaking, but what I think it tells us is that we need to spend more time focusing on what is the diagnosis, rather than what is it not, and what treatment options can we offer these long-suffering patients,” Dr Staller commented.
In that regards, the recommended diagnostic approach in IBS should include faecal calprotectin testing in those with diarrhoea symptoms, Coeliac testing, for those due a colonoscopy; random colon biopsies to assess for microscopic colitis, and malabsorption bile acid testing, he said. Small intestinal bacterial overgrowth (SIBO) testing should be retired he said, based on the latest data, while routine colonoscopy is unnecessary for those with standard IBS symptoms.
Alarm symptoms for further testing include iron-deficiency anaemia, blood in the stools, older age, unintentional weight loss, palpable abdominal mass, and family history of organic GI disease.
Dr Staller shared interesting data showing the association between psychological conditions and symptoms (anxiety, early life trauma, etc), and the development of IBS and disease severity; and he reminded delegates of the biopsychosocial model (and brain/gut
News 6 JULY-AUGUST 2021 NEWS
Dr Kyle Staller
axis) of GI disease.
Regarding treatment, beyond motility agents, he cited data for gluten-free and FODMAP diets, which showed that FODMAP diets have good results in addressing symptoms, while probiotics are likely to provide some benefit with, on the whole, products containing Bifidobacterium (either alone or in a combination) showing good efficacy. Though he noted that the quality of data on probiotics remains inadequate and contradictory.
While there is a lot of interest in faecal
microbiota transplantation (FMT), it has shown mixed results to date “and it is not necessarily benign either”, so the jury is still out, Dr Staller reported, adding that there is a lot more to learn about the role of the microbiome in relation to IBS.
Neuromodulators (“so off-label use of antidepressants like SSRIs”) can have a role in some patients.
Looking at non-pharmacological approaches for the treatment of IBS symptoms, Dr Staller said that cognitive behavioural therapy (CBT) and
hypnotherapy have been shown to be effective in studies. “Of course, the problem in Ireland and the US is a lack of available therapists who are skilled in managing IBS.” That said, he noted that there are new apps that provide CBT support for IBS symptoms with more in development.
For those with severe IBS symptoms, Dr Staller said “a multidisciplinary approach really targeting the brain/gut axis” is necessary, and commented that he is seeing a lot of younger females recently with significant symptoms and disability.
GOOD UPTAKE OF NEW HAEMOCHROMATOSIS VENESECTION SERVICE IN GENERAL PRACTICE
PRISCILLA LYNCH
The long-awaited roll-out of the HSE general practice venesection service for haemochromatosis patients has been very successful to date, with high up-take especially in more rural and peripheral areas, according to Prof Suzanne Norris, Consultant Hepatologist, St James’s Hospital, Dublin.
Prof Norris gave an update on the condition at the virtual Irish Society of Gastroenterology (ISG) 2021 Summer Meeting, where she presented data on the GP therapeutic phlebotomy service for eligible haemochromatosis patients, which only formally launched in 2020, following its approval in the HSE’s 2017 Model of Care for hereditary haemochromatosis (HH), and the necessary GP contract negotiations in 2018.
Despite the impact of the pandemic, a total of 5,887 HH phlebotomy claims were made by 720 GPs for 2,175 patients in 2020.
“This is a fantastic first year of the primary care programme for venesection services being provided by our GP colleagues. This is hugely beneficial for patients. It means venesection is being provided close to where you live. When you look at the geographical spread of where these GPs are located and providing the services, there is a huge number of patients accessing the services in CHO 2, which is
Mayo, Galway, and Roscommon, and also CHO 4, which is Kerry and Cork…,” as well as other more rural and peripheral areas outside the Dublin north-east region.
Prof Norris presented an overview of various studies on the impact of HH, and the arguments for screening to enable earlier detection and morbidity risk reduction. Ireland has a very high prevalence of HH compared to most countries, at 1.5 per cent (1:83) for HH c282Y mutation.
The Hemochromatosis and Iron Overload Screening (HEIRS) study, which evaluated the prevalence, genetic and environmental determinants, and potential clinical, personal, and societal effects of iron overload and haemochromatosis in a multicentre, multi-ethnic sample of 101,168 primary care adults (25 years+) in the US and Canada, showed that women with ferritin >1,000 were three times more likely to have significant liver disease, while men with ferritin >1,000 were six times more likely to have significant liver disease. Further research from the same group showed that patients with HH had a much higher risk of diabetes, liver disease, and liver cancer, but no increased risk of stroke and heart disease, she reported.
Arguments in favour of screening for haemochromatosis, Prof Norris said,
include “the fact that Ireland has the highest prevalence of any country, the consequences of late diagnosis can be very severe, it is such a simple and easy disease to diagnose with cheap, widely available tests, and the treatment is very simple”.
On the other hand, arguments against screening include that “despite its prevalence in Ireland very few people will develop life-threatening disease”, she noted.
“Many patients with haemochromatosis may never need venesection, probably about 50 per cent. And there is an argument that the health system has higher priorities, and there is the argument about genetic discrimination against those who are diagnosed as having homozygosity who will never develop iron overload, but could experience discrimination in terms of life insurance, mortgage approval, and so on.”
However, there is good evidence for targeted screening in higher at-risk populations, including those with type 2 diabetes or cardiac disease (atypical arthropathy) or male sexual dysfunction, close relatives of HH patients, those with abnormal LFTs with raised iron markers, etc, though Prof Norris pointed out that elevations in ferritin levels are common, and in type 2 diabetics can be due to liver fat.
News JULY-AUGUST 2021 7
WOMEN IN HEALTHCARE URGED TO APPLY FOR MCGINTY SCHOLARSHIP FOR NUI GALWAY MBA

Female health professionals are being encouraged to apply for a women-only scholarship for NUI Galway’s MBA programme.
The McGinty Scholarships were established by alumna Dr Geraldine McGinty, a physician executive and radiologist, to empower a new cohort of women who will lead improved and impactful outcomes for patients and healthcare staff.
The McGinty Scholarships are available each year to support two women – one physician and one allied healthcare professional in the MBA programme at NUI Galway.
Established in 2020, the scholarships were introduced to encourage and enable female physicians and allied healthcare professionals to engage in the MBA programme, to support them on a career path to leadership in the healthcare sector.
Speaking about the value of women in healthcare leadership, Dr McGinty said: “Despite women making up the majority of
Dr Geraldine McGinty
the healthcare workforce they are typically underrepresented in the highest levels of leadership. We know diverse teams drive better results and outcomes so making sure women are prepared to assume senior leadership roles is a key goal.”
Emergency Medicine physician Dr
Odharna Ní Dhomhnalláin received the inaugural McGinty scholarship. She said: “Healthcare practitioners bring a unique insight, particularly with regard to patient care and healthcare problems that we encounter in our day-to-day practice. The MBA has been very helpful in broadening my thinking and exposing me to the business knowledge that I need in order to pursue leadership and management positions in the future.”
Ann Cosgrove, Chief Operations Officer at Saolta University Healthcare Group, said: “The hospital services operate with a predominantly female workforce, with women delivering and managing clinical services across our health service. Ensuring more women reach leadership roles will strengthen our teams. I am delighted that this scholarship has been made available to further develop key leadership pathways for women in the healthcare sector.”
Full details can be found at www. nuigalway.ie/mba.
SUNSMART VIDEO SERIES ENCOURAGES EVERYONE TO ENJOY THE SUN SAFELY
The Irish Skin Foundation (ISF) and Dr Sinead Field, Consultant Dermatologist at University Hospital Limerick, in association with the HSE’s National Cancer Control Programme (NCCP), University of Limerick Hospital Group (ULHG), and the Healthy Ireland SunSmart campaign, have launched a series of five video animations, to encourage people to build SunSmart behaviours into their everyday routine, especially from April to September when the intensity of sunburnproducing ultraviolet radiation (UV) is greatest.
Skin cancer is the most common form of cancer in Ireland, with over 13,000 cases diagnosed annually. This is twice the number compared to 10 years ago and is projected to more than double again by 2045. Yet, most skin cancers could be prevented.
Prof Anne-Marie Tobin, Consultant
Dermatologist, HSE Clinical Lead in Dermatology says: “In dermatology, almost half of the work we do refers to skin cancer, and yet it is one of the most preventable forms of cancer. The risk factors for developing skin cancers are from sun and UV exposure, which are avoidable risk factors. It’s important to educate the public that most people living in Ireland have fair skin, which burns easily and tans poorly, so they are particularly vulnerable to UV damage and skin cancer and need to adjust their behaviours accordingly.”
The messaging throughout the video series highlights key skin cancer preventative behaviours and focuses primarily on the four priority groups identified in the National Skin Cancer Prevention Plan 2019-2022; children and young people, outdoor workers, those who participate in outdoor leisure activities, and sunbed users. The videos
encourage people to follow the SunSmart 5 Ss: Slip-on clothing that covers your skin, Slop on sunscreen, Slap on a wide-brimmed hat, Seek shade, and Slide on sunglasses.
Dr Sinead Field, Consultant Dermatologist, University Hospital Limerick, said of the launch of the video animation series, that traditional health promotion campaigns have had to be reimagined in light of Covid-19 public health restrictions. “Our aim in developing these animations was to bring the SunSmart messaging to life by creating a novel skin cancer awareness campaign in response to these changed circumstances and explore how digital health promotion initiatives can support all of us in adopting healthy sun protective behaviours.”
The National Skin Cancer Prevention Plan
News 8 JULY-AUGUST 2021 NEWS
sets out to enhance cross-sectoral collaboration to increase awareness and adoption of skin cancer preventative behaviours. The ISF is a member of the Irish Cancer Prevention Network (ICPN) established by the NCCP, Irish Cancer Society, Marie Keating Foundation and Breakthrough Cancer Research, who work
collaboratively to support cancer risk reduction initiatives such as Healthy Ireland SunSmart, with the National Screening Service and ISF. The videos will be played on visual display units throughout ULHG hospitals and hospital social media channels this summer, as part of a research initiative to evaluate the effectiveness
of these assets in raising awareness of sun protective behaviours amongst staff. To view the videos and learn more about being SunSmart visit the ISF website: www.irishskin.ie, the HSE website: www.hse.ie or the SunSmart hub. Follow the #SunSmart campaign on social for more information.
Recruitment
PRACTICE NURSE REQUIRED
Friendly group practice in South West Dublin seeking to recruit a permanent part-time practice nurse to join our team. Experience in practice nursing is desirable, but not essential. Suitable candidates from various nursing backgrounds will be considered. Job training offered, to build necessary skill set, if required.
Contract: Permanent
Hours: Mon-Fri, 15-19 hours per week. Afternoons initially. Flexible schedule.
Salary: Dependent upon experience.
Please contact glenfamprac@eircom.net to apply or Tel 01 626 0562 for further information
PRACTICE NURSE REQUIRED
Practice nurse required for North Dublin City practice. Experience helpful, but not essential for right candidate. Duties include, but not limited to, phlebotomy, ECG, vaccines, smears tests and managing smear recall system, stock ordering, and chronic disease management. Hours flexible. Salary negotiable. Please email cv to practicenursevacancy@outlook.com
MEMBERSHIP OFFICER REQUIRED
This is an exciting IGPNEA opportunity. We are ideally looking for someone who has previous membership experience and also experience in managing and maintaining large databases.
A background in general practice nursing is desirable, but not essential. This role will be 7.5 hours per week.
More details can be found on our website www.irishpracticenurses.ie, under 'Public News' To apply please email admin@irishpracticenurses.ie (interviews will take place the last week in July)
NURSE REQUIRED
Part-time, two days per week plus optional extra sessions.
Drummartin Clinic blends both conventional and functional medicine and uses advanced cutting-edge therapies, which are otherwise only available in the US and mainland EU.
Our patients are mostly people suffering from ‘difficult-to-treat’ conditions such as CFS, IBS, fibromyalgia, PMS, severe hormonal imbalances, allergies, and autoimmune disorders.
The clinic team is small (currently five people) and we work closely together. We value humour and there is also a big ‘feel-good’ factor when we see our patients ‘getting their lives back’.
The role will include phlebotomy and administration of intravenous treatments. You will work as part of a team with Kathryn our senior nurse and Dr Magovern and will be well-mentored and supported clinically. Remuneration €27-30 per hour.
You will be an experienced nurse with a high degree of personal initiative: A team player who is a good listener, enjoys professional development, and is empathetic and humorous.
To apply please email your CV to vacancies@drummartinclinic.ie with ‘NURSE’ in the subject line
If you would like to place a recruitment advert in the next edition, please contact Louis@mindo.ie.
News JULY-AUGUST 2021 9
EVERY MOVEMENT COUNTS:
HSE/SOUTH EAST COMMUNITY HEALTHCARE

active mentally and physically during their hospitalisation. The principle was subsequently stretched across several disciplines and spheres of healthcare and health and wellbeing in the community.
Illustrating the benefits of ‘Get up, Get dressed, Get moving’ across health services, the HSE’s Director of Nursing/National Lead Older Persons Services/Clinical and Integrated Programmes, Deirdre Lang, said: “‘Get up, Get dressed, Get moving’ is more important now than ever, as we begin to see if not also undo the impact of socially isolating by our older and more vulnerable populations. Remaining at home for long periods has left significant numbers of people with reduced mobility, experiencing deconditioning, muscle weakness, and joint pain. Reduced mobility has a knock-on effect and many people have put on weight, are experiencing joint and muscle pain, and report feeling consistently low.”
A national campaign, developed by the Office of the Nursing and Midwifery Services Director in partnership with the Health and Social Care Professions Office, HSE, and entitled ‘Get up, Get dressed, Get moving’ is being implemented to great effect across counties Waterford and Wexford.
The aim of ‘Get up, Get dressed, Get moving’ is to maintain the mobility of patients, residents, and health service users and to guard against their deconditioning. The network members includes all services across the spectrum of healthcare (including acute hospitals, mental health, care of older persons, and disability services) and works in partnership with academics, researchers, sporting organisations, and Age Alliance. It has particular resonance as people decondition and become frailer at this and coming stages of Ireland’s pandemic experience.
The impetus for ‘Get up, Get dressed, Get moving’ originated in advice being offered by physiotherapists to older inpatients in hospitals – that is, to stay

“‘Get up, Get dressed, Get moving’ promotes physical activity in any form that meets the needs and ability of the individual – which can be from sitting to standing from a chair to running five kilometres. The key message of ‘Get up, Get dressed, Get moving’ is that every movement counts.”
“The plan for the remainder of 2021 is to roll-out ‘Get up, Get dressed, Get moving’ in acute hospitals, at home, a scale-up of the work being undertaken in Waterford/ Wexford Mental Health Services and the development of work with the National Ambulance Service, intensive care units, and social inclusion groups.”
Speaking about where examples of ‘Get up, Get dressed, Get moving’ have been implemented locally, the HSE/South East Community Healthcare’s Acting Principal Psychology Manager for Wexford Mental Health Services, Dr Denise Rogers, says: “We have seen significant improvements in the quality-of-life of service in those mental health settings where ‘Get up, Get dressed, Get moving’ is now part of the overall approach.”
10 JULY-AUGUST 2021 News NEWS
 Author: Eamonn Brady MPSI
Author: Eamonn Brady MPSI
TACKLING DRY SKIN AND DERMATITIS
There are many causes of dry skin. Among the most common causes are conditions like dermatitis, eczema, psoriasis, and seborrheic dermatitis, writes Eamonn Brady
Common causes/ types
Dermatitis
The simple definition of dermatitis is inflammation of the skin. Different types of dermatitis include contact dermatitis, seborrheic dermatitis (dandruff) and atopic dermatitis (eczema). Symptoms include swollen, reddened and itchy skin. About 80 per cent of dermatitis cases are ‘contact dermatitis’, caused by an allergic response to a substance with which skin has been in contact. This can include latex, detergents or jewelry, such as nickel. Symptoms are often mild. Treatment involves avoiding contact with the offending substance. Skin hydration with an emollient is important (more details below). A topical steroid such as hydrocortisone 1 per cent cream may be required.
Eczema
Eczema is a type of dermatitis called atopic dermatitis. It is a chronic inflammatory skin condition that involves a complex interaction between environmental and genetic factors. It generally starts in childhood, with many growing out of it. Eczema affects over 30 per cent of children before they reach school age and 1-to-3 per cent of adults in the UK (Irish figures are similar). It is often hereditary
and there is often a link with asthma and hay fever. Eczema has become common in recent years; the cause of this is uncertain. There are theories such as the ‘hygiene theory’, which is discussed in more detail later in this article. Skin hydration can control eczema and in more severe cases, steroid creams may be temporarily required.
Psoriasis
Psoriasis affects between one-in-100 to three-in-100 of the population. It is caused by inflammation of the skin. It typically develops as patches of red, scaly skin. Plaque psoriasis is the most common type of psoriasis (about 80 per cent of cases). Symptoms are dry, red skin lesions, known as plaques, that are covered in silver scales. They normally appear on the elbows, knees, scalp and lower back, but can appear anywhere on the body. The plaques are normally itchy, sore, or both. In severe cases, the skin around the joints may crack and bleed. Appropriate treatment will keep psoriasis under control, but there is not a definitive cure. Skin hydration is important; other treatment options for more severe psoriasis include topical steroids, topical vitamin D analogues (ie, Calcipotriol) and coal tar preparations.
Seborrhoeic dermatitis
Seborrhoeic dermatitis is
characterised by red, scaly patches that develop on the scalp, face, and upper trunk. It is more likely to affect men than women. It is often aggravated by changes in humidity, changes in seasons, trauma (ie, scratching), or emotional stress. The usual onset occurs with puberty. It peaks at age 40 years and is less severe in older people. Approximately 1-to-3 per cent of adults suffer from seborrhoeic dermatitis. Dandruff is a mild form of seborrhoeic dermatitis and is estimated to affect 15-to-20 per cent of the population. The cause of seborrhoeic dermatitis is unknown. There is evidence that a type of fungus called malassezia has an influence. Seborrhoeic dermatitis most commonly affects the sides of the nose and the nasolabial folds (skin folds that run from each side of nose to corner of mouth), eyebrows, glabella (space between eyebrows and above the nose), and scalp. There are many treatment options for seborrhoeic dermatitis. Shampoos containing antifungal agents like ketoconazole or ciclopirox appear to be the most effective in the control of scalp seborrhoeic dermatitis, including dandruff.
The 'hygiene hypothesis' and autoimmune conditions like eczema
The 'hygiene hypothesis' is a theory that lack of exposure
Feature Dermatitis 12 JULY-AUGUST 2021
in early childhood to infectious agents means that the child’s immune system has not been activated sufficiently during childhood. This lack of exposure is down to our super-clean world of modern living, including antibacterial washes, vaccinations, and general sterility where children are not exposed to germs in a similar manner to previous generations of children. The theory hypotheses that because the immune system is ‘not activated’ during childhood, this leads to the immune system becoming oversensitive to common substances such as pollen, dust-mite and animal fur, leading to the higher incidence of autoimmune conditions like asthma, hay fever, and eczema in recent years.
One of the first scientific explanations of this theory was by a lecturer in epidemiology from the London School of Hygiene and Tropical Medicine, David P Strachan, who published a paper on the theory in the British
Medical Journal in 1989. He noticed that children from larger families were less likely to suffer from autoimmune conditions like asthma and eczema. Families have become smaller in the Western world over the last 40 years, meaning less exposure to germs and infections; it is over the same period that
health authorities have seen an explosion in autoimmune conditions, such as asthma and eczema.
Further studies have been conducted since then, supporting the theory. For example, studies show that autoimmune diseases are less common in developing countries, however, when immigrants from developing countries come to live in developed countries where living environments are more sterile, these immigrants suffer from increased levels of autoimmune conditions like asthma, and the rate of autoimmune conditions increases the longer immigrants live in developed countries.
It is a difficult issue to tackle for healthcare professionals advising parents who want the best for their children; common sense tells us all that cleanliness is important. It is difficult to advise on the best balance for parents in relation to this theory. No journal or book will give exact advice. In my opinion, a balanced view is to ensure children are administered important vaccines but ‘allow kids be kids’, let children play outside with friends, and try not to worry about them encountering dirt and germs, but always be cautious with children with life-threatening food allergies.
Treatment options
Diet
In adults, food allergies or food intolerance do not appear to be a factor in dry skin conditions such as eczema and psoriasis, so avoiding foods is not any benefit. In infants, avoidance of certain foods can be helpful, but healthcare professional advice is important. Common food triggers include eggs, nuts, peanut butter, chocolate, milk, seafood, and soya.
Maintaining adequate skin hydration
Evaporation of water on the skin leads to dry skin, especially in people suffering from dry skin conditions, such as dermatitis, eczema or psoriasis; skin

Feature Dermatitis JULY-AUGUST 2021 13
The 'hygiene hypothesis' is a theory that lack of exposure in early childhood to infectious agents means that the child’s immune system has not been activated sufficiently during childhood
hydration is a key component of their overall management. Thick creams (ie, Diprobase) which have a low water content, or ointments (ie, petroleum jelly, emulsifying ointment), which have zero water content, will better protect against dry skin than lotions. Hydration is best applied immediately after bathing, when skin is hydrated. Improve hydration by soaking in a bath containing a bath additive such as Oilatum for 10-to-20 minutes. I discuss moisturisers and emollients in more detail below.
Use of steroids
Topical corticosteroids, such as hydrocortisone 1 per cent cream, may be prescribed by a GP (or over-the-counter (OTC) from the pharmacy) for many dryskin conditions. The face and skin folds are areas that are at high risk of thinning and marking with corticosteroids, so care and moderation are important. The GP may prescribe more potent corticosteroid creams such as Clobetasone 0.05 per cent (ie, Eumovate), betamethasone 0.01 per cent (ie, Betnovate) or clobetasol 0.05 per cent (ie, Dermovate) for short periods during bad flare-ups.
In relation to potency, topical corticosteroids are classed as follows:
Mildly potent: Hydrocortisone 1 per cent.
Moderately potent (two-to-25 times as potent as hydrocortisone): Clobetasone (ie, Eumovate), alclometasone (ie, Modrasone).
Potent (100-to-150 times as potent as hydrocortisone): Betamethasone (ie, Betnovate), Mometasone (ie, Elocon).
Very potent (up to 600 times as potent as hydrocortisone): Clobetasol (ie, Dermovate).
Corticosteroids, especially the more potent versions, should be used for the shortest period possible and use of the most potent ones should be under strict medical supervision. The patient may need to be referred to a dermatologist in more severe cases.
When using a corticosteroid and a moisturiser, it is good practice to use the corticosteroid first and to put on the moisturiser after half an hour to allow the skin time to absorb the corticosteroid. In more severe cases, treatment may include
tacrolimus (Protopic Ointment) for eczema or UVB phototherapy and psoralen plus ultraviolet A (PUVA) therapy for psoriasis.
Therapies with no evidence base
Supplementation with essential fatty acids, pyridoxine, vitamin E, multivitamins, and zinc salts has no proven value. Reactions to washing powders are rare and avoidance of biological washing powders is of no benefit.
more effective moisturisers are. There is no limit to the number of times that you can apply a moisturiser. Always apply moisturisers in a downward motion, in the direction of hair growth. Gently massage it into the skin. Apply enough to moisten the skin without leaving it greasy. To help you remember to apply it, keep samples in various locations at home, at work and in your bag or pocket. Choose one that you like and feels comfortable. Always avoid perfumed products.
Emulsifying ointment
Moisturiser and emollient therapy
(more detail)
No matter what type of dry skin condition, keeping the skin well moisturised is key to managing the condition. Using moisturisers and emollients is key.
Emollient therapy
Always use soap substitutes for washing your skin at all times, ie, Silcock’s base, aqueous cream, emulsifying ointment or any brand name soap substitute.
Do not let soap, shower gel, bath foam or shampoo contact your skin.
Avoid perfumed products – spray on clothes if necessary.
If possible, wash hair over the bath or sink.
Drying
Pat-dry the skin gently. Avoid scrubbing skin with a towel.
How and how often to use moisturisers
Moisturise your skin immediately after washing while it is still damp; it is more effective when applied at this stage. The more often you moisturise your skin, the
Run a lukewarm water bath. Put two tablespoons of emulsifying ointment into a jug of almost-boiling water. Whisk into creamy froth and add to bath water. Emulsifying ointment makes the bath slippery, so caution is needed when getting in and out of the bath. Emulsifying ointment can be kept soft by storing it in the hot press. Stay no longer than 10 minutes in the bath. Pat skin dry afterwards and if prescribed steroidal skin cream, apply to affected area then wait 10-to-15 minutes and apply moisturiser in a downward motion.
Practical advice to manage dry skin conditions
Nails should be kept short and well filed to reduce damage from scratching.
Avoid strong detergent for washing clothes; use liquid detergent.
Double-rinse after washing; do not use a fabric softener.
Keep the skin cool, use 100 per cent cotton, keep wool away from skin.
Keep dust down; the house dust mite causes a problem for some people with eczema.
Adults should wear protective gloves when doing housework.
Avoid pets and animals if possible or at best, keep pets out of a sufferer’s bedroom
References available on request
Disclaimer: Brands mentioned in this article are meant as examples only and not meant as preference to other brands.
Feature Dermatitis 14 JULY-AUGUST 2021
The face and skin folds are areas that are at high risk of thinning and marking with corticosteroids
NATURE. NURTURED BY SCIENCE.

Our triple oat complex harnesses the goodness from the oat and combines it with protective ceramides. Creating a formula that helps to improve the skin’s natural microbiome balance, leaving skin more resilient and healthy looking from day 1. That’s why 90% of customers like yours say they felt immediate comfort after using Aveeno® Dermexa Daily Emollient Cream.1



So when you’re next faced with the question – howcanItreatmydryandirritatedskin?

Recommend Aveeno ® Dermexa


1. HTC Survey of 144 participants, January 2021 IE-AV-2100044 OAT FLOUR
WHOLE OAT EXTRACT OAT OIL
CERAMIDES
Author: Theresa LowryLehnen RGN, Post Grad Coronary Care, Clinical Nurse Specialist, Registered Nurse Prescriber and Associate Lecturer at Institute of Technology Carlow
MELANOMA: AN OVERVIEW
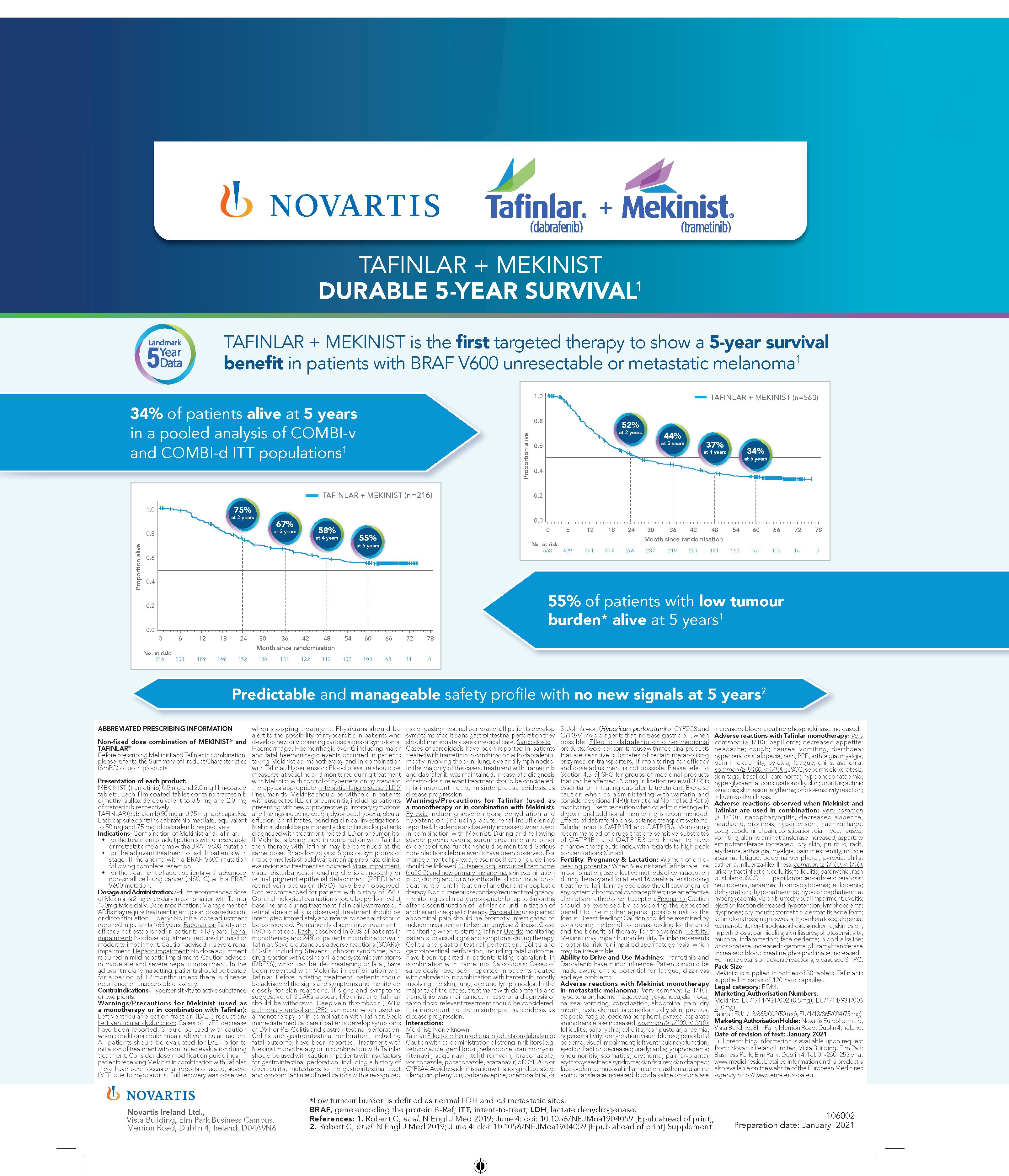
Skin cancer is the most common cancer in Ireland, with 11,660 cases diagnosed in 2019.14
Melanoma is a serious form of skin cancer that develops from pigment-producing cells found in the upper layer of skin known as melanocytes. Less common than basal cell (BCC) and squamous cell carcinomas (SCC), melanoma is more serious because of its ability to spread rapidly to other organs, if not treated at an early stage.1





Melanoma is usually curable when it is detected and treated early. Once a melanoma has spread deeper into the skin or other parts of the body, it becomes more difficult to treat and can be fatal.1
Excluding non-melanoma skin cancers, melanoma is the fourth most common cancer in Ireland, with approximately 160 deaths and 1,100 new cases diagnosed each year.13 From once being a rare cancer, the average lifetime risk for melanoma has now reached one-in-50 in many Western populations.
Since the 1960s the incidence of melanoma has increased in Caucasian populations and become one of the most frequent cancers in fair-skinned populations.6
Australia and New Zealand have the highest incidents of melanoma in the world and there are also high rates in Northern Europe and North America. It is less common in Asia, Africa, and Latin America.3
Statistics from the National Cancer Registry Ireland (NCRI) show that the incidence of melanoma in Ireland continues to rise. With approximately 20 cases diagnosed per 100,000 persons per year, rates have increased by over
5 per cent per year in men since 1994,12 while female incidence rates have also increased over time, but at a lower rate of 2.7 per cent per year. Since 1994, mortality rates for melanoma in Ireland have increased by 2.3 per cent annually in females and 4.7 per cent per year in males.12
Unlike other solid tumours, melanoma mostly affects young and middle-aged people. The median age of diagnosis is 57 years and the incidence increases linearly after
Feature Melanoma 16 JULY-AUGUST 2021
FIGURE 1: Superficial spreading melanoma FIGURE 2: Nodular melanoma
FIGURE 3: Lentigo maligna melanomas
FIGURE 4: Acral lentiginous melanomas
FIGURE 5: Amelanotic melanoma
Approximately 70 per cent of all melanomas are superficial spreading melanomas, which are more common in people with pale skin and freckles
From once being a rare cancer, the average lifetime risk for melanoma has now reached one-in-50 in many Western populations
Melanoma
the age of 25 years until the age of 50 years and then slows, especially in females.6 More than a quarter of melanoma skin cancers are diagnosed in people under the age of 50.2
Melanomas typically occur on the skin, but may also rarely occur in the mouth, intestines, eye (uveal melanoma) underneath a nail or on the sole of the foot. They occur most commonly on the legs in women and on the back in men. 4
Melanoma is considered a multi-factorial disease arising from an interaction between genetic susceptibility and environmental exposure.6 The primary cause of melanoma is ultraviolet light (UV) exposure in those with low levels of the skin pigment melanin. When skin is exposed to UV radiation from the sun or tanning beds, it causes skin damage, which triggers melanocytes to produce more melanin. Eumelanin and pheomelanin are two types of melanin in the skin. While eumelanin has the ability to protect the skin from sun damage, pheomelanin does not. Fairskin contains more pheomelanin and darker-skin contains more eumelanin. People with fair skin are more susceptible to sun damage, burning and developing melanoma than dark-skinned people due to a lack of eumelanin. Melanoma occurs when DNA damage caused by UV radiation triggers mutations in the melanocytes, resulting in uncontrolled cellular growth.1
Other factors contributing to an increased risk of developing a melanoma include being immunosuppressed, a family history of melanoma, a previous diagnosis of skin cancer, previous skin damage caused by sunburn or radiotherapy treatment and phenotypic characteristics, such as pale skin, red or blonde hair, blue eyes, and a large number of freckles. Repeated sunburn, either by the sun or artificial sources of light, increases the risk of melanoma in people of all ages. The risk of developing skin cancer increases with age. Rare genetic conditions such as xeroderma pigmentosum also increase the risk.1,2
The most important host risk factors are the number of melanocytic nevi, family history and genetic susceptibility. Melanocytic nevi commonly known
The ABCDE checklist can help differentiate between a normal mole and a melanoma:7
A-Asymmetry: Irregular in shape, with two parts that look very different
B-Border: Irregular or jagged in shape
C-Colour: Changes in colour
D-Diameter: The mole is larger than six millimetres wide (1/4 inch wide)
E-Evolving: The mole or spot has changed during the past few weeks or months. Change in size, shape, colour, elevation, bleeding, itching or crusting
as moles, are benign accumulations of melanocytes or nevus cells and may be congenital or acquired. Approximately 25 per cent of melanoma cases occur in conjunction with a pre-existing nevus. The total nevus count is positively correlated with melanoma risk and varies depending on the number, size, and type of nevi.6
There are four main types of skin melanoma; superficial spreading melanoma, nodular melanoma, lentigo maligna melanoma, and acral lentiginous melanoma. Another type called amelanotic melanomas are quite rare.10
Superficial spreading melanoma
Approximately 70 per cent of all melanomas are superficial spreading melanomas, which are more common in people with pale skin and freckles. They initially tend to grow outwards rather than downwards, however, if they do grow downwards into the deeper skin layers, they can spread to other parts of the body.
Nodular melanoma
Nodular melanomas are faster-developing and can quickly grow downwards into the deeper layers of skin if not removed. They usually appear as a changing skin lump and are often black or red in colour. Nodular melanomas most commonly occur on the head, neck, chest or back, and bleeding or oozing is a common symptom.
Lentigo maligna melanoma
Lentigo maligna melanomas account for approximately 10 per cent of melanomas. They most commonly affect older people, especially those who have spent a lot of time outdoors. They develop slowly over a number of years and appear on areas that are often exposed to the sun, such as the face. Lentigo maligna melanomas are initially flat and develop sideways on the surface layers of skin. They can resemble freckles, but are usually larger, darker and more defined than a normal freckle. They gradually get bigger and may change shape. At a later stage, they can grow downwards into the deeper layers of skin and form nodules.
Acral lentiginous melanoma
Acral lentiginous melanomas are a rare type of melanoma. They usually occur on the palms of the hands and soles of the feet, but can also develop around a nail, most commonly the thumb or big toenail. They can occur in all skin types, but are most common in people with dark skin. Amelanotic melanomas are also rare, accounting for about five-in-100 melanomas. They usually have little or no colour, but may occasionally be pink or red, or have light brown or grey edges.
Diagnosis and staging
Early detection of malignant melanoma remains a crucial factor in reducing mortality. Compared to other cancers, malignant melanoma has the advantage of its cutaneous location, allowing early detection through non-invasive approaches. Pathological examination however, remains the gold standard for diagnosis. The prognosis is directly proportionate to the depth of the neoplasm, which in turn increases with time.6
Normal moles (nevi) are usually round or oval, with a smooth edge, and ≤6mm in diameter.2 The first sign of a melanoma is often a new mole or a change in the appearance of an existing mole. Indications include changes in a mole’s colour, increase in size, irregular edges, itchiness, skin
Feature
JULY-AUGUST 2021 17
breakdown, and bleeding.
Other tools to help improve early diagnosis include the Glasgow seven-point checklist, which includes three major criteria – change in size, shape, colour, and four minor criteria – sensory change, diameter of 7mm or greater, presence of inflammation and crusting or bleeding. This checklist has been less widely adopted than the ABCDE criteria. Another paradigm is the ‘ugly duckling’ sign, based on the perception that a pigmented lesion ‘looks different from all of its neighbours’. This criteria has been shown to be sensitive for melanoma detection.6
Referral to a specialist is required if a melanoma is suspected. The melanocytic nevi (mole) will be removed and sent for biopsy (excision biopsy). If cancer is confirmed, another procedure will be required to remove a wider area of skin to make sure the cancerous cells have been removed. Further tests will be carried out if there is a concern the cancer has spread into other organs, bones or the bloodstream.2
Sentinel lymph node biopsy is used to determine whether the cancer has spread beyond the primary into the lymphatic system. The sentinel nodes are the first lymph nodes into which a tumour drains. Sentinel node biopsy involves injecting
a tracer material to locate the sentinel nodes, which are removed and analysed in a laboratory. Because only a few lymph nodes are removed, the risk of lymphoedema is small. If the sentinel nodes are clear of melanoma, the cancer is unlikely to have spread, and removing additional lymph nodes is unnecessary.
spread. Different systems used include the TNM (tumour, node, metastasis), number staging system (0-4) or the Clark or Breslow scale to describe how deeply the melanoma has gone into the skin.9
Treatment
Treatment of melanoma can include single or combined therapies, depending on the patient’s health, stage, and location of the tumour. Therapeutic approaches include surgical resection, chemotherapy, photodynamic therapy, immunotherapy, biochemotherapy, and targeted therapy. The main treatment for melanoma is surgery, and if diagnosed and treated at an early stage, surgery is usually successful.11 Radiotherapy after surgery usually consists of a course of five treatments a week for a number of weeks. Chemotherapy is now rarely used to treat melanoma and targeted treatments and immunotherapy are the preferred treatment options.2
Stage 0 – melanoma is on the surface of the skin
Stage 1A – melanoma is less than 1mm thick
Stage 1B – melanoma is 1-2mm thick, or less than 1mm thick and the surface of the skin is broken (ulcerated) or its cells are dividing faster than usual
Stage 2A – melanoma is 2-4mm thick, or it is 1-2mm thick and ulcerated
Stage 2B – melanoma is thicker than 4mm, or 2-4mm
If cancer is detected an operation to remove the remaining lymph nodes known as a completion lymph node dissection or completion lymphadenectomy is performed.8 Other tests carried out include CT scan, MRI scan, PET scan, and blood tests. Staging of a melanoma determines how deep it has grown and how far it has
Number Staging System2
thick and ulcerated
Stage 2C – melanoma is thicker than 4mm and ulcerated
Stage 3A – melanoma has spread into one-to-three nearby lymph nodes, but they are not enlarged. The melanoma is not ulcerated and has not spread further
Stage 3B – melanoma is ulcerated and has spread into one-to-three nearby lymph nodes but they are not enlarged. Or the melanoma is not ulcerated and has spread into one-to-three
nearby lymph nodes and they are enlarged. Or the melanoma has spread to small areas of skin or lymphatic channels, but not to nearby lymph nodes
Stage 3C – the melanoma is ulcerated and has spread into one-to-three nearby lymph nodes and they are enlarged. Or it has spread into four or more lymph nodes nearby
Stage 4 – the melanoma cells have spread to other parts of the body, such as the lungs, brain or other areas of the skin
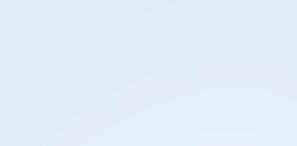
If undiagnosed until an advanced stage (stage IV), treatment is given to help slow the cancer’s growth, reduce symptoms, and extend life expectancy. This usually involves treatment that target specific genetic changes in the melanoma, such as BRAF inhibitors, or checkpoint therapies that boost the body’s immune responses to the melanoma.2
If a melanoma has spread to other parts of the body, the prognosis is less favourable.7 Metastatic melanoma is one of the most serious types of skin cancer, and accounts for most skin cancer deaths in Ireland. The five-year survival rate for patients with stage IV melanoma is under 20 per cent, compared with over 50 per cent if the disease is diagnosed at stage III. Unresectable cancers cannot be removed through surgery.
Newer treatments such as immunotherapy and targeted treatments are showing encouraging results in advanced melanoma. A number of different medications are available, some of which can be used as a monotherapy or as combination therapy. Immunotherapy
Feature Melanoma 18 JULY-AUGUST 2021
TABLE 1: Melanoma stages
Educating people to regularly check their skin and seek help for notable changes can help lead to an early diagnosis of melanoma and increase the chances of successful treatment
therapy to show a or metastatic melanoma
patients with new signals at 5 years
agents that increase gastric pH, when of dabrafenib on other medicinal concomitant use with medicinal products sensitive substrates of certain metabolising transporters, if monitoring for efficacy adjustment is not possible. Please refer to SPC for groups of medicinal products affected. A drug utilisation review (DUR) is initiating dabrafenib treatment. Exercise co-administering with warfarin and additional INR (lnternational Normalised Ratio) Exercise caution when co-administering with additional monitoring is recommended. dabrafenib on substance transport systems: OATP1B1 and OATP1B3. Monitoring of drugs that are sensitive substrates OATP1B1 and OATP1B3 and known to have therapeutic index with regards to high peak (Cmax). Pregnancy & Lactation: potential use effective methods of contraception and for at least 16 weeks after stopping Tafinlar may decrease the efficacy of oral or hormonal contraceptives; use an effective method of contraception. exercised by considering the expected mother against possible risk to the Breast-feeding: benefit of breastfeeding for the child of therapy for the woman. impair human fertility. Tafinlar represents for impaired spermatogenesis, which irreversible. and Use Machines: minor influence. Patients should be the potential for fatigue, dizziness problems. reactions with Mekinist monotherapy melanoma: haemorrhage, cough; dyspnoea, diarrhoea, vomiting, constipation, abdominal pain, dry dermatitis acneiform, dry skin, pruritus, oedema peripheral, pyrexia, asparate increased. paronychia; cellulitis; rash pustular; anaemia; dehydration; vision blurred; periorbital impairment; left ventricular dysfunction; decreased; bradycardia; lymphoedema; stomatitis; erythema; palmar-plantar erythrodysaesthesia syndrome; skin fissures; skin chapped; mucosal inflammation; asthenia; alanine increased; blood alkaline phosphatase
SURVIVA
[Epub ahead of print]; [Epub ahead of print] 18 24 30 36 42 48 54 60 66 72 78 314 269 237 219 201 181 169 161 103 16 0
dehydrogenase. 10.1056/NEJMoa1904059
medications include; ipilimumab, nivolumab, and pembrolizumab. Approximately 40-to-50 per cent of people with melanoma have gene mutations. Targeted treatments, such as vemurafenib, dabrafenib and trametinib can be used to specifically target these gene mutations to help slow or stop the cancer cells growing.
In 2019 the HSE approved reimbursement for encorafenib in combination with binimetinib for the treatment of adults with unresectable or metastatic melanoma with a mutation known as BRAF V600. Just over 1,000 patients in Ireland have melanoma, of whom about half have the BRAF mutation. More than 97 per cent of BRAF mutations are in the BRAF V600 gene.
In February this year (2021), after a long advocacy campaign by cancer patients, the HSE also announced that it was to reimburse adjuvant immunotherapies for stage III melanoma patients in Ireland.
While the HSE had been reimbursing three different kinds of immunotherapy drugs for melanoma patients previously, it was only for those who were at a more advanced stage. Instead, stage III patients were continually monitored through a ‘watch and wait’ strategy, though patients with certain private health insurance plans could access these drugs.
However, the HSE now reimburses nivolumab, which is used as monotherapy for the adjuvant treatment of adults with melanoma, whose cancer involves lymph nodes or metastatic disease, who have undergone complete resection.
Pembrolizumab is also in the process of being approved for reimbursement in this cohort. This can be used as monotherapy for the adjuvant treatment of adults with stage III melanoma and lymph node involvement, who have undergone complete resection also.
Survival and prevention
Survival from melanoma has increased in Ireland since the 1990s due largely to improvements in treatment for late stage tumours, as well as more patients presenting with earlier stage disease.12 The National Cancer Strategy 2017-2026 outlines the HSE’s plans for cancer prevention and
control and prioritises the development of a national skin cancer prevention plan targeting children, outdoor workers, sunbed users and those who pursue outdoor leisure activities.12 Addressing the rising incidence of skin cancer, the strategy prioritised the need to develop and implement the national skin cancer prevention plan (2019-2022).15
Melanoma is not always preventable, but a number of measures can be taken to reduce its occurrence. It is important that people are made aware of the dangers of UV radiation from the sun and artificial sources such as sunbeds. Wearing sunscreen is important and recommended even in winter, using a broad-spectrum, high UVA protection water resistant (UVA/UVB)
References
1. SCF (2020) Melanoma Overview. Skin Cancer Foundation. Available at: www.skincancer.org/skin-cancerinformation/melanoma/
2. HSE (2019) Overview Skin Cancer (Melanoma). Health Service Executive. Available at: www.hse.ie/conditions/ melanoma-skin-cancer/skin-cancermelanoma-overview.html
3. WHO (2014) World Cancer Report 2014 Chapter 5.14. World Health Organisation. ISBN 978-9283204299
4. CDC (2020) What are the symptoms of skin cancer? Centre for Disease Control and Prevention. Available at: www.cdc.gov/cancer/skin/basic_info/ symptoms.htm
5. NIH (2020) Moles to Melanoma: Recognising the ABCDE Features. National Cancer Institute. Division of Cancer Epidemiology and Genetics. Available at: https://moles-melanomatool.cancer.gov/
6. Rasterelli M, Tropea S, Rossi C, Alaibac M (2014). Melanoma: Epidemiology, Risk Factors, Pathogenesis, Diagnosis and Classification. In vivo: International Journal of Experimental and Clinical Pathophysiology and Drug Research. Available at: http://iv.iiarjournals. org/content/28/6/1005.long?utm_ medium=email&utm_source=transaction
7. ISF (2020) Skin Cancer. Irish Skin Foundation. Available at: https:// irishskin.ie/melanoma-skin-cancer/
8. Mayo Clinic (2020) Sentinel Node Biopsy. Available at: www.mayoclinic.org/testsprocedures/sentinel-node-biopsy/about/ pac-20385264#:~:text=Sentinel%20
sunscreen with a sun protection factor (SPF) of at least 30+ for adults and 50+ for children. It is advisable to seek shade and cover the skin as much as possible when in the sun, protect the face, ears and neck with a wide brimmed hat and wear sunglasses. Babies and young children are particularly vulnerable to sun exposure, and should always be kept out of direct sunlight.7
Educating people to regularly check their skin and seek help for notable changes can help lead to an early diagnosis of melanoma and increase the chances of successful treatment.2 Timely recognition, detection, rapid treatment and follow-up is key to improved outcomes and survival rates from malignant melanoma.
node%20biopsy%20is%20a,into%20 which%20a%20tumor%20drains
9. Cancer Research UK (2020) Melanoma Skin Cancer: Stages and Types. Available at: www.cancerresearchuk. org/about-cancer/melanoma/stagestypes
10. MacMillan Cancer Support (2020) Cancer Information and Support Melanoma. Available at: www.macmillan.org. uk/cancer-information-and-support/ melanoma
11. Domingues B, Lopes J, Soares P, Pópulo H (2018). Melanoma treatment in review. Immunotargets Ther. 2018; 7: 35-49. doi: 10.2147/ITT.S134842
12. NCRI (2017) Incidence of melanoma in Ireland on the rise, particularly in men. National Cancer Registry Ireland.
13. Irish Cancer Society (2020) Melanoma. Available at: www.cancer.ie/cancerinformation-and-support/cancer-types/ skin-cancer/melanoma
14. Irish Cancer Society (2020) Cancer Statistics. Available at: www.cancer. ie/cancer-information-and-support/ cancer-information/about-cancer/ cancer-statistics
15. DOH (2019) National Skin Cancer Prevention Plan 2019 – 2022. Department of Health, Ireland. Available at: www.gov.ie/en/publication/4655d6national-skin-cancer-prevention-plan2019-2022/?referrer=www.health.gov.ie/ blog/publications/national-skin-cancerprevention-plan-2019-2022/
Feature Melanoma 20 JULY-AUGUST 2021
CONTINUED STRIDES IN HIV TREATMENT
Emily Clarke Gifford speaks to Clinical Lead of the HSE's Sexual Health and Crisis Pregnancy Programme, Prof Fiona Lyons, about the challenges Covid-19 has posed for people living with HIV, new treatments, and the stigma still faced by this population
It is estimated that there are over 6,000 people living with human immunodeficiency virus (HIV) in Ireland. According to provisional data from the Health Protection Surveillance Centre (HPSC), published last year, there were 539 diagnoses of HIV notified in 2019. The organisation HIV Ireland has raised concern that this is the highest level in Ireland since records began.
In 2018, there were 523 diagnoses of HIV notified, according to HPSC data for that year.
In addition to the existing issues such as ensuring diagnosis, and combatting ongoing societal stigma, people with HIV are facing new challenges due to the Covid-19 pandemic.
Covid-19
Speaking to NiGP, Consultant in Genitourinary Medicine at St James’s Hospital, Dublin, and Clinical Lead of the HSE’s Sexual Health and Crisis Pregnancy Programme, Prof Fiona Lyons, said that maintaining treatment regimens for people with HIV was prioritised during the pandemic.
“The bottom line very early on in the pandemic was certainly the key priority for services, and [that] was to maintain treatment for people who were living with HIV,” as well as seeing those who were newly diagnosed, Prof Lyons confirmed.
She explained that people’s access to testing has been “impacted at different stages in the last 15 months”. While Prof
Lyons said this “hasn’t been easy”, she hoped that access will improve as society emerges from the “worst” of the pandemic.
Prof Lyons said that travelling to receive medications was a new challenge that people with HIV faced. This was due to the stress some patients felt when collecting medication and having to go to the clinics, while Covid-19 restrictions were in place.
bespoke to the individual circumstances,” said Prof Lyons.
A lot of work was done to ensure “everyone went for their treatments, including working with people on an individual basis to ensure they did not miss out on their medication”, she said
Future treatments
HIV treatments have always been free of charge in Ireland and Prof Lyons outlined that there is a “vast array” of treatments available to people.
In a 2018 audit, it was found that 90 per cent of people who were attending HIV services were on treatment and over 90 per cent had viral suppression, she explained.
In terms of new medication, injectable cabotegravir/rilpivirine has been approved by regulators in North America and Europe as an antiretroviral HIV treatment. Rilpivirine is from a class of drugs known as non-nucleoside reverse transcriptase inhibitors. Cabotegravir is from a class of drugs known as integrase inhibitors. The two work together to reduce the viral load of HIV in a person’s body.
She added that “some of our patients are stuck overseas; that was a really big challenge for patients and trying to make sure that they were maintained on treatment”.
In response to this, Irish HIV clinics had to arrange for medical files to be sent abroad so people had access to medication where they were based. “There's no onesize-fits-[solution]…. It had to be very
Recently, data released from the phase 3 ATLAS study on long-acting cabotegravir and rilpivirine for the treatment of HIV showed continued virologic suppression to 96 weeks.
The European Medicines Agency approved both a once-monthly and an
Interview HIV Update JULY-AUGUST 2021 21
We know that if we can get the information out there to people that effective treatment prevents transmission through sexual contact, then that's going to help with that stigma that people experience
every-other-month regimen. In the US and Canada, only the monthly regimen received approval.
Prof Lyons told NiGP that the treatment will go through the Irish approval process in due course.
In a panel discussion at the Conference on Retroviruses and Opportunistic Infections 2021, Prof Diane Havlir, Professor of Medicine and Chief of the HIV/AIDS Division at the University of California, San Francisco, US, said that the next decade promises to be an era of long-acting HIV products.
Long-acting treatments give more
options to patients who find it difficult to take medication on a daily basis.
Stigma
Although HIV treatments have been available since the 1980s, people living with HIV still face significant stigma.
According to HIV Ireland’s 2019 report 'HIV-related stigma and discrimination in Ireland today', 84 per cent of those living with HIV agreed that they were viewed negatively by Irish society.

Among the general public, 54 per cent of people agreed that people with HIV were viewed negatively, ranking third to drug
users and Travellers in terms of stigma. Despite this, 77 per cent of the population expressed sympathy and understanding towards those living with HIV/ AIDS. However, 23 per cent said they would be worried about eating a meal that was prepared by someone with HIV and 37 per cent agreed that if a family member were to contract the virus, they would keep their HIV status a secret. The report said the more personal the experience of HIV, the greater the perceived stigma and discrimination.
Prof Lyons noted that “misinformation is always going to drive stigma”.
Interview HIV Update 22 JULY-AUGUST 2021
HIV Ireland has recommended tracking the level of stigma and discrimination against people living with HIV as this information is “crucial to understand the phenomenon of stigma in Ireland”.
The report added that more information is needed to create an awareness of the rights of people living with HIV regarding employment, health, social services, education, and housing.
Just over half (56 per cent) of people living with HIV are aware that it is illegal to discriminate against a person with HIV.
Employers, unions, schools and other educational institutions, primary health care providers, and housing bodies, need to have a greater awareness that to discriminate on the basis of HIV status is illegal under the Employment Equality Act 1998 and the Equal Status Acts 2000 and 2004.
In response to stigma and misinformation, the HSE launched a campaign on the issue in January 2020. Campaign posters with the tagline, ‘Effective treatment means you can’t pass HIV onto partners’ appeared on public transport, social venues, and college locations across the country, as well as on digital platforms. The campaign also referenced the global U=U campaign (‘undetectable equals untransmittable’).
Prof Lyons explained that the campaign aimed to emphasise that “people who are on treatment cannot transmit HIV”.
“That is something that should serve to reduce the amount of stigma, because a lot of the stigma is around people's fear that they're going to acquire HIV,” she said.
While there is an abundance of material on HIV treatments available online, Prof Lyons emphasised the need for more accessible information.
“We know that if we can get the information out there to people that effective treatment prevents transmission through sexual contact, then that's going to help with that stigma that people experience.”
While there is no cure for HIV, current treatments can offer people a “functional cure”, said Prof Lyons. When on treatment, people living with HIV have viral suppression and can live a full life.
Prof Lyons said the situation where people on treatment can enjoy a similar life expectancy to the general population represented “massive progress in medicine”.
Regarding her work in the area, Prof
Lyons said that “it’s been an amazing journey for me as a doctor", going from a situation where patients had limited life expectancy to now, where patients can expect to live a relatively normal life.
COULD GENERAL PRACTICE NURSES PLAY MORE OF A ROLE IN HIV SCREENING?
Priscilla Lynch
Implementing routine general practice nurse-led HIV screening for all new patients in general practice increases testing rates, improves detection and leads to earlier diagnosis, a recent UK study found.
The paper, published in The Lancet’s clinical journal EClinical Medicine, examined the impact of introducing an automatic, rapid screening offer for patients when they register with a surgery.
The study researchers compared outcomes from 13 practices in east London that implemented nurse-led routine HIV screening into their business-as-usual working, with their earlier randomised control trial in which staff from 20 practices received initial training plus regular support to provide HIV screening.
The initial trial, which ran between 2010 and 2012, found the approach increased both the number of HIV tests and the number of diagnoses. CD4 counts at diagnosis were high – suggesting that the infection was picked up when the immune system was still healthy.
In this study, people diagnosed during the 'routine implementation' period had average CD4 scores at diagnosis of 425 cells/ micro litre – higher than the 351 recorded during the initial trial period and the 327 recorded for newly-diagnosed patients of the comparator group of practices.
HIV testing was 55 per cent higher in implementation practices than comparator practices, diagnosis rates were 106 per cent higher and CD4 count at diagnosis was typically 35 per cent up.
Importantly, most of the new diagnoses were among people in groups at the highest risk of late diagnosis – heterosexuals, and black African and Caribbean adults. Both
those groups are under-represented at sexual health services where they would be offered HIV testing – which can mean they are diagnosed later.
The researchers caution that the wide range in confidence levels around data, mean the results on the latter two outcomes are suggestive, but not conclusive.
Study co-lead Dr Werner Leber, a GP and Clinical Lecturer in Primary Care at Queen Mary University of London, said the 'implementation phase' confirmed that GP practices could successfully integrate HIV screening – particularly of new patients –into business as usual.
Dr Leber said: "During our initial research study we found that offering HIV tests to new patients did pick up previously undiagnosed cases of HIV. The data collected outside the clinical trial environment and published today shows that the intervention is effective in routine care within modern GP practices."
Study co-lead Dr Jasmina PanovskaGriffiths, a Senior Research Fellow and Lecturer at UCL, said: "Our study shows that implementation of nurse-led HIV screening in general practices can be delivered effectively, leading to increased HIV testing that may be associated with increased and earlier HIV diagnosis. It also appears that most of the new diagnoses are amongst people who are less likely to attend sexual health services where they would be offered HIV testing."
HIV testing in general practice is recommended under international guidelines yet primary care screening rates remain low, noted the authors. In Ireland there have been calls for many years for the roll-out of a rapid screening service for HIV in primary care.
Interview HIV Update JULY-AUGUST 2021 23
We carry the full range of consumables and small equipment. So if you’re in the market for a scalpel blade or a stethoscope please call our team on 01-9030125. We would love to hear from you!







-
Noreen & Daniel
Fetal Doppler MD800

Product: 100221






Portable doppler complete with 3MHz probe. Screen displays fetal heart & fetal heart rate waveform.
€110.00+vat
Welch Allyn Sets
From a bulb to a complete Welch Allyn Diagnostic Centre - We are partnered with Welch Allyn to meet any and all requirements you may have. Bulbs, Otoscope Tips, Pocket Sets and Wall Systems; chat to our team today!




sales@fitzmedicalsupplies.ie
01-9030125 OPEN 9:00-5:30 €99.00+ freeshipping NEXT DAY DELIVERY PRICES Ex-VAT www.fitzmedicalsupplies.ie
Packs
IUCD
Author: Sarah O’Connor, CEO, Asthma Society of Ireland
SUPPORTING ASTHMA PATIENTS DURING THE PANDEMIC
In late February 2020, the Asthma Society of Ireland’s team realised that an outbreak of Covid-19 was a very likely event in Ireland and we began to plan accordingly. We used initial Community Foundation funding to buy laptops to move our operations online, we adapted the working of our Asthma Adviceline so that all telephone calls could be managed remotely and we assessed which programmes would need to be paused in the event of the pandemic outbreak. On one hand, this makes us sound prescient and forward-thinking, but on the other hand, we had no idea what we were about to face.
Our Covid-19 response team – advocacy and awareness response
We established a Covid-19 response team, comprising of our Advocacy and Research Manager, Advocacy Officer, CEO, Communications team, and our Medical Advisory board, and our staff triaging and managing calls, who all worked tirelessly to ensure we had accurate information, advice and recommendations in relation to asthma and Covid-19 on our website and social media. In the initial weeks from March until July 2020, we created updates of our Covid-19 FAQ, getting input and approval from our clinical advisors and the HSE National Respiratory Clinical Programme.
When the scale of the challenge
became clear, we realised we couldn’t afford to rely on our one-to-one services and we focused on how to scale up our patient supports to help us in answering the incredible volume of queries and very real anxieties from patients and their carers. Where visits to our website had stood at over 410,000 in 2019, we had in excess of that figure visiting www.asthma.ie in the six weeks from the initial pandemic outbreak alone. With each iterative wave of concern from patients, we proactively responded with medical guidance, advice and support through our own channels, digital media and traditional media. With each of these waves, we listened to patients and advocated to the Minister for Health, Department of Health, HSE and Respiratory Clinical Programme for what patients needed.
Asthma Adviceline
Our flagship patient support service, our Asthma Adviceline service (1800
44 54 64), truly came into its own during the pandemic. It is hard to convey the scale of the challenge here. Twenty years in existence, our specialist respiratory nursing team delivering this service have built up extraordinary expertise in supporting and educating patients over the telephone. In order to maximise the impact of the nurse appointment, our team operated a triage system for months, ensuring that the patients most in need of advice, support, and guidance had access to the nurse. All other patients were supported by members of our patient services team, providing advice approved by the National Clinical Programme signposting to HSE materials and supports, and offering guidance and reassurance as required.
Ordinarily, the Asthma Society has one full-time receptionist taking adviceline calls; this increased from March until June 2020 to five full time staff triaging and managing calls and scheduling nurse appointments. In 2020, the triage team managed 6,816 incoming/ outgoing support calls to the adviceline. We provided 4,416 nurse appointments across the asthma and COPD adviceline, a 148 per cent increase from 2019.
Despite a focus on Covid-19 related queries, Asthma Action Plans were discussed in 88 per cent of adviceline nurse appointments – helping patients to understand the need for

Feature Asthma JULY-AUGUST 2021 25
improved asthma control and providing a key intervention recognised internationally to prevent asthma deaths.
New service –WhatsApp nurse support
In May 2020, in conjunction with an Asthma Awareness Week theme focused on supporting asthma patients through the pandemic, we launched a new Sláintecarefunded service – a nurse WhatsApp support messaging service. Staffed by a respiratory specialist nurse team, it offered support, guidance and advice for patients. With 610 users from May to December 2020, the service involved 5,064 patient chats with the nurse. Some were quick queries and others long, extended conversations about asthma management. Healthcare professionals can refer patients to this service and using it could not be simpler – patients send a message on WhatsApp to 086 059 0132 with their question, or concern and the nurse responds to support them with advice, best practise asthma management, videos or links – depending on what they need.

While the Asthma Society was reactive in the initial weeks after the pandemic outbreak, by May 2020 we were in listening mode and our 2,400 respondent strong survey helped us to listen to patients and give them the supports they needed. We created a whole host of specially designed Covid-19 supports tailored to their needs:


An Asthma Self-Management masterclass,
Covid-19 asthma and COPD management leaflets,



A Protecting the Cocooners pack, webpage and video guidance programme,
A Back to School/Back to Normal awareness programme to support children returning to school or people returning to work,
A series of respiratory supports including wellness, patient education webinars, and awareness building (in conjunction with
other respiratory charities, with the support of Bank of Ireland),


A Winter Wellness campaign,
Videos and leaflets to support patient sub-groups particularly impacted by Covid-19 outbreaks – like members of the Traveller community and the Roma community,
Asthma and Covid-19 patient packs, through Careplus pharmacies.
The Covid-19 legacy
Over 16 months in, we are left trying to understand the collective trauma of the pandemic – for all of us in Ireland. For those of us in the Asthma Society, that trauma is very real. Our fundraising has been
seriously impacted and we have not been able to retain our full team as a result. There has been no improvement into 2021 and we are challenged with continuing our work. The Society cannot continue to provide its services without a substantial upturn in funding and fundraising – we may have to lose services in advocacy, awareness, research, and patient supports. This is a very serious realisation for us and for our patients – and all while our latest research launched during Asthma Awareness Week 2021, which shows that one-in-four patients avoided an emergency department visit when they needed it for fear of contracting Covid-19. We have never been more needed and we have never been less able to continue to meet the needs of patients. By 2030, we want to end asthma deaths in Ireland, but we need our work and services to survive to accomplish that goal. We need your help to do that – as healthcare professionals who can create meaningful asthma interventions with patients, boosting their asthma management skills, but also as Asthma Society donors. Please go to www.asthma.ie to become a healthcare professional member of the Society and to donate on a monthly basis.
Feature Asthma 26 JULY-AUGUST 2021
Despite a focus on Covid-19 related queries, Asthma Action Plans were discussed in 88 per cent adviceline nurse appointments
THE IMPORTANCE OF FOLATE AWARENESS
Anna Wedderburn presents an overview of the need for adequate folate intake and its effects on overall health
Folate, also known as vitamin B9, is a water-soluble vitamin that is obtained through diet. Folate was first isolated in 1941, and it is now known to play an important role in the synthesis of DNA and RNA, the methylation of DNA, the metabolism of amino acids, and the formation of red and white blood cells. This vitamin allows for healthy and fully-functional cell division, and is therefore of particular importance during periods of rapid growth and development, such as pregnancy. It is also thought that folate plays a role in mental health and cardiovascular health, among other aspects of health.
The man-made version of folate is known as folic acid. Folic acid is much more stable than folate, and is more bioavailable within the body. For this reason, naturally-occurring folates in foods are limited in their ability to influence blood folate levels.
Folate is absorbed into the bloodstream from the gut. From here, it moves to the liver for processing. Any excess folate passes to the kidneys and is then excreted from the body as urine.
Folate is naturally present in a wide variety of foods, including: Liver, dark leafy vegetables, legumes, egg yolk, avocado, asparagus, and broccoli.
Health risks associated with low folate levels Mental health
A low folate status has been linked to an increased risk for depression and a poor response to antidepressant treatment. Although folic acid does not appear to be as effective as an antidepressant by itself, supplementation does appear to boost the impact of antidepressants in some individuals, particularly in women who are taking fluoxetine. Low folate has also been associated with schizophrenia, dementia, Alzheimer's disease, and anxiety.
Cardiovascular disease and stroke
High levels of homocysteine in the body is associated with an increased risk for cardiovascular disease and stroke. Folic acid supplements have been demonstrated to lower levels of homocysteine in the blood, potentially reducing the risk of cardiovascular disease and stroke. However, there is still controversy surrounding the role of folate in preventing cardiovascular disease and stroke, with some studies yielding conflicting results.
Megaloblastic anaemia
A lack of folate within the body can lead to megaloblastic anaemia. In megaloblastic anaemia, red blood cells do not form properly – they are larger than normal, are oval-shaped instead of round, and there are fewer of them. Symptoms include pale skin, decreased appetite, irritability, fatigue, diarrhoea, and a smooth and tender tongue.
Pregnancy and neural tube defects
The importance of folate in the development of an embryo during pregnancy was discovered in

1991. Folate deficiencies prior to and during the early stages of pregnancy can lead to neural tube defects in offspring. In an embryo, the neural tube is the structure that develops into the entire nervous system. Neural tube defects occur in embryos 21-to-28 days after conception, at a time when most women do not know they are pregnant. Women who are deficient in folate are more likely to give birth to children with neural tube defects such as anencephaly (absence of a major portion of the brain and skull), encephalocoele (sac-like protrusions of the brain and the membranes that cover the brain through openings in the skull), and spina bifida (underdeveloped spinal cord and backbone). The optimal folate status for neural tube defect protection is greater than 907nmol/L.
As neural tube formation occurs so early in embryonic development, it is recommended that women take 400ug of folic acid a day three months prior to conception, and for 12 weeks into pregnancy. It is important to note that these recommendations specifically refer to folic acid supplements, as folic acid is more bioavailable than folate, as opposed to relying on naturallyoccurring folate within foods. It has been demonstrated that folic acid supplementation can reduce neural tube defects by up to 70 per cent. As folic acid has such a significant role in preventing neural tube defects, it is actually recommended that all women of reproductive age and who are sexually active take 400ug of folic acid daily, as from the years 2014 to 2019, there were 121 million unintentional pregnancies annually across the globe.
Ireland is not exempt from this. Studies have reported that only 40-to-45 per cent of pregnancies in Ireland are planned, while uptake of folic acid in Ireland has been reported to be low during pregnancy, and even lower
Feature Folate JULY-AUGUST 2021 27
prior to conception. In a study in 2015, it was found that in Ireland, only 36 per cent of women of reproductive age had levels of folate in their blood that would be considered to be protective against neural tube defects. Furthermore, almost 50 per cent of the indigenous Irish population have variations in a gene that codes for an enzyme involved in folate metabolism. These variations decrease the body’s ability to metabolise folate, contributing to an increased risk of folate deficiency. This genetic mutation, alongside the low levels of folic acid supplementation in women in Ireland, perhaps makes it unsurprising that the rates of neural tube defects in Ireland are among the highest in the world.
Fortification of foods, such as flour and cereals, with folic acid is mandatory in some countries. This has a significant impact on incidence of neural tube defects. In Canada, the US and Chile, for example, mandatory fortification of these food types led to a 27-to-50 per cent decrease in rates of neural tube defects.
In Ireland and most other EU countries, fortification of foods with folic acid is not mandatory, but fortification of foods with folic acid is thought to reduce the risk of neural tube defects by 11-to-14 per cent.
The statistics surrounding folate levels and pregnancy in Ireland suggest that there is a lack of awareness in women who are of reproductive age when it comes to the importance of folic acid for embryo development, particularly prior to conception. This is where general practice nurses and other community healthcare staff have the potential to play an important role in raising awareness. It is unlikely that women who are thinking about becoming pregnant will schedule an appointment with their doctor to discuss pregnancy, unless they are having issues with conception. It is quite likely, however, that they or their partner will visit a pharmacy to buy a pregnancy test or will have a smear test or bring older children to the practice for immunisation. This could provide a good opportunity to discuss the importance of folic acid in the lead-up to pregnancy.
Recommended amounts of folate intake
The recommended daily allowance for folate for the different demographics is listed in
Table 1. The allowances are based on the ‘dietary folate equivalent’ (DFE) unit. DFEs are used as folic acid has a higher bioavailability than folate that is found in food. It is estimated that 85 per cent of folic acid taken with food is bioavailable, whereas approximately 50 per cent of folate naturally present in food is bioavailable. Based on these bioavailabilities, DFEs are defined as follows:
1ug DFE = 1ug food folate.
1ug DFE = 0.6ug folic acid consumed with food.
1ug DFE = 0.5ug folic acid on empty stomach.
Women who have a history of neural tube defects in their family are advised to take more than the recommended amount of folic acid stated above. Women with this medical history should discuss folic acid supplementation with their doctor prior to conceiving. The doctor may decide to give them a prescription for a supplement with a higher concentration of folic acid.
It is recommended that folic acid supplements should not be given to infants under the age of one, unless advised by a
healthcare professional to do so.
Folic acid supplements
Over-the-counter
vs prescription
Folic acid is available as a prescription, but also as an over-the-counter (OTC) medication. In most cases, OTC folic acid supplementation is sufficient. Prescription folic acid supplements contain a higher concentration than OTC supplements and are used for individuals severely deficient in folate, those with absorption issues, or in women who have a family history of neural tube defects. The OTC folic acid supplements, such as Clonfolic tablets, generally contain 400ug of folic acid.
Side-effects
There are potential side-effects to taking folic acid, although they are rare. They include nausea, loss of appetite, bloating, and wind. Toxicity from folic acid is even more rare, although high-dose supplementation is still not advised unless under medical supervision. As folate is water-soluble and readily excreted from the body in the urine, overdoses are not a major concern.
Allergies
Allergic reactions to folic acid are extremely rare. The reactions that have been reported include erythema, skin rash, itching, general malaise, and respiratory difficulty.
Interactions with other medications
Although folic acid supplementation is advisable and considered to be very safe, it may interact with the following medications:
Anticonvulsants: Folic acid might decrease the blood concentration of drugs such as fosphenytoin (Cerebyx), phenytoin (Dilantin, Phenytek) or primidone (Mysoline).
Barbiturates: Folic acid may decrease the effectiveness of central nervous system depressants.
Methotrexate: Folic acid could interfere with the effectiveness of this medication used to treat cancer.
Pyrimethamine (Daraprim): Folic acid may reduce the effectiveness of this drug.
Feature Folate 28 JULY-AUGUST 2021
References on request LIFE STAGE RECOMMENDED AMOUNT Birth to 6 months 65ug DFE Infants 7-12 months 80ug DFE Children 1-3 years 150ug DFE Children 4-8 years 200ug DFE Children 9-13 years 300ug DFE Teens 14-18 years 400ug DFE Adults 19+ years 400ug DFE Pregnant teenagers and women 600ug DFE Breastfeeding teenagers and women 500ug DFE
1:
Table
Folate daily recommendations
Allergic Rhinitis
Author: Theresa LowryLehnen, CNS, GPN, RNP, PhD, National PRO of the Irish General Practice Nurses Educational Association
ALLERGIC RHINITIS IN FOCUS
One of the most common autoimmune conditions, allergic rhinitis can significantly impact quality-of-life, but a range of effective treatments are available
Allergic rhinitis (AR) is an inflammatory disorder of the nasal mucosa induced by immunoglobulin E (IgE)-mediated reactions to inhaled allergens. It is one of the most common chronic conditions globally causing a major health burden and is associated with substantial economic costs. AR often co-occurs with asthma and conjunctivitis and is also associated with atopic dermatitis and nasal polyps. It is estimated that up to 50 per cent of people with asthma and up to 30 per cent of people with eczema also have AR. Classic symptoms of the disorder are nasal congestion, nasal itch, rhinorrhoea and sneezing. A less recognised symptom is post-nasal drip. AR is frequently associated with allergic conjunctivitis with redness, tearing, and itching of the eyes. Approximately 60 per cent of patients with AR have concomitant allergic rhino conjunctivitis. AR symptoms can be debilitating, resulting in sleep disturbance, fatigue, depressed mood and decreased function that impairs quality-of-life and productivity.

cent of individuals diagnosed with the condition develop symptoms before the age of 20 years. Older children have a higher prevalence than younger children with a peak occurring at ages 13-to-14 years. During early childhood, boys are more likely to be affected by AR
than girls, during puberty girls have a higher incidence, and by age 20 and over the prevalence rates among men and women are equal.
AR has long been considered a disorder of the nose and nasal passages, however, evidence suggests that it may represent a
AR adversely affects the daily living activities of nearly 1.38 million Irish people and affects up to 30 per cent of adults and 40 per cent of children in industrialised countries. Approximately 80 per Figure 1: Stepwise treatment approach to allergic rhinitis
Feature
JULY-AUGUST 2021 29
component of a systemic airway disease involving the entire respiratory tract. Allergen provocation of the upper airways not only leads to a local inflammatory response, but may also lead to inflammatory processes in the lower airways, and this is supported by the fact that rhinitis and asthma frequently co-exist. AR affects 60-to-80 per cent of people with asthma. Some patients have AR alone, whereas others have AR and asthma with or without other allergic manifestations, although few patients have asthma alone. Although it is well established that rhinitis can lead to asthma, the exact phenotype of AR prone to developing asthma is still unclear. It is possible that poly-sensitised individuals can more commonly develop asthma.
Traditionally categorised as seasonal or perennial, AR is better classified according to symptom duration (intermittent or persistent) and severity (mild, moderate or severe). ARIA (Allergic Rhinitis and its Impact on Asthma) guidelines classify AR as intermittent or persistent depending on the duration of symptoms, with persistent rhinitis occurring for more than four days a week for more than four weeks in a row, and as mild, moderate or severe, depending on whether sleep and daily activities are affected or whether symptoms are troublesome ( Figure 2).
Risk factors for AR include antibiotic use, inhalant and occupational allergens, as well as genetic factors. Common triggers include dust mites, animal allergens, pollens, spores, and moulds.
Pathophysiology
AR is an autoimmune condition and symptoms occur when the immune system overreacts to a normally harmless substance such as pollen. When the body encounters an allergen, cells in the lining of the nose, mouth and eyes release histamine – triggering symptoms of an allergic reaction. Allergic reactions do not occur the first time a person comes into contact with an allergen. The allergic immune response begins with a sensitisation phase when the patient
that promote immunoglobulin E (IgE) production by plasma cells. Crosslinking of IgE bound to mast cells by allergens, in turn, triggers the release of mediators, such as histamine and leukotrienes, which are responsible for arteriolar dilation, increased vascular permeability, itching, rhinorrhoea, mucous secretion, and smooth muscle contraction in the lung. The mediators and cytokines released during the early phase of an immune response trigger a further cellular inflammatory response, which results in the recurrent symptoms that often persist.
Diagnosis
A thorough history and physical examination are important for establishing a diagnosis of AR. History should include questions regarding a family background of atopic disease, the impact of symptoms on quality-of-life and the presence of comorbidities, such as asthma, mouth breathing, snoring, sleep apnoea, sinus involvement, otitis media, and nasal polyps. Clinical history should note when and where symptoms occur and any exacerbating and relieving factors. Chest, ears, throat, abdomen and skin should be examined for other symptoms and a review of any treatments and their efficacy carried out. Testing for allergen-specific IgE using skin prick or blood tests to identity the allergen can support the diagnosis. Other tests may include a nasal endoscopy, nasal inspiratory flow test, and CT scan.
is first exposed to an allergen without experiencing clinical symptoms. In AR, numerous inflammatory cells, including mast cells, CD4-positive T-cells, B-cells, macrophages, and eosinophils, infiltrate the nasal lining upon exposure to an allergen. In allergic individuals, the T-cells infiltrating the nasal mucosa are predominantly Th2 and release cytokines, eg, interleukin [IL]-3, IL-4, IL-5, and IL-13
Rhinitis has important co-morbidities. Asthma should always be assessed for in patients with AR and if needed an objective measurement, such as spirometry, carried out owing to the frequent co-occurrence of these disorders. Patients should also undergo ear inspection as otitis media with effusion may be a co-morbidity in children with rhinitis and in adults with severe forms of rhinosinusitis. The general examination should include skin examination for atopic dermatitis and assessment of thyroid function by checking for slow relaxation after the ankle jerk and for eye signs, such as puffiness, redness and/ or bulging (hypothyroidism) in patients
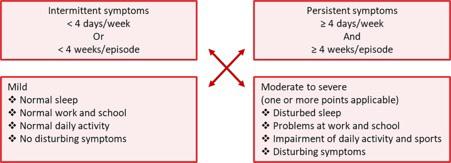
Feature
30 JULY-AUGUST 2021
Allergic Rhinitis
Figure 2: ARIA classification of severity of allergic rhinitis
Some patients have AR alone, whereas others have AR and asthma with or without other allergic manifestations, although few patients have asthma alone
Allergic Rhinitis
with obstructive rhinitis. Children’s growth should be assessed, as the combined use of intra nasal corticosteroids (INCS) and inhaled corticosteroids can reduce height at high doses. The presence of features such as conjunctivitis, nasal allergic crease, allergic salute or double creases beneath the eyes all suggest an allergic diathesis. Nasal examination is required in patients with moderate to severe AR or in those with uncontrolled symptoms despite optimal treatment. Examination should include assessment of the external appearance followed by internal examination, preferably with a nasoendoscope although an otoscope may suffice in children. Position of the nasal septum, size and colour of the inferior turbinates together with the appearance of the mucosa and the presence and nature of any secretions, polyps, bleeding, tumours, crusting or foreign bodies should be noted.
Treatment
Therapeutic options for AR include avoidance measures, nasal saline irrigation, oral antihistamines, INCS, combination INCS/antihistamine sprays, leukotriene receptor antagonists (LTRAs), and allergen immunotherapy. Other therapies that may be useful for some patients include decongestants and oral corticosteroids.
It is important to differentiate over-thecounter (OTC) and prescription therapies for AR. Nasal decongestant sprays are highly effective if used infrequently. Available options include Sudafed nasal spray (xylometazoline HCL), Otrivin (xylometazoline HCL), and Afrin (oxymetazoline HCL). Despite being available OTC, caution should be advised as incorrect use can lead to adverse effects. It is important that patients are aware that these decongestant sprays are not recommended for monotherapy in chronic AR.
First-line treatment of AR involves reduced exposure and avoidance of relevant allergens and irritants, such as house dust mites, moulds, pets and pollens, etc, that trigger the condition. Nasal saline irrigation is most effective when used for mild symptoms or before intranasal glucocorticoid
(INGC) application. INGC options include Avamys, Nasonex, and Flixonase. If symptoms remain refractory to an INGC, a second generation oral antihistamine will be prescribed.
Second-generation oral anti-histamines such as loratadine and cetirizine are first-line pharmacological treatments recommended for all patients with AR. They require once-daily dosage, are non-drowsy and are available OTC without prescription. Second-generation antihistamines offer several advantages over classical H1 antihistamines, such as lack of sedation and impairment of performance, longer duration of action, and absence of anti-cholinergic side-effects. However, loratadine is best avoided in elderly patients and patients with liver problems.
First-generation sedating antihistamines,
oral antihistamines may, with caution, be used in pregnancy or in women who are breastfeeding; for example, cetirizine.
Other first-line therapeutic options for patients with mild persistent or moderate/ severe symptoms are INCS and they can be used alone or in combination with oral antihistamines. When used regularly and correctly, INCS effectively reduce inflammation of the nasal mucosa and improve mucosal pathology. Studies and meta-analyses have shown that INCS are superior to antihistamines and LTRAs in controlling symptoms of AR, including nasal congestion and rhinorrhoea.
INCS are not systemically absorbed. The most common adverse effects are local, including nasal irritation, stinging and epistaxis, and can usually be prevented by aiming the spray slightly away from the nasal septum. Long-term use does not damage nasal mucosa or induce glaucoma, and growth effects in children seem to be minimal. Some INCS, such as budesonide, can be safely used during pregnancy at the recommended therapeutic dose after a thorough medical evaluation.
such as diphenhydramine and chlorpheniramine, are also effective in relieving symptoms, however, they have been shown to negatively impact cognition and functioning, may affect the patient’s ability to drive and operate machinery and are not routinely recommended for the treatment of AR. They should not be used in patients with prostatic hypertrophy or narrow-angle glaucoma.
The advantages of oral antihistamines are once-a-day administration, rapid and effective action and low cost. However, they are less effective than INCS, particularly for nasal congestion which is a common symptom of AR. Oral antihistamines are often sufficient for the treatment of mild AR, and many patients prefer oral medications to other formulations. Some
If INCS are not effective, a combination corticosteroid/antihistamine spray, such as Dymista, can be used. LTRAs should be considered when oral antihistamines, INCS, and/or combination corticosteroid/ antihistamine sprays are not well tolerated or are ineffective in controlling the symptoms of AR. For patients with AR refractory to INGCs and concomitant asthma, a trial of an LTRA, such as montelukast, is advised. If combination pharmacological therapy with oral antihistamines, INCS, combination corticosteroid/antihistamine sprays and LTRAs is not effective or is not tolerated, then allergen immunotherapy should be considered.
Immunotherapy
Allergen-specific immunotherapy (AIT) is currently the only potential treatment for allergies including AR that can modify the underlying course of the diseases. AIT is indicated for AR, allergic rhinoconjunctivitis and/or asthma when
Feature
JULY-AUGUST 2021 31
For a sustained effect, AIT should be applied for a minimum of three years, either continuously or pre-seasonally
Allergic Rhinitis
symptoms remain uncontrolled with avoidance measures and appropriate pharmacotherapy in adherent patients. The aim of AIT is to induce tolerance to the allergens and therefore reduce the symptoms of allergic diseases.
By gradually increasing the patient’s exposure to the allergen that causes the allergy, the patient becomes tolerant to it. Immunotherapy is only used in patients with severe symptoms and must be done by a specialist. AIT for the management of allergic disease has entered a new phase. Safe, effective, oral sub-lingual immunotherapy (SLIT) preparations are becoming increasingly available for use in allergy de-sensitisation as opposed to allergy injections. The use of AIT by 'allergy shots/injections' was severely curtailed in Ireland and the UK from 1986 when a number of deaths were reported with its use in general practice, particularly in those patients who had unstable underlying asthma. The situation has changed over the past decade however, with strong evidence that AIT can effectively treat AR , eradicate it and even prevent the development of asthma in allergic children if used early enough. For a sustained effect, AIT should be applied for a minimum of three years, either continuously or pre-seasonally. Benefit may not appear until the end of the first year of treatment, but may persist for many years beyond the course of treatment. Prolonged desensitisation using increasing doses of the culprit allergen both by subcutaneous immunotherapy (SCIT) and SLIT reduces rhinitis symptoms which have been refractory to INGC and oral antihistamines.
Grazax and Oralair are two licenced SLIT preparations available for grass pollen AR in Ireland. If patients have co-existing asthma, it must be recognised and treated and their lung function test must be normal. Patients must be advised to place the tablet under the tongue for one-totwo minutes and then swallow it. Grazax should be commenced two-to-four months before the pollen season starts in late May/ June and continued daily for a total of three
years. Oralair is commenced at the same time for a period of six months per year for three successive years if there is an effect seen after the first season.
SLIT is now viewed as a significant advance in the treatment of allergic diseases. It is very effective in the treatment of rhinitis with long-lasting benefits seen after the treatment is discontinued. It is the only treatment that offers the possibility of reducing long-term costs and the burden of allergies by changing the natural course of the disease.
Other emerging therapies
Biological therapies represent a potential step forward in providing individualised care for patients with uncontrolled severe upper airway diseases. Biologics like omalizumab and dupilumab have demonstrated efficacy in patients with chronic AR and with nasal polyps. These monoclonal antibodies target type 2 inflammatory cytokines, including IL-4, IL-5, 1L-13 and IgE and have convincing evidence in proof of concept studies. The immediate goals in biologic therapies for allergies and asthma are to develop biomarkers to identify patients most likely to respond to these therapies and to monitor disease severity. As experience with biological therapies continues to grow, they are expected to move from their current position as add-on therapies for severe allergic disease to play a more prominent role in treatment strategies for many more allergy patients.
House dust allergy tips
Allergy-proof covers for mattresses, duvets and pillows;
Choose wood or hard vinyl floor coverings instead of carpet;
Fit roller blinds that can be easily wiped clean;
Regularly clean cushions, soft toys, curtains and upholstered furniture, either by washing or vacuuming them;
Use synthetic pillows and acrylic duvets instead of woollen blankets or feather bedding;
Using a vacuum cleaner fitted with a high-efficiency particulate air (HEPA) filter
can remove more dust than an ordinary vacuum cleaner;
Use a clean damp cloth to wipe surfaces – dry dusting can spread allergens further.
Pets
If a pet cannot permanently be removed from the house:
Keep pets outside as much as possible or limit them to one room, preferably without carpet;
Do not allow pets in bedrooms;
Wash pets at least once a fortnight;
Groom dogs regularly outside;
Regularly wash bedding and soft furnishings a pet has been on;
Taking an antihistamine one hour before entering a house with a pet can help reduce symptoms.
Pollen
To avoid exposure to pollen:
Check weather reports for the pollen count and stay indoors when it is high;
Avoid line-drying clothes and bedding when the pollen count is high;
Wear wraparound sunglasses to protect eyes from pollen;
Keep doors and windows shut during mid-morning and early evening, when there's most pollen in the air;
Shower, wash hair and change clothes after being outside;
Avoid grassy areas, such as parks and fields, when possible;
If you have a lawn, consider asking someone else to cut the grass for you.
Mould spores
To help prevent mould spores:
Keep your home dry and well ventilated;
When showering or cooking, open windows, but keep internal doors closed to prevent damp air spreading through the house, and use extractor fans;
Avoid drying clothes indoors, storing clothes in damp cupboards and packing clothes too tightly in wardrobes;
Prevent damp and condensation in the home.
References on request
Feature
32 JULY-AUGUST 2021
Author: Theresa LowryLehnen, CNS, GPN, RNP, PhD, and National PRO, Irish General Practice Nurses Educational Association
SOCIAL PRESCRIBING:
IMPORTANCE OF HIGH QUALITY RESEARCH AND COMPARATIVE EVALUATION
The benefits of social prescribing are many, including positive emotional, cognitive and social outcomes, and an increase in connectedness for people within their communities
Social prescribing is a process of providing people with non-medical sources of support and interventions within the community to improve their physical, emotional and mental wellbeing. As a model, it is a relatively new concept in Ireland, although social prescribing and similar approaches have been practised in the NHS and UK for many years, with schemes dating back to the 1990s, and earlier. In a growing number of locations around Ireland, health professionals now have access to a social prescribing referral service that aims to reduce loneliness and social isolation by linking people with non-medical sources of support within their local community. Recognising that people’s health is determined primarily by a range of social, economic and environmental factors, social prescribing aims to address people’s needs in a holistic way and support individuals to take greater control of their own health. There is clear evidence of the inextricable relationships between physical health, mental wellbeing and social interaction. Social prescribing expands the range of options available to health professionals and service users in order to address needs that cannot be met by a health service response alone.
Social prescribing adopts a broad, holistic framework, with an emphasis on personal experiences, relationships and social conditions. It is a formal means of enabling primary care services to refer people to a variety of holistic, local, non-clinical projects and programmes in the community and is intended to reduce social exclusion for isolated and vulnerable people,
of General Practitioners (ICGP) agree that people with mild to moderate depression should be referred to services including the voluntary and community sector. The benefits of social prescribing are many, including positive emotional, cognitive and social outcomes, and an increase in connectedness for people within their communities.
and those enduring mental health problems. Social prescribing is available for people aged over 18 years and utilises non-medical supports to address the needs of people who are experiencing social exclusion or isolation, have vague or unexplained symptoms of depression or anxiety, are frequent attendees at their GP or who have poor social supports. Both the HSE and the Irish College
Social prescribing services are available in over 30 locations around the country, supported by Sláintecare, Healthy Ireland and the HSE as well as communitybased organisations such as local development companies and family resource centres. Projects are funded differently in every area. Social prescribing is supported by a number of national policies and strategies specifically addressing the themes of partnerships and cross sectoral work, empowering people and communities and recognising the importance of the social determinants of health. The Healthy Ireland Framework 20132025 supports the Government’s response to Ireland’s changing health and wellbeing profile and aims for “a healthy Ireland where everyone can enjoy physical and mental health and wellbeing to their full potential”. Its goals are to increase the proportion
Feature Social Prescribing JULY-AUGUST 2021 33
Social prescribing services are available in over 30 locations around the country, supported by Sláintecare, Healthy Ireland and the HSE...
of people who are healthy at all stages of life, reduce health inequalities, protect the public from threats to health and wellbeing, and create an environment where every individual and sector of society can play their part in achieving a healthy Ireland. Social prescribing is a key programme in meeting and achieving Healthy Ireland’s aims.
It is also closely aligned with the HSE’s transformation of the health service model of care under Sláintecare, which aims to ensure an integrated model of care based on the principles of ‘right care, right place, right time’. A core objective of Sláintecare is the shift of care from the acute sector to the community setting, bringing ‘care closer to home’. The Sláintecare Integration Fund has already funded a number of social prescribing projects across the country, and recognises the contribution that it can offer to the reform of the healthcare system. Social prescribing addresses many

of the goals of Sláintecare by increasing community supports for people with chronic diseases, those who are feeling vulnerable, isolated and lonely, and those who are frequent attenders of general practice with social-related issues. It creates opportunities for people to get involved in caring for their own health and wellbeing, and strengthens links between community and medical services.
How it works
The social prescribing coordinator plays a key role and acts as a link between health professionals and community supports and activities. Social prescribing coordinators come from a range of health, social carerelated or community development backgrounds, including nursing, teaching, life-coaching and personal development. Equally as important as experience and qualifications are their personal characteristics, inter-personal skills, attitude
and approach to the role and their ability to act as a link between the primary care team and the community and voluntary sector.
Social prescribing coordinators support individuals to access interventions such as exercise classes, social groups and creative activities, volunteering opportunities, men’s sheds employment services and educational courses. They work in conjunction with health services, relieving pressure on primary care teams whilst increasing the uptake of local supports and services. In most cases social prescribing begins with a referral from a healthcare professional, typically from members of the primary care team, including GPs, GPNs, community mental health and public health nurses. Referrals can also come from other professionals such as a psychologist, counsellor, social worker or from the individual themselves.
Following referral, the social prescribing coordinator will arrange an initial meeting with the participant. The aim of this meeting is for the coordinator to gain an understanding of the presenting issues from a social, rather than a medical, perspective. The coordinator works with the participant, usually over a period of six weeks holding between one and four meetings, depending on the needs of the individual, and helps them identify activities and opportunities which they have enjoyed in the past or would like to try out. The coordinator supports the participant to identify challenges and barriers to participation, puts strategies in place to overcome them and follows up on progress at subsequent meetings. Participation is entirely voluntary and the GP is informed of the individual’s involvement in the programme after the first meeting. Social prescribing empowers individuals to find solutions, which improve their health and wellbeing, often using services provided by the voluntary and community sector.
Social prescribing link workers across the country have adapted supports in innovative and safe ways to respond to the challenges presented by Covid-19. While Covid-19 has changed the way that many
Feature Social Prescribing 34 JULY-AUGUST 2021
supports and activities are currently accessed, there is still a wide variety of online and active supports available and social prescribing is more relevant than ever as a support for community connection during the pandemic.
Long-term outcomes for participants can include improved health and wellbeing, community connectedness, reduction in loneliness and social isolation, improved confidence and lower levels of anxiety and depression. For health professionals, outcomes can include reduced clinical workload through a reduction of visits from patients who require non-medical supports. Such schemes provide practitioners with a non-medical referral option that can be delivered alongside existing primary care services to improve individuals’ health and wellbeing. For the community, long-term outcomes include improved knowledge and connection between healthcare providers and services, and community and voluntary organisations.
Research and evaluation
Quality research and comparable evaluations is necessary to assess the success of social prescribing services. Researchers have highlighted the challenges of measuring results of the services’ complex interventions. Gold standard reviews of social prescribing programmes have not found robust evidence of effectiveness and there are few studies comparing social prescribing to usual care. While many social prescribing services present positive findings, high-quality research and comparable evaluation needs to be conducted as many studies are small scale, focus on progress rather than outcomes, and the evaluation methodologies used are variable in quality. Existing evaluation practice varies greatly across Ireland.
In August 2019, Health and Wellbeing, HSE, the National Office of Suicide Prevention, and the Department of Health commissioned an evaluability assessment of social prescribing in Ireland. This assessment was a key input to the development of a monitoring
and evaluation framework for social prescribing in Ireland. The evaluability assessment within this report was limited to 12 social prescribing projects in operation identified by the HSE at the project commencement stage. Key findings from the evaluability in practice assessment found the need for a minimum data outcomes framework and commitment to building more evidence for social prescribing by embedding outcome data collection into service delivery. One of the key areas of challenge relates to the availability of outcomes data and evidencing the outcomes of social
need support to do this. Issues relating to multi-annual funding cycles and underresourced projects were noted and there appeared to be limited onus on projects to provide impact data to funders. Projects need clear direction from commissioners and primary care teams on what is useful for them and what helps them to recommission and fund.
prescribing projects in a reliable way, which is not possible without additional data collection. A need for guidance around evaluation of social prescribing in a more accessible, clear and structured way was highlighted as uncertainty remains around what to measure, how to measure it and which tools should be used. Challenges around the capacity and resources of organisations to measure outcomes and impacts and the importance of shared resources and shared learning for evaluation was identified. Many different social prescribing delivery models and projects exist at different stages and levels of operating. Buy-in from primary care teams differs from project to project, is largely determined by personal relationships, and has an impact on access to ‘system level’ data. The use of external data such as national datasets and randomised controlled trials (RCTs) to build the case would be useful, but projects
Social prescribing operates differently in each location around Ireland depending on the profile of the local area. Many social prescribing projects are carrying out evaluations on the impact of their services on the health and wellbeing of individuals attending social prescribing. Some evaluations are carried out by the service itself and others are being undertaken as part of funded research projects in collaboration with universities including Trinity College Dublin, Royal College of Surgeons Ireland, and Queen’s University Belfast. Research and evaluation is important for the development and sustainability of social prescribing in Ireland. Measuring the longer-term impacts of social prescribing requires the participation of primary care teams and other parts of the health system, both in the referral of participants and the provision of data to enable analysis.
Although there is a need for more robust and systematic evidence on the effectiveness of social prescribing, there is a growing body of evidence at home and abroad that it can lead to a range of positive health and wellbeing outcomes. In the UK, 59 per cent of GPs agree that social prescribing can help reduce their workload. The Impact Report: Adult Mental Health and Wellbeing Social Prescribing in Hackney (2015) highlighted significant positive results; with an 81 per cent improvement in social networks, 76 per cent of participants reported improved coping strategies, 57 per cent took up physical exercise, and 75 per cent improved their levels of self-esteem. The UK Department of Health is encouraged by the impact social prescribing is having on individuals and
Feature Social Prescribing JULY-AUGUST 2021 35
For health professionals, outcomes can include reduced clinical workload through a reduction of visits from patients who require non-medical supports
the NHS has pledged to make the service available to every GP practice across England within the next five years. Social prescribing studies and interventions in Ireland have pointed to improvements in quality-of-life, emotional, mental, and general wellbeing, and reduced levels of depression and anxiety. The Donegal Social Prescribing Evaluation Report 2015 highlighted a significant positive impact on wellbeing, reduced anxiety and depression levels: With a 20 per cent reduction in GP attendance for participants, a significant increase in levels of community involvement, and overall general satisfaction for the participants, stakeholders and health professionals involved. Referrers, participants and community organisations that took part in the evaluation provided favourable accounts of their engagement. One general practice in Dublin that implemented social prescribing in 2016 noted that 19 per cent of patients accounted for 50 per cent of their consultations between JanuaryJune 2017. Many of these consultations involved social issues and the stress and anxiety associated with them, such as isolation, unemployment, housing, and addiction issues. Three months were spent researching links in the area and 350 resources for referral were identified. The impact of the initiative at this practice helped over 300 patients, accounted for a 35 per cent reduction in attendance among patients who availed of social prescribing, and led to a reduction of almost 1,000 GP consultations over two years (2017/18).
Mainstreaming social prescribing
Social needs such as depression, anxiety and loneliness account for approximately 20 per cent of visits to healthcare professionals in Ireland. Mainstreaming social prescribing is a key commitment of the Social Prescribing Network Ireland to promote its benefits and reduce health inequalities. The HSE Mental Health and Wellbeing Programme, in collaboration with representatives from across the HSE and the community and voluntary sector, is in the process of developing a
framework for how social prescribing can be mainstreamed and integrated across the health service at community healthcare network level. This framework is expected be completed and launched sometime this year. Meaningful evaluation must be acknowledged as a crucial component of social prescribing. Generating useful findings for practitioners and funding stakeholders should allow for effective adaptation of processes and outcomes should offer value. Clarity in terms of what is expected from evaluation by funders would assist projects with evaluation design and implementation. Collecting and analysing data is challenging.
References
Bickerdike L, Booth A, Wilson, P, Farley K, Wright K. (2017). Social prescribing: Less rhetoric and more reality. A systematic review of the evidence. BMJ Open. 2017 Apr 7; 7 (4):e013384. doi: 10.1136/ bmjopen-2016-013384
DOH (2021). Sláintecare in Action 2019. Social Prescribing. Available at: www.gov. ie/en/publication/cf284-slaintecare-inaction-2019/#social-prescribing
Donegal Social Prescribing Evaluation Report (2015). Available at: www.hse.ie/ eng/services/list/4/mental-health-services/ nosp/research/reports/donegal-socialprescribing-evaluation.pdf
E-Zine (2021). All Ireland Social Prescribing Network. Available at: https://thewellbeingnetwork.ie/wpcontent/uploads/2021/03/AISPN-E-zineMar-21.pdf
ESRI (2020). The impact of social prescribing on general practice use. Economic and Social Research Institute, Ireland. Available at: www.esri.ie/events/ the-impact-of-social-prescribing-ongeneral-practice-use
Family Action Impact Report (2015). Adult Mental Health and Wellbeing. Social Prescribing. UK. Available at:
Relationship development, data collection and analysis are both time and resource intensive, and this needs to be recognised at the planning and funding stages. Close relationships with practitioners are essential to enable rigorous, unbiased data collection and generate the deeper contextual understanding required for meaningful qualitative analysis. While the complexities involved make it challenging to meaningfully evaluate the outcomes, the rising prevalence, popularity and positive impact of social prescribing on health and wellbeing heightens the importance of developing effective methods to do so.
www.family-action.org.uk/content/ uploads/2014/03/Family-Action-ImpactReport-2015-Social-Prescribing.pdf
HSE Healthy Carlow. Carlow Social Prescribing (2021). Healthy Carlow. Available at: http:// catherines.ie/what-we-do-st-catherines/socialprescribing-programme/
HSE Healthy Waterford. (2021). Waterford Social Prescribing. Healthy Waterford. Available at: w ww.healthywaterford.ie/ projects/social-prescribing/
HSE Healthy Waterford (2017). Social prescribing: A selected bibliography. Health Service Executive. Available at: www.healthywaterford.ie/wp-content/ uploads/2017/03/Social-prescribingbibliography_31-March.pdf
HSE (2020). Building Capacity for the Evaluation of Social Prescribing Assessment. Health Service Executive. Available at: www.hse.ie/eng/services/ list/4/mental-health-services/connectingfor-life/publications/social-prescribing.pdf
HSE (2021). Social Prescribing. Health Service Executive. Available at: www. hse.ie/eng/about/who/healthwellbeing/ social-prescribing/
NHS (2021). Social Prescribing. National Health Service, UK. Available at: https://
w ww.england.nhs.uk/personalisedcare/ social-prescribing/
Pescheny J, Pappas Y, Randhawa G. (2018). Facilitators and barriers of implementing and delivering social prescribing services: A systematic review. BMC Health Serv Res. 2018 Feb 7;18(1):86. doi: 10.1186/s12913-018-2893-4
Pescheny J, Randhawa G, Pappas Y. (2020). The impact of social prescribing services on service users: A systematic review of the evidence. Eur J Public Health 2020 Aug 1; 30 (4):664-673. doi: 10.1093/ eurpub/ckz078. PMID: 31199436
SAPC (2020). How do we evaluate social prescribing interventions: A utilisationfocused approach. Society for Academic Primary Care. UK. Available at: https:// sapc.ac.uk/conference/2020/abstract/ how-do-we-evaluate-social-prescribinginterventions-utilisation-focused
The Kings Fund (2020). What is Social Prescribing? Available at: www.kingsfund. org.uk/publications/social-prescribing
Woodall J, Trigwell J, Bunyan, AM, et al. Understanding the effectiveness and mechanisms of a social prescribing service: A mixed method analysis. BMC Health Serv Res 18, 604 (2018). https:// doi.org/10.1186/s12913-018-3437-7
Feature Social Prescribing 36 JULY-AUGUST 2021
ON THE COMPLEXITY OF CALORIES
Can you remember what a calorie is? Let me see. My recollection is that it’s the energy required to raise the temperature of a litre of water by... er... um... a certain amount?
So, clearly I had to check and it turns out that it’s the amount of energy needed to raise the temperature of 1g of water by 1ºC or, to be precise, 4.1868 joules.
Well, I’m sure you’re glad we cleared that up. The ‘calories in, calories out’ theory has been with us, in developing forms, since AntoineLaurent de Lavoisier built the first calorimeter shortly before losing his head – literally –during the French Revolution. The American physiologist Wilbur Atwater developed the modern concept in the closing years of the 19th Century, burning food to see how much energy it contains.
Indeed, when using student volunteers in the course of his metabolic studies, he would set fire to their faeces. Where other scientists would have perhaps tried to find a way around this challenging and malodorous business, Atwater didn’t flinch. Although, I should add that I can’t find any reference to how he actually managed the incineration process.
His motivation was not about calorific restriction. Instead, he was concerned that the poor were not getting enough calories in their diet and he wanted to be able to make scientific recommendations to help improve their lot.

Anyway, it’s a curious thought that ‘calories in, calories out’ is still the mantra well over a century after Atwater refined it. It underpins the ‘eat less, move more’ school of weight control thinking and has resulted in the dietary obsession that was kick-started by the US Senate in 1977 when it recommended a low fat, low cholesterol diet for all. The fat was, of course, replaced by sugar and salt and global obesity trebled between 1975 and 2016.
At this stage it is estimated that 1.9 billion people are overweight. It comes as no surprise that the incidence of type 2 diabetes has more than doubled over the past 40 years.
Incidentally, the most obese country in the world, with 74.6 per cent of the population overweight, is American Samoa. The least obese is Vietnam with a shade over 2 per cent. The US weighs in at 36.2 per cent, the UK at 27.8 per cent, Ireland at 25.3 per cent, and foodloving France at 21 per cent.
Of course, the demonisation of fat was an obsession of another American scientist, Ancel Keys, and the object of his so-called lipid hypothesis about which I’ve written here before. The process, however, was clandestinely encouraged by the US sugar industry and in 2016 a researcher at the University of California found the smoking gun.

Documents uncovered by Prof Stanton Glantz of UC San Francisco showed that in 1967 the Sugar Research Foundation, a sugar industry body now known as the Sugar Association, paid Harvard scientists to publish cherry-picked studies that minimised links between sugar consumption and heart disease, while pointing the finger at dietary fat. The publication that unleashed this on the world was no less than the New England Journal of Medicine (NEJM) The NEJM has required disclosure of financial assistance only since 1984.
“They were able to derail the discussion of sugar for decades,” Glantz told The New York Times.
None of the Harvard scientists are still alive,
but one of them, David Mark Hegsted went on to be head of nutrition at the US Department of Agriculture where he drafted the 1977 government dietary guidelines.
It appears that the sugar lobby is still trying very hard to shape the narrative on diet. It was reported in 2015, again by The New York Times, that Coca-Cola had provided millions of dollars in funding to scientists who “sought to play down the link between sugar and obesity”. Shortly afterwards it was revealed that the US confectionery industry was funding research with an almost comical theme: To suggest that children who eat sweets weigh less than those who don’t. One is left wondering where they found a cohort of the latter, but never mind.
The Sugar Association, when questioned about the 1967 outrage, admitted that it should have been more transparent, but added that industry-funded research had shown that sugar does not have a unique role in heart disease. My emphasis.
Speaking of diet and calories, I came across an interesting snippet the other day: It seems that chopping and cooking food makes calories more easily accessible during digestion. Richard Wrangham, a primatologist at – once again – Harvard, suggests that the evolution of humankind needed the development of cooking. I shall remember that when I’m next rattling the pans.
I also learned more about a subject I mentioned here before: Resistant starch. The theory is that, say bread or pasta, that has been cooked, cooled, and reheated (like toast or microwaved leftover tagliatelle) has its glycaemic index (GI) lowered. I now read that scientists in Sri Lanka have found that the GI of rice that is cooked, anointed with coconut oil, cooled and reheated is halved. I can’t find a reference to an in vivo study, but it’s encouraging for those of us who like an occasional carb fest.
This puts me in mind of the joys of toasted sourdough with maybe some goose or pork rillettes and the perfect wine to accompany such an indulgence.
Lifestyle Food JULY-AUGUST 2021 37
It’s a curious thought that ‘calories in, calories out’ is still the mantra well over a century after Atwater refined it, writes Tom Doorley
DAY-TO-DAY BANKING: WHAT ARE THE OPTIONS?
Mr Paul Redmond outlines how customers can respond to recent changes in the banking market
In February 2021, the announcement came that Ulster Bank, a popular high street bank, with branches in every town and city in Ireland and Northern Ireland, had decided to exit the Irish market. Following on from that in early March, Bank of Ireland decided to close 103 branches and in May KBC, a recent entry to the Irish banking world, also announced their imminent departure from Ireland.
Although customers are being told to remain using these banks and their facilities for the immediate future, as the wind down of these banks will be gradual and take some time, at some point in the next year we will have to decide how best to carry out our day-to-day banking.
For products such as mortgages, these banks have already clarified that there is no need to switch – the banks in question will forward on their loan books to another bank and everything will remain the same as what is in place currently. However, it is not quite the same story for our everyday banking; we all tend to use the one bank for all our banking needs, such as current accounts, credit cards, some savings, and maybe some personal lending. We have the apps on our mobile phones, making it all convenient and under the one roof.
With the banks closing up, we will be instructed, with plenty of notice, to begin the process of moving these banking products to another bank. This can create apprehension and questions: What are our options? Do we have only the three main high street banks available? What are their costs? And more generally, what is involved?
Current accounts
We all need a regular bank account that we can use daily, we need a Visa debit card that we can take out cash at ATM machines, tap for our purchases if below €50, or pay with the card if the purchase exceeds this amount. In particular, within the last 16 months as a result of Covid-19, we have never used our current accounts more, as we shopped online and tried to avoid using cash.
So, what should we look for when deciding?
The first factor is to consider the monthly cost of operating a regular current account? The website www.CCPC.ie is an excellent impartial site that compares all the costs of every provider, breaking it down into the monthly cost and what you get for that fee. Some banks offer a one-off monthly fee and within that all direct debits, standing orders, ATM withdrawals, transactions etc, are included. Others will charge you a small fee for each tap. It is worth looking at how you bank. Is the one-off monthly fee a better option as you tap regularly or do you hardly avail of that?
Another option to consider is how adaptable the bank account will be to digital facilities. With the recent connections to Apple and Google pay, are these important to how you bank? Many of these transactions are free so should be considered when comparing.

The most obvious reason most people rarely switch their bank accounts is the actual switching process. Most of us have regular direct debits, payments; salaries are lodged, along with social welfare payments etc. It can be a daunting task to have to inform and co-ordinate these through the creation of a new account.
With the Central Bank switching code, the new bank will provide a switching service to you.
They will help you with the entire process and will agree a time when activity on your account is less frequent to avoid any missed payments. The switching packs from the new bank will cover all areas. It is also a good time to review all the direct debits on your account and decide if they are still live and active or can be deleted.
Credit cards
Again, most of us have our credit card with our current account provider. It helps payments stay on track and accounts can be viewed online within the same site. Changing credit cards is not so daunting as current accounts and many providers offer great enticement to switch. Pay particular attention to introductory rates, balance transfers, the APR rate, and the cost of taking out cash on credit cards.
Savings accounts
As with all the products above, now is a time to look for a better home for your savings. Banks are not giving good rates on regular savings. There has even been talk of introducing negative rates for those with cash in savings accounts. If you have substantial savings, do you need access to it all immediately? Can you separate it into an emergency cash fund and diversify into other savings areas where the return is better?
With the departure of these high street banks and branches closing, it is clear that the future for banking is changing considerably. The need for a local branch is lessening and the digitalisation of all retailers' services allow us to perform all our banking on our mobile phones or through the bank’s website. Remember, there is no immediate need to close accounts. You will be given sufficient time, so take that time to choose wisely.
Mr Paul Redmond (CPA,QFA, FAIA) is Managing Partner of RDA Accountants Limited. He is a member of the Institute of Certified Public Accountants. He is also a Fellow of the Association of International Accountants and a qualified financial advisor.
38 JULY-AUGUST 2021 Life Finance
PRODUCT NEWS
NOURISH AND REPAIR OVERWASHED AND SANITISED DRY HANDS WITH BIO-OIL DRY SKIN GEL

DATASCAN LAUNCHES NEW SERVICE TO SUPPORT GPS
Datascan Document Services, Ireland’s specialist medical records processing service provider, has launched a new service to support GP practices across Ireland.
The new fixed price service, Datascan GP, is a batch scanning service for incoming patience correspondence to GP practices and provides a secure method for processing patient information.
through scanning and processing of incoming correspondence, which can be time consuming process and will allow staff to focus more on patient-centred tasks.
As we finally start to emerge from the pandemic and the country opens up to a glorious summer of joyful meetups with family and friends, our hands – which have been washed and sanitised every step of the way during this time – are more deserving than ever of extra care and attention. The use of aqueous soaps and alcohol-based products, while key to reducing infection, can strip the skin of its natural protective layer (sebum), leaving those hands dry, cracked and painful. Bio-Oil Dry Skin Gel uses pioneering technology to restore and deeply moisturise dry skin, and is the perfect way to bring your hands to their prepandemic softness.
The standard creams, lotions and body butters that are currently used in the treatment of dry skin are made using up to 70 per cent water, but as our skin is water repellent, the majority of this evaporates on contact. Bio-Oil Dry Skin Gel is formulated using
87 per cent oil for an intensely hydrating product. As well as providing deep moisturisation, the oils used include Lavender oil and Camomile oil, which work to calm the red irritated skin resulting from constant washing.
With 92 per cent of women with dry skin conditions such as eczema, noting that their skin felt instantly moisturised and 82 per cent recording a significant improvement in just two days, Bio-Oil Dry Skin Gel is the new hero product for dry skin. We recommend applying a small amount of Bio-Oil Dry Skin Gel after washing hands for at least 20 seconds in warm, soapy water or applying hand sanitiser. Available in 50ml, 100ml, and 200ml, pop one in your handbag, car, and bathroom to ease irritated and cracked hands.
Available at Lloyds, McCabe’s, McCauley’s, and Bio-Oil stockists nationwide.
See www.bio-oil.com for more information.
The new service will enable GPs to process increased patient correspondence due to Covid-19 screening, testing referrals and vaccinations, to ensure all records are up to date during this time.
Through the new service, documents are scanned, matched to a patient’s ID, and delivered via encrypted secure cloud to the GP’s practice. The service is designed to be used as frequently as required and uses the trusted An Post register post service for tracked delivery of the Datascan GP secure document pouches. All data is encrypted with the most up to date security systems for processing patient data, in line with Datascan’s ISO27001 accreditation.
Having up-to-date patient information is vital to GPs and enables them to provide excellent patient care in their practices. Datascan GP saves time and money for practices
Orla Cafferty, CEO of Datascan said: “Our new GP service provides an easy-to-use secure facility for GPs, that allows for better access to patient information, which in turn will enhance the experience for all involved. The service is flexible and can be adapted to the needs of individual GP practices. GPs across Ireland have been under increased pressure during the pandemic, due to their involvement in Covid-19 testing and the roll-out of the vaccination programme. As a result, there has been a large volume of excess documentation and correspondence. Datascan GP is easy to set up and will ultimately save time and money, as staff are freed up to focus on other vital tasks.”
The service operates on a subscription basis, whereby GP practices pay a fixed price per month for scanning. After initial set up, the cost to process a standard batch of scanning is roughly the same as for one GP consultation. Find out more about the Datascan GP service by visiting: https://datascan.ie/ datascan-gp/
Product News JULY- AUGUST 2021 39
Across
ACROSS
1 State of mental strain (6)
1 - State of mental strain (6)
2 Consequently (9)
Down
2 - Consequently (9)
5 Plan; strategy (6)
8 Profound (4)
5 - Plan; strategy (6)
9 Bendy (8)
10 Yellow citrus fruit (5)
8 - Profound (4)
11 Rubbish (7)
14 Contentious (13)
9 - Bendy (8)
16 Regain strength (7)
18 Measure of the purity of gold (5)
3 Notable feat (7)
4 Strongbox (4)
5 Person aged 13-to-19 (8)
6 Ascend (5)
7 Unwell (3)
12 Promise with certainty (9)
13 Truly (8)
10 - Yellow citrus fruit (5)
20 Animal that hunts (8)
11 - Rubbish (7)
22 Moral obligation (4)
23 Force; vigour (6)
24 Aureate (6)
14 - Contentious (13)
16 - Regain strength (7)
15 Thing causing outrage (7)
17 Command (5)
19 Haul (4)
21 Flee (3)
18 - Measure of the purity of gold (5)
20 - Animal that hunts (8)
3 - Notable feat (7)
4 - Strongbox (4)
5 - Person aged 13 - 19 (8)
6 - Ascend (5)
7 - Unwell (3)
12 - Promise with certainty (9)
13 - Truly (8)
15 - Thing causing outrage (7)
17 - Command (5)
40 JULY-AUGUST 2021
Crossword
SCRIBBLE BOX DOWN
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24
Latest module
Common infant feeding issues
This module by Prof Afif EL-Khuffash, Consultant Neonatologist, Rotunda Hospital, Dublin discusses the commonest infant feeding issues (colic, gastro-oesophageal reflux disease, and cow’s milk allergy) and how to manage them.
Infantile colic commonly persists up to six months of age. True or false?
Successful completion of this module will earn you 2 CPD credits visit www.medilearning.ie/nursecpd.ie
Free CPD – accessible on android, iPhone and tablet
Free independent CPD for Irish nurses A B C






















































































































































LCP FAST AND EFFECTIVE RESOLUTION OF COW’S MILK ALLERGY SYMPTOMS WITHIN 3-14 DAYS From Birth Call to order samples 1800 923 404 1. Infants symptomatic on an Extensively Hydrolysed Formula 2. Faltering Growth 3. Severe Gastrointestinal Allergies 4. Anaphylaxis 4 Red Flag Indicators for when to use Neocate LCP3-5 For more information visit www.nutricia.ie Email: support.ireland@nutricia.com Neocate LCP is a Food for Special Medical Purposes for the dietary management of cow’s milk allergy, multiple food allergies, and for infants who require an amino acid based formula from birth. It must be used under medical supervision after consideration of all feeding options, including breastfeeding. Accurate at time of publication: April 2021 REFERENCES: 1. De Boissieu et al. J. Pediatrics. 1997; 131(5); 744-747. 2. Vanderhoof, J.A. et al. J. Pediatrics. 1997; 131(5) 741-4. 3. Meyer et al. J Allergy Clin Immunol Pract. 2018; 6(2):383-399 4. Fox et al. Clin Transl Allergy. 2019; 9:40 5. Luyt et al. Clin Experimental Allergy. 2014; 44:642-672 Available in pharmacies nationwide. GMS CODE: 81137 1,2 This information is intended for Healthcare Professionals only.