Consultant challenges
Comprehensive coverage of this year’s IHCA AGM and Annual Meeting, which took place virtually earlier this month

Tackling thrombosis in 2020
Consultant Haematologist Dr Barry Kevane spoke with Pat Kelly about the need to identify patients at risk of thrombosis and how Covid-19 has affected haematology services
PAGE 12
Suspicious minds
Mr Niall Rooney, Legal Counsel in Medisec, provides advice for medical practitioners on the growing issue of patients recording consultations

PAGE 17
The art of vaccination persuasion
Many anti-vaxxers are not set in their beliefs and are open to having their minds changed, according to Dr Lucia Gannon
PAGE 18
HSE ‘was not monitoring’ use of derogations policy


CATHERINE REILLY
The HSE has not been collecting any national data on healthcare workers brought back to work while restricting their movements due to Covid-19, or examining whether this has led to further infections, the Executive has informed health sector unions.
However, Clinical Lead of the HSE Workplace Health and Wellbeing Unit, Dr Lynda Sisson, told the Medical Independent (MI) “we are collecting that data now”.
Dr Sisson also said questionnaires have been sent to acute and community sites in regard to the number of derogated workers. She said the guidance is currently with the pandemic infection control team for ongoing review.
“We do believe, however, derogations are necessary in some cases, so derogation guidance will continue. What we will be doing in the next few weeks is monitoring it much more closely than we have
been able to so far.”
Asked if the policy had been overused, Dr Sisson said: “We just don’t know that as yet. But we will be looking to see that it is used judiciously and appropriately.”
However, health sector unions have expressed “grave” concern about the operation of the policy.
Director of Industrial Relations at the Irish Nurses and Midwives Organisation, Mr Tony Fitzpatrick, told MI local managers have been “derogating left, right, and centre, because they don’t have staff, or they cannot get replacement staff”.
This situation presented a “significant risk to patients, but also to colleagues working within those services”.


He added that healthcare worker infection was an “issue we are raising constantly with the HSE”. The IMO has also expressed concern.
In early October, the health unions jointly informed the HSE there were “several questions” outstanding after a meeting with the Executive. These questions related to the
“negative impact” of the derogations policy on the ability to provide a safe working environment; the ability to ensure asymptomatic healthcare workers were not infectious; the “absence” of a testing policy to balance this policy; the “absence” of any measurement of related infections among other staff or patients following the managerial decision to derogate under this policy.
According to the unions’ correspondence, Dr Sisson told the meeting that derogations were granted by local management and no records were held at national level on the number, location or grade. There was no national surveillance of the potential impact of derogations on spread of the virus.
The HSE policy permits derogations for healthcare workers who are restricting their movements (eg, as a close contact) if deemed “essential to critical service needs”. The policy does not apply to close contacts of a suspected or confirmed case in their home; or those with a positive Covid-19 test.

Under the policy, ‘essential’ healthcare workers entering Ireland who would otherwise be required to restrict their movements, may also be derogated. While the policy requires that occupational health should be informed, it is question-
able to what extent this is occurring.

“If we’re not informed of healthcare workers being derogated following travel then it’s very difficult for us to provide monitoring and ensure they are aware of the risks,” commented one specialist.
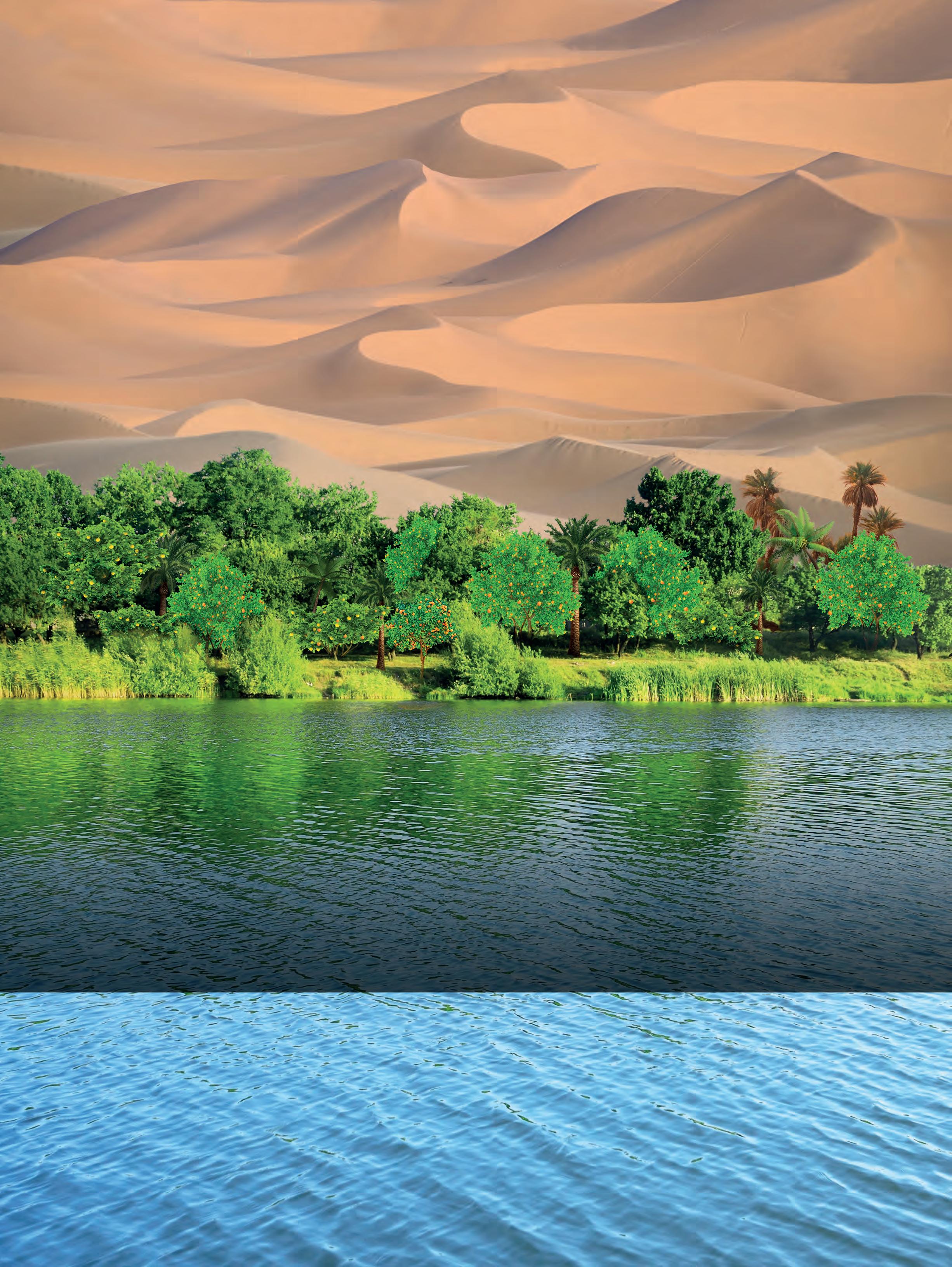
As part of the Sláintecare-funded expansion of the heart failure service developed by Portiuncula University Hospital (PUH) and Galway Primary Care, an echocardiogram and holter monitoring service has been rolled out to three primary care centres in Galway (Ballinasloe, Mountbellew, Portumna) and to Monksland in Roscommon. Pictured L-R are: Dr Aidan Flynn, Consultant Cardiologist, PUH; and Ms Valerie Teehan, Cardiac Physiologist, Ballinasloe Health Centre

Medical Council’s education and training processes not sustainable
CATHERINE REILLY

The Medical Council has conducted an “internal audit” of its legal responsibilities in medical education and training due to concern that the current processes are not sustainable.
The regulator’s annual report for 2019 outlined a risk of not fulfilling all statutory responsibilities in this area “due to insufficient capacity to address the associated increased workload”.
The internal audit led to the development of a high-level quality improvement plan and identified key areas for improvement.
“This is very much in its infancy at present and will be considered by ETC [education and training committee] in October,” a Council spokesperson told the Medical Independent

According to the annual report, the current practice of assessing every medical programme (basic and specialist); every organisation that delivers these pro-
grammes (medical school and postgraduate); and inspecting the places where intern and specialist training is undertaken on a five-year cycle is “neither sustainable nor the best use of resources”.
In 2018 the Medical Council commissioned Health Care Informed to commence a project to develop a single suite of standards across the medical education continuum. This project is still underway with a completion date in 2021. The new standards will go out for consultation with key stakeholders before being finalised. Once approved by Council, a process and approach will be developed to support and implement the new standards.
“Our education and training rules currently state an accreditation cycle is for a period of five years,” said the Council’s spokesperson. “As part of the quality improvement plan we will be reviewing the education and training rules and the duration of accreditation/inspection cycle.”
OUR PAPER IS NOW COMPOSTABLE, AS WELL AS RECYCLABLE NEWS 1-14 ● OPINION 15-18 ● MCQS 20 ● CLINICAL 23-48 ● LIFE ● MOTORING 50-51 ● QUIZZES 52 ● RECRUITMENT 53-55 26 OCTOBER 2020 ● ISSUE 25 VOLUME 11 ● NEXT ISSUE 5 NOVEMBER 2020 €5.95
PAGE 8-10
▼ This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 of the SmPC for how to report adverse reactions. Legal Category: S1A. Marketing Authorisation Holder: Pfizer Europe MA EEIG, Boulevard de la Plaine 17, 1050 Bruxelles, Belgium. For further information on this medicine please contact: Pfizer Medical Information on 1800 633 363 or at medical.information@pfizer.com XELJANZ® in combination with methotrexate (MTX) is indicated for the treatment of moderate to severe active rheumatoid arthritis (RA) in adult patients who have responded inadequately to, or who are intolerant to one or more disease-modifying antirheumatic drugs. XELJANZ® in combination with MTX is indicated for the treatment of active psoriatic arthritis (PsA) in adult patients who have had an inadequate response or who have been intolerant to a prior disease-modifying antirheumatic drug (DMARD) therapy. PP-XEL-IRL-0552 | Date of preparation: August 2020 INDIC A T E D FOR RA | Ps A THI S I S MODE RN MED I CIN E REGISTER FOR OUR NEXT GP EDUCATIONAL WEBINAR ‘WOMEN AND MEN’S HEALTH’ SATURDAY 28TH NOVEMBER CME Accreditation applied for. Practice Nurses and Physiotherapists welcome. RSVP: events@beaconhospital.ie










THI S I S MODE RN MED I CIN E REGISTER FOR OUR NEXT GP EDUCATIONAL WEBINAR ‘WOMEN AND MEN’S HEALTH’ SATURDAY 28TH NOVEMBER. To receive notification of our webinars email events@beaconhopsital.ie INTRODUCING OUR NEW CONSULTANTS
Ms Emma Cashman Consultant ENT Surgeon, Adults & Paediatrics
Dr Michel de Wildt Consultant Urologist
Mr Fardod O’Kelly Consultant Paediatric & Adolescent Urologist
Dr Lisa Prior Consultant Medical Oncologist
Dr Amy Rigby Consultant in Respiratory & GIM
Dr Eddy Ferrufino Rivera Consultant in Respiratory & GIM
Dr Basabjit Das Consultant in Pain Management & Anaesthesiology
Mr Brendan Fennessy Consultant ENT Surgeon, Adults & Paediatrics
Mr Deepak Thomas Consultant Oral Surgeon
Ongoing concern over drop in cervical smears
NIAMH CAHILL
The number of women who had a cervical smear test in September fell by almost 14 per cent when compared to September 2019, according to the HSE.
In September 2019, around 18,300 people had a cervical smear test compared to around 16,000 this year, said a HSE spokesperson.
Over 118,000 HPV cervical screening invites have been issued since CervicalCheck recommenced on 6 July, HSE data showed.
Despite this, just 31,000 cervical screening tests have taken place in primary care since the programme restarted.
Around half of the tests processed have been for women who presented with invite letters. The rest have been for those whose GP believed would benefit from early testing.
“The number of people who received a cervical screening test through CervicalCheck between the start of January and the end of August this year was 57,925. Since July 2020, 65.5 per cent of people screened in primary care were under 45 years,” said a HSE spokesperson.
“The National Screening Service is making considerable effort to increase uptake of cervical screening amongst those who have received priority invitations.
Healthcare worker contact tracing ‘not
CATHERINE REILLY
“Our restart plan involves offering screening to those people who have been waiting the longest for screening, proportionally, and new entrants to the programme. After this we are inviting those on routine recall screening.”
It understood that some GP surgeries are not currently undertaking screening tests.
According to Dublin GP Dr Ray Walley, whose practice is undertaking smear tests, GPs have been advised by CervicalCheck they can only perform smear tests on patients with a CervicalCheck invitation.
He said that GPs have no visibility on which patients are issued with invitations and that the success of the programme in the past has been down to the personal relationship built up over several years between patients, nurses, and GPs.

According to the HSE, a targeted advertising campaign to encourage those who have received invites to attend for screening has been running since July. The campaign is also aimed at raising awareness of the new HPV cervical screening test.
The advertising campaign will continue and expand to include out of home advertising.
“In the new year, we will plan media activities for Q2, 2021 onwards,” according to the HSE.
HPSC issues guidance on Covid-19 and ventilation

NIAMH CAHILL
The effect of ventilation on the transmissibility of SARSCoV-2 remains unclear, according to updated guidance by the Health Protection Surveillance Centre (HPSC).
The guidance provides general recommendations for schools, commercial and public buildings, excluding healthcare settings, on how to boost ventilation.
According to the document, crowded indoor spaces are associated with increased SARS-CoV-2 transmission.
It stated: “Out of 318 outbreaks (classified as three or more cases in a single setting) examined in China, only one could be traced back to transmission in an outdoor space.”
Furthermore, “activities involving forceful expulsion of air, such as singing, loud, excessive talking, and high-exertion fitness routines have been associated with
Effective contact tracing has not been “humanly possible” in some healthcare settings due to under-resourcing of occupational health departments, the Medical Independent (MI) has been informed.
In spring, departments received redeployed staff, but most have since been taken back. In some areas, there are local arrangements to support occupational health departments in contact tracing. However, as Covid-19 cases have escalated, the ability to do this work is under increasing strain.
Occupational health specialists reported to MI that services were stretched
pre-pandemic, with one doctor describing current work pressures as “horrendous”.
Another warned: “There is no software for healthcare worker contact tracing, we haven’t been provided with any contact tracers. It is a very serious situation and very misleading I think, in the sense the public and other healthcare workers… I presume assume things are not like this.”
“The consequences are you could have possibly people going into work who shouldn’t be at work; you have people not being swabbed who need to be swabbed.”
Dr Lynda Sisson, Clinical Lead of the HSE Workplace Health and Wellbeing Unit, told MI: “We have a plan in place to develop a contact tracing system that will remove the everyday contact tracing from the occupational health departments in a matter of months. We are looking at every possible avenue to assist occupational health to focus on the key core competencies for the occupational health teams.”
Dr Sisson said specialist input from occupational health “would be part of the model”. See news feature, p4-6

BEAUMONT HOSPITAL RECEIVES INTERNATIONAL RECOGNITION FOR EXCELLENCE IN CARDIOVASCULAR CARE

Beaumont Hospital is proud to announce the certification of our Cardiac Rehabilitation programme by the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR). This certification is recognition of Beaumont Hospital’s commitment to improving the quality of life of patients by ensuring the delivery of high-quality patient-centered care.
Covid-19 outbreaks.”
As yet, there is no conclusive evidence that the virus remains viable or infective in aerosolised form in “real world situations”, stated the guidance.
It concluded that “further research is needed to determine what contribution, if any, airborne transmission makes to the Covid-19 pandemic”.
In schools, it is advised that teachers are provided with instructions on how to manage classroom ventilation.
“In classrooms that rely on natural ventilation, consider opening the windows 15 minutes before the classroom is occupied to ventilate the room. Similarly, leave windows open for 15 minutes after the classroom is emptied,” the guidance outlined.
Separately, the HPSC has produced guidance for healthcare professionals on SARS-CoV-2 and influenza testing this winter.

The Hospitals multi award-winning Cardiac Rehabilitation programme is internationally recognized as a centre of excellence for cardiac rehabilitation and secondary prevention due in no small part to the dedication and expertise of the staff who provide the service. This comprehensive programme of care provides supervised exercise, training, education, stress management and psychological supports for patients with cardiovascular problems (e.g. heart attacks, coronary artery bypass graft surgery, heart failure and implantable devices) to recover faster and live healthier. CR is not only proven to be cost-effective, but reduces mortality, morbidity and hospital readmissions.
To earn accreditation, Beaumont Hospital’s CR programme participated in a rigorous application process requiring extensive documentation of the programme’s practices and its performance was benchmarked against key performance indictors (KPIs) associated with the highest international standards of cardiac rehabilitation. AACVPR Program Certification is the only peer-review accreditation process designed to review individual programmes for adherence to standards and guidelines developed and published by AACVPR and other related professional societies. Each program’s application is reviewed by the AACVPR Program Certification Committee, and certification is awarded by the AACVPR Board of Directors.
AACVPR-certified programs are recognized as leaders in the cardiovascular rehabilitation field because they offer the most advanced practices available and have proven track records of high-quality patient care. Beaumont Hospital is the first CR centre in Europe to successfully achieve certification of this standard of care – which is valid for three years. Well earned by all the staff in Cardiac Rehab

THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 3 News
Pictured in the CR unit are Caitlin Brycleland, Deirdre Dodd, Jonathan Gallagher, Breda Hannon, Professor Ricky Sheahan, Amanda Murphy, Helen Newton. Missing from the picture are Alison Cahill, Triona Slack, Ger Tonge and Isabela Caramlau
humanly possible’ in some areas
Behind the lines of Irish occupational medicine
As long-standing issues around resourcing and recognition deepen during the pandemic, specialists in occupational medicine warn of a ‘tipping point’. Catherine Reilly reports
Occupational health departments are the ‘engine rooms’ of healthcare – or as one observer described, the ‘thin line protecting the frontline’. From pre-placement assessments to blood exposure management, immunisations to health surveillance, they are paramount to healthcare workers’ health and safety.
But what if the ‘engine room’ overheats?
Several specialists in occupational medicine spoke to the Medical Independent (MI) about key concerns for their specialty: Resourcing; workload; burnout; governance structure; morale; recognition. They were worried for the health of colleagues. “It is not just the doctors, it is our nursing staff, they are drained and burned out as well,” one noted. “I am concerned for them and I am concerned for us.”
The workload has exploded “20-fold” due to Covid-19, one specialist said. Services were already stretched pre-pandemic and little extra resourcing has materialised, MI was informed.
Departments are undertaking Covid-19 contact tracing in healthcare; arranging staff testing; guiding and supporting contacts or those diagnosed (including ‘long Covid’ cases); assessing and advising atrisk staff; and monitoring staff derogated by management.
The work of occupational health is often led by one specialist physician, with nursing and administrative support. They cover acute and community sites with thousands of staff.
There are 16 whole-time equivalent physicians in the public system and one vacancy, according to the HSE.
In early October, a specialist told MI departments were at “a tipping point”.
“When you take the extra pre-placements; the seasonal influenza vaccinations; the high-risk and very high-risk assessments for Covid and fitness for duty; the contact tracing piece; management of healthcare workers who are positive; the healthcare workers who have ‘long Covid’ symptoms and rehabilitating them, on top of the normal workload, and managing the team you have been given and trying to do it in a safe manner, it is a colossal challenge.
“I wouldn’t want healthcare workers to think we are not going to meet their re -
quirements,” they added carefully. “But I don’t know at what personal cost to ourselves.”
‘Soul destroying’
Another specialist told MI, “right now, most of our normal work is suspended.” This situation was “testing” local relationships with managers.
“Because naturally managers need people at work, they need guidance, they need reports. We are not able to do anything in a timely manner …it is soul destroying, it is dire.”
“We are getting a huge number of referrals,” they continued. “One of the biggest workloads is at-risk workers …it varies between people who may not fit into a risk group and people who are very, very high risk. The issue is there are hundreds of people not at work until [assessments] get done. We cannot get through them all, and we are getting loads, and we are still getting them.”
In spring, redeployed staff were assigned to work in contact tracing; these staff had since been taken back, they said. There was no weekend or out-of-hours nursing or administrative support.
“There is no software for healthcare worker contact tracing, we haven’t been provided with any contact tracers. It is a very serious situation and very misleading I think, in the sense, the public and other healthcare
workers… I presume assume things are not like this.
“The consequences are you could have possibly people going into work who shouldn’t be at work; you have people not being swabbed who need to be swabbed
“[The situation] is inhuman and no sign of any assistance from anywhere…”
The HSE Winter Plan promises more resourcing for occupational health. The details are currently being finalised, stated the HSE.
The plan anticipates increased absenteeism and doubling of referrals to occupational health “due to staff exhaustion, and post-Covid-19 fatigue”; doubling of influenza vaccination clinics; sustained and increased levels of contact tracing (estimated at c. 2,000 staff cases per month, for assessment, testing and contact tracing); and increased need for pre-employment assessment and training.
Doctors emphasise that departments need to be properly resourced for an increase in pre-placement assessments – new staff must be cleared by occupational health.

“It is not a paper screen, a pre-placement encompasses providing the healthcare workers with vaccines to protect themselves, such as hepatitis B; varicella-zoster virus; measles, mumps, rubella, pertussis; seasonal influenza; and that is multiple visits.”
Some staff recruited from overseas require tuberculosis clearance involving a chest x-ray, and a blood test.
“So, complex pre-placement health assessments which are not conducive to box ticking exercises.”
As winter approached, this specialist said a “perfect storm” was brewing.
Clarity
The pandemic has placed unprecedented demands on occupational health. It has also deepened pre-existing challenges and concerns.
The governance structure is a source of discontent among some specialists. A lack of clarity around the structure is cited.
One specialist said occupational medicine has been “gerrymandered by the HR fraternity”.
Many occupational health physicians report to Dr Lynda Sisson, Clinical Lead of the HSE Workplace Health and Wellbeing Unit, which is in the HR Division. Dr Sisson is also a HSE Deputy Director of Human Resources and the current Dean of the Faculty of Occupational Medicine.


Speaking to MI, Dr Sisson said she has
“line management responsibility for many of the occupational health physicians, but we work very well in collaboration with each other”.
The unit allocates and appoints to phys ician roles. Dr Sisson said this “would be done in consultation with the services”.
Dr Sisson said the HSE had taken a number of steps to assist occupational health departments, including outsourcing some pre-placements and expanding access routes to influenza vaccination.
“We have a plan in place to develop a contact tracing system that will remove the everyday contact tracing from the occupational health departments in a matter of months,” she said (see panel on page 6). “We are looking at every possible avenue to assist occupational health to focus on the key core competencies for the occupational health teams.”
Dr Sisson said she is currently in contact with departments in regard to Winter Plan and budget funding.
She praised the work of the teams amid the pandemic pressures.
“It has been very challenging, not least because we are a very small group of people and we have had a huge amount of demands placed on us.”
Consultant status
The ongoing denial of consultant status is a festering sore, which will challenge the retention of trainees.
Higher specialist training in occupational medicine is a four-year programme, funded by the HSE and managed by the Faculty. Doctors can obtain specialist registration with the Medical Council after completing training. However, they do not get a consultant contract in the public health service (they are recognised as consultants in the NHS).
The 2010 report by management consulting firm the Hay Group recommended consultant status for occupational medicine specialists. Recently, Ernst and Young has been engaged by the HSE to “review” services (the HSE said the cost of this exercise was commercially sensitive).
“Nobody else is getting reviews, and in the middle of a pandemic they want to do a review of what we are doing,” a specialist told MI. “Obviously as you can imagine we are not best happy about this.”
“We are beginning to think there is pattern here where ‘we want another investigation into what you are doing, what you
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 News Feature CATHERINE
4
REILLY catherine@mindo.ie
Dr Lynda Sisson
are not doing…’.”
According to the HSE, it commissioned the review as the services had “changed and expanded over the years”.
The HSE said consultant status “is the subject of ongoing deliberations with wider stakeholders”.
“Our specialty is always about keeping our heads below the parapet, always being in the background,” said one doctor. “You would see colleagues in your department; you don’t go to the consultant room because you are always the ‘physician for healthcare workers’, in some aspects.”
But lack of official recognition eats away. “There is a bit of an imposter syndrome, to be honest, when you are dealing with respiratory physicians, microbiology consultants, infectious diseases consultants, and you are sitting there and you are not recognised….”
It is not just about a group ‘wanting more’, stated this doctor. There are more far-reaching implications.
“If we don’t sort out the terms and conditions we are going to leak people to the private sector the whole time, then we are left with non-specialists in our departments. Healthcare is probably the trickiest occupa-
tional healthcare service to provide, where you have got biological exposures; labs; fitters; maintenance; you’ve got people driving, absolutely everything in the Health Service Executive.”
IMO Industrial Relations Director Mr Anthony Owens said: “We had pursued it [consultant status]. There is an added impetus to it now because of the huge pressures the pandemic has caused on the delivery of occupational medicine, occupational health services…. We are looking for serious engagement with the HSE and Department of Health to get this sorted out.”
What contracts have specialists been given?
“Here is the peculiar thing, they are on a range of contracts which incorporate many of the elements of the consultants contract, but not all of them,” said Mr Owens.
“Salary is certainly a part of it but there is other stuff in the contract they don’t get, such as the rest days and so on, and the guarantee of support of teams as set out in the contract, which again, I would say is nearly as important.”
Some new entrants were put on a defunct pay scale, which Mr Owens described as “an egregious abuse” of these doctors. “This is a
defunct pay scale that applies to nobody else, it is not in the Department of Health consolidated pay scales, all 100-odd pages of it. It was plucked off a shelf and applied to new entrants into occupational medicine.”
Stranger still, Mr Owens said the HSE has also advertised and appointed other specialists in occupational medicine onto the recognised consultant contract salary scale, even while applying a defunct scale in other situations.
‘Grave concern’ about impact of HSE derogation policy
Health sector trade unions “remain gravely concerned” about the operation of the HSE Covid-19 derogation policy, authored by the Workplace Health and Wellbeing Unit. Local managers are derogating “significant numbers of staff to return to work” amid shortages and pressurised services.
The HSE policy permits derogations for healthcare workers who are restricting their movements (eg, as a close contact) if deemed “essential to critical service needs”. The policy does not apply to close contacts of a suspected or confirmed case in their home, due to the higher risk of transmission; or those with a positive Covid-19 test.
Derogations are decided by management, who must notify the occupational health department. Management must complete a risk assessment and send a copy to occupational health, when a healthcare worker is derogated.
According to the policy, healthcare workers will be actively monitored twice daily by their line manager/designate. Occupational health must be informed of those requiring active monitoring. “Daily active monitoring will also be carried out by occupational health for these HCWs [healthcare workers], usually via daily text message system.”
An occupational medicine specialist told MI the position of occupational health is that close contacts should be stood down from work.
In early October, the health unions informed the HSE there were “several questions” outstanding after a meeting with the Executive.
These questions related to the “negative impact” of the policy on the ability to provide a safe working environment; the ability to ensure asymptomatic healthcare workers were not infectious; the “absence” of a testing policy to balance this policy; the “absence” of any measurement of related infections among other staff or patients following the managerial decision to derogate under this policy.
At the meeting, the health unions had asked how many derogations were granted, the location and grade. They also asked if any derogations were linked to
subsequent case(s).
According to the unions’ correspondence, Clinical Lead of the Workplace Health and Wellbeing Unit, Dr Lynda Sisson, told the meeting that derogations were granted by local management and no records were held at national level on the number, location or grade. There was no national surveillance on the potential impact of derogations on spread of the virus.
In light of the rate of healthcare worker infection, the derogation policy should be reviewed and amended urgently, according to the unions. In the interim, they said a national oversight process must be put in place.
To date, over 9,700 healthcare workers (described as people who work in health facilities) have had a confirmed diagnosis of Covid-19. This represents over 20 per cent of all confirmed cases. According to the Health Protection Surveillance Centre, there have been 340 healthcare workers hospitalised, and eight have died. The national public health emergency team is considering serial testing requirements for asymptomatic people who work in healthcare settings.
IMO Director of Industrial Relations Mr Anthony Owens told MI the level of healthcare worker infection was “concerning and something we are monitoring”. He said there are questions around “ongoing capacity shortages” and “how that is going to impact on members as services reopen”.
Director of Industrial Relations at the Irish Nurses and Midwives Organisation, Mr Tony Fitzpatrick, said local managers have been “derogating left, right and centre, because they don’t have staff, or they cannot get replacement staff”.
This situation presented a “significant risk to patients but also to colleagues working within those services”.
He added that healthcare worker infection was an “issue we are raising constantly with the HSE”.
Of members who have had Covid-19 infection, “there is a cohort, and we are getting more and more contact from them, who have been adversely affected” in the form of ‘post-Covid’ syndrome.
“We have members with myocardi-
tis, with tachycardia, ongoing breathing problems, ongoing lethargy, circulatory problems in regard to pains in their legs, and not being able to get back to work,” he said.
Mr Kevin Figgis, Organiser for the Allied Health Professionals Sector, SIPTU, said it appeared derogations were conceded on an “‘we will leave it up to yourself locally’ basis”.
“What is the template, what is the barometer you use of ‘these are the risks of bringing the person back, versus the benefits; and the benefits outweigh the risks’? Or is it just the case that someone comes in and applies pressure?”
He also highlighted the “high level of infection among healthcare workers” as worrying.
Mr Figgis emphasised that the pandemic is exacting its toll on the health workforce. He said healthcare workers who need to be absent from work, due to Covid-19, must be fully supported and not lose out financially – and provided examples where this has not occurred.
“These are people who every day go to work to help the sickest of the sick and protect all of us. That is really what they are trying to do, and they do it in the face of the infection.
“I don’t think, sometimes, people totally remember that they don’t have a day off from this; they have fought this since the middle of March when the first call of emergency was made. They have fought it from day one; there has been no reprieve.”
Dr Sisson told MI that data is now being collected, while an international review of the literature has been requested. The derogation guidance is currently with the pandemic infection control team for ongoing review.
“We do believe, however, derogations are necessary in some cases, so derogation guidance will continue. What we will be doing in the next few weeks is monitoring it much more closely than we have been able to so far.”
Is the policy overused?
“We just don’t know that as yet. But we will be looking to see that it is used judiciously and appropriately.”
Faculty
MI understands the issue of consultant status was raised recently with the Faculty of Occupational Medicine by trainees seeking its support.
This request is “under discussion at the moment, it is on the agenda of the board”, Dr Sisson told MI
She also said a HSE business case on consultant status is with the Department of Health. Asked if the issue affects trainee recruitment, she said: “I certainly think it doesn’t help.”
Asked if her roles in the HSE meant she was precluded from making certain comments as Dean, such as on the consultant contract issue, Dr Sisson said: “There is a conflict of interest policy in the RCPI. As a matter of fact, at every board meeting, all members are asked to declare if they have a conflict of interest with a particular agenda item, and if they do they would step away from this item. That would be the same for everybody.”
Disillusioned
Currently, the mood among trainees is downcast. “Our SpRs are incredibly disillusioned”, a specialist told MI
“Most of them were not aware they weren’t going to be getting a consultant post at the end of their training.”
Another specialist said: “When you are a trainee and you see ‘specialist training in occupational medicine’ the last thing you’d expect at the end of your training is that you don’t get the same recognition as every other trainee.”
There were 13 trainees in occupational medicine in 2019/2020 and an approved first year intake of three, according to HSE data. A minimum requirement of 18 training places was required by 2022 to meet health service needs, according to a HSE workforce paper titled The Future Requirements For Occupational Health Physicians in the Health Service (Workplace Health and Wellbeing Unit, 2017)
Private practice
Trainees in occupational medicine rotate to private companies during their training to acquire a range of industry-specific experience. According to the HSE workforce paper, “a number of graduates from the training programme are recruited to the private/independent sector.”
The services of private companies are also contracted by some public hospitals. The level of agency/outsourced provision stood at 25 per cent in 2017, according to the HSE workforce paper.
It said “a number” of privately contracted physicians were not specialists, but held Licentiateship of the Faculty of Occupational Medicine (LFOM).
Approximately two of these doctors were working toward Membership of the Faculty (MFOM) and specialist registration with the Medical Council in any three-year period.
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 5 Feature News
Continues on p6 ▸
Some new entrants were put on a defunct pay scale, which Mr Owens described as ‘an egregious abuse’ of these doctors
“This is an area that has been identified as an area of potential growth as a career pathway as an alternative career.”
Within public occupational medicine, there is a view that awarding of consultant status would be disadvantageous to private companies, as it would lead to enhanced terms and conditions in the field.
MI contacted one of the leading occupational health providers, Medmark, for feedback on its position. Medmark also provides services to the public health service.
Dr Paul Gueret, founding partner of the company, told MI: “I, both as a specialist occupational physician and an occupational physician with Medmark, as a national provider of occupational health services, can state without hesitation, that we as individual physicians and as an organisation support the demands of our specialist colleagues within the HSE to be granted consultant status.”
Dr Gueret said he was “not aware” of the perception that granting consultant status in the HSE would be disadvanta-
geous to the private sector. Dr Gueret added that “perhaps more importantly I do not believe it is pertinent to the debate on consultant status for our colleagues in the HSE.”
Dr Gueret, a former Dean of the Faculty of Occupational Medicine, noted that hospitals had historically been set up with a hierarchical structure, which recognised the seniority of the consultant.
“With this long-established structure in place, those doctors who do not have consultant status may find themselves lower down the hierarchy and with a lesser degree of influence on medical matters as a consequence.
“The importance of hospital consultant status is not just because specialist occupational physicians working in the health service deserve it, because I believe that they do, but because it is necessary to have this status for occupational health matters in the health service to be given appropriate attention.
“The Covid pandemic has thrust hospital occupational health services forward to the frontline and demonstrated their importance in maintaining the health service staff in
HEALTHY DATA MEANS TRUE INTEROPERABILITY AND MORE INFORMED CARE.

work, without whom there would be no health service.
“These issues, however, did not begin with Covid, nor will they end when the pandemic is over. For people’s health at work in the health service to be given its necessary relevance, consultant status is not just fully deserved but necessary.”
LFOM
Asked about the role of LFOM-qualified doctors in Medmark, Dr Gueret said the company has a large team of physicians. He said the majority are on the Council’s specialist register for occupational medicine.
“We ask that all doctors working within the practice aspire to this and we support their journey through the various examinations, training and qualifications that are ultimately required to achieve specialist recognition.
“The LFOM offers a valuable initial academic qualification, which can then be built upon by further study, and the MFOM. For me, the important requirement is that they work exclusively within occupational medicine and do so supported by a team of colleagues both specialist and non-specialist, in an environment where they have access to supervision, training and mentoring from senior colleagues.
“In my opinion this immersive professional experience allows them to gain the necessary skills to manage the complex caseload that they are often presented with. From the perspective of Medmark we are not certain that this can be achieved by those who work predominantly within a different specialty but engage part-time in the practice of occupational medicine.”
Dr Gueret also stated SpR salaries in the private sector “are funded solely by the private sector for their duration in the private sector”.
Are public occupational health services edging towards greater private provision?
“I think our time for action is short,” Mr Owens of the IMO told MI. “If one thinks about Sláintecare for a moment, the trajectory of Sláintecare would seem to be the provision of more and more services within the public realm, so I would think that occupational medicine would be one of those services that is built up and bolstered in the public realm.
“There is absolutely a place, I appreciate, for the contractors as well, but that is not what I am talking about here, I am talking about [building up] the public side.”
HSE plan ‘centre of excellence’ for healthcare contact tracing
A contact tracing in healthcare pilot initiative is being developed by the HSE. But there are doubts over how helpful this could prove.
According to the HSE, the contact tracing pilot is “a HSE initiative under the test trace strategy”. The plan is to develop “a centre of excellence for contact tracing for all healthcare workers”.
“You will have seen all the public health specialists saying contact tracing teams don’t replace the public health expertise when it comes to contact tracing and we would probably have a similar opinion, in that local knowledge is very important,” said an occupational medicine specialist.
“A contact tracing team based in Cork don’t know the ins and outs of a particular unit up in Dublin, the nuances around it, that kind of thing. Now, if it does work it will be fantastic, but it remains to be seen if it will help us or not.
“In the meantime, we have to cover weekends and we are trying to put contingency in place. We are worried... It is going to be a very long winter and we barely made it through the first wave unscathed.”
Obtaining the contacts list from managers is not always a smooth exercise, according to another specialist.
InterSystems makes your data healthy so it’s accessible, useable, and ready for action. HealthyData.com
“In this area, there are hundreds and hundreds of managers, like any other area. Some managers will do their best. Some won’t. Some are not skilled sufficiently. Some are not even there at the weekends or they might be on a day off. It is extremely variable and I wouldn’t say that is a reliable way of doing things.”
Clinical Lead of the Workplace Health and Wellbeing Unit Dr Lynda Sisson told MI the contact tracing initiative would facilitate specialist input.
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 News Feature 6
HD05 166x255 2020.indd 1 15/10/2020 10:38
Continued from p5 ▸
Control and protect in asthma1,2 RELVAR ELLIPTA (fluticasone furoate/vilanterol)
Relvar Ellipta is indicated for the regular treatment of asthma in adults and adolescents aged 12 years and older where use of a combination medicinal product (long-acting β 2-agonist and inhaled corticosteroid) is appropriate: patients not adequately controlled with inhaled corticosteroids and ‘as needed’ inhaled short acting β 2-agonists or patients already adequately controlled on both inhaled corticosteroid and long-acting β 2-agonist 3
For Healthcare Professionals only. Images used are for illustrative purposes only. Relvar is well tolerated. Most common adverse events are nasopharyngitis and headache3 PM-IE-FFV-ADVT-190011 September 2020
Relvar Ellipta was developed in collaboration with
References: 1. Woodcock A et al. Lancet 2017; 390:2247–2255. 2. Bateman ED et al. Thorax 2014; 69:312–319.
Relvar® Ellipta® (fluticasone furoate/vilanterol [as trifenatate]) inhalation powder. Each single inhalation of fluticasone furoate (FF) 100 micrograms (mcg) and vilanterol (VI) 25mcg provides a delivered dose of 92mcg FF and 22mcg VI. Each single inhalation of FF 200mcg and VI 25mcg provides a delivered dose of 184mcg of FF and 22mcg of VI. Indications:

Asthma: Regular treatment of asthma in patients ≥12 years and older where a long-acting β 2-agonist and inhaled corticosteroid combination is appropriate and where patients are not adequately controlled on inhaled corticosteroids and “as needed” short-acting inhaled β 2-agonists, or where patients are already controlled on both inhaled corticosteroid and long-acting β 2-agonist.
COPD (Relvar 92/22mcg only): Symptomatic treatment of adults with COPD with a FEV1<70% predicted normal (post-bronchodilator) and an exacerbation history despite regular bronchodilator therapy). Dosage and administration: Inhalation only. Asthma: Patients with asthma should be given the strength of Relvar Ellipta containing the appropriate fluticasone furoate (FF) dosage for the severity of their disease. Prescribers should be aware that in patients with asthma, FF 100 mcg once daily is approximately equivalent to fluticasone propionate (FP) 250 mcg twice daily, while FF 200 mcg once daily is approximately equivalent to FP 500 mcg twice daily. Adults and adolescents ≥12 years: one inhalation once daily of: Relvar 92/22mcg for patients who require a low to mid dose of inhaled corticosteroid in combination with a long-acting β 2-agonist. If patients are inadequately controlled then the dose can be increased to one inhalation once daily Relvar 184/22mcg. Relvar 184/22mcg can also be considered for patients who require a higher dose of inhaled corticosteroid in combination with a long-acting β 2-agonist. Regularly review patients and reduce dose to lowest that maintains effective symptom control. COPD: one inhalation once daily of Relvar 92/22mcg.
Contraindications: Hypersensitivity to the active substances or to any of the excipients (lactose monohydrate & magnesium stearate). Precautions: Pulmonary tuberculosis, severe cardiovascular disorders, heart rhythm abnormalities, thyrotoxicosis, uncorrected hypokalaemia or patients
3. Relvar Ellipta SmPC, 2019, available on www.medicines.ie
predisposed to low levels of serum potassium. chronic or untreated infections, diabetes mellitus. Paradoxical bronchospasm – substitute alternative therapy if necessary. In patients with hepatic with moderate to severe impairment 92/22mcg dose should be used. Acute symptoms: Not for acute symptoms, use short-acting inhaled bronchodilator. Warn patients to seek medical advice if short-acting inhaled bronchodilator use increases. Therapy should not be abruptly stopped without physician supervision due to risk of symptom recurrence. Asthma-related adverse events and exacerbations may occur during treatment. Patients should continue treatment but seek medical advice if asthma symptoms remain uncontrolled or worsen after initiation of Relvar. Systemic effects: Systemic effects of inhaled corticosteroids may occur, particularly at high doses for long periods, but much less likely than with oral corticosteroids. Possible Systemic effects include: Cushing’s syndrome, Cushingoid features, adrenal suppression, decrease in bone mineral density, growth retardation in children and adolescents, cataract, glaucoma. More rarely, a range of psychological or behavioural effects including psychomotor hyperactivity, sleep disorders, anxiety, depression or aggression (particularly in children). Increased incidence of pneumonia, including pneumonia requiring hospitalisation, has been observed in patients with COPD receiving inhaled corticosteroids. If a patient presents with visual disturbance they should be considered for referral to an ophthalmologist for evaluation of possible causes which may include cataract, glaucoma, or rare diseases such as central serous chorioretinopathy. Physicians should remain vigilant for the possible development of pneumonia in patients with COPD as the clinical features of such infections overlap with the symptoms of COPD exacerbations. Risk factors for pneumonia include: current smoking, older age, low body mass index and severe COPD. The incidence of pneumonia in patients with asthma was common at the higher dose of Relvar (184/22mcg). Patients with rare hereditary problems of galactose intolerance, the total lactase deficiency or glucose-galactose malabsorption should not use Relvar. Interactions with other medicinal products:
Interaction studies have only been performed in adults. Avoid β -blockers. Caution is advised when co-administering with strong CYP 3A4 inhibitors (e.g. ketoconazole, ritonavir, cobicistat-containing products). Concomitant administration of other sympathomimetic medicinal products may potentiate the adverse reactions of FF/VI. Relvar should not be used in conjunction with other long-acting β 2-adrenergic agonists or medicinal products containing long-acting β 2-adrenergic agonists. Pregnancy and breast-feeding: Experience limited. Balance risks against benefits. Side effects: Very Common (≥1/10): Headache, nasopharyngitis. Common (≥1/100 to <1/10): Candidiasis of the mouth and throat, pneumonia, bronchitis, upper respiratory tract infection, influenza, oropharyngeal pain, sinusitis, pharyngitis, rhinitis, cough, dysphonia, abdominal pain, arthralgia, back pain, muscle spasms, fractures, pyrexia. Uncommon (≥1/1,000 to <1/100): Hyperglycaemia, vision blurred, extrasystoles. Rare (≥1/10,000 to <1/1,000): Hypersensitivity reactions including anaphylaxis, angioedema, rash and urticaria; palpitations, tachycardia, tremor, anxiety, paradoxical bronchospasm. Marketing authorisation (MA) Holder: GlaxoSmithKline (Ireland) Limited, 12 Riverwalk, Citywest Business Campus, Dublin 24, Ireland. MA Nrs: 92/22mcg 1x30 doses [EU/1/13/886/002]; 184/22mcg 1x30 doses [EU/1/13/886/005].
Legal category: POM B. Last date of revision: June 2019. Code: PI-2046. Further information available on request from GlaxoSmithKline, 12 Riverwalk, Citywest Business Campus, Dublin 24. Tel: 01-4955000.
Adverse events should be reported to the Health Products Regulatory Authority (HPRA) using an Adverse Reaction Report Form obtained either from the HPRA or electronically via the website at www.hpra.ie. Adverse reactions can also be reported to the HPRA by calling: (01) 6764971. Adverse events should also be reported to GlaxoSmithKline on 1800 244 255.
 ALL REPORTS BY DAVID LYNCH
ALL REPORTS BY DAVID LYNCH
32nd IHCA AGM, Saturday 10 October 2020, Virtual Annual General Meeting and Conference

Minister ‘strongly’ commits to end ‘pay inequality’
Minister for Health Stephen Donnelly told this year’s IHCA AGM and annual conference that he “strongly” supports the Association’s calls for the end to pay inequality for ‘new-entrant’ consultants.
The IHCA has demanded the end of consultant salary inequity imposed by the Government on appointments since 2012.
Minister Donnelly said his Government recently agreed to pass enabling legislation to address a number of contract and pay issues.
“On the back of the Government’s decision, I announced we will be seeing some contracts for public health doctors, we will be introducing a new Sláintecare contract.
“I know there are differing views within the IHCA about this contract and we will continue to engage... but what it will see is full pay restoration in line with the existing type A contract and it will have additional benefits as well, which are being thought through at the moment.”
More specifically on the issue of pay inequality, the Minister said the “big outstanding question is pay restoration or pay inequality for type B and type C contracts”.
“This is something I committed to do unambiguously in opposition... and it is something that I am unambiguously and strongly committed to as Minister,” he stated.
“I believe it is one of the changes necessary to unlocking reform and to addressing
[consultant] retention in the public system.
It is a policy I am pursuing strongly.”
In the conference’s closing remarks, Dr Gabrielle Colleran, IHCA Vice President and Consultant Radiologist, Children’s Health Ireland (CHI) at Temple Street, said that the IHCA “welcomed” the Minister’s statement of “support for pay parity for all consultants”.
“But we as an Association have to be really clear that until the Government honour the negotiated 2008 contract and pay all of us equally we can never trust any contract while they are still reneging on their legal obligations to the negotiated contract,” Dr Colleran said.
“So there is an urgent need for a reset button for pay parity so we can trust that they will deal with us in a trustful, authentic way [in the manner] we deal with them and our patients.”
HSE CEO Mr Paul Reid, who also addressed the conference, said that he believed the IHCA “should acknowledge that we have had a net increase of 152 consultants this year across the health service”.
However, he did voice his support for pay parity for consultants and acknowledged the negative impact the present situation had on recruitment and retention of consultants.
“I’m playing a part of bringing that discussion to Government and I do see a po-
Use of telemedicine ‘exploded’ during pandemic
The use of telemedicine has “exploded” during the Covid-19 crisis and more training for doctors is required, the IHCA annual conference was told.
Dr Graham Billingham, Chief Medical Officer, MedPro, Berkshire Hathaway, told attendees that “it is forecast that this will be a US$29 billion industry going forward and that between 10 and 20 per cent of all office visits in the future may be from telemedicine”.
Dr Billingham presented research from the experience in the United States. It was noted at the conference that the recent trend towards telemedicine use has also been reflected in other developed nations, including Ireland.
In the US, during the current crisis, hospital and clinic visits dropped and telemedicine consultations increased.
“It wasn’t one for one, they didn’t completely displace hospital visits and as hospital visits have come back over the last four months, telemedicine has dropped back down, to currently between 10-20 per cent,” said Dr Billingham.
He noted that recent months have exposed how 10 per cent of the US population has limited access to Wi-Fi “so we had a digital divide... we [are also] very concerned about doing adequate physical exams through telemedicine”.
Telemedicine’s limitations where there are language barriers, and in delivering consultations for people with an intellectual or cognitive disability, was also referenced.
“We have seen a marked increase in patient volume,” continued Dr Billingham.
“Patients are more complex, almost every speciality was involved with telemedicine. There is a marked increase in the use of this technology and we all know
that technology has learning curves associated with it and we have been struggling with those in order to meet the needs of our patients.
“We don’t think telemedicine is going away and we expect to see more development in this area and it should be easier in the future for practitioners to deliver the service.”
The experience during the pandemic was that telemedicine seemed to work better for GPs with established patients rather than new patients.
Also addressing the conference, Dr Rob Hendry, Medical Director, Medical Protection Society, said telemedicine has pros and cons.
“But as we get used to it, probably through the training side I think we can get the good bits as well as the limitations.”
“Doctors have almost been on a selftaught crash course during this [pandemic],” he said.
“There is going to be a lot more training. We certainly have been producing a series of training webinars and so forth. A lot of specialities have adopted it and come at it in different ways.
“I think GPs probably have been more used to assessing people remotely. I was speaking to one person who was running a fracture clinic and using video, and that is perhaps where they were not used to doing it. Training is important. Technology will be improving, there is huge investment going into new platforms.
“I think for some specialities it may well become mainstream. For example, certainly speaking to a number of rheumatologists, a number of them have found that really positive and we have also had some good feedback from psychiatrists on its use.”
tential resolution soon,” he said.
Mr Reid also raised the issue of reforms in the context of pay.
“But I do think it needs everybody to jump together... I would also say that you, as the IHCA, have made it very clear that pay is a big issue in terms of improving care,” Mr Reid said.

“But I also would challenge that this can’t be just about pay issues; it has to be about reform, it has to be about changing work practices. And we do really need to look at having two systems of healthcare in Ireland – public and private.”
Mr Reid said while he believed there is a role for both, “it is interesting that one system has quite a massive waiting list that you have been talking about a lot this morning and in essence the private system doesn’t.”
“We really need to look at what are the issues that emerge from that, can we do it differently?”
Speaking before Minister Donnelly, IHCA President Prof Alan Irvine, Consultant Dermatologist at CHI at Crumlin, said there was a need to “rapidly escalate how we recruit consultants”.
“It takes too long to do this; it is 20 months in many cases,” according to Prof Irvine.
“In response to the [HSE] Winter Plan, we pointed out where there need to be measurable timelines – measurable timelines around consultant recruitment and time-
lines around promises on bed capacity.
“We know there is enabling legislation that has been approved around Cabinet and we want to see that worked out quickly and get some real practical solutions.”
He said there were two aspects to pay inequality – fairness and justice and “equal pay for equal work”.
“But if you move beyond that, it is simply not a pragmatic response because you can’t recruit people if you treat them that way. Or at least you can’t recruit them in the numbers and scale and pace that you want. So it is a real false economy.”
Speaking at the opening of the conference, Mr Martin Varley, Secretary General of the IHCA, said that “the key request we have and the discussions we are having with Government and the Minister first and foremost is end the pay inequality that was introduced in 2012”.
“That will allow us fill the 500 vacant permanent posts, that will allows us bring down waiting lists,” Mr Varley said.
The conference also passed a motion supporting the “urgent restoration of pay parity for all consultants appointed on or transferring to the 2008 consultant contract after 1 October 2012”.
The motion called on the Association to “pursue this by whatever means necessary, as determined by the IHCA National Council”.
Looming winter difficulties for consultants
The first winter of the Covid-19 pandemic is going to be “really difficult” for consultants and patients, the IHCA annual conference was told.
Mr Martin Varley, IHCA Secretary General, said that hospitals were looking into “a winter like no other”.
The recently published HSE Winter Plan received some praise during the conference. However, there was also criticism of aspects of the document.
“Credit is due to Minister [Stephen] Donnelly, Paul Reid, and their colleagues on one notable difference in this year’s Winter Plan to previous ones – timing,” IHCA President Prof Alan Irvine told the conference.
“A Winter Plan published before winter is a rarity.”
Dr Gabrielle Colleran, IHCA Vice President, said that “if we look at this winter plan, €600 million is a lot of money... it is a significant injection, you know it is multiples of what we got last year”.
But she added that “the challenge for this winter budget in reality is that we shouldn’t need a winter budget”.
“We should have adequate capacity for winter surges in our system,” she said.
“So by virtue of the fact that we need it, it is almost an admission of failure that the current resourcing and strategy isn’t adequate and isn’t working.”
From the perspective of consultants, Dr Colleran said many are already concerned about what this winter promises.
“I think it is clear from the talks
and from our members that we are heading into a really difficult winter,” she said.
“I think most of us who are working in the sector are already concerned at the way we are seeing trolley numbers.
Dr Colloran said consultants are seeing scheduled care cancelled and staffing deficits due to positive Covid-19 and close contact cases.
“We are having multiple members having to stay home, which impacts our ability to deliver care.”
HSE CEO Mr Paul Reid defended the Winter Plan in his speech to the conference.
“We have secured the biggest investment ever with this Winter Plan from Government with €600 million,” he said.
“To be frank, I was a little bit disappointed with the IHCA response to it.”
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 8 News
Mr Martin Varley



Consultants’ efforts praised amid burnout concerns
There was significant praise for the work of consultants during the Covid-19 pandemic voiced at the IHCA annual conference. However, serious concerns about burnout were also expressed.
“We have a marked increase in burnout with nurses and physicians,” Dr Graham Billingham, Chief Medical Officer, MedPro, Berkshire Hathaway, told attendees about the US experience.
“Healthcare workers were already burnt out and Covid has added additional strain. We know that burnout is associated with medical error,” he said.
“It was a problem before Covid and it is exacerbated now, under the tremendous strain and long hours and clinical exhaustion.”
In terms of measures that could alleviate burnout, Dr Billingham said more training on the issue would be helpful.
“Clinicians are not very good at reaching out for help,” he said.
“We need to be able to allow those conversations and be able to support them... as clinicians we need to support one another, having a cup of coffee, make time for each other and opening those avenues... [we need] staggered shifts to ensure people have adequate time.”
He said that Covid-19 is “not going away and I think everyone needs to approach Covid as a marathon, not a sprint... we need to have sustainability in our healthcare systems and support out colleagues.”
IHCA President Prof Alan Irvine described Covid-19 as a ‘wicked’ problem.
“Something that doesn’t have, frankly, easy or straightforward solutions. It only has solutions that are, in some ways, unsatisfactory for many,” he told the conference.
“I want to say the response of consultants and wider healthcare professionals in the com-
munity has been really truly remarkable and it has been a great source of pride for me to be your President for this year and next. It makes me very determined to represent you as best I possibly can.”
HSE CEO Mr Paul Reid and Minister for Health Stephen Donnelly also praised the work of consultants during the crisis.
“Covid-19 has turned our world upside down,” Minister Donnelly said.
“When I spoke to you last year, Ireland had the lowest level of critical care beds in Europe.
“We had the lowest level of hospital consultants and the highest waiting lists and our healthcare system simply did not have the resources it needed to meet the healthcare demands of our society.
“And yet when Covid did arrive, what we saw from already overstretched healthcare professionals, was quite an extraordinary response and I would like to thank everyone at the conference this morning for your professionalism and your dedication and skill and resilience this year.”
Speaking directly to consultants, Minister Donnelly said “because of your efforts, our hospitals weren’t overrun, our ICU capacity was increased to the level required, and the survival rates from ICU were very strong.
“The response came at a very high cost. It meant our clinicians going for long periods without seeing their friends, families, and loved ones. It meant endlessly working shifts and rotas.
“This work from all of you saved many lives. It came at times at an unbearable cost and I would like to acknowledge that several healthcare workers lost their lives this year while keeping the rest of us safe and I would like to recognise this morning their sacrifice.”
Health service ‘backed into corner’ by crisis
The pandemic has backed the Irish health service into a corner, the IHCA President Prof Alan Irvine told his Association’s annual conference.
He said that current bed capacity levels are “dangerous... we need to run the capacity at around 85 per cent”.
Prof Irvine added that the long waiting lists are “reckless”
“There is no doubt that people will suffer for being too long on waiting lists for conditions that are time sensitive... and there are about 500 consultant posts vacant.
“That is unsustainable, you can’t run a service [that way].”
While calling for serious investment in beds and expansion in capacity, Prof Irvine also looked for reform in how bed capacity is presented.
“We know it is not just the number of beds, we would like to see transparency around the number of beds,” he said.
“Let’s have a dashboard of success rather than a trolley guard dashboard of failure, to create some sense of positivity and forward momentum in our system.
“What I would love to see is weekly or monthly updates
saying ‘we added this number of ICU beds’, or ‘this number of acute care beds’, or ‘we reduced the waiting list by this much’.
“Having a sense of really moving forward – too much of the dialogue is dominated by negativity; we really need to create positivity by delivering transparency.”
Prof Irvine pointed to recently created capacity through modular units, and in the Citywest facility in Dublin, as pointers of what positive measures could be undertaken.
He also said there needed to be more regional and local decision-making in the health service.
“We really want to see devolved decision making where local people are given a framework that can adapt and find local solutions in their communities.”
Minister for Health Stephen Donnelly told the conference that bed capacity needed to be built up “while at the same time modernising the care pathways”.
“We have got to support people in their home, treat people in the community if we can, and then we need a world class,
A unique conference for a unique year
The 32nd IHCA AGM and annual conference was a unique event this year, because of the pandemic, it took place entirely online. In terms of attendance, the virtual conference was deemed a success.
Dr Gabrielle Colleran, who was recently re-elected as Vice President of the Association, said this year’s event was “our highest attendance ever so far, so we are really delighted with that level of participation”.
The Association’s Mem -
Something that is starting to cause concern is the next generation. We are seeing massive disruption in training. We know with certain areas, such as dentistry, students are having to do another final year because they are simply not getting enough hands-on experience. We are also seeing a problem with deskilling in surgery... I know a number of surgeons and colleges and associations have raised concerns about that.”
bership Secretary Dr Conor O’Riordan, Consultant Radiologist, St Luke’s Hospital, Kilkenny, noted a further increase in IHCA members this year to 3,168.


“If you look at it from a decade-long view, you can see there is a 35 per cent increase on what we had back in 2010,” he said. With another increase this year, “we expect further increases in the years ahead”.
Prof Clare Fallon, IHCA Treasurer and Consultant in
We know delivering complex bed capacity isn’t a question of just calling Mattress Mick. We know for every intensive care bed we need six highly trained nurses; we need senior decision-makers. We know it’s the same for acute beds; we need a lot more support in general.”
properly resourced hospital system for those who need it.”
He added it was “critical now that our health system is stabilised”.
“The coming months may well be the most challenging in living memory for our healthcare system.”
Geriatric Medicine, Regional Hospital Mullingar, said: “It has been a strong year financially for the Association with the vast majority of the income from ordinary members’ subscriptions, which is up on the previous financial year.”
She described the IHCA as in “quite a healthy situation” in terms of finance.
Motions were passed at the conference calling for increased ICU capacity; reduction in waiting times for radiology; encouraging consultants to get the seasonal influenza vaccine; and for parity of esteem for mental and physical health.
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 10 News
32nd IHCA AGM, Saturday 10 October 2020, Virtual Annual General Meeting and Conference
We see this across all areas of healthcare. People are afraid to interact with healthcare and to come into healthcare settings because of fear of Covid-19.”
Dr Noirin Russell, Clinical Director of CervicalCheck and Consultant Obstetrician and Gynaecologist, Cork University Maternity Hospital, highlighting that nearly 90 per cent of women have not responded to an invitation to undergo cervical cancer screening in recent months
Dr Rob Hendry, Medical Director, Medical Protection Society
Prof Alan Irvine, IHCA President, on capacity concerns
FROM THE CONFERENCE
VOICES
There is no doubt that people will suffer for being too long on waiting lists for conditions that are time sensitive
In the management of type 2 diabetes 1




THE POWER TO ACCOMPLISH
MORE Multiple benefits * Proven protection †
JARDIANCE is indicated for the treatment of adults with insufficiently controlled type 2 diabetes mellitus as an adjunct to diet and exercise 1
- as monotherapy when metformin is considered inappropriate due to intolerance






- in addition to other medicinal products for the treatment of diabetes
















The most prescribed SGLT2i in Ireland 3
* In addition to glucose lowering, JARDIANCE demonstrated reduction in weight and blood pressure; JARDIANCE is not indicated for weight loss or reduction of blood pressure.1
† EMPA-REG OUTCOME® was a randomised, double-blind, placebo-controlled cardiovascular outcomes trial. Patients were randomised to receive either JARDIANCE 10 mg once daily, JARDIANCE 25 mg once daily or placebo, on top of standard of care. Primary endpoint was 3-point MACE: Time to fi rst occurrence of cardiovascular death, non-fatal MI, non-fatal stroke. 14% relative risk reduction for combined endpoint of cardiovascular death, non-fatal MI, or non-fatal stroke (ARR 1.6%). 2



References

1. JARDIANCE (empaglifl ozin) Summary of Product Characteristics 2019. Available at: http://www.medicines.ie/medicine/16081/SPC/Jardiance+10+mg+and+25+mg+Film-Coated+Tablets
2. Zinman B, Wanner C, Lachin JM et al. Empaglifl ozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117-2128. (& Supplementary Appendix)
Prescribing Information (Ireland) JARDIANCE® (empagliflozin)




















Film-coated tablets containing 10 mg or 25 mg empagliflozin. Indication: Jardiance is indicated for the treatment of adults with insufficiently controlled type 2 diabetes mellitus as an adjunct to diet and exercise: as monotherapy when metformin is considered inappropriate due to intolerance; in addition to other medicinal products for the treatment of diabetes.For study results with respect to combinations, effects on glycaemic control and cardiovascular events, and the populations studied, refer to the Summary of Product Characteristics. Dose and Administration: The recommended starting dose is 10 mg once daily. In patients tolerating empagliflozin 10 mg once daily who have eGFR ≥ 60 ml/min/1.73 m2 and need tighter glycaemic control, the dose can be increased to 25 mg once daily. The maximum daily dose is 25 mg. When used with sulphonylurea or insulin a lower dose of these may be considered to reduce the risk of hypoglycaemia. Renal impairment: The glycaemic efficacy is dependent on renal function. No dose adjustment is required for patients with an eGFR ≥60 ml/min/1.73 m2 or CrCl ≥60 ml/min. Do not initiate in patients with an eGFR <60 ml/min/1.73 m2 or CrCl <60 ml/min. In patients tolerating empagliflozin whose eGFR falls persistently below 60 ml/min/1.73 m2 or CrCl below 60 ml/min, the dose of empagliflozin should be adjusted to or maintained at 10 mg once daily. Discontinue when eGFR is persistently below 45 ml/min/1.73 m2 or CrCl persistently below 45 ml/min. Not for use in patients with end stage renal disease (ESRD) or on dialysis. Hepatic impairment: No dose adjustment is required for patients with hepatic impairment. Not recommended in severe hepatic impairment. Elderly patients: No dose adjustment is recommended based on age. In patients 75 years and older, an increased risk for volume depletion should be taken into account. Not recommended in patients 85 years or older. Paediatric population: No data are available. Method of administration: The tablets can be taken with or without food, swallowed whole with water. If a dose is missed, it should be taken as soon as the patient remembers; however, a double dose should not be taken on the same day.
Contraindications: Hypersensitivity to the active substance or to any of the excipients. Warnings and Precautions: Rare cases of diabetic ketoacidosis (DKA), including life-threatening and fatal cases, have been reported in patients treated with SGLT2 inhibitors, including empagliflozin.

Consider the risk of DKA in the event of non-specific symptoms such as nausea, vomiting, anorexia, abdominal pain, excessive thirst, difficulty breathing, confusion, unusual fatigue or sleepiness and assess patients for ketoacidosis immediately, regardless of blood glucose level. In patients where DKA is suspected or diagnosed, treatment should be discontinued immediately. Treatment should be interrupted in patients who are hospitalised for major surgical procedures or acute serious medical illnesses. Monitoring of ketones is recommended in these patients. Measurement of blood ketone levels is preferred to urine. Treatment with empagliflozin may be restarted when the ketone values are normal and the patient’s condition has stabilised. Before initiating empagliflozin, consider


factors in the patient history that may predispose to ketoacidosis. Use with caution in patients who may be at higher risk of DKA. Renal impairment: See under Dose and Administration; Monitor renal function prior to initiation and at least annually. Cases of hepatic injury have been reported with empagliflozin in clinical trials. A causal relationship between empagliflozin and hepatic injury has not been established. Haematocrit increase was observed with empagliflozin treatment. Osmotic diuresis accompanying therapeutic glucosuria may lead to a modest decrease in blood pressure.
Therefore, caution should be exercised in patients with known cardiovascular disease, patients on anti-hypertensive therapy with a history of hypotension or patients aged 75 years and older. In case of conditions that may lead to fluid loss (e.g. gastrointestinal illness), careful monitoring of volume status and electrolytes is recommended. Temporary interruption of treatment with empagliflozin should be considered until the fluid loss is corrected. Elderly: See under Dose and Administration; special attention should be given to volume intake of elderly patients in case of co-administered medicinal products which may lead to volume depletion (e.g. diuretics, ACEinhibitors). Temporary interruption of empagliflozin should be considered in patients with complicated urinary tract infections. Cases of necrotising fasciitis of the perineum (Fournier’s gangrene), have been reported in patients taking SGLT2 inhibitors. This is a rare but serious and potentially life-threatening event that requires urgent surgical intervention and antibiotic treatment. Patients should be advised to seek medical attention if they experience a combination of symptoms of pain, tenderness, erythema, or swelling in the genital or perineal area, with fever or malaise. Be aware that either uro-genital infection or perineal abscess may precede necrotising fasciitis. If Fournier’s gangrene is suspected, Jardiance should be discontinued and prompt treatment should be instituted. An increase in cases of lower limb amputation (primarily of the toe) has been observed in long-term clinical studies with another SGLT2 inhibitor, counsel patients on routine preventative footcare. Experience in New York Heart Association (NYHA) class I-II is limited, and there is no experience in clinical studies with empagliflozin in NYHA class III-IV. Due to its mechanism of action, patients taking Jardiance will test positive for glucose in their urine. The tablets contain lactose and should not be used in patients with rare hereditary problems of galactose intolerance, total lactase deficiency, or glucose-galactose malabsorption. Interactions: Use with diuretics may increase the risk of dehydration and hypotension. Insulin and insulin secretagogues may increase the risk of hypoglycaemia therefore, a lower dose of insulin or an insulin secretagogue may be required. The effect of UGT induction (e.g. induction by rifampicin or phenytoin) on empagliflozin has not been studied. Co-treatment with known inducers of UGT enzymes is not recommended due to a potential risk of decreased efficacy. If an inducer of these UGT enzymes must be coadministered, monitoring of glycaemic control to assess response to Jardiance is appropriate.
PC-IE-100924 V1 Date of preparation: August 2020

Interaction studies suggest that the pharmacokinetics of empagliflozin were not influenced by coadministration with metformin, glimepiride, pioglitazone, sitagliptin, linagliptin, warfarin, verapamil, ramipril, simvastatin, torasemide and hydrochlorothiazide. Interaction studies conducted in healthy volunteers suggest that empagliflozin had no clinically relevant effect on the pharmacokinetics of metformin, glimepiride, pioglitazone, sitagliptin, linagliptin, simvastatin, warfarin, ramipril, digoxin, diuretics and oral contraceptives. Fertility, pregnancy and lactation: There are no data from the use of empagliflozin in pregnant women. As a precautionary measure, it is preferable to avoid the use of Jardiance during pregnancy. No data in humans are available on excretion of empagliflozin into milk. Jardiance should not be used during breast-feeding. No studies on the effect on human fertility have been conducted for Jardiance. Undesirable effects: Frequencies are defined as very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1,000 to <1/100), rare (≥1/10,000 to <1/1,000), not known (cannot be estimated from the available data). Very common: hypoglycaemia (when used with sulphonylurea or insulin). Common: vaginal moniliasis, vulvovaginitis, balanitis and other genital infections, urinary tract infection (including pyelonephritis and urosepsis), thirst, pruritus (generalised), rash, increased urination, serum lipids increased. Uncommon: urticaria, volume depletion, dysuria, blood creatinine increased/ glomerular filtration rate decreased, haematocrit increased. Rare: DKA. Not known: necrotising fasciitis of the perineum (Fournier’s gangrene), angioedema. Prescribers should consult the Summary of Product Characteristics for further information on side effects. Pack sizes: 10 mg; 28 tablets, 25 mg: 28 tablets. Legal category: POM. MA numbers: 10 mg/28 tablets EU/1/14/930/013; 25 mg/28 tablets EU/1/14/930/004. Marketing Authorisation Holder: Boehringer Ingelheim International GmbH, D-55216Ingelheim am Rhein, Germany. Prescribers should consult the Summary of Product Characteristics for full prescribing information. Additional information is available on request from Boehringer Ingelheim Ireland Ltd, The Crescent Building, Northwood, Santry, Dublin 9. Prepared in July 2020



Adverse events should be reported. Reporting forms and information can be found at https://www.hpra.ie/homepage/about-us/report-an-issue. Adverse events should also be reported to Boehringer-Ingelheim Drug Safety on 01 2913960, Fax: +44 1344 742661, or by e-mail: PV_local_UK_Ireland@ boehringer-ingelheim.com

 3. Data on File. Boehringer Ingelheim
3. Data on File. Boehringer Ingelheim
Tackling thrombosis in 2020
Ahead of World Thrombosis Day, Consultant Haematologist
Dr Barry Kevane spoke with Pat Kelly about the need to identify patients at risk of thrombosis and how those with Covid-19 are at increased risk of the condition
Thrombosis is the third-largest cause of mortality worldwide and experts in the field have long been calling for increased awareness among members of the public and the medical profession alike to help save lives from this preventable but potentially deadly condition.
Ahead of World Thrombosis Day, which took place on 13 October, Dr Barry Kevane, Consultant Haematologist in the Mater Misericordiae University Hospital in Dublin and Ireland East Hospital Group, spoke with the Medical Independent (MI) about the efforts he and his colleagues are making to address the lack of awareness around thrombosis. Dr Kevane is also principal investigator with the University College Dublin (UCD) Conway SPHERE research group and has a special interest in venous thromboembolism (VTE). His main research interests are in thrombosis and haemostasis and he has recently been granted a funding award from Science Foundation Ireland (SFI) to undertake research investigating the mechanisms underlying coagulopathy associated with Covid-19.
Dr Kevane began by explaining the objectives of World Thrombosis Day, a campaign run by the International Society of Thrombosis and Haemostasis (ISTH) to raise awareness of the burden of morbidity and mortality associated with VTE, as well as support national foundations to do the same at regional levels. The organisation Thrombosis Ireland has run a number of successful campaigns in Ireland to this end, including a ‘Stop the Clot’ roadshow involving a double-decker bus that travelled to different regions within the Hospital Groups, providing information to patients and their families at hospitals and community centres. This was recognised as being a highly successful and effective campaign, even in the context of all other global efforts. Similar events this year have been restricted because of Covid-19 but an online VTE Dublin conference, run from the Mater Hospital, recently brought together Irish and international experts to discuss VTE prevention and treatment, and exchange expertise. However, Dr Kevane and his colleagues also work all-year-round with patient groups, such as Thrombosis Ireland, to raise awareness of the risk of VTE.
Mortality
“Until recently, VTE has not been very well recognised as a cause of cardiovascular deaths,” Dr Kevane told MI. “VTE, which comprises mostly deep-vein thrombosis and pulmonary embolism, is the third-leading cause of cardiovascular death, behind myocardial infarction and stroke. While we don’t have good mortality data in Ireland, across the EU, there are approximately 500,000 deaths as a result of VTE [per annum], which is more deaths than prostate cancer, road traffic accidents, HIV and breast cancer combined. There is a huge burden of mortality as a direct consequence of VTE, which is often not recognised, either by healthcare professionals or the general public.”
In addition to that mortality rate, there is also a significant burden of chronic disease associated with VTE. Among patients who develop deep-vein thrombosis (DVT) in lower limbs, 50 per cent or more develop related chronic complications. In pa-
tients with pulmonary embolism (PE), a significant proportion of these also go on to develop significant chronic complications that affect their quality-of-life and ability to work, and overall health.
“According to HSE figures, we would estimate that there are around 11,000 cases of VTE in Ireland each year. One of the things that has been very much to the fore recently, both among people who treat VTE and patients and their relations, is the problem of targeting hospital-acquired VTE,” Dr Kevane told MI. “While most people who ask about blood-clotting risk think about things like long-haul travel or hormonal contraception, what we now know is that the majority of all VTE cases are hospital-acquired – about 60-to-70 per cent of all cases of DVT or PE occur as a consequence of admission to hospital and that’s often because in hospital people are immobilised or they are having surgery, for example. So this is a huge proportion of blood-clotting events.”
Dr Kevane continued: “We also have data now to show that the majority of these events that happen as a result of hospitalisation are preventable and it is now recognised that hospital-acquired VTE is the leading cause of potentially preventable
of cases that are linked to hospital admission occur following discharge – the risk doesn’t necessarily disappear when the patient is discharged from hospital… the risk of clotting persists for a period of time after they are discharged.” Dr Kevane explained that these patients are at risk for up to 90 days after they are discharged from hospital: “So when patients are discharged from hospital, even though their anticoagulant treatment may be stopped at that point, it’s really important that they are educated on the symptoms of VTE because they are potentially at risk for another 90 days and that’s a huge problem.”
In order to address this risk, Thrombosis
Ireland has issued a VTE Alert Card with information on hospital-acquired VTE, including common symptoms, which is distributed to the relevant patients when they are discharged from hospital.
Covid-19 risk
death associated with hospital admissions. A lot of people might assume that the leading cause [of deaths related to hospital admissions] is hospital-acquired infections, but it is actually hospital-acquired blood clots.”
However, there are highly effective measures that can be taken to prevent these events, explained Dr Kevane. These include standardised risk assessments of each patient on admission to hospital and then targeting high-risk patients with anticoagulant medication. The HSE estimated that between 60-to-80 per cent of patients who are admitted to hospital, if they are assessed appropriately when admitted, would be deemed to be at high-risk and therefore would benefit from anticoagulants. To that end, the HSE published guidelines in 2018 recommending that all hospitals take it upon themselves to ensure that all patients admitted to hospital are assessed and treated appropriately.
In addition, this year, the HSE launched a new key performance indicator for all hospitals, whereby they must report their rates of hospital-acquired VTE. “This is a major step forward in our eyes because it re-focuses all of our minds on the issue of hospital-acquired VTE and hopefully will motivate hospitals around the country to address the problem,” said Dr Kevane. “It’s also important to remember that up to half
The risk of blood-clotting associated with Covid-19 manifested early in the outbreak, Dr Kevane pointed out. “Very early on when the pandemic started in Asia, it became apparent that patients with severe disease showed evidence of abnormal blood-clotting activation in their routine laboratory tests,” said Dr Kevane. “Following on from that, there were reports of really high rates of VTE among patients with Covid-19, particularly those with severe Covid-19 admitted to an ICU. At the moment, there is a lot of uncertainty regarding the extent to which Covid-19 may increase the risk of hospital-acquired VTE above that which we would see in other scenarios, such as patients admitted to hospital with influenza.
“We may potentially need to alter the way we treat patients and alter our preventative strategy,” he continued. “There are a number of ongoing clinical trials at the moment looking at potentially escalating the dosing of the anticoagulant medications that are usually used in preventing VTE in hospitalised patients… the risk of VTE does seem to be higher specifically among the Covid-19 population; it does appear that the Covid-19 virus seems to have effects on blood cells and components of the vascular system, particularly the lungs, that potentially increase the risk of clotting above what is usually seen.”
In common with almost all other specialties, Covid-19 has affected haematology services nationwide and Dr Kevane’s clinic is no exception. Regarding his clinic, Dr Kevane said: “What is really important is
that patients who develop acute symptoms of VTE do not feel that they shouldn’t attend the emergency department. An acute VTE is a potentially fatal event and it’s important that while people recognise that while there is a risk of Covid-19 with any type of hospital encounter, it’s also very important that they don’t ignore the acute symptoms of VTE and should always attend an ED in that scenario, regardless of what they hear on the news regarding Covid-19 numbers, because of the potential risk of a fatal outcome.”
Many patients are being very successfully followed virtually in Dr Kevane’s clinic, he told MI. “We go to significant lengths to try and limit the amount of encounters a patient will have with healthcare professionals and hospital visits in order to reduce their risk of contracting Covid, but we always stress to patients that it’s really important that in the event of acute VTE that they attend the ED.” Symptom overlap
As well as patient awareness, Dr Kevane was asked if healthcare professionals also need to be more cognisant of the condition, particularly bearing in mind the potential for symptom overlap with other diseases or conditions. “Thrombosis can be misdiagnosed because symptoms can often mimic other problems,” he explained. “One of the big challenges that we have had in recent months with the Covid-19 pandemic is that because, obviously, Covid-19 presents with respiratory symptoms, but also possibly pulmonary embolism but also often with shortness of breath, chest pain and occasionally coughing-up blood.
“So because these symptoms can overlap, it can be quite difficult to clinically differentiate between diagnoses and because of the high rates of VTE we are seeing in Covid patients, it can be incredibly challenging. The chest-related symptoms of VTE, such as chest pains, shortness of breath and palpitations, can often mimic other disorders and similarly, symptoms of DVT, such as pain, swelling and redness of the skin can also mimic other conditions, such as skin infections. It is always a challenge to differentiate DVT from other conditions, which is why it is really important that if there is a suspicion, that the patient should be assessed as soon as possible and given the appropriate diagnostic investigations.”
In conclusion, Dr Kevane touched on current research he is conducting on the mechanisms underlying coagulopathy in Covid-19. “We started a few months ago in collaboration with some colleagues in the UCD Conway Institute,” he said. “So myself, Prof Fionnuala Ní Áinle and Prof Patricia Maguire work together and we have a research group, which is directed by Prof Maguire and Prof Ní Áinle, called UCD SPHERE. This project is a collaboration between ourselves and other clinicians in the Mater Hospital and also St Vincent’s Hospital, and we also have a group of international collaborators.”
The work has been ongoing for a number of months, explained Dr Kevane, and he and his colleagues are investigating blood coagulation in Covid-19 patients and its interplay with inflammation in the COCOON study.
“We have completed some of the initial work and have submitted some of that for publication – I presented on some of that preliminary data at the recent VT Dublin meeting.”

THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 News Interview 12
Dr Barry Kevane
Until recently, VTE has not been very well recognised as a cause of cardiovascular deaths
Lipocomb


Rosuvastatin / Ezetimibe Lipocomb
GET LOWER
Lipocomb® (rosuvastatin/ezetimibe) Abbreviated Prescribing Information: Please refer to the Summary of Product Characteristics before prescribing.
COMPOSITION*: Lipocomb 10 mg/10 mg, 20 mg/10 mg hard capsules contain 10 mg rosuvastatin zinc (ros)/10 mg ezetimibe (eze), 20 mg ros/10 mg eze.
INDICATIONS*: Treatment of hypercholesterolemia as an adjunct to diet as substitution therapy in adult patients adequately controlled with the individual substances given concurrently at the same dose level as in the fixed dose combination, but as separate products. DOSAGE AND ADMINISTRATION*: One capsule once daily of the given strength with or without food. Lipocomb is not suitable for initial therapy. Treatment initiation or dose adjustment if necessary should only be done with the monocomponents and after setting the appropriate doses the switch to the fixed dose combination of the appropriate strength is possible. Appropriate lipid-lowering diet should continue during treatment. Children and adolescents: not recommended.
Elderly patients: A start dose of 5 mg rosuvastatin is recommended in patients > 70 years. The combination is not suitable for initial therapy. Patients with renal insufficiency: No dose adjustment is necessary in patients with mild to moderate renal impairment. The recommended start dose is rosuvastatin 5 mg in patients with moderate renal impairment (creatinine clearance < 60 ml/ min). The use of rosuvastatin in patients with severe renal impairment is contraindicated for all doses (see section CONTRAINDICATIONS*). Hepatic impairment: No dosage adjustment is required in patients with mild hepatic insufficiency (Child Pugh score 5 to 6). Treatment with Lipocomb is not recommended in patients with moderate (Child Pugh score 7 to 9) or severe (Child Pugh score >9) liver dysfunction. Lipocomb is contraindicated in patients with active liver disease (see section CONTRAINDICATIONS*).
Patients of Asian ancestry or pre-disposing factors to myopathy: recommended starting dose is rosuvastatin 5 mg. The fixed dose combination is not suitable for initial therapy. Monocomponent preparations should be used to start the treatment or to modify the dose. Genetic polymorphisms: for patients that have types of polymorphisms that can lead to increased rosuvastatin exposure, a lower daily dose of Lipocomb is recommended.
Concomitant therapy: risk of myopathy increased when Lipocomb taken with medicinal products that interact with transporter proteins (OATP1B1 and BCRP) and increase rosuvastatin exposure, including ciclosporin, regorafenib, velpatasvir, combination of ritonavir with atazanavir, or combinations of ritonavir with ombitasvir and paritaprevir and dasabuvir, or combination of ritonavir with lopinavir and/or tipranavir, , combination of grazoprevir with elbasvir, combination of glecaprevir with pibrentasvir. Whenever possible, alternative medications should be considered, and, if necessary, consider temporarily discontinuing Lipocomb therapy. In situations where co-administration of these medicinal products with Lipocomb is unavoidable, the benefit and the risk of concurrent treatment and rosuvastatin dosing adjustments should be carefully considered.
CONTRAINDICATIONS*: Hypersensitivity to the active substances or to any of the excipients, active liver disease including unexplained persistent elevations of serum transaminases and any serum transaminase elevation exceeding 3x the upper limit of normal (ULN). During pregnancy and breastfeeding and in women of childbearing potential not using appropriate contraceptive measures (see section PREGNANCY* and BREASTFEEDING*), severe renal impairment (creatinine clearance < 30 ml/min), myopathy, concomitant ciclosporin (see section INTERACTIONS*). WARNINGS*:
Skeletal Muscle Effects: effects on skeletal muscle e.g. myalgia, myopathy, and, rarely, rhabdomyolysis have been reported in rosuvastatin-treated patients with all doses and in particular with doses > 20 mg. Stop treatment if myopathy is suspected based on muscle symptoms or is confirmed by a creatine kinase level. Liver effects: liver function tests should be carried out 3 months following the initiation of rosuvastatin treatment. Stop rosuvastatin or reduce dose if serum transaminase level is greater than 3 times the upper
limit of normal. In secondary hypercholesterolaemia caused by hypothyroidism or nephrotic syndrome, the underlying disease should be treated before starting Lipocomb. Not recommended in patients with moderate or severe hepatic insufficiency. Renal effects: Proteinuria observed with higher doses of rosuvastatin, in particular 40 mg. Creatine Kinase (CK) Measurement: should not be measured following strenuous exercise or plausible alternative cause of CK increase. A confirmatory test should be carried out within 5-7 days if CK levels are significantly elevated at baseline (CK > 5xULN). If repeat tests confirms baseline CK >5xULN, treatment should not be started. Fusidic acid: Lipocomb must not be co-administered with systemic formulations of fusidic acid or within 7 days of stopping fusidic acid treatment. There have been reports of rhabdomyolysis (including some fatalities) in patients receiving fusidic acid and statins in combination. Where the use of systemic fusidic acid is considered essential, statin treatment should be stopped throughout duration of fusidic acid treatment. Statin therapy may be re-introduced seven days after last dose of fusidic acid. In cases of prolonged systemic fusidic acid is needed, the need for coadministration of Lipocomb and fusidic acid should only be considered on a case by case basis and under close medical supervision. Before treatment: Use with caution in patients with pre-disposing factors for myopathy/ rhabdomyolysis, including renal impairment, hypothyroidism, personal or family history of hereditary muscular disorders, previous history of muscular toxicity with another HMG CoA reductase inhibitor or fibrate, alcohol abuse, age > 70 years, situations where an increase in plasma levels may occur, or concomitant use of fibrates. Whilst on treatment: CK levels should be measured in patients with inexplicable muscle pain, weakness or cramps, particularly if associated with malaise or fever. Stop treatment if CK levels are markedly elevated (>5xULN) or if muscular symptoms are severe and cause daily discomfort. Routine monitoring of CK levels in asymptomatic patients not warranted. Rare reports of an immune-mediated necrotising myopathy (IMNM) during or after treatment with statins. Combination with gemfibrozil is not recommended. The combined use of Lipocomb with fibrates or niacin should be carefully weighed against the potential risks of such combinations. Race: increased exposure to rosuvastatin in Asian patients. Protease inhibitors: Increased systemic exposure to rosuvastatin observed in subjects receiving rosuvastatin concomitantly with various protease inhibitors in combination with ritonavir. Concomitant use with certain protease inhibitors not recommended unless the dose of Lipocomb is adjusted. Interstitial lung disease: Stop statin therapy if suspected. Diabetes mellitus: Statins as a class raise blood glucose and in some patients, at high risk of future diabetes, may produce level of hyperglycemia where formal diabetes care is appropriate. Risk outweighed by reduction in vascular risk with statins, and should therefore not be a reason for stopping statin treatment. Patients at risk (fasting glucose 5.6 to 6.9 mmol/L, BMI>30kg/m2, raised triglycerides, hypertension) should be monitored according to national guidelines. Fibrates: safety and efficacy of ezetimibe administered with fibrates have not been established. If cholelithiasis suspected in patient receiving Lipocomb and fenofibrate, gallbladder investigations are indicated and this therapy should be discontinued. Anticoagulants: Monitor international normalised ratio (INR) if Lipocomb is added to warfarin, another coumarin anticoagulant, or fluindione. Paediatric population: Not recommended. Liver disease and alcohol: Use with caution in patients who consume excessive quantities of alcohol and/or have a history of liver disease. INTERACTION(S)*: Contraindicated: Ciclosporin. Not recommended: protease inhibitors (see section DOSAGE AND ADMINISTRATION*), transporter protein inhibitors, gemfibrozil and other lipid-lowering products, fusidic acid. Other interactions: antacid, erythromycin, vitamin K antagonists, oral contraceptives/hormone replacement therapy (HRT), colestyramine, statins. Drug interactions resulting from cytochrome P450-mediated metabolism are not expected.
PREGNANCY AND BREASTFEEDING*: Lipocomb is contraindicated in pregnancy and breast-feeding. Women of childbearing potential should use appropriate contraceptive measures. FERTILITY*: DRIVE AND USE MACHINES*: dizziness may occur during treatment (see section UNDESIRABLE EFFECTS*). UNDESIRABLE EFFECTS*: Common: diabetes mellitus, headache, dizziness, constipation, nausea, abdominal pain, diarrhoea, flatulence, myalgia, asthenia, fatigue, ALT and/or AST increased. Uncommon: decreased appetite, paraesthesia, hot flush, hypertension, cough, dyspepsia, gastrooesophageal reflux disease, nausea, dry mouth, gastritis, pruritus, rash, urticaria, arthralgia, muscle spasms, neck pain, back pain, muscular weakness, pain in extremity, chest pain, pain, asthenia; oedema peripheral, ALT and/or AST increased, blood CPK increased, gammaglutamyltransferase increased, liver function test abnormal. Rare: thrombocytopenia, hypersensitivity reactions including angioedema, pancreatitis, increased hepatic transaminases, myopathy (including myositis), rhabdomyolysis. Very rare: polyneuropathy, memory loss, jaundice, hepatitis, arthralgia, haematuria, gynecomastia. Not known: thrombocytopenia, hypersensitivity (including rash, urticaria, anaphylaxis and angioedema), depression, peripheral neuropathy, sleep disturbances (including insomnia and nightmares), dizziness, paraesthesia, cough, dyspnoea, diarrhoea, pancreatitis, constipation, hepatitis, cholelithiasis, cholecystitis, Stevens-Johnson syndrome, erythema multiforme, immunemediated necrotising myopathy, tendon disorders, sometimes complicated by rupture, arthralgia, myalgia, myopathy/rhabdomyolysis, oedema, asthenia.
OVERDOSE*: PROPERTIES*: Rosuvastatin is a selective and competitive inhibitor of HMG CoA reductase. Ezetimibe is in a new class of lipid-lowering compounds that selectively inhibit the intestinal absorption of cholesterol and related plant sterols. PRESENTATION*: Pack of 30 capsules of Lipocomb 10 mg/10 mg, and 20 mg/10 mg. Marketing Authorisation Holder: EGIS Pharmaceuticals PLC, Kereszturi ut 30-38, H-1106 Budapest, Hungary. PA1470/004/001-002. Legal Classification for Supply: POM. Local Representative in Ireland: Servier Laboratories (Ireland) Ltd, Block 2 West Pier Business Campus, Old Dunleary Road, Dun Laoghaire, Co. Dublin. Tel (01) 6638110, Fax (01) 6638120, www.servier.ie
* For complete information, please refer to the complete Summary of Product Characteristics for Lipocomb® at www.hpra.ie
Date of last revision of text: June 2019 (Date of last approved SmPC: March 2019)
1920 C1 LCB Ad
1. Mach et al. 2019 ESC/EAS Guidelines for the Management of Dyslipidaemias, European Heart Journal (2019) 00, 1-78’ * Patients with: documented CVD, Diabetes Mellitus with organ damages, Severe CKD (chronic kidney disease), a calculated 10 year risk of fatal CVD ≥ 10%, Familial Hypercholesterolaemia with CVD/risk factor. **Patients with: Markedly elevated single risk factors (in particular cholesterol > 8mmol/L or BP ≥ 180/110 mmHg), Familial Hypercholesterolaemia, Diabetes Mellitus, Moderate CKD (chronic kidney disease), a calculated 10 year risk of fatal CVD ≥ 5% and <10%.
GET LOWER
riskLDL-C target
High*<1.4mmol/L
Ezetimibe
ESC TREATMENT TARGETS1 CV
High**<1.8mmol/L Very
Rosuvastatin /
your patient’s LDL-C down even lower to <1.8mmol/L1
Get
Positive developments within the field of cystic fibrosis
At the recent European Cystic Fibrosis Society conference, held online on 24-25 September, Prof Ed McKone, Consultant Respiratory Physician, St Vincent’s University Hospital, Dublin, outlined the evolving natural history of cystic fibrosis (CF) in Ireland, the clinical characteristics of CF at the different life phases and the treatment challenges that arise therein.
There have been large improvements over the last 60 years in CF survival. Many of these improvements were being seen even before the advent of CFTR modulators –the cystic fibrosis transmembrane conductance regulator modulator therapies, which are designed to correct the malfunctioning protein made by the CFTR gene in people with CF. Much of the improvements in survival and life expectancy have been attributed to antipseudomonal antibiotics, improved nutrition, the expertise of the multidisciplinary care teams and our ability to detect CF early and begin treatment.
New research published in the European Journal of Human Genetics has shed light on some of the outcomes over 6.5 years of the inclusion of CF in the Newborn Screening Programme in Ireland. The overall incidence of CF was found to be one-in-2,570 births, with an estimated carrier frequency of one-in-25.3. This is lower than the previously reported one-in-19 carrier frequency in Ireland.
The likely cause of this decrease in incidence in the Republic of Ireland is increased ethnic diversity arising from inward migration. The authors recommended that in the case of counselling for a couple of Irish origin, the carrier rate of one-in-19 should still be used. Ireland continues to have one of the highest incidences of CF in the world.
Transition
Prof McKone noted the decline in physical markers of health experienced by people with CF in adolescence and early adulthood. The transition from paediatric to adult care and greater self-management of their condition is a critical time for people with CF. This period is characterised by a decline in lung function and nutritional status, increases in the detection of pseudomonas and MRSA bacteria, and is associated with increasing rates of depression and anxiety.

In a joint Cystic Fibrosis Ireland (CFI) and Health Research Board-funded study, Vice Dean for Graduate Studies in the College of Medicine and Health in University College Cork (UCC) Prof Eileen Savage (PhD) and colleagues from University College Cork (UCC) used a multivariate analysis to examine the association between socio-demographic variables (age, sex), physical (FEV1, BMI) and mental health variables and health-related quality-of-life (HRQOL) among a sample of adolescents and adults with CF aged >14 in Ireland. The study found that mental health variables, specifically depression and anxiety, were more strongly associated with HRQOL than physical variables. The results indicate that as CF disease progresses and physical health declines, maintaining mental health is essential to ensure people with CF have the highest HRQOL possible.
Dr Jennifer Cronly (PhD), School of Nursing and Midwifery, UCC, and Prof Savage also investigated the role of agency in empowering young people to take control of their own disease management during adolescence. Their research highlighted the threats negative interactions with healthcare professionals may have for this patient group in the development of agency. The authors noted the need for respect and encouragement of young people as they go through the process of transition and to allow adolescents to have an active role in the decision-making process around their own care.
Covid-19
Mental health concerns are not only prevalent during adolescence, but throughout the life course for people with long-term health conditions. The coronavirus pandemic has had an unprecedented impact on those with underlying health conditions including people with CF. In the early
period of the pandemic, people with CF were considered extremely medically vulnerable and were advised to cocoon for their own safety. This caused high levels of stress and concern.
A survey undertaken by CFI in late March 2020 identified high levels of anxiety among people with CF and their carers, and observed major concerns about the unknown health implications of coronavirus and CF, fears of possible medication shortages or supply issues, and the mental health and practical implications of cocooning. In light of new data on the nature of Covid-19 disease and CF, people with CF are now considered high risk from Covid-19 if their CF is stable, and extremely medically vulnerable if their
en by people with CF and their family members and carers to prevent infection.
These enhanced precautions, and the duration for which people with CF have had to endure them, may not come without consequences. Prof Patricia Fitzpatrick, Professor of Epidemiology and Biomedical Statistics in University College Dublin, is currently leading a research project to assess the impact the Covid-19 pandemic and cocooning have had on the daily lives of people with CF. The research will investigate how people with CF and their parents/ carers have managed their daily lives throughout the pandemic; assess their access to hospital visits and routine CF care; examine precautions taken by them; and report on the impact on mental health and the stress management techniques used to cope.
Ivacaftor/tezacaftor/elexacaftor
While Covid-19 has cast a grey uncertainty across the future, for many people with CF the horizon is looking brighter than ever. On 21 August, it was announced that the European Commission had granted marketing authorisation for Kaftrio (ivacaftor/tezacaftor/elexacaftor) in a combination regimen with ivacaftor to treat people with CF aged 12 and over with one F508del mutation and one minimal function mutation, or two F508del mutations in the CFTR gene. Thanks to the innovative ‘Portfolio Agreement’ signed in 2017 between the HSE and Vertex Pharmaceuticals, the treatment regime is expected to be available to eligible patients in Ireland as early as October 2020.
Ms Sally Ann Lynch and Ms Tara Clark, Department of Clinical Genetics, Children’s Health Ireland at Crumlin, suggest that up to 95 per cent of people with CF may be eligible for a modulator therapy in Ireland based on their genotypes. A recent European study using CF registry data (currently unpublished) goes further and found that up to 97.7 per cent of adults with CF in Ireland will be eligible for at least one of the modulator drugs – this would be the highest proportion of eligible adults throughout Europe.
RECOVER
Ivacaftor/tezacaftor/elexacaftor has been shown to be effective in multiple clinical trials, however, the real-world impact of this drug on the lives of people with CF may be even greater. The RECOVER project, led by Prof Paul McNally, Associate Professor of Paediatrics, RCSI, will investigate the real-world effect of the new CF medications on clinical outcomes in people with CF. The project is funded by the Cystic Fibrosis Foundation in the United States of America (€2.85 million), the CF Trust (UK) (£112,000), and Cystic Fibrosis Ireland (€100,000). RECOVER is a multi-centre cohort study which will take place in eight sites across Ireland and the UK over a three-year period.
CF is unstable or they are post-transplant. While data has shown that coronavirus is not as severe in people with CF as originally feared, it is not a benign disease.
Data from the European Cystic Fibrosis Registries up to 18 September identified 138 cases of Covid-19 among people with CF. Where information was known, 20 per cent (n=27) of these infections were asymptomatic and 79 per cent (n=102) were symptomatic. Among symptomatic patients, 60 per cent required hospitalisation, 16 per cent of these were treated in ICU and sadly 25 per cent (n=4) of those in ICU died. The incidence of Covid-19 among people with CF in the EU was 0.2 per cent with a 2.9 per cent case fatality rate. Both of these are lower than the incidence and case fatality rate among the general population in the EU for the same time period (4.5 per cent and 0.5 per cent respectively). This may reflect the enhanced precautions tak-
It will collect information on a range of health data and clinical end-points such as lung clearance index, chest CT, gastrointestinal symptoms and inflammation, and medication adherence. ‘Real-world’ studies examine how drugs impact on a broad range of patients, many of whom would have been excluded from the initial clinical trials due to poor underlying health or the existence of comorbidities. The data can confirm trial findings and shed light on the overall impact of the drug on the day-to-day lives of people with CF and not just on a limited range of biomarkers or a specific cohort.
With more and more people with CF living for longer, clinicians are having to detect and treat current and emerging ageing comorbidities in this group, including those already known to be associated with older age and those possibly resulting from long-term use of new therapies. People with CF are also turning their minds to the need for better educational opportunities, long-term careers and pension planning. A normal life is becoming less of an extraordinary ambition for people with CF.
Cystic Fibrosis Ireland is committed to leaving no one behind in the quest for improved quality-of-life for all people with cystic fibrosis.
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 News Feature 14
Ms Sarah Tecklenborg, Senior Research and Policy Coordinator, Cystic Fibrosis Ireland, provides an overview of the latest Irish cystic fibrosis research, including the impact of Covid-19 on people with the condition
The transition from paediatric to adult care and greater self-management of their condition is a critical time for people with CF
Prof Eileen Savage
READER COMMENTS
REACTION TO DR GABRIELLE COLLERAN’S COLUMN, ‘LET’S NOT RUSH TO JUDGEMENT AND INSTEAD REFLECT ON OUR OWN PRIVELEGE’, 15 OCTOBER
“Excellent article by @ProfSuperJunior on not rushing to judgement and vilifying young people in response to Covid. Also important points on the need for additional permanent capacity in healthcare through beds and staffing to reduce long wait times.”
David Cullinane TD, @davidcullinane, 15 October
“Agree ++ that privilege transcends everything – education too. Stop the schools again and the impact will be harshest on those lower socio-economically.”
Mary Curtin, @Marytcurtin, 15 October
“Well worth a read! Lets understand for many of us in our community it is more manageable to comply with restrictions. Be quick to praise, but be slow to judge. You might not understand the context.” John Moran, @moranjohna1, 15 October
“That’s a great piece Gabrielle. Until you see it written down, it’s easy to overlook how privileged some people are. I’m always extremely aware of how lucky I am to live in a safe place, but never really checked my own privilege when it comes to driving to work etc. Food for thought.” Carol Smurf, @CarolSmurf, 15 October
“Covid-19 is not a socially neutral disease ... we are not ‘all in this together’. Social inequity means there are those who are at a far greater risk of contracting it and indeed dying from it.” BeeNiBee, @BeeNiBee, 15 October
REACTION TO OUR NEWS STORY, ‘HPSC DIRECTOR ROLE FILLED ON INTERIM BASIS PENDING REFORMS’, 15 OCTOBER
“One of the least-discussed pieces of Covid trivia in Ireland is that the director of the HPSC (the person who would do most pandemic planning) has been vacant for years because they can’t attract candidates. They’re asking people to give up consultant jobs in other jurisdictions, to take up a non-consultant role in Ireland.”
Dr Niall Conroy, @NICU_doc_salone, 15 October

“So the permanent HSPC director post hasn’t been filled since ... 2016?”
Annette McGuckin, @McguckinAnnette, 15 October
REACTION TO OUR NEWS FEATURE, ‘WHEN THE RACE FOR A VACCINE IS OVER’, 15 OCTOBER
“We are calling for a rolling percentage […] of #vaccines obtained by bilateral deals to go to low- and middle-income countries. Read more from MSF Dr Manuel Martin’s conversation with @DavidLynWriter in @med_indonews #Covid-19.”
MSF Access Campaign, @MSF_access, 15 October

“Nobody is safe until everyone is safe. Though published before today’s #Budget2021 commitment to the EU advance purchase agreement, this lays out the issues involved #Covid-19 #vaccines.” Susi Geiger, @complexmarkets, 13 October
REACTION TO OUR IHCA AGM PREVIEW ARTICLE BY THE ASSOCIATION’S SECRETARY GENERAL MR MARTIN VARLEY, ‘THE GOVERNMENT NEEDS TO END, AS A MATTER OF URGENCY, THE SALARY DISCRIMATION AGAINST CONSULTANTS APPOINTED SINCE 2012, 5 OCTOBER
“Yes - A two-tier health service and a two-tier salary system must be replaced by a one-tier health service with a one-tier salary system.” Mary O’Brien Sheehan, @OBrienSheehan, 10 October
Editor: Paul Mulholland paul@mindo.ie
News Editor: Catherine Reilly catherine@mindo.ie
Clinical Editor: Priscilla Lynch priscilla@mindo.ie
Journalists: David Lynch, david@mindo.ie , Niamh Cahill, niamh@mindo.ie, Pat Kelly, pat@greenx.ie
Sub-Editor: Emer Keogh emer@greenx.ie
Designer: Laura Kenny laura@greenx.ie
Advertisements: Graham Cooke graham@greenx.ie
Recruitment: Louis O’Hegarty louis@mindo.ie
Digital Marketing: Emma McInerney emma@greenx.ie
Managing Director: Graham Cooke graham@greenx.ie twitter.com/med_indonews facebook.com/MedicalIndependent
If you have anything you would like to share, please email: info@mindo.ie
Beacon Hospital’s ‘Battles of the Sexes; Women & Men’s Health’ GP Educational Webinar is taking place on Saturday, November 28th 2020

Places are free of charge but pre-registration is essential. Register by emailing events@beaconhospital.ie CME Accreditation applied for.
The Medical Independent is published by GreenCross Publishing Ltd., Top Floor, 111 Rathmines Road Lower, Dublin 6, Ireland Tel: 01 441 0024 Web: www.medicalindependent.ie. GreenCross Publishing (est. 2007) is owned by Graham Cooke (graham@greenx.ie). © Copyright GreenCross Publishing Ltd. 2020. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form by any means – electronic, mechanical or photocopy recording or otherwise – whole or in part, in any form whatsoever for advertising or promotional purposes without prior written permission of the publishers. The Medical Independent endeavours to ensure accuracy of information given and of claims made in articles and advertisements. Nevertheless, no responsibility is accepted in respect of such information or claims. Any opinions expressed by contributors are entirely their own and do not purport to be the views of The Medical Independent
For subscriptions, contact: Daiva Maciunaite, daiva@greenx.ie Ireland €200 incl VAT. UK and International €275.00
PAUL MULHOLLAND
Light at the end of the tunnel for consultant agreement?
The IHCA AGM and annual conference 2020 was full of familiar themes: Restoring pay parity for ‘new-entrant’ consultants; the health service’s deficits in staff and capacity; and physician burnout.
But there is little that is familiar in this era of lockdowns and physical distancing.
You had to look no further than the format in which the annual conference was held to realise we are living in a new reality. Like so many organisations, the IHCA has had to adapt to physical distancing guidelines, with the conference taking place virtually. The IHCA, as well as the colleges and medical societies, should be commended for the way they have used technology to allow their meetings to go ahead in the most difficult of circumstances. Rarely has it been so important for doctors to come together to share their expertise and experiences.
Physician burnout was a problem before Covid-19. The pandemic has made the problem even worse, according to Dr Graham Billingham, Chief Medical Officer, MedPRo, Berkshire Hathaway.
Speaking about the pandemic experience in the US, Dr Billingham told the conference the issue of burnout has been “exacerbated now, under the tremendous strain and long hours and clinical exhaustion”.
As has been said before, Covid-19 has highlighted weaknesses in healthcare systems and societies.
In Ireland, our low consultant numbers and chronic capacity deficits, risk being ruthlessly exposed unless the virus’ spread is checked.
A few days after the conference, which took place on Saturday 10 October, the Budget was announced. The Association welcomed the additional €4 billion that will be made available for the health service.
According to the IHCA President Prof Alan Irvine, this extra funding deserves to be “recognised and provides much needed backing at a crucial time”.
“Financial backing for beds at acute, community and intensive care levels is
positive,” Prof Irvine said.
“Moving quickly to use this funding while in tandem providing transparency on bed delivery numbers at hospital level will give confidence to patients and healthcare professionals alike.”
At the conference, Minister for Health Stephen Donnelly committed to ending the pay disparity for new-entrant consultants, who took up posts after 2012. The IHCA welcomed this commitment, but would be aware that Minister Donnelly’s predecessor made similar remarks.
On foot of recommendations from the de Buitléir report, the Government intends to introduce a Sláintecare ‘public-only’ consultant contract. While the pandemic delayed progress, the Programme for Government provides for the introduction of the contract. Recently, the Government approved the drafting of legislation to amend the FEMPI Acts to facilitate its introduction. The proposed amendments will enable serving consultants to switch to the Sláintecare contract, in addition to new consultants being recruited under the contract as recommended by the de Buitléir group.
The Government hopes the contract will be introduced early in 2021 following engagement with the representative bodies. Whether it will secure agreement is not certain given concerns the IHCA, as well as the IMO, have already expressed about the de Buitléir recommendations.
However, the IHCA’s positive response to the Budget announcement indicates, at least, a thawing of relations. The Association specifically commended Minister Donnelly for securing the additional healthcare resources.
Prof Irvine said addressing the health services’ deficit in consultant numbers is a “three-legged stool”: Namely, funding; enabling legislation to reverse the 2012 pay cut; and agreement.
“On all three, we are finally seeing a chink of light,” he said.
Given the darkness brought by the pandemic, chinks of light are in short supply these days and should be appreciated where they are found.
MINDO CARTOON

15 Editorial
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020
Letters to: The Editor, The Medical Independent, Greencross Publishing Ltd, Top Floor, 111 Rathmines Road Lr, Dublin 6 or email paul@mindo.ie
2020 IRISH ANTICOAGULATION FORUM WEBINAR SERIES

Tuesday 17th November 13:00 - 14:00
Topic: Clinical Considerations when anticoagulating NVAF patients with Diabetes Mellitus:
Tailoring anticoagulant treatment to reduce vascular complications in diabetes mellitus patients receiving anticoagulation
Speaker: Prof. Reinhold Kreutz is the Director of the Department of Clinical Pharmacology and Toxicology at Charité – Universitätsmedizin Berlin, Germany, and Professor of Hypertension and Clinical Pharmacology. Prof. Kreutz’s current research interests focus on clinical pharmacology of cardiovascular drugs, clinical and experimental hypertension with a focus on the genetics of hypotensive target organ damage, and drug therapy in the elderly. Prof Kreutz also serves as the president of the European Society of Hypertension and will speak about tailoring anticoagulant treatment for non-valvular atrial fibrillation patients with Diabetes Mellitus, in order to mitigate vascular complications in this at risk patient group.
Chair: Prof. Brendan McAdam, Consultant Cardiologist, Beaumont Hospital, and Associate Professor of Medicine, RCSI School of Medicine

CPD points approved. Certificates of attendance will be issued to attendees
To register for the upcoming webinars please scan the QR code or use the following link: https://www.irishanticoagulationforum.ie/ en/register-for-iaf-webinars.php
If you would like further information please email: travelandeventsireland @bayer.com
Prof. Reinhold Kreutz
Limited
Atrium, Blackthorn Road
Dublin 18, Ireland
This meeting has been organised and sponsored by Bayer Limited. Views and opinions expressed by speakers are not necessarily those of Bayer Limited
Bayer
The
Sandyford,
PP-XAR-IE-0534-1 NVAF, non-valvular atrial fibrillation
Suspicious minds: How to react if a patient has been recording you without your knowledge
Mr Niall Rooney, Legal Counsel in Medisec, provides advice for medical practitioners on the growing issue of patients recording consultations
Smartphones have been described as weapons of mass distraction. Whether you embrace the technology or regard our reliance on smartphones as an addiction, they are everywhere and are, undoubtedly, here to stay. You may even be reading this article on your own smartphone or tablet. Although these devices can perform amazing tasks, how users take advantage of one basic functionality of the smartphone – the ability to record video or audio – is causing increasing concern.
Have your conversations been recorded without your knowledge?
At Medisec, we have been receiving steadily increasing numbers of calls from doctors looking for advice where they suspect or know that their consultations have been recorded. Of course, because of how ubiquitous these devices are and how quick and easy they are to use, it is likely we are only hearing about a small fraction of the consultations that may have been recorded without the doctor ever realising it.
Every patient and every situation is different, but a common scenario we hear about involves the patient secretly using their smartphone to make an audio recording of an in-person consultation with their doctor. The recorded discussions invariably include details about the patient’s symptoms or condition and the advice given by their doctor.

Is it legal for the patient to record a doctor patient consultation?
Where the patient is recording only their own personal and medical information for personal use, this activity falls outside of the scope of General Data Protection Regulation (GDPR). The logic being that the data they are processing by recording the consultation is confidential to the patient but not to the doctor and that they are free to do as they like with their own data. If the doctor was to record the same consultation, GDPR would apply to that recording.
Although the act of a patient recording their own personal data during a consultation may not fall foul of GDPR, there are other rights and laws that may limit what a patient can do with the audio recording. For example, if the recording included the doctor’s own personal information, the doctor’s constitutional right to privacy or rights under European Convention on Human Rights may limit how the patient could use the recording.
If the recording was altered or edited such as to ridicule and damage the reputation of the doctor, publication of the recording could be the basis for a claim for defamation. Equally, repeated recording or persistent use of recordings to bully or abuse online could amount to the offence of harassment.
Can secret recordings be relied on in evidence?
Although there is no general rule on the admissibility of covert recordings, courts and regulators both in Ireland and the UK
have appeared reluctant to exclude evidence solely on the basis that the record may have been obtained in breach of data protection law. As long as the recordings are considered to be ‘relevant and probative’, it would appear they are likely to be admitted into evidence.
There have been several recent examples in Ireland of the courts admitting covert video and audio recordings into evidence, most notably the covert RTÉ Investigates recordings from the Áras Attracta nursing home in 2015 and in the prosecution of a member of the Kinahan gang earlier this year, where covert recordings from a car were admitted to support the conviction for conspiracy to murder. Forensic checks by IT experts will often be required to ensure the recordings have not been altered or edited in any way.
Why would the patient want to record the consultation?
Many within the medical profession believe doctors should embrace the recording of consultations. They point to genuine reasons why a patient may wish to record a consultation – such as where they have difficulty hearing, understanding or retaining information or advice imparted by their doctor during the consultation. Support for this view can be found in various studies carried out in the US and the UK, which suggest that patients immediately forget between 40 and 80 per cent of what they were told during a consultation and that up to 50 per cent of what is remembered is incorrect.
well as supplementing the contemporaneous notes taken by the doctor, having a copy can also eliminate some of the fears that may exist about editing or tampering with the recording or somehow misrepresenting what was said.
A significant number of doctors, if not the majority, do not welcome the idea of audio recording of consultations. Some find the idea of a recording device in the room an unnecessary distraction from delivering good medical care, analogous to the speaker forgetting some or all of their lines when a microphone is put in front of them. Others point to the fact that audio recordings do not fully capture everything from a consultation, such as the look and feel of a symptom (perhaps a bruise or a rash,) or the non-verbal communications that are an important part of the consultation. For others, there is a fear about how a recording may be used or misused.
This latter grouping tends to regard it as a breach of the doctor-patient relationship of trust and confidence for the patient to record a consultation covertly, contending that there are more acceptable ways of addressing any genuine reasons why a patient might be tempted to press the record button.
Can you end the consultation?
Those embracing the recording of consultations also argue that far from being something to fear, a reliable recording of a consultation will in fact protect doctors by providing proof of their professional and ethical conduct. If the patient has made a recording of the consultation, it is advisable to request a copy for the patient’s chart. As
Without any legislation that prohibits a patient from making a recording of their personal medical consultation, the issue becomes what can or should doctors who do not want their consultations recorded do when they find themselves in this position.
As a starting point, before assuming an improper motive, we would always advise doctors who find themselves in this situation to start by having an open and honest conversation with a patient so as to uncover any genuine reasons the patient may have for wanting to record a consultation. It is
worth remembering that the reason could well be a source of embarrassment for the patient. It is also an opportunity for the doctor to explain why they are uncomfortable having the consultation recorded and to explore the alternative options to recording the consultation such as speaking more slowly, using visual aids, having a relative or friend in the room or writing to the patient after the consultation.
If the patient refuses to stop recording the consultation, it is undoubtedly a difficult situation for a doctor to contend with. However, we advise against terminating the consultation there and then. In addition to the continuing duty of care to act in the best interests of the patient, terminating the consultation before assessing the needs and circumstances of the patient would introduce a risk that the patient may come to some harm if they have a serious or urgent condition. From a practical perspective, a refusal to proceed with the consultation is likely to be recorded and may only serve to give the patient cause to complain about the doctor.
If the patient plans to record all future consultations despite the doctor’s objections, it is important to consider whether the patient’s actions demonstrate a breakdown in the relationship of mutual trust and confidence that exists between a doctor and patient. The Medical Council recognises that good care depends on doctors working together with patients with mutual respect. Although the act of recording a consultation may not of itself be enough of a reason to ask the patient to find a new doctor, if the doctor-patient relationship has broken down irretrievably it may be in the patient’s best interests to be seen by another doctor. As every patient and every situation can be different, we suggest that any doctor who finds themselves in this situation contact their indemnifier for advice that is specific to their situation.
17 THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 Medico-Legal Opinion
They point to genuine reasons why a patient may wish to record a consultation – such as where they have difficulty hearing, understanding or retaining information or advice imparted by their doctor during the consultation
The State Epidemiologist who inspires tattoos
Is Sweden’s approach to Covid-19 a cautionary tale, or a realistic response in the absence of a vaccine?
DR MUIRIS HOUSTON

Idoubt that even the most ardent fan of our Chief Medical Officer (CMO), Dr Tony Holohan, has his image tattooed on their arm. But given the chasm between his approach to Covid-19 and that of Swedish State Epidemiologist Anders Tegnell, the absence of a CMO tattoo-wielding Irish citizen is but one example of the difference between Ireland and Sweden when it comes to the coronavirus.
Following a period of leave to be with his terminally ill wife, Dr Holohan returned to his post with a bang in early October. Clearly concerned about rising infection numbers, he called an unexpected meeting of the national public health emergency team (NPHET) on a Sunday, at the end of which the emergency team recommended an immediate move nationally from level 2 to level 5, the most severe response in the State’s established virus response plan.
In the end, the Government chose to move to level 3 rather than level 5 amid mounting public anxiety about NPHET’s severe advice. And there was some overt political reaction to the modus operandi of the emergency team, culminating in an extraordinary attack
by
Tanaiste Leo Varadkar, live on the Today with Claire Byrne show on RTÉ.
Contrast this scenario with that in Sweden. Under the guidance of Tegnell, the country eschewed a broad lockdown approach. It meant that as the rest of Europe saw a summer reduction in Covid-19 cases, Sweden had its highest number of new cases recorded on June 24, 2020, when the number reached 1,698. The numbers subsequently dropped, albeit with an uptick in recent days.
As a result of his singular approach, Tegnell has become one of the best known and most controversial figures of the global coronavirus crisis. His approach to Covid-19 – to keep schools, restaurants, fitness centres, and borders open – has placed Sweden on a unique coronavirus trajectory. A majority of Swedes have largely supported his approach. As a result, there are stories (and photographic evidence) of his bespectacled face tattooed on citizens’ bodies.
But there have also been calls for him to resign after thousands of older people in nursing homes died. Sweden recorded the fifth highest death rate from coronavirus per capita in Europe – about 10 times higher than neighbours Norway and Finland. Globally his stubbornness has been criticised, with The New York Times calling Sweden a “pariah state” and “the world’s cautionary tale”.
In a recent interview with the Financial Times (FT), Tegnell argues against quick fixes and a short-term approach based on some future magic bullet solution. “We see a disease that we’re going to have to handle for a long time into the future and we need to build up systems for doing that,” he says.
He reckons other countries will be more vulnerable to spikes of infection, without the level of immunity he believes now exists in Sweden. But he rejects accusations the country has followed a herd immunity approach.
Tegnell is not a fan of national lockdowns. Instead, his approach has been about having a strategy that can work for years if needs
The art of vaccination persuasion
Many anti-vaxxers are not set in their beliefs and are open to having their minds changed
DR LUCIA GANNON

“Iam the second to last of 13 siblings, five of whom died of vaccine-preventable diseases in infancy. Born to poor immigrant parents, I remember well my mother’s account of the causes of their deaths. Three from pertussis and two from measles. Even after many years had passed, she spoke of the death of her angels with a great deal of emotion. Imagine losing not one, two, three or four, but five babies. It was common in the pre-vaccine era. Like our family, many families lost several children to these diseases. We forget. Time blurs our memory of these common tragedies of yesteryear.”
Excerpt from a letter to the Immunisation Action Coalition from Prof E J (Gene) Grangarosa, Emeritus Professor, Emory University, Atalanta, Georgia 2000.
We sat, muffled in jackets under the large canopy and ordered coffee from the waitress with the black mask. Six women, we occupied two and a half tables, following the social distancing guidelines, our meeting time arranged to beat the mid-morning coffee crowd. We had come together for the first face-to-face meeting of the Killenaule Book Club (KBC) since March and
the early morning September sun shone favourably through the gaps in the overhead covering as if delighted to see such a gathering.
Unsurprisingly, the conversation turned to Covid-19, how it had impacted us and the likelihood of a vaccine coming soon. “What do you think about the flu vaccine?,” one friend asked. “Do you think I should get it this year?” I answered that I got the flu vaccine every year, even before Covid and that I thought everyone should get it.
A tap on my shoulder caused me to turn abruptly, to see a man I did not recognise standing over me, holding his phone out as if he wanted me to look at something.
Surprised by his proximity, I automatically pushed my chair away from him. “I heard you say that everyone should get the flu vaccine,” he said. “You shouldn’t say that. I wouldn’t touch it. Did you know that it has mercury in it?” I noticed that other customers had arrived on the plaza and most of them were looking in our direction. “I’m sorry,” I said, “I am a doctor and I know the constituents of the flu vaccine. I get it every year and have never had any side effects.”
(As it happened, I didn’t know all of the constituents of the vaccine, but that was
beside the point. I knew that the benefits outweighed the risks, and that was good enough for me.) I turned my back on the man and resumed my conversation, feeling as if I had just swatted away a fly. Later, I couldn’t help thinking about the incident and how I might have handled it better. Anti-vaxxers have been around for as long as the vaccines themselves. Despite the overwhelming evidence that vaccination is safe and effective, these people continue to spread misinformation. As a GP, I consider vaccination to be one of the most essential tasks that I perform. I take every opportunity to encourage appropriate antenatal, childhood, adult, and travel vaccination. The relationship of trust that GPs have with their patients means that most GP practices have a very high uptake
be, rather than the constant chopping and changing seen in the rest of Europe. “We don’t see it as viable to have this kind of drastic closing down, opening and closing. You can’t open and close schools. That is going to be a disaster. And you probably can’t open and close restaurants and stuff like that either too many times. Once or twice, yes, but then people will get very tired and businesses will probably suffer more than if you close them down completely,” he says.
He takes a broad view of public health. As a result, children’s sports carried on, as did drinking and eating out with friends, and shopping. Life did not carry on entirely as normal. Universities and schools for children over 16 switched to online learning, gatherings of more than 50 were banned, and people were asked to work from home. Those over-70 were asked to self-isolate.
Tegnell does not see the future availability of a coronavirus vaccine as a silver bullet. “I’m not very fond of easy solutions to complex problems and to believe that once the vaccine is here we can go back and live as we always have done. I think that’s a dangerous message to send because it’s not going to be that easy,” he tells the FT
Sweden’s constitution means the governance of public health is different to that in Ireland and most other countries. Politicians do not make the big decisions – Sweden’s public health agency does. Which probably means fans of the Republic’s CMO are unlikely to sport adulatory tattoos anytime soon.
of vaccinations. And so, immunisation has become the victim of its success. Most people nowadays do not know anyone who has died from influenza, pertussis, or measles. As the diseases disappear, so too does our memory of them.
The absence of these diseases creates fertile soil for anti-vaxxers and the unsuspecting public can fall victim to misinformation. Research has shown that approximately 15 per cent of those who are opposed to vaccination are committed anti-vaxxers. The other 85 per cent are open to persuasion.
In my defensive state, I had decided that the man who approached me was an entrenched anti-vaxxer who was not worth challenging. But I may have been wrong. This man may have believed that he was doing good. He may have accidentally landed in an anti-vaccination bubble while researching vaccines and not been able to get out of it. In retrospect, because immunisation is such a significant health issue, I could have given this man a little of my time. I could have replied that influenza is still a severe disease that causes hundreds of thousands of people to become ill and die every year. There may have been no need to say any more than that to make him reconsider his beliefs.
With knowledge comes responsibility. Doctors are responsible for promoting good health both inside and outside the surgery. No one wants to be bothered with medical issues when meeting friends for coffee, but neither do we want to miss an opportunity to change someone’s mind for the better. It may save a life.
18 Opinion THE MEDICAL INDEPENDENT | 26 OCTOBER 2020
In the end, the Government chose to move to level 3 rather than level 5 amid mounting public anxiety about NPHET’s severe advice
A tap on my shoulder caused me to turn abruptly, to see a man I did not recognise standing over me, holding his phone out as if he wanted me to look at something
Read more by Dr Lucia Gannon at www.mindo.ie
@LuciaGannon
Read more by Dr Muiris Houston at www.mindo.ie @muirishouston
When a DPP-4 inhibitor is needed
Simplicity. Reinforced.
References:
1. TRAJENTA® (linagliptin) Summary of Product Characteristics. Available at: https://www.medicines.ie/medicines/trajenta-5-mg- lm-coated-tablets-34014/
2. McGill JB, et al. Diabetes Care. 2013;36:237–44
3. Rosenstock J, et al. JAMA. 2019;321:69–79
4. Rosenstock J, et al. Cardiovasc Diabetol. 2018;17:39
5. ICGP Guidelines: A Practical Guide to Type 2 Diabetes December 2019. Available at: https://www.icgp.ie/go/library/catalogue/item
Prescribing Information (Ireland) TRAJENTA® (Linagliptin)
Film-coated tablets containing 5 mg linagliptin. Indication: Trajenta is indicated in adults with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control as: monotherapy when metformin is inappropriate due to intolerance, or contraindicated due to renal impairment; combination therapy in combination with other medicinal products for the treatment of diabetes, including insulin, when these do not provide adequate glycaemic control. Dose and Administration: 5 mg once daily. If added to metformin, the dose of metformin should be maintained and linagliptin administered concomitantly. When used in combination with a sulphonylurea or with insulin, a lower dose of the sulphonylurea or insulin, may be considered to reduce the risk of hypoglycaemia. Renal impairment: no dose adjustment required. Hepatic impairment: pharmacokinetic studies suggest that no dose adjustment is required for patients with hepatic impairment but clinical experience in such patients is lacking. Elderly: no dose adjustment is necessary based on age. Paediatric population: the safety and efficacy of linagliptin in children and adolescents has not yet been established. No data are available. Take the tablets with or without a meal at any time of the day. If a dose is missed, it should be taken as soon as possible but a double dose should not be taken on the same day. Contraindications: Hypersensitivity to the active substance or to any of the excipients. Warnings and Precautions: Linagliptin should not be used in patients with type 1 diabetes or for the treatment of diabetic ketoacidosis. Caution is advised when linagliptin is used in combination with a sulphonylurea and/or insulin; a dose reduction of the sulphonylurea or insulin may be considered. Acute pancreatitis has been observed in patients taking linagliptin. Patients should be informed of the characteristic symptoms
of acute pancreatitis. If pancreatitis is suspected, Trajenta should be discontinued; if acute pancreatitis is confirmed, Trajenta should not be restarted. Caution should be exercised in patients with a history of pancreatitis. Bullous pemphigoid has been observed in patients taking Linagliptin. If bullous pemphigoid is suspected, Trajenta should be discontinued. Interactions: Linagliptin is a weak competitive and a weak to moderate mechanism-based inhibitor of CYP isozyme CYP3A4, but does not inhibit other CYP isozymes. It is not an inducer of CYP isozymes. Linagliptin is a P-glycoprotein substrate and inhibits P-glycoprotein mediated transport of digoxin with low potency. Based on these results and in vivo interaction studies, linagliptin is considered unlikely to cause interactions with other P-glycoprotein substrates. The risk for clinically meaningful interactions by other medicinal products on linagliptin is low and in clinical studies linagliptin had no clinically relevant effect on the pharmacokinetics of metformin, glibenclamide, simvastatin, warfarin, digoxin or oral contraceptives (please refer to Summary of Product Characteristics for information on clinical data). Fertility, pregnancy and lactation: Avoid use during pregnancy. A risk to the breast-fed child cannot be excluded. A decision must be made whether to discontinue breast-feeding or to discontinue/abstain from linagliptin therapy taking into account the benefit of breast-feeding for the child and the benefit of therapy for the woman. No studies on the effect on human fertility have been conducted for linagliptin. Undesirable effects: Adverse reactions reported in patients who received linagliptin 5 mg daily as monotherapy or as add-on therapies in clinical trials and from post-marketing experience. Frequencies are defined as very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥ 1/1,000
to < 1/100), rare (≥ 1/10,000 to < 1/1,000) or very rare (<1/10,000).
Adverse reactions with linagliptin 5 mg daily as monotherapy: Common: lipase increased. Uncommon: nasopharyngitis; hypersensitivity; cough; rash; amylase increased. Rare: pancreatitis; angioedema; urticaria; bullous pemphigoid. Adverse reaction with linagliptin in combination with metformin plus sulphonylurea: Very common: hypoglycaemia. Adverse reaction with linagliptin in combination with insulin: Uncommon: constipation. Prescribers should consult the Summary of Product Characteristics for further information on side effects. Pack sizes: 28 tablets. Legal category: POM. MA number: EU/1/11/707/003.
Marketing Authorisation Holder: Boehringer Ingelheim International GmbH, D-55216 Ingelheim am Rhein, Germany. Prescribers should consult the Summary of Product Characteristics for full prescribing information. Additional information is available on request from Boehringer Ingelheim Ireland Ltd, The Crescent Building, Northwood, Santry, Dublin 9. Prepared in December 2019.
Adverse events should be reported.
Reporting forms and information can be found at https://www.hpra.ie/homepage/about-us/ report-an-issue. Adverse events should also be reported to Boehringer-Ingelheim Drug Safety on 01 2913960, Fax: +44 1344 742661, or by e-mail: PV_local_UK_Ireland@boehringer-ingelheim.com
PC-IE-100689 V1 Date of preparation: January 2020 This advertisement is intended for health care professionals practicing in Ireland only HbA1c Demonstrated CV AND KIDNEY SAFETY PROFILE 3,4 PROVEN EFFICACY for adults with T2D 1,2
CONVENIENCE through always one dose, once daily
UNIQUE
1*
other
diabetes should be undertaken as per ICGP guidelines as appropriate.
for a BROAD RANGE of adults with T2D 5mg once daily * Renal and
monitoring in patients with type 2
5
HUG4032 Trajenta MI [IRE] 273x395 v3 AW.indd 1 20/01/2020 16:34
MULTIPLE CHOICE QUESTIONS
Question 1
Chronic obstructive pulmonary disease

A. Presenting features include shortness of breath at rest.
B. In under 35-year-olds, may be caused by an alpha-1 antitrypsin deficiency.

C. Is defined as severe if FEV1 is 30-49 per cent of predicted.
D. Advise parting with pets, especially cats or dogs.
E. First-line management is an inhaled corticosteroid.
Question 2
Out-toe gait
A. Is caused by femoral anteversion.
B. Child stands with legs markedly externally rotated at the hip.
C. Presentation should lead to careful examination of the hips.
D. In more than half of cases is associated with flat feet.

E. Normally corrects spontaneously, once walking is established.
Question 3
Branchial cysts
A. Peak incidence is in young adults.
B. In the majority of cases, presents as a smooth swelling at the anterior border of the sternomastoid muscle.
C. May become infected.
D. Will move on swallowing.
E. Treatment is by excision.
Question 4
Exceptions to the general rule of confidentiality allow a GP to share confidential information about a patient without his or her specific consent, if asked to do so
A. By the patient’s legal adviser.
B. By the police.
C. By solicitors representing the patient’s spouse.
D. When acting as a witness in court.
E. By healthcare workers also responsible for the patient’s clinical management.

Question 5
E. FALSE. Tension headache can last for days and will often get worse during the day.
D. TRUE. Tension headache tends to be bilateral.
C. TRUE. Or photophobia.
B. TRUE. With tension, patient usually able to function normally.
A. FALSE. Suggests tension, migraine headache is pulsating.
ANSWER 5
Clinical features of headache that would support a diagnosis of migraine rather than of tension headache include
A. Pressure or band-like pain.
B. Aggravated by routine activities.
C. Associated with phonophobia.
D. Unilateral.
E. Gets worse during the day.
E. TRUE. Recipients must appreciate rule of professional secrecy.
D. TRUE. Doctor, unlike lawyer, has no privilege in court.
C. FALSE. Must be declined without written consent or court order.
B. FALSE. No more right to confidential information than anyone else, except where there is a statutory duty on the doctor to provide it.
A. TRUE. Presumed to be acting on instructions of his client.
ANSWER 4
E. TRUE. Delay if acutely inflamed, as risk of creating a branchial fistula.
D. FALSE. Also feels fluctuant and does not transilluminate.
C. TRUE. May present with intermittent swelling associated with pain and infection.
B. TRUE. Over 80 per cent here, in the upper third of the neck.
A. TRUE. Though often present in childhood.
ANSWER 3
E. TRUE. Resolves once walking well.
D. FALSE. May look as if have flat feet, but is more apparent than real.
C. TRUE. To exclude congenital dislocation, which also causes external rotation of the leg.
B. TRUE. On examination may be 90 degrees external rotation and no internal rotation at the hip.
A. FALSE. Femoral retroversion. Common in first two years of life.
ANSWER 2
E. FALSE. Bronchodilators.
D. FALSE. May be indicated in asthma.
C. TRUE. <30 per cent is very severe.
In over-35s, is prolonged history of smoking or occupational exposure to dust as underlying causes.
Shortness of breath on exercise; chronic cough; sputum production; and a history of frequent episodes of bronchitis. B.
20 MCQs THE MEDICAL INDEPENDENT | 26 OCTOBER 2020
1 A. FALSE.
TRUE.
ANSWER
Pneumococcal disease is a very serious disease
Those with the following conditions should be vaccinated with PPV231 Everybody aged 65 years and over Also those aged over 2 years with;
· Diabetes mellitus
· Chronic heart, respiratory or liver disease


· Chronic renal disease, nephrotic syndrome,renal transplant
· Sickle cell disease
· Those with missing or non functioning spleens
· Disorders of the immune system including cancer
· People receiving chemotherapy or other treatments that suppress the immune system
· Persons with HIV infection or AIDS
* Asplenia or splenic dysfunction (splenectomy, sickle cell disease, coeliac syndrome); chronic renal, heart, lung, liver disease, diabetes mellitus, complement deficiency, immunosuppressive conditions; CSF leak, cochlear implant recipients or candidates for implants; children < 5 years with history of invasive disease.
‡ If vaccination has been given during chemotherapy or radiotherapy revaccination 3 months after treatment is indicated.
** Those with no spleen, with splenic dysfunction, immunosuppression including HIV infection, nephrotic syndrome, renal transplant or chronic renal disease.
Algorithm provided by National Immunisation Office1 Now
to you by
(pneumococcal vaccine, polyvalent, MSD)
Supported
PNEUMOVAX® 23 solution for injection in pre-filled syringe. Pneumococcal Polysaccharide Vaccine.
ABRIDGED PRODUCT INFORMATION Refer to Summary of Product Characteristics before prescribing. PRESENTATION PNEUMOVAX 23 is supplied as a single Pre-filled syringe (0.5 mL) with 2 needles. Each dose contains 25 micrograms of each of 23 different polysaccharides of Streptococcus pneumoniae. INDICATIONS For active immunisation against pneumococcal disease in children aged from 2 years, adolescents and adults. Refer to SPC section 5.1 for information on protection against specific pneumococcal serotypes.
DOSAGE AND ADMINISTRATION The immunisation schedules for PNEUMOVAX 23 should be based on official recommendations.
Primary vaccination: Adults and children 2 years of age or older - one single dose of 0.5 millilitre by intramuscular or subcutaneous injection. Not recommended for use in children below 2 years of age. Special dosing: It is recommended that pneumococcal vaccine is given at least two weeks before elective splenectomy or the initiation of chemotherapy or other immunosuppressive treatment. Vaccination during chemotherapy or radiation therapy should be avoided and the vaccine should not be administered any sooner than three months after completion of such therapy. Persons with asymptomatic or symptomatic HIV infection should be vaccinated as soon as possible after diagnosis is confirmed. Revaccination: Healthy adults and children should not be revaccinated routinely. Revaccination at intervals of less than three years is not recommended because of an increased risk of adverse reactions. Revaccination may be considered for adults at increased risk of serious pneumococcal infection who were given pneumococcal vaccine more than five years earlier or for those known to have rapid decline in pneumococcal antibody levels. Revaccination after 3 years may be considered for selected populations (e.g. asplenics) who are known to be at high risk of fatal pneumococcal infections and for children from 2 to 10 years old at high risk of pneumococcal infection. CONTRAINDICATIONS Hypersensitivity to the active substance(s) or to any of the excipients. PRECAUTIONS AND WARNINGS As with any vaccine, adequate treatment provisions including epinephrine (adrenaline) should be available for immediate use should an acute anaphylactic reaction occur. Vaccination should be delayed in the presence of significant febrile illness, other active infection or when a systemic reaction would pose a significant risk, except where delay involves greater risk. The vaccine should never be injected intravascularly; precautions should be taken to make sure the needle does not enter a blood vessel. The vaccine should not be injected intradermally as injection by that route is associated with increased local reactions. If the vaccine is administered to patients who are immunosuppressed due to either an underlying condition or medical treatment (e.g. immunosuppressive therapy), the expected serum antibody response may not be obtained after a first or second dose, so such patients may not be as well protected against pneumococcal disease as immunocompetent individuals. Required prophylactic pneumococcal antibiotic therapy should not be stopped after vaccination. Patients at especially increased risk of serious pneumococcal infection (e.g., asplenics and those who have received immunosuppressive therapy), should be advised regarding the possible need for early antimicrobial treatment in the event of severe, sudden febrile illness. The vaccine may not be effective in preventing infection resulting from basilar skull fracture or from external communication with cerebrospinal fluid. As with any vaccine, vacci-
Pneumococcal disease is a very serious disease www.pneumo.ie
nation with PNEUMOVAX 23 may not result in complete protection in all recipients. INTERACTIONS Pneumococcal vaccine can be administered simultaneously with influenza vaccine as long as different needles and injection sites are used. The concomitant use of PNEUMOVAX 23 and ZOSTAVAX resulted in reduced immunogenicity of ZOSTAVAX in a small clinical trial. However, data collected in a large observational study did not indicate increased risk for developing herpes zoster after concomitant administration of the two vaccines. PREGNANCY AND LACTATION The vaccine should not be used during pregnancy unless clearly necessary (the potential benefit must justify any potential risk to the fetus). It is unknown whether this vaccine is excreted in human milk. Caution should be exercised when it is administered to a nursing mother. The vaccine has not been evaluated in fertility studies. SIDE EFFECTS Very common side effects: Fever and injection site reactions such as pain, soreness, erythema, warmth, swelling and induration. Other reported side effects that may potentially be serious include thrombocytopenia in patients with stabilised idiopathic thrombocytopenic purpura, haemolytic anaemia in patients who have had other haematologic disorders, leukocytosis, anaphylactoid reactions, serum sickness, angioneurotic oedema, Guillain-Barré Syndrome, radiculoneuropathy, febrile convulsions and injection site cellulitis. For a complete list of undesirable effects please refer to the Summary of Product Characteristics. PACKAGE QUANTITIES Single pack containing one 0.5 mL dose pre-filled syringe with two separate needles. Legal category: POM. Marketing authorisation number: PA 1286/055/002. Marketing Authorisation holder: Merck Sharp & Dohme Ireland (Human Health) Limited, Red Oak North, South County Business Park, Leopardstown, Dublin 18, Ireland. Date of revision: November 2019. © Merck Sharp & Dohme Ireland (Human Health) Limited 2019. All rights reserved. Further information is available on request from: MSD, Red Oak North, South County Business Park, Leopardstown, Dublin 18 D18 X5K7 or from www.medicines.ie. Date of preparation: July 2020. WS064
Adverse events should be reported. Reporting forms and information can be found at www.hpra.ie Adverse events should also be reported to MSD (Tel: 01-299 8700)
Reference 1. http://www.hse.ie/eng/health/immunisation/pubinfo/adult/pneumo/ by
^ Revaccination not indicated for any person who has received a dose of PPV23 at age ≥65 years.
· Those who have received or are about to receive cochlear transplants Brought
in pre filled syringe presentation IE-PNX-00025 Red Oak North, South County Business Park, Leopardstown, Dublin 18, D18X5K7 Ireland www.pneumo.ie 4520_Pneumococcal_Algorithm_A4_Ad_July2020_v.indd 1 20/08/2020 19:32
#

Chronic pain and analgesia
An overview of taking a holistic approach to pain control, as well as pain’s impact on the patient, including its causes and treatment options
In general terms, most people associate pain with some direct cause. It could be from a sports injury, or toothache, perhaps an accident that has resulted in a broken limb. In cases like these, you have an attributable acute pain, which you can then do something about. If it is a toothache, you go to the dentist, the problem gets fixed, and the pain is gone. If it is a broken arm, you go to hospital, have the usual procedures — x-rays, plaster, etc, are carried out and with the right convalescence, the patient returns to normal.
For many though, pain is something which is not acute or for which there is a simple ‘cause and effect’ route to fix the problem. Pain is a constant factor in their lives, something which they manage every day. The reason they have pain may be attributable to one or more different causes; however, it is evident that their pain can have a wholly debilitating effect, not just on their quality-of-life, but also for those around them. This is chronic pain.
The 2006 National Disability Survey Ireland (CSO, 2008) stated that pain was one of the most common disability types reported. Almost 50 per cent of individuals reported pain as the main cause of their disability and of those, 34 per cent indicated arthritis as being the most common cause of injury or illness.
• 15 per cent of sufferers reported losing a job due to their chronic pain.
• 19 per cent were diagnosed with depression due to chronic pain.
What is chronic pain?
Chronic pain can be defined as pain which has lasted longer than what would be considered as a ‘normal’ healing time, perhaps as part of recovery from illness or injury – generally more than three months.
Chronic pain may be attributable to an event, such as an accident, developing from acute pain. Opinion differs as to whether previous acute pain is always the root cause of chronic pain or simply appears, sometimes without an initial cause.
In some cases, especially in relation to sports injury in contact sports, the underlying chronic pain may appear some time after an event.
Pain may also be related to another condition. Surveys show that in Ireland, 35 per cent of reported chronic pain was arthritis-related. It may be site-specific, ie, back, knee, and wrist, however, 80 per cent of sufferers in Ireland report that their pain relates to more than one site.
Types of chronic pain
Almost 20 per cent stated the pain disability was caused by an accident or injury.
The Pain in Europe survey, published in 2006 by Harald Breivik, indicated for Ireland that:
• 13 per cent of the Irish population and 27 per cent of Irish households were affected by chronic pain.
• 21 per cent of people with chronic pain reported pain so severe they sometimes wish to die.
• The average age of individuals with chronic pain was 48, with only a slightly higher gender bias towards women (W 52 per cent – M 48 per cent).
• The average duration of chronic pain was 4.9 years, although almost 20 per cent of individuals with chronic pain had experienced it for >20 years.
• Almost 70 per cent of individuals with chronic pain reported pain on a daily basis.
• 34 per cent felt pain impacted on their employment.
Pain can be classified either by type of pain, or by body region. Classes of pain types include:
• Nociceptive pain: Aching, boring, worse on movement, anatomically defined, fluctuates in severity.
• Neuropathic pain: Burning sensation, sharp stabbing type, tingling, transient limb pain (shooting), associated with allodynia (experience of pain from a non-painful stimulation of the skin, such as light touch), hypersensitivity, or other sensory changes.
• Mixed nociceptive and neuropathic pain: Combination of symptoms.
• Visceral pain: Dull, non-specific, difficult to pinpoint.
• Autonomic symptoms: Physiological changes (colour, temperature), sweating.
Causes of chronic pain
The cause of chronic pain is often difficult to determine and there are often many aspects
to consider. It is this indeterminate nature that can present the biggest obstacle to health professionals to establishing proper diagnosis of the condition.
Chronic pain can be attributed to a wide range of identifiable causes – acute injury, arthritis, migraine, or fibromyalgia, for example.
A general classification is detailed below.
Other causes
Chronic pain may arise from anatomical site-related general medical conditions. Site-specific pain includes:
• Abdominal (ie, peptic ulcer, irritable bowel syndrome, pancreatitis, hernias, diverticular disease).
• Gynaecological (ie, endometriosis).
Musculoskeletal
Osteoarthritis
Rheumatoid arthritis
Osteomyelitis
Osteoporosis
Ankylosing spondylitis
Myofascial diseases
Polymyalgia
rheumatica
Polymyositis
Fractures
Chronic or repetitive overuse
Carpel tunnel syndrome
Muscular strains
Faulty posture
Mechanical low-back pain

• Obstetric (ie, symphysis pubis dysfunction).
• Urological (ie, interstitial cystitis).
• Cardiovascular (ie, ischaemic heart disease, coronary heart disease, angina, peripheral vascular disease, etc).
• Chronic pain may also result from disease conditions including:
• Rheumatological – conditions such as rheumatoid arthritis, osteoarthritis or fibromyalgia.
• Endocrine – conditions such as hypothyroidism (joint pain), diabetes.
• Infectious – diseases such as hepatitis C, postherpetic neuralgia.
• Malignancy – cancer pain and pain from treatment (ie, radiation, chemotherapy or surgery) [Source: Warrell et al (2004); BMJ Best Practice (2009)]
Treatment
Before moving on to treatment, it is worth noting that, according to figures from the Pain in Europe study (Breivik et al, 2006), 40 per cent of respondents, when asked to describe their care, said it was “inadequate”. Leading on from that, there is substantial evidence based on World Health Organisation (WHO) figures that chronic pain is massively undertreated across the globe. This is due to a variety of factors, such as access to medicines and specialist help.
Another contributing factor comes from sufferers themselves. Individuals with chronic pain often do not seek help for their pain. This occurs for a variety of reasons, including religion, fear, finance, culture and a feeling that healthcare professionals may feel the individual’s pain is ‘imaginary’. Indeed, the fear of stigma and disbelief, especially with females, is the most common reason in Ireland for not seeking help with chronic pain.
Cluster headaches
Migraine
Trigeminal neuralgia
Giant cell (temporal) arteritis
Glaucoma
Smoking
Alcohol
Temporo-mandibular joint dysfunction
Drug or substance overuse or misuse
Diabetic sensorimotor polyneuropathy (up to 25 per cent of diabetics)
Spinal stenosis
Brachial plexus traction injury
Thoracic outlet syndrome
Postherpetic neuralgia
Multiple sclerosis
Alcoholism
Thyroid disease
Pernicious anaemia
Infections (ie, HIV), polyneuropathies
Polyradiculopathies
Depression
Anxiety
Personality disorders
Sleep disturbances
23 THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 Pain Clinical
EAMONN BRADY, MPSI, Owner of Whelehans Pharmacies in Mullingar
For many though, pain is something which is not acute or for which there is a simple ‘cause and effect’ route to fix the problem
Headache and/or migraine Neurological Psychological causes
Table 1: General pain classification
Chronic low back pain and interventions for chronic pain
Chronic low back pain (LBP) is one of the most common presenting complaints seen in general practice. The lifetime prevalence is greater than 80 per cent with a point prevalence of approximately 23 per cent, with approximately 12 per cent of these being severely disabled by LBP. Despite these facts, little is understood about the pathogenesis of chronic pain. This results in a plethora of pain treatments without a large evidence base. Ageing, sedentary lifestyles, increasing body mass index (BMI), smoking, a high co-prevalence of psychosocial dysfunction, and low socioeconomic status are important contributors to the prevalence of LBP. The socioeconomic impact of chronic pain is significant with many patients unable to work or return to work after LBP becomes chronic. A significant portion of the country’s GDP is spent on patients with chronic pain; or an estimated 2.86 per cent of GDP per year.
The internationally accepted definition of pain has changed recently. The International Association for the Study of Pain (IASP) has adopted the following definition for pain: “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”
Updated notes accompanying the new definition are as follows:
1. Pain is always a personal experience that is influenced to varying degrees by biological, psychological, and social factors.
2. Pain and nociception are different phenomena. Pain cannot be inferred solely from activity in sensory neurons.
3. Through their life experiences, individuals learn the concept of pain.
4. A person’s report of an experience as pain should be respected.
5. Although pain usually serves an adaptive role, it may have adverse effects on function and social and psychological wellbeing.
6. Verbal description is only one of several behaviours to express pain; inability to communicate does not negate the possibility that a human or a non-human animal experiences pain.
Risk factors
Risk factors for development of LBP can be divided into:
• Patient factors – physical exercise, stress, lifting weights, sitting for long periods, sedentary lifestyle.
• Lifestyle factors – BMI, smoking, alcohol consumption, habitual physical activity, poor sleep quality.
• Psychological factors – depression and post-traumatic stress disorder (PTSD).
Pathogenesis of chronic pain
The pathogenesis of chronic pain has become better understood over the last 25 years. However, the mechanisms involved which contribute to the chronicity of pain are still unknown.
In recent times, the relation between pain and the immune system has been established, pain being one of the four cardinal signs of inflammation. Depression, lethargy, anxiety, sleep disturbance, and hyperalgesia occur commonly in patients with both chronic pain and sickness behaviour.
The neuroimmune interface includes T-cells, macrophages, and glial cells (astrocytes and microglia), which all play a role in modulation of neurotransmission.
The nervous system and immune system
share a common language of neuropeptides that allows for bidirectional communication. This can become maladaptive, enhancing inflammatory pain signalling; this may lead to pain becoming chronic. Preclinical evidence, mostly using rodent models of peripheral nerve injury, provides compelling evidence to support the concept that pain chronicity is a centrally mediated neuroimmune phenomenon.
Experimental models demonstrate how cytokines, chemokines, and neurotrophins interact with neuronal activity resulting in pain behaviour and that a peripheral injury results in major changes not only at the site of injury, but also at the dorsal root ganglion (DRG) and dorsal horn. Preclinical models of neuropathic pain are associated with immune cell infiltration into the DRG and dorsal horn with altered neural signalling to higher centres. Peripheral nerve damage leads to increased afferent expression of the neurotransmitters.
Treatment options
Management options for chronic pain are divided into non-pharmacological, pharmacological and interventional.
Non-pharmacological
The multidisciplinary approach should be used in the management of most types of chronic pain. Evaluation and treatment by a range of healthcare professionals may be sufficient for
Selective serotonin reuptake inhibitors (SSRIs) such as duloxetine are also prescribed for chronic pain. However, a lack of a statistically significant effects of SSRI therapy was noted in recent meta-analysis. A high degree of heterogeneity amongst study methods and primary objectives was noted as a contributing factor.
Anti-epileptic drugs have shown a modest reduction in pain intensity in patients with diabetic neuropathy, fibromyalgia and postherpetic neuralgia. However, the abuse potential of these drugs has become an issue in recent years. A risk-benefit analysis must be performed when commencing and continuing these drugs.
Opioids have a minimal to no role to play in the management of chronic pain. The potential for adverse and even fatal outcomes when prescribed for chronic pain has made them an unsuitable therapy for long-term treatment.
Capsaicin and lignocaine therapy have shown modest benefit in specific pain conditions such as postherpetic neuralgia, painful polyneuropathies including diabetic and HIV-related neuropathy, and postmastectomy/surgical neuropathic syndromes. Capsaicin 8 per cent patches have shown benefit in cases of postherpetic neuralgia cases whilst topical capsaicin cream may be of limited benefit in the conditions listed above.
Lignocaine therapy can be given intravenously or topically. Intravenous administration must be in a monitored environment only. Topical
flammation and acute pain post-procedure. Most conventional RF lesions are applied at probe temperatures of between 60-90 degrees for 90 to 120 seconds in clinical procedures. RF thermal lesions produce irreversible protein denaturation when the tissue temperature rises above 60 degrees. Destruction of myelinated fibres, coagulative necrosis, haemorrhages, and massive oedema can be found in the RF lesion. Even though sensory and motor tests are performed before the ablation, undesirable motor deficit instead of sensory loss may remain for a certain period of time.
Pulsed radiofrequency of dorsal root ganglion (PRF DRG)
In patients presenting with radicular pain, PRF to the DRG at the relevant level may be performed. Pulsed RF is performed at less than 42 degrees. Use of this temperature or lower avoids possible heat complications, such as neuritis, motor dysfunction, and deafferentation pain (or anaesthesia dolorosa). Similarly to RFA, it uses a 500kHz current, applying two bursts/second with each pulse lasting 20 minutes over a 120 second interval. It creates an electromagnetic field at the front of the cannula, using a radiofrequency current in short, high–voltage bursts. After pulsed RF, the internal ultrastructural components of the axons show microscopic damage, including abnormal mitochondrial membranes and morphologic changes of the mitochondria, and disruption/disorganisation of the microfilaments and microtubules. However, the temperature used is not sufficient to cause coagulative necrosis and as such, is not neurodestructive.
Nerve regeneration after nerve ablation in patients with chronic pain usually corresponds with recurrence of pain in a clinical pain practice setting.
Nerve regeneration is initiated through three mechanisms within 30 minutes of an injury:
(1) Remyelination;
(2) Collateral sprouting from preserved axons;
(3) Regeneration.
patients with mild to moderate types of pain. Additionally, certain patients may respond more favourably to a holistic approach by the members of the multidisciplinary team conferring with each other and the patient.
Pharmacological
Multiple medications are currently prescribed for the management of chronic pain.
Simple analgesics such as paracetamol may be prescribed but are unlikely to have a benefit in these patients with the concurrent risk of liver toxicity.
NSAIDs may be appropriate at the lowest effective dose for the shortest time possible. The inherent renal, cardiac and gastrointestinal side-effects have been reduced with use of COX2 inhibitors, but a reduced risk still remains. NSAIDs have no effect on neuropathic pain.
Tricyclic antidepressants (TCAs) such as amitriptyline and nortriptyline have the strongest evidence for use in chronic pain, in particular neuropathic pain, with a number needed to treat (NNT) of three-to-four (and number needed to harm of 14). Interestingly, work done by our research group has showed that use of TCAs modulate the phenotype and function of T-cells in the cerebrospinal fluid of patients with chronic neuropathic pain in this case. This suggests a possible immunomodulatory effect of TCAs with a direct biological effect on immune cells in vivo.
lignocaine plasters have a limited amount of data also for their use in postherpetic neuralgia. Small cross-over studies suggest an improvement in pain between 30-50 per cent but a large randomised controlled trial is lacking.
Interventions for pain
The following procedures are performed in an operating theatre using fluoroscopyguided imaging.
Conventional radiofrequency ablation/rhizotomy
Radiofrequency ablation (RFA) uses a constant high frequency (500kHz) current, which creates a thermal neurodestructive lesion at the active tip of an insulated cannula. RFA is currently applied to the medial branch of the posterior ramus for the treatment of spinal facet joint pain (axial pain). The RF generator produces an alternating current to induce coagulative necrosis at the target tissue. The electrical field generated causes charged molecules to oscillate and generate heat in the surrounding tissues, varying between 60-90 degrees.
A shortcoming of RFA is lesioning occurs on one side of the targeted nerve only. Ideally, more than one lesioning per session may be performed allowing the lesioning to reach the whole nerve, from the epineurium to myelinated or unmyelinated nerve fibres. However, the caveat is the increased likelihood of acute in-
Collateral sprouting may contribute to reinnervation in partial nerve injuries, especially when less than 20-30 per cent of all the axons are affected. When more than 90 per cent of the axons are injured, the primary nerve repair mechanism is regenerated from the injury site. The success of regeneration from the proximal stump depends on its distance from the injury site.
Spinal cord stimulation (SCS)
Insertion of a spinal cord stimulator is a treatment option for patients with either post laminectomy syndrome (persistent pain after at least one spinal surgery) or complex regional pain syndrome. It consists of placing a series of electrical contacts into the epidural space overlying the dorsal columns at a vertebral level that, when activated, achieve as near as possible 100 per cent topographical coverage of the pain area of the body. This may consist of either pain being ‘replaced’ by paraesthesia in the affected area or newer systems are available that are paraesthesia-free.
The neuroimmune mechanism of SCS appears to be associated with lower levels of proinflammatory vascular epidermal growth factor (VEGF) in cerebrospinal fluid (CSF) after stimulation is commenced. Patients with paraesthesia-free stimulators placed had higher levels of anti-inflammatory interleukin-10 in CSF with associated improvement in pain scores, sleep and symptoms of depression.
25 THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 Pain Clinical
DR DEBORAH GALVIN Consultant in Pain Medicine, St James’s Hospital, Dublin
Opioids have a minimal to no role to play in the management of chronic pain. ...outcomes when prescribed for chronic pain has made them an unsuitable therapy for long-term treatment
Majority of migraine sufferers experiencing more frequent and severe migraines during pandemic – survey
Migraine sufferers are experiencing more frequent and severe migraines since the start of the pandemic, a new survey in Ireland has found. The survey, carried out by the Migraine Association of Ireland (MAI) and Novartis Ireland, shines a light on the impact that pandemic restrictions are having on migraine sufferers in Ireland. Conducted to coincide with Migraine Awareness Week (September 6-12), the survey was carried out online among 120 adults living with migraine in Ireland. It shows that 58 per
cent of respondents were suffering more frequent migraines, with 69 per cent of this group reporting their symptoms of migraine have become more severe since the pandemic began.
Just over a third (34 per cent) of respondents were in the 35-to-44 age group; 40 per cent were in the 45-to-54 age group; and the remaining respondents were in the 18-to24 (3 per cent), 25-to-34 (17 per cent), and 55-to-65+ (6 per cent) age groups.
Of those respondents who said their migraine had become more frequent, 84 per cent said that this was due to
stress caused by the Covid-19 pandemic. Other factors cited as triggering a moderate-to-severe increase in migraines included changes to their routine (67 per cent), a lack of sleep (63 per cent), and increased screen time (60 per cent).
A smaller number of respondents, 18 per cent, reported a decrease in the frequency of their migraines since the introduction of the Covid-19 restrictions. Similarly, 13 per cent of respondents reported a decrease in the severity of their migraines.
Working hours
The survey also found that among the individuals who were experiencing more frequent migraines, over one-third (37 per cent) were working from home, 21 per cent said that their working hours had increased during the pandemic, and 20 per cent were no longer working.
With regard to the availability of appointments with healthcare professionals, 52 per cent of respondents to the survey said that their appointments were either cancelled or postponed since the start of the pandemic. Almost half (49 per cent) of all respondents who experienced an increase in migraines reported cancelled or postponed appointments. While 41 per cent of all respondents have had a virtual health-related consultation since the pandemic began, most of this group (68 per cent) rated their consultation as either ‘good’ or ‘excellent’.
Stress
Commenting on the results, Dr Martin Ruttledge, Consultant Neurologist, Beaumont Hospital and Hermitage Medical Clinic, Dublin, said: “It’s worrying that the survey shows that many migraine sufferers are either experiencing more severe or frequent migraines. However, it is not unexpected, as we know that stress is a very common exacerbating factor in this condition, and it has been a very stressful period for everybody over the last four-to-five months with the Covid pandemic. Migraine, especially the more chronic forms, can be a very disabling neurological disorder, and the worldwide uncertainty in recent months has only made the situation worse.
products affecting hepatic function, glucose-6-phosphate dehydrogenase deficiency, haemolytic anaemia, glutathione deficiency, dehydration, chronic malnutrition, weight less than 50kg, elderly, in patients with underlying sensitivity to aspirin and/or to non-steroidal antiinflammatory drugs (NSAIDs), hypotension, benign prostatic hyperplasia, urethral stenosis, adrenal insufficiency (Addison’s disease), hypothyroidism, multiple sclerosis, chronic colitis ulcerative, and diseases that present with reduced respiratory capacity such as emphysema; kyphoscoliosis. Severe obesity or convulsive disorders. Use with great care in those whose condition may be exacerbated by opioids, such as those who are on concurrent CNS depressant drugs, with prostatic hypertrophy and inflammatory or obstructive bowel disorders.
Careful risk-benefit assessment: required in patients with opioid dependence, chronic constipation, impaired consciousness, compromised respiratory function and chronic obstructive airway disease. CYP2D6 metabolism: In deficiency or absence of CYP2D6 an adequate analgesic effect will not be obtained; in extensive or ultra-rapid opiate/codeine metabolisers an increased risk of opioid toxicity.
dependence. Tolerance, psychological and physical dependence (addiction) develop with prolonged use of high doses with withdrawal symptoms, such as restlessness and irritability, after sudden discontinuation of the drug. Cross-tolerance with other opioids exists. Rapid relapses can be expected in patients with pre-existing opiate dependence (including those in remission). Administration must be discontinued gradually after prolonged treatments. Caution is particularly recommended for use in children, adolescents, young adults and in patients with a history of drug and/or alcohol abuse. Sodium content: Each effervescent tablet contains 388mg sodium. Patients with rare hereditary problems of fructose intolerance should not take this medicine. If the patient has a productive cough, codeine may impede expectoration. Interactions: Please refer to the SPC for full details of interactions. Pregnancy and Lactation: This product should not be used during pregnancy or lactation. Life-threatening adverse events or neonatal death may occur even at therapeutic doses. Adverse
“Patients should seek advice from their primary care doctors and other healthcare professionals if they are struggling. We are still having face-to-face and virtual consultations in our migraine clinic, and many GPs are reviewing their patients regularly, both in person and by phone. There are effective treatments available for many migraine sufferers and we are still available for our patients.”
Discussing the survey results, Patrick Little, CEO, Migraine Association of Ireland, said they show that the pandemic is proving to be a stressful time for migraine sufferers, with respondents reporting a sharp increase in the frequency and severity of migraines.
500mg every 8 hours. Hepatic Impairment or Gilbert’s Syndrome: dose must be reduced or the dosing interval prolonged. Contraindications: In all paediatric patients (0-18 years of age) who undergo tonsillectomy and/or adenoidectomy for obstructive sleep apnoea syndrome; in the event of impending childbirth or in case of risk of premature birth; in women during breastfeeding, in known CYP2D6 ultra-rapid metabolisers, hypersensitivity to paracetamol or codeine or any of the excipients; in patients with acute asthma, respiratory depression, acute alcoholism, head injuries, raised intracranial pressure and following biliary tract surgery or cholecystectomy, or patients currently receiving or within 14 days of stopping monoamine oxidase inhibitor therapy. Precautions and Warnings: Administer with caution: impaired cardiac function, hepatic impairment, chronic alcoholism, renal impairment (GFR≤50ml/min), Gilbert’s Syndrome (familial non-haemolytic jaundice), concomitant treatment with medicinal
Concomitant use of opioids and benzodiazepines: reserve only for use in patients for whom alternative treatment options are inadequate. If a decision is made to prescribe concomitantly with benzodiazepines, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of sedation and respiratory depression. Concomitant use of opioids and alcohol: not recommended. Children with compromised respiratory function: Not recommended. Extensive use: to relieve headaches or migraines, especially at high doses, may induce headaches. In such cases the analgesic should not continue to be taken without medical advice. Prolonged use: risk-benefit of continued use should be assessed regularly by the prescriber. Care should be observed if prolonged therapy is contemplated. Monitoring after prolonged use should include blood count, liver function and renal function.
Hepatotoxicity: may occur with paracetamol even at therapeutic doses, after short treatment duration and in patients without pre-existing liver dysfunction. Severe-cutaneous adverse reactions (SCARs): Very rare cases of serious skin reactions such as Stevens-Johnson syndrome (SJS), and Toxic epidermal necrolysis (TEN) have been reported with the use of paracetamol. Patients should be advised of the signs and symptoms and monitored closely for skin reactions. If symptoms or signs of SJS and TEN (e.g. progressive skin rash often with blisters or mucosal lesions) occur, patients should stop treatment immediately and seek medical advice. Patients should be advised not to exceed the recommended dose and not take other paracetamol containing products concurrently. Dependence: Codeine has a primary potential for
Reactions: Related to Paracetamol component: Very rare: thrombocytopenia, neutropenia, leukopenia, erythema, urticaria, rash. Not known: agranulocytosis, haemolytic anaemia, in particular in patients with underlying glucose 6-phosphate-deshydrogenase deficiency, hypersensitivity, such as anaphylactic shock, angioedema, bronchospasm, toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome (SJS), acute generalized exanthematous pustulosis, fixed drug eruption, cytolytic hepatitis, which may lead to acute hepatic failure. Related to Codeine component: Not Known: Hypersensitivity, confusional state, dysphoria, euphoria. Long-term use also entails risk of drug dependence. Seizure, headache, somnolence, dizziness, sedation, miosis, tinnitus, respiratory depression, constipation,
“We are particularly concerned that over four-fifths of those surveyed said that COVID-related stress is causing them to suffer from more frequent migraines, especially at a time when some appointments with healthcare professionals were being postponed.”
Tips for patients to manage migraine during Covid-19
• Keep a migraine diary – identify any potential triggers and make a note of how they affect you.
• Establish a daily routine and stick to it as much as possible.
• Practice good sleep hygiene – go to sleep and wake up at a similar time daily.
• Limit screen time – take regular breaks from your phone, TV or desktop during the day.
• Practice self-care – exercise, eat healthy meals regularly, and stay hydrated.
• If consuming alcohol do so in moderation.
• Reduce stress – try yoga, meditation or mindfulness.
• Stay in touch – maintain contact with friends, family and support groups.
For more information on migraines and the Migraine Association of Ireland, visit www.migraine.ie or call 1850 200 378

Clinical Pain 26 THE MEDICAL INDEPENDENT | 26 OCTOBER 2020
SOLPADOL® PROVIDES EFFECTIVE PAIN RELIEF FOR ACUTE MODERATE-TO-SEVERE PAIN 1,2 SOLPADOL® – THE ONLY COMBINATION OF ITS KIND* AVAILABLE IN IRELAND IN BOTH CAPLET AND EFFERVESCENT FORM 3 *codeine (30 mg)/ paracetamol (500 mg)
DISTRESSING PAIN References: 1. Solpadol (caplet) Summary of Product Characteristics. 2. Solpadol (effervescent) Summary of Product Characteristics. 3. IQVIA IRLH/IRLP combined data, 2019. Accessed May 2020. MAT-IE-2000317 | Date of preparation: May 2020 Prescribing Information: Solpadol 500mg/30mg Caplets and Effervescent Tablets Please refer to the Summary of Product Characteristics (SmPC) before prescribing. Presentations: Solpadol 500mg/30mg Effervescent Tablets: Effervescent tablet containing 500mg paracetamol and 30mg codeine phosphate hemihydrate. Solpadol Caplets 500mg/30mg Tablets: Capsule-shaped tablet containing 500mg paracetamol and 30mg codeine phosphate. Indications: For the relief of severe pain. Indicated in patients older than 12 years of age for the treatment of acute moderate pain which is not considered to be relieved by other analgesics such as paracetamol or ibuprofen (alone). Dosage and Administration: Both presentations are for oral administration. Effervescent Tablets should be dissolved in at least half a tumbler full of water. The lowest effective dose should be used and for the shortest period of time. Maximum (max.) daily dose of codeine should not exceed 240mg. The duration of treatment should be limited to 3 days and if no effective pain relief is achieved the patients/carers should be advised to seek the views of a physician. Max. daily dose of paracetamol should not exceed 60mg/ kg/day (up to a max. of 2g per day) in the following situations or unless directed by a physician: weight less than 50kg, chronic alcoholism, dehydration or chronic malnutrition. Adults (≥18 years): 2 tablets every 4-6 hours. Max. 4 doses in any 24 hours. Do not exceed 8 tablets in 24 hours. Elderly: Dosage should be reduced to half the adult dose and titrated to the individual’s need and overall medical condition. Children (16-18 years): 1-2 tablets every 6 hours to a max. of 4 doses in any 24 hours. Do not exceed 8 tablets in 24 hours. Children (12-15 years): 1 tablet every 6 hours to a max. of 4 doses in any 24 hours. Do not exceed 4 tablets in 24 hours. Children <12 years: should not be used due to the risk of opioid toxicity. Renal failure: 10-50 ml/min: 500mg every 6 hours.
DISARM
<10 ml/min:
vomiting, nausea, dry mouth, pruritus, urinary retention, fatigue and hypotension. Visuomotor coordination and visual acuity may be adversely affected in a dose-dependent manner at higher doses or in particularly sensitive patients. Please refer to the SPC for more details. Legal Category: POM. Marketing Authorisation Numbers: PA540/159/1 & PA540/159/3. Marketing Authorisation Holder: Sanofi-Aventis Ireland Ltd., T/A SANOFI, Citywest Business Campus, Dublin 24, Ireland. Further information is available from: Sanofi, 18 Riverwalk, Citywest Business Campus, Dublin 24 or contact IEmedinfo@sanofi.com Tel: (01)4035600. Date of preparation: May 2020. Adverse events should be reported. Reporting forms and information can be found at www.hpra.ie; email: medsafety@hpra.ie Adverse events should also be reported to Sanofi Ireland Ltd. Tel: 01 403 5600. Alternatively, send via email to IEPharmacovigilance@sanofi.com 11447_Solpadol_10X4_AdCopy_MAY20_01.indd 1 28/05/2020 11:51




Gutcast: Living Better with Inflammatory Bowel Disease (IBD) Feature Series
Managing fatigue with IBD
“The intensity of the fatigue, even in remission, is very high and can be easily compared to people who have just finished chemotherapy.”
Clinical Fatigue, including “brain fog,” is consistently rated by patients as the most troubling physical symptom of their inflammatory bowel disease (IBD). Gutcast, a new podcast series developed by the Irish Society for Colitis and Crohn’s Disease (ISCC) in partnership with Janssen Sciences Ireland UC, provides information, guidance and support for people living with IBD.
The sixth episode of Gutcast features Eimear O’Shea, a senior physiotherapist at St. James’s Hospital, Dr Anthony O’Connor, Consultant Gastroenterologist at Tallaght University Hospital and Elaine Neary, a dietician in gastroenterology at Tallaght University Hospital. Together with Amy Kelly, host of Gutcast and Director of ISCC, they explore the differences between tiredness and fatigue and discuss how best to manage clinical fatigue arising from IBD.

In this episode, all three healthcare experts agree that sleep, diet, exercise and the support of family and friends are extremely important in managing fatigue, the intensity of which could be easily compared to people who had just finished chemotherapy.
Clinical fatigue
Dr O’Connor explains that clinical fatigue is not just tiredness, which everybody experiences. Clinical fatigue involves a perception of generalised weakness, where people have difficulty in initiating activities, suffer quick fatiguability, have a reduced capacity to maintain activity and mental fatigue, and where they have difficulty with concentration and sometimes with emotional stability and memory.
“Clinical fatigue is consistently rated by people living with IBD as the most troubling physical symptoms of their condition and even when they are in remission, up to 40% of people with IBD will have clinical levels of fatigue. When you’re in a flare, that goes up to about 80%-85%, so it’s extremely common. The intensity of the fatigue, even in remission, is very high and can be easily compared to people who have just finished chemotherapy. The other thing about fatigue is that it doesn’t always correlate very well with how your disease is doing. Your bloods can be fine. Your stool markers can be fine. You can have a colonoscopy that looks okay and you can still have crippling fatigue. That’s frustrating for patients in some respects because sometimes the doctors and nurses haven’t got much to say to them as ostensibly the treatments they’re getting are working, but the patient is still left with this symptom.”
Elaine Neary agrees that while clinical fatigue could often strike people more during flare ups, it can linger all through remission as well. The causes are multi-factorial: interrupted sleep, pain, stress, anxiety associated with symptoms and sometimes side effects from medication.
Mental fatigue
Outlining the multi-faceted nature of the fatigue experienced, Dr O’Connor comments, “Many people living with IBD describe mental fatigue to me as a sort of a ‘brain fog’ where they just don’t feel mentally as sharp as they might have felt beforehand. It’s a huge problem and can be caused by nutritional deficiencies, stress and anxiety. The gut and the brain are very closely linked. The
microbiome, the generally friendly bacteria that line your bowel, seems to have a very important role in mediating what goes on between the gut and the brain.”
Elaine Neary outlines that when people mention a “fuzzy brain” or a “foggy mind”, health professionals know patients are struggling with extreme exhaustion. It is something that hugely affects their quality of life, from emotions to working, relationships and food-related quality of life. ”It’s very frustrating and people often feel it is related to lack of eating or poor intake but sometimes it’s unexplained and I think that’s another frustrating aspect of it.”
Nutrition
Ms Neary says up to 80% of people with IBD are malnourished and 75% lose weight with the condition. “IBD is also an anorexigenic disease. Those inflammatory chemicals can reduce their appetite and because of that they don’t eat enough and are not getting sufficient calories. There’s also a sitophobia, which is a fear of eating because of symptoms, they are restricting themselves and not getting the required nutrients. If somebody is fatigued, we would check to see if they’re absorbing their nutrients, if their medications are working. Sometimes there can be deficiencies that prevent medications from working.
If proteins in their bloods are low like albumin or if their Vitamin D is low, their medications might not be working correctly. We would also check their haematinics, their iron levels, their B12 and their folate because if they’re low, they may be causing anaemias and that will cause fatigue. We would be stressing that they should drink at least ten cups or glasses of water per day because a big cause of fatigue is dehydration. We try to remind them that thirst is the final stage of hydration so not to wait until they are thirsty to drink. We recommend that they would eat every three hours and that they maintain a balanced diet. Starchy and refined carbohydrates are very important for energy.”
Exercise
Eimear O’Shea says that when people living with IBD are suffering from fatigue, exercise can be one of the first things to go. However, exercise is particularly important for people with IBD, who can have weaker bones and higher levels of osteoporosis and osteopenia, due to calcium deficiency and the use of steroids. “Exercise can actually help with fatigue and has an anti-inflammatory effect. If done in the right way, at the right levels, it can help to reduce systemic inflammation and reduce symptoms and flare ups. Start
very small, then you can try and push it out a bit more. Walking, cycling, gentle yoga, Pilates or a gym with a bathroom nearby. Whatever you enjoy and whatever works for you. You could exercise at lunchtime or in the evening and finish your exercise in time to have an hour or two to relax before bed.”
Dr O’Connor believes that most of us have two waves of tiredness in our body clock, “One around half eight, nine o’clock and then another around 11, half 11. The advice is usually to ride one of those waves. You might see someone going to the gym at half eight, quarter to nine and they’re exhausted
can also have a big impact on their sex life, which again impacts on their quality of life and psychological well-being. Depression and anxiety occur more commonly in the IBD population and a lot of their anxieties are very real. He suggests that doctors, nurses and other professionals need to be a little bit braver about addressing these issues.
Communicating with employers
Dr O’Connor says the CCUK Group, Crohn’s & Colitis United Kingdom, have a wonderful booklet that patients who are newly diagnosed can give to their employer to explain to them all the aspects of the disease, including fatigue. Gutcast can be a helpful tool managers or colleagues to gain a greater understanding of IBD and the challenges a patient may face.
“I think most employers are reasonable and know that employees living with IBD need to be accommodated for. That can mean just sitting down and making sensible arrangements with them. If you feel particularly fatigued on a Thursday or Friday, maybe somebody might restructure their hours a bit and do some more on a Monday or maybe have fewer demanding duties at particular times. Communication is the key and I think you’ll find doctors and nurses are very happy to provide letters and explanations to employers about these factors because they’re very important.”
and they can’t do everything they want to do because their body is getting its first wave of, ‘it’s time for me to go to sleep now.’”
Sleep and Personal Life
Eimear O’Shea says sleep is important as well as trying to make sure that you are as prepared for sleep as possible, so that you get the best night’s sleep that you can.
Elaine Neary says if people don’t get seven to eight restful hours of sleep a night, it can affect the way their GI tract functions. “We would talk to people about ‘sleep hygiene’ and try to get them into a routine of going to sleep, only when they are feeling sleepy, no blue light, electronics at night time, not taking naps during the day, even though they feel so fatigued, and not exercising too close to bed as well because that would probably keep them awake. Obviously, they should also avoid alcohol and nicotine at night time.”
Dr O’Connor says if people are fatigued, it
The “Managing Fatigue” episode of Gutcast provides patients with an important resource to take control of their IBD. It can also be helpful for family and friedns to listen to in order to understand the condition and be able to support their loved ones.
Gutcast brings together healthcare professionals and people living with Crohn’s disease and ulcerative colitis to give their opinions and advice on a variety of topics including mental health, fatigue, managing work and social life, sex and relationships and getting the most out of your healthcare appointments. Each Gutcast episode has been compiled in response to feedback from people living with IBD with the aim of providing practical advice and to address questions they may not feel comfortable openly discussing.
Please tune in to hear more on these topics and encourage those you are treating for IBD to go to ISCC.ie/gutcast where they can listen to the episodes and learn more about supports available. Or they can search ‘Gutcast’ on the Apple Pocast app, Spotify, Google Play music or wherever they get their podcasts.
Date of Preparation August 2020, EM-35133
Spotlight Cross-Immunology 28 THE MEDICAL INDEPENDENT | 26 OCTOBER 2020
Dr Anthony O'Connor, Amy Kelly, Elaine Neary and Eimear O'Shea
You might see someone going to the gym at half eight quarter to nine and they're exhausted and they can't do everything they want to do because their body is getting its first wave of, 'it's time for me to go to sleep now'
Sex and relationships
Getting the most from appointments Managing fatigue
The first podcast for people living with IBD in Ireland


Gutcast is a unique resource for patients that brings together experts and people living with Crohn’s disease and ulcerative colitis to provide information and advice on how to manage IBD.
iMR code: EM-35097
Topics include:
IBD & COVID-19
What I wish I’d known
Mental Health
Work and social life
To access more information about Gutcast for HCPs open the camera on your phone and scan here:
Sex and relationships
Getting the most from appointments
Managing fatigue
Personal stories of IBD >
Personal stories of IBD >
To access more information about Gutcast for HCPs open the camera on your phone and scan here:
Direct your patients to ISCC.ie/Gutcast to learn more or to listen wherever they get their podcasts.
Direct your patients to ISCC.ie/Gutcast to learn more or to listen wherever they get their podcasts.
Date of preparation: July 2020
Hosted by Amy Kelly, Director of ISCC and living with Crohn’s disease
iMR code: EM-35097 Date of preparation: July 2020
Spotlight Gallery










 Prof Ivan Casserly (Speaker)
Dr Corinna Sadlier (Speaker) & Dr John Sheehan (Chairperson)
Dr Raymond Walley (Chairperson)
Dr Oisin O’Connell (Speaker)
Dr James Dollard (Speaker)
Prof Luke O’Neill (Speaker)
Francis Lynch, A.Menarini General Manager Ireland and UK
Nicola McNamara, A.Menarini Medical Representative
Annual A.Menarini National GP Masterclasses
Prof Ivan Casserly (Speaker)
Dr Corinna Sadlier (Speaker) & Dr John Sheehan (Chairperson)
Dr Raymond Walley (Chairperson)
Dr Oisin O’Connell (Speaker)
Dr James Dollard (Speaker)
Prof Luke O’Neill (Speaker)
Francis Lynch, A.Menarini General Manager Ireland and UK
Nicola McNamara, A.Menarini Medical Representative
Annual A.Menarini National GP Masterclasses
Significantly improves exercise duration and reduces angina frequency1

Prescribing Information: Ranexa (ranolazine). Please consult the Summary of Product Characteristics (SPC) for full prescribing information. Presentation: Prolonged-release tablets containing 375 mg, 500 mg or 750 mg of ranolazine. 750 mg tablet contains E102 and lactose. Use: Ranexa is indicated as add-on therapy for the symptomatic treatment of patients with stable angina pectoris who are inadequately controlled or intolerant to first-line antianginal therapies (such as beta-blockers and/or calcium antagonists). Dosage and administration: Oral administration. Patients should be instructed to list their medication to their health care professional at each visit. Adults: Initial dose is 375 mg twice daily. After 2-4 weeks, dose should be titrated to 500 mg twice daily and, according to patient’s response, further titrated to 750 mg twice daily. Concomitant treatment with moderate CYP3A4 and P-glycoprotein (P-gp) inhibitors: Careful dose titration is recommended. Renal impairment: Careful dose titration is recommended in mild to moderate renal impairment, and contraindicated in severe renal impairment. Hepatic impairment: Careful dose titration is recommended in mild hepatic impairment, and contraindicated in moderate to severe hepatic impairment. Elderly: Dose titration in the elderly should be exercised with caution. Low weight: Dose titration in patients with low weight should be exercised with caution. Congestive Heart Failure (CHF): Dose titration in moderate to severe CHF should be exercised with caution. Paediatric patients: No data in children below the age of 18 years. Ranexa tablets should be swallowed whole and not crushed, broken or chewed. They may be taken with or without food. Contra-indications: Hypersensitivity to the active substance or to any of the excipients. Severe renal impairment. Moderate or severe hepatic impairment. Concomitant administration of potent CYP3A4 inhibitors. Concomitant administration of Class Ia or Class III antiarrhythmics other than amiodarone. Warnings and Precautions: Caution should be exercised when prescribing or up titrating ranolazine to patients in whom an increased exposure is expected. QT prolongation: Caution should be observed when treating patients with a history of congenital or a family history of long QT syndrome, in patients with known acquired QT interval prolongation, and in patients treated with drugs affecting the QTc interval. Interactions: Co-administration with CYP3A4 inducers is expected to lead to lack of efficacy. Renal impairment: Check renal function at regular intervals during treatment. Interactions: CYP3A4 inhibitors: Increase plasma concentrations of ranolazine. Combining ranolazine with potent CYP3A4 inhibitors is contraindicated. CYP3A4 inducers: Avoid initiation with Ranexa during administration of CYP3A4 inducers. CYP2D6 inhibitors: May increase plasma concentrations of ranolazine. Effect of ranolazine on other medicinal products: Dosage adjustment of sensitive CYP3A4 substrates and CYP3A4 substrates with a narrow therapeutic range may be required. Lower doses of CYP2D6 substrates may be required. Caution with CYP2B6 substrates. Monitor digoxin levels following initiation and termination of Ranexa. Limit dose of simvastatin to 20mg once daily in patients taking Ranexa. Limit dose of atorvastatin and consider clinical monitoring in patients taking Ranexa. Monitor blood levels of tacrolimus when co-administering with Ranexa and adjust tacrolimus dose accordingly. Also recommended for other CYP3A4 substrates with a narrow therapeutic range. Drugs transported by the Organic Cation Transporter-2 (OCT2): Plasma exposure of metformin increased in subjects with type 2 diabetes mellitus when co-administered with Ranexa. The exposure of other OCT2 substrates may also be affected. Theoretical risk that concomitant treatment with drugs known to prolong the QTc interval may increase the possible risk of ventricular arrhythmias. Pregnancy and lactation: Ranexa should not be used during pregnancy unless clearly necessary. Ranexa should not be used during breast-feeding. Effect on fertility unknown. Side-effects: Generally mild to moderate in severity and often develop within the first 2 weeks of treatment. Common (1-10%): dizziness, headache, constipation, vomiting, nausea, asthenia. Uncommon (0.1–1%): anorexia, decreased appetite, dehydration, anxiety, insomnia, confusional state, hallucination, lethargy, syncope, hypoaesthesia, somnolence, tremor, postural dizziness, paraesthesia, blurred vision, visual disturbance, diplopia, vertigo, tinnitus, hot flush, hypotension, dyspnoea, cough, epistaxis, abdominal pain, dry mouth, dyspepsia, flatulence, stomach discomfort, pruritus, hyperhydrosis, pain in extremity, muscle cramp, joint swelling, muscular weakness, dysuria, haematuria, chromaturia, fatigue, peripheral oedema, increased blood creatinine, increased blood urea, prolonged QT corrected interval, increased platelet or white blood cell count, decreased weight. In a long term study, acute renal failure was also reported with an incidence less than 1% in placebo and ranolazine patients. Rare (0.1-0.01%): hyponatremia, disorientation, amnesia, depressed level of consciousness, loss of consciousness, coordination abnormal, gait disturbance, parosmia, impaired hearing, peripheral coldness, orthostatic hypotension, throat tightness, pancreatitis, erosive duodenitis, oral hypoaesthesia, angioedema, allergic dermatitis, urticaria, cold sweat, rash, acute renal failure, urinary retention, erectile dysfunction, elevated levels of hepatic enzyme. Increased incidence of congestive heart failure and transient ischaemic attacks seen in patients with history of chronic angina who had incomplete revascularisation after percutaneous coronary intervention and treated within 2 weeks with ranolazine (1000 mg twice daily [dose not approved in Europe]) in a placebo-controlled post-PCI trial. Elderly, renal impairment and low weight: In general, adverse events occurred more frequently among elderly patients and patients with renal impairment. Adverse events in patients with low body weight were similar to those of patients with higher weight. Please consult the SPC for further information. Pack size: 60 tablets. Legal category: POM. Marketing authorisation numbers: EU/1/08/462/001-006
Marketing Authorisation holder: Menarini International Operations Luxembourg S.A. Marketed by: A. Menarini Pharmaceuticals Ireland Ltd. Further information is available on request from A. Menarini Pharmaceuticals Ireland Ltd, 2nd Floor, Castlecourt, Monkstown Farm, Monkstown, Glenageary, Co. Dublin A96 T924 or may be found in the SPC. Last updated: April 2019.


Date of item: August 2019. IR-RAN-03-2019
References: 1. Chaitman, B.R., et al. JAMA, 2004; 291(3): p. 309-16.
ALL REPORTS BY PAT KELLY
Irish Cardiac Society, 71st Annual Scientific Meeting, 1-3 October 2020
ICS embraces virtual conference format
The Irish Cardiac Society (ICS) 71st Annual Scientific Meeting was opened by outgoing ICS President Prof Jim Crowley, who thanked those who attended in its virtual format and expressed his hope that next year’s meeting could return to its normal face-to-face setting.
“I would like to thank the speakers for contributing,” said Prof Crowley. “We have a very high standard in terms of the quality of presentations and I hope you will find that enjoyable, and hopefully next year we will be back to the live [face-to-face] format, although we don’t know where we will be until we sort out the pandemic. But certainly, this current format lends itself to certain presentations and I think it is likely that this format will continue to provide us with interesting meetings and methods for educating ourselves in the
Rise of the machines in cardiology
field of cardiology and other areas of medicine.”
Prof Crowley also acknowledged the importance of sponsors’ input to the meeting, noting that their symposia “have added to the academic input of this meeting”.
The Thursday and Friday had sessions in association with the Irish Nurses Cardiovascular Association and the Irish Cardiac
The first of the Saturday sessions was chaired by Prof Aaron Peace, Consultant Cardiologist and Research and Development Director of the Western Health and Social Care Trust (WHSCT).
Prof Peace introduced Prof Nico Bruining, Head, eCardiology, Clinical Epidemiology and Innovation (KEI), Thoraxcentre, Erasmus MC, Rotterdam, The Netherlands, and Editor-in-Chief of the European Heart Journal — Digital Health

Prof Peace noted that Covid-19 has been “a catalyst to digital cardiology and the provision of virtual care and we are seeing an increase in the use of tools such as the AliveCor device”, which allows patients to take a medical-grade ECG in just 30 seconds.
Prof Bruining addressed the meeting on the topic ‘Developments in Digital Cardiology’ and told the attendees: “The European Society of Cardiology (ESC) realised a few years ago that e-health, now mainly called digital health, was rapidly gaining more importance and that more attention needed to be given to it.”
Prof Bruining explained that in his own centre, he and his colleagues are examining how they can practically implement these new technologies. “That starts with first collecting all the clinical data that we generate from an admitted patient… AI software is also used in subcomponents in the care process, such as image and signal analysis.”
Clinical Physiologists and heard presentations on a variety of topics ranging from virtual drug titrations and remote self-care, to echo reporting and Covid-19. Consultant Cardiologist, Mater Misericordiae University Hospital, Dublin, Prof Jim O’Neill also delivered a presentation to the Friday session entitled ‘Cardiac Transplant’, as well as a range of oral abstracts, moderated postersw and general posters.
He pointed out that the ECS has developed a ‘roadmap’ for digital activities that it wants to undertake, which was outlined in a position statement from the Society.

Artificial intelligence
“A good illustration of the growing interest in artificial intelligence (AI) is the rapidly-increasing number of publications about the use of machine learning in the titles,” said Prof Bruining. “AI is a focus of attention at the moment… AI can be extremely helpful in processing the ever-growing amount of data that we collect on patients. The most optimal information would be if the software could serve us for clinical decision support, something that has been at the top of our wish-list for many years, but may now be realised.”
Steering the ship in choppy waters
Incoming President of the ICS Prof Vincent Maher, Consultant Cardiologist, Tallaght University Hospital, Dublin, has outlined his hopes and plans for the Society during his tenure, adding that he views the financial inequality brought about by the new-entrant consultant contract as unfair and a disincentive to consultants potentially returning to Ireland.
Speaking to the Medical Independent (MI), Prof Maher discussed taking leadership of the Society during the Covid-19 pandemic. “What’s going on generally at the moment is quite surreal. I am taking over as President having already been Treasurer of the Society, including during the last six months of this crisis, so it’s not as if this situation is brand new to me, but it is a challenge,” said Prof Maher. “I have to commend the work that has been done by my predecessor [Prof Jim Crowley] and Barbra Dalton [ICS Executive Administrator] in pulling together a good conference this year. The attendance was significantly up from previous years because of the virtual links but the closeness, the bonding and sharing of information – so much goes on [at faceto-face conferences] that just doesn’t happen in the virtual world, but it is what it is. We can’t be seen as a body to deny the existence of this; we just have to find a way around it.”
He also referred to “Zoom fatigue”, which is setting in for a lot of people who would normally be attending face-to-face conferences at this time of year. “So, how to make events interesting and novel is a challenge, but I’m up for it.”
Lockdown
Prof Maher
sense of relief after it was decided recently that Ireland would not be placed under another level 5 general lockdown, bearing in mind the potential effects on cardiology services and waiting lists. “There is an air of uncertainty about all of this,” he told MI. “This is the second wave; there is a fatigue factor out there because of lockdowns and restrictions. Nonetheless, we have not learned how to manage this virus much differently than when it first appeared. We are a bit more informed, we know certain therapeutic interventions that are appropriate, but we have no cure and until we have a vaccine that is highly effective, we are always going to be looking over our shoulders on how to manage patients with Covid.
“And of course, it’s not the only show in town,” he continued. “All the other ailments are still there and Covid has to be fit into its place. So whilst I am relieved, it is only for the actual point of the emotional impact that this is having on people, and relieved that we are not going down what some people would see as a draconian route. I was relieved about that, but not to the point that we should not listen to what the national public health emergency team (NPHET) is saying, because ultimately, if we become overwhelmed with this virus, people will die unnecessarily. If too many patients have Covid, people will die and nursing homes will be affected, and all those patients waiting for cardiac treatment would be denied treatment, so it has to be managed appropriately. So I am happy at the moment to see how things go, but I am very conscious that we may have to change rapidly if things deteriorate.
“Hopefully, NPHET and Government will steer us on the right course and we are conscious that services can become over-
A number of practical AI solutions have already been implemented, he explained, particularly in the area of cardiovascular imaging analysis, including calcium detection in CT images, among other applications. “Echocardiography is the workhorse in the cardiovascular system and it must all be processed,” said Prof Bruining. “That can become a huge amount of work in busy centres and AI can also be deployed here to help out.” In this regard, Prof Bruining pointed to a study by Attia et al, which described the process to construct a fully-automated pipeline for the assessment of cardiac structure, function and disease detection. The authors describe this pipeline as “fully scalable, as evidenced by our analysis of >14,000 echocardiograms for this article on a 14-node compute cluster, all in a period of <3 weeks”.
Computer models
Another emerging form of image analysis is to confer the images to a patient-specific computer model, he said, and use it for further calculations. Prof Bruining presented the conference with an example of a practical application of this in a patient undergoing reconstruction of a microvalve, as well as case studies of other patients to help determine patient-specific potential paravalvular leakage in transcatheter aortic valve replacement prosthesis prior to implantation.
whelmed, but are also conscious of the need to maintain the morale of individuals.”

Diaspora
In his closing comments during the conference, Prof Maher referred to the importance of the Irish Diaspora and the role these doctors can play in improving healthcare in Ireland when they return. However, he was asked if the pay conditions imposed on ‘new-entrant’ consultants under their controversial contract would prove to be a disincentive for them to work within the Irish system. “Our heartstrings pull us back to Ireland, and I was no different to anyone else,” said Prof Maher. “When you come home in the current situation, to have a salary that will challenge you financially compared to the people who are already established… that discrepancy between these bright people coming home and those already established can be a disincentive – I feel there should be equal pay for equal work.
“It’s a competition; the people who are most experienced and most published will clearly have an advantage and for them to come home and not be on a par for doing the exact same work is a little unfair. The degree of remuneration for consultants generally is high [compared to the general population] and if you are in any profession and you come home and are placed in a lower tier, having established yourself internationally and are then paid less than your peers, that is a disincentive.”
Regarding the Society, Prof Maher touched on the conference collaboration between the ICS and the Mayo Clinic, which saw a major conference held in the RCSI last year. “We were going to run a second one of those, but that is on hold at the moment,” he said. “The
Mayo Clinic is a fantastic centre and there are other fantastic centres in Europe, so we may create a link where we can have a similar symposium where we have the best of European expertise joining us in a conference. But of course, all of this is on hold at the moment. If my world is going to be virtual for the next two years then so be it, but we can’t let all the good work being done fall to the wayside.”
World expertise
Prof Maher concluded: “There are very few cardiovascular ailments that do not have a lead-in period of years before complications arise,” he told MI. “A myocardial infarction, for example, is the end result of life-long atherosclerosis. Similarly, valves that finally fail – they have been deteriorating for years; the heart muscle has been stiffening for years, until we get to a stage where it is very difficult to manage, so I am hoping that we can try to tap into world expertise on how diseases progress over time and how we can delay disease progression, and perhaps reverse disease advancement.
“We need to look at disease trajectory and small things that can be manipulated to change that trajectory – basically, ‘a stitch in time saves nine’ and that would be a major interest of mine… of course, lifestyle is part of that, but you can’t ‘lifestyle-away’ your genes. You can be a slim, fit young person and still have severe cholesterol problems. Understanding how to manipulate that with the right therapeutics over the long-term is important… we tend to be too focused on the complications phase rather than the disease progression and intervening, and I would like to bring that to the fore in symposia during my tenure.”
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 32
Conference Coverage
was also asked if he felt a certain
Prof Nico Bruining
COMBINING POWER AND CONFIDENCE
AGAINST LDL-C IN THE TREATMENT OF HYPERCHOLESTEROLAEMIA
COMBINING POWER AND CONFIDENCE
AGAINST LDL-C IN THE TREATMENT OF HYPERCHOLESTEROLAEMIA
20 mg /10 mg Rosuvastatin + Ezetimibe 10 mg /10 mg Rosuvastatin + Ezetimibe
Suvezen is indicated for substitution therapy in adult patients who are adequately controlled with rosuvastatin and ezetimibe given concurrently at the same dose level as in the fixed combination, but as separate products, as adjunct to diet for treatment of primary hypercholesterolaemia (heterozygous familial and non-familial) or homozygous familial hypercholesterolaemia1
Indication: Suvezen
Rosuvastatin + Ezetimibe
10 mg /10 mg
Rosuvastatin + Ezetimibe
20 mg /10 mg
Suvezen is indicated for substitution therapy in adult patients who are adequately controlled with rosuvastatin and ezetimibe given concurrently at the same dose level as in the fixed combination, but as separate products, as adjunct to diet for treatment of primary hypercholesterolaemia (heterozygous familial and non-familial) or homozygous familial hypercholesterolaemia1






Rosuvastatin + Ezetimibe NOW AVAILABLE
with caution in patients who consume excessive quantities of alcohol and/or have a history of liver disease. Renal effects: Proteinuria has been observed in patients treated with higher doses of rosuvastatin and was transient or intermittent in most cases. Proteinuria has not been shown to be predictive of acute or progressive renal disease. An assessment of renal function should be considered during routine follow-up of patients treated with a dose of 40 mg. Diabetes mellitus: Some evidence suggests that statins raise blood glucose and in some patients, at high risk of future diabetes, may produce a level of hyperglycaemia where formal diabetes care is appropriate. This risk, however, is outweighed by the reduction in vascular risk with statins and therefore should not be a reason for stopping statin treatment. Patients at risk (fasting glucose 5.6 to 6.9 mmol/l, BMI >30 kg/m2, raised triglycerides, hypertension) should be monitored both clinically and biochemically according to national guidelines. Interstitial lung disease: Exceptional cases have been reported with some statins, especially with long term therapy. Presenting features can include dyspnoea, non-productive cough and deterioration in general health (fatigue, weight loss and fever). If it is suspected, statin therapy should be discontinued. Protease inhibitors: Increased systemic exposure to rosuvastatin has been observed in subjects receiving rosuvastatin concomitantly with various protease inhibitors in combination with ritonavir. Consideration should be given both to the benefit of lipid lowering by use of Suvezen in HIV patients receiving protease inhibitors and the potential for increased rosuvastatin plasma concentrations when initiating and up titrating rosuvastatin doses in patients treated with protease inhibitors. The concomitant use with certain protease inhibitors is not recommended unless the dose of rosuvastatin is adjusted. Fibrates: The safety and efficacy of ezetimibe administered with fibrates have not been established. If cholelithiasis is suspected in a patient receiving Suvezen and fenofibrate, gallbladder investigations are indicated and therapy should be discontinued. Anticoagulants: If Suvezen is added to warfarin, another coumarin anticoagulant, or fluindione, the International Normalised Ratio (INR) should be appropriately monitored. Fusidic acid: Suvezen must not be co-administered with systemic formulations of fusidic acid or within 7 days of stopping fusidic acid treatment. In patients where the use of systemic fusidic acid is considered essential, statin treatment should be discontinued throughout the duration of fusidic acid treatment. There have been reports of rhabdomyolysis (including some fatalities) in patients receiving fusidic acid and statins in combination. The patient should be advised to seek medical advice immediately if they experience any symptoms of muscle weakness, pain or tenderness. Statin therapy may be reintroduced seven days after the last dose of fusidic acid. In exceptional circumstances, where prolonged systemic fusidic acid is needed, e.g., for the treatment of severe infections, the need for co-administration of Suvezen and fusidic acid should only be considered on a case by case basis and under close medical supervision. Suvezen contains lactose monohydrate and sodium: Patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucosegalactose malabsorption should not take this medicine. This medicinal product contains less than 1 mmol sodium (23 mg) per tablet, that is to say essentially ‘sodium-free’. Pregnancy, Breastfeeding and Fertility: No clinical data are available on the use of ezetimibe during pregnancy. Potential risk from inhibition of HMG-CoA reductase outweighs the advantage of treatment during pregnancy. If a patient becomes pregnant during use of Suvezen, treatment should be discontinued immediately. Animal studies have shown excretion of medicinal product through breast milk. However, there are no data in humans. No clinical trial data on the effects of fertility in humans. Interactions: Contraindicated combinations: Ciclosporin. Not-recommended combinations: Fibrates and other lipidlowering products, protease inhibitors, transporter protein inhibitors and fusidic acid. Other possible interactions: Cytochrome P450 enzymes, antacids, colestyramine, anticoagulants, Vitamin K antagonists, erythromycin, Oral contraceptive/hormone replacement therapy. When coadministering rosuvastatin with other medicinal products known to increase exposure to rosuvastatin, doses should be adjusted (see SPC for full details). The maximum daily dose should be adjusted so that the expected rosuvastatin exposure would not likely exceed that of a 40 mg daily dose of rosuvastatin taken without interacting medicinal products. Adverse Reactions: Adverse drug reactions previously reported with one of the individual components (ezetimibe or rosuvastatin) may be potential undesirable effects with Suvezen. Common (≥1/100 to <1/10): diabetes mellitus, headache, dizziness, constipation, nausea, abdominal pain, diarrhoea, flatulence, myalgia, ALT and/or AST increased, asthenia and fatigue. Uncommon (≥1/1,000 to <1/100): decreased appetite, paraesthesia, hot flush, hypertension, cough, dyspepsia, gastroesophageal reflux disease, nausea, dry mouth, gastritis, pruritus, rash, urticaria, arthralgia, muscle spasms, neck pain, back pain, muscular weakness, pain in extremity, ALT and/or AST increased, blood CPK increased, gamma-glutamyltransferase increased, liver function test abnormal, chest pain, pain, asthenia, oedema peripheral. Rare (≥1/10,000 to <1/1,000): thrombocytopenia, hypersensitivity reactions including angioedema, pancreatitis, increased hepatic transaminases, myopathy (including myositis), rhabdomyolysis, lupus-like syndrome and muscle rupture. Very rare (<1/10,000): polyneuropathy, memory loss, jaundice, hepatitis, arthralgia, haematuria, gynaecomastia. Not known: thrombocytopenia, hypersensitivity (including rash, urticaria, anaphylaxis and angioedema), depression, peripheral neuropathy, sleep disturbances (including insomnia and nightmares), dizziness, paraesthesia, cough, dyspnoea, diarrhoea, pancreatitis, constipation, hepatitis, cholelithiasis, cholecystitis, Stevens Johnson syndrome, erythema multiforme, immune-mediated necrotising myopathy, tendon disorders (sometimes complicated by rupture), myalgia, myopathy/rhabdomyolysis, oedema, asthenia. New single-pill combination of rosuvastatin and ezetimibe available in 3 doses*
40 mg /10 mg
Legal Category: POM. NEW 40 mg /10 mg Rosuvastatin + Ezetimibe NOW AVAILABLE
New single-pill combination of rosuvastatin and ezetimibe available in 3 doses*
Prescribing Information: Suvezen (rosuvastatin/ ezetimibe) film-coated tablets Please refer to the Summary of Product with caution in patients who consume excessive quantities of alcohol and/or have a history of liver disease. Renal effects: Proteinuria
NEW
SAIE.ZEN.19.09.0201j – December 2019 * Suvezen is available in 3 doses in Ireland. Suvezen 10mg/10mg, 20mg/10mg and 40mg/10mg: Each film-coated tablet contains 10mg; 20mg or 40mg of rosuvastatin (as rosuvastatin calcium) respectively, and 10mg ezetimibe. Reference: 1. Suvezen Summary of Product Characteristics LDL-C: Low-density lipoprotein Cholesterol Prescribing Information: Suvezen (rosuvastatin/ ezetimibe) film-coated tablets Please refer to the Summary of Product Characteristics (SPC) for full prescribing details. Presentations: Suvezen 10mg/10mg, 20mg/10mg and 40mg/10mg: Each film-coated tablet contains 10mg; 20mg or 40mg of rosuvastatin (as rosuvastatin calcium) respectively, and 10mg ezetimibe.
is indicated for substitution therapy in adult patients who are adequately controlled with rosuvastatin and ezetimibe given concurrently at the same dose level as in the fixed combination, but as separate products, as adjunct to diet for treatment of primary hypercholesterolaemia (heterozygous familial and non-familial) or homozygous familial hypercholesterolaemia. Dosage and Administration: The patient should be on and continue, an appropriate lipid-lowering diet, during treatment with Suvezen. Suvezen is not suitable for initial therapy. Treatment initiation or dose adjustment, if necessary, should only be done with the monocomponents and after setting the appropriate doses the switch to the fixed dose combination of the appropriate strength is possible. Patient should use the strength corresponding to their previous treatment. The recommended dose is one Suvezen tablet daily. To be administered at any time of the day, with or without food. The tablet should be swallowed whole with a drink of water. If co-administered with bile acid sequestrant (BAS), administration of Suvezen should occur either ≥2 hours before or ≥4 hours after administration of a BAS. Special populations: Paediatric (<18 years): Safety and efficacy has not been established. Elderly (>70 years): Starting dose of 5 mg rosuvastatin is recommended. The combination is not suitable for initial therapy. Hepatic impairment: Mild: No dosage adjustment is required. Moderate/Severe: Treatment with Suvezen is not recommended. Renal impairment: Mild: No dose adjustment is necessary. Moderate (creatinine clearance <60 ml/min): The recommended start dose is rosuvastatin 5mg. Race: The recommended start dose is rosuvastatin 5 mg for patients of Asian ancestry due to increased systemic exposure. The fixed dose combination is not suitable for initial therapy. Monocomponent preparations should be used to start the treatment or to modify the dose. Suvezen 40 mg/10 mg tablets are contraindicated in these patients. Genetic polymorphisms: In patients who are known to have specific types of genetic polymorphisms that can lead to increased rosuvastatin exposure, a lower daily dose of Suvezen is recommended. Dosage in patients with pre-disposing factors to myopathy: The recommended start dose is rosuvastatin 5mg in patients with predisposing factors to myopathy. Suvezen 40 mg/10 mg tablets are contraindicated in some of these patients. Concomitant therapy: The risk of myopathy (including rhabdomyolysis) is increased when Suvezen is administered concomitantly with certain medicinal products that may increase the plasma concentration of rosuvastatin (e.g. ciclosporin and certain protease inhibitors including combinations of ritonavir with atazanavir, lopinavir, and/or tipranavir). Whenever possible, alternative medications should be considered, and, if necessary, consider temporarily discontinuing Suvezen therapy. In situations where coadministration of these medicinal products with Suvezen is unavoidable, the benefit and the risk of concurrent treatment and rosuvastatin dosing adjustments should be carefully considered. Contraindications: Hypersensitivity to the active substances or excipients. Pregnancy, breast-feeding and in women of childbearing potential not using appropriate contraceptive measures. Active liver disease or any serum transaminase elevations which are unexplained, persistent or exceeding 3x the upper limit of normal (ULN). Severe renal impairment (creatinine clearance <30 ml/min); myopathy or receiving concomitant ciclosporin. 40mg/10mg dose contraindicated in patients with predisposing factors for myopathy/rhabdomyolysis; such factors include: Moderate renal impairment (creatinine clearance <60 ml/min), hypothyroidism, personal or family history of hereditary muscular disorders, previous history of muscular toxicity with another HMGCoA reductase inhibitor or fibrate, alcohol abuse, situations where an increase in plasma levels of rosuvastatin may occur, Asian patients, concomitant use of fibrates. Precautions and Warnings: Skeletal muscle effects: have been reported in rosuvastatintreated patients with all doses and in particular with doses >20 mg. As with other HMG-CoA reductase inhibitors, reporting rate for rhabdomyolysis is associated with use at doses >40mg. Post-marketing experience with ezetimibe, cases of myopathy and rhabdomyolysis have been reported. If myopathy is suspected based on muscle symptoms or is confirmed by a creatine phosphokinase (CPK) level, Suvezen and any of these other agents that the patient is taking concomitantly should be immediately discontinued. All patients starting therapy with Suvezen should be advised of the risk of myopathy and told to report promptly any unexplained muscle pain, tenderness or weakness, particularly if associated with malaise or fever. Creatine kinase (CK) measurement: CK should not be measured following strenuous exercise or in the presence of a plausible alternative cause of CK increase. If CK levels are significantly elevated at baseline (>5xULN) a confirmatory test should be carried out within 5-7 days. If the repeat test confirms a baseline CK >5xULN, treatment should not be started. Patients with pre-disposing factors for myopathy/rhabdomyolysis: Caution should be exercised in these patients. Risk: benefit of treatment should be considered and clinical monitoring is recommended. CK levels should be measured in these patients. Therapy should be discontinued if CK levels are markedly elevated (>5xULN) or if muscular symptoms are severe and cause daily discomfort. If symptoms resolve and CK levels return to normal, then consideration should be given to re-introducing treatment at the lowest dose. Immune-mediated necrotising myopathy (IMNM): Clinically characterised by proximal muscle weakness and elevated serum CK, has been reported very rarely during or after treatment with statins, including rosuvastatin, despite discontinuation of statin treatment. In clinical trials an increase in the incidence of myositis and myopathy has been seen in patients receiving other HMG-CoA reductase inhibitors together with fibric acid derivatives. Suvezen should not be used in any patient with an acute, serious condition suggestive of myopathy or predisposing to the development of renal failure secondary to rhabdomyolysis (e.g. sepsis, hypotension, major surgery, trauma, severe metabolic, endocrine and electrolyte disorders; or uncontrolled seizures). Liver effects: In controlled coadministration trials in patients receiving ezetimibe with statin, consecutive transaminase elevations ≥3×ULN have been observed. It is recommended that liver function tests be carried out prior to, and 3 months following, the initiation of treatment. Rosuvastatin should be discontinued or the dose reduced if the level of serum transaminases is ≥3xULN. The reporting rate for serious events is higher at the 40mg dose. In patients with secondary hypercholesterolaemia caused by hypothyroidism or nephrotic syndrome, the underlying disease should be treated prior to initiating therapy with rosuvastatin. Liver disease and alcohol: As with other HMG-CoA reductase inhibitors, rosuvastatin should be used Marketing Authorisation Numbers: 10mg/10mg: PA0540/193/001; 20mg/10mg: PA0540/193/002; 40mg/10mg: PA0540/193/003. Marketing Authorisation Holder: Sanofi-Aventis Ireland Ltd. T/A SANOFI, Citywest Business Campus, Dublin 24, Ireland. Further information is available from: Sanofi, 18 Riverwalk, Citywest Business Campus, Dublin 24 or contact IEmedinfo@sanofi.com Tel.: (01) 4035600. Date of Preparation: December 2019. Adverse events should be reported. Reporting forms and information can be found at www.hpra.ie; email: medsafety@hpra.ie Adverse events should also be reported to Sanofi Ireland Ltd. Tel: 01 403 5600. Alternatively, send via email to IEPharmacovigilance@sanofi.com
Irish Cardiac Society, 71st Annual Scientific Meeting, 1-3 October 2020

The ‘Jekyll and Hyde’ of atherosclerosis
In a session chaired by Dr Ian Menown, Consultant Cardiologist and Director of Invasive Cardiology at the Craigavon Cardiac Centre, Co Armagh, attendees at the conference heard a presentation from Prof Alberto Zambon, Director at the Lipoprotein Core Laboratory, Centre for Atherosclerosis Prevention and Treatment, Department of Medicine, University of Padua, Italy. Prof Zambon spoke on the topic of ‘Triglycerides in Atherosclerosis: A Strange Case of Dr Jekyll and Mr Hyde’.
“It’s a strange story, because if we look at lipoproteins, we have a clear idea of the lipoproteins that are dangerous for our arteries,” said Prof Zambon. “But then we have a range of proteins where we are not exactly sure what they do – are they bad or good, do they do anything or do something?” In his presentation, Prof Zambon focused on the mild-to-mod -
erate range of triglycerides in the range of 2-to-10mmol/L not associated with increased risk of pancreatitis, but with an increased risk of cardiovascular disease.
“Triglycerides might not be dangerous, but the cholesterol in the triglyceride-rich lipoproteins is what drives the results in
these studies and that is the reason why once you adjust for the cholesterol inside the lipoprotein, the risk [of coronary heart disease] is flattened.”
Prof Zambon presented a range of studies on the topic to illustrate his point and explained that the cause of ischaemic heart disease is not triglycerides by themselves, but “it is the cholesterol inside the triglyceride-rich lipoproteins that counts. That is why when you adjust for it, the effect of triglycerides is gone”.
‘Pears and apples’ He provided an overview of the results of studies on the genetics and pathophysiology of coronary heart disease, telling the conference: “Comparing triglyceride-rich lipoproteins and LDL is like comparing pears and apples, but they share one common feature – each of these lipoproteins contains one molecule of LDL.”
Prof Zambon told the attendees: “I believe there is plenty of evidence and robust data to suggest that triglycerides are the ‘Mr Hyde’ of lipoproteins, not the ‘Dr Jekyll’. Raised triglyceride
The evolution of catheter ablation
The next presenter in the Saturday morning session was Dr Ed Cronin, Associate Professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, US, who addressed the meeting on the topic ‘Catheter ablation of ventricular arrhythmias’. Dr Cronin provided an overview of the history of the development of ablation in ventricular tachycardia since the first procedure in 1982, as well as case studies and highly-cited papers, which he has authored, including the global consensus document 2019 HRS/EHRA/APHRS/LAHRS Expert Consensus Statement on Catheter Ablation of Ventricular Arrhythmias.
Dr Cronin also outlined the process of drafting a recommendation and stressed how “this process is very detailed, because every single word has to mean exactly what you want it to mean” and involves meetings, redrafting, consensus, and eventually a voting process. “It’s easy to criticise clinical documents, but it’s a lot harder to write them,” he told the meeting.
Future advances
Dr Cronin touched on potential future advances in the medium term for VT ablation. “There are two things that deserve particular mention,” he told the conference. “The first is electroporation, or pulse field ablation, which has been very exciting for atrial fibrillation. It’s a little

ironic because it harkens back to DC current ablation; it is essentially the same energy, but delivered in a very different way and in a very controlled way compared to the first VT ablation 38 years ago. These catheters… were actually designed for atrial fibrillation ablation and I think it’s something we are going to be using for atrial fibrillation before too long, and routinely for pulmonary vein isolation. It’s really nicely positioned for that application because the left atri -
tinued. “It might be useful for areas like the LV summit that might be anatomically challenging, where there are coronary arteries in the way, etc. The other area it might be used for is large-scale substrate ablation in the LV, which would probably be very useful, because ablation lesions in the LV, especially in scar, are actually not terribly effective at the moment. At best, they are about 5mm deep and we have not seen a reduction in LV function with catheter abla -
concentration is likely a marker of cholesterol – remember, we are always talking about how cholesterol carried in triglyceride-rich lipoproteins is indeed a causal risk factor for cardiovascular disease and keep in mind, one triglyceride-rich lipoprotein is as atherogenic for your arteries as one LDL.”
Prof Zambon concluded: “Available evidence suggests that the inflammatory components of the plaque in atherosclerosis are indeed modulated by the triglyceride-rich lipoproteins. I have shown that plaque regression seems to be greater when both LDL-C and TG plasma levels are controlled or at their goals and at near-optimal LDL-C levels, short- to medium-term risk of cardiovascular events remains high when triglycerides are high, particularly higher than 2 or 2.5mmol. There are studies showing that approaching, on top of LDL-C, using triglyceride-lowering agents effectively reduces cardiovascular risk in patients with elevated triglycerides.”
al myocardium is very thin and there are structures around it like the oesophagus that are very important and that you want to protect. Pulse field ablation can be very tissue-specific, so you can injure only cardiac tissue and not oesophageal tissue.
“For VT ablation, first of all for focal VTs, the existing radiofrequency catheters are very good, so they would have to design a new catheter,” Dr Cronin con -
tion in VT… part of the reason is probably that abrasion lesions are not that big or deep anyway, so we would find it hard to cause a reduction in LV function.”
Imaging
Dr Cronin explained that his concern in pulsed-field ablation in that setting is that it is possible to create very large lesions with this technology, “and that’s something we have to be very careful of”. He

also spoke about non-invasive radio ablation for VT.
“The idea is that you image the patient, perhaps do an EP [electrophysiology] study for induction or perhaps even mapping of VT, often in the context of a prior ablation that has been unsuccessful, and you fuse these different imaging modalities,” which would include a CT scan, to build an anatomical model of the heart to highlight areas to be treated, said Dr Cronin. These areas are then treated with radi-
ation therapy via a standard radiation scanner.
“This is obviously a very novel use [of this technology], and I would say it seems to be very complex to do and there are a lot of steps to it. There are also questions over radiation and toxicity and whether this could cause problems such as coronary stenosis, lung damage or other tissue damage over time. But there are some very exciting results and there is a lot to learn,” Dr Cronin concluded.
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 34
Conference Coverage
I believe there is plenty of evidence and robust data to suggest that triglycerides are the ‘Mr Hyde’ of lipoproteins, not the ‘Dr Jekyll’
Pulse field ablation can be very tissue-specific, so you can injure only cardiac tissue and not oesophageal tissue
Prof Alberto Zambon
Dr Ed Cronin
Entresto ® is indicated in adult patients for treatment of symptomatic chronic heart failure with reduced ejection fraction. HFrEF=heart failure with reduced ejection fraction.

ABBREVIATED PRESCRIBING INFORMATION - ▼ Entresto film-coated tablets
This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 of the SmPC for how to report adverse reactions. Please refer to Summary of Product Characteristics (SmPC) before prescribing. Presentation: Film-coated tablets of 24 mg/26 mg, 49 mg/51mg and 97 mg/103 mg of sacubitril and valsartan respectively (as sacubitril valsartan sodium salt complex). Indications: In adult patients for treatment of symptomatic chronic heart failure with reduced ejection fraction. Dosage and administration: The recommended starting dose of Entresto is one tablet of 49 mg/51 mg twice daily, doubled at 2-4 weeks to the target dose of one tablet of 97 mg/103 mg twice daily, as tolerated by the patient. In patients not currently taking an ACE inhibitor or an ARB, or taking low doses of these medicinal products, a starting dose of 24 mg/26 mg twice daily and slow dose titration (doubling every 3 - 4 weeks) are recommended. A starting dose of 24 mg/26 mg twice daily should be considered for patients with SBP ≥100 to 110 mmHg, moderate or severe renal impairment (use with caution in severe renal impairment) and moderate hepatic impairment. Do not co-administer with an ACE inhibitor or an ARB. Do not start treatment for at least 36 hours after discontinuing ACE inhibitor therapy. Entresto may be administered with or without food. The tablets must be swallowed with a glass of water. Contraindications: Hypersensitivity to the active substances or to any of the excipients. Concomitant use with ACE inhibitors. Do not administer until 36 hours after discontinuing ACE inhibitor therapy. Known history of angioedema related to previous ACE inhibitor or ARB therapy. Hereditary or idiopathic angioedema. Concomitant use with aliskiren-containing medicinal products in patients with diabetes mellitus or in patients with renal impairment (eGFR <60 ml/min/1.73 m2). Severe hepatic impairment, biliary cirrhosis and cholestasis. Second and third trimester of pregnancy. Warnings/
Precautions: Dual blockade of the renin angiotensin-aldosterone system (RAAS): Combination with an ACE inhibitor is contraindicated due to the increased risk of angioedema. Entresto must not be initiated until 36 hours after taking the last dose of ACE inhibitor therapy. If treatment with Entresto is stopped, ACE inhibitor therapy must not be initiated until 36 hours after the last dose of Entresto. Combination of Entresto with direct renin inhibitors such as aliskiren is not recommended. Entresto should not be co administered with another ARB containing product. Hypotension: Treatment should not be initiated unless SBP is ≥100 mmHg. Patients with SBP <100 mmHg were not studied. Cases of symptomatic hypotension have been reported in patients treated with Entresto during clinical studies, especially in patients ≥65 years old, patients with renal disease and patients with low SBP (<112 mmHg). Blood pressure should be monitored routinely when initiating or during dose titration with Entresto. If hypotension occurs, temporary down-titration or discontinuation of Entresto is recommended. Impaired or worsening renal function: Limited clinical experience in patients with severe renal impairment (estimated GFR <30 ml/min/1.73m2). There is no experience in patients with end-stage renal disease and use of Entresto is not recommended. Use of Entresto may be associated with decreased renal function, and downtitration should be considered in these patients. Hyperkalaemia: Entresto should not be initiated if the serum potassium level is >5.4 mmol/l.
Monitoring of serum potassium is recommended, especially in patients who have risk factors such as renal impairment, diabetes mellitus or hypoaldosteronism or who are on a high potassium diet or on mineralocorticoid antagonists. If clinically significant hyperkalaemia occurs, consider adjustment of concomitant medicinal products or temporary down-titration or discontinuation of Entresto. If serum potassium level is >5.4 mmol/l discontinuation should be considered. Angioedema: Angioedema has been reported with Entresto. If angioedema occurs, discontinue Entresto immediately and provide appropriate therapy and monitoring until complete and sustained resolution of signs and symptoms has occurred. Entresto must not be re administered. Patients with a prior history of angioedema were not studied. As they may be at higher risk for angioedema, caution is recommended if Entresto is used in these patients. Black patients have an increased susceptibility to develop angioedema. Patients with renal artery stenosis: Caution is required and monitoring of renal function is recommended. Patients with NYHA functional
classification IV: Caution should be exercised due to limited clinical experience in this population. Patients with hepatic impairment: There is limited clinical experience in patients with moderate hepatic impairment (Child Pugh B classification) or with AST/ALT values more than twice the upper limit of the normal range. Caution is therefore recommended in these patients. B-type natriuretic peptide (BNP): BNP is not a suitable biomarker of heart failure in patients treated with Entresto because it is a neprilysin substrate. Interactions: Contraindicated with ACE inhibitors, 36 hours washout is required. Use with aliskiren contraindicated in patients with diabetes mellitus or in patients with renal impairment (eGFR <60 ml/min/1.73 m2). Should not be co-administered with another ARB. Use with caution when co-administering Entresto with statins or PDE5 inhibitors. No clinically relevant drug-drug interaction was observed when simvastatin and Entresto were co-administered. Monitoring serum potassium is recommended if Entresto is co-administered with potassium-sparing diuretics or substances containing potassium (such as heparin). Monitoring renal function is recommended when initiating or modifying treatment in patients on Entresto who are taking NSAIDs concomitantly. Interactions between Entresto and lithium have not been investigated. Therefore, this combination is not recommended. If the combination proves necessary, careful monitoring of serum lithium levels is recommended. Co-administration of Entresto and furosemide reduced Cmax and AUC of furosemide by 50% and 28%, respectively, with reduced urinary excretion of sodium. Co-administration of nitroglycerin and Entresto was associated with a treatment difference of 5 bpm in heart rate compared to the administration of nitroglycerine alone, no dose adjustment is required. Co-administration of Entresto with inhibitors of OATP1B1, OATP1B3, OAT3 (e.g. rifampicin, ciclosporin), OAT1 (e.g. tenofovir, cidofovir) or MRP2 (e.g. ritonavir) may increase the systemic exposure of LBQ657 or valsartan. Appropriate care should be exercised. Co-administration of Entresto with metformin reduced both Cmax and AUC of metformin by 23%. When initiating therapy with Entresto in patients receiving metformin, the clinical status of the patient should be evaluated. Fertility, pregnancy and lactation: The use of Entresto is not recommended during the first trimester of pregnancy and is contraindicated during the second and third trimesters of pregnancy. It is not known whether Entresto is excreted in human milk, but components were excreted in the milk of rats. Entresto is not recommended during breastfeeding. A decision should be made whether to abstain from breast feeding or to discontinue Entresto while breast feeding, taking into account the importance of Entresto to the mother. Adverse reactions: Very common: Hyperkalaemia, hypotension, renal impairment. Common: Anaemia, hypokalaemia, hypoglycaemia, dizziness, headache, syncope, vertigo, orthostatic hypotension, cough, diarrhoea, nausea, gastritis, renal failure, acute renal failure, fatigue, asthenia. Uncommon: Hypersensitivity, postural dizziness, pruritis, rash, angioedema. Please refer to SmPC for a full list of adverse events for Entresto. Legal Category: POM. Pack sizes: Entresto 24 mg/26 mg - 28 tablet pack; Entresto 49 mg/51 mg - 28 and 56 tablet pack; Entresto 97 mg/103 - 56 tablet pack. Marketing Authorisation Holder: Novartis Europharm Limited, Vista Building, Elm Park, Merrion Road, Dublin 4, Ireland. Marketing Authorisation Numbers: Entresto 24 mg/26 mg film coated tablets EU/1/15/1058/001; Entresto 49 mg/51 mg film coated tablets EU/1/15/1058/002-003; Entresto 97 mg/103 mg film coated tablets EU/1/15/1058/006. Full prescribing information is available on request from Novartis Ireland Ltd, Vista Building, Elm Park Business Park, Merrion Road, Dublin 4. Tel: 01 2601255 or at www. medicines.ie Date of Creation of API Text: May 2018.
This medicinal product is subject to additional monitoring. Reporting suspected adverse reactions of the medicinal product is important to Novartis and the HPRA. It allows continued monitoring of the benefit/risk profile of the medicinal product. All suspected adverse reactions should be reported via www.hpra.ie or email to medsafety@hpra.ie. Adverse events could also be reported to Novartis preferably via www.report.novartis.com or by email: drugsafety.dublin@novartis.com or by calling 01 2080 612.
REFERENCES: 1. Velazquez EJ, Morrow DA, DeVore AD, et al. Angiotension-Neprilysin Inhibition in Acute Decompensated Heart Failure [published correction appears in N Engl J Med. 2019 Mar 14;380(11):1090]. N Engl J Med. 2018;380(6):539-548. Doi: 10.1056/NEJM0a1812851. 2. DeVore AD, Braunwald E, Morrow DA, et al. Initiation of Angiotensin-Neprilysin Inhibition After Acute Decompensated Heart Failure: Secondary Analysis of the Open-label Extension of the PIONEER-HF Trial. JAMA Cardiol. 2020;5(2):202–207. doi:10.1001/jamacardio.2019.4665. 3. Claggett B, Packer M, McMurray JJV, et al; for the PARADIGM-HF Investigators. Estimating the long-term treatment benefits of sacubitril–valsartan. N Engl J Med. 2015;373(23):2289-2290. 4. Lewis EF, Claggett BL, McMurray JJV, et al. Health-related quality of life outcomes in PARADIGM-HF. Circ Heart Fail. 2017;10(8):e003430. 5. ENTRESTO® Summary of product characteristics (SmPC) available at www.medicines.ie 6. McMurray JJV, Packer M, Desai AS, et al; for the PARADIGM-HF Investigators and Committees; Angiotensin-neprilysin inhibtion versus Enalapril in heart failure. N Engl J Med. 2014;371(11):993-1004.
March 2020 | IE02/ENT20-CNF013
Irish Cardiac Society, 71st Annual Scientific Meeting, 1-3 October 2020

Strong range of virtual presentations at 2020 conference
The always highly-anticipated Brian Maurer Young Investigator Award, supported by Servier, this year featured a varied range of speakers and topics, ranging from ventricular arrhythmia to PCSK9 inhibition. This year’s judging panel comprised Prof Jim Crowley, President, ICS; Prof Albert McNeill, Past-President, ICS; and Prof Ken McDonald, Past-President, ICS.
The finalist presenters and their topics were: Dr Ailis Pollock, St James’s Hospital, Dublin, on ‘Covid-19 and QTc: Is hydroxychloroquine worth the risk? A review of QT prolongation in hospitalised Covid-19 patients treated with hydroxychloroquine and azithromycin’.
Dr Max Waters, Tallaght University Hospital, Dublin, Ireland, then delivered a presentation on ‘A hierarchal analysis of eligibility for PCSK9 inhibition in Ireland: Bridging the divide between the NCPE managed access protocol and ESC/EAS guidelines’.
Next to present was Dr Angela McInerney, Cardiovascular Institute, Hospital Clínico San Carlos, IdISSC, Madrid, Spain, on ‘Impact of morbid obesity and obesity phenotype on outcomes post-transcatheter aortic valve replacement’.
The final presentation was delivered by Dr Bronagh Kelly, Adult Congenital Heart Disease Department, Royal Victoria Hospital, Belfast, Northern Ireland, who presented her observations on ‘Predictors of ventricular arrhythmia identified from follow-up of tetralogy of fallot’.
Perspectives on heart failure
Due to the virtual nature of this year’s ICS Scientific Meeting, attendance was increased compared to previous years and delegates had access to oral abstracts, general posters and moderated posters that covered all aspects of cardiology, from valve replacement and balloon angioplasty, to cardiac toxicity and hypertension, as well as a range of other specialist subjects.
Several abstracts and posters also presented data on various aspects of heart failure (HF). One of the poster presentations by Drs Ronan Cusack, Avinash Radhakrishna and John Barton of the Department of Cardiology at University Hospital Galway was titled ‘Treatment of heart failure in 2020: CHAMPs or Chumps?’
The authors conducted an audit of prescribing trends in a tertiary referral centre at University Hospital Galway, within a specialist-led heart failure outpatient clinic service “to evaluate our performance in comparison to these large studies”. In their conclusion, the authors noted: “Despite the strong body of evidence underpinning GDMT, gaps in prescribing habits still exist with specialist heart failure outpatient services.”
low-up period of 17.5 months, and there was no difference in mean hospitalisations for ADHF between the groups. In our catchment area, our HFmrEF have a similar phenotype to our HFpEF and HFrEF cohorts.”
Among the other presentations focused on HF was an oral presentation by Ms Loreena Hill, Lecturer in the School of Nursing and Midwifery at Queen’s University Belfast, on ‘Heart failure patient and caregiver needs and expectations regarding self-management via digital health – the PASSION-HF project’. Ms Hill and colleagues sought to assess the needs and requirements of HF patients and their informal caregivers in regard to a virtual doctor. The study was conducted against the backdrop that HF healthcare services are not sufficient to meet the needs of an ageing population with increasing comorbidities and disease complexity, together with the unequal distribution of medical care in ru-
During his closing comments at the conference, Prof Crowley announced that the winner of this year’s award was Dr Angela McInerney.
The Intervention Case Competition, held on the Friday evening of the conference and supported by AstraZeneca, also saw an extremely
high standard of presentations and was chaired by Prof Aaron Peace and Prof Tom Kiernan. The evening saw four presentations: Dr Jack Laffan on the topic ‘It’s stuck again: Retrieval of a retrograde equipment lodged in a vein graft during CTO angioplasty’; Dr Angela McInerney on ‘IVUS-guided management of iatrogenic right coronary artery dissection’; Dr William Gibson and Dr Stephen O’Connor on ‘Transcatheter aortic valve implantation reverses haemolytic anaemia in the setting of previous transcatheter mitral paravalvular leak closure’; and Dr Christopher Balfe on ‘A narrow escape from a coronavirus Covid-19 mimic’: First presentation of severe mitral stenosis and pneumonia during the coronavirus pandemic’.
The judging panel noted the high standard of all the presentations and decided that the winner was Dr Angela McInerney. “The originality and complexity of these cases was fantastic and there was great educational content in all the presentations,” said Prof Aaron Peace in his closing remarks.
It was also announced at the meeting that the recipient of the Brian McGovern Scholarship this year was Dr Sean Fitzgerald. The organisers commented: “We were very fortunate this year, thanks to the continued support of Daiichi Sankyo, to be in position to award the Brian McGovern Scholarship once again and I am delighted to announce that the 2020 Brian McGovern Recipient is Dr Sean Fitzgerald,” said the ICS in an announcement. “Dr Fitzgerald has recently commenced an lnterventional Cardiology Fellowship at the Heart Centre Leipzig at the University of Leipzig, Germany, comprising both clinical and research components under the supervision of Prof Helger Thiele and we look forward to receiving his update at next year’s meeting.”

They observed that despite compelling evidence, there is low usage of SGLT2 inhibitors and this “is likely explained in part [due] to the lack of established guidelines on its optimal use within treatment algorithms. We would expect this to be addressed in the next update to the European Cardiology Society (ESC) Guidelines for Acute and Chronic Heart Failure.”
Another poster presentation entitled ‘A review of patients with heart failure with mid-range ejection fraction (HFmrEF): Comorbidities and outcomes’ was delivered by researchers from the Department of Cardiology, St James’s Hospital, Dublin.
The researchers sought to compare the comorbidities of HFmrEF patients with those of HFpEF and HFrEF patients, and aimed to compare hospitalisations for acute decompensation HF, and mortality between these groups. The participants comprised 286 new patients referred to one of three HF clinics. In their conclusion, the authors wrote: “In our cohort of annual referrals to our three HF clinics, comorbidities were similar in HFmrEF as compared with HFpEF and HFrEF, aside from previous CABG surgery (in which there were fewer in HFmrEF as compared with HFpEF and HFrEF) and HTN (of which there were more in HFpEF). There was a numerically higher proportion of devices in the HFrEF group.
“Mortality was similar across the three groups over our fol-
ral and urban regions. Taken together, these factors have resulted in an imminent need to identify alternative healthcare approaches, said Ms Hill.
Using an exploratory mixed-method study within The Netherlands, UK, Ireland, and Germany, qualitative, guided interviews were supplemented by a standardised questionnaire in the study. In their conclusions, the authors wrote: “Patients want reassurance 24/7, independently of the availability of healthcare services, combined with personalised medical advice regarding day-to-day management of their HF. In a next step, we are planning a multi-centre clinical trial to test the first prototype of the e-health product (DoctorMe).”
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 36
Conference Coverage
The originality and complexity of these cases was fantastic and there was great educational content in all the presentations
Prof Jim Crowley
Despite the strong body of evidence underpinning GDMT, gaps in prescribing habits still exist with specialist heart failure outpatient services
® difference
Ferinject®
makes a real difference to patients
consider patients with capacity, tolerability number
difference patients
Ferinject (ferric carboxymaltose) makes a real difference to patients
Ferinject® is indicated for the treatment of iron deficiency: when oral preparations are ineffective, oral iron preparations cannot be used, or there is a clinical need to deliver iron rapidly. The diagnosis of iron deficiency must be based on laboratory tests.
ESC
0.9% m/V NaCl but not diluted to Step 3: Post-iron repletion assessments. Ferinject or any of its excipients. parenteral iron products. Anaemia overload or disturbances in utilisation
precautions: Parenterally administered iron anaphylactic/anaphylactoid reactions. known allergies, a history of severe and in patients with immune or reports of hypersensitivity reactions (acute allergic coronary arteriospasm Ferinject should only be administered manage anaphylactic reactions where full (including 1:1000 adrenaline solution). minutes following administration. If intolerance occur during administration, immediately. Parenterally administered iron hypophosphataemia which in most cases is transient of hypophosphataemia requiring in patients with existing risk factors high-dose intravenous iron. In patients with only be administered after careful monitoring of iron status is recommended to data on the use of single doses of more haemodialysis-dependent chronic kidney disease patients. in case of acute or chronic infection, recommended that treatment with ongoing bacteraemia. In patients with
stepwise approach: Step 1: Determination of the iron need; The individual iron need for repletion using Ferinject is determined based on the patient’s body weight and haemoglobin (Hb) level. The table in the SmPC should be used to determine the iron need. Step 2: Calculation and administration of the maximum individual iron dose(s); Based on the iron need determined, the appropriate dose(s) of Ferinject should be administered: A single Ferinject administration should not exceed: • 15 mg iron/kg body weight (for administration by intravenous injection) or 20 mg iron/kg body weight (for administration by intravenous infusion) The maximum recommended cumulative dose of Ferinject is 1,000 mg of iron (20 mL Ferinject) per week. Administration rates for intravenous injection: For iron doses of 100mg to 200mg, there is no prescribed administration time. For doses >200mg to 500mg, Ferinject should be administered at a rate of 100mg iron/min. For doses >500mg to 1,000mg, the minimum administration time is 15 min. Administration of intravenous drip infusion: For iron doses of 100mg to 200mg, there is no prescribed administration time. For doses >200mg to 500mg, Ferinject should be administered in a minimum of 6 mins. For doses >500mg to 1,000mg, the minimum administration time is
The 2016 ESC guidelines recommend to consider ferric carboxymaltose in symptomatic patients with HFrEF and iron deficiency1
15 mins. Ferinject must be diluted in 0.9% m/V NaCl but not diluted to concentrations less than 2 mg iron/mL. Step 3: Post-iron repletion assessments. Contraindications:
Known serious hypersensitivity to other parenteral iron products. Anaemia not attributed to iron deficiency. Iron overload or disturbances in utilisation of iron. Special warnings and precautions: preparations can cause potentially fatal anaphylactic/anaphylactoid reactions.
The risk is enhanced for patients with known allergies, a history of severe asthma, eczema or other atopic allergy, and in patients with immune or inflammatory conditions. There have been reports of hypersensitivity reactions which progressed to Kounis syndrome (acute allergic coronary arteriospasm that can result in myocardial infarction). Ferinject should only be administered in the presence of staff trained to manage anaphylactic reactions where full resuscitation facilities are available (including 1:1000 adrenaline solution).



chronic infection a benefit/risk evaluation has to be performed. Caution should be exercised to avoid paravenous leakage when administering Ferinject. Special populations: not be exceeded in haemodialysis-dependent chronic kidney disease patients. The use of Ferinject has not been studied in children. A careful risk/benefit evaluation is required before use during pregnancy. Ferinject should not be used during pregnancy unless clearly necessary and should be confined to the second and third trimester. Foetal bradycardia may occur during administration of parenteral irons, as a consequence of hypersensitivity. The unborn baby should be carefully monitored during administration to pregnant women. Undesirable effects: headache, dizziness, flushing, hypertension, nausea, injection/infusion site reactions. Rare (≥1/10,000 to <1/1,000): Anaphylactoid/anaphylactic reactions. Frequency not known: Kounis syndrome. Please consult the SmPC in relation to other undesirable effects.
Date of Authorisation:
Boieldieu, Tour Franklin La Défense 8, 92042 Paris La Défense Cedex, France
Ferinject® improves symptoms: functional capacity, QoL and NYHA class2 Ferinject® offers a well-characterised tolerability
Ferinject® is a registered trademark
Document number: IE-FCM-2000075
Each patient should be observed for 30 minutes following administration. If hypersensitivity reactions or signs of intolerance occur during administration, the treatment must be stopped immediately. Parenterally administered iron preparations can cause hypophosphataemia which in most cases is transient and without clinical symptoms. Cases of hypophosphataemia requiring medical attention were reported, mainly in patients with existing risk factors and after prolonged exposure to high-dose intravenous iron. In patients with liver dysfunction, parenteral iron should only be administered after careful risk/benefit assessment. Careful monitoring of iron status is recommended to avoid iron overload. There is no safety data on the use of single doses of more than 200mg iron in haemodialysis-dependent chronic kidney disease patients. Parenteral iron must be used with caution in case of acute or chronic infection, asthma, eczema or atopic allergies. It is recommended that treatment with Ferinject is stopped in patients with ongoing bacteraemia. In patients with ESC, European Society of Cardiology; HFrEF: heart failure with reduced ejection fraction; NYHA, New York Heart Association; QoL, quality of life.
Date of preparation: 07/20
Adverse events should be reported. Reporting forms and information can be found at: https://www.hpra.ie/.
Adverse events should also be reported to Vifor Pharma UK Ltd.
Email: medicalinfo_UK@viforpharma.com
a number
profile from clinical experience
of therapeutic areas3–5
® (ferric carboxymaltose)
across
Ferinject
Ferinject® is a registered trademark. IE-FCM-2000119. Date of preparation: October 2020. Ferinject® (ferric carboxymaltose) Prescribing Information – Ireland For full prescribing information refer to the Summary of Product Characteristics (SmPC) Active ingredient: Ferric carboxymaltose (50mg/mL) Presentation: Solution for injection/infusion. Available as a 10mL vial (as 500mg of iron) and 20mL vial (as 1000mg of iron). Indication: Treatment of iron deficiency when oral iron preparations are ineffective or cannot be used or if there is a clinical need to deliver iron rapidly. The diagnosis must be based on laboratory tests. Dosage and Administration: The posology of Ferinject follows a
References: 1. Ponikowski P et al. Eur Heart J 2016;37:29–200. 2. Ponikowski P et al. Eur Heart J 2015;36;657–68. Characteristics. 4. Funk F et al. Arzneimittelforschung 2010;60(6a):345–53. 5. Vifor Pharma, Data on File 118.
Association; QoL, quality of life. Ferinject® Summary of Product
carboxymaltose) makes a real
therapeutic areas3–5
guidelines recommend to consider carboxymaltose in symptomatic patients with iron deficiency1 improves symptoms: functional capacity, NYHA class2 offers a well-characterised tolerability clinical experience across a number
Conference Coverage
Irish Cardiac Society, 71st Annual Scientific Meeting, 1-3 October 2020

Putting together the pieces of the cardiology ‘jigsaw’
Closing the 2020 meeting, outgoing ICS President Prof Jim Crowley told the attendees: “It has been both an honour and a privilege to serve my term as President of the ICS. This last year has been unprecedented because of the pandemic and has brought a lot of challenges to the Society, but I think the Society has performed an important role in helping both my colleagues as consultants, and also the trainees in responding to the pandemic. The Society has helped in continuing to highlight the cardiology needs of society in general and I hope this is going to be a continuing role for the Society in years to come.”
Prof Crowley continued: “We remain committed to supporting members and expanding our work and my sincere thanks goes to every member of the board, and indeed many of my colleagues over the past two years, for giving
their support, engagement and free time to this organisation. It is now my great pleasure to hand over to Prof Vincent Maher, who will guide the Society for the next two years until 2022.”
Prof Maher closed-out the meeting by expressing his hopes for the immediate future of the Society and he paid tribute to the outgoing President and council, also revealing the incoming members who will serve on it for the next two years. “This is a great honour,” said Prof Maher. “I’m really feeling privileged to be the President of this wonderful Society and I feel like I am standing on the shoulders of giants… these are very challenging times and I am so proud of everyone’s work in producing this great conference.”
Benefits and drawbacks
Prof Maher also touched on the drawbacks and benefits
of having this year’s meeting on a virtual basis. “While we miss our social interactions, there have been many advantages from having the virtual events and hopefully, this time next year we may have a combination of that, or at least get back to some of the previous interactions we had,” he said.
Describing Prof Crowley as a “wonderful leader”, Prof Maher said: “These are unprecedented times and you, together with [Prof] Albert [McNeill] and [Prof] Ken [McDonald], brought us the Mayo Clinic experience [joint conference], you also improved our financial regulation, brought us towards full charitable status – and I am delighted that you will still be on the council to help us complete that –and you have given us a new website, so you will be a very tough act to follow.”
Prof Maher also paid tribute to Ms Barbra Dalton, Executive Administrator for the ICS and organiser of the conference: “Barbra has been such a special person for the Society,” he said. “Without your energy, enthusiasm and work ethic, we would not be as good as we are. You have worked tirelessly for the smooth running, growth and development of our Society, and for the trainees you have been like a family member.”
He also paid tribute to the work of Prof Aaron Peace and Dr Lana Dixon while they served as council members and he welcomed the new members, who include Prof Crowley; Secretary Prof Brendan McAdam; Treasurer Dr Carl Vaughan; Dr Patricia Campbell, Assistant Secretary; Dr Angie Brown, Irish Heart Foundation representative; Dr Ross Murphy and Dr Briain MacNeill as NSD representatives; and he also warmly welcomed council members Dr Deirdre Ward, Dr Christine Hughes, Mr Alastair Graham, Dr Stephen O’Connor, and Dr Peter McKavanagh. “I am honoured to work with such a strong committee,” said Prof Maher.
Reaching out to the Diaspora will enhance our knowledge, help research collaboration and increase opportunities for our trainees
‘Great picture’
Referring to this year’s lockdown, Prof Maher said one of the activities he and his family used to pass the time included completing jigsaw puzzles. “In a jigsaw, every piece has a different shape, size, and image, but when you put them all together, you get a great picture.
“Likewise, in cardiology, whether you are responsible for ensuring the quality of a diagnostic test, making a complex management decision, guiding a patient through self-directed treatment adjustment, performing a skilled, complex intervention or operation, or advising on the latest therapeutic or device – everybody is part of this cardiovascular health initiative. As with a jigsaw, every piece counts and every person is needed.”

Prof Maher said he hoped the new ICS website and new enhanced connectivity would help to connect all of Ireland’s cardiovascular talent, both at home and abroad. “Reaching out to the Diaspora will enhance our knowledge, help research collaboration and increase opportunities for our trainees.”
Prof Maher added: “We are all aware that cardiological disease processes progress for years before their final complications. Understanding, for example, how valves thicken, hearts stiffen, conduction systems weaken, and atherosclerosis progresses – the more we understand and the more we can intervene and delay these processes, the more we may even reverse the disease in some instances. I hope someday we may have a symposium to address these issues.”
Finally, Prof Mahon acknowledged the role of industry in the conference, “without whom we would not be able to do this… and I hope that we will enjoy better times in the future to interact.”
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 38
Free CPD – now accessible on android, iPhone and tablet Check your answer against the latest module on doctorcpd.ie. Successful completion of this module will earn you 2 CPD credits Type 2 diabetes and insulin initiation was devised by Dr Caoimhe Casey and Dr Ronan Canavan, Consultant Endocrinologist, St Columcille’s Hospital and St Vincent’s University Hospital, Dublin. A B C Latest module The main risks with insulin therapy are DKA and hypoglycaemia. True or False? doctorcpd.ie Free independent CPD for Irish doctors by Irish doctors
done with the individual components. Paediatric population: should not be used.
CONTRAINDICATIONS* Dialysis patients. Patients with untreated decompensated heart failure. Severe renal impairment (Clcr < 30 mL/min). Moderate renal impairment (Clcr 30-60 mL/min) for Coverdine 10mg/2.5mg/5mg and 10mg/2.5mg/10mg. Hypersensitivity to the active substances, to other sulfonamides, to dihydropyridine derivatives, any other ACE-inhibitor or to any of the excipients. History of angioedema (Quincke’s oedema) associated with previous ACE inhibitor therapy (see Warnings section). Hereditary/idiopathic angioedema. Second and third trimesters of pregnancy (see Warnings and Pregnancy and lactation sections). Lactation (see Pregnancy and lactation section). Hepatic encephalopathy. Severe hepatic impairment. Hypokalaemia. Severe hypotension. Shock, including cardiogenic shock. Obstruction of the outflow-tract of the left ventricle (e.g. high grade aortic stenosis). Haemodynamically unstable heart failure after acute myocardial infarction. Concomitant use of Coverdine with aliskiren-containing products in patients with diabetes mellitus or renal impairment (GFR < 60mL/min/1.73m²) (see Interaction section), concomitant use with sacubitril/valsartan (see WARNING* and INTERACTIONS*), extracorporeal treatments leading to contact of blood with negatively charged surfaces (see INTERACTIONS*), significant bilateral renal artery stenosis or stenosis of the artery to a single functioning kidney (see WARNING*). WARNINGS* Special warnings: Dual blockade of the renin-angiotensin-aldosterone system (RAAS): ACE-inhibitors and angiotensin II receptor blockers should not be used concomitantly in patients with diabetic nephropathy. Neutropenia/agranulocytosis/thrombocytopenia/anaemia: caution if collagen vascular disease, immunosuppressant therapy, treatment with allopurinol or procainamide, or combination of these complicating factors, especially if pre-existing impaired renal function. Monitoring of white blood cell counts. Renovascular hypertension: increased risk of hypotension and renal insufficiency in patient with bilateral renal artery stenosis or stenosis of the artery to a single functioning kidney. Diuretics may be a contributory factor. Loss of renal function may occur (minor changes in serum creatinine) even in patients with unilateral renal artery stenosis. Hypersensitivity/angioedema, intestinal angioedema: stop treatment and monitor until complete resolution of symptoms. Angioedema associated with laryngeal oedema may be fatal. Concomitant use of mTOR inhibitors (e.g. sirolimus, everolimus, temsirolimus): patients may be at increased risk for angioedema (e.g. swelling of the airways or tongue, with or without respiratory impairment). Combination with sacubitril/valsartan (contraindicated due to the increased risk of angioedema). Sacubitril/valsartan must not be initiated until 36 hours after taking the last dose of perindopril therapy. Perindopril therapy must not be started until 36 hours after the last dose of sacubitril/valsartan. Concomitant use of other NEP inhibitors (e.g. racecadotril) and ACE inhibitors may also increase the risk of angioedema. Anaphylactoid reactions during desensitization: Caution in allergic patients treated with desensitization and avoid if venom immunotherapy. Temporarily withdrawal of ACE-inhibitor at least 24 hours before desensitization. Anaphylactoid reactions during LDL apheresis: Temporarily withholding ACE-inhibitor prior to each apheresis. Haemodialysis patients: consideration to use dialysis membranes other than high flux or antihypertensive agents other than ACE inhibitors. Primary aldosteronism: use not recommended in patients with primary hyperaldosteronism (not responding to drugs acting through inhibition of the renin-angiotensin system). Pregnancy: no initiation during pregnancy, stop treatment and start alternative therapy if appropriate. Hepatic encephalopathy: stop treatment. Photosensitivity: stop treatment. Precautions for use: Renal function: In certain hypertensive patients without pre-existing apparent renal lesions and for whom renal blood tests show renal insufficiency, stop treatment and restart at a low dose or with one constituent only. Monitoring of potassium and creatinine, after two weeks of treatment and then every two months during therapeutic stability period. If bilateral renal artery stenosis or single functioning kidney: not recommended. Risk of arterial hypotension and/or renal insufficiency (in cases of cardiac insufficiency, water and electrolyte depletion, in patients with low blood pressure, renal artery stenosis, congestive heart failure or cirrhosis with oedema and ascites): start treatment at low doses and increase progressively. Hypotension and water and sodium depletion: Risk of sudden hypotension in presence of pre-existing sodium depletion (in particular if renal artery stenosis): Monitoring of plasma electrolytes, re-establish blood volume and pressure, restart treatment at a reduced dose or with only one of the constituents. Sodium levels: More frequent monitoring in elderly and cirrhotic patients. Potassium levels: Hyperkalaemia: Monitoring of serum potassium if renal insufficiency, worsening of renal function, age (> 70 years), diabetes mellitus, intercurrent events, in particular dehydration, acute cardiac decompensation, metabolic acidosis and concomitant use of potassium-sparing diuretics, potassium supplements or potassium salts, or other drugs associated with increases in serum potassium. Hypokalaemia: high risk for elderly and/or malnourished subjects, cirrhotic patients with oedema and ascites, coronary patients, patients with renal failure or heart failure, long QT interval: monitoring of serum potassium. May favor the onset of torsades de pointes, which may be fatal. Calcium levels: hypercalcemia: stop treatment before investigating the parathyroid function. Renovascular hypertension: if renal artery stenosis: start treatment at hospital at low dose; monitor renal function and potassium. Dry cough. Atherosclerosis: start treatment at low dose in patients with ischaemic heart disease or cerebral circulatory insufficiency. Hypertensive crisis. Cardiac failure/severe cardiac insufficiency: Caution if heart failure. Severe cardiac insufficiency (grade IV): start treatment under medical supervision with reduced initial dose. Aortic or mitral valve stenosis / hypertrophic cardiomyopathy: Caution if obstruction in the outflow tract of the left ventricle. Diabetic patients: If insulin dependent diabetes mellitus, start treatment under medical supervision with reduced initial dose; monitor blood glucose during the first month and/or in the case of hypokalaemia. Black people: higher incidence of angioedema and apparently less effective in lowering blood pressure than in non-blacks. Surgery / anaesthesia: stop treatment one day before surgery. Hepatic impairment: Mild to moderate: caution. Rarely, ACE inhibitors have been associated with a syndrome that starts with cholestatic jaundice and progresses to fulminant hepatic necrosis and (sometimes) death. Stop treatment if jaundice or marked elevations of hepatic enzymes. Uric acid: hyperuricemia: Increased tendency to gout attacks. Elderly: testing of renal function and potassium levels before treatment start. Dosage increase with care. Excipients: sodium-free. INTERACTION(S)* Contraindicated: Aliskiren in diabetic or impaired renal patients, Extracorporeal treatments, Sacubitril/Valsartan. Not recommended: Lithium, Aliskiren in patients other than diabetic or impaired renal patients, Concomitant therapy with ACE inhibitor and angiotensin-receptor blocker, Estramustine, Potassium-sparing drugs (e.g triamterene,amiloride,…), Potassium salts, Co-trimoxazole (trimethoprim/sulfamethoxazole),Dantrolene (infusion), Grapefruit or grapefruit juice. Special care: Baclofen, Non-steroidal anti-inflammatory medicinal products (included acetylsalicylic acid at high doses), Antidiabetic agents (insulin, hypoglycaemic agents), Non-potassium-sparing diuretics and Potassium-sparing diuretics (eplerenone, spironolactone), Racecadotril, mTOR inhibitors (e.g. sirolimus, everolimus, temsirolimus), Torsades de pointes inducing drugs, Amphotericin B (IV route), glucocorticoids and mineralocorticoids (systemic route), tetracosactide, stimulant laxatives, Cardiac glycosides, Allopurinol, CYP3A4 inducers, CYP3A4 inhibitors. To be taken into consideration: Imipramine-like antidepressants (tricyclics), neuroleptics, other antihypertensive agents and vasodilatators, tetracosactide, Allopurinol, cytostatic or immunosuppressive agents, systemic corticosteroids or procainamide, Anaesthetic drugs, Diuretics (thiazide or loop diuretics), Gliptines (linagliptine, saxagliptine, sitagliptine, vildagliptine), Sympathomimetics, Gold, Metformin, Iodinated contrast media, Calcium (salts), Ciclosporine, Atorvastatin, digoxin, warfarin, Tacrolimus, Simvastatin. PREGNANCY AND BREASTFEEDING* Contraindicated during the second and third trimesters of pregnancy and lactation. Not recommended during the first trimester of pregnancy. FERTILITY* Reversible biochemical changes of spermatozoa in some patients treated by calcium channel blockers. DRIVE & USE MACHINES* May be impaired due to low blood pressure that may occur in some patients, especially at the start of treatment. UNDESIRABLE EFFECTS* Very common: oedema. Common: dizziness, headache, paraesthesia, vertigo, somnolence, dysgeusia, visual impairment, diplopia, tinnitus, palpitations, flushing, hypotension (and effects related to hypotension), cough, dyspnoea, abdominal pain, constipation, diarrhoea, dyspepsia, nausea, vomiting, change of bowel habit, pruritus, rash, rash maculo-papular, muscle spasms, ankle swelling, asthenia, fatigue. Uncommon: rhinitis, eosinophilia, hypersensitivity, hypoglycaemia, hyperkalaemia reversible on discontinuation, hyponatraemia, insomnia, mood altered (including anxiety), depression, sleep disorder, hypoaesthesia, tremor, syncope, tachycardia, arrhythmia (including bradycardia, ventricular tachycardia and atrial fibrillation), vasculitis, bronchospasm, dry mouth, urticaria, angioedema, alopecia, purpura, skin discoloration, hyperhidrosis, exanthema, photosensitivity reaction, pemphigoid, arthralgia, myalgia, back pain, micturition disorder, nocturia, pollakiuria, renal failure, erectile dysfunction, gynaecomastia, pain, chest pain, malaise, oedema peripheral, pyrexia, weight increased, weight decreased, blood urea increased, blood creatinine increased, fall. Rare: confusional state, blood bilirubin increased, hepatic enzyme increased, psoriasis aggravation.



Very rare: agranulocytosis, aplastic anaemia, pancytopenia, leukopenia, neutropenia, haemolytic anaemia, thrombocytopenia, allergic reactions, hyperglycaemia, hypercalcaemia, hypertonia, neuropathy peripheral, stroke possibly secondary to excessive hypotension in high-risk


patients angina pectoris, myocardial infarction, possibly secondary to excessive hypotension in high risk patients, eosinophilic pneumonia, gingival hyperplasia, pancreatitis, gastritis, hepatitis, jaundice, hepatic function abnormal, erythema multiforme, Stevens-Johnson Syndrome, exfoliative dermatitis, toxic epidermal necrolysis, Quincke’s oedema, acute renal failure, haemoglobin decreased and haematocrit decreased. Not known: Potassium depletion with hypokalaemia, particularly serious in certain high risk populations, extrapyramidal disorder (extrapyramidal syndrome), myopia, vision blurred, torsades de pointes (potentially fatal), possibility of onset of hepatic encephalopathy in case of hepatic insufficiency, possible worsening of pre-existing systemic lupus erythematosus, electrocardiogram QT prolonged, blood glucose increased, blood uric acid increased. Raynaud’s phenomenon. Syndrome of inappropriate antidiuretic hormone secretion (SIADH) can be considered as a very rare complication associated with ACE inhibitor therapy. OVERDOSE* PROPERTIES* Perindopril is an inhibitor of the angiotensin converting enzyme (ACE inhibitor) which converts angiotensin to angiotensin II. Indapamide is a sulfonamide derivative with an indole ring, pharmacologically related to the thiazide group of diuretics. Amlodipine is a calcium ion influx inhibitor of the dihydropyridine group (slow channel blocker or calcium ion antagonist) and inhibits the transmembrane influx of calcium ions into cardiac and vascular smooth muscle PRESENTATION* Box of 30tablets of Coverdine 5mg/1.25mg/5mg,

Coverdine® (perindopril arginine/indapamide/amlodipine) Abbreviated Prescribing Information: Please refer to the Summary of Product Characteristics before prescribing. COMPOSITION* Coverdine 5mg/1.25mg/5mg film-coated tablets contains 5 mg perindopril arginine (per)/1.25 mg indapamide (ind)/5 mg of amlodipine (amlo); Coverdine 5mg/1.25mg/10mg film-coated tablets: 5 mg per/1.25 mg ind/10 mg amlo; Coverdine 10mg/2.5mg/5mg film-coated tablets: 10 mg per/2.5 mg ind/5mg amlo; Coverdine 10mg/2.5mg/10mg film-coated tablets: 10 mg per/2.5 mg ind/10 mg amlo. INDICATIONS* Substitution therapy for treatment of essential hypertension, in patients already controlled with perindopril/indapamide fixed dose combination and amlodipine, taken at the same dose level. DOSAGE AND ADMINISTRATION* One tablet per day, preferably in the morning and before a meal. The fixed dose combination is not suitable for initial therapy. If a change of the posology is required, titration should be
5mg/1.25mg/10mg, 10mg/2.5mg/5mg and 10mg/2.5mg/10mg. LES LABORATOIRES SERVIER, 50 rue Carnot, 92284 Suresnes cedex France. PA0568/024/002-005. Legal Classification for Supply: POM. Local Representative in Ireland: Servier Laboratories (Ireland) Ltd, Block 2 West Pier Business Campus, Old Dunleary Road, Dun Laoghaire, Co. Dublin. Tel (01) 6638110, Fax (01) 6638120, www.servier.ie. * For complete information, please refer to the complete Summary of Product Characteristics for Coverdine® at www.medicines.ie Date of last revision of text: January 2020 (Date of last approved SmPC: July 2019) Date of preparation: January 2020. 1920C2CDEPressAD. References: 1. Tòth K, on behalf of the PIANIST Investigators. Am J Cardiovasc Drugs. 2014. DOI 10.1007/s40256-014-0067-2. 2. Pall D et al, Hypertonia és Nephrologia. 2012;16(3-4):119-123. 3
ALL REPORTS BY ANNA WEDDERBURN
56th Annual Irish Neurological Association Meeting, 1-2 October 2020

Neurological manifestations of Covid-19
Prof Patrick Mallon, Professor of Microbial Diseases

in
the
UCD
School of Medicine and Consultant in Infectious
Diseases in St Vincent’s University Hospital, spoke at the 56th Annual Irish Neurological Association Meeting about the neurological manifestations arising from SARSCoV-2 infection. “There are a lot of knowledge gaps surrounding the neurological symptoms of Covid-19,” Prof Mallon warned the virtual audience, before detailing what has been observed in St Vincent’s University Hospital over the last six months with regard to Covid-19 and the brain.
There have been atypical presentations of Covid-19 in the elderly in the form of delirium, something that was noted as early as March. A number of elderly individuals, later proven to have Covid-19, did not present with the typical influenza-like illness –they had no temperature response and no respiratory symptoms. Instead, these individuals presented with acute delirium, of which there were “variable backgrounds of cognitive state”. As a result of this, St Vincent’s University Hospital widened their scope of clas-
sification for potential Covid-19. Now, individuals coming from a nursing home with any atypical presentation are “regarded as Covid until proven otherwise”.
Many young people have presented to the hospital with what appeared to be severe lymphocytic meningitis “on the background of an influenza-like illness”, which was often accompanied by a SARSCoV-2 positive PCR result. The cerebrospinal fluid (CSF) of these patients tested negative for SARSCoV-2, while the MRI findings were not consistent with encephalitis.
There have been a number of SARS-CoV-2 infected patients, from a range of different ages, presenting with new onset seizures.
Prof Mallon stated that it is difficult “within the setting of a pandemic” to discern whether these individuals “just happen to have a Covid-19 infection” or whether these seizures are arising secondary to acute Covid-19 infection. This is not something they have been able to differentiate to date.
Many Covid-19 patients have also suffered strokes over the last six months.
Prof Mallon said, once again, it is hard to discern whether the strokes arose from Covid-19, or whether
they simply presented alongside Covid-19. However, as Covid-19 is already associated with other thrombotic complications such as pulmonary embolism and venous thromboembolism, Prof Mallon and his colleagues believe that the vascular abnormalities resulting from Covid-19 are likely to be contributing to higher incidences of stroke in Covid-19 patients.
Prof Mallon also touched on post-Covid syndrome, or long-Covid syndrome, and the associated neurological symptoms arising from this complication. He reported that it appears to be the individuals who did not suffer Covid-19 severely and initially required no hospital attention who are acquiring post-Covid syndrome. These patients are presenting with a number of prolonged objective and subjective symptoms. The main neurological complaint from these patients is ‘brain fog’. More specifically, patients are suffering from a lack of concentration and have difficulties with basic arithmetic. At this point, Prof Mallon referenced the case of a woman in her 50s who contracted Covid-19 six months ago. Prior to infection, this woman was running her own business,
which is spread across a number of locations in Ireland. After taking some time off during her illness, this woman returned to work and found she was no longer able to do the arithmetic associated functions required to run a business. Furthermore, when she
Socioeconomic deprivation related to increased incidences of epilepsy in Cork
Dr Eimer Maloney, Cork University Hospital, reported her findings in relation to the impact of socioeconomic deprivation on the incidence of epilepsy in Cork. For this presentation, she was awarded first place in both the Harold Miller Prize for best overall presentation and the John Kirker Prize for best epilepsy-related presentation.
The definition given by Dr Maloney for socioeconomic deprivation was “an absence of essential or desirable attributes, possessions and opportunities, which are considered no more than the minimum by a society”. In recent years, socioeconomic status and socioeconomic deprivation have been associated with an increased risk for a number of different diseases. In terms of epilepsy, it has been found that the prevalence of this disease is highest in areas of relative deprivation. This is not only seen at a global level, but also regionally within a country or even within a city.
Dr Maloney explained the two current theories behind these disease patterns. The first theory is ‘social drift,’ where a long-term illness, such as epilepsy, causes an individual to move, or drift down the social scale, thus resulting in a higher prevalence of disease in lower socioeconomic groups – ie, having a chronic illness leads to so-
cial deprivation. The second theory is ‘social causation’, which states that experiencing socioeconomic deprivation leads to an increased risk of developing certain diseases – ie, social deprivation leads to illness. In order to discern whether it is social drift or social causation that is causing the higher rates of disease in lower socioeconomic groups, the socioeconomic status of individuals must be noted at the time of disease onset, excluding the possibility of social drift.
This is what Dr Maloney and her colleagues decided to do in the context of Cork city and county, an area containing a population of just under 550,000. The HP deprivation index, which is based on census data, was used to assign a deprivation score to the different areas of Cork. Based on the areas in which they lived, the population of Cork was divided into a scale of five categories of deprivation, with each category containing approximately 108,000 individuals. Category one contained the most deprived individuals of Cork, while category five contained the least deprived individuals of Cork.
Dr Maloney then did a retrospective chart review of the incidences of first unprovoked seizure, first provoked seizure, diagnosis of epilepsy, and seizure mimic (defined as a working diagnosis of seizure being considered, but then an alternate diagnosis
subsequently being reached) for 2017. Using the hospital registered address of patients, it was noted which category of deprivation each diagnosis belonged to. From this, the annual incidence of each diagnostic seizure was calculated for the different levels of deprivation per 100,000 population, the findings of which were significant.
had a first unprovoked seizure. Comparing these numbers using an incidence ratio, which is similar to relative risk, it was found that a person living in one of the most deprived areas of Cork was almost 1.8 times more likely to be diagnosed with a first unprovoked seizure than a person living in one of the least deprived areas. Similar
returned to play bingo with her son, she found that she was also unable to follow the numbers within the game. “This is of ongoing and significant concern to the woman, as it was six months ago that she contracted the virus,” Prof Mallon said.
least deprived areas.
Dr Maloney also investigated this occurrence in individuals below the age of 18. The same results were found. Children living in the most deprived areas of Cork were more likely to have a seizure diagnosis than children living in the least deprived areas. This reached statistical significance for three out of the four seizure diagnoses. Statistical significance was not reached for seizure mimics, although the same trend was visible.
The new diagnosis of epilepsy by aetiology was also investigated in the context of socioeconomic deprivation in Cork. The aetiologies investigated were structural, genetic, and unknown. All three aetiologies were found to be higher in socially deprived areas, demonstrating that this phenomenon is multifactorial – it is not just one aetiology that is accounting for an increased incidence of epilepsy in socioeconomically deprived areas.
Dr Maloney first described the results of the first unprovoked seizure diagnoses. In category one, the most deprived category, 83 individuals per 100,000 population had a first unprovoked seizure, whereas in category five, the least deprived category, only 46 individuals per 100,000 population
trends were seen across the other seizure diagnoses. Individuals living in the most deprived areas of Cork were 1.6 times more likely to have a first provoked seizure;1.8 times more likely to have a new diagnosis of epilepsy; and 1.3 times more likely to have a seizure mimic compared to those living in the
Although this research was confined to Cork city and county, Dr Maloney said that “there is no real reason” to limit the implications of this study to Cork city and council, as “it likely reflects a national trend”. Dr Maloney also pointed out that this study underlines the need for healthcare provision to reflect the increased burden of disease in more socioeconomically deprived areas, which unfortunately is often not the case.
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 40 Conference
Coverage
The definition given by Dr Maloney for socioeconomic deprivation was ‘an absence of essential or desirable attributes, possessions and opportunities, which are considered no more than the minimum by a society’
Prof Patrick Mallon
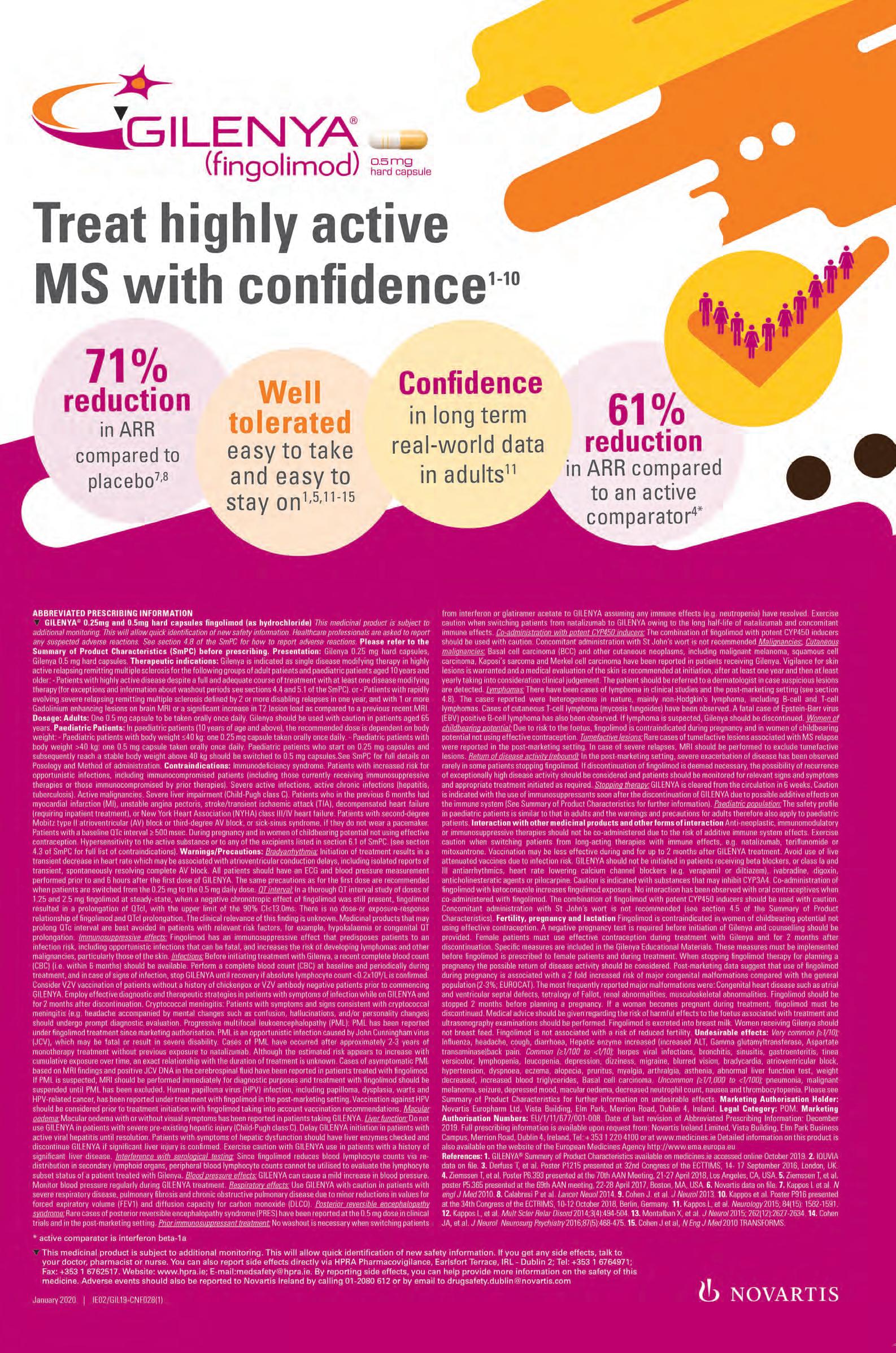
GROWING REAL-WORLD EXPERIENCE
GROWING REAL-WORLD EXPERIENCE
As of August 2020… MORE THAN
As of August 2020… MORE THAN
170,000
170,000
MS patients have been treated with OCREVUS® (ocrelizumab) globally 1
As of August 2020… MORE
THAN
MS patients have been with OCREVUS® (ocrelizumab)
170,000
MS patients have been with OCREVUS® (ocrelizumab)
ABRIDGED PRESCRIBING INFORMATION (API). For full prescribing information refer to the Summary of Product Characteristics [SmPC]. OCREVUS®t (ocrelizumab) 300 mg concentrate for solution for infusion t This medicine is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See box below for details on how to report. Indications: Treatment of adult patients with relapsing forms of multiple sclerosis (RMS) with active disease defined by clinical or imaging features. Treatment of adult patients with early primary progressive multiple sclerosis (PPMS) in terms of disease duration and level of disability, and with imaging features characteristic of inflammatory activity, (refer to SmPC for full details). Dosage and Administration: Treatment should be initiated and supervised by specialised physicians experienced in the diagnosis and treatment of neurological conditions with access to appropriate medical support to manage severe reactions such as serious infusion-related reactions (IRRs), hypersensitivity reactions and/or anaphylactic reactions. Premedication for IRRs: Administer the following two premedication prior to each infusion to reduce the frequency and severity of IRRs: (a) 100 mg intravenous (IV) methylprednisolone (or equivalent) approximately 30 min prior to each infusion and (b) antihistamine approximately 30-60 min prior to each infusion. In addition, premedication with an antipyretic (e.g. paracetamol) may also be considered approximately 30-60 min prior to each infusion. Initial dose: 600 mg dose administered as two separate IV infusions (first as a 300 mg infusion, followed 2 weeks later by a second 300 mg infusion). Subsequentdoses: a single 600 mg IV infusion every 6 months. Administer the first subsequent dose of 600 mg 6 months after the first infusion of the initial dose. Refer to SmPC for full details. If patients did not experience a serious infusion-related reaction (IRR) with any previous Ocrevus infusion, a shorter (2-hour) infusion can be administered for subsequent doses. A minimum interval of 5 months should be maintained between each dose. Refer to the SmPC for full details. Infusion Adjustments in case of IRRs: In case of IRRs during any infusion, refer to the SmPC for full details of adjustments for life-threatening IRRs, severe IRRs and mild to moderate IRRs. Dose interruption and slowing (for mild/moderate and severe IRRs) will result in a change in the infusion rate and increase the total duration of the infusion, but not the total dose. No dose reductions of Ocrevus are recommended. Delayed or Missed Doses: If an infusion of Ocrevus is missed, administer it as soon as possible; do not wait until the next planned dose. Maintain a treatment interval of 6 months (with a minimum of 5 months) between doses. Special Populations: Based on the limited data available, no posology adjustment is needed in patients > 55 years of age. Patients enrolled in the ongoing clinical trials continue to be dosed with 600 mg ocrelizumab every 6 months after they become 55 and older. The safety and efficacy of Ocrevus in patients with renal/hepatic impairment has not been formally studied. Patients with mild renal/hepatic impairment were included in clinical trials. No experience in patients with moderate or severe renal/hepatic impairment. No data available in children and adolescents aged 0 - 18 years. Refer to SmPC for further details. Method of Administration: Prepare Ocrevus using aseptic technique. Dilute the product into an infusion bag containing isotonic 0.9% sodium chloride to a final drug concentration of approximately 1.2 mg/mL. For instructions on dilution before administration, refer to SmPC. After dilution, administer Ocrevus as an IV infusion through a dedicated line. Use an infusion set with a 0.2 or 0.22 micron inline filter. Do not administer as an IV push or bolus. Infusion Instructions: Initial dose (600mg) divided into 2 infusions: Infusion 1/Infusion 2 (2 weeks later). Initiate infusion (300 mg in 250 mL) at a rate of 30 mL/hour for 30 min. The rate can be increased in 30 mL/hour increments every 30 min. to a max of 180 mL/hour. Each infusion should be given over approx. 2.5 h. Subsequent doses: 600mg (single infusion every 6 months) Option 1: (Infusion of approx. 3.5 hours duration) Initiate infusion (600 mg in 500 mL) at a rate of 40 mL/hour for 30 min. The rate can be increased in 40 mL/hour increments every 30 min to a max of 200 mL/hour. Each infusion should be given over approx. 3.5 hours. Option 2: Infusion of approximately 2 hours duration. Initiate the infusion at a rate of 100 mL/hour for the first 15 minutes. Increase the infusion rate to 200 mL/hour for the next 15 minutes. Increase the infusion rate to 250 mL/hour for the next 30 minutes. Increase the infusion rate to 300 mL/hour for the remaining 60 minutes. Each infusion should be given over approximately 2 hours. Monitor all patients during infusion and for at least one hour after the completion of the infusion. Physicians should alert patients that an IRR can occur within 24 hours of infusion. Withholding of antihypertensive treatments should be considered for 12 hours prior to and throughout each infusion as hypotension is a symptom of IRRs. Patients with a history of congestive heart failure (New York Heart Association III & IV) were not studied. Contraindications: Hypersensitivity to ocrelizumab or to any of the excipients listed in the SmPC; current active infection; patients in a severely immunocompromised state; known active malignancies. Special Warnings and Precautions: Traceability: Record the name and the batch number of the administered product to improve traceability of biological products. IRRs: Ocrevus is associated with IRRs, which may be related to cytokine release and/or other chemical mediators. Symptoms of IRRs may occur during any infusion, but have been more frequently reported during the first infusion. IRRs can occur within 24 hours of the infusion. These reactions may present as pruritus, rash, urticaria, erythema, throat irritation, oropharyngeal pain, dyspnoea, pharyngeal or laryngeal oedema, flushing, hypotension, pyrexia, fatigue, headache, dizziness, nausea and tachycardia. Interrupt the infusion immediately and permanently if the patient experiences severe pulmonary symptoms such as bronchospasm or asthma exacerbation, and administer symptomatic treatment. Monitor the patient until the pulmonary symptoms have resolved because initial improvement of clinical symptoms could be followed by deterioration. Hypersensitivity Reactions: A hypersensitivity reaction could also occur (acute allergic reaction to medicinal product). Type 1 acute hypersensitivity reactions (IgE-mediated) may be clinically indistinguishable from IRR symptoms. A hypersensitivity reaction may present during any infusion, although typically would not present during the first infusion. For subsequent infusions, more severe symptoms than previously experienced, or new severe symptoms, should prompt consideration of a potential hypersensitivity reaction. Patients with known IgE mediated hypersensitivity to ocrelizumab must not be treated (refer to SmPC for further details). If a hypersensitivity reaction is suspected during infusion, the infusion must be stopped immediately and permanently. Infections: delay administration in patients with active infection until it is resolved. Verify the patient’s immune status before dosing since severely immunocompromised patients should not be treated. The frequency of grade 4 (lifethreatening) and grade 5 (fatal) infections was low in all treatment groups, but in PPMS it was higher with Ocrevus compared with placebo for life-threatening (1.6% vs 0.4%) and fatal (0.6% vs 0%) infections. All life-threatening infections resolved without discontinuing Ocrevus. In PPMS, patients with swallowing difficulties are at a higher risk of aspiration pneumonia. Ocrevus treatment may further increase the risk of severe pneumonia in these patients. Physicians should take prompt action for patients presenting with pneumonia. Progressive Multifocal Leukoencephalopathy (PML): a risk of PML cannot be ruled out since John Cunningham (JC) virus infection resulting in PML has been observed in patients treated with anti-CD20 antibodies and other MS therapies, and associated with risk factors. Physicians should be vigilant for the early signs and symptoms of PML, which can include any new onset, or worsening of neurological signs or symptoms, as these can be similar to MS disease. If PML is suspected, withhold Ocrevus dosing. The following evaluations should be considered: Magnetic Resonance Imaging (MRI) scan preferably with contrast (compared with pre-treatment MRI), confirmatory cerebro-spinal fluid (CSF) testing for John Cunningham (JC) Viral Deoxyribonucleic acid (DNA) and repeat neurological assessments. If PML is confirmed, discontinue treatment permanently. HepatitisBvirus(HBV)reactivation: has been reported in patients treated with anti-CD20 antibodies and in some cases resulting in fulminant hepatitis, hepatic failure and death. Perform HBV screening in all patients before starting treatment. Do not treat patients with active HBV (confirmed by positive results for HBsAg and anti HB testing) with Ocrevus. Patients with positive serology (i.e. negative for HBsAg and positive for HB core antibody (HBcAb +); carriers of HBV (positive for surface antigen, HBsAg+) should consult liver disease experts before treatment starts and should be monitored and managed following local medical standards to prevent hepatitis B reactivation. Malignancies: an increased number of malignancies (including breast cancer) have been observed in clinical trials in patients treated with Ocrevus, compared to control groups. The incidence was within the background rate expected for an MS population. Consider individual benefit risk in patients with known risk factors for malignancies and in patients who are being actively monitored for recurrence of malignancy. Do not treat patients with a known active malignancy with Ocrevus. Patients should follow standard breast cancer screening per local guidelines. In the controlled period of the clinical trials, incidence of non-melanoma skin cancers was low and there was no imbalance between treatment groups. An increase in incidence was observed between years 3 and 4 of
ABRIDGED PRESCRIBING INFORMATION (API). For full prescribing information refer to the Summary mg concentrate for solution for infusion t This medicine is subject to additional monitoring. This will are asked to report any suspected adverse reactions. See box below for details on how to report. Indications: (RMS) with active disease defined by clinical or imaging features. Treatment of adult patients with early and level of disability, and with imaging features characteristic of inflammatory activity, (refer to SmPC and supervised by specialised physicians experienced in the diagnosis and treatment of neurological reactions such as serious infusion-related reactions (IRRs), hypersensitivity reactions and/or anaphylactic prior to each infusion to reduce the frequency and severity of IRRs: (a) 100 mg intravenous (IV) methylprednisolone (b) antihistamine approximately 30-60 min prior to each infusion. In addition, premedication with an antipyretic prior to each infusion. Initial dose: 600 mg dose administered as two separate IV infusions (first as Subsequentdoses: a single 600 mg IV infusion every 6 months. Administer the first subsequent dose of full details. If patients did not experience a serious infusion-related reaction (IRR) with any previous Ocrevus doses. A minimum interval of 5 months should be maintained between each dose. Refer to the SmPC for infusion, refer to the SmPC for full details of adjustments for life-threatening IRRs, severe IRRs and mild severe IRRs) will result in a change in the infusion rate and increase the total duration of the infusion, Delayed or Missed Doses: If an infusion of Ocrevus is missed, administer it as soon as possible; do not (with a minimum of 5 months) between doses. Special Populations: Based on the limited data available, enrolled in the ongoing clinical trials continue to be dosed with 600 mg ocrelizumab every 6 months after with renal/hepatic impairment has not been formally studied. Patients with mild renal/hepatic impairment or severe renal/hepatic impairment. No data available in children and adolescents aged 0 - 18 years. Refer using aseptic technique. Dilute the product into an infusion bag containing isotonic 0.9% sodium chloride on dilution before administration, refer to SmPC. After dilution, administer Ocrevus as an IV infusion through filter. Do not administer as an IV push or bolus. Infusion Instructions: Initial dose (600mg) divided into 250 mL) at a rate of 30 mL/hour for 30 min. The rate can be increased in 30 mL/hour increments every 2.5 h. Subsequent doses: 600mg (single infusion every 6 months) Option 1: (Infusion of approx. 3.5 hours 30 min. The rate can be increased in 40 mL/hour increments every 30 min to a max of 200 mL/hour. approximately 2 hours duration. Initiate the infusion at a rate of 100 mL/hour for the first 15 minutes. Increase infusion rate to 250 mL/hour for the next 30 minutes. Increase the infusion rate to 300 mL/hour for the hours. Monitor all patients during infusion and for at least one hour after the completion of the infusion. infusion. Withholding of antihypertensive treatments should be considered for 12 hours prior to and throughout history of congestive heart failure (New York Heart Association III & IV) were not studied. Contraindications: SmPC; current active infection; patients in a severely immunocompromised state; known active malignancies. and the batch number of the administered product to improve traceability of biological products. IRRs: and/or other chemical mediators. Symptoms of IRRs may occur during any infusion, but have been more of the infusion. These reactions may present as pruritus, rash, urticaria, erythema, throat irritation, hypotension, pyrexia, fatigue, headache, dizziness, nausea and tachycardia. Interrupt the infusion immediately symptoms such as bronchospasm or asthma exacerbation, and administer symptomatic treatment. Monitor improvement of clinical symptoms could be followed by deterioration. Hypersensitivity Reactions: A hypersensitivity product). Type 1 acute hypersensitivity reactions (IgE-mediated) may be clinically indistinguishable from although typically would not present during the first infusion. For subsequent infusions, more severe prompt consideration of a potential hypersensitivity reaction. Patients with known IgE mediated hypersensitivity details). If a hypersensitivity reaction is suspected during infusion, the infusion must be stopped immediately infection until it is resolved. Verify the patient’s immune status before dosing since severely immunocompromised threatening) and grade 5 (fatal) infections was low in all treatment groups, but in PPMS it was higher fatal (0.6% vs 0%) infections. All life-threatening infections resolved without discontinuing Ocrevus. In pneumonia. Ocrevus treatment may further increase the risk of severe pneumonia in these patients. Physicians Progressive Multifocal Leukoencephalopathy (PML): a risk of PML cannot be ruled out since John Cunningham treated with anti-CD20 antibodies and other MS therapies, and associated with risk factors. Physicians should any new onset, or worsening of neurological signs or symptoms, as these can be similar to MS disease. should be considered: Magnetic Resonance Imaging (MRI) scan preferably with contrast (compared with Cunningham (JC) Viral Deoxyribonucleic acid (DNA) and repeat neurological assessments. If PML is confirmed, has been reported in patients treated with anti-CD20 antibodies and in some cases resulting in fulminant before starting treatment. Do not treat patients with active HBV (confirmed by positive results for HBsAg negative for HBsAg and positive for HB core antibody (HBcAb +); carriers of HBV (positive for surface antigen, and should be monitored and managed following local medical standards to prevent hepatitis B reactivation. cancer) have been observed in clinical trials in patients treated with Ocrevus, compared to control population. Consider individual benefit risk in patients with known risk factors for malignancies and in not treat patients with a known active malignancy with Ocrevus. Patients should follow standard breast trials, incidence of non-melanoma skin cancers was low and there was no imbalance between treatment
ABRIDGED PRESCRIBING INFORMATION (API). For full prescribing information refer to the Summary mg concentrate for solution for infusion t This medicine is subject to additional monitoring. This will are asked to report any suspected adverse reactions. See box below for details on how to report. Indications: (RMS) with active disease defined by clinical or imaging features. Treatment of adult patients with early and level of disability, and with imaging features characteristic of inflammatory activity, (refer to SmPC and supervised by specialised physicians experienced in the diagnosis and treatment of neurological reactions such as serious infusion-related reactions (IRRs), hypersensitivity reactions and/or anaphylactic prior to each infusion to reduce the frequency and severity of IRRs: (a) 100 mg intravenous (IV) methylprednisolone (b) antihistamine approximately 30-60 min prior to each infusion. In addition, premedication with an antipyretic prior to each infusion. Initial dose: 600 mg dose administered as two separate IV infusions (first as Subsequentdoses: a single 600 mg IV infusion every 6 months. Administer the first subsequent dose of full details. If patients did not experience a serious infusion-related reaction (IRR) with any previous Ocrevus doses. A minimum interval of 5 months should be maintained between each dose. Refer to the SmPC for infusion, refer to the SmPC for full details of adjustments for life-threatening IRRs, severe IRRs and mild severe IRRs) will result in a change in the infusion rate and increase the total duration of the infusion, Delayed or Missed Doses: If an infusion of Ocrevus is missed, administer it as soon as possible; do not (with a minimum of 5 months) between doses. Special Populations: Based on the limited data available, enrolled in the ongoing clinical trials continue to be dosed with 600 mg ocrelizumab every 6 months after with renal/hepatic impairment has not been formally studied. Patients with mild renal/hepatic impairment or severe renal/hepatic impairment. No data available in children and adolescents aged 0 - 18 years. Refer using aseptic technique. Dilute the product into an infusion bag containing isotonic 0.9% sodium chloride
GROWING REAL-WORLD EXPERIENCE
on dilution before administration, refer to SmPC. After dilution, administer Ocrevus as an IV infusion through
The First and Only therapy approved
for both RMS and PPMS2
Relapsing forms of multiple sclerosis (RMS) with active disease defined by clinical or imaging features2
Early primary progressive multiple sclerosis (PPMS) in terms of disease duration and level of disability, and with imaging features characteristic of inflammatory activity2
Full details available in the OCREVUS SmPC available at www.medicines.ie
treatment due to basal cell carcinoma, which was not observed in subsequent years. The incidence remains within the background rate expected for an MS population. Treatment of severely immunocompromised patients: do not treat these patients until the condition resolves. In other auto-immune conditions, use of Ocrevus concomitantly with immunosuppressive medications resulted in an increase of serious infections including and not limited to, atypical pneumonia and pneumocystis jirovecii pneumonia, varicella pneumonia, tuberculosis, histoplasmosis. In rare cases, some of these infections were fatal - refer to SmPC for further details. It is not recommended to use other immunosuppressives concomitantly with Ocrevus except corticosteroids for symptomatic treatment of relapses. Knowledge is limited as to whether concomitant steroid use for symptomatic treatment of relapses is associated with an increased risk of infections in clinical practice. In the Ocrevus MS pivotal studies, administration of corticosteroids for the treatment of relapse was not associated with an increased risk of serious infection. When initiating Ocrevus after an immunosuppressive therapy or initiating an immunosuppressive therapy after Ocrevus, consider the potential for overlapping pharmacodynamic effects. Caution should be exercised when prescribing Ocrevus taking into consideration the pharmacodynamics of other disease modifying MS therapies. Vaccinations: The safety of immunisation with live or live-attenuated vaccines, following Ocrevus therapy has not been studies and vaccination with live-attenuated or live vaccines is not recommended during treatment and not until B-cell repletion (in clinical trials, the median time for B-cell repletion was 72 weeks). In a randomised open-label study, RMS patients were able to mount humoral responses, although decreased, to tetanus toxoid, 23-valent pneumococcal polysaccharide with or without a booster vaccine, keyhole limpet hemocyanin neoantigen, and seasonal influenza vaccines (refer to SmPC). It is recommended to vaccinate patients treated with Ocrevus with seasonal influenza vaccines that are inactivated. Physicians should review the immunisation status of patients being considered for treatment with Ocrevus. Patients who require vaccination should complete their immunisation at least 6 weeks prior to initiation of Ocrevus (refer to SmPC). Exposureinuteroandvaccinationof neonatesandinfantswithliveor live attenuated vaccines: Due to the potential depletion of B cells in infants of mothers who have been exposed to Ocrevus during pregnancy, it is recommended that vaccination with live or live-attenuated vaccines should be delayed until B-cell levels have recovered; therefore, it is recommended that vaccination with live or live-attenuated vaccines be delayed until B-cell levels have recovered; therefore, measuring CD19-positive B-cell levels in neonates and infants, prior to vaccination is recommended. It is recommended that all vaccinations other than live or live-attenuated should follow the local immunisation schedule and measurement of vaccine-induced response titers should be considered to check whether individuals have mounted a protective immune response because the efficacy of the vaccination may be decreased. The safety and timing of vaccination should be discussed with the infant’s physician (refer to SmPC). Sodium: contains less than 1 mmol sodium (23 mg) per dose, i.e. essentially sodium-free. Interactions: No formal drug interaction studies have been performed, as no drug interactions are expected via cytochrome P450 enzymes, other metabolising enzymes or transporters. The safety of immunisation with live or live-attenuated vaccines, following Ocrevus therapy has not been studied. Data are available on the effects of tetanus toxoid, 23-valent pneumococcal polysaccharide, keyhole limpet hemocyanin neoantigen, and seasonal influenza vaccines in patients receiving Ocrevus. Refer to SmPC. It is not recommended to use other immunosuppressives concomitantly with Ocrevus except corticosteroids for symptomatic treatment of relapses. Refer to SmPC. Fertility, Pregnancy and Lactation: Women of childbearing potential should use contraception while receiving Ocrevus and for 12 months after the last infusion. Ocrevus is a humanised monoclonal antibody of an immunoglobulin G1 subtype and immunoglobulins are known to cross the placental barrier. There is a limited amount of data from the use of Ocrevus in pregnant women. Postponing vaccination with live or liveattenuated vaccines should be considered for neonates and infants born to mothers who have been exposed to Ocrevus in utero. No B cell count data have been collected in neonates and infants exposed to ocrelizumab and the potential duration of B-cell depletion in neonates and infants is unknown (refer to section 4.4 of SmPC). Transient peripheral B-cell depletion and lymphocytopenia have been reported in infants born to mothers exposed to other anti-CD20 antibodies during pregnancy. Animal studies (embryo-foetal toxicity) do not indicate teratogenic effects. B-cell depletion in utero was detected. Reproductive toxicity was observed in pre and post-natal development studies (refer to section 5.3 of SmPC). Ocrevus should be avoided during pregnancy unless the potential benefit to the mother outweighs the potential risk to the foetus. It is unknown whether ocrelizumab/ metabolites are excreted in human milk. Available pharmacodynamic/toxicological data in animals have shown excretion of ocrelizumab in milk (for details see section 5.3 of SmPC). A risk to neonates and infants cannot be excluded. Women should be advised to discontinue breast-feeding during Ocrevus therapy. Preclinical data reveal no special hazards for humans based on studies of male and female fertility in cynomologous monkeys. Effects on ability to drive and use machines: Ocrevus has no or negligible influence on the ability to drive and use machines. Undesirable Effects: The most important and frequently reported adverse drug reactions (ADRs) were IRRs and infections. The following is a summary of the very common (≥ 1/10) and common (≥ 1/100 to < 1/10) ADRs that have been reported in association with the use of Ocrevus in 1311 patients (3054 patient years) during the controlled treatment periods of MS clinical trials. Verycommon(≥1/10): upper respiratory tract infection, nasopharyngitis, influenza, blood immunoglobulin M decreased and IRRs, (refer to SmPC for full details). Common (≥ 1/100 to < 1/10): sinusitis, bronchitis, oral herpes, gastroenteritis, respiratory tract infection, viral infection, herpes zoster, conjunctivitis, cellulitis, cough, catarrh, blood immunoglobulin G decreased and neutropenia. Refer to SmPC for full listing of adverse events and further details. Description of selected adverse reactions: AlternativeShorterInfusionof SubsequentDoses: In a study (MA30143 Shorter Infusion Substudy) designed to characterise the safety profile of shorter (2-hour) Ocrevus infusions in patients with Relapsing-Remitting Multiple Sclerosis, the incidence, intensity, and types of symptoms of IRRs were consistent with those of infusions administered over 3.5 hours. The overall number of interventions needed was low in both infusion groups, however, more interventions (slowing down or temporary interruptions) were needed to manage IRRs in the shorter (2-hour) infusion group compared to the 3.5- hour infusion group (8.7% vs. 4.8%, respectively). Refer to SmPC for further details. LaboratoryAbnormalities: Immunoglobulins: Treatment with Ocrevus resulted in a decrease in total immunoglobulins over the controlled period of the studies, mainly driven by reduction in IgM. Clinical trial data have shown an association between decreased levels of IgG (and less so for IgM or IgA) and serious infections. See SmPC section 4.8 for instructions on reporting adverse events. Special Precautions for Storage: Store in a refrigerator (2ºC – 8ºC). Do not freeze. Keep the vials in the outer carton in order to protect from light. Legal Category: Product subject to medical prescription which may not be renewed (A). Presentations and Marketing Authorisation Numbers: EU/1/17/1231/001 for 300 mg/10 mL (pack size of one). Marketing Authorisation Holder: Roche Registration GmbH, Emil-Barell-Strasse 1, 79639 Grenzach-Wyhlen, Germany. Ocrevus ® is a registered trade mark. Further information is available from Roche Products (Ireland) Limited, 3004 Lake Drive, Citywest, Naas Road, Dublin 24. Telephone: (01) 4690700. Fax: (01) 4690791. Date of API Preparation: May 2020. t This medicine is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions.
In the event of a suspected adverse event, please report it to:
The Drug Surveillance Centre, Roche Products (Ireland) Limited
Telephone: (01) 4690700 Fax: (01) 4690793
Email: ireland.drug_surveillance_centre@roche.com
Alternatively, suspected adverse reactions should be reported to:
HPRA Pharmacovigilance, The Health Products Regulatory Authority (HPRA)
Telephone: (01) 6764971 Fax: (01) 6762517
Website: www.hpra.ie Email: medsafety@hpra.ie
M-IE-00000091 based on Ocrevus SmPC dated 30 April 2020. References:
1. Roche data on file (M-GB-00001508).
2. Ocrevus 300 mg concentrate for solution for infusion Summary of Product Characteristics 30 April 2020, available on www.medicines.ie. Date of item: October 2020. M-IE-00000288
Conference Coverage
56th Annual Irish Neurological Association Meeting, 1-2 October 2020

VP shunt silicone allergy: A case study
Dr Martin Leer, Royal Victoria Hospital Belfast, spoke of his experience with an 18-yearold female patient with a background of benign external hydrocephalus – a build-up of cerebrospinal fluid (CSF) in the brain. Ventriculoperitoneal (VP) shunting is the most common neurosurgical procedure performed for the management of hydrocephalus. There is a high complication rate of 11-25 per cent within the first year and multiple revisions are often required, leading to costly and lengthy hospital stays for patients.
The patient in this case study had required multiple shunt revisions throughout childhood, and at the time of presentation, it had been five years since her most recent revision. She presented with a wound breakdown over the shunt site after sustaining trauma to the area. A new bactiseal VP shunt was placed, and the patient subsequently had a number of episodes of headache, neck and abdominal pain, and vomiting – symptoms of shunt malfunction. Four months after the shunt insertion, there was a marked fibrotic reaction along the course of the shunt, and an area of
wound dehiscence over an incision on the chest wall. This prompted a shunt exploration. The ratio of CSF white cell count (WCC) to red cell count (RCC) was elevated, with a CSF WCC of 9/µl and a CSF RCC of less than 1/µl. The shunt was removed and empirical antibiotics were prescribed given the clinical suspicion of infection. The CSF WCC returned to normal, and a new VP shunt was placed. Within 12 hours of the operation, the patient developed a rapid meningitis response. CSF sampling revealed a WCC of 291/µl, 70 per cent of which were lymphocytes, with a RCC of 638/µl. CSF glucose and protein were normal. CSF leucocytosis didn’t normalise with removal of the shunt and replacement with a bactiseal external ventricular drain, followed by a two-week course of empirical intravenous antibiotics and subsequent intrathecal antibiotics. Her peripheral blood samples revealed an eosinophilia at this time, and none of the CSF sample analysis revealed any causative organism on microscopy or culture. Dr Leer reported that at this stage, a silicone allergy was diagnosed.
New EEG referral form: Potential to increase efficiency and save money
Dr Emily O’Brien, St Vincent’s University Hospital, presented the results of an audit investigating the efficiency of the inpatient electroencephalogram (EEG) service in St Vincent’s University Hospital from October 2019 to April 2020 at the conference.
A total of 130 inpatient referrals were included in this audit, and it became apparent that improving the efficiency of the EEG service could lead to a significant amount of money being saved. The cost of an EEG at St Vincent’s University Hospital is €210, while the cost of 24 hour overnight stay is €900. Some 32 patients included in this audit were kept in hospital for at least one night “for the sole purpose of receiving an inpatient EEG”. This resulted in an excess cost of €28,800 over the seven-month period, demonstrating that there are “huge savings to be made across the board with a more efficient EEG service”.
However, the cost was not the primary reason for this audit being carried out. Over the winter months, St Vincent’s University Hospital is often overloaded with EEG referrals. Thus the reasoning behind carrying out this audit was to improve the efficiency of the EEG service.
Dr O’Brien and colleagues decided to investigate the indications for urgency in patient EEG referrals. Dr O’Brien reviewed the information on the EEG referral forms and gave each case an urgency score from oneto-10, with one being the least urgent and 10 being the most urgent. Dr O’Brien also took a history from the patient on arrival, gathered information from their hospital chart, and spoke with the patients’ relatives who may have witnessed any of the events in question. “Through this, it became clear whether each patient’s EEG was really urgent or not,” said Dr O’Brien, and new urgency scores were reassigned to each case.
As the additional information collected by Dr Brien made significant changes to the perceived urgency of each case compared to the referral form alone, the research
team decided to investigate the quality of referrals the hospital received – the quality was found to be low. There was often a lack of clarity in the forms, and there were issues with legibility. It was concluded that a significant reason for this was the referral form itself. This led to Dr O’Brien updating the referral form, as detailed below.
The old referral form consisted of a number of open-ended questions with large blank spaces for physicians to fill out. In contrast to this, the new referral form is now largely made up of yes/no questions, and tick the box answers. There is also a section on the new form to fill in the date of the most recent event, as an EEG within 24 hours of the event is of particular value. This was thought to be an important addition to the form, as only 15 per cent of referral forms included in the audit included the date of the event. The new form also contains a section for a brief clinical summary of the patient, and space for a “one-liner” that describes the clinical question the team wants to answer with the EEG in order to facilitate more informative results and to help identify any unsuspected abnormalities. A section asking about any medications the patient is on was also included in the new form, as patients on anti-epileptic drugs are considered to be less at risk than those not on these drugs, and if a patient is on sedatives, this may affect the results of the EEG.
Dr O’Brien also highlighted that two patients included in the audit did not attend their outpatient EEG appointment. One of these patients was a suspected epilepsy case. When Dr O’Brien followed up on this patient, it was found that he had frequent emergency department admissions and was of no fixed abode. She concluded that more effort should have been made to treat this patient as an inpatient and that although some cases might not be clinically urgent, circumstances may suggest potential for urgency in some situations as well.
This was discussed with the immunology team, who reported that no specific testing could confirm this allergy. A silicone-free shunt was successfully inserted without complication or subsequent meningitis and the patient is currently symptom free.
Dr Leer highlighted that although silicone elastomers have been presumed to be immunologically inert, delayed hypersensitivity reactions to silicone have been noted, most significantly in relation to the use of silicone breast implants. Dr Leer believes that it is likely that “silicone allergy is an under-recognised cause of shunt complications”, and that a delay in this diagnosis can result in “prolonged courses of antibiotics and external ventricular drainage”.
In patients whom it is suspected a silicone allergy exists, presentation is generally associated with signs of shunt malfunction. This may be attributed to infection of obstruction of the distal catheter with eosinophils and giant cells accumulating at the catheter tip. The CSF may not show overt signs of infection, but the presence of eosinophils will help
Awards
aid the suspected diagnosis. If made early, this diagnosis will reduce the likelihood of repeated hospital admissions and the need for repeated shunt revisions. There are few reports of VP shunt silicone allergy in the literature, but within these reports there are accounts of some serious consequences associated with VP shunt silicone allergy such as a bowel perforation due to erosion by the shunt tubing.
Dr Leer informed the audience that silicone-free polyurethane shunts are comparable to standard silicone shunts with regard to both their function and resistance to malfunction, as the products have similar properties.
Dr Leer concluded that the case report and literature review highlight a rare complication of VP shunting, which can mimic infection or obstruction. The features of this reaction include a predominantly lymphocytic CSF pleocytosis, lack of organisms seen on CSF microscopy or culture, a peripheral eosinophilia and marked tissue reaction to the silicone shunt.
HAROLD MILLER PRIZE FOR BEST OVERALL PRESENTATION
• 1st Eimer Maloney, Cork University Hospital
‘Association between social deprivation and the incidence of first seizures, new diagnosis of epilepsy and seizure mimics.’
• 2nd Olwen Murphy, Johns Hopkins University
‘Early factors associated with later conversion to multiple sclerosis in patients presenting with isolated myelitis.’
JOHN KIRKER PRIZE FOR BEST EPILEPSY RELATED PRESENTATION
• 1st Eimer Maloney, Cork University Hospital
‘Association between social deprivation and the incidence of first seizures, new diagnosis of epilepsy and seizure mimics.’
• 2nd Maeve Bradley, Connolly Hospital
‘An audit of medical admissions for seizures in a model three hospital in Ireland.’
MARK GIBSON PRIZE FOR BEST MOVEMENT DISORDER RELATED PRESENTATION
• 1st Josephine Hebert, Tallaght University Hospital
‘Inherited cerebellar ataxias: Five-year experience of the National Ataxia Clinic in Ireland.’
• 2nd Ciara Hunt, Beaumont Hospital
‘Undiagnosed neuropathology in fallers: Findings from a 10-year autopsy series.’
PRIZE FOR BEST NEUROSURGICAL PRESENTATION
• 1st Ping Hei Cheng, Royal Victoria Hospital, Belfast
‘Management, complications, and neurological outcomes of aneurysmal subarachnoid haemorrhage in elderly patients.’
• 2nd Jack Phillips, Beaumont Hospital
‘Audit of road traffic accidents and whiplash injuries in medical legal practice.’
DR JOHN LYNCH AWARD FOR BEST POSTER PRESENTATION
• 1st Ciara Gorman, Tallaght University Hospital
• 2nd Damien Ferguson, St Vincent’s University Hospital
HUGH STAUNTON PRIZE FOR BEST UNDERGRADUATE OR INTERN PRESENTATION
• 1st Ciara Hunt, Beaumont Hospital
‘Undiagnosed neuropathology in fallers: Findings from a 10-year autopsy series.’
• 2nd Josephine Hebert, Tallaght University Hospital
‘Inherited cerebellar ataxias: Five-year experience of the National Ataxia Clinic in Ireland.’
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 44
IBRANCE®▼PALBOCICLIB PRESCRIBING INFORMATION:
Please refer to the Summary of Product Characteristics (SmPC) before prescribing IBRANCE 75 mg, 100 mg or 125 mg hard capsules. Presentation:
Hard capsules containing 75 mg, 100 mg or 125 mg palbociclib. Indications:
Treatment of hormone receptor (HR) positive, human epidermal growth factor receptor 2 (HER2) negative locally advanced or metastatic breast cancer: in combination with an aromatase inhibitor; or in combination with fulvestrant in women who have received prior endocrine therapy. In pre- or perimenopausal women, the endocrine therapy should be combined with a luteinizing hormone releasing hormone (LHRH) agonist. Dosage: Therapy should be initiated and supervised by a physician experienced in the administration of anti-cancer medicinal products. The recommended dose is 125 mg of palbociclib once daily for 21 consecutive days followed by 7 days off treatment (Schedule 3/1) to comprise a complete cycle of 28 days.
When coadministered with palbociclib, the aromatase inhibitor should be administered according to the dose schedule reported in the SmPC. Treatment of pre/perimenopausal women with the combination of palbociclib plus letrozole should always be combined with an LHRH agonist (see SmPC section 4.4). Capsules should be swallowed (should not be chewed, crushed, or opened prior to swallowing). It should be taken with food, preferably a meal to ensure consistent palbociclib exposure (see SmPC section 5.2). Palbociclib should not be taken with grapefruit or grapefruit juice (see SmPC section 4.5). Dose modification of IBRANCE is recommended based on individual safety and tolerability. Management of some adverse reactions may require temporary dose interruptions/delays, and/or dose reductions, or permanent discontinuation. For dose reduction guidelines for management of adverse reactions, haematologic and non-haematologic toxicities, refer to SmPC section 4.2. Permanently discontinue IBRANCE in patients with severe interstitial lung disease (ILD)/pneumonitis. For patients who experience a maximum of Grade 1 or 2 neutropenia in the first 6 cycles, complete blood counts for subsequent cycles should be monitored every 3 months, prior to the beginning of a cycle and as clinically indicated. No dose adjustments of IBRANCE are required for patients with mild or moderate hepatic impairment (Child-Pugh classes A and B)For patients with severe hepatic impairment (Child-Pugh class C), the recommended dose of IBRANCE is 75 mg once daily on Schedule 3/1 (see SmPC section 5.2). No dose adjustments of IBRANCE are required for patients with mild, moderate or severe renal impairment (creatinine clearance [CrCl] ≥15 mL/min) (see SmPC section 5.2). No dose adjustment of IBRANCE is necessary in patients ≥65 years of age (see section 5.2). Contraindications: Hypersensitivity to the active substance or to any of the excipients (see SmPC section 6.1) use of preparations containing St. John’s Wort (see SmPC section 4.5). Warnings and Precautions: Ovarian ablation or suppression with an
For more information visit www.pfizerpro.ie/product/ibrance
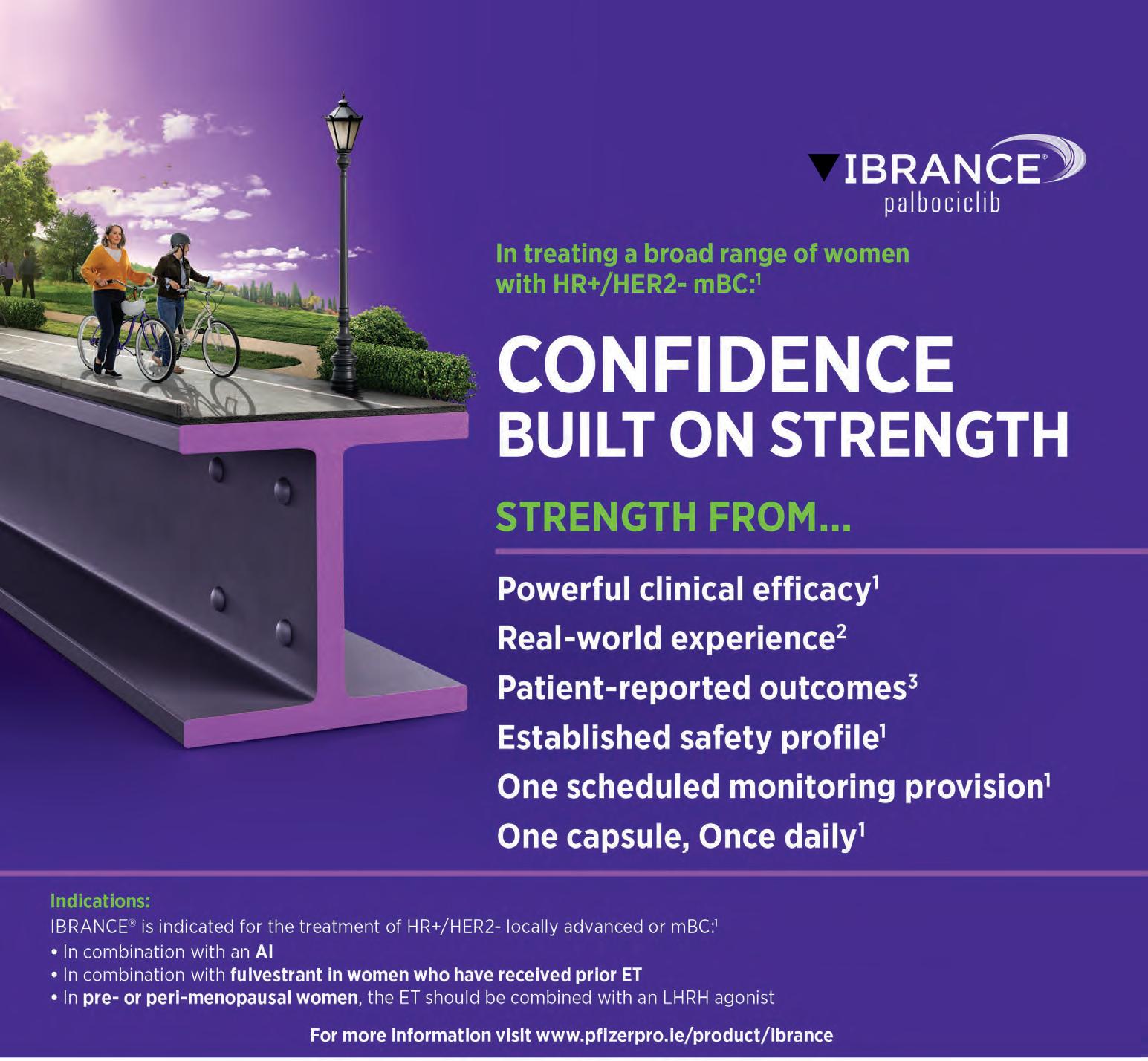
LHRH agonist is mandatory when pre/perimenopausal women are administered IBRANCE in combination with an aromatase inhibitor, due to the mechanism of action of aromatase inhibitors. Palbociclib in combination with fulvestrant in pre/perimenopausal women has only been studied in combination with an LHRH agonist. Dose interruption, dose reduction, or delay in starting treatment cycles is recommended for patients who develop Grade 3 or 4 neutropenia. Appropriate monitoring should be performed (see SmPC sections 4.2 and 4.8). Severe, life- threatening, or fatal ILD and/ or pneumonitis can occur in patients treated with cyclin dependent kinase 4/6 (CDK4/6) inhibitors, including IBRANCE when taken in combination with endocrine therapy. Across clinical trials (PALOMA-1, PALOMA-2, PALOMA-3), 1.4% of IBRANCE-treated patients had ILD/pneumonitis of any grade, 0.1% had Grade 3, and no Grade 4 or fatal cases were reported. Additional cases of ILD/pneumonitis have been observed in the postmarketing setting, with fatalities reported. Monitor patients for pulmonary symptoms and interrupt IBRANCE treatment immediately in patients suspected to have developed ILD/pneumonitis, see SmPC section 4.2, 4.4 and 4.8. Since IBRANCE has myelosuppressive properties, it may predispose patients to infections. Infections have been reported at a higher rate in patients treated with IBRANCE in randomised clinical studies compared to patients treated in the respective comparator arm. Grade 3 and Grade 4 infections occurred respectively in 5.6% and 0.9% of patients treated with IBRANCE in any combination (see SmPC section 4.8). Patients should be monitored for signs and symptoms of infection and treated as medically appropriate (see SmPC section 4.2). Physicians should inform patients to promptly report any episodes of fever. Strong inhibitors of CYP3A4 may lead to increased toxicity (see SmPC section 4.5). Avoid concomitant use of strong CYP3A inhibitors during treatment with palbociclib. Coadministration should only be considered after careful evaluation of the potential benefits and risks. If coadministration with a strong CYP3A inhibitor is unavoidable, reduce the IBRANCE dose to 75 mg once daily. When the strong inhibitor is discontinued, increase the IBRANCE dose (after 3–5 half-lives of the inhibitor) to the dose used prior to the initiation of the strong CYP3A inhibitor (see SmPC section 4.5). Coadministration of CYP3A inducers may lead to decreased palbociclib exposure and consequently a risk for lack of efficacy. Therefore, concomitant use of palbociclib with strong CYP3A4 inducers should be avoided. No dose adjustments are required for coadministration of palbociclib with moderate CYP3A inducers (see SmPC section 4.5). Women of childbearing potential or their male partners must use a highly effective method of contraception while taking IBRANCE (see SmPC section 4.6). IBRANCE contains lactose. Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency, or glucose-galactose malabsorption
PP-IBR-IRL-0323
should not take this medicine. Drug Interactions: The concomitant use of strong CYP3A inhibitors including, but not limited to: clarithromycin, indinavir, itraconazole, ketoconazole, lopinavir/ritonavir, nefazodone, nelfinavir, posaconazole, saquinavir, telaprevir, telithromycin, voriconazole, and grapefruit or grapefruit juice, should be avoided (see sections 4.2 and 4.4). No dose adjustments are needed for mild and moderate CYP3A inhibitors. The concomitant use of strong CYP3A inducers including, but not limited to: carbamazepine, enzalutamide, phenytoin, rifampin, and St. John’s Wort should be avoided (see SmPC sections 4.3 and 4.4). No dose adjustments are required for moderate CYP3A inducers. The dose of sensitive CYP3A substrates with a narrow therapeutic index (e.g., alfentanil, cyclosporine, dihydroergotamine, ergotamine, everolimus, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus) may need to be reduced when coadministered with IBRANCE as IBRANCE may increase their exposure.
Based on in vitro data, palbociclib is predicted to inhibit intestinal Pglycoprotein (P-gp) and breast cancer resistance protein (BCRP) mediated transport. Therefore, administration of palbociclib with medicinal products that are substrates of P-gp (e.g., digoxin, dabigatran, colchicine, pravastatin) or BCRP (e.g., rosuvastatin, sulfasalazine) may increase their therapeutic effect and adverse reactions. Based on in vitro data, palbociclib may inhibit the uptake transporter organic cationic transporter OCT1 and then may increase the exposure of medical product substrates of this transporter (e.g., metformin). Pregnancy & Lactation: Females of childbearing potential who are receiving this medicinal product, or their male partners should use adequate contraceptive methods (e.g., double-barrier contraception) during therapy and for at least 3 weeks or 14 weeks after completing therapy for females and males, respectively (see SmPC section 4.5). There are no or limited amount of data from the use of palbociclib in pregnant women. Studies in animals have shown reproductive toxicity (see SmPC section 5.3). IBRANCE is not recommended during pregnancy and in women of childbearing potential not using contraception. Based on male reproductive organ findings (seminiferous tubule degeneration in testis, epididymal hypospermia, lower sperm motility and density, and decreased prostate secretion) in nonclinical safety studies, male fertility may be compromised by treatment with palbociclib (see SmPC section 5.3). Thus, men may consider sperm preservation prior to beginning therapy with IBRANCE. Driving and operating machinery: IBRANCE may cause fatigue and patients should exercise caution when driving or using machines. Side Effects: The most common (≥20%) adverse reactions of any grade reported in patients receiving palbociclib in randomised clinical studies were neutropenia, infections, leukopenia, fatigue, nausea, stomatitis, anaemia, diarrhoea, alopecia, and thrombocytopenia. The most common (≥2%)
| Date of preparation: July 2020

Grade ≥3 adverse reactions of palbociclib were neutropenia, leukopenia, anaemia, fatigue, infections, alanine aminotransferase (ALT) increased and aspartate aminotransferase (AST) increased. Dose reductions or dose modifications due to any adverse reaction occurred in 38.4% of patients receiving IBRANCE in randomised clinical studies regardless of the combination. Very common adverse events (>1/10) are neutropenia, infections, leukopenia, fatigue, anaemia, asthenia, pyrexia, nausea, stomatitis, alopecia, diarrhoea, thrombocytopenia, vomiting, rash, decreased appetite, dry skin, AST increased, ALT increased and aspartate aminotransferase (AST) increased. Commonly reported adverse events (>1/100 to <1/10), are, dysgeusia, epistaxis, ILD/pneumonitis, lacrimation increased, vision blurred, dry eye, febrile neutropenia. Refer to SmPC for further information on side effects. Refer to section 4.8 of the SmPC for further information on side effects, including description of selected adverse reactions. Legal Category: S1A.
Marketing Authorisation Numbers: EU/1/16/1147/001 – 75mg (21 capsules); EU/1/16/1147/003 – 100mg (21 capsules) EU/1/16/1147/005 – 125mg (21 capsules). Marketing Authorisation Holder: Pfizer Europe MA EEIG, Boulevard de la Plaine 17, 1050 Bruxelles, Belgium. For further information on this medicine please contact: Pfizer Medical Information on 1800 633 363 or at EUMEDINFO@pfizer.com. For queries regarding product availability please contact: Pfizer Healthcare Ireland, Pfizer Building 9, Riverwalk, National Digital Park, Citywest Business Campus, Dublin 24 + 353 1 4676500.
▼This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 of the SmPC for how to report adverse reactions.
Last revised: 06/2020
Ref: IB 8_0
References:
1. IBRANCE® Summary of Product Characteristics.
2. Taylor-Stokes G, et al. Breast. 2019;43:22-27. 3. Rugo HS,et al. Ann Oncol. 2018;29(4):888-894.
AI = aromatase inhibitor; ET = endocrine therapy; HR+/HER2- = hormone receptor-positive, human epidermal growth factor receptor 2-negative; LHRH = luteinising hormone releasing hormone; mBC = metastatic breast cancer; SmPC = summary of product characteristics.
Conference Preview
Gathering Around Cancer 2020, 5-6 November, virtual meeting live from Croke Park Convention Centre, Dublin






Gathering together, while standing apart
We preview this year’s Gathering Around Cancer meeting, which will take place on a virtual basis early next month
This year, due to the prevailing Covid-19 public health restrictions, the Gathering Around Cancer annual meeting will be delivered on a virtual platform and be broadcast live from Dublin on the 5 and 6 November.
“In this, the eighth iteration of the meeting, the goal of gathering the Irish oncology Diaspora and their mentors and friends, to learn from each other and to share research ideas, has never been as relevant,” according to the Prof David Gallagher, Consultant Medical Oncologist and Consultant Medical Geneticist, St James’s Hospital; and Prof John McCaffrey, Consultant Medical Oncologist, Mater Misericordiae University Hospital, of the meeting’s organising committee.
“Gathering together while standing apart,” is the maxim of this year’s meeting.
As in previous years, the meeting aims to focus on the topics that change the way the management of cancer is approached, with a focus on clinical updates, amending care pathways during this pandemic, while still fostering research collaborations.
The organisers have responded to feed-
back regarding topics and areas of interest from delegates and will be asking for feedback during and after this year’s event.
“In particular, in areas of speciality nursing, and the allied medical professions, it would be very useful to tell us about the topics you would like discussed and the speakers whom you would like to address the meeting in the future,” according to the organisers.
Irish investigators abroad
The first session of the meeting focuses on Irish investigators abroad. Presentations range from leveraging molecular data in trial design and for biomarker identification, to the role of stereotactic radiation in oligometastatic disease. The speakers during the session are: Dr Deirdre Kelly, Princess Margaret Cancer Centre, Toronto; Dr Jack Gleeson, Memorial Sloan Kettering Cancer Centre, New York; Dr Grainne O’Kane, Princess Margaret Cancer Centre, Toronto; Dr Dan Cagney, Dana Farber Cancer Institute, Boston; and Dr Louise Connell, Memorial Sloan Kettering Cancer Centre, New York.
Covid-19
The second session of the meeting will be on areas of specialist interest, while the third and final session of the first day is on lessons learned during the Covid-19 pandemic. Dr Melissa Lumish and Dr Yelena Janjigian, Memorial Sloan Kettering Cancer Centre, New York, will speak about chemotherapy and Covid-19 outcomes in patients with cancer.
Dr Anne Horgan, University Hospital Waterford, will give a talk entitled ‘Treating older patients with cancer during Covid-19’.
Dr Colm Henry, Chief Clinical Officer, HSE, and Prof Paddy Mallon, St Vincent’s University Hospital, Dublin, will also give talks on the lessons learned during the pandemic and the overall national strategy to limit the spread of the virus.
Burnout
The topic of the keynote speech is ‘resilience and burnout’, which will be delivered by Dr Dean Bajorin, Memorial Sloan Kettering Cancer Centre, New York.

Dr Bajorin’s expertise is in the treatment of genitourinary tumours, particularly bladder and testicular cancers.
His research on testicular cancer has been directed toward decreasing the side effects of chemotherapy drugs and evaluating biological characteristics of tumours to predict treatment response.
Dr Bajorin has received a number of honours and awards for his work, including, in 2011, the Statesmen Award from the American Society of Clinical Oncology (ASCO), which recognises certain members for more than 20 years of extraordinary volunteer service, dedication, and commitment.
Among other contributions he also helped ASCO shape a new strategic plan to address the looming shortage of oncologists in the United States by 2020 – including the development of innovative practice arrangements.
Updates
The second day of the meeting will consist of updates on the following areas: Medical oncology; breast cancer; genitourinary cancer; and gastro-intestinal cancer. The closing remarks of the conference will be delivered by Prof McCaffrey and Prof Gallagher. A total of 12 CPD credits have been awarded for this meeting by the RCPI.
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 48
Pictured L to R: Prof Sir Michael Stratton, Wellcome Sanger Institute, Cambridge; Prof David Gallagher, St James’s Hospital, Dublin; and Prof Rosalind Eeles, Royal Marsden Hospital and Institute of Cancer Research, UK
Mr Michael Farrell, the Mater Private Hospital, Dublin
Delegates at the Gathering Around Cancer conference last year
Prof John McCaffrey, Mater Misericordiae University Hospital, Dublin
Conference Gallery archive More on www.mindo.ie Gathering Around Cancer 2019, 7-8 November, Croke Park Convention Centre, Dublin
Prof Ciaran Johnston, St James’s Hospital, Dublin Dr Karen Cadoo, Memorial Sloan Kettering, New York
SUTENT® Capsules (sunitinib malate)

PRESCRIBING INFORMATION – IRELAND
Please refer to the Summary of Product Characteristics (SmPC) before prescribing SUTENT 12.5 mg, 25 mg or 50 mg. Presentation: Hard gelatin capsules containing sunitinib malate equivalent to 12.5 mg, 25 mg and 50 mg sunitinib. Indications: For the treatment of unresectable and/or metastatic malignant gastrointestinal stromal tumour (GIST) in adults after failure of imatinib treatment due to resistance or intolerance; advanced and/or metastatic renal cell carcinoma (MRCC) in adults; unresectable or metastatic, well differentiated pancreatic neuroendocrine tumours (pNET) with disease progression in adults. Dosage: Therapy should be initiated by a physician experienced in the administration of anticancer agents. The recommended dose for GIST and MRCC is 50 mg taken orally, once daily, with or without food, for 4 consecutive weeks, followed by a 2-week rest period, to comprise a complete cycle of 6 weeks. For pNET 37.5 mg taken orally once daily without a scheduled rest period. Dose modifications in 12.5 mg steps may be applied based on individual safety and tolerability. Daily dose should not exceed 75 mg nor be decreased below 25 mg for GIST or MRCC, the maximum daily dose administered during the phase 3 pNET study was 50 mg. The safety and efficacy of Sutent in patients below 18 years of age have not been established and no recommendation on a posology can be made. Contra-indications: Hypersensitivity to the active substance or to any of the excipients. Special warnings and precautions for use: Co-administration of potent CYP3A4 inhibitors or inducers should be avoided if possible, or the dose of sunitinib altered. Depigmentation of the hair or skin and occasional rash affecting the palms of hands and soles of feet commonly occur during treatment. Pyoderma gangrenosum, generally reversible after drug discontinuation, has been reported. Severe cutaneous reactions have been reported, including cases of erythema multiforme (EM) and cases suggestive of Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), some of which were fatal. If signs or symptoms of SJS, TEN, or EM are present, sunitinib treatment should be discontinued. Haemorrhagic events, some of which were fatal have been reported. Serious, sometimes fatal gastrointestinal complications have occurred in patients with intra-abdominal malignancies. Patients should be screened for hypertension and controlled as appropriate. Temporary suspension is recommended in patients with severe hypertension that is not controlled with medical management. Decreased absolute neutrophil and platelet counts occurred during clinical trials and complete blood counts should be performed at the beginning of each treatment cycle. Cardiovascular events, including CHF, cardiomyopathy and myocardial ischemia and myocardial infarction, some of which were fatal, have been reported. Closely monitor for clinical signs and symptoms of CHF and consider baseline and periodic evaluations of LVEF especially in patients with cardiac risk factors and/or history of coronary artery disease. If clinical manifestations of CHF present, discontinuation of sunitinib is recommended. The administration of sunitinib should be interrupted and/or dose reduced in patients without clinical evidence of CHF but with a LVEF <50% and >20% below baseline. Sunitinib should be used with caution in patients with a known history of QT interval prolongation, patients who are taking antiarrhythmics or medicinal products that can prolong QT intervals, or patients with relevant pre-existing cardiac disease, bradycardia, or electrolyte disturbances. Treatment-related venous thromboembolic events have been reported. Arterial thromboembolic events (ATE), sometimes fatal, have been reported including cerebrovascular accident, transient ischaemic attack, and cerebral infarction. The use of vascular endothelial growth factor (VEGF) pathway inhibitors in patients with or without hypertension may promote the formation of aneurysms and/or artery dissections. Thrombotic Microangiopathy (TMA), including thrombotic thrombocytopenic purpura (TTP) and haemolytic uraemic syndrome (HUS), sometimes leading to renal failure and/or a fatal outcome, has been reported with sunitinib as monotherapy and in combination with bevacizumab. Sunitinib therapy should be discontinued in patients who develop TMA and prompt treatment is required. Baseline lab measurements and monitoring of thyroid function during treatment are required and patients treated as per standard medical practice. Pancreatitis and serious pancreatic events, some with fatal outcome have been reported. Hepatotoxicity has been observed in patients treated with sunitinib. Monitor liver function tests at baseline during each cycle of treatment, and as clinically indicated. If symptoms of pancreatitis or hepatic failure are present, treatment with sunitinib should be discontinued and the patient provided with appropriate supportive care. Cases of renal impairment, renal failure and/or acute renal failure, in some cases with fatal outcome, have been reported. Baseline urinalysis is recommended. Patients should be monitored for the development or worsening of proteinuria. Sunitinib should be discontinued in patients with nephrotic syndrome. If fistula formation occurs, treatment with sunitinib should be interrupted. Cases of impaired wound healing have been reported during sunitinib therapy and the decision to resume sunitinib therapy following a major surgical intervention should be based upon clinical judgment of recovery from surgery. Osteonecrosis of the jaw (ONJ) has been reported, the majority of cases occurred in patients who had received prior or concomitant treatment with IV bisphosphonates. Caution should therefore be exercised when sunitinib and IV bisphosphonates are used either simultaneously or sequentially. Prior to treatment with sunitinib either along with or subsequent to IV bisphosphonates, a dental examination and appropriate preventative dentistry should be considered. Invasive dental procedures are also an identified risk factor and should be avoided if possible. In case of angioedema due to hypersensitivity, treatment with sunitinib should be interrupted and medical care provided. Patients with seizures and signs/symptoms consistent with reversible posterior leukoencephalopathy syndrome should be controlled with medical management, including control of hypertension as above and temporary suspension of sunitinib is recommended. Cases of Tumour Lysis Syndrome, some fatal,
have been reported. Patients should be monitored closely and treated as clinically indicated and prophylactic hydration should be considered. Serious infectionswith or without neutropenia, including some with a fatal outcome, have been reported. Uncommon cases of necrotising fasciitis, including of the perineum, sometimes fatal, have been reported. Sunitinib therapy should be discontinued in patients who develop necrotising fasciitis, and appropriate treatment should be promptly initiated. During sunitinib treatment, decreases in blood sugar leading to loss of consciousness have been reported. In case of symptomatic hypoglycemia, sunitinib should be temporarily interrupted. Blood glucose levels in diabetic patients should be checked regularly in order to assess if anti-diabetic drug dosage needs to be adjusted to minimize the risk of hypoglycaemia. Other interactions: None. Fertility, pregnancy and lactation: Women of childbearing potential should be advised to use effective contraception and avoid becoming pregnant while receiving treatment with Sunitinib. Sunitinib should be used during pregnancy only if the potential benefit to the mother justifies the potential risk to the foetus and is not recommended during breast-feeding. Fertility may be compromised during treatment with sunitinib. Driving and operating machinery: Patients should be advised that they may experience dizziness during treatment with sunitinib. Undesirable effects: The most important treatment-related serious adverse reactions associated with sunitinib, some fatal, are renal failure, heart failure, pulmonary embolism, gastrointestinal perforation, haemorrhages (e.g. respiratory tract, gastrointestinal, tumour, urinary tract, and brain haemorrhages) and colitis (colitis and colitis ischaemic). Very common adverse events are neutropenia, thrombocytopenia, anaemia, leukopoenia, hypothyroidism, decreased appetite, insomnia, dizziness, headache, taste disturbance, hypertension, dyspnoea, epistaxis, cough, stomatitis, abdominal pain, vomiting, diarrhoea, dyspepsia, nausea, constipation, skin discolouration, palmar-plantar erythrodysaesthesia syndrome, rash, hair colour changes, dry skin, pain in extremity, arthralgia, back pain, mucosal inflammation, fatigue, oedema, pyrexia. Commonly reported adverse events are viral infections, respiratory infections, abscess, fungal infections, urinary tract infection, skin infections, sepsis, lymphopoenia, dehydration, hypoglycaemia, depression, neuropathy peripheral, paraesthesia, hypoaesthesia, hyperaesthesia, periorbital oedema, eyelid oedema, lacrimation increased, myocardial ischemia, ejection fraction decreased, deep vein thrombosis, hot flush, flushing, pulmonary embolism, pleural effusion, haemoptysis, dyspnoea exertional, oropharyngeal pain, nasal congestion, nasal dryness, gastro-oesophageal reflux disease, dysphagia, gastrointestinal haemorrhage, oesophagitis, abdominal distention, abdominal discomfort, rectal haemorrhage, gingival bleeding, mouth ulceration, proctalgia, cheilitis, haemorrhoids, glossodynia, oral pain, dry mouth, flatulence, oral discomfort, eructation, skin exfoliation, skin reaction, eczema, blister, erythema, alopecia, acne, pruritus, skin hyperpigmentation, skin lesion, hyperkeratosis, dermatitis, nail disorder, myalgia, musculoskeletal pain, muscle spasms, muscular weakness, renal failure, renal failure acute, chromaturia, proteinuria, chest pain, pain, influenza like illness, chills, weight decreased, white blood cell count decreased, lipase increased, platelet count decreased, haemoglobin decreased, amylase increased, aspartate aminotransferase increased, alanine aminotransferase increased, blood creatinine increased, blood pressure increased, blood uric acid increased. Refer to SmPC for information on other adverse effects. Legal Category: S1A. MARKETING AUTHORISATION NUMBER(S) EU/1/06/347/001 - EU/1/06/347/008. Not all pack sizes may be marketed. The Marketing Authorisation Holder: Pfizer Europe MA EEIG, Boulevard de la Plaine 17, 1050 Bruxelles, Belgium. For further information on this medicine please contact: Pfizer Medical Information on 1800 633 363 or at EUMEDINFO@pfizer.com. For queries regarding product availability please contact: Pfizer Healthcare Ireland, Pfizer Building 9, Riverwalk, National Digital Park, Citywest Business Campus, Dublin 24 + 353 1 4676500. Last revised: 10/2019. Ref: ST 27_0
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions to Pfizer on 1800 633 363 or they can be reported directly via the HPRA Pharmacovigilance, Earlsfort Terrace. IRL-Dublin 2. Tel +353 1 6764971. Fax: +353 1 6762517. Website: www.hpra.ie, Email: medsafety@hrpa.ie.
References:
1. Motzer RJ, et al. J Clin Oncol 2009;27:3584–3590.
3. Rini BI, et al. ECC. 25–29 September 2015. Vienna, Austria. Abstract: 17LBA. 4. Motzer RJ, et al. J Clin Oncol 2014;32:2765–2772.
2. Motzer RJ, et al. N Engl J Med 2013;369:722–731.
7. Castellano D, et al. Cancer Treat Rev 2013;39:230–240. 8. Schmidinger M, et al. Cancer Invest 2010;28:856–864. 9. Sutent Summary of Product Characteristics.
5. Négrier S. Oncology 2012;82:189–196. 6. Schmidinger M, et al. Ther Adv Urol 2012;4:253–265.
Date of Preparation: November 2019 PP-SUT-IRL-0128
Life Motoring

The BMW you have dreamed about becomes reality


What if I told you that you could have it all? Your cake and eat it too. A fourdoor, family car that looks fresh and sporty; that’s a plug-in hybrid; that produces almost 300hp; that handles like a sporty coupe and all for (potentially) less than €50,000? Oh, and did I mention it’s a BMW? That ringing in your ears is not your alarm clock, this is not a dream; it’s the sound of your soul realising that perfection does exist. It is attainable and it’s called the BMW 330e. I have driven and written about a lot of boring cars. The BMW 330e I tested for a week, however, is poetry in motion. I’ve owned two 3-Series, a 1994 e36 316 and a 2005 e46 318,
and both were painfully slow, but very pretty. This new hybrid 330e is a very different beast, with its silent, torquey, electric city cruising, its mix-and-match dual carriageway driving and barnstorming motorway performance. All while looking great, being comfortable, and making the most of modern technology.
This new 330e is no slouch in the tech department, with a decent infotainment system and a cool satnav feature that plans your route and optimises your battery and engine usage to make the most of your fuel consumption for the given journey. It also has 360 cameras that also act as dashcams. The 330e is also packing a new Xtraboost system, which gives the driver an extra 40hp for 10 seconds when you floor it in sport mode. A delicious orchestra of fake engine note is also pumped into the cabin, added to the theatre of the Xtraboost.

Inside the car is beautifully finished with sporty, figure-hugging seats in the front and space for three six foot males to sit relatively comfortably in the back. There is a nice, central armrest back there, with cupholders, but a noticeable lack of USB charging points. In the front there is a range of digital information on the dash and on the infotainment system, which, if I’m honest, I found to be a little
busy and cluttered. There are plenty of cupholders, a small glovebox, and whatever material the steering wheel was made out of felt like some manner of futuristic rubber. The boot is smaller than it should be because of the large battery and fuel tank and BMW rudely plonk two bags of cables in there too, with no cubby hole or something for them. The car handles very well for all the weight in the back, it accelerates beautifully, but the brakes can be a little jerky.
50 THE MEDICAL INDEPENDENT | 26 OCTOBER 2020
MORGAN FLANAGAN CREAGH
Read more at www.mindo.ie @MorganFlanaganC
However, this car’s party piece is the tax breaks you could avail of that might bring the overall costs plummeting down. If the current Government doesn’t remove the SEAI grant for plug-in-hybrids you should be able to claim back €5,000 on the purchase of this car, not to mention the potential rebate on vehicle registration tax, which could take around €7,500 off the price of the car.

The model I tested started at €52,480 and if all the Govern-
ment supports remain in place it could be yours for a relatively thrifty €44,980. I must note that my test model had a multitude of bells and whistles that put the final price up to €55,378, without the reductions.
Class is timeless, as is the 3-Series. If you have babies the boot will be too small for your buggy etc. Otherwise, you should drop what you’re doing, go to the dealership and test drive this car immediately.


Motoring Life
Prices∗ (incl VAT and VRT)
G20 330e M Sport Saloon XB1G 2.0i €52,480.00
Mineral White €0.00
Black with grey contrast stitching
Vernasca leather €0.00
Sub Total €52,480.00
OPTIONS
M Sport Plus Pack €2,898.99
• 19” RFT Bicolour Jet Black 791 M light double-spoke alloy wheels
• M sport braking system
• Adaptive M sport suspension
• Variable sport steering
• Sun protection glass
• M seat belts
• M rear spoiler
• BMW Individual high-gloss shadow Line with extended contents
• Run-flat tyres
• Sport seats, front
• Aluminium mesh effect interior trim
• Speedometer w/KMH readout
• M steering wheel
• M aerodynamic bodystyling
•Exterior trim, high-gloss shadowline
•Headlining, anthracite €0.00
Sub Total €2,898.99
Standard Options
• M sport package
• LED foglights, front
• Sport automatic transmission
• Alarm system (Thatcham 1)
• Acoustic glazing
• First-aid kit and triangle
• Exterior mirrors - folding with anti-dazzle
• Rear-view mirror, auto dimming
• Split-folding rear seats
• Seat heating, front
• eDrive exterior sound
• Ambient lighting
• Automatic air conditioning
• Cruise control with brake function
• Adaptive LED Headlights
• Active guard plus
• Passenger airbag deactivation, front
• Head restraints, rear and folding
• Parking assistant
• DAB digital radio
• BMW TeleServices
• Legal emergency call
• eDrive services
• BMW online services
• Connected package professional
• BMW live cockpit professional
Total Vehicle Price €55,378.99
51 THE MEDICAL INDEPENDENT | 26 OCTOBER 2020
BMW G20 330E M SPORT SALOON
There are plenty of cupholders, a small glovebox, and whatever material the steering wheel was made out of felt like some manner of futuristic rubber
Life Mindo Quizzes
26 October 2020
Q1 Rafael Nadal equalled Roger Federer’s record of how many Grand Slam singles titles, after winning the French Open last month?
Q2 Who won the 2020 Giro d’Italia?
Q3 Who did the Exeter Chiefs defeat to win their first Heineken European Champions cup?
Q4 Name the former Premier League manager who has just released his autobiography, My Life in Red and White?
Q5 Which two teams are contesting baseball’s World Series this month?
Q6 Which Scottish football club play at Easter Road?
The winner of the 5 October Sporting Quiz Competition is Dr Donal Nugent, Co Galway
The winner of the 5 October 2020 Crossword is Dr Eadaoin O’Keane, Co Wicklow
Q1 Which golfer won the Dubai Duty Free Irish Open? A: John Catlin
Q2 For the first time ever two of cycling’s grand tours will overlap, when staged this month. They are the Giro d’Italia and which other event? A: Vuelta Espana
Q3 Who won the Russian Grand Prix in Sochi last month? A: Valtteri Bottas
Q4 Which Italian club knocked Shamrock Rovers out of the Europa league last month? A: AC Milan
Q5 The All-Ireland GAA championship will finally commence in the coming weeks. Who are the defending hurling champions? A: Tipperary
Q6 Name the Cork teenager who knocked world champion Ronnie O’Sullivan out of the European Masters snooker championships last month? A: Aaron Hill
ACROSS
8 Relating to a company (9)
9 One circuit of a track (3)
10 Not at all (5)
11 Have (7)
12 Permission (7)
13 Among (4)
17 Tilt to one side (4)
18 Greatest amount possible (7)
22 Convey a thought in words (7)
24 Later (5)
DOWN
1 Perfume (5)
2 Prior (8)
Down
1 - Perfume (5)
3 Activity of travelling for pleasure (7)
4 Occur (6)
5 Wild animal ( 5)
2 - Prior (8)
3 - Activity of travelling for pleasure (7)
6 Primary colour (4)
7 One event in a sequence (7)
4 - Occur (6)
14 Large pile of something (8)
15 Forbidden by law (7)
5 - Wild animal (5)
16 Organic nutrient (7)
13 - Among (4)
25 Put a question
17 - Tilt to one side (4)
18
- Greatest amount possible (7)
22 - Convey a thought in words (7)
24 - Later (5)
25 - Put a question to (3)
26 - Doubt about someone's honesty (9)
19 Suppor t; help (6)
20 Compact (5)
6 - Primary colour (4)
7 - One event in a sequence (7)
21 Impress on paper (5)
23 Prod (4)
14 - Large pile of something (8)
15 - Forbidden by law (7)
16 - Organic nutrient (7)
19 - Support; help (6)
20 - Compact (5)
21 - Impress on paper (5)
23 - Prod (4)
52
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 Post your answers to: Mindo Quizzes, The Medical Independent, Greencross Publishing Ltd, Top Floor, 111 Rathmines Road Lr, Dublin 6. Closing date for entries is 5 November 2020
QUIZ WIN €50 CROSSWORD COMPETITION 26 October 2020 WIN €50 Solution to Crossword Competition
SPORTS
Answers to Sports Quiz Competition Solution to Sudoku C I V I C B R E A T H E O E I A U O M R R N S T O R Y M U S I C I A N H S I I U N H O N E Y T R O P I C A L R E T N T P M S E F P L E A S A N T E N T R Y A S N E I E O U T S I D E R A G R E E N A A D H Z C G T A S T R E T C H E N E M Y 4 5 7 3 1 2 8 9 6 1 8 6 9 5 7 2 4 3 9 2 3 6 4 8 1 5 7 8 1 4 2 3 5 6 7 9 6 7 2 4 9 1 3 8 5 5 3 9 7 8 6 4 2 1 2 6 8 5 7 3 9 1 4 7 4 1 8 6 9 5 3 2 3 9 5 1 2 4 7 6 8 1 2 3 4 5 6 7 8 9 10 11 12 1314 15 16 17 1819 20 21 22 23 24 25 26 Across 8 - Relating to a company (9) 9 - One circuit of a track (3) 10 - Not at all (5) 11 - Have (7) 12 - Permission (7)
to (3) 26 Doubt about someone’s honesty (9)
7 9 4 5 7 9 6 3 7 2 3 5 8 4 7 3 6 1 2 2 9 4 3 6
SUDOKU SCRIBBLE BOX
5 OCTOBER 2020 ANSWERS, SOLUTIONS, AND WINNERS
CLONMEL HEALTHCARE ACQUIRES TIPOL, CO-TIPOL AND TEFIN IN IRELAND Clonmel Healthcare has announced that it has acquired the brands Tipol, Co-Tipol and Tefin in Ireland.
The full Tipol range includes:
● Tipol 75mg Suppositories (see note 1) Paracetamol.
● Tipol 125mg Suppositories (see note 1) Paracetamol.
● Tipol 250mg Suppositories (see note 2) Paracetamol.
● Tipol 500mg Suppositories (see note 2) Paracetamol.
● Tipol Max 1,000mg Suppositories (see note 2) Paracetamol.
● Tipol Suppositories (paracetamol) are the only complete range of paracetamol suppositories with dosing tables by both age and bodyweight for infants (3kg and over), children and adults.
The full Co-Tipol range includes:
● Co-Tipol 500mg/30mg Suppositories (see note 1) Paracetamol + Codeine.
● Co-Tipol Max 1,000mg/60mg Suppositories (see note 1) Paracetamol plus Codeine.


The full Tefin range includes:
● Tefin 75mg Suppositories (see note 2) Ibuprofen.
● Tefin 150mg Suppositories (see note 2) Ibuprofen.
Tefin Suppositories Ibuprofen 75mg and 150mg are the only ibuprofen suppositories on the GMS and community drug schemes.

In the past few months Clonmel Healthcare has worked very closely with Carysfort Healthcare to ensure the smooth transition, particularly relating to customer care and distribution.
MEDTECH RISING LEADERS’ CONFERENCE SETS OUT VISION TO MAKE IRELAND GLOBAL LEADER IN PATIENT-CENTRED MEDTECH
To mark the sixth annual European MedTech Week, the Irish Medtech Association, the Ibec group that represents the sector, has launched ‘Medtech Rising: The Business Leaders’ Conference’, jointly hosted with Enterprise Ireland and IDA Ireland. In light of Covid-19, the event will be held virtually on 2-3 December. European MedTech Week is a special week dedicated to showcasing the value of life-changing technologies developed by the medtech industry.
Irish Medtech Association Director Ms Sinead Keogh said: “Ireland is one of the top five global medtech hubs, ensuring that business leaders get the latest industry foresight and share best practice is essential to our success. That’s why Medtech Rising is an unmissable event, with speakers like Medtronic Chairman and Intel Chairman Omar Ishrak, Alcon President and General Manager Global Surgical Franchise Jeannette Bankes joining policymakers, clinicians and other experts to share their insights on the latest global trends.
“The medtech industry’s role in saving and transforming lives has been highlighted by the Covid-19 pandemic. Ireland stands out internationally as one of the top five producers of Covid related goods according
to the OECD, after Germany, the US, Switzerland and China. That’s why we’re proud to exceptionally introduce a ‘Covid-19 Response Recognition Award’ for the Irish Medtech Awards 2020.”
IDA Ireland’s Head of Medical Technologies Ms Rachel Shelly said: “Ireland’s position as a location of choice for the medtech industry and its role as an agile, resilient hub within global supply chain networks has been reinforced since the outbreak of the pandemic. With continued global uncertainty ahead, global conferences like Medtech Rising are essential to equip business leaders with the latest industry insight and perspectives.”
Enterprise Ireland Manager of Lifesciences Ms Deirdre Glenn added: “When the Covid-19 pandemic first emerged and as it quickly took hold across the world, a substantial number of Enterprise Ireland client companies immediately set about responding through innovation. Irish companies operating in areas such as medical devices, diagnostics, medical sub-supply and digital health have managed to pivot in a rapidly changing business environment, proving the resilience and strength of the sector in Ireland.”
Full prescribing information is available on request. Contact Clonmel Healthcare on 01 620 4000 if further information is required.
Note 1. Medicinal product subject to medical prescription.
Note 2. For retail sale through pharmacy only.
WATERSTONE CLINIC
Clinical Associate in Reproductive Medicine Opportunity to Train
Waterstone Clinic is one of Ireland’s leading providers of fertility and women’s health services. At the forefront of IVF technology for over 18 years, Waterstone Clinic continues to expand and will open its new premises in Dublin later this year.
Applications are invited for the post of Clinical Associate in Reproductive Medicine
This is a trainee position where applicants will be given the opportunity to develop skills in assisted conception, including patient consultation, ultrasound scanning and theatre procedures including oocyte retrieval and embryo transfer.
The successful candidate may have some OBGYN experience or be currently working in a GP practice with an interest in women’s health. Applicants must be eligible for full IMC registration and have some practical gynaecological skills. We are seeking highly motivated individuals who will be committed to maximising outcomes for patients.
To Apply
Send your CV and cover letter to HR at careers@waterstoneclinic.ie

To discuss in strict confidence, contact Clinic Director Susan Waterstone susan@waterstoneclinic.ie
For more information, see www.waterstoneclinic.ie/careers DUBLIN
PREMISES AVAILABLE
Irish Practice Nurse Association have an exciting opportunity for someone with the drive and eagerness to participate in and contribute to the growth of our organisation in the role of Membership & Social Media Officer, working remotely 15 hours a week.

RESPONSIBILITIES & DUTIES
Work as part of a team
Provide administrative support to build and maintain membership
Maintain central registration facility in line with Data Protection policy
Website management and co-ordination - including the management of educational content on digital platforms
Respond to member’s queries in a timely manner
Maximise IPNA’s profile and Membership through Social Media platforms
Support annual conference committee
Other duties as assigned by the elected IPNA National Chairperson
Full Job specification is available by contacting Caroline Daughton IPNA administrator Email admin@irishpracticenurses.ie

Closing date for applications Friday 27th Nov
Medical suites available in Dublin 2 (close
to dawson street luas)
Medical Suites available at 26 Clare Street, Dublin 2. Adjacent to the National Gallery.
Suitable for a range of medical uses including GP Practice - Private or GMSOut-of-Hours Service or Walk In Clinic - Physio Clinic - Beauty Clinic, etc.
Full medical planning permission.
These suites would suit many uses due to the high footfall passing the door every day. The suites are 5 minutes walk from Grafton Street with several amenities close by. There is direct access from all areas of Dublin to the suites via the Dart and Bus and The Luas runs to Dawson Street, 5 minutes walk away. There is a big concentration of new businesses in the area. Trinity College, Merrion Square and Pearse Street are on the doorstep. Very favourable and flexible terms.
2 Suites available ❚ self-contained ❚ bathroom/waiting room/consulting rooms ❚ 440sq feet and 690sq feet ❚ both newly renovated ❚ high speed broadband, etc. Please contact Mary Anne on 087 6394946 for further information or to arrange viewing
Product Focus RXDX THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 53
24062020_MEDICALSUITESD2_MINDO.indd 1 24/06/2020 18:17
| CORK | KILDARE| LIMERICK
WATERFORD
|
CENTRES FOR REPRODUCTIVE MEDICINE
Classifieds & Recruitment
Advertise today, email louis@mindo.ie
GP REQUIRED
GP REQUIRED FOR CORK CITY PRACTICE
GP required for busy Cork City centre practice. Fully computerised. Fully supported with 2 doctors, 2 nurses, admin staff, and practice manager. No house calls. Parking provided.
4-to-6 sessions available per week.
Please contact Maria for more details at maria.odriscoll@gtv.ie
PRACTICE NURSE REQUIRED
SINGLE HANDED PRACTICE IN KILKENNY CITY requires full-time practice nurse with drive and motivation. Experience desired, but not essential. CV to kilkennydoc2020@gmail.com
ASSISTANT REQUIRED
FULL-TIME ASSISTANT REQUIRED FOR PLEASANT RURAL PRACTICE IN COOLE, CO WESTMEATH.
GP REQUIRED WITH INTEREST IN WOMEN’S HEALTH IN DUNDALK
GP required on a long-term basis either full-time or part-time. Full computerised. We have full nursing and administrative support with no out-of-hours or weekend work. We are a longestablished family-friendly progressive practice. If interested and would like more information:
Please email to: parkavenuesurgery@gmail.com
ROOMS TO RENT
CLINICAL ROOMS TO RENT ABOVE BUSY GP PRACTICE AT KIMMAGE MEDICAL CENTRE ON KIMMAGE ROAD WEST. Suitable for allied medical/healthcare practitioners. For further information please contact bercoveney@hotmail.com or call 086 851 8183
To advertise, email Louis at louis@mindo.ie
GP REQUIRED LONG-TERM – CO LOUTH
• Permanent GP required in an established, well located, busy and growing practice

• Partnership opportunity with immediate profit-share option for the right person
• Immediate start available with long-term potential
• Between 6 – 8 sessions available immediately and increasing
• Excellent nurse and admin support
• Fully computerised using Socrates

• MICGP/MRCGP or equivalent essential
Contact: dundealgandoc@gmail.com
54
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020 Thursday 5th & Friday 6th November 2020 For further information please contact the conference secretariat, Global Teamwork: Tel: 01 265 0001 Email: kelly@globalteamwork.ie www.gatheringaroundcancer.com Register now VIRTUAL MEETING 2020 REGISTER NOW 35591_GAC_ad_170x252mm_Layout 1 25/09/2020 11:35 Page 1
1 hour from Dublin. Attractive terms and
conditions on offer. Please forward CV and references to drpatcullen@gmail.com
Advertise today, email louis@mindo.ie

NATIONAL BASIC SPECIALIST TRAINING IN PSYCHIATRY
JULY 2021 INTAKE
Applications are invited for the Basic Specialist Training Deaneries accredited by the College of Psychiatrists of Ireland. Details of the individual Deaneries and how to apply are available on the College’s website www.irishpsychiatry.ie
Trainees who successfully complete the BST programme will be automatically eligible for Higher Specialist Training in Psychiatry.
Closing date for receipt of applications is Thursday, 3rd December 2020 at 5pm.
Shortlisting will apply and will be based on information supplied by applicants on their application form. Successful applicants must be entered on the Trainee Specialist Division of the Medical Register maintained by the Medical Council of Ireland by 12th July 2021 to take up their appointment.
Shortlisted candidates will be interviewed on Thursday, 28th January 2021
Monday 30th November 2020 15.00 – 18.10 & Tuesday 1st December 2020 09.00 – 12.00 REGISTRATION



NATIONAL HIGHER SPECIALIST TRAINING IN PSYCHIATRY
JULY 2021 INTAKE
Applications are invited for the College of Psychiatrists of Ireland accredited National Higher Training Schemes in:


(i) Child and Adolescent Psychiatry and






(ii) Specialties of Adult Psychiatry


Applicants are also invited to apply for a part-time/flexible training.
Details on how to apply are available on the College’s website www.irishpsychiatry.ie

Closing date for receipt of applications is Friday 15th January 2021 at 5pm
Shortlisting will apply and will be based on information supplied by applicants on their application form.
Successful applicants must be entered on the Trainee Specialist Division of the Medical Register maintained by the Medical Council of Ireland by 12th July 2021 to take up their appointment.
Interviews for shortlisted candidates will take place on Wednesday 24th February 2021 for both Adult and CAP.
Please enter code: NHIR2020 Supported by:
55 Recruitment & Classifieds
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020
On the Medical Council of Ireland’s “Your Training Counts” National Trainee Survey, training in Psychiatry has received the highest D-RECT score (overall Trainee satisfaction) for the last two years.
On the Medical Council of Ireland’s “Your Training Counts” National Trainee Survey, training in Psychiatry has received the highest D-RECT score
Trainee satisfaction)
the last two
(overall
for
years.
NEW HORIZONS IN RHEUMATOLOGY
Virtual
Event managed by:
A
Experience
IS
FREE To register visit: www.newhorizonsinrheumatology.com
For further information please contact: fiona@ccis.ie REGISTER NOW!
If you have anything you would like to share, please email: info@mindo.ie
An embarrassment of data riches — Covid-19 tracking apps in South Korea

detailing their movements leading up to diagnosis.
The problem, as some see it, is the sheer level of detail contained in the text, as well as the fact that the app is not optional. The texts sent to Covid-positive people’s neighbours contain details such as the infected person’s age and gender and a record of their movements almost to within seconds. In many cases, this data is harvested using closed-circuit television and credit card transactions, including the identity of the shops they visited and what time they were there. This includes visits to so-called
As you can imagine, this has placed a number of South Korea’s citizens in a bit of a sticky wicket. The text information includes not only which buildings a person has visited, but also the rooms they were in, whether or not they wore masks, and even whether they used the toilet there. All this information is then loaded in excruciating
The building blocks were already there, as South Korea enacted laws to allow authorities to collect such detailed personal information following the MERS outbreak there in 2015. During Covid-19, checking such details became a daily routine, along with checking the weather forecast
However, for some, the information is so detailed as to make a person identifiable. An alert text sent to residents in a certain area read: “A 43-year-old man, resident of Nowon district, tested positive for coronavirus. He was at his work in Mapo district attending a sexual harassment class. He contracted the virus from the instructor of the class.” Further texts included the fact that he had been in
Another case involved a women in her 60s who went to work, had a buffet lunch with friends and attended a wedding on the same day. Nothing to see here, apart from the fact that she had recently been hospitalised with injuries she claimed were sustained in a car accident. Naturally, the internet went wild and she was actually tracked down by TV news reporters and put on the spot to deny allegations of insurance fraud.
On another occasion, a man was vilified for visiting an area of Seoul known for prostitution, leading to a barrage of taunts and venom on social media. It later transpired that the man had simply eaten a meal in that general area, which the authorities subsequently described as a
Another problem with this system is that it causes people to avoid certain places, such as Covid testing centres, even though they are thoroughly disinfected regularly.
And of course, there are the vultures and scavengers who are always there, ready to take advantage of the hardship of others. Reports have emerged of blackmailers contacting restaurants, claiming that they are Covid-19 positive and threatening to ruin businesses by splashing it all over social media that they had visited the establishment, unless of course a sum of money was forthcoming in exchange
As the saying goes, a little information can be a dangerous thing. Perhaps too much can be equally dangerous.
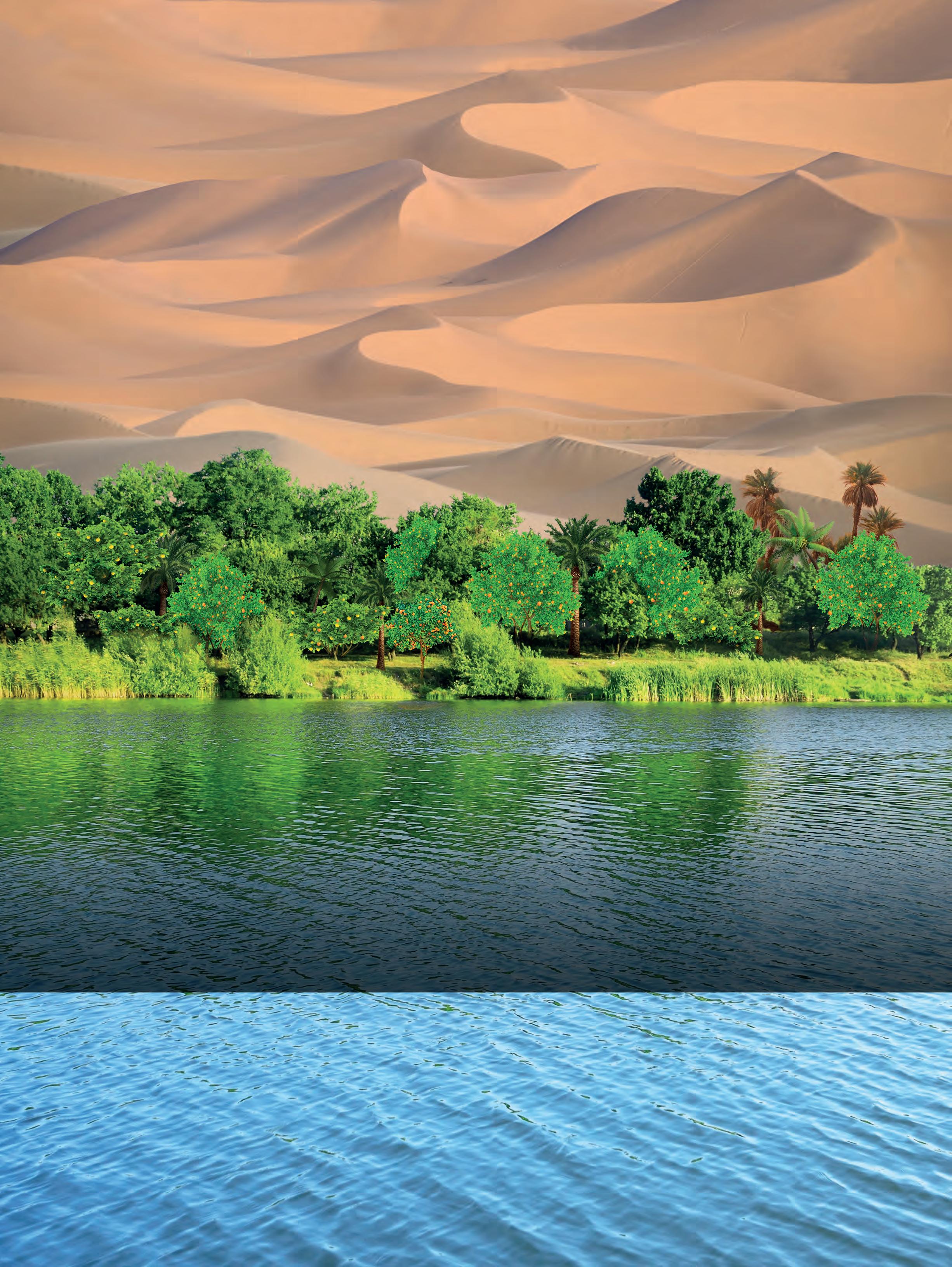
THE MEDICAL INDEPENDENT | 26 OCTOBER 2020
56































 ALL REPORTS BY DAVID LYNCH
ALL REPORTS BY DAVID LYNCH






























































 3. Data on File. Boehringer Ingelheim
3. Data on File. Boehringer Ingelheim





































 Prof Ivan Casserly (Speaker)
Dr Corinna Sadlier (Speaker) & Dr John Sheehan (Chairperson)
Dr Raymond Walley (Chairperson)
Dr Oisin O’Connell (Speaker)
Dr James Dollard (Speaker)
Prof Luke O’Neill (Speaker)
Francis Lynch, A.Menarini General Manager Ireland and UK
Nicola McNamara, A.Menarini Medical Representative
Annual A.Menarini National GP Masterclasses
Prof Ivan Casserly (Speaker)
Dr Corinna Sadlier (Speaker) & Dr John Sheehan (Chairperson)
Dr Raymond Walley (Chairperson)
Dr Oisin O’Connell (Speaker)
Dr James Dollard (Speaker)
Prof Luke O’Neill (Speaker)
Francis Lynch, A.Menarini General Manager Ireland and UK
Nicola McNamara, A.Menarini Medical Representative
Annual A.Menarini National GP Masterclasses