A Legacy of Trusted Paediatric Care













Gertrude’s Garden Children’s Hospital is an idea born of adventure, love, and compassion.
Born of adventure because Ewart Scott Grogan chose to pursue adventure over the arts in his younger days. It is adventure that led him to Southern Africa and eventually moving to Kenya in 1903. Of love because when Grogan proposed to marry his fiancée Gertrude Edith Watt, her father thought him not good enough and Grogan had to make a trip from Cape Town to Cairo to prove himself worthy of Gertrude. He made the trip in two and half years and married Gertrude. Of love because when Gertrude died, Grogan established a Children’s Hospital and Children’s Convalescent Home in her memory. And of compassion because the desire to set up a children’s convalescent home is said to have come as a suggestion from Gertrude a few years before she died. “I wish we could do something special for the children of Kenya, something of permanent value” was her suggestion.
Grogan and the founding team registered a Trust in 1944, and a legal entity was incorporated on October 2, 1946, to run the Gertrude’s Garden Children’s Hospital. Grogan donated the piece of land in Muthaiga and a building to house the convalescent home and later hospital, with services commencing early 1947. In starting the hospital, Grogan was not only honouring the memory of his wife, but also giving life to her suggestion to do something of permanent value for the children of Kenya.
Over the years, generations of Trustees and staff have worked to actualize the dream and vision of Ewart Grogan. While each generation has made an invaluable contribution, the contributions of Gerald Edward Nevill (FRCS) and Felicity Fenwick stand out. Gerald Neville was an eminent surgeon who served on the hospital’s Board of Trustees for many decades. It was during his 42-year tenure as the Chairman of the Management Board that the organization grew into a modern paediatric hospital. Felicity Fenwick served as the hospital matron (Head Nurse) and administrator for 43 years, during which period she established nursing standards at the hospital.
Seventy-five years later, Gertrude’s Children’s Hospital is today (in 2022) a well-established, World-class Paediatric Multispecialty Referral, Training and Research Hospital. The hospital remains a legacy of adventure, love, and compassion. We continue to increase our geographical reach, to incorporate new technologies into our care processes, to provide healthcare solutions to more complex illnesses, to improve the quality of paediatric care in the Eastern Africa region, and is so doing to keep doing something of permanent value for the Children of Kenya and Eastern Africa for generations to come.

Gertrude’s Children’s Hospital is a not-for-profit organization established in 1947. Gertrude’s Children’s Hospital is the most established paediatric multi-specialty hospital in Eastern and Central Africa, providing healthcare to children in Kenya as well as those referred from neighbouring countries. The hospital attends to over 400,000 patients annually through a network of 17 medical centres, using a self-sustaining financing model.
Gertrude’s Children’s Hospital is licensed to provide healthcare to children, teens, and young adults up to 21 years of age and provides the full range of healthcare services including preventive care, accident and emergency, outpatient care, inpatient medical and surgical care, and rehabilitation services. The hospital provides specialist care covering over twenty-seven aspects of paediatric specialization, and also runs a teens’ clinic providing comprehensive healthcare to teenagers and young adults. Gertrude’s Children’s hospital is licensed and recognized as a Level 5 Healthcare Facility, a Tertiary Referral, Teaching & Research Hospital.
The hospital employs more than 800 professionals and works with over 300 independent practitioners to provide high quality healthcare services. The hospital allocates substantial resources towards staff training and development with greater emphasis on specialized training. The hospital has a fully accredited Ethical Review Board that oversees research activities which range from operations research to clinical trials. The Gertrude’s Institute of Child Health and Research coordinates all training activities including specialized training for nurses, fellowship training for doctors, as well as accredited short courses.
Gertrude’s Children’s Hospital has put in place a very robust quality and safety program that ensures continuous improvement in line with internationally acceptable benchmarks. As a member of the Children’s Hospitals Association, USA, Gertrude’s Children’s Hospital benchmarks its care processes and outcomes with the best children’s hospitals in the world. Gertrude’s Children’s Hospital is the first paediatric hospital in Sub-Saharan Africa to be accredited by the Joint Commission International (JCI), USA. The JCI accreditation is the gold standard for best practices in healthcare quality, safety, and management.
The hospital, through the Gertrude’s Hospital Foundation, works with different partners to provide much needed care to children from less privileged families, establish highly specialized services, provide specialized training, and improve the quality of paediatric care in sub- Saharan Africa.

Gertrude’s Children’s Hospital aims to be the leading provider of world-class children’s healthcare in Eastern Africa.
The mission of Gertrude’s Children’s Hospital is to improve the health of children and adolescents in Eastern Africa through the provision of high-quality healthcare, education, research, and advocacy.
Professionalism
We hold ourselves to the highest level of professional conduct and accountability in line with legal, regulatory, and best practice requirements.
Respect
We treat our patients and their families with compassion, empathy and respect. We acknowledge and respect the diversity and contribution of our clients, colleagues, and other stakeholders.
Integrity
We espouse high ethical principles and deal honestly with everybody.
We foster teamwork within the organization and work collaboratively with partners to deliver the best possible value to our customers.
Excellence
We seek to achieve the highest standards of clinical care and service excellence at every moment and apply innovative ways to continuously improve the quality of our services.

Seventy-five years after Colonel Ewart Scott Grogan started a Children’s Healthcare facility in memory of his wife Gertrude Edith Watt, the world-class hospital that Gertrude’s Children’s Hospital has evolved into is testament that his vision lives on.

His gift of land to build a children’s hospital at Muthaiga, has over the last seventy-five years translated into a legacy of compassion, love and hope for millions of children and families in Eastern Africa who have for multiple generations benefitted from high quality paediatric care.
It is a legacy of many illnesses prevented by way of millions of vaccines administered through the preventive care program
It is a legacy of many hospitalizations averted through the robust primary care program
It is a legacy of many lives fulfilled for the many children that went on to grow, have careers, and start families of their own.
It is a legacy of many healthcare workers trained to improve access to pediatric care in Kenya and Sub – Saharan Africa.
It is legacy of many deaths prevented and a big contribution to reducing under-five mortality
It is a legacy of integrated high quality paediatric care now provided to more than 400,000 children annually across 17 healthcare facilities
As we look back and celebrate this legacy, we are very grateful that successive Trustees and staff have translated Grogan’s vision into the current internationally recognized multi-specialty paediatric referral, teaching, and research hospital. We now look forward to the future as we expand the reach and depth of services provided by the hospital so that millions more of children and families can access high quality paediatric care for generations to come.
The Muthaiga Hospital is transforming into a Centre of Excellence for multiple pediatric specialties to provide tertiary and quaternary care to children throughout the Eastern Africa region, and as well carry our specialist training and research. Through physical presence and use of technology, the primary and secondary care services will be expanded to reach many parts of the country. Through the Gertrude’s Hospital Foundation, many needy children in Kenya, who would otherwise not access care, will receive live saving medical interventions.
As we celebrate the past seventy – five years, we are confident that the legacy of compassion, love, and hope that is Gertrude’s Children’s Hospital will live on for generations to come.
Alec Davis, Dr. Robert Nyarango Chairman Board of Trustees Chief Executive Officer
Page 9/84

Vaccination Visits
Vaccines Administered
Inpatients (Days)
Surgeries
2005
2003 & 2004
• Opening of 1st & 2nd Outpatient Medical Centres
• Start of Nursing School
• Recognition as a Training Hospital
• Launch of Child Development Centre
2007 & 2008
• Opening of New Outpatient Wing
• Start of Specialist Clinics
• Endocrinology Fellowship Program
2014
• Recognition as a Research Hospital
• Opening of Chandaria Medical Centre
2012 & 2013
• Opening of 10th Medical Centre
• First Open Heart Surgery
2009 & 2010
• Opening of 6th Medical Centre
• Introduction of Standard Treatment Guidelines
• Establishment of Gertrude’s Hospital Foundation
• Switch to Electronic Medical Record
2015 & 2016
• Start of Telemedicine Services (Garissa)
2018 & 2019
• Enhancement of minimally invasive surgeries
• Accreditation by Joint Commission
International (JCI)
• Laboratory ISO 15189:2012 Certified
• Opening of 16th Medical Centre
• Training School accredited by TVET as a middle level college
2020 & 2021
2022 & 2023
• Opening of our 18th Medical Centre
• Launched 1st Access Clinic
• Launch of Hospital Medicine Brands
• Scale up of Telemedicine Services
• Re-accredited by Joint Commission
International (JCI)
• Established Molecular Diagnostics

The hospital has modeled its quality and patient safety program on the Joint Commission International standards.

Gertrude’s Children’s Hospital is accredited by the Joint Commission International (JCI). All the hospital facilities (branches) have been independently audited and accredited by the Joint Commission International (JCI), USA. Gertrude’s Children’s Hospital is currently the only children’s hospital in Sub – Saharan Africa that is JCI accredited.

The JCI accreditation is the internationally recognized gold standard for healthcare quality and safety. The accreditation confirms that the Joint Commission, the world’s most trusted authority in healthcare quality and safety, applying the most stringent world-class standards, has independently evaluated, and verified that Gertrude’s Children’s Hospital meets international healthcare quality and safety standards.
You may find the list of accredited organizations in the two websites below: https://www.jointcommissioninternational.org/about-jci/accredited-organizations/
https://www.worldhospitalsearch.org/
A hospital accredited by the JCI has been independently evaluated and confirmed to meet over 300 standards of healthcare quality and safety. As part the quality and safety standards, Gertrude’s Children’s has met the below standards as confirmed by JCI.
1) Meets all the international patient safety goals.
2) Provides clinical care through evidence-based practice and using well defined practice guidelines and clinical pathways
3) Provides safe surgery, anaesthesia, and sedation services.
4) Manages and uses medication in a safe manner.
5) Provides safe and effective diagnostic (laboratory & radiology) services.
6) Provides patient centered care.
7) Implements effective processes to prevent and control infections.
8) Provides a safe facility for patients, families, and staff.
9) Is ethical in governance, management, and clinical practices.
10) The competency of all its medical staff is verified, and their practice regularly evaluated.
11) Effectively manages information including the confidentiality of patient information.
12) Has a consistent culture of safety and commitment to continuous improvement.
13) Provides effective clinical emergency and resuscitation care and all its doctors and nurses are trained in emergency resuscitation.
14) Uses blood and blood products safely
When you choose a health care organization that is JCI accredited, you know you are receiving care from a leading practice organization whose quality and safety has been independently confirmed using the most rigorous and internationally accepted benchmark.
A health care organization that has met JCI’s exacting standards is allowed to display the Gold Seal of Approval® as a sign of this distinctive accomplishment.
So, when you are looking for a world-class health care organization, look for the JCI Gold Seal like the one on the left.

Gertrude’s Children’s hospital has over many years continually improved its service delivery models to improve customer experience at all its care touch points.
1) Short Service Times: In all the hospital facilities its is our aim that sick children and their families don’t wait long for care. Using our triage system, we ensure that 100% of emergency patients are attended to immediately.
2) Paperless Processes: Over the last twenty years, we have focused on eliminating paper-based processes to ensure that our clients are not saddled with endless filling of forms during their care process. Indeed, our outpatient and inpatient care processes are now 95% paperless and we are working with all our partners to eliminate the remaining 5%.
3) Integrated Care Delivery: We have successfully integrated our care delivery system all the way from primary care to quaternary care. All our clients are attended to on one integrated medical record regardless of which of our facilities or services they use. The integration ensures our preventive care is linked to curative care and facilitates continuity of care.
4) Customer Feedback: Over many years our services have received excellent rating from our customers with our overall customer satisfaction score remaining above 90% and net promoter score above 55%.
We believe that our clients (parents) entrust us with the care of their children. Similarly, all our partners trust us to do the best in our dealings with them. Therefore, ethical practice in both clinical care practice and business dealings in a cornerstone of our quality and patient safety program. In addition to four internal policy document that guide ethical conduct, we work with various external parties to ensure our practice and conduct is always exemplary.
Gertrude’s Children’s Hospital was one of the early adopters of the Global Compact tenets and Blue Company certification.
Our quality and safety program is very data driven, and we literally measure everything and benchmark with international benchmarks where applicable to ensure that our quality not only meets international best practice but that it also improves over time.
We measure and track the safety, timeliness, effectiveness, efficiency, patient centredness, and equity of our clinical care and services. Below is an outline of our service areas and the number of quality measures we track in each:
1) Accidents/emergency & outpatient care - 15 quality measures
2) Staff qualification and education - 10 quality measures
3) Anaesthesia and surgical care - 18 quality measures
4) Radiology - 14 quality measures
5) Laboratory/pathology - 15 quality measures
6) Clinical care - 31 quality measures
7) Inpatient care - 18 quality measures
8) Pharmacy and medication use - 14 quality measures
9) Facility management - 15 quality measures
10) Purchasing and finance -14 quality measures
11) Information management – 12 quality measures
12) Infection control and prevention – 14 quality measures
13) Blood and blood products use – 14 quality measures
14) Resuscitation services – 10 quality measures
15) International patient safety goals – 11 quality measures

Gertrude’s Children’s Hospital is accredited by the Joint Commission International (JCI). The Joint Commission International (JCI) accreditation is the internationally recognized gold standard for healthcare quality and safety.

All Gertrude’s Children’s Hospital Laboratories are ISO15189:2012 Certified, through Kenya Accreditation Services (KENAS).

Gertrude’s Children’s Hospital is a member of the Children’s Hospital Association (CHA), USA. The CHA is the voice for more than 220 children’s hospitals that advances public policy enabling hospitals to better serve children and builds awareness of child health issues. It is the premier resource for paediatric data and analytics driving improved clinical and operational performance among its member hospitals.
The Gertrude’s Institute of Child Health and Research is accredited by the Resuscitation Council (UK) to offer resuscitation training in Advanced Paediatric Life Support (EPALS) and Paediatric Immediate Life Support (PILS).
Safe Kids Worldwide is a global organization dedicated to preventing injuries in children. Gertrude’s Hospital Foundation is a member of Safe Kids Worldwide and has been working with international and local partners to improve child safety in Kenya.


Gertrude’s Children’s Hospital is a certified Blue Company. The Blue Company certification is an initiative of volunteer corporations and institutions with the objective of encouraging companies to fight corruption in all its forms. The Blue Company initiative is backed by the United Nations Global Compact (UNGC).

The Inpatient Readmission Rate is defined as the percentage of patients discharged from the hospital (inpatient) who are readmitted to the inpatient within 30 days of discharge1. This measure evaluates the quality of care given during the admission period and the coordination of care after discharge. The measure does not include planned readmissions. Unplanned readmission would indicate ineffective care, premature discharge, inadequate patient education, inadequate adherence to treatment after discharge. Against an international benchmark6 of 4.49, Gertrude’s children’s hospital has performed consistently well over the years as per graph below. Our readmission rate has averaged 2.6% in the past one year.

We have established practice guidelines and clinical pathways to standardize medical care. This is supported with multidisciplinary ward rounds, and ongoing review of the care provided. We also provide patient and family education regarding the illness they are being treated for and improved the care coordination and communication with patients/families to improve adherence to treatment after discharge.
While severely ill patients will be admitted to receive care as inpatients, it is our desire that they spend the shortest time in the ward. The inpatient average length of stay is a measure of how many days patients stay in the wards from admission to discharge. This is an indirect measure of the effectiveness of care provided during hospitalization.
The average length of stay varies globally between 2.5days and 4days. Our aim is to maintain an average stay of less than 3 days. As indicated in the graph below, we have maintained a low average length of stay.

Note: the lower the number the better the performance.
It is our desire to maintain a low inpatient average length of stay without compromising the quality of clinical care provided. To this end we continue to review our clinical pathways to achieve quicker and better patient healing and recovery.
Definition & why we measure:
Delay in care (including administration of first dose of prescribed treatment) may negatively impact care outcomes and length of hospital stay.9 Better care outcomes are achieved if treatment is given within the “golden hour” i.e., the first hour of admission14. Our aim is to always start treatment within one hour from the time a decision to admit is made. The chart below tracks our performance.

Note: the higher the number the better the performance.
We administer all first doses of treatment wherever the patient is in the admission process. The first dose does not need to wait until the patient gets into a ward bed. This process is tracked monthly, and improvements made where applicable.
Because there are risks associated with anaesthesia use and surgery, it is the intention of healthcare providers that patients go to theatre only when it is necessary. It is thus our hospital’s intention that surgical interventions are effective the first time they are carried out without the need to go back for repeat surgery or due immediate or delayed complications.5
Return to theatre due to complications is an important indicator of the quality of the surgical treatment and surgical risk management.3,9 This measure does not include planned repeat or additional surgeries as part of the care process.
From the chart below, the performance of our theatres has been consistently good against a benchmark of 3.8%.

Note: the lower the number the better the performance.
Our surgical care process is supported by international best practice clinical pathways and a very effective pre-surgical and pre-anaesthesia assessment of patients to ensure effective and safe surgeries. We also keep reviewing our surgical and anaesthesia equipment to ensure they are paediatric age appropriate and upgrade them regularly to the most current and safer options. We rigorously review every unplanned return to theatre, identify areas of improvement, and implement systemwide improvements. Because surgical related complications are expected and may not be eliminated completely, we educate all our clients on post – surgical care and more importantly on what to look out for both to minimize complications and as well to seek timely interventions.

This is a patient safety goal adopted internationally to ensure safe surgery4,13. The World Health Organization (WHO) has prescribed a surgical safety checklist that must be used to confirm the identity of the patient, the surgery being conducted, the site of the surgery, among and other things before any surgery. The use of the checklist avoids operating on the wrong patient or carrying out the wrong procedure both of which can cause harm to the patient. The surgical team must go through this checklist through a process called “time out” before any surgery is done. What we measure is to confirm that this time out process is indeed carried at a 100% compliance rate. Achieving this at 100% over the years has contributed to the overall safety of our surgical care.
The hospital has adopted this standard as policy with the checklists being used at all our theatres and for all procedures at 100% through the process of timeout. Additionally, we have created the right culture to ensure any member of the team is able to stop a procedure from proceeding if time out is not conducted.
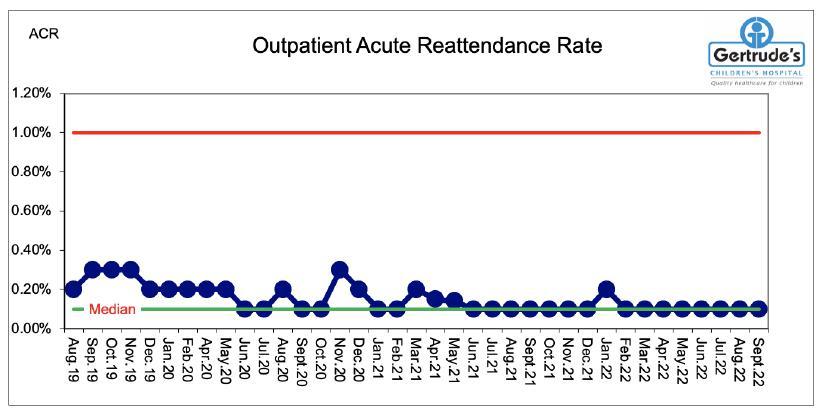
It is expected that accurate diagnosis is made during the first outpatient visit to hospital and appropriate treatment is given. Often due to disease progression, inadequate adherence to treatment, inadequate response to treatment, or missed diagnosis, a patient may return to the hospital for care. Within best practice, it is accepted that up to 1% of patients will return to the hospital within 72 hours due to unresolved illness. When this number goes above 1% then there is need to worry about the quality or effectiveness of the outpatient care. This measure does not include planned revisits for review, follow up care or chronic care management. The unplanned outpatient reattendance rate is regarded as a measure of the quality/ appropriateness of care rendered and home care planning during the initial visit.2,11
Our intention is to limit unplanned outpatient reattendance both to ensure appropriate care during the initial visit and to reduce the cost of care to the patient. From the chart below we have consistently achieved a revisit rate that is below 0.5%.
Note: the lower the number the better the performance.
We consistently review our outpatient care to confirm that it is in line with the defined standard practice guidelines and clinical pathways and address identified gaps. This is supported with continuing medical education for all our teams, regular drills targeting specific care areas, and ongoing clinical audits to ensure care standardization.10

Definition & why we measure:
A central line is a catheter placed into a large vein usually in the neck, chest, arms, or groin. It allows healthcare workers to give medication, fluids, and nutrition to patients. These lines directly accesses a patient’s blood stream and therefore increases the risk of infections if not handled correctly. A central line blood stream infection (CLABSI) occurs when bacteria or other microorganisms enter through the patient’s central line and then into the blood stream. The microorganisms may cause infection leading to prolonged hospital stay, increased cost of care, or medical complications.
We have maintained zero Central Line Associated Blood infections per 1000 bed days in the last 26 months.
Note: the lower the number the better the performance.
To minimize the risk of central line associated infections, we use central lines only when necessary and for the shortest time possible. However, for patients who must use these devices, our doctors and nurses apply evidence-based methods and procedures to insert and care for central lines. This is supported by ongoing audits and education.

The clients that we serve are best placed to judge the quality of our services. To this end we carry out regular customer feedback reviews using internal and external/independent mechanisms. We track overall customer satisfaction with the aim of achieving 90% or more, and the net promoter score with the aim of achieving 55% or more. The trends below indicate that our customers have consistently given us good ratings.

Note: the higher the number the better the performance.
Over the years we have endeavored to listen to what our clients need and work towards delivering the same. Our service design, facilities location, technology adoption, new staff induction/orientation, staff training, and care delivery have been client driven. We incorporate client feedback into our quality improvement programs.
1. Bice T. ICU Readmissions: Good for Reflection on Performance but Not a Reflection of Quality. Crit Care Med. 2016 Sep;44(9):1790-1. doi: 10.1097/CCM.0000000000001809. PMID: 27526001; PMCID: PMC4988323.
2. Credé, S.H., O’Keeffe, C., Mason, S. et al. (2017). What is the evidence for the management of patients along the pathway from the emergency department to acute admission to reduce unplanned attendance and admission? An evidence synthesis. BMC Health Serv Res 17, 355 https://doi.org/10.1186/s12913-017-2299-8
3. Griffin FA, Classen DC. Detection of adverse events in surgical patients using the Trigger Tool approach. Qual Saf Health Care. 2008 Aug;17(4):253-8. doi: 10.1136/qshc.2007.025080. PMID: 18678721
4. Keiler R, Quicho R, Jorgerson C, Pew C, Fry H.M, Harris J, Hinkley C.C. (2020). Joint Commission International Accreditation Standards for Hospitals (7th ed.). Oak Brook, Illinois, USA: Joint Commission Resources.
5. Marini H, Merle V, Derrey S, et al Surveillance of unplanned return to the operating theatre in neurosurgery combined with a mortality–morbidity conference: results of a pilot survey BMJ Quality & Safety 2012;21:432-438.
6. Martin L, Nelson E, Rakover J, Chase A. Whole System Measures 2.0: A Compass for Health System Leaders. IHI White Paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2016. (Available at ihi.org)
7. Niven DJ, Bastos JF, Stelfox HT. Critical care transition programs and the risk of readmission or death after discharge from an ICU: a systematic review and meta-analysis. Critical care medicine. 2014;42(1):179-87. doi:10.1097/CCM.0b013e3182a272c0
8. Österlind J, Gerhardsson J, Myrberg T. Critical care transition programs on readmission or death: A systematic review and meta-analysis. Acta Anaesthesiol Scand. 2020 Aug;64(7):870-883. doi: 10.1111/aas.13591. Epub 2020 Apr 17. PMID: 32232833.
9. Pujol N, Merrer J, Lemaire B, Boisrenoult P, Desmoineaux P, Oger P, Lebas C, Beaufils P. (2015) Unplanned return to theater: A quality of care and risk management index? Orthop Traumatol Surg Res. Jun;101(4):399-403. doi: 10.1016/j.otsr.2015.03.013. Epub 2015 May 4. PMID: 25952709.
10. Rotter T, Kinsman L, James EL, Machotta A, Gothe H, Willis J, Snow P, Kugler J. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database of Systematic Reviews 2010, Issue 3. Art. No.: CD006632. DOI: 10.1002/14651858.CD006632.pub2. Accessed 18 November 2021.
11. Sun, Y., Heng, B.H., Tay, S.Y. et al. (2015) Unplanned 3-day re-attendance rate at Emergency Department (ED) and hospital’s bed occupancy rate (BOR). Int J Emerg Med 8, 32. https://doi.org/10.1186/s12245-015-0082-3
12. Weiss AJ, Elixhauser A. Overview of Hospital Stays in the United States, 2012: Statistical Brief #180. 2014 Oct. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006 Feb-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK259100/
13. WHO Patient Safety & World Health Organization. ( 2009) . WHO guidelines for safe surgery 2009: safe surgery saves lives. World Health Organization. https://apps.who.int/iris/handle/10665/44185
14. Wheeler, D.S. Is the “golden age” of the “golden hour” in sepsis over? Crit Care 19, 447 (2015). https://doi.org/10.1186/s13054-015-1167-3

We offer the full range of preventive care services incorporating primary prevention, secondary prevention, and tertiary prevention, and currently reach more than 100,000 clients annually.
We work with families, other medical institutions, and public health institutions to implement a primary prevention program in all our facilities. Our services include:
1) Prevention of infectious diseases through vaccination
2) Prevention of dental related conditions through oral hygiene programs
3) Prevention of disease transmission through population-based interventions
4) Prevention of accidents and emergencies through the Safekids® program
5) Wellness programs and health education
Our secondary prevention program is aimed at early detention of childhood illnesses/conditions to implement early interventions aimed at either providing definitive treatment and/or preventing disease progression. The overall aim of this service is to ensure that the growth and development of the children is not affected due to late intervention. Most children identified early and given appropriate treatment grow to live a full life. Some of our secondary prevention programs include:
1) Hearing screening and audiology care
2) Congenital Heart Disease screening and intervention
3) Neurodevelopmental assessment and intervention
4) Comprehensive neonatal screening and intervention
5) Population based screening and early diagnosis programs and interventions
6) Antiparasitic programs,
7) Addiction prevention programs
8) Annual wellness checks for children, adolescents, young adults, and interventions
The tertiary prevention services include comprehensive multidisciplinary treatment to prevent morbidity and mortality due to already established illness. We work with parents and care givers as partners in care to ensure optimal management at home to meet defined care outcomes, reduce acute episodes of illness, prevent medical complications, prevent disease progression, reduce emergency room visits, reduce hospitalization, reduce pain, and improve the overall quality of life of the patients. Our aim is that whatever the condition being managed, the children affected should go on with their school/ college, play, sleep, travel, and other aspects of their lives without interuption. Some of our tertiary prevention programs include:
1) The Sickle Cell Care Program
2) The Asthma Care Program
3) The HIV Care Program
4) The Neurodevelopmental and Neurology Care Program
5) The Orthopaedic, Spinal, and Sport Injury Care Program
6) The Mental Health Care Program
7) The Substance Use Rehabilitation Program
8) The Home Care Program for children with special needs or on device support
9) The Diabetes Care Program
For more information about preventive care services please email outpatient@gerties.org

We have 17 outpatient medical centres across various counties; 2 in Kajiado, 2 in Kiambu, 1 in Kisumu, 1 in Mombasa, 1 in Machakos and 10 in Nairobi all easily accessible to families. The facilities operate from 8:00 am - 8:00 pm on weekdays and 9:00 am - 7:00 pm on Sundays and Public holidays, while the hospital in Muthaiga operates 24 hours daily.
All the oupatient medical centres offer the services below:
1) Paediatric Accident and Emergency
2) Paediatric Outpatient
3) Paediatric Specialists clinics
4) Well Baby Services including vaccination
5) Nutrition clinic
6) International Travel Vaccination
7) Pharmacy Services
8) Laboratory Services
9) Dental Services (except The Junction Medical Centre)
10) Radiology and Day Surgery (Doonholm and Muthaiga Medical Centres)
11) Speech and Language Therapy (Muthaiga, Doonholm and Mombasa Medical Centres)
12) Sports Medicine (Muthaiga and Doonholm Medical Centres)
13) Occupational therapy at Muthaiga, Buruburu, Doonholm and Mombasa Medical Centres
We offer the below specialist outpatient services: 1.
17. Paediatric Haematology
18. General Paediatrics
19. Paediatric Neonatology
20. Paediatric Maxillofacial
21. Well baby Services
22. Paediatric Dental Services
23. Paediatric developmental and rehabilitation care -Speech therapy, Occupational therapy, Physiotherapy
24. Audiology (Hearing Care) Clinic
25. Infectious Diseases Clinic
26. Antenatal Clinic
27. Sickle Cell Clinic
28. Genomics





Lavington Medical Centre, Othaya Road off Gitanga Road, Lavington. Tel: 0709529002



Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Nairobi West Medical Centre, Tmall 3rd Floor, Langata Road. Tel: 0709529004
Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Embakasi Medical Centre, Nakumatt Building 1st Floor, next to City Cabanas Tel: 0709529006

Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Kitengela Medical Centre, Kitengela Mall 3rd Floor. Tel: 0709529008
Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Doonholm Medical Centre, Doonholm Roundabout, Manyanja Road, Donholm. Tel: 0709529003
Mon to Sat: 8:00am - 8:00pm
Sun & Public holidays: 9:00am - 7:00pm
Pangani Medical Centre, Juja Road.
Tel: 0709529005
Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Komarock Medical Centre, Mwangaza Road Phase II, Komarock. Tel: 0709529007
Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Rongai Medical Centre, Next to Tuskys Supermarket 1st Floor Tel: 0709529009
Mon to Sat: 8:00am - 8:00pm
Sun & Public holidays: 9:00am - 7:00pm



Thika Medical Centre, Zuhura place, 1st Floor, Tel: 0709529010
Mon to Sat: 8:00am to 7:00pm
Sun & Public holidays: 9:00am to 7:00pm
The Point Mall, Rabia Road, Buruburu. Tel: 0709529012
Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Sarit Medical Centre, Sarit Centre 2nd Floor. Tel: 0709529014

Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Syokimau Medical Centre, Gateway Mall, 3rd Floor. Tel: 0709529016

Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Links Plaza, 1st Floor, Links Road, Nyali, Mombasa
Tel: 0709529011
Mon to Sat: 8:00am - 8:00pm
Sun & Public holidays: 9:00am - 7:00pm
Thika Road Mall Medical Centre, TRM, 2nd Floor, Thika Road.



Tel: 0709529013
Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Junction Medical Centre, The Junction, 4th Floor, Ngong Road Tel: 0709529015
Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm
Kisumu Medical Centre
Mito Jura Road, adjacent to St. Theresa’s Catholic Church, Kibuye, off Jomo Kenyatta Highway.
Tel: 0709529017
Mon to Sat: 8:00am to 8:00pm
Sun & Public holidays: 9:00am to 7:00pm

Gertrude’s Hospital Foundation, in partnership with M-Pesa Foundation and Gertrude’s Children’s Hospital, would like to improve access and convenience to healthcare services in rural and underserved areas in Kenya though their telemedicine program - the Daktari Smart program. This will help to reduce the number of referrals of sick children and optimize the capacity and reach of healthcare delivery systems allowing level IV and V hospitals have access to specialists. The program is being implemented in Baringo, Homabay, Lamu, Samburu and two other counties.
The telemedicine platform is a Health Presence Communication Equipment which comprises of electronic medical devices such as the electronic stethoscope, vital signs monitor, dermascope camera, ultrasound machine, otoscope and ECG (electrocardiogram). Different from the conventional video conferencing, the telemedicine platform allows the health worker at the local partner health facilities, to place the probes on the patient and the specialist at Gertrude’s Children’s Hospital is able to see the patient and hear the sounds real time without interpretation from the health worker at the local facility. The bandwidth requirement for the equipment is low, ranging from 5Mbps to 10Mbps. This means that the platform can be installed in rural and underserved areas that do not have fibre connectivity.
The screens are also used for video conferencing to facilitate regular capacity building for health workers serving in the local health facilities; and training of social workers and community health volunteers (CHVs) in the local community who are instrumental in social mobilization.
In the first 3 years of the project, it is expected that the following outcomes will be achieved:
1. Provision of care and treatment to ~32,400 children via telemedicine.
2. Improved capacity of 300 health workers working in the various health facilities to correctly diagnose and treat sick children, as well as link children who require advanced care.
3. Improved capacity of 360 community health volunteers to provide community education on child health.
4. Establishment of regional telemedicine centres with electronic medical devices which will act as paediatric referral centres.


Gertrude’s Children’s hospital has nineteen pharmacies throughout its network that provide high quality pharmacy services including paediatric pharmaceutical products as part of patient care.
Over many years now the pharmacy department has defined a hospital formulary list that includes carefully selected medicines, nutritional products, and other non-pharmaceutical products that meet the hospitals rigorous evaluation process to be used for patient care. The hospital works with the Pharmacy and Poisons Board, manufacturers and suppliers of pharmaceuticals to ensure the products used at the hospital meet all the requisite requirements for quality, safety and efficacy for use in children.
The pharmacy department prepares some liquid formulation not available commercially for individual patient use through its extemporaneous preparations process. The department has in place a sterile preparation room that meets ISO Class 5 certification for sterility and safety that is used for preparation of intravenous, chemotherapy, parenteral nutritional admixtures before administration to patients.
The Gertrude’s pharmacy at Muthaiga is a World Health Organization (WHO) certified Medicines and Poisons Information Centre that supports clinicians at Gertrude’s Children’s Hospital and indeed other hospitals as well as the public with information to support management of situations of accidental or other forms of poisoning. The Pharmacy also serves as a comprehensive paediatric medicines information centre. The department has published a number of guidelines to support rational use of medicines in children. The information centre may be reached through telephone number 0708 988 400.
The pharmacy department has contracted a reputable pharmaceutical manufacturer in the United Kingdom (Britain) to manufacture some products for the hospital. This arrangement ensures quality is maintained and the opportunities for counterfeiting eliminated because the chain of distribution is reduced. The products are branded and packed for Gertrude’s Children’s Hospital at the factory and dispatched straight to the hospital appointed warehouse.
The Gertrude’s Children’s Hospital pharmacy department has been recognized regionally for implementation of an effective antimicrobial stewardship program. This program has over the years improved the responsible use of antimicrobials (including antibiotics) and indeed reduced their use for conditions that don’t require antimicrobial treatment. This ensures that antimicrobial resistance is reduced and the molecules/medicines remain effective and available for future generations.


Our Laboratory is fully accredited and conforms to ISO 15189:2012 Standards and Joint Commission International accreditation (JCI) standards patient safety and quality.
1. Laboratory Services provided:
1) Microbiology cultures/virology and bacteriology.
2) Coagulation and Thrombosis: To determine blood-clotting disorders.
3) Hematology: To investigate blood diseases e.g., general check-up, blood cancers and monitoring of treatment.
4) Autoimmune disease testing; For all autoimmune disease diagnosis and treatment monitoring.
5) Blood Bank Services: Blood donation, blood processing and storage and blood transfusion services. We have aphaeretic blood components harvester.
6) Chemistry: To test for natural chemical levels in the blood, urine, and other body fluids
7) Comprehensive immunochemistry services.
8) Drugs of abuse testing.
9) Immunological tests For CD4 /CD8 testing and other Immunity levels testing.
10) Newborn screening.
11) Molecular Tests; For all PCR tests/FISH studies
12) Genetic Tests
13) Pathologists advisory and consultancy services
2. Health Screenings Services.
1) Wellness checks.
2) Well -Woman check
3) Well -Man check
4) Well -Child check
5) Well- Baby check
6) Pre-employment check-ups
7) Pre-college/school check ups
3. Disease Screening.
1) Thyroid disease screening
2) Sickle cell disease screening
3) Cholesterol and Glucose screening
4) Warfarin therapy monitoring (INR)
5) Fats and lipid profiles screening
6) Basic and comprehensive metabolic profiles
7) Cancer screening for children and adults
8) Drugs of abuse screening.
4. Heavy Metal Poisoning checks; includes Lead /Mercury /Copper and other heavy metals levels

The radiology department at Gertrude’s Children’s Hospital provides a wide range of imaging services using age-appropriate equipment and processes that meet the unique needs of children.
Services include the full range of X - ray services, ultrasound including 3D and 4D scans, Computerized tomography (CT) scans, dental imaging including orthopantomograms (OPG), intra-oral periapical imaging, bitewings, and temporo-mandibular joint x-rays.
The department also provides Transracial Doppler Imaging, and angiography services.
Portable and theatre-based imaging services are also available.
The radiology department carries out fluoroscopy examinations for abdominal, urological imaging and interventional imaging for biliary stenting, renal stenting, biliary drainage among others.
The radiology unit ensures the highest quality and safety of patients, their families, and staff as summarized below:
1) The hospital has in place clinical pathways to guide use of imaging services to avoid overuse and hence reduce overexposure for children
2) The department has installed age-appropriate equipment to ensure minimum radiation exposure for children and adults that may use the service
3) For children that may require sedation before imaging procedure, a multidisciplinary team of clinicians trained in providing safe sedation is available to give the service.
4) The department has in place comprehensive emergency response including resuscitation services to cater for any medical emergencies
5) All the hospital radiology units are licensed by the respective regulatory agencies and inspected regularly. Radiation monitoring is done around the clock to ensure ongoing safety.
6) The radiology services at Muthaiga are available on a twenty-four-hour basis to cater for any emergency imaging requirements
7) A multi-disciplinary team of highly competent staff including radiographers, radiologists, anaesthesiologists, paediatric nurses, provide services at the unit.

For patients that will require inpatient care, we provide inpatient services at our Muthaiga hospital. Patients from birth to 21 years of age are admitted for inpatient care from our network of outpatient facilities, from other hospitals, those evacuated from neighbouring countries, and those that come in for elective surgeries from Africa, Europe, and other parts of the world.
Our inpatient rooms and services are designed to support the clinical care delivery, provide a healing environment for quick recovery of patients, and to meet the needs of working parents. All our inpatient rooms have two beds - a cot for the sick child and a bed for the parent/guardian. The parent’s accommodation is at no extra cost. In addition to medical care, clients receive excellent hospitality services including a wide selection of meals, entertainment facilities including a television, free Wi-Fi, an indoor and outdoor play area. Clients also have a big selection of inpatient rooms in line with patient needs and family preferences. Our clients have consistently rated our inpatient services high with net promoter score of 80% and satisfaction rate above 90%.
Our aim is to have an overall short stay in the hospital. Through a rigorous application of clinical pathways and integration of care using a multi-disciplinary approach, we have maintained short average length of inpatient stay. Over one third of our surgical interventions are done as day surgeries without the need to spend a night in the hospital. We have a dedicated surgical ward admission and discharge process to facilitate efficiency transition of care.
All our inpatient care is provided by specialists well skilled in paediatric care. All doctors granted practice privileges at the hospital and therefore allowed to take care of both medical and surgical inpatients are specialists in their area of practice. Inpatient paediatric nurses are experienced in managing paediatric patients. All doctors and nurses are trained and certified in emergency care delivery including resuscitation while all other staff that work in the inpatient have been trained in basic life support/first aid. The inpatient unit is covered by doctors on a twenty-four-hour basis for any emergencies. Physiotherapists, occupational therapists, play therapists, psycho-social therapists, counselors and nutritionists provide supportive medical care to inpatients where required. The hospital has an interdenominational prayer room & chaplaincy services to complement medical care.
For patients and families coming for inpatient care from other countries or from counties away from Nairobi, the hospital has in place logistical arrangements to facilitate safe travel and comfortable stay at the hospital. The arrangements include flight arrangements with some airlines, airport transfers, ambulance evacuation, and accommodation. The hospital provides accommodation at subsidized cost at the hospital grounds for such families that may require accommodation for a few days during their children’s stay at the hospital.
International clientele may call our medical tourism section through 020 720 6000 or 020 720 6292 to seek guidance or to facilitate access to services at the hospital.

We run a fully integrated developmental service through the Gordon Bell Child Development Centre. A multidisciplinary team of specialists attends to children referred from the hospital’s facilities network, from partner hospital and schools for assessment and interventions for a variety of physiological, behavioural, or learning challenges. These conditions include neurological, developmental delay and disorders, genetic conditions, and congenital conditions.
Paediatric neurodevelopmental specialists and neurologists carry out assessment of patients referred to the program to determine their diagnosis, cause of the condition affecting them, and the optimal treatment/interventions.
The speech and language therapy program evaluates and treats children with speech and language challenges airing from a number of causes including delayed speech development, autism spectrum disorder, cleft/lip and craniofacial anomalies, cerebral palsy, genetic/chromosomal disorders, hearing impairment, trauma and other medical causes.
The audiology service includes hearing testing using otoacoustic emission assessment, brainstem audiometry, tympanometry, and other assessments and provision of the most appropriate interventions which may include fitting hearing aids, speech/language therapy, or cochlear implantation. The hospital works in partnership with the Oticon Foundation to provide hearing aids at a highly subsidized rate.
The occupational therapy program evaluates and provides treatment to children with challenges with cognitive or motor skills, sensory integration and processing, self-care skills, and other related deficits. The causes of these challenges range from neurodevelopmental delays, medical and surgical conditions. The main aim of the occupational therapy interventions is to improve the patients’ ability to do things for themselves enhance their independence.
The physical therapy program evaluates and corrects movement and muscular related conditions in children through a range of physiotherapy interventions. Paediatric physical therapy promotes independence, increases participation, facilitates motor development and function, improves strength and endurance, enhances learning opportunities, and eases challenges with daily living.
The genomic medicine program focuses on diagnosis and management of genetic conditions. The genetic conditions may be identified through the neonatal screening programs or diagnosed as part of the care process in patients referred for specialist care. While genetic conditions are rare, their identification helps provide targeted treatment, may provide an explanation to complex medical conditions, provides useful information to support genetic counselling for families, helps families to understand and better cope with and manage the patients’ conditions.
The hospital supports the Rare Diseases Society, which is a support group of parents of children with rare/genetic conditions.
The developmental paediatric program also provides care to children with Autism Spectrum Disorder, Down Syndrome, Attention Deficit Hyperactivity Disorder, among other conditions.


Gertrude’s Children’s Hospital runs the East Africa children’s Heart Program which is an integrated program combining all aspects of paediatric cardiology and cardiothoracic care through a multidisciplinary approach. The hospital works in partnership with institutions within the Eastern Africa region to improve access to early diagnosis and treatment of heart conditions in children.
The service is provided by a multidisciplinary team of paediatric nurses with training in paediatric cardiac care, paediatric critical care nurses, paediatric cardiologists, paediatric anaesthesiologists, paediatric cardiothoracic surgeons, paediatric intensivists, and paediatric perfusionists.
The hospital provides the following cardiology and cardiothoracic care services
1) Electrocardiography (EKG or ECG), digital x-rays, stress tests, and echocardiograms (Echo)
2) Paediatric cardiac CT scans CT angiography
3) Fetal diagnosis of heart conditions and new-born consultations
4) Paediatric cardiologist consultations and care
5) Rheumatic Heart Disease management
6) Congenital Heart Disease early diagnosis program
7) Closed and open-heart surgeries
8) Cardiac catheterization in partnership with other centres
9) The full range of paediatric cardiothoracic surgeries/procedures
10) Cardiac Critical Care management
For more information about of preventive care services please email specialistclinics@gerties.org

The dentistry program provides general and specialized dental services to children, teens, and adults. The bulk of dental services is provided through outpatient services available in our outpatient facilities. Some dental services like emergency care to dental trauma, full mouth restoration may require surgical intervention provided under general anaesthesia in the theatre.
The common dental services offered at our facilities include:
1) General dental check up
2) Dental age assessment
3) Dental cleaning - full-mouth scaling, polishing & fluoride application
4) Tooth fillings and sealants - coloured as well as metallic fillings for dental cavities
5) Anaesthetic/cosmetic dentistry - masking of discoloured teeth with tooth-coloured materials; bleaching to whiten teeth
6) Root canal treatment including pulp therapy for milk teeth with very deep cavities
7) Treatment of missing teeth with dentures, crowns & bridgework
8) Space maintenance for early loss of milk teeth
9) Dental surgery - simple extractions, disimpactions (surgical extractions), surgical exposures, suturing & splinting of teeth
10) Mouth-guards - protective gear for children in contact sports, those who wear braces and those who grind their teeth
11) Dental treatment for apprehensive children – under conscious sedation & general anaesthesia
12) Orthodontic assessment and treatment – for teeth alignment with removable and fixed braces; removal and fixed habit-breakers for thumb & lip-suckers.
13) Prevention of dental related conditions through oral hygiene programs
Maxillofacial surgery is a special type of dentistry focused on surgical treatment of disease, injury, or defects in the face, jaw, or mouth. Maxillofacial surgery may be required for the following conditions:
1) To correct misaligned jaws
2) To correct congenital (present at birth) abnormalities such as cleft lip and palate
3) Diagnose and treat cysts, tumours, cancers in the face, head, neck, mouth, jaw
4) Diagnose and treat causes of chronic facial pain.
5) Reconstruction surgery to repair injury to the jaws, facial bones, teeth, maxillofacial tissue
6) To carry out bone grafting to replace missing bones in the face, jaw, or month
7) To treat temporomandibular joint disorders
8) To fix dental implants for cosmetic of other reasons
Clinical teams trained in pain management, sedation, and anaesthesia support the dental services to achieve optimal pain management and to ensure the safety of sedation and/or anaesthesia services. Some outpatient dental procedures require that the child is sedated during the dental procedure. This is done is select dental units in our network of about 20 dental chairs. Adequate emergency response services including advanced life support are provide at all points where sedation and/or anaesthesia services are provided. All dentist that work at our facilities are trained and certified in resuscitation care.
Requisite diagnosis capacity including IOPA, OPG, Bitewings and other forms of imaging is available to ensure optimal diagnosis.

All the hospital’s 17 facilities have a well-equipped accident and emergency unit with capacity to handle paediatric emergencies, provide paediatric advanced life support care including emergency resuscitations services. All the doctors and nurses that work in the hospital have been trained and their competency in emergency care certified through the Resuscitation Council of the United Kingdom (RCUK) training program. All other staff including non-medical staff have been trained in basic life support.
The hospital’s triage system supported by decision support tools integrated into the hospital’s information management system helps identify emergency cases to enable immediate interventions. Similarly, through the paediatric early warning signs monitoring program, all admitted patients are monitored to identify patients that may require emergency/immediate interventions.
The emergency unit in Muthaiga is equipped with an emergency theatre to handle any cases that may require emergency surgical care on a twenty four hour basis.
The pharmacy at Muthaiga is a WHO recognized poison information centre to support poisoning related emergencies.
Emergency response services including emergency trolleys (Crash Carts) are available in all patient care units including all outpatient care units, all wards, all theatres, the critical care unit, and all units where sedation services are provided. We carry out emergency response drills every week in all our facilities to ensure adequate preparation for real emergency situations.
We work with partners providing ambulance services for quick evacuation of patients.

We run a 15-bed mixed model critical (intensive) care unit that takes care of patients with severe illness that requires very close monitoring or complex interventions. All patients both medical and surgical that require intensive care are managed in the unit. The facility is equipped with state-of-the-art medical equipment with two rooms set up as isolation (negative pressure) units for management of patient with highly infectious conditions.
The critical care unit is run by a highly skilled team comprising of paediatric intensivists, paediatric critical care nurses, resident doctors, counsellors, nutritionists, clinical pharmacists among others using a closed ICU model. We maintain a one - to - one nurse to patient ratio at the critical care unit.
The critical care unit has been regularly and rigorously inspected and audited by regulatory and accrediting agencies for safety, quality, infection control, care protocols, and outcomes over the years. The critical care unit is, as part of the hospital, accredited by JCI for quality and safety.
The critical care unit serves as a referral centre for many hospitals in Easten Africa with more than 60% of patient managed there transferred in from other hospitals.
The critical care unit also serves as a training centre for paediatric critical care nurses and paediatric intensivists from the hospitals internal training programs and in partnership with other institutions ( universities and hospitals).
The paediatric otolaryngology program is by far one of the largest and most integrated programs at the hospital. Most children are affected by upper respiratory track illnesses including infections and their quality of life - including feeding, growth, school, and sleep among other aspects – is usually negatively affected by these conditions. Moreover, many children experience recurrent upper respiratory tract infections with increased use of medicines which may be reduced through appropriate interventions.
The hospitals otolaryngology program includes:
1) Outpatient paediatric medical interventions using well defined clinical pathways
2) Outpatient otolaryngologist (ENT specialist) consultations and medical treatments
3) Outpatient otolaryngologist (ENT specialist) office-based procedures
4) ENT surgeries of which about 30% are day surgeries (the patient does not need to be hospitalized)
5) Rehabilitative care including speech therapy, and other audiology services
6) Assistive devices support including hearing aids, cochlear implants
The hospital carries out over 100,000 otolaryngology related interventions annually and works with partner institutions to benchmark outcomes.

The paediatric nephrology program focuses on management of the kidney related conditions. Patients are often referred to the paediatric nephrology care from our network of facilities or from other healthcare practitioners in the region.
Children and adolescents managed through this care program may have one of more of the below listed conditions:
1) Infection affecting the kidneys, or urinary tract
2) Acute kidney injury
3) Blood in urine
4) Haemolytic uremic syndrome – clots in the kidney blood vessels
5) Persistent bedwetting in older children
6) High blood pressure
7) Kidney stones
8) Too much protein in urine
9) Kidney failure
10) Backward flow of urine from the bladder to the kidneys (Vesicoureteral reflux)
11) Congenital abnormalities of the urinary tract
12) Constriction in the flow of urine
13) Polycystic kidney disease
Treatment may be given using medicines only or surgery or both. Sometimes dialysis is done until the normal kidney function is restored. In some cases, kidney transplant may be required.
The hospital runs a program to treat and support older children with bedwetting challenges.

The paediatric neurology specialty focuses on medical interventions for illnesses of the brain and nervous system while the neurosurgery provides surgical interventions in the same focus areas. A wide range of conditions, including the below listed, are managed through the neurology/neurosurgery program.
1) Head or spinal cord injury/trauma
2) Convulsive disorders including epilepsy
3) Certain headaches,
4) Neuromuscular conditions,
5) Neurodevelopmental conditions,
6) Cerebral palsy
7) Hydrocephalus,
8) Spina bifida
9) Stokes
10) Brain or spinal cord tumours
11) Craniofacial disorders
The neurology and neurosurgery program applies requisite equipment and tests to guide the diagnosis and treatment of the conditions identified. For some conditions, rehabilitation therapy is require as part of the treatment. Some conditions like epilepsy require long term treatment using a combination of medicines.
Gertrude’s Children’s Hospital is able to source for age-appropriate medicine formulations for treatments of paediatric neurological conditions and as well provide the required treatment monitoring.
The hospital provides appropriate diagnostic equipment and services including X-Ray, CT Scan, MRI, Transracial Doppler Imaging, EEG (electroencephalogram) to support neurological/neurosurgical care.

Children, teens, and young adults have unique orthopaedic care requirements because they are very active and likely to experience injuries. Because their muscles and bones are still growing the interventions provided need to ensure good immediate outcomes and as well limit long term complications.
The Orthopaedic and Spinal Care program provides expert evaluation and treatment, including surgery where required, of all musculoskeletal and spinal injuries. Orthopaedic care is provided by multidisciplinary teams of orthopaedic and spinal surgeons, neurosurgeons, neurologists, accident and emergency doctors, physiotherapists, orthopaedic technicians, anaesthesiologists, and other medical staff working at the accident and emergency department, outpatient orthopaedic clinics, and theatres.
The program is supported with excellent diagnostic services including X – Ray, CT scan, MRI; orthopaedic technician services including fixing of casts; rehabilitation services including physiotherapy and training to use assistive devices.
Sports medicine focuses on providing care to children, teens, and young adults that suffer sports related injuries.
The program also provides corrective surgery to children born with limb deformities.
The spine surgery program is focused on treating spine injury programs and congenital/developmental spine deformities.

To address children unique needs for pain management during procedures and surgery, Gertrude’s Children’s Hospital has established a paediatric sedation, anaesthesia, and pain management service.
In view of the risks that come with sedation and anaesthesia, all the medical practitioners including anaesthesiologists have had specific training in inducing, monitoring and weaning children off sedation and anaesthesia. More importantly they have the right mix of skills to manage any complications that may arise from sedation or anaesthesia. All units where sedation or anaesthesia is provided are equipped with emergency response equipment.
The pain management program is implemented throughout the hospital to ensure children are as pain free as possible during their care process. Pain management protocols are also used to address pain that is associated with specific conditions or procedures like sick cell disease, cancer, major surgery etc.
We carry out over 5,000 paediatric surgeries in a year ranging from general paediatric surgeries to paediatric specialties specific surgeries. The hospital theaters are well equipped with state of the art and paediatric ageappropriate equipment. For a number of surgeries, the laparoscopic (minimally invasive) option is available and preferable.
Surgical care is provided by highly skilled multi-disciplinary teams of paediatric surgeons, theatre nurses, paediatric anaesthesiologists, with support from other medical specialists. Post - surgical nursing care is provided by highly skilled paediatric nurses. Most of the surgical interventions are billed through standard and predictable bundled care packages which include the cost of surgery and post – surgical care. The below listed surgeries are among those performed at the hospital:
1. General paediatric surgeries
2. Cardiac (Heart) & Cardiothoracic Surgeries
3. Dental and Maxillofacial surgeries
4. Ear, Nose, and Throat (ENT) Surgeries
5. Cleft Lip & Palate and Craniofacial Surgeries
6. Neurosurgeries
7. Ophthalmic (eye) surgeries
8. Gastrointestinal procedures and surgeries
9. Orthopaedic and spinal surgeries
10. Urologic surgeries
11. Dermatological Surgeries
12. Plastic and reconstructive surgeries
13. Vascular surgeries
14. Pulmonology/respiratory tract procedure surgeries
The entire sedation, pain management, anaesthesia, and surgical care process is rigorously audited and accredited for safety and quality. The hospital benchmarks its surgical processes and outcomes with international best practice and has consistently achieved the required standards.

Respiratory illnesses account for a big portion of hospital visits with asthma being the most prevalent non-communicable paediatric condition. The respiratory medicine program provides preventive, diagnostic, and curative services.
Preventive services include parent/public education to prevent asthma development, asthma, primary prevention of infections that cause respiratory illnesses, prevention of complications from chronic respiratory conditions, prevention of allergies, and home management of emergencies relating to acute and/or severe respiratory conditions.
Diagnostic services include pulse oximetry, spirometry and other lung function tests, laboratory tests including microscopy and molecular testing to diagnose infectious respiratory conditions, bronchoscopy, apnea diagnosis, and determination of causes of allergies.
Interventions include treatment of respiratory infections, management of allergic conditions, management of acute and chronic respiratory conditions like asthma, croup, and cystic fibrosis. For chronic illness, the parents/caregivers are part of the management team as most of the care is provided at the home setting on an ongoing basis. Other conditions that affect the respiratory function include congenital lung malformations, dysphagia, muscular dystrophy, scoliosis require a wider team of experts to provide treatment. Some of the treatments will require surgery.
Respiratory care is provided by a multidisciplinary team of paediatric pulmonologists, pharmacists, nurses, pathologists, respiratory therapists and indeed in most cases the parent/caregiver is spart of the care delivery team. The Asthma care program provides ongoing care for many children through and integrated preventive, diagnostic/monitoring, and treatment approach that aims at improving the children’s quality of life.
The respiratory care program also includes emergency care to treat respiratory related emergencies including but not limited to aspiration, choking , acute asthmatic exacerbation.

The endocrinology program focuses on diagnosis and management of disorders that results from the improper functioning of the endocrine system, which includes the glands that secrete hormones, the receptors that respond to hormones and the organs that are directly impacted by hormones.
A multidisciplinary team consisting of paediatric endocrinologists, paediatric nurses with training in endocrinology, pathologists, clinical pharmacists, nurse counsellors, child psychologists, and developmental paediatricians provide endocrinology services addressing prevention, diagnosis, treatment, and monitoring. The overall aim of the program is to achieve early diagnosis, implement early treatment, and to improve the long-term quality of life of the patients/clients receiving care. The endocrinology program benefits from primary, secondary, and tertiary prevention interventions.
Diabetes care accounts for a big part of the endocrinology program. Diabetes care includes screening and early diagnosis, patient/family education to support care at home, school based interventions to support school going children that have diabetes, nutritional counselling and support, psychosocial care, and transition care to ensure teens and young adults continue with optimal care for diabetes from paediatric care treatment programs, and improved access to insulin.
The conditions managed through the endocrinology program include:
1) Type 1 diabetes, which starts in childhood or adolescence (Juvenile), in which the body does not produce any insulin
2) Type 2 diabetes, which starts in adolescence or adulthood, in which the insulin produced by the body does not work optimally.
3) Adrenal gland disorders, in which the adrenal glands make either too much or too little hormone, including congenital adrenal hyperplasia, and Cushing’s Syndrome
4) Growth disorders including delayed puberty, early puberty, growth hormone deficiency, short stature
5) Hypoglycaemia, in which blood glucose levels are low
6) Bone disorders including low bone density, rickets, osteoporosis, osteogenesis imperfecta (brittle bone disease), low calcium, high calcium, rickets.
7) Disorders of Sexual development including ambiguous genitalia
8) Pituitary disorders including diabetes insipidus, lipodystrophy, panhypopituitarism pituitary cysts, pituitary cancers
9) Thyroid disorders including hyperthyroidism, hypothyroidism, thyroid cancers
10) Genetic endocrine disorders

The haematology and oncology specialty focuses on providing high quality holistic care for blood conditions/illnesses and childhood cancer. A multidisciplinary team of paediatric haematology and oncologists, paediatric nurses, pathologists, clinical pharmacists, paediatricians, and surgeons provide integrated diagnosis, treatment, monitoring and post-treatment care.
Haematology and oncology service incorporates an early diagnosis program aimed at early detection of illnesses, early treatment, and improved care outcomes.
The haematology service treats a number of conditions including those listed below:
1) Anaemias including aplastic anaemia, thalassaemia, haemolytic anaemia, iron deficiency anaemia, megablastic anaemia
2) Bleeding and clotting disorders including haemophilia, Idiopathic Thrombocytopenic Purpura
3) Neutropenia
4) Vascular abnormalities
5) Inherited and acquired bone marrow failure
Sickle Cell Disease (SCD) management is a focused haematological service that is aimed at prevention, diagnosis, treatment, and long-term management of SCD and its complications. The SCD management program includes:
1. Screening and early diagnosis and genetic counselling
2. Pain management
3. Transfusion services including use of blood, blood products and/or blood substitutes were indicated .
4. Stroke prevention
5. Prevention and/or management of pulmonary ( like acute chest syndrome) and other possible complication s from SCD
6. Treatment with hydroxyurea
7. Imaging services including transcranial Doppler studies for stroke prevention, abdominal ultrasound for gallstones, imaging of the bones and joints to evaluate vascular necrosis, and imaging of the brain for detection of silent or overt stroke and narrowed blood vessels. Imaging techniques are also used to identify chronic organ damage from red cell sickling.
8. Psychosocial care for patients and families
9. Coordination of support group activities
10. SCD research

The paediatric oncology care includes
1) Screening and early diagnosis and counselling
2) Pain management
3) Transfusion services including use of blood, blood products and/or blood substitutes were indicated .
4) Laboratory and imaging tests for definitive diagnosis and monitoring of treatment
5) Management of haematological malignancies including leukemias, lymphomas
6) Management of solid tumours including brain cancers, kidney cancers, eye cancers, solid soft tissue cancers, bone cancers
7) Pre- and post-bone marrow transplant care and coordination of transplant services
8) Chemotherapy to treat cancer, blood disorders, and other conditions mostly done as a day (outpatient) service
9) Enzyme replacement therapy
10) Monoclonal antibody therapy
11) Immunoglobulin therapy and other immune therapy
12) Sedated lumbar puncture, bone marrow biopsy and intrathecal chemotherapy
13) Transfusion of red blood cells or platelets
14) Genetic testing
15) Psychosocial care for patients and families
16) Coordination of support group activities

The Gertrude’s Institute of Child Health and Research (GICHR) is located at the hospital’s Muthaiga campus. The main objective of the institute is to improve the quality of paediatric and adolescent care in Eastern Africa through focused education and research.
The institute is accredited by the Nursing Council of Kenya and the Technical and Vocational Education and Training Authority (TVETA).
The instate runs a full accredited paediatric nurse training school that provides specialist paediatric nurse training programs for both internally employed nurses and nurses from various institutions and countries in Africa. The institute established the first paediatric nursing and paediatric critical care nursing higher diploma courses in the Eastern Africa region and has so far trained over 500 nurses.
The certificates (credentials) for nursing programs are awarded by the Nursing Council of Kenya. The nursing courses are summarized below:
1. Higher Diploma in Paediatric Critical Care Nursing: One year program for already qualified and registered nurses. Application deadline is in March and August for April and September intakes.
2. Higher Diploma in Paediatric Nursing: One year program for already qualified and registered nurses. Application deadline is in March and August for April and September intakes.
3. Kenya Registered Community Health Nurse (KRCHN): A three year general nursing course for post – secondary school students with an aggregate KCSE grade of C plain with similar individual grades in English, Biology and a C- minus grade in mathematics or physics, or chemistry. Application deadline is in February and August for March and September intakes.
The institute runs paediatric sub-specialist training in collaboration with the respective specialties, universities, other hospitals, recognized professional associations, and professional regulatory authorities through either a collegiate (residency) or taught model. The hospital is a rotation site for paediatric endocrinology, paediatric critical care, paediatric neurology, paediatric cardiothoracic surgery, general paediatrics, radiology, pathology.
The Institute is accredited by the Resuscitation Council of the United Kingdom (RCUK) and runs the following two – day emergency courses certified by RCUK.
1) European Advance Life Support(EPALS)
2) Certificate in Paediatric Initial Life Support(PILS)
The Institute is also accredited by the America Heart Association to run the below two - day courses.
1) Paediatric Advanced Life Support
2) Advance Cardiac Life Support
The instate also runs a one- day certified Basic Life Support/Paediatric First Aid program
1) Paediatric Phlebotomy
In this three-week course, nurses, clinical officers, emergency medical technicians, healthcare assistants, and laboratory technicians are equipped with the knowledge and skills to provide safe and effective phlebotomy services to paediatric patients.
2) Emergency Medical Technician (EMT)
This seven – month course equips emergency medical technicians with the requisite knowledge and skills to provide paramedical care to patients before or during evacuation to hospital.
3) Certificate in Health Care Assistant Course(HCA)
This six-month course equips Health Care Assistants- (non-licensed caregivers) - with the requisite knowledge and skills to provide care to patients in the home setting or in hospitals under supervision. Applications for the course are accepted by December and June for the January and July intakes.
The Hospital is accredited by the National Commission for Science, Technology, and Innovation (NACOSTI) as a research institution. To this end the hospital has in place an Ethical Review Board that provides oversight for all research activities. The full range of research from operations research to clinical trials is carried out at the hospital.
The hospital has participated in six clinical trials successfully with four currently ongoing.



‘Healthy children, transformed communities, a better world.’
Gertrude’s Hospital Foundation was established by the registered Trustees of Gertrude’s Garden (Gertrude’s Children’s Hospital) in 2010 to provide quality healthcare to needy and vulnerable children in the society. The Foundation’s paediatric health intervention programmes provide quality diagnostic, treatment and care at no cost to children in the community especially those located in hard-to-reach areas in Kenya. Our mission is to ensure we improve access to quality healthcare services to needy and disadvantaged children in Kenya and the Eastern Africa region through the integration of care, research, education and technology.
The Foundation mobilizes resources and works with partners to support specialized treatment and care for over 20,000 children annually at the Gertrude’s Children’s Hospital. The Foundation also provides fellowship grants and scholarships for advanced training of paediatric specialists and nurses across more than 27 specializations. To date, the Foundation has impacted more than 300,000 beneficiaries and facilitated training for over 50 Paediatricians and 100 nurses trained since founding.
We are persuaded that by expanding access to quality healthcare, we can transform the course of every child’s development for good. We aim to achieve this at scale through resource mobilization and development of high impact strategic partnerships in order to offer hope to a generation that would otherwise not enjoy the full benefit of good health and realization of their full potential.
The 2023-2027 Strategic Plan seeks to ensure delivery of our mandate and impact at scale in the Eastern Africa region. The strategic Plan is anchored on 3 core pillars to deliver its impact at scale;
This is the main pillar of the Foundation. We champion the establishment of national systems to provide tertiary and specialist care for chronic NCDs including cancer, heart disease, diabetes, sickle cell disease, and neurodevelopmental disorders among many others. The coordination of the diagnosis, treatment and data management of these complex diseases and conditions is carried out by Gertrude’s Children’s Hospital.
This pillar anchors our major specialist health programmes including The Cancer Initiative, Cardiac Programme, HIV/Aids Programme, Cleft Lip & Palate Surgery Program, Children with Special Needs program, Laikipia Outreach Program and Telemedicine Program.
Specialist care depends on the availability of specialist skills. We work with partners to address the deficit in human resources for health through channelling fellowship grants to train healthcare workers in the care & management of childhood diseases as well as conduct research in clinical areas, population health and other education-associated research.
The Foundation plays a critical influencing role in driving the achievement of sustainable development goals (SDGs) for children. Through a thought leadership agenda, we engage other organizations from the public, private and the development sectors to drive advocacy of 18 Global SDG indicators concerned with children. We do this by sharing data, insights and fresh knowledge that enables collaborative action towards development and implementation of laws, policies and practices that promote holistic child development. Under this pillar we address health and developmental needs of children and adolescents through education, play, nutrition, culture especially among vulnerable communities living in Arid and Semi-arid areas (ASAL) in Kenya.
Specialist paediatric health services require heavy investment. The Foundation fundraises for the enhancement of Gertrude’s Children’s Hospital critical healthcare infrastructure and enhances the capacity of other public, mission based and community managed facilities in Kenya by directing partner support for equipping of needed facilities, purchase of medical supplies and setup of tertiary and specialist care.
The Foundation collaborates with the Kenyan national & county governments and the National Health Insurance Fund (NHIF). We are leading the agenda in engaging the government, NHIF and other healthcare stakeholders to establish national systems to identify, treat and provide care for noncommunicable diseases including cancer, diabetes, congenital heart diseases, neurodevelopmental conditions in children, etc.
The Foundation is strategically placed to deliver high impact holistic child health and development programmes across Kenya and the region. We are a partner of choice for private sector and donor organisations looking to invest in transformational healthcare and developmental impact for children in this geographical landscape. We understand the gaps that need to be addressed to ensure achievement of child focused SDG goals. Our impact programmes are delivered through collaborations with other reputable local and global partners ensuring that donor funds are committed to attain the highest level of transformational impact for children and their communities
To get in touch for partnerships, please contact: The Head of Foundation
P.O. Box 42325 – 0010, Nairobi Kenya
Email: foundation@gerties.org or ksimiyu@gerties.org
A special thank you to our partners: