GeriNotes





5 Contemporary Climate-Related Challenges to Geriatric Health and Clinical Practice by Cindy Lane Moore, PT, DPT, PhD, MPH
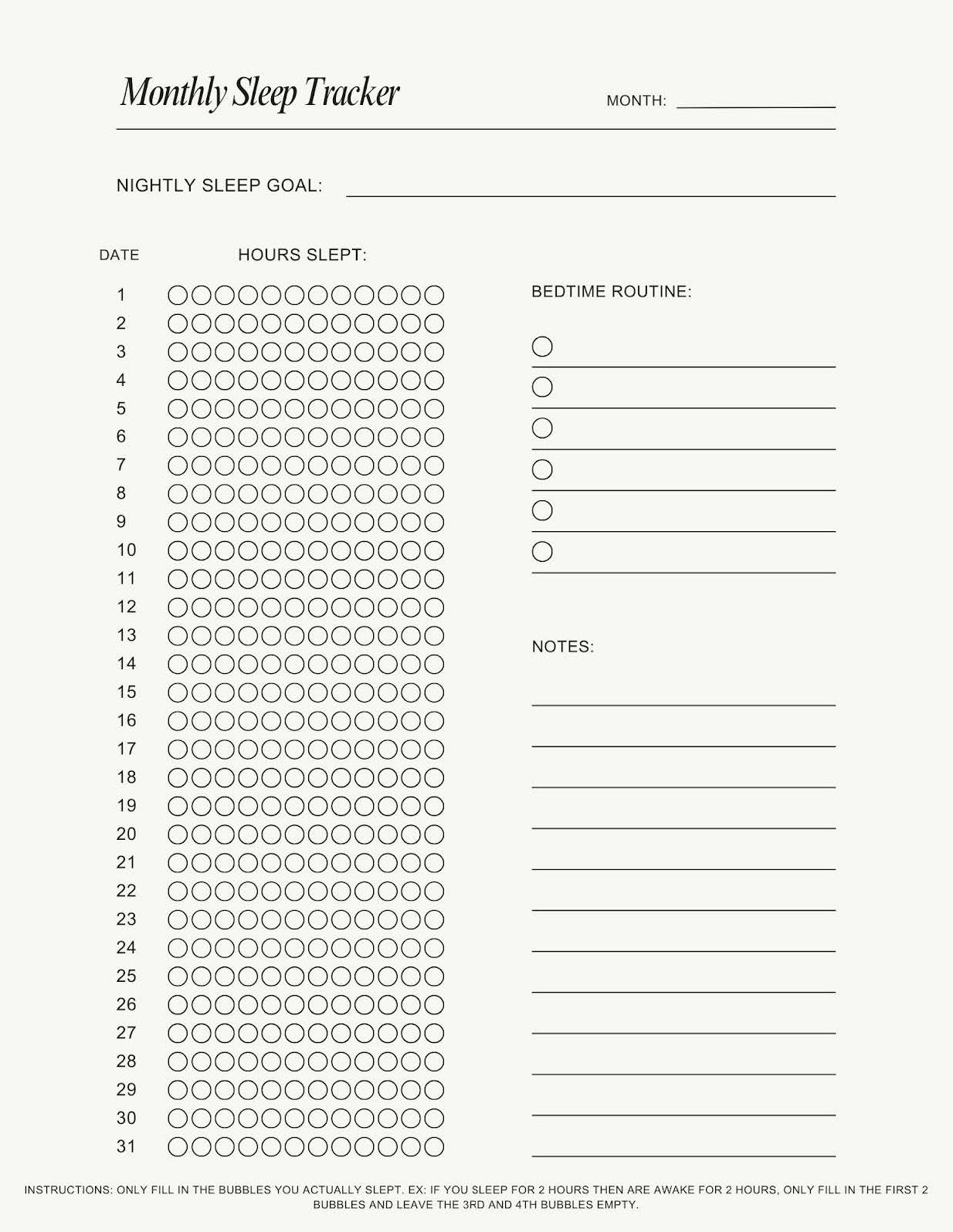
11 Sleep and Cognition Handouts: The Link Between Cognitive and Mental Health and Sleep: Part 3 of 3 by Alex Alexander, PT, DPT and Cathy Stucker, PT, DSc, CMPT
16 Advocacy is Essential to Advancing the Profession by Ellen R. Strunk, PT, MS
17 Journal Club: The Effects of Manual Therapy Interventions on Kyphosis in Older Adults by Danielle Simon, PT, DPT and Zachary Ammons, PT, DPT
20 Residency Corner: The 3-Meter Backward Walk Test: A Review by Holly J. Roberts, PT, PhD, Rovin Ian Antonio, SPT, and Teri Lake-Coblio, SPT
APTA Geriatrics, An Academy of the American Physical Therapy Association
APTA Geriatrics Board of Directors
President: Cathy Ciolek, PT, DPT, FAPTA
Vice President: Myles Quiben, PT, DPT, MS, PhD
Secretary: Mariana Wingood, PT, DPT, PhD
Treasurer: Ken Miller, PT, DPT
Chief Delegate: Beth Black, PT
Director: Jill Fitzgerald, PT, DPT
Director: Suzanne Ryer, PT, DPT
Director: Annalisa Na, PT, DPT, PhD
Director: Kaelee Brockway PT, DPT
APTA Geriatrics Special Interest Group Chairs
Balance & Falls: Caryl Ventura,, PT, DPT
Bone Health: Aliya Decates-Miller, PT, DPT, Cognitive & Mental Health: Alexandra Alexander, PT, DPT Global Health for Ageing Adults: Mindy Oxman Renfro, PT, DPT, PhD
Health Promotion & Wellness: Heidi Moyer, PT, DPT
Residency & Fellowship: Chelsea Lavelle, PT, DPT
Skilled Nursing Facilities: Rich White, PT, DPT
Questions for APTA Geriatrics leaders and staff can be submitted to geriatrics@aptageriatrics.org
APTA Geriatrics, An Academy of the American Physical Therapy Association 1818 Parmenter St, Ste 300 Middleton, WI 53562
APTA Geriatrics Staff
Executive Director: Christina McCoy, CAE
Education Manager: Jonathan Vega
Program Coordinator: Taylor St. John
Membership Manager: Kim Thompson
Marketing and Communications Manager: Abby Wicker/ Alex Connelly
Financials Manager: Gina Staskal, CNAP


We are excited for GeriNotes to be moving to a new format for future articles. Look for communication about this change in the upcoming months.
Michele Stanley Editor, GeriNotes

Register for the free Journal Club discussion webinars and earn 1.5 contact hours. Questions for presenters may be emailed to gerinoteseditor@gmail.com before or on the day of the webinar. See what's coming up at https://aptageriatrics.thinkific.com/collections

GeriNotes
GeriNotes Editorial Board
Michele Stanley, PT, DPT
Debra Barrett, PT
Jennifer Bottomley, PT, MS, PhD
Kathy Brewer, PT, DPT, MEd
Chris Childers, PT, PhD
Jennifer Gindoff, PT, DPT, DHSc
Jill Heitzman, PT, DPT, PhD
William Staples, PT, DPT, DHSc, FAPTA
Ellen Strunk, PT, MS
GeriNotes Editor
Michele Stanley, PT, DPT
gerinoteseditor@gmail.com
Copyright © 2025 All rights reserved.
Published in January April June August
November
Copy Deadlines
February 1
April 1
July 1
September 15
November 1
GeriNotes is the official magazine of the Academy of Geriatric Physical Therapy. It is not, however, a peer-reviewed publication. Opinions expressed by the authors are their own and do not necessarily reflect the views of the APTA Geriatrics. The Editor reserves the right to edit manuscripts as necessary for publication.
APTA Geriatrics does not endorse, publish, or promote products, services, or events sponsored or hosted by for-profit commercial entities. For-profit companies and corporations may request to advertise on any of APTA Geriatrics’ platforms at the published rates. All advertisements that appear in or accompany GeriNotes are accepted on the basis of conformation to ethical physical therapy standards. Advertising does not imply endorsement by APTA Geriatrics. Mission: To provide engaging content that empowers the community of physical therapy clinicians to build expertise and expand the delivery of evidence‐informed care that promotes health and wellness in aging adults.
Vision: To create an evolving online community through which clinicians develop their knowledge and skills based in shared ideals that are person‐centered; and promote a world where aging adults move, live, and age well.
The Fragility Fracture Network (FFN) Annual Meeting
Oct 1-4, Porto, Portugal

by Kathleen K Mangione, PT, PhD, FGA, FAPTA and Jason R. Falvey, PT, DPT, PhD
The Fragility Fracture Network (FFN) is an international organization created to address the growing burden of fragility fracture patients to our health care system and societies. The vision of the FFN is a world where anybody who sustains a fragility fracture achieves the optimal recovery of independent function and quality of life, with no further fractures. Their mission is to optimize the multidisciplinary management of the patient with a fragility fracture, including secondary prevention.
The FFN hosts annual meetings addressing the full pathway of care for fragility fracture patients including perioperative care, surgical treatment, rehabilitation, secondary prevention, and policy change. This year the annual meeting will be in Porto, Portugal from Oct 1-4, 2025. Besides being a beautiful location, fabulous food and wine, and engaging colleagues, there are many educational sessions focused for the physical therapy community.

Physical therapist researchers from around the world will be presenting topics including:
1. Exercise and other non-pharmacological strategies for recovery after vertebral fracture
2. Pain assessment and management in acute fragility fracture: tailoring approaches in patients with delirium, dementia, and depression
3. Motivational interviewing and social support for older adults after hip fracture
4. World Falls Prevention Society workshop: New technologies for fall risk assessment and prevention in older people
5. Opt-In RCT: OsteoPorosis Tailored exercise adherence Intervention
6. The AFTER trial results: ankle fracture rehabilitation
7. Bridging evidence and clinical practice: a workshop on early postoperative rehabilitation following a hip fracture
Membership in the FFN is free and online educational resources are available for members. Please consider joining us in Porto in October.
by Cindy Lane Moore, PT, DPT, PhD, MPH
Climate Change is Affecting Geriatric Health and Clinical Practice
Increased intensities and frequencies of heat, air pollution, and weather disaster events can adversely affect health across the lifespan. Older adults are particularly vulnerable for a variety of physiological, environmental, and social reasons. The purpose of this article is to help physical therapists (PTs) and physical therapist assistants (PTAs) appreciate and address climate-related geriatric health risks by incorporating environment-informed assessment, intervention, and education in their clinical practice. These contemporary adaptations to physical therapy practice can optimize the health, function, mobility and safety of the clients and communities we serve.
Heat-related illness (HRI) including heat stress, heat exhaustion, and heat stroke threatens people of all ages,
but older adults are particularly vulnerable.1 Extreme heat is dangerous; it increases risk of emergency department visit and hospitalization for heat-related illness such as fluid and electrolyte disorders, heat stroke, cardiovascular disease, respiratory disorders, renal disease, acute kidney failure, urinary tract infection, septicemia, and mental disorders.2-5 Global heat-related deaths for those aged 65+ increased by 85% over the past two decades (2000-2020), and are expected to increase 370% between 2014-2060 under a 2C global temperature increase scenario.6 Factors increasing HRI risk include physical and financial barriers to accessing cooler environments, poor heat safety judgment, and diminished thermoregulation due to physiological changes with aging, medications, and medical conditions such as diabetes and heart failure (Table 1) 3
Physical therapy professionals consider clients’ environments, medical conditions, and types of medications when assessing and addressing their fall risk. They can similarly consider those factors for HRI
Factors increasing risk for heat-related
• Decreased thermoregulation from medications
• Decreased thermoregulation from health conditions, such as diabetes and heart failure
• Decreased thermoregulation from normal physiological aging, such as reduced sweating capacity, skin vasodilation, and thermal discomfort perception
• Decreased heat safety judgement from cognitive impairments
• Physical or financial barriers to accessing a cooler environment
Recognition of and response to heat-related illness:
• Heat cramps
– Symptoms: leg, arm or abdomen severe muscle cramping during/after strenuous exercise in high heat (related to heavy sweating and salt depletion)
– Hydrate and avoid alcohol or caffeine. Rest in a cool area. Seek medical help if cramps do not resolve in one hour. Minimize activity for several hours after cramps resolve to reduce risk of progression to heat exhaustion or heat stroke.
• Heat exhaustion
– Symptoms: nausea or vomiting; extreme thirst; dizziness; fatigue; weakness; clammy skin; rapid breathing and/or pulse
– Hydrate and avoid alcohol or caffeine. Rest in a cool environment. Cool bath/shower. Seek medical attention if symptoms do not resolve.
• Heat stroke is a medical emergency! Body temperature can rise to 106F+ in less than 10 minutes.
– Symptoms: red/hot/dry skin; no sweating; strong/rapid or slow/weak pulse
– Call for emergency help immediately. Move victim to a shady/cool area. While awaiting help, cool victim as much as possible by cool water bath/shower/spray, wrapping in cool wet towels/sheets, applying cold to armpits
Prevention by older adult and caregiver
• Avoid strenuous activity, which may include exercise program modifications
• Optimize body coolness (wearing loose, lightweight clothing; taking cool showers or baths
• Optimize living space coolness (fans; air conditioning if hot / >90F; minimize stove/oven use)
• Know how to access cool spaces / cooling center if needed
• Stay hydrated (don’t wait until thirsty to drink; if on diuretics and/or fluid restriction, ask physician how much to drink in hot weather)
• Plan and implement frequent safety check-ins, such as twice daily checks with family/neighbors during hot days
risk reduction. Many older physical therapy patients take medications potentially impairing thermoregulation (Table 2), and many also have health conditions predisposing them to HRI. Even healthy older adults may be susceptible due to age-related reduced thermoregulatory function, hemodynamic stability, body fluid regulation, and perception of thermal and physical strain during heat exposure.3,7,8
Physical therapy professionals can incorporate HRI risk reduction into their practice. This may include instruction in preventing, identifying and responding to heat-related illness. Clinicians delivering home care services during high event days may instruct patients/caregivers in heat safety and cooling resources; clinicians in outpatient settings or preparing patients for discharge to home may consider doing the same. Heat safety posters and fliers may be placed on clinic walls and/or be made available in waiting rooms, admission packets, and community health fairs. Clients may benefit from explicit instruction in how to tailor activity types (including HEPs) and timing to the heat index and how to access safe planning information.9 For example, the National Weather Service color-coded HeatRisk tool provides a seven-day heat danger forecast indicating regions where those who are moderately and extremely sensitive to heat and even where the general population should exercise caution.
Enhancing older adults’ mobility and function may facilitate their performance of heat safety tasks such as closing window blinds, donning cooler clothing, and moving to cooler locations. Mobility gains may also enable clients to become more connected to people and resources within their communities, combatting the social isolation that amplifies heat mortality risks.10,11 Clinicians may need to educate patients and caregivers about how some medications, while critical for disease management, may require extra caution during heatwaves.(Table 2) For example, anticholinergics and psychotropics may diminish body thermoregulation during extreme heat, triggering altered respiratory and heart rate and altered blood pressure, viscosity, and coagulability.12 Extreme heat may also raise integumentary concerns. Patients may need to be instructed to more frequently remove prosthetic/orthotic devices or change compression garments during extreme heat to enable skin and device drying to facilitate body cooling and reduce the risk of bacterial or fungal infections.
Climate warming impacts geriatric health in additional ways. Warmer weather is also associated with progression of conditions such as Parkinson’s Disease.13 Climate-change related expansion of vector-borne diseases such as Lyme’s and West Nile adversely affects older adults who have weaker immune systems, and are at greater risk of serious illness and poor treatment outcomes.14-17 Geriatric immune dysregulation also makes older adults more susceptible to allergic reactions and inflammatory responses, including allergies from
inhaled irritants such as pollen.18,19 Temperature rise in many geographic regions has been accompanied by increased pollen season duration and intensity, negatively impacting quality of life and sometimes requiring affected persons to mask and/or limit outdoor activities on high pollen count days. Allergies can be more than an inconvenience; in older adults allergic rhinitis and upper airway exposure to inflammatory triggers such as pollen and other pollutants increases risk of stroke and of hospitalization related to other pathologies.18 As noted in Table 2, antihistamines are among the many medications that alter thermoregulation.Heat and air pollution were identified as 2 factors most negatively affecting cardiovascular and respiratory morbidity and mortality in older adults, and also affecting mental health and cognitive function.20 Heat can increase level of air pollution and vice versa, and their co-occurrence compounds respiratory and cardiovascular risk.12 These 2 environmental factors synergistically increase the potency and range of pollen and other allergens and appear to exacerbate general age-related declines in immune function (“immunosenescence”) and inflammation (“inflammaging”), resulting in increased problems with allergies, asthma, and other conditions.21,22
Clinicians understand that air pollution can cause respiratory problems. Asthma and chronic obstructive pulmonary disease (COPD) exacerbations from air pollution including ground level ozone and particulate matter decrease lung function and increase emergency visits and hospitalizations for people of all ages, even healthy adults.23 Chronic conditions and compromised immune function related to aging or other causes pose additional risks.24,25 Alveolar inflammation and oxidative stress may cause respiratory system cellular damage, and reduced airway mucus composition and secretion rates may contribute to reduced mucociliary clearance.26 Like smoking, environmental pollutants can reduce cilia length and its beating frequency and synchronization.26
Clinicians may be less aware of air pollution’s harmful impacts beyond the respiratory system. Air pollution exposure negatively impacts older adults’ performance-based physical functioning.27 Particulate matter exposure is linked to cardiovascular, endocrine, ocular, and cognitive and neurodegenerative disorders.24,26 How can such wide-ranging effects occur? Inhaled fine particulate matter can cross from the alveoli into the bloodstream and move throughout the body, resulting in systemic inflammation, oxidative stress, autonomic and endothelial dysfunction causing blood vessel narrowing and stiffening leading to heart attacks, peripheral artery disease, and other circulatory conditions.24 Particulate matter exposure also alters heart tissue structure and function, increasing risk for arrhythmias, heart failure and ischemic events.24 Toxic heavy metals riding “piggyback”
Diuretics
Beta blockers
Antihypertensives
Calcium channel blockers
Angiotensin Converting Enzyme Inhibitor (ACEIs)
Angiotension II Receptor blockers (ARBs)
Angiotensin Receptor-Neprilsyn Inhibitors (ARNIs)
Anti-platelets
Antianginals Nitrates
Antiseizure
Antihistamines w/ cholinergic properties
Analgesics
Antibiotics
Antiretrovirals
Thyroid replacement
Furosemide, Hydrochlorothiazide, Acetazolamide
Atenolol, Metoprolol, Propranolol
- electrolyte imbalance - ↓ thirst sensation
- hypovolemia, dehydration, fainting/ falls risk)
- ↓ superficial vasodilation
- ↓sweating - ↓BP, ↑ risk fainting /falls
Amlodipine, Felodipine, Nefedipine - ↓ BP, ↑ risk fainting/falls - electrolyte imbalance
ACEIs: Enalapril, Lisinopril, Ramipril
ARBs: Losartan, Valsartan ARNIs: Sacubitril - ↓ BP, ↑ risk fainting & falls - ↓ thirst sensation
Clopidogrel, Aspirin - ↑ superficial vasodilation
Glyceryl Trinitrate, Isosorbide, Mononitrate - ↑ hypotension
Topiramate - ↓sweating
Oxcarbazepine - ↑ sweating - ↑ urination
Carbamazepine - dizziness & weakness
Promethazine, Doxylamine, Diphenhydramine - ↓ sweating - impaired thermoregulation
NSAIDS - kidney injury w/ dehydration
Aspirin
- ↑ heat production with O/D - kidney injury w/ dehydration
Acetaminophen - heat-related liver injury - ↑ hepatoxicity risk
Sulfonamides - kidney injury risk w/ dehydration
Indinavir - kidney injury risk w/ dehydration
Levothyroxine - excessive sweating
Psychiatric
Stimulants
Hallucinogens
Mood stabilizer
Antipsychotics
Selective Serotonin Reuptake Inhibitors (SSRI
Serotonin and Norepinephrine Reuptake Inhibitors (SNRI)
Lithium
- diabetes insipidus induced water loss: risk for fainting, falls - electrolyte imbalance - dehydration-related ↑ toxicity
Haloperidol, Olanzapine, Quetiapine, Risperidone - impaired sweating - impaired temperature
SSRI: Fluoxetine, Sertraline
SNRI: Duloxatine, Ventlafaxine - ↑ sweating
Tricyclic antidepressants (TCSa) Amitriptyline, Clomipramine - ↓ sweating
Amphetamine, Methylphenidate - ↑ body temperature
Cocaine - ↓ sweating - ↓ dilation of skin blood vessels - impaired heat perception
Methylenedioxy-methamphetami ne (MDMA) & alternatives - ↓ sweating - ↓ dilation of skin blood vessels - impaired heat perception
Alcohol - ↑ sweating - ↑ urination - impaired heat perception
*Adapted from U.S. Centers for Disease Control and Prevention (2024) Heat and edications — guidance for clinicians.
on particulate matter may initiate and stimulate cancer cell growth.24 Additionally, air pollution may contribute to diabetes risk by visceral adipose inflammation, altered liver lipid metabolism, and low levels of DNA methylation. Dose-response correlations have been found between ambient nitrogen dioxide and Parkinson’s disease,28 and between fine particulate matter and stroke and depressed mood.29,30 Physical therapy professionals can promote patient and community adaptive behaviors to minimize air pollution exposures. These may include tailoring or limiting outdoor activities and/or masking in accordance with air quality. Free zip code-based air quality index readings and activity guides are available in English and Spanish for particle pollution and ozone.These offer tips for safe activity modifications for sensitive groups such as older adults. This information can be incorporated into patient education and posted in clinics. In keeping with their ethical obligation to “do no harm”, PTs and PTAs can also support health system and community sustainability efforts to reduce air pollution.31-34
Older adults are particularly vulnerable to post-weather disaster morbidity and mortality. Approximately threequarters of Hurricane Katrina deaths occurred in those aged 60+.35 Prolonged and limited recovery from weather disasters may be as consequential as the initial event. For example, weather disasters are associated with increased cardiovascular risks persisting many months after the event.12 Much of cyclone- and hurricane-related mortality and morbidity are related to challenges experienced in the days, weeks, and months after landfall, both for those forced to evacuate and those sheltering and remaining in place.12,36,37
Disaster-related disruptions of medical care can result in chronic disease onset or progression.38-40 Evacuation and shelter-in-place present profound challenges and risks for older adults and/or those with disabilities who have insufficient physical, social, and financial resources to accommodate health needs and mobility limitations.41,42 Disaster survivors may encounter a variety of medication management barriers: unavailability, unaffordability, lack of safe storage conditions, inaccessible personal medication lists and histories limiting patients’ recall of what to take when and obtain refills.38 Medical monitoring and assistive devices may be damaged, lost, or nonfunctional due to power outages, and post-disaster food procurement and storage options for chronic disease-specific diets may be limited.25,38,43 Disaster-related mental health impacts have been broadly investigated and include post-traumatic stress disorder, depression, general anxiety, grief, and sense of loss.44 Climate change increases chances of experiencing multiple disasters, significantly elevating mental health impacts.45 Older adults and people with chronic conditions are at elevated risk for post-disaster mental health problems due to
social, physical and financial vulnerabilities.46 Extreme weather events, increased rainfall, and rising temperatures alter ecosystems and contribute to the spread of waterborne and vector-borne diseases to which immunocompromised older adults are particularly vulnerable.47
As weather disasters become more commonplace, physical therapy professionals need to consider offering more detailed, individualized patient and caregiver education regarding how to stay safe during and after extreme weather events, under shelter-in-place, and/or evacuation. This may include providing information on resources specific to the patients’ municipality or zip code such as special needs registries for emergency responders, alternatives to electricity-powered devices during power outages, and recommended “go bag” contents. Physical therapists may connect patients and caregivers with publicly available emergency preparedness resources such as the American Association of Clinical Endocrinology’s My Diabetes Emergency Plan. Older adults have been found to benefit from having a well-developed emergency plan with rich components, such as what to do in various circumstances, in order to facilitate prompt responses to urgent situations.48
Physical therapy interventions to improve mobility and function may enable older adults to physically prepare for and respond to weather disasters requiring evacuation or shelter in place, and to maintain social connections critical for disaster survival.22 After extreme weather events, patients may have difficulty getting to all their medical appointments, making it especially important for home care or other PTs and PTAs who are seeing patients – in person or virtually — to notice and address adverse event red flags.38,42
Physical therapy professionals can contemporize geriatric care in several ways: Assessing and addressing climate-related health problems. While most people are concerned about climate change, our clients and communities may not understand how to minimize acute and long-term exposures and harms. We can teach them, help them address the climate-related harms they are experiencing, and prepare for future heat, air quality and weather disaster events, and do so within the scope of physical therapy practice. This is consistent with the World Physiotherapy’s policy statement.49 Physical therapy treatment interventions and intensities may need adjustments to accommodate patients’ climate change-related exacerbations of chronic cardiovascular, respiratory, mental health and other conditions. Because heat, air pollution, and weather disasters can contribute to a variety of mental health problems, PTs may need to refer patients to support services.
Effective disaster planning can help clients, health entities, and the communities they serve promptly resume function after disasters strike. Clinicians may use digital technologies including telehealth to continue services when extreme heat, poor outdoor air quality, or weather disasters preclude patient travel to treatment facilities or clinician travel to offices or patients’ homes. even when patients and offices cannot be accessed in person.50 By optimizing elders’ ability to participate in community events and communications, we help them improve their quality of life and access to social capital that can source disaster recovery or support safety during heat waves.41 Higher levels of community social cohesion protects against extreme heat and weather disaster mortality and may partially offset adverse health effects that disproportionately affect disadvantaged and vulnerable populations.51
Physical therapy professionals can encourage their health systems to participate in networks such as Practice Greenhealth or The Joint Commission’s Sustainable Healthcare Certification program or to embrace sustainability in other ways.52,53 They can support assistive devices (wheelchairs, braces, transfer aids), exercise equipment and wearables refurbishment and re-use, reducing waste and the need for new resource intensive production while saving money. Refurbishing ambulation assistive devices generated 98% less carbon emissions than buying new devices.54 An APTA position statement supports environmentally responsible practice and “enhanced public awareness of the effect of the environment on human movement, health, and safety”.55 Physical therapy contributes to environmental stewardship by helping people stay healthy and enabling them to avoid more environmentally harmful procedures like surgery and products like medicines.33,34 Clinicians are viewed by the public as trusted messengers and able to advocate for greener practices and environmental justice at municipal, state and federal levels.
Physical therapy professionals use a holistic approach to optimize older adults’ health, wellness, function and safety. Integrating climate-informed care into geriatric physical therapy care practice aligns with these goals and acknowledges climate change as a “threat multiplier” that compounds health risks from advanced age.56 Climate-informed geriatric physical therapy practice adaptations including assessing and addressing climate-related health problems, supporting resilience, and advocating for healthier environments for all.
1. U.S. Centers for Disease Control & Prevention. Heat health: Clinical Overview of Heat. https://www.cdc.gov/heat-health/hcp/ clinical-overview/index.html
2. Bobb JF, Obermeyer Z, Wang Y, Dominici F. Cause-specific risk of hospital admission related to extreme heat in older adults. JAMA Dec 24-31 2014;312(24):2659-67. doi:10.1001/jama.2014.15715
3. Meade RD, Akerman AP, Notley SR, et al. Physiological factors characterizing heat-vulnerable older adults: A narrative review. Environ Int . Nov 2020;144:105909. doi:10.1016/j.envint.2020. 105909
4. Hopp S, Dominici F, Bobb JF. Medical diagnoses of heat wave-related hospital admissions in older adults. Prev Med . May 2018;110:81-85. doi:10.1016/j.ypmed.2018.02.001
5. Li M, Shaw BA, Zhang W, Vásquez E, Lin S. Impact of Extremely Hot Days on Emergency Department Visits for Cardiovascular Disease among Older Adults in New York State. Int J Environ Res Public Health . Jun 14 2019;16(12)doi:10.3390/ijerph16122119
6. Tipaldo JF, Balk D, Hunter LM. A framework for ageing and health vulnerabilities in a changing climate. Nature Climate Change . 2024/10/25 2024;doi:10.1038/s41558-024-02156-2
7. Figueiredo T, Midão L, Rocha P, et al. The interplay between climate change and ageing: A systematic review of health indicators. PLoS One . 2024;19(4):e0297116. doi:10.1371/journal.pone.0297116
8. Millyard A, Layden JD, Pyne DB, Edwards AM, Bloxham SR. Impairments to Thermoregulation in the Elderly During Heat Exposure Events. Gerontol Geriatr Med . Jan-Dec 2020;6:2333721420932432. doi:10.1177/2333721420932432
9. U.S. Centers for Disease Control & Prevention. About heat and your health. Accessed April 11, 2025. https://www.cdc.gov/heat-health/ about/index.html
10. Nunes AR. General and specified vulnerability to extreme temperatures among older adults. Int J Environ Health Res Oct 2020;30(5):515-532. doi:10.1080/09603123.2019.1609655
11. Thiamwong L, Kim D, Emrich CT. Health Disparities and Maladaptive Behavior in Response to Extreme Heat: Impacts on Mental Health Among Older Adults. J Psychosoc Nurs Ment Health Serv . Aug 2024;62(8):2-4. doi:10.3928/02793695-20240711-01
12. Kazi DS, Katznelson E, Liu C-L, et al. Climate Change and Ca diovascular Health: A Systematic Review. JAMA Cardiology . 2024;9(8):748-757. doi:10.1001/jamacardio.2024.1321
13. Bongioanni P, Del Carratore R, Dolciotti C, Diana A, Buizza R. Effects of Global Warming on Patients with Dementia, Motor Neuron or Parkinson's Diseases: A Comparison among Cortical and Subcortical Disorders. Int J Environ Res Public Health . Oct 18 2022;19(20)doi:10.3390/ijerph192013429
14. Boršič K, Blagus R, Cerar T, Strle F, Stupica D. Clinical Course, Serologic Response, and Long-Term Outcome in Elderly Patients with Early Lyme Borreliosis. J Clin Med . Dec 2 2018;7(12) doi:10.3390/jcm7120506
15. U.S. Centers for Disease Control and Prevention. West Nile: Symptoms, diagnosis and treatment. Accessed April 10, 2025. https://www.cdc.gov/west-nile-virus/symptoms-diagnosistreatment/index.html
16. Fay R, Keyel A, Ciota A. Chapter Three - West Nile virus and climate change. In: Roossinck MJ, ed. Adv Virus Res . Academic Press; 2022:147-193.
17. Hosseini M, Zargoush M, Ghazalbash S. Climate crisis risks to elderly health: Strategies for effective promotion and response. Health Promot Int . 2024;39(2)doi:10.1093/heapro/daae031
18. De Martinis M, Sirufo MM, Ginaldi L. Allergy and Aging: An Old/ New Emerging Health Issue. Aging Dis . Apr 2017;8(2):162-175. doi:10.14336/ad.2016.0831
19. Di Lorenzo G, Melluso M, Rodolico A, Seidita A. Allergic Diseases in the Elderly. Transl Med UniSa . 2023;25(2):52-62. doi:10.37825/22399747.1046
20. Montoro-Ramírez EM, Parra-Anguita L, Álvarez-Nieto C, Parra G, López-Medina IM. Climate change effects in older people's health: A scoping review. J Adv Nurs . 2024;n/a(n/a)doi: https://doi. org/10.1111/jan.16270
21. Sampath V, Aguilera J, Prunicki M, Nadeau KC. Mechanisms of climate change and related air pollution on the immune system leading to allergic disease and asthma. Semin Immunol . May 2023;67:101765. doi:10.1016/j.smim.2023.101765
22. Anu A, Sonia G, Ismail K. Effect of climate change on health in older persons. WJCM . 2023;5(2):79-84. doi:10.18772/26180197.2023. v5n2a
23. Di Q, Wang Y, Zanobetti A, et al. Air Pollution and Mortality in the Medicare Population. N Engl J Med . Jun 29 2017;376(26): 2513-2522. doi:10.1056/NEJMoa1702747
24. Amnuaylojaroen T, Parasin N. Pathogenesis of PM(2.5)-Related Disorders in Different Age Groups: Children, Adults, and the Elderly. Epigenomes . Mar 31 2024;8(2)doi:10.3390/epigenomes8020013
25. Gamble JL, Balbus J, Berger M, et al. Populations of Concern . 2016:247-286. The impacts of climate change on human health in the United States: A scientific assessment https://doi.org/10.7930/ J0Q81B0T
26. Marczynski M, Lieleg O. Forgotten but not gone: Particulate matter as contaminations of mucosal systems. Biophys Rev (Melville) . Sep 2021;2(3):031302. doi:10.1063/5.0054075
27. de Zwart F, Brunekreef B, Timmermans E, Deeg D, Gehring U. Air Pollution and Performance-Based Physical Functioning in Dutch Older Adults. Environ Health Perspect . Jan 19 2018;126(1):017009. doi:10.1289/ehp2239
28. Cao Z, Yuan Y, White AJ, et al. Air Pollutants and Risk of Parkinson's Disease among Women in the Sister Study. Environ Health Perspect . Jan 2024;132(1):17001. doi:10.1289/ehp13009
29. Hameed S, Karim N, Wasay M, Venketasubramanian N. Emerging Stroke Risk Factors: A Focus on Infectious and Environmental Determinants. J Cardiovasc Dev Dis . Jan 11 2024;11(1)doi:10.3390/ jcdd11010019
30. Jo K. Evaluating the Effects of Long-Term Exposure to Fine Particulate Matter (PM(2.5)) on Depressive Mood among Korean Older Adults Using Multilevel Analysis. Iran J Public Health . Aug 2024;53(8):1785-1795. doi:10.18502/ijph.v53i8.16284
31. Environmental Physiotherapy Association. How to make your physiotherapy clinic more environmentally sustainable. https://environmentalphysio.com/practice/how-to-make-yourphysiotherapy-clinic-more-sustainable/
32. Maric F, Griech SF, Davenport TE. Advancing Environmental Stewardship in Physical Therapy: Connect, Learn, Act. Cardiopulm Phys Ther J . 2022;33(1):2-4. doi:10.1097/cpt.0000000000000189
33. Palstam A, Sehdev S, Barna S, Andersson M, Liebenberg N. Sustainability in physiotherapy and rehabilitation. Orthopaedics and Trauma . 2022;
34. Stanhope J, Maric F, Rothmore P, Weinstein P. Physiotherapy and ecosystem services: improving the health of our patients, the population, and the environment. Physiother Theory Pract . Feb 2023;39(2):227-240. doi:10.1080/09593985.2021.2015814
35. Becquart NA, Naumova EN, Singh G, Chui KKH. Cardiovascular Disease Hospitalizations in Louisiana Parishes’ Elderly before, during and after Hurricane Katrina. Int J Environ Res Public Health . 2019;16(1):74.
36. Dosa D, Feng Z, Hyer K, Brown LM, Thomas K, Mor V. Effects of Hurricane Katrina on nursing facility resident mortality, hospitalization, and functional decline. Disaster Med Public Health Prep . Sep 2010;4 Suppl 1(0 1):S28-32. doi:10.1001/dmp.2010.11
37. Lawrence WR, Lin Z, Lipton EA, et al. After the Storm: Short-term and Long-term Health Effects Following Superstorm Sandy among the Elderly. Disaster Med Public Health Prep . Feb 2019;13(1):28-32. doi:10.1017/dmp.2018.152
38. Arrieta MI, Foreman RD, Crook ED, Icenogle ML. Providing continuity of care for chronic diseases in the aftermath of Katrina: from field experience to policy recommendations. Disaster Med Public Health Prep . Oct 2009;3(3):174-82. doi:10.1097/DMP.0b013e3181b66ae4
39. Bell SA, Horowitz J, Iwashyna T. Home Health Service Provision After Hurricane Harvey. Disaster Med Public Health Prep . Feb 2020;14(1):56-62. doi:10.1017/dmp.2019.27
40. Lynch KA, Merdjanoff AA. Impact of Disasters on Older Adult Cancer Outcomes: A Scoping Review. JCO Glob Oncol . Jun 2023;9:e2200374. doi:10.1200/go.22.00374
41. Meyer MA. Elderly Perceptions of Social Capital and Age-Related Disaster Vulnerability. Disaster Med Public Health Prep . Feb 2017;11(1):48-55. doi:10.1017/dmp.2016.139
42. Wu Y, Wen B, Gasevic D, et al. Climate Change, Floods, and Human Health. N Engl J Med . 2024;391(20) : 1949-1958. doi:doi:10.1056/ NEJMsr2402457
43. Chalupka S, Trombley J. Climate Change and the Health of Older Adults. In: McDermott-Levy R, Jackman-Murphy K, Leffers J, Cantu A, eds. Environmental Health in Nursing . 3rd ed. Alliance of Nurses for Healthy Environments; 2013.
44. Dodgen D, Donato D, Kelly N, et al. Ch. 8: Mental Health and Well-Being. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment . U.S. Global Change Research Program; 2016:217–246.
45. Lowe SR, McGrath JA, Young MN, et al. Cumulative Disaster Exposure and Mental and Physical Health Symptoms Among a Large Sample of Gulf Coast Residents. J Trauma Stress . Apr 2019;32(2):196-205. doi:10.1002/jts.22392
46. Somasundaram DJ, van de Put WA. Management of trauma in special populations after a disaster. J Clin Psychiatry . 2006;67 Suppl 2:64-73.
47. Nichols G, Lake I, Heaviside C. Climate Change and Water-Related Infectious Diseases. Atmosphere . 2018;
48. Cong Z, Liang D, Luo J. Which Household Emergency Plans are More Helpful in Tornadoes? Through the Lens of Gerontology. Disaster Med Public Health Prep . Feb 2022;16(1):139-146. doi:10.1017/dmp.2020.194
49. World Physiotherapy. Policy statement: Climate change and health . 2023. June 2023. https://world.physio/policy/ps-climate-changeand-health
50. Zischke C, Simas V, Hing W, Milne N, Spittle A, Pope R. The utility of physiotherapy assessments delivered by telehealth: A systematic review. J Glob Health . 2021;11:04072. doi:10.7189/jogh.11.04072
51. Klinenberg E. Heat wave: A social autopsy of disaster in Chicago . 2nd ed. University of Chicago Press; 2015.
52. Joint Commission. Sustainable Healthcare Certification. https://www.jointcommission.org/what-we-offer/certification/ certifications-by-setting/hospital-certifications/sustainablehealthcare-certification/
53. Practice Greenhealth. Why sustainability: Health care's opportunity. https://practicegreenhealth.org/why-sustainability
54. NHS England. Walking aid re-use. https://www.england.nhs.uk/ahp/ greener-ahp-hub/specific-areas-for-consideration/walking -aid-reuse/
55. American Physical Therapy Association. Support of environmentally responsible practice by the American Physical Therapy Association. Updated August 13, 2020. https://www.apta.org/apta-and-you/ leadership-and-governance/policies/support-of-environmentallyresponsible-practice
56. Smyer MA. Greening Gray: Climate Action for an Aging World. Public Policy & Aging Report . 2017;27(1):4-7. doi:10.1093/ppar/prw028

Cindy Lane Moore, PT, DPT, PhD, MPH, is a Board-Certified Clinical Specialist in Geriatric Physical Therapy and Staff Development Coordinator for Rehabilitation at Redeemer Health Home Care and Hospice. Cindy co-founded the Environmental Physical Therapy Catalyst Group within APTA’s Academy of Leadership and Innovation to promote environmental-informed physical therapy practice across settings and specialties. She served as lead author for several chapters in the book Climate Change and Disability: A Collaborative Approach to a Sustainable Future (in press). She welcomes comments and questions and can be reached atcinmoore77@verizon.net.

The Link Between Cognitive and Mental Health and Sleep: Part 3 of 3
by Alex Alexander, PT, DPT and Cathy Stucker, PT, DSc, CMPT
This is the continuation and finale to the Cognitive and Mental Health 3-part series on the importance of recognizing the role that sleep has on cognition. This was introduced in the November 2024 and January 2025 issues of GeriNotes (Unlocking Sleep: The Link Between Cognitive and Mental Health and Sleep).
The following 4 pages are designed to be stand alone printable Hand-outs for use in your clinic and may be reproduced with proper credit to: ©APTAGeriatrics, Cognitive and Mental Health SIG, May 2025. All rights reserved.
The sleep decision tree is a tool to be utilized to help determine the next course of action based on patient symptoms. Created by Alex Alexander, PT, DPT and Cathy Stucker, PT, DSc, CMPT
Do you have trouble sleeping?
Have you been told you snore loudly, gasp for air or stop breathing while sleeping?
Complete STOPBANG Questionaire
5-8
Responses?
Do you have trouble falling asleep or wake up often?
Complete Insomnia Severity Index
Score > 15?
Do you have the urge to move yor legs while resting?
Provide Sleep Education Handout
Complete the Restless Leg Syndrome Rating Scale
Score 31-40= Very Severe Score of 21-30=Severe
Refer to Sleep Specialist
Many things can make it hard to sleep, such as: Stress and Worry: Feeling stressed can make it hard to relax and fall asleep.
Bad Sleep Habits: Staying up late or not having a regular bedtime can confuse your body.
Health Problems: Pain, sleep apnea, and restless legs can keep you awake.
Caffeine and Medications: Drinks like coffee or some medicines can make it harder to sleep. Your Environment: A noisy, bright, or uncomfortable bedroom can stop you from sleeping well.
Sleep is very important for your body and mind. It helps you stay healthy by letting your body rest, repair itself, and build energy for the next day. Good sleep also helps you focus, learn new things, and remember important information. Without enough sleep, you are at a higher risk of problems like heart disease, diabetes, weight gain, and feeling sad or anxious.
Keep it Dark: Use curtains to block light and dim the lights at night.
Keep it Cool: The best temperature for sleeping is around 60-67°F.
Block Out Noise: Use earplugs or a sound machine to help you sleep.
Choose Comfy Bedding: Get a good mattress, soft sheets, and pillows.
Keep It Clean: A tidy room without distractions helps you relax.
Keep it Quiet: Avoid falling asleep with the TV on.
1. Stick to a Schedule: Go to bed and wake up at the same time every day.
2. Relax Before Bed: Read, listen to calming music, or take a warm bath. Try Mindfulness practices such as those available for free on Palouse Mindfulness.
3. Avoid Caffeine and Alcohol: Don’t drink alcohol or caffeinated coffee, soda, or tea close to bedtime.
4. Stay Active: Exercise during the day, but not within 2 hours of bedtime.
5. Don’t Eat Big Meals Late: Eat a light snack if you are hungry before bed.
6. Use Your Bed for Sleep: Don’t do homework, watch TV, or play on your phone in bed.
There are several apps* to help with relaxation and sleep. The following list is not exhaustive, but may be a good place to start:
• Sleep Cycle
• Calm
• Headspace
• BetterSleep
• Meditation Moments
• Breathe: Sleep & Meditation
*Some apps do charge fees.
WHITE NOISE:
A steady, higherpitched sound like a fan or static. It blocks out sudden noises and helps light sleepers.
BROWN NOISE:
A deeper, rumbling sound like thunder or ocean waves. It can feel more calming and relaxing for sleep.
You can ask Alexa or Google to play white noise or brown noise while you sleep or use a phone app!

Talk to your doctor if you:
• Can’t sleep well for a long time
• Snore loudly or stop breathing while sleeping
• Feel extremely tired during the day even after sleeping at night
• Notice mood changes or trouble paying attention
• Have symptoms like restless legs or suddenly falling asleep during the day
References
1. National Sleep Foundation. "Healthy Sleep Tips." https://www.thensf.org/sleep-tips/
2. Mayo Clinic. "Sleep Disorders." https://www.mayoclinic.org/diseases-conditions/sleep-disorders/symptoms-causes/syc-20354018
3. Harvard Health Publishing. "Blue Light Has a Dark Side." https://www.health.harvard.edu/
4. Palouse Mindfulness: Mindfulness-Based Stress Reduction: https://palousemindfulness.com/index.html
Additional Resources on Sleep Hygiene:
1. https://www.choosept.com/health-tips/13-tips-improve-sleep
2. https://academic.oup.com/ptj/article/97/8/826/3831304
3. https://www.apta.org/apta-and-you/leadership-and-governance/policies/role-pt-apta-sleep-health
by Ellen R. Strunk, PT, MS
Physical therapists (PTs) and physical therapist assistants (PTAs) provide invaluable clinical care to older adults across a wide range of settings. As the body of knowledge surrounding the care of older adults continues to expand, our techniques and treatment approaches evolve and become more refined. However, many therapists may overlook a critical aspect of their role: understanding how these services are paid for. While knowledge in specialized clinical areas is essential, an inadequate understanding of payment policies—such as policy objectives, coverage rules, and billing requirements —can lead to underpayment, overpayment, and even situations that may be perceived as fraudulent or abusive. Furthermore, when therapists fail to grasp how payment policies are developed and enforced, they miss an opportunity to advocate for their patients and the profession itself. A lack of awareness about these payment systems can result in patients not receiving the services they need, despite their eligibility. This highlights the importance of advocacy in shaping policies that govern the coverage of and payment for physical therapy services.
Health policy is the framework that guides society’s decisions regarding health goals, priorities, and the allocation of resources to achieve these objectives. At its core, health policy strives to contain costs, improve access to care, and ensure that services are equitable. Advocacy is the process that amplifies the voices of individuals and groups, allowing them to influence policy decisions and hold governments accountable for providing adequate healthcare, especially for marginalized populations. Health policies, especially those that govern the practice of physical therapy, are shaped by collective input. When stakeholders—patients, practitioners, and organizations—engage in advocacy efforts, they help steer policy decisions in a direction that improves healthcare delivery. Physical therapists, particularly those serving older adults, must be involved in these advocacy efforts to ensure policies reflect the needs of both the profession and the patients they serve.
Health policy is a delicate balancing act. Policymakers must make decisions that not only improve access to healthcare and enhance quality but also manage costs. Understanding how health policy works—and how payment policies, in particular, are developed—can
provide physical therapists with a clearer picture of the limitations and opportunities within the healthcare system. With this knowledge, PTs can advocate more effectively for changes that will allow them to practice to the full extent of their education, training, and expertise. Advocacy is a critical element of this process. It’s the mechanism through which physical therapists can drive the changes that ultimately benefit patients and the profession as a whole. Legal, legislative, and regulatory advocacy involves educating stakeholders, influencing policymakers, and pushing for the enactment of policies that align with the goals of improving patient health and advancing the physical therapy profession. Whether it’s pushing for more equitable reimbursement rates, better access to care for older adults, or policies that support expanded services, advocacy enables PTs to ensure that their patients’ needs are met.
Regardless of their practice setting, political stance, or expertise in policy, physical therapists have a professional obligation to engage in health policy and advocacy efforts. Complying with existing laws, regulations, and policies is part of being a healthcare professional. However, active participation in the advocacy process is equally important. By doing so, PTs ensure that the policies governing their practice are effective, fair, and aligned with the evolving needs of the populations they serve. It is easy to get started. The APTA’s Advocacy Network can provide you with all the tools you need to learn and become more engaged. With just one click, you can sign up to begin receiving alerts and important legislative updates.

Ellen
R. Strunk is President and Owner of Rehab Resources & Consulting,
Inc., a company providing consulting services and training to providers in postacute care settings with a focus on helping customers understand the CMS prospective payment systems. She also lectures nationally on the topics of pharmacology for rehabilitation professionals, exercise and wellness for older adults, and coding/ billing/ documentation to meet medical necessity guidelines and payer regulations.
by Danielle Simon, PT, DPT and Zachary Ammons, PT, DPT
Editor’s Note: This clinical case commentary was part of content for the June 2025 Journal Club. These case studies are intended to demystify the more formal statistics and format of a peer-reviewed article and translate key concepts into clinically usable information. Join us for Journal Club on the third Tuesdays of January, March, June, July, August, October, and November at 8 pm ET to discuss current concepts with a wide range of peers.
Case study presentation based on the research article from Journal of Geriatric Physical Therapy: Feasibility of a 4-Week Manual Therapy and Exercise Intervention on Posture and Function in Community- Dwelling Older Adults. Hughes, Lynne C. PT, PhD; Galloway, Rebecca V. PT, PhD; Fisher,Steve R. PT, PhD. J Geriatr Phys Ther. 2022;46(3):151-160. doi:10.1519/JPT.00000000000003601
Postural impairments and kyphosis are common in patients encountered at the Cleveland VA Hospital. This article and case study was an opportunity for two physical therapy residents, one in geriatrics and the other in orthopedics, to combine specialties and collaborate within specializations to assess manual therapy interventions and exercises within this population. It is reported that around 20 to 40% of older adults have hyper-kyphosis, which has a direct correlation with decreased quality of life and impaired physical performance.² Kyphosis increases the risk of fractures and mortality in older adults. Mortality is also associated with the severity of kyphosis, causing decreased vital capacity which can lead to pulmonary complications. Kyphosis can also be related to an increased incidence in vertebral fractures in older women and those at risk with decreased bone density.³ Commonly, clinicians tend to stray away from utilizing manual therapy techniques on older adults. When combined with an exercise program, utilizing manual therapy to decrease kyphosis may be beneficial for older adults. Exercises that target postural control are essential to include in an exercise program to improve independence with activities of daily living and prevent falls This model allows the clinician to look at the entire older person and address multiple impairments.
Two different patients met the inclusion criteria of the Hughes, et al. journal study. Zachary Ammons, PT, DPT, orthopedic physical therapy resident at the Cleveland VA, completed the manual therapy interventions as detailed within the article. Danielle Simon, PT, DPT, geriatric physical therapy resident at the Cleveland VA analyzed the data and compiled the research/clinical implications. Each subject was treated separately three times per week over four weeks (12 total sessions) with a combination of manual therapy and therapeutic exercise during 30–60-minute sessions. Their outcome measures and measurements were completed at baseline, at 2 weeks, and at 4 weeks for comparison. Both patients were screened and selected utilizing the article’s inclusion and exclusion criteria. Inclusion criteria
include men and women greater than 50 years of age, visible and measurable increase in thoracic kyphosis/ forward head, and ability to walk across a small room without an assistive device. Exclusion criteria are collagen disease, musculoskeletal disease with autoimmune component, BMI greater than 35, and inability to tolerate physical touch associated with treatment.
Joint mobilizations were completed at grade three during week 1, grades three and four during week 2, and at grade four during weeks 3 and 4. Joint mobilizations included supine first rib mobilization grade three and amplitude 4 into depression. The cervical spine was positioned in slight side flexion and rotation toward the side being mobilized to put the upper trapezius on slack. Prone thoracic and cervical spine joint mobilization were completed at grade three and amplitude 4, as well as PA mobilizations with 8 oscillations then released for breathing. This was repeated three to five times until improved spinal mobility was noted by the treating therapist. Each subject completed standing open books, standing scapular rows, scapular pull downs, standing serratus anterior punches, drawing the bow, quadruped reach across, and bridges with resistance bands. During week 1 both subjects completed the above exercise regimen for two sets of ten repetitions with a green resistance band. During week 2, they completed three sets of ten repetitions with a green resistance band. During week 3, they completed each exercise for two sets of ten repetitions with a blue resistance band, and week 4 they completed three sets of ten repetitions with a blue resistance band. The stretches included in the exercise program were: suboccipital release, supine upper trapezius stretch, supine pectoralis stretch, scalene stretch, child’s pose, standing hip flexor stretch, and standing hamstring stretch. Each stretch was held for two minutes throughout weeks 1 through 4.
Subject 1: Ms. C is a 68-year-old female who lives in a 2-story home with her husband. She is completely
independent at baseline, physically active (attends a local gym 2-3 times per week), walks her dogs frequently, and golfs recreationally. Pertinent medical history includes anxiety, GERD, hyperlipidemia, and osteoarthritis. Reason for referral is neck pain with right shoulder pain. Her primary goal is to decrease her pain levels with movement. Subject 2: Mr. T is a 74-year-old male who lives alone in an apartment with elevator access. He is independent with activities of daily living, but his children live nearby and assist with his transportation to/from appointments, laundry, and grocery shopping. He is not physically active and spends most of his time in his apartment if he is not at an appointment. Pertinent medical history includes hyperlipidemia, low back pain, hypertension, history of prostate cancer, and pre-diabetes. Reason for referral is shoulder pain with radiating pain. His main goal is to decrease the pain and improve posture, as he would like to start playing guitar again.
See Tables 1 and 2 below.
Height: Height was measured with a tape measure in centimeters, Ms. C started at 155 cm and Mr. T at 185.9cm. Following four weeks of interventions, Mr. T increased 0.20 cm and was measured at 186.1cm. Ms. C’s height increased by 0.75 cm at 155.75 cm following 4 weeks.
Acromion to Table: Subject was positioned in supine, then measured the linear distance between posterolateral acromion and mat in centimeters with a tape measure. Ms. C’s baseline measurement was 7.5 cm, and after four weeks improved to 7.1cm. Mr. T’s baseline measurement was 12.2 cm, after four weeks improved to 12.1 cm.
2MWT: Instructed the subject to cover as much ground as possible in two minutes. Walking was completed inside in the same hallway and measured with a measuring wheel in feet. The MDC is 139 ft for a
range of adults.¹ Ms. C started at 577 ft and after four weeks improved to 612 ft. Mr. T started at 561 ft and improved to 606 ft.
PSFS: This measure is a self-reported questionnaire to rank the perceived difficulty in activity limitations. It consists of 3 activities that are affected by posture, and subjects are instructed to rate its difficulty from 0 to 10. The MDC is 2.8 for community dwelling older adults.¹ Mr. T started at 2, and after four weeks improved to 6. Ms. C started at 3.67 and improved to 6. The MDC was met for Mr. T by improving greater than +2.8 at +3.
Functional Reach: Instructed the subject to reach as far as they can without taking a step. The yardstick was mounted on the wall at level of acromion and measured the distance at the third metacarpal in standing upright position after reaching forward. There is one practice trial, followed by two more trials recorded for an average distance. The normative value is 26.2cm.¹ Mr. T’s baseline was 19.05cm, and after four weeks recorded at 22.8 cm. Ms. C’s baseline was 25.4 cm, and after four weeks was at 27.31 cm.
5xSTS: The five-time sit to stand is an assessment of lower extremity function/functional strength by rising and sitting from a chair five times as quickly as possible with arms folded across the chest. The ability to stand up once without use of arms assessed before timing five repetitions. The MDC is more than 2.5 seconds in older adult females. The normative values are 11.4 seconds in people aged 60-69, and 14.8 seconds for adults aged 80-89.¹ Mr. T’s baseline was measured at 23.7 seconds, improving to 20.4 seconds after four weeks. Ms. C’s baseline was 16.4 seconds which improved to 14.2 seconds after four weeks of treatment.
TUG: Instructed the subject to move at normal pace from sitting to standing, walk 3m, turn around, walk back and sit down. First a practice trial is performed, then three more trials are recorded for average time in seconds.
There is correlation between greater thoracic kyphosis angle and longer time to complete the Timed Up and Go.¹
The MDC for community dwelling older adults is 2.08 seconds.¹ Ms. C completed the TUG in 8.75 seconds at baseline and improved to 8.0 seconds after four weeks. Mr. T completed the TUG in 14.1 seconds at baseline and improved to 9.96 seconds after four weeks.
Block Test: To complete the block test, position the subject in supine. Wood blocks of various heights are placed under the head to align the face parallel to the mat with the cervical spine in neutral. The total height of blocks is then recorded. Greater block height indicates higher thoracic kyphosis.¹ At baseline, Ms. C’s block height was 10.4 cm, and following four weeks was 9.9cm. Mr. T’s block height was 15.5cm at baseline and 15.2cm following four weeks of interventions.
Discussion
In each category for both subjects, there were noticeable improvements following 4 weeks of manual therapy and exercises to improve thoracic kyphosis. If this case study was conducted again, it would be beneficial to include more subjects and include subjects of different age ranges (40-50, 50-60) to account for any effects in populations that are not considered geriatric. It could also be beneficial to include more manual therapy techniques and compare which techniques were the most effective by selecting subjects for different manual therapy techniques.
Throughout the process of completing this case report, the interprofessional collaboration between a geriatric physical therapy resident and an orthopedic physical therapy resident are highlighted. We learned the importance of posture and its effects on balance, pain, and quality of life in older adults, and plan to implement more manual therapy and exercises to decrease kyphosis in our practice. There were difficulties with selecting test subjects, having subjects be willing to participate 3 days per week for 4 weeks, and screening out subjects that met the inclusion and exclusion criteria. Both the geriatric and orthopedic residents collaborated to screen test subjects, collect, and interpret the data. The orthopedic resident completed all the manual therapy interventions to decrease risk for discrepancies between manual therapy techniques. The examination techniques including the Block Test and Acromion to Table measures can be utilized in an outpatient setting or geriatric clinic to observe kyphosis and postural impairments to use as objective data. Geriatric clinics may use more of the outcome measures discussed in this article as an opportunity to improve quality of life and posture in older people. Utilizing these outcome measures and interventions could be beneficial in demonstrating improvements in balance, functional strength, decreased fall risk, gait speed, posture, quality of life, and pain levels. Based on the results of the interventions, manual therapy,
postural strengthening, and stretching exercises may have an impact on decreasing the effects of kyphosis, improve posture, and improve functional outcomes if completed routinely.
1. Hughes LC, Galloway RV, Fisher SR. Feasibility of a 4-Week Manual Therapy and Exercise Intervention on Posture and Function in Community-Dwelling Older Adults: A Pilot Study. J Geriatr Phys Ther. 2022;46(3):151-160. doi:10.1519 JPT.0000000000000360
2. Katzman WB, Wanek L, Shepherd JA, Sellmeyer DE. Age-related hyperkyphosis: its causes, consequences, and management. J Orthop Sports Phys Ther. 2010;40(6):352-360. doi:10.2519/ jospt.2010.3099
3. Ensrud KE, Black DM, Harris F, Ettinger B, Cummings SR. Correlates of kyphosis in older women. The Fracture Intervention Trial Research Group. J Am Geriatr Soc. 1997;45(6):682-687. doi:10.1111/j.1532-5415.1997.tb01470.x
4. Alfieri FM, Riberto M, Abril-Carreres A, et al. Effectiveness of an exercise program on postural control in frail older adults. Clin Interv Aging. 2012;7:593-598. doi:10.2147/CIA.S36027


Danielle Simon, PT, DPT is a Geriatric Physical Therapy Resident at the Cleveland VA Medical Center. She graduated from Ohio University with a Bachelor’s in Exercise Physiology, and Walsh University with a Doctorate in Physical Therapy. Her primary areas of interest in physical therapy are neurologic conditions, medically complex patient presentations, and pelvic health within the geriatric population.
Zach Ammons, PT, DPT is currently an Orthopedic Resident PT at Cleveland VA.. When he is not s pending time in the PT realm, he enjoys family walks,hikes and traveling.prior to earning his DPT, he worked as PTA Primarily in SNFs where he was able to enjoy this opportunity blending geriatric care with manual skills.

by Holly J. Roberts, PT, PhD, Rovin Ian Antonio, SPT, and Teri Lake-Coblio, SPT
Up to one-fourth of older adults fall each year.1 Falls are the most common type of accidents in people 65 years or older, and injuries caused by these episodes may increase mortality risk.1 Risk factors for falls include fear of falling, a previous history of falls, decreased functional mobility, poor balance, muscle weakness, and slow gait speed as well as chronic conditions such as diabetes mellitus, osteoarthritis, depression, and pain.2–4 Fallrelated incidents have widespread effects on individuals and society. The cost of non-fatal falls for Medicare, Medicaid, and private insurers was $28.9 billion, $8.7 billion, and $12.0 billion, respectively, in 2015.5 Accurately identifying fall risk is vital to mitigate injuries and mortality, and reducing the substantial financial costs associated with falls.
Guidelines for identifying older adults at risk for falls often include a multi-pronged approach including fall history, concern about falling, and physical performance using a screening tool.6 However, many commonly used screening tools such as the Timed Up and Go (TUG), Berg Balance Scale (BBS), Short Physical Performance Battery, and Dynamic Gait Index have ceiling effects in community-dwelling older adults.7–10 Gait speed has been shown to be slower in older adults who fall compared to older adults who do not fall.11 Most fall risk assessment guidelines use 0.8 meters/second (m/s) or 1.0 m/s as a cut-off for identifying individuals who may be at risk for falls.6
Backward walking, which is necessary for common tasks such as opening a door, backing up to a chair, or avoiding an obstacle, has been identified as a sensitive tool for identifying age-related changes in mobility and balance.12,13 Across the adult lifespan, individuals demonstrate shorter stride length, shorter swing phase, increased double-leg stance time, increased base of support, and decreased velocity when backward walking as compared to forward walking.13–15 However, the magnitude of the changes and variability between backward and forward walking is more pronounced in older adults.13,14 The increased variability in the spatiotemporal parameters associated with backward walking may be due to an increased demand in dynamic balance and gait. Due to the general lack of visual cues during backward walking, there is a higher reliance on neuromuscular control, proprioception, and protective reflexes.13,14 Researchers have identified a difference in self-selected and maximal backward walking speed between individuals who had fallen and those without a history of falls.13,16
Assessment of backward walking may be a useful tool to identify older adults with deficits in balance and gait.17
The 3-Meter Backwards Walk Test (3MBWT) is a novel clinical assessment test that objectively measures backward walking speed.12 To complete the test, individuals are instructed to walk backwards a distance
of 3 meters as quickly, but as safely as possible. They are allowed to look behind them if needed, but are not permitted to run. The purpose of this review is to explore the current research on the 3MBWT in older adults and to identify areas for future research.
The 3MBWT has been validated for use with community-dwelling older adults,18,19 and older adults with subacute stroke,20,21 chronic stroke,21 Parkinson disease,22,23 dementia,24 and status-post total hip arthroscopy.25 (See Table.) DeMark, et al. found strong correlations between the 3MBWT and backward walk speed measured on a GAITRite © 21 Performance on the 3MBWT is moderately to strongly correlated with other performance-based outcome measures such as the TUG,18,19,22–24 BBS,22,24,26 Four Square Step Test,18,22 10 Meter Walk Test,22,24 and Activities-specific Balance Confidence Scale.22
Several studies have examined the reliability of the 3MBWT when administered to older adults. (See Table.) The 3MBWT consistently shows excellent test-retest reliability (ICC=0.96 – 0.97),19,20,22,24,25 intra-rater reliability (ICC=0.94 – 0.97),20,21 and interrater reliability (ICC=0.91 –0.95).21,24
Several retrospective cohort studies examined the ability of scores on the 3MBWT to discriminate among older adults who have fallen and those who do not report a past fall.18,22,23 Carter, et al. determined a cut-off score of 4.5 seconds to discriminate between community-dwelling older adults who reported a previous fall and those who did not.18 Cut-off scores to discriminate between people who have fallen and individuals who do not self-report a previous fall range from 4.2 seconds to 10.31 seconds in individuals with Parkinson disease 18,22 and 4.5 seconds in residents of a retirement community.18
Six studies have determined the minimal detectable change (MDC) of the 3MBWT in older adults.19,21,22,24–26 (See Table 3.) The MDC for community dwelling older adults is 1.52 seconds.19
In individuals with stroke, the MDC 95 ranges from 0.07 to 0.11 m/s.21 Kocamen, et al. determined that the smallest amount of change that can occur before a measurement error is considered in people with subacute stroke is 1.57 seconds,26 though the participants in their study were slightly younger than those who participated in the study by DeMark. The highest MDC occurs for people who are status post total hip arthroscopy.25
Cognition has been identified as an essential factor
in the maintenance of postural stability during forward gait. Healthy older adults demonstrate a reduction in gait velocity and an increased stride time variability when a secondary task is added during forward gait testing.27 Cognitive and executive function impairment in older adults have been consistently associated with increased fall risk.28 The inclusion of a secondary task in forward gait has been an accepted way to assess the interaction between cognition and mobility.29–32 The cost associated with adding a secondary task to gait may also apply to backward walking. Leon-Llamas et al. examined performance on the 3MBWT under single and dual-task conditions in middle age women with fibromyalgia.33 Times on the 3MBWT with a dual cognitive task were correlated with performance on the TUG (ICC=0.68-0.88).33 To date, adding a dual task condition to the 3MBWT has not been examined in older adults.
The 3MBWT appears to be a promising test for evaluating dynamic gait in older adults. However, several areas of research need to be explored. Although times on the 3MBWT can discriminate between people who have fallen and those who have not fallen, to date, no studies have demonstrated the predictive ability of the 3MBWT to identify older adults who may fall. Prospective studies are needed to determine whether the 3MBWT can identif individuals with an increased risk for falls and to establish cutoff scores to determine the level of risk. Concurrent validity of the 3MBWT with other tests of gait speed and dynamic gait also needs to be established. Finally, inclusion of a secondary task may improve the accuracy of a fall risk assessment. Studies are needed to determine whether adding a secondary cognitive task to the 3MBWT would improve the ability to identify individuals who may fall.
The 3MBWT may be a valuable tool for assessing dynamic gait and identifying fall risk in older adults. Its proven validity and reliability across various populations highlight its potential to enhance clinical fall risk assessments. However, further research is necessary to explore its predictive capabilities, establish clear cutoff scores, and investigate the impact of dual-task conditions on test performance. Addressing these gaps will provide clinicians with a more comprehensive understanding of the 3MBWT’s utility, ultimately improving fall prevention strategies for older adults.
References
1. Kakara R. Nonfatal and Fatal Falls Among Adults Aged ≥65 Years — United States, 2020–2021. MMWR Morb Mortal Wkly Rep . 2023;72. doi:10.15585/mmwr.mm7235a1
2. Xu Q, Ou X, Li J. The risk of falls among the aging population: A systematic review and meta-analysis. Front Public Health . 2022;10:902599. doi:10.3389/fpubh.2022.902599
3. Kyrdalen IL, Thingstad P, Sandvik L, Ormstad H. Associations between gait speed and well-known fall risk factors among community-dwelling older adults. Physiother Res Int J Res Clin Phys Ther . 2019;24(1):e1743. doi:10.1002/pri.1743
Carter, et al [18]
Carter, et al [23]
59 residents of retirement community w/o h/o neuro deficits (mean age 71.5 yrs)
175 ambulatory People w/PD; age range 5th thru 8th decade
4.5 sec to identify retrospective h/o falls TUG 5TSTS 4 square Step test
4.2 sec to identify retrospective h/o falls; AUC= 0.699, sens71.4% spec 64% TUG
TUGcog 5TSTS 10MWT
Chan, et al [24]
50 adults with Dementia (83.3+/-7. 8 years)
Ozden, et al [25
DeMark, et al [21]
10 MWT BBS TUG
29 people at least 6 mos Post THA (75.6 +/- 10.0 yrs) NR Harrison Hip Score
34 n w/ subacute CVA (60.4 +/-12.4 yrs); 29 n chronic CVA(57.2 +/- 12.6 yrs) N)
Kocer, et al [22]
Koc -aman, et al [26]
Kocaman, et al [26]
N= 36 w/PD (63.19 +/- 9.04 yrs) & 33 heathy older adults (65.27 =/- 6.89 yrs) 10.31 sec, AUC=0.886 w/ sensitivity 82.6%, specificity 84.6%
Backward walk speed using GAITRite
Ex test /retest (ICC=0.96) Ex IRR (ICC=0.917 /retest.96) Ex IRR (ICC=0.917 (ICC=0.96) Ex IRR (ICC=0.917
Ex test/ Retest reliability (ICC = 0.983))
Ex Intra RR for subacute CVA (ICC=0.96); chronic CVA(ICC=0.9 4). EX InterRR subacute ICC=0.99; chronic CVA ICC =0.99)
10MWT TUG
BBS
4SSTABC MDSS -UPDRS Hoehn & Yahr Scale
41n w/sub-acute CVA (35-78 yrs, median 59) NR BBS TUG
Ozden, et al [19] N= 65 community dwelling adults (68.9+/-3.7 years) NR TUG 5TSTS
Ex testRetest Reliability (ICC= 0.965)
Mod to high Correlation w/TUG (r=0.823); 5TSTS (r=0.608) 4SST (r=0.651)
If fall in past yr, slower 3MBWT than no falls(5.5s v4.0 sec, P<0.001) IF higher disease severity slower MBWT F3.159=21.255
Mod corr w/BBS (p=0.60); Strong corr 10 MWT(p=0..8 4) & TUG(p=0.82
Mod corr w/Harrison Hip Score (r=0.49)
Concurrent validity w/ GAITRite for subacute CVA (ICC =0.96), chronic CVA (ICC ==0.97)
High Corr w/TUG (r=0.858), BBS (t=0.816), 4SST (r=0.774) Hoehn/Yahr (p=0.714); Mod correlate w/ 10MWT (r=0.674), ABC (r=0.592)
Ex test-retest rel (ICC=0.97): INTRA rater reliability (ICC=0.97)
Ex test/r Retest Reliability (ICC=0.94)
MDC[95] = 0.1m/s
No diff in 3MBWT Between people who fell in past yr/nonfallers (p=0.36)
MDC 95
MDC 95=0.07m/s (subacute CVA); MDC95 =0.11 m/s (chronic CVA)
MDS-UPDRS (r=0.628) MDC= 2.13 sec
Mod to high Corr w/BBS (r=0.691) & TUG (r=0.849)
People w/ h/0 falls slower 3MBWT than those who did not fall (p= 0.001)
Strong corr w/TUG (r=0.649); poor Correlation w/ 5TSTS (r=0.238) MDC = 1.52 sec
Abbreviations: 5TSTS, Five Times Sit to Stand; 10MWT, 10 Meter Walk Test; ABC, Activities-specific Balance Confidence Scale; BBS, Berg Balance Scale; MDC, Minimal Detectable Change; h/o: history of; ICC, Intraclass Correlation Coefficient; MDSS UPDRS Movement Disorders Society Sponsored Unified Parkinson’s Disease Rating Scale; m/s, meters per second; NR, Not reported; PD, Parkinson disease; TUG, Timed Up and Go; TUGcog, TUG Cognitive; Corr, correlation; w/, with
4. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas . 2013;75(1):51-61. doi:10.1016/j.maturitas.2013.02.009
5. Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc . 2018;66(4):693-698. doi:10.1111/jgs.15304
6. Colón-Emeric CS, McDermott CL, Lee DS, Berry SD. Risk Assessment and Prevention of Falls in Older Community-Dwelling Adults: A Review. JAMA . Published online March 27, 2024. doi:10.1001/jama.2024.1416
7. Schoene D, Wu SMS, Mikolaizak AS, et al. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc . 2013;61(2):202-208. doi:10.1111/jgs.12106
8. Pettersson B, Nordin E, Ramnemark A, Lundin-Olsson L. Neither Timed Up and Go test nor Short Physical Performance Battery predict future falls among independent adults aged ≥75 years living in the community. J Frailty Sarcopenia Falls . 2020;5(2):24-30. doi:10.22540/JFSF-05-024
9. Chen H, Smith SS. Item Distribution in the Berg Balance Scale: A Problem for Use With Community-Living Older Adults. J Geriatr Phys Ther 2001 . 2019;42(4):275-280. doi:10.1519/ JPT.0000000000000208
10. Pardasaney PK, Latham NK, Jette AM, et al. Sensitivity to change and responsiveness of four balance measures for communitydwelling older adults. Phys Ther . 2012;92(3):388-397. doi:10.2522/ ptj.20100398
11. Adam CE, Fitzpatrick AL, Leary CS, et al. The Association between Gait Speed and Falls in Community Dwelling Older Adults with and without Mild Cognitive Impairment. Int J Environ Res Public Health . 2021;18(7):3712. doi:10.3390/ijerph18073712
12. Carter V, Jain T, James J, Cornwall M, Aldrich A, de Heer HD. The 3-m Backwards Walk and Retrospective Falls: Diagnostic Accuracy of a Novel Clinical Measure. J Geriatr Phys Ther 2001 . Published online November 1, 2017. doi:10.1519/JPT.0000000000000149
13. Fritz NE, Worstell AM, Kloos AD, Siles AB, White SE, Kegelmeyer DA. Backward walking measures are sensitive to age-related changes in mobility and balance. Gait Posture . 2013;37(4):593-597. doi:10.1016/j.gaitpost.2012.09.022
14. Laufer Y. Age- and gender-related changes in the temporal-spatial characteristics of forwards and backwards gaits. Physiother Res Int 2003;8(3):131-142. doi:10.1002/pri.281
15. Raffegeau TE, Kellaher GK, Terza MJ, Roper JA, Altmann LJ, Hass CJ. Older women take shorter steps during backwards walking and obstacle crossing. Exp Gerontol . 2019;122:60-66. doi:10.1016/j. exger.2019.04.011
16. Yada TT, Taulbee L, Balasubramanian C, Freund J, Vallabhajosula S. Can backward walking speed reserve discriminate older adults at high fall risk? Physiother Can . 73(4):353-357. doi:10.3138/ptc2019-0086
17. Taulbee L, Yada T, Graham L, et al. Use of Backward Walking Speed to Screen Dynamic Balance and Mobility Deficits in Older Adults Living Independently in the Community. J Geriatr Phys Ther . 2021;44(4):189. doi:10.1519/JPT.0000000000000290
18. Carter V, Jain T, James J, Cornwall M, Aldrich A, de Heer HD. The 3-m Backwards Walk and Retrospective Falls: Diagnostic Accuracy of a Novel Clinical Measure. J Geriatr Phys Ther . 2019;42(4):249-255. doi:10.1519/JPT.0000000000000149
19. Özden F, Özkeskin M, Bakırhan S, Şahin S. The test-retest reliability and concurrent validity of the 3-m backward walk test and 50-ft walk test in community-dwelling older adults. Ir J Med Sci . 2022;191(2):921-928. doi:10.1007/s11845-021-02596-1
20. Abit Kocaman A, Aydoğan Arslan S, Uğurlu K, Katırcı Kırmacı Zİ, Keskin ED. Validity and Reliability of The 3-Meter Backward Walk Test in Individuals with Stroke. J Stroke Cerebrovasc Dis . 2021;30(1):105462. doi:10.1016/j.jstrokecerebrovasdis.2020.105462
21. DeMark LA, Fox EJ, Manes MR, Conroy C, Rose DK. The 3-Meter Backward Walk Test (3MBWT): Reliability and validity in individuals with subacute and chronic stroke. Physiother Theory Pract . 2023;39(12):2698-2705. doi:10.1080/09593985.2022.2085638
22. Kocer B, Soke F, Ataoglu NEE, et al. The reliability and validity of the 3-m backward walk test in people with Parkinson’s disease. Ir J Med Sci . 2023;192(6). doi:10.1007/s11845-023-03384-9
23. Carter VA, Farley BG, Wing K, de Heer H “Dirk”, Jain TK. Diagnostic accuracy of the 3-Meter Backward Walk Test in persons with
Parkinson disease. Top Geriatr Rehabil . 2020;36(3):140. doi:10.1097/TGR.0000000000000272
24. Chan WLS, Cheung YT, Lee YW, Teo AM, Wo HK, Wong Y. Reliability, Validity, and Minimal Detectable Change of the Backward Walk Test in Older Adults With Dementia. J Geriatr Phys Ther . 2022;45(3):145. doi:10.1519/JPT.0000000000000306
25. Özden F, Coşkun G, Bakırhan S. The test-retest reliability, concurrent validity and minimal detectable change of the 3-m backward walking test in patients with total hip arthroplasty. J Arthrosc Jt Surg . 2021;8(3):288-292. doi:10.1016/j.jajs.2020.11.002
26. Abit Kocaman A, Aydoğan Arslan S, Uğurlu K, Katırcı Kırmacı Zİ, Keskin ED. Validity and Reliability of The 3-Meter Backward Walk Test in Individuals with Stroke. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc . 2021;30(1):105462. doi:10.1016/j.jstrokecerebrovasdis.2020.105462
27. Dubost V, Kressig RW, Gonthier R, et al. Relationships between dual-task related changes in stride velocity and stride time variability in healthy older adults. Hum Mov Sci . 2006;25(3):372-382. doi:10.1016/j.humov.2006.03.004
28. Muir-Hunter SW, Wittwer JE. Dual-task testing to predict falls in community-dwelling older adults: a systematic review. Physiotherapy . 2016;102(1):29-40. doi:10.1016/j.physio.2015.04.011
29. Beck Jepsen D, Robinson K, Ogliari G, et al. Predicting falls in older adults: an umbrella review of instruments assessing gait, balance, and functional mobility. BMC Geriatr . 2022;22(1):615. doi:10.1186/ s12877-022-03271-5
30. Omana H, Madou E, Montero-Odasso M, Payne MW, Viana R, Hunter SW. The effect of dual-task testing on the balance and gait of people with lower limb amputations: A systematic review. PM R . 2023;15(1):94-128. doi:10.1002/pmrj.12702
31. Chen A, Kirkland MC, Wadden KP, Wallack EM, Ploughman M. Reliability of gait and dual-task measures in multiple sclerosis. Gait Posture . 2020;78:19-25. doi:10.1016/j.gaitpost.2020.03.004
32. Raffegeau TE, Krehbiel LM, Kang N, et al. A meta-analysis: Parkinson’s disease and dual-task walking. Parkinsonism Relat Disord . 2019;62:28-35. doi:10.1016/j.parkreldis.2018.12.012
33. Leon-Llamas JL, Villafaina S, Murillo-Garcia A, Domínguez-Muñoz FJ, Gusi N. Test-retest reliability and concurrent validity of the 3 m Backward Walk Test under single and dual-task conditions in women with fibromyalgia. J Clin Med . 2022;12(1):212. doi:10.3390/ jcm12010212



Rovin Ian Antonio, SPT, is a student physical therapist at the University of Puget Sound School of Physical Therapy.
Teri Lake-Coblio, SPT, is student physical therapist at the University of Puget Sound School of Physical Therapy.
Holly Roberts, PT, PhD is a boardcertified specialist in neurologic physical therapy (emeritus). She is the Director and Associate Professor at the University of Puget Sound School of Physical Therapy.