ADVOCATE

EASTERN DIAMONDBACK RATTLESNAKE AND OTHER FLORIDA PIT VIPER ENVENOMATIONS IN THE DOG AND CAT
- Page 10
Michael Schaer, DVM, DACVIM, ACVECC
Cory Woliver, DVM
Ashley E. Allen-Durrance, DVM, DACVECC
TIPS FOR PERFORMING A COMPREHENSIVE SMALL ANIMAL ORTHOPEDIC EXAM

- Page 16
Michael H. Jaffe, DVM, MS, CCRP, DACVS
EDUCATING IS ADVOCATING - Page 24
Beckie Mossor, BIS, RVT
HURRICANE PREPAREDNESS KIT 2022 - Page 31 for veterinarians and veterinary practices
ISSUE 2 | 2022
7207 Monetary Drive Orlando, Florida 32809
Phone – 407.851.3862
Toll-free – 800.992.3862
Fax – 407.240.3710
info@fvma.org
www.fvma.org
OFFICERS
Dr. Marta P. Lista
President
Dr. Jacqueline S. Shellow
President-elect
Dr. Alex 'Steve' Steverson Treasurer
Dr. Mary Smart
Past President
DISTRICT REPRESENTATIVES
Dr. Julie Moodoyan

District 1–Big Bend
Dr. Thomas E. Hester
District 2–Northeast
Dr. Todd Fulton
District 3–Central
Dr. Donald S. Howell
District 4–Tampa Bay
Dr. Beth Keser
District 5–Treasure Coast
Dr. Robert L. Swinger
District 6–South Florida
Dr. Barbara Lewis
District 7–Southwest
Dr. John R. Wight
District 8–Northwest
Dr. Christine M. Storts
District 9–Space Coast
Dr. Ernest C. Godfrey
AVMA Delegate
Dr. Richard B. Williams
AVMA Alternate Delegate
Dr. Sally DeNotta
FAEP Representative to the FVMA Executive Board
President's Message
Thank you for your FVMA membership.
We have great people involved in the FVMA, mostly volunteers, and all of us are passionate about veterinary medicine. Your FVMA Executive Board and committee members represent the diversity of our membership from our expansive careers, diverse work environments, and diverse backgrounds and cultures. FVMA leadership is as diverse as our members. FVMA staff helps us to implement our ideas and improve existing programs. I like to describe the board as the membership think tank. I encourage you to get to know your district representative and let them know your concerns.
With the board’s help, I’ve been focusing on our collaboration with UFCVM. Increasing our association’s presence on campus will help to expose our next generation to the different options available to them. The FVMA is providing our newest veterinarians with the tools to be our next leaders and entrepreneurs as they begin their journeys and continue to move our profession forward. I encourage you to list your practices on the UFCVM externship database for third and fourth-year students and help expose students to FVMA member practices.
Our other focus area is promoting entrepreneurism and supporting veterinarians and their businesses. Did you know that according to the latest Merck-AVMA Wellbeing Study a good practice climate is the most powerful predictor of good mental health, high levels of well-being and lower levels of burnout? The four elements that go into this are:
• Strong sense of belonging to a team
• High degree of trust between team members
• Candid and open communication between team members
• Sufficient time to provide high-quality patient care
This is such great information because it is something we can all work on whether we are practice owners or not. The FVMA is perfectly positioned to help us in our endeavors and help veterinarians thrive both professionally and personally. Our award-winning FVMA anthem video highlights our many roles and dedication. Our video also serves to promote the importance of veterinary medicine to the public. In addition, we are building on our years of establishing veterinarians as the trusted source of information on pets and animal health in Tallahassee to actively work with our legislators and pass telemedicine legislation that benefits veterinarians, clients and pets.
I hope to meet many of you at The Gulf-Atlantic Veterinary Conference (TGAVC) 2022. In addition to top-notch CE and wet labs, the JW Marriott in North Miami has its own water park, spa and run path. Serving #DVMmoms and our families well is a priority of the FVMA.
The FVMA is an association of, by and for our members. The FVMA Executive Board’s diversity brings balance to our association and allows us to best represent the membership. I am interested in hearing from you, our members. How best can the FVMA help you? Email me at president.fvma@fvma.org
Yours in Service, Martica
Lista, DVM
Scan QR Code to watch FVMA Anthem Video

TO ADVANCE THE VETERINARY MEDICAL PROFESSION, PROMOTE ANIMAL HEALTH AND WELL-BEING, AND PROTECT PUBLIC HEALTH. FVMA
Opinions and statements expressed in the FVMA Advocate reflect the views of the contributors and do not represent the official policy of the Florida Veterinary Medical Association (FVMA), unless so stated. Placement of an advertisement does not represent the FVMA's endorsement of the product or service.
MISSION:
Please share this video with your friends, family and clients to promote the importance of veterinary medicine to the public. 2 | FVMA Advocate
KNOW YOUR DISTRICT Representatives
District
Dr. John R. Wight district8rep@fvma.org

district4rep@fvma.org



district3rep@fvma.org
There are nine districts covering the state and each district has a representative who serves as a member of the FVMA Executive Board. Each district is made up of local associations.

District
Representative Dr. Julie Moodoyan district1rep@fvma.org
District
Representative Dr. Thomas E. Hester district2rep@fvma.org
DISTRICT 9 SPACE COAST
District 9 Representative Dr. Christine M. Storts district9rep@fvma.org


District
Representative Dr. Beth S. Keser district5rep@fvma.org


District
Representative Dr. Barbara Lewis district7rep@fvma.org
District 6 Representative Dr. Robert L. Swinger district6rep@fvma.org
 8 Representative
1
2
5
7
District 3 Representative Dr. Todd Fulton
District 4 Representative Dr. Donald S. Howell
DISTRICT 8 NORTHWEST
DISTRICT 1 BIG BEND
DISTRICT 2 NORTHEAST
DISTRICT 5 TREASURE COAST
DISTRICT 6 SOUTH FLORIDA
DISTRICT 7 SOUTHWEST
DISTRICT 3
CENTRAL
DISTRICT 4 TAMPA BAY
FVMA DISTRICTS
8 Representative
1
2
5
7
District 3 Representative Dr. Todd Fulton
District 4 Representative Dr. Donald S. Howell
DISTRICT 8 NORTHWEST
DISTRICT 1 BIG BEND
DISTRICT 2 NORTHEAST
DISTRICT 5 TREASURE COAST
DISTRICT 6 SOUTH FLORIDA
DISTRICT 7 SOUTHWEST
DISTRICT 3
CENTRAL
DISTRICT 4 TAMPA BAY
FVMA DISTRICTS
| 3 www.fvma.org @thefvma @the__fvma @thefvma
In 2021, the Florida Veterinary Medical Association (FVMA) launched the Power of Ten, a much-anticipated leadership program focused on developing the potential of young veterinary professionals (graduated 2013–2022) in Florida, heightening their profile in the FVMA and organized veterinary medicine.

We are currently seeking candidates for the 2023–2024 program from you and young veterinarians you know!
Ten applicants will be selected to participate in the Power of Ten. Selected applicants will join a network of peers in a series of learning experiences and mentoring sessions during the course of a year. They will also get free attendance to and participation in FVMA Annual Conference and The Gulf-Atlantic Veterinary Conference.
The program is intended to be a pathway to help the selected recent graduates maneuver and successfully handle the challenges of their new professional environments.
The FVMA anticipates that the Power of Ten will also create a sense of community and build lasting bonds with other members of the leadership academy class.
In-person learning experiences will be scheduled to minimize the impact on the participants’ working hours. The entire program is designed to garner support from practice owners who recognize their key responsibility in developing veterinary leaders.

Participants will have the opportunity to engage in workshops, webinars and other special offerings exclusive to the Power of Ten.
Participants will receive full-tuition scholarships to the program, and the FVMA will publicly recognize Power of Ten graduates in an appropriate fashion.
Please note: the application process will include candidate interviews following the application deadline. Candidates must have graduated between 2013–2023.
APPLICATION DEADLINE: October 1, 2022

4 | FVMA Advocate
WE HAVE UPDATED OUR POWER OF TEN APPLICATION PROCESS to be simpler and easier!
Florida Practices for Sale
FL, NEW LISTING! West Coast, City South of Tampa, SA Solo Practice Grossing
$1.2M+ Located in a Lease Facility in a Busy Plaza. ADI $316K PRX Only (FL25S)
FL, West Coast Area, SA Solo DVM, +/ -3500SSF Lease Facility, Open 4.5 days a week plus 1 Saturday per month, located between Lakeland and Tampa, $850K Gross. PRX Only (FL33V)
FL, Homestead - Miami suburb. Solo DVM, well-established, 3000SF facility, wellequipped, 3 exam rooms, $1.3M+ Gross. Seller available to stay on fulltime. Buyer’s ADI $250K. 30 miles to Key Largo, FL. PRX & RE (FL83H)
FL, Titusville, East Coast – Open Mon-Fri. Solo DVM. +/- 2940SF free-standing facility. .60 acre housing 3 exam rooms with Abaxis in -house blood machines. Revenues of $850K+. Buyer’s after debt income ≈$180K. PRX & RE (FL40T)
FL, NEW LISTING! West of Jacksonville. 100% SA, Solo DVM, $1M Gross. Freestanding facility. Information forthcoming. PRX & RE (FL95J)
For listings nationwide, add yourself to Practice Watch from our website. 800.333.1984 | southeast@simmonsinc.com | simmonsinc.com

IN THIS ISSUE 3 | Know Your District Representatives 4 | Power of Ten Application 6 | Member Spotlight 8 | Is now a good time to buy or start-up? 10 | Eastern Diamondback Rattlesnake and Other Florida Pit Viper Envenomations in the Dog and Cat 16 | Tips for Performing a Comprehensive Small Animal Orthopedic Exam 20 | Upcoming Events 2021-2022 24 | Educating is Advocating 28 | Disaster Relief Chair - Dr. Terry Clekis 31 | Hurricane Preparedness Kit 34 | Practice Pulse 36 | In Remembrance 37 | Classified Ads Simmons Says: Exit Strategy Spend 25% or less on drugs & supplies. Organize production reports for accuracy. Upgrade equipment. Remove nonfunctional equipment. Update facility. Call Simmons!
| 5 www.fvma.org @thefvma @the__fvma @thefvma
Dan Bieck, DVM
When FVMA member Dr. Dan Bieck traveled to Mongolia with Christian Veterinary Mission to teach veterinary professionals modern practices, he said the outlook of Mongolian natives taught him the most.
The Des Moines, Iowa, veterinarian arrived in Mongolia in May and quickly began working alongside V.E.T.Net, a nongovernmental organization working in Mongolian veterinary medicine and education.

With a schedule that included lectures, devotions and overseeing veterinary procedures, the hands-off approach Dr. Bieck and his colleagues implemented on the mission meant Mongolian veterinarians could learn by practicing with their own hands.
With uncommon breeds and language barriers, the surprises that walked into the clinics presented challenges the experienced veterinarians of Mongolia met with composure and skill.
MEMBER SPOTLIGHT
Images courtesy of Dr. Dan Bieck.
6 | FVMA Advocate
“We had some big, massive dog come in. I had never seen this sort of dog before,” Dr. Bieck said of a patient with a habit of eating rocks. “All the veterinarians had been out one, maybe two years, and the veterinarian I was working with had done one exploratory on a tiny cat. And man, he’s got some great hands; his surgical skills were higher than many of the graduates we see in the United States.”
Dr. Bieck said his experiences with the people left the biggest impact on him, as they remained willing to learn and be themselves despite the obstacles that faced them.
“The people are so genuine, so honest,” he said. “Ninety-five percent of the communication in most of the surgeries I have helped with have been nouns and body language.”
Dr. Bieck remarked on the constant generosity of Mongolian locals, with each person he encountered being adamant on learning despite the language barriers between them.
“Anything you can do is going to be of significant help,” he said. “Everyone is so nice and so eager to learn.”
Dr. Bieck is no stranger to persevering through hardship, having struggled with burnout and stress earlier in his career.
After graduating from Iowa State University College of Veterinary Medicine in 1998, Dr. Bieck practiced small animal medicine in Charleston, South Carolina for 12 years before purchasing Happy Tails Pet Hospital in Illinois to move closer to family.
The hospital grew to a staggeringly successful practice, increasing revenue and clientele by significant margins, but doing so sometimes came at the expense of Dr. Bieck’s personal well-being. “We spent so much time and bandwidth focused on our practice that we were missing our only son growing up and missing out on a large portion of our faith,” Dr. Bieck said.
Having made significant strides in his career goals, Dr. Bieck and his wife elected to sell the practice in 2018 to Heartland Veterinary Partners, who agreed to continue to run the practice with the same kind-hearted, progressive and affordable ideals that made Dr. Bieck’s practice so beloved initially. This gave Dr. Bieck time to focus on better aligning his personal life and allowed him to spend more time with his wife, Jenny, and their son, Noah.
“I would advise all young veterinary professionals to practice balance,” Dr. Bieck said. “Priority should be placed on family and on finding happiness in your individual life, so that you can maximize fulfillment in your professional life, too."
After achieving better personal balance, Dr. Bieck accepted a role with Heartland Veterinary Partners as university relations manager for its campus division, where he serves as a mentor for the veterinarians of the future, much like he did on his Mongolian mission trip.

 Dr. Bieck, his son Noah and his wife Jenny.
Above: Dr. Bieck pictured in Mongolia. Opposite: Dr. Bieck pictured with his dogs after arriving home in Des Moines following his mission in Mongolia.
Dr. Bieck, his son Noah and his wife Jenny.
Above: Dr. Bieck pictured in Mongolia. Opposite: Dr. Bieck pictured with his dogs after arriving home in Des Moines following his mission in Mongolia.
| 7 www.fvma.org @thefvma @the__fvma @thefvma
IS NOW A GOOD TIME TO BUY OR START UP?
by Carly Watson Tobler | Simmons & Associates Southeast, Inc.
Between corporate consolidators buying practices on every corner, the national shortage of associate veterinarians, and the COVID-19 pandemic, veterinarians are beginning to question whether this is a good time to consider practice ownership. With the rewards available to owners, it is always a good time to purchase a veterinary practice. The catch is that it must be the right practice. Start-ups, on the other hand, are riskier no matter the market.
Purchasing a practice with open doors, client flow and a minimum of $500K in revenues is a purchase worth considering, provided the practice’s profitability supports the value and commercial financing. Ideally, it is in a healthy community and preferably a growing area. It should absolutely be a practice that the buyer sees potential in.
Interest rates are still low, though starting to rise, so now is a good time to borrow money for the purchase or start-up. The circulating rumor that veterinarians with high student loan debt cannot afford to borrow funds for the purchase is just not true. Commercial financing will lend up to 100% of the purchase price. If a down payment is required, it is industry standard that the seller finances any balance of the price allowing the buyer to have few out-ofpocket expenses. That said, lenders do prefer for the buyer to have some liquidity for a rainy day. “Gifts” from family or friends to get over the financing hurdle is a creative way many buyers get around this lender equity requirement. Below is an example of the equity or “net worth” a practice owner can build in 10 years of ownership compared to the career associate veterinarian.
Start-ups are risky in general, though there are still untouched markets, especially in fast-growing suburbs, so occasionally there
WELL-PAID ASSOCIATE IN A SMALL ANIMAL PRACTICE IN USA ANYWHERE.
Annual Compensation: $100,000.00
Invests 10%: $833.33 monthly for 10 years at a return of 8% per year
After 10 years:
Savings: $153,000.00
Equity: $0.00*
Net Worth: $153,000.00
is a gold mine waiting to be tapped into. In today’s environment, however, one should be cautious opening a practice. With pandemic fluctuations still present, as well as curbside services and mask requirements in some areas, you must be certain that you can overcome the inevitable hurdles. Pandemic aside, statistically it takes about five years to see a return on your investment from opening a business.
To be successful in ownership, whether buying or starting up, one must have interest and ability in the business aspect of running a practice. The medical aspect is the natural part for a veterinarian. You should consider having a strong practice manager on your team.
Successful ownership takes hands-on actions with strong management and interpersonal skills. If you want nothing to do with handling production, financial statements, public relations, business marketing, human resources and general problem solving, then ownership might not be for you. Ownership is not for everyone and is not an easy paycheck. The high reward of a successful practice is well-deserved by the owner who puts in the work to get there.
Whether buying or opening a practice, be sure you have solid representation on your side. Hire a broker or start-up consultant with veterinary-specific experience. Every transaction is unique and has challenges to overcome. You want a representative whose sole focus is veterinary practices and knows this industry better than any other. If ownership is in your future, it is never too soon to start researching your options and devising a plan to get to the ownership table. Start today!
PURCHASE A PRACTICE FOR $625,000
UNDER TYPICAL FINANCING TERMS.
Annual Compensation: $165,000.00*
Invests 10%: $1,375.00 monthly for 10 years at a return of 8% per year
After 10 years:
Savings: $252,000.00
Equity in practice: $1,018,000**
Net Worth: $1,270,000.00
* Assuming no salary increase as practice grows. ** Assuming all practice loans are paid in full and a 5% annual practice growth rate.
8 | FVMA Advocate
SAVE THE DATES
OCTOBER 6–9, 2022
SAWGRASS MARRIOTT


1000 Tournament Players Club Blvd, Ponte Vedra Beach, FL 32082
World-class, equine-exclusive continuing education




“The
APRIL 20–23, 2023
SIGNIA BY HILTON


ORLANDO BONNET CREEK
14100 Bonnet Creek Resort Ln, Orlando, FL 32821
World-class, continuing education for every member of the veterinary team.

TO LEARN MORE, VISIT WWW.FVMA.ORG/CONFERENCES OR CALL 800.992.3862
EQUESTRIAN CENTER 1750 Nw 80th Ave, Ocala, Fl 34482
JANUARY 20–22, 2023 WORLD
Horse Capital of the
World,”
FVMA/FAEP Upcoming Events 2022-23
EASTERN DIAMONDBACK
RATTLESNAKE AND OTHER FLORIDA PIT VIPER ENVENOMATIONS IN THE DOG AND CAT
 Image courtesy of Canva.
Michael Schaer, DVM, DACVIM, ACVECC
Cory Woliver, DVM
Ashley E. Allen-Durrance, DVM, DACVECC
Image courtesy of Canva.
Michael Schaer, DVM, DACVIM, ACVECC
Cory Woliver, DVM
Ashley E. Allen-Durrance, DVM, DACVECC
10 | FVMA Advocate
Crotalus adamanteus (Figure 1), one of the more dangerous snakes in the United States and the most dangerous pit viper in Florida, is indigenous to the southeastern United States (North and South Carolinas, Georgia, Florida, Alabama, Mississippi, and Louisiana). Crotalids characteristically have two elongated canalicular upper maxillary teeth that fold back against the roof of the mouth (solenoglyphous fangs). When striking a victim with its mouth wide open, the snake’s maxilla and fangs are rotated forward about 90 degrees and thus become effective stabbing instruments. The venom is released through a slit located at the distal segment of the fang rather than the tip. Other characteristic identifying features of the crotalids include vertically elliptical pupils, a deep pit (hence, the name pit viper) between the eye and the nostril, which functions as a heat receptor organ, and a somewhat triangular head. Crotalus adamanteus can grow as long as seven feet and can live beyond 20 years.
Pit vipers in Florida do not hibernate because of the consistent warm and temperate temperatures. In general, most snakebites occur between June and October and are less frequent between December and March.

Penetration and envenomation are rapidly followed by the onset of swelling, hemorrhage and pain around the wound. A deeply penetrating fang puncture into the muscle plane or directly within an arteriole and subsequent envenomation can result in shock within minutes and call for an accelerated treatment strategy. Not all venomous snakebites result in envenomation. From one-third to one-half of all human victims show little or no evidence of envenomation (“dry bites”), but such data is more difficult to assess in animals. Variables that influence the severity of snakebite include (1) the location, depth, and the number of bites, (2) the amount of venom injected, (3) the species and the size of the snake involved, (4) the age and the size of the victim, (5) the victim’s sensitivity to venom, and (6) the microbes present in the snake’s mouth. Bite wounds to the tongue or oral cavity are particularly dangerous because of subsequent soft tissue swelling and upper airway obstruction. Other facial bites in the dog and cat are not associated with airway obstruction. Periocular bites can result in blindness. The after-effects of head wounds are particularly relevant for dogs, as 70-80% of the dogs treated at the University of Florida Small Animal Hospital (UFSAH) have been struck in the face. Limb and trunk involvements are more common in the cat. Envenomations at all body sites are potentially lethal.
The amount of venom released depends on when the snake last ate and the degree to which it feels threatened. Most pit vipers can meter the amount of released venom. If a snake has not eaten recently, a large volume of venom will be available for release at the time of the strike. In addition, a large snake can usually inject a greater amount of venom than a smaller snake, thus making it more life-threatening to the victim. The toxic effects
are inversely proportional to a victim’s size. However, the overall toxicity is dependent on the amount of venom inoculated. This amount is impossible to quantitatively measure, thus requiring a thorough assessment of the clinical signs that usually parallel the amount of venom injected.
VENOM TOXICITY OVERVIEW
Familiarity with the components and effects of venom and an understanding of the pathophysiology of snake venoms are essential for effective treatment. Most pit viper snake venoms have direct or indirect toxic effects on the victim’s blood cells, heart, blood vessels, respiratory and nervous systems. The brain is uniquely resistant to any direct toxic effects of most rattlesnake venoms, the exceptions being select species with a neurotoxin component (Mojave, Timber, Southern Pacific). The primary effects of the venom released by pit vipers in the southeastern United States include local tissue damage, hemolysis, coagulopathy, thrombocytopenia, edema, hypovolemia and, with some pit vipers, neurotoxicity. Neurotoxic effects are brought about by a complex mixture of five-15 enzymes, metal ions, biogenic amines, lipids, free amino acids, large and small proteins, and polypeptides. Kidney damage associated with these regional pit vipers is mostly due to acute kidney injury caused by the combined effects of hypovolemia and pigmenturia (hemoglobin and myoglobin).
The Water Moccasin (found throughout Florida) and the Timber Rattlesnake (found primarily in North Florida) are the second and third most venomous pit vipers in Florida, respectively. Copperhead envenomations in Florida are confined to the northwestern part of the state, with most of these involvements limited to necrogenic damage to soft tissues; however, some do have systemic involvement. The venom components might vary amongst the different types of snakes, and the clinical signs will range from moderate to severe.
Figure 1. The Eastern diamondback rattlesnake is widely distributed in Florida and ranks amongst the top 10 most venomous snakes in the world. Image courtesy of Cory Woliver.
| 11 www.fvma.org @thefvma @the__fvma @thefvma
Pygmy rattlesnake venom contains proteolytic enzymes, phosphodiesterase, and L-amino-oxidase, which will cause pain and tissue swelling. Its small size and small volume of venom generally cause mild signs.
First Aid
First aid measures for pit viper envenomation in the dog and cat are not recommended because of the potential for iatrogenic damage and lack of efficacy. The best action is to seek immediate veterinary care. Do not use bandaging or ice compression as these measures can compromise circulation to an affected limb.

Triaging and Patient Severity Assessment Guidelines
Triaging the emergency patient should first focus on temperature, pulse, respiration, posture and mentation. Examination of the bite sites should note the degree of swelling and any active bleeding. The majority of cases are usually able to ambulate, but a minimally compensated patient can deteriorate soon thereafter. The initial laboratory tests should include the packed cell volume (PCV) and total solids (TS) and a blood smear to look for echinocytes and platelets. Any signs of hemolysis should be noted. Coagulation tests should be done on animals with moderate and severe signs. These tests include prothrombin and partial thromboplastin times (PT, PTT), activated clotting time (ACT), or whole blood clotting time (WBCT). Urine should be observed for pigmenturia (hemoglobinuria, myoglobinuria). Cardiac monitoring with an electrocardiogram and blood pressure assessment should be done on all recumbent patients.
PATIENT ASSESSMENT AND INITIAL TREATMENT
MILD. Patient acts normal and vitals are normal. Bite site localized and minimally progressive over the first two hours. Most of these animals will be treated with intravenous lactated Ringer’s with several hours or overnight observation. Antivenom might not be necessary in clinically stable patients with minimal signs.
MODERATE. Able to stand and walk. Ambulation slow, mentation “quiet,” bite site swelling slowly and progressively over the first two hours. Cardiac rhythm can initially be normal, but ventricular arrhythmias can follow. Coagulation status might vary from normal to abnormal because of on-going fibrinogenolysis. Temperature, pulse and respiration (TPR) are stable, but heart rate (HR) and respiratory rate mildly increased. Pulses and capillary refill time (CRT) are normal. Note that the patient’s status can suddenly become severe within a short time, so observe frequently. Intravenous crystalloids and antivenom are recommended for these patients.
SEVERE. Patient recumbent with dull mentation, HR rapid, pulses weak and CRT prolonged. Rapid progression of swelling over the first two hours (Figure 2). Gross bleeding tendency. Cardiac tachyarrhythmias commonly occur within the first 24 hours. Neurological abnormalities might accompany Timber rattlesnake envenomations. A more detailed Severity Score sheet is available elsewhere for a more detailed assessment of organ systems (Witsil 2015; see Recommended Readings). Abnormal clotting tests should be repeated regularly every two to four hours during hospitalization to assess the adequacy of the patient’s response to treatment and to detect persistent coagulopathy that might require additional antivenom treatment. Urine output and BUN or serum creatinine levels should also be measured to detect any acute kidney injury (AKI) resulting from ischemia and/or hemolysis. A CK > 5000 and myoglobinuria (Figure 3) will reflect ongoing rhabdomyolysis and the potential threat to renal tubular function from circulating myoglobin. Intensive care with IV crystalloids and antivenom is essential for these patients. Fatalities involving severe envenomation cases over the past 10-20 years at the University of Florida have averaged about 10%.
TREATMENT
Intravenous Fluids and Blood Products
Essential treatments initially include intravenous fluids and antivenom. Physiologic balanced isotonic polyionic intravenous crystalloid solutions (lactated Ringer’s, Normasol, Plasmalyte) are essential for providing patient circulatory stabilization.
Figure 2. This Labrador has severe envenomation signs including hypotension, coagulopathy and hemolysis. He required eight vials of antivenom over the first four hours and additional doses subsequently. Somnolence is typical for such patients, but they are very treatable Image courtesy of Dr. M. Schaer.
12 | FVMA Advocate
Many dog and cat snakebite victims will be hypotensive and therefore require resuscitative (bolus) amounts of intravenous fluids (10-20 ml/kg IV over 10-15 minutes; cats approximately one-half that amount). Blood pressure and/or CRT monitoring along with heart and respiratory rates will be the best guides for further resuscitative fluid therapy. Animals that remain hypotensive after fluid resuscitation may require vasopressor treatment (see below). Once the animal is hemodynamically stable, maintenance IV fluid therapy is indicated (40-60 mL/kg/day), adjusted according to need. It is important to take the volume of fluids needed for antivenom dilution into consideration for the total fluid volume administered, especially for animals weighing < 5 kg to avoid IV fluid overload. Synthetic colloids (dextran and hetastarch) can potentially impair platelet function and should therefore not be administered. Most animals will stabilize with IV crystalloid and antivenom treatments. Some may require packed red blood cell transfusions due to anemia caused by bleeding and hemolysis. Blood product administration is based on clinical signs (lethargy, tachycardia, bounding pulses, etc) in conjunction with anemia (PCV usually less than 25%). Blood product administration will be required with severe acute hemorrhage. An assessment of total solids may be a better indicator of status. Plasma might be required if the coagulopathy persists despite the patient having received adequate amounts of fluids and antivenom.
Vasopressors
Vasopressor treatment is indicated when blood pressure cannot be stabilized after appropriate fluid resuscitation and antivenom administration. Blood pressure will be easier to correct when venom is appropriately neutralized. Persistent hypotension usually calls for increased amounts of antivenom before electing to use vasopressors. Norepinephrine at 0.05-1.0 µg/kg/min by constant rate infusion (CRI) is a commonly used approach. Do not delay blood pressure stabilization with vasopressors if the patient's condition is not improving with antivenom and fluids, as this can lead to end organ damage.


Analgesics
Analgesic drugs should be used, if necessary, but it is important to minimize the initial doses to avoid pharmacologic-induced mental depression which will impair patient evaluation. They are rarely used beyond the first 48 hours, the exception being soft tissue discomfort caused by progressive necrosis between the third and fifth hospital days. Commonly used analgesics include intravenous opioids (methadone, hydromorphone and fentanyl administered as a titratable CRI) or oral gabapentin for those less severely affected. Nonsteroidal anti-inflammatory drugs are not recommended as they can impair platelet function and potentiate acute kidney injury.
Glucocorticoids and Antihistamines
These drugs have no proven benefit during the acute phases, and their use should be reserved to treat hypersensitivity reactions. Pre-treatment to avoid allergic reactions is not necessary with the highly purified antivenom products used in North, Central and South America. Pretreatment also will not typically prevent a hypersensitivity reaction.
Antibiotics
The majority of snake bites in dogs and cats are not complicated by bacterial infection, therefore having no indications for antibiotics initially. Snake venom is noted to have antibacterial properties which typically minimize the chance of immediate infection. Exceptions occur when tissue necrosis, abscessation and putrefaction occur after the bite. In these situations, broadspectrum antibiotics are recommended. This is a common practice in the Southern Hemisphere countries that have to deal with Bothrops and Lachesis sp. envenomations. Tetanus antitoxin is not recommended in dogs and cats because of the absence of reported cases of this infectious complication.
Figures 3a and 3b. Myoglobinuria has a range of pigment intensity from light tea to dark tea-like pigment.
3a 3b
Image courtesy of Dr. M. Schaer.
| 13 www.fvma.org @thefvma @the__fvma @thefvma
Antivenom Use and Types
The use of polyvalent crotalid antivenom is the mainstay of therapy for moderate to severe envenomation; however, the cost of large quantities of antivenom limits its affordability as a treatment for some pet owners. Early and ample doses of intravenous antivenom treatment for victims with moderate to marked symptoms have been stressed repeatedly in humans, and the same practice should be followed in animal patients. Under optimal conditions, antivenom should be given within four hours after the snakebite. Although the full beneficial effect diminishes when antivenom is given after this period, it is still recommended up to and sometimes 24 hours after envenomation. For most mild to moderate envenomations, one to four vials of antivenom are sufficient. For severe envenomations, typically six to ten vials are administered during the first four to six hours of hospitalization. A publication by Bush in Toxicon (2013) describes administering the usual loading dose according to the severity assessment followed by one to two vials of antivenom using slow CRI infusion every four to six hours for one to three days in order to prevent the re-envenomation syndrome caused by continued venom absorption from the bite site. This technique has been adapted for the patients in our hospital. If the bite results in the injection of a large quantity of venom deep into well-vascularized soft tissues or directly into a vessel (“arteriolized”), death may occur early despite vigorous antivenom treatment.
Anaphylaxis and anaphylactoid reactions are possible complications of horse serum-derived antivenom treatment. Do not let the fear of anaphylaxis deter you from administering ample amounts early in treatment when dealing with moderate and severe envenomations, even if the animal has received previous antivenom treatment. Any early signs of anaphylaxis, such as vomiting, salivation, defecation or restlessness, should be immediately treated with epinephrine (use 1:1000 concentration and administer 0.01 mg/kg IM; can repeat q 15-20 min for up to three treatments) while discontinuing the antivenom until the patient is stable. Epinephrine can also be administered as an intravenous constant rate infusion (starting dose 0.05 µg/ kg/min) depending on the severity of signs and the ability to provide constant intensive monitoring as found in tertiary medical facilities. Diphenhydramine (an H1 blocker) should be given at a dose of 2 mg/kg IM. Glucocorticoids are unable to act fast enough to counteract the immediate effects (aside from their dysgenomic effect) of anaphylaxis, although they are helpful for the treatment of delayed signs and serum sickness which can occur between five-14 days after the beginning of antivenom treatment. Anaphylaxis is also accompanied by the loss of significant fluid loss from the vascular space which worsens the hypotension caused by envenomation, thereby requiring a rapid infusion of isotonic crystalloid solution such as lactated Ringer’s for patient stabilization.
Boehringer-Ingelheim Antivenin™ [BI(formerly Wyeth and Fort Dodge) Antivenin Crotalidae Polyvalent (ACP)] is an antivenom composed of whole IgG derived from horses and is prepared in a lyophilized form. It is effective against most North and South American pit vipers, except the Mojave rattlesnake. It has extra antigens because of the Fc component, which makes it more capable of causing immune allergic reactions (>30% incidence in humans, but <10% in dogs in the authors’ experience.). It can distribute throughout much of the interstitial space and can remain in circulation for 82 hours, thus having a very long half-life. In general, the dose will range from one to two vials for mild signs (only localized minimally progressive swelling and pain), two to four vials for moderate signs (progressive swelling and coagulopathy), and five-10+ vials for severe signs (recumbency, hypotension, cardiac dysrhythmias, neuropathy, hemolysis and coagulopathy). When using any antivenom, the authors recommend that epinephrine is pre-drawn at a dose of 0.01 mg/kg for IM injection at the earliest signs of anaphylaxis.
Rattler Antivenin™ (MG Biologics), Crotalidae polyvalent, is an equine-origin antivenom that contains antibodies against Prairie, Mojave, Western Diamondback and Eastern Diamondback rattlesnakes. The label shows effectiveness against Copperhead or Water Moccasin snakes as well. Rattler Antivenin™ comes in a frozen, liquid form and is a whole IgG product, which might be associated with increased allergic reactions. The manufacturer recommends a dose not to exceed two packages in most instances.
VenomVet™ (MT Venom) is an F(ab')2 antivenom produced by MT Venom in Argentina and licensed for use in dogs in the United States. The authors have also found it safe and effective for treating cats. It is effective against many North American pit vipers. It is prepared as a liquid that comes ready for use. It has a moderate elimination half-life of 36 hours and has a better volume of distribution compared to the whole IgG products. It has no Fc component, thereby making it less antigenic and having an allergy incidence of <10%. The dose for treating moderate signs calls for two to four vials IV initially with repeated dosage given every two to four hours depending on signs and coagulation status.
Crofab® (BTG International Inc.) is a Fab antivenom derived from sheep. It is the purest antibody product, and it has the widest distribution throughout the body. Its high price and short duration of action usually preclude its use in veterinary patients.
Selected References 1. Bush, S.P., Seifert, S.A., Oakes, J., Smith, S.D., Phan T.H., Pearl S.R., Reibling, E.T., 2013. Continuous IV crotalidae polyvalent immune Fab (ovine) (FabAV) for selected North American rattlesnake bite patients. Toxicon. 69, 29-37.
14 | FVMA Advocate
2. Lavonas, E.J., Ruha, AM., Banner, W., Bebarta V., Bernstein, J.B. Bush, S.P, Kerns ll, W.P., Richardson, W.H. Seifert S.A., Tanen, D.A., Curry, S.C., Dart, R.C., 2011. Unified treatment algorithm for the management of crotaline snakebite in the United States: results of an evidence –informed consensus workshop. BMC Emergency Medicine. 11. 2-15.



3. Schaer M, Buckley G, Conner BJ, et al.,2015. Severe pit viper envenomation with extended clinical signs and treatment complications in a dog. J Am Anim Hosp Assoc; 51(5). 329-37.

4. Witsil aj, Wells RJ, et al. 272 cases of rattlesnake envenomation in dogs: Demographics and treatment including safety of F(ab’2 ) antivenom use in 236 patients. Toxicon 2015,Oct; 105:19-26

MICHAEL SCHAER
DVM, DACVIM, DACVECC
Dr. Michael Schaer is currently professor emeritus and adjunct professor in emergency and critical care medicine.

ASHLEY E. ALLENDURRANCE
DVM, Diplomate ACVECC
Dr. Allen is a clinical assistant professor of emergency and critical care.


CORY WOLIVER
DVM
Dr. Woliver is a clinical lecturer of emergency and critical care.

Photo credit: www.123rf.com/profile_sam74100 Best Friends Forever Pet Moving Solutions Worldwide • Nationwide airanimal.com
TIPS FOR PERFORMING A COMPREHENSIVE SMALL ANIMAL ORTHOPEDIC EXAM
 Michael H. Jaffe, DVM, MS, CCRP, DACVS
Michael H. Jaffe, DVM, MS, CCRP, DACVS
16 | FVMA Advocate
Image courtesy of Canva
Orthopedic injuries in dogs are a common reason for patients presenting to the veterinarian. Many orthopedic injuries can be diagnosed based on a good orthopedic exam coupled with high-quality radiographs. A structured, well-executed orthopedic exam in small animals is critical to the diagnosis of many orthopedic injuries. The orthopedic exam is intended to first localize the source of lameness to a specific limb, second to further localize the source of lameness to a specific joint, and third to identify specific findings that aid in developing a comprehensive rule-out list.
I like to begin the orthopedic exam the moment the patient comes into my sight. I begin by watching how the patient moves, stands, sits down and gets up. Clues to the affected limb often become apparent right away based on the patient’s gait. Performing a formal gait exam where the patient is observed walking to and from the observer, as well as across the observer’s vision, will also help to localize the affected limb. Trotting (if the patient is able) and stepping up or stepping down are also helpful in unmasking the lameness.
Following performance of a thorough general physical exam, a complete neurological exam should always be included. Neurologic abnormalities such as a cervical disc lesion may manifest as a lameness due to a root signature. Lumbosacral injuries will mimic disorders affecting the hips or rear limbs. Because of this, whenever I approach any lameness case, I keep in mind that there are four broad categories of lameness:
• Orthopedic injuries (true injuries to the bone and joints)
• Neurologic injuries (think root signatures and peripheral nerve injuries)
• Immune-mediated and infectious causes (immune-mediated polyarthritis, etc.)
• Muscle and tendon soft tissue injuries
The goal of this exam is to decrease the number of possible causes for the lameness, if able, and focus our list of differential diagnoses.
In general, it is best to examine all four limbs of the patient, despite one limb showing obvious lameness. Many patients have a bilateral injury causing lameness, and it is easy to miss this if we only focus on the obviously lame limb. I prefer to save the most obviously lame limb for examination last if able. If I begin with the most painful limb, this may result in hyperesthesia due to wind-up, which may skew any findings in other limbs. It is best to employ the help of a trained assistant to restrain the patient in a safe manner as eliciting a painful response when doing an orthopedic exam is not uncommon, and it is best to keep everyone safe from injury, including the patient. I advise starting your exam of the limbs from distal at the toes and working proximally. You should perform your exam by isolating and examining each individual bone and joint.
Paws
When evaluating the paws, begin by examining each individual toenail and toe/footpad. I look for any evidence of a puncture, cut pad or broken nail as well as nailbed injuries that may result in lameness. I look at the interdigital web between each toe for foreign bodies, masses and lacerations. I then take each toe through its full range of motion (ROM) and palpate each phalange separately. Working my way proximally, I evaluate the metacarpophalangeal and metatarsophalangeal joints for pain and normal ROM. I continue by palpating along each individual metacarpal and metatarsal bone for any pain, swelling or injury.
Carpus and Antebrachium
The carpus is a complex set of bones and ligaments. Evaluation of the carpus involves evaluation of ROM in both flexion and extension as well as checking for collateral ligament injury. Normally, the carpus should be able to flex to a point where the toe pads can touch the caudal portion of the antebrachium. The carpus normally extends ~10 degrees of hyperextension from the antebrachium. It is helpful to keep a goniometer handy to evaluate for hyperextension and measure range of motion if it is abnormal. One must palpate the carpal joint for effusion and check for any popping or clicking observed on manipulation. There should be very little collateral movement of the carpus. If you are unsure of your findings, you can check the opposite limb’s motion for comparison unless bilateral injury is suspected. Palpation along the antebrachium should be performed evaluating the radius and ulna individually feeling for any abnormalities and pain, taking note of any muscle atrophy present. Distal radial bone tumors may be noted and assessment for angular deformities should be evaluated.
Elbow
Manipulation of the elbow is performed to evaluate for crepitus, effusion, pain and ROM. The elbow should be able to fully extend comfortably, and its range of motion should be smooth and full. Full ROM in the elbow is ~135 degrees from maximal flexion to full extension. Any pop or click should be noted and crepitus or effusion determined. Supination and pronation can be assessed, but collateral instability is difficult to detect.
Humerus and Shoulder
Palpation along the humerus for pain and assessment of muscle atrophy should be performed. Panosteitis is common in the distal humeral diaphysis and osteosarcoma is often seen in the proximal humerus. Manipulation of the shoulder involves assessment of full flexion, extension and abduction. Assessing normal ROM and any popping or pain in the glenohumeral joint should be explored. Soft tissue structures such as supraspinatus muscle and biceps brachii muscle tendons should be checked. The biceps tendon is best assessed by full flexion of the shoulder
| 17 www.fvma.org @thefvma @the__fvma @thefvma
with full extension of the elbow with concurrent palpation across the shoulder joint and the intertubercular groove. Dogs with biceps tenosynovitis will exhibit great discomfort with this manipulation. Muscle atrophy of the shoulder should be assessed.

Scapula, Axilla and Cervical Spine
Few injuries involve the scapula itself except for fractures and rarely bone tumors. Palpation along the scapular spine and scapula is generally quick and easy. Muscles cranial and caudal to the scapula should be assessed for atrophy as this may be noted with cervical disc injuries. Palpation should be performed in the axilla for masses and lymphadenopathy. The cervical spine should be taken through its full range of motion and palpated for pain indicating potential cervical neuropathy.
Tarsus and Crus
The tarsus should be taken through its full range of motion and assessed for collateral instability. Tarsal injuries such as intertarsal luxations may present with hyperextension at the intertarsal or tarsal-metatarsal joint. Tarsal collateral instability, both medial and lateral, should be carefully checked individually with both the tarsus in extension and flexion. Short collateral ligament injuries will demonstrate instability with the tarsus in flexion, and long collateral ligament injuries will demonstrate instability with the tarsus in extension. Both short and long ligaments may be damaged concurrently as well. Palpation along the tibia and fibula should focus on pain, muscle atrophy and angular changes. Assessment of the calcanean tendon is best performed with both the stifle and tarsus concurrently in 90 degrees of flexion. An intact tendon should be taut. Any laxity or swelling of the distal tendon may indicate calcanean tendon disruption.
Stifle
Because of the great number of injuries to structures of the stifle, great attention should be paid to manipulation of this joint. Cranial cruciate ligament (CrCL) rupture, patellar luxation and chronic osteoarthritis are the most common injuries noted in the stifle. Flexion and extension should be assessed for instability, patellar luxation, crepitus, effusion, meniscal clicks and pain. Evaluation for suspected CrCL injuries can be performed by evaluation for cranial drawer or tibial thrust. I find tibial thrust easier to evaluate in large, awake dogs and cranial drawer easier to assess in smaller and sedated large dogs. Proper technique for assessment of cruciate ligament integrity involves identifying correct landmarks for holding the leg when performing this test.
Landmarks for assessment of cranial drawer:

• Patella
• Lateral fabella
• Tibial tuberosity
• Fibular head
With the stifle held at normal standing angle, these structures are grasped, and the stifle is assessed for drawer. For tibial thrust, I like to place my index finger across the stifle from the patella and my fingertip on the tibial tuberosity. With the stifle held at normal standing angle, flexion of the tarsus will show cranial tibial thrust in a cruciate injured stifle.
Assessment for medial and/or lateral patellar luxation is best performed with the stifle in extension. The patella location is first assessed as dogs with grades 3 and 4 patellar luxations will have their patella luxated. Gentle lateral or medial pressure on the patella will determine whether it luxates (if in normal location) or it is reduced (if luxated).
Landmarks for performing a cranial drawer test in dogs with a suspected cranial cruciate ligament rupture include the patella, lateral fabella, tibial tuberosity and fibular head. Image courtesy of Dr. Michael Jaffe.
18 | FVMA Advocate
As part of a good orthopedic exam, all long bones should be palpated and each joint should be taken through their full range of motion. Image courtesy of Dr. Michael Jaffe.
Femur
Palpation along the femur for pain, muscle atrophy and angular changes may reveal pain in the proximal femur with panosteitis as well as fractures and bone tumors at the distal femur. Muscle atrophy may be noted in dogs with chronic arthritis or thoracolumbar/lumbosacral (L-S) neuropathies.

Coxofemoral Joint
The hip may have several potential abnormalities including luxations, fractures, hip laxity, neoplasia and osteoarthritis. Flexion, extension and abduction of the hip should be carefully assessed for pain, crepitus and reduced ROM. Dogs with hip dysplasia and osteoarthritis will typically have decreased ROM of the hip specifically on extension, and pain on abduction. In puppies with suspected hip dysplasia, an Ortolani should be performed to check for possible coxofemoral laxity. Coxofemoral luxations can be detected based on how the leg is held normally, muscle atrophy, palpation of the trochanteric notch and abnormal ROM where the femoral head may be palpable with cranial-dorsal luxations. Suspected iliopsoas muscle injury may be detected by extending and internally rotating the hip while palpating the insertion of the iliopsoas muscle across the medial proximal portion of the femur (at the lesser trochanter insertion).
Pelvis and Thoracolumbar Spine
The pelvis should be palpated for symmetry of the ilial wings, as well as pain. Muscle atrophy across the pelvis may be seen with neurologic disorders and chronic osteoarthritis. A rectal exam may be performed to palpate along the pubis, ischium and medial hip joint. Palpation dorsally across the lumbosacral (L-S) joint may induce pain with L-S disorders. If elevation of the tail induces pain, this too may indicate an L-S disorder. Palpation across the thoracolumbar spine may induce pain indicating a potential herniated intervertebral disc or other vertebral abnormality.
In conclusion, an organized systematic approach to the orthopedic exam performed the same way every time will help clinicians localize the source to the correct limb and location. A list of differential diagnoses may then be developed. From there, further diagnostics such as imaging, arthrocentesis and other diagnostics will help further elucidate the cause of the lameness and guide treatment plans.
Dr. Michael Jaffe is a graduate of the University of Missouri College of Veterinary Medicine. He completed a one-year companion animal internship and a three-year small animal surgery residency at LSU where he also received his master’s degree. Dr. Jaffe is currently an associate professor and service chief of small animal surgery at Mississippi State University CVM. Dr. Jaffe became a diplomate of the American College of Veterinary Surgeons in 2002 and a certified canine rehabilitation practitioner in 2017.
 MICHAEL H. JAFFE DVM, MS, CCRP, DACVS
Landmarks for performing a tibial thrust test in dogs with a suspected cranial cruciate ligament rupture include placing your finger from the patella to the tibial tuberosity with the leg maintained at a normal standing angle. By flexing the tarsus in dogs with a cranial cruciate ligament injury, the examiner’s fingertip on the tibial tuberosity will be thrust forward.
Image courtesy of Dr. Michael Jaffe.
MICHAEL H. JAFFE DVM, MS, CCRP, DACVS
Landmarks for performing a tibial thrust test in dogs with a suspected cranial cruciate ligament rupture include placing your finger from the patella to the tibial tuberosity with the leg maintained at a normal standing angle. By flexing the tarsus in dogs with a cranial cruciate ligament injury, the examiner’s fingertip on the tibial tuberosity will be thrust forward.
Image courtesy of Dr. Michael Jaffe.
| 19 www.fvma.org @thefvma @the__fvma @thefvma
Excellence & Enrichment | Fresh & Energizing
Offering More Than 300 Hours of Cutting-edge CE
The FVMA invites you to The Gulf-Atlantic Veterinary Conference from Sept. 22–25, 2022, for its worldclass program of engaging lectures and hands-on instruction.



SPEAKERS AND INSTRUCTORS:
• RICK ALLEMAN, DVM, PhD, DABVP, DACVP
• TERESA ARRISON, CVT, VTS (Dentistry)
• LENORE BACEK, DVM, MS, DACVECC
• LARRY BAKER, DVM, FAVD, DAVDC
• JAN BELLOWS, DVM, DAVDC, DABVP
• KIM BISSING, BS, CPDT-KA
• SØREN BOYSEN, DVM, DACVECC
• SUSAN CARASTRO, DVM, MS, DACVO
• ED CARLSON, CVT, VTS (Nutrition)
• SERGE CHALHOUB, BSc, DVM, DACVIM (SAIM)
• KRISTIN COLEMAN, DVM, MS, DACVS-SA
• LORELEI D’AVOLIO, LVT, VTS (Exotics), CVPM
• DIANE DELMAIN, DVM, DABVP (Feline)
• CORAL DOHERTY, RVT, CPHSA
• LAURA GARRETT, DVM, DACVIM (Oncology)
• ADAM GONZALES, DVM, DACVIM (Small Animal)
• RALPH HARVEY, DVM, MS, DACVAA
• WENDY HAUSER, DVM
• PETER HELMER, DVM, DABVP (Avian)
• MICHAEL JAFFE DVM, MS, CCRP, DACVS
• ROBERT KENNIS, DVM, MS, DACVD
• PATTY LATHAN, VMD, MS, DACVIM
• JESSICA MARTINEZ, MS, DVM, DACVO
• LINDA MESSINGER, DVM, DACVD
CONTINUING EDUCATION HOURS:
MORE THAN 300 CE HOURS
-12 hands-on wet labs
-Maximum of 28 CE hours for veterinarians
-Maximum of 18 CE hours for veterinary technicians
• ANNIE MILLS, LVT, VTS (Dentistry)
• TERRY O’NEIL, CPA, CVA
• JEANNE PERRONE, MS, CVT, VTS (Dentistry)
• MONICA PERRY, BS, CVPM
• PHILIP RICHMOND, DVM, CAPP, CPHSA, CPPC, CCFP
• SHEILAH ROBERTSON, BVMS (Hons), PhD, DACVAA, DECVAA, DACAW, DECAWBM (AWSEL), MRCVS
• LIZA RUDOLPH, BAS, RVT, VTS (CP-CF) (SAIM)
• HOWARD B. SEIM III, DVM, DACVS
• CHRISTINE SENNECA, DVM, DACVIM (Neurology)
• KELLY SIGLE, DVM, DACVO

• MEG SLEEPER, DACVIM (Cardiology)
• ALYSSA SULLIVANT, DVM, MS, DACVIM
• ROBERT SWINGER, DVM, DACVO
• RACHEL TEICHBERG, CVPM, CVBL
• KENNETH WALLER III, DVM, MS, DACVR
• STUART WALTON, BVSc (Hons), BSc Agr (Hons), MANZCVS (SAIM), DACVIM
• HEATHER WAMSLEY, BS, DVM, PhD, DACVP - Clinical
• HEIDI WARD, DVM, DACVIM (Oncology)
• PETER WEINSTEIN, DVM, MBA
• AMELIA WHITE , DVM, MS, DACVD
• JACQUELINE WHITTEMORE, DVM, PhD, DACVIM (SAIM)
• MICHAEL WONG, DVM, DACVIM (Neurology)
AAVSB RACE, Provider #50-27127: Course #20-922170
Florida Board of Veterinary Medicine DBPR FVMA Provider #0001682
Sponsor of Continuing Education in New York State
EARLY BIRD RATE ENDS AUGUST 24, 2022
⊲ MORE THAN 300 CE HOURS
⊲ LEADING SPEAKERS
⊲ HANDS-ON WET LABS
⊲ ENGAGING LECTURES
⊲ DON’T MISS OUT!
Stimulating CE at an Iconic South Florida Destination

TOPICS INCLUDE:
• Anesthesia/Pain Control
• Avian/Exotic
• Cardiology
• Clinical Pathology
• Dentistry
• Dermatology
• Emergency Medicine
• Exotic Medicine
• Feline Medicine
• Gastroenterology
• Infectious Disease
• Internal Medicine
• Laser Therapy
• Neurology
• Nutrition
• Oncology
• Ophthalmology
• Pain Management & Anesthesia
COMPREHENSIVE WET LABS

• Practice Management
• Rehab & Orthopedics
• Surgery
• Technician Medicine
• Ultrasound
• Wellness
• QPR session with Dr. Richmond (Saturday)
• Ultrasound
Kenneth Waller III
DVM, MS, DACVR
Søren Boysen
DVM, DACVECC
Serge Chalhoub
BSc, DVM, DACVIM (SAIM)
• Surgery
Howard Seim III, DVM, DACVS
• Dentistry

Jan Bellows
DVM, DAVDC, DABVP
Jeanne Perrone
MS, CVT, VTS (Dentistry)

• Ophthalmology
Robert Swinger, DVM, DACVO
• Laser Therapy

Kim Bissing, BS, CPDT-KA

Limited availability! Reserve your seat today!
Scan QR Code to learn more!
PRE-REGISTRATION & HOTEL RESERVATION
EXHIBIT HALL ACTIVITIES
The Gulf-Atlantic Veterinary Conference offers attendees an unmatched opportunity for networking. Our industry partners showcase an unparalleled display of the very latest innovations and advancements available to veterinary professionals.

• Experience a dynamic showcase of more than 80 exhibitors
• Speak one-on-one with industry professionals regarding the newest technologies

• Learn about the latest products and services available


• Network with veterinary colleagues and industry experts


• Enjoy the Welcome Reception and complimentary breaks
• Participate in Cover-all Bingo for a chance to win prizes, including grand prize of $1,000.00 check!

• Try your luck at the FVMA Foundation Wine Toss game!
• Registration includes complimentary lunch on Friday and Saturday in the Exhibit Hall

Scan QR code to see who is exhibiting!

SPECIAL THANKS TO THE FOLLOWING
Industry Partners
JW Marriott Miami Turnberry Resort & Spa







19999 West Country Club Drive, Aventura, FL 33180
RESERVATION DEADLINE IS AUGUST 24, 2022

EXCLUSIVE TGAVC RATE $249/NIGHT*

Book over the phone by calling 786.279.6770 or 888.236.2427
Mention Group Code: “FVMA”
Room rate does not include $20 resort fee (discounted from $47). Resort fee provides free admission to Tidal Cove Waterpark Complex.




Room Block Deadline: August 24, 2022 Or until room block is sold out. After August 24, 2022, room rate will increase, if rooms are available.
To learn more about JW Marriott Miami Turnberry and book your room, scan the QR Code

ROOMSpecialRATE $249
Partners & Sponsors

FOR THEIR

GENEROUS SUPPORT:
EDUCATING IS ADVOCATING
by Beckie Mossor, BIS, RVT
 Image courtesy of Shutterstock
Image courtesy of Shutterstock
24 | FVMA Advocate
Educating is advocating. Over the past few years of lecturing about client communication, this has become my tagline. Well, that and veterinary technician is not a consolation prize, it is a profession, but that is another article for another time. This line has become a constant reminder in my lectures because I find a nearly ubiquitous hesitation from veterinary professionals to discuss several areas of wellness. From my own experience in practice and discussions with hundreds of veterinary professionals across the nation, the discomfort often comes from a feeling of "selling," the resistance from clients, and our personal experiences. The hesitance or complete omission of essential conversations in the clinic could have lifelong, even life-ending consequences for our patients. Flipping the narrative in our heads and for our clinics can lead to best practices for our patients.
Protocols
Protocols create foundations for conversations within the clinic. Creating protocols provides guidelines that aid team members to be on the same page when discussing treatments and preventions with clients. When the whole team is on the same page, repeats recommendations and follows up accordingly, there is less confusion around best practices in the clinic. When protocols vary by practitioner, department or worse, are not defined at all, there may be an increased likelihood of confusion, oversight or varying levels of importance in the communication of patient needs. Not to mention frustration for the support staff who must accommodate a protocol for each practitioner.
By creating protocols for all areas of practice and each department, teams have a reference for ensuring all recommendations for patients are the same, and no area of prevention or care is overlooked. But it is also essential for each team member to understand the protocol and the importance behind it. Understanding the why can help team members feel more educated in discussing protocols, regardless of their role in the clinic. For clients, hearing the protocols repeated by each team member can help reinforce their importance. Clients will also feel more confident in the team's understanding of the treatment plan.
Last, protocols create an opportunity to discuss important health prevention topics: preventatives, nutrition, obesity, breeding/ spay or neuter decisions, behavior, and other sometimes tricky conversations. These conversations may be considered difficult for several reasons: a high level of sensitivity or controversy, confirmation bias, or even the seemingly obvious nature of the need. When we use checklists and clinic policy procedures for conversations, we ensure all discussions are essential and covered with every client. The worst feeling is when a client returns with a patient with a preventable condition or disease because they genuinely did not know or understand the treatment or husbandry need, and the clinic missed an educational opportunity.
Educate Effectively
Clinics are busier than ever, mid and post- COVID-19. There is less face-to-face communication, less time and less ability to connect directly with clients. This overwhelming period, let alone the regular hustle and bustle of clinics, may make it feel even harder to educate clients, discuss protocols and the importance of preventative measure opportunities. But it is entirely possible to work smarter, not harder, connect with and educate clients.
One mistake in approaching client education is the assumption that educating the client means to brain dump, verbally, at the client, in the few minutes allotted with them. On the best days, in the best scenario, a few minutes in the veterinary clinic may not be considered an ideal learning environment. While there are often efforts to create a less distracting environment and usually pages of photocopied information sent home, a less than ideal amount of information is likely communicated to and retained by the distracted client. Setting people up for success on both sides of the exam table can equate to better outcomes for our patients. So, lean into the easy way to communicate with clients, the internet! Hosting live discussions, making a video library and having a resource library on your website are great ways to optimize time and reach. Clients connect with the internet and social media, and there is no shortage of outlets to reach clients of all ages. You may also find team members have a fun time creating content, which they are more likely to share. When a client can learn in an environment that serves them, they are more likely to retain the information shared and to come back for more learning.
Another common mistake is the communication approach between clinics, staff and clients. It is natural to approach client conversations and education with science and data – proof. So, this is often the approach taken in discussions and content sharing. It is essential to understand the empathy point for each client concerning their pet. When the client's focus is understood,

| 25 www.fvma.org @thefvma @the__fvma @thefvma
educating and advocating can be tailored to meet the client's interests and are more likely to be retained when the importance is made more personal. Empathy points may emphasize longevity, health, reduction of zoonotic disease or athletic ability. When these points relate to the treatment plan, the client better understands the importance of what is being discussed and is more likely to accept the treatment plan.

Along the same lines of communication, word choice is essential. The term "recommendation" has not been used throughout this article. Instead, it is replaced with a treatment plan or protocol. When using words like "optional" or "recommend," the impact may be lost. Clients may feel confused or underestimate the importance of the product or service discussed. Ensuring team members use the correct language in discussing clinic protocols for treatment and prevention can prevent potential misconceptions around importance.
Veterinary clinics can be a client go-to for questions and learning when clinics provide engaging content. Remember, the whole team is made up of valuable and trusted individuals. Clients depend on each team member to ensure all information is communicated

regarding caring for their pets. Clinic teams have more potential to ensure education is a priority in the clinic when organized protocols and recommendations are made. Communication skills are as essential to patient outcomes as the technical skills used to prevent diseases and treat illness. Overcoming discomfort around conversations and being innovative in educational approaches are crucial aspects of advocating for patients through education.
BECKIE MOSSOR RVT
Beckie is a Registered Veterinary Technician living in Southport, NC. She has enjoyed a diverse career in small animals, large animal, mixed practices, management, private consulting, and academia. She is currently the Program Director for Gurnick Academy of Medical Arts Veterinary Technician Program and co-founder of Veterinary Advancements, a private consulting firm. And when possible, deploys with the ASPCA Disaster Recover Team.

26 | FVMA Advocate ® THE EPICUR OATH Safer, consistent medications. For a list of drugs, visit epicurpharma.com 888.508.5032 Traditionally compounded medications available from a 503B Manufacturer overseen by the FDA Drugs manufactured following cGMP, the same regulations used by pharmaceutical companies Approved for distribution One of the largest portfolios of 503B drugs for animal health







WORLD-CLASS PROGRAM OF CUTTING-EDGE LECTURES AND HANDS-ON INSTRUCTION. For more information SCAN QR CODE TO SIGN UP FOR REGISTRATION DETAILS www.fvma.org/conferences OR CALL 800.992.3862 WORLD EQUESTRIAN CENTER, OCALA, FLORIDA JANUARY 20-22, 2023 2023 OCALA EQUINE CONFERENCE | 27 www.fvma.org @thefvma @the__fvma @thefvma WHAT'S YOUR EXIT STRATEGY? Y O U R T R U S T E D V E T E R I N A R Y B R O K E R . NATIONAL PRACTICE SALES CORPORATE SALES VALUATIONS ASSOCIATE BUY-INS BUYER REPRESENTATION 9 1 2 . 2 6 8 . 2 7 0 1 | H E L L O @ P S A V E T . C O M W W W . P R A C T I C E S A L E S A D V I S O R S . C O M REBECCA
DVM,
ROBINSON DAVIS, CBI BRENNAN MCGOLDRICK,
MBA

Images courtesy of Dr. Terry Clekis
28 | FVMA Advocate
DISASTER RELIEF COMMITTEE CHAIR SPOTLIGHT Terry Clekis, DVM
From an early age, Dr. Terry Clekis always knew he wanted to become a veterinarian. After completing his undergraduate studies at the College of Charleston and graduate studies in reproductive physiology at the University of Georgia, Dr. Clekis went on to attend and graduate from the University of Georgia’s veterinary school in 1983.


After gaining experience as an associate veterinarian and hospital owner in the Charleston, South Carolina area, and St. Petersburg, Florida, Dr. Clekis purchased Braden River Animal Hospital in 2002 and built the current, state-of-the-art facility behind the original building in 2007. After many successful years at Braden River Animal Hospital, Dr. Clekis further expanded the grounds by building a new boarding and grooming center adjacent to Braden River Animal Hospital to help offer comprehensive care. In 2017, he expanded to the greater Sarasota-Bradenton area and opened North River Animal Hospital in Parrish, Florida.



Today, Dr. Clekis is instrumental and influential in setting the direction for veterinary medicine. He is widely known for his expertise in wellness care, and he routinely speaks on the use of cutting-edge products and protocols related to veterinary medicine. Dr. Clekis has also been featured in many local, state and national publications such as Veterinarian Compendium and the Merial Monitor. Under his leadership, Braden River Animal Hospital is one of the few nationally recognized clinical trial research sites for all major animal health pharmaceutical companies. He is also well-known for his work in organized veterinary medicine and disaster relief.
When Dr. Clekis moved back to Florida in 1992, he began working with Bill Goldston, who became his mentor. Dr. Clekis credits Dr. Goldston’s involvement in the Florida Veterinary Medical Association (FVMA) and American Veterinary Medical Association (AVMA) as his driving force for joining organized veterinary medicine.
“He taught me that it was important to give back to organized veterinary medicine. Before then, I would go to meetings and stuff like that, but I never really thought I was one of those ‘joiner’ kind of guys,” Dr. Clekis said. “It was under his guidance and suggestions, suggestions more like ‘You're going to the freaking
meetings!’ that I learned it was important to give back to the profession that's been supporting me.”
Dr. Clekis was instrumental in starting and serving as president of the Manatee County Veterinary Medical Society. In 2007, he was awarded a Gold Star Award by the FVMA, which recognizes outstanding contributions to veterinary medicine. In 2019, he was awarded Veterinarian of the Year for his outstanding leadership, service and dedication to his team while offering aid in the Florida Panhandle after Hurricane Michael. He was a board member of the Southeast Guide Dog Association, the Manatee County Humane Society and the American Heartworm Society. Dr. Clekis is an active member of the AVMA, the FVMA, and the Florida Veterinary Corps.
| 29 www.fvma.org @thefvma @the__fvma @thefvma
Dr. Clekis said one of his greatest passions involves giving back to the veterinary community and supporting younger veterinary professionals. His reputation landed him an invite to serve as a facilitator for Veterinary Management Group (VMG), where he organizes biannual meetings of twenty veterinarians from across the country to discuss best business practices in an ever-changing industry.
As Dr. Clekis became involved in organized veterinary medicine, he began to lean toward disaster relief. And then, in 2004, four hurricanes, Charlie, Francis, Ivan and Gene, rocked Florida and brought Dr. Clekis truly into the disaster community. An advocate of preparedness, he cites having a plan as the most important thing veterinarians and their offices can do to be ready.

“The more people know and are thinking about this, the more prepared we will be,” he said. “Preparation will help ensure that the animals in the state are well taken care of. Disaster preparedness starts at home. Priority is to take care of your family first and expand that to your business, staff, clients, etc. Once your family and business are secured that’s half the battle, only then you can start reaching out to your colleagues to assist.”
Dr. Clekis has served as the FVMA’s Disaster Response Committee Chair since 2010, where he is responsible for ensuring that all veterinary hospitals have a plan of action for their clients and patients in the event of a natural disaster. Thinking about his veterinary legacy, Dr. Clekis hopes the disaster preparedness committee will be organized, selfsufficient and more than a committee of one – himself. At the end of his tenure, he aims for it to be a self-perpetuating, well-oiled machine that anyone can step into – and he encourages the veterinary community to step up. Having a plan, distributing disaster preparedness information to clients, and reaching out locally to emergency operations centers and other county officials. He notes that it’s key to establish relationships before disaster strikes.
“The more you can reach out locally the better the response, rather than waiting on state or national responses. You need to be prepared yourself. I’m in a very unique position to have these relationships with industry, with the state, the FVMA, the University of Florida and just by the nature of my personality, I know a lot of people. Disaster medicine is a relationship business. The time to meet people is not during a disaster but before. It’s amazing to know I can bring people together and facilitate a response, just based on who I know.”
Dr. Clekis enjoys being a vital part of the Manatee County and Bradenton communities. Whether in the hospital, educating on disaster preparedness or on the road with his family in their RV, Dr. Clekis is committed to ensuring that he does everything in his power to build long-term relationships with anyone he comes in contact with.

When asked about why he has dedicated so much time and effort to this work, he only has one answer: “To give back to the community that has welcomed me with open arms.”

30 | FVMA Advocate
HURRICANE PREPAREDNESS KIT 2022 for veterinarians and veterinary practices
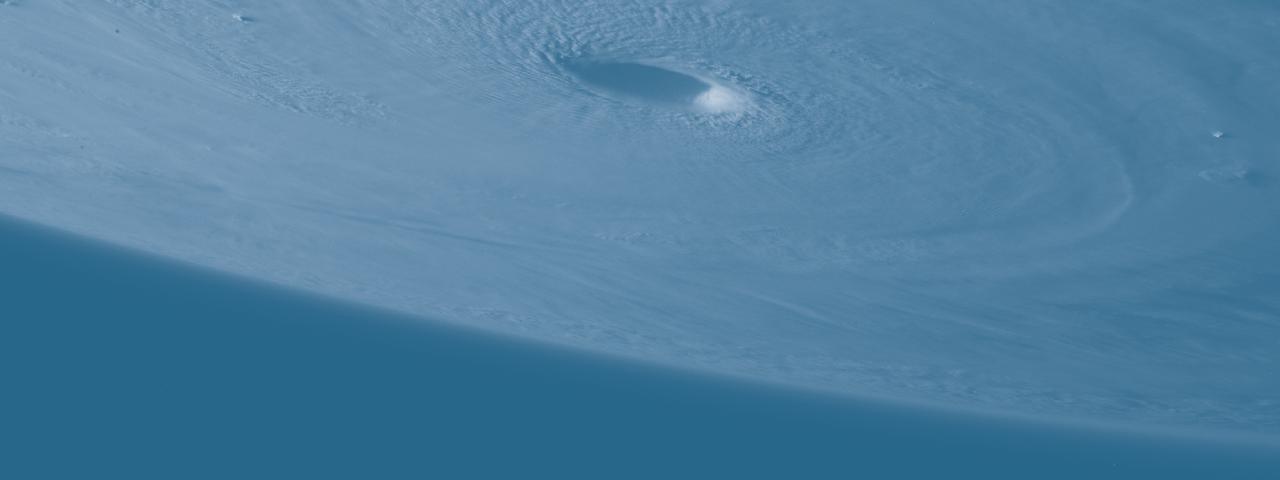
Another hurricane season has arrived. While hurricanes have gotten larger and deadlier in recent years, last year's storm fears were eclipsed by the COVID-19 pandemic. This year marks a return to rainy rituals and serves as a reminder of the importance of preparation. It's vital to stock up and be aware of potential storms that may head Florida's way.
During uncertain times, remain prepared for, not scared of, what lies ahead. Your clients choose to bring animals into their homes, and these animals cannot fend for themselves when huge storms approach. The following tools will help pet owners and veterinary practices prepare for major storms.
ADVICE TO PASS ALONG TO YOUR CLIENTS
While many clients will have previously weathered hurricanes with their pets, some may be first-time pet owners or may have just moved to an area with hurricanes. Remind your clients that pets should be kept inside during the storm and indoor accommodations made for them to ‘go potty.’ It is also important to make sure the client knows that if they choose to evacuate, the pet should go with them. If it’s not safe for the pet owner, it’s not safe for their pets. As hurricanes approach, and chaos ensues, consider emailing your clients with the following recommendations.
KEEP YOUR PET IN DISASTERREADY CONDITION
• Ensure all of your pets’ collars and tags have up-to-date contact information.
▶ Microchipping a pet is one of the best ways to find them again should they become lost.
• Have proper equipment for pets to ride in the car with you (this is especially important for cats or exotics, who may not leave your house often).
• Pet carriers are needed at many shelters and can serve as a safe space for a nervous pet. They are highly recommended
when transporting your pet. The pet carrier should be the correct size (the pet should be able to stand, turn around and lay down comfortably). Be sure to label the carrier with your pet's name, breed, sex, date of birth, your current address and contact numbers, and any important medical information.
• Collar or harness with ID tag, rabies tag and a leash.
▶ Carry at least one slip leash. A simple slip-type webbing or nylon leash will ensure you have a way to restrain a dog (or even a cat) in the event they slip out of their collar or harness.
WHAT TO INCLUDE IN YOUR PET'S DISASTER KIT
• At least three days to two weeks’ worth of food and water specifically for your pet stored in sealed containers.
▶ If your pet’s regular diet includes canned food, remember to have a manual can opener with you.
▶ Don’t forget bowls to serve your pet’s meals.
• At least two weeks’ worth of any medication they require in a sealed, airtight container.
• Important documents such as any registration information, adoption papers and vaccination documents. Photocopied records of your rabies certificate, vaccinations and medical summaries should be stored in a waterproof container.
• A first aid kit particularly for your pet. May include bandage rolls, tape and scissors; antibiotic ointment; flea and tick prevention; latex gloves, isopropyl alcohol and saline solution. A pet first aid reference book is a good idea too.
• Hygiene and grooming supplies. Any sanitation items and products you need to clean and clean up after your pet. Consider pet litter and litter box if appropriate, newspapers, paper towels, plastic trash bags and household chlorine bleach.
• A picture of you and your pet together will help you document ownership and allow others to assist you in the event you become separated. If it is a printed photo, consider noting the pet's species, breed, age, sex, color and distinguishing characteristics on the back of the photo.
• Familiar items, such as treats, toys and bedding can help reduce stress for your pet. Toys will also help keep your pet occupied.
| 31 www.fvma.org @thefvma @the__fvma @thefvma
ASK, DON’T ASSUME
Be sure to secure accommodations for your pet before the storm. Every time a hurricane approaches, false information circulates on social media. A common myth is that there are laws requiring all hotels to allow pets in their rooms during an evacuation notice. This statement is not true and can put you in a tough spot if all other pet-friendly hotels in your area are already booked. Ask ahead of time if the location you plan to evacuate to is comfortable with every pet you will be bringing when you arrive there. There are also plenty of websites where you can verify if a hotel or shelter will be pet-friendly.
• Compile a seven-day supply of food and water for staff and patients, along with any medications that might be needed for this seven-day period.
• Write down a list of contacts that can be used throughout the duration of the emergency operations period, should any challenges arise.
BUILDING & PERSONNEL SECURITY
Your local fire department is a great resource for inspections and evacuation drills. Each municipality has specific instructions in the event of an impending disaster.
• Outline all preferred means of reporting emergencies, as well as the main point of contact in such emergencies.
• Establish an office phone tree and pre-plan opportunities for conference calls with anyone who will be off-site during the storm.
• Secure your practice to prevent any crime, such as theft and looting.
PREPARING YOUR CLINIC
Whether you plan to evacuate or ride out the storm, every effective disaster plan for veterinary practices and clinics consists of seven basic parts. All seven of these will be critical to the success of your company during a major storm.
• Emergency relocation of boarded and hospitalized animals
• Backups of medical records
• Continuity of operations
• Building and personnel security
• Fire prevention
• Chemical spill prevention
• Insurance coverage/legal issues
Be sure to hand out your completed hurricane plan in advance, so you aren’t trying to create and disseminate a plan at the last minute.
EMERGENCY RELOCATION OF BOARDED & HOSPITALIZED ANIMALS
• Make sure leashes, carriers and other species-specific supplies are brought along.
• Plan for appropriate, pre-arranged animal transportation along with a temporary animal holding location.
▶ Include a 24-hour client contact list, which can also be accessed off-site.
• Inform staff, clients and legal counsel of your planning processes for these animals.
MEDICAL RECORD BACKUP
• Keep medical records and digital copies of important documents backed up on an off-site computer.
CONTINUITY OF OPERATIONS
• Have alternative power sources to avoid issues, should the power go out for an extended period of time.
▶ If you purchase backup generators, make sure staff is well-versed in the maintenance and operation of them.
FIRE PREVENTION
• Identify any/all fire hazards in the workplace.
• Go over proper handling and storage procedures with the rest of the staff.
• Appoint employees who will be responsible for maintaining this equipment.
CHEMICAL SPILL PREVENTION
• Create a plan to address appropriate responses to all foreseeable emergencies, which may include hazardous chemical spills.
▶ Employees will need to be trained on the proper equipment required to respond to these issues, should they arise.
▶ Each Florida county’s extension service has information on how to respond to chemical disasters, which was provided by the University of Florida’s Institute of Food and Agricultural Services (UF/IFAS).
INSURANCE COVERAGE & LEGAL ISSUES
• Make sure your insurance is up to date.
▶ Speak to your agent ahead of time, preferably before the impending disaster.
▶ AVMA PLIT’s insurance carriers accept claims from uninsured customers in affected areas.
▶ If you are insured through AVMA PLIT and you need to file a claim, you can find filing information at avmaplit.com. This site also offers additional resources to assist with commercial damage assessments, reestablishing security after a natural disaster and minimizing interruptions for your business. AVMA LIFE will sometimes extend the grace period for premium payments for an additional 60 days following a natural disaster. If you are insured through AVMA LIFE and have questions or need assistance, call 800.621.6360 or visit avmalife.org.
For more information, visit CDC.gov and search “Pet Safety in Emergencies.”
32 | FVMA Advocate
POST-DISASTER RESOURCES
FVMA FOUNDATION ASSISTANCE
Any FVMA member who assists in rescue, relief and recovery efforts during a natural disaster is encouraged to apply for reimbursement through the FVMA Foundation. Member veterinarians who provide emergency boarding to animals may also be eligible. Any members who are facing an unreimbursed loss as a result of a storm may also be considered for FVMA grant assistance. For more information, contact the FVMA at 800.992.3862 or visit www.fvma. org/disaster-relief.
ADDITIONAL GRANT AND REIMBURSEMENT ASSISTANCE
AVMA member veterinarians participating in rescue and emergency care related to a natural disaster may apply for reimbursement through their charity, the American Veterinary Medical Foundation (AVMF). For more information visit www.avmf.org and search “disaster reimbursement grants.”
FEMA AID
Those impacted by damage from these disasters can also apply for FEMA aid. There are specific loan programs for businesses and private non-profit organizations, as well as homeowners and renters in affected counties. To learn more, visit www. fema.gov or www.disasterassistance.gov.
The IRS offers tax relief to areas designated by FEMA as qualifying for either individual or public assistance. The IRS has a declaration permitting a postponement of certain deadlines for taxpayers who have a business in, or live in, disaster areas. If you receive a late filing or late payment penalty notice from the IRS, call the telephone number on the notice in order to abate the penalty. The IRS will also waive any usual fees and expedite requests for copies of previously filed tax returns for those who were affected.
Affected taxpayers in a federally declared disaster area also have the option of claiming disaster-related casualty losses on their federal income tax return. You may also deduct personal property losses that were not previously covered by insurance or other reimbursements.
BUSINESS RELOCATION REMINDER
If your practice suffers damage from a storm and you need to relocate, contact the Florida Department of Business and Professional Regulation to apply for a new establishment license for the new location. For more details, visit the Florida DBPR website at www.myfloridalicense.com.
FVMA FOUNDATION DISASTER RELIEF FUND
When tragedy strikes, the FVMA Foundation is proud to work on the front lines and behind the scenes to help veterinary professionals get back on their feet. A major contributor to helping restore practices and rescue animals during natural events like hurricanes, the FVMA Foundation strives to maintain the veterinary medical profession during tough times.

Donations to the FVMA Foundation help us fund our rescue and rebuilding initiatives, and go directly to veterinary professionals when they need it most. Scan

QR code to Donate Today! | 33 www.fvma.org @thefvma @the__fvma @thefvma
PRACTICE Pulse
QUESTION: I have an adult female German Shepherd mix that presented to our practice after being found four weeks ago. We scanned the patient and learned she had a microchip. After contacting the microchip company, we were informed that this pup was also found four weeks prior by someone else and they had attempted to contact the owner without success. At this point, the people who brought the dog into my clinic would like to keep this patient; however, I am inquiring about how long we must wait to officially transfer ownership and more importantly, am I legally allowed to vaccinate her for rabies at this time?
A: The person who brought the animal to you and takes responsibility of care for the animal is your client. Your records should reflect that. So, despite you finding out the dog was microchipped, and the microchip holder cannot be found, your responsibility really is to ‘your client.’ Dogs are property in Florida. Under the law, the greatest indication of ownership over personal property is possession. The person who brought the animal to you for care is, effectively, already the owner of the animal. A legitimate VCPR is established when the client brings the patient to the veterinarian, arranges for treatment and assumes the financial responsibility for same. You now have a duty to maintain that relationship confidential. If you had found out who owned the microchip, you could not have contacted the "microchip owner" without authorization from this client, as you would’ve breached your duty to him/her to maintain confidentiality. Finally, you should treat the animal as your duty of care dictates.
QUESTION: A practitioner in my area who recently retired has asked: 'What is the recommended timeframe for a practitioner to continue to carry liability insurance in case of a claim that arises post-retirement for a case the practitioner was managing prior to retirement?'
A: Regarding liability coverage after retirement, FVMA legal counsel advises: The statute of limitations for professional services malpractice is two years. Carrying malpractice insurance – “tail coverage” – for two years after retirement would cover this.
QUESTION: My incoming new grad did not pass the NAVLE. Sadly, I think this may be a more frequent occurrence after two years of COVID disruption for current senior students. She is scheduled for a re-take and is studying hard. If she doesn't pass the second time, is there a limit on the amount of time that she can practice under my supervision without a license? Is there a limit in Florida as to how many times she can take the NAVLE? Is there anything else I should be considering or aware of?
A: The way we read the statute, the unlicensed veterinarian may no longer practice veterinary medicine under supervision.
(5) An unlicensed doctor of veterinary medicine who has graduated from an approved college or school of veterinary medicine and has completed all parts of the examination for licensure is permitted, while awaiting the results of such examination for licensure or while awaiting issuance of the license, to practice under the immediate supervision of a licensed veterinarian. A person who fails any part of the examination may not continue to practice, except in the same capacity as other nonlicensed veterinary employees, until she or he passes the examination and is eligible for licensure.
The exemption to practice under supervision is allowed until the candidate receives notice that she did not pass. This veterinarian can only now practice as a veterinary technician until she passes the NAVLE. There is no limit however, on the number of times a candidate can take the exam.
Nevertheless, the employer veterinarian needs to know that veterinary technicians can do a lot of things:
61G18-17.005 Tasks Requiring Immediate Supervision.
(1) All tasks which may be delegated to a veterinary aide, nurse, laboratory technician, intern, or other employee of a licensed veterinarian shall be performed only under the “immediate supervision” of a licensed veterinarian as that phrase is defined in Section 474.202(5), F.S., with the exception of the following tasks which may be performed without the licensed veterinarian on the premises:
(a) The administration of medication and treatment, excluding vaccinations, as directed by the licensed veterinarian; and
(b) The obtaining of samples and the performance of those diagnostic tests, including radiographs, directed by the licensed veterinarian.
(2) The administration of anesthesia and tranquilization by a veterinary aide, nurse, laboratory technician, intern, or other employee of a licensed veterinarian requires “immediate supervision” as that phrase is defined in Section 474.202(5), F.S.
(3) The administration of any vaccination by a veterinary aide, nurse, technician, intern or other employee of a licensed veterinarian which is not specifically prohibited by Rule 61G1817.006, F.A.C., requires “immediate supervision” as that phrase is defined in Section 474.202(5), F.S.
34 | FVMA Advocate
GOT A QUESTION? THE FVMA CAN HELP.
One of the benefits of an FVMA membership is our helpline (800.992.3862), which is available to members Monday through Friday from 8 a.m.-5 p.m. Our helpline also provides insight to the FVMA staff of the challenges and concerns of our members. In this feature, we will highlight topics from the questions we received in preceding weeks as a part of an effort to keep our members up to date on current concerns, as well as regulatory and legislative changes.
The only things a veterinary technician cannot do are listed in the following rule:
61G18-17.006 Diseases which Only a Veterinarian May Immunize or Treat.
For the purpose of implementing the exemption provisions of Section 474.203(5)(a), F.S., the Board recognizes that the following diseases are communicable to humans and are of public health significance, and that only a veterinarian may immunize or treat an animal for these diseases:
(1) Brucellosis.
(2) Tuberculosis.
(3) Rabies.
(4) Equine Encephalomyelitis.
QUESTION: I am a veterinarian in a multi-veterinarian practice. The prescribing veterinarian is out on vacation. The client has stopped by to request a refill. Can I authorize the refill without having examined the animal? Our policy has been that we must have seen the pet within the past year to receive prescription item.
A: If you have access to the patient records and can confirm that the animal is on that medication for a legitimately diagnosed condition, you may authorize/prescribe.
If someone off the street handed the veterinarian “records” that the individual brought him/herself and asked the veterinarian to prescribe based on those records without ever seeing the patient, that veterinarian would be well on his/her way to needing legal counsel. On the other hand, if your colleague in the same practice has seen the patient and you can access the records without any question whatsoever about their accuracy, and you authorized a refill, you are covering for your colleague.
QUESTION: What is the current law in regards to veterinarians dispensing cannabis from outpatient hospitals? I know there is a difference between CBD oils that do not contain THC and those that do. So I am asking about both types.
A: New hemp rules were promulgated by the Florida Department of Agriculture and Consumer Services (“FDACS”). These rules went into effect on January 2, 2020. The most important rule is Rule 5E-3.003, F.A.C., which addresses Hemp extract in pet food, pet treats, specialty pet food and specialty pet treats.
Pet food, pet treats, specialty pet food and specialty pet treats may contain Hemp extract, but not more than 0.3% total delta-
9-tetrahydrocannabinol concentration on a dry weight basis. Veterinarians may sell the above products without obtaining any additional licenses or permits.
Veterinarians may sell the above products, as long as the products are not claimed to be “drugs.” This means that the label must not contain claims indicating the product is intended for diagnosis, cure, mitigation, treatment or prevention of disease.
If veterinarians sell the above products, they must make sure that the labels on the container comply with Section 581.217, Fla. Stat., as well as Rule 5E-3.005, F.A.C.: The container must include:
a. A scannable barcode or quick response code linked to the certificate of analysis of the hemp extract batch by an independent testing laboratory;
b. The batch number;
c. The Internet address of a website where batch information may be obtained;
d. The expiration date;
If specific cannabinoids are claimed, the number of milligrams of each cannabinoid per serving must be declared on the label. The serving size shall be displayed on the label of the product.
Pet food, pet treats, specialty pet food and specialty pet treats consisting of or containing Hemp extract shall be labeled “Not for human consumption.”
Bottom line: Veterinarians should only obtain these products from reputable distributors that are in compliance with Florida laws and rules.
Read more on rule [SE-3 (5)] here:
https://www.fdacs.gov/Cannabis-Hemp/Hemp-CBD-in-Florida/ Hemp-and-Animal-Feed
END NOTE: The ultimate responsibility in the practice of veterinary medicine lies with the licensed veterinarian. Professional discretion must always be exercised.
| 35 www.fvma.org @thefvma @the__fvma @thefvma
In Remembrance
Dr. Robert Flake Chambliss Jr., DVM
Robert Flake Chambliss Jr., 83, passed away on May 28, 2022. He was born in Tampa on October 24, 1938, and attended local schools: Mitchell, Wilson and Plant High School. After graduating from Plant High School in 1956, he completed his pre-veterinary studies at the University of Florida where he was a member of Kappa Alpha Order. He earned his DVM from Auburn University in 1963. Dr. Flake spent one year in Clovis, New Mexico, in a feedlot and ranch practice and two years as a post veterinarian in the U.S. Army stationed at Fort Hood, Texas. After discharge from the army, he practiced for a short while with a small animal practice in Dallas, Texas. He returned to Tampa in 1968 to raise his family and practice at Tampa Veterinary Hospital, where he continued until retirement in 2008. He was a member of local, state and national veterinary organizations. Dr. Flake also served

on the Hillsborough County Animal Advisory Committee for several years after retirement. He was a past member of Merrymakers, Ye Mystic Krewe of Gasparilla, and Palma Ceia Golf & Country Club and a current member of Tampa Yacht & County Club.
Dr. Flake was predeceased by his parents R. Flake Sr. and Elizabeth Chambliss; son, Robert “Bob” Chambliss III; and brother, Clayton G. Chambliss. He is survived by his loving wife, Judy Poppell Chambliss; daughter, Dr. Natalie C. Light (husband, Jeff of Dallas, Texas); and granddaughter, Eleanor “Ellie” K. Light of London, U.K.; cousins: Julia Chambliss (husband, Jack Fowler) and Jim Chambliss (wife, Alyson); nephews: Noland & Callis Chambliss; step-children, Victoria C. Martin (husband, Ray of Wilmington N.C.); stepgrandchildren: Nelson Martin (Frankie), Ashley Martin, Raymond Martin (Hannah), Allison Tiisler (Rob), and step great-grandchildren: Holden and Colby Martin. The family deeply appreciates the loving care provided by the dedicated nursing staff at Canterbury Tower Health Center, and the many years of care and support by Dr. Rafael W. Blanco, Florida Cancer Specialists.
L. Bennett Flanders, DVM
L. Bennett Flanders (known by many as Doc Flanders), 84, passed away May 4, 2022, in Lakeland, Florida. He was born in Toombs County, Georgia, to Arlie and Florence Flanders.
For his senior year, Dr. Flanders specifically enrolled at Lyons Senior High School to play football. There, he met Judy Jarriel, who he married in June 1960. Shortly thereafter, in the fall of 1960, Dr. Flanders entered the University of Georgia Veterinary School. He graduated in June 1964, worked for almost a year in avian research for the veterinary school and then moved to Lakeland

in 1965. He began his veterinary practice at Crystal Lake Animal Hospital and remained there for over 30 years – later retiring from the practice he established at Kathleen Animal Hospital. As he was retiring, he pursued his lifelong dream of cattle ranching and established the thriving LBF Ranch, LLC. Dr. Flanders was an active member of the Polk County Cattlemen’s Association and a member of the FVMA for over 25 years. He was also a lover of the Georgia Bulldogs.
Dr. Flanders was preceded in death by his parents and his two sisters, Arlene Smith and Faye Lollis. He is survived by his wife, Judy Flanders, and two daughters: Lori Germany (Eric) and their children Joseph, Jordan, and Jennifer; and Carrie Bayhan (David) and their children Elleri and Ben. He is also survived by many beloved nieces and nephews.
36 | FVMA Advocate
CLASSIFIED ADVERTISEMENTS
VETERINARIANS WANTED
LOOKING FOR COMPASSIONATE IN-HOME EUTHANASIA
VETERINARIAN TO JOIN OUR TEAM AT THE HOSPICE VET: The discussion of when to say goodbye is one of the hardest, and most important, conversations a veterinarian can have with their clients. Discussing a family’s options is a skill that takes empathy, understanding, and compassion...we consider it a privilege to have these tough conversations with people leading up to their pet's euthanasia at home. Currently a single veterinarian practice, we are looking for a Veterinarian who shares our drive to offer aboveand-beyond service to the pets and people of our community.
We help clients who may have difficulty utilizing traditional veterinary services, have anxious pets, or who simply appreciate the comfort that an in-home service provides. We also offer in-home quality of life consultations prior to euthanasia as well as aftercare for the pet.
Whether you are a new graduate looking to establish your foundation, or an experienced veterinarian looking to rediscover your passion for patient care, we are looking for someone dedicated to end of life care with a sole focus on in-home euthanasia. Our ideal candidate:
- Is ready to begin building heartfelt client relationships
- Has the ability to make decisions confidently and effectively while managing time and tasks appropriately
- Values the unique needs of the individual client and patient
- Is a compassionate team player who can uphold our great reputation
We pride ourselves on being a locally owned and operated practice in beautiful Northeast Florida. Contact us at: 904-5213440 or thehospicevetpm@gmail.com
ASSOCIATE
VETERINARIAN(S) WANTED
– NAPLES, FL:
Quality of life, quality of practice, what more could an associate want? Well, how about mentorship, teamwork, and even eventual ownership? Gulfshore Animal Hospital has all of these to offer to the veterinary associate fortunate enough to join our 4-doctor practice. We have been a top ranking AAHA practice since 1996. Our clientele demands excellent veterinary care and personalized professional service, and our team delivers. Learn all the skills you will ever need from the combined 70 plus years of experience of our 2 doctor owners. Enjoy the satisfaction and fulfillment that true team comradery can bestow in a practice. And lastly, after ensuring Gulfshore Animal Hospital is the right fit for you, realize the sense of achievement and independence that potential practice ownership can confer. Naples is ranked among the top most desirable beach destinations in the US; a great place to visit, but an even greater place to work and live. If this sounds like an inviting offer, it is! We can promise you that the visit alone to our beautiful town will be well worth it. Applicants must have a passion for surgery and be proficient in routine dental and surgical procedures. Please email your resume to drdave@gulfshoreanimalhospital.com
VETERINARIAN(S) WANTED – NAPLES, FL: Our
Shelter Veterinarians provide medical/surgical care and treatment for the animals at the shelter; perform spay/neuter surgery on shelter pets prior to adoption; educate/advise the staff and the community in the care of animals; oversee medical treatment and care of animals; examine, diagnose and perform treatment and surgery as needed. Veterinarians supervise, train and direct the work of the veterinary team. If you would like additional information, please contact Director Marcy Perry at Marcy.Perry@colliercountyfl.gov
Collier County Government is an Equal Opportunity Employer and maintains a Drug Free Workplace. Veterans and their spouses/ families may receive preferential treatment.
ASSOCIATE VETERINARIAN WANTED IN SUNNY FLORIDA—APOLLO BEACH, FL: Currently we are a twodoctor growing practice in Apollo Beach, Florida looking to add a full-time associate veterinarian. Great opportunity for new or recent graduates. We have modern in-house equipment, including digital radiographs (regular and dental), Abaxis cbc (HM5) and chemistry (VetScan) machines, electrosurgical unit, CryoPen, GE Logiq E ultrasound unit, Class 4 laser, Doppler blood pressure and more. We offer competitive benefit packages including health care, dental, vision, PTO, retirement (401K), short term disability/ maternity leave, and CE. Our hours are from 8-5:30 Mon-Friday, Sat 8-1. No after hour duties. We have an amazing staff that are knowledgeable, helpful and function well as a team. Practice owner is friendly and easy going. Our team focuses on providing exceptional patient and client care. Our staff currently includes 7 full-time employees and 6 part-time employees, 2 are currently enrolled in veterinary technician programs. Our clinic is located in Apollo Beach Florida, with easy access to Tampa, St. Petersburg, Brandon, and Sarasota. Our clinic is located 15 miles south of Tampa in a quaint town built around canals that lead to Tampa Bay. Other outdoor activities include boating, fishing, and golfing which are abundant. Our doctors work a 4-day work week overall. We value a quality of life outside the clinic for all of our employees. We also have optional team building events outside of work. This last year we had a beach outing, movie outing, and went to Busch Gardens Howl-O-Scream.
Salary range $100,000 new graduates, $120,000140,000 for experienced veterinarians. Email resume to drjdiana.abah@gmail.com or call 813-732-2570
| 37 www.fvma.org @thefvma @the__fvma @thefvma
VETERINARIAN(S) WANTED – GAINESVILLE AND OCALA: Veterinarians needed for small animal general practice in Gainesville and Ocala. No weekends. Excellent pay and benefits. $25,000 hiring bonus. Email jstewart@ruralking.com
WE WANT YOU! 4-DAY WORK WEEK!: We WANT YOU!! Full and Part time Small Animal Associate Veterinarian positions available. New GRADUATES WELCOME. Enjoy practicing quality medicine in beautiful suburban West Palm Beach. Enjoy your time off and don’t get burnt out. We have 4-day work week (38 hrs.) for FT position. No afterhours Emergency. AAHA Certified practice. Excellent compensation package includes Great salary, Health Insurance, 401k, CE and much more. If this sounds good to you, send resume to lindsey@animalhealthcare.com
ASSOCIATE VETERINARIAN(S) WANTED-FORT
LAUDERDALE: AAHA accredited hospital • Fort Lauderdale • Full time/ Part time
Contact Teresa Jackson, info@arborpethospital.com • 954565-1896
ASSOCIATE VETERINARIAN WANTED IN SUNNY FLORIDA—APOLLO BEACH, FL: Well established practice for sale $50,000 below appraisal. Will finance at 5% interest, with only 5% down. Central FL. 407 529 5651 Dr. Adkins.
VETERINARIAN WANTED – ORLANDO, FL: Well established downtown Orlando (5) doctor small animal practice is seeking a full time associate to join our team. Great schedule and benefits. Pay is pro-sal (base plus production bonuses). Very beautiful and busy practice with an amazing support staff. Email: amcoforlando@aol.com or Call: 407.898.6261
VETERINARIAN(S) WANTED-OSCEOLA COUNTY: Osceola County is a 1,506 square mile area that serves as the south/ central boundary of the Central Florida Region and the Greater Metropolitan Area. Osceola's economic base is dominated by tourism, serving as a "gateway" to Disney World and other Central Florida attractions.
The Osceola County Animal Services Department is an “Open Access” shelter with managed intake and the only shelter in Osceola County, serving almost 400,000 residents. It provides medical care, shelter and adoption services for a variety of animals. Reporting to the Director of Animal Services, the Animal Services Veterinarian is quite unique in that it provides the opportunity for a DVM to provide care for a large variety of animals not just cats and dogs. The Shelter is held in high regard within the community and supported by more than 100 volunteers currently. This position has three support staff members. Requires the appropriate education, certification and experience combination. If the successful candidate is licensed out of state, the Director will allow up to six months for Florida testing and licensing to be obtained.
Salary range: $95,929.60 to $139,110.40 plus sign on bonus
Please apply on-line by April 29, 2022 at www. allianceRC.com. For questions, contact David McDonald at dmcdonald@alliancerc.com or Sherrill Uyeda at suyeda@alliancerc.com or (562) 901-0769. EEO/ADA.

PRACTICE FOR SALE/LEASE
PRACTICE FOR SALE-NORTH PALM BEACH COUNTY: Solo practitioner in a very busy small animal practice. Affluent North Palm Beach County community. Upscale clientele. Major urban thoroughfare with great visibility. Grossed $650K in 2021. Easily 1.5 vet practice. Huge upscale potential. Be your own boss. Control your own destiny. Asking $395K. Contact Dr. Bob Miles at (561) 379-8748 (cell) or crbobmiles@aol.com
Florida Practices for Sale
BREVARD COUNTY (Listing FL116)
Small animal practice with gross revenue over $1.12M. Up 9% through June 2022! Beautiful real estate is included. Seller transition of 2 years.
PINELLAS COUNTY (Listing FL111)
Small animal practice with gross revenue over $1.73M. Average annual growth rate over 8%!
1,942 SF facility with 2 exam rooms. Real estate is included.
psbroker.com | 800.636.4740 | info@psbroker.com
Veterinary Practice Sales & Valuations
PS Broker has more listings available Nationwide! 38 | FVMA Advocate
agreeable sc hedule.






New- SE Florida -Currently solo Dr. grossed $1.5M in 2021, upscale lease s pace w/5 exam rooms, plenty of growth potential, owner willing to stay on for a period of time.


New- SW Florida Coast- 1.25 Dr. grossed $1.26M in 2021, very nice location, well equipped, Prx and RE av ailable.
New- Greater Orlando area- Solo Dr. grossed $925K in 2021, well established, well equipped, Prx. and RE available.

S W Florida Coast- Solo Dr. small animal with a beautiful 4 exam room hospital. 2021 gross revenue ~$875K-Great location, well equipped, after debt inco m e of about $200K
























North-Central Fl. -Solo Dr. 202 1 gross $1. 6 M s till growing, everything you need make a great living. Motivated Seller!!

Central Fl. -Equine Pr actice Unique Opportunity 1 Dr. Hospital barn, treatment area, surgical suite, equipped trucks... 2021 gross $690K Could easily convert facility to small animal clinic.






When Selling or Buying a Veterinary Practice... The only Veterinary Practice Broker Solely Focused on Florida! Showcase Properties of Central Florida Inc. Richard Alker, DVM Florida Representative 850.814.9962 e-mail: Richard@TPSGSales.com www.TotalPracticeSolutionsGroup.com Practice Sales Buyer Representation Associate Buy-Ins Exit Strategies Appraisals Call on
Price Reduction as of April
Solo Dr. grossing $1.1M, 2 exam rooms,
$ 215 K. Owner will stay with
New
2022- Coastal Panhandle- -
tenured staff, ADI
mutually




PRSRT STD U.S. Postage PAID Orlando, FL Permit #793 Florida Veterinary Medical Association 7207 Monetary Drive Orlando, FL 32809 Practice Gross Revenue $2.9M $1 4M $4 7M $1 3M $2 7M $5 3M $3 1M $10.5M $3.8M $14.5M $4M $11.2M $13.5M $15.2M Practice Sales Price Your exit can be LIFE CHANGING. Ask us how Recent Transactions Sold: Doyle Watson, DVM 800.333.1984 ▪ www.simmonsinc.com southeast@simmonsinc.com S i m m o n s & A s s o c i a t e s S o u t h e a s t , I n c . Licensed real estate broker in FL, GA, SC & NC p r a c t i c e s a l e s ▪ p r a c t i c e a p p r a i s a l s ▪ b u y e r a g e n c y ▪ s a l e f a c i l i t a t i o n ▪ e x i t s t r a t e g y Contact us for a complimentary and confidential conversation.














 8 Representative
1
2
5
7
District 3 Representative Dr. Todd Fulton
District 4 Representative Dr. Donald S. Howell
DISTRICT 8 NORTHWEST
DISTRICT 1 BIG BEND
DISTRICT 2 NORTHEAST
DISTRICT 5 TREASURE COAST
DISTRICT 6 SOUTH FLORIDA
DISTRICT 7 SOUTHWEST
DISTRICT 3
CENTRAL
DISTRICT 4 TAMPA BAY
FVMA DISTRICTS
8 Representative
1
2
5
7
District 3 Representative Dr. Todd Fulton
District 4 Representative Dr. Donald S. Howell
DISTRICT 8 NORTHWEST
DISTRICT 1 BIG BEND
DISTRICT 2 NORTHEAST
DISTRICT 5 TREASURE COAST
DISTRICT 6 SOUTH FLORIDA
DISTRICT 7 SOUTHWEST
DISTRICT 3
CENTRAL
DISTRICT 4 TAMPA BAY
FVMA DISTRICTS






 Dr. Bieck, his son Noah and his wife Jenny.
Above: Dr. Bieck pictured in Mongolia. Opposite: Dr. Bieck pictured with his dogs after arriving home in Des Moines following his mission in Mongolia.
Dr. Bieck, his son Noah and his wife Jenny.
Above: Dr. Bieck pictured in Mongolia. Opposite: Dr. Bieck pictured with his dogs after arriving home in Des Moines following his mission in Mongolia.









 Image courtesy of Canva.
Michael Schaer, DVM, DACVIM, ACVECC
Cory Woliver, DVM
Ashley E. Allen-Durrance, DVM, DACVECC
Image courtesy of Canva.
Michael Schaer, DVM, DACVIM, ACVECC
Cory Woliver, DVM
Ashley E. Allen-Durrance, DVM, DACVECC













 Michael H. Jaffe, DVM, MS, CCRP, DACVS
Michael H. Jaffe, DVM, MS, CCRP, DACVS



 MICHAEL H. JAFFE DVM, MS, CCRP, DACVS
Landmarks for performing a tibial thrust test in dogs with a suspected cranial cruciate ligament rupture include placing your finger from the patella to the tibial tuberosity with the leg maintained at a normal standing angle. By flexing the tarsus in dogs with a cranial cruciate ligament injury, the examiner’s fingertip on the tibial tuberosity will be thrust forward.
Image courtesy of Dr. Michael Jaffe.
MICHAEL H. JAFFE DVM, MS, CCRP, DACVS
Landmarks for performing a tibial thrust test in dogs with a suspected cranial cruciate ligament rupture include placing your finger from the patella to the tibial tuberosity with the leg maintained at a normal standing angle. By flexing the tarsus in dogs with a cranial cruciate ligament injury, the examiner’s fingertip on the tibial tuberosity will be thrust forward.
Image courtesy of Dr. Michael Jaffe.



































 Image courtesy of Shutterstock
Image courtesy of Shutterstock