QUARTERLY BULLETIN

Frontier Celebrates 100 th Anniversary of Its Inception


Frontier Celebrates 100 th Anniversary of Its Inception
By making a recurring gift to FNU, you are investing in the lives of Frontier students year-round. Giving monthly represents an ongoing commitment to Frontier Nursing University and student achievement. When you commit to even $5 per month, your gift will help with student scholarships, DEI programming, hands-on training materials, and so much more.

12
12
Visit frontier.edu/give-to-fnu/, use the enclosed remittance envelope, or scan the QR code above to make your first monthly gift today!



Glossary of Credential Abbreviations
In the Quarterly Bulletin, we often list the abbreviated credentials of the healthcare professionals featured in these stories. While space does not permit a comprehensive list of all these credentials, here are a few of the more common ones used in the Quarterly Bulletin and their meanings:
CNEP: Community Based Nurse-Midwifery Education Program
CNM: Certified Nurse-Midwife
DNP: Doctor of Nursing Practice
FNP: Family Nurse Practitioner
MSN: Master of Science in Nursing
PMHNP: Psychiatric-Mental Health Nurse Practitioner
WHNP: Women’s Health Nurse Practitioner
Frontier Nursing University Quarterly Bulletin, ISSN 0016-2116, Copyright © 2025 by Frontier Nursing University, is published quarterly by Frontier Nursing University, 2050 Lexington Road, Versailles, KY 40383. Business and Editorial Offices: 2050 Lexington Road, Versailles, KY 43083. Accounting and Circulation Offices: Frontier Nursing University, 2050 Lexington Road, Versailles, KY 43083. Periodicals postage is paid at Versailles, KY, and additional mailing offices (if applicable).
Brooke A. Flinders, DNP, RN, APRN-CNM, FACNM President
Shelley Aldridge, BA Chief Operations Officer
Paula Alexander-Delpech, Ph.D., PMHNP-BC, APRN, Dean of Inclusive Excellence and Student Success
Marc Blevins, MS, CISA
Chief Information and Digital Officer
Dr. Diane John, PhD, ARNP, FNP-BC, CNE
Interim Dean of Nursing
Bobbi Silver Chief Advancement Officer
Kylie Waters, CPA, MBA Chief Financial Officer
Jenkins Michelle Lawhorn, DNP, CNM, RNC-OB, Regional Clinical Faculty (faculty representative)
Chris Turley, MS, BS, Diversity, Equity, and Inclusion Coordinator (staff representative)
Academic Administration
Audra Cave, DNP, FNP-BC Department Chair
Family Nursing
Khara’ Jefferson, DNP, APRN, FNP-C DNP Director
Rachel Risner, Ph.D., DNP, APRN, C-FNP, CNE
Associate Dean of Academic Affairs
Kevin Scalf, DNP, APRN, PMHNP-BC, CNEcl, Department Chair of PsychiatricMental Health
Eileen Thrower, Ph.D., APRN, CNM, CNE, FACNM
Department Chair of Midwifery and Women’s Health

Dear Friends,
It’s a New Year’s tradition to make a resolution, usually related to self-improvement or achievement. For those who take these resolutions seriously, it is generally a very personal and often challenging task, but one worth dedicating a year to.
In 2025, FNU has plenty of goals and objectives – our resolutions, you might say:
• We are conducting a national search for our new Dean of Nursing following Dr. Joan Slager’s remarkable eight-year tenure as our dean.
• We are entering into a year-long strategic planning process to help frame our next three years.
• We are looking forward to opportunities to better serve our students and to expand the reach of advanced practice nurses and nursemidwives.
In addition to our resolutions, we are celebrating! Why? Here are a few reasons:
• 2025 is the 100th anniversary of the inception of the Frontier Nursing Service.
• We began the year with students of color representing a record-high 32.3% of our total enrollment.
• We are establishing a Frontier Nursing University Alumni Hall of Fame, with the first inductees being honored in September.
• In July, we will host our 15th annual Diversity Impact Conference
• We are touring the country – and beyond – with a cruise and multiple events with our alumni and friends.
As you can see, this is a special year at Frontier. We cherish this opportunity to look back at the past century and reflect on our journey and the mission that continues to guide us. We are so grateful to have such a connected and supportive community. We can’t wait to celebrate with you!
Sincerely,
Dr. Brooke A. Flinders DNP, RN, APRN-CNM, FACNM

Throughout 2025, Frontier Nursing University is celebrating the 100th anniversary of the inception of the Frontier Nursing Service (FNS). Founded as the Mary Breckinridge Kentucky Committee for Mothers and Babies in 1925, the organization was renamed the Frontier Nursing Service in 1928.
In 1928, the Hyden (Kentucky) Hospital opened as FNS became the first organization in America to use nurses trained as midwives under the direction of a single physician. That same year, the FNS Courier program began. The Couriers assisted nurses with everyday chores such as delivering supplies to the clinics and caring for the horses that the nurses used to traverse the mountains to reach the women and children in their care. In 1933, Metropolitan Life Insurance Company published a summary of the first 1,000 FNS births. The summary concluded that the services provided by FNS significantly decrease maternal and neonatal mortality.
The Frontier Graduate School of Midwifery, since renamed Frontier Nursing University, was founded in 1939 by FNS as a part of its demonstration project in the care of the mother and child in rural areas of Kentucky. Frontier has over 10,000 alumni from all 50 states and a current enrollment of 2,700 students.
“We are so excited to celebrate the incredible and impactful 100-year history of Frontier,” said FNU President Dr. Brooke A. Flinders. “This is a great opportunity to reflect on how we got here and be reminded of the importance of the work we are doing to educate and prepare nurse-midwives and nurse practitioners to improve the healthcare in their communities across the country.”
FNU’s celebratory plans include an “Alumni & Friends” cruise in April and a nationwide presidential tour where alumni, students, and supporters can meet Dr. Flinders. FNU is also introducing a new series called “On the Trail.” This series of videos, which will be on FNU’s YouTube page, will take viewers behind the scenes for Frontier.
In September, FNU will induct its first Alumni Hall of Fame class and announce its annual service award recipients during commencement weekend.
The year-long celebration has already begun with the university’s “Century of Stories.” These stories will be posted throughout the year on the Frontier.edu website and feature the people, moments, initiatives, and stories that shaped Frontier’s first 100 years.
2025 marks the 100th anniversary of the inception of the Frontier Nursing Service. We are celebrating by capturing and sharing many of the countless stories that make up our history. Whatever your connection to FNU, we want to hear your FNU story.
Please scan the QR code to share your story and help us celebrate all FNU has accomplished.

Throughout 2025, FNU President, Dr. Brooke A. Flinders will visit regions across the U.S. to meet with the Frontier community. Watch your email or visit Frontier.edu for more information about these tour stops:
February 17-21: Georgia, North Carolina, and South Carolina
April 14-17: Florida and the Alumni and Friends Cruise
June 23-27: Northern California, Oregon, and Washington
August 11-15: New York and Pennsylvania
October 20-24: Washington, D.C., Virginia, and Maryland
December 8-12: Illinois and Indiana



Frontier is excited to introduce a new series called “On the Trail with Frontier Nursing University.” This video series takes you behind the scenes of Frontier, whether we are on campus in Versailles, Kentucky, or on the road meeting with graduates in their home communities.
This series is designed to foster connections and engage others, highlighting nursemidwives, nurse practitioners, and all our community members' impact on health care nationwide.
New episodes will be released every other month. You can watch the series on
FNU’s YouTube page and our social media channels.
On Thursday, September 25, 2025, Frontier Nursing University will induct its first Alumni Hall of Fame members. The FNU Alumni Hall of Fame is being created to celebrate and recognize the incredible individuals whose contributions have influenced and formed the university's past, present, and future success.
In addition to the Alumni Hall of Fame induction ceremony, FNU will honor its

On January 1, 2025, Frontier Nursing University lost a special member of the FNU family when Christian Graham passed away suddenly. Christian served as an Academic Advisor at FNU beginning in March 2024, and in that time, he touched the lives of so many with his kindness and dedication. His loss is deeply felt by the students he served and everyone who had the privilege of working with him.
annual Service Award Winners as part of the many events leading up to commencement on Saturday, September 27.
The Distinguished Service to Society Award recognizes a graduate who goes above and beyond to provide exceptional service in their communities.
The Distinguished Service to Alma Mater Award honors a graduate who has supported Frontier through volunteer efforts and/or donor support.
The Distinguished Preceptor Award recognizes a graduate who has provided
Though his time at Frontier was short, it did not take long for Christian to make a lasting impact. To help honor his life, his work, and the joy he brought to his coworkers and the students he served, Frontier will place a memorial bench in front of the Student Services building on the FNU campus. We hope to raise $2,500 from the FNU community to help pay for this bench in honor of Christian. You can support this effort by visiting Frontier.edu/give and selecting “Christian Graham Memorial” in the gift designation drop-down menu.
Christian was born in Richmond, Kentucky, on February 16th, 1990, and graduated from the University of Louisville. In addition to his work at Frontier, he also worked as an instructor at Kentucky State University. He had a passion for education and serving others.
His father-in-law, Robby Morton, was also an academic advisor at Frontier. We grieve for Robby, Christian’s friends, and family, including his daughter Chance.
Thank you for helping us ensure that Christian’s memory will live forever at FNU.
long-standing support and commitment to the mission and work of Frontier Nursing Service and Frontier Nursing University by precepting students.
The Unbridled Spirit Award honors a former Courier dedicated to serving others, who has ongoing, long-standing stewardship of Frontier, and has demonstrated conviction, courage, and a zest for adventure.
The Lifetime Service Award recognizes an individual or organization providing long-standing support and commitment to the mission and work of Frontier Nursing Service and Frontier Nursing University.

We are heartbroken to share that FNU PMHNP student Evan Giblin passed away unexpectedly on February 6, 2025. Evan was on track to complete his program in the summer of 2025. He sadly leaves behind his wife Skylar, who, at the time of the production of this issue, was expecting their first child.
Scan the QR code to support Evan’s family.

Effective March 1, FNU named Dr. Diane John, PhD, ARNP, FNP-BC, CNE, as the Interim Dean of Nursing in the wake of former Dean Dr. Joan Slager’s retirement.
Dr. John is a board-certified Family Nurse Practitioner and Associate Professor. She earned a doctoral degree (PhD) from Barry University and a master’s degree from Florida Atlantic University. She has spent

Frontier Nursing University announced in December that Kylie Waters, CPA, MBA, is the university’s new Chief Financial Officer. Waters has over 20 years of financial leadership experience in healthcare and academic settings, including positions as Chief Financial Officer and Vice President of Finance.
Waters obtained her Bachelor of Science in Accounting from the University of Kentucky and Master of Business
over 40 years in the nursing profession, including more than 20 years in academia.
Dr. John joined FNU as faculty in 2012 and has served as curriculum and course design coach, committee member/leader, and mentor for faculty and students. Her contributions to the nursing profession include scholarly presentations and publications, and she has served as a grant reviewer for numerous HRSA (federal grants). Her focus has been and remains on health promotion, cardiovascular health, epidemiology, intimate partner violence, and other topics.
Dr. John has served as program director for an entry-level BSN program and program director for an RN-BSN program. As a nurse educator and community advocate,
she founded Independent Nurse Providers (INP), a for-profit organization supported by advanced practice nurses who provide healthcare and education for local organizations. She has received meaningful grant funding to engage, educate, and support the community.
Dr. John worked with Dr. Slager throughout January and February to ensure a seamless transition.
Administration from Morehead State University.
“We are thrilled to welcome Kylie Waters to Frontier Nursing University,” said FNU President Dr. Brooke A. Flinders. “Her impressive education and experience, particularly in academic and healthcare settings, makes her well qualified to direct the university’s financial management.”
Waters has additional experience as a Certified Public Accountant for PricewaterhouseCoopers, LLP and Dean Dorton, PLLC. She has taught accounting as an instructor and has published in the Journal of Nursing Home Research and Long-Term Care Management.
“My family originates from McCreary and Perry counties, and I am proud to join Frontier Nursing University,” Waters said. “It is an honor to be part of a mission-driven institution doing important work impacting healthcare in underserved communities nationwide.”
Frontier Nursing University (FNU) announced two new members of the university’s President’s Cabinet. FNU Regional Clinical Faculty (RCF) Jenkins Michelle Lawhorn, DNP, CNM, RNC-OB, and Diversity, Equity, and Inclusion (DEI) Coordinator Chris Turley, MS, BS, will serve on the President’s Cabinet throughout 2025.
FNU’s President’s Cabinet collaborates with the Board of Directors and university leadership to offer internal guidance and expertise on initiatives, policies, and operations that support FNU’s mission, vision, and culture of caring. To expand diverse perspectives within the Cabinet, FNU adds two members on a rotating basis, one faculty and one staff member, to serve for a one-year term. Nomination and selection criteria prioritize candidates capable of offering insights currently underrepresented within the Cabinet. Dr. Lawhorn and Turley will also be mentored by the members of the President’s Cabinet throughout the year, facilitating transparency and education about how leadership decisions are made.
Dr. Lawhorn is a two-time FNU graduate, obtaining a Master of Science in Nursing with an emphasis in midwifery and a Doctor of Nursing Practice. A graduate of Clemson University, she holds additional certifications in inpatient obstetrics nursing and electronic fetal monitoring.
In addition to serving as a faculty member, Lawhorn continues to practice as a nurse-midwife at the University of North Carolina Health. She provides full-scope midwifery care in both the community and hospital settings.
“As a former student, current preceptor, and faculty member at Frontier Nursing University, I hope to share my viewpoint based on my diverse connections with the university to help influence future decision-making,” Dr. Lawhorn said. “As an FNU Student Mentor, Student Interest Group Advisor, and Clinical Bound Team Lead, I plan to bring the transparent voice of our students to the Cabinet since they are the ones we serve. As a young faculty member, I would love to witness multiple leaders in action and learn from their complementary styles, strengthening my leadership style and skills."


Dr. Jenkins Michelle Lawhorn Chris Turley
DEI Coordinator Chris Turley joined FNU in May 2019. He holds a Master of Science in Sports Administration and a Bachelor of Science in Sports Management from Eastern Kentucky University. Chris has over ten years of experience with federal grant management, program development, and marketing.
Turley earned the governor's prestigious designation of a “Kentucky Colonel” for his community engagement work. He developed programs to help over 2,500 At-Promise participants gain vocational/technical skills to advance their careers and expand their opportunities.
While at Frontier, Turley has been instrumental in the execution of the Diversity Impact Conference, the quarterly speaker series, and in facilitating federal grant scholarship and stipend programs. He completed the inaugural DEI staff ambassador program at FNU. He has co-chaired the faculty/staff council and the Mission and Philosophy committee. Currently, he is the chair of the Diversity Impact Planning Ad-hoc Committee and serves on the Culture of Caring and the Diversity, Equity, Inclusion, and Belonging committees.
Turley has a strong base dealing with issues concerning race relations, as he had to deal with similar problems growing up in a marginalized communwity in Kentucky. He was a part of a task force that dealt with those issues in a small hometown in Kentucky. This was the first of many steps into educating and empowering others regarding diversity and inclusion.
“As a staff member in the Office of Diversity, Equity, and Inclusion at Frontier Nursing University, I hope to bring my shared professional and life experiences and diverse connections with FNU to help influence future policies and decision-making from the President’s Cabinet,” Turley said. “As an FNU DEI staff ambassador and DEI professional, I plan to be a voice for continued growth in diversity, equity, and inclusion for our students, faculty, and staff at the university.”
With their extensive backgrounds, these new President’s Cabinet members will help provide perspective and emphasize DEI initiatives and goals.

• Help expand access to quality, compassionate care to diverse, rural, and underserved populations.
• Earn an honorarium based on the percentage of time spent precepting students.
• Gain access to FREE CEUs, including sessions on pharmacology and other current topics.
• Promote your profession through the education and guidance of your future peers.
• Gain access to the latest clinical guidelines to stay current in practice.
• Earn a 10% discount on all non-matriculating courses at FNU.
• In 2024, a total of 1,442 FNU students worked with 4,312 preceptors.
• The average FNU student needs three clinical sites to complete all required experiences.
• The need is great, and the competition for clinical sites is heavy.
• The demand for preceptors is constant.
You saw it on the cover of this issue of the Quarterly Bulletin – “The Gift of Precepting.” It’s a phrase we use often at Frontier Nursing University, and while its meaning might seem straightforward enough, there is significant nuance in those words.
The word “gift” implies that someone is giving and someone is receiving. In the case of precepting, however, both the preceptor and the preceptee give and receive.
The gift made by the preceptor is relatively apparent. The preceptor gives the student the gifts of their time, expertise, experience, and wisdom.
Seeing the student’s passion for continued growth and learning is no small gift in return, but there’s more to it than that. Preceptors often find that, in addition to the good vibes that come from giving back to the profession, precepting also comes with some unexpected gifts.
We all find ourselves in a rut at times. A student's excitement and unique perspective can be a sorely needed injection of energy. Fresh from their studies, students can also offer up-to-date knowledge and information. And in some cases, the right student might just become the new full-time member your team was looking for.
The two-way transaction between preceptor and student bears yet another gift – the most important if you think about it. As a preceptor, you represent the final step as the student prepares for a new role as an advanced practitioner. That means the gift of better healthcare for their patients and their communities.
That is truly a gift that keeps on giving. That’s why we celebrate our preceptors annually in the Quarterly Bulletin and with our Preceptor Celebration Week. We are so grateful for the countless preceptors who have shared their time and expertise.
We hope the stories, data, and information in the following pages inspire everyone to consider precepting. Please join us in experiencing the joy of giving and receiving the gift of precepting.
Sincerely,
Dr. Diane John, PhD, ARNP, FNP-BC, CNE Interim Dean of Nursing
We surveyed our preceptors from the past year, and they told us about their experience as preceptors for FNU students. Total respondents: 621
Please let us know why you chose to precept FNU student(s) (choose all that apply):

Responses Iwanttogivebacktomyprofessionthroughtheeducationandguidanceofmyfuturepeers.Iwanttohelpexpandaccesstoquality, compassionate care,toruralandunderservedpopulations.Iwanttoearnanhonorariumbaseduponthe percentageoftimeIspendpreceptingstudents.IwanttogainaccesstofreeCEUs.IwanttoremainanactivepartoftheFNUcommunityanditsrichlegacy.Itisawaytoreceivecredittowardmyrecertification. Itisanexpectationofmyemployer.Other(pleasespecify)
How likely will you serve as a Preceptor for an FNU student again?
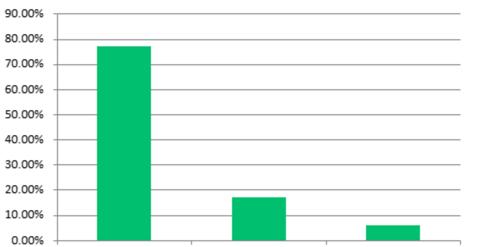
Do you feel supported by FNU if you have concerns or issues while precepting?
How satisfied were you with your experience as a Preceptor for an FNU student?

Responses
How satisfied are you with the ease of completing the MidCourse Development Assessment Tool (MDAT)/ End of Course Development Assessment Tool (EDAT)?
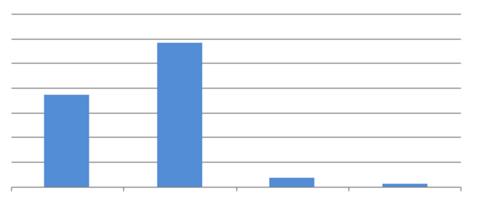
Responses
This activity is approved for six contact hour(s) of continuing education (which includes 0 hour(s) of pharmacology) by Frontier Nursing University. Activity ID 2502-001. This activity was planned in accordance with ANCC Commission on Accreditation Standards and Policies.
This course will provide the participant with information about the roles, responsibilities and expectations of the clinical preceptor in guiding and mentoring advanced practice nursing students in a variety of settings. It is divided into small segments to allow for learning at your own pace.
Integrating the Community of Inquiry theoretical framework, participants will explore teaching learning strategies that address adult learners, learn ways to create high-quality clinical experiences incorporating diversity, the existence of bias, and attention to techniques to assess student readiness to engage in clinical learning. Ways to effectively manage the clinical learning environment and evaluate student achievement of objectives will also be discussed. Legal and ethical issues regarding student and patient confidentiality that need to be considered when providing clinical learning experiences will be addressed.

1. Explain the roles and responsibilities of the clinical preceptor.
2. Apply evidence-based strategies to the preceptor role.
3. Integrate the three presences of the Community of Inquiry as a model for Nurse Practitioner students to meet Nurse Practitioner Core Competencies and role transition.
4. Incorporate knowledge of learning styles and adult learning principles to facilitate, instruct, model, and encourage student learning in the clinical setting.
5. Summarize the use of assessment methods, including direct observation, formative and summative assessments, and actionable feedback to guide student learning.
6. Recognize legal and ethical issues and constraints that impact the clinical learning environment.
7. Cultivate an environment that facilitates student role transition from RN to APRN through role modeling, coaching, and mentorship that focuses on APRN professional roles, values, and relationships within and outside of the profession.
8. Discuss factors that contribute to an effective and secure learning environment in the clinical setting that consider personal/cultural factors, bias, and inclusivity.
9. Examine methods of clinical student evaluation, including psychomotor skills, therapeutic interventions, and APRN role development.
Scan to visit the Gift of Precepting CE page.
10. Explore effective strategies for problem-solving in the clinical setting, including preventing potential problems, problem identification, and interventions.

“Despite juggling many responsibilities to address the healthcare needs of her local community, Michelle Quale, FNP, CNM, dedicates time to mentoring the next generation of healthcare professionals through precepting. She has mentored several Frontier Nursing University students throughout the years.
A resident of Glencoe, Minnesota, Quale serves as a family nurse practitioner and certified nurse-midwife with Glencoe Regional Health, working with a rural population. Her multifaceted role encompasses family practice, birth center, wound center, urgent care, hospitalist duties, and even providing healthcare services to the local jail.
With several years of experience in precepting, Quale has become a guiding force for numerous FNU students. For Quale, precepting is not just about imparting knowledge; it’s a journey of mutual learning. She said the students' enthusiasm fuels her passion for continuous growth and development.
“It facilitates our own learning,” she said.
April Trebelhorn, a colleague of Quale, credited her for playing a crucial role in encouraging her to step out of her comfort zone and pursue the essential steps for professional growth.
“Michelle has been an amazing preceptor and role model for me. She is compassionate, organized, has amazing attention to detail, and is a down to earth provider that her patients trust and connect with,” she said. “She has tremendous patience. I admire the time she spent with me explaining and answering questions. She pushed me to be the best version of myself and get out of my comfort zone, which ended in me feeling more comfortable with my next chapter of becoming a nurse practitioner. I will forever be grateful for her shared compassion and knowledge.”

Dr. Jennifer Carter, DNP, WHNP, earned her MSN and DNP from FNU. With over six years of experience as a preceptor, she is committed to educating future nurse practitioners while serving her patients and community.
“Being a preceptor allows me to grow in my own practice and encourages me to continue to study and be the best Nurse Practitioner I can be,” she said. “I find myself learning from the students through their experiences and study of current practice.”
A resident of Greenville, Texas, Dr. Carter serves as a WHNP with Zapata Women’s Health in Greenville. Working in a predominantly rural area, Dr. Carter cares for women from all socioeconomic backgrounds in her practice, and her patients range from menarche through menopause. A day in her clinic may include educating young teens about birth control, managing ante and postpartum care, advising on hormone replacement therapy, and addressing gynecological issues in elderly patients.
Throughout her precepting journey, Dr. Carter has had the opportunity to mentor two FNU students. She said her passion for teaching strongly influenced her decision to become a preceptor.
“I have a strong desire to instill good practice habits in future nurse practitioners and to help them build confidence in patient care,” she said.
Over the years, Dr. Carter said she has realized that the joy of precepting lies in building relationships.
“I enjoy building friendships with the students and watching them interact with the patients and develop their own relationships with the patients and their families,” she said. “Being a preceptor is definitely a commitment of time and energy, but it is well worth it to be able to impart your knowledge and experience on the future of healthcare.”
Jessica VanScoyoc, a former student under Dr. Carter’s mentorship, said she was provided with a learning environment where she felt empowered to grow in her skillset.
“She encouraged me to be hands-on right away and her teaching style allowed me to increase my confidence as a future WHNP,” VanScoyoc said.

After many years of compassionately serving patients as a Certified Nurse-Midwife (CNM) and educating nursing students and new nurses, FNU graduate Alneader (Neada) KennerWoodard recently started precepting nurse-midwifery students. Her first was FNU student Valrie Haye-Smith.
As a registered nurse, Kenner-Woodard has been able to precept new nurses in the labor and delivery department. Later, as a nursing professor, she guided and supported nursing students as they pursued their licenses. When she was approached by Haye-Smith, she realized that precepting nurse-midwifery students was the next logical step in her nursing journey.
“A deep passion for nursing education and mentorship has consistently driven me,” she said. “I am committed to sharing my knowledge, empowering others, and contributing to advancing the nursing profession.”
Kenner-Woodard works with Riverside Regional Medical Center in Newport News, Virginia. In her role, she provides patient-centered, holistic care for women throughout all stages of life. After earning a Bachelor of Science in Biology from Old Dominion University and her Associate of Applied Science in Nursing from Riverside College of Health Careers, Neada earned a Master of Science in Nursing in Nurse-Midwifery from FNU. She is certified by the American Midwifery Certification Board.
Although Kenner-Woodard has been a midwife since 2016, she said she was initially unsure about her ability to serve as a preceptor for student nurse-midwives. However, she said her education at FNU motivated her to mentor Haye-Smith.
“Throughout my midwifery education, Frontier emphasized the importance of fostering midwifery excellence and contributing to the growth of the profession,” she said. “I am glad that I was able to do my part in upholding that mission, and I look forward to serving again in the future.”
As a preceptor, Kenner-Woodard said she derives great pleasure from understanding her students and helping them grow into who they aspire to be. She said this mutually beneficial connection fosters personal and professional development for both parties.
“By assisting Valrie in honing her midwifery abilities and clinical judgment, I was able to make a lasting impact on her midwifery philosophy that will influence how she interacts with and cares for her patients,” she said. “Simultaneously, I enhanced my leadership, communication, and critical thinking skills by determining the best ways to support her.”
Kenner-Woodard said precepting is not just about helping one student but the entire future of the midwifery profession.
“Each student you guide will carry a piece of your philosophy with them, which means that your unique approach to midwifery is reaching more women who need it,” she said. “Although it can be challenging at times, the impact you have on both your students and the families they serve makes it all worthwhile.”
While serving as a preceptor for Haye-Smith, Kenner-Woodard said she received invaluable support from FNU faculty member Liz Niederegger. According to Niederegger, Kenner-Woodard strives to form respectful, therapeutic relationships with her patients, and she effectively passed on these values in precepting her first nursemidwifery student.
“This student needed a dedicated, driven, kind, compassionate, and persistent preceptor that could meet her where she was and allow her to truly find herself and blossom into the midwife she will be,” Niederegger said. “The transformation of this student has been miraculous, and I believe Neada deserves credit and recognition for every moment of effort.”

Frontier Nursing University graduate Bailey Desin, PMHNP, FNP, has been instrumental in helping FNU students grow into confident and skilled practitioners. Working at Mission Health’s Sweeten Creek Mental Health and Wellness Center in Asheville, North Carolina, Desin regularly precepts students in a demanding psychiatric setting, providing them with invaluable hands-on experience in both acute and outpatient care.
Desin is the first psychiatric-mental health nurse practitioner (PMHNP) to work in this acute environment at Mission Hospital, where she primarily manages the acute stabilization unit and covers various other units as needed. Her adaptability, willingness to mentor, and focus on patient-centered care make her an essential part of her team.
Desin has already precepted five Frontier students, demonstrating her dedication to paying it forward by investing in the next generation of nurse practitioners. Her passion for supporting students extends beyond clinical teaching—she seeks to instill confidence and practical skills they can carry into their careers.
Desin earned a Master of Science in Nursing in Frontier’s Family Nurse Practitioner program and a post-graduate certificate with a PMHNP specialization. She also holds a Master’s in Nursing Education, emphasizing her commitment to continuous learning and professional development.
“Offering students a clinical experience is rewarding and helps maintain up-to-date practice,” she said. “I like to give back to my alma mater and provide students with a unique psychiatric clinical experience.”
FNU student Eric Dunn said Desin’s enthusiasm for her alma mater and willingness to take on challenging roles underscores her dedication to advancing the NP profession.
“Bailey has been wonderful to work with, and I’ve learned so much from our time together,” Dunn said. “She’s also enthusiastic about being a Frontier alum and precepting its students.”
“I enjoyed my time as a preceptor. It is a joy to see the student’s progress from beginning to end.”
“The FNU student was very well prepared for her clinical experience and very professional. She was excellent in her ability to learn and interact. This process was enjoyable for me, and it was easy to use the evaluation site.”
“I enjoyed my time as a Preceptor for Frontier Nursing University and look forward to having local students at our office in the future.”
“I've enjoyed precepting FNU students. They are well prepared and very collegial.”
“I greatly enjoy precepting Frontier midwifery students. They are always a joy to work with.”
“I am always happy to precept with Frontier. The regular emails of gratitude for precepting are appreciated, and the access to CEUs is wonderful!”
“It is a pleasure to serve as a preceptor for the nurse practitioner students. I hope they come away with valuable information to make their practice successful.”
• Nurse-Midwife
• Family Nurse Practitioner
• Women’s Health Care Nurse Practitioner
• Psychiatric-Mental Health Nurse Practitioner
FNU needs preceptors with the following credentials and qualifications:
• Valid, unencumbered U.S. license to practice required
• One year of relevant experience in an advanced practice role
• Master’s Degree or higher in nursing related field (we do allow BSN for midwives, but an MSN is preferred)
• MDs and DOs (clinical time % based upon program)
• For PMHNP students: therapists with a master’s degree and licensure in the state of practice
To learn more about precepting, contact The FNU Department of Clinical Outreach and Placement. Our staff will be happy to:
• Answer questions about the process to become a preceptor
• Provide support to preceptors when using the online preceptor profile portal
• Answer questions regarding preceptor honorariums
You can reach our department via email at ClinicalAdvising@ frontier.edu

I was born in Watertown, South Dakota, but my family moved to Garden City, Kansas, when I was a baby. We later relocated to the Kansas City area, specifically Peculiar, Missouri, when I was in fifth grade. Aside from my military assignments worldwide, I have considered the Kansas City area home ever since.
My path into nursing was driven by a passion for helping others and a desire to work in a field that is both dynamic and intellectually challenging. Early on, I recognized the impact that nurses have on patient care, from bedside support to advanced practice roles. Nursing offered me the opportunity to combine clinical expertise with leadership, problem-solving, and advocacy, which ultimately led me to pursue advanced training and military service as a healthcare provider.
Shane Hagen, DNP (Class 36), is an Adult-Gerontology Acute Care Nurse Practitioner (AGACNP-BC), Family Nurse Practitioner (FNP-BC), and Major in the U.S. Army Reserves. He also owns Valor Wellness and Aesthetics in Overland Park, Kansas. He recently took the time to answer our questions about his unique and impactful life in service to others.
Shane Hagen, DNP (Class 36), AGACNP-BC, FNP-BC
Please share your education, training, and military experience.
I have completed multiple advanced degrees, including a Doctor of Nursing Practice (DNP) from Frontier Nursing University, along with dual board certifications as a Family Nurse Practitioner (FNP) and Adult-Gerontology Acute Care Nurse Practitioner (AGACNP). Additionally, I have an MSN degree with an emphasis on Nursing Education and Administration.
My education, combined with over two decades of clinical experience, has provided me with a diverse skill set that spans primary care, emergency medicine, critical care, and case management.
My military career in the U.S. Army Reserves, where I hold the rank of Major, has vastly expanded my scope of practice beyond traditional civilian settings. In combat environments, such as during my deployment to Iraq, I adapted to the Army’s evolving medical needs, providing care in high-intensity and resource-limited settings for both service members and local nationals.

The ability to think critically, act decisively, and balance both patient care and operational responsibilities has been instrumental in shaping my approach to medicine. Throughout my career, I have been fortunate to have had incredible mentors who helped me navigate the complexities of advanced practice while maintaining the highest standards of patient care.
Have you experienced any pushback from patients or colleagues as a male nurse?
I have been welcomed into this field with open arms by my peers, physicians, and patients. However, there have been occasional instances where patients have requested not to have a male nurse. I fully respect a patient’s right to request a provider of a specific gender, as much of what we do in healthcare is sensitive in nature. I believe that as long as patients receive quality care, they should have autonomy in choosing their healthcare providers.
Tell me about your current practice, scope of practice, etc.
I own Valor Wellness and Aesthetics, a practice that blends my clinical expertise, military experience, and passion for healthcare, located in Overland Park, Kansas. We offer primary care, aesthetic medicine, wellness services, and VA community partnerships for various military veteran services.
My goal was to create a practice that reflects the diverse healthcare experience I’ve gained over the years, allowing me to serve patients in multiple capacities, from preventative care to regenerative treatments.
One of the advantages of practicing in Kansas is that Nurse Practitioners have Full Practice Authority (FPA), allowing me to practice autonomously. This independence enables me to not only treat patients without physician oversight but also choose my own mentors and collaborators, fostering strong professional relationships that enhance patient care.
What are your long-term goals for yourself and your practice?
My long-term goal is to continue growing Valor Wellness and Aesthetics into a leading integrative healthcare practice, bridging the gap between traditional medicine and innovative treatments. I also remain committed to veteran advocacy, ensuring that service members receive the healthcare they deserve.
Beyond clinical practice, I am passionate about mentoring future healthcare professionals and advancing the field of nursing education. Having served as a professor and program director in multiple nursing institutions, I plan to stay engaged in shaping the next generation of nurse practitioners.
Frontier Nursing University provided me with a strong academic foundation and the practical skills necessary for both clinical practice and business ownership. The curriculum emphasized evidence-based practice, leadership, and rural healthcare, which directly translated into my ability to manage a practice, optimize patient outcomes, and navigate the complexities of independent practice. The university’s emphasis on community-focused care also reinforced my commitment to providing high-quality, patient-centered services at my clinic.
Is there anything else you would like to share?
I am incredibly grateful for the opportunities I’ve had in both civilian

and military healthcare settings. My experiences have reinforced the importance of adaptability, lifelong learning, and mentorship in shaping a successful career. Whether in a combat environment, a university classroom, or my own clinic, my goal has always been to provide exceptional care, advocate for patients, and contribute to the advancement of healthcare.
The Men in Nursing student-interest group aims to generate dialogue about professional development and leadership for male nursing students. This group, which is facilitated by faculty advisors Dr. Joshua Barnes and Dr. Thomas Gale, provides opportunities for conversation around the following aspects of males in the nursing profession:
• Facilitating professional development for men in nursing
• Discussing challenges and triumphs that males in nursing face
• Learning about strategies for success and obtaining information about key organizations for male nurses
• Facilitating strong collegial relationships between male nursing students, male nurses, and other nurses in the discipline
For more information about FNU’s Student Interest Groups, please contact the Office of Diversity, Equity, and Inclusion at Diversity-Inclusion@frontier.edu

Military personnel are known for their discipline, preparation, and commitment to service. As a former Naval Officer, Frontier Nursing University graduate Jake Mearse, CNM (Class 137), PMHNP, DNP, continues to display those same traits as he breaks down barriers in service to those in his community.
Today, Dr. Mearse is a certified nursemidwife with his own practice, offering home births and clinical care in Midway, Georgia. Being a male nurse-midwife does not make him one of a kind, but he’s in rare territory. The American Midwifery Certification Board’s Demographic Report released in January 2024 found that less than 1 percent (88 out of 14,198) of all AMCBcertified midwives identified as male. There’s no data on how many of those 88 served in the U.S. Navy for 25 years, but it’s safe to assume it is an exclusive group.
“I’m third generation Navy, so that was kind of expected almost. That’s what our family does,” said Mearse, who grew up in Bend, Oregon, and joined the Navy when he was 18. “While I was in the Navy, I got into the medical field as a Navy Hospital Corpsman and served aboard submarines mostly in that
role. Eventually, the Navy sent me to nursing school.”
The Navy’s Medical Enlisted Commissioning Program allows sailors and Marines to earn a nursing degree and become a Navy Nurse Corps Officer. Mearse utilized this opportunity to attend Hawaii Pacific University while stationed at Pearl Harbor.
“I had absolutely no interest in labor and delivery or midwifery or anything related to that,” Mearse said. “I spent most of my time as a nurse in the ER/trauma world. I loved the ER/trauma nursing. I was deployed in the Middle East a couple of times doing Mobile Trauma Bay. Once I got a commission, I worked as an RN full time.”
Mearse met his wife April in the Navy, and in 2004, they had their first child with the help of FNU graduate Michelle Munroe, DNP (Class 11), APRN, CNM, FACNM, FAAN.
“She was our midwife for two of our kids,” said Mearse, who now has seven children.
“She’s the one who talked me into becoming a midwife. She pulled me aside during a prenatal visit and said, ‘I think you might want to look into doing this. You might be good at this.’
every time you say, ‘I want to go into labor and delivery’, they say, ‘That’s very nice, you’re going back to the ER.’ So, I had to do it on my own time.”
During his last few years in the Navy, Mearse used his accrued leave time to finish his midwifery training. He then entered the Navy’s “Duty Under Instruction” program in which participants stay in active duty while pursuing a degree. He attended the University of Washington with plans to become a nurse-midwife, but the Navy approved him for the psychiatric-mental health nursing curriculum instead.

That seed that Michelle planted in my head just kept growing. Unfortunately, if you are a nurse and you’re a 6-1, 200-pound man,
“The whole time I was going through my DNP program studying psychiatric nursing, I was taking extra classes in women’s health, labor and delivery, trying to get as close into that world as I could,” Mearse said. “I wanted to be a midwife.”
Inspired by Dr. Munroe, Mearse approached FNU about enrolling in the nurse-midwifery program.
“Best decision I ever made,” Mearse said. “The biggest thing that was helpful with Frontier was the flexibility of the program. I was coming to them saying, look I’ve got my DNP in a field I don’t necessarily want to spend the rest of my life, and I’m active-duty military, so I’m going to have long stretches where I can’t do school and I’ll have to jump back into it. Frontier was the only school that said, ‘You know what, tell us what you need, and we’ll make it work.’ They were just incredible.”
Still, Mearse faced more hurdles before achieving his goal of becoming a nursemidwife. He encountered significant pushback against the idea of a man being a midwife.
“On my very first day of clinical rotations, at my first clinical site, I was with a group practice, and one of the midwives in the

group pulled me aside and said, “‘Just so you know, I don’t think men belong in midwifery. I do not want to help you.
Please don’t ask me for anything.”’ It was a little discouraging Day 1,” Mearse said. “I had a very similar experience in a midwifery job that I took. One of my new partners pulled me aside and said, ‘I am not working with you. I am offended that you’re here. I don’t believe that men belong here, and I will do anything I can to get you out of here.’”
Mearse said that the only times he has experienced such gender discrimination, it has come from colleagues, not patients. He noted that patients who asked for a different provider cited cultural or religious reasons.

primary care, including IUDs, contraception management, and colposcopies.
“For the most part, in my experience, patients don’t really care what your gender is. They just want to be taken care of,” Mearse said.
Mearse took a position at an Army hospital at Fort Stewart in southeast Georgia, and he and his family fell in love with the area. In 2002, Mearse opened Coastal Midwifery and Women’s Health, which was a success from day one.
“Before I had even advertised or even posted on social media that I would be doing home births, we started getting calls,” he said. “We got full really fast. Now we are at a point where we are having to turn moms away every month because we are full.”
Mearse strives to keep his schedule to five or fewer home births per month, and the clinic is open three days a week. At the clinic, Mearse provides full-scope gynecology and
To make access to care as convenient and accessible as possible, the clinic is open from 1:00 to 10:00 p.m.
“Our hours are based on what I remember being a dad in the military and never getting to go to appointments because all of the OB offices were always open 9-5 Monday through Friday,” Mearse said. “We decided to do things a little differently. We are open from 1 p.m. to 10 p.m., and we do two weekdays and Saturday because we really want families to be able to participate. We want to make this as family-friendly as we possibly can.”
Accordingly, running the clinic is very much a family project. Mearse’s wife, April, who is also a Navy veteran, is not medically trained but attends all the births to provide support and helps run the clinic.
“People come to the practice because they want a midwife. They stay with the practice because they meet April,” Mearse said. “Our kids are getting older now, but April is kind of the surrogate mom, especially to a lot of these young military moms who are 20, 21 years old, on the other side of the country from home. She helps set things up and take things down, but her most important role is being a hand-holder and encourager. She has that experienced mom energy where she can hold a young woman’s hand and say, ‘I’ve done this seven times. We’re going to get you through it. You’re going to be OK.’ I love the fact that a lot of our clients will text April instead of me.”
Yes, Jake and April have seven children, who are also active participants in the clinic's day-to-day operations. They strip the beds, clean, and prepare rooms for the next client. They also help interact with the other children brought into the clinic, which features separate playrooms for older and younger children.
“We’re largely a military community, and we will have moms come in for their appointment, and they’ve got other little kids and the dad’s deployed,” Mearse said. “Because we have my kids there to help, moms can feel comfortable coming into their appointment they can relax and do their appointment without worrying about what the kids are doing.”
Mearse schedules 60-minute time slots for all his patients, ensuring ample time for questions and discussions about their care.
“We want our patients to be able to ask questions and get to know us and us to get to know them,” Mearse said. “I love the fact that we have a lot of moms who will come in and just hang out in the clinic even if they’re not being seen that day. They just want to come and sit and chat and drink coffee and be there. It’s wonderful.”
As veterans, Jake and April are particularly excited to be able to offer care to a large number of military families.
“When we first started this, one of the commitments we made is that we were going to try and make this affordable for military families,” Mearse said of the military discounts offered at Coastal Midwifery and
Women’s Health. “We are just 10 minutes down the road from Fort Stewart. Even though we’re not able to do this for free for military families – I wish we could – they end up paying sometimes less than half of what they would pay elsewhere. If we’re making just enough to break even, I’m fine with that. We’re able to serve these people that are serving our country.”

Mearse hopes to be able to offer even greater access to care soon. He plans to hire another nurse-midwife as soon as she graduates.
“Right now, we are turning a number of moms away each month because we’re full, so it will be nice to be able to take more moms because there will be two of us,” Mearse said. “I’ve been on call 365 days a year for three-and-a-half years now. It will be amazing to be able to take a vacation and leave the practice in someone else’s hands for a little bit.”
“I love the fact that we have a lot of moms who will come in and just hang out in the clinic even if they’re not being seen that day.”
— Jake Mearse
Two FNU DNP students were invited to share their poster presentations at the Institute for Healthcare Improvement Forum in December. Dr. Michelle Duane,
DNP (Class 51), APRN, ANP-BC, FNPBC, AGACNP-BC, presented “Improving Patient-Center Advanced Care Planning in a Safety-Net Clinic” and Dr. Bethany Stairs,
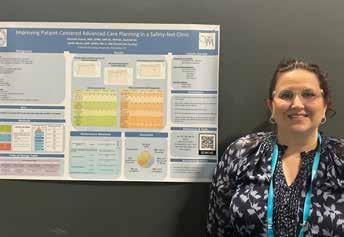
Dr. Michelle Duane
DNP (Class 51), APRN, ANP-BC, FNP-BC, AGACNP-BCP
DNP (Class 51), MBA, FNP-BC, presented “Improving Effective Risk Assessment and Colon Cancer Screening at an Urban Federally Qualified Health Center.”
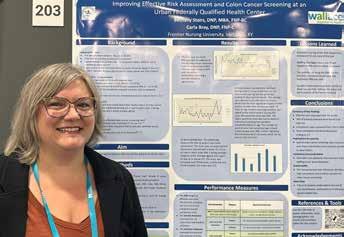
Dr. Bethany Stairs
DNP (Class 51), MBA, FNP-BC
Two FNU students in the DNP program attended the DNPs of Color Conference held in Philadelphia last October. Nina M. Brown, MSN, CNM, and Hara Oyedeji, MSN, MSEd, APRN, PMHNP-BC, attended the conference with the support of sponsorship from FNU. Afterward, both students shared written reflections on their experiences.
“It was an honor to be selected as a recipient of FNU's generous sponsorship so that I could attend this year’s conference,” Hara wrote. “The opportunity to be amongst other DNP and Doctoral level professionals provides inspiration and aspiration to continue making a difference in the nursing profession and healthcare.”
“Thank you to FNU for their support of not just my attendance but also the DOC organization,” Hara continued. “FNU continues to impress me in their efforts of allyship in the areas of DEI and ensuring that their faculty also represents those
Nina M. Brown MSN, CNM

they serve and educate. I intend to use this as a building block for my continued professional development as I would like to be in a position to present at a future DOC Conference and represent FNU. I am continuously inspired that my trajectory will eventually also lead me back into a leadership and/or faculty role after I have graduated with my DNP.”
“What initially prompted me to want to attend was the fact that I am a current DNP student and desired some motivation and encouragement to keep me going in the program,” Nina wrote. “I felt that this would be an opportunity for me to mingle with like-minded individuals who share
Hara Oyedeji MSN, MSEd, APRN, PMHNP-BC

a common goal of either seeking their doctorate in nursing or have already earned it. My journey to earning my DNP has been faced with a few obstacles along the way, one being unforeseen medical issues that I experienced in 2022, which caused me to have to take an academic hiatus as I pursued my education.”
“Being a new midwife and a full-time doctoral student has had its challenges,” Nina continued. “Being able to attend the DNP conference allowed me to find my ‘why’ again. This conference was nothing short of amazing and I consider myself blessed to have had the opportunity to share in this experience.”
In December, DNP student Alexandra Peters, DNP (Class 51) and FNU course coordinator
Ann Schaeffer, DNP, CNM, M.Ed., CNE, FACNM, received notification that their submission “Improving Effective Hypertension Management in a Rural Primary Care Clinic Using American Heart Association Guidelines" will be published in the Journal of Practical Nurse Education and Practice.
Alexandra Peters
DNP (Class 51)

Ann Schaeffer
DNP, CNM, M.Ed., CNE, FACNM

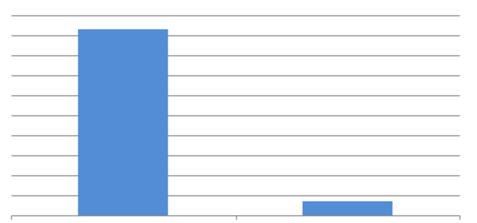
FNU recently received the American Association of Nurse Practitioners (AANP) Family Nurse Practitioner (FNP) Board Pass Rates for students who took the AANP FNP certification exam in 2024. Here is the performance breakdown:



Paula Lawrence Patricia Otis

Marli Parobek, DNP (Class 32), was named the recipient of the 2025 American Association of Nurse Practitioners (AANP) State Award for Outstanding Contributions. She was recognized for her pioneering work on Vashon Island, Washington, as the only psychiatric prescriber, for precepting students, and for contributing to the private practice of psychiatry on Vashon. In June, Dr. Parobek will receive the award at the AANP National Conference in San Diego.

Paula Lawrence, MSN, CNM (Class 73) and Patricia Otis, MSN, CNM (Class 94) are members of the nurse-midwifery team that received the Outstanding Clinical Practice Award from the American College of Nurse-Midwives (ACNM). They both practice at Bassett Medical Center in Cooperstown, New York. ACNM bases the award on the demonstration of evidencebased care, shared decision-making, individualized care, and judicious use of intervention, among other factors.

Jade Potter, MSN, WHNPBC (Class 205), IBCLC, was selected to the “Knoxville 40 Under 40” Class of 2024. The program
honors young professionals who are making significant contributions to their fields and communities in East Tennessee. Potter is the owner and founder of Milk + Honey Health, LLC, which provides lactation consultants and specialists who prepare customized plans for every family experiencing breastfeeding problems.
Karen Tepper, DNP (Class 35), was awarded the 2024 GAPNA (Gerontological Advanced Practice Nurses Association) Excellence in Clinical Practice Award. Among her routine clinical pursuits, Dr. Tepper led a Test to Treat pilot program with other leadership across the Veterans Affairs (VA) New England, VA Central Office Access to Care, and Office of Health Transformation. This model was scaled across 11 VHA Clinical Contact Centers (CCC). The CCCs differ from traditional call centers by offering multiple services through more virtual modalities, such as video visits. As the Director of the VISN 1 CCC, Dr. Tepper’s guidance yielded benefits, including earlier treatment of COVID-19, preventing cases from becoming severe, and reducing the burden on the healthcare system. Nurse practitioners served as the providers conducting virtual visits, demonstrating key roles in patient assessment, triage, treatment, and follow-up.

Robyn Weller (CNEP Class 33) was selected as the Certified Nurse-Midwife (CNM) of the Year for Kaiser Southern California Permanente Medical Group. Weller has been
a full-scope CNM with Kaiser since 2006. She also authored a book entitled Happy Mama Postpartum Self-Care.

Lori Bellwood, DNP (Class 05), CNM, recently joined Northern Light Women’s Health in Waterville, Maine. She provides gynecological, contraceptive, family planning, and preventative well-woman care from adolescence through menopause.
Buchanan Joins
Ridge Regional Hospital

Blue Ridge Regional Hospital in Spruce Pine, North Carolina, recently welcomed Dale Buchanan, DNP (Class 41), to its surgery team.
Welcomes Melanie Clark

Melanie Clark, MSN, FNP (Class 72), recently joined Gifford Health Care in Chelsea, Vermont. She is a family nurse practitioner on the primary care team at the Chelsea Health Center.

In January, ObjectiveHealth, a Nashvillebased integrated research and technology platform company, announced veteran clinical research executive Steve Clemons, MSN, FNP (Class 55), as its CEO. Clemons previously co-founded VitaLink Research and was COO of Rymedi, a health data management software company.

Ephraim McDowell Health in Danville, Kentucky, recently welcomed Jody Coomer, FNP-C (Class 110), APRN, to their medical staff. She specializes in treating conditions of the endocrine system.

Gifford Health Care in Vermont recently welcomed Lydia Corriveau, MSN, CNM (Class 202) to their gynecology, obstetrics, and midwifery team. Corriveau’s previous nursing experience includes labor and delivery, oncology, and critical care.

Katie Dahlstrom, PMHNP (Class 197), APRN, CNP, recently joined the Sanford Oakes Clinic in Sanford, North Dakota.
She specializes in mental health services, treating people of all ages experiencing conditions such as anxiety, attention deficit hyperactivity disorder, depression, mood and personality disorders, post-traumatic stress disorder, and schizophrenia.

Grace Dible, DNP (Class 50), CNM, presented her quality improvement project “Implementing Holistic Postpartum Care Utilizing the American College of Obstetricians and Gynecologists’ Postpartum Toolkit” at the American Association of Birth Centers Birth Institute in November. Dible is a Clinical Assistant Professor at Indiana University-Purdue University in Indianapolis, Indiana.

Natasha Freethy, CNM, DNP (Class 53), recently joined the Women’s Health Center in Honesdale, Pennsylvania. She facilitates births at Wayne Memorial Hospital’s New Beginnings Birthing Suites. Freethy’s scope of practice encompasses women’s reproductive health across the lifespan, including annual exams, birth control counseling, and postmenopausal care.

Kaitlyn Kerr, MSN, CNM (Class 164), recently joined Southcoast Health Obstetrics & Gynecology, working in their Fall River and New Bedford locations in Massachusetts.

Stephanie Lowe, DNP (Class 12), CNM, recently joined Ballad Health Medical Associates
OB/GYN in Marion, Virginia. Lowe offers a broad range of services and treatments, including breastfeeding, contraceptive management, hormone therapy, menopause care, menstrual disorders, natural family planning, pap smear testing, STI testing, and women’s preventive care.

Wound Solutions Group in New York, New York, recently appointed Dr. Lee Ann Lung, DNP (Class 20), APRN, FPN-C, WOCN, as Chief Medical Officer and Wound & Ostomy Nurse Practitioner and Educator.
“By embracing the latest medical advancements and techniques, we are not only transforming the way wound care is

delivered but are also driving better recovery outcomes and improving the overall quality of life for our patients,” Dr. Lung said.
Family Healthcare Network in Porterville, California, recently added Andrea Oseguera, MSN CNM (Class 202), to its OB/ GYN team. She previously worked as a labor and delivery nurse at other healthcare facilities, including Adventist Health

Bakersfield, Sierra View Medical Center, and Palmdale Regional Medical Center.

Daniela Paul, MSN, CNM (Class 58), recently joined Carilion Clinic in Roanoke, Virginia. As part of the nurse-midwifery team, she offers various services, including gynecologic and prenatal care, contraception options, and hospital-based births.
Brielle Jenson Stoyke, CNM, PMHNP-BC (Class 194) recently published Confessions of a Midwife. The autobiography details her work as a certified nurse-midwife (2000-2021) in various birth settings, including hospitals, home births, and a free-standing birth center. She currently works as a psychiatric-mental health nurse practitioner at Oak Ridge Center in Apple Valley, Minnesota.

Dr. Cordelia Nnedu,
Named Dean of the Tuskegee
University
School of Nursing and Allied Health

Dr. Cordelia Nnedu, Ph.D., CNM (Class 48), MSN was recently named announced as the new Dean of the Tuskegee University School of Nursing and Allied Health. Dr. Nnedu has been a faculty member at Tuskegee University for over three decades.
Dr. Nnedu is certified as a nurse-midwife by the American Midwifery Certification board (AMCB), as a nurse educator by the National League for nursing (NLN), and as a Women’s Health Care Nurse-Practitioner by National Certification Corporation (NCC). She was inducted into the Academy of Nursing Education Fellows (ANEF) in the fall of 2021, and she became a Fellow in the American Academy of Nursing (FAAN) in the fall of 2024. Dr. Nnedu’s research areas of interest include retention of minorities in baccalaureate nursing programs and the utilization of evidence-based strategies to address the impact of negative perinatal outcomes in minority women. team, she offers various services, including gynecologic and prenatal care, contraception options, and hospital-based birth
Frontier Nursing University is establishing an Alumni Mentoring Program, and we invite you to participate as a mentor or a mentee. This is a unique opportunity to make a meaningful impact on fellow alumni by sharing your expertise, insights, and career advice, should you choose to serve as a mentor. If you want to participate in the program as a mentee, we will connect you with an FNU graduate who has identified your chosen focus area(s) as subjects in which they are particularly accomplished. Additionally, we seek alumni to mentor our Student Interest Groups, including Men in Nursing, Student Veterans, Students of Color, Neurodiversity, Latin@ Students, and LGBTQA+ Students.
To help us shape this mentoring program, we’d love to hear from you! Please take a few minutes to complete our Alumni Mentoring Program Interest Survey. Your input will allow us to tailor the program to meet the needs of both mentors and mentees. For more information, please email Caitlin Rivard, Director of Alumni Engagement, at caitlin.rivard@frontier. edu
Take the Survey Here:



Check with an admissions counselor to see if you are eligible for the Companion DNP program.
Don’t miss your opportunity to save $6,000! Contact FNUadmissions@frontier.edu or visit frontier.edu/dnp
This is an important update regarding the frontier.edu email addresses for all Frontier Nursing University alumni.
After careful consideration and research, we’ve discovered that most alumni discontinue using their frontier.edu email addresses shortly after graduation. As FNU continues to grow, with more than 1,000 students graduating each year, maintaining these accounts has become increasingly costly and resource-intensive. Beginning on August 1, 2025, alumni will retain access to their frontier.edu email accounts for one year after graduation. We encourage you to update your information with us so we may contcinue to share news and resources.
To report a new email address, please contact us scan this QR code.
We know that change can be challenging, and we genuinely appreciate your understanding and patience. We are committed to serving all FNU alumni and believe this updated structure will help us do so more effectively.
If you have any questions or concerns, please reach out to alumni@frontier.edu. Thank you for your continued support and for being a valued part of the Frontier Nursing University community.



The Frontier Nursing University Office of Alumni Relations is here to support YOU! Our purpose is to offer helpful programs and services that support our graduates. Alumni are an integral part of FNU’s development because you demonstrate the excellence of FNU in everyday practice. You are also our primary recruiters and most loyal donors. We deeply appreciate your commitment to FNU.
The Alumni Association is open to all graduates of FNU. We currently have more than 8,000 alumni in all 50 states and many countries around the world. We encourage you to explore the services, programs, and activities offered and become involved. There are several ways to stay in touch with friends and connect to FNU, including conference receptions, case days, e-newsletters, and the FNU Alumni Facebook Group. Please ensure we have your most recent contact information to take advantage of all member services. Email us at alumniservices@frontier. edu.
Is your Frontier.edu email not working? Please contact support@frontier.edu to reset your password.
We are looking to spotlight FNU community members in our blog! Tell us your story by scanning the QR code and filling out the form or email stories@frontier.edu. Then, someone will contact you soon. These spotlight stories help us shine a light on all of the amazing accomplishments and the impact our community members have on their home communities and the University community.
FNU Faculty to Present at NCNA Nurse Practitioner Symposium


Dr. Torica Fuller DNP, MSN, FNP-BC, FNP-C, WHNP-BC, CDP, CGRN, CPN, NRCME

Dr. Wendy Smith DNP, MSN, APRN, FNP-BC
FNU faculty members Dr. Torica Fuller, DNP, MSN, FNP-BC, FNP-C, WHNPBC, CDP, CGRN, CPN, NRCME, and Dr. Wendy Smith, DNP, MSN, APRN, FNP-BC, are scheduled to present “Contraceptive Safety in Primary Care: US MEC Updates 2024” at the North Carolina Nurses Association Nurse Practitioner Symposium on April 15 in Wilmington, North Carolina.
Receives Barbara Lumpkin Award

FNU Associate Professor Dr. Vicky Stone Gale, DNP, APRN, FNP-BC, FAANP, FNAP, received the Barbara Lumpkin Award at the Florida Nurses Association (FNA) 2024 FNA Icon Awards Celebration, held on November 21. The event celebrated the remarkable achievements of nurses who exemplify leadership, innovation, advocacy, and dedication to the profession and their communities.
The Office of Diversity, Equity, and Inclusion (DEI) provides strategic leadership, advocacy, and education efforts to address DEI throughout the university community. This award is offered in collaboration with the Diversity, Equity, Inclusion, and Belonging Committee. This award celebrates staff who go above and beyond in their efforts to foster an inclusive and equitable academic environment, recognizing their vital role in shaping a diverse and inclusive university community.

Megan Arbour PhD, CNM, CNE, FACNM Faculty Knowledge and Attitudes of Neurodiversity in Nursing Education: A Multi-Site Survey, NONPF April 9-13, 2025, Denver, Colorado.

Kristin Gianelis MSN, DNP Jefferson, K. & Gianelis, K. (2025, January 17). Utilizing Cohort-Style Learning with DNP Students to Build a Culture of Belonging. AACN Doctoral Education Conference, Coronado, California.

Sharanna Johnson DNP, MSN-Ed, APRN, FNP-BC, CN Jefferson, K. & Johnson, S. (2025, April 11). Promoting and Prioritizing Person-Centered Mental Health and Well-Being for Future Doctoral Leaders. NONPF 51st Annual Conference: Re-envisioning NP Education to Lead the Future, Denver, CO, United States.

Sybilla Myers DNP, FNP Myers, S. (2025, April 9-13). Adapting Standardized Tools to Driver Quality Improvements with Checklists in Diverse Settings. NONPF 51st Annual Conference. Denver, Colorado.

Audrey Perry DNP, M.Ed.(c), CNM, APRN, A-GNP-C, CNE, FACNM Tenney, E., Perry, A., Belcheff, T. & Delpech, P. (2024). Reimagining Nursing Education: Embedding Cultural Safety in a Graduate Curriculum. Podium. AACN Transform Conference.

Penny Wortman CNM, DNP Andrighetti, T. & Wortman, P. (January 2025). Having trouble making your birth realistic? Come hear from two midwife simulationists on ways to enhance fidelity. International Meeting on Simulation in Healthcare. Orlando, Florida.

Khara’ Jefferson DNP, APRN, FNP-C, CHC
Gianelis, K. & Jefferson, K. (2025, April 11). Building a Culture of Belonging in Graduate Nursing Education through Cohort-Style Learning. NONPF 51st Annual Conference: Re-envisioning NP Education to Lead the Future, Denver, Colorado, United States.
Dr. Diana Jolles and Dr. Jennifer Stapleton Help Author Study on Home Birth Outcomes


Dr. Diana Jolles PhD, CNM, FACNM
“The paper is a result of many years of collaboration and cumulative effort by community birth midwives across the United States,” Dr. Jolles said. “Many Frontier Alumni, preceptors, and students have been involved in entering data into the American Association of Birth Centers Perinatal Data Registry or the Midwives Alliance of North America Statistical Platform ‘MANA Stats’. Following in the footsteps of the Frontier Nursing Service, this paper is a demonstration of how important it is for advanced practice providers to continue to collect and analyze practice statistics to support midwiferyled, community-based, population health models of care.”
Behdokht Rouhi and Catherine Collins-Fulea Author Published Study

Dr. Jennifer Stapleton DNP (Class 1)
FNU faculty Dr. Diana Jolles, PhD, CNM, FACNM, and FNU graduate Dr. Jennifer Stapleton, DNP (Class 1), participated in a national study led by Oregon State University. The report, titled Planned Home Births in the United States Have Outcomes Comparable to Planned Birth Center Births for LowRisk Birthing Individuals, was published in Medical Care. The study found that in low-risk pregnancies, mothers and children are just as safe with a planned home birth as they are with a planned birth center birth.

Dr. Catherine Collins-Fulea DNP, CNM, FACNM, FAAN
Dr. Behdokht Rouhi DNP, ANP-BC (Class 43)
A study by FNU DNP graduate Dr. Behdokht Rouhi (Class 43) and FNU faculty Dr. Catherine Collins-Fulea, DNP, CNM, FACNM, FAAN, was published in the Journal of Hospice & Palliative Nursing in December.
Improving Patient-Centered Care for EndStage Renal Disease Patients at a Community Palliative Setting, Rouhi, Behdokht DNP (Class 43) ANP-C, ACHPN; Collins-Fulea, Catherine DNP, CNM, FACNM, FAAN.
We know you want to stay informed about all that is happening at FNU. To make sure you don’t miss communications such as the Quarterly Bulletin or our monthly e-newsletters, please take a moment to make sure we have your updated contact information. Please send your updated contact information, including your preferred email address, phone number, and mailing address, to alumniservices@frontier.edu. Thank you!


CHAIR
Mrs. Tia Andrew, Hamilton Parish, Bermuda
Ms. Sarah Bacon, Brooklyn, NY
Mrs. Andrea Begley, Hyden, KY
Dr. Heather Bernard, Hamilton, NY
Gov. Steven Beshear, Lexington, KY
Mrs. Betty Brown, Louisville, KY
Mrs. Amy Pennington Brudnicki, Richmond, KY
Dr. Timothy Bukowski, Chapel Hill, NC
Dr. Wallace Campbell, Berea, KY
Miss Anna Carey, Hyden, KY
Mrs. Jean Chapin, Oldwick, NJ
Mrs. Lois Cheston, Topsfield, MA
Bill Corley, Indianapolis, IN
Mrs. Julia Breckinridge Davis, Winston-Salem, NC
Mrs. Selby Ehrlich, Bedford, NY
Mrs. Robert Estill, Raleigh, NC
Mrs. Noel Smith Fernandez, Pomona, NY
Ms. Mary Ann Gill, Versailles, KY
Mr. John Grandin, Chestnut Hill, MA
Dr. Joyce Fortney Hamberg, Southgate, KY
Dr. Horace Henriques, Lyme, NH
Mr. & Mrs. John Hodge, Berwyn, PA
Mrs. Robin Frentz Isaacs, Lincoln, MA
Mrs. Rosemary Johnson, Versailles, KY
Mrs. Mary Carol Joseph, Hyden, KY
Ms. Deborah M. King, Westport, MA
Mrs. Patricia Lawrence, Westwood, MA
Mrs. Marian Leibold, Cincinnati, OH
Dr. Ruth Lubic, Washington, DC
Mr. Robert Montague, JD, Urbanna, VA
Dr. Judy Myers, Ph.D., RN, New Albany, IN
Ms. Barbara Napier, Irvine, KY
Ms. Sandra Napier, Stinnett, KY
Mr. Dean Osborne, Hyden, KY
Mrs. Helen Rentch, Midway, KY
Mrs. John Richardson, Washington, DC
Mrs. Linda Roach, Lexington, KY
Mrs. Georgia Rodes, Lexington, KY
Mrs. Sandra Schreiber, Louisville, KY
Maria Small, MD, MPH, Durham, NC
Mrs. Sherrie Rice Smith, Franklin, WI
Mrs. Austin Smithers, Lyme, NH
Mrs. Robert Steck, Arlington, MA
Mrs. Mary Clay Stites, Louisville, KY
Mr. Richard Sturgill, Paris, KY
Ms. Mary Frazier Vaughan, Lexington, KY
Mrs. LouAnne Roberts Verrier, Austin, TX
Dr. Patience White, Bethesda, MD
Ms. Vaughda Wooten, Hyden, KY
Michael Carter, DNSc, DNP, New Orleans, LA
VICE CHAIR
Michael T. Rust, MPH, Louisville, KY
SECRETARY
Nancy Hines, Shepherdsville, KY
TREASURER
Emma Metcalf, RN, MSN, CPHQ, Louisville, KY
Board Members
Elaine Bolle, BA, MBA, Chapel Hill, NC
William (Bill) Corley, MHA, Carmel, IN
Vernell DeWitty, Ph.D., MBA, RN, FAAN, Silver Spring, MD
Jean Johnson, Ph.D., RN, FAAN, Cabin John, MD
Marcus Osborne, MBA, Bentonville, AR
Tim Raderstorf, DNP, RN, FAAN, Columbus, OH
Kerri Schuiling, PhD, CNM, FACNM, FAAN, Marquette, MI
Peter Schwartz, MD, Port St. Lucie, FL
Maria Small, MD, MPH, Durham, NC
Michael Steinmetz, CPA, CMA, CSCA, Bellevue, WA
May Wykle, Ph.D., RN, FAAN, FGSA, Cleveland, OH
Student Representatives
Bridget Ehrhart-Bennett (DNP Class 53), South Webster, OH
Kathleen "Kate" Corbett (FNP Class 209), Victoria, British Columbia
Foundation Board Members
Peter Coffin, Chair, BA, Chestnut Hill, MA
Derek Bonifer, MBA, BA, Louisville, KY
Constance Brotherton, MA, BA, Lexington, KY
Brooke A. Flinders, DNP, RN, APRN-CNM, FACNM, Lexington, KY
Peter Schwartz, MD, Port St. Lucie, FL
President Emerita
Dr. Susan Stone, CNM, DNSc, FAAN, FACNM Distinguished Chair of Midwifery and Nursing
Board Members Emeritus
Wallace Campbell, Ph.D., Berea, KY
John Foley, BBA, Lexington, KY
Marion McCartney, CNM, FACNM, Washington, DC
Nancy Fugate Woods, Ph.D., RN, FAAN, Seattle, WA
(Thru 2/17/25)
The following people contributed to Frontier in memory of their friends or loved ones. The names in bold are the deceased.
In honor of the nurses who died from COVID at the beginning of the pandemic
Julie Richards
Dr. Lisa Chappell
Sally Weiss
Christian Graham
MOlufunmilola Ademola
Shelley Aldridge
Paula Alexander-Delpech
Shawn Allison
Taisha Bates
Michelle Beck
Dana Brewer
DeAnna Brown
Te’sia Carter
Audra Cave
Jennifer Cooley
Kiersten Crabtree
Kellen Cross
Dilcia Diaz
Jodi Dickey
Torshea Epps
Celine Ferland
Heather Figi
Brooke Flinders
Eva Fried
Torica Fuller
Kathy Gardner
Tauscha Gerald
Ashley Gher
Mary Gillmore-Kahn
Arissa Grizzle
Pamela Hamilton
Donna Harmon
Jennifer Howard
Sarah Juett
Wes Justice
Juanita Kahler
Jim Kelsey
Jenkins Lawhorn
Heidi Loomis
Florence Nakimera
Aimee Niles
Helen Omorogbe
Nancy Pesta Walsh
Erica Schroeder
Sharon Tankersley
Eileen Thrower
Kristine Twite Lehnen
Lisa Uncles
Kimberley Williams
Terrance Michael Johnson
Angela Allen
Diana Morgan Olcott
Leslie Olcott
Marguerite Pike
Susan Marie Peeples
Ernestine Rose
Wilson Uncles
Lisa Betina Uncles
Dr. Jan Weingrad
Deborah Weingrad

This and past issues of the Quarterly Bulletin are available to view and download for free at ISSUU.com/ frontiernursinguniversity.